Abstract
Background
Spontaneous coronary artery dissection (SCAD) is an under-recognized cause of acute coronary syndrome in women.
Case Presentation
We present a 40-year-old female who presented with recurrent STEMI due to recurrent SCAD 10 days after the index presentation in a different coronary territory. She was successfully treated both times with drug eluting stents. MRI showed an evidence of transmural infarction but her ejection fraction was only mildly reduced. She had good short term outcome.
Conclusion
High index of suspicion is crucial for early diagnosis and prompt medical and interventional management in patients with SCAD.
Keywords: Spontaneous coronary artery dissection, left anterior descending, STEMI, percutaneous intervention, coronary angiography, MRI
1. INTRODUCTION
Spontaneous coronary artery dissection (SCAD) is an under-recognized cause of acute coronary syndrome in women. It usually has a benign course but a high rate of recurrence. Although essential, early diagnosis is frequently challenging and a high index of suspicion is crucial for prompt management [1].
2. CASE PRESENTATION
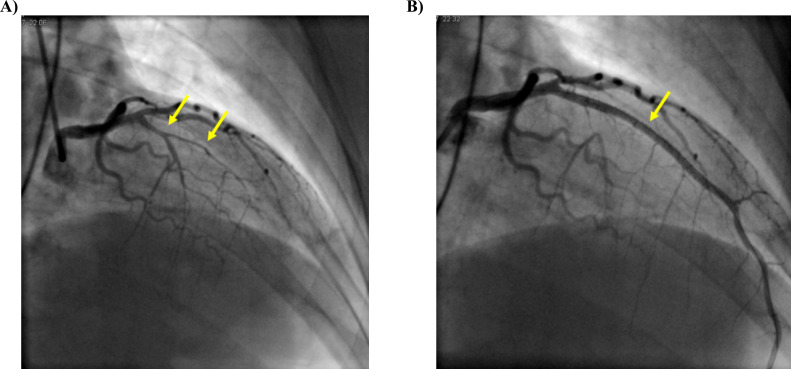
A 40-year-old female with no cardiac risk factors presented with anterior ST elevation myocardial infarction (STEMI). She was started on medical therapy and emergent coronary angiography showed severe mid left anterior descending (LAD) artery obstruction secondary to SCAD (Fig. 1A) while her other coronaries were angiographically normal. She underwent percutaneous intervention (PCI) with restoration of flow (Fig. 1B) and resolution of symptoms. She was discharged home but presented 10 days later with inferior STEMI. Coronary angiography patent LAD stent and a spontaneous dissection of the proximal right coronary artery resulting in severe obstruction (Fig. 2A). Emergent PCI was done with restoration of flow (Fig. 2B) and improvement of symptoms. Cardiac magnetic resonance imaging showed decreased perfusion (Fig. 3A) and evidence of late gadolinium enhancement (Fig. 3B) consistent with transmural infarction of the basal to mid inferior and septal segments in addition to sub-endocardial infarction involving the distal anterior and septal segments with mildly depressed systolic function. Left ventricular ejection fraction was 48%. A complete autoimmune workup revealed no abnormalities apart from elevated C reactive protein. The patient was discharged home a few days later on medical therapy.
Fig. (1).
A: Severe mid left anterior descending (LAD) artery occlusion secondary to SCAD (arrows). B: Restoration of flow after percutaneous intervention and stent placement. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Fig. (2).
A: Spontaneous dissection of the proximal right coronary artery resulting in severe obstruction (arrow). B: Restoration of flow after percutaneous intervention and stent placement. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Fig. (3).
A: Decreased perfusion in the mid inferior and septal segments on magnetic resonance imaging. B: Significant late gadolinium enhancement indicating transmural infarction in the mid inferior and septal segments. (A higher resolution / colour version of this figure is available in the electronic copy of the article).
3. DISCUSSION
SCAD is a rare cause of acute coronary syndrome and a high index of suspicion is essential for early diagnosis. In patients with acute presentation and ongoing symptoms, emergent PCI has an excellent outcome. After a primary SCAD event, the 10-year SCAD recurrence rate can be as high as 29%. Recurrence timing is unpredictable with a median time to second episode ranging from few days to more than 10 years and it can occur in previously unaffected coronary arteries. Spontaneous coronary artery dissection is an increasingly recognized cause of acute coronary syndrome in young females. This entity is being diagnosed more often because of increased physician awareness, more familiarity with different angiographic presentations, and the relatively quick and easy access to coronary angiography most patients presenting with acute coronary syndrome have. More than 90% of affected individuals are females and among those less than 5% are pregnancy related [2]. There are 2 distinct mechanisms, the first includes an intimal tear and subsequent development of intramural hematoma that compresses the true lumen and has a pathognomonic angiographic appearance. The second mechanism involves rupture of the vasa-vasorum and has an atypical angiographic appearance unless
a reverse intimal rupture happens [2]. In both cases, the presence of intramural hematoma is essential for diagnosis and compression of the true lumen is what causes the clinical symptoms. Predisposing factors include underlying vasculopathy involving the media like fibromuscular dysplasia, pregnancy related changes, connective tissue disorders, systemic inflammatory disease, and hormonal therapy. Spontaneous dissection is usually precipitated by intense exercise or emotional stress, labor and delivery, intense Valsalva type activities, and recreational drugs [3]. Most patients present with acute coronary syndrome [4], however, presentation can vary from stable angina to sudden cardiac death. High index of suspicion is important for early diagnosis and prompt management. Factors that should raise the suspicion for spontaneous coronary dissection in patients presenting with acute coronary syndrome include myocardial infarction in young women, absence of traditional cardiovascular risk factors, no atherosclerosis in other arteries, and the presence of a predisposing or precipitating factor as discussed above [5]. Coronary angiography remains the gold standard for diagnosis and there are three identified angiographic variants. The first is the pathognomonic appearnce that shows contrast dye staining of the arterial wall with multiple radiolucent lumens, the second shows diffuse stenosis that is usually long with abrupt demarcation from within normal segments and the third mimics atherosclerosis [5]. Intracoronary imaging tools like intravascular ultrasound and optical coherence tomography are crucial for confirming the diagnosis especially in ambiguous cases. They are also important in guiding management when percutaneous angiography is indicated [6]. Medical therapy is indicated in all patients and includes dual antiplatelet therapy for a year and then lifetime aspirin and beta blockers. There is an ongoing clinical trial to evaluate the role of angiotensin converting enzyme inhibitors and statins in patients with spontaneous coronary artery dissection [2]. Most of these lesions heal with medical therapy, however, in some cases, intervention is needed. Indications for revascularization include persistent or recurrent ischemia, cardiogenic shock, sustained ventricular tachycardia or ventricular fibrillation, and left main dissection [7]. Technical difficulties of PCI in SCAD include the inability to gain true lumen access, extension of dissection, and need for multiple or long stents increasing the risk of stent thrombosis and restenosis. Another challenge is sealing the entry point with an appropriate stent. Furthermore, intramural hematoma tends to undergo resorption with time causing stent malapposition which increases the risk of thrombosis especially after stopping dual antiplatelet therapy. Bioabsorbable stents have the theoretical advantage of avoiding the long-term effects of malapposition [1, 2, 6]. Results of percutaneous angioplasty and coronary artery bypass are suboptimal in this patient population given the diffuse nature of the disease and the fact that many of these lesions heal subsequently causing graft shutdown and stent malopposition [2]. This patient population is prone to recurrent spontaneous coronary artery dissections with an incidence of 15% at 2 years and 27% at 4-5 year follow-up [3, 8]. Recurrence timing is unpredictable with a median time to second episode ranging from few days to more than 10 years and it can occur in previously unaffected coronary arteries. However, very short term recurrence as described in our case is rare.
CONCLUSION
We presented a young female patient who presented with recurrent STEMI due to recurrent SCAD 10 days after the index presentation in a different coronary territory. She was successfully treated both times with drug eluting stents. MRI showed an evidence of transmural infarction but her ejection fraction was only mildly reduced. She had good short term outcome. A high index of suspicion is crucial for early diagnosis and prompt medical and interventional management in patients with SCAD.
ACKNOWLEDGEMENTS
Declared none.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed were taken from patients.
STANDARD OF REPORTING
CARE guidelines and methodology were followed in this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Rahman A., Al Emam A.R.A., Almomani A., Gilani S.A., Khalife W.I. Spontaneous coronary artery dissection: One disease, variable presentations and different management approaches. Int. J. Angiol. 2016;25(3):139–147. doi: 10.1055/s-0035-1563604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saw J., Mancini G.B.J., Humphries K.H. Contemporary review on spontaneous coronary artery dissection. J. Am. Coll. Cardiol. 2016;68(3):297–312. doi: 10.1016/j.jacc.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 3.Saw J., Aymong E., Sedlak T., et al. Spontaneous coronary artery dissection: Association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ. Cardiovasc. Interv. 2014;7:645–655. doi: 10.1161/CIRCINTERVENTIONS.114.001760. [DOI] [PubMed] [Google Scholar]
- 4.Lettieri C., Zavalloni D., Rossini R., et al. Management and longterm prognosis of spontaneous coronary artery dissection. Am. J. Cardiol. 2015;116(1):66–73. doi: 10.1016/j.amjcard.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 5.Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter. Cardiovasc. Interv. 2014;84(7):1115–1122. doi: 10.1002/ccd.25293. [DOI] [PubMed] [Google Scholar]
- 6.Mahmood M.M., Austin D. IVUS and OCT guided primary percutaneous coronary intervention for spontaneous coronary artery dissection with bioresorbable vascular scaffolds. Cardiovasc. Revasc. Med. 2016;18(1):5–9. doi: 10.1016/j.carrev.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 7.Al Emam A.R.A., Almomani A., Gilani S. Spontaneous coronary artery dissection and hemodynamic instability: Can emergent PCI be life saving? Report of two cases and literature review. Int. J. Angiol. 2014;23(4):275–280. doi: 10.1055/s-0033-1349163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakashima T., Noguchi T., Haruta S., et al. Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the Angina Pectoris – Myocardial Infarction Multicenter Investigators in Japan. Int. J. Cardiol. 2016;207:341–348. doi: 10.1016/j.ijcard.2016.01.188. [DOI] [PubMed] [Google Scholar]