Abstract
Background
Splints/orthoses are often recommended to patients with rheumatoid arthritis (RA) to decrease pain, reduce swelling, and/or prevent deformity. These orthoses include resting hand splints, wrist supports, finger splints, and special shoes and shoe inserts.
Objectives
To assess the effectiveness of splints/orthoses in relieving pain, decreasing swelling, and/or preventing deformity, and to determine the impact of splints/orthoses on strength, mobility, and function in people with RA.
Search methods
We searched the Cochrane Field of Physical and Related Therapies Register, Cochrane Musculoskeletal Group Register, Cochrane Controlled Trials Register to issue 4, 2001, MEDLINE, EMBASE, the PEDro data base, and Current Contents up to January 2002, using the search strategy developed by the Cochrane Collaboration. Unpublished studies were sought by handsearching conference proceedings and contacting key experts.
Selection criteria
All randomized control trials (RCTs) and controlled clinical trials (CCTs), case‐control and cohort studies comparing the use of specific orthoses against placebo, another active intervention (including another type of orthoses), or regular treatment were selected according to an a priori protocol.
Data collection and analysis
Two reviewers independently selected the studies and extracted data. The methodological quality of the RCTs and CCTs was assessed using a validated scale.
Main results
Twelve papers reporting on 10 studies met the inclusion criteria. These studies dealt with the following: working wrist splints (5), resting hand and wrist splints (2), special shoes and insoles (3). There is evidence that wearing wrist splints during work statistically significantly decreases grip strength and does not affect pain, morning stiffness, pinch grip, or quality of life after up to six months of regular wear. We found no evidence that resting wrist and hand splints change pain, grip strength, Ritchie Index, or number of swollen joints. However, participants who wore these splints for two months reported that they preferred use to non‐use, and padded resting splints to unpadded ones. The one study of special shoes provided evidence of significant benefits of wearing extra‐depth shoes for two months, including less pain on walking and stair climbing, and more minutes of pain free walking time. Extra‐depth shoes with semi‐rigid insoles provided better pain relief than extra‐depth shoes alone when worn over 12 weeks. Supporting insoles prevented progression of hallux valgus angle but did not affect pain or function.
Authors' conclusions
There is insufficient evidence to make firm conclusions about the effectiveness of working wrist splints in decreasing pain or increasing function for people with RA. Potential adverse effects, such as decreased range of motion, do not seem to be an issue although some of these splints decrease grip strength and dexterity. Similarly, preliminary evidence suggests that resting hand and wrist splints do not seem to affect range of motion (ROM) or pain, although participants preferred wearing a resting splint to not wearing one. There is evidence that extra‐depth shoes and molded insoles decrease pain during weight‐bearing activities such as standing, walking, and stair‐climbing. Supported insoles may be effective in preventing progression of hallux abductus angle but do not appear to have any impact on pain.
Plain language summary
Working wrist splints and extra‐depth shoes appear to be helpful for people with rheumatoid arthritis
Ten studies examined the effects of working wrist splints, resting hand and wrist splints, and wearing special shoes/ insoles in people with rheumatoid arthritis. Although there is no evidence that wearing resting wrist and hand splints changed pain, grip strength, or number of swollen joints, participants who wore these splints for two months preferred to wear them, and also preferred padded splints. One study provided evidence that wearing extra‐depth shoes for two months resulted in significant benefits of less pain on walking and stair climbing. Extra‐depth shoes with semi‐rigid insoles provided better pain relief than extra‐depth shoes alone.
Background
Currently, rheumatoid arthritis (RA) affects approximately 0.5 to 1% of the population in industrialized countries (Suarez‐Almazor 2001). This figure is expected to rise as members of the post Second World War generation enter their senior years. Splints/orthoses are often prescribed as an adjunct to medical treatment (Ouellette 1991).
Splints and orthoses are "any medical device added to a person's body to support, align, position, immobilize, prevent or correct deformity, assist weak muscles, or improve function" (Deshaies 2002). We use both terms in this review, even though they are interchangeable, as there is a tendency among clinicians to use one or the other term when referring to specific devices. Splints/orthoses for the treatment of rheumatoid arthritis include rigid or flexible wrist orthoses, static or dynamic finger orthoses, and specialized shoes and insoles. Goals of splint/orthotic use include reduction of pain and/or swelling, prevention of contractures, and/or provision of joint stability (Melvin 1989). While such interventions usually carry a relatively low cost, they do require skilled fabrication, and follow‐up. They also require a commitment on the part of the participant to wear what is often a rather cumbersome device.
Objectives
To assess the effectiveness of orthoses in relieving pain, decreasing swelling, and preventing deformity. To determine the impact of orthoses on strength, mobility, and function.
Methods
Criteria for considering studies for this review
Types of studies
All randomized controlled trials (RCTs) and controlled clinical trials (CCTs), case‐control and cohort studies comparing the use of specific orthoses against placebo, another active intervention (including another type of orthoses), or regular treatment were selected according to an a priori protocol, which included a requirement for at least five participants in each group. Only studies written in English or French were considered.
Types of participants
People 18 years of age and older who had been diagnosed with rheumatoid arthritis. Studies including diverse populations were accepted if 50% or more of the participants were diagnosed with rheumatoid arthritis.
Types of interventions
Rigid, semi‐rigid, or soft orthotics designed to provide support and/or pain relief at any joint, with the exception of joints of the neck or back.
Types of outcome measures
Studies were considered for inclusion if OMERACT outcomes were measured, that is, number of tender joints per participant, number of swollen joints per participant, pain, physician's global assessment, participant's global assessment, functional status, acute phase reactants, and radiological evidence of damage (OMERACT 1993). Studies were also considered for inclusion if any of the following additional outcomes were measured: duration of morning stiffness, muscle strength, endurance, range of motion (ROM), postural status, gait status, walking speed, walking distance, cadence, stride length, systemic components, concomitant medication use, adverse side effects, quality of life, length of stay, discharge disposition, cardiopulmonary capacity, return to work. Compliance was not considered as an outcome measure.
Search methods for identification of studies
We searched the Cochrane Field of Physical and Related Therapies Register, Cochrane Musculoskeletal Group Register, Cochrane Controlled Trials Register (CCTR) to issue 4, 2001, MEDLINE, EMBASE, and the PEDro databases up to January 2002 (see Appendix for search details) (Dickersin 1994). The electronic search was complemented by handsearches of the following: 1) bibliographic references of identified studies; 2) Current Contents up to November 1998 (to identify articles not yet indexed in MEDLINE); 3) abstracts published in special issues of specialized journals or in conference proceedings. Reference lists were handsearched for additional studies reported in published papers, presentations at scientific meetings, and personal communications. Content experts were contacted for additional studies and unpublished data.
Data collection and analysis
Two of three reviewers (MAO, MF, and SR) determined the studies to be retrieved. These reviewers independently extracted data from the retrieved studies using a pre‐developed form. They also independently assessed the methodological quality of the RCTs and CCTs. This data was checked by a third and fourth reviewer (LB, ME).
Results
Description of studies
Twelve papers were identified that reported on 10 eligible studies with a total of 449 participants. Unfortunately none of the studies were similar enough to allow pooling of results. Five studies examined the effects of the use of working wrist splints. Three of these papers considered the effects of splint wear versus no splint (Anderson 1987, Pagnotta 1998, Kjeken 1995), while the two others were head to head studies of different splints (Tijhuis 1998, Stern 1996a, Stern 1996b). Two studies examined the effects of resting splints for the wrist and hand, one examining the effect of wear versus non‐wear (Janssen 1990) while the other was essentially a head to head trial (Callinan 1996). Effects of foot orthoses and special shoes were reported in three studies. One examined the effects of extra‐depth shoes versus regular footwear (Fransen 1997). Another was a trial of soft insoles in extra‐depth shoes versus extra‐depth shoes alone, and semi‐rigid insoles in extra‐depth shoes versus extra‐depth shoes alone (Chalmers 2000). The third examined the effects of Rohadur supporting insoles versus placebo insoles (Budiman‐Mak 1995, Conrad 1996).
Risk of bias in included studies
Methodological quality of the studies was assessed using a validated scale (Jadad 1996) focusing on the presence and quality of randomization, double‐blinding, and description of withdrawals and drop‐outs. Out of a possible total of 5 points, quality rating ranged from 1 to 5, with five of the ten studies receiving a score of 2 and three receiving a score of 3. Points were lost primarily for failure to describe randomization procedures, and failure to blind evaluators and/or participants. Withdrawals were well‐described and exceeded 20% in only one study, where 21% of participants were lost to follow‐up (Budiman‐Mak 1995).
Effects of interventions
Working wrist splints Three studies examined the effects of wearing working wrist splints versus no splint (Anderson 1987, Kjeken 1995, Pagnotta 1998). Grip strength was measured immediately after the splint was donned when four different types of splints (dorsal custom molded low temperature thermoplastic, palmar custom molded low temperature thermoplastic, palmar plastazote and polythene custom molded gauntlet, and ready‐made elastic) were applied to the dominant or non‐dominant hand. Results were expressed as mean difference (MD) with 95% confidence intervals (CI). The only significant differences were in lower grip strength of the non‐dominant hand, with both the palmar custom molded (MD ‐29.10 mm Hg [95% CI: ‐54.04 to ‐4.16]) and the elastic ready‐made splints (MD ‐33.01mmHg [95% CI: ‐62.01 to ‐4.01]) (Anderson 1987). In a separate evaluation of a ready‐made elastic splint after one week of use there were no differences in work performance or pain while using shears or a screwdriver, and no difference in dexterity with or without the splint (Pagnotta 1998). Finally, participants who wore a ready‐made elastic splint for six months demonstrated smaller losses in passive dorsal‐volar range of motion (ROM) compared with those who did not wear the splint. They showed, however, no differences in pain (at rest of in motion), grip strength, morning stiffness, pinch grip, forearm joint circumference, or quality of life (Kjeken 1995).
In head to head studies of two working wrist splints (a ready‐made elastic gauntlet or a custom‐molded medium temperature thermoplastic splint), there was no difference, after two weeks of wear, on pain, joint tenderness, passive ROM, or grip strength with or without the orthoses (Tijhuis 1998). Similarly, there were no differences found with three different types of ready‐made elastic splints (Alimed, Futuro, Rolyan) after one week of wear, on dexterity measured with or without the splint (Stern 1996a), or grip strength measured with the splint removed (Stern 1996b).
Resting wrist and hand splints In studies of resting splints, after one month of wear participants preferred using a splint (low temperature thermoplastic splint or a padded medium temperature thermoplastic splint) to no splint (relative ratio 5.5 [95% CI: 2.1 to 14.5]) (Callinan 1996). There were, however, no differences found in pain, grip strength, Ritchie Index, or number of swollen joints among participants who wore splints for six months versus those who did not (Janssen 1990).
Special shoes and insoles With regard to studies of special shoes and insoles, participants who wore extra‐depth shoes for two months were found to have less pain (100 mm visual analogue pain score [VAS]) when either walking (MD ‐18.70 [95% CI: ‐28.46 to ‐8.94]) or stair climbing (MD ‐27.00 [95% CI: ‐37.83 to ‐16.17]), and more minutes pain free walking time (MD 18.20 [95% CI: 8.22 to 28.18]), compared with those who wore regular footwear. No changes were seen on non‐weight bearing pain, fatigue, or subjective wellness (Fransen 1997). Participants who wore semi‐rigid insoles in extra‐depth shoes over 12 weeks reported better pain scores as measured on 100 mm VAS scale than when they wore extra‐depth shoes alone (MD 1.90 [95% CI: ‐3.27 to ‐0.51]). However, no difference was found in functional evaluations or joint counts. When participants wore soft insoles in extra‐depth shoes there was no difference on any measure compared to when they wore extra‐depth shoes alone. Surprisingly therefore, after having experienced all three combinations, nearly half voiced a preference for the soft insoles, and nearly half preferred the semi‐rigid insoles. Those who chose soft insoles had similar pain with both types of insoles, while participants who preferred semi‐rigid insoles experienced significantly more pain with soft insoles (Chalmers 2000). Finally, after up to three years of wear, individuals who used posted insoles demonstrated less progression of hallux abductus angle (RR 3.6 [95% CI: 2.19 to 5.93) (Budiman‐Mak 1995) but no difference in pain or function (Conrad 1996).
Discussion
Study of the effectiveness of wrist and hand splints in individuals with rheumatoid arthritis is a complex proposition. For example, working wrist splints are recommended in order to limit circumduction and reduce torque during heavy wrist activities (Cordery 1998). Generally patients are instructed to wear the splints during activities they feel are heavy. However, it is recognized that these splints may limit the dexterity required in certain activities, or the splints may become too soiled to be practical (Stern 1997). Therefore, both wearing time and amount and type of stress on the joints may vary widely among study participants, depending on the types of activities which they usually carry out. While efforts to standardize wearing time have been attempted in some studies (e.g. by requesting wearing the splints for at least four hours per day), it has been more difficult to standardize the amount of stress on the joints. It may not be realistic to assume that joint stress will average out in treated and control groups if, for example, the splinted group tends to feel more secure with heavy activities and is therefore exposed to greater joint stress.
Additionally, some of the outcomes measured in studies of working wrist splints were probably included, not because it was felt that treatment would lead to gains in these measures, but rather, to monitor potential adverse effects. Range of motion (ROM), dexterity, and possibly grip strength, fall into this category. No reference to these outcomes as potential adverse effects could be found in splinting textbooks yet clinicians must consider the potential for decreasing ROM and dexterity (potential adverse effects) when recommending the use of working wrist splints. Where these outcomes are actually potential adverse effects, a finding of no difference between treated and control participants could actually reflect a positive overall outcome if the patient was provided with pain relief during at least some of their daily activities.
The difficulty of studying the effectiveness of wrist and hand splints in rheumatoid arthritis is further illustrated with resting wrist and hand splints. These splints are designed to provide pain relief through immobilization of actively inflamed joints. Given the fluctuating course of the disease, it is difficult to know what the length of follow‐up should be when pain relief is only likely to be evident during times of active joint inflammation.
Overall, the quality of the included studies was only fair. Most studies failed to receive higher ratings through failure to use a placebo and/or to document whether evaluators were unaware of the participant's study group. In only one of the studies was a placebo shoe insert, which was not built up to provide support, used (Budiman‐Mak 1995, Conrad 1996). However, it should be noted that it may be difficult, if not impossible, to provide placebos and to blind participants to the treatment allocation in most studies with orthotics. Splints/orthoses provide support for a body part. How can this appear to be done without the patient knowing that no support is being provided? On the other hand, problems related to blinding of evaluators are not difficult to deal with since, in most cases, the splint/orthosis can be removed or otherwise hidden from the evaluator. However, in only five studies was it reported that evaluators were unaware of group allocation (Budiman‐Mak 1995, Chalmers 2000, Conrad 1996, Janssen 1990, Tijhuis 1998). This could certainly be addressed in future studies to improve quality.
Other general problems in the studies reviewed included the analysis of cross‐over trials as parallel trials (leading to potential over‐estimation of results), and small trial size (number less than 100 in all trials, and less than 50 in four). However, given that the treatment results were, for the most part, in the expected direction, it is too early to conclude that the non‐significant results demonstrate the lack of effectiveness of the orthotics examined.
To our knowledge, this is the first critical review of splints/orthoses in the treatment of rheumatoid arthritis. A previous literature review outlined the biomechanical and physiological conceptual basis for splinting the hand in rheumatoid arthritis (Ouellette 1991) but did not provide a critical synthesis of outcome studies.
Authors' conclusions
Implications for practice.
Given the limitations in study designs, it is difficult to make conclusions from the identified studies of wrist and hand splints. It appears, though, that working wrist splints do not have short or long term detrimental effects for grip strength or range of motion (ROM), nor is there any clear indication that they provide pain relief. However, ready‐made elastic wrist gauntlets are relatively inexpensive and, since they may provide pain relief for some patients in some activities, it seems reasonable to try patients with these orthoses until further data becomes available.
The effectiveness of resting hand and wrist splints for night‐time use in reducing pain and swelling was tested in only one study. In another study of patient preference following one month of use, participants were found to prefer wearing the splints to not wearing them. There is not currently enough evidence to make a recommendation for practice.
There is preliminary evidence to support the use of extra‐depth shoes, with or without semi‐rigid insoles, to relieve pain on walking and weight‐bearing. Supported insoles appear to limit progression of hallux valgus angle but do not decrease pain or enhance function.
The potential of orthotics to provide pain relief for varying periods of time in certain patients, and at a relatively low cost, tends to support the current practice of recommending that patients try out various splints/orthoses in different activities in order to determine whether these splints are helpful to them.
Implications for research.
Research in this area is in its infancy. To date, research questions have been poorly articulated and the rationale for the study designs needs to be more explicit. It was noted that a number of studies were excluded due to the fact that they examined compliance rather than effectiveness (Feinberg 1981, Feinberg 1992, Nicholas 1982). This is rather disconcerting given the fact that effectiveness has not been established, and there is, therefore, sound theoretical rationale for avoiding dogmatic application of splints (Melvin 1989).
We strongly recommend immediate study of the most commonly prescribed orthotics (especially resting hand and wrist splints, and splints prescribed to limit joint deformity such as the metacarpal ulnar deviation or MUD splint), with study questions which clearly address effects on pain, function, ROM and deformity. Furthermore, the hypotheses underlying follow‐up time must be clearly articulated. Sample sizes must be large enough to ensure adequate power. Adverse effects must be considered. Placebos should be considered where possible. As well, in most cases it is possible to remove the orthosis prior to follow‐up to ensure blind evaluation. This should be done when possible and reported clearly.
What's new
| Date | Event | Description |
|---|---|---|
| 9 November 2008 | Amended | Converted to new review format. CMSG ID: C077‐R |
Acknowledgements
Many thanks to Maria Judd for providing editorial and technical assistance.
Data and analyses
Comparison 1. Working wrist gauntlet versus no splint (immediate).
1.1. Analysis.

Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 1 Grip strength of dominant hand (mmHg)‐ dorsal working splint vs no splint.
1.2. Analysis.

Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 2 Grip strength of dominant hand (mmHg) ‐ Palmar splint vs no splint.
1.3. Analysis.
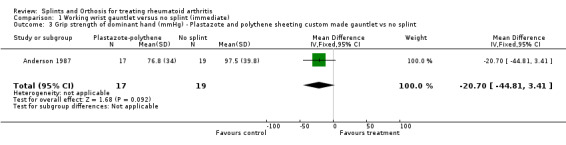
Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 3 Grip strength of dominant hand (mmHg) ‐ Plastazote and polythene sheeting custom made gauntlet vs no splint.
1.4. Analysis.

Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 4 Grip strength of dominant hand (mmHg) ‐ Elastic with metal stay ready made gauntlet vs no splint.
1.5. Analysis.
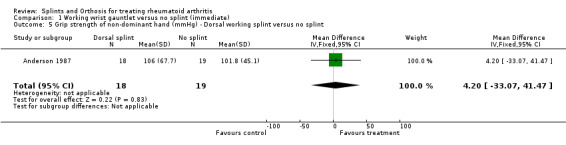
Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 5 Grip strength of non‐dominant hand (mmHg) ‐ Dorsal working splint versus no splint.
1.6. Analysis.

Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 6 Grip strength of non‐dominant hand (mmHg) ‐ Palmar splint versus no splint.
1.7. Analysis.
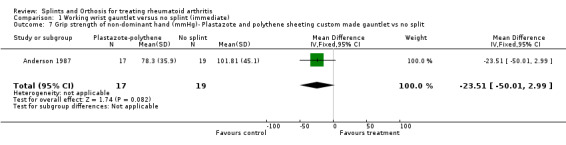
Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 7 Grip strength of non‐dominant hand (mmHg)‐ Plastazote and polythene sheeting custom made gauntlet vs no split.
1.8. Analysis.
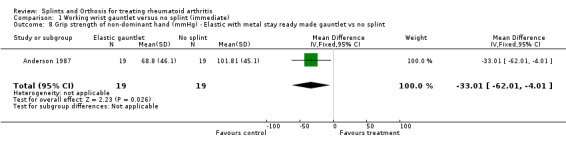
Comparison 1 Working wrist gauntlet versus no splint (immediate), Outcome 8 Grip strength of non‐dominant hand (mmHg) ‐ Elastic with metal stay ready made gauntlet vs no splint.
Comparison 2. Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Work performance output in 10 sec. using screwdriver (engals) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐213.0 [‐445.31, 19.31] |
| 2 Work performance output in 10 sec. using shears (engals) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 49.0 [‐214.18, 312.18] |
| 3 Dexterity (VAS 0 to 10) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 4.40 [‐3.97, 12.77] |
| 4 Pain on using screwdriver (VAS) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐0.45 [‐1.40, 0.50] |
| 5 Pain on using shears (VAS) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐0.52 [‐1.48, 0.44] |
2.1. Analysis.

Comparison 2 Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear), Outcome 1 Work performance output in 10 sec. using screwdriver (engals).
2.2. Analysis.
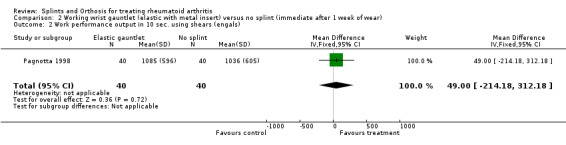
Comparison 2 Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear), Outcome 2 Work performance output in 10 sec. using shears (engals).
2.3. Analysis.

Comparison 2 Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear), Outcome 3 Dexterity (VAS 0 to 10).
2.4. Analysis.
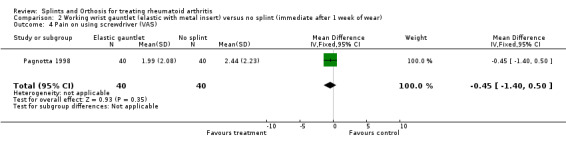
Comparison 2 Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear), Outcome 4 Pain on using screwdriver (VAS).
2.5. Analysis.

Comparison 2 Working wrist gauntlet (elastic with metal insert) versus no splint (immediate after 1 week of wear), Outcome 5 Pain on using shears (VAS).
Comparison 3. Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain on motion (VAS:1‐100mm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐7.5 [‐20.93, 5.93] |
| 2 Pain at rest (VAS:1‐100mm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐1.73, 1.23] |
| 3 Activity pain (pouring water)(VAS:1‐100mm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.06, 1.06] |
| 4 Wrist pain on motion (VAS:1‐100mm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐7.00 [‐21.20, 7.20] |
| 5 Grip strength (mmHg) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐4.0 [‐24.04, 16.04] |
| 6 Morning stiffness (min.) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐41.88, 41.88] |
| 7 Active dorsal and volar joint motion (degrees) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 7.5 [‐4.80, 19.80] |
| 8 Passive dorsal and volar joint motion (degrees) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 12.5 [0.55, 24.45] |
| 9 Active ulnar and radial joint motion (degrees) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐7.23, 7.23] |
| 10 Active pronation and supination (degrees) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐30.35, 20.35] |
| 11 Pinch grip (mmHg) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐1.0 [‐25.12, 23.12] |
| 12 Joint circumference (cm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.42, 0.52] |
| 13 Forearm circumference (cm) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | 0.2 [‐0.23, 0.63] |
| 14 HAQ (score 0‐3) | 1 | 55 | Mean Difference (IV, Fixed, 95% CI) | ‐0.25 [‐0.52, 0.02] |
3.1. Analysis.
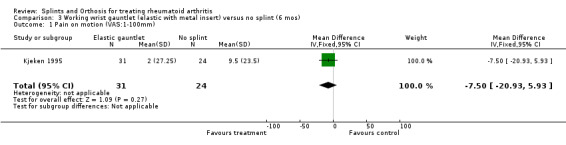
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 1 Pain on motion (VAS:1‐100mm).
3.2. Analysis.
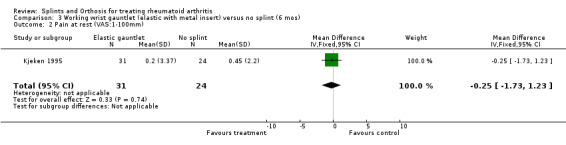
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 2 Pain at rest (VAS:1‐100mm).
3.3. Analysis.
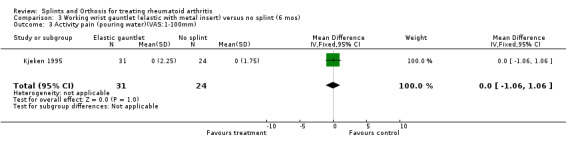
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 3 Activity pain (pouring water)(VAS:1‐100mm).
3.4. Analysis.
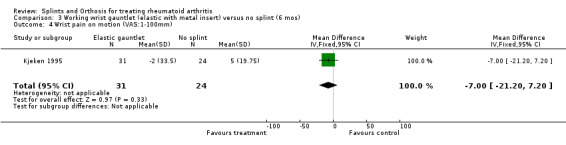
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 4 Wrist pain on motion (VAS:1‐100mm).
3.5. Analysis.
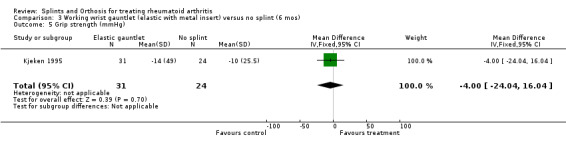
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 5 Grip strength (mmHg).
3.6. Analysis.
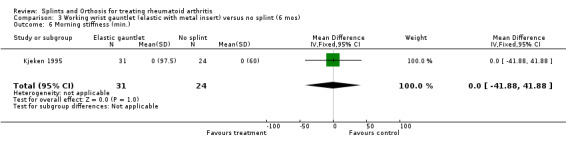
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 6 Morning stiffness (min.).
3.7. Analysis.
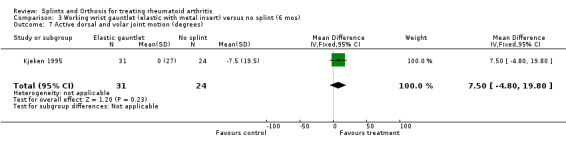
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 7 Active dorsal and volar joint motion (degrees).
3.8. Analysis.
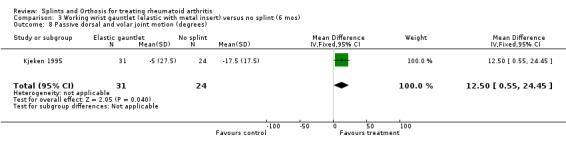
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 8 Passive dorsal and volar joint motion (degrees).
3.9. Analysis.

Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 9 Active ulnar and radial joint motion (degrees).
3.10. Analysis.
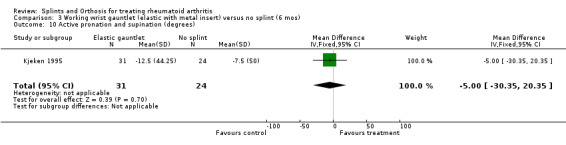
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 10 Active pronation and supination (degrees).
3.11. Analysis.
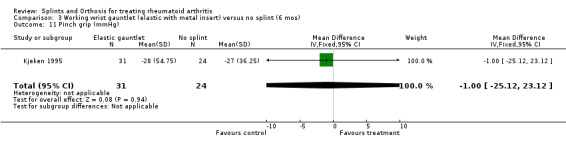
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 11 Pinch grip (mmHg).
3.12. Analysis.
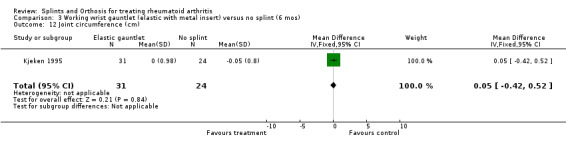
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 12 Joint circumference (cm).
3.13. Analysis.
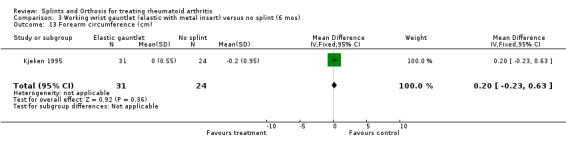
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 13 Forearm circumference (cm).
3.14. Analysis.
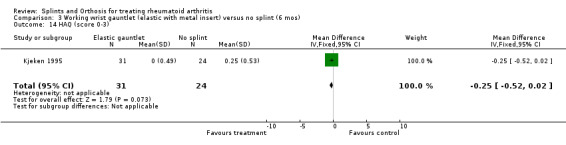
Comparison 3 Working wrist gauntlet (elastic with metal insert) versus no splint (6 mos), Outcome 14 HAQ (score 0‐3).
Comparison 4. Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain in wrist (VAS:1‐10cm) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐0.97, 2.97] |
| 2 Tender joint count wrist and hand (Ritchie scale) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐3.77, 2.57] |
| 3 Number of swollen joints | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 1.50 [‐1.30, 4.30] |
| 4 Total passive wrist ROM (degrees) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐18.0 [‐91.77, 55.77] |
| 5 Grip strength (kPa) with orthosis | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐10.93, 18.93] |
| 6 Grip strength (kPa) without orthosis | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐18.35, 12.35] |
4.1. Analysis.

Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 1 Pain in wrist (VAS:1‐10cm).
4.2. Analysis.
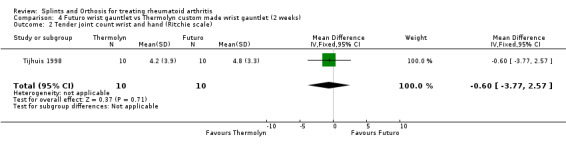
Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 2 Tender joint count wrist and hand (Ritchie scale).
4.3. Analysis.
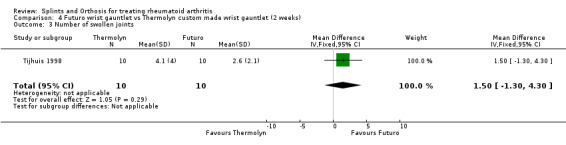
Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 3 Number of swollen joints.
4.4. Analysis.
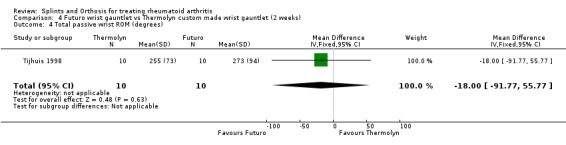
Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 4 Total passive wrist ROM (degrees).
4.5. Analysis.

Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 5 Grip strength (kPa) with orthosis.
4.6. Analysis.
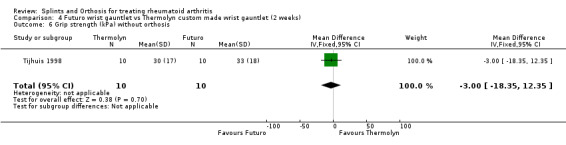
Comparison 4 Futuro wrist gauntlet vs Thermolyn custom made wrist gauntlet (2 weeks), Outcome 6 Grip strength (kPa) without orthosis.
Comparison 5. Futuro wrist gauntlet vs Alimed wrist gauntlet (immediately after 1 week of wear).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unilateral dexterity (splint on) (Purdue Pegboard placing) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐1.21, 1.09] |
| 2 Bilateral dexterity (splint on) (Purdue Pegboad assembly) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐4.22, 4.14] |
| 3 Grip strength (splint off) (kg) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | 0.42 [‐4.10, 4.94] |
5.1. Analysis.

Comparison 5 Futuro wrist gauntlet vs Alimed wrist gauntlet (immediately after 1 week of wear), Outcome 1 Unilateral dexterity (splint on) (Purdue Pegboard placing).
5.2. Analysis.

Comparison 5 Futuro wrist gauntlet vs Alimed wrist gauntlet (immediately after 1 week of wear), Outcome 2 Bilateral dexterity (splint on) (Purdue Pegboad assembly).
5.3. Analysis.
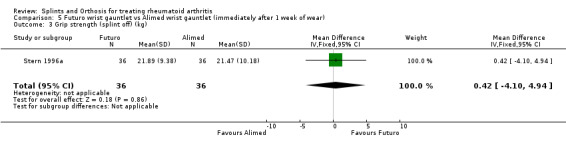
Comparison 5 Futuro wrist gauntlet vs Alimed wrist gauntlet (immediately after 1 week of wear), Outcome 3 Grip strength (splint off) (kg).
Comparison 6. Alimed wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unilateral dexterity (splint on) (Purdue Pegboard placing) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐1.45, 0.83] |
| 2 Bilateral dexterity (splint on) (Purdue Pegboard placing) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐4.35, 4.21] |
| 3 Grip strength (splint off) (kg) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | ‐0.56 [‐5.18, 4.06] |
6.1. Analysis.
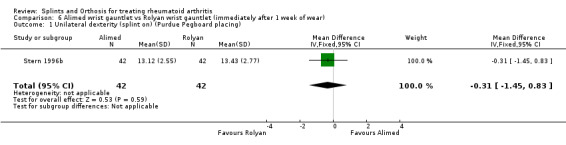
Comparison 6 Alimed wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 1 Unilateral dexterity (splint on) (Purdue Pegboard placing).
6.2. Analysis.

Comparison 6 Alimed wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 2 Bilateral dexterity (splint on) (Purdue Pegboard placing).
6.3. Analysis.

Comparison 6 Alimed wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 3 Grip strength (splint off) (kg).
Comparison 7. Futuro wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Unilateral dexterity (splint on) (Purdue Pegboard placing) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐1.56, 0.82] |
| 2 Bilateral dexterity (splint on) (Purdue Pegboard assembly) | 1 | 84 | Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐4.28, 4.06] |
| 3 Grip strength (splint off) (kg) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐4.57, 4.29] |
7.1. Analysis.

Comparison 7 Futuro wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 1 Unilateral dexterity (splint on) (Purdue Pegboard placing).
7.2. Analysis.
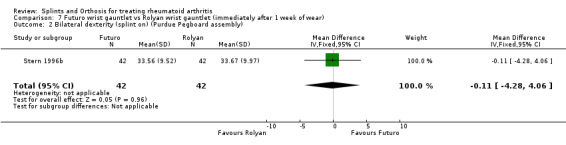
Comparison 7 Futuro wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 2 Bilateral dexterity (splint on) (Purdue Pegboard assembly).
7.3. Analysis.
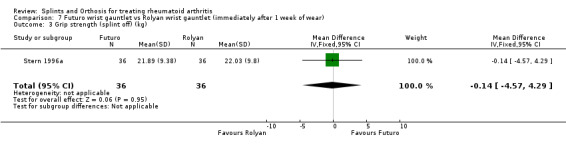
Comparison 7 Futuro wrist gauntlet vs Rolyan wrist gauntlet (immediately after 1 week of wear), Outcome 3 Grip strength (splint off) (kg).
Comparison 8. Resting hand and wrist splint vs no splint (1‐6 months).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preference (1 month) (# of patients prefering soft or hard splint vs no splint) | 1 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.5 [2.09, 14.49] |
| 2 Grip strength (6 months) | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 1.74 [‐6.36, 9.83] |
| 2.1 Grip strength ‐ right (mmHg) (6 months) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | 3.0 [‐7.64, 13.64] |
| 2.2 Grip strength left (mmHg) (6 months) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐12.47, 12.47] |
| 3 Number of swollen joints (6 months) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐3.2 [‐7.50, 1.10] |
| 4 Ritchie Index (6 months) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐3.26, 2.86] |
| 5 Pain score (out of 48) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
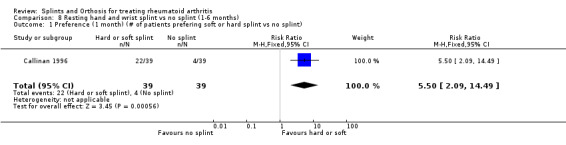
Comparison 8 Resting hand and wrist splint vs no splint (1‐6 months), Outcome 1 Preference (1 month) (# of patients prefering soft or hard splint vs no splint).
8.2. Analysis.

Comparison 8 Resting hand and wrist splint vs no splint (1‐6 months), Outcome 2 Grip strength (6 months).
8.3. Analysis.
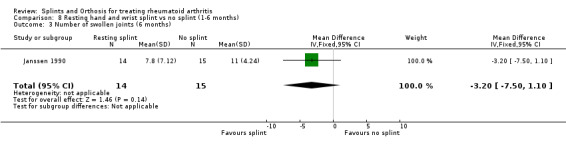
Comparison 8 Resting hand and wrist splint vs no splint (1‐6 months), Outcome 3 Number of swollen joints (6 months).
8.4. Analysis.

Comparison 8 Resting hand and wrist splint vs no splint (1‐6 months), Outcome 4 Ritchie Index (6 months).
8.5. Analysis.

Comparison 8 Resting hand and wrist splint vs no splint (1‐6 months), Outcome 5 Pain score (out of 48).
Comparison 9. Circumferential cotton‐padded splint wrap versus pan‐type hard thermoplastic splint (1 month).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Preference (# of patients prefering the soft splint vs the hard splint) | 1 | 78 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [1.00, 2.85] |
9.1. Analysis.
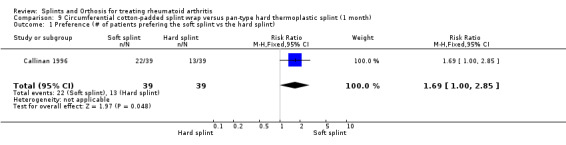
Comparison 9 Circumferential cotton‐padded splint wrap versus pan‐type hard thermoplastic splint (1 month), Outcome 1 Preference (# of patients prefering the soft splint vs the hard splint).
Comparison 10. Extra‐depth shoes versus regular footwear (2 months).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 change on Stanford Health Assessment Questionnaire (HAQ) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.2 [‐0.35, ‐0.05] |
| 2 change on Pain on walking (VAS) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐18.7 [‐28.46, ‐8.94] |
| 3 change on Pain on stair climibing (VAS) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐27.0 [‐37.83, ‐16.17] |
| 4 change on Pain on non‐weight bearing (VAS) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐15.04, 5.04] |
| 5 change in Fatigue (VAS) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐14.8 [‐31.40, 1.80] |
| 6 change in Subjective well‐being (VAS) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐12.5 [‐27.25, 2.25] |
| 7 change in Pain free walking time (minutes) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 18.2 [8.22, 28.18] |
10.1. Analysis.
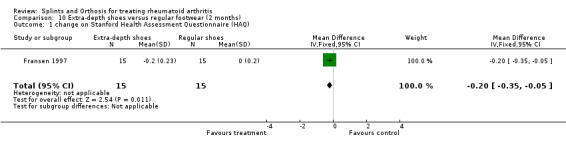
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 1 change on Stanford Health Assessment Questionnaire (HAQ).
10.2. Analysis.
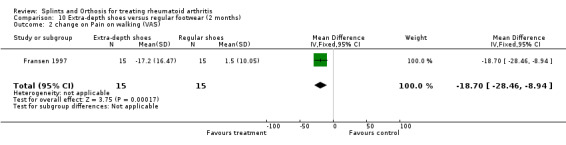
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 2 change on Pain on walking (VAS).
10.3. Analysis.

Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 3 change on Pain on stair climibing (VAS).
10.4. Analysis.
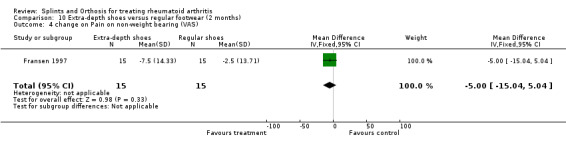
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 4 change on Pain on non‐weight bearing (VAS).
10.5. Analysis.
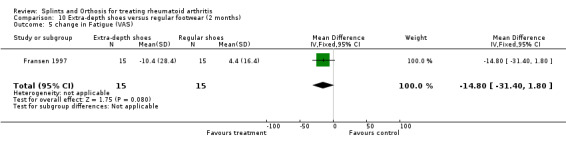
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 5 change in Fatigue (VAS).
10.6. Analysis.
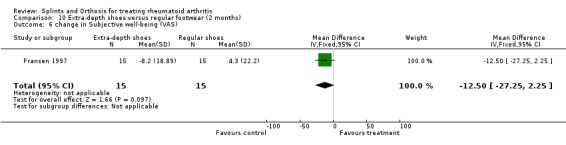
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 6 change in Subjective well‐being (VAS).
10.7. Analysis.
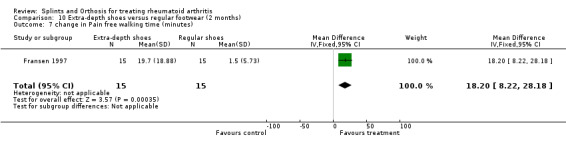
Comparison 10 Extra‐depth shoes versus regular footwear (2 months), Outcome 7 change in Pain free walking time (minutes).
Comparison 11. Semi‐rigid insoles vs extra‐depth shoes (12 weeks).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain (VAS: 1‐10cm) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐1.9 [‐3.29, ‐0.51] |
| 2 RB Walking (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐2.0 [‐13.61, 9.61] |
| 3 RB Stairs (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐5.51, 7.11] |
| 4 RB Stand (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐9.30 [‐62.35, 43.75] |
| 5 Toronto Activities of Daily Living measure (TADL) walking | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.62, 0.62] |
| 6 TADL stairs | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.12, 0.12] |
| 7 50' walking (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐2.15, 2.55] |
| 8 Lower extremity joint count (# of painful joints) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐4.89, 4.49] |
| 9 MTP joint count (# of painful joints) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.67, 1.67] |
11.1. Analysis.
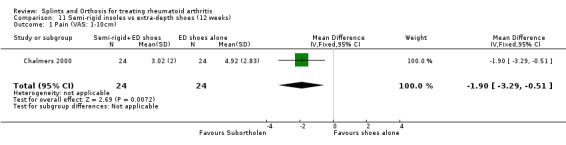
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 1 Pain (VAS: 1‐10cm).
11.2. Analysis.
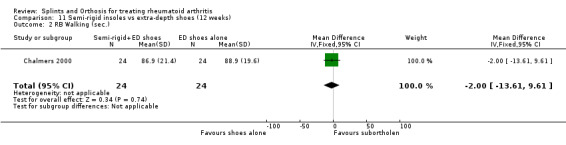
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 2 RB Walking (sec.).
11.3. Analysis.

Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 3 RB Stairs (sec.).
11.4. Analysis.
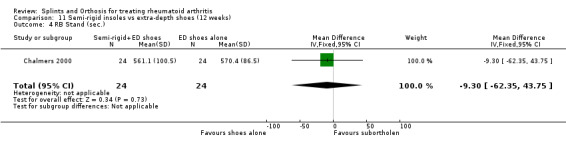
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 4 RB Stand (sec.).
11.5. Analysis.
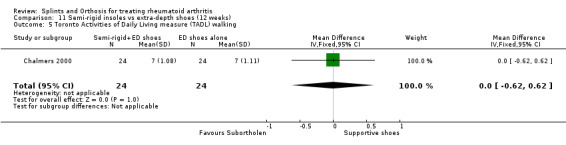
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 5 Toronto Activities of Daily Living measure (TADL) walking.
11.6. Analysis.

Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 6 TADL stairs.
11.7. Analysis.
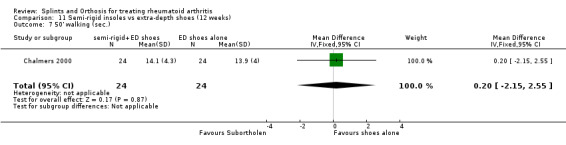
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 7 50' walking (sec.).
11.8. Analysis.
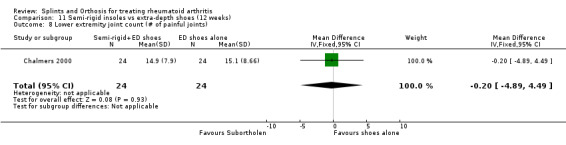
Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 8 Lower extremity joint count (# of painful joints).
11.9. Analysis.

Comparison 11 Semi‐rigid insoles vs extra‐depth shoes (12 weeks), Outcome 9 MTP joint count (# of painful joints).
Comparison 12. Soft insoles versus extra‐depth shoes (plastazote) (12 weeks).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain (VAS: 1‐10 cm) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.92 [‐2.39, 0.55] |
| 2 RB Walking (sec) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 2.5 [‐8.67, 13.67] |
| 3 RB Stairs (sec) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [‐5.78, 7.18] |
| 4 RB Stand (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 13.60 [‐49.24, 76.44] |
| 5 Toronto Activities of Daily Living measure (TADL) walking | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.54, 0.74] |
| 6 TADL stairs | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.12, 0.12] |
| 7 50' walking (sec.) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐2.29, 2.29] |
| 8 Lower extremity joint count (# of painful joints) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐2.40 [‐7.31, 2.51] |
| 9 MTP joint count (# of painful joints) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.90, 1.50] |
12.1. Analysis.

Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 1 Pain (VAS: 1‐10 cm).
12.2. Analysis.
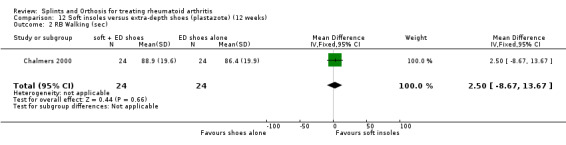
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 2 RB Walking (sec).
12.3. Analysis.
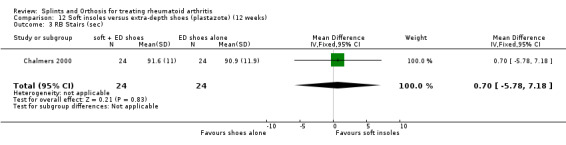
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 3 RB Stairs (sec).
12.4. Analysis.
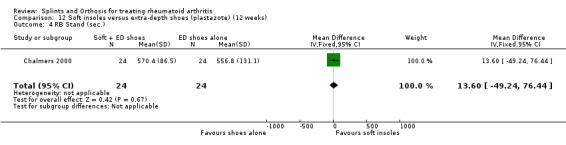
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 4 RB Stand (sec.).
12.5. Analysis.
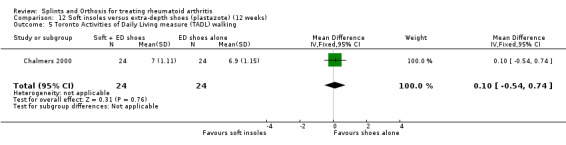
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 5 Toronto Activities of Daily Living measure (TADL) walking.
12.6. Analysis.
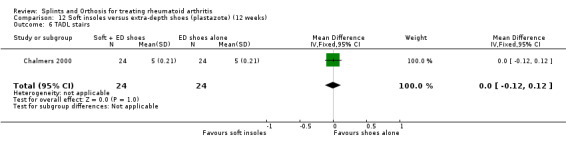
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 6 TADL stairs.
12.7. Analysis.
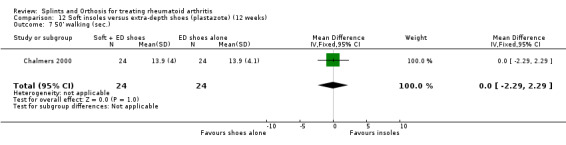
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 7 50' walking (sec.).
12.8. Analysis.
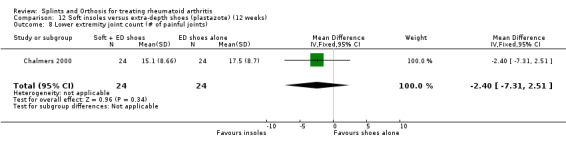
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 8 Lower extremity joint count (# of painful joints).
12.9. Analysis.
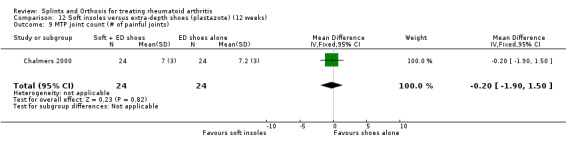
Comparison 12 Soft insoles versus extra‐depth shoes (plastazote) (12 weeks), Outcome 9 MTP joint count (# of painful joints).
Comparison 13. Rohadur posted foot orthosis vs placebo insole (End of therapy ‐ 3 yrs).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hallux abductus angle remained < 21 degrees | 1 | 98 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.60 [2.19, 5.93] |
| 2 Painful foot joint count | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.55, 0.95] |
| 3 Foot Function Index | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐10.29, 7.49] |
| 4 Foot pain (adapted from Melzack) | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐2.18, 2.58] |
13.1. Analysis.

Comparison 13 Rohadur posted foot orthosis vs placebo insole (End of therapy ‐ 3 yrs), Outcome 1 Hallux abductus angle remained < 21 degrees.
13.2. Analysis.
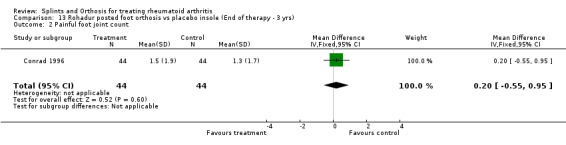
Comparison 13 Rohadur posted foot orthosis vs placebo insole (End of therapy ‐ 3 yrs), Outcome 2 Painful foot joint count.
13.3. Analysis.

Comparison 13 Rohadur posted foot orthosis vs placebo insole (End of therapy ‐ 3 yrs), Outcome 3 Foot Function Index.
13.4. Analysis.
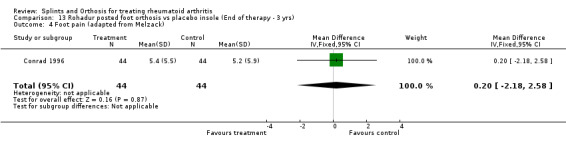
Comparison 13 Rohadur posted foot orthosis vs placebo insole (End of therapy ‐ 3 yrs), Outcome 4 Foot pain (adapted from Melzack).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anderson 1987.
| Methods | Randomized, single intervention study. Sample size at entry: 92 | |
| Participants | RA Female Mean Age Group 1: 51.3 SD: 16.7 Group 2: 51.1 SD: 15.8 Group 3: 56.9 SD: 12.5 Group 4: 55.7 SD: 13.0 Group 5: 57.3 SD: 10.4 | |
| Interventions | Wrist Orthoses 1‐Dorsal Working Splint 2‐Palmar Working Splint 3‐Gauntlet Working Splint 4‐Elastic Ready‐Made Splint 5‐No splint (control group) | |
| Outcomes | 1‐Hand grip strength (mmHg) immediately after donning splint | |
| Notes | R=randomization B=blinding W=withdrawals R=2 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Budiman‐Mak 1995.
| Methods | Randomized, Parallel Group, Placebo controlled, Double‐blind,Sample size at entry: 102 | |
| Participants | Diagnosis of RA, functional class I and II, subjects were between 18 and 75 yrs of age, had foot pain, had radiologic changes of stage I and II in one or both feet, had active disease defined either as 6 or more joints that were painful on palpation and tender on motion or had 3 or more swollen joints with greater or equal to 45 min. of joint stiffness in the morning. Treatment Mean age: 60.2 yrs, Control Mean age: 58.8 yrs, Disease duration for treatment group: 9.8 yrs, and for control group: 6.1 yrs | |
| Interventions | Foot orthoses: 1‐Functional posted foot by Rohadur 2‐Placebo orthosis (thin flexible leather shell molded over a plaster impression of the patient's foot, covered with thin naugahyde of the same color and design as the thermoplastic functional posted foot orthosis) | |
| Outcomes | 1‐ Progression of hallux abductus angle by treatment status | |
| Notes | R=2 B=2 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Callinan 1996.
| Methods | Randomized, Crossover Study, Sample size at entry: 45 (one group over time) | |
| Participants | Diagnosis of RA, presence of hand pain, morning stiffness or both. Mean age: 51 yrs Mean Disease Duration: 14.5 yrs. 36 Females and 3 Males | |
| Interventions | Hand‐Wrist Extension Splints: 1‐ Hard Splint: circumferential 2‐Conventional resting mitt‐type Soft Splint | |
| Outcomes | 1‐ Compliance 2‐ Preference | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chalmers 2000.
| Methods | Crossover Study, Sample size at entry : 28 (they received in random order 3 interventions for 12 wks trials, separated by 2 wks washout). | |
| Participants | Diagnosis of RA, minimum 2 subluxed MTP joints bilaterally and MTP joint pain as most significant foot problem. Mean age for men : 63 yrs, for women : 60 yrs. Mean disease duration: 15 yrs | |
| Interventions | Foot/Ankle orthoses: 1‐ Subortholen 2‐ Plastazote 3‐ Extra‐Depth shoes | |
| Outcomes | 1‐ RB*walking 2‐ RB stairs 3‐ RB stand 4‐ TADL** walking 5‐ TADL stairs 6‐ TADL sub walk 7‐ 50' walking 8‐ Lower extremity joint count 9‐ MTP joint count 10‐Pain (VAS) *RB= Robinson Bashall Functional Assessment ** TADL= Toronto Activities of Daily Living Measure | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Conrad 1996.
| Methods | Randomized, Parallel group, Sample size at entry for experimental group:52, Control group:50. NB: This is the same study as Budiman‐Mak | |
| Participants | Patients aged between 18 and 75yrs old, foot pain, definite RA, functional class I or II, radiological changes of stage I or II in one or both feet, 6 or more painful joints or 3 or more swollen joints, or sedimentation of 28mm or more per hour, flexible functional discrepancies in their feet, measured as calcaneal valgus stance positions that could be controlled by a functional foot orthosis, minimum ROM in feet and ankle making ambulation position. Disease duration: longer than 2 yrs. | |
| Interventions | Foot/Ankle orthosis: 1‐Functional posted foot orthosis 2‐Placebo orthosis (thin naugahyde shoe insert) | |
| Outcomes | 1‐Painful foot joint count 2‐Total painful joint count 3‐Foot pain 4‐FFI pain scale 5‐Disability scale 6‐Activity limitation scale 7‐Total score(FFI) 8‐Total disability (AIMS) | |
| Notes | R=1 B=2 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Feinberg 1981.
| Methods | Single intervention study. Sample size at entry: 50 | |
| Participants | Patients with RA that have never been splinted with resting splints prior to study. | |
| Interventions | Wrist/Hand splint: Group 1: compliant group that wore the splint more than 50% of the prescribed time Group 2: Non‐compliant group that wore the splint less than 50% of the prescribed time. | |
| Outcomes | 1‐Pain severity and changes (wrist/hand) 2‐ROM and changes 3‐Duration of morning stiffness and changes | |
| Notes | R=0 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Feinberg 1992.
| Methods | Randomized, Sample size at entry for experimental group: 22, Control group: 24 | |
| Participants | Subjects with RA, Functional class I or II, Control group mean age: 48.84yrs, Experimental group mean age: 48.84yrs, Control group mean disease duration: 4.44yrs, Experimental group mean disease duration: 4.64yrs | |
| Interventions | Experimental group: Patient education (learning principles and assessment of the patient's expectations about the clinical encounter) plus hand resting splint wear. Control group: hand resting splint | |
| Outcomes | 1‐Wrist and hand pain severity 2‐Duration of morning stiffness 3‐Days of splint use 4‐Days of splinting use during the 1st 28 days | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Fransen 1997.
| Methods | Randomized, Sample size at entry for the experimental group: 15, Control group: 15 | |
| Participants | Diagnosis of RA, foot pain of at least 1 year duration and stabilization of arthritis medications | |
| Interventions | Experimental group: Extra‐Depth shoes Control group: normal shoes | |
| Outcomes | 1‐ Walk pain (VAS) 2‐ Stair pain (VAS) 3‐ NWB pain (VAS) 4‐ Fatigue 5‐ Well‐being 6‐ Walk‐time 7‐ HAQ* score * Health Assessment Questionnaire | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Janssen 1990.
| Methods | Randomized, parrallel group study. Sample size at entry: 29 | |
| Participants | RA (at least 4 swollen wrist or finger joints and not more htan 3 redressable deformities) | |
| Interventions | Treatment group: Resting splints a=on alternate hands every night for 1 yr. | |
| Outcomes | 1‐ No. of swollen joints 2‐ Ritchie Index 3‐ Pain score 4‐ Grip strength (kPa) | |
| Notes | R=1 B=0 W=0 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kjeken 1995.
| Methods | Randomized, Parallel group, Sample size at entry for Treatment group: 36, Control group: 33. | |
| Participants | Adults with either RA or persistent seronegative arthritides, a diagnosis of inflammatory arthritis disease with at least 2 of the following signs: sweeling, pain on motion, and limited motion, Involvement of the dominant wrist joint. Orthoses group mean age: 62 yrs, Control group mean age: 66yrs. | |
| Interventions | Wrist orthoses: 1‐ Treatment group:Rehband elastic wrist orthosis (10‐15 degrees of dorsiflexion) 2‐Control group: no splint wear. | |
| Outcomes | 1‐Morning stiffness 2‐Pain at rest (wrist) 3‐Pain on motion 4‐Wrist pain on motion 5‐Active dorsal and volar joint motion 6‐Passive dorsal and volar joint motion 7‐Active ulnar and radial joint motion 8‐Active pronation and supination 9‐Pinch grip 10‐Grip strength 11‐Activity pain (cutting cheese) 12‐Activity pain (pouring water) 13‐Joint circumference 14‐Forearm circumference 15‐HAQ score | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Nordenskiöld 1990.
| Methods | Randomized, Parallel Group, Sample size at entry: 104 | |
| Participants | Treatment Group: Diagnosis of RA, Functional classes 2 and 3, Treatment group mean age: 53 yrs, Control group mean age: 40 yrs. | |
| Interventions | Soft Volar Wrist Orthoses (neutral position) 1‐Camp Splint with larger thumb opening 2‐Rehband Splint with more material on the dorsal side | |
| Outcomes | 1‐Mean Grip Strength of R and L hands 2‐Average pain experienced durind ADL with and without wrist orthosis | |
| Notes | R=1 B=0 W=0 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Pagnotta 1998.
| Methods | Crossover study, sample at entry: 110 | |
| Participants | Diagnosis of RA, splinting of the dominant hand indicated by pain either at rest or on exertion. Chronic pain. Total mean age: 52.4, SD: 13.9yrs, range: 25‐81yrs. Disease duration: 9.2yrs, SD: 12.3yrs. | |
| Interventions | Commercial working wrist splint (Futuro Kendall #33) | |
| Outcomes | Work performance out put in 10 sec.:
1‐Shears
2‐Screwdriver
3‐Dexterity Pain: 1‐Shears 2‐Srewdriver |
|
| Notes | R=0 B=0 W=0 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Rennie 1996.
| Methods | One group over time, Sample size at entry: 26 subjects (27 hands) | |
| Participants | Diagnosis of RA, Mean age: 64 yrs | |
| Interventions | Ulnar Deviation Finger orthosis (MCP) | |
| Outcomes | Ulnar Drift Angle (degrees) | |
| Notes | R=0 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Stern 1996a.
| Methods | One over time, Crossover study, sample size at entry : 36 | |
| Participants | Definite RA, functional class 2 or 3, dominant wrist active extension of equal or greater than 20 degrees, Group mean age: 56.5, SD:13.6. | |
| Interventions | Wrist orthoses: 1‐Kendall‐Futuro #33 2‐Alimed Freedom Long 3‐Rolyan D‐Ring | |
| Outcomes | 1‐Grip strength (kg) | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stern 1996b.
| Methods | Block‐ randomized, Crossover Study, Sample size at entry: 42 (one group over time) | |
| Participants | Subjects falling within functional class 2 or 3 and demonstrated active wrist extension greater or equal to 20 degrees and reported wrist involvement (pain at rest, pain during function or wrist instability) of the dominant hand, Mean Age: 56,50 yrs, Mean of Disease Duration: 11.05 yrs, 20 males and 22 females. | |
| Interventions | Wrist orthoses : 1‐ Futuro 33 2‐ Rolyan D‐Ring 3‐ Alimed Freedom Long Frequency of splint wearing: used intermittently during functional tasks for a minimum of 4 hrs/day accross 5 of the 7 days of wear (1 wk wash‐out between orthoses). | |
| Outcomes | 1‐ Placing (# of pins placed) 2‐ Assembly (# of pieces assembled) 3‐ Writing (sec.) 4‐ Writing (log) 5‐ Card turning (sec.) 6‐ Pick up small objects (sec.) 7‐ Feeding (sec.) 8‐ Checkers (sec.) 9‐ Empty cans (sec.) 10‐ One pound cans (sec.) (For Purdue Pegboard and Jebson‐Taylor Tests) | |
| Notes | R=1 B=0 W=1 (all subjects completed the study) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stern 1997.
| Methods | Randomized study. Sample size at entry:42 (one group over time) | |
| Participants | RA (functional class 1 or 2, active wrist extension greater than 20 degrees, wrist involvement of the dominant hand ‐pain at rest, pain during function or wrist instability) Total sample mean: 11.05 yrs, SD: 11.03 Total sample mean: 56.50 yrs SD: 13.60 yrs | |
| Interventions | Wrist Orthoses: 1‐Futuro (gauntlet: dorsal opening) 2‐Alimed (gauntlet: dorsal‐radial opening) 3‐Rolyan (gauntlet: dorsal opening) | |
| Outcomes | 1‐Increase in hand or wrist strength | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Swigart 1999.
| Methods | Single Interventions, Sample size at entry: 114 | |
| Participants | Diagnosis of RA, Total sample mean age: 53.8 yrs | |
| Interventions | Thumb splint: Long Opponens Splint Holding the thumb in abd. Comparison is made between differant stages of the disease as well as subjects that underwent surgery or not. | |
| Outcomes | 1‐Symptom Improvement | |
| Notes | R=0 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Tijhuis 1998.
| Methods | Randomized crossover study, Sample size at entry: Futuro group: 5 Thermolyn group: 5 (they both tried the two types of splints) | |
| Participants | Patients with RA and a swollen and a painful wrist of the dominant hand Gender: 2 men, 8 women, Mean age: 47.3 yrs, range: 28‐71. Disease Duration: 6.4 yrs, range: 1‐15 | |
| Interventions | Futuro and Thermolyn Splints worn for two weeks each with a one week wash‐out period between splints. | |
| Outcomes | 1‐Pain in Wrist (VAS) 2‐Tender joint count in wrist 3‐Swelling of wrist 4‐Wrist ROM (degrees) 5‐Grip Strength with orthosis (kPa) 6‐Grip strength without orthosis (kPa) | |
| Notes | R=1 B=0 W=1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Backman 1988 | Only 3 subjects were used for the study |
| Bennett 1965 | Not a clinical trial |
| Convery 1967 | No numerical data |
| Craxford 1982 | This article makes a comparison between Conservative and Surgical Methods, and we decided to exclude surgery data from this research. |
| Gruen H | Not a clinical trial |
| Gumpel 1981 | No results data available. Study was not completed. |
| Kim 1995 | The proportion of OA patients is greater than the RA patients. |
| Kock 1980 | Not a clinical trial |
| McKnight 1982 | No SD available. Only changes between hands reported with no raw data values for baseline period. Therefore, we are unable to calculate absolute value at end of treatment. |
| McKnight 1992 | Patients were wearing two types of gloves at the same time on both hands. There was no control period. |
| Moncur 1990 | No control group and only subjective data |
| Nicholas 1982 | There are no times intervals available and no mention of the type of splint patients were wearing. |
| Ouellette 1991 | Literature review |
| Palchik 1990 | No data is available concerning the significance (p value), and there is no mention of what statistical tests they have done. |
| Souter 1971 | Not a clinical trial |
| Stern 1994 | The subjects used in this study were healthy women with a mean age of 26.26 yrs. Rheumatoid arthritis was never mentioned in this article. |
Contributions of authors
ME and LXXB were responsible for writing the manuscript, extracting and analyzing the data, selecting trials, quality assessment of trials JM devised the search strategies MF, MAO and SR helped with study selection, data extraction and quality assessment GW and PT contributed methological expertise
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Anderson 1987 {published data only}
- Anderson K, Maas F. Immediate effect of working splints on grip strength of arthritic patients. Australian Occupational Therapy Journal 1987;34(1):26‐31. [1‐SO] [Google Scholar]
Budiman‐Mak 1995 {published data only}
- Budiman‐Mak E, Conrad KJ, Roach KE, Moore JW, Lertratanakkul Y, Koch AE, Skosey JL, Froelich C, Joyce‐Clark N. Can Foot Orthoses Prevent Hallux Valgus Deformity in Rheumatoid Arthritis ? A Randomized Clinical Trial. Journal of Clinical Rheumatology 1995;1(6):313‐321. [17‐SO] [DOI] [PubMed] [Google Scholar]
Callinan 1996 {published data only}
- Callinan NJ, Mathiowetz V. Soft Versus Hard Resting Hand Splints in RA: Pain Relief, Preference, and Compliance. The American Journal of Occupational Therapy 1996;50(5):347‐353. [3‐SO] [DOI] [PubMed] [Google Scholar]
Chalmers 2000 {published data only}
- Chalmers AC, Busby C, Goyert J, Porter B, Schulzer M. Metatarsalgia and RA‐ A Randomized, Single Blind, Sequential Trial Comparing two Types of Foot Orthoses and Supportive Shoes. The Journal of Rheumatology 2000;27(7):1643‐1647. [13‐SO] [PubMed] [Google Scholar]
Conrad 1996 {published data only}
- Conrad KJ, Budiman‐Mak E, Roach KE, Hedeker D. Impacts of foot orthoses on pain and disability in rheumatoid arthritis. Journal of Clinical Epidemiology 1996;49(1):1‐7. [4‐SO] [DOI] [PubMed] [Google Scholar]
Feinberg 1981 {published data only}
- Feinberg J, Brandt KD. Use of Resting Splints by Patients with Rheumatoid Arthritis. The American Journal of Occupational Therapy 1981;35(3):173‐78. [6‐SO] [DOI] [PubMed] [Google Scholar]
Feinberg 1992 {published data only}
- Feinberg J. Effect of the Arthritis Health Professional on Compliance with Use of Resting Hand Splints by Patients with Rheumatoid Arthritis. Arthritis Care and Research 1992;5(1):17‐23. [5‐SO] [DOI] [PubMed] [Google Scholar]
Fransen 1997 {published data only}
- Fransen M, Edmonds J. Off‐the‐Shelf Orthopedic Footwear for People with RA. Arthritis Care and Research 1997;10(4):250‐6. [14‐SO] [DOI] [PubMed] [Google Scholar]
Janssen 1990 {published data only}
- Janssen M, Phiferons JPWM, Velde EA. The Prevention of Hand Deformities with Resting Splints in Rheumatoid Arthritis Patients. A randomized Single Blind One Year Follow‐Up Study. Arthritis and Rheumatism 1990;33:123. [SO‐28] [Google Scholar]
Kjeken 1995 {published data only}
- Kjeken I, Moller G, Kvien TK. Use of Commercially Produced Elastic Wrist Orthoses in Chronic Arthritis: A Controlled Study. Arthritis Care and Research 1995;8(3):108‐13. [8‐SO] [DOI] [PubMed] [Google Scholar]
Nordenskiöld 1990 {published data only}
- Nordenskiöld U. Reduction of Pain and Increase in Grip Force for Women with Rheumatoid Arthritis. Arthritis Care and Research 1990;3(3):158‐62. [21‐SO] [PubMed] [Google Scholar]
Pagnotta 1998 {published data only}
- Pagnotta A, Baron M, Korner‐Bitensky N. The effect of a static wrist orthosis on hand function in individuals with Rheumatoid Arthritis. The Journal of Rheumatology 1998;25(5):879‐85. [20‐SO] [PubMed] [Google Scholar]
Rennie 1996 {published data only}
- Rennie HJ. Evaluation of the Effectiveness of a Metacarpophalangeal Ulnar Deviation Orthosis. Journal of Hand Therapy 1996;9:371‐7. [23‐SO] [DOI] [PubMed] [Google Scholar]
Stern 1996a {published data only}
- Stern EB, Ytterberg SR, Krug HE, Mullin GT, Mahowald ML. Immediate and short‐term effects of three commercial wrist extensor orthoses on grip strength and function in patients with RA. Arthritis Care and Research 1996;9(1):42‐50. [24‐SO] [DOI] [PubMed] [Google Scholar]
Stern 1996b {published data only}
- Stern EB, Ytterberg SR, Krug HE, Mahowald ML. Finger Dexterity and Hand Function: Effect of Three Commercial Wrist Extensor Orthoses on Patients with R.A.. Arthritis Care and Research 1996;9(3):197‐205. [16‐SO] [DOI] [PubMed] [Google Scholar]
Stern 1997 {published data only}
- Stern EB, Ytterberg SR, Krug HE, Larson LM, Portoghese CP, Kratz WN, Mahowald ML. Commercial Wrist Extensor Orthoses: A Descriptive Study of Use and Preference in Patients with Rheumatoid Arthritis. Arthritis Care and Research 1997;10(1):27‐35. [11‐SO] [DOI] [PubMed] [Google Scholar]
Swigart 1999 {published data only}
- Swigart CR, Eaton RG, Glickel SZ, Johnson C. Splinting in the Treatment of Arthritis of the First Carpometacarpal Joint. The Journal of Hand Surgery 1999;24A(1):86‐91. [22‐SO] [DOI] [PubMed] [Google Scholar]
Tijhuis 1998 {published data only}
- G. J. Tijhuis, T. P. M. Vliet Vlieland, A. H. Zwinderman, J. M. W. Hazes. A Comparison of the Futuro Wrist Orthosis with a Synthetic Thermolyn Orthosis: Utility and Clinical Effectiveness. Arthritis Care and Research 1998;11(3):217‐22. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Backman 1988 {published data only}
- Backman CL, Deitz JC. Static wrist splint: Its effect on hand function in three women with RA. Arthritis Care and Research 1981;1(3):151‐60. [none] [Google Scholar]
Bennett 1965 {published data only}
- Bennett RL. Orthetic Devices to Prevent Deformities of the Hand in Rheumatoid Arthritis. Arthritis and Rheumatism October 1965;8(5):1006‐18. [DOI] [PubMed] [Google Scholar]
Convery 1967 {published data only}
- Convery FR, Conaty JP, Nickel VL. Dynamic Splinting of the Rheumatoid Hand. Orthotics and Prosthetics 1967:249‐54. [Google Scholar]
Craxford 1982 {published data only}
- Craxford AD, Stevens J, Park C. Management of the deformed rheumatoid forefoot. Clinical Orthopaedics and Related Research 1982;166(166):121‐6. [27‐SO] [PubMed] [Google Scholar]
Gruen H {published data only}
- Gruen H. Splinting in the Rheumatic Diseases. In : Rehabilitation of Rheumatic Conditions 257‐63. [Google Scholar]
Gumpel 1981 {published data only}
- Gumpel JM, Cannon S. A cross‐over comparison of ready‐made fabric wrist‐splints in RA. Rheumatology and Rehabilitation 1981;20:113‐5. [12‐SO] [DOI] [PubMed] [Google Scholar]
Kim 1995 {published data only}
- Kim JM, Moon MS. Squatting following total knee arthroplasty. Clinical Orthopaedics and Related Research 1995;313:177‐86. [19‐SO] [PubMed] [Google Scholar]
Kock 1980 {published data only}
McKnight 1982 {published data only}
- Kock Rd, Bird DA. Orthoses For Rheumatoid Fingers. Orthotics and Prosthetics 1980;34(2):25‐32. [Google Scholar]
- McKnight PT, Schomburg FL. Air pressure splint effects on hand symptoms of patients with Rheumatoid Arthritis. Archives of Physical and Medical Rehabilitation 1982;63:560‐4. [10‐SO] [PubMed] [Google Scholar]
McKnight 1992 {published data only}
- McKnight PT, Kwoh CK. Randomized, Controlled Trial of Compression Gloves in Rheumatoid Arthritis. Arthritis Care and Research 1992;5(4):223‐7. [no number] [DOI] [PubMed] [Google Scholar]
Moncur 1990 {published data only}
- Moncur C, Ward JR. Heat‐moldable shoes for management of forefoot problems in Rheumatoid arthritis. Arthritis Care and Research 1990;3(4):222‐6. [28‐SO] [Google Scholar]
Nicholas 1982 {published data only}
- Nicholas JJ, Gruen H, Weiner G, Crawshaw C, Taylor F. Splinting in RA: I. Factors Affecting Patient Compliance.. Archives of Physical Medicine and Rehabilitation 1982;63:92‐4. [26‐SO] [PubMed] [Google Scholar]
Ouellette 1991 {published data only}
- Ouellette EA. The Rheumatoid Hand : Orthotics as Preventative. Seminars in Arthritis and Rheumatism October 1991;21(2):65‐72. [DOI] [PubMed] [Google Scholar]
Palchik 1990 {published data only}
- Palchik NS, Mitchell DM, Gilbert NL, Schulz AJ, Dedrick RF, Palella. Nonsurgical management of the boutonniere deformity. Arthritis Care and Research 1990;3(4):227‐32. [18‐SO] [Google Scholar]
Souter 1971 {published data only}
- Souter WA. Splintage in the Rheumatoid Hand. Hand 1971;3(2):144‐51. [DOI] [PubMed] [Google Scholar]
Stern 1994 {published data only}
- Stern EB, Sines B, Teague TR. Commercial wrist extensor orthosis: Hand function, comfort, and interference across five styles. Journal of Hand Therapy 1994;7:237‐44. [25‐SO] [PubMed] [Google Scholar]
Additional references
Cordery 1998
- Cordery J, Rocchi M. Joint protection and fatigue management. In: J Melvin, G Jensen editor(s). Rheumatologic Rehabilitation Series. Vol. 1, Baltimore, MD: American Occupational Therapy Association, 1998:279‐322. [Google Scholar]
Deshaies 2002
- Deshaies LD. Upper extremity orthoses. In: CA Trombly, MV Radomski editor(s). Occupational Therapy for Physical Dysfunction. 5th Edition. Baltimore MD: Lippincott, Williams & Wilkins, 2002:313‐49. [Google Scholar]
Dickersin 1994
- Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. BMJ 1994;309:1286‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clinical Trials 1996;17(1):1‐12. [DOI] [PubMed] [Google Scholar]
Melvin 1989
- Melvin, JL. Rheumatic disease in the adult and child. 3rd Edition. F.A. Davis, 1989. [MEDLINE: ] [Google Scholar]
OMERACT 1993
- OMERACT. Conference on outcome measures in rheumatoid arthritis. Journal of Rheumatology 1993;20:526‐91. [PubMed] [Google Scholar]
Suarez‐Almazor 2001
- Suarez‐Almazor M, Foster W. Rheumatoid arthritis. In: S Barton editor(s). Clinical Evidence. London: British Medical Journal, 2001:832‐49. [Google Scholar]


