Abstract
Rationale
Adaptive servo ventilation (ASV) is contraindicated in patients with systolic heart failure (HF) who have a left ventricular ejection fraction (LVEF) below 45% and predominant central sleep apnoea (CSA). However, the effects of ASV in other HF subgroups have not been clearly defined.
Objective
The European, multicentre, prospective, observational cohort trial, FACE, evaluated the effects of ASV therapy on morbidity and mortality in patients with HF with sleep-disordered breathing (SDB); 3-month outcomes in patient subgroups defined using latent class analysis (LCA) are presented.
Methods
Consecutive patients with HF with predominant CSA (±obstructive sleep apnoea) indicated for ASV were included from 2009 to 2018; the non-ASV group included patients who refused/were noncompliant with ASV. The primary endpoint was time to composite first event (all-cause death, lifesaving cardiovascular intervention or unplanned hospitalisation for worsening of chronic HF).
Measurements and main results
Baseline assessments were performed in 503 patients, and 482 underwent 3-month follow-up. LCA identified six discrete patient clusters characterised by variations in LVEF, SDB type, age, comorbidities and ASV acceptance. The 3- month rate of primary outcome events was significantly higher in cluster 1 patients (predominantly men, low LVEF, severe HF, CSA; 13.9% vs 1.5%–5% in other clusters, p<0.01).
Conclusion
For the first time, our data identified homogeneous patient clusters representing clinically relevant subgroups relating to SDB management in patients with HF with different ASV usage, each with a different prognosis. This may improve patient phenotyping in clinical practice and allow individualisation of therapy.
Keywords: sleep apnoea
Key messages.
What is the key question?
How can different subgroups of heart failure patients with sleep-disordered breathing be described in relation to their clinical characteristics and the impact of adaptive servo ventilation therapy?
What is the bottom line?
Heart failure patients with sleep apnoea are a highly heterogeneous group that can be classified into six clinically relevant subgroups, each of which has a different prognosis.
Why read on?
Grouping patients with heart failure and sleep apnoea into subgroups can assist in clinical decision-making and inform appropriate therapy choices. The patient groups defined in this study could help individualise therapeutic strategies targeted at reducing morbidity and mortality in patients with heart failure and sleep-disordered breathing.
Introduction
Heart failure (HF) is an important public health problem due to the significant morbidity, mortality and healthcare expenditure associated with the disease.1 2 However, ‘HF’ covers a variety of different phenotypes or subtypes. Most commonly, HF is divided into categories based on the left ventricular ejection fraction (LVEF): HF with reduced ejection fraction (HFrEF) when LVEF is <40%, HF with mid-range ejection fraction (HFmrEF) when LVEF is 40%–49%, and HF with preserved ejection fraction (HFpEF) when LVEF is ≥50%0.3
Most currently available pharmacological therapies for HF have been studied primarily in HFrEF and are recommended in this patient subset.3 However, patients with HFpEF have a mortality rate similar to that in those with LVEF ≤50%,4 and there are currently no evidence-based treatments that have been shown to improve mortality in HFpEF,5 highlighting the need for new and effective therapies in these patients.
Sleep-disordered breathing (SDB), including obstructive and central sleep apnoea (OSA and CSA) is a common HF comorbidity, occurring in up to 70% of patients.6–8 The presence of OSA and/or CSA has a negative impact on prognosis in patients with HF.9 Use of positive airway pressure (PAP) therapy to treat SDB in patients with HF has been reported to have a number of beneficial effects on intermediate endpoints and surrogate markers,10–14 and some mortality benefits have been reported.15 However, large randomised, controlled trials have failed to document any significant benefit of PAP therapy on hard clinical endpoints.16–19 Nevertheless, some HF patient subgroup might benefit from the use of PAP, as suggested by a trend for improved outcomes in patients with HFpEF from the CAT-HF study.17 Therefore, rather than taking a ‘one size fits all’ approach to the management of patients with HF and SDB, it may be more useful to identify specific subgroups (ie, different patient phenotypes) and prescribe therapy on a more targeted basis.
The FACE trial used real-world data to evaluate the effect of PAP therapy with adaptive servo ventilation (ASV) on morbidity and mortality in patients with HFrEF, HFmrEF or HFpEF and central SDB or coexisting CSA/OSA. This paper presents 3-month data in patient subgroups defined using latent class analysis (LCA).
Methods
Study design
The FACE study is a European, multicentre, prospective observational cohort trial (NCT01831128).20 The protocol was approved by the relevant ethics committee(s) at each centre (See online supplemental file 1). The trial was conducted in accordance with local laws/regulations, International Conference on Harmonisation-Good Clinical Practice, ISO 14155 Standard Operative Procedures and the Declaration of Helsinki and its current revision. The FACE study was overseen by an independent Executive Steering Committee (See online supplemental file 1).
thoraxjnl-2021-217205supp001.pdf (166.2KB, pdf)
Participants
Consecutive patients with HFrEF, HFmrEF or HFpEF according to current European Society of Cardiology guidelines3 21 who had predominant CSA±OSA, an indication for ASV therapy, and no contraindication for PAP therapy were eligible. A comprehensive list of inclusion and exclusion criteria is available in the design paper.20 A protocol modification was made in May 2015 after release of preliminary data from the SERVE-HF study,16 so that patients with HFrEF meeting SERVE-HF inclusion criteria (LVEF below 45% and CSA) were no longer enrolled. The non-ASV group included patients who refused or were noncompliant with ASV therapy (device usage <3 hour/night). The first subject was enrolled in November 2009 and enrolment was completed at the end of September 2018.
ASV therapy
ASV therapy (PaceWave, AutosetCS; ResMed) was initiated in hospital; pressure settings were titrated based on respiratory monitoring and patients were instructed to use the device for ≥5 hours every night. Full details of therapy titration have been reported previously.20 Device data (eg, leak, residual apnoea-hypopnoea index (AHI) and compliance) were downloaded at the first 3-month follow-up visit and then at least every 6 months.
Follow-up
Clinic visits occurred at inclusion, and at 3, 12 and 24 months’ follow-up.20 At each visit, primary endpoint events occurring since the last visit were recorded, functional status was determined (based on the New York Heart Association (NYHA) classification), and patients completed the Minnesota Living with Heart Failure Questionnaire and the Epworth Sleepiness Scale (ESS). This analysis focuses on 3-month follow-up visit data.
Outcomes
Primary outcome
The primary endpoint is the time to first event of the composite of all-cause death, life-saving cardiovascular intervention or unplanned hospitalisation (or unplanned prolongation of a planned hospitalisation) for worsening of chronic HF, consistent with the SERVE-HF study primary endpoint.16
Secondary outcomes
Additional hierarchical endpoints were the same as the primary endpoint but with cardiovascular death rather than all-cause death, and the same as the primary endpoint but with all-cause unplanned hospitalisation rather than unplanned hospitalisation for worsening of chronic HF (as per SERVE-HF). Other secondary endpoints were time to death (cardiovascular or all cause); time to unplanned hospitalisation; proportion of follow-up days during which patients are alive and not hospitalised; number of hospitalisations and changes in disease-specific quality of life, HF symptoms and medical treatment.
Statistical analysis
A sample of 300 patients was calculated to be sufficient to detect a 50% reduction in morbidity and mortality with PAP therapy (based on observational study data22 23 with 5% alpha and 90% power. The target was 400 to allow for dropouts. This was revised to a target of 300 patients with LVEF >45% (HFmrEF and HFpEF) after enrolment of patients with LVEF ≤45% was suspended (see previous publication for full details).20
Statistical analyses were performed using SAS V.9.4 and R V.3.6.1, and a p value threshold of 0.05. All primary and secondary endpoints were evaluated in the modified intention-to-treat population (all enrolled patients meeting the eligibility criteria). All available data were included in the analyses, unless consent for data usage was revoked.20 No analyses were performed for health-related quality of life, HF symptoms and medication usage because the proportion of missing data for these parameters was too high to perform imputation. Other variables with <20% missing values were imputed. When missingness was considered as missing at random, we applied a threshold as suggested by Madley-Dowd et al.24 Multiple imputations were handled as proposed by Sterne et al.25 To perform these multiple imputations: 10 imputed datasets were constituted using a Monte-Carlo Markov Chain for quantitative variables and fully conditional specification for qualitative variables. Imputed data sets were combined using Rubin’s rules.
An LCA classification method was used to identify homogeneous subgroups from a heterogeneous population and define patient subgroup profiles (based on baseline data at inclusion, including both the ASV and non-ASV groups). The principle is to minimise the distance between two individuals with similar characteristics and maximise distance between two individuals with different characteristics. LCA is an unsupervised classification method for which the optimal cluster number is not determined a priori, but based on statistical criteria (integrated completed likelihood).26 Moreover, LCA is a probabilistic method for which an individual is assigned to one cluster only based on his/her highest probability of belonging to this cluster. Variables of interest to run the LCA were 22: age, gender, body mass index, smoking status, alcohol consumption, depressive disorder, chronic obstructive pulmonary disease, hypertension, dyslipidaemia, stroke or transient ischaemic attack, atrial fibrillation, other arrhythmias, chronic HF with HFrEF, Ischaemic myocardiopathy, use of continuous PAP before ASV (yes or no), NYHA class I/II, LVEF (%), systolic blood pressure level, central AHI, obstructive AHI and time duration with oxygen saturation below 90% (T90). The set of variables used in the LCA was built to achieve a compromise between clinically meaningful variables, robustness of variables (low proportion of missing data) and avoiding collinearity between variables.
To illustrate the main differences between groups after clustering, a simple description of variables used in the clustering process was performed and overall comparisons were conducted using the χ2 test (qualitative variables) or Kruskal-Wallis test (qualitative variables). Given that the objective was only to provide descriptions and trends, no correction for multiple comparisons was performed.
Three-month event-free survival (primary and secondary endpoints) was estimated using the Kaplan-Meier method and compared between the different clusters using a two-sided log-rank test. Change in NYHA class was analysed using a likelihood χ2 test, and continuous endpoints were evaluated using analysis of covariance (ANCOVA) with the baseline value as a covariate (if available); variables with right-skewed distributions within each treatment group were log transformed before analysis.
Results
Patients
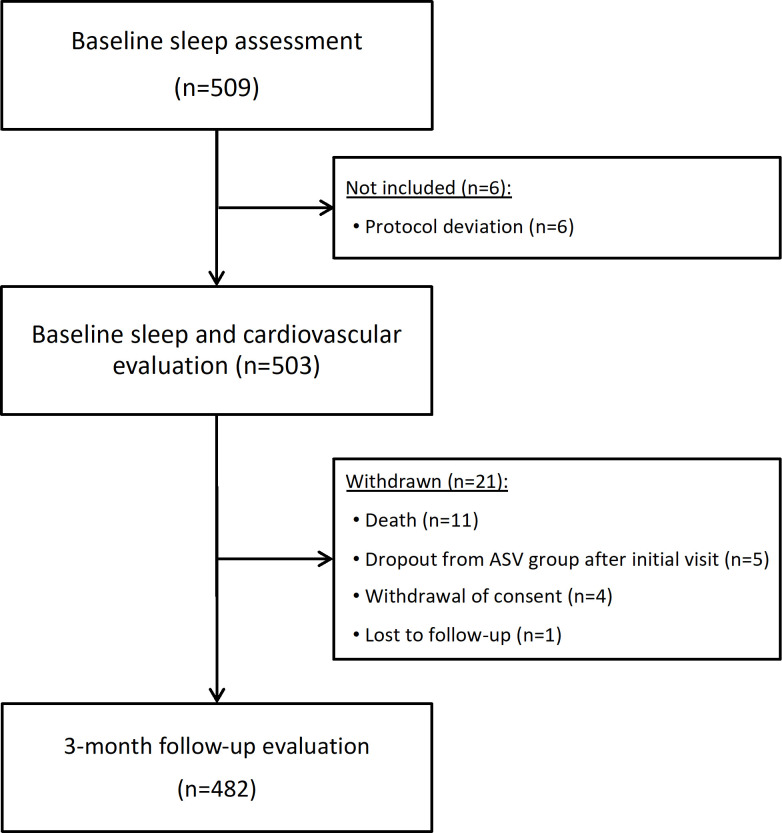
Baseline screening (sleep assessment) was performed in 509 patients, 6 were excluded and 503 underwent baseline assessments, and 482 remained in the study at 3-month follow-up (figure 1). The study population was elderly, predominantly men and nonsleepy (ESS score 4–11), HF was most often of ischaemic origin, and the most common indication for ASV was the presence of CSA (±OSA) (table 1). Baseline characteristics by patient subgroups based on SDB or HF type have been detailed previously.20 Median IQR AHI at baseline was 42 (30–55)/hour, median (IQR) oxygen desaturation (≥3%) index was 36 (23–51) and 49% of patients showed a periodic breathing pattern (CSR).
Figure 1.
Patient flow chart.
Table 1.
Baseline characteristics of the overall study population20
| Overall (n=503) | |
| Male, n (%) | 442 (88) |
| Age, years | 72 (64–79) |
| Body mass index, kg/m2 | 28 (25–32) |
| Current smoker, n (%) | 232 (46) |
| Alcohol use, n (%) | 66 (14) |
| Cardiac stimulator/defibrillator, n (%) | 136 (27) |
| Heart failure aetiology, n (%) | |
| Ischaemic | 259 (52) |
| Dilated cardiomyopathy | 36 (7) |
| Hypertension | 73 (15) |
| Valvular | 31 (8) |
| Alcoholic | 5 (1) |
| Other | 85 (17) |
| Left ventricular ejection fraction, % | 49 (34–58) |
| New York Heart Association class, n (%)* | |
| I | 82/438 (19) |
| II | 190/438 (43) |
| III | 146/438 (33) |
| IV | 20/438 (5) |
| Comorbidities, n (%) | |
| Hypertension | 360 (72) |
| Diabetes | 188 (38) |
| Dyslipidaemia | 292 (58) |
| Stroke/transient ischaemic attack | 113 (23) |
| Atrial fibrillation | 202 (40) |
| Other arrhythmias | 96 (19) |
| Chronic obstructive pulmonary disease | 58 (12) |
| Depression | 36 (7) |
Values are median (IQR) or number of patients (%).
*Data were available in 422 patients.
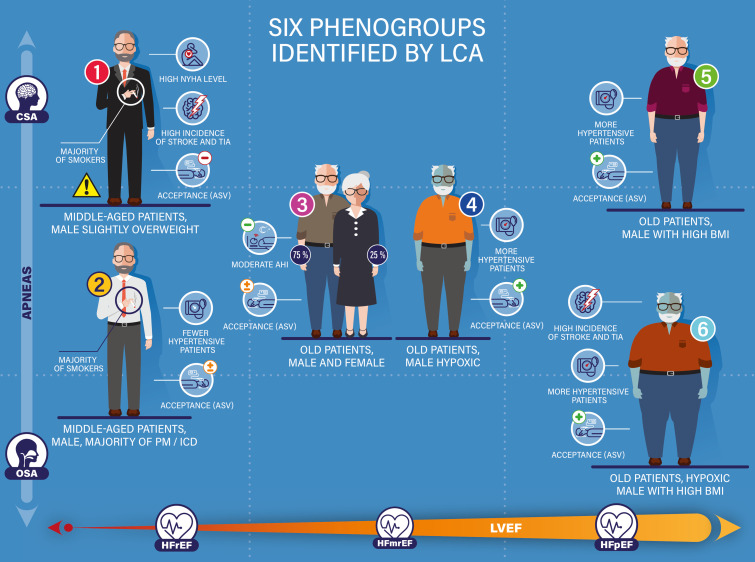
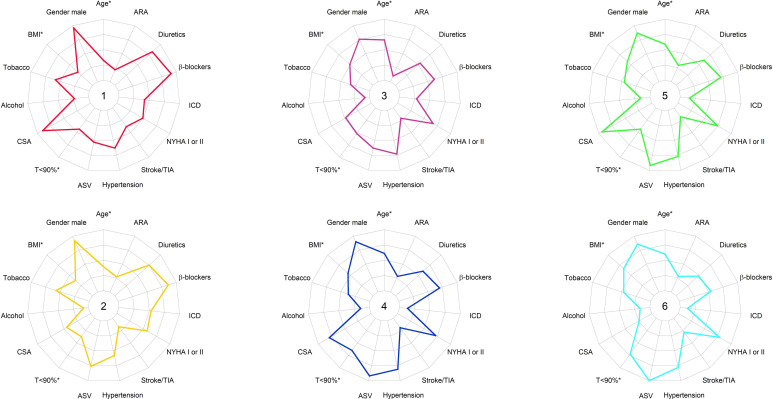
Cluster analysis
Six distinct, well-defined and different patient clusters were identified using LCA, illustration of clinical presentation of each cluster is presented in figure 2. Features of each cluster characterisation are pictured with specification in figure 3. Patients had a high probability of belonging to their own cluster (0.91–0.95). The most important parameters that discriminated between clusters were obstructive AHI, central AHI, LVEF (%), NYHA class I/II, T90 and the presence of HFrEF. As expected, there were significant differences in patient demographics (table 2), HF disease characteristics (table 3) and SDB features (table 4) between clusters resulting directly from the LCA methodology. Interestingly, ASV adherence and ASV refusal differed significantly between clusters although these variables were not included in the LCA model. Cluster 1 was the population that had characteristics reflecting those of the population enrolled in SERVE-HF.16
Figure 2.
Illustration of each cluster, by patient clinical characteristics and comorbidities. AHI, apnoea hypopnoea index; ASV, assisted servo ventilation device; BMI, body mass index; CSA, proportion of patients with central sleep apnoea; HFrEF, HFmrEF and HFpEF, heart failure with reduced, mid-range and preserved ejection fraction, respectively; ICD, implanted cardiac device (PM pacemaker, defibrillator, cardiac re-synchronisation); LVEF, left ventricular ejection fraction; NYHA, New York Heart Association class; OSA, proportion of patients with obstructive sleep apnoea T<90%, time spent with oxygen saturation below 90%; TIA, transient ischaemic attack.
Figure 3.
Features of each cluster, by patient characteristics, cardiovascular risk factors, heart failure characteristics, therapeutics and medication, hypoxic burden and ASV acceptance. Variables are expressed as percentages, with quantitative variables (*) dichotomised based on the median value (ie, BMI, age and T90) on the basis of median (see tables 2–4 for absolute values) and shown here as percentages on the radial axis (from 0% to 100%). ARA, angiotensin receptor antagonist; ASV, acceptance of assisted servo ventilation device; BMI, body mass index; CSA, proportion of patient with central sleep apnoea; ICD, implanted cardiac device (pacemaker, defibrillator, cardiac re-synchronisation); NYHA, New York Heart Association class; T<90%, time spent with oxygen saturation below 90%; TIA, transient ischaemic attack.
Table 2.
Patient characteristics by cluster
| Cluster 1 (n=79) |
Cluster 2 (n=89) |
Cluster 3 (n=67) |
Cluster 4 (n=99) |
Cluster 5 (n=119) |
Cluster 6 (n=50) |
P value* | |
| Male, n (%) | 76 (96.2) | 82 (92.1) | 51 (76.1) | 89 (89.9) | 103 (86.6) | 43 (86) | <0.01 |
| Age, years | 66 (57–74) | 68 (61–76) | 74 (66–81) | 76 (66–80) | 74 (66–79) | 75 (64–78) | <0.01 |
| Body mass index, kg/m2 | 26 (23–29) | 26 (24–30) | 28 (25–31) | 28 (25–32) | 29 (25–32) | 30 (27–33) | <0.01 |
| Current smoker, n (%) | 46 (58.2) | 51 (57.3) | 22 (32.8) | 37 (37.4) | 54 (45.4) | 23 (46) | <0.01 |
| Alcohol use, n (%) | 18 (22.8) | 7 (7.9) | 5 (7.5) | 14 (14.1) | 18 (15.1) | 8 (16) | 0.06 |
| Comorbidities, n (%) | |||||||
| Hypertension | 50 (63.3) | 52 (58.4) | 49 (73.1) | 80 (80.8) | 92 (77.3) | 39 (78) | <0.01 |
| Depression | 4 (5.1) | 8 (9) | 4 (6) | 8 (8.1) | 6 (5) | 6 (12) | 0.58 |
| Dyslipidaemia | 50 (63.3) | 55 (61.8) | 32 (47.8) | 66 (66.7) | 66 (55.5) | 27 (54) | 0.16 |
| Stroke/transient ischaemic attack | 30 (38.0) | 15 (16.9) | 14 (20.9) | 19 (19.2) | 21 (17.6) | 14 (28.0) | <0.01 |
| Diabetes | 29 (36.7) | 31 (34.8) | 25 (37.9) | 44 (44.4) | 40 (33.6) | 19 (38) | 0.68 |
| Chronic obstructive pulmonary disease | 9 (13.4) | 14 (11.8) | 7 (8.9) | 8 (16.0) | 10 (11.2) | 10 (10.1) | 0.85 |
Values are median (IQR) or number of patients (%).
*Kruskal-Wallis test (quantitative variables) or χ2 test (qualitative variables).
Table 3.
Heart failure characteristics and treatment by cluster
| Cluster 1 (n=79) |
Cluster 2 (n=89) |
Cluster 3 (n=67) |
Cluster 4 (n=99) |
Cluster 5 (n=119) |
Cluster 6 (n=50) |
P value* | |
| Left ventricular ejection fraction, % | 30 (20–35) | 35 (30–45) | 50 (44–55) | 52.7 (46–60) | 54 (50–65) | 56.5 (52–63) | <0.01 |
| Systolic HF, n (%) | 75 (96.2) | 68 (81) | 30 (48.4) | 35 (35.7) | 29 (25) | 16 (34.8) | <0.01 |
| NYHA class I or II, n (%) | 39 (49.4) | 51 (57.3) | 45 (67.2) | 71 (71.7) | 88 (73.9) | 39 (78.0) | <0.01 |
| HF aetiology, n (%) | |||||||
| Ischaemic | 44 (55.7) | 57 (65.5) | 29 (45.3) | 48 (49) | 58 (48.7) | 24 (48) | <0.01 |
| Dilated cardiomyopathy | 15 (19) | 10 (11.5) | 5 (7.8) | 2 (2) | 2 (1.7) | 2 (4) | |
| Hypertension | 5 (6.3) | 10 (11.5) | 6 (9.4) | 17 (17.3) | 21 (17.6) | 14 (28) | |
| Valvular | 4 (5.1) | 3 (3.4) | 4 (6.3) | 9 (9.2) | 13 (10.9) | 5 (10) | |
| Alcoholic | 5 (6.3) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Other | 6 (7.6) | 7 (8) | 20 (31.3) | 22 (22.4) | 25 (21) | 5 (10) | |
| MLHFQ score | 28 (16–54) | 32 (21–49) | 30 (23–56) | 23 (15–44) | 23 (11–44.5) | 32 (16–58) | 0.09 |
| NT-proBNP, pg/mL | 2215 (771–3730) | 1840 (766–4770) | 2026 (769–4136) | 1116 (462–2958) | 734 (287–2310) | 1250 (619–2140) | <0.01 |
| Implanted cardiac device, n (%) | 33 (41.8) | 47 (52.8) | 19 (28.4) | 13 (13.1) | 18 (15.1) | 6 (12.0) | <0.01 |
| Atrial fibrillation, n (%) | 35 (44.3) | 26 (29.2) | 31 (46.3) | 40 (40.4) | 49 (41.2) | 22 (44) | 0.27 |
| Other arrhythmias, n (%) | 15 (19) | 18 (20.2) | 10 (14.9) | 19 (19.2) | 26 (21.8) | 8 (16) | 0.89 |
| Medication, n (%) | |||||||
| Ivabridine | 11 (13.9) | 9 (10.1) | 3 (4.5) | 4 (4) | 3 (2.5) | 0 (0) | <0.01 |
| Beta-blockers | 72 (91.1) | 77 (86.5) | 41 (61.2) | 69 (69.7) | 84 (70.6) | 27 (54) | <0.01 |
| Diuretics | 65 (82.3) | 67 (75.3) | 36 (53.7) | 59 (59.6) | 73 (61.3) | 24 (48) | <0.01 |
| Angiotensin receptor blockers | 17 (21.5) | 24 (27) | 7 (10.4) | 28 (28.3) | 35 (29.4) | 14 (28) | 0.07 |
| Aldosterone blockers | 46 (58.2) | 35 (39.3) | 11 (16.4) | 13 (13.1) | 19 (16) | 4 (8) | <0.01 |
| Cardiac glycosides | 2 (2.5) | 2 (2.2) | 2 (3) | 6 (6.1) | 6 (5) | 3 (6) | 0.68 |
| ACE inhibitors | 57 (72.2) | 57 (64) | 37 (55.2) | 43 (43.4) | 57 (47.9) | 21 (42) | <0.01 |
| Statins | 50 (63.3) | 62 (69.7) | 34 (50.7) | 59 (59.6) | 77 (64.7) | 27 (54) | 0.17 |
Values are median (IQR) or number of patients (%).
*Kruskal-Wallis test (quantitative variables) or χ2e test (qualitative variables).
ACE, angiotensin-converting enzyme; MLHFQ, Minnesota Living with Heart Failure Questionnaire; NT-pro-BNP, amino terminal-pro B-type natriuretic peptide; NYHA, New York Heart Association.
Table 4.
Sleep-disordered breathing characteristics by cluster
| Cluster 1 (n=79) |
Cluster 2 (n=89) |
Cluster 3 (n=67) |
Cluster 4 (n=99) |
Cluster 5 (n=119) |
Cluster 6 (n=50) |
P value* | |
| Central sleep apnoea, n (%) | 71 (89.9) | 40 (44.9) | 32 (47.8) | 78 (78.8) | 112 (94.1) | 12 (24) | <0.01 |
| Central AHI, /h | 26 (21–32) | 14 (8–19) | 10 (5–16) | 33 (26–41) | 42 (31–55) | 8.5 (3–13) | <0.01 |
| Obstructive AHI, /h | 3 (1–6) | 20 (16–25) | 4 (1–9) | 20 (14–27) | 2 (0–5) | 40 (32–48) | <0.01 |
| Time with oxygen saturation<90%, min | 32 (6–87) | 23 (3–62) | 45 (5–103) | 74 (23–141) | 31 (4–83) | 91 (38–113) | <0.01 |
| CPAP usage before ASV, n (%) | 8 (10.1) | 8 (9.0) | 20 (29.9) | 14 (14.1) | 37 (31.1) | 18 (36.0) | <0.01 |
| Agreed to ASV therapy, n (%) | 42 (53.2) | 68 (76.4) | 42 (62.7) | 92 (91.9) | 109 (91.6) | 50 (100) | <0.01 |
Values are median (IQR) or number of patients (%).
*Kruskal-Wallis test (quantitative variables) or χ2 test (qualitative variables).
AHI, apnoea-hypopnoea index; ASV, adaptive servo ventilation; CPAP, continuous positive airway pressure; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Three-month outcomes by patient cluster
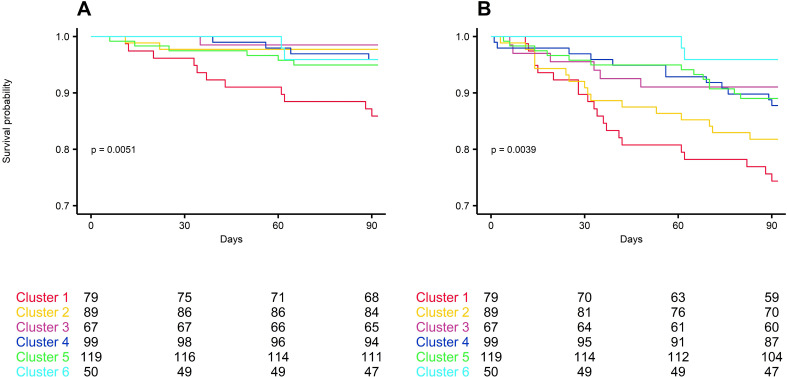
There were a number of significant differences between patient clusters with respect to the occurrence of endpoint events (p<0.01 (primary outcomes) and p=0.004 (secondary outcomes)) (figure 4). Cluster 1 had the highest rate of primary endpoint events (13.9% vs 1.5%–5% in the other clusters) (table 5). Cluster 1 also had a higher rate of cardiovascular death or HF-related hospitalisation (10.1% vs 1.5%–4.2%; p=0.07) (table 5).
Figure 4.
Three-month Kaplan-Meier survival curves for the primary (A), all-cause death, life-saving cardiovascular intervention or hospitalisation for worsening heart failure) and secondary (B), all-cause death, or all-cause hospitalisation) outcome by cluster.
Table 5.
Three-month outcomes by cluster
| Event rate, n (%) | Cluster 1 (n=79) |
Cluster 2 (n=89) |
Cluster 3 (n=67) |
Cluster 4 (n=99) |
Cluster 5 (n=119) |
Cluster 6 (n=50) |
P value* |
| All-cause death, life-saving CV intervention or hospitalisation for worsening HF | 11 (13.9) | 2 (2.2) | 1 (1.5) | 4 (4) | 6 (5) | 2 (4) | <0.01 |
| CV death or HF-related hospitalisation | 8 (10.1) | 2 (2.2) | 1 (1.5) | 3 (3) | 5 (4.2) | 1 (2) | 0.07 |
| All-cause death or all-cause hospitalisation | 20 (25.3) | 16 (18) | 6 (9) | 12 (12.1) | 13 (10.9) | 2 (4) | <0.01 |
| All-cause hospitalisation | 16 (20.3) | 16 (18) | 6 (9) | 11 (11.1) | 13 (10.9) | 1 (2) | 0.02 |
| HF-related hospitalisation | 6 (7.6) | 2 (2.2) | 1 (1.5) | 3 (3) | 5 (4.2) | 1 (2) | 0.35 |
| All-cause death | 5 (6.3) | 0 (0) | 0 (0) | 1 (1) | 4 (3.4) | 1 (2) | 0.05 |
| CV death | 2 (2.5) | 0 (0) | 0 (0) | 0 (0) | 2 (1.7) | 0 (0) | 0.25 |
*Kruskal-Wallis test (quantitative variables) or χ2 test (qualitative variables).
CV, cardiovascular; HF, heart failure.
Discussion
The first analysis of FACE study data showed that patients with HF with an indication for ASV are a heterogeneous population. Using LCA, patients could be categorised based on important characteristics, resulting in six patient clusters with distinct and clinically relevant characteristics. These different clusters were showing differences in ASV acceptance and prognosis after only 3 months of follow-up.
The highly heterogeneous nature of the enrolled patient population reflects clinical practice. The decision to take an LCA approach to FACE study data was made because it was thought that this would better stratify patients and allow more robust determination of the impact of ASV on outcomes in subgroups based on clinical characteristics. The six homogenous patient clusters identified represent clinically relevant subgroups of patients with HF who each behave similarly in clinical settings. For example, cluster 1 has characteristics that reflect those of the SERVE-HF study population,16 being mostly men and having low LVEF and predominant CSA. The impact of different factors, including ASV therapy, on prognosis in each cluster will become clearer after longer follow-up, although each cluster had a different prognosis at 3 months; this is likely due to the interplay of a variety of factors. Interestingly, the most important variable that discriminated between clusters was the characterisation of the SDB itself (ie, obstructive and central AHI). This seemed to better discriminate clusters with different prognosis than either LVEF (%) and NYHA class. After AHI, the next most important discriminating parameters were greater hypoxic burden (T90)27 28 and low ejection fraction.
Different HF phenotypes are recognised in the latest European HF guidelines.3 Phenotype-specific management of HF29–31 and SDB in HF32 33 is something that is gaining increased recognition. Along with LVEF, a number of other different characteristics can contribute to the phenotype in patients with HF, as shown in the present FACE study cluster analysis. Comorbidities are important, and interindividual variation in SDB phenotype has been documented among patients with HFrEF,33 highlighting the need for individualised treatment.
The patient clusters identified in this study could be used as the basis for clinical phenotyping in routine practice. Our clinical experience suggests that grouping patients into subgroups to assist in clinical decision-making and inform appropriate therapy choices already occurs to some extent. The process could be formalised by clearer definition of different phenotypes of patients with HF and SDB. This might help identify HF and SDB patient subgroups likely to benefit from ASV therapy and who show good adherence to treatment. In particular, the finding that ASV adherence differed between clusters provides practical information. Initial acceptance of ASV was not included as a variable in the LCA model and, therefore, our findings for this parameter are not likely to be related to selection bias. Moreover, we suggest that the clinical phenotyping obtained by LCA might be useful in clinical practice as a tool for clinicians deciding whether or not to propose ASV to an individual patient.
Clinicians are justifiably concerned about using ASV in patients with HF after the SERVE-HF results. Extensive scientific discussions have been published about the SERVE-HF study, providing a thorough understanding of its strengths and weaknesses.34–37 These discussions also offer some suggestions about additional research priorities that need to be addressed.38 39 However, in the present study, patients with characteristics that reflect those of the SERVE-HF study population are only a small subset of the wider group of patients with HF with SDB (eg, they comprised only one of six clusters in the current analysis) and other patient subgroups still have the potential to benefit from therapy.40 41
Further analysis of FACE study data is planned after 2 years’ follow-up, and this will investigate the effects of ASV on primary endpoint events, overall and in the six patient clusters. It is hoped that the findings will provide clinically useful parameters to guide the selection of patients with HF most likely to benefit from ASV therapy.
Interestingly, in patient clusters for whom ASV is not indicated (clusters 1 and 2; LVEF <45%) or not clearly indicated (cluster 3; moderate AHI), the proportion of patients who accepted ASV therapy was significantly lower than that in clusters 4, 5 and 6. Although the inclusion of patients with a low LVEF occurred before release of the SERVE-HF findings, one potential explanation for our findings of differential uptake of ASV between clusters might be weaker recommendation by the physician. Another hypothesis that should be investigated is that refusal by the patient might result from lower confidence with using ASV therapy or the presence of fewer symptoms amenable to treatment with ASV.
Study limitations
The main limitation of the FACE study is the nonrandomised design, which does not control for bias as well as a prospective randomised controlled clinical trial. However, although randomised trials are powerful research tools, these are not usually representative of a typical patient population and, therefore, have poor external validity and may not be widely applicable to real-world practice. Nevertheless, lack of randomisation means that sources of bias cannot be controlled for. For example, the decision to accept or decline ASV might contribute to any effects seen because willingness to use ASV (or not) might be indicative of other health behaviours that could influence outcomes. Furthermore, as for all cohort and observational studies, some confounding factors can be missed, mainly time-dependent confounders. One of the key limitations of cluster analysis is the data-driven aspect of these methods. Nevertheless, there is a high probability for each cluster, which allows good cluster discrimination, and the number of clusters is in accordance with both the statistical criteria used and the clinical relevance of the clusters. External validation in another independent population would provide important data on the robustness of each cluster. Finally, amendments to the study inclusion criteria after release of the SERVE-HF study result (ie, ASV contraindication in HFrEF with CSA) affected future patient recruitment and this could have potentially influenced the study findings.
Conclusion
Patients with HF with SDB are a highly heterogeneous group. LCA allowed patients to be grouped into clinically meaningful clusters that showed different prognosis and outcomes at 3-month follow-up. It may, therefore, be appropriate to define patient phenotype by creating a complete picture of each patient with HF before initiating PAP therapy. Our findings have the potential to provide important information to help individualise therapeutic strategies targeted at reducing morbidity and mortality in patients with HF and SDB.
Acknowledgments
Medical writing assistance for manuscript preparation was provided by Nicola Ryan, independent medical writer, funded by ResMed France.
Footnotes
Collaborators: FACE study investigators Valérie Attali; Maria-Anna Balice; Laurent Barthel; Rosa Buendia; Bertien Buyse; Laurent Boyer; Marie-Pierre Cadars; Pascal Cornec; Geoffroy De Faverges; Toufik Didi; Frédéric Gagnadoux; Thibaud Gentina; François Goupil; Jean-Maurice Guillemot; Carmen Iamandi; Richard Isnard; François Jounieaux; Christian Koltes; Alain Le Coz; Benoit Lequeux; René Lerest; Lionel Lerousseau; Jean-Pierre Mallet; Francis Martin; Jean-Claude Meurice; Ala Noroc; Frédéric Ortuno; Philippe Papola; Audrey Paris; Hélène Pastinelli; Christophe Perrin; Carole Philippe; Sandrine Pontier; Arnaud Prigent; Pascaline Priou; Vincent Puel; Claudio Rabec; Benjamin Richard; Claude Richard; Marijke Rutten; Manuel Sastry; Murielle Salvat; Kamila Sedkaoui; Bharati Shivalkar; Dries Testelmans; Johan Verbraecken.
Contributors: Study conception and design: M-PO, JLP, TD, J-MD, FL and RT. Acquisition of data: M-PO, JLP, TD, J-MD, RT, AP, FG, JV. Statistical analysis: SB, RT. Analysis or interpretation of data: M-PO, JLP, TD, J-MD, FL, SB and RT. Drafting of the manuscript: RT. Critical revision of the manuscript for important intellectual content: M-PO, JLP, TD, J-MD, FL, AP, FG, JV, SB and RT. Study supervision: M-PO, JLP, TD, J-MD, FL and RT are the guarantors of the study. All authors approved the final version of the manuscript.
Funding: Resmed sponsored the study and owns the data. All study data are stored at Grenoble Alpes University data platforms. The analyses presented here were performed by Grenoble Alpes University quantitative scientists independent of the sponsor. Grenoble Alpes University has the right to publish regardless of the outcome. All the authors, including authors employed by the sponsor, reviewed and approved the manuscript and vouch for the accuracy and completeness of the data. RT, SB and J-LP are supported by the French National Research Agency in the framework of the 'Investissements d’avenir' program (ANR-15-IDEX-02) and the 'e-health and integrated care and trajectories medicine and MIAI artificial intelligence' Chairs of excellence from the Grenoble Alpes University Foundation. This work was partially supported by MIAI @ Grenoble Alpes, (ANR-19-P3IA-0003).
Competing interests: JLP, TD, JMD, RT and MPO are FACE study investigators and steering committee members for ResMed. AP and FG are FACE study investigators for ResMed. RT has received unrestricted research grants from ResMed, Vitalaire, Philips and the AGPMC Foundation, consultant fees from ResMed, Inspire, Navigant and Jazz Pharmaceuticals, and travel grants from Agiradom. TD reports grants and fees from Pfizer, ResMed, GSK, Alnylam, Akcea Therapeutics, Ionis, Sanofi-Aventis, and Novartis. JAV reports grants and personal fees from ResMed, Bioproject and Jazz Pharmaceuticals, personal fees from Philips, Sanofi, Agfa-Gevaert and Springer, and grants from AirLiquide, Westfalen Medical, SomnoMed, Vivisol, Total Care, Medidis, Fisher & Paykel, Wave Medical, OSG, MediqTefa, NightBalance, Heinen & Löwenstein, AstraZeneca, Accuramed, Bekaert Deslee Academy and UCB Pharma, all outside the submitted work. MPO. has received unrestricted research grants from ResMed and Philips, consultant fees from ResMed, Somnomed and Jazz Pharmaceuticals, speaker fees from ResMed, Philips, LinaNova and Jazz Pharmaceuticals, and travelling grants from ISIS medical, Orkyn, SOS Oxygene and Vitalaire. SB has no conflicts of interest to declare. FL is an employee of ResMed.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
FACE study investigators:
Valérie Attali, Maria-Anna Balice, Laurent Barthel, Rosa Buendia, Bertien Buyse, Laurent Boyer, Marie-Pierre Cadars, Pascal Cornec, Geoffroy De Faverges, Toufik Didi, Frédéric Gagnadoux, Thibaud Gentina, François Goupil, Jean-Maurice Guillemot, Carmen Iamandi, Richard Isnard, François Jounieaux, Christian Koltes, Alain Le Coz, Benoit Lequeux, René Lerest, Lionel Lerousseau, Jean-Pierre Mallet, Francis Martin, Jean-Claude Meurice, Ala Noroc, Frédéric Ortuno, Philippe Papola, Audrey Paris, Hélène Pastinelli, Christophe Perrin, Carole Philippe, Sandrine Pontier, Arnaud Prigent, Pascaline Priou, Vincent Puel, Claudio Rabec, Benjamin Richard, Claude Richard, Marijke Rutten, Manuel Sastry, Murielle Salvat, Kamila Sedkaoui, Bharati Shivalkar, and Dries Testelmans
Data availability statement
The data are not freely available and access must be granted by the steering committee but we welcome any potential collaboration with other researchers. For further information, please email RT (RTamisier@ chu-grenoble.fr).
Ethics statements
Patient consent for publication
Not required.
References
- 1. Roger VL. Epidemiology of heart failure. Circ Res 2013;113:646–59. 10.1161/CIRCRESAHA.113.300268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Owan TE, Hodge DO, Herges RM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006;355:251–9. 10.1056/NEJMoa052256 [DOI] [PubMed] [Google Scholar]
- 3. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–200. 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 4. Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 2006;355:260–9. 10.1056/NEJMoa051530 [DOI] [PubMed] [Google Scholar]
- 5. Bolam H, Morton G, Kalra PR. Drug therapies in chronic heart failure: a focus on reduced ejection fraction. Clin Med 2018;18:138–45. 10.7861/clinmedicine.18-2-138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Oldenburg O, Lamp B, Faber L, et al. Sleep-Disordered breathing in patients with symptomatic heart failure: a contemporary study of prevalence in and characteristics of 700 patients. Eur J Heart Fail 2007;9:251–7. 10.1016/j.ejheart.2006.08.003 [DOI] [PubMed] [Google Scholar]
- 7. Paulino A, Damy T, Margarit L, et al. Prevalence of sleep-disordered breathing in a 316-patient French cohort of stable congestive heart failure. Arch Cardiovasc Dis 2009;102:169–75. 10.1016/j.acvd.2008.12.006 [DOI] [PubMed] [Google Scholar]
- 8. Lévy P, Kohler M, McNicholas WT, et al. Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 2015;1:15015. 10.1038/nrdp.2015.15 [DOI] [PubMed] [Google Scholar]
- 9. Khayat R, Jarjoura D, Porter K, et al. Sleep disordered breathing and post-discharge mortality in patients with acute heart failure. Eur Heart J 2015;36:1463–9. 10.1093/eurheartj/ehu522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hastings PC, Vazir A, Meadows GE, et al. Adaptive servo-ventilation in heart failure patients with sleep apnea: a real world study. Int J Cardiol 2010;139:17–24. 10.1016/j.ijcard.2008.08.022 [DOI] [PubMed] [Google Scholar]
- 11. Nakamura S, Asai K, Kubota Y, et al. Impact of sleep-disordered breathing and efficacy of positive airway pressure on mortality in patients with chronic heart failure and sleep-disordered breathing: a meta-analysis. Clin Res Cardiol 2015;104:208–16. 10.1007/s00392-014-0774-3 [DOI] [PubMed] [Google Scholar]
- 12. Oldenburg O, Schmidt A, Lamp B, et al. Adaptive servoventilation improves cardiac function in patients with chronic heart failure and Cheyne-Stokes respiration. Eur J Heart Fail 2008;10:581–6. 10.1016/j.ejheart.2008.04.007 [DOI] [PubMed] [Google Scholar]
- 13. Sharma BK, Bakker JP, McSharry DG, et al. Adaptive servoventilation for treatment of sleep-disordered breathing in heart failure: a systematic review and meta-analysis. Chest 2012;142:1211–21. 10.1378/chest.12-0815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sun H, Shi J, Li M, et al. Impact of continuous positive airway pressure treatment on left ventricular ejection fraction in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. PLoS One 2013;8:e62298–305. 10.1371/journal.pone.0062298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kasai T, Narui K, Dohi T, et al. Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 2008;133:690–6. 10.1378/chest.07-1901 [DOI] [PubMed] [Google Scholar]
- 16. Cowie MR, Woehrle H, Wegscheider K, et al. Adaptive Servo-Ventilation for central sleep apnea in systolic heart failure. N Engl J Med 2015;373:1095–105. 10.1056/NEJMoa1506459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. O'Connor CM, Whellan DJ, Fiuzat M, et al. Cardiovascular Outcomes With Minute Ventilation-Targeted Adaptive Servo-Ventilation Therapy in Heart Failure: The CAT-HF Trial. J Am Coll Cardiol 2017;69:1577–87. 10.1016/j.jacc.2017.01.041 [DOI] [PubMed] [Google Scholar]
- 18. McEvoy RD, Antic NA, Heeley E, et al. Cpap for prevention of cardiovascular events in obstructive sleep apnea. N Engl J Med 2016;375:919–31. 10.1056/NEJMoa1606599 [DOI] [PubMed] [Google Scholar]
- 19. Bradley TD, Logan AG, Kimoff RJ, et al. Continuous positive airway pressure for central sleep apnea and heart failure. N Engl J Med 2005;353:2025–33. 10.1056/NEJMoa051001 [DOI] [PubMed] [Google Scholar]
- 20. Tamisier R, Damy T, Davy J-M, et al. Cohort profile: face, prospective follow-up of chronic heart failure patients with sleep-disordered breathing indicated for adaptive servo ventilation. BMJ Open 2020;10:e038403. 10.1136/bmjopen-2020-038403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McMurray JJV, Adamopoulos S, Anker SD, et al. Esc guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of cardiology. developed in collaboration with the heart failure association (HFA) of the ESC. Eur Heart J 2012;33:1787–847. 10.1093/eurheartj/ehs104 [DOI] [PubMed] [Google Scholar]
- 22. Damy T, Margarit L, Noroc A, et al. Prognostic impact of sleep-disordered breathing and its treatment with nocturnal ventilation for chronic heart failure. Eur J Heart Fail 2012;14:1009–19. 10.1093/eurjhf/hfs085 [DOI] [PubMed] [Google Scholar]
- 23. Jilek C, Krenn M, Sebah D, et al. Prognostic impact of sleep disordered breathing and its treatment in heart failure: an observational study. Eur J Heart Fail 2011;13:68–75. 10.1093/eurjhf/hfq183 [DOI] [PubMed] [Google Scholar]
- 24. Madley-Dowd P, Hughes R, Tilling K, et al. The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol 2019;110:63–73. 10.1016/j.jclinepi.2019.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338:b2393. 10.1136/bmj.b2393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Marbac M, Sedki M. Variable selection for model-based clustering using the integrated complete-data likelihood. Stat Comput 2017;27:1049–63. 10.1007/s11222-016-9670-1 [DOI] [Google Scholar]
- 27. Azarbarzin A, Sands SA, Taranto-Montemurro L, et al. The sleep Apnea-Specific hypoxic burden predicts incident heart failure. Chest 2020;158:739–50. 10.1016/j.chest.2020.03.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bourdier G, Détrait M, Bouyon S, et al. Intermittent hypoxia triggers early cardiac remodeling and contractile dysfunction in the time-course of ischemic cardiomyopathy in rats. J Am Heart Assoc 2020;9:e016369. 10.1161/JAHA.120.016369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lewis GA, Schelbert EB, Williams SG, et al. Biological phenotypes of heart failure with preserved ejection fraction. J Am Coll Cardiol 2017;70:2186–200. 10.1016/j.jacc.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 30. Samson R, Jaiswal A, Ennezat PV, et al. Clinical phenotypes in heart failure with preserved ejection fraction. J Am Heart Assoc 2016;5. 10.1161/JAHA.115.002477. [Epub ahead of print: 25 Jan 2016]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shah SJ, Kitzman DW, Borlaug BA, et al. Phenotype-Specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation 2016;134:73–90. 10.1161/CIRCULATIONAHA.116.021884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Javaheri S, Brown LK, Abraham WT, et al. Apneas of heart failure and phenotype-guided treatments: Part one: OSA. Chest 2020;157:394-402. 10.1016/j.chest.2019.02.407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Arzt M, Oldenburg O, Graml A, et al. Phenotyping of sleep-disordered breathing in patients with chronic heart failure with reduced ejection Fraction-the SchlaHF registry. J Am Heart Assoc 2017;6. 10.1161/JAHA.116.005899. [Epub ahead of print: 29 Nov 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bradley TD. SERVE-HF on-treatment analysis: does the on-treatment analysis serve its purpose? Eur Respir J 2017;50. 10.1183/13993003.01516-2017. [Epub ahead of print: 31 08 2017]. [DOI] [PubMed] [Google Scholar]
- 35. Eulenburg C, Wegscheider K, Woehrle H, et al. Mechanisms underlying increased mortality risk in patients with heart failure and reduced ejection fraction randomly assigned to adaptive servoventilation in the SERVE-HF study: results of a secondary multistate modelling analysis. Lancet Respir Med 2016;4:873–81. 10.1016/S2213-2600(16)30244-2 [DOI] [PubMed] [Google Scholar]
- 36. Javaheri S, Brown LK, Randerath W, et al. SERVE-HF: more questions than answers. Chest 2016;149:900–4. 10.1016/j.chest.2015.12.021 [DOI] [PubMed] [Google Scholar]
- 37. Somers V, Arzt M, Bradley TD, et al. Servo-Ventilation therapy for sleep-disordered breathing. Chest 2018;153:1501–2. 10.1016/j.chest.2018.03.052 [DOI] [PubMed] [Google Scholar]
- 38. Orr JE, Ayappa I, Eckert DJ, et al. Research priorities for patients with heart failure and central sleep apnea. An official American thoracic Society research statement. Am J Respir Crit Care Med 2021;203:e11–24. 10.1164/rccm.202101-0190ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Haruki N, Floras JS. Sleep-Disordered Breathing in Heart Failure - A Therapeutic Dilemma. Circ J 2017;81:903–12. 10.1253/circj.CJ-17-0440 [DOI] [PubMed] [Google Scholar]
- 40. Carnevale C, Georges M, Rabec C, et al. Effectiveness of adaptive Servo ventilation in the treatment of hypocapnic central sleep apnea of various etiologies. Sleep Med 2011;12:952–8. 10.1016/j.sleep.2011.07.008 [DOI] [PubMed] [Google Scholar]
- 41. d’Ortho MP, Woehrle H, Arzt M. Current and future use of adaptive servo-ventilation. Eur Respir Pulm Dis 2016;2:18–22. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2021-217205supp001.pdf (166.2KB, pdf)
Data Availability Statement
The data are not freely available and access must be granted by the steering committee but we welcome any potential collaboration with other researchers. For further information, please email RT (RTamisier@ chu-grenoble.fr).