Dear Editor,
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in 2019 and is the causative agent of the worldwide Coronavirus disease 2019 (COVID-19) pandemic, which is associated with substantial mortality.1,2 The Pfizer-BioNTech COVID-19 vaccine was the first approved vaccine that exhibited 95% effectiveness against COVID-19.1,3 Although rare post vaccination neurological complications are well described.4 Here, we report a case of a male with transverse myelitis (TM) after receiving the second dose of the Pfizer-BioNTech COVID-19.
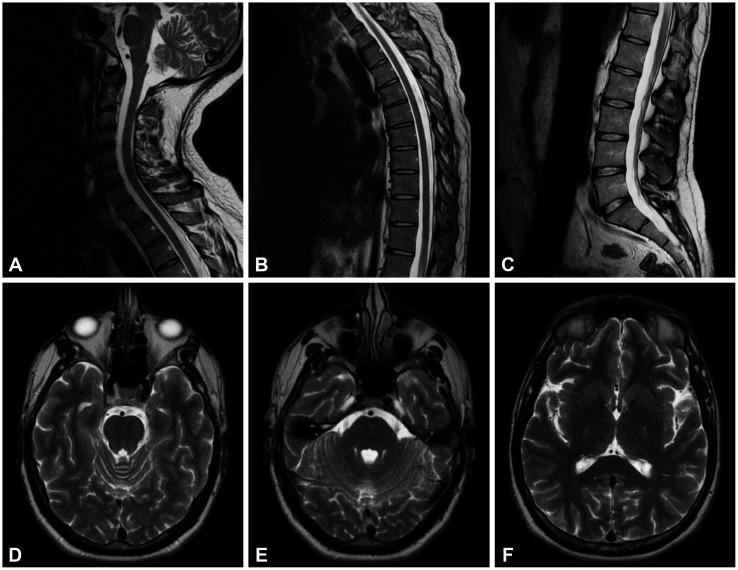
A 33-year-old male presented with 2 weeks of progressive weakness of the lower limbs. The complaints started 2 days after receiving his second dose of the Pfizer-BioNTech COVID-19. For the first 2 days he found it very difficult to walk, and he also noticed the sensation of incomplete emptying of the bladder and nocturnal low back pain. He did not have any relevant past medical history. He denied a history of infection or previous systemic complaints, illicit drug use, recent medications, travels, or any other epidemiological context. Since the symptoms persisted, he was admitted to the emergency room for evaluation. The neurological examination revealed mild paraparesis with a proximal muscle strengths of 4+ and 4 in the left and right legs, respectively. The Achilles reflexes were more brisk than the others. Superficial cutaneous-abdominal reflexes were absent and plantar reflexes were equivocal. There was a decreased thermic sensation below the T12 dermatomal level. An extensive workup evaluation was performed. Laboratory results (including autoimmune and infectious serologies, including for COVID-19) were negative. The findings of cervical, thoracic, and lumbar spine magnetic resonance imaging (MRI) were unremarkable (Fig. 1A, B and C). Additional brain MRI (Fig. 1D, E and F) did not produce any clinically relevant findings. A CSF study showed mononucleated pleocytosis (24 cells) and mild hyperproteinorrhachia (56 mg/dL). CSF bacteriological cultures and PCR for neurotropic virus and Borrelia burgdorferi were negative. There was slight cerebral barrier function disorder, but the oligoclonal bands were negative. The symptoms of the patient gradually reduced without additional treatment, and he became asymptomatic, after 3 months of follow-up.
Fig. 1. The findings of T2-weighted MRI of the spinal cord (A-C; sagittal) and brain (D-F; axial) were unremarkable.
We report a case of a male who experienced a monophasic transitory neurological dysfunction compatible with TM after receiving the second dose of the Pfizer-BioNTech COVID-19 vaccine. Although no lesions were visible in spine MRI (note that imaging performed during the convalescent phase can miss a cord lesion5), there was a demonstration of CSF inflammation. Additionally, other possible etiologies (compressive, acute SNC infection, primary demyelinating diseases, malignancy, or systemic autoimmune) were excluded. The patient’s clinical course was favorable and there was no need for any kind of treatment.
TM is a rare immune-mediated process that results in varying degrees of weakness, sensory alterations, and autonomic dysfunction. TM involves breakdown of the blood-brain barrier and pleocytosis of the CSF within a focal area of the spinal cord.4 Up to 40% of cases do not have relevant MRI findings.6 Several cases of TM have been reported after the administration of the different vaccines, including those for HBV, HPV, seasonal influenza, measles-mumps-rubella (MMR), polio, and diphtheria, with symptoms occurring from a few days to 3 months following inoculation.4,7 More recently, during the trial phase an association was found between the recombinant Oxford-AstraZeneca COVID-19 vaccine, and two instances of TM, but in one of those cases the association was the association was likely to have been coincidental.2,8 After the beginning of mass vaccination, there was another case report of TM associated with the Oxford-AstraZeneca COVID-19 vaccine, with symptom onset occurring at 8 days after vaccine administration, which was responsive to intravenous methylprednisolone.9
Three mechanisms via which vaccines can induce TM have been proposed 1) molecular mimicry; 2) epitope spreading, or 3) polyclonal activation of B lymphocytes.4 Neurological side effects in clinical trials of the Pfizer-BioNTech COVID-19 vaccine were rare, and only included Bell’s palsy.1,8 After the vaccine started to be rolled out around the world, one case of Guillain-Barré syndrome after the first dose of the Pfizer-BioNTech COVID-19 vaccine was reported.10 The technology underlying the Pfizer-BioNTech COVID-19 vaccine relies on messenger RNA (mRNA), and since the mRNA technique is new in vaccine manufacturing, potential adverse effects are not yet known, especially neurological ones.1 We hypothesize that the immune response to this vaccine triggered a transitory autoimmune process in our patient.
To our knowledge, this is the first reported case of TM after receiving the Pfizer-BioNTech. This case highlights that is essential to follow possible vaccine side effects in the real world, including neurological ones. However, it should be remembered that the risk of neurological complications or other adverse effects associated with COVID-19 vaccination is very low and that the benefits of vaccination outweigh any potential risks or side effects.
Footnotes
Ethics Statement: Informed consent was obtained from the patient.
- Conceptualization: Gonçalo Cabral.
- Data curation: Gonçalo Cabral.
- Formal analysis: Gonçalo Cabral.
- Funding acquision: Gonçalo Cabral, Carolina Gonçalves, Filipa Serrazina.
- Investigation: Gonçalo Cabral, Carolina Gonçalves.
- Methodology: Gonçalo Cabral, Carolina Gonçalves, Filipa Serrazina.
- Project administration: Gonçalo Cabral.
- Resources: Gonçalo Cabral, Carolina Gonçalves.
- Software: Gonçalo Cabral, Carolina Gonçalves, Filipa Serrazina. Supervision: Francisca Sá.
- Validation: Francisca Sá.
- Visualization: Francisca Sá.
- Writing—original draft: all authors.
- Writing—review and editing: all authors.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding Statement: None
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
References
- 1.El-Shitany NA, Harakeh S, Badr-Eldin SM, Bagher AM, Eid B, Almukadi H, et al. Minor to moderate side effects of Pfizer-BioNTech COVID-19 vaccine among Saudi residents: a retrospective cross-sectional study. Int J Gen Med. 2021;14:1389–1401. doi: 10.2147/IJGM.S310497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agmon-Levin N, Kivity S, Szyper-Kravitz M, Shoenfeld Y. Transverse myelitis and vaccines: a multi-analysis. Lupus. 2009;18:1198–1204. doi: 10.1177/0961203309345730. [DOI] [PubMed] [Google Scholar]
- 5.Jacob A, Weinshenker BG. An approach to the diagnosis of acute transverse myelitis. Semin Neurol. 2008;28:105–120. doi: 10.1055/s-2007-1019132. [DOI] [PubMed] [Google Scholar]
- 6.Scotti G, Gerevini S. Diagnosis and differential diagnosis of acute transverse myelopathy. The role of neuroradiological investigations and review of the literature. Neurol Sci. 2001;22 Suppl 2:S69–S73. doi: 10.1007/s100720100038. [DOI] [PubMed] [Google Scholar]
- 7.Principi N, Esposito S. Do vaccines have a role as a cause of autoimmune neurological syndromes? Front Public Health. 2020;8:361. doi: 10.3389/fpubh.2020.00361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goss AL, Samudralwar RD, Das RR, Nath A. ANA investigates: neurological complications of COVID-19 vaccines. Ann Neurol. 2021;89:856–857. doi: 10.1002/ana.26065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh Malhotra H, Gupta P, Prabhu V, Kumar Garg R, Dandu H, Agarwal V. COVID-19 vaccination-associated myelitis. QJM. 2021;114:591–593. doi: 10.1093/qjmed/hcab069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waheed S, Bayas A, Hindi F, Rizvi Z, Espinosa PS. Neurological complications of COVID-19: Guillain-Barre syndrome following Pfizer COVID-19 vaccine. Cureus. 2021;13:e13426. doi: 10.7759/cureus.13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.