Abstract
Introduction
Trauma training for front-line providers is a critical component of injury mitigation and trauma systems strengthening. Although the Advanced Trauma Life Support (ATLS) course is standard in much of the world, cost and administrative barriers are prohibitive to deploying the course in many low and middle income countries (LMICs). The purpose of this study was to identify alternative trauma training courses used in LMICs by scoping review and compare their effectiveness.
Methods
Several peer-reviewed and grey literature databases were searched for relevant articles describing trauma training courses for front-line medical providers in LMICs. Studies were included if: performed in a LMIC; utilized a general trauma training course other than ATLS; trainees were hospital-based medical providers; study included some type of outcome measure.
Results
A total of 34 manuscripts met inclusion criteria. The majority of courses were novel, hospital-initiated courses and ranged in length from 1 day to 1 week. Physicians were the most common target audience, followed by medical students and nurses. Courses were taught in 24 different countries throughout the Middle East, Asia, Latin America and Africa. Comparison of pre- and post-test knowledge was the most common metric used and nearly all courses demonstrated a statistically significant knowledge gain. One study demonstrated a reduction in mortality for injured patients after course implementation. The majority of courses were a collaboration between universities in a high income country and local faculty/practitioners in the LMIC where the course was taught. Reported cost per participant ranged from $10 to $232 USD.
Conclusions
Several trauma courses are currently being utilized in LMICs effectively with increases in knowledge gained and at a lower reported cost than ATLS. More research is needed to link trauma training courses to patient outcomes.
Keywords: Trauma training, Low- and middle- income countries, Injury, Emergency medicine, Trauma care
African relevance
-
•
Training providers in trauma care is important for strengthening trauma systems, but ATLS can be cost-prohibitive in LMICs.
-
•
We conducted a scoping review to identify non-ATLS trauma courses in LMICs and compare these in cost and effectiveness.
-
•
Several trauma courses are being utilized in LMICs with success in knowledge uptake and at a lower estimated cost than ATLS.
Background
Injury is a major cause of morbidity and mortality worldwide resulting in 4.9 million annual deaths globally [1]. Low and middle income countries (LMICs) are disproportionately affected by injury with more than 90% of injury deaths occurring in these countries [2]. Equipping front-line hospital staff with a systematic approach to the evaluation and treatment of trauma patients is crucial to improve care of the injured in a timely manner. While this type of training has become standard for emergency medicine and surgery personnel in high-income countries (HICs), most providers in LMICs have limited access to trauma training courses.
The American College of Surgeons (ACS) has long advertised their Advanced Trauma Life Support (ATLS) course as an international standard in trauma care. While the idea of a single common international standard is appealing, there are significant barriers to deploying ATLS in LMICs including significant cost to the host country and lack of approved personnel 3., 4.. One study from Mongolia reported an annual budget of $10,709 USD to run a minimum cost ATLS program using locally trained instructors, but this did not include the $84,875 USD required to initially train the Mongolian instructors [4].
New international ATLS programs must be requested by a recognized surgical association in the requesting country and ATLS site directors are required to be surgeons [5]. Although engaged surgeons are vital for successfully implementing any trauma training or trauma improvement initiatives, the drivers of trauma improvement are frequently other non-surgical front-line providers. This is increasingly true as emergency medicine develops as a specialty in many LMICs and efforts to improve trauma resuscitation in those areas are frequently led by emergency physicians. For many countries the creation of a recognized surgical society represents an extra layer of burden when most major healthcare initiatives are typically undertaken through the Ministry of Health or local hospitals themselves.
In addition, ATLS is designed for high resource settings where advanced imaging such as CT scanners and bedside ultrasound machines are commonly available and may limit relevance in the resource-constrained context which is common in LMICs. ATLS also limits attendees to physicians and advanced practice providers (nurse practitioners and physician assistants) which is problematic in the resource-limited setting where task shifting is common and many (or all) front-line providers of the injured are non-physicians [6].
The purpose of this study was to identify alternative trauma training courses used in LMICs and determine what evidence is available to support the effectiveness of these courses. This review also sought to evaluate the reported cost associated with these courses. Given the limited knowledge in this area and broad research question, a scoping review was chosen as the most appropriate methodology.
Methods
PubMed, Web of Science, Google Scholar, and African Journals Online databases were used to identify relevant peer-reviewed research articles describing trauma training courses for medical providers in LMICs. In addition a grey literature search was undertaken using OpenDOAR and Bielefeld Academic Search Engine (BASE). Studies were included if: performed in a LMIC; utilized a general trauma training course other than ATLS; trainees were hospital-based medical providers including but not limited to nurses, physicians, residents, medical students, and clinical officers; study included some type of outcome measure such as knowledge or confidence gained or change in care provided to trauma patients. Studies were excluded if the course described took place in a high-income country; training course used was ATLS; trainees were prehospital providers, community health workers or laypersons; the course focused primarily on a narrow portion of trauma care such as trauma in obstetrics, orthopedics or burn care; trauma training was a small part of a larger curriculum such as an emergency medicine residency or broader course; gave no details of training methods or details of the structure of the education; or if a subjective course evaluation or nontechnical skill evaluation (such as teamwork) was the only measurement tool used.
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) checklist was used and the protocol was registered with Open Science Framework (OSF) 7., 8.. Two independent reviewers performed searches of all databases using the search terms provided in Appendix A. Titles and abstracts were reviewed by each reviewer and articles that appeared to meet inclusion criteria were obtained and full text articles were reviewed. Disagreements between reviewers were resolved through consensus. Exclusion criteria were applied in both abstract and full manuscript review. The following data were extracted from studies meeting inclusion criteria: description of course; location of training; number and cadres of medical professionals trained; cost or funding; any relevant outcome measures. The outcome measures for each included study were evaluated using the Kirkpatrick Model, a widely accepted framework for evaluating training outcomes [9]. The Kirkpatrick Model as adapted to trauma training courses is presented in Table 1.
Table 1.
Kirkpatrick model for training evaluation [9].
| Kirkpatrick level | Description | Outcome measures in trauma courses |
|---|---|---|
| Level 1 - reaction | Degree to which participants find training favorable and relevant to their job | Subjective course evaluations |
| Level 2 - learning | Degree to which participants acquire intended knowledge, skills, confidence and commitment | Objective pre- and post-tests Confidence measurements |
| Level 3 - behavior | Degree to which participants apply what they learned while on the job | Objective assessment of skills such as OSCE, simulation cases or evaluation of real-time trauma cases |
| Level 4 - results | Degree to which targeted outcomes occur as a result of training | Changes in trauma morbidity or mortality, objective trauma system improvements |
Results
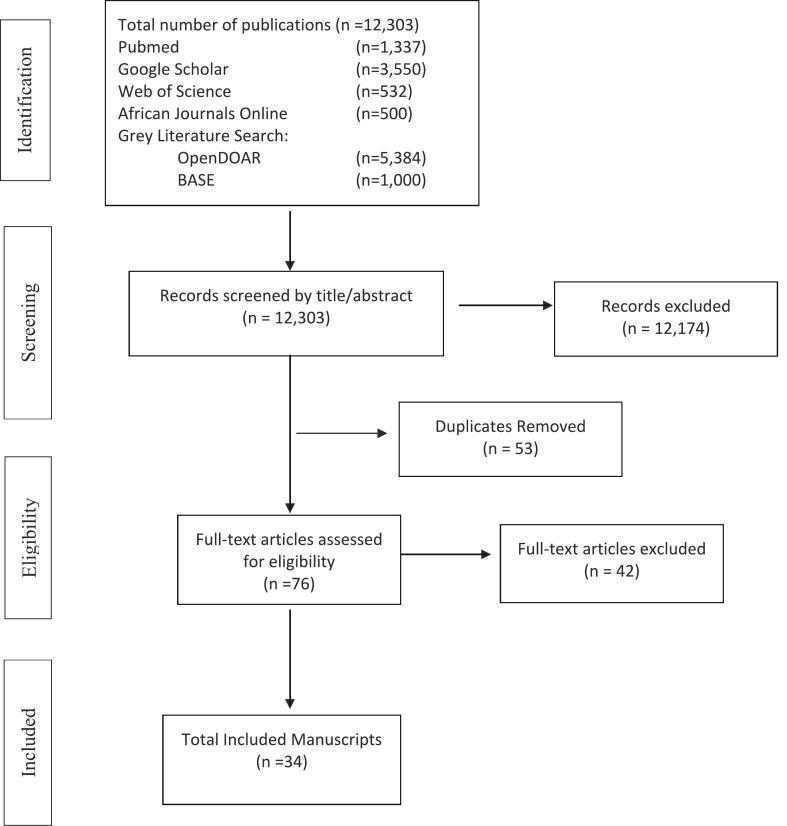
Searches in all six databases identified a total of 12,303 articles (Fig. 1). After screening titles and abstracts, 12,174 articles were eliminated leaving 129 full-text articles. Fifty-three of these were duplicates identified in more than one database search. After removing duplicates, 76 full-text articles were reviewed in detail. Forty-two of these articles did not meet inclusion criteria and were eliminated, leaving 34 articles meeting all inclusion criteria (Fig. 1).
Fig. 1.
Study inclusion flowchart.
The 34 studies meeting criteria provided trauma training in 24 different countries throughout the Middle East, Asia, Latin America and Africa (Table 1) 10., 11., 12., 13., 14., 15., 16., 17., 18., 19., 20., 21., 22., 23., 24., 25., 26., 27., 28., 29., 30., 31., 32., 33., 34., 35., 36., 37., 38., 39., 40., 41., 42., 43.. Twelve of the 34 studies reported on novel or pilot trauma courses developed by local or international faculty specifically for the local context 32., 33., 34., 35., 36., 37., 38., 39., 40., 41., 42., 43.. The Primary Trauma Care (PTC) course was the most common replicated course with 9 manuscripts reporting on this 2 day course 10., 11., 12., 13., 14., 15., 16., 17., 18.. The PTC is an open-access course published by the World Health Organization and freely available in 14 different languages 15., 44..
The ACS Trauma Evaluation and Management (TEAM) course was the next most commonly described course with 5 studies describing this course 19., 20., 21., 22., 23.. The remaining 8 studies utilized one of the following courses: Trauma Team Training Course (2 studies), Rural Trauma Team Development Course (2 studies), Acute Trauma Care, Better and Systematic Team Training (BEST) Course, Emergency Room Trauma Course, and Kampala Advanced Trauma Course.
Length of courses ranged from 1 day to 1 week with the majority of courses falling in the two to three day range. Novel courses tended to be longer with 3 of the 12 novel courses lasting 5 days or 40 h 37., 39., 43.. Most courses included a combination of didactic sessions with hands-on practical experience. Mannequin simulation and live actor moulage were the most commonly described methods for practicals. Live animal labs were used in two studies for a variety of procedures 43., 40.. Some studies described using goat cadavers to practice chest tube insertion, interosseous needle insertion, and central venous cannulation 17., 31., 36., 37.. Uma et al. used chicken bones to practice interosseous needle insertion [12]. Pringle et al. described converting a basic low-cost mannequin into a chest-tube insertion simulator by placing pork-ribs and a saline bag into the mannequin's chest cavity [39]. Only two manuscripts did not mention any practical or hands-on skill sessions 23., 27.. Several studies mentioned table-top group scenario discussions as a course component, but these were less frequently used than simulation. The majority of courses described an “ABC” approach and utilized some version of a primary and secondary survey, similar to ATLS.
Physicians were the most common target audience followed by medical students and nurses. Eleven of the courses were delivered to physicians only 17., 18., 30., 31., 34., 36., 39., 40., 41., 42., 43.. Another 8 courses had an audience composed exclusively of medical students (including all five of the TEAM courses) and the remaining courses were learners from multiple cadres 12., 13., 19., 20., 21., 22., 23., 38..
While most studies evaluated courses at a single site, four articles described a course taught in more than one African country 14., 15., 16., 26.. Three of these four manuscripts evaluated PTC courses taught in the 10 member countries of the College of Surgeons of East, Central and Southern Africa (COSECSA) 14., 15., 16.. COSECSA organized and delivered the courses in conjunction with the University of Oxford through the COSECSA-Oxford-Orthopedic Link (COOL) programme. COOL was funded by the UK Department or International Development and the Tropical Health Education Trust. This course was done in a 2:1:2 cascading manner, meaning that there was an initial 2 day provider course, followed by a 1 day instructor course, followed by a 2 day provider course taught by the instructors trained the day before. Although COSECSA organized the courses, international faculty from HICs were used to teach the initial 2 day provider course.
In addition to COSECSA's involvement in delivering the PTC course, the organization also partnered with Emory to provide the Acute Trauma Care course in Kenya and Zambia [26]. The only other manuscripts which mentioned a national or international surgical society's involvement in organizing or deploying a training course was the Panamerican Trauma Society teaching the “Basic Trauma Course” in Ecuador [34]. Hanche-Olsen et al. described a nation-wide initiative in Botswana called “Better and Systematic Team Training” (BEST) course for 977 participants throughout Botswana's government hospitals. This is one of the few studies that also described a larger effort to create more advanced trauma systems by encouraging each hospital to create a local trauma committee, develop a trauma registry and create a defined trauma team with alarm criteria [29].
Comparison of pre- and post-test knowledge was by far the most common metric used to evaluate the courses with only four of the thirty-four articles not reporting this data 14., 29., 31., 40.. Despite the differences in course length and content, all of these courses demonstrated a statistically significant knowledge gain among its participants. Nine of the studies evaluated knowledge retention by administering a second post-test months after the original training 11., 14., 18., 20., 24., 33., 34., 37., 38.. Retention testing ranged from 2 months to 2 years after the training. In four of the seven studies that evaluated knowledge retention, scores dropped below the post-course test but remained higher than the pre-test. In two studies, average scores on the retention test were higher than immediate post-course scores. Figueroa et al. was the only study that showed a drop in retention scores to below pre-test scores [34]. Tolppa et al. followed three separate training groups out to 12 months post-course (Group A), 16 months post-course (Group B) and 24 months post-course (Group C) and found that retention test scores were higher than pre-test scores among all three groups (p < 0.001) but when compared to immediate post-test scores the results were not statistically significant [11]. Retention was also tested using Objective Structured Clinical Examination (OSCE) style evaluation of skills in two of the studies, both showing reduction in scores over time 24., 38..
Most articles used simple confidence and knowledge gained measurements (Kirkpatrick level 2) and did not attempt to evaluate any change in practice patterns or patient mortality after course implementation. Seven studies used an OSCE style evaluation of skills obtained during the trauma course (Kirkpatrick level 3) 17., 24., 25., 30., 38., 39., 41.. Four of these studies included both a pre- and post-course OSCE with statistically significant improvement on the post-course OSCE 17., 30., 38., 39..
Three studies attempted some measurement of hospital system improvement or mortality benefit from the training (Kirkpatrick level 4) 14., 29., 40.. Noordin et al. compared in-hospital mortality and ICU length of stay for trauma activation patients at a tertiary care center in Pakistan before initiation of a two day trauma course (Group A) and after initiation of a two-day trauma course (Group B). Group B had lower mortality rates than Group A, but longer ICU stays (Table 2). The longer ICU length of stay was explained by a higher percentage of transferred patients with higher Injury Severity Scores in Group B compared to Group A [40]. Ologunde et al. used an electronic survey administered immediately after and six months after PTC course completion through the COOL initiative to evaluate hospital and departmental changes to the care of trauma patients. The study showed subjective improvement in management of trauma patients, as well as a majority of respondents reporting some departmental or institutional changes in trauma management at six months [14]. Hanche-Olsen et al. developed a checklist and questionnaire adapted from the World Health Organization's (WHO) “Guidelines for Essential Trauma Care” which included an assessment of 64 pieces of equipment and 59 trauma-related skills 29., 45.. The checklist and questionnaire was administered at each hospital prior to training and 2 years after training. The authors found that 55% of hospitals had instituted a local trauma committee, 14.8% had developed a trauma registry and 19% of hospitals had developed a defined trauma team with alarm criteria. Over the two year period, trauma room equipment to manage airway and breathing had improved, however there was no change in availability of circulatory equipment or availability of laparotomy for trauma patients [29].
Table 2.
Summary of included studies.
| First author | Course location | Course audience | Course assessment | Results | Kirkpatrick level of evaluation |
|---|---|---|---|---|---|
| Primary trauma care courses | |||||
| Muzzammil M, 2021 [10] | Pakistan | Physicians (n = 3770) Medical students (n = 2200) Postgrad trainees (n = 782) Paramedics (n = 1100) |
30 MCQ pre- and post-test Confidence matrix |
Mean MCQ score increased from 60% to 82% Confidence score increased from 70% to 93% (p values not reported) |
2 |
| Tolppa T, 2020 [11] | Democratic Republic of Congo | Physicians (n = 36) Nurses (n = 23) |
20 MCQ pre- and post-test 8 Item confidence matrix (CM) Post-test and CM repeated at 12 months (Group A, n = 13); 16 months (Group B, n = 9); 24 months (Group C, n = 29) |
Mean MCQ score increased from 43.8% to 70.5% (p < 0.001) Confidence score increased from 57% to 81% (p < 0.001) Retention testing: Group A: MCQ = 71%, CM = 75% Group B: MCQ = 70%, CM = 87.5% Group C: MCQ = 65.5%, CM = 67% |
2 |
| Uma K, 2020 [12] | India | Senior medical students (n = 327) | 20 MCQ pre- and post-test | Mean MCQ score increased from 30% to 56% (p < 0.001) | 2 |
| Sadiq MA, 2018 [13] | Pakistan (Foundation University Medical School, Islamabad) |
Senior medical students (n = 77) | 30 MCQ pre-and post-test | Mean MCQ score increase from 53.3% to 70% (p < 0.000) | 2 |
| Ologunde R, 2017 [14] | COSECSA Countries (Burundi, Ethiopia, Kenya, Malawi, Mozambique, Rwanda, Tanzania, Uganda, Zambia, Zimbabwe) | Physicians (n = 253) Nurses (n = 98) Clinical officers (n = 40) Medical students (n = 44) |
Post-course trauma systems survey (immediately post-course and 6 months) | 6 months post-course 92.7% of participants reported improvement in trauma management; 26% reported an increase in staffing for trauma; 29% reported improvement in equipment to care for trauma patients; 24.8% reported perceived change in mortality rates for trauma patients | 4 |
| Peter NA, 2016 [15] | COSECA Countries | Physicians (n = 450), Nurses (n = 260), Clinical Officers (n = 119), Medical Students (n = 111) | 30 MCQ pre- and post-test 8 Item confidence matrix |
Mean MCQ score increased from 58% to 77% (p < 0.05) Confidence increased 68% to 90% (p < 0.05) |
2 |
| Nogaro MC, 2015 [16] | COSECSA Countries | Physicians (n = 240) Non-physicians (105) |
30 MCQ pre- and post-test 8 Item confidence matrix |
Mean MCQ score increased from 70% to 87% (p < 0.05) Confidence increased 73% to 95% (p < 0.05) |
2 |
| Jawaid M, 2013 [17] | Pakistan | Physicians (n = 21) | 30 MCQ pre- and post-test 20 point OSCE |
Median MCQ score increased from 65% to 83.3% (p < 0.0001) Median OSCE Scenario score increased from 17.5% to 47.5% (p < 0.0001) |
2 and 3 |
| Amiri H, 2013 [18] | Iran | Physicians (n = 64) | 30 MCQ pre- and post-test, retention post-test randomly administered between 6 and 12 months | Median MCQ score increased from 62.8% to 89% (p < 0.001) and for delayed post-test to 73.9% (p < 0.001) | 2 |
| Trauma Evaluation and Management (TEAM) courses | |||||
| Soomro R, 2020 [19] | Pakistan | Senior medical students (n = 294) | 20 MCQ test given afterward teaching (Group A, n = 105), ward teaching plus TEAM book and video (Group B, n = 92), ward teaching plus full TEAM course (Group C, n = 97) | Mean MCQ score was 30% in Group A, 40% in Group B, and 45% in Group C (p = 0.000) | 2 |
| Berndtson AE, 2019 [20] | Ghana | Senior medical students (n = 62) | 18 MCQ pre- and post-test, 6 month retention post-test | Mean MCQ score increased from 44.2% to 69.1% (p < 0.001) and for 6 month post-test to 81.6% (p < 0.01) | 2 |
| Hill KA, 2018 [21] | Kenya | Senior medical students (n = 61) | 20 MCQ pre- and post-test | Mean MCQ score increased from 57% to 72% (p < 0.001) | 2 |
| Delgado-Reyes L, 2016 [22] | Mexico | Pre-Clinical medical students (n = 71) Clinical cycle medical students (n = 44) |
20 MCQ pre- and post-test | Mean MCQ score increased by 24.4% (p < 0.01) for pre-clinical group Mean MCQ score increased by 22.5% (p > 0.05) for clinical group |
2 |
| Ali J, 2003 [23] | Jamaica | Senior medical students (n = 32) compared with control group of senior medical students | 20 MCQ pre-and post-test | TEAM group increased mean score from 53.1% to 69.4% TEAM group post-test scores (69.4%) higher than No Team post-test (52.2%) (p < 0.0001) |
2 |
| Trauma Team Training (TTT) courses | |||||
| Pemberton J, 2013 [24] | Guyana | Physicians (n = 20) Nurses (n = 17) Paramedical (n = 10) |
15 MCQ pre- and post-test, 4 month retention post-test OSCE graded group simulation post-course and at 4 months |
Mean MCQ score increased from 72.6% to 84.6% (p < 0.0001) and for 4 month post-test to 80% (p < 0.0001) Mean OSCE score dropped from 76% to 63.8% (p < 0.0001) at 4 months post-course |
2 and 3 |
| Bergman S, 2008 [25] | Tanzania | Physicians (n = 7) Nurses (n = 13) |
15 MCQ pre- and post-test OSCE graded group simulation |
Mean MCQ score increased from 60% to 86.6% (p = 0.0004) Teams scored range of 84% to 96% on group simulation |
2 and 3 |
| Acute Trauma Care (ATC)-Fundamental Critical Care Support (FCCS) combined courses | |||||
| MacLeod JBA, 2010 [26] | Zambia Kenya |
Medical officers (n = 27) COSECA trainees (surgeons) (n = 21) Clinical officers (n = 13) Nurses (n = 14) |
20 MCQ pre-test 30 MCQ post-test 37 Item confidence matrix |
Mean MCQ score increased by 12.3% (p < 0.0001) Confidence increased from 78% to 94% (p < 0.0001) for trauma scenarios and from 66% to 86% (P < 0.0001) for procedures |
2 |
| Rural Trauma Team Development Course (RTTDC) | |||||
| Ali J, 2015 [27] | India | Total (n = 43); Participant cadres undifferentiated | 20 MCQ pre- and post-test | Mean MCQ score increased from 32% pre-test to 66% post-test (p < 0.0001) | 2 |
| Ali J, 2014 [28] | Pakistan | Physicians (n = 10) Nurses (n = 2) |
20 MCQ pre- and post-test | Mean MCQ score increased from 65% pre-test to 70% post-test (p < 0.05) | 2 |
| Better and Systematic Team Training (BEST) Courses | |||||
| Hanche-Olsen TP, 2015 [29] | Botswana | Total (n = 977); Participant cadre numbers undifferentiated but included general surgeons, medical officers, nurses, xray techs, lab techs, physiotherapists | Prospective systems analysis adapted from WHO “Guidelines for Essential Trauma Care” performed at all 27 government hospitals in Botswana before course and 2 year follow-up 64 Item equipment checklist 59 Item trauma skills checklist |
55% of hospitals instituted a local trauma committee 14.8% of hospitals developed a trauma registry Equipment and skills for assisting airway and breathing increased in most hospitals, particularly for pediatric population Availability of diagnostic imaging did not improve |
4 |
| Emergency room trauma courses | |||||
| Shrestha, 2018 [30] | Nepal | Physicians (n = 97) (new interns) |
25 MCQ pre- and post-test 25 Item OSCE |
Mean MCQ score increased from 64.2% pre-test to 89.8% post-test (p = 0.000) Mean OSCE score increased from 33.2% pre-test to 78.6% post-test (p = 0.000) |
2 and 3 |
| Kampala Advanced Trauma Courses (KATC) | |||||
| Ullrich SJ, 2020 [31] | Uganda | Physicians (n = 106) | Confidence matrix assessed through post-course survey administered average 1 year after course completion | 80% of participants were confident performing all skills with the exception of venous cutdown | 2 |
| Novel/pilot courses | |||||
| Babu BV, 2021 [32] | India “AIIMS Trauma Assessment and Management” (ATAM) |
Physicians (n = 315) Nurses (n = 345) Medical students (n = 33) Paramedical/Allied Health (n = 50) |
30 MCQ pre- and post-test Self-rated knowledge, skill, confidence, and capability pre- and post-training on 10 point scale |
Mean MCQ increased from 51.6% to 75% (p < 0.0001) Mean self-rated scores: Knowledge 45% to 75%; Skill 44% to 76%; Confidence 46% to 78%; Capability 47% to 78% (p < 0.0001) |
2 |
| Taylor S, 2021 [33] | Dominican Republic | Resident physicians (n = 29) Medical students (n = 36) |
40 MCQ pre- and post-test and 2 month retention | Mean MCQ increased from 37.2% pre-test to 63.5% post-test and 52.2% at 2 months (p < 0.0001) | 2 |
| Figueroa JF, 2020 [34] | Ecuador “Basic Trauma Course” |
Resident physicians (n = 39) | 30 MCQ pre- and post-test and 1 year retention | Mean MCQ increased from 23.9% to 25.5% post-test (p < 0.01) and 23.8% at 1 year | 2 |
| Tang H, 2020 [35] | China “China Trauma Care Training” |
Physicians (n = 854) Nurses (n = 357) |
20 MCQ pre- and post-test | Mean MCQ increased from 71% to 84.2% (p < 0.001) | 2 |
| Anderson GA, 2018 [36] | Uganda “Emergency Ward Management of Trauma” |
Physicians (n = 15) | 20 MCQ pre- and post-test | Mean MCQ scores improved from 67.5% pre-test to 86.3% post-test (p < 0.001) | 2 |
| Oussi N, 2018 [37] | Malawi | Physicians (n = 13) Nurses (n = 2) |
33 MCQ pre- and post-test and 6 month post-test 5 Question confidence matrix |
Mean MCQ scores improved from 69% to 81.5% post-test(p = 0.001) and 77.8% (p = 0.003) 6 months post- test Confidence score increased 12% |
2 |
| Wanjiku G, 2017 [38] | Kenya | Medical students (n = 22) | 23 MCQ pre- and post-test and 9 month retention 36 Question confidence matrix OSCE scored with 116 point check list |
Mean MCQ scores improved from 62% to 73% post-test (p < 0.0001) to 75% at 9 months OSCE scores improved from 32.6% to 70% post-course and to 61.7% at 9 months Confidence score increased from 60% to 94% post-course and to 91.8% at 9 months |
2 and 3 |
| Pringle K, 2015 [39] | Nicaragua | Physicians (n = 33) | 26 MCQ pre- and post-test OSCE scored with 100 point check list |
Mean MCQ scores improved from 58% pre-test to 75% post-test (p < 0.001) Mean Simulation scores improved from 39% to 68% (p < 0.01) |
2 and 3 |
| Noordin S, 2011 [40] | Pakistan | Physicians (all residents and faculty from multiple specialties, number not given) | Quasi-experimental cohort study: Compared in-hospital mortality, hospital and ICU length of stay for patients prior to course implementation (Group A) and after course (Group B) | Group B (n = 574) had lower mortality rate (5.7%) compared to Group A (n = 435) (9.7%, p = 0.019) ICU stay was longer for Group B 2.3 days compared to Group A 1.7 days (p = 0.006); Hospital stay was shorter for Group B (5.9 days) compared to Group A (6.3 days) but not statistically significant |
4 |
| Aboutanos MB, 2007 [41] | Ecuador | Physicians (n = 26) | 30 MCQ pre- and post-test OSCE (Pass/Fail) |
Mean MCQ scores improved from 72% to 79% post-test (p < 0.032) 76% participants passed OSCE |
2 and 3 |
| Tchorz KM, 2007 [42] | India “Essential Principles and Practices of Trauma Care” |
Physicians (n = 32) | 20 MCQ pre- and post-test | Mean MCQ scores improved from 70.7% to 87.5% post-test (p = 0.000) | 2 |
| Mock CN, 2004 [43] | Ghana “Kwame Nkrumah University of Science and Technology Trauma Course” |
Physicians (n = 83) | 30 MCQ pre- and post-test | Mean MCQ scores improved from 69% to 80% post-test (p < 0.001) | 2 |
Nine of the papers gave an estimated cost for the course 10., 15., 16., 26., 31., 37., 39., 42., 43.. Papers reporting cost per participant ranged from $10 USD per participant to $232 USD per participant 10., 15.. Other papers reported an overall cost ranging from $2000 USD to $8200 USD excluding cost of external international course faculty 26., 16.. Peter et al. estimated their cascading model PTC course to cost approximately $232 USD per participant compared to an estimated $820 USD per participant for an ATLS course [15]. Oussi et al. reported a total cost of $800 USD (or $26.60 per participant) for their novel course, estimating cost to be 100 times less than that of an ATLS course [37]. Pringle et al. provided a detailed cost analysis of their 5 day novel course which cost $86 USD per participant ($2844 total), but only $8.82 per participant for recurring courses [39].
The majority of courses were a collaboration between a HIC University and local faculty/practitioners in the LMIC where the course was taught. The majority of papers did not mention how the course was funded. Of the 14 studies which indicated a funding source, the majority of courses were funded by partner universities in HICs or NGOs 10., 14., 15., 16., 24., 26., 31., 33., 36.. Mock et al. was the only course which was completely funded by the host country Ministry of Health (Ghana) while Hanche-Olsen reported shared funding between the Norwegian government and Botswana Ministry of Health 43., 29.. China trauma care training (CTCT) was developed and funded by the Chinese Medical Doctor Association and AIIMS Trauma Assessment and Management (ATAM) course was funded by the National Task Force Project of Indian Council of Medical Research 35., 32..
Discussion
A variety of courses are being utilized to provide trauma training to front-line providers in LMICs. Nearly all the courses included in this review were able to demonstrate a gain in knowledge, confidence, or skill in evaluating and treating injured patients. Only a single study attempted to evaluate a change in mortality rates or direct patient outcomes for injured patients after implementing a trauma course [40]. Given the challenges of maintaining a trauma registry in many LMICs, particularly when electronic medical records are not available, this is not surprising. In fact, a 2014 Cochrane review of patient outcomes after ATLS course implementation revealed no previous studies that adequately evaluated these metrics, although some studies did show trauma system improvements and knowledge gains [46]. One study in Rwanda utilized a trauma registry to evaluate the emergency department mortality of injury patients before and after training staff in both ATLS and International Surgery Trauma Team Training (TTT) showing an non-statistically significant reduction in mortality of all trauma patients but a statistically significant drop in mortality among those most severely injured [47]. Further research evaluating the impact of such courses on patient mortality would support increased funding for such initiatives.
Most of the courses took a similar teaching approach to ATLS with a primary and secondary survey model. This suggests that ATLS has become the global “gold standard” for trauma evaluation, but that its utility in a low-resource setting coupled with the financial and logistical challenges of implementing the course has limited its reach. Requirements for surgical societies to be the requesting and driving force behind new ATLS sites seems particularly burdensome. The creation and oversight of regional surgical societies are helpful in setting standards and creating trauma systems [48]. Emergency Medicine societies can take on this role as well, as evidenced by the Emergency Medicine Association of Tanzania (EMAT). Founded in 2011, EMAT has taken a leading role in developing trauma systems throughout Tanzania by providing PTC courses throughout the country and creating national standards for trauma and prehospital care [49]. However, requiring involvement of regional medical societies of any specialty to deliver trauma education creates barriers to training and seems to be unnecessary given that the majority of studies included in this review were initiated at the hospital level. Although regional trauma, surgical and emergency medicine societies are important to strengthening trauma care delivery, their formation should not be a pre-requisite to initiating trauma training or improving trauma capacity.
There is limited data available in regards to actual cost in implementing ATLS in LMICs. The Mongolian study discussed earlier estimated a minimal annual budget of $10,709 USD ($187 per trainee) and another $84,875 USD required to initially train the Mongolian instructors [4]. Peter et al. and Oussi et al. both cited their courses to be significantly cheaper than an ATLS alternative 15., 37.. Oussi cited an $80,000 ATLS startup cost which it used to make the comparison and determine their course was 100 times cheaper 37., 50.. The largest cost center for ATLS appears to be personnel, including international faculty 4., 5.. The studies included here were able to defer those costs by either using local faculty exclusively or using volunteer international faculty who donated their time. While it is difficult to compare exact costs of each course presented here against a hypothetical ATLS course in the same location, it appears likely that the majority of these courses can be delivered at a lower cost than ATLS.
Although broad search terms were used and multiple databases searched, this study is limited by selection bias which is inherent to this type of study methodology. A grey literature search was performed using BASE and OpenDOAR which provided some additional studies. However, there are certainly many other avenues for identifying grey literature which may have revealed other articles meeting inclusion criteria. Short courses which included trauma care as a component of a broader curriculum were also excluded from this review in order to limit extraneous topics which could serve as confounders. However, this approach may have excluded courses with significant trauma components such as the WHO's and International Committee of the Red Cross' (ICRC) Basic Emergency Care Course [51]. We also excluded courses which focused on prehospital trauma training. While these courses all provide important life-saving skills which may improve trauma mortality, our objective was to compare courses with a similar scope as ATLS.
Most of the courses included in the review demonstrated a statistically significant uptake of knowledge, suggesting that all are adequate to effectively train staff. However, none of the studies included in this review directly compared these alternative courses to ATLS or to each other. This creates some limitations in our ability to compare the courses in terms of effectiveness and cost. Most of the included studies relied on partners from HICs to fund the courses. This could be due to selection bias however, as it is possible that courses funded by HICs are more likely to seek publication and there may be larger locally driven initiatives for trauma training that are not published in the literature.
Conclusions
Several trauma courses are currently being utilized in LMICs effectively with increases in knowledge gained and at a lower reported cost than ATLS. More research is needed to link trauma training courses to patient outcomes.
Authorship contribution statement
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: HB contributed 50%, CT contributed 40%, PP contributed 10%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.afjem.2021.11.004.
Appendix A. Supplementary data
Supplementary material
References
- 1.World Health Organization . 2018. The Top 10 Causes of Death.https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death [Cited 2020, November 17] Available from. [Google Scholar]
- 2.World Health Organization . 2020, November 17. Global Burden of Disease: 2004 Update.https://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf?ua=1 Available from. [Google Scholar]
- 3.Petroze R.T., Byiringiro J.C., Ntakiyiruta G., et al. Can focused trauma education initiatives reduce mortality or improve resource utilization in a low-resource setting? World J Surg. 2015;39(4):926–933. doi: 10.1007/s00268-014-2899-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kornfeld J.E., Katz M.G., Cardinal J.R., Bat-Erdene B., Jargalsaikhan G., Nunez J. Cost analysis of the mongolian ATLS program: a framework for low- and middle-income countries. World J Surg. 2019;43(2):353–359. doi: 10.1007/s00268-018-4795-3. [DOI] [PubMed] [Google Scholar]
- 5.American College of Surgeons . 2020, November 30. International Promulgation: Advanced Trauma Life Support Program for Health Care Professionals.https://www.facs.org/-/media/files/quality-programs/trauma/atls/intnlpromulgation.ashx Available from. [Google Scholar]
- 6.Hammerstedt H., Maling S., Kasyaba R., et al. Addressing world health assembly resolution 60.22: a pilot project to create access to acute Care Services in Uganda. Ann Emerg Med. 2014;64(5):461–468. doi: 10.1016/j.annemergmed.2014.01.035. [DOI] [PubMed] [Google Scholar]
- 7.Tricco A.C., Lillie E., Zarin W., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 8.Brown H.A., Tidwell C., Prest P. 2020, September 19. Trauma training in low- and middle-income countries: A scoping review of ATLS alternatives. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kirkpatrick D.L., Kirkpatrick J.D. 3rd edition. Berrett-Koehler Publishers, Inc.; San Francisco: 2006. Evaluating training programs: the four levels. [Google Scholar]
- 10.Muzzammil M., Minhas M.S., SAA Ramzan Ali, Jooma R., Minhas M.O., Jabbar S. Primary trauma care course: alternative basic trauma course in developing countries. “The need of the hour”. Int J Clin Pract. 2021;75 doi: 10.1111/ijcp.14327. doi:10.111/ijcp.14327. [DOI] [PubMed] [Google Scholar]
- 11.Tolppa T., Vangu A.M., Balu H.C., Matondo P., Tissingh E. Impact of the primary trauma care course in the Kongo central province of the Democratic Republic of Congo over two years. Injury. 2020;51(2):235–242. doi: 10.1016/j.injury.2019.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Uma K., Harshad D., Dhanashree D. Impact of trauma workshop on knowledge, attitude and practice conducted on undergraduate MBBS students. Perspectives in Medical Research. 2020;8(3):81–85. doi: 10.47799/pimr.0803.17. [DOI] [Google Scholar]
- 13.Sadiq M.A., Rehman K.U., Tariq N., Bashir E.A. Impact of primary trauma care workshop on the cognitive domain of final year medical students. J Surg Pak. 2018;23(2):64–67. [Google Scholar]
- 14.Ologunde R., Le G., Turner J., et al. Do trauma courses change practice? A qualitative review of 20 courses in eastcentral and southern Africa. Injury. 2017;48(9):2010–2016. doi: 10.1016/j.injury.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Peter N., Pandit H., Le G., Nduhiu M., Moro E., Lavy C. Delivering a sustainable trauma management training programme tailored for low-resource settings in east, central and southern African countries using a cascading course model. Injury. 2016;47(5):1128–1134. doi: 10.1016/j.injury.2015.11.042. [DOI] [PubMed] [Google Scholar]
- 16.Nogaro M.C., Pandit H., Peter N., et al. How useful are primary trauma care courses in sub-saharan Africa? Injury. 2015;46(7):1293–1298. doi: 10.1016/j.injury.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 17.Jawaid M., Memon A.A., Masood Z., Alan S.N. Effectiveness of the primary trauma care course: is the outcome satisfactory? Pak J Med Sci. 2013;29(5):1265–1268. doi: 10.12669/pjms.295.4002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Amiri H., Gholipour C., Mokhtarpour M., Vahdati S.S., Aghdam Y.H., Bakhshayeshi. Two-day primary trauma care workshop: early and late evaluation of knowledge and practice. Eur J Emerg Med. 2013;20(2):130–132. doi: 10.1097/MEJ.0b013e32835608c6. [DOI] [PubMed] [Google Scholar]
- 19.Soomro R., Ali S. Trauma evaluation and management TEAM® course for medical students in Pakistan. Pak J Med Sci. 2020;36(6):1257–1262. doi: 10.12669/pjms.36.6.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berndtson A.E., Morna M., Debrah S., Coimbra R. The TEAM (Trauma evaluation and Management) course: medical student knowledge gains and retention in the USA versus Ghana. Trauma Surg Acute Care Open. 2019;4(1):1–4. doi: 10.1136/tsaco-2018-000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill K.A., Johnson E.D., Lutomia M., et al. Implementing the trauma evaluation and management (TEAM) course in Kenya. J Surg Res. 2018;232:107–112. doi: 10.1016/j.jss.2018.05.066. [DOI] [PubMed] [Google Scholar]
- 22.Delgado-Reyes L., Gasca-Gonzalez O.O., Delgado-Guerrero F., Reyes-Arellano W. Effectiveness of trauma evaluation and management course for Mexican senior medical students: when to implement it? Cir Cir. 2016;84(3):220–224. doi: 10.1016/j.circir.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Ali J., McDonald A., Newnham M. Improving medical undergraduate trauma education through the trauma evaluation and management programme at Mona. West Indian Med J. 2003;52(1):45–48. [PubMed] [Google Scholar]
- 24.Pemberton J., Rambaran M., Cameron B.H. Evaluating the long-term impact of the trauma team training course in Guyana: an explanatory mixed-methods approach. Am J Surg. 2013;205(2):119–124. doi: 10.1016/j.amjsurg.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 25.Bergman S., Deckelbaum D., Lett R., et al. Assessing the impact of the trauma team training program in Tanzania. J Trauma. 2008;65(4):879–883. doi: 10.1097/ta.0b013e318184a9fe. [DOI] [PubMed] [Google Scholar]
- 26.Macleod J.B.A., Okech M., Labib M., Aphivantrakul P., Lupasha E., Nthele M. Evaluation of trauma and critical care training courses on the knowledge and confidence of participants in Kenya and Zambia. World J Surg. 2010;35(1):9–16. doi: 10.1007/s00268-010-0810-z. [DOI] [PubMed] [Google Scholar]
- 27.Ali J., Kumar S., Gautam S., Sorvari A., Misra M.C. Improving trauma Care in India: the potential role of the rural trauma team development course (RTTDC) Indian J Surg. 2015;77(S2):227–231. doi: 10.1007/s12262-012-0775-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ali J., Khawaja K.K., Zubair M., Khatib J.A., Sorvari A. The rural trauma team development course in Pakistan – potential for improving trauma care. J Surg Pak. 2014;19(1):6–11. [Google Scholar]
- 29.Hanche-Olsen T.P., Alemu L., Viste A., Wisborg T., Hansen K.S. Evaluation of training program for surgical trauma teams in Botswana. World J Surg. 2014;39(3):658–668. doi: 10.1007/s00268-014-2873-8. [DOI] [PubMed] [Google Scholar]
- 30.Shrestha R., Khadka S.K., Thapa S., et al. Improving knowledge, skill and confidence in novice medical doctors in trauma management with principles of ABCDE. Kathmandu Univ Med J. 2018;61(1):69–73. [PubMed] [Google Scholar]
- 31.Ullrich S.J., Kilyewala C., Lipnick M.S., et al. Design, implementation and long-term follow-up of a context specific trauma training course in Uganda: lessons learned and future directions. Am J Surg. 2020;219(2):263–268. doi: 10.1016/j.amjsurg.2019.10.048. [DOI] [PubMed] [Google Scholar]
- 32.Babu B.V., Vishwanathan K., Ramesh A.C., et al. Participants’ perception of the AIIMS trauma assessment and management (ATAM) course for management of polytrauma: a multi-institutional experience from India. J Clin Orthop Trauma. 2021;12(1):130–137. doi: 10.1016/j.jcot.2020.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taylor S., Avrith N., Loo G., et al. Impact of a focused trauma course on retention of provider skills, knowledge and confidence at a regional hospital in the Dominican Republic. Injury. 2021;52(9):2526–2533. doi: 10.1016/j.injury.2021.06.001. [DOI] [PubMed] [Google Scholar]
- 34.Figueroa J.F., Loyola C., Martinez F., Salamea J.C. Efficacy of the basic trauma course in family medicine resident physicians in southern Ecuador: it is time to innovate education in trauma. Panam J Trauma Crit Care Emerg Surg. 2020;9(2):97–100. doi: 10.5005/jp-journals-10030-1286. [DOI] [Google Scholar]
- 35.Tang H., Liu D., Yang D., et al. Cross-sectional study of the educational background and trauma knowledge of trainees in the “China trauma care training” program. Mil Med Res. 2020;7(3):1–13. doi: 10.1186/s40779-020-0232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Anderson G.A., Kayima P., Ilcisin L., et al. Development of a comprehensive trauma training curriculum for the resource-limited environment. J Surg Educ. 2018;75(5):1317–1324. doi: 10.1016/j.jsurg.2018.02.014. [DOI] [PubMed] [Google Scholar]
- 37.Oussi N., Sadeghi M., Qureshi J.S., Mabedi C., Elbe P., Enochsson L. Short- and long-term results of low cost trauma training in a low-income resource-poor country. MedEdPublish. 2018;7(3) doi: 10.15694/mep.2018.0000218.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wanjiku G., Janeway H., Foggle J., et al. Assessing the impact of an emergency trauma course for senior medical students in Kenya. Afr J Emerg Med. 2017;7(4):167–171. doi: 10.1016/j.afjem.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pringle K., Mackey J., Ruskis J., Modi P., Foggle J., Levine A. A short trauma course for physicians in a resource-limited setting: is low-cost simulation effective? Ann Emerg Med. 2013;62(4) doi: 10.1016/j.annemergmed.2013.07.098. [DOI] [PubMed] [Google Scholar]
- 40.Noordin S., Allana S., Ahmad T., Bhatti A., Zafar H., Wajid M.A. Evolution of trauma management at a tertiary care hospital: a cohort study. Int J Surg. 2011;9(1):75–78. doi: 10.1016/j.ijsu.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 41.Aboutanos M.B., Rodas E.B., Aboutanos S.Z., et al. Trauma education and Care in the Jungle of Ecuador, where there is no advanced trauma life support. J Trauma. 2007;62(3):714–719. doi: 10.1097/ta.0b013e318031b56d. [DOI] [PubMed] [Google Scholar]
- 42.Tchorz K.M., Thomas N., Jesudassan S., et al. Teaching trauma Care in India: an educational pilot study from Bangalore. J Surg Res. 2007;142(2):373–377. doi: 10.1016/j.jss.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 43.Mock C.N., Quansah R., Addae-Mensah L., Donkor P. The development of continuing education for trauma care in an African nation. Injury. 2005;36(6):725–732. doi: 10.1016/j.injury.2004.12.044. [DOI] [PubMed] [Google Scholar]
- 44.Primary Trauma Care Foundation Primarytraumacare.org
- 45.Mock C., Lormand J.D., Goosen J., Joshipura M., Peden M. World Health Organization; Geneva: 2004. Guidelines for Essential Trauma Care. [Google Scholar]
- 46.Jayaraman S., Sethi D., Chinnock P., Wong P. Advanced trauma life support training for hospital staff (review) Cochrane Database Syst Rev. 2014;8:1–15. doi: 10.1002/14651858.CD004173.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petroze R.T., Byringiro J.C., Jayaraman S., et al. A systematic review of the impact of focused trauma education in low-resource settings. East Cent Afr J Surg. 2014;19(3):3–11. [Google Scholar]
- 48.Choi J., Carlos G., Nassar A.K., Knowlton L.M., Spain D.A. The impact of trauma systems on patient outcomes. Curr Probl Surg. 2021;58(1):1–21. doi: 10.1016/j.cpsurg.2020.100840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nicks B.A., Sawe H.R., Juma A.M., Reynolds T.A. The state of emergency medicine in the United Republic of Tanzania. Afr J Emerg Med. 2012;2(3):97–102. doi: 10.1016/j.afjem.2012.06.002. [DOI] [Google Scholar]
- 50.Quansah R., Abantanga F., Donkor P. Trauma training for nonorthopaedic doctors in low- and middle-income countries. Clin Orthop Relat Res. 2008;466(10):2403–2412. doi: 10.1007/s11999-008-0401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization and the International Committee of the Red Cross; Geneva: 2018. Basic emergency care: approach to the acutely ill and injured. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material