Abstract
Modern-day regulatory systems governing conditions for how health products enter national markets constitute a barrier of access for traditional herbal medicines on an international level. Regulatory intentions are focused on ensuring that consumers are being provided with safe, efficacious and high-quality products that, however, collaterally limit opportunities for traditional herbal medicinal products, especially those that do not already have a long-standing tradition of use established in the respective national marketplaces. This case study investigates and compares how a Southern African herbal medicine with great potential as an anxiolytic and mild antidepressant - Mesembryanthemum tortuosum L. [syn. Sceletium tortuosum (L.) N.E.Br.] aerial parts - fares internationally in today’s regulatory environments. It is argued that inadvertent regulatory favoritism combined with the lack of means for adequate protection of intellectual property may obstruct innovation by creating an almost insurmountable economical hurdle for successful product development and introduction of botanicals from developing countries into most of the world’s health product markets.
Keywords: Mesembryanthemum tortuosum, sceletium, anxiety, depression, regulations
1. INTRODUCTION
Historically, the Western exploration and exploitation of paradigms of traditional medicine were driven and supported by some or a combination of the following: pure chance, entrepreneurship, colonialism, medical need, and, last but not least, the absence of regulatory barriers and the Nagoya Protocol. Only then was it possible for traditional Southern African herbal medicines such as devil’s claw (Harpagophytum procumbens DC. and/or H. zeyheri Decne.), Umckaloabo (Pelargonium sidoides DC. and/or P. reniforme Curt.), African potato (Hypoxis hemerocallidea Fisch., C.A.Mey. & Avé-Lall.), Cape aloe (Aloe ferox Mill.), buchu (Agathosma spp.) and many more herbal medicines from Asian traditions like Traditional Chinese Medicine (TCM) and Ayurveda to establish themselves in the European and/or Northern American marketplace, mostly within the last 150 years.
The plant, generally known as sceletium, kanna, channa or kougoed (Mesembryanthemum tortuosum L.), is a succulent herb commonly found in the dry western parts of South Africa [1]. It is a traditional medicinal plant utilized for relieving abdominal pain, hunger and to enhance mood.
More recently, it has attracted wider scientific attention for its potential in the treatment for depression and anxiety, to promote well-being, and provide stress relief. A number of potential mechanisms for its observed clinical effects have been described. The main active constituents have been identified as mesembrine alkaloids and some of their individual properties have been investigated [1-3].
While known and used by local healers for centuries [4-8], sceletium did not benefit from an early introduction into any of the First World’s marketplaces, resulting in a variety of regulatory barriers for product development and the introduction of sceletium-based products into the international marketplace.
Part 1 of this case study reviews taxonomy, ecology, ethnobotany and available data on pharmacology and safety from pre-clinical and clinical investigations. Part 2 elucidates exemplarily modern regulatory systems with a focus on key markets and with respect to individual regulatory categories and their requirements for placing sceletium products in the marketplace.
2. SCELETIUM
2.1. Taxonomy and Nomenclature
Mesembryanthemum tortuosum [syn. Sceletium tortuosum (L.) N.E. Br.] (Aizoaceae) is a short-lived perennial succulent herb with a creeping habit. Its roots are fibrous, the branches are slender and weakly lignified, with the basal ones becoming robust with age. Leaves are flat and succulent, connate at the base and become skeletonized around the vegetative buds in the arid summer season. Flowers are mostly solitary, stalked or sessile, 20-40 mm in diameter, almost invariably yellow but occasionally white or pink. The fruit capsules are 4- to 5- (to 6)-locular, very light, breaking off to be dispersed by wind. Seeds are 1.5-2 mm in diameter, D-shaped, black or brown [9].
The species and its populations show considerable geographical variation, resulting in several regional forms historically considered to represent distinct species (see the synonymy of M. tortuosum below).
Eight species were recognized in a revision of the genus Sceletium (which now forms part of the genus Mesembryanthemum) namely S. crassicaule, S. emarcidum, S. exalatum, S. expansum, S. rigidum, S. strictum, S. tortuosum and S. varians [2, 9]. Klak et al. [10] provided an alternative classification of the Sceletium group which is shown below, with all major synonyms indicated. This classification is currently accepted by the South African National Biodiversity Institute and all major international botanical institutions and databases:
Mesembryanthemum archeri (L.Bolus) Klak [syn. Sceletium archeri L.Bolus; S. rigidum L.Bolus].
M. crassicaule Haw. [syn. S. crassicaule (Haw.) L.Bolus; S. albanense L.Bolus].
M. emarcidum Thunb. [syn. S. emarcidum (Thunb.) L.Bolus ex H.Jacobsen; S. anatomicum (Haw.) L.Bolus; S. dejagerae L.Bolus].
M. exalatum (Gerbaulet) Klak [syn. S. exalatum Gerbaulet].
M. expansum L. [syn. S. expansum (L.) L.Bolus; S. regium L.Bolus].
M. ladismithiense Klak [syn. S. strictum L.Bolus].
M. tortuosum L. [syn. S. tortuosum (L.) N.E.Br.; L. boreale L.Bolus; S. compactum L.Bolus; S. framesii L.Bolus; S. gracile L.Bolus; S. joubertii L.Bolus; S. namaquense L. Bolus. var. namaquense; S. namaquense var. subglobosum L.Bolus; S. ovatum L.Bolus; S. tugwelliae L.Bolus].
M. varians Haw. [syn. S. varians (Haw.) Gerbaulet; S. subvelutinum L.Bolus forma luxurians L.Bolus].
Sceletium has become a convenient commercial name that mainly refers to M. tortuosum, the only species that has been used to any extent in traditional medicine and in product and crop development in South Africa. When used as a common name, sceletium is written in lower case and in roman script; when used in the botanical (taxonomic) sense, Sceletium is written in upper case and in Latin, hence, the italics script.
2.2. Ecology and Distribution
Mesembryanthemum species of the Sceletium group occur in the karroid (calcareous soil) regions of the Western and Northern Cape Provinces, South Africa, in the triangle of the Montagu, Aberdeen, and Namaqualand districts. Carefully selected plant material has been successfully cultivated on a small commercial scale as an essential prerequisite to ongoing research and development. The first trial plantings were carried out in 1996, based on material obtained during an ecogeographical survey and chemical variation study. Trial plantings showed that M. tortuosum can easily be cultivated and raw material became available in small commercial quantities in 2000; the product was regularly included in herbal beverage teas since 2002, but the details were not recorded (Van Wyk, unpublished data).
2.3. Ethnobotany
Sceletium species have an exceptionally long recorded history of use, with the first documented reports of its use by Van Riebeeck (ca. 1660) as an item of trade of the Khoi. It has likely been used by hunter-gatherers and pastoralists from prehistoric times. An early illustration of a sceletium plant can be found in the journal of Cape of Good Hope Governor van der Stel’s expedition to Namaqualand in 1685 [11] who stated that the product, on account of its “agreeable, hearty taste”, has considerable potential as a commercial product. There are two surviving copies of the painting, both show a typical sceletium flower and the characteristic skeletonized leaves which is reflected in the genus name Sceletium, accompanied by the following information, translated from the original Dutch: “This plant is found with the Namaquas and then only on some of their mountains. It is gathered in October and is called Canna. It is held by them and surrounding tribes in as great esteem as the betel or areca with the Indians.” In 1738, Kolben noted kanna (or channa) to be the “greatest Chearer of the Spirits, and the noblest Restorative in the World” [12]. In 1924, Kolben was referencing a plant used by the Khoi for enjoyment, which they “chewed, kept in their mouth for some time, thus becoming excited…” [1]. The traditional use as masticatory is also described by Commelin in 1692 [13], Thunberg ca. 1770 [4], and numerous other sources [1, 6, 12, 14-23].
The Afrikaans vernaculars kougoed and kauwgoed are derived from “kou” (to chew) and “goed” (stuff) and were first recorded in about 1830 [8] and reported to be the leaves of a species of Sceletium [17]. “This native of the Karoo appears to possess narcotic properties. The Khoikhoi, who know it as Kauwgoed, are in the habit of chewing it and become intoxicated, while the farmers use it in the form of a decoction or tincture, as a good sedative” [6]. Meiring reported common use for its soporific effect on young children, relaxing them when suffering from “acidity”. A few drops of fresh leaf juice were given to a child who would consequently rest quietly for a few hours [24]. Hartwich [15] and Zwicky [23] concluded that the indigenous population clearly used the plant more for recreational purposes than as medicine. The earliest mention of the product being used in tinctures and infusions dates from Pappe (1857). Jacobsen [16] specifically states that sceletium is used as tea, as do Van Wyk [21] and Smith et al. [12]. Sceletium as a sedative is used as a tea (infusion or decoction) or tincture. Indigenous healers in Namaqualand use it to treat alcohol abuse, lending to it being called 'onse droë drank' (our dry liquor). No withdrawal symptoms are recorded for chronic use [25]. Mesembryanthemum tortuosum was once a commodity in the Cape, stores in Namaqualand stocked it until the 1990s. To this day, minute quantities added to breast milk are given to infants for colic [4, 12, 19-22, 26].
Past and present indigenous uses of sceletium species [25] include use for:
enhancing sociability, and as a euphoriant or intoxicant.
general well-being, elevating mood, improving memory.
treating alcoholism.
endurance, reducing fatigue, thirst and hunger.
sedation and calming, and for insomnia.
pain, headache and toothache.
nausea, colic, abdominal cramps and constipation.
asthma.
2.4. Preparation
Traditionally, Mesembryanthemum tortuosum is harvested by local people from October through to January. The above ground plant material is collected, crushed with a large stone on a flat rock and the pulp is put into a plastic bag (In former times sheepskin bags were used). The plastic bag is tied to exclude air, and the material is allowed to macerate in the hot sun for eight days with intermittent mixing. It is then spread out on a flat rock to dry in the sun, resulting in the traditional fermented kanna, which is light brown fibrous clumps [25]. In some cases, the fresh foliage or whole plant is simply crushed and placed in the sun to dry, or the fresh plant material is baked in the hot sand under fire [1]. Alternative and more production-oriented local methods include shade-drying the plants or using drying racks.
2.5. Chemistry
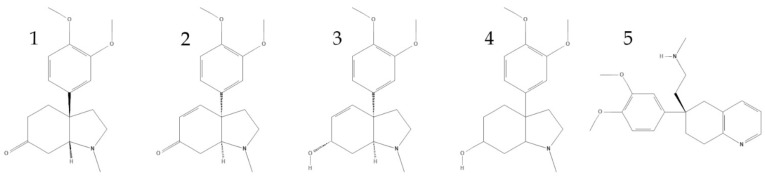
The alkaloid chemistry of M. tortuosum in wild populations is highly variable in terms of both alkaloid content and relative alkaloid composition. Total alkaloid content of wild M. tortuosum can range from 0.05% of dry weight to almost 3.0% in outliers. The average range of total alkaloid content of traditionally favoured wild M. tortuosum varieties is 0.2% for the “mak” (mild) variety to 2% for the “trek” (strong) variety. The major alkaloids in M. tortuosum believed to contribute to the psychoactivity include mesembrine, mesembrenone, mesembrenol, mesembranol, Δ7-mesembrenone, and tortuosamine [25, 27]. Commercial extracts of M. tortuosum for the nutraceutical and pharmaceutical industries need to demonstrate batch-to-batch consistency for both alkaloid content and relative composition. Validated analytical methods have been described for quantifying the major mesembrine-type alkaloids, including mesembrine, mesembrenol, mesembrenone, mesembranol, Δ7-mesembrenone, and epimesembranol [28, 29].
2.6. In-Vitro Pharmacology
A proprietary branded M. tortuosum extract Zembrin® [HG&H Pharmaceuticals; an aqueous-ethanolic dry extract, dry botanical to extract ratio (DER) range ~2:1 (w/w), standardized to contain 0.4% total alkaloids], was confirmed in-vitro to be a serotonin reuptake inhibitor (SRI) with an IC50 on the 5-HT transporter (SERT) of 4.3 μg/ml. Isolated pure mesembrine was found to be the most active alkaloid against the 5-HT transporter (SERT), with a Ki of 1.4 nM. Zembrin® was found to also be an inhibitor of the phosphodiesterase-4 (PDE4) enzyme. Isolated pure mesembrine, mesembrenone and mesembrenol were found to inhibit PDE4B with IC50 values of 7.8 μg/ml, 0.47 μg/ml and 16 μg/ml, respectively [2]. While Harvey et al. [2] did not find a significant activity of Zembrin® or isolated mesembrine alkaloids on acetylcholinesterase or cannabinoid receptors, Lubbe et al. [30] reported activity of a sceletium extract on a cannabinoid receptor 1 (CB-1) receptor binding assay, and compounds other than the alkaloids were thought to contribute to this activity. In the same study, the extract inhibited acetylcholinesterase.
Another study confirmed in vitro the ability of mesembrine, mesembrenone, mesembrenol, and mesembranol to permeate across porcine intestinal, sub-lingual, and buccal tissues both as purified compounds and as crude extracts with water, methanol, and an acid-base as solvents [31].
Another proprietary extract of sceletium with a relatively high content of mesembrine, Trimesemine™ (70% stabilized mesembrine w/w, Botanical Resource Holdings (PTY) Ltd), was found to down-regulate SERT expression similarly to the antidepressant citalopram. In addition, vesicular monoamine transporter-2 (VAMT-2) was upregulated significantly in response to the extract [32]. In an in vitro study with human adrenocortical carcinoma cells, Trimesemine™ altered glucocorticoid, mineralocorticoid and androgen production [33].
Bennett et al. investigated the immunomodulatory effects of Trimesemine™, both basally and in the context of acute endotoxin stimulation, by assessing mitochondrial viability and cytokine release of primary human monocytes in response to being treated with either 0.01 mg/ml or 1 mg/ml extract with and without E. coli LPS stimulation. Sceletium caused increased mitochondrial viability and up-regulated IL-10 release under basal conditions. Decreased mitochondrial viability caused by LPS was completely prevented with sceletium, without negatively affecting the acute inflammatory response to LPS stimulation [34].
2.7. Pre-clinical Studies
Three exploratory studies using milled M. tortuosum plant material in domestic cats and/or dogs brought to a veterinary clinic, both with and without mental disturbances, demonstrated no adverse reactions and positive effects on mood and behaviour at levels of 20-100 mg/kg bw orally daily for between 7 and 180 days [35-37].
In a model of restraint-induced psychological stress, it was found that a dose of only 5mg/kg of sceletium extract (although not stated in the paper, this was Lot #8587 of Zembrin®) given by gavage reduced restraint stress-induced self-soothing behaviour, as well as decreased stress-induced corticosterone levels [38]. This dose is equivalent to a total alkaloid dose of 20 μg/kg bw/day.
The effects of an M. tortuosum alkaloid enriched fraction were examined in the chick anxiety-depression model [39]. In two experiments, male Silver Laced Wyandotte chicks (4-6 days old) were given IP vehicle, imipramine (10 mg/kg), or M. tortuosum fraction (10, 20, 30 mg/kg and 50, 75, 100 mg/kg, respectively) after which distress vocalizations (DVoc) were continuously recorded for 60 mins. The sceletium fraction at 75 and 100 mg/kg showed an anxiolytic effect during the anxiety phase, indicating benefit to some stress-related disorders.
The effect of single doses of sceletium extract Zembrin® on rat brain electrical activity was studied using wireless EEG recordings in free-living rats. Three doses of the sceletium extract Zembrin® and vehicle (0, 2.5, 5.0 and 10.0 mg/kg, equivalent to total mesembrine alkaloids of 0, 10, 20 and 40 μg/ kg) were given by gavage. The resulting electropharmacograms (plotted from Fast Fourier Transformation of the analogue EEG recording for each frequency range) of Zembrin® were compared to the databased electropharmacograms of reference herbal extracts and the first generation pharmaceutical PDE4-inhibitor rolipram. Zembrin® had a similar electropharmacogram to rolipram and the electropharmacograms for extracts of Ginkgo biloba L. and Rhodiola rosea L. The results provide support for future translational clinical studies investigating Zembrin® in the treatment of Mild Cognitive Impairment, and depression [40].
2.8. Clinical Studies
To date there have been no clinical studies of Mesembryanthemum tortuosum or extracts in a clinical population. The formal clinical studies reported on in this section have been conducted in healthy volunteers. A small number of clinical case reports have been published reporting on the successful use of capsules and tablets of milled M. tortuosum plant material, and M. tortuosum extract Zembrin® for treating major depression and generalized anxiety in clinical practice. Over the last decade a number of psychiatrists have integrated the use of standardized and characterized sceletium extracts into clinical practice, pioneered by Dr. Olga Gericke in Cape Town, and Dr. Richard P. Brown in New York who has prescribed sceletium in more than 30 patients during the past four years [25, 41].
Acute effects of Zembrin® were studied in a double-blind, placebo-controlled, cross-over pharmaco-fMRI model investigating anxiety-related activity in the amygdala and the connected neurocircuitry. 16 healthy university student participants were scanned while performing an emotion-matching task under low and high perceptual loads. Amygdala reactivity to neutral and fearful faces was attenuated, for Zembrin® compared to placebo in the bilateral amygdala (p < 0.01) after a single 25 mg (equivalent to 100 μg total mesembrine alkaloids) dose of Zembrin®. Amygdala-hypothalamus coupling was also reduced, as shown by connectivity analysis on the emotion-matching task. For the first time, attenuating effects of a sceletium extract on the threat circuitry of the human brain was demonstrated, and supporting evidence provided for the extract’s anxiolytic potential by attenuating subcortical threat responsivity [42].
In a randomized double-blind placebo-controlled cross-over clinical study normal healthy older adults (total n = 21) (mean age: 54.6 years ± 6.0 years; male/female ratio: 9/12) received either a 25 mg capsule of M. tortuosum extract Zembrin® (equivalent to 100 µg total mesembrine-alkaloids) or placebo capsule once daily for three weeks. The primary endpoint was to examine the neurocognitive effects of the extract using the CNS Vital Signs battery of tests. Zembrin® at 25 mg daily dosage significantly improved executive function (p < 0.022) and cognitive set flexibility (p < 0.032) compared with the placebo group. Positive changes in mood and sleep were also found, and the extract was well tolerated [43].
In a randomised, double-blind placebo-controlled clinical trial, the effect of a single dose of 25 mg or 50 mg of M. tortuosum extract Zembrin® (equivalent to 100 μg and 200 μg of total mesembrine alkaloids, respectively) was studied in comparison to placebo in sixty healthy male (n = 30) and female (n = 30) subjects between 40 and 75 years of age. The investigation aimed at characterizing the activities of the two doses of extract in comparison to placebo in terms of brain electrical activity during cognitive as well as emotional challenges. A combination of EEG and eye tracking was used, which allows for analysis of EEG spectral changes over very short time epochs of 364 ms duration. In the presence of the sceletium extract, spectral EEG analysis revealed statistically significant increases of delta (p < 0.01 during the cognitive challenge of arithmetic calculation and during watching a monotonous animal video, an emotional and attentional challenge) and theta spectral power (p < 0.10) during these same challenges) within the frontal brain. This indicates a positive effect of the extract on the electrical activity of the brain during cognitive processing. Further, alpha1 and alpha2 spectral power in the frontal brain was increased during challenges. Such increases of spectral alpha1 power may be interpreted as a greater degree of calmness while increases in alpha2 waves have been related to memory. Beta2 waves increased during mental performance in the presence of the 50 mg dosage of the extract, but not in the 25 mg dose, in parietal, occipital and temporal brain regions. It was concluded that in comparison to placebo, the sceletium extract induced frequency changes in the brain, which have been related to enhanced attention and memory. These results may represent a positive action of Zembrin® on cognitive and emotional processes in the brain [44].
In a randomized, double-blind, placebo-controlled clinical study, the effect of 25 mg or 50 mg of M. tortuosum extract Zembrin® (equivalent to 100 μg and 200 μg of total mesembrine alkaloids, respectively) was studied in comparison to placebo after daily repetitive intake for six weeks. Sixty healthy male (n = 32) and female (n = 28) subjects between 50 and 80 years old were recruited. Six cognitive tests were performed: number connection and number identifying test, calculation performance test, d2-test, memory test, and reaction time test, and three questionnaires included the Hamilton Anxiety Rating Scale (HAM-A), Profile of Mood States, and a sleep questionnaire. Increases of delta activity during performance of the d2-test, the number identification and number connection tests in the fronto-temporal brain region were revealed. Higher theta activity was seen during relaxation and performance of the d2-test after intake of 50 mg of Zembrin®. Statistically relevant increases of alpha1 spectral power were seen in the relaxed state. Statistically significant improvement was seen in the arithmetic calculation test and number connection test. The HAM-A anxiety score showed a statistically significant decrease (p = 0.03) after six weeks intake within the 50 mg Zembrin® group. The results indicate that Zembrin® improves some aspects of cognitive function and decreases anxiety in healthy older adults [45].
In two small randomized, double-blind, placebo-controlled clinical studies, the effect of a single dose of 25 mg of extract M. tortuosum (Zembrin®) on stress and anxiety was studied in 26 healthy male volunteers (mean age 19.6 years). Post hoc analysis revealed a difference for the extract group at prestress (p = 0.024, d = 1.11) with the anxiety level being significantly lower in the Zembrin® group. No significant treatment effects were found on any other outcome measure [46]. The studies were underpowered and used a single dose of only 25 mg extract. Future studies should be adequately powered and include a higher dose arm and repeat dosing.
In a randomized, placebo-controlled clinical study, the effect of 8 days supplementation of 25 mg extract M. tortuosum (Zembrin®) taken once daily was studied in 60 healthy, recreationally trained young male (n = 48) and female (n = 12) adults. The study looked at the effect on alertness and ‘energy’ using a visual analogue scale (VAS), on mood using Profile of Mood States (POMS) questionnaire, and at reactive performance assessments using multiple object tracking and visual tracking speeds on the Neurotracker 3D multiple object tracking device, reaction time was measured for the upper body on the Dynavision D2 Visuomotor training Device and reactive agility was measured using the FITLIGHT trainer device. Compared to placebo there was no significant effect of the sceletium supplementation on VAS, or POMS and no difference in average reaction time. There was significant effect (p < 0.001) of the supplement compared to placebo for reactive agility requiring decision making on the direction of movement [47]. This exploratory study had several flaws, and no firm conclusions on functionality can be drawn from it.
2.9. Dosage Considerations
Traditional use as a masticatory suggests that a daily dose of sceletium is between 500 and 1,500 mg. The African Herbal Pharmacopoeia reports a daily total alkaloid intake of between 2 and 12 mg daily [27]. However, the total alkaloid content of the plant is very variable and may be from 0.05 to 2.3% of the dry weight. Thus, the amount of plant material used as a masticatory can be expected to contain 0.25-34.5 mg of total alkaloids. Teas use about 500 mg of sceletium per day, which at 2% alkaloid content would yield about 10 mg total alkaloids if fully recovered into the herbal tea liquid. Dietary supplement products in the Republic of South Africa and online markets deliver between 50 and 680 mg of sceletium (both dried aerial parts and extracts) daily with a highly varied alkaloid content (1-13.6 mg total alkaloids at 2%).
Clinical studies on Zembrin® used a dose of 25-50 mg daily of Zembrin® (equivalent to 50-100 mg of the cultivated selection of plant material). Since Zembrin® is standardized to 0.4% total alkaloids, the total alkaloids ingested daily in the clinical studies ranges from 100-200 μg. Clinical case reports [41] corroborate treatment of anxiety and depression using 75-100 mg Zembrin® per day, which is a daily dose of total alkaloids of 300-400 μg.
A wide range of total mesembrine alkaloids are ingested from traditional use of sceletium plant material, and from the diverse manufactured sceletium supplements sold via Internet. The use of standardized and characterized plant material or extracts, with quantified total alkaloid content and relative alkaloid composition, is essential for this botanical to ensure safety, efficacy, and reproducibility.
2.10. Safety
The safety of M. tortuosum has been evaluated in several human clinical studies, and in animals.
2.10.1. Animal Studies
Hirabayashi et al. [35, 36] and Hirai et al. [37] found no adverse effects with sceletium powder (assuming 2% alkaloids) in dogs treated with 20 mg/kg per day, in dogs treated with up to 90 mg/kg per day, and in cats treated with 100 mg/kg per day.
Mesembrine demonstrated analgesic properties without abuse liabilities or ataxia, and a crude extract of the plant, containing 1.5% mesembrine, showed antidepressant properties but did produce ataxia [48].
Sceletium extract Zembrin® was studied in a 14-day repeated dose oral toxicity study conducted at 0, 250, 750, 2500, and 5000 mg/kg body weight/day (equivalent to total mesembrine alkaloids of 0, 1, 3, 10, and 20 mg/kg bw/day). A 90-day sub-chronic repeated dose oral toxicity study was conducted on sceletium extract Zembrin® at 0, 100, 300, 450, and 600 mg/kg bw/day (equivalent to total mesembrine alkaloids of 0, 0.4, 1.2, 1.8, and 2.4 mg/kg bw/day). Since sceletium is known to be psychoactive, a functional observation battery, including spontaneous locomotor activity measured using the LabMaster ActiMot light-beam frames system, was employed. Parameters such as locomotion, rearing behaviour, spatial parameters and turning behaviour were investigated. No mortality or treatment-related adverse effects were observed in the rats in the 14- or 90-day studies. In the 14- and 90- day studies, the No Observed Adverse Effect Levels (NOAEL) for Zembrin® were 5000 and 600 mg/ kg bw/d, respectively, the highest dose groups tested [3], equivalent to a NOAEL for total mesembrine alkaloids of 20 mg/kg bw/day and 2.4 mg/kg bw/day.
2.10.2. Human Studies
The safety and tolerability of two doses (8 mg and 25 mg once daily) of Zembrin®, was evaluated in 37 healthy adult volunteers over a three-month period in a randomized, double-blind, parallel-group, placebo-controlled study. Of the 37 subjects, 12, 12, and 13 subjects received 8 mg extract, 25 mg extract and placebo treatment, respectively. Safety and tolerability were assessed using vital signs, physical examination, 12-lead electrocardiogram (ECG), haematology, biochemistry, and urinalysis, and adverse events (AEs). There were no apparent differences between the three treatments with any of these criteria. The most commonly reported AE was headache, with some abdominal pain and upper respiratory tract infections, all with greater incidence in the placebo group than in the treatment groups. Efficacy was not assessed, but unsolicited positive effects on well-being were noted by some participants taking extract, including improved coping with stress and sleep [49].
The safety and tolerability of the same extract was further assessed (in addition to its neurocognitive effects) in a randomized double-blind placebo-controlled cross-over study. 21 normal healthy subjects (mean age: 54.6 years ± 6.0 years; male/female ratio: 9/12) received either 25 mg extract or placebo once daily for three weeks. CNS Vital Signs and Hamilton depression rating scales (HAM-D) were measured, and side effects monitored. The 25 mg daily dosage significantly improved cognitive set flexibility and executive function, compared with placebo, and positive changes in mood and sleep were found. The extract was well tolerated [43].
2.10.3. Herb-drug Interaction Potential
There are no reports to date of severe adverse reactions or herb-drug interactions and no in vivo or in vitro studies implicating M. tortuosum in drug interactions. Nonetheless it would be wise to avoid pharmaceuticals which are known to alter serotonin uptake or release, i.e., drugs used to treat depression and other psychiatric disorders. These include selective serotonin reuptake inhibitors (SSRis, e.g., fluoxetine, paroxetine, sertraline, citalopram, and escitalopram) as well as the serotonin and noradrenaline reuptake inhibitors (SNRIs, e.g., duloxetine, venlafaxine). However, the mode of action of many antidepressants is complex and as a general principle, should not be used concurrently with sceletium. Some pharmaceuticals, such as roflumilast, and other natural-occurring phytochemicals such as luteolin, are known to have PDE-4 inhibitory activity, so potential for herb-drug interaction should be borne in mind as sceletium extracts become more widely available. The first-generation PDE-4 inhibitor rolipram had undesirable side effects of nausea and vomiting limiting its use, however roflumilast, a next generation selective PDE4 inhibitor without these effects was approved in 2010 in the European Union for treating severe COPD associated with chronic bronchitis, and in 2011 was approved by the US Food and Drug Administration (FDA) for reducing COPD exacerbations.
The metabolism of the sceletium alkaloids mesembrine and mesembrenone was investigated in rat urine and pooled human liver preparations [50]. The metabolites were identified using gas chromatography-mass spectrometry (GC-MS) and liquid chromatography coupled to linear ion trap high resolution mass spectrometry (LC-HR- MSn). Both alkaloids were O- and N-demethylated, dihydrated, and/or hydroxylated at different positions. Most of the phase I metabolites identified in rat urine could also be detected in the human liver preparations. After a low dose application of mesembrine, mainly the O- and N-demethyl-dihydro, hydroxy, and bis-demethyl-dihydro metabolites, and in case of mesembrenone only the N-demethyl and the N-demethyl-dihydro metabolite, could be detected in rat urine.
The O-demethylation of mesembrine was catalysed by CYP1A2, CYP2B6, CYP2C19, and CYP2D6, and the N-demethylation by CYP1A2, CYP2B6, CYP2C19, CYP2D6, CYP3A4, and CYP3A5. The O-demethylation of mesembrenone was catalysed by CYP2C9, CYP2C19, and CYP2D6, and the N-demethylation by CYP2C19, CYP2D6, and CYP3A4 [50]. The clinical significance of this metabolism is not yet known.
3. REGULATIONS
Many herbal ingredients from indigenous cultures and traditional paradigms of medicine have made a successful career in first-world markets as foods, food supplements, cosmetics or medicines. Historically, it was the explorers, the settlers and the traders, who more or less freely dispersed the ingredients of their traditional apothecaries. Trade, migration and, last but not least, entrepreneurship contributed to establishing elements of Ayurveda, TCM, Unani, and Kampo etc. in markets like Europe and the USA at a time when these markets were largely unregulated. Those were also the heydays for Southern African traditional medicines such as Umckaloabo [51], devil’s claw, buchu and many more, as well as food and beverage ingredients such as rooibos [Aspalathus linearis (Burm.f.) R.Dahlgren], etc. [21, 52]. Spirited individuals introduced traditional remedies primarily into the European marketplace and subsequently others. These remedies, over time, transformed into well-researched phytopharmaceuticals.
More recently, and despite a plethora of further interesting “candidates” [53], this trend has slowed, primarily due to increasingly stringent regulations affecting First World markets. From a commercial point of view, the higher the barrier of entry, the greater are the investment needs. In the days of ethical product development, governed by the principles of the Nagoya protocol, patenting as a means to protect such investment has become controversial. While Access-Benefit-Sharing (ABS) agreements protect traditional knowledge at its source, it has become increasingly difficult to protect proprietary (manufacturing) knowledge in the marketplace. As a result, manufacturers shy away from product development with new botanical ingredients, because economic opportunity does not justify the investment. This dilemma is - to a varying degree - exasperated by national regulations. Regulatory barriers as well as regulatory “loopholes” form a highly heterogeneous landscape of opportunity, ranging from relatively open to almost entirely closed systems. Consequently, one and the same product may have to be force-fitted into different national regulatory categories, all the way to where best regulatory intentions prevent it from reaching the consumer altogether, because the cost associated with market entry becomes forbidding.
It must be stressed that it is not the intention of the authors to polarize between industry and regulators but rather to initiate a thought process and consequent discussion which may lead to strategies for resolving or alleviating aforementioned problems. In the following, sample markets, their regulatory categories and whether and how sceletium products may or may not fit into them are described.
3.1. Access to Sceletium in the Country of Origin
Environmental management in South Africa is governed by the National Environmental Management: Biodiversity Act 10 of 2004 (NEMBA) [54]. NEMBA gives effect to the provisions of the Nagoya Protocol on a national level and is managed by the Department of Environment Forestry and Fishery (DEFF). It stipulates the management and conservation of biological diversity within South Africa, as well as the use of indigenous biological resources in a sustainable manner, the fair and equitable sharing among stakeholders of benefits arising from bioprospecting involving indigenous biological resources. It also regulates the creation and maintaining of a list of threatened or protected species (TOPS).
Chapter 6 of NEMBA deals with provisions for Bioprospecting, Access and Benefit-Sharing (BABS) in South Africa. Associated with this chapter is the BABS Regulation of 2008 as amended in 2015 [55-57]. The purpose of these regulations is to prescribe the notification process for the discovery phase and the permit system applying to biotrade, bioprospecting and export of indigenous genetic and biological resources. It also provides details for benefit-sharing (BSA) and material transfer agreements (MTA).
NEMBA is currently under revision - specifically Chapter 6. The simplified and streamlined revised version is hoped to be complete in 2021.
ABS practice is further governed by the Indigenous Knowledge Systems Bill which was finally signed into law in August 2019 as the “Protection, Promotion, Development and Management of Indigenous Knowledge Act, 2019” [58]. This Act is a sui generis piece of legislation that endeavours to provide legislative protection for indigenous knowledge and its commercialization. It recognizes “indigenous knowledge” as a form of intellectual property.
The Act defines a new concept of “indigenous knowledge” as “knowledge which has been developed within an indigenous community and has been assimilated into the cultural and social identity of that community and includes (a) knowledge of a functional nature, (b) knowledge of natural resources as well as (c) indigenous cultural expressions”. It is important to note here, that all three conditions (a), (b) and (c) have to be met to qualify as “indigenous knowledge”.
The Act makes provision for the establishment of the National Indigenous Knowledge Systems Office (NIKSO). A repository of “indigenous knowledge” has been started under the guidance of the Department of Science & Innovation. In NIKSO, the DEFF, the DSI and the Department of Trade, Industry and Competition (DTIC) will in future jointly adjudicate on questions of traditional and indigenous knowledge pertaining to bioprospecting and biotrade. So far, there have been no regulations published to enact this legislation - this is expected during 2021.
Indigenous knowledge is seen as a national asset that needs to be fostered, developed and protected. One of the purposes of NIKSO is in “facilitating the redress of rights and benefits to indigenous communities which have previously been deprived of such rights and benefits”. The Act has therefore a strong political agenda of empowerment and transformation of South African society.
All utilization of indigenous biological or genetic resources in South Africa falls under NEMBA and an application for the use of any of these needs to be made prior to accessing and using the resource. Every entity in the supply and value chain from harvester / grower / trader / processor / manufacturer needs to have some form of permit to access and utilize indigenous biological resources. MTAs and BSAs to access the biological resource and for related TK must be concluded at every level of transaction.
The current Act and Regulations recognizes four distinctly different areas of utilization and where permits have to be obtained for: (a) Discovery Phase Research, (b) Bioprospecting, (c) Biotrade and (d) Research other than bioprospecting (e.g., taxonomy).
An applicant can be any natural or legal person being registered in South Africa. Foreign entities applying for a permit need to do so jointly with a South African natural or legal person e.g., a company, legal firm or research institution. A specific application form for each type of permit needs to be filled in, accompanied by supporting documents.
Discovery Phase Research relates to research on indigenous resources and activities pertaining to development or application of such resources, at a point where the nature and outcome of potential commercialization is not yet clear.
Once the research has been concluded and commercialization is envisaged, a bioprospecting permit has to be applied for. Bioprospecting is defined as “any research or development of indigenous biological or genetic resources for commercial or industrial exploitation and includes:
the systematic search, collection or gathering of biological resources.
the utilization of traditional knowledge or uses for R&D purposes.
research, development or modification of any traditional uses for commercial purposes.
the trading and exporting of biological resources in order to develop and produce products, such as drugs, industrial enzymes, food flavours, fragrances, cosmetics, emulsifiers, oleoresins, colours, extracts and essential oils etc.
the commercialization of the research which includes activities such as filing of a patent, obtaining or transferring intellectual property rights.
commencing product development, conducting of market research and seeking pre-market approval for products.
cultivation, propagation, cloning or other means to develop and produce products” [58].
In cases where only trade in indigenous biological or genetic resources takes place, a biotrade permit needs to be applied for. “Biotrade means the buying and selling of milled, powdered, dried, sliced or extract of indigenous genetic and biological resources for further commercial exploitation” [58]. It is important to note here that a simple plant extract e.g., a tincture, an essential oil, a pressed vegetable oil or similar will fall into this category - these materials are fractions of the plant and are simply removed from the plant and not altered.
The implementation of the Nagoya Protocol has a very strong political component. It is intended to address the wrongs of the past and to be a tool for poverty alleviation as well as to bring marginalized rural people into the economic mainstream.
The Nagoya Protocol typically excludes commonly used food plants. In South Africa, this is not the case - as can be seen in the recently concluded bioprospecting negotiations around rooibos tea. Also, in deviation from common practice in other countries, there is no cut-off date e.g., the date that the legislation implementing the Nagoya Protocol was ratified nationally - in South Africa all biological or genetic resources - including food plants - fall under NEMBA regardless of when they were accessed or utilized for the first time.
The ownership of traditional knowledge is often not well defined. Different interpretations do exist amongst traditional groupings that claim to be the custodians and therefore the rightful owner of traditional knowledge. In such cases, the relevant Government Departments (DEFF and DSI) can be called upon to provide clarity.
Summarily, every time that an indigenous ingredient changes hands and ownership, an MTA and BSA need to be concluded. This leads to a very cumbersome and complex web of documentation and agreements that have to be carefully designed and maintained during the duration of the validity period of a given permit. Since more than one indigenous community has claimed TK and thus “ownership” of sceletium, any attempt to obtain the necessary permits for harvest, processing and export will kickstart a lengthy administrative process, which, for anybody ethical enough to follow, in a best-case scenario, will slow down, and in some cases, even inhibit any commercialization attempt. A lot of trade in indigenous biological resources remains “illegal” because trade is not yet tightly monitored by authorities.
3.2. Sceletium Products in the European Union
To this day, Europe is a global leader in the formulation, extraction, manufacture of botanical ingredients for herbal medicines and supplements, plant-based fragrances, flavours and cosmetics. In addition to traditional European herbal medicine practice, some of the most important “alternative” systems of medicine emerged from Europe, such as homeopathy, and anthroposophy. This long and extensive tradition has resulted in an equally pronounced focus on safety and efficacy of herbal products. A resulting array of increasingly complex rules and regulations has developed in European countries over the last century concerning the manufacture and dissemination of herbal medicines, cosmetics and food products. The creation and expansion of the European Union brought with it substantial challenges to harmonization of regulations concerning medicines, food and cosmetic products, as many member states to this day prefer to consider health and safety of their citizens a national concern and not one to be surrendered to a central EU administration. Regulations discussed in the following oftentimes have been subject to acrimonious struggles between desiring and needing harmonization within the EU and defending and retaining national authority concerning health and safety. As all centralized EU legislation needs to be ratified by its members, both the speed by which member states adopt regulations and their interpretation in a national context vary widely. As a result, regulatory approval can be faster and easier in some member states than others [59].
Most botanical raw materials (Herbal Drugs) can be traded/exported/imported without specific requirements to safety and quality. Nonetheless, Good Agricultural and Collection Practices (GACP) ought to be adhered to if the botanical will be used as an active ingredient of a registered or licensed herbal medicinal product [60] and once they are processed into finished products stricter and category specific requirements apply. Intermediate products intended for further processing do not fall under the definition of a finished product and thus not subject to marketing authorization. However, to ensure their consistent quality, processing of intermediate products for medicinal, food or cosmetics products is governed by Good Manufacturing Practices (GMP) [61]. Furthermore, products containing botanicals non-native or novel to Europe must fully comply with EU legislation, specifically with requirements concerning quality, safety and efficacy.
Food ingredients and food products, including food supplements are defined as “Any substance or product, whether processed, partially processed or unprocessed, intended to be, or reasonably expected to be ingested by humans” [62]. Foods are split into subcategories including foods and foodstuffs as defined in national food safety legislation; food (dietary) supplements covered by Directive 2002/46/EC as amended [63]; food for specific groups are covered by Regulation 609/2013 as amended [64], distinguishing foods for specific medical purposes, total diet replacement for weight reduction, and foods for infants and young children, also being regulated in Regulation 2016/127 as amended [65]; and novel foods which are regulated in Regulation 2015/2283 [66]. Novel foods are ingredients without history of significant consumption within the EU prior to May 1997. To market a novel food, companies must apply for authorization, presenting evidence and undergo a safety assessment. The regulation differentiates between “typical” novel foods (article 10) and traditional foods from third countries (article 14), which originate from primary production (i.e., are minimally processed) and have history of safe food use, “confirmed with compositional data and from experience of continued use for at least 25 years in the customary diet of a significant number of people in at least one third country” [66]. Food ingredients, being additives (including sweeteners), flavourings, solvents and genetically modified organisms (GMOs), are covered by other regulations. Health claims for food products need to be authorized according to Regulation 1924/2006 as amended [67], articles 13.1, 13.5 and 14. Claims to treat, prevent or cure disease are prohibited for food. The European Food Safety Authority (EFSA) is responsible for assessing and verifying the scientific merit of the health claims.
Core regulatory categories open to herbal medicinal products are Traditional Herbal Medicinal Products (THMP), well-established medicinal use (WEU) and botanical drug with full market authorization (MA), all characterized in Directive 2004/24/EC, and Directive 2001/83/EC as amended, respectively [68, 69]. A simplified procedure for registration of THMP applies to herbs, and nutrients, i.e., vitamins and/or minerals if ancillary, requires evidence of efficacy based exclusively on long term use (30+ years preceding application, 15+ years of use in EU), needs indication(s) suitable for over-the-counter (OTC) use without supervision based on traditional use only, has to be of specified strength and posology (oral, external, or inhalation only). Traditional Herbal Registrations (THR) are intended to be obtained under national rule, nonetheless, select EU member states offer alternative procedures including mutual recognition, centralized and decentralized procedures as specified in the Annex to Regulation 726/2004 as amended [70] Notice to Applicants, Volume 2, Chapter 1. A procedure for registration of WEU herbal medicinal products requires presentation and assessment of full pharmaceutical and quality information with bibliographic evidence for efficacy. Health claims can be based on literature and established use. A MA is a complete and independent, stand-alone drug license application, requiring full drug development procedure, full application (pharmacological / toxicological, clinical and quality information), and clinical evidence for efficacy required (trials), leading to strong health claims in accordance with clinically proven efficacy (study results).
The procedural aspects concerning authorization procedures for food additives and flavourings are laid down in Regulation 1331/2008 [71] and further elaborated in Regulation 234/2011 [72].
Cosmetics in the EU are governed by Regulation 1223/2009 as amended [73], in force since 2013. It defines cosmetics as “any substance or mixture intended to be placed in contact with the external parts of the human body (epidermis, hair system, nails, lips and external genital organs) or with the teeth and the mucous membranes of the oral cavity with a view exclusively or mainly to cleaning them, perfuming them, changing their appearance, protecting them, keeping them in good condition or correcting body odours” [73]. Core aspects of this regulation address safety requirements and undesirable effect reporting, among others, as well as a centralized notification procedure for all cosmetic products placed on the EU market.
This regulatory landscape creates a conundrum for certain ingredients such as sceletium. In the food (and food supplement) category, it would be considered ‘novel’, however, despite it being regulated as a food in its country of origin, competent authorities may likely not consider it suitable due to its predominant history as a traditional herbal medicine. At the same time, as it has not been present in the EU marketplace for at least 15 years, and likely also may not be considered suitable for OTC products, it fails to qualify as a THMP. It has no flavour, fragrance or cosmetic uses. This only leaves one category for legal market access, through MA. Drug development, in turn, requires substantial investments and bears substantial risks to such investments. The amount of research already conducted and in the public domain gives little “appetite” to market forces that would have the ability to stem such investment as there is next to no opportunity to protect product development from competition and ensure profitability. Thus, the ingredient becomes a “hot potato”, while interesting, unique and potentially beneficial in a therapeutic setting, nobody reasonably can or wants to “touch it”. And indeed, there are no legal products containing sceletium in the European marketplace to this date.
3.3. Sceletium Products in the USA
Regarding the Convention on Biological Diversity (CBD) and the aforementioned Nagoya Protocol, the United States is the only country in the entire world that has not ratified the treaty. Therefore, American companies are generally unaware of ABS regulations of other countries.
The regulatory frameworks for finished products in the United States, generally relevant for botanical raw materials or their processed forms such as extracts, include conventional food, dietary supplement, medical device, medical food, over-the-counter (OTC) botanical drug, OTC homoeopathic drug, prescription (Rx) botanical drug, and non-drug cosmetic [74]. Somewhat less relevant but still possible for botanical ingredients are the frameworks for food for special dietary uses, and special dietary and nutritional additives.
Neither the botanical drug route [75] nor the new drug application route appear to be affordable or practical for the marketing of sceletium ingredients and products in the US market. In the 21st century, the US FDA has approved only two botanical drugs (out of over 600 applications). Both drugs are prescription-only medicines with narrow indications for use, (1) an ointment containing a semi-purified extract of green tea [Camellia sinensis (L.) Kuntze] leaf for treating genital/perianal warts; and (2) prepared dragon’s blood (Croton lechleri Müll.Arg.) latex for treating HIV-related diarrhoea. And, in the same timeframe, there has been just one “new drug” approval for a substance of botanical origin, a cannabidiol (CBD) oral solution, extracted and purified from Cannabis sativa L.; also, prescription medicine indicated for the treatment of seizures associated with, Lennox-Gastaut syndrome and Dravet syndrome. Both are rare and severe forms of epilepsy [76]. Thus, most oral ingestion botanical substances in the US market are classified as botanical dietary supplements, in the space between food and drug [77].
For a botanical substance to be used as an ingredient of a conventional food or beverage product, it must be considered by the FDA to be “Generally Recognized As Safe” (GRAS) for it intended use, i.e. there should be (a) evidence of common use of the substance in a conventional food product prior to January 1958; or (b) premarket approval from the FDA for the substance as a new food additive in the meantime; or (c) a positive evaluation filed by FDA of a voluntarily submitted GRAS Notice application; or an (d) Independent Conclusion of GRAS status (formerly known as a “self-determination” of GRAS status). The FDA makes no distinction between a GRAS Notice submitted to the agency and an Independent Conclusion of GRAS status [78].
Other types of food products in the United States include dietary supplements and medical foods. In the case of botanical dietary supplements, passage of the Dietary Supplement Health and Education Act of 1994 (DSHEA) provided a dividing line in time between so-called Old Dietary Ingredients (ODIs) and New Dietary Ingredients (NDIs). ODIs have evidence of having been marketed in the United States as a component of a dietary supplement type product prior to October 15, 1994, while NDIs do not have such evidence of use as a dietary supplement prior to the passage of DSHEA. An enterprise that intends to market an NDI-containing dietary supplement product in most cases must submit a premarket New Dietary Ingredient Notification (NDIN) to the FDA for review and approval [79]. Foods for special dietary uses are those that, as per 21CFR §105.3 supply particular dietary needs which exist by reason of a physical, physiological, pathological or other condition (e.g. convalescence, pregnancy, lactation, allergic hypersensitivity to food, underweight, and overweight); or by reason of age (e.g. infancy and childhood); or to supplement or fortify the ordinary or usual diet with any vitamin, mineral, or other dietary property. Medical food products are foods, as defined in the Orphan Drug Act, which are “formulated to be consumed or administered enterally or orally under the supervision of a physician, and, which is intended for the specific dietary management of a disease or condition with distinctive nutritional requirements” [80]. Kelp (Macrocystis pyrifera, Laminaria digitata, L. saccharina, and L. cloustoni) is an example of a special dietary and nutritive additive in foods taken for iodine deficiency [81].
In February of 2011, GRAS affirmation (Independent Conclusion of GRAS Status) was confirmed for a very specific extract of M. tortuosum and the marketers of Zembrin® announced entry into the US market in 2012 [82]. Although components of a dietary supplement product do not need to be GRAS for their intended use, GRAS substances should generally be acceptable for use in dietary supplement products [83].
It is also possible that the submission of an NDIN for botanicals would not be necessary due to documented evidence of their use in or as conventional food since the 1960’s, albeit not necessarily in the US population.
There remain grey areas in US food regulations that are intended to differentiate GRAS substances (whether notified or self-affirmed), ODIs and NDIs. While this provokes understandable differences in interpretation, it also provides some degree of uncertainty for product marketing companies.
With regard to sceletium-containing dietary supplements, there are over 40 products listed in the National Institutes of Health Dietary Supplements Label Database [84]. There are also OTC homoeopathic drug products offered at various dilutions [85].
Other than minor use in some homoeopathic OTC drug products, sceletium is not found in the US market as a component of botanical drug products (OTC or Rx) or of new drug products.
3.4. Sceletium Products in Australia
Medicinal plant ingredients in Australia are primarily regulated as ‘complementary medicines’ when they are intended for therapeutic use. While some medicinal plants are also found in the food category, it is generally expected that substances sold as foods are a ‘traditional food’, meaning that they have a long history of use in Australia and New Zealand (NZ) as food, and are sold for consumption primarily as a food, rather than sold for therapeutic use. If they are considered a ‘non-traditional food’ in Australia and NZ, they may be deemed a ‘non-novel food’ or a ‘novel food’ by the statutory authority ‘Food Standards Australia New Zealand’ (‘FSANZ’) that sets food regulations within the Food Standards Australia New Zealand Act 1991. A novel food is a non-traditional food that requires an assessment of the public health and safety considerations, particularly having regard to the potential for adverse effects in humans and other key aspects of processing and consumption.
Generally, most businesses seeking to supply a new herb for therapeutic purposes within Australia will enter the complementary medicines pathway, regulated by the Therapeutic Goods Administration (‘TGA’), the body that regulates all medicines and medical devices under the Therapeutic Goods Act 1989. All medicines regulated through the TGA are included onto a national database, the ‘Australian Register of Therapeutic Goods’ or ‘ARTG’. There are three possible categories in which complementary medicines can be entered onto the ARTG:
‘Listed’ Medicines: the most common category. There are approximately 11,000 listed medicines on the ARTG. This category has a list of ingredients that are pre-assessed for safety and quality and therefore deemed to be lower risk, known as ‘permissible ingredients.’ They must not be scheduled in the Poisons Standard at the permitted quantity. Some herbs are permitted for use, but they may have a restriction on an herbal component - for example, cinnamon extracts are not permitted to contain more than 0.001% of coumarin, as coumarin is scheduled in the Poisons Standard. The Listed Medicine category also has a list of therapeutic ‘permissible indications’, therapeutic uses that are low risk and therefore suitable for consumer self-selection. They can refer to health maintenance or enhancement, or the symptomatic relief of non-serious conditions only. Companies can select to create a Listed Medicine by creating an online ARTG application for the product and selecting permissible ingredients and permissible indications. They also must select manufacturers that have been approved under the TGA’s manufacturing standards, which is a GMP system of controls under the international PIC/S scheme (Pharmaceutical Inspection Co-operation Scheme) for medicinal products. The individual product does not undergo pre-evaluation by the TGA before it can be supplied on the Australian market.
‘Listed Assessed’ Medicines is a newly introduced category waiting to be utilized. It uses the same pre-assessed permissible ingredients but must include an ‘intermediate level’ therapeutic indication, such as relief of symptoms of a serious condition, or the prevention/alleviation of a non-serious condition. The evidence for the indication must be pre-assessed by the TGA.
‘Registered medicines’ contain either a high-level claim (such as treatment of a condition) or an ingredient that is included in the Poisons Standard (for example, an herb, vitamin, mineral or other substance that is restricted entirely or restricted in high doses). Some registered medicines are only permitted for sale pharmacies, or by prescription from a medical practitioner. They are fully assessed for safety, quality and efficacy before supply to the market There are between 40 and 50 registered complementary medicines.
Mesembryanthemum tortuosum/Sceletium tortuosum is not currently included on the list of pre-assessed ‘permissible ingredients’ that may be used in Listed medicines, and it is not included in any Registered medicines. It has not been included in the Poisons Standard as a restricted substance. Nor has it been assessed as to its novel food status. Accordingly, M. tortuosum would need further evaluation to determine its suitability for use, or requirements on permissible use in Australia before it could be supplied.
Where a person submits the safety and quality data as part of an application to the TGA to have a new substance approved for use in Listed Medicines, the applicant is eligible to claim two years exclusive use of a substance (or to approved licensees) in Listed Medicines. In December 2019, the TGA announced that some assessment reports by comparable overseas bodies could be used by the TGA to replace a full TGA evaluation for either safety, quality, or efficacy. Listed comparable overseas bodies include the European Food Safety Authority (EFSA), the European Medicines Agency (EMA), and Health Canada.
The safety profile of a substance, if it is approved for use, might be subject to specific restrictions. Restrictions are based on known safety or quality parameters and can include the quantity of the substance allowed in the daily dose, the plant part, the preparation type, the solvent medium for extracts, a limitation on certain components within an herb, or a limitation on frequency of dose.
Psychotropic substances are highly likely to attract more scrutiny in relation to safety and safety-related restrictions to ensure that the product is used appropriately by the community and reduce the risk of any adverse events. Australia is known to have tighter restrictions on herbal medicinal products with psychotropic effects including caffeine-containing herbs, Piper methysticum G.Forst. (kava) and Cannabis sativa L. (cannabis products).
3.5. Sceletium Products in Canada
Though there are several ways in which herbal medicines and ingredients can come to market in Canada, such as prescription drugs and supplemented foods, the majority of these products are regulated as Natural Health Products (NHPs). Considered a subset of drugs under Food and Drugs Act of 1985, NHPs are captured by the Natural Health Products Regulations (NHPR) These are a specific set of regulations developed to reflect the distinct nature of the products and complexity of the sector.
The NHPR came into effect in January 2004 but given the new challenges faced in regulating such a diverse sector as well as the large number of products to be regulated, complete implementation did not occur until 2014. Contained with the NHPR are provisions outlining such things as the definition of an NHP and the labelling and importation of NHPs together with parts dealing with specific elements of the framework notably product licenses, site licenses, good manufacturing practices and clinical trials including human subjects [86].
Defining a product as an NHP is complex and not dependent simply on the nature of the product but several other factors as well such as approved use, mode of administration. To accomplish this, two specific schedules were developed within the regulations. Schedule 1 lists product types and categories captured by regulations including such as things as herbal medicines, traditional medicines, homeopathic medicines, vitamins, minerals, probiotics, amino acids and essential fatty acids. Schedule 2 sets out a number of exclusionary criteria from the NHPR such administration by breaking the dermis and being captured by other regulatory frameworks such as the Tobacco Act or the Controlled Drugs and Substances Act. From a regulatory standpoint, an NHP is anything captured by schedule 1 but not included on schedule 2. An important additional factor is that, NHPs are limited to products used for self-care with products requiring a prescription regulated like other prescription medicines and falling outside of the NHPR [86].
The Canadian NHP regulatory framework is primarily premarket in nature requiring a product license application to be made to Health Canada and approved before a product can be marketed for sale in Canada. As a subset of drugs, permitted claims for NHPs are not only limited to health promotion, risk reduction and those related to structure and function but can include treatment of diseases suitable for self-care. NHPs can make conventional health care claims as well as ones from traditional and complementary healing paradigms such as traditional Asian medicine and medical herbalism. Approved NHPs on the market are identified by either an 8-digit Natural Product Number (NPN) or Homeopathic Medicine Number (DIN-HM) that must appear on the label [86]. Information about all approved NHP applications can be found a searchable database titled the Licensed Natural Health Products Database [87]1. In addition, information regarding individual ingredients can be found on the Natural Health Products Ingredients Database [88].
For an NHP to make an approved claim, the applicant must provide appropriate supporting evidence for review. As with other health products, a risk-based approach is taken in determining the type and amount of evidence required. To facilitate the application process, Health Canada has developed a number of resources of pre-cleared information (PCI) defined as “any form of information supporting the safety, efficacy or quality of a medicinal ingredient or natural health product that NHPD has reviewed and determined to be acceptable” [89]. The most notable forms of PCI are a series of single, multi-ingredient and product regulatory monographs. These monographs capture many of the more widely seen and marketed ingredients and products such as individual nutrients, medicinal herbs and combination products such as multi-vitamins and throat lozenges. The monographs are detailed containing set parameters for such as things are dosage, permissible claims, mandatory warnings and contraindications and dosages. When products contain more than one ingredient defined by a monograph, the final multi ingredient NHP must take information from each separate monograph [89].
Operationally different levels and sources of evidence supporting claims have been categorized into three different classes: Class 1 refers to applications that comply with all the parameters of a Health Canada NHP monograph; Class 2 refers to applications are general and/or traditional in nature supported entirely by a combination of Health Canada NHP monographs; and Class 3 are for applications which require a more in depth and more complete assessment [90].
More detailed information about the process found in Health Canada document guidance document titled Natural Health Products Management Applications Policy [90].
Since 2016, Health Canada has been considering how best to regulate products used for self-care such as NHPs, cosmetics and non-prescription drugs in a cohesive and integrated manner. Since consultations and deliberations are still on going, the final outcome is yet to be determined but could impact on how products containing herbal ingredients such as M. tortuosum are regulated in Canada in the future [91].
Regarding NHPs containing M. tortuosum, according to the Licensed NHP Database as of August 20202, since 2014 there have been eleven NHP licenses which are active and approved for sale in Canada. Three of these licenses, two with the same brand name, contain M. tortuosum as the only ingredient with the other 8 being multi-ingredient approving products containing other ingredients and nutrients notably adaptogens, those that improve cognitive ability and those that have antioxidant properties. The single ingredient NHPs containing M. tortuosum have the permissible claim of: “Helps support cognitive function in adults. Helps to support cognitive performance in a healthy aging population”. Similar claims, or elements of it, are also permitted for most but not all of the multi-ingredient NHPs containing M. tortuosum together with those allowed for other ingredients where possible in many cases taken from a Health Canada NHP monograph.
Since contained within a licensed NHP, an entry for M. tortuosum can be found in the Natural Health Products Ingredient Database [92]2.
In the context of the three review classes, without reviewing the various product license applications, it is not possible to precisely say how these NHPs containing M. tortuosum were reviewed. Also, it is important to note that the approval process operationally has changed in recent years. Since there is no Health Canada prepared NHP monograph for M. tortuosum it would not be reviewed through the Class 1 pathway. The most likely approach taken currently for these products would be through the Class 3 pathway which could be expedited based upon the quality and completeness of the application or evidence contained within a master file held by the Department.
If a company wished to market a drug containing M. tortuosum for a prescription level claim, though very challenging, the opportunity exists to apply through the conventional approval mechanism for pharmaceutical drugs. No information was found regarding M. tortuosum being legally available in a supplemented food within Canada.
3.6. Sceletium Products in the Russian Federation
In Russia, Federal Law No 29-FZ [93] “On the quality and safety of food products” regulates the quality of food products and their safety. Food products are products “in natural or processed form for human consumption as food (including children's foods and dietary foods), bottled drinking water, alcoholic products (including beer), non-alcoholic beverages, chewing gum, and also raw food materials, food additives and biologically active additives” [93]. The terms “food additives” and “biologically active additives” are used in this law for functional food and dietary supplements, respectively. Food additives are claimed as “natural or artificial substances and their compounds specially introduced into food products in the process of their manufacture for the purpose of imparting certain properties to and/or preserving the quality of food products”, while biologically active additives are “natural (identical to natural) biologically active substances designed for consumption with food or for introduction into the composition of food products” [93].
New food products manufactured in the Russian Federation are subject to state registration, while imported food products and materials are subject to state registration prior to their importation into the Russian Federation.
There are several restrictions regarding the advertising of biologically active and food supplements. Article 25 of the Federal Law No 38-FZ “On advertising” [94] details these.
In each case an advertisement of biologically active supplements shall be accompanied with a warning that the object of the advertisement is not a medicine.
In 2010 the “Uniform sanitary and epidemiological and hygienic requirements for products subject to sanitary and epidemiological supervision (control)” were implemented for the use in countries of the Eurasian Economic Union (Republic Armenia, Republic of Belarus, Republic of Kazakhstan, Kyrgyz Republic, and Russian Federation) [95]. According to this document, a “food additive” is “any substance (or mix of substances) not consumed by human directly as a food and meant to be included in food product when produced for technological purposes (function), including giving it a certain organoleptic properties and (or) preservation of quality and safety for determined period of use, which can perform several technological functions” [95]. The “biologically active additives to food” are “products containing nutrient and (or) biologically active substances (their concentrates) of natural or artificial origin (identical to the natural), as well as prebiotic components and probiotic microorganisms, which are meant to be taken at the same time with food for optimization of human ration and which are not the only source of food or dietary nutrition” [95]. Article 55 “Hygienic requirements for safety and food value of food products” requires to declare “that biologically active substances, food components and products, and their sources, used for manufacturing of biologically active substances, must not have adverse impact on human health and must not contain psychotropic, narcotic, poisonous or potent substances, as defined by the applicable legislation of the Customs Union member states” [95].
Phytotherapy and zootherapy are a part of officinal medicine in Russia [96-98]. The Federal Law No. 61-FZ [99] “On Circulation of Medicines” establishes the priority of the state regulation of safety, quality and efficacy of medicines in the process of their circulation. This law determines medicines as “substances or combinations thereof coming in contact with the human or animal body, penetrating into the organs and tissues of the human or animal body, used for prophylaxis, diagnostics (except for substances or combinations thereof not coming in contact with the human or animal body), treatment of disease, rehabilitation, as well as for maintenance, prevention or interruption of pregnancy, as may be derived from blood, blood plasma, human or animal organs and tissues, plants and minerals by synthesis methods or using biological technologies” [99]. All herbal and animal-derived medicinal products are governed by this law in the process of their circulation in Russia. Any products that are derived from natural raw materials (plants, animals, minerals) and in the descriptions of which it is mentioned that they can be used for prophylaxis automatically fall under the concept of “medicines”. Therefore, biologically active additives cannot have an indication “for prophylaxis”.
According to a resolution of the Russian Federation government “On improving control over the sale of narcotic substances” [100], mesembrine, a main alkaloid of M. tortuosum, was considered a psychotropic substances and included in the list of narcotic substances, psychotropic substances and their precursors the circulation of which is prohibited in the Russian Federation. “Psychotropic medicines are medicinal products and pharmaceutical substances containing psychotropic substances and included in the List of narcotic substances, psychotropic substances and their precursors” [100]. The circulation of psychotropic medicines is subject of special regulation and control in Russia [99]. Taking in consideration above mentioned facts, products containing M. tortuosum will be considered as psychotropic medicine.
Some specific aspects of psychotropic substances and medicines are regulated by the Federal Law No. 3-FZ [101] “About drugs and psychotropic substances”. The Article 16 of this law indicate that the development of new narcotic and psychotropic medicines is allowed only by the state order and in the state unitary companies and in the state research institutions with a license provided by the legislation of the Russian Federation on licensing certain types of activities. The import/export of psychotropic substances and medicines is a subject of special licensing. Sceletium products in Russia could be lawfully used only after market authorization as medicine according to the Federal Law No. 61-FZ and under strict control.
CONCLUSION
Traditional San and Khoikhoi uses of Mesembryanthemum tortuosum [25] and subsequent colonial use [6] provided the departure point for the phytochemical, pharmacological and clinical exploration of extracts and isolated compounds from the plant. While the clinical research base is still exploratory and to date limited to studies in healthy subjects, the emerging clinical evidence is congruent with some traditional uses, pharmacological mechanisms of action, in vitro permeation studies of the major alkaloids, and with in vivo studies of safety and efficacy. Standardized and characterized extracts of Mesembryanthemum tortuosum have a low side-effect profile, and have great potential, not only as
dietary supplements, but also as botanical medicines, for managing anxiety, depression, cognitive impairment. Extracts of the plant should also be explored as potential supportive treatments for schizophrenic patients where dorsolateral prefrontal cortex-dependent cognitive impairment is prominent, in addition to treatment with pharmaceutical antipsychotic medication [102].
Albeit their overarching concerns for consumers to be exposed to safe and efficacious products, healthcare systems and their regulations evolved within national legislation and addressed the specific characteristics and needs of individual nations - while appropriate and justified - with great heterogeneity. Especially, rules governing market access for botanical products vary widely. Harmonisation of healthcare regulations is a relatively recent phenomenon, still emerging and largely regional. In the interest of universally applicable market access requirements for traditional herbal medicinal products, efforts should be increased to harmonise regulations further on an international level.
While all products destined for the drug category should be tested and documented with the same rigor, it appears that a universal “traditionally used herbal medicine” category, that is distinct from that of food (supplements), applies the same quality standards as for drugs, but replaces drug-like clinical and toxicological requirements with soft claims derived from traditional use and assumes safety based on longstanding traditional use, but is not territorial, i.e., restricted to a national or federal territory, would be desirable. The USA has such provisions in place, but as of yet only for food stuffs, the EU offers a similar path to market for “traditional foods from third countries”. However, neither apply to botanicals traditionally used strictly as medicines (only recreational use or use as a food ingredient would provide the necessary bridge here), and even if they did, would not offer opportunity for associating health claims. It seems almost ironic that sceletium owes its USA market exposure to its recreational use in beverage teas just because, by pure chance, it is regulated as food in its country of origin.
None of the regulatory systems included in this review, except for Canada, offer provisions under which sceletium products could gain market access as a (traditional) botanical medicine, other than through a full drug registration procedure. That said, there may be national regulatory systems not covered in this review which make provisions for traditional botanical medicines; however, these would be of limited commercial relevance.
In summary, developers of botanical products with health benefits based on traditional use must consider a range of concerns which include but are not limited to:
Ensure sustainable supply.
Observe provisions of the Nagoya Protocol in terms of ownership of indigenous knowledge and access-benefit-sharing.
Identify a suitable regulatory category for a given product in the target market.
For aforementioned reasons, the latter may be the most difficult to achieve. This is true for sceletium, where obstacles range from scheduled substance class, via the absence of evidence for traditional use other than in the country of origin, to insufficient clinical safety data. While the standardized M. tortuosum extract Zembrin® has enjoyed extensive safe use in diverse dietary supplements on the USA and Canadian markets for more than a decade now, investment in definitive clinical research is still needed for this extract and all other standardized and characterized sceletium extracts to allow them to realize their therapeutic potential, and to address regulatory hurdles. Until then, sadly, consumer access to sceletium products will remain highly restricted.
Fig. (1).
Sceletium alkaloids: 1 mesembrine, 2 mesembrenone, 3 mesembrenol, 4 mesembranol, and 5 tortuosamine.
ACKNOWLEDGEMENTS
Declared none.
Footnotes
It is important to note that because an NHP is approved for sale in Canada does not mean that the product is actually being sold on the Canadian market.
Listed as S. tortuosum.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
Thomas Brendler discloses past consulting assignments with HG&H Pharmaceuticals and PLT Health Solutions, the North American distributor of Zembrin®. Both Thomas Brendler and Josef Brinckmann are employed by the manufacturer of a tea product containing sceletium. Ulrich Feiter is the founder and CEO of a company that provides cultivation, processing and regulatory services for a wide range of botanicals, including sceletium. Nigel Gericke is a trustee of a family trust with a minor shareholding in HG&H Pharmaceuticals but is not actively involved in HG&H Pharmaceuticals or commercial sceletium products.
REFERENCES
- 1.Gericke N., Viljoen A.M. Sceletium-a review update. J. Ethnopharmacol. 2008;119(3):653–663. doi: 10.1016/j.jep.2008.07.043. [DOI] [PubMed] [Google Scholar]
- 2.Harvey A.L., Young L.C., Viljoen A.M., Gericke N.P. Pharmacological actions of the South African medicinal and functional food plant Sceletium tortuosum and its principal alkaloids. J. Ethnopharmacol. 2011;137(3):1124–1129. doi: 10.1016/j.jep.2011.07.035. [DOI] [PubMed] [Google Scholar]
- 3.Murbach T.S., Hirka G., Szakonyiné I.P., Gericke N., Endres J.R. A toxicological safety assessment of a standardized extract of Sceletium tortuosum (Zembrin®) in rats. Food Chem. Toxicol. 2014;74:190–199. doi: 10.1016/j.fct.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 4.Forbes V.S. Carl Peter Thunberg Travels at the Cape of Good Hope 1772-1775; Van Riebeeck Society: Cape Town, RSA, 1986. [Google Scholar]
- 5.Gordon D. From Rituals of Rapture to Dependence: The Political Economy of Khoikhoi Narcotic Consumption, c.1487-1870. S. Afr. Hist. J. 1996;35(1):62–88. doi: 10.1080/02582479608671247. [DOI] [Google Scholar]
- 6.Pappe L. Florae Capensis Medicae Prodromus. W; Britain Press: Cape Town, RSA. 1857. [Google Scholar]
- 7.Prada Samper J.M.d. The plant lore of the/Xam San://Kabbo and≠ Kasiŋ’s identification of Bushman medicines. Culturas Populares. Revista Electrónica. 2007;4:1–17. [Google Scholar]
- 8.Smith C.A. Common Names of South African Plants; Department of Agricultural Technical Services: Pretoria, RSA, 1966.
- 9.Gerbaulet M. Revision of the genus Sceletium NE Br. (Aizoaceae). Bot. Jahrb. Syst. Pflanzengesch. Pflanzengeogr. 1996;118(1):9–24. [Google Scholar]
- 10.Klak C., Bruyns P.V., Hedderson T.A.J. A phylogeny and new classification for Mesembryanthemoideae (Aizoaceae). Taxon. 2007;56(3):737–756. doi: 10.2307/25065857. [DOI] [Google Scholar]
- 11.Van der Stel S. Journey to Namaqualand in 1685; Human and Rossouw: Cape Town, RSA, 1979.
- 12.Smith M.T., Crouch N.R., Gericke N., Hirst M. Psychoactive constituents of the genus Sceletium N.E.Br. and other Mesembryanthemaceae: a review. J. Ethnopharmacol. 1996;50(3):119–130. doi: 10.1016/0378-8741(95)01342-3. [DOI] [PubMed] [Google Scholar]
- 13.Wijnands D.O., Wilson M.L., Toussaint van Hove T. Jan Commelin’s monograph on Cape flora. Cape Town: RSA; 1996. pp. 38–39. [Google Scholar]
- 14. Pharmaceutical compositions containing mesembrine and related compounds. US Patent #6288104, 1997.
- 15.Hartwich C. Die menschlichen Genussmittel. Ihre Herkunft, Verbreitung, Geschichte, Anwendung, Bestandteile und Wirkung. Leipzig, Germany: Tauchnitz; 1911. [Google Scholar]
- 16.Jacobsen H. Handbook of Succulent Plants: Mesembryanthemums (Ficoidaceae). London, UK: Blandford Press; 1960. [Google Scholar]
- 17.Laidler P. The magic medicine of the Hottentots. S. Afr. J. Sci. 1928;25:433–447. [Google Scholar]
- 18.Scott G., Hewett M.L. Pioneers in ethnopharmacology: The Dutch East India Company (VOC) at the Cape from 1650 to 1800. J. Ethnopharmacol. 2008;115(3):339–360. doi: 10.1016/j.jep.2007.10.020. [DOI] [PubMed] [Google Scholar]
- 19.Van Wyk B-E., Gericke N. People’s plants: A guide to useful plants of Southern Africa. Pretoria, RSA, : Briza publications: ; 2000. [Google Scholar]
- 20.van Wyk B.E. A review of Khoi-San and Cape Dutch medical ethnobotany. J. Ethnopharmacol. 2008;119(3):331–341. doi: 10.1016/j.jep.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 21.van Wyk B.E. A broad review of commercially important southern African medicinal plants. J. Ethnopharmacol. 2008;119(3):342–355. doi: 10.1016/j.jep.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 22.Watt J.M., Breyer-Brandwijk M.G. The Medicinal and Poisonous Plants of Southern and Eastern Africa. London, UK: Livingstone; 1962. [Google Scholar]
- 23.Zwicky E. Über Channa, ein Genussmittel der Hottentotten (Mesembrianthemum expansum L. und tortuosum L.). Zurich: Zürcher and Furrer; 1914. [Google Scholar]
- 24.Meiring I. Notes on some experiments with the active principle of Mesembrianthemum tortuosum L. Trans S. Afr. Philos. Soc. 1895;9(1):48–50. doi: 10.1080/21560382.1895.9526314. [DOI] [Google Scholar]
- 25.Gericke N. 2018. Kabbo’s! [Google Scholar]
- 26.Watt J.M. African plants potentially useful in mental health. 1968. [PubMed]
- 27.Brendler T., Eloff J.N., Gurib-Fakim A., Phillips L.D. African Herbal Pharmacopoeia. Port Louis, Mauritius: AAMPS; 2010. p. 205. [Google Scholar]
- 28.Patnala S., Kanfer I. HPLC analysis of mesembrine-type alkaloids in Sceletium plant material used as an African traditional medicine. J. Pharm. Pharm. Sci. 2010;13(4):558–570. doi: 10.18433/J3DK5F. [DOI] [PubMed] [Google Scholar]
- 29.Shikanga E.A., Kamatou G.P.P., Chen W., Combrinck S., Viljoen A.M. Validated RP-UHPLC PDA and GC-MS methods for the analysis of psychoactive alkaloids in Sceletium tortuosum. S. Afr. J. Bot. 2012;82:99–107. doi: 10.1016/j.sajb.2012.05.004. [DOI] [Google Scholar]
- 30.Lubbe A., Khatib A., Yuliana N.D., Jinap S., Verpoorte R. Cannabinoid CB1 receptor binding and acetylcholinesterase inhibitory activity of Sceletium tortuosum L. Int. Food Res. J. 2010;17:349–355. [Google Scholar]
- 31.Shikanga E.A., Hamman J.H., Chen W., Combrinck S., Gericke N., Viljoen A.M. In vitro permeation of mesembrine alkaloids from Sceletium tortuosum across porcine buccal, sublingual, and intestinal mucosa. Planta Med. 2012;78(3):260–268. doi: 10.1055/s-0031-1280367. [DOI] [PubMed] [Google Scholar]
- 32.Coetzee D.D., López V., Smith C. High-mesembrine Sceletium extract (Trimesemine™) is a monoamine releasing agent, rather than only a selective serotonin reuptake inhibitor. J. Ethnopharmacol. 2016;177:111–116. doi: 10.1016/j.jep.2015.11.034. [DOI] [PubMed] [Google Scholar]
- 33.Swart A.C., Smith C. Modulation of glucocorticoid, mineralocorticoid and androgen production in H295 cells by Trimesemine™, a mesembrine-rich Sceletium extract. J. Ethnopharmacol. 2016;177:35–45. doi: 10.1016/j.jep.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 34.Bennett A.C., Smith C. Immunomodulatory effects of Sceletium tortuosum (Trimesemine™) elucidated in vitro: Implications for chronic disease. J. Ethnopharmacol. 2018;214:134–140. doi: 10.1016/j.jep.2017.12.020. [DOI] [PubMed] [Google Scholar]
- 35.Hirabayashi M., Ichikawa K., Fukushima R., Uchino T., Shimada H. Clinical application of South African tea on dementia dog. Japanese Journal of Small Animal Practice. 2002;21:109–113. [Google Scholar]
- 36.Hirabayashi M., Ichikawa K., Yoshi A., Uchino T., Shimada K. Clinical effects of South African tea for cat. . Japanese journal of small animals practice . 2004;23:85–88. [Google Scholar]
- 37.Hirai M., Ichikawa K., Yoshi A. Clinical effect of SA tea for demential animal. Japanese Journal of Small Animal Practice. 2008;24:27–31. [Google Scholar]
- 38.Smith C. The effects of Sceletium tortuosum in an in vivo model of psychological stress. J. Ethnopharmacol. 2011;133(1):31–36. doi: 10.1016/j.jep.2010.08.058. [DOI] [PubMed] [Google Scholar]
- 39.Carpenter J.M., Jourdan M.K., Fountain E.M., Ali Z., Abe N., Khan I.A., Sufka K.J. The effects of Sceletium tortuosum (L.) N.E. Br. extract fraction in the chick anxiety-depression model. J. Ethnopharmacol. 2016;193:329–332. doi: 10.1016/j.jep.2016.08.019. [DOI] [PubMed] [Google Scholar]
- 40.Dimpfel W., Schombert L., Gericke N. Electropharmacogram of Sceletium tortuosum extract based on spectral local field power in conscious freely moving rats. J. Ethnopharmacol. 2016;177:140–147. doi: 10.1016/j.jep.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 41.Gericke N. In: Sceletium tortuosum.Complementary and Integrative Treatments in Psychiatric Practice; Gerbarg, P.L.; Muskin, P.R. Brown R.P., editor. Arlington, VA, USA: American Psychiatric Association Publishing; 2017. [Google Scholar]
- 42.Terburg D., Syal S., Rosenberger L.A., Heany S., Phillips N., Gericke N., Stein D.J., van Honk J. Acute effects of Sceletium tortuosum (Zembrin), a dual 5-HT reuptake and PDE4 inhibitor, in the human amygdala and its connection to the hypothalamus. Neuropsychopharmacology. 2013;38(13):2708–2716. doi: 10.1038/npp.2013.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chiu S., Gericke N., Farina-Woodbury M., Badmaev V., Raheb H., Terpstra K., Antongiorgi J., Bureau Y., Cernovsky Z., Hou J., Sanchez V., Williams M., Copen J., Husni M., Goble L. Proof-of-Concept Randomized Controlled Study of Cognition Effects of the Proprietary Extract Sceletium tortuosum (Zembrin) Targeting Phosphodiesterase-4 in Cognitively Healthy Subjects: Implications for Alzheimer's Dementia. Evidence-based complementary and alternative medicine : . 2014. [DOI] [PMC free article] [PubMed]
- 44.Dimpfel W., Gericke N., Suliman S., Dipah G.N.C. Psychophysiological Effects of Zembrin® Using Quantitative EEG Source Density in Combination with Eye-Tracking in 60 Healthy Subjects. A Double-Blind, Randomized, Placebo-Controlled, 3-Armed Study with Parallel Design. Neurosci. Med. 2016;7(3):114–132. doi: 10.4236/nm.2016.73013. [DOI] [Google Scholar]
- 45.Dimpfel W., Gericke N., Suliman S., Dipah G.N.C. Effect of Zembrin® on Brain Electrical Activity in 60 Older Subjects after 6 Weeks of Daily Intake. A Prospective, Randomized, Double-Blind, Placebo-Controlled, 3-Armed Study in a Parallel Design. World J. Neurosci. 2016;7(1):140–171. doi: 10.4236/wjns.2017.71011. [DOI] [Google Scholar]
- 46.Reay J., Wetherell M.A., Morton E., Lillis J., Badmaev V. Sceletium tortuosum (Zembrin®) ameliorates experimentally induced anxiety in healthy volunteers. Hum. Psychopharmacol. 2020;35(6):1–7. doi: 10.1002/hup.2753. [DOI] [PubMed] [Google Scholar]
- 47.Hoffman J.R., Markus I., Dubnov-Raz G., Gepner Y. Ergogenic Effects of 8 Days of Sceletium Tortuosum Supplementation on Mood, Visual Tracking, and Reaction in Recreationally Trained Men and Women. J. Strength Cond. Res. 2020;34(9):2476–2481. doi: 10.1519/JSC.0000000000003693. [DOI] [PubMed] [Google Scholar]
- 48.Loria M.J., Ali Z., Abe N., Sufka K.J., Khan I.A. Effects of Sceletium tortuosum in rats. J. Ethnopharmacol. 2014;155(1):731–735. doi: 10.1016/j.jep.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Nell H., Siebert M., Chellan P., Gericke N. A randomized, double-blind, parallel-group, placebo-controlled trial of Extract Sceletium tortuosum (Zembrin) in healthy adults. J. Altern. Complement. Med. 2013;19(11):898–904. doi: 10.1089/acm.2012.0185. [DOI] [PubMed] [Google Scholar]
- 50.Meyer G.M.J., Wink C.S.D., Zapp J., Maurer H.H.G.C-M.S.G.C-M.S. LC-MS(n), LC-high resolution-MS(n), and NMR studies on the metabolism and toxicological detection of mesembrine and mesembrenone, the main alkaloids of the legal high “Kanna” isolated from Sceletium tortuosum. Anal. Bioanal. Chem. 2015;407(3):761–778. doi: 10.1007/s00216-014-8109-9. [DOI] [PubMed] [Google Scholar]
- 51.Brendler T., van Wyk B.E. A historical, scientific and commercial perspective on the medicinal use of Pelargonium sidoides (Geraniaceae). J. Ethnopharmacol. 2008;119(3):420–433. doi: 10.1016/j.jep.2008.07.037. [DOI] [PubMed] [Google Scholar]
- 52.Stander M.A., Brendler T., Redelinghuys H., Van Wyk B.E. The commercial history of Cape herbal teas and the analysis of phenolic compounds in historic teas from a depository of 1933. J. Food Compos. Anal. 2019;76:66–73. doi: 10.1016/j.jfca.2018.11.001. [DOI] [Google Scholar]
- 53.Van Wyk B.E. The potential of South African plants in the development of new medicinal products. S. Afr. J. Bot. 2011;77(4):812–829. doi: 10.1016/j.sajb.2011.08.011. [DOI] [Google Scholar]
- 54.South African Government . National Environmental Management: Biodiversity Act 2004 (Act No. 10 of 2004). Government Gazette; 2004. p. 26436. [Google Scholar]
- 55.South African Government . National Environmental Management: Biodiversity Act (10/2004): Commencement of Bio-Prospecting, Access and Benefit-Sharing Regulations, 2008; Regulations on Bio-Prospecting, Access and Benefit-Sharing. Government Gazette; 2008. p. 30739. [Google Scholar]
- 56.South African Government . National Environmental Management: Biodiversity Act 2004 (Act No. 10 of 2004) Threatened of Protected Species Regulations - published for public comment. Government Gazette; 2015. p. 38600. [Google Scholar]
- 57.South African Government . National Environmental Management: Biodiversity Act (10/2004): Amendments to the regulations on Bio-prospecting, access and benefit-sharing. Government Gazette; 2015. p. 38809. [Google Scholar]
- 58.South African Government . Act No. 6 of 2019: Protection, Promotion, Development and Management of Indigenous Knowledge Act. Government Gazette; 2019. p. 1082. [Google Scholar]
- 59.Brendler T., Phillips L.D. European Union Market Access Categories and Regulatory Requirements for Novel Natural Products. . In: Gurib-Fakim A., Phillips L.D., editors. Novel Plant Bioresources; 2014. pp. 107–124. [Google Scholar]
- 60.European Medicines Agency Guideline on Good Agricultural and Collection Practice (GACP) for Starting Material of Herbal Origin, 2006.
- 61.European Commission EudraLex - Volume 4 - Good Manufacturing Practice (GMP) guidelines, 2018.
- 62.European Commission Regulation (EC) No 178/2002 of the European Parliament and of the Council of 28 January 2002 laying down the general principles and requirements of food law, establishing the European Food Safety Authority and laying down procedures in matters of food safety. Last consolidated in 2019, 2002.
- 63.European Commission Directive 2002/46/EC of the European Parliament and of the Council of 10 June 2002 on the approximation of the laws of the Member States relating to food supplements as amended, 2019.
- 64.European Commission Regulation (EU) No 609/2013 of the European Parliament and of the Council of 12 June 2013 on food intended for infants and young children, food for special medical purposes, and total diet replacement for weight control and repealing Council Directive 92/52/EEC, Commission Directives 96/8/EC, 1999/21/EC, 2006/125/EC and 2006/141/EC, Directive 2009/39/EC of the European Parliament and of the Council and Commission Regulations (EC) No 41/2009 and (EC) No 953/2009, 2017.
- 65.European Commission 2017.
- 66.European Commission 2015.
- 67.European Commission 2014.
- 68.European Commission 2004.
- 69.European Commission 2019.
- 70.European Commission 2019.
- 71.European Commission 2008.
- 72.European Commission 2012.
- 73.European Commission 2019.
- 74.Brinckmann J.A. Labelling of Natural Products: The United States Market. Geneva, Switzerland: International Trade Centre; 2011. p. 24. [Google Scholar]
- 75.US Food and Drug Administration . Botanical Drug Development Guidance for Industry. College Park, MD, USA: 2016. [Google Scholar]
- 76.US Food and Drug Administration . FDA Approves First Drug Comprised of an Active Ingredient Derived from Marijuana to Treat Rare. Severe Forms of Epilepsy; 2018. [Google Scholar]
- 77.Brinckmann J.A., Fletcher E.J., Das R., Flaster T. 2019.
- 78.US Food and Drug Administration . Substances Generally Recognized as Safe. Final Rule. College Park, MD, USA: Federal Register; 2016. pp. 54960–55055. [Google Scholar]
- 79.US Food and Drug Administration . How to Submit Notifications for a New Dietary Ingredient. College Park, MD, USA: 2019. [Google Scholar]
- 80.US Food and Drug Administration . Nutrition labeling of food, 21 CFR § 101.9. Washington, D.C., USA: Government Printing Office; 2019. [Google Scholar]
- 81.US Food and Drug Administration . Special Dietary and Nutritive Additives, 21 CFR § 172 Subpart D. Washington, D.C., USA: Government Printing Office; 2019. [Google Scholar]
- 82.2012.
- 83.US Food and Drug Administration. Center for Food Safety and Applied Nutrition Guidance for Industry: Considerations Regarding Substances Added to Foods, Including Beverages and Dietary Supplements. 2014.
- 84.National Institutes of Health. Office of Dietary Supplements 2019.
- 85.HBC Health Solutions . Sceletium Tortuosum Sublingual. Los Angeles, CA, USA: 2019. [Google Scholar]
- 86.Government of Canada Natural Health Products Regulations. 2020.
- 87.Government of Canada . Licensed Natural Health Products Database. LNHPD; 2019. [Google Scholar]
- 88.Government of Canada Natural Health Products Ingredients Database. 2020.
- 89.Government of Canada Pre-Cleared Information. 2020.
- 90.Government of Canada Natural Health Products Management of Applications Policy. 2020.
- 91.Government of Canada Self-Care Products. 2019.
- 92.Government of Canada 2020.
- 93.Russian Federation On the quality and safety of food products. 2000.
- 94.Russian Federation On advertising. 2006.
- 95.Customs Union Commission 2010.
- 96.Prokopov I.A., Kovaleva E.L., Minaeva E.D., Pryakhina E.A., Savin E.V., Gamayunova A.V., Pozharitskaya O.N., Makarov V.G., Shikov A.N. Animal-derived medicinal products in Russia: Current nomenclature and specific aspects of quality control. J. Ethnopharmacol. 2019;240:111933. doi: 10.1016/j.jep.2019.111933. [DOI] [PubMed] [Google Scholar]
- 97.Shikov A.N., Pozharitskaya O.N., Makarov V.G., Wagner H., Verpoorte R., Heinrich M. Medicinal plants of the Russian Pharmacopoeia; their history and applications. J. Ethnopharmacol. 2014;154(3):481–536. doi: 10.1016/j.jep.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 98.Shikov A.N., Narkevich I.A., Flisyuk E.V., Luzhanin V.G., Pozharitskaya O.N. 2021. [DOI] [PubMed] [Google Scholar]
- 99.Russian Federation On Circulation of Medicines. 2010.
- 100.Federal Service for Drug Control . On improving control over sales of narcotic substances, and precursors of narcotic substances and psychotropic substances. Russian Federation: 2013. [Google Scholar]
- 101.Russian Federation About drugs and psychotropic substances. 1998.
- 102.Nahas Z., George M.S., Horner M.D., Markowitz J.S., Li X., Lorberbaum J.P., Owens S.D., McGurk S., DeVane L., Risch S.C. Augmenting atypical antipsychotics with a cognitive enhancer (donepezil) improves regional brain activity in schizophrenia patients: a pilot double-blind placebo controlled BOLD fMRI study. Neurocase. 2003;9(3):274–282. doi: 10.1076/neur.9.3.274.15563. [DOI] [PubMed] [Google Scholar]