Abstract
Objective
Hydrothermal duodenal mucosal resurfacing (DMR) is a safe, outpatient endoscopic procedure. REVITA-2, a double-blind, superiority randomised controlled trial, investigates safety and efficacy of DMR using the single catheter Revita system (Revita DMR (catheter and system)), on glycaemic control and liver fat content in type 2 diabetes (T2D).
Design
Eligible patients (haemoglobin A1c (HbA1c) 59–86 mmol/mol, body mass index≥24 and ≤40 kg/m2, fasting insulin >48.6 pmol/L, ≥1 oral antidiabetic medication) enrolled in Europe and Brazil. Primary endpoints were safety, change from baseline in HbA1c at 24 weeks, and liver MRI proton-density fat fraction (MRI-PDFF) at 12 weeks.
Results
Overall mITT (DMR n=56; sham n=52), 24 weeks post DMR, median (IQR) HbA1c change was −10.4 (18.6) mmol/mol in DMR group versus −7.1 (16.4) mmol/mol in sham group (p=0.147). In patients with baseline liver MRI-PDFF >5% (DMR n=48; sham n=43), 12-week post-DMR liver-fat change was −5.4 (5.6)% in DMR group versus −2.9 (6.2)% in sham group (p=0.096). Results from prespecified interaction testing and clinical parameter assessment showed heterogeneity between European (DMR n=39; sham n=37) and Brazilian (DMR n=17; sham n=16) populations (p=0.063); therefore, results were stratified by region. In European mITT, 24 weeks post DMR, median (IQR) HbA1c change was –6.6 mmol/mol (17.5 mmol/mol) versus –3.3 mmol/mol (10.9 mmol/mol) post-sham (p=0.033); 12-week post-DMR liver-fat change was –5.4% (6.1%) versus –2.2% (4.3%) post-sham (p=0.035). Brazilian mITT results trended towards DMR benefit in HbA1c, but not liver fat, in context of a large sham effect. In overall PP, patients with high baseline fasting plasma glucose ((FPG)≥10 mmol/L) had significantly greater reductions in HbA1c post-DMR versus sham (p=0.002). Most adverse events were mild and transient.
Conclusions
DMR is safe and exerts beneficial disease-modifying metabolic effects in T2D with or without non-alcoholic liver disease, particularly in patients with high FPG.
Trial registration number
Keywords: endoscopic procedures, fatty liver, diabetes mellitus, duodenal mucosa
Summary box.
What is already known about this subject?
More than half of patients with type 2 diabetes mellitus are unable to sustain adequate glycaemic control with the current standard of care.
Current approaches do not adequately target underlying disease pathophysiology (ie, insulin resistance (IR) and hyperinsulinaemia).
Bariatric surgeries that bypass nutrient contact from the duodenum (eg, Roux-en-Y gastric bypass) improve glycaemic control and insulin sensitivity.
Duodenal mucosal resurfacing is a minimally invasive, outpatient endoscopic procedure that targets duodenal pathology to treat insulin-resistance–related metabolic disease, including type 2 diabetes mellitus. Published data from earlier open-label studies have shown statistically significant improvements in haemoglobin A1c (HbA1c), alanine transaminase, aspartate transaminase, weight and homeostatic model assessment of IR through 12-month follow-up.
What are the new findings?
In this first prospective, double-blind, sham-controlled study of Revita duodenal mucosal resurfacing, a single duodenal mucosal resurfacing procedure was well tolerated, safe, and elicits clinically and statistically significant improvements in HbA1c levels and liver fat content in European patients with poorly controlled type 2 diabetes mellitus.
These results confirm that the duodenal mucosa is a therapeutic target for type 2 diabetes with or without non-alcoholic fatty liver disease/non-alcoholic steatohepatitis.
How might it impact on clinical practice in the foreseeable future?
These data provide insight into a potential therapeutic opportunity for duodenal mucosal resurfacing to favourably impact both type 2 diabetes and non-alcoholic fatty liver disease/non-alcoholic steatohepatitis in a manner that can modify the natural history of these chronic and progressive diseases.
Introduction
The global prevalence of type 2 diabetes mellitus (T2D) and non-alcoholic fatty liver disease, due in part to the widespread adoption of diets with high sugar and fat content, is increasing at an alarming rate.1–3 Insulin resistance (IR) and hyperinsulinemia play an important role in the pathological progression and decompensation of multiple organ systems in these conditions.3 4 Despite the fact that over 50 unique pharmacological agents are currently approved to treat T2D, and the benefits of dietary interventions are well established, most patients with T2D are unable to sustain adequate glycaemic control (recommended haemoglobin A1c (HbA1c) levels≤53 mmol/mol).5 6 Poor adherence and persistence to prescribed therapies, drug-to-drug interactions, side effects, and patient dissatisfaction are fundamental barriers to the real-world effectiveness of current approaches to manage T2D.7 8
Bariatric/metabolic surgeries that bypass nutrient contact from the duodenum, such as Roux-en-Y gastric bypass and biliopancreatic diversion, originally intended to aid weight loss, have demonstrated compelling evidence to provide sustainable improvements in patients with T2D.9–11 Bariatric/metabolic surgery is safe with a low mortality rate (0.1%–0.5%), similar to that observed after cholecystectomy or hysterectomy.12 Nevertheless, only 1% of eligible patients undergo this type of surgery.13 14 Endoscopic procedures are emerging as an effective and minimally invasive approach to treat obesity and/or T2D, closing the gap between pharmacological therapy and bariatric/metabolic surgery.
Duodenal mucosal resurfacing (DMR) is a minimally invasive endoscopic procedure performing circumferential mucosal lift and hydrothermal ablation of the duodenal mucosa.15 The first-in-human safety trial showed that DMR is safe and able to improve glycaemic control in proportion to the length of the ablated duodenal mucosal segment.16 17 The following multicentre, open-label REVITA-1 trial in 46 patients with poorly controlled T2D showed a significant reduction of baseline HbA1c at 24 weeks after DMR of −10±2 mmol/mol (−0.9%±0.2%; p<0.001).18
Herein, we report the results of the first double-blind, multicentre, randomised controlled trial with a single DMR procedure, which assessed the efficacy and safety of DMR in patients with T2D with or without NAFLD versus a sham endoscopic procedure.
Methods
Additional protocols and complete procedures are described in the online supplemental material and methods section.
gutjnl-2020-323608supp001.pdf (2.4MB, pdf)
Trial design and oversight
REVITA-2 was a randomised, double-blind (patient and endocrinologist), sham-controlled trial conducted across 11 sites (nine in Europe (Italy, UK, Belgium and Netherlands) and two in Brazil) from 11 September 2017 to 15 December 2018 (online supplemental figure 1).
A data monitoring committee oversaw this study (see online supplemental methods for details).
Randomisation and masking
Patients (see online supplemental table 1 for complete eligibility criteria) were randomised (1:1) to undergo the DMR or sham procedure by using a central web-based random allocation system (see online supplemental methods for details). Endocrinologists and patients were unaware of the treatment assignment until the 24-week follow-up visit.
Procedures
DMR was performed with the single catheter Revitasystem (Revita DMR(catheter and system), Fractyl Laboratories, Lexington, Massachusetts, USA) as previously described (online supplemental figure 2).16–18 A full DMR procedure was defined as five sequential ablations of 2 axial centimetres each, starting within 3 centimetres distal to the Ampulla of Vater towards the Ligament of Treitz, totalling 10 axial centimetres of circumferentially ablated tissue in the duodenum during a single endoscopic session. The sham procedure consisted of placing the DMR catheter over the guidewire into the stomach and leaving it in place for 30 min prior to removing it from the patient.
Study endpoints and assessments
The two primary efficacy endpoints were the absolute change from baseline at 24 weeks in HbA1c in all patients and absolute change from baseline at 12 weeks in liver MRI proton density fat fraction (MRI-PDFF), specifically in those patients with NAFLD at baseline (liver MRI-PDFF >5%). The primary safety endpoints assessed were the incidence of device-related and procedure-related serious adverse events (SAEs), unanticipated adverse device events (UADEs), and AEs of special interest (AESIs), including hypoglycaemic events, through 24 weeks. Adverse events were recorded from the time the informed consent document was signed. The prespecified safety analysis tabulated the difference in the proportion of patients who experienced ≥1 major complication (DMR vs sham).
Secondary endpoints assessed were the relative change in liver MRI-PDFF from baseline at week 12 in patients with baseline liver MRI-PDFF >5% and absolute change from baseline at 24 weeks in fasting plasma glucose (FPG) levels, weight, and homeostatic model assessment of IR (HOMA-IR).
Exploratory endpoints assessed were absolute change from baseline at 24 weeks in triglycerides, low-density lipoprotein cholesterol, high-density lipoprotein, alanine transaminase (ALT), and aspartate transaminase levels, and change in oral antidiabetic medication from baseline at week 24. In addition, the percentage of patients achieving HbA1c levels<53 mmol/mol or liver fat content reduction >30% at the end of the study as well as the number of antihyperglycaemic drugs during the trial were assessed (see online supplemental table 2).
Rescue medications: persistent hyperglycaemia was a criterion to receive rescue medication, which was prescribed, per protocol (PP), with increasing doses of oral medications and/or insulin according to clinical practice guidelines (see online supplemental table 3).19 20 Patients continued in the trial after receiving rescue medication.
Statistical analysis
The primary efficacy endpoints were planned to be tested for superiority of DMR versus sham with adjustment for multiple endpoints using the Hochberg procedure.21 Under this procedure, DMR was considered beneficial over sham for both primary endpoints if the one-sided p value for each endpoint was <0.05; and/or, if the one-sided treatment comparison p value was<0.025 for one endpoint, then DMR was considered beneficial over sham for that given endpoint.
Intention-to-treat and PP analyses
The primary analysis population for primary and secondary endpoints was the modified intention-to-treat (mITT) population, defined as all randomised patients in whom the study procedure was attempted and who had a baseline measurement for ≥1 primary endpoint. The PP population was defined as the subset of mITT patients who received the treatment to which they were randomised and strictly adhered to the protocol.
Safety analyses were completed in all patients in whom the treatment (DMR or sham) was initiated and included all AEs revealed during the follow-up, independent of duration. AEs and SAEs are presented as the number and percent of patients; overall counts were compared using the two-sided Clopper-Pearson 95% CI of the incidence rates.
The following additional analyses were conducted: (1) proportion of all patients who achieved an HbA1c level <53 mmol/mol at 24 weeks post procedure; (2) proportion of patients with baseline MRI-PDFF >5% who achieved a relative liver MRI-PDFF reduction >30% from baseline at week 12; (3) stratification of end-study HbA1c by baseline FPG levels. The change in oral antidiabetic medication from baseline at week 24 (increase, neutral, or decrease) was assessed in patients with 24 weeks of follow-up.
Statistical analyses were performed using Statistical Analysis Software V.9.4 or later (SAS Institute) or R V.3.3.2 or later. See supplemental material for additional analyses details and powering assumptions.
Analysis of normality and homogeneity in the study populations
Assessments of normality and homogeneity were performed as specified in the statistical analysis plan. The normality tests assessed whether each variable was normally distributed. Assessments of homogeneity evaluated consistency in treatment effect across geographic regions (Belgium, Brazil, Italy, Netherlands and UK) with a prespecified treatment-by-region interaction p value of<0.10 (see online supplemental methods for details).
An exploratory analysis using partial least-squares-discriminant analysis (PLS-DA) was performed to further understand and assess the interaction by regions in the prespecified study populations. PLS-DA is a useful exploratory analysis showing patterns related to a treatment effect without testing a formal hypothesis; in other words, it provides a comparative and clear visual of different patterns in two samples (see online supplemental methods for details).
HOMA-IR and Matsuda Index Calculation
Fasting IR was measured based on the HOMA-IR calculated as (FPG * fasting insulin)/135, where FPG level was measured in mmol/L and fasting insulin was measured in pmol/L.22
The Matsuda Index was calculated as 10000/(G0·I0·Gm·Im)0.5, where G0 and I0 are premeal values for glucose and insulin and Gm and Im are mean post-meal values during the first 120 min of the liquid meal tolerance test with glucose and insulin values in mmol/L and mU/L, as validated for a meal test.23 24 Since the square root of the denominator takes into account the correction of nonlinear values distribution, these values are reported as mean±SD.
Role of the funding source
The funder of the study participated in study design, data collection, data analysis, data interpretation and writing of the report. The corresponding author (GM) had full access to all the data in the study and had final responsibility for the decision to submit the manuscript for publication.
Patient and public involvement
Patients were not directly involved in the design, recruitment or conduct of the study.
Results
Patient baseline characteristics
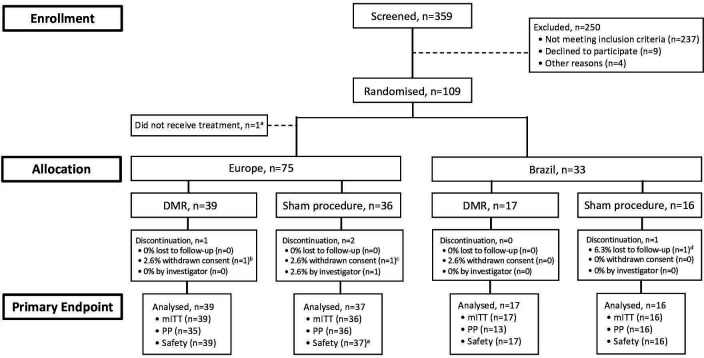
Between 11 September 2017 and 15 December 2018, 359 patients were screened and 250 were excluded from the study (figure 1). 109 patients were randomised (although one did not receive treatment due to oesophageal varices) 1:1 either to DMR (n=56) or to sham procedure (n=52); 75 in Europe (39 DMR, 36 sham procedure) and 33 in Brazil (17 DMR, 16 sham procedure).
Figure 1.
Patient disposition. Between 1 March 2017, and 15 December 2018, 109 of 359 patients assessed for eligibility were randomised. One patient at a European study site did not receive treatment due to oesophageal varicesa; therefore, the modified intention-to-treat (mITT) population included 108 patients—75 in Europe (39 to duodenal mucosal resurfacing (DMR) and 36 to sham) and 33 in Brazil (17 to DMR and 16 to sham). Prespecified assessments of normality and homogeneity (see the Methods section for details) revealed that the European and Brazilian populations were not poolable. Therefore, all efficacy analyses were stratified into two populations (Europe and Brazil). aThe one patient who withdrew and did not receive treatment was followed for safety, but not efficacy. Last completed visit was at week 4a, week 21 (phone call)b, and day 7 (phone call)d. PP, per protocol.
Overall, 71 patients (65.7%) were white, 7 (6.5%) were black, 2 (1.8%) were Asian, 3 (2.8%) belonged to other races and 25 (23.1%) preferred not to disclose their race.
Patient demographics and baseline characteristics were well balanced between the DMR and sham procedure groups (table 1). Men accounted for 69.4% of the patients. At baseline, the median body mass index was 31.5 (4.7) kg/m2 in the DMR group and 30.7 (5.7) kg/m2 in the sham group. The median baseline HbA1c levels were 65.6 (8.7) mmol/mol in the DMR group and 66.1 (10.4) mmol/mol in the sham group. The median duration of diabetes was 10.0 (6.0) years and 9.1 (8.8) years among patients who underwent DMR or sham procedure, respectively. Most patients (85.5% in the DMR group and 82.7% in the sham group) had more than 5% fat accumulation in the liver as detected at baseline by MRI-PDFF.
Table 1.
Baseline characteristics and demographics and change from baseline (modified intention-to-treat population*)
| Parameter | Overall | Europe† | Brazil | ||||||
| DMR N=56 | Sham N=52 | P value | DMR N=39 | Sham N=36 |
P value | DMR N=17 | Sham N=16 | P value | |
| Age, years | 58.0 (13.5) | 58.5 (14.0) | 0.747 | 59.0 (13.0) | 56.5 (14.0) | 0.627 | 56.0 (13.0) | 59.5 (11.5) | 0.164 |
| Sex, n (%) | 0.963 | 0.93 | 0.866 | ||||||
| Female | 17 (30.4) | 16 (30.8) | 9 (23.1) | 8 (22.2) | 8 (41.7) | 8 (50.0) | |||
| Male | 39 (69.6) | 36 (69.2) | 30 (76.9) | 28 (77.8) | 9 (52.7) | 8 (50.0) | |||
| Race, n (%) | 0.974 | 0.658 | 0.562 | ||||||
| White | 37 (66.1) | 34 (65.4) | 25 (64.1) | 21 (58.3) | 12 (70.6) | 13 (81.3) | |||
| Black | 4 (7.1) | 3 (5.8) | 0 | 0 | 4 (23.5) | 3 (18.8) | |||
| Asian | 1 (1.8) | 1 (1.9) | 0 | 1 (2.8) | 1 (5.9) | 0 | |||
| Other | 1 (1.8) | 2 (3.8) | 1 (2.6) | 2 (5.6) | 0 | 0 | |||
| Undisclosed | 13 (23.2) | 12 (23.1) | 13 (33.3) | 12 (33.3) | 0 | 0 | |||
| Weight, kg | |||||||||
| Baseline | 93.0 (15.9) | 92.6 (26.4) | 0.438 | 93.1 (16.5) | 94.5 (24.6) | 0.644 | 89.0 (15.6) | 87.8 (19.8) | 0.627 |
| Week 24 | 90.0 (17.5) | 87.4 (26.0) | 0.707 | 91.0 (17.5) | 92.6 (27.0) | 0.937 | 86.8 (19.7) | 83.2 (22.6) | 0.678 |
| Change from baseline (week 24) | |||||||||
| Absolute | −2.5 (4.5) | −1.5 (3.3) | 0.021 | −2.4 (2.8) | −1.4 (2.4) | 0.012 | −4.1 (5.6) | −2.1 (5.7) | 0.285 |
| Relative (%) | −2.8 (4.5) | −1.8 (3.5) | 0.037 | −2.6 (3.4) | −1.5 (2.9) | 0.013 | −4.5 (5.7) | −2.8 (5.6) | 0.403 |
| BMI, kg/m2 | |||||||||
| Baseline | 31.5 (4.7) | 30.7 (5.7) | 0.206 | 31.4 (4.5) | 30.4 (6.1) | 0.16 | 32.3 (4.7) | 31.6 (6.2) | 0.928 |
| Week 24 | 30.6 (5.2) | 29.9 (5.5) | 0.563 | 30.6 (5.0) | 29.7 (6.3) | 0.376 | 30.6 (5.6) | 30.8 (5.9) | 0.828 |
| Change from baseline (week 24) | |||||||||
| Absolute | −0.9 (1.5) | −0.5 (1.1) | 0.025 | −0.8 (1.2) | −0.5 (0.9) | 0.011 | −1.4 (1.9) | −0.8 (1.9) | 0.28 |
| Relative (%) | −2.8 (4.5) | −1.8 (3.5) | 0.042 | −2.6 (3.4) | −1.5 (2.9) | 0.013 | −4.5 (5.7) | −2.8 (5.6) | 0.365 |
| HbA1c levels, mmol/mol | |||||||||
| Baseline | 65.6 (8.7) | 66.1 (10.4) | 0.839 | 65.0 (7.6) | 66.1 (9.3) | 0.45 | 70.5 (9.8) | 65.6 (14.2) | 0.213 |
| Week 24 | 55.2 (16.4) | 61.2 (18.0) | 0.436 | 59.6 (16.4) | 63.9 (14.2) | 0.132 | 51.9 (5.5) | 48.6 (8.7) | 0.104 |
| Change from baseline (week 24) | |||||||||
| Absolute | −10.4 (18.6) | −7.1 (16.4) | 0.147 | −6.6 (17.5) | −3.3 (10.9) | 0.033 | −20.2 (14.2) | −17.5 (9.8) | 0.104 |
| Relative (%) | −16.7 (28.6) | −10.6 (23.3) | 0.184 | −9.6 (27.1) | −3.8 (18.3) | 0.034 | −27.6 (14.9) | −25.6 (12.9) | 0.105 |
DMR, duodenal mucosal resurfacing; HbA1c, haemoglobin A1c.
mITT analysis and post-hoc analyses
In the overall mITT population (DMR n=56; sham n=52), the median change in HbA1c from baseline at 24 weeks post procedure was −10.4 (18.6) mmol/mol in the DMR group compared with −7.1 (16.4) mmol/mol in the sham group (p=0.147; treatment difference −3.3 mmol/mol). In patients with baseline liver MRI-PDFF >5% (DMR n=48; sham n=43), the median absolute change in liver MRI-PDFF from baseline at 12 weeks was −5.4 (5.6)% in the DMR group compared with −2.9 (6.2)% in the sham group (p=0.096; treatment difference −2.5%).
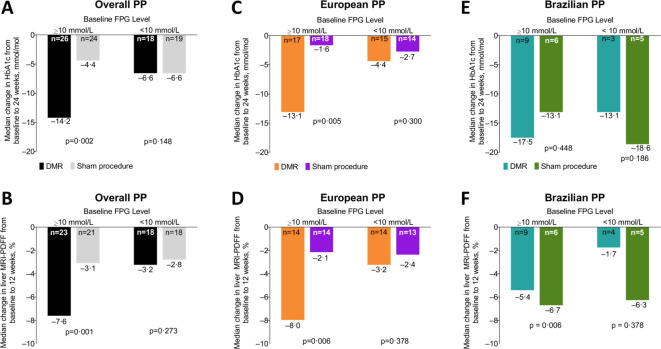
A post-hoc analysis of pooled data from the overall PP population stratified by baseline FPG levels demonstrated that in patients with FPG ≥10 mmol/L, the median (IQR) reduction in HbA1c at week 24 post procedure was –14.2 (17.5) mmol/mol post DMR compared with –4.4 (15.3) mmol/mol in the sham group (p=0.002); whereas, in patients with FPG <10 mmol/L, the median reductions in HbA1c were similar between groups (p=0.148; figure 2A). In patients with baseline liver MRI-PDFF >5% and FPG ≥10 mmol/L, the median absolute change in liver MRI-PDFF was significantly greater in the DMR group compared with patients who underwent the sham procedure (p=0.001; figure 2B). Similar results were observed in the European PP population for both HbA1c and liver fat content changes (figure 2C, D) and in the Brazilian PP population, but only for liver fat content (figure 2E, F).
Figure 2.
Post-hoc analysis of change in haemoglobin A1c (HbA1c) levels and liver MRI proton density fat fraction (MRI-PDFF) stratified by baseline fasting plasma glucose (FPG) level status (per-protocol (PP) populations). Median HbA1c per cent change from baseline to 24 weeks (duodenal mucosal resurfacing (DMR) versus sham procedure) in the overall (A), European (C) and Brazilian (E) PP patients with baseline FPG ≥10 mmol/L compared with patients with baseline FPG <10 mmol/L. In patients with baseline liver MRI-PDFF >5%, median liver MRI-PDFF per cent change from baseline to 12 weeks (DMR vs sham procedure) in the overall (B), European (D), and Brazilian (F) PP patients with baseline FPG ≥10 mmol/L compared with FPG <10 mmol/L. Treatment comparison of one-sided p value based on analysis of covariance model with multiple imputation on the rank values (modified ridit scores). Via multiple imputation, analysis is based on all patients in the population of interest. The overall PP population includes patients from both European and Brazilian study sites. The European PP population consists of patients from Italy, UK, Belgium and Netherlands.
Primary and secondary endpoints by region
Demographics and baseline characteristics were similar (table 1), but prespecified interaction testing by region showed heterogeneity between patients in Europe (DMR N=39; sham N=36) and patients in Brazil (DMR N=17; sham N=16) for the HbA1c outcome (p=0.063). As such, European and Brazilian regions were analysed separately for all clinical outcomes. A post-hoc PLS-DA confirmed these regions were separate groups with different variance/covariance structures (online supplemental figure 3). The primary endpoints were found to be not normally distributed and are therefore presented as median (IQR).
PLS-DA is a linear classification model that is able to predict the class of new samples. We used PLS-DA as a post-hoc analysis that confirmed the European and Brazilian populations were separate groups with different variance/covariance structures (figure 3). This analysis including all patients, regardless of treatment group, showed that the first two components of PLS-DA explained 35% of the variance that contributed to the separation of the European and Brazilian populations. The general predictive performance of the PLS-DA model in correctly classifying the patients as belonging to the European or to the Brazilian groups was very good as shown by the area under the curve of 0.89. Therefore, due to heterogeneity demonstrated by multiple statistical methods and the unexpected differences seen between Europe and Brazil in the sham arms (table 2), analyses were stratified by region.
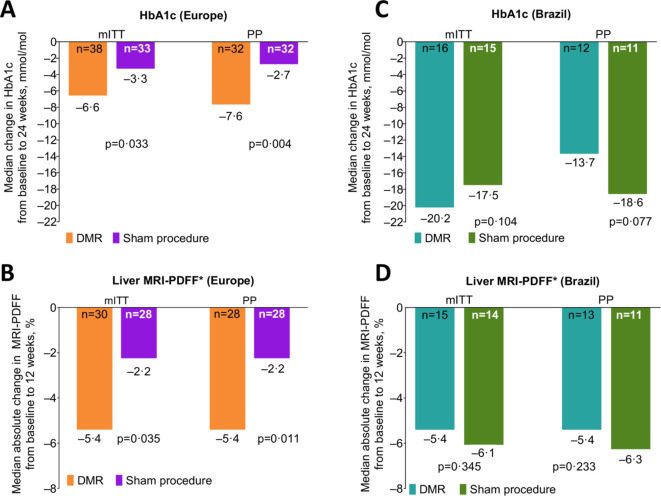
Figure 3.
Haemoglobin A1c (HbA1c) levels and liver MRI proton density fat fraction (MRI-PDFF) at 24 weeks post duodenal mucosal resurfacing (DMR) (primary endpoint). Median per cent change in HbA1c levels (DMR vs sham procedure) from baseline to 24 weeks in the European (A) and Brazilian (B) modified intention-to-treat (mITT) and per-protocol (PP) populations. Median absolute per cent change in liver MRI-PDFF (DMR vs sham procedure) from baseline to 24 weeks in patients with baseline MRI-PDFF >5% (*) in the European (C) and Brazilian (D) mITT and PP populations. Treatment comparison one-sided p value based on analysis of covariance model with multiple imputation on the rank values (modified ridit scores). Via multiple imputation, analysis is based on all patients in the population of interest where post rescue values are first set to missing. Data for continuous variables are on non-imputed unadjusted descriptive statistics based on patients with non-missing values.
Table 2.
Change from baseline in haemoglobin A1c (HbA1c) levels, liver MRI proton density fat fraction (MRI-PDFF) and weight (sham-treated modified intention-to-treat population)
| Parameter | Europe N=37 |
Brazil N=16 |
| HbA1c levels at 24 weeks, mmol/mol | n=33 | n=15 |
| −3.3 (10.9) | −17.5 (9.8) | |
| Liver MRI-PDFF >5% at baseline, n (%) | 28 (75.7) | 14 (87.5) |
| Absolute change in liver MRI-PDFF at 12 weeks, % | −2.2 (4.3) | −6.1 (7.8) |
| Weight at 24 weeks, kg | n=34 | n=15 |
| −1.4 (2.4) | −2.1 (5.7) |
Data are presented as median (IQR), unless otherwise indicated.
In the European mITT population, the median change in HbA1c from baseline at 24 weeks post procedure was –6.6 (17.5) mmol/mol in the DMR group compared with –3.3 (10.9) mmol/mol in the sham procedure group (p=0.033; treatment difference –3.3 mmol/mol; figure 3A). In patients with baseline liver MRI-PDFF >5%, the median absolute change in liver MRI-PDFF from baseline at 12 weeks revealed a reduction of liver fat content by 5.4 (6.1)% in the DMR group compared with 2.2 (4.3)% in the sham procedure group (p=0.035; treatment difference –3.2%; figure 3B). Similar results were observed in the European PP population and using a prespecified mixed-model repeated measures analysis (MMRM) (described within the online supplemental material).
In the Brazilian mITT population, change from baseline in HbA1c levels (figure 3C) was not significantly different in DMR compared with sham in the primary analysis, but was significantly lower in the prespecified sensitivity MMRM analysis (p=0.104 and p=0.034, respectively). In Brazil, there was no significant difference between treatment groups in liver MRI-PDFF (figure 3D).
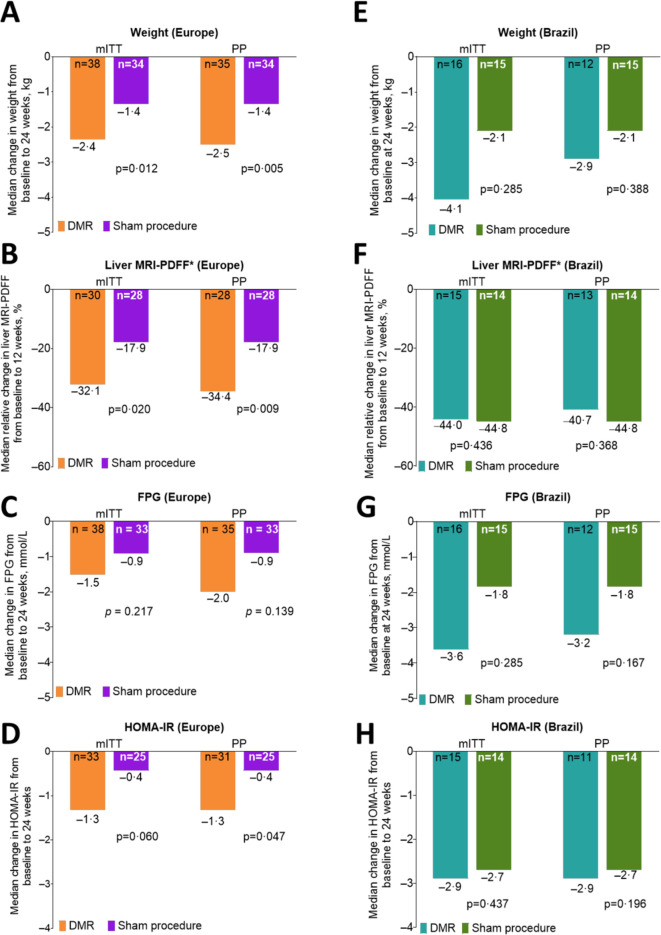
In the European mITT population, the median reduction in weight 24 weeks post procedure was significantly greater in the DMR group (–2.4 (2.8) kg) than in the sham group (–1.4 (2.4) kg; p=0.012; treatment difference –1.0 kg; figure 4A). At 12 weeks post procedure, European patients with baseline liver MRI-PDFF >5% had a significantly greater reduction of the median relative liver MRI-PDFF from baseline in the DMR group compared with the sham group (–32.1% (20.6%) vs –17.9% (25.6%); p=0.020; treatment difference –14.2%; figure 4B). Median reduction in FPG levels from baseline at 24 weeks post procedure was numerically lower in the DMR group compared with sham procedure group (–1.5 mmol/L (4.6 mmol/L) vs –0.9 mmol/L (3.0 mmol/L); p=0.217; treatment difference –0.6 mmol/L; figure 4C), and median reduction in HOMA-IR was numerically lower in the DMR group compared with the sham group (–1.3 (2.5) vs –0.4 (1.5); p=0.060; treatment difference –0.9; figure 4D). Sensitivity analysis of HOMA-IR reached statistical significance in non-imputed complete case analysis for missing secondary endpoint data (p=0.028), indicating an insulin-sensitising mechanism of DMR. The mean (SD) increase in Matsuda Index, a post-hoc analysis of insulin sensitivity (higher numbers denoting better insulin sensitivity), was greater in the DMR group compared with the sham group (1.2±2.7 vs 0.2±1.5; p=0.035; treatment difference 1.0).
Figure 4.
Clinically meaningful reductions in weight, liver fat and homeostatic model assessment of insulin resistance (HOMA-IR) with duodenal mucosal resurfacing (DMR). Median weight (kg) change from baseline to 24 weeks (DMR vs sham procedure) in the European (A) and Brazilian (B) modified intention-to-treat (mITT) and per-protocol (PP) populations. Median relative liver MRI proton density fat fraction (MRI-PDFF) per cent change from baseline to 12 weeks in patients with baseline MRI-PDFF >5% (*) in the European (C) and Brazilian (D) mITT and PP populations. Median fasting plasma glucose (FPG; millimoles per litre) change from baseline to 24 weeks (DMR vs sham procedure) in the European (E) and Brazilian (F) mITT and PP populations. Median HOMA-IR change from baseline to 12 weeks (DMR vs sham procedure) in the European (G) and Brazilian (H) mITT and PP populations. Data for continuous variables are on non-imputed unadjusted descriptive statistics based on patients with non-missing values. Treatment comparison one-sided p value based on analysis of covariance model on ranks (modified ridit scores) where post rescue values are first set to missing. Last rank carried forward on ranks was used for missing data for FPG levels, weight and HOMA-IR endpoints. HOMA-IR was determined as (FPG * fasting insulin)/135, where FPG levels were measured in millimoles per litre and fasting insulin is measured in picomoles per litre.
The mITT analysis of the relative changes in weight, liver fat content (MRI-PDFF), FPG and HOMA-IR in the Brazilian population did not show any significant difference between DMR and sham groups (figure 4E–H, respectively).
In the European mITT population, the DMR group had significantly more patients achieving HbA1c levels<53 mmol/mol at 24 weeks compared with the sham group (26.3% vs 9.1%; p=0.031; online supplemental figure 4A). Similarly, 53% of patients in the DMR group with baseline MRI-PDFF >5% achieved a relative liver MRI-PDFF reduction >30% from baseline at week 12, compared with 22% in the sham procedure group (p=0.008; online supplemental figure 4B).
Finally, most patients experienced no change or had an increased use in oral antidiabetic medication from baseline at week 24 in both the European and Brazilian mITT populations (online supplemental table 4).
Time of procedure
The median total catheter indwelling time in the entire sample was 56∙.0 min (26∙.0 min).
Safety analysis
All patients were included in the safety analysis, 76 in Europe (DMR n=39; sham n=37) and 33 in Brazil (DMR n=17; sham n=16). Most AEs were mild and transient; the most common were abdominal pain, diarrhoea, hyperglycaemia, hypoglycaemia, nasopharyngitis and headache. In the European population, no device-related or procedure-related SAEs or UADEs were reported through 24 weeks post procedure (table 3). Approximately 33% of patients in the DMR group (n=13) experienced a device-related or procedure-related AESI, compared with 27% of patients (n=10) in the sham procedure group. The most common (occurring in ≥5% of patients) device-related or procedure-related AESIs occurring ≤30 days post procedure were abdominal pain and hypoglycaemia. Similar number of events and percentage of patients with events of hypoglycaemia (related to procedure) were found in both groups (4 events; 7.7% (3/39) patients with event in DMR group and 8 events; 10.8% (4/37 patients with events in the sham group)). There was an absence of pancreatitis, infection and thermal injury. Follow-up endoscopy was performed (n=32); overall, the duodenum appeared normal with complete healing.
Table 3.
Device-related/procedure-related adverse events through 24 weeks post procedure (safety population)
| Europe | Brazil | |||||||||||
| DMR N=39 | Sham N=37 | DMR N=17 | Sham N=16 | |||||||||
| # of events | n (%) | 95% CI‡ | # of events | n (%) | 95% CI‡ | # of events | n (%) | 95% CI‡ | # of events | n (%) | 95% CI‡ | |
| Summary (through 24 weeks post-treatment) | ||||||||||||
| SAE | 0 | 0 | (0.0 to 9.0) | 0 | 0 | (0.0 to 9.5) | 3 | 2 (11.8) | (1.5 to 36.4) | 0 | 0 | (0.0 to 20.6) |
| UADE | 0 | 0 | (0.0 to 9.0) | 0 | 0 | (0.0 to 9.5) | 0 | 0 | (0∙0 to 19.5) | 0 | 0 | (0.0 to 20.6) |
| AESI | 19 | 13 (33.3) | (19.1 to 50.2) | 16 | 10 (27.0) | (13.8 to 44.1) | 74 | 12 (70.6) | (44.0 to 89.7) | 76 | 10 (62.5) | (35.4 to 84.8) |
| Most common (≥5%) AESIs by preferred term (≤30 days post-treatment) | ||||||||||||
| Abdominal pain | 9 | 7 (17.9) | (7.5 to 33.5) | 2 | 2 (5.4) | (0.7 to 18.2) | 6 | 5 (29.4) | (10.3 to 56.0) | 2 | 2 (12.5) | (1.6 to 38.4) |
| Diarrhoea | 1 | 1 (2.6) | (0.1 to 13.5) | 2 | 2 (5.4) | (0.7 to 18.2) | 1 | 1 (5.9) | (0.2 to 28.7) | 1 | 1 (6.3) | (0.2 to 30.2) |
| Nausea | 1 | 1 (2.6) | (0.1 to 13.5) | 0 | 0 | (0.0 to 9.5) | 2 | 2 (11.8) | (1.5 to 36.4) | 0 | 0 | (0∙0 to 20∙6) |
| Vomiting | 1 | 1 (2.6) | (0.1 to 13.5) | 0 | 0 | (0.0 to 9.5) | 1 | 1 (5.9) | (0.2 to 28.7) | 0 | 0 | (0∙0 to 20∙6) |
| Hypoglycaemia | 3 | 3 (7.7) | (1.62 to 20.9) | 3 | 2 (5.4) | (0.7 to 18.2) | 11 | 6 (35.3) | (14.2 to 61.7) | 21 | 7 (43.8) | (19.8 to 70.1) |
| Most common (≥5%) AESIs by preferred term (>30 days post-treatment) | ||||||||||||
| Abdominal pain | 1 | 1 (2.6) | (0.1 to 13.5) | 2 | 2 (5∙4) | (0.7 to 18.2) | 0 | 0 | (0.0 to 19.5) | 0 | 0 | (0.0 to 20.6) |
| Hypoglycaemia | 1 | 1 (2.6) | (0.1 to 13.5) | 4 | 2 (5∙4) | (0.7 to 18.2) | 53 | 5 (29.4) | (10.3 to 56.0) | 52 | 8 (50.0) | (24.7 to 75.4) |
Data are presented as n (%), with n as the number of patients with an event.
*The primary safety analysis population was defined as all patients in whom the treatment (DMR or sham) was initiated.
†European safety population included patients from Italy, UK, Belgium and Netherlands.
‡Two-sided Clopper-Pearson 95% CI of the incidence rates.
AESI, adverse event of special interest; DMR, duodenal mucosal resurfacing; SAE, serious adverse event; UADE, unanticipated adverse device effect.
In the Brazilian population, 11.8% of patients (n=2) in the DMR group experienced SAEs related to the procedure (table 3). One SAE was a precautionary hospitalisation for evaluation for a patient who noted mild haematochezia 8 days after a DMR procedure. The haematochezia was ascribed to a visible external haemorrhoid; however, the investigator adjudicated it as possibly related to procedure. The other SAE was a jejunal perforation caused by manipulation of the endoscope used in the procedure during the performance of an upper endoscopy, requiring surgical repair with no further sequelae. Hypoglycaemia (related to procedure) was reported in 47% (8/17) of patients in the DMR group and 56% (n=9/16) in the sham group with 64 and 74 events in each arm, DMR versus sham, respectively. Follow-up endoscopy was performed (n=17); overall, the duodenum appeared normal with complete healing.
Discussion
In REVITA-2, a randomised, double-blind, sham-controlled, multicentre trial in patients with poorly controlled T2D with or without NAFLD, a single DMR procedure was well tolerated. Due to the regional heterogeneity revealed by interaction testing, the European and Brazilian populations were analysed separately. Though there was less power to detect a statistical difference between DMR and sham arms, in the European population DMR elicited a greater improvement than sham procedure in both primary endpoints (HbA1c and liver fat content via MRI-PDFF), as well as in secondary measures of insulin sensitivity and body weight. Significant differences in weight loss, HbA1c and hypoglycaemic events were found between the two European and Brazilian populations after unblinding, including in the sham arms. The fact that HbA1c in the sham group was reduced by 3.3 mmol/mol in the European population (consistent with prestudy assumptions), but by 17.5 mmol/mol in the Brazilian population (much greater than prestudy assumptions or even the magnitude of benefit from more potent anti-diabetic drugs) suggest these patients had a more intensive approach in their treatment of diabetes on study enrolment than the European ones, which led to the clinical and statistical differences observed between these populations. This is also true for dieting, since the weight loss was almost double in the Brazilian population as compared with the European population, which may explain the differences in observed treatment effect on MRI-PDFF in the European versus Brazilian populations. Despite the large sham effect size and smaller sample size, Brazilian patients treated with DMR also trended towards evidence of glycaemic efficacy. In Brazil, improvements in HbA1c levels compared with sham-treated patients were not significant in the primary statistical analysis of the cohort but were statistically significant on the mixed-model repeated measures sensitivity analyses.
Overall, we can affirm that in patients with marked hepatic IR (FPG ≥10 mmol/L and who represent up to 65% of patients with T2D),25 DMR demonstrates meaningful improvements in both HbA1c and liver MRI-PDFF compared with the sham procedure. The post-hoc results in the overall population stratified by baseline FPG ≥10 mmol/L or <10 mmol/L are remarkable due to the magnitude of the effect size relative to sham in the high baseline FPG population: difference of –9.8 mmol/mol (3.0%) in HbA1c and –4.5% liver fat content between DMR and sham. This striking difference was also seen in the European population with high baseline FPG, with HbA1c reduction of −13.1 mmol/mol in DMR versus −1.6 mmol/mol in sham (p=0.005) at 24 weeks and MRI-PDFF reductions of −8.0% vs −2.1% (p=0.006) at 12 weeks. Consistent with this, DMR demonstrated statistically significant benefits on markers of IR in the European population, including HOMA-IR and Matsuda Index. Future studies enriching for patients with greater degrees of IR, such as high-baseline FPG patients, may result in a more-pronounced treatment effect of DMR on glycaemic and hepatic parameters.
Unlike for T2D, there are no proven pharmacological therapies available to treat patients with NAFLD. Meanwhile, the downstream consequences of NAFLD are now becoming more apparent with accelerated incidence rates of non-alcoholic steatohepatitis (NASH), cirrhosis, liver transplant and hepatocellular carcinoma being reported in patients with T2D.26 27 We wanted to understand the extent of fatty liver in our patient population at baseline and throughout the study, therefore performed MRI-PDFF on patients at baseline and at week 12. Although the REVITA-2 study did not require a NAFLD diagnosis in patients at baseline, approximately 85% of patients had fatty liver, confirming prior evidence of the growing epidemiological overlap with T2D. Altogether, the prevalence of fatty liver in the overall REVITA-2 study population supports the concept and emphasises further the need for a call for action to implement effective screening programmes and methods to detect presymptomatic stages of NAFLD/NASH and liver fibrosis in patients with T2D. This approach could completely change the paradigm of how the epidemic of NAFLD/NASH is addressed today.28 In REVITA-2, patients with NAFLD (liver MRI-PDFF >5%)29 at baseline in the European cohort or in those patients with FPG ≥10 mmol/L showed a large magnitude and a clinically meaningful reduction in liver fat content at week 12, confirming earlier findings of non-invasive measurements (including reductions in ALT levels through 2 years).24–26 Additionally, the European cohort has statistically significant differences between the DMR and sham arms with regards to the number of patients that had a decline of 30% or more in MRI-PDFF from baseline at week 12. Emerging data over the recent years have suggested that a 30% relative reduction in liver fat content as assessed by MRI-PDFF may be associated with histological improvement in NASH. Most recently, a multicentre study validated this association.30 Liver biopsies were not performed in REVITA-2 as it was not our objective to confirm NASH in our patient population. These data provide insight into a potential therapeutic opportunity for DMR, at least in a selected population, to favourably treat both T2D and NAFLD/NASH in a manner that can modify the natural history of these chronic and progressive diseases.
Results from REVITA-2 confirm that DMR has a favourable safety profile. No UADEs were reported through 24 weeks post treatment, and there were no clinical or laboratory signs of AEs related to malabsorption, anaemia, pancreatitis, biliary complications or infection. Two SAEs were seen in the Brazilian safety population. During the study, a significantly larger number of asymptomatic events of hypoglycaemia were observed in Brazil than in Europe. After unmasking, it became clear that this is most likely due to the overall lower levels of ambient glycaemia in the Brazilian population relative to the European patients and also raises important considerations of the use of DMR in conjunction with antihyperglycaemic agents that have a known risk of causing hypoglycaemia (ie, sulfonylureas). Further assessment of the long-term (48 week) safety and efficacy of DMR is underway.
Limitations of this feasibility study include the relatively small patient population and heterogeneity between European and Brazilian populations. Moreover, the trial was not stratified for baseline characteristics relative to the secondary outcomes; therefore, differences in baseline insulin concentrations, length of time with T2D and number of baseline medications were found, and this may be contributing to differences in outcomes. Next, while full type-1 error was incorporated for the two primary endpoints, we acknowledge that there is a lack of control for false discovery rate in this study for our secondary and exploratory endpoints; therefore, those results should be interpreted with appropriate context. In relation to the differences in statistical and clinical results seen between the European and Brazilian populations, it is important to acknowledge that adherence to previously prescribed medications could not be objectively assessed in this study and race was not collected in the majority of the patient population in Europe. In a follow-up study, it will also be important to confirm the MRI-PDFF results with additional non-invasive tests such as fibroscan to evaluate Revita DMR’s potential to additionally improve liver fibrosis. Lastly, this short-term study concluded at 48 weeks. Follow-up data on the 48 week DMR results are forthcoming, as well as plans for a pivotal study (Revita T2Di; NCT04419779) in T2D insulin-treated patients. This will be important research to confirm the metabolic benefits seen thus far in patients with T2D with or without NAFLD, provide long-term follow-up (including biopsies of the duodenal mucosa to further understand the long-term morphological changes), and provide the opportunity to understand the biological mechanisms likely behind the benefit of DMR on the treatment of these pathological conditions.
In conclusion, DMR is a safe procedure that significantly improved glycaemic control and reduced liver fat content in the European population compared with the sham procedure. In addition, a post-hoc analysis in the overall population showed that patients with high baseline FPG levels (≥10 mmol/L) had significantly greater reductions in HbA1c post-DMR, versus sham.
Acknowledgments
The authors are very grateful to all the patients, families and caregivers that agreed to participate in the REVITA-2 study. They would also like to recognise all the investigators and supporting team members that made this study possible.
Footnotes
Twitter: @IBDdoc
Correction notice: This article has been corrected since it published Online First. The affiliations for Prof Repici have been updated.
Collaborators: Investigators of the REVITA-2 Study: Eduardo Grecco, Ana Teresa Santomauro (ABC Hospital, Sao Paulo, Brazil); Jacques Bergman, Max Nieuwdorp (Academic Medical Center Amsterdam, Amsterdam, Netherlands); John Morris, Russell Drummond, David Carty (Glasgow Royal Infirmary, Glasgow, UK); Jacques Devière, Laurent Crenier (Hopital Erasme, Brussels, Belgium); Eduardo Moura, Cintia Cercato (Hospital Das Clinical, Sao Paulo, Brazil); Alessandro Repici, Andrea Lania, Nazerena Betella (Humanitas Research Hospital, Milano, Italy); David Hopkins, Bu Hayee, Amyn Haji (King's College London, London, UK); Krish Ragunath, Iskander Idris, Carolyn Chee (Queen's Medical Centre, Nottingham, Nottingham, UK); Geltrude Mingrone, Guido Costamagna, Caterina Guidone (Università Cattolica del Sacro Cuore, Rome, Italy); Rehan Haidry, Rachel Batterham (University College Hospital, London, London, UK); Raf Bisschops, Ann Mertens (UZ Leuven, Leuven, Belgium).
Contributors: GM, ACGvB, JD, DH, EM, CC, GC, RH, EG, MGN, GA, AR, BH, AH, AJM, RB and JJGHMB participated in data collection and interpretation. AJS, DLB, MDC and NSS participated in data interpretation. HR, JCL-T, KW and VB contributed to the study design and participated in data analysis and interpretation. All authors reviewed the manuscript critically for important intellectual content and approved the final version of the manuscript to be submitted.
Funding: This study was funded by Fractyl.
Competing interests: GM has received funding/grant support from Novo Nordisk, Fractyl Laboratories, Metacure, Keyron, and honorarium for consultancy from Johnson & Johnson, Novo Nordisk, and Fractyl Laboratories. JD has received research support from Fractyl Laboratories Inc for IRB-approved studies. DH has received honorarium for consultancy and/or speaker fees from Novo Nordisk, Sanofi, Astra Zeneca, Roche, Sunovion, and Fractyl Laboratories. EM has received honorarium for consultancy from Olympus do Brasil and Boston Scientific. CC has received funding/grant support from Novo Nordisk and honorarium for consultancy from Novo Nordisk and Eurofarma. DLB reports that he serves or has served on advisory boards for Cardax, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, Level Ex, Medscape Cardiology, PhaseBio, PLx Pharma and Regado Biosciences. He is or was a member of the board of directors for Boston VA Research Institute, Society of Cardiovascular Patient Care, and TobeSoft. He is or was chair for the American Heart Association Quality Oversight Committee, and is or was on data monitoring committees for Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Contego Medical (chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), and the Population Health Research Institute. He reports honoraria from the American College of Cardiology (senior associate editor, Clinical Trials and News, ACC.org; vice-chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (editor in chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (editor in chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (guest editor and associate editor), K2P (cochair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national coleader, funded by Bayer), Slack Publications (chief medical editor, Cardiology Today–Intervention), Society of Cardiovascular Patient Care (secretary/treasurer), WebMD (CME steering committees). He reports other relationships with Clinical Cardiology (deputy editor), NCDR-ACTION Registry Steering Committee (chair), and VA CART Research and Publications Committee (chair). He reports research funding from Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Idorsia, Ironwood, Ischemix, Lexicon, Lilly, Medtronic, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi Aventis, Synaptic, and The Medicines Company. He reports royalties from Elsevier (editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease). He is or was a site coinvestigator for Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), and Svelte. He is or was a trustee for the American College of Cardiology. He reports unfunded research for FlowCo, Merck, Novo Nordisk, and Takeda. HR, JCL-T, KW, and VB are full-time employees of Fractyl Laboratories and may hold Fractyl stock and/or stock options. GC has received research grant support from Boston Scientific and Apollo and is on the advisory board for Cook Medical, Olympus, and Ethicon. RH has received funding/grant support/honorarium for consultancy from Cook Endoscopy, Pentax Europe, Medtronic, C2 Therapeutics, and Fractyl Laboratories to support research infrastructure. EG has received consulting fees from Fractyl Laboratories Inc, Apollo Endosurgery, and Medtronic. MGN has received honorarium for consultancy from Fractyl Laboratories, GI Windows, GI Dynamics, Apollo, and for speaker bureaus for Ethicon, Medtronic, and Olympus. GPA has been a consultant and advisory board member for Agios Pharmaceuticals, Amryt Pharma, AstraZeneca, GlaxoSmithKline and Pfizer. AR has received grant support from Norgine, Fujifilm, Boston Scientific and ERBE, and served as a member of advisory boards for Medtronic, Boston Scientific, EndoStart, EndoKey, Alfasigma and FujiFilm. AJM has received honorarium for consultancy from Fractyl Laboratories and Cook Medical. ACGvB, BH, RB, AH, MDC and NSS have nothing to disclose. AJS has been a consultant for Conatus, Gilead, Elsevier, Echosens, Malinckrodt, Immuron, Intercept, Pfizer, Salix, Uptodate, Boehringer, Ingelhiem, Novartis, Nimbus, Nitto Denko, Hemoshear, Lilly, Novo Nordisk, Fractyl Laboratories, Allergan, Chemomab, Affimmune, Teva, Ardelyx, Terns, ENYO, Birdrock, Albireo, Sanofi, Jannsen, Takeda, Zydus, BASF, Amra, Perspectum, OWL, Poxel, Servier, Second Genome, General Electric, and 89Bio. He is a stock/shareholder at Exhalenz Stock, Akarna, Durect, Indalo and Tiziana. He has received grant/research support from Novartis, Merck, Galectin, Bristol Myers, Merck, Sequana, Boehringer Ingelheim, Echosense, Salix, Malinckrodt, Cumberland, and Gilead.JJGHMB has received research support from Fractyl Laboratories for IRB-based studies and has received a consultancy fee for a single advisory board meeting for Fractyl Laboratories in September 2019.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Investigators of the REVITA-2 Study:
Eduardo Grecco, Ana Teresa Santomauro, Jacques Bergman, Max Nieuwdorp, John Morris, Russell Drummond, David Carty, Jacques Devière, Laurent Crenier, Eduardo Moura, Cintia Cercato, Alessandro Repici, Andrea Lania, Nazerena Betella, David Hopkins, Bu Hayee, Amyn Haji, Krish Ragunath, Iskander Idris, Carolyn Chee, Geltrude Mingrone, Guido Costamagna, Caterina Guidone, Rehan Haidry, Rachel Batterham, Raf Bisschops, and Ann Mertens
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Institutional review boards or ethics committees at each participating institution approved the protocol and informed consent documents prior to enrolment. All eligible patients provided written informed consent at screening. The trial was conducted in accord with the Declaration of Helsinki and International Conference on Harmonisation.
References
- 1. Hu FB. Globalization of diabetes: the role of diet, lifestyle, and genes. Diabetes Care 2011;34:1249–57. 10.2337/dc11-0442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. The Lancet . The diabetes pandemic. The Lancet 2011;378:99. 10.1016/S0140-6736(11)61068-4 [DOI] [PubMed] [Google Scholar]
- 3. Samuel VT, Shulman GI. Nonalcoholic fatty liver disease as a nexus of metabolic and hepatic diseases. Cell Metab 2018;27:22–41. 10.1016/j.cmet.2017.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med 2017;23:804–14. 10.1038/nm.4350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. de Pablos-Velasco P, Parhofer KG, Bradley C, et al. Current level of glycaemic control and its associated factors in patients with type 2 diabetes across Europe: data from the Panorama study. Clin Endocrinol 2014;80:47–56. 10.1111/cen.12119 [DOI] [PubMed] [Google Scholar]
- 6. Juarez DT, Ma C, Kumasaka A, et al. Failure to reach target glycated A1c levels among patients with diabetes who are adherent to their antidiabetic medication. Popul Health Manag 2014;17:218–23. 10.1089/pop.2013.0099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European association for the study of diabetes (EASD). Diabetes Care 2018;41:2669–701. 10.2337/dci18-0033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Resnick HE, Foster GL, Bardsley J, et al. Achievement of American diabetes association clinical practice recommendations among U.S. adults with diabetes, 1999-2002: the National health and nutrition examination survey. Diabetes Care 2006;29:531–7. 10.2337/diacare.29.03.06.dc05-1254 [DOI] [PubMed] [Google Scholar]
- 9. Cummings DE. Metabolic surgery for type 2 diabetes. Nat Med 2012;18:656–8. 10.1038/nm.2773 [DOI] [PubMed] [Google Scholar]
- 10. Dirksen C, Hansen DL, Madsbad S, et al. Postprandial diabetic glucose tolerance is normalized by gastric bypass feeding as opposed to gastric feeding and is associated with exaggerated GLP-1 secretion: a case report. Diabetes Care 2010;33:375–7. 10.2337/dc09-1374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jacobsen SH, Olesen SC, Dirksen C, et al. Changes in gastrointestinal hormone responses, insulin sensitivity, and beta-cell function within 2 weeks after gastric bypass in non-diabetic subjects. Obes Surg 2012;22:1084–96. 10.1007/s11695-012-0621-4 [DOI] [PubMed] [Google Scholar]
- 12. Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Diabetes Care 2016;39:861–77. 10.2337/dc16-0236 [DOI] [PubMed] [Google Scholar]
- 13. Funk LM, Jolles S, Fischer LE, et al. Patient and referring practitioner characteristics associated with the likelihood of undergoing bariatric surgery: a systematic review. JAMA Surg 2015;150:999–1005. 10.1001/jamasurg.2015.1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Afonso BB, Rosenthal R, Li KM, et al. Perceived barriers to bariatric surgery among morbidly obese patients. Surg Obes Relat Dis 2010;6:16–21. 10.1016/j.soard.2009.07.006 [DOI] [PubMed] [Google Scholar]
- 15. de Moura EGH, Ponte-Neto AM, Tsakmaki A, et al. Histologic assessment of the intestinal wall following duodenal mucosal resurfacing (DMR): a new procedure for the treatment of insulin-resistant metabolic disease. Endosc Int Open 2019;7:E685–90. 10.1055/a-0862-0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rajagopalan H, Cherrington AD, Thompson CC, et al. Endoscopic duodenal mucosal resurfacing for the treatment of type 2 diabetes: 6-month interim analysis from the first-in-human proof-of-concept study. Diabetes Care 2016;39:2254–61. 10.2337/dc16-0383 [DOI] [PubMed] [Google Scholar]
- 17. Haidry RJ, van Baar AC, Galvao Neto MP, et al. Duodenal mucosal resurfacing: proof-of-concept, procedural development, and initial implementation in the clinical setting. Gastrointest Endosc 2019;90:673–81. 10.1016/j.gie.2019.03.024 [DOI] [PubMed] [Google Scholar]
- 18. van Baar ACG, Holleman F, Crenier L, et al. Endoscopic duodenal mucosal resurfacing for the treatment of type 2 diabetes mellitus: one year results from the first international, open-label, prospective, multicentre study. Gut 2020;69:295–303. 10.1136/gutjnl-2019-318349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO) . EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Diabetologia 2016;59:1121–40. 10.1007/s00125-016-3902-y [DOI] [PubMed] [Google Scholar]
- 20. American Diabetes Association . Standards of medical care in diabetes--2008. Diabetes Care 2008;31:S12–54. 10.2337/dc08-S012 [DOI] [PubMed] [Google Scholar]
- 21. HOCHBERG Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika 1988;75:800–2. 10.1093/biomet/75.4.800 [DOI] [Google Scholar]
- 22. Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- 23. Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 1999;22:1462–70. 10.2337/diacare.22.9.1462 [DOI] [PubMed] [Google Scholar]
- 24. Selimoglu H, Duran C, Kiyici S, et al. Comparison of composite whole body insulin sensitivity index derived from mixed meal test and oral glucose tolerance test in insulin resistant obese subjects. Endocrine 2009;36:299–304. 10.1007/s12020-009-9213-z [DOI] [PubMed] [Google Scholar]
- 25. Colagiuri S, Cull CA, Holman RR, et al. Are lower fasting plasma glucose levels at diagnosis of type 2 diabetes associated with improved outcomes?: U.K. prospective diabetes study 61. Diabetes Care 2002;25:1410–7. 10.2337/diacare.25.8.1410 [DOI] [PubMed] [Google Scholar]
- 26. Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73–84. 10.1002/hep.28431 [DOI] [PubMed] [Google Scholar]
- 27. Oni ET, Agatston AS, Blaha MJ, et al. A systematic review: burden and severity of subclinical cardiovascular disease among those with nonalcoholic fatty liver; should we care? Atherosclerosis 2013;230:258–67. 10.1016/j.atherosclerosis.2013.07.052 [DOI] [PubMed] [Google Scholar]
- 28. Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: a systematic review and meta-analysis. J Hepatol 2019;71:793–801. 10.1016/j.jhep.2019.06.021 [DOI] [PubMed] [Google Scholar]
- 29. European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO) . EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–402. 10.1016/j.jhep.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 30. Loomba R, Lim JK, Patton H, et al. AGA clinical practice update on screening and surveillance for hepatocellular carcinoma in patients with nonalcoholic fatty liver disease: expert review. Gastroenterology 2020;158:1822–30. 10.1053/j.gastro.2019.12.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
gutjnl-2020-323608supp001.pdf (2.4MB, pdf)
Data Availability Statement
Data are available upon reasonable request.