Abstract
Information on the current practices and quantification of lymphedema service may be beneficial to promote and improve the current health care system. Therefore, this study aimed to describe the characteristics of lymphedema practitioners, and lymphedema patients' profiles, and provide a comprehensive picture of lymphedema service provision in Saudi Arabia. A cross‐sectional study design used an online survey to gather data. The survey included information about demographic and professional characteristics of lymphedema practitioners, lymphedema profiles, questions on the services provided, and perceived barriers in providing services. Eighteen lymphedema practitioners (38%) responded to the survey. Most of the respondents were physical therapists (94%), who had completed 135 hours of basic training course, and were certified as lymphedema therapists (89%). Most of these practitioners were in Riyadh (58%), Jeddah (25%), and Dammam (17%). About 75% of patients seen by practitioners had secondary lymphedema, predominately breast cancer‐related lymphedema (47%). The average number of lymphedema practitioners per service is three. The perceived barriers reported included an inadequate number of certified therapists (100%), difficulties with transportation and lack of financial support (each; 72%), and limited space for lymphedema practice/management (89%). The results suggest lymphedema practitioners provide reasonable services for lymphedema patients; however, services are still limited and needs are unmet. Therefore, more staffing is required to promote awareness of the condition and related services, to develop and implement appropriate educational strategies, and improve geographical and multidisciplinary coordination of the services in Saudi Arabia.
Keywords: lymphedema, quality management, service provision
ABBREVIATIONS
- CDT
complete decongestive therapy
- SOTA
Saudi Occupational Therapy Association
- SPTA
Saudi Physical Therapy Association
1. BACKGROUND
Lymphedema is a chronic incurable, progressive swelling because of obstruction or impaired development of the lymphatic system resulting in accumulation of protein‐rich fluid in the interstitial space. 1 , 2 Lymphedema can affect people of all ages and can occur in the limbs and the corresponding quadrant of the trunk, head and neck, or the genitals. 1 Primary lymphedema is hereditary because of dysfunction or malformation of the lymphatic system. Secondary lymphedema may develop secondary to cancer, or cancer‐related therapeutic interventions, 1 , 3 or secondary to non‐cancer‐related conditions, such as vascular insufficiency, trauma, infection, and inflammation. 3 , 4
Lymphedema can lead to pain and discomfort as a frequent symptom, with a heightened vulnerability to acute skin infection resulting in frequent hospitalisation and long‐term use of antibiotics. 5 Lymphedema may produce serious physical, social, and psychological morbidity. 6 Furthermore, increased limb size can interfere with mobility and influence body image with a consequent effect on quality of life. 6 , 7 There is no cure for lymphedema; however, there are several options for treatment aiming to control symptoms and reduce recurrence rate, including complete decongestive therapy (CDT), and exercise therapy. 8 , 9 Additional management options include pneumatic pumps, 10 low‐level laser therapy, 11 and kinesio taping. 12
Understanding the complex nature of lymphedema and its treatment requires competence in risk assessment, early detection, health promotion, and complex interventions. 10 , 12 , 13 , 14 Within this context, lymphedema practitioners play an important role in service provision leading to improved lymphedema management and increased patient knowledge and self‐management of lymphedema. 15 , 16 However, there is a limited provision of lymphedema education and a lack of knowledge or awareness among health care professionals, leading to underestimation of the conditions prevalence and inequality of services. 17 , 18 , 19 , 20 A few reports about service provision have been published in Australia, 18 , 19 Ireland, 20 and the United Kingdom. 21 , 22 , 23 These reports showed gaps regarding the provision of current services; randomly located, disjointed, and under‐resourced. 18 , 19 , 20 , 21 , 22 , 23
Lymphedema has been a rising condition in Saudi Arabia over the last 10 years because of an increase in the incidence of cancer, its related surgical and radiotherapy interventions, and survival, prevalence of obesity, and the ageing population. 24 , 25 , 26 , 27 A recent study showing the significance of lymphedema estimated the incidence of breast cancer‐related lymphedema (BCRL) to be 14.5%. 28
To our knowledge, few practitioners are qualified to provide lymphedema services, with other job requirements (eg, physical therapy services, and administration). Detailed information regarding profiles of the lymphedema practitioners, patient characteristics, and availability of lymphedema services and structure has not been well documented. Therefore, collecting data on the current practices and lymphedema services may be beneficial to identify current gaps in the services and provide scope for future development. The purposes of this survey were to: (a) describe professional profiles of the lymphedema practitioners treating lymphedema patients in Saudi Arabia; (b) describe the characteristics of patients seen by the practitioners; (c) explore the availability of lymphedema services and referral pathways; and (d) determine the potential barriers to lymphedema management from therapists' perspectives.
2. METHODS
2.1. Study design and participants
This study was a descriptive, cross‐sectional online national survey. The potential sample included all members of the Saudi physical therapy lymphedema group. This group is a special interest group of the Saudi Physical Therapy Association (SPTA) and the Saudi Occupational Therapy Association (SOTA) which includes practitioners participating in providing lymphedema services. The Institutional Review Board of the College of Applied Medical Sciences, King Saud University, Saudi Arabia, approved the study (Protocol No, College of Applied Medical Sciences 079‐3839).
2.2. Survey questionnaire
The study questionnaire was modified and adapted from a literature review 18 , 19 , 20 , 21 , 22 , 23 and questionnaire developed by American Lymphedema Framework Projects 29 to report the differences and understand the health care services provided in these clinical settings. Before distribution, the survey was pilot‐tested by three health care practitioner experts in lymphedema management to ensure clarity, feasibility, and comprehensiveness. The online version comprised 53 questions; included in four different sections to get a snapshot of the current practice of lymphedema management. The first section was comprised of demographic and work‐related characteristics of lymphedema practitioners. The second section was about lymphedema patient profiles, such as current caseload, types of lymphedema, percentage of primary and secondary lymphedema, percentage of male and female patients, age groups, initial causes, and percentage of the area involved. The third section was about the current assessment, interventions, risk reduction, and factors influencing their decisions on lymphedema management. The fourth section was about the service provisions, standards of care, and barriers to the services.
The response options included the selection of the proposed answer: yes/no, 4 Likert scales (eg, never used, rarely used, occasionally used, and frequently used), and 5 Likert scales (eg, strongly agree, agree, neutral, disagree, and strongly disagree).
2.3. Data collection
An online survey was administered via a secure online platform, Google Survey. The contact email addresses were identified from the databases of SPTA and SOTA. One week before disseminating the survey, an email containing invitations, a link to the web survey, and detailed information about the aim of the study and a statement that assured participants' confidentiality and anonymity of their response was delivered to the participants. A consent form was not required, as consent was assumed by completion of the survey. The invitation was sent under the signature of the study groups. Email invitations and reminders were sent three times over a 3‐month period. At the end of this 3‐month period, the survey was closed. The electronic data were kept on a password‐secured computer and hard‐copy data were kept in locked research files.
2.4. Statistical analysis
Data obtained from the surveys were entered into Microsoft Excel 2016 and imported to SPSS (version 25.0, IBM Corporation, New York). One of the authors checked the data for errors by comparison with the raw data, correcting any data entry anomalies. Descriptive statistics including percentages, frequency distributions, means, and medians were used to summarise therapists' characteristics, and provide data on current practices for lymphedema treatment. The 5‐point Likert scale categories were combined into two opposing categories. ‘Strongly disagree’ and ‘disagree’ were grouped together, as well as ‘strongly agree’ and ‘agree’. The level of significance was set at P < 0.05. Responses were collected and analysed, initially using the Google Survey software and again with SPSS (version 21.0, IBM).
3. RESULTS
3.1. Demographic and professional profile of lymphedema practitioners
Of the 51 respondents who were invited to participate in the study, 18 completed and returned the survey with an overall response rate of (35%). Thirty respondents (59%) did not complete the survey, as their clinical setting does not provide a lymphedema service, and/or they practiced without a training certificate. Three respondents' data (6%) were excluded from analysis as they had >50% of missing data.
Table 1 represents respondents' demographics and professional characteristics. The highest proportion of respondents reported being between 21 and 40 years of age (83%), female (78%), and Saudi (78%). Respondents comprised more physical therapists (94%) than occupational therapists (6%). Thirty‐eight of the respondents reported having a master's degree, and/or postgraduate diploma, while 72% of lymphedema practitioners had less than 5 years of working experience. The respondents worked in a variety of settings, whereby 67% identified as lymphedema practitioners working in more than one work setting (eg, inpatient and outpatient); 33% of practitioners worked in a single setting with the most common being outpatient (83%) and home care (6%).
TABLE 1.
Demographic and professional profile of lymphedema practitioners (n = 18)
| Characteristics | Frequency | |
|---|---|---|
| N | % | |
| Genders | ||
| Female | 14 | 77.77 |
| Male | 4 | 22.22 |
| Age (years) | ||
| 21‐30 | 4 | 22.22 |
| 31‐40 | 11 | 61.11 |
| 41‐50 | 3 | 16.67 |
| >50 | 0 | ‐ |
| Nationality | ||
| Saudi | 14 | 77.77 |
| Non‐Saudi | 4 | 22.22 |
| Educational background | ||
| Physical therapist | 17 | 94.44 |
| Occupational therapists | 1 | 5.56 |
| Years of lymphedema practitioners experienced | ||
| 0‐1 year | 6 | 33.33 |
| 2‐5 years | 7 | 38.89 |
| 6‐10 years | 1 | 5.56 |
| >10 years | 4 | 22.22 |
| Practice settings | ||
| Combination (outpatients/inpatient) | 12 | 66.67 |
| Outpatient clinics | 5 | 27.77 |
| Home care | 1 | 5.56 |
| Sources of lymphedema educations/training | ||
| Undergraduate | 4 | 22.22 |
| Postgraduate diploma | 1 | 5.56 |
| Basic lymphedema training/certificate | 16 | 88.89 |
| Advanced/specialised lymphedema courses/training | 7 | 38.89 |
| Methods for addressing educational needs and training | ||
| Undergraduate modules on lymphatic system and lymphedema | 13 | 72,22 |
| Self‐directed learning | 9 | 50 |
| Postgraduate modules on lymphatic system and lymphedema | 5 | 27.78 |
| Workshop/conference/seminar/lecture | 5 | 27.78 |
| Supervised clinical placement and in‐service training | 4 | 22.22 |
| Sufficient opportunity for professional development | ||
| No | 14 | 77.77 |
| Yes | 4 | 22.22 |
Regarding training modes, most respondents (89%) had completed 135 hours of basic lymphedema training as a highest source for lymphedema education, while 39% had completed advanced lymphedema training courses. The most common preferred methods to address educational needs were undergraduate modules (72%) and self‐directed learning (50%) followed by postgraduate module and workshops/conferences/seminars (each = 28%), while 22% of respondents showed that supervised clinical placement and in‐service training would be useful.
As shown in Figure 1, the highest proportion of lymphedema practitioners rated themselves as ‘Excellent’ or ‘Very good’ in terms of knowledge (83%), competence, and confidence (each 67%), while 56% of practitioners rated themselves as ‘Excellent’ or ‘Very good’ in terms of how experienced they felt. However, 78% of practitioners did not think there were sufficient opportunities for professional development.
FIGURE 1.
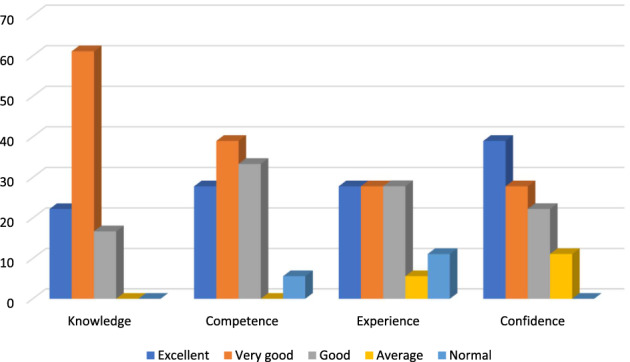
Practitioners' ratings of the professional development
3.2. Lymphedema patient profile
Table 2 lists characteristics of patients seen by the lymphedema practitioners. Most lymphedema patients were female (68%). The highest mean percentage of lymphedema patients reported being between 19 and 65 years of age (75%), followed by geriatric ≥65 years (17%) and paediatric aged 1 to 18 years (8%). Classification of lymphedema was secondary (75%) and caused by cancer (53%), with 47% suffering from BCRL, followed by venous insufficiency (11%), tissue damage and inflammation (8%), and immobility/dependency (3%). The most common location of lymphedema was in the unilateral upper limb (50%), followed by bilateral lower limb (36%), and unilateral lower limbs (33%), trunk/breast (16%), head and neck (1%), and genitals (4%). According to the survey, lymphedema practitioners reported that on average 17.5% of the patients had mixed lymphedema (wound + lymphedema).
TABLE 2.
Lymphedema patient profile
| Characteristics | Mean ± SD | Range |
|---|---|---|
| Gender (%) | ||
| Female | 68% | |
| Male | 32% | |
| Age groups, years | ||
| 1‐18 years | 7.50 ± 8.67 | 0‐30 |
| 19‐65 years | 75.05 ± 19.74 | 20‐100 |
| ≥65 years | 17.44 ± 16.55 | 0‐70 |
| Lymphedema classification N (%) | ||
| Primary | 25.22 ± 20.73 | 0‐90 |
| Secondary | 74.78 ± 20.78 | 10‐100 |
| Cancer‐related lymphedema | ||
| Breast cancer‐related | 47.06 ± 25.96 | 0‐98 |
| Other cancer‐related | 6.39 ± 7.64 | 0‐30 |
| Non‐cancer‐related lymphedema | ||
| Vascular | 10.50 ± 10.17 | 0‐40 |
| Trauma/inflammation | 7.61 ± 8.48 | 0‐30 |
| Immobility/dependency | 3.33 ± 3.77 | 0‐10 |
| Sites of lymphedema | ||
| Unilateral upper limb | 50.00 ± 38.35 | 0‐98 |
| Bilateral upper limb | 6.22 ± 12.07 | 0‐50 |
| Unilateral lower limb | 33.17 ± 31.84 | 0‐90 |
| Bilateral lower limb | 36.00 ± 32.53 | 0‐100 |
| Head and neck | 1.28 ± 2.71 | 0‐10 |
| Trunk/breast | 15.94 ± 23.57 | 0‐80 |
| Genitals | 4.27 ± 11.83 | 0‐50 |
| Lymphedema Management | ||
| Lymphedema management | 82.50 ± 18.60 | 50‐100 |
| Wound care+ lymphedema management | 17.50 ± 18.49 | 0‐50 |
3.3. Characteristics of lymphedema service and standards of care
Table 3 describes characteristics of lymphedema service. There are 12 lymphedema services in Saudi Arabia, according to the survey responses received. Most of these services are in Riyadh (58%; n = 7), Jeddah (25%; n = 3), and Dammam (17%; n = 2). Of the 12 services, 9 are governmental hospitals, while 3 services are private clinics. All lymphedema services provided both oncology‐related lymphedema and non‐oncology‐related lymphedema services.
TABLE 3.
Characteristics of lymphedema service
| Characteristics | Frequency | |
|---|---|---|
| N | % | |
| Geographical location of services | ||
| Riyadh | 7 | 58.33 |
| Jeddah | 3 | 25 |
| Dammam | 2 | 16.67 |
| Location of services | ||
| Governmental hospital | 9 | 75 |
| Private clinics | 3 | 25 |
| Types of lymphedema services | ||
| Comprehensive lymphedema service | 13 | 72.22 |
| Standard lymphedema service | 5 | 27.78 |
| Other types of lymphedema services | ||
| Soft tissue mobilisation | 13 | 72.22 |
| Wound management | 9 | 50.00 |
| Pneumatic compression pump | 6 | 33.33 |
| Kinesio taping | 6 | 33.33 |
| Laser | 3 | 16.67 |
| Hydrotherapy | 2 | 11.11 |
| Capacity of lymphedema services/month; mean ± SD (range) | ||
| Initial consultation | 22.11 ± 18.88 | (0‐70) |
| Intensive treatment | 10.17 ± 8.96 | (0‐28) |
| Follow‐up appointments | 21.50 ± 22.50 | (0‐70) |
| Patients seen by practitioner/month; mean ± SD (range) | ||
| Initial consultation | 13.94 ± 13.63 | (0‐50) |
| Intensive treatment | 9.56 ± 6.81 | (0‐80) |
| Follow‐up appointments | 19.22 ± 18.92 | (0‐70) |
| Patients on waiting list/month (mean ± SD (range) | ||
| Initial consultation | 3.67 ± 6.49 | (0‐20) |
| Intensive treatment | 4.56 ± 9.24 | (0‐40) |
| Follow‐up appointments | 3.72 ± 11.67 | (0‐50) |
| Average number of staffs employed in each service (mean ± SD (range) | ||
| Doctors | 1.17 ± 1.65 | (0‐5) |
| Physical therapists | 2.67 ± 0.90 | (1‐4) |
| Occupational therapists | 0.39 ± 0.78 | (0‐3) |
| Nurses | 0.39 ± 0.78 | (0‐2) |
| Social workers | 0.28 ± 0.57 | (0‐2) |
| Psychologists | 0.28 ± 0.57 | (0‐2) |
| Administrative staff | 0.72 ± 1.48 | (0‐5) |
| Referral sources to lymphedema practitioners (respondents/responses) | 18/63 | |
| Oncology surgeons | 14 | 77.77 |
| Radiation oncologists | 13 | 72.22 |
| Dermatologists | 11 | 61.11 |
| Podiatrists | 7 | 38.89 |
| Primary care physicians | 8 | 44.45 |
| Medical oncologists | 4 | 22.22 |
| Patient self‐referrals | 3 | 16.67 |
| Vascular specialists | 3 | 16.67 |
| Number of referral per month | ||
| <10 | 8 | 44.44 |
| 11‐20 | 8 | 44.44 |
| >20 | 2 | 11.11 |
Abbreviations: MLD, manual lymph drainage; SDL, self‐lymph drainage.
Practitioners reported that the average multidisciplinary staffs employed within lymphedema services were six (range 1‐6), with the highest proportion being physical therapists (3; range 1‐4). The average number of social workers, psychologists, and/or psychiatrists employed in the lymphedema services is low (range 0‐2).
Regarding the treatments used in lymphedema services, most of lymphedema practitioners (72%) offered five or more treatment options of CDT. This treatment was comprised of manual lymphatic drainage (78%), compression bandaging (83%), compression garments (89%), skin care (83%), remedial exercise, and risk‐reduction education (each 94%), while 28% of practitioners provided less than four elements of CDT. The practitioners listed varieties of interventions they used as part of treatment besides CDT. These included soft tissue mobilisation (72%), pneumatic compression and kinesio taping (each 33%), low‐level laser therapy (17%), and hydrotherapy (11%). Furthermore, 50% of the practitioners reported that, on average 18% of lymphedema patients received wound management either in physical therapy department, surgical, and/or vascular units. Practitioners reported their caseloads varied with an average of 43 patients per month (14 for the initial consultation, 9 for intensive treatment, and 19 for follow‐up). For patients on a waiting list, lymphedema practitioners have approximately four patients for the initial consultation, four for intensive treatment, and four for follow‐up on the waiting list (approximately 12 patients). The perceived capacity of patients seen in the lymphedema services by practitioners varied for: initial consultation (22; range 0‐70), intensive treatment (10; range 0‐28), and follow‐up (22; range 0‐70).
Referral sources were collected, allowing each respondent (n = 18) to contribute multiple responses (n = 63). Referrals for services came from a variety of reported referral sources whereby oncology surgeons (78%), radiation oncologists (72%), dermatologists (61%), and primary care physicians (44%) were strong referral sources. Podiatrists (39%) and medical oncologists (22%) were also common sources of referral, while vascular specialists and patient self‐referral were the lowest referral source (each 17%). The highest proportion (89%) of respondents had referral rates <20 cases/month, while the remainder (11%) had referral rates of >20 cases/month.
Figure 2 illustrates the practitioner ratings of the standard of care received by patients with different lymphedema diagnoses. Eighty‐nine percent of the lymphedema practitioners reported patients with BCRL receiving a rating of the highest standard of care, while 56% of practitioners rated the standard of care as high or very high for patients with lymphedema secondary to other types of cancer. Approximately, less than 28% of lymphedema practitioners rated the standard of care as high or very high for both primary lymphedema and non‐cancer‐related lymphedema.
FIGURE 2.
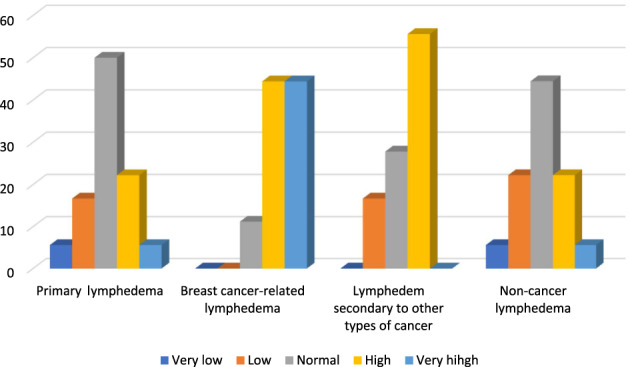
Practitioners' ratings of the standard of care received by patients with different types of lymphedema
3.4. Potential barriers to lymphedema practice
As shown in Table 4, the most common barriers reported by lymphedema practitioners were professional/work‐related (44%‐100%), with an inadequate number of certified therapists most frequently identified (100%). Limited space for practice/management (89%) and lack of awareness of lymphedema management among other medical professionals (78%) were among the most commonly encountered difficulties. Other barriers identified were insufficient information regarding lymphedema management for patients (72%) and access to trained therapists (72%), and lack of awareness of lymphedema management among physical therapists (61%). The least common barriers were lack of administrative support (50%) and lack of adequate referral systems (44%).
TABLE 4.
Potential barriers reported during the lymphedema management (N = 18)
| Barrier category | Barriers | Strongly agree/agree N (%) | Strongly disagree/disagree N (%) |
|---|---|---|---|
| Professional/work‐related | Lack of awareness of lymphedema management among therapists | 11 (61.11) | 3 (16.67) |
| Inadequate number of certified therapists | 18 (100) | ‐ | |
| Lack of awareness of lymphedema management among other medical professions | 14 (77.77) | 1 (5.56) | |
| Insufficient information regarding lymphedema management for patients | 13 (72.22) | 2 (11.11) | |
| Limited space for lymphedema practice/management | 16 (88.89) | 2 (11.11) | |
| Insufficient access to trained therapists, particularly in rural area | 13 (72.22) | 3 (16.67) | |
| Lack of administrative support | 9 (50%) | 6 (33.33) | |
| Lack of adequate referral system | 8 (44.44) | 2(11.11) | |
| Client‐family‐related | Lack of financial support | 13 (72.22) | 4 (22.22) |
| Difficulties with transportation and logistics | 13 (72.22) | 4 (22.22) | |
| Lack of social support and motivation | 12 (66.67) | 5 (27.78) | |
| Limited physical activities | 12 (66.67) | 3 (16.67) | |
| High cost of treatment | 11 (61.11) | 4 (22.22) | |
| Poor treatment compliance among lymphedema patients | 11 (61.11) | 3 (16.67) | |
| Patient dissatisfaction with treatment program | 6 (33.33) | 7 (38.89) |
The client‐family‐related issues were the lesser commonly reported barriers by respondents (33%‐72%). Furthermore, lack of financial support and difficulties with transportation were the most common barrier identified (each = 72%). Interestingly, poor compliance and dissatisfactions with the treatment was among the least common barriers identified (61% and 33%, respectively). Other barriers identified through the free‐text option included: specific funding obstacles, caregivers and administrative issues, garment fitting and costs, and psychological assessment and support.
4. DISCUSSION
To our knowledge, this survey was the first to identify and characterise lymphedema services provisions in Saudi Arabia. The findings from this study suggest that skilled lymphedema practitioners provide a good and reasonable lymphedema services. However, the existing lymphedema services are not sufficient, are disjointed, and lack defined staffs.
The first aim of this study was to explore the profile of the practitioners working in lymphedema services. The results reported that most of the respondents were physical therapists (94%) who completed 135 hours of basic training course and were certified as lymphedema therapists (89%). These findings reflect that skilled physical therapists are a primary resource responsible for lymphedema management. These findings were supported by the published literature of the past 10 years whereby physical therapists predominantly represent (27%‐50%) of disciplines involved in delivering most of the lymphedema services. Furthermore, results from the United States, 29 , 30 Ireland, 31 , 32 Scotland, 33 Australia, 34 Canada, 30 , 35 , 36 and England 37 confirmed that 23% to 93% of lymphedema practitioners worldwide have completed 135 hours of basic training course. However, the literature and clinical practice guidelines suggest lymphedema practitioners came from multidisciplinary specialists, including physical therapists, in addition to occupational and massage therapists, nurses, and physicians. 29 , 36 , 38 To our knowledge, there is insufficient data to identify other specialised groups interested in lymphedema practice in Saudi Arabia, reflecting the small number of practitioners in Saudi Arabia who treat lymphedema. The highest proportion of certified practitioners reported in the current study as physical therapists could be related to selection bias secondary to the methods of survey administrations.
In the current study, the highest proportion of practitioners were female (78%), which reflect the conservative culture of Saudi Arabia, where males and females are treated by same genders, as the highest proportion of lymphedema cases are related to breast cancer treatment, occurring predominantly in women. This finding is not aligned with the published literature, 29 , 36 , 38 where there are no restrictions regarding genders and most of the respondents are free to treat male or female patients.
In the current study, 78% of lymphedema practitioners highlighted the perceived need for further learning and educational updating. This finding agrees with Sneddon et al who recommended that most of lymphedema practitioners need further education and practical training for updating their skills. 33 Davies et al reported that 64% of lymphedema practitioners (n = 54) showed that their educational needs were mostly/completely met. 36 The variability in response rate might be related to questions asked in the survey, and unmet educational needs related to lymphedema in the last 5 years for practitioners.
Regarding the preferred modes to cover their educational needs, most of the respondents (72%) indicated that undergraduate educational modules about the lymphatic system and lymphedema would be a useful resource to address some unmet educational needs. This finding has been outlined in the literature review, 29 , 30 , 31 , 32 , 33 , 34 , 36 and as a recommendation from the educational forum of the International Lymphedema Framework 2012. 39 , 40 By contrast, 50% of the practitioners showed that self‐directed learning would be useful and might be an important alternative for both workshops/conferences and supervised clinical placement training to meet their lymphedema educational needs. The reason provided for these modes of delivery included higher caseload and lack of funding and time to attend related conferences and workshops. Therefore, it is important to support and facilitate lymphedema education across Saudi Arabia.
In the current study, 78% of practitioners believed they did not have sufficient opportunities for professional development and only 56% of the practitioners rated themselves as excellent in terms of how experienced they felt, which reflects a lower level of experiences among the practitioners. These finding are in agreement with results of Murray et al, 31 where 94% of lymphedema practitioners do not think they have sufficient opportunities for professional development. Reasons might be attributed to the fact that 72% of practitioners have <5 years of experiences and treating lymphedema patients represents only part of their caseload, as the majority of the practitioners (67%) work in various clinical setting.
The second aim of this study was to identify characteristics of lymphedema patients. The current findings showed that lymphedema cases were much higher among adult and elderly patients and the majority were females (68%). These findings are consistent with previous studies by Moffatt et al who reported that lymphedema can occur at any age, with significant increase in the rate with age. 41 , 42 Furthermore, results from Turkey 43 and Japan 44 reported that most of lymphedema patients were females (93% and 60%‐95%, respectively). In the current study, secondary lymphedema is more common (75%) with the majority being oncology‐related (54%), and 47% being BCRL. These findings are support by published literature from the United States, 29 Ireland, 31 and Turkey, 43 where 84%, 87%, and 85% of lymphedema were secondary, respectively. In addition, recent international survey by Anderson and colleague in 2019 confirmed that 80% of patients had secondary lymphedema, of whom 53% had oncology‐related lymphedema. 38 Saudi patients had fewer wounds (17.5%), compared with other studies. 43 , 44 This pattern of lymphedema might be because of higher prevalence of breast cancer in Saudi Arabia 24 and rehabilitation services treating a high proportion of breast cancer patients, rather than dermatology or vascular surgery services.
A further key study aim was to explore lymphedema services and standard of care. The current survey found that the vast majority of practitioners worked in double settings (lymphedema services and outpatient/inpatient physical therapy services (67%), which were hospital‐based, in larger urban areas, with a lesser percentage practicing in home care (6%). There are insufficient numbers of health care staffing; with the vast majority being physical therapists (average = 2.67; range 1‐4), while the average number of other health care professions within each service was less than one per service. This pattern of services was similar to those reported in recent surveys and literature where lymphedema practitioners worked in varieties of clinical settings, including hospital‐based outpatients and inpatients (60%), private clinic (38%), and home care (9%), with a heterogeneous distribution of lymphedema services. 29 , 34 , 35 , 38 , 45 , 46 , 47 This pattern resulted in lower number of hours dedicated to lymphedema services; inadequate time to address lymphedema patient demand and higher caseload of the services; and loss of skill, competence, and confidence for practitioners. 31
In these results, fewer respondents reported working in a service that had a social worker and psychologist, similar to the findings from other countries, such as Australia 34 and Ireland 31 , 32 who reported that their services might provide social, psychological, or psychiatric employment. These findings contradicted the best practice guidelines and literature reviews that suggest lymphedema management requires multidisciplinary and multimodal services, 32 , 40 , 41 , 45 , 48 , 49 as lymphedema has a significant impact on the patient's emotional, physical, social, and psychological aspect. 6 , 41 , 42 , 50 , 51
Treatment with CDT was available in almost all clinical settings, where 72% of practitioners provide four or more elements of the ‘gold standard’ of CDT, with a lesser percentage of respondent practitioners providing ‘standard’ lymphedema management (defined as less than four services) which are essential for the effective management of lymphedema as reported by international consensus. 48 Recent surveys reported CDT was the most common intervention. 29 , 30 , 35 , 46 Anderson et al reported that 55% of therapists offered seven or more treatment options. 38 Variability in the delivery of intermittent pneumatic compression, kinesio taping, and low‐level laser for treatment of lymphedema as found in the current survey may reflect a lack of evidence regarding these modalities, despite their therapeutic benefits. 52
In the current survey, there are variations in referral sources with high access for oncology‐related referrals and low access for non‐oncology‐related referrals. These findings are consistent with results of Hunley et al who reported strong referral sources from cancer‐related sources and primary care physicians. 30 Vascular specialists, podiatrists, and patient self‐referral were the lowest sources of referrals. This might be because of the lack of awareness of lymphedema management among different health care professions, 31 , 34 , 51 , 53 , 54 demonstrating difficulties in integrating lymphedema services across disciplines.
Lymphedema practitioners often face barriers to their practice. In the current study, two themes emerged. The first theme is a professional/work‐related issue, which reflects the importance of knowledge and awareness of lymphedema and work settings conditions among health care practitioners. General analysis of this theme shows lack of certified lymphedema therapists and lack of awareness among health care profession of lymphedema as a diagnosable and treatable health condition. Similar findings were postulated even across the United States, 29 , 36 Canada, 35 Ireland, 31 and Scotland. 33
Most practitioners in the current study did not receive undergraduate health professional education about lymphedema. This finding aligned with a published survey by Bowman et al who reported that most health care practitioners did not receive formalised teaching on lymphedema during undergraduate health professional education. These findings reflected a great need to organise and promote training/education on lymphedema. Therefore, lymphedema should be included in the curricula of medical and allied health practitioners in undergraduate degrees to close the knowledge gap and to increase the evidence base so that physicians can be convinced of the effectiveness of the components of lymphedema treatment.
The work settings showed limited space for lymphedema practice (89%), lack of access (72%), and lack of adequate referral sources (44%). These reflected heterogeneity and inadequate geographical location of lymphedema services across Saudi Arabia, as most mapped lymphedema services and therapists are restricted to large hospitals in large cities, making it more difficult to seek qualified therapy. These issues lead to perception about the poorer standard of services provided to patients who had non‐cancer‐related lymphedema, compared with patients living in large cities and having cancer‐related lymphedema. These results are like the findings from previous studies of service provision from Australia, 35 Ireland, 31 the United Kingdom, 42 and Scotland, 33 which highlighted that patients living in rural areas may receive poorer lymphedema service, despite differences in culture and/or health care systems between these countries.
A second theme was the client‐family‐related issues. According to responses of lymphedema practitioners (range 61%‐72%), the results suggest difficulty in transportation, lack of financial support, lack of social support, and limited physical activity secondary to lymphedema were considered as perceived barriers for lower rate of compliance among lymphedema patients, from therapists' perceptions. These results are similar to previous studies of service provision from Australia 35 and the United Kingdom. 42
A strength of this study is that it is the first survey to identify and characterise the provision of lymphedema services in Saudi Arabia, and findings will interest those working in the lymphedema field and service providers. However, the major limitation of the study is the small sample size (n = 18 practitioners) which likely reflects the small number of practitioners who treat lymphedema. The limited sample size might also be due to the complexity of the questionnaire, and, therefore, it may not truly represent the population.
5. CONCLUSION
The study has shown the status and characteristics of lymphedema therapists and their perceptions of services provided to lymphedema patients in Saudi Arabia. The results suggest lymphedema practitioners provide a reasonable service for lymphedema patients' treatments; however, service provisions are still limited and needs are unmet. Therefore, more staffing is required to promote awareness of the condition and related services, to develop and implement appropriate educational strategies, and improve geographical and multidisciplinary coordination of the services in Saudi Arabia.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
M.O. drafted the manuscript, and conducted data analysis of the study. N.A.D. and R.G. were involved in designing of the study, data analysis, and manuscript revision. J.A. provided overall guidance to revise the survey, prepare and revise the manuscript, and serve as a mentor. All authors read and approved the final version of the manuscript.
ACKNOWLEDGEMENT
The authors appreciate the support from the Research Center, College of Applied Medical Sciences, and the Deanship of Scientific Research, King Saud University, Riyadh, Kingdom of Saudi Arabia.
Omar MTA, Al‐Dhwayan NM, Gwada RFM, Armer JM. Lymphedema rehabilitation: Provision and practice patterns among service providers: National survey. Int Wound J. 2022;19(2):339–350. 10.1111/iwj.13634
DATA AVAILABILITY STATEMENT
The dataset analysed during the current study, as included in this manuscript, are available from the corresponding author on reasonable request.
REFERENCES
- 1. International Society of Lymphology . The diagnosis and treatment of peripheral lymphedema: 2013 consensus document of the International Society of Lymphology. Lymphology. 2013;46(1):1‐11. [PubMed] [Google Scholar]
- 2. Kayıran O, De La Cruz C, Tane K, Soran A. Lymphedema: from diagnosis to treatment. Turk J Surg. 2017;33:51‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Moffatt CJ, Franks PJ, Doherty DC, et al. Lymphodema: an underestimated health problem. Q J Med. 2003;96:731‐738. [DOI] [PubMed] [Google Scholar]
- 4. Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer. Cancer. 2010;116:5138‐5149. [DOI] [PubMed] [Google Scholar]
- 5. Fu MR. Breast cancer‐related lymphedema: symptoms, diagnosis, risk reduction, and management. World J Clin Oncol. 2014;5(3):241‐247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fu MR, Ridner SH, Hu SH, Stewart BR, Cormier JN, Armer JM. Psychosocial impact of lymphedema: a systematic review of literature from 2004 to 2011. Psychooncology. 2013;22:1466‐1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim SI, Lim MC, Lee JS, et al. Impact of lower limb lymphedema on quality of life in gynecologic cancer survivors after pelvic lymph node dissection. Eur J Obstet Gynecol Reprod Biol. 2015;192:31‐36. [DOI] [PubMed] [Google Scholar]
- 8. Torres Lacomba M, Yuste Sánchez MJ, Zapico Goñi A, et al. Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomized, single blinded, clinical trial. BMJ. 2010;340:b5396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lasinski BB, McKillip Thrift K, Squire D, et al. A systematic review of the evidence for complete decongestive therapy in the treatment of lymphedema from 2004 to 2011. PM R. 2012;4(8):580‐601. [DOI] [PubMed] [Google Scholar]
- 10. Rogan S, Taeymans J, Luginbuehl H, Aebi M, Mahnig S, Gebruers N. Therapy modalities to reduce lymphoedema in female breast cancer patients: a systematic review and meta‐analysis. Breast Cancer Res Treat. 2016;159:1‐14. [DOI] [PubMed] [Google Scholar]
- 11. Baxter GD, Liu L, Petrich S, et al. Low level laser therapy (Photobiomodulation therapy) for breast cancer‐related lymphedema: a systematic review. BMC Cancer. 2017;17:833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gatt M, Willis S, Leuschner S. A meta‐analysis of the effectiveness and safety of kinesiology taping in the management of cancer‐related lymphoedema. Eur J Cancer Care (Engl). 2017;26(5):e12510. [DOI] [PubMed] [Google Scholar]
- 13. Finnane A, Janda M, Hayes SC. Review of the evidence of lymphedema treatment effect. Am J Phys Med Rehabil. 2015;94(6):483‐498. [DOI] [PubMed] [Google Scholar]
- 14. Armer JM, Feldman JL, Ostby PL, et al. Simplifying evidence‐based management of breast cancer‐related lymphedema. Expert Rev Qual Life Cancer Care. 2016;15:389‐402. [Google Scholar]
- 15. Borman P. Lymphedema diagnosis, treatment, and follow‐up from the view point of physical medicine and rehabilitation specialists. Turk J Phys Med Rehab. 2018;64:179‐197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fialka‐Moser V, Korpan M, Varela E, et al. The role of physical and rehabilitation medicine specialist in lymphoedema. Ann Phys Rehabil Med. 2013;56:396‐410. [DOI] [PubMed] [Google Scholar]
- 17. Neubauer M, Schoberwalter D, Cenik F, Keilani M, Crevenna R. Lymphedema and employability—review and results of a survey of Austrian experts. Wien Klin Wochenschr. 2017;129(5–6):186‐191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Australasian Lymphology Association . Lymphoedema National Service Equity Survey 2002. Australasian Lymphology Association: Milton, Queensland, Australia; 2003. https://www.aogp.com.au [Google Scholar]
- 19. BreastCare Victoria . A Review of Lymphoedema Services in Victoria. Melbourne, Victoria, Australia: Victorian Government Department of Human Services; 2005. [Google Scholar]
- 20. Department of Health, Social Services and Public Safety (DHSSPS) . Lymphoedema Services: Report of the Lymphoedema Services Review Group. Belfast, Northern Ireland: DHSSPS; 2004. [Google Scholar]
- 21. Morgan PA. Health professionals' ideal roles in lymphoedema management. Br J Community Nurs. 2006;11:5‐8. [Google Scholar]
- 22. Richmond K. A review of lymphoedema services in Wales. Received in private correspondence from the Welsh Association of Lymphoedema Services (WALS); 2003.
- 23. Todd M. Lymphoedema: sizing up the problem. Br J Community Nurs. 2006;11(8):3‐4. [Google Scholar]
- 24. Althubiti MA1, Nour Eldein MM. Trends in the incidence and mortality of cancer in Saudi Arabia. Saudi Med J 2018; 39(12):1259–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Al‐Quwaidhi AJ, Pearce MS, Critchley JA, Sobngwi E, O'Flaherty M. Trends and future projections of the prevalence of adult obesity in Saudi Arabia, 1992–2022. East Mediterr Health J. 2014;20(10):589‐595. [PubMed] [Google Scholar]
- 26. Warren LE, Miller CL, Horick N, et al. The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys. 2014;88:565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jammallo LS, Miller CL, Singer M, et al. Impact of body mass index and weight fluctuation on lymphedema risk in patients treated for breast cancer. Breast Cancer Res Treat. 2013;142:59‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moshref SS, Jamal YS, Al Gaithy ZK, et al. Frequency of breast cancer surgery related arm lymphedema at King Abdulaziz University Hospital 2008‐2015, a tertiary center experience, Jeddah, Saudi Arabia. JKAU Med Sci. 2017;24(2):17‐28. [Google Scholar]
- 29. Armer JM, Paskett ED, Fu M, et al. A survey of lymphedema practitioners across the US. J Lymphoedema. 2010;5(2):95‐97. [Google Scholar]
- 30. Hunley JH, Campione E, Jackson K, Feldman J. Lymphoedema practice patterns: the current state of the industry. J Lymphoedema. 2020;15(1):65‐70. [Google Scholar]
- 31. Murray M. Living with Lymphedema in Ireland: A Mixed Methods Exploration of Patient and Service Provider Perspectives [Unpublished MSc thesis]. Dublin: Dublin City University; 2010.
- 32. A Working Group Report . Lymphoedema and lipoedema treatment in Ireland: a model of care for Ireland – a Working Group Report; 2018.
- 33. Sneddon MC, Franks PJ, Pearson J. Lymphedema: Service Provision and Needs in Scotland. Final Report. Glasgow. University of Glasgow; 2008.
- 34. BreastCare Victoria . A Review of Lymphedema Services in Victoria Sept 2003‐June 2004. Melbourne, Australia: Department of Human Services; 2003. [Google Scholar]
- 35. Hodgson P, Towers A, Keast D, Kennedy A, Pritzker R, Allen J. Lymphedema in Canada: a qualitative study to help develop a clinical, research and education strategy. Curr Oncol. 2011;18:e260‐e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Davies R, Fitzpatrick B, O'Neill A, Sneddon M. Lymphoedema education needs clinicians: a national study. J Lymphoedema. 2012;7(2):14‐24. [Google Scholar]
- 37. British Lymphology Society (BLS) . Framework for Education. BLS: Gloucester, UK; 2001. [Google Scholar]
- 38. Anderson EA, Anbari AB, Armer NC, Armer JM. Lymphoedema therapists: a national and international survey. J Lymphoedema. 2019;14(1):22‐24. [PMC free article] [PubMed] [Google Scholar]
- 39. International Lymphoedema Framework . Conference proceedings. Towards global implementation of best practice: opportunities and challenges. Montpellier ILF Conference, June 2012.
- 40. International Lymphoedema Framework . Template for management: developing a lymphoedema service; 2007. www.soffed.co.uk/lymphorg
- 41. Williams AF, Moffatt CJ, Franks PJ. A phenomenological study of the lived experiences of people with lymphedema. Int J Palliat Nurs. 2004;10:279‐280. [DOI] [PubMed] [Google Scholar]
- 42. Todd M. Lymphedema: sizing up the problem. Br J Community Nurs. 2006;11(8):3‐4. [Google Scholar]
- 43. Borman P, Moffatt C, Murray S, et al. LIMPRINT study: the Turkish experience. Lymphat Res Biol. 2019;17:202‐210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Dai M, Nakagami G, Sugama J, et al. The prevalence and functional impact of chronic edema and lymphedema in Japan: LIMPRINT study. Lymphat Res Biol. 2019;17(2):195‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Shimony A, Tidhar D. Lymphedema: a comprehensive review. Ann Plast Surg. 2008;60(2):228. [DOI] [PubMed] [Google Scholar]
- 46. Polo KM, Rundquist PJ, Krumdick ND, Gamble GL. National survey of lymphedema therapists' dosing of complete decongestive therapy in breast cancer survivors with lymphedema. Internet J Allied Health Sci Pract. 2017;16(1):1‐8. [Google Scholar]
- 47. Keast DH, Allen JO, Despatis M, Brassard A. Chronic oedema/lymphoedema: under‐recognised and undertreated. Int Wound J. 2015;12(3):328‐333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Medical Education Partnership (MEP) . International Consensus Best Practice for the Management of Lymphoedema. London, UK: Medical Education Partnership; 2006. [Google Scholar]
- 49. Clinical Resource Efficiency Support Team (CREST) . Guidelines for the Diagnosis, Assessment and Management of Lymphoedema. Belfast, Northern Ireland: CREST; 2008. [Google Scholar]
- 50. Morgan PA, Moffatt CJ, Doherty DC. Achieving consensus in lymphedema care. J Lymphedema. 2006;1(1):22‐31. [Google Scholar]
- 51. Bulley C. A needs assessment of lymphoedema services in Fife and resulting recommendations. Prim Health Care Res Develop. 2007;8:128‐140. [Google Scholar]
- 52. Rodrick JR, Poage E, Wanchai A, Stewart BR, Cormier JN, Armer JM. Complementary, alternative, and other noncomplete decongestive therapy treatment methods in the management of lymphedema: a systematic search and review. PM R. 2014;6:250‐274. quiz 274. [DOI] [PubMed] [Google Scholar]
- 53. Chance‐Hetzler J, Armer J, Van Loo M, et al. Prospective lymphedema surveillance in a clinic setting. Pers Med. 2015;5:311‐325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sitzia J, Woods M, Hine P, Williams A, Eaton K, Green G. Characteristics of new referrals to twenty‐seven lymphoedema treatment units. Eur J Cancer Care. 1998;7:255‐262. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset analysed during the current study, as included in this manuscript, are available from the corresponding author on reasonable request.


