Abstract
Introduction
Routine ultrasound may be used in abortion services to determine gestational age and confirm an intrauterine pregnancy. However, ultrasound adds complexity to care and results may be inconclusive, delaying abortion. We sought to determine the rate of ectopic pregnancy and the utility of routine ultrasound in its detection, in a community abortion service.
Methods
Retrospective case record review of women requesting abortion over a 5-year period (2015–2019) with an outcome of ectopic pregnancy or pregnancy of unknown location (PUL) at a service (Edinburgh, UK) conducting routine ultrasound on all women. Records were searched for symptoms at presentation, development of symptoms during clinical care, significant risk factors and routine ultrasound findings.
Results
Only 29/11 381 women (0.25%, 95% CI 0.18%, 0.33%) had an ectopic pregnancy or PUL (tubal=18, caesarean scar=1, heterotopic=1, PUL=9). Eleven (38%) cases had either symptoms at presentation (n=8) and/or significant risk factors for ectopic pregnancy (n=4). A further 12 women developed symptoms during their clinical care. Of the remaining six, three were PUL treated with methotrexate and three were ectopic (salpingectomy=2, methotrexate=1). In three cases, the baseline ultrasound indicated a probable early intrauterine pregnancy.
Conclusions
Ectopic pregnancies are uncommon among women presenting for abortion. The value of routine ultrasound in excluding ectopic pregnancy in symptom-free women without significant risk factors is questionable as it may aid detection of some cases but may provide false reassurance that a pregnancy is intrauterine.
Keywords: abortion, induced, mifepristone, abortion, therapeutic, family planning services, patient safety
Key messages.
Ectopic pregnancy is uncommon among women presenting for abortion.
Ultrasound is indicated for women with symptoms or significant risk factors for ectopic pregnancy who request abortion.
While routine ultrasound may identify a small number of low-risk women with ectopic pregnancies, it complicates abortion care and may falsely indicate an intrauterine pregnancy.
Introduction
Routine ultrasound for all women requesting an abortion is used habitually by many UK abortion services to confirm an intrauterine pregnancy (IUP), and exclude ectopic pregnancy, despite guidance from the Royal College of Obstetricians and Gynaecologists (RCOG) that routine ultrasound is not necessary.1 Ultrasound is not required for assessing gestational age as it can be done clinically to a reasonable accuracy and small discrepancies do not affect management.1 A review investigating the outcomes of no-scan protocols outside the UK suggested that the risk of ectopic pregnancy is low and that routine ultrasound is not always reliable for identifying ectopic pregnancies.2 Additionally, for women presenting at under 6 weeks’ gestation it may not be possible to visualise a yolk sac, which is widely considered to be the first definitive ultrasound sign of an IUP,3 4 resulting in delays to treatment until IUP is confirmed. Delaying treatment for these women can cause unnecessary investigations and distress. Heller and Cameron3 conducted a retrospective review of a cohort of over 1000 women which suggested that medical abortion before evidence of a yolk sac, but with ultrasound features of a probable IUP (eccentric sac and decidual reaction), is effective and appropriate if there are no symptoms (pain and/or bleeding), or significant risk factors for ectopic pregnancy. A case note review of over 2600 women reported that medical abortion before definite ultrasound evidence of an IUP is as effective as at later gestations, and with a lower rate of incomplete abortion.5 Both these studies were evaluated in a systematic review6 conducted as part of the 2019 National Institute of Health and Care Excellence (NICE) guideline7 on abortion care which recommended that medical or surgical abortion before ultrasound evidence of an IUP was not associated with significantly different rates of missed ectopic pregnancy.
Approximately 11 per 1000 pregnancies are ectopic, with about 11 000 ectopic pregnancies each year in the UK.8 9 However, there is evidence that the rate of ectopic pregnancy in the population of women presenting for abortion may be lower. In a study of over 200 000 women who had received medical abortion at up to 9 weeks’ gestation from Planned Parenthood Health Centres in the United States between 2009 and 2010, there were seven ectopics per 100 000 pregnancies.10 In early pregnancy, as well as ectopic pregnancies being diagnosed, pregnancies of unknown location (PUL) may also be diagnosed, where a pregnancy cannot be positively identified on scan either within the uterus or outside. These are often later diagnosed as either an IUP or ectopic; however, they are sometimes managed as ‘presumed ectopics’ and treated, usually with medical methods, such as methotrexate.
While ultrasound is a key investigation in women with symptoms or significant risk factors, the utility of routine ultrasound for detecting ectopic pregnancy in asymptomatic women presenting for abortion without risk factors remains unclear. Furthermore, during the current pandemic with COVID-19, RCOG guidelines for care of women requesting abortion have been adapted to minimise face-to-face contact, with a shift towards telemedicine.11 These guidelines support not using ultrasound for women who are in early pregnancy, certain of their last menstrual period and who do not have symptoms or significant risk factors for an ectopic including unilateral abdominal pain, intrauterine device, history of tubal damage, or prior ectopic pregnancy.11
The Chalmers Centre is a National Health Service (NHS) Community Sexual and Reproductive Health service which provides abortion services to Edinburgh and the surrounding region with over 2400 women presenting each year.12 Prior to COVID-19, routine ultrasound for gestational assessment, performed by a team of ultrasonographers, was standard practice.3
We aimed to determine the rate of ectopic pregnancies (including PUL managed as ectopic) among women presenting for abortion; how they were detected; the utility of routine ultrasound in their detection; and so determine the safety of not doing routine ultrasound. We therefore undertook a retrospective review of women who presented for abortion to our service using this routine ultrasound model whose outcome of the pregnancy was a confirmed ectopic pregnancy or PUL managed as ectopic pregnancy; whether they had symptoms or risk factors at baseline for ectopic; and the findings of the routine ultrasound. In addition, we aimed to determine if symptoms suspicious of an ectopic developed during the course of their care.
Methods
This study was a retrospective review of women presenting to the Chalmers abortion service with a subsequent confirmed ectopic or PUL over a 5-year period (January 2015–December 2019 inclusive). The usual flow of clinical care at the time of the study is detailed in Box 1. The Chalmers clinic database was searched for an outcome of ectopic pregnancy or PUL over the study period among all women presenting for abortion. The clinical records of cases were scrutinised for presence of symptoms (unilateral pain and/or bleeding) at baseline and if they developed later during the care journey, significant risk factors (as per RCOG guidelines11) and ultrasound findings at presentation and management. TRAK, the regional hospital electronic database, was also searched to obtain further details of management of the ectopic pregnancy. All women with ectopic pregnancies in the region are referred to and managed by the NHS hospital services in the region that use TRAK.
Box 1. The usual flow of clinical care (pre COVID-19 guidelines).
Women self-refer to the abortion service or are referred by their general practitioner (GP) as soon as they have a positive pregnancy test result. There is no need to wait until a certain gestation before referral is accepted.
All women attend an in-person clinic appointment at which they undergo a transabdominal ultrasound scan performed by an ultrasonographer at the centre, unless they have had a previous ultrasound scan elsewhere in the health service during this pregnancy. A transvaginal scan is done if the views are suboptimal or if the pregnancy is not visualised by the transabdominal scan.
If an intrauterine pregnancy is identified* and the criteria of the 1967 Abortion Act are met, women are offered either medical or surgical abortion as per their preference. Medical abortion could be in a clinical setting or at home depending on gestation, social circumstances and the patient’s request.
If the results are inconclusive (eg, empty uterus) then serial serum human chorionic gonadotropin (hCG) measurements are obtained. If the hCG level rises appropriately (>66% over 48 hours), the woman is invited for a repeat scan in 7–10 days. An ectopic pregnancy is suspected if there is a suboptimal rise or plateau, and the woman is referred to the regional early pregnancy unit (EPU) for further investigation, monitoring and treatment.
If an ectopic pregnancy is identified on the scan, women are referred to the regional EPU, which will then arrange treatment depending on guidance at the time (ie, salpingectomy, methotrexate or, more recently, conservative management).
*Includes probable early intrauterine pregnancy (ie, eccentrically placed sac of >3 mm with decidual reaction).
All women with symptoms indicative of an ectopic pregnancy were referred to the early pregnancy unit (EPU) at the regional hospital for further management including conservative (serial human chorionic gonadotropin (hCG) monitoring), medical (methotrexate) or surgical management.
Data on cases were entered into Microsoft Excel and analysed using descriptive statistics.
Ethical approval was not required. The project was approved by the NHS Lothian Sexual and Reproductive Health Quality Improvement Team. Patients and the public were not involved in the study design. The data had patient identifiable information removed and conformed to the Caldicott guidelines.13
Results
Over the study period, 11 381 women presented to the service requesting an abortion. Of these, 29 cases had an ultimate diagnosis of confirmed ectopic pregnancy or PUL, giving a rate of 0.25% (95% CI 0.18%, 0.33%). The women were aged 16 to 40 years with a mean age of 27.9 years (95% CI 25.8%, 30.0%).
Symptoms that would raise suspicion of an ectopic pregnancy (unilateral abdominal pain and/or bleeding) at initial presentation were present in 8/29 women (28%). Four women (including one woman who was one of the eight symptomatic cases) had significant risk factors for ectopic pregnancy, namely previous ectopic pregnancy (n=2), pelvic inflammatory disease (n=1) and an intrauterine device (IUD) in situ (n=1).
Twelve women who were asymptomatic at baseline went on to develop symptoms suspicious for ectopic pregnancy during their clinical care, prior to their diagnosis and treatment. This group included two women who presented to emergency services with severe pain and were subsequently diagnosed with a ruptured ectopic (one was a heterotopic pregnancy confirmed on histology). For both these women, their baseline ultrasound indicated a probable early IUP (eccentrically placed intrauterine sac with decidual reaction). Six women did not have symptoms at baseline visit or subsequent visits during their care. This group included two women who were positively identified as ectopic pregnancy on baseline ultrasound, one who had a caesarean scar ectopic originally thought to be IUP (eccentrically placed intrauterine sac) and three women with PUL.
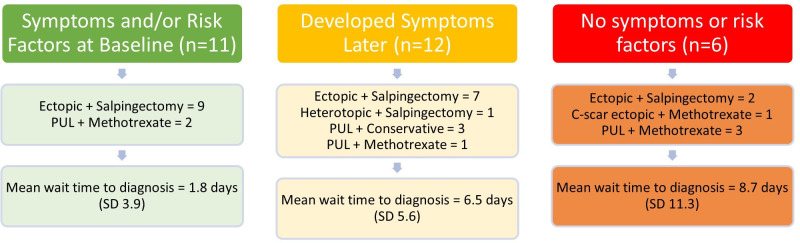
Figure 1 categorises the women based on whether they had symptoms of ectopic pregnancy, significant risk factors or neither; the treatment they received; and the time from presentation to diagnosis of ectopic pregnancy or PUL. Table 1 shows the baseline ultrasound findings and subsequent diagnosis and treatment. Table 2 shows the gestational age of the pregnancies at point of diagnosis, if documented.
Figure 1.
Cases categorised by symptoms and risk factors at presentation. C, caesarean; PUL, pregnancy of unknown location.
Table 1.
Ultrasound findings and subsequent diagnosis
| Ultrasound finding at baseline | Women (n) | Final diagnosis | Treatment |
| Empty uterus only | 10 | Ectopic=6 PUL=4 |
Salpingectomy=6 Methotrexate=3 Conservative=1 |
| Empty uterus and adnexal lesion | 13 | Ectopic=10 PUL=3 |
Salpingectomy=10 Methotrexate=1 Conservative=2 |
| Fluid-filled intrauterine area | 3 | Ectopic=1 PUL=2 |
Salpingectomy=1 Methotrexate=2 |
| Intrauterine sac without decidual reaction | 1 | C-scar ectopic=1* | Methotrexate=1 |
| Intrauterine sac with decidual reaction | 2 | Heterotopic=1* Ectopic=1* |
Salpingectomy=2 |
*Initially considered and managed as an intrauterine pregnancy.
C, caesarean; PUL, pregnancy of unknown location.
Table 2.
Gestational age at diagnosis of ectopic pregnancy
| Estimated gestational age (weeks) | n |
| ND | 11 |
| ≤6 | 13 |
| ≤7 | 3 |
| ≤8 | 2 |
ND, not documented.
Discussion
Main findings
This study showed that the rate of ectopic pregnancies and PUL in over 11 000 women presenting to the abortion service is low and was less than the general population rate reported by other studies.8 9 This finding aligns with studies that suggest a lower rate of ectopic pregnancies in women presenting for abortions.3 10 14 Ultrasound was potentially useful in six (0.05%) cases for identifying ectopic pregnancies (or PUL), where the woman did not have symptoms or risk factors.
These six women could potentially have been ‘missed’; however, these cases require further scrutiny. Of these six women, three were diagnosed as PUL and treated with methotrexate and none of their ultrasound scans showed features suspicious of ectopic pregnancy. Two women had ultrasound scans that positively identified an ectopic pregnancy at their first visit and were referred for salpingectomy the same day – it is possible they would have gone on to develop symptoms that would have alerted them to the ectopic pregnancy had they not been scanned. The final woman was diagnosed initially with an IUP that later transpired to be a caesarean scar ectopic – this was detected on a later ultrasound when she presented for IUD insertion and was found to have a positive low-sensitivity pregnancy test. Caesarean scar pregnancies are rare (incidence 1.5/10 000 of all pregnancies),15 their natural progression is not well understood and there are no validated diagnostic criteria for them, although they can have severe outcomes. The other two women who were considered to have an IUP on baseline scan but were subsequently identified as an ectopic and heterotopic, respectively, developed symptoms following abortion treatment, and so the initial scan was falsely reassuring.
There is no evidence that receiving medical abortion treatment causes an adverse effect on an ectopic pregnancy. The risk of proceeding to medical abortion without scan is that of a potentially delayed or missed diagnosis of ectopic pregnancy. When abortions are done without ultrasound, therefore, women must be given clear advice on when to seek help, for example, with ongoing pain or persistently positive pregnancy tests.11
Women with ectopic pregnancy are increasingly being offered conservative management rather than medical or surgical intervention, as long as the woman is clinically well, the ectopic pregnancy is within certain parameters on ultrasound, and hCG levels are trending downwards.16 Given that many of the women in this cohort were clinically stable at baseline, including the six women without risk factors or symptoms, they may have been offered conservative management within current ectopic guidelines and so we cannot know if they have been disadvantaged by not receiving an initial ultrasound.
In response to the 2020 novel coronavirus (COVID-19) outbreak, specific guidance was issued encouraging the management of abortion care via telemedicine where possible and discouraging routine ultrasound. Instead, ultrasound was offered when women reported symptoms or risk factors for ectopic pregnancy and clear ‘safety-net’ information was provided to women who had not been scanned to make contact if they developed signs or symptoms of ectopic pregnancy following their abortion care treatment.11 While the cohort of patients investigated in this study were managed prior to the introduction of the COVID-19 guidelines, the findings support the guidelines by presenting the low rate of ectopic pregnancy and promoting focused ultrasound referrals (based on symptoms and risk factors). Of the women in our cohort, just over one-third with diagnosed ectopic pregnancy would have been invited for ultrasound scan based on symptoms and risk factors. Two-thirds of the remainder developed symptoms of ectopic pregnancy during their clinical course, and while they would not have received an ultrasound at baseline under COVID-19 guidance, they would have received safety-net information that would prompt them to seek further care and subsequent investigation and timely diagnosis.
Furthermore, since the introduction of telemedicine without routine ultrasound, women have been receiving abortions earlier (almost 50% of abortions were performed under 7 weeks’ gestation in England and Wales from January to June 2020, compared with almost 40% for the same period in 2019).17 Consequently, some women with ectopic pregnancies may be detected and treated earlier than in previous care pathways. For example, alongside increased index of suspicion, women may present with unexpectedly little bleeding post-misoprostol, or with developing symptoms of an ectopic pregnancy that are addressed earlier than they would have been previously, especially if they formerly had to wait a week or more for a repeat ultrasound after an inconclusive baseline ultrasound.
Strengths and limitations
The strength of this study is that the cohort of women having abortions is large and that all outcomes could be verified from the regional electronic case record system. Of course, given the study’s retrospective design, it is limited by the quality of case notes. All ultrasound scans in the service are conducted by ultrasonographers who also work in the regional EPU. While this is a strength in terms the quality of the ultrasound scan performed in all cases, we also recognise that this may mean that the findings could possibly differ in those of services where ultrasound is not conducted to the same level. As this is not a randomised controlled trial, it is not possible to determine whether delayed diagnosis of ectopic pregnancy would be greater in the routine scan or no routine scan group.
What this study adds to the existing literature
Our study findings continue to question the utility of routine ultrasound for women requesting abortion as, while it may have helped identify three ectopic pregnancies and three PUL, it was unclear if it would have changed the ultimate management of those cases. In addition, three cases overall (one ectopic, one caesarean scar and one heterotopic) gave rise to false reassurance that an IUP was present. While ultrasound is important in cases at high-risk of ectopic pregnancy and recommended by the RCOG,11 routine ultrasound adds burden and complexity to abortion care. It limits access by increasing appointment times and cost, while inconclusive results trigger delays and further investigations. Moreover, scans (full bladder or vaginal route) can be uncomfortable and may highlight incidental findings such as physiological cysts or fibroids that may lead to unnecessary additional investigations, the impact of which were not investigated in this study.
It is hoped that the national data gathered on the management of women requesting abortion during COVID-19 without routine ultrasound according to current RCOG guidance will inform future guidelines in this area.11
Conclusions
Ectopic pregnancies are uncommon among women presenting for abortion and the value of routine ultrasound to exclude ectopic pregnancy is questionable as it may aid detection of some cases but may also provide false reassurance that a pregnancy is intrauterine.
Acknowledgments
The authors thank Anne Johnstone, Clinical Research Nurse, Chalmers Centre for her assistance with ensuring the accuracy of the data collected.
Footnotes
Twitter: @doctorjjrw
Contributors: CID collected and analysed the data. JJR-W analysed the data. STC designed the study and analysed the data. All authors contributed to the writing of the manuscript.
Funding: The study was conducted by staff at the MRC Centre for Reproductive Health, which is supported by grant MR/N022556/1.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Due to the small numbers of participants in the study and the potential for identification, no further data are available.
Ethics statements
Patient consent for publication
Not required.
References
- 1. Royal College of Obstetricians & Gynaecologists . The care of women requesting induced abortion (Evidence-based Clinical Guideline No. 7). Available: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/the-care-of-women-requesting-induced-abortion/ [Accessed 10 Mar 2020].
- 2. Kaneshiro B, Edelman A, Sneeringer RK, et al. Expanding medical abortion: can medical abortion be effectively provided without the routine use of ultrasound? Contraception 2011;83:194–201. 10.1016/j.contraception.2010.07.023 [DOI] [PubMed] [Google Scholar]
- 3. Heller R, Cameron S. Termination of pregnancy at very early gestation without visible yolk sac on ultrasound. J Fam Plann Reprod Health Care 2015;41:90–5. 10.1136/jfprhc-2014-100924 [DOI] [PubMed] [Google Scholar]
- 4. Bottomley C, Van Belle V, Mukri F, et al. The optimal timing of an ultrasound scan to assess the location and viability of an early pregnancy. Hum Reprod 2009;24:1811–7. 10.1093/humrep/dep084 [DOI] [PubMed] [Google Scholar]
- 5. Bizjak I, Fiala C, Berggren L, et al. Efficacy and safety of very early medical termination of pregnancy: a cohort study. BJOG 2017;124:1993–9. 10.1111/1471-0528.14904 [DOI] [PubMed] [Google Scholar]
- 6. Schmidt-Hansen M, Cameron S, Lord J, et al. Initiation of abortion before there is definitive ultrasound evidence of intrauterine pregnancy: a systematic review with meta-analyses. Acta Obstet Gynecol Scand 2020;99:451–8. 10.1111/aogs.13797 [DOI] [PubMed] [Google Scholar]
- 7. National Institute for Health and Care Excellence (NICE) . Abortion care. NICE guideline [NG140], 2019. Available: https://www.nice.org.uk/guidance/ng140 [Accessed 3 Nov 2020].
- 8. Royal College of Obstetricians & Gynaecologists . Diagnosis and management of ectopic pregnancy. Available: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg21/ [Accessed 31 Aug 2019].
- 9. Tay JI, Moore J, Walker JJ. Ectopic pregnancy. West J Med 2000;173:131–4. 10.1136/ewjm.173.2.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cleland K, Creinin MD, Nucatola D, et al. Significant adverse events and outcomes after medical abortion. Obstet Gynecol 2013;121:166–71. 10.1097/AOG.0b013e3182755763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Royal College of Obstetricians & Gynaecologists . Coronavirus (COVID-19) infection and abortion care. Available: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-abortion/ [Accessed 15 Jul 2020].
- 12. Smith JL, Cameron S. Current barriers, facilitators and future improvements to advance quality of abortion care: views of women. BMJ Sex Reprod Health 2019;45:207–12. 10.1136/bmjsrh-2018-200264 [DOI] [PubMed] [Google Scholar]
- 13. Department of Health . Caldicott Priniciples. Information governance toolkit. Available: https://www.igt.hscic.gov.uk/Caldicott2Principles.aspx [Accessed 10 Mar 2020].
- 14. Shannon C, Brothers LP, Philip NM, et al. Ectopic pregnancy and medical abortion. Obstet Gynecol 2004;104:161–7. 10.1097/01.AOG.0000130839.61098.12 [DOI] [PubMed] [Google Scholar]
- 15. Harb HM, Knight M, Bottomley C, et al. Caesarean scar pregnancy in the UK: a national cohort study. BJOG 2018;125:1663–70. 10.1111/1471-0528.15255 [DOI] [PubMed] [Google Scholar]
- 16. National Institute for Health and Care Excellence (NICE) . Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guideline [NG126], 2019. Available: https://www.nice.org.uk/guidance/ng126/chapter/Recommendations#expectant-management-2 [Accessed 17 Sep 2020]. [PubMed]
- 17. GOV.UK . Abortion statistics for England and Wales during the COVID-19 pandemic, 2020. Available: https://www.gov.uk/government/publications/abortion-statistics-during-the-coronavirus-pandemic-january-to-june-2020/abortion-statistics-for-england-and-wales-during-the-covid-19-pandemic
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the small numbers of participants in the study and the potential for identification, no further data are available.