Abstract
No standardized PCR method is available for the laboratory diagnosis of the pertussis syndrome. Consensus recommendations for the use of PCR in the diagnosis of Bordetella pertussis infections have been proposed, and the aim of this study was to develop a method that fulfills all of these criteria. A rapid-cycle shared-primer PCR method with a microwell format and probe hybridization detection step (POR) was developed using novel oligonucleotides targeted to the outer membrane porin gene (Bordetella spp.). In specimens positive for Bordetella spp., B. pertussis was differentiated from Bordetella parapertussis and Bordetella bronchiseptica by hybridization with organism-specific oligonucleotide probes. An internal control was developed using overlap extension PCR and mouse β-actin DNA. The analytical specificity was 100%. The analytical sensitivity was comparable to that of nested IS481 and IS1001 PCR (∼1 organism per reaction). The clinical sensitivity and specificity were ascertained using 705 specimens (from 705 patients). The results were compared to those of a nested-PCR method targeting the insertion sequences IS481 and IS1001. Fifty-one specimens were positive for B. pertussis by POR and IS481 PCR. Two specimens which fulfilled a clinical definition of pertussis were positive by POR and negative by IS481 PCR. A total of 652 specimens were negative by both methods. B. parapertussis was not detected in any specimens. PCR inhibition was detected in 21 out of 705 specimens (2.98%). Thus, a rapid (4 h, including specimen preparation) PCR method which fulfills all of the consensus recommendations was developed and validated for the detection of B. pertussis.
The diagnosis of Bordetella pertussis infections by nucleic acid amplification-based methods has, in general, been shown to be both highly sensitive and specific (13), yet an agreed-upon standardized method has not yet been adopted. The following consensus international recommendations have been published (11). (i) Sample processing should be kept to a minimum. (ii) Nasopharyngeal aspirates (NPA) are the preferred specimens. (iii) Differentiation between B. pertussis and Bordetella parapertussis is necessary. (iv) Carryover control (e.g., uracil-N-glycosylase) should be used to minimize contamination. (v) Appropriate controls (positive and negative) should be used. (vi) In detection systems, probes should be used for added specificity and sensitivity. (vii) Confirmation of questionable results with an alternative target is necessary. (viii) One hundred percent of culture-positive results should be nucleic acid amplification positive. (ix) Other commensals and pathogens should test negative. (x) Testing of samples from a healthy population assumed to be negative for the pathogen is required. (xi) Use of an internal control to check for inhibition of the reaction is required. However, as yet no method has been offered which fulfills all of these criteria. In a previous study (1), we developed a nested-PCR method utilizing the insertion sequences IS481 (B. pertussis) and IS1001 (B. parapertussis). Although the method had high analytical and clinical sensitivity and specificity and differentiated between B. pertussis and B. parapertussis, it was not useful for the routine diagnostic laboratory. Our efforts since then have been directed at developing a simpler method. In this study, we describe a rapid-cycle method which fulfills all of the consensus international recommendations and evaluate it using nested PCR utilizing both prospective specimens and specimens from a previous study (1). The results show that this method would be highly suited to serve as a standardized B. pertussis PCR method.
MATERIALS AND METHODS
Bacterial strains and genomic DNA.
The bacterial strains and genomic DNA for sensitivity and specificity studies were the same as those described previously (1). Additional strains tested were Bordetella avium strain TC9 and Bordetella hinzii strain TC58, both kindly donated by Patrick Blackall from the Queensland Department of Primary Industries Animal Research Institute, Brisbane, Australia, and four Bordetella holmesii strains.
Patient specimens.
Specimen collection, initial treatment, and storage were as previously described (1). A total of 705 specimens (from 705 patients) were tested. The specimen types were as follows: NPA, 608; throat (posterior pharyngeal) swabs, 82; and sputum, 15. Six hundred fifteen specimens were from patients with respiratory symptoms. Sixty-five NPA were from healthy asymptomatic adults, initially thought to be contacts in a pertussis outbreak which was later confirmed as an influenza A outbreak. Twenty-five throat swabs were collected from healthy adult volunteers. Samples were removed from the freezer (−20°C) and thawed at 37°C for 30 min. Twenty microliters was added to 80 μl of sterile DNase- and RNase-free water, vortexed for 30 s, heated in a dry block heater for 20 min at 99.9°C, and then pulse centrifuged in a bench microcentrifuge (set at 11,300 × g) for 30 s. Positive and negative controls were treated identically to specimens. Specimens in which inhibitory substances were detected (see the method described below) underwent a DNA extraction procedure using the High Pure PCR template kit (Boehringer Mannheim, Sydney, Australia) according to the manufacturer's instructions prior to retesting.
PCR methods.
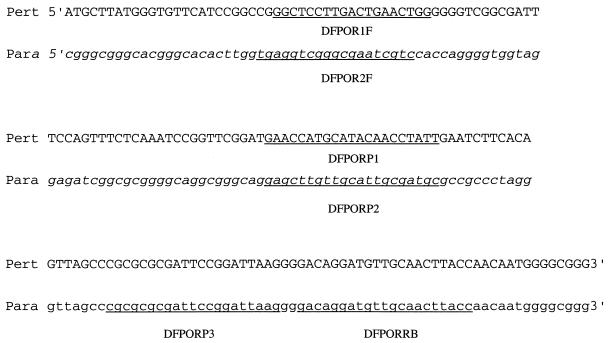
Nested IS481 PCR was performed as previously described (1). Pertussis toxin operon (PTO) PCR was also performed as described previously (D. J. Farrell, M. McKeon, G. Daggard, and T. K. S. Mukkur, Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother., abstr. 1569, p. 225, 1999). Oligonucleotides for POR used in this study were designed (Fig. 1) using previously published sequence data (5) and are listed in Table 1. They were synthesized commercially by Life Technologies.
FIG. 1.
Primers and probes used for the PCR assay. The nucleotide sequence, located upstream from the outer membrane porin gene (obtained from reference 5), shows a 3′ homogenous region between B. pertussis (Pert) and B. parapertussis (Para) and a 5′ variable region. Primers and probes are underlined. The sequence for the primer DFPORRB is the reverse complement of the underlined region. Sequence in italics shows Para sequence that differs from Pert sequence.
TABLE 1.
Oligonucleotides used in this study to detect B. pertussis and B. parapertussis
| Oligonucleotide |
Sequence |
|---|---|
| DFPOR1F | 5′GGCTCCTTGACTGAACTGG3′ |
| DFPOR2F | 5′TGAGGTCGGGCGAATCGTC3′ |
| DFPORRB | 5′Biotin-GGTAAGTTGCAACATCCTGTC3′ |
| DFPORP1 | 5′GAACCATGCATACAACCTATT3′ |
| DFPORP2 | 5′GAGCTTGTTGCATTGCGATGC3′ |
| DFPORP3 | 5′CGCGCGCGATTCCGGATTAAG3′ |
| DFPORFMB | 5′GGCTCCTTGACTGAACTGGCTGTGGCATCCATGAAAC3′ |
| DFPORRMB | 5′GGTAAGTTGCAACATCCTGTCGCATAGAGGTCTTTACGGA3′ |
| DFMBAP | 5′TCAATTCCATCATGAAGTGTGACGTTGA3′ |
For the POR PCR, 10 μl of treated specimen was added to 40 μl of a master mixture (made immediately before use) containing 5 μl of 10× PCR buffer; PCR nucleotide mixture (Boehringer Mannheim) (200 μM dATP, dCTP, and dGTP; 600 μM dUTP); 12.5 pmol (each) of primers DFPOR1F, DFPOR2F, and DFPORRB; 2.0 U of platinum Taq polymerase (Life Technologies) per reaction mixture; 2.5 mM MgCl2 (Life Technologies); and titrated internal control. One microliter of uracil-DNA glycosylase (heat labile) (Boehringer Mannheim) was added to each master mixture and incubated at room temperature for 10 min before amplification. Amplification was performed in a GeneAmp 9600 thermal cycler (Perkin-Elmer Applied Biosystems, Melbourne, Australia) with the following parameters: 2 min at 95°C followed by 44 cycles of 10 s at 94°C, 10 s at 56°C, and 5 s at 72°C, with the last cycle concluding with a reaction for 5 min at 72°C.
Detection of amplified products was performed using a modification of the PCR digoxigenin (DIG) enzyme-linked immunosorbent assay (ELISA) kit (Boehringer Mannheim). The oligonucleotide probes DFPORP1, DFPORP2, DFPORP3, and DFMBAP were labeled with DIG-ddUTP or -dATP using the DIG oligonucleotide 3′ end labeling kit (Boehringer Mannheim) according to the manufacturer's instructions. Unless specified, the reagents described in the following methodology are those present in the PCR DIG ELISA kit. Twenty microliters of denaturation solution (reagent 1a) was added to each streptavidin-coated microwell. Five microliters of each amplified specimen was added to each of two wells. The contents of the microwell plate were gently mixed and allowed to sit at room temperature for 10 min. During this time, probes were prepared for addition to the microwells. DIG-labeled probes (DFPORP3 for Bordetella spp. and DFMBAP for the internal control) were diluted 1/200 in hybridization buffer (reagent 2) and gently mixed by inversion. Two hundred microliters of diluted probe was added to the appropriate microwells, and the plate was covered with a plastic plate cover and incubated at 45°C on a heating block for 30 min. During hybridization, the conjugate was prepared by diluting the anti-DIG-peroxidase 1/100 with conjugate dilution buffer (reagent 4). At 30 min, the plate was washed six times on an automated enzyme immunoassay plate washer (Sorin; CSL Biosciences, Melbourne, Australia) using PCR ELISA buffer. One hundred microliters of the prepared conjugate was added to each well, and the plate was covered and incubated at 37°C for 30 min in a plate incubator (Sanofi Diagnostics, Sydney, Australia). The plate was then washed six times. One hundred microliters of freshly combined TMB substrate (Roche Diagnostics, Sydney, Australia) was added to each well. The reaction was stopped exactly 5 min after the addition of the substrate by adding 100 μl of 10% H2SO4.
A cutoff for the positive result was obtained from the mean of five readings (from five separate runs) of a specimen diluted to approximately one viable CFU/reaction mixture, and an equivocal result was determined from a similar series using 1/5 to 1/2 dilutions of the positive cutoff specimen. A specimen was considered negative for Bordetella spp. if the absorbance measured at 450 nm with a reference measurement at 620 nm (A450/620) was ≤0.2, positive if the A450/620 was ≥0.8, and equivocal if the A450/620 was >0.2 and <0.8. Any run in which a negative control was positive or a positive control was negative was repeated. Any specimen in which the internal control value was <0.5 was considered to have PCR inhibition, and a DNA purification step was performed using the High Pure PCR template kit before the test was repeated.
If a positive signal for Bordetella spp. was obtained, the hybridization step was repeated using the probes DFPORP1 (for B. pertussis) and DFPORP2 (for B. parapertussis and B. bronchiseptica).
In Iowa, to check that B. holmesii did not cross-react with the assay, the method was performed with four strains of B. holmesii with appropriate positive and negative controls. No testing of clinical isolates described in this study was performed. Modifications of the method described above were as follows. POR PCR was performed using biotinylated primers. Amplified products were detected and interpreted as previously described (7), using a colorimetric microwell assay in which unlabeled POR capture probes were immobilized in plate wells. Wells that contained hybridized PCR product generated color after the addition of avidin horseradish peroxidase and tetramethylbenzidine substrate. Following washing and color development steps, the plates were read in a microwell plate reader at A450.
Construction of an assay-specific internal control.
In this study, mouse cDNA was prepared from BALB/c mouse spleens used for a different study. Mouse cDNA was used, as it was available; however, a simple DNA extract of mouse DNA would suffice. Hybrid primers (DFPORFMB and DFPORRMB) were designed using the sequence for mouse β-actin (GenBank accession no. X03672); the nucleotide sequences are listed in Table 1. A master mixture was prepared which had the following final concentrations: 1× PCR buffer (Life Technologies); 200 μM (each) dATP, dCTP, dTTP, and dGTP (Pharmacia Biotech); 10 pmol of specific oligonucleotide per reaction mixture; platinum Taq, 2.0 U/reaction mixture; and 1.5 mM MgCl2. Two microliters of mouse cDNA was added to 47.5 μl of master mixture, and amplification was performed on a GeneAmp 9600 thermal cycler using the following parameters: 94°C for 2 min; 29 cycles of 94°C for 30 s, 55°C for 30 s, 72°C for 1 min; and 72°C for 5 min. Products were visualized on a 2% Tris-borate-EDTA agarose gel using ethidium bromide.
The resulting amplicon was of the same size as the amplicon for the B. pertussis assay and had the same sequences at either end but contained mouse DNA in the internal region. The internal control was then amplified by the diagnostic PCR method to produce a large amount of internal control. The internal control was then serially diluted and amplified in the standard B. pertussis assay, and the cutoff for positivity was determined. One dilution higher than the cutoff concentration was the concentration used in the master mixture. If PCR-inhibitory substances were present in the specimen, they would be detected by failure to amplify the internal control, which was detected in a separate microwell using an oligonucleotide probe (DFMBAP) specific for mouse β-actin DNA.
RESULTS
Analytical specificity was 100% using the strains previously described (1), B. avium strain TC9, B. hinzii strain TC58, and four B. holmesii strains (Table 2). No positive results were obtained for 65 NPA or 25 throat swabs collected from 90 asymptomatic healthy adults. The analytical sensitivity of the assay was between 1 and 10 CFU per reaction mixture. Table 3 shows that analytical sensitivity was not adversely affected for B. pertussis or B. parapertussis if either organism was present in minimal numbers and the other in large numbers.
TABLE 2.
Specificities of the individual probes in the POR assay for Bordetella spp.
| Species | No. of strains positive for probe (target species)
|
||
|---|---|---|---|
| DFPORP1 (B. pertussis) | DFPORP2 (B. parapertussis, B. bronchiseptica) | DFPORP3 (B. pertussis, B. parapertussis, B. bronchiseptica) | |
| B. pertussis (21)a | 21 | 0 | 21 |
| B. parapertussis (6) | 0 | 6 | 6 |
| B. bronchiseptica (3) | 0 | 3 | 3 |
| B. avium (2) | 0 | 0 | 0 |
| B. hinzii (2) | 0 | 0 | 0 |
| B. holmesii (4)b | 0 | 0 | 0 |
| Non-Bordetella (30) (from reference 1) | 0 | 0 | 0 |
Number of individual strains tested is given in parentheses.
Tested by the modified POR method in the Iowa laboratory.
TABLE 3.
Absorbances for reactions containing different amounts of B. pertussis (strain Tohama I) and B. parapertussis (strain ATCC 15237)
| No. of bacteriaa
|
A450/620b
|
|||
|---|---|---|---|---|
| B. pertussis | B. parapertussis | DFPOR1 | DFPOR2 | DFPOR3 |
| 1 | 107 | 0.03 | 2.2 | 2.25 |
| 10 | 107 | 1.2 | 2.3 | 2.1 |
| 100 | 105 | 2.25 | 2.35 | 2.4 |
| 103 | 103 | 2.3 | 2.15 | 2.25 |
| 105 | 100 | 2.15 | 1.95 | 2.1 |
| 107 | 10 | 2.4 | 1.6 | 2.35 |
| 107 | 1 | 2.25 | 0.25 | 2.05 |
CFU per reaction mixture.
Average of three readings.
In the comparison between POR and IS481 nested PCR for 705 clinical specimens, 51 specimens were positive and 652 specimens were negative for both tests. No tests were positive for IS481 and negative for POR; however, two POR-positive and IS481-negative specimens were obtained. The two specimens that produced discrepant results came from two patients who fulfilled a clinical definition of pertussis (14) and were also positive by PTO PCR. PCR inhibition was detected in 21 of 705 specimens (2.98%). Inhibitors were detected more frequently in extremely mucoid specimens, of which 8 were sputum and 13 were NPA. After DNA extraction, no inhibitors were detected for any of the 21 specimens. One of the inhibitory specimens was positive for B. pertussis after DNA extraction.
DISCUSSION
Disadvantages of the nested IS481-IS1001 method arise from the inherent problems of nested-PCR assays, in particular, the increased risk of carryover of amplified DNA. In addition, the carryover cannot be minimized by the use of the uracil-N-glycosylase carryover prevention system. Because of these problems, this method should only be performed in laboratories with staff experienced in nested-PCR techniques, and hence it is not suitable for routine laboratory use. The next step was to develop a simpler assay, using the IS481-IS1001 assay as a “gold standard” to evaluate the analytical and clinical parameters.
The two main candidates considered as appropriate targets were the repetitive insertion sequence IS481 and the regulatory region of the pertussis toxin gene. IS481 is present in all strains of B. pertussis tested so far at a rate of 50 to 100 copies per chromosome (1, 9, 10). IS481 would seem like an appropriate target due to its high copy number, yet many have questioned its use. Grimprel et al. (3) argued that the copy number might vary between strains and that insertion sequences may also be present in other Bordetella species. To assess the specificity of the insertion sequence, Glare et al. (2) performed hybridization studies with 45 different species of bacteria (from 24 genera) using a ClaI fragment as a probe. Strong hybridization occurred for B. pertussis, weak hybridization was observed for B. bronchiseptica (after prolonged autoradiography), and no hybridization was observed for any other species. In all studies except that of Glare et al. (2), the specificity of IS481-based PCR has been 100% when tested against a multitude of non-pertussis bordetellae, and a high correlation has been observed with clinical pertussis and culture. On the other hand, Glare et al. (2) reported a 12-bp difference compared to the sequence published by McLafferty et al. (9), suggesting that the insertion sequence is not absolutely conserved. Also, a recent study (8) showed that an IS481 PCR cross-reacted strongly with six strains of B. holmesii. Unfortunately, the carriage rate and clinical significance of B. holmesii are unknown, confounding assays that target IS481.
In the first attempt to develop a simpler assay, the pertussis toxin operon was used as a target, and the PTO assay performed well, both analytically and clinically, against nested IS481-IS1001 (Farrell et al., Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother.). Although ptx is present as a single-copy gene, a comparison of PTO and IS481 as targets showed equivalent sensitivities (4). On the other hand, identical PCR protocols were used for both IS481 and PTO, yet the published melting temperatures (Tm) of the primers differed by 14 and 16°C between the two methods (4). One could argue that with better optimization the IS481 PCR might have been a great deal more sensitive than PTO PCR. There are arguments for not using PTO as a target. (i) The pertussis toxin gene is also present but not expressed in B. parapertussis and B. bronchiseptica due to multiple mutations located in the ptx promoter region (6). On the other hand, an immunoglobulin G response to pertussis toxin in patients with parapertussis infections has been described, indicating that expression of the toxin genes may occur (5). (ii) Mutations in the pertussis toxin S1 subunit have recently been described; Mooi et al. (12) provide evidence that contemporary strains of B. pertussis differ in the genetic sequence of the S1 subunit, possibly through vaccine-driven evolution. For diagnostic methods, it may be wise not to use genes that code for antigens present in commercial vaccines. In addition, polymorphisms in the pertussis toxin promoter region have also been described (15).
The region upstream of the outer membrane porin gene has been used as a target for diagnostic PCR in only one previous study (5). The assay described in that study had a sensitivity of 79% against culture when gel detection was used and a sensitivity of 95% when DIG immunoblotting was used. In the present study, new primers and probes were designed using the outer membrane porin sequence data described by Li et al. (5). A rapid-cycle protocol was designed; a carryover prevention system (uracil-N-glycosylase) was included; probe detection allowed differentiation among Bordetella spp.; an assay-specific internal control was developed, allowing specimen preparation to be minimal; and the assay was evaluated against a gold standard method targeting a different gene. This method is the first to fulfill the international consensus requirements for the use of PCR in the detection of B. pertussis, as proposed by Meade and Bollen (11) and outlined above. The assay does not distinguish between B. parapertussis and B. bronchiseptica, but this should only cause concern in interpreting results from specimens obtained from immunocompromised patients, as B. bronchiseptica is only rarely part of the normal flora of humans. Nevertheless, interpretation of a positive B. parapertussis-B. bronchiseptica POR result should be considered with caution. The POR PCR assay allows a rapid, accurate, standardized, and simplified approach to the laboratory diagnosis of pertussis.
ACKNOWLEDGMENTS
This study was funded in part by the Private Practice Trust Fund, Toowoomba Health Region (D.J.F.), and the Project Team Research Project Grant of the University of Southern Queensland (T.K.S.M.).
The support of the pediatricians and general practitioners from the Darling Downs region is gratefully acknowledged. Specimens were from the Queensland Health Pathology Service Gold Coast (David Alfredson), Townsville and Mount Isa Laboratories, and Sullivan and Nicolaides and Partners Laboratories, Brisbane and Lismore (Lynne Wright). Strains of bacteria were from J. Faoagali, M. Nolan, J. Bates, R. Reed, R. McDougall, C. Coulter, Pat Blackall, and Alison Weiss.
REFERENCES
- 1.Farrell D J, Daggard G, Mukkur T K S. Nested duplex PCR to detect Bordetella pertussis and Bordetella parapertussis and its application in diagnosis of pertussis in nonmetropolitan South East Queensland, Australia. J Clin Microbiol. 1999;37:606–610. doi: 10.1128/jcm.37.3.606-610.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glare E M, Paton J C, Premier R R, Lawrence A J, Nisbet I T. Analysis of a repetitive DNA sequence from Bordetella pertussis and its application to the diagnosis of pertussis using the polymerase chain reaction. J Clin Microbiol. 1990;28:1982–1987. doi: 10.1128/jcm.28.9.1982-1987.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grimprel E, Bégué P, Anjak I, Betsou F, Guiso N. Comparison of polymerase chain reaction, culture, and Western immunoblot serology for diagnosis of Bordetella pertussis infection. J Clin Microbiol. 1993;31:2745–2750. doi: 10.1128/jcm.31.10.2745-2750.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Houard S, Hackel C, Herzog A, Bollen A. Specific identification of Bordetella pertussis by the polymerase chain reaction. Res Microbiol. 1989;140:477–487. doi: 10.1016/0923-2508(89)90069-7. [DOI] [PubMed] [Google Scholar]
- 5.Li Z, Jansen D L, Finn T M, Halperin S A, Kasina A, O'Connor S P, Aoyama T, Manclark C R, Brennan M J. Identification of Bordetella pertussis infection by shared-primer PCR. J Clin Microbiol. 1994;32:783–789. doi: 10.1128/jcm.32.3.783-789.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Locht C, Keith J M. Pertussis toxin gene: nucleotide sequence and genetic organization. Science. 1986;232:1258–1264. doi: 10.1126/science.3704651. [DOI] [PubMed] [Google Scholar]
- 7.Loeffelholz M J, Thompson C J, Long K S, Gilchrist M J R. Comparison of PCR, culture, and direct fluorescent-antibody testing for detection of Bordetella pertussis. J Clin Microbiol. 1999;37:2872–2876. doi: 10.1128/jcm.37.9.2872-2876.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loeffelholz M J, Thompson C J, Long K S, Gilchrist M J R. Detection of Bordetella holmesii using Bordetella pertussis IS481 PCR assay. J Clin Microbiol. 2000;38:467. doi: 10.1128/jcm.38.1.467-467.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McLafferty M A, Harcuss D R, Hewlett E L. Nucleotide sequence and characterization of a repetitive element from the genome of Bordetella pertussis with characteristics of an insertion sequence. J Gen Microbiol. 1988;134:2297–2306. doi: 10.1099/00221287-134-8-2297. [DOI] [PubMed] [Google Scholar]
- 10.McPheat W L, McNally T. Isolation of a repeated DNA sequence from Bordetella pertussis. J Gen Microbiol. 1987;133:323–330. doi: 10.1099/00221287-133-2-323. [DOI] [PubMed] [Google Scholar]
- 11.Meade B D, Bollen A. Recommendations for the use of the polymerase chain reaction in the diagnosis of Bordetella pertussis infections. J Med Microbiol. 1994;41:51–55. doi: 10.1099/00222615-41-1-51. [DOI] [PubMed] [Google Scholar]
- 12.Mooi F R, van Oirschot H, Heuvelman K, van der Heide H G J, Gaastra W, Willems R J L. Polymorphism in the Bordetella pertussis virulence factors P.69/pertactin and pertussis toxin in the Netherlands: temporal trends and evidence for vaccine-driven evolution. Infect Immun. 1998;66:670–675. doi: 10.1128/iai.66.2.670-675.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Müller F C, Hoppe J E, Wirsing von König C H. Laboratory diagnosis of pertussis: state of the art in 1997. J Clin Microbiol. 1997;35:2435–2443. doi: 10.1128/jcm.35.10.2435-2443.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Health and Medical Research Council. Surveillance case definitions. Canberra, Australia: National Health and Medical Research Council; 1994. [Google Scholar]
- 15.Nygren M, Reizenstein E, Ronaghi M, Lundeberg J. Polymorphism in the pertussis toxin promoter region affecting the DNA-based diagnosis of Bordetella infection. J Clin Microbiol. 2000;38:55–60. doi: 10.1128/jcm.38.1.55-60.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]