The COVID-19 pandemic has affected screening, diagnosis, and treatment of cancer. During the first lockdown in Bavaria, Germany, hospital admissions, surgery, and other procedures were postponed (20 March to 15 May 2020). Studies in Germany and other countries have shown:
Declines in cancer incidence and referrals for suspected cancer (1, 2)
Delay of elective surgery (3)
We set out to describe the effects of the first COVID-19 wave on incident cancer cases and cancer treatments. In particular, we focused on surgery for early-stage cancers (stage I).
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Methods
Data were retrieved from the population-based Bavarian Cancer Registry (to 26 March 2021). We included all incident cancer cases and cancer treatments reported by providers with timely registration. This inclusion criterion was met by 29 of 42 certified oncology centers and organ cancer centers, 36 of 210 hospital departments, and 231 of 621 outpatient facilities in five of the seven administrative regions of Bavaria. Comparison of our study sample with data for all providers in 2019 showed no differences in stage distribution, apart from a lower proportion of cases with unknown stage X (13% versus 34%).
The main outcomes were the number of incident cancer cases (ICD-10 C00–C69 without C44, C73/C74) according to stage (I, II, III, IV, X), treatments according to treatment type (surgery, radiotherapy, systemic treatment), and surgery for stage I cancer according to tumor site (breast, prostate, colorectum, lung, skin/melanoma).
We calculated the number of incident cancer cases and cancer treatments with the corresponding 95% confidence intervals (CI) in 2019 and 2020, stratified by month, based on a Poisson approach. We estimated the relative changes on the basis of a t-distribution using the Estimated Annual Percentage Change (EAPC) function in the statistical software R. For the main outcomes, we used an exact binomial test (two-sided) with an α error of 0.05 to test whether the differences were significant. The problem of multiple testing was accounted for by Bonferroni correction (α error of 0.003 with 16 significance tests) and calculation of a correspondingly adjusted CI. All statistical analyses were performed in R, version 4.0.2.
Results
The total number of incident cancer cases from January to September decreased from 7361 in 2019 to 7123 in 2020 (-3.2%, 95% CI [–7.9%; 1.6%]; p = 0.024), which was not significant after correction for multiple testing (table). Stratified by stage, a significant decline occurred in incident cancer cases of stage I (-10.5% [–18.2%; –2.0%]; p <0.001) but not in stages II–IV or unknown stage X. Stratified by site, the largest decreases were for stage I incident cancer cases of the colorectum and prostate.
Table. Incident cases for all cancer stages and surgeries in cancer stage I by tumor site from January to September 2020 compared to 2019.
| Incident cases |
Numbers
2019 |
Numbers
2020 |
Difference 2019/2020
(% [95-%-CI]) |
| All sites | 7361 | 7123 | −238 (−3.2 [−7.9; 1.6]) |
| Breast | 1498 | 1471 | −27 (−1.8 [−8.6; 5.5]) |
| Prostate | 1213 | 1217 | 4 (0.3 [−7.3; 8.6]) |
| Colorectum | 945 | 925 | −20 (−2.1 [−10.6; 7.2]) |
| Lung | 694 | 620 | −74 (−10.7 [−19.8; −0.4]) |
| Melanoma | 396 | 381 | −15 (−3.8 [−16.4; 10.7]) |
|
Surgeries
stage I |
Numbers
2019 |
Numbers
2020 |
Difference 2019/2020
(% [95-%-CI]) |
| All sites | 2472 | 2264 | −208 (−8.4 [−16.0; −0.2]) |
| Breast | 646 | 645 | −1 (−0.2 [−15.3; 17.7]) |
| Prostate | 159 | 175 | 16 (10.1 [−20.4; 52.1]) |
| Colorectum | 269 | 198 | −71 (−26.4 [−44.2; −2.9]) |
| Lung | 99 | 93 | −6 (−6.1 [−38.7; 43.9]) |
| Melanoma | 361 | 258 | −103 (−28.5 [−43.8; −9.1]) |
CI, Confidence interval
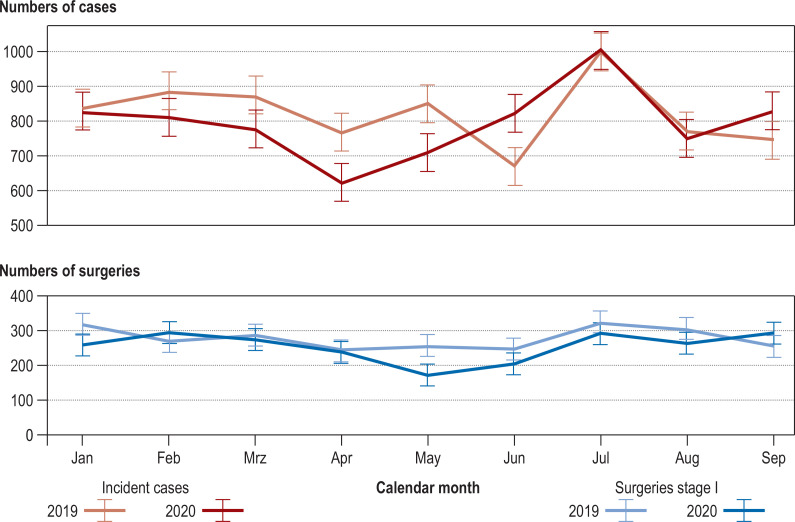
The Figure shows the monthly number of incident cancer cases for all sites in 2020 in comparison with 2019. Total cases decreased by –10.7% [–19.0%; –1.6%], –18.5% [–26.7%; –9.4%], and –16.5% [–24.5%; –7.8%] in March, April, and May 2020 compared with 2019. For June 2020, the number of incident cancer cases was 22.7% [10.7%; 35.9%] higher than in 2019 (figure).
Figure.
Number of incident cases for all cancer stages and surgeries in cancer stage I for all sites from January to September in 2019 and 2020 including 95% confidence intervals.
The number of cancer treatments declined significantly in the period January to September 2020 compared with 2019 for all treatment types combined (–4.0% [–6.9%; –1.1%], p <0.001) and for radiotherapy (–6.1% [–11.1%; –0.8%]; p <0.001). After correction for multiple testing, the changes for systemic therapy were no longer significant (–4.0% [–8.8%; 1.0%]; p = 0.009). While overall surgery did not decline significantly (–2.3% [–7.1%; 2.6%]; p = 0.080), surgery in incident cancer cases of stage I decreased significantly (figure). Significant changes were found for all sites combined (–8.4% [–16.0%; –0.2%]; p = 0.001), colorectum (–26.4% [–44.2%; –2.9%]; p <0.001), and melanomas (–28.5% [–43.8%; –9.1%]; p <0.001), but not for breast, prostate, or lung (table).
Discussion
The research showed that incident cancer cases and cancer treatments in Bavaria, Germany, declined in the period January to September 2020 compared with 2019, although the reduction in incident cases was not significant. The incident cancer cases dropped particularly in April, while the highest decrease in treatments followed a month later, in May. The reductions were most pronounced for stage I cancers, particularly with regard to surgery for colorectal cancer and melanomas. Studies in Germany and other countries have shown similar decreases in incident cancer cases (1, 2). With regard to cancer treatments, we identified a decrease in radiotherapy, as observed by others (5), but not in systemic treatments (4). The considerable reductions in certain months are a cause of concern, as even minor delays in the diagnosis and treatment of cancer may lead to worse outcomes.
A limitation of our study is that we cannot exclude a selection bias, as providers with timely reporting may differ from the overall population of providers. This may lead to underestimation—or overestimation—of the impact of the COVID-19 pandemic on incident cancer cases and cancer treatments. Active countermeasures such as public awareness campaigns are required to restore the uptake of screening services and treatment, particularly for the entities colorectum and melanoma.
References
- 1.Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.17267. e2017267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piontek D, Klagges S, Schubotz B, Werner C, Wulff J. Documented new cases of cancer in the clinical cancer registries of the German state of Saxony during the COVID-19 pandemic. Dtsch Arztebl Int. 2021;118:328–329. doi: 10.3238/arztebl.m2021.0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bakouny Z, Hawley JE, Choueiri TK, et al. COVID-19 and cancer: current challenges and perspectives. Cancer Cell. 2020;38:629–646. doi: 10.1016/j.ccell.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark JJ, Dwyer D, Pinwill N, Clark P, Johnson P, Hackshaw A. The effect of clinical decision making for initiation of systemic anticancer treatments in response to the COVID-19 pandemic in England: a retrospective analysis. Lancet Oncol. 2021;22:66–73. doi: 10.1016/S1470-2045(20)30619-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spencer K, Jones CM, Girdler R, et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22:309–320. doi: 10.1016/S1470-2045(20)30743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]