Abstract
Background
In response to the spread of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and the impact of coronavirus disease 2019 (COVID‐19), governments have implemented a variety of measures to control the spread of the virus and the associated disease. Among these, have been measures to control the pandemic in primary and secondary school settings.
Objectives
To assess the effectiveness of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic, with particular focus on the different types of measures implemented in school settings and the outcomes used to measure their impacts on transmission‐related outcomes, healthcare utilisation outcomes, other health outcomes as well as societal, economic, and ecological outcomes.
Search methods
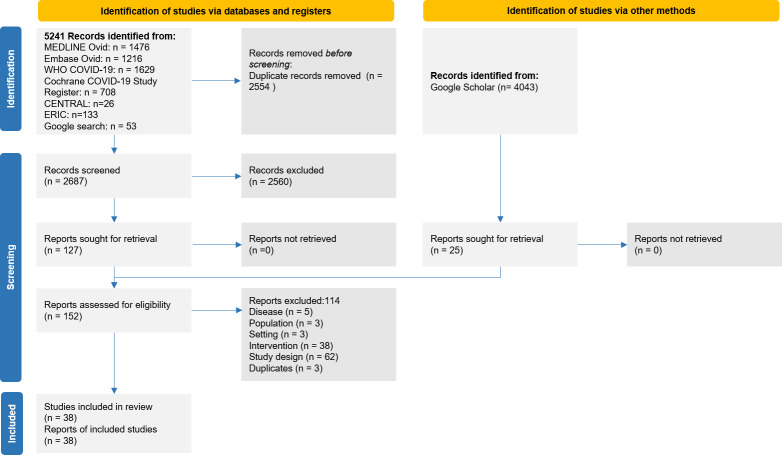
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, and the Educational Resources Information Center, as well as COVID‐19‐specific databases, including the Cochrane COVID‐19 Study Register and the WHO COVID‐19 Global literature on coronavirus disease (indexing preprints) on 9 December 2020. We conducted backward‐citation searches with existing reviews.
Selection criteria
We considered experimental (i.e. randomised controlled trials; RCTs), quasi‐experimental, observational and modelling studies assessing the effects of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic. Outcome categories were (i) transmission‐related outcomes (e.g. number or proportion of cases); (ii) healthcare utilisation outcomes (e.g. number or proportion of hospitalisations); (iii) other health outcomes (e.g. physical, social and mental health); and (iv) societal, economic and ecological outcomes (e.g. costs, human resources and education). We considered studies that included any population at risk of becoming infected with SARS‐CoV‐2 and/or developing COVID‐19 disease including students, teachers, other school staff, or members of the wider community.
Data collection and analysis
Two review authors independently screened titles, abstracts and full texts. One review author extracted data and critically appraised each study. One additional review author validated the extracted data. To critically appraise included studies, we used the ROBINS‐I tool for quasi‐experimental and observational studies, the QUADAS‐2 tool for observational screening studies, and a bespoke tool for modelling studies. We synthesised findings narratively. Three review authors made an initial assessment of the certainty of evidence with GRADE, and several review authors discussed and agreed on the ratings.
Main results
We included 38 unique studies in the analysis, comprising 33 modelling studies, three observational studies, one quasi‐experimental and one experimental study with modelling components.
Measures fell into four broad categories: (i) measures reducing the opportunity for contacts; (ii) measures making contacts safer; (iii) surveillance and response measures; and (iv) multicomponent measures. As comparators, we encountered the operation of schools with no measures in place, less intense measures in place, single versus multicomponent measures in place, or closure of schools.
Across all intervention categories and all study designs, very low‐ to low‐certainty evidence ratings limit our confidence in the findings. Concerns with the quality of modelling studies related to potentially inappropriate assumptions about the model structure and input parameters, and an inadequate assessment of model uncertainty. Concerns with risk of bias in observational studies related to deviations from intended interventions or missing data. Across all categories, few studies reported on implementation or described how measures were implemented. Where we describe effects as 'positive', the direction of the point estimate of the effect favours the intervention(s); 'negative' effects do not favour the intervention.
We found 23 modelling studies assessing measures reducing the opportunity for contacts (i.e. alternating attendance, reduced class size). Most of these studies assessed transmission and healthcare utilisation outcomes, and all of these studies showed a reduction in transmission (e.g. a reduction in the number or proportion of cases, reproduction number) and healthcare utilisation (i.e. fewer hospitalisations) and mixed or negative effects on societal, economic and ecological outcomes (i.e. fewer number of days spent in school).
We identified 11 modelling studies and two observational studies assessing measures making contacts safer (i.e. mask wearing, cleaning, handwashing, ventilation). Five studies assessed the impact of combined measures to make contacts safer. They assessed transmission‐related, healthcare utilisation, other health, and societal, economic and ecological outcomes. Most of these studies showed a reduction in transmission, and a reduction in hospitalisations; however, studies showed mixed or negative effects on societal, economic and ecological outcomes (i.e. fewer number of days spent in school).
We identified 13 modelling studies and one observational study assessing surveillance and response measures, including testing and isolation, and symptomatic screening and isolation. Twelve studies focused on mass testing and isolation measures, while two looked specifically at symptom‐based screening and isolation. Outcomes included transmission, healthcare utilisation, other health, and societal, economic and ecological outcomes. Most of these studies showed effects in favour of the intervention in terms of reductions in transmission and hospitalisations, however some showed mixed or negative effects on societal, economic and ecological outcomes (e.g. fewer number of days spent in school).
We found three studies that reported outcomes relating to multicomponent measures, where it was not possible to disaggregate the effects of each individual intervention, including one modelling, one observational and one quasi‐experimental study. These studies employed interventions, such as physical distancing, modification of school activities, testing, and exemption of high‐risk students, using measures such as hand hygiene and mask wearing. Most of these studies showed a reduction in transmission, however some showed mixed or no effects.
As the majority of studies included in the review were modelling studies, there was a lack of empirical, real‐world data, which meant that there were very little data on the actual implementation of interventions.
Authors' conclusions
Our review suggests that a broad range of measures implemented in the school setting can have positive impacts on the transmission of SARS‐CoV‐2, and on healthcare utilisation outcomes related to COVID‐19. The certainty of the evidence for most intervention‐outcome combinations is very low, and the true effects of these measures are likely to be substantially different from those reported here. Measures implemented in the school setting may limit the number or proportion of cases and deaths, and may delay the progression of the pandemic. However, they may also lead to negative unintended consequences, such as fewer days spent in school (beyond those intended by the intervention). Further, most studies assessed the effects of a combination of interventions, which could not be disentangled to estimate their specific effects. Studies assessing measures to reduce contacts and to make contacts safer consistently predicted positive effects on transmission and healthcare utilisation, but may reduce the number of days students spent at school. Studies assessing surveillance and response measures predicted reductions in hospitalisations and school days missed due to infection or quarantine, however, there was mixed evidence on resources needed for surveillance. Evidence on multicomponent measures was mixed, mostly due to comparators. The magnitude of effects depends on multiple factors. New studies published since the original search date might heavily influence the overall conclusions and interpretation of findings for this review.
Plain language summary
Measures implemented in the school setting to contain the COVID‐19 pandemic
What was studied in the review?
In order to reduce the spread of the virus that causes COVID‐19, many governments and societies put mitigation measures in place in schools. However, we do not know whether these measures work with regards to reducing the spread of the virus, or how these measures affect other aspects of life, such as education, the economy or society as a whole.
What are measures implemented in the school setting?
Measures in the school setting can be grouped into the following four broad categories.
1. Measures reducing the opportunity for contacts: by reducing the number of students in a class or a school, opening certain school types only (for example primary schools) or by creating a schedule by which students attend school on different days or in different weeks, the face‐to‐face contact between students can be reduced.
2. Measures making contacts safer: by putting measures in place such as face masks, improving ventilation by opening windows or using air purifiers, cleaning, handwashing, or modifying activities like sports or music, contacts can be made safer.
3. Surveillance and response measures: screening for symptoms or testing sick or potentially sick students, or teachers, or both, and putting them into isolation (for sick people) or quarantine (for potentially sick people).
4. Multicomponent measures: measures from categories 1, 2 and 3 are combined.
What is the aim of the review?
We aimed to find out which measures implemented in the school setting allow schools to safely reopen, stay open, or both, during the COVID‐19 pandemic.
What did we do?
We searched for studies that looked at the impact of these types of measures in the school setting on the spread of the virus that causes COVID‐19, the impact on the healthcare system (i.e. how many hospital beds are needed), as well as important social aspects (i.e. how often students attended school). The studies could focus on students, teachers and other school staff, as well as on families and the whole community. They could use real‐life data (observational studies) or data from computer‐generated simulations (modelling studies).
What are the main results of the review?
We found 38 relevant studies. Most of these were modelling studies (33 studies). Five studies used real‐world data. Twenty studies were conducted in North or South America, 16 in Europe and two in China.
Below we summarise the main findings by category.
1. Measures reducing the opportunity for contacts
We found 23 modelling studies assessing measures to reduce the opportunity for contacts. All studies showed reductions in the spread of the virus that causes COVID‐19 and the use of the healthcare system. Some studies also showed a reduction in the number of days spent in school due to the intervention.
2. Measures making contacts safer
We found 11 modelling studies and two real‐world studies looking at measures, such as mask wearing in schools, cleaning, handwashing, and ventilation. Five of these studies combined multiple measures, which means we cannot see which specific measures worked and which did not. Most studies showed reductions in the spread of the virus that causes COVID‐19; some studies, however, showed mixed or no effects.
3. Surveillance and response measures
We found 13 modelling studies and one real‐world study assessing surveillance and response measures. Twelve studies focused on mass testing and isolation measures, while two looked specifically at symptom‐based screening and isolation. Most studies showed results in favour of the intervention, however some showed mixed or no effects.
4. Multicomponent measures
We found three studies that looked at multicomponent interventions, where it was not possible to determine the effect of each individual intervention. These included one modelling study and two real‐world studies. These studies assessed physical distancing, modification of activities, cancellation of sports or music classes, testing, exemption of high‐risk students, handwashing, and face masks. Most studies showed reduced transmission of the virus that causes COVID‐19, however some showed mixed or no effects.
How confident are we in the findings of this review?
Our confidence in these results is limited. Most studies used models, that is, they estimated the effects of the interventions rather than observing outcomes. As the models are built on assumptions about how the virus spreads and how people behave, we lack real‐world evidence. Many studies were published as 'preprints' without undergoing rigorous checks of published studies, which further limits our confidence. Also, the studies were very different from each other (for example, with regards to the levels of transmission in the community).
What are the key messages?
Reopening schools or keeping schools open while having a broad range of measures in place can reduce transmission of the virus that causes COVID‐19. Such measures can also reduce the number of people who will need to go to hospital due to developing COVID‐19. We still know very little about other consequences of these measures, such as those linked to education, resources, and physical or mental health, as this knowledge is mostly based on studies modelling the real world. More studies set in the real world using real‐world data are needed.
How up to date is this evidence?
The evidence is up‐to‐date to December 2020.
Summary of findings
Background
Description of the condition and intervention
On 11 March 2020, the World Health Organization (WHO) declared a global pandemic of the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and the associated disease, COVID‐19 (WHO 2020a). To contain the spread of SARS‐CoV‐2, national and subnational governments have implemented a variety of measures (Prem 2020), including many non‐pharmaceutical interventions (Smith 2020; WHO 2019).
A multitude of settings, such as workplaces, public spaces, as well as means of transportation were affected by these non‐pharmaceutical interventions. One of the most debated settings, however, was schools. In the context of the current pandemic, 192 countries had closed schools in order to reduce transmission of SARS‐CoV‐2 by mid‐April 2020, affecting more than 90% (nearly 1.6 billion) of the world’s student population (UNESCO 2021). School closures aim to reduce contacts between students and school staff by preventing them from being in close contact with each other, with the goal of reducing viral transmission between and within these groups – and with the ultimate goal of limiting levels of community transmission. Proactive (closing schools regardless of any identified cases) and reactive (closing schools in reaction to an identified case) school closures have been used historically to contain outbreaks (Chowell 2011; Isfeld‐Kiely 2014). While some studies demonstrate that closures can lead to reductions in viral transmission (notably in relation to influenza infections), others suggest that closures alone are not enough to prevent community transmission, in particular in the absence of other measures (Walsh 2021). They may, however, be able to delay the peak of an epidemic and therefore allow time to implement other interventions, such as vaccinations (Fung 2015; Lee 2010). During the COVID‐19 pandemic, transmissions within schools as well as school clusters (i.e. one case being responsible for a cluster of cases) have been reported in primary and secondary schools (Otte im Kampe 2020; Stein‐Zamir 2020). It has, however, been shown that the incidence in schools was highly dependent on the level of community transmission and that the cases associated with schools did not play a major role in driving the pandemic (Aleta 2020; Gandini 2021; Ismail 2021).
The decision to close schools was fuelled by the uncertain role of children in the transmission of SARS‐CoV‐2. It is widely acknowledged that children of all ages are susceptible to SARS‐CoV‐2 infection (Aspinall 2020; Bershteyn 2020; Dong 2020; Han 2021), but younger children appear to be less susceptible to infection (Koh 2020; Viner 2021a). Transmission of SARS‐CoV‐2 by infected younger children (under approximately 12 years) appears to be lower than transmission by adults, although robust evidence is lacking (Viner 2021a). Adolescents, however, seem to be comparable to adults with respect to transmission of SARS‐CoV‐2 (Dattner 2020; Fontanet 2020; Park 2020). When infected, most paediatric patients (< 18 years) with COVID‐19 present with mild symptoms (Davies 2020; Dong 2020; Han 2021; Laws 2021; Lee 2021), and have lower rates of hospitalisation, severe hospitalisation, and death than other age groups (Castagnoli 2020; Choi 2020; Götzinger 2020; Zimmermann 2021). There is limited evidence that 'long COVID', where various symptoms persist for more than 60 days in symptomatic and even asymptomatic cases, also affects children (Buonsenso 2021).
The evidence on the effectiveness of school closures in reducing transmission is unclear (Bin Nafisah 2018; Rashid 2015), while there is increasing evidence on significant negative implications associated with school closures for children, teachers, other school staff, parents, and for society as a whole (Christakis 2020; Golberstein 2020; Kneale 2020; Smith 2020; UNESCO 2021; Viner 2020). Notably, school closures can have negative impacts on educational outcomes and child development, and on the physical, mental, and social health of children and adolescents (Golberstein 2020, UNESCO 2020a). School closures may even lead to a decrease in gross domestic product due to the loss of economic productivity of parents and others caring for children (Kneale 2020). As well as having implications for economic productivity, school closures may also have implications for community transmission, particularly if closures are implemented before work closures, as there may be transmission from the home to the workplace. This might be particularly important in cases where parents work in healthcare settings.
In light of these negative consequences, most countries have moved beyond general school closures and instead sought ways to safely reopen schools during the pandemic (Bonell 2020; Couzin‐Frankel 2020; Dibner 2020; WHO 2020b). In order to ensure that schools can safely reopen, or stay open, or both, countries have implemented a wide range of measures at the national or state level (e.g. legislation), at the level of the school, at the level of cohorts within the school (e.g. grades, classes, or faculty/school staff), and at the individual level (including among high‐risk individuals). These measures include organisational interventions, such as cohorting, staggered attendance, reduced class sizes, mask‐wearing policies, handwashing policies, and other interventions to either reduce contacts within schools or to make these contacts safer (Aspinall 2020; Isphording 2020; Macartney 2020; Monod 2020). They also comprise structural interventions, such as enhanced cleaning and ventilation practices (Curtius 2020; NCIRS 2020 ), as well as surveillance and response measures, such as preventative testing, tracing, self‐isolation rules for identified cases and quarantine rules for suspected cases and their contacts (Di Domenico 2020a; Head 2020).
Why it is important to do this review
Several reviews have sought to understand the role of children and schools in the transmission of SARS‐CoV‐2 and their influence on the course of the pandemic (Fadlallah 2020; NCCMT 2021; Public Health Ontario 2020; Viner 2021a). While one review examined the effectiveness of school closures (Walsh 2021), we are not aware of any review that assessed the impacts of the broad range of measures implemented in the school setting in a systematic and comprehensive manner. Also, the reviews conducted to date have not assessed the impacts that these measures have on outcomes not related to SARS‐CoV‐2 transmission, such as transmission of other viral respiratory diseases, other health outcomes (physical, psychosocial), and broader societal, economic and ecological outcomes (Viner 2021a).
In October 2020, in consultation with the World Health Organization (WHO), the review authors developed a scoping review to map the evidence of various measures implemented in the school setting to safely reopen schools and/or keep schools open during the COVID‐19 pandemic (Krishnaratne 2020). The scoping review identified 42 studies assessing a range of measures undertaken globally. Included studies used experimental, quasi‐experimental, and observational designs, as well as various mathematical and epidemiological modelling techniques. It classified measures into three broad intervention categories: organisational measures to reduce transmission of SARS‐CoV‐2 (e.g. mask‐wearing policies, reduced class sizes, and staggered attendance), structural/environmental measures to reduce transmission of SARS‐CoV‐2 (e.g. enhanced cleaning and ventilation practices), and surveillance and response measures in relation to SARS‐CoV‐2 infections (i.e. testing, tracing, self‐isolation and quarantine measures). While the review specified four key outcome categories (transmission‐related outcomes; healthcare utilisation; other health outcomes; and societal, economic and ecological implications), most studies focused on transmission‐related outcomes. No studies described outcomes concerned with psychosocial health and well‐being among students and school staff, or economic implications for parents and other carers.
The vast majority of the identified studies used various modelling techniques to assess the impact of various measures in schools, each with its own set of data and assumptions that may not have been a true reflection of the real‐world setting. The scoping review concluded that there is an urgent need for empirical studies assessing the effectiveness of the measures to reduce contacts and to make contacts safer within the school setting (Krishnaratne 2020).
The scoping review informed the development of this rapid review to synthesise the evidence on the effectiveness of measures implemented in the school setting to contain the COVID‐19 pandemic.
Objectives
To assess the effectiveness of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic, with particular focus on the different types of measures implemented in school settings and the outcomes used to measure their impacts.
The review aims to address the following key question.
How effective are different types of measures implemented in the school setting at reducing transmission between students, teachers and other school staff, and in the wider community during the COVID‐19 pandemic?
It also seeks to examine the following subquestions.
What are the implications of these measures for non‐transmission‐related outcomes (e.g. healthcare utilisation, other health outcomes, and societal, economic and ecological outcomes)?
How are these measures implemented within the school setting?
Methods
In this review, we included studies that quantitatively assess the impact of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic. This rapid review was informed by a preceding scoping review (Krishnaratne 2020) that included a logic model that describes our a priori, evidence‐informed understanding of the system in which the various measures are implemented (Figure 1). We used this in planning the data extraction and evidence mapping, and adapted it inductively over the course of the scoping review to include categories and subcategories as they emerged. We used the revised logic model to describe the identified evidence in the scoping review (Figure 2). Together with the resulting evidence gap map (Figure 3), it showed a significant gap in the evidence with regards to non‐transmission‐related outcomes.
1.
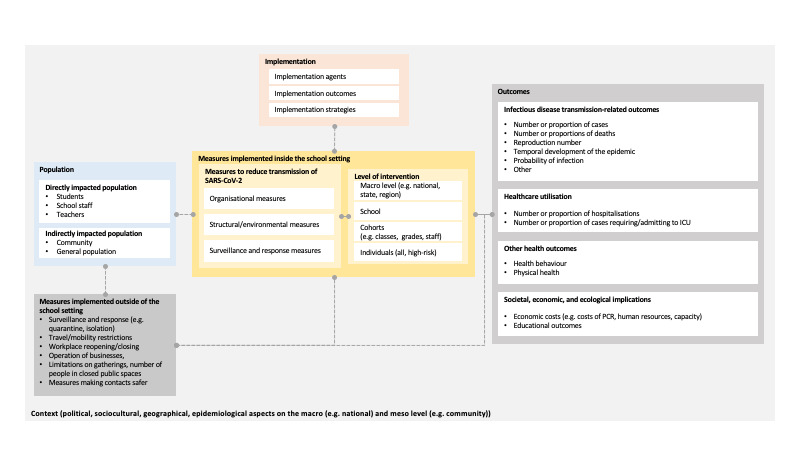
A priori logic model
2.
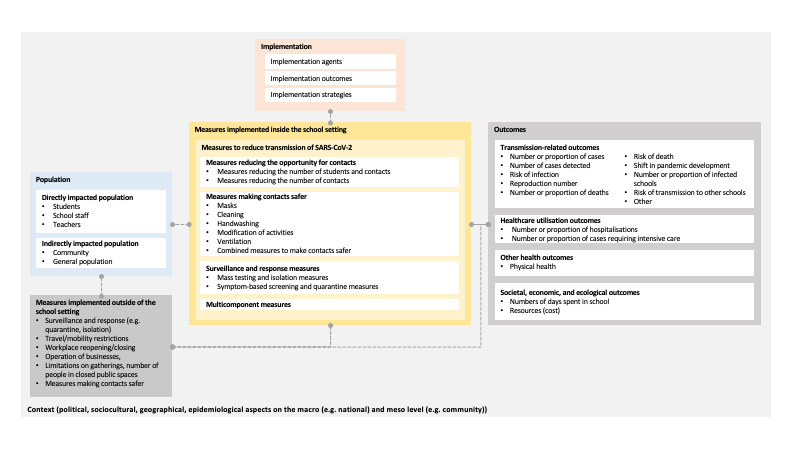
A posteriori logic model
3.
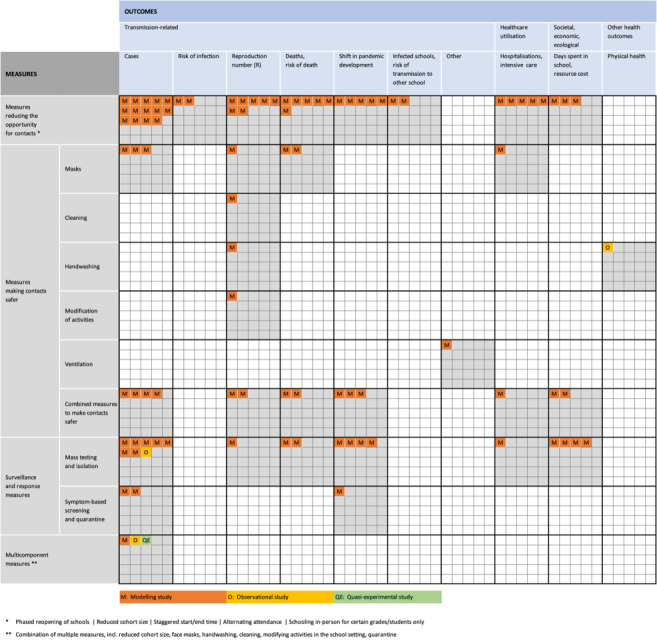
Evidence gap map in which each square represents the case in which a single included study evaluated a type of school measure (rows) against an outcome category (columns); additionally, the study type is provided (colour)
We used the revised logic model as a basis for the a priori logic model informing this rapid review. The criteria for considering studies for this review, described below, are in line with the logic model.
To conduct this review, we largely adhered to the rapid review guidance issued by Cochrane (Garritty 2020), apart from double screening all titles, abstracts and full texts in order to avoid overlooking relevant studies. At least one review author checked all data extractions. One review author conducted risk of bias assessment, but this was checked and validated by at least two review authors. A minimum of two review authors applied GRADE. Moreover, in order to assure the methodological rigour of this review, we created several mechanisms. First, we assigned data extraction, risk of bias assessment and synthesis to very experienced review authors. In addition, we involved a team with extensive experience on modelling studies to support us with the data extraction, synthesis and quality assessment. All steps were piloted with the suggested number of items (i.e. piloting of text/abstract screening with 50 records; piloting of full‐text‐screening with 10 studies; piloting of data extraction with five studies). We held regular team meetings and kept a list of rolling questions where we discussed arising questions. The protocol for this rapid review was reviewed and approved by Cochrane and published with the Open Science Framework (Krishnaratne 2021). Where we adapted these methods, we transparently report on this in the Discussion section.
Criteria for considering studies
Types of studies
We included studies that provide a quantitative measure of impact, including experimental and quasi‐experimental studies, observational studies, and mathematical modelling studies. Non‐pharmaceutical interventions to respond to the COVID‐19 pandemic had to be decided on and implemented very quickly, often without the possibility to plan and conduct high‐quality evaluation studies.
Broadly, we included the following types of studies, but considered all studies providing a quantitative measure of impact, regardless of whether they fell specifically under one of the following categories.
1. Experimental and quasi‐experimental studies:
randomised controlled trials (RCTs) including cluster‐RCTs;
interrupted time series studies;
controlled before‐after studies and difference‐in‐differences studies;
instrumental variable studies;
regression discontinuity studies.
2. Observational studies:
cohort studies;
case‐control studies.
3. Mathematical modelling studies:
compartmental models (e.g. SEIR‐type models comprising multiple compartments, such as S: susceptible, E: exposed, I: infectious, R: recovered);
agent‐based models;
Bayesian hierarchical models (i.e. models comprising several submodels to integrate observed data as well as uncertainty);
spatial models (i.e. modelling disease transmission spatially).
We included mixed methods studies that allowed for extraction of quantitative impact measures. For certain measures, e.g. symptom screening or testing within schools, we expected to identify a wide range of diagnostic test accuracy studies; we included such studies only if their implementation as part of a school‐related measure and the resulting impact was evaluated.
We considered studies published in journals as well as those published on preprint servers.
We excluded the following types of studies and publications.
Studies not providing a quantitative measure of impact (e.g. studies providing only a graphical summary of the development of the number of cases over time in relation to the introduction of control measures, qualitative studies).
Diagnostic studies that did not provide a quantitative measure of impact beyond sensitivity and specificity (e.g. test accuracy studies assessing the sensitivity and specificity of different screening or diagnostic tests).
Non‐empirical studies (e.g. commentaries, editorials, literature reviews not reporting primary empirical data).
Systematic reviews (although these were used for backward and forward citation tracking; Appendix 1).
Conference abstracts and reports.
Setting
For this review, we considered schools as any setting with the primary purpose to provide regular education to children between 4 and 18 years of age. Most countries distinguish between primary or elementary education and secondary education. The school could be either an institution where students live on the premises (e.g. boarding school) or a day school. We defined the school setting as the school, the school grounds, vehicles to arrive at, return from or move around in or between school premises, or any setting related to any activity organised by or linked to the school. Measures might affect activities carried out in the classroom, during breaks, during dining, in hallways, in bathrooms, in faculty rooms, or during transportation and movement around the campus. Further, by measures ‘in and around’ the school, we refer to activities such as public transportation to and from the school, as well as activities between students, staff, and other populations that take place before/after school, which would not have taken place if schools were not open. These include structured activities, such as the participation in sports or other extracurricular activities, as well as informal activities, such as leisure time before and after school, long lunch breaks for older students, and businesses/cafés visited by students and staff throughout the school day. The context surrounding schools was also considered in the synthesis and interpretation of results. Whilst setting refers to the physical location of an intervention, context has been defined as “a set of characteristics and circumstances that consist of active and unique factors within which the implementation is embedded” (Pfadenhauer 2017). In addition, implementation has been defined as, “an actively planned and deliberately initiated effort with the intention to bring a given intervention into policy and practice within a particular setting” (Pfadenhauer 2017). Thus, we also considered how the intervention interacts with the setting, as well as context and implementation aspects to produce various outcomes.
Types of participants
Different groups of people are impacted by measures implemented in the school setting. These include those directly impacted in the school setting, such as students, their teachers, and other school staff. Other populations impacted less directly and outside of the school setting include carers, families and friends of students, as well as members of the wider community in which schools are embedded. Specifically, we included studies that described populations at risk of becoming infected with SARS‐CoV‐2, or developing COVID‐19 disease, or both.
Particular populations of interest in this review were:
students between 4 and 18 years of age (selected studies that include participants outside of this age range, e.g. studies of a German school which also included some 19‐year‐old students, were included);
teachers working in the school setting;
other staff working in the school setting; and
individuals indirectly impacted by the school setting (i.e. general population, parents/carers).
We excluded studies targeting non‐human transmission.
Types of interventions
We included studies that assessed the effectiveness of measures implemented in the school setting and the wider community during the COVID‐19 pandemic. These can be implemented at: (i) the macro level (e.g. national or regional legislation); (ii) the school level; (iii) the level of groups, including student cohorts, classes, grades or faculty/school staff; and (iv) the level of the individual, including students and teachers at elevated risk of infection or adverse health consequences of COVID‐19, as well as students with special learning needs, or from disadvantaged families, or both.
In the scoping review, we categorised interventions into three broad categories, i.e. organisational measures to reduce transmission of SARS‐CoV‐2; structural/environmental measures to reduce transmission of SARS‐CoV‐2; and surveillance and response measures in relation to SARS‐CoV‐2 infections. In the process of conducting this review, we found that most studies focus on transmission‐related outcomes, and that many interventions are being implemented in combination with each other. As a result, we arranged these a priori intervention categories into the following four broad intervention categories.
Measures reducing the opportunity for contacts: policies addressing the timing and organisation of school activities (e.g. cohorting, alternating physical presence, and staggered arrival/departure, breaks, and extracurricular activities, blended learning).
Measures making contacts safer: policies addressing the behaviour of students, or school staff, or both (e.g. mask mandates, distancing regulations, and handwashing guidelines). Measures altering the physical environment (e.g. enhanced cleaning and ventilation practices, adding physical barriers to help individuals avoid contact, and adaptations to transportation).
Surveillance and response measures: strategies to screen, or test, or both, individuals, or groups, or both (e.g. polymerase chain reaction (PCR) testing of students or staff with symptoms, antigen testing of students or staff without any symptoms) and subsequent action (e.g. reactive dismissal of potentially infected individuals, stay‐at‐home orders for students or staff who have come into contact with an infected individual).
Multicomponent measures: strategies using a combination of at least two of the aforementioned categories.
In Table 5, the intervention categories as well as the respective subcategories are described in detail.
1. Overview of intervention categories.
| Broad intervention category | Included interventions |
| Measures reducing the opportunity for contacts |
|
| Measures making contacts safer |
|
| Surveillance and response measures |
|
| Multicomponent measures |
|
We excluded studies if:
they only described interventions not directly intended to reduce the transmission of SARS‐CoV‐2 (e.g. improvements to online learning platforms); or
they only described interventions not implemented in the school setting (as defined above), including a range of containment and mitigation measures (e.g. community‐based quarantine, personal protective measures, hygiene measures, bans on mass gatherings and other social‐distancing measures).
Types of outcomes
Based on the categories used in the scoping review, we searched for and classified outcomes into four broad categories, i.e. transmission‐related outcomes; healthcare utilisation; other health outcomes; and societal, economic and ecological outcomes. Therefore, we considered the following primary outcomes under these categories.
1. Transmission‐related outcomes:
cases avoided due to the intervention (e.g. number, proportion, rate of cases observed or predicted with and without the intervention)
number or proportion of deaths;
shift in pandemic development due to the intervention (e.g. probability of pandemic, time to or delay in pandemic arrival or peak, size of pandemic peak, change in the effective reproduction number);
other transmission‐related outcomes (e.g. risk of transmission between schools, number of reactive closures due to cases, number of schools with cases).
2. Healthcare utilisation outcomes:
number or proportion of hospitalisations;
number or proportion of cases requiring intensive care.
3. Other health outcomes:
physical, social and mental health outcomes directly related to school measures, both positive and negative.
4. Societal, economic and ecological outcomes:
costs, human resources and capacity, educational outcomes (e.g. days spent in school).
We did not consider studies reporting on other outcomes (e.g. diagnostic test accuracy).
Search methods for identification of relevant studies
Our search strategy was structured around two main search components focused on: (i) SARS‐CoV‐2/COVID‐19; and (ii) control measures implemented in the school setting. We largely followed the search strategy that was used for the scoping review of school measures; this was developed for MEDLINE and adapted for other databases. We limited results to the year 2020, the point at which publications about schools and the COVID‐19 pandemic began to appear. We did not apply a study design filter as we considered a wide range of study types for inclusion.
An experienced information specialist adapted and ran systematic searches on 9 December 2020 in the following electronic databases.
Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) (1946 to present).
Ovid Embase (1996 to present).
Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library (inception to present).
Educational Resources Information Center (ERIC) via the Institute of Education Science at the US Department of Education (2002 to present).
We also searched the following COVID‐19‐specific databases on 9 December 2020.
The Cochrane COVID‐19 Study Register (covid-19.cochrane.org), which contains study references from ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), PubMed, Embase, CENTRAL, medRxiv and other handsearched articles from publishers’ websites.
The WHO COVID‐19 Global literature on coronavirus disease (search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov), which contains primarily research (published and/or prepublication) journal articles from PubMed, Web of Science, Global Index Medicus, Embase, and the CDC Database of COVID‐19 Research Articles. MedRxiv, BioRxiv, ChemRxiv and SSRN also include prepublications. In addition, Lanzhou University submits on a daily basis citations from CNKI as well as a number of Chinese journal publishers.
Moreover, we searched Google to identify relevant items not captured in any of the six databases. See Appendix 2 for the search strategies used.
We performed a further top‐up search in August 2021 and added those results to Studies awaiting classification; we will incorporate these studies into the review at the next update.
Inclusion of non‐English language studies
We did not impose any restrictions with regards to languages. Due to the language skills represented on the team, we considered studies published in Armenian, English, French, German, Italian, Russian and Spanish. Where necessary, we sought help with translation for any other languages. We, however, did not identify any study meeting our inclusion criteria published in a language other than English.
Data collection and analysis
Selection of studies
After deduplication, we used standardised title and abstract screening guidance to calibrate the screening procedures with all review authors involved with the screening using the same 50 titles and abstracts. We discussed and resolved all issues and revised the screening guidance accordingly. Two review authors then screened all titles and abstracts in duplicate, excluding only those studies which were clearly irrelevant. Studies that were marked as unclear were moved forward to the next stage.
We conducted a pilot of the full‐text screening; all review authors involved with full‐text screening assessed a set of 10 full‐text studies at the outset (Garritty 2020). The team discussed any open questions or issues, as well as how to harmonise screening across all review authors. Two review authors then screened the remaining full texts in duplicate. Any discrepancies were discussed by the two screening review authors, and any unclear cases were discussed with a third review author and/or the review team. At this stage, a final decision regarding inclusion/exclusion was made.
We used EndNote X9 to manage the collection and deduplication of records. For title and abstract screening, we used Rayyan, a web‐based application, designed for citation screening for systematic reviews (Ouzzani 2016). We documented and reported reasons for the exclusion of full texts using Microsoft Excel (Microsoft 2018)
We recorded reasons for excluding studies during full‐text screening.
Data extraction and management
Two review authors (shared among ShK, HL and LMP) independently extracted study characteristics and data from all included studies using a data extraction form in Microsoft Excel.
We extracted the following main categories of data; relevant subcategories can be found in the full data extraction form (see Appendix 3):
study information;
study design;
population and setting;
intervention;
outcomes and results;
implementation;
context.
We piloted and accordingly revised the data extraction form using five purposively selected heterogeneous studies meeting the inclusion criteria.
Assessment of risk of bias in and quality appraisal of included studies
For experimental/quasi‐experimental and observational studies, one review author (from LMP, HL, ShK) assessed the risk of bias of each included study, using the appropriate tool, and a second review author checked the assessment. The same process was followed for modelling studies, undertaken by review authors with modelling expertise (TL, ClK, AB). Conflicts, questions, or uncertainties were discussed between these review authors, or among the larger review team, or both.
We assessed risk of bias for effects reported for all outcomes, using multiple tools.
For experimental studies, we had planned to use the Cochrane RoB 2 tool (Higgins 2021); however, we did not find any relevant studies and therefore did not use this tool.
For quasi‐experimental and observational studies, we used ROBINS‐I for the assessment of non‐randomised studies of interventions (Sterne 2016); given that we identified different types of quasi‐experimental and observational studies, we also referred to the Cochrane Handbook for Systematic Reviews of Interventions for additional guidance on assessing risk of bias of different types of non‐randomised studies (Sterne 2021). We treated the effect of assignment (intention‐to‐treat) as the effect of interest and assessed risk of bias for the following domains: confounding, selection of participants into the study, classification of interventions, deviation from intended interventions, missing data, measurement of outcomes, and selection of reported result. We judged each domain as low, moderate, serious or critical risk of bias based on a series of signalling questions. In applying ROBINS‐I, important confounding factors that each study would ideally be controlled for should be defined a priori. Given the measures implemented in the school setting, we expected that relevant studies would be conducted at the cluster level. Based on the body of evidence identified in the scoping review (Krishnaratne 2020), important confounding factors would be related to between‐group differences (where multiple groups/cohorts are assessed) such as age, sex and socioeconomic status. Further, we anticipated that many of the studies would include co‐interventions that could differ between intervention groups and have an impact on outcomes. Such co‐interventions can be implemented in the school setting (e.g. handwashing and mask policies) and in the wider community (e.g. stay‐at‐home policies, social‐distancing measures, travel restrictions). We managed ROBINS‐I assessments using Google Sheets (https://docs.google.com/spreadsheets/). Due to the nature of the results presented, we applied the ROBINS‐I tool to the study as a whole rather than to specific outcome results, as recommended in the guidance. We followed ROBINS‐I and Cochrane Handbook guidance regarding studies at critical risk of bias, meaning that we excluded any study at critical risk of bias from the analysis.
For observational screening studies that assessed the effect of screening and intervention beyond just looking at diagnostic accuracy, we used the QUADAS‐2 tool developed for studies assessing diagnostic accuracy (Whiting 2011). The tool assesses risk of bias in each of the following four key domains: patient selection, index test, reference standard, and flow and timing. Risk of bias is assessed as to whether the selection of patients could have introduced any bias into the study, whether the conduct or interpretation of the index test could have introduced bias, whether the reference standard, its conduct, or its interpretation could have introduced bias, and whether the patient flow could have introduced bias. We only assessed one study using this tool, the criteria for which can be found in Appendix 4.
There is currently no standardised method for assessing the risk of bias or appraising the quality of modelling studies within the systematic review community. In the rapid review of travel‐related control measures, Burns A 2020 describe the challenge of critically appraising modelling studies by referring to a rapid review of the methodological literature that sought to identify and summarise studies describing criteria for assessing the quality of mathematical modelling studies). This review suggested that an assessment of the quality of a modelling study should capture the aspects of: (i) model structure; (ii) input data; (iii) different dimensions of uncertainty; (iv) transparency; and (v) validation. Based on these findings, Burns A 2020 developed a tool for the assessment of modelling studies which we applied in this review (Appendix 5). The tool comprises 10 questions, each of which can be given a rating of ‘no to minor concerns’; ‘moderate concerns’ or ‘major concerns’. This tool does not combine multiple criteria into a summary score. Therefore, we used this tool in our assessment of modelling studies, including studies that used only modelling as well as experimental studies with a modelling component.
Contacting study authors
In our review protocol, we had specified that we would contact study authors in case of missing information. The overall reporting of studies was reasonable, and it was therefore not necessary to contact study authors.
Data synthesis
Based on the very heterogeneous evidence base identified in the scoping review, we anticipated that meta‐analyses would likely not be possible in most or all cases. We considered the published Synthesis Without Meta‐analysis (SWiM) guidance as a basis for the reporting of results (Campbell 2020a). We summarised and reported the extracted data for each of the four broad intervention categories and the specific interventions contained within them. We used these categories for our synthesis and we present findings in a tabular, narrative or graphical manner. We analysed and presented findings from empirical studies and modelling studies separately. A third review author double‐checked all data presented in the tables, text and graphics. When assessing observational studies which reported adjusted and unadjusted outcomes, we aimed to assess adjusted outcomes as much as possible.
Assessment of heterogeneity and subgroup analyses
In the absence of meta‐analyses, we did not conduct a statistical assessment of heterogeneity, nor did we statistically assess differences between subgroups. We narratively explored the influence of potentially important sources of heterogeneity on the impact of interventions. In modelling studies, we did this by examining multiple scenarios presented using varying key parameters. We focused on heterogeneity in terms of population, intervention, or outcomes, and across contexts. We considered the following sources of heterogeneity.
School type (i.e. primary, secondary), or age group of students, or both.
Class size.
Community transmission at the time at which the intervention was implemented (i.e. impacts of measures are likely to be different in countries or regions according to the disease prevalence or transmission patterns within communities, regions or countries).
Other local or national measures implemented (e.g. workplace closure, travel‐related control measures).
Level of the intervention (i.e. intervention implementation at the macro, school, or individual level).
Intervention trigger (i.e. cause for the initiation of implementation within or outside of the school setting).
Geographical location (i.e. region or country).
Socioeconomic status of target population.
The scoping review findings suggested that it would likely not be possible to undertake most of these subgroup analyses, due to the information rarely being reported.
Assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of evidence for bodies of evidence within four broad intervention categories (Hultcrantz 2017). An initial assessment jointly made by ShK, HL, and LMP was shared with other review authors (TL, ClK, AB, JB) and a joint decision regarding the certainty of evidence ratings was made. The completed GRADE tables for each intervention category can be found in (Table 1; Table 2; Table 3; Table 4).
Summary of findings 1. Summary of findings: measures reducing the opportunity for contacts.
| Reducing opportunity for contacts: reducing the number of students and contacts* | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 13 modelling studies (Baxter 2020; Bershteyn 2020; Burns A 2020; Di Domenico 2020a; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Mauras 2020; Panovska‐Griffiths 2020a; Shelley 2020) | All studies except for one predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the number or proportion of cases. One study predicted mixed effects (Shelley 2020). The variation in the magnitude of effect might be explained by the level of community transmission, susceptibility of individuals to a SARS‐CoV‐2 infection as well as implementation of community‐based interventions. | Very lowa,c,d,f ⨁◯◯◯ |
| Risk of infection | 2 modelling studies (Cohen 2020; España 2020) | Both studies predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the risk of infection. In one study, relative to a scenario with operating schools at full capacity and without face masks, a reduction in students led to a proportional reduction in the risk of infection (España 2020). In another study, reducing the number of students to 50% by introducing alternating attendance schedules led to a predicted risk of infection in students between 0.2% to 3.1% and 0.4% to 4.3% in teachers and staff (Cohen 2020). One study predicted that the lowest risk of infection can be achieved by limiting attendance to primary school students and reducing their cohort size by 50% (risk of infection in teachers: 0.2% to 0.7%; risk of infection in students: 0.1% to 1.0%) (Cohen 2020). The variation in the magnitude of effect might be explained by varying levels of susceptibility of individuals to a SARS‐CoV‐2 infection, age of the students targeted by the intervention as well as the level of community transmission. | Very lowb,c,f ⨁◯◯◯ |
| Reproduction number | 6 modelling studies (Cohen 2020; Keeling 2020; Landeros 2020; Lee 2020; Phillips 2020; Zhang 2020) | All but one study predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the reproduction number. One study predicted no consistent trend across different scenarios of alternating schedules and reduction of students (Cohen 2020). The variation in the magnitude of effect might be explained by the level of community transmission as well as the age of students targeted by the intervention. | Very lowb,c,d,f ⨁◯◯◯ |
| Number or proportion of deaths | 5 modelling studies (Baxter 2020; Germann 2020; Head 2020; Keeling 2020; Panovska‐Griffiths 2020a) | All studies predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the number or proportion of deaths when compared to schools operating without measures in place. In all populations (general population; teachers and staff; students), the number of deaths was reduced by reducing the number of students. The variation in the magnitude of effect might be explained by the level of community transmission, age of students, susceptibility of children to a SARS‐CoV‐2 infection as well as implementation of community‐based interventions. | Very lowb,c,f ⨁◯◯◯ |
| Risk of death | 1 modelling study (España 2020) | One study predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the risk of death in various populations (students, teachers, general population) when compared to operating schools without any measures. If only 50% of all students attend school, the risk of death can be reduced to 3.0% (95% CI 3.0% to 3.0%) in teachers, in family members to 0.4% (95% CI 0.4% to 0.5%) and in the general population to 4.0% (95% CI 4.0% to 5.0%) if countermeasures such as face masks are in place. | Very lowb,c,e,f ⨁◯◯◯ |
| Shift in pandemic development | 5 modelling studies (Alvarez 2020; Germann 2020; Landeros 2020; Mauras 2020; Phillips 2020) | All studies predicted that reducing the number of students and thus reducing the number of contacts between students led to a positive shift in the pandemic development when compared to schools operating without measures in place. In all studies, the reduction in the number of students was predicted to slow the pandemic development, reduce the length of an outbreak or time until the maximum intensive care bed capacity would be achieved. The variation in the magnitude of effect might be explained by the implementation of community‐based interventions. | Very lowb,c,f ⨁◯◯◯ |
| Number or proportion of infected schools | 1 modelling study (Aspinall 2020) | One study predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the number of schools with at least one infected individual when compared to operating schools without any measures. With all students attending, the proportion and number of schools with at least one infected individual on the premises ranged between 4% and 20% (661 to 3310 primary schools); if only a third of all primary school students attending, the risk could be reduced to 1% and 5.5% of primary schools (178 to 924 schools). The variation in the magnitude of effect might be explained by the level of community transmission. | Very lowb,c,e,f ⨁◯◯◯ |
| Risk of transmission to other schools | 1 modelling study (Munday 2020) | One study predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the risk of transmission to another school when compared to operating schools without measures in place. While the risk ranged between 0.42% and 3.6% for 100% attendance, it was the lowest if only certain grades of primary school attended school, with the risk ranging between 0.01% and 0.09%. The variation in the magnitude of effect might be explained by the level of community transmission. | Very lowb,c,e,f ⨁◯◯◯ |
| Outcome category: healthcare utilisation | |||
| Number or proportion of hospitalisations | 2 modelling studies (Germann 2020; Head 2020) | Both studies predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the number or proportion of hospitalisations when compared to operating school without any measures. The variation in the effect might be explained by the level of community transmission, susceptibility of individuals to a SARS‐CoV‐2 infection as well as implementation of community‐based interventions. | Very lowb,c,f ⨁◯◯◯ |
| Number or proportion of cases requiring intensive care | 3 modelling studies (Alvarez 2020; Di Domenico 2020a; Keeling 2020) | All studies predicted that reducing the number of students and thus reducing the number of contacts between students led to a reduction in the number or proportion of cases requiring intensive care when compared to operating school without any measures. The variation in effect might be explained by the level of community transmission, age of students, susceptibility of individuals to a SARS‐CoV‐2 infection as well as implementation of community‐based interventions. | Very lowb,c,f ⨁◯◯◯ |
| Outcome category: societal, economic andecological outcomes | |||
| Number of days spent in school | 3 modelling studies (Cohen 2020; Gill 2020; Phillips 2020) | Three studies assessed the number of days spent in school. Of these, two studies predicted that reducing the number of students and thus reducing the number of contacts between students led by design to a reduction in the number of planned days spent in school (60% to 83% of all school days to be spent at home as shown by one study) when compared to operating schools without measures in place. In one study, the number of days lost to classroom closures varies between 76.0 ± 59.5 SD for a ratio of students to teacher of 8:1 and 1157.7 ± 684.3 SD for a ratio of 30:1. The variation in the magnitude of effect might be explained by the level of community transmission. | Very lowb,c,d,f ⨁◯◯◯ |
| Reducing opportunity for contacts: reducing contacts* | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 3 modelling studies (Cohen 2020; Gill 2020; Head 2020) | All studies predicted that reducing the number of contacts between students led to a reduction in the number or proportion of cases. One study reported a reduction in the cumulative infection rate from between 6.4% and 17.2% for students and between 9.5% and 24.6% for teachers and school staff, depending on the level of community transmission (Cohen 2020). The variation in the magnitude of effect might be explained by the level of community transmission and susceptibility of individuals to a SARS‐CoV‐2 infection. | Very lowb,c,f ⨁◯◯◯ |
| Reproduction number | 3 modelling studies (Cohen 2020; Phillips 2020; Rozhnova 2020) | Two studies predicted that compared to operating schools without reducing the number of contacts, a reduction in the number of contacts between students led to a reduction in the reproduction number. One study graphically predicted that reducing the number of contacts while maintaining the number of students at 100% did not have a large impact on the reduction in the reproduction number (Phillips 2020). The variation in the magnitude of effect might be explained by the susceptibility of individuals to a SARS‐CoV‐2 infection. | Very lowb,c,f ⨁◯◯◯ |
| Shift in pandemic development | 2 modelling studies (Landeros 2020; Phillips 2020) | One study predicted that reducing the number of contacts between students led to a positive shift in the pandemic development (Landeros 2020). Implementing an alternating attendance schedule by creating rotating cohorts with a weekly rotating schedule extends the period of instruction from 10 to 12 weeks to 18 to 22 weeks until reaching the stopping rule on cumulative prevalence of 5%. With regards to the length of an outbreak, one study predicts that an alternating attendance schedule, while maintaining the number of students, performs slightly better with regards to mean and median outbreak lengths than a non‐alternating attendance schedule (Phillips 2020), but probably not in a significant way (results presented graphically). | Very lowb,c,d,f ⨁◯◯◯ |
| Outcome category: healthcare utilisation | |||
| Number or proportion of hospitalisations | 2 modelling studies (Germann 2020; Head 2020) | Two studies predicted that reducing the number of contacts between students led to a reduction in the number and proportion of individuals requiring hospitalisation. The variation in the magnitude of effect might be explained by the susceptibility of individuals to a SARS‐CoV‐2 infection, co‐interventions, the level of community transmission, as well as the age of students. | Very lowb,c,d,f ⨁◯◯◯ |
| Outcome category: societal, economic and ecological outcomes | |||
| Number of days spent in school | 3 modelling studies (Cohen 2020; Gill 2020; Phillips 2020) | Two studies predicted that reducing the number of contacts by implementing an alternating attendance schedule or enforcing that students remain within their classroom led to more days spent in school than when the number of contacts are not reduced (Gill 2020; Phillips 2020). One study predicted no effect: reducing the number of contacts between cohorts alongside other countermeasures (non‐pharmaceutical interventions; screening) predictably leads to an equal percentage of school days spent at home as if no measures would be in place (~5% to 10%) (Cohen 2020). | Very lowb,c,d,f ⨁◯◯◯ |
CI: confidence interval; SARS‐CoV‐2: severe acute respiratory syndrome coronavirus 2; SD: standard deviation.
*We differentiate between measures reducing the number of students and contacts (i.e. reducing the number of students on school premises automatically reduces the number of contacts with or without additional contact‐reducing measures being implemented) and measures reducing contacts (i.e. contacts between students as well as between students and school staff can also be reduced through forming cohorts with all students present on school premises).
aDowngraded ‐2 for risk of bias due to major concerns about the structural assumptions and input parameters in the majority of studies contributing to the outcome. bDowngraded ‐1 for risk of bias due to moderate or major concerns about the structural assumptions and input parameters. cDowngraded ‐1 for indirectness due to moderate or major concerns about the external validation of the model. dDowngraded ‐1 for inconsistency due to mixed or inconsistent effects in the studies contributing to the outcome. eDowngraded ‐1 for imprecision due to only one study contributing to the outcome. fDowngraded ‐1 for imprecision due to moderate or major concerns about the assessment of uncertainty in the studies in the majority of studies contributing to the outcome.
Summary of findings 2. Summary of findings: measures making contacts safer.
| Intervention subcategory: making contacts safer ‐ face masks | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 3 modelling studies (España 2020; Head 2020; Panovska‐Griffiths 2020b) | Three studies look at masks among other measures implemented in the school setting, and reduction in the cases avoided due to the intervention, reporting on outcomes such as (cumulative) number of cases or attack rates. In the studies that allow for drawing conclusions with regard to the effect of masks, wearing masks reduced the number of cases. Studies found that full school reopening with high‐face‐mask adherence/a mandatory mask policy, significantly reduced the increase in community infections due to school reopening (3 times the number of infections), compared to scenarios with low mask adherence/no mandatory policy (España 2020; Panovska‐Griffiths 2020b). This included a reduction from 81.7 times to 3.0 times the number of infections in the community (España 2020), and a reduction from 57% to 46% of those with symptomatic infections needing to be tested in the community under 30% effective coverage of masks (Panovska‐Griffiths 2020b). A further study found a reduction in the excess proportion of infections in the school setting at a moderate level of community transmission with mandatory masks among teachers and staff (1.73, 95% CI 2.32 to 6.29), as well as students (2.51, 95% CI 0.05 to 6.95), compared to reopening with no countermeasures (teachers and staff: 14.83, 95% CI 0.93 to 29.25), students: 14.18, 95% CI 1.63 to 26.77) (Head 2020). Insight from individual studies shows factors which may impact upon the magnitude of effect, such as the initial level of COVID‐19 incidence, as well as the assumed compliance with wearing masks. | Very lowb,c,f ⨁◯◯◯ |
| Reproduction number | 1 modelling study (Sruthi 2020) | One study showed the positive effect of a mask policy on the reproduction number. The study showed that wearing masks in secondary schools in Switzerland led to an estimated reduction in the general population of R by 0.011 (95% CI 0.008 to 0.0127). However, there is no consideration of compliance in the model. | Very lowa,c,e ⨁◯◯◯ |
| Number or proportion of deaths | 2 modelling studies (España 2020; Head 2020) | Two studies examined impact of a mask policy on the number or proportion of deaths as an outcome, finding positive results. Head 2020 found a lower proportion of excess deaths experienced by students (0 (95% CI 0 to 0)) and school staff and teachers (0.44 (95% CI 0 to 0.44)) if schools reopened with mandatory mask wearing, compared to school reopening with no countermeasures (students: 0.01 (95% CI 0 to 0.01); school staff and teachers: 2.97 (95% CI 0 to 47.17)). These findings assumed moderate community transmission. España 2020 focused on the general population, finding that, under a scenario with high capacity and high face‐mask adherence, there would be a decrease in the ratio of the cumulative number of deaths in the overall population of 1.5 (95% CI 1.5 to 1.6). | Very lowb,c,f ⨁◯◯◯ |
| Outcome category: healthcare utilisation | |||
| Number or proportion of hospitalisations | 1 modelling study (Head 2020) | One study looked at the impact of a mask policy on the number or proportion of hospitalisations and found positive results. The study demonstrated that mandatory mask wearing in schools when reopening would lead to reduced hospitalisations among students, staff, household members and community members compared to reopening with no measures in place. The study predicts that mandatory mask wearing in schools when reopening all schools would lead to reduced hospitalisations among students, staff, household members and community members. For teachers/staff, the excess rate of hospitalisations per 10,000 of the subpopulation would be reduced to 4.2 (95% CI ‐47.39 to 48.09) from 40.5 (95% CI ‐46.95 to 146.64). For students this decreases to 0.07 (95% CI 0.00 to 0.01) from 0.08 (95% CI 0.00 to 0.08). The size of this effect is moderated by level of community transmission, type of school and whether children are considered half or equally susceptible as adults. In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Very lowb,c,e ⨁◯◯◯ |
| Intervention subcategory: making contacts safer ‐ cleaning | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Reproduction number | 1 modelling study (Kraay 2020) | One study assessed the impact of an enhanced cleaning policy on the reproductive number and showed positive results. The study found that compared to eight‐hourly and four‐hourly surface cleaning and disinfection, hourly cleaning and disinfection alone could bring the fomite R below 1 in some office settings, particularly combined with reduced shedding, but would be inadequate in schools. This study did not take into account direct transmission through droplet spray, aerosols and hand‐to‐hand contact. | Very lowb,c,e ⨁◯◯◯ |
| Intervention subcategory: making contacts safer ‐ handwashing | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Reproduction number |
1 modelling study (Kraay 2020) | One study assessed the impact of handwashing on the reproduction number and suggested no impact. While results are only presented in a graphical way, it predicted that handwashing (hourly with 100% effectiveness) compared to no handwashing did not make a difference with regards to the projected reproduction number from fomite transmission. | Very lowb,c,e ⨁◯◯◯ |
| Outcome category: other health outcomes | |||
| Physical health | 1 observational/experimental study (Simonsen 2020) | One study found that 6.5% (2000 of 30,907; 95% CI 6.2 to 6.8) of children had hand eczema prior to school closures, 14.1% (4363 of 30,907; 95% CI 13.7 to 14.5) of students had hand eczema before reopening of schools on 15 April 2020. This prevalence increased to 50.5% (15,595 of 30,907; 95% CI 49.9 to 51.0) after the children returned to school and the strict hand hygiene regimen (handwashing for 45 to 60 seconds every 2 hours; after arrival, before and after meals, after toilet visits, after coughing or sneezing or whenever hands were visibly dirty) was implemented, which was a statistically significant increase of 36.3% (P < 0001). | Lowe ⨁⨁◯◯ |
| Intervention subcategory: making contacts safer ‐ modification of activities | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Reproduction number | 1 modelling study (Lazebnik 2020) | One study assessed the impact of changing the length of the school day and found that keeping schools open with longer school hours (8 to 9 hours) each day would reduce R by 0.83 compared to a policy in which children go to school every other day for five hours. | Very lowa,c,e ⨁◯◯◯ |
| Intervention subcategory: making contacts safer ‐ ventilation | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Concentration of aerosol particles containing RNA virus in the room and inhaled dose of RNA virus for a susceptible person | 1 modelling study (Curtius 2020) | One study assessed the effect of four air purifiers equipped with HEPA filters in a high school classroom in Germany with an infected person in the room with regards to the inhaled dose of particles containing RNA virus. This dose is reduced by a factor of six. The density of people in the room can be considered an effect modifier. | Very lowa,c,e ⨁◯◯◯ |
| Intervention subcategory: making contacts safer ‐ combined measures to make contacts safer | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 4 modelling studies (Cohen 2020; Germann 2020; Gill 2020; Monod 2020) | All studies looked at the impact of combined measures to make contacts safer on the number or proportion of cases and found positive results overall. Those which reported on community level transmission found a reduction in total number of infections, although specific figures were not reported (Gill 2020), and reduction in the number of cases from 59.7 million when schools reopened with no countermeasures to 2.3 million and 2.0 million in 40% partial online learning scenarios, with 'ideal social distancing' (assumed 50% reduction in contacts due to face masks, hygiene, and distancing measures) (Germann 2020). Those which reported on school level outcomes found that implementing a variety of infection control measures led to a reduction in the cumulative COVID‐19 infection rate among students, teachers, and staff over four‐fold (Cohen 2020), and a reduction in total number of infections, although specific figures were not reported (Gill 2020). | Very lowb,c,f ⨁◯◯◯ |
| Reproduction number | 2 modelling studies (Cohen 2020; Phillips 2020) | Two studies examined effective reproduction number as an outcome, with both studies finding a positive effect. Both studies presented results graphically, making it difficult to determine effect sizes. One study showed that all modelled scenarios with combined measures to make contacts safer would reduce the effective reproduction number to < 1, compared with full school reopening with full attendance and no measures in place (Cohen 2020). The other study compared high with low‐transmission settings in primary schools and suggested that the effective reproduction number is consistently lower in a low‐transmission setting (Phillips 2020). | Very lowa,c,f ⨁◯◯◯ |
| Number or proportion of deaths | 2 modelling studies (Germann 2020; Monod 2020) | Two modelling studies assessed combined measures to make contacts safer on the number or proportion of deaths as an outcome, finding mixed results, one positive (Germann 2020), and one unclear result (Monod 2020). One study found that when fewer workplaces were open, all four 40% partial online learning scenarios, with alternating days or weeks of attendance were found to reduce deaths. Although a larger decrease to 25,474 and 27,874 was observed in scenarios where a 50% reduction in contacts due to mask wearing or reduced social distancing with minimal mask use was assumed within the model, compared to 230,451 deaths during full school reopening with no countermeasures (Germann 2020). However, the other study estimated a 12.6% (95% CI 7.4% to 22.7%) increase in deaths among children and the general population as a result of schools reopening with countermeasures, compared to keeping schools closed (Monod 2020). | Very lowb,c,f ⨁◯◯◯ |
| Shift in pandemic development | 1 modelling study (Germann 2020) | One study assessing combined measures to make contacts safer compared high with low‐transmission settings in primary schools. With results presented in a graphical way, they implied that the mean duration of the outbreak is shorter in low‐transmission than high‐transmission settings in all student to teacher ratios except for the 30:1 ratio. | Very lowb,c,e,f ⨁◯◯◯ |
| Outcome category: healthcare utilisation | |||
| Number or proportion of hospitalisations | 1 modelling study (Germann 2020) | One study looked at the impact of combined measures to make contacts safer on the number or proportion of hospitalisations, and found that when fewer workplaces were open, all partial online learning scenarios, with ideal social distancing (defined as a 50% reduction in contacts due to physical distancing, hygiene and masks), were found to avert between 543,977 and 1,708,197 hospitalisations. Moreover, for these scenarios, hospitalised cases during the peak four weeks ranged from 59,056 to 354,878, compared to a baseline scenario of 685,747 with schools reopening with full attendance and no measures in place. | Very lowb,c,e ⨁◯◯◯ |
| Outcome category: societal, economic and ecological outcomes | |||
| Number of days spent in school | 2 modelling studies (Gill 2020; Phillips 2020) | Two studies examined the outcome of number of days spent in school. One study found that at very low community infection rates (10 reported infections per 100,000 population over the last seven days), most students can expect to attend nearly every day even in schools operating full‐time, as long as schools implement multiple interventions. It is not possible to determine effect size due to lack of reporting (Gill 2020). The other study compared high with low transmission settings in primary schools. Except for a ratio of 30:1, the number of student days lost to closure was consistently higher in low transmission settings. The predicted number of student days lost was 76.0 ± 59.5 for a ratio of 8:1, 270.2 ± 195.6 for a ratio of 15:1 and 1157.7 ± 684.3 for a ratio of 30:1 in a low transmission setting while it was 111.2 ± 72.8; 389.9 ± 202.0 and 1093.9 ± 396.1 for a high transmission setting (Phillips 2020). | Very lowa,c ⨁◯◯◯ |
CI: confidence interval.
aDowngraded ‐2 for risk of bias due to major concerns about the structural assumptions and input parameters in the majority of studies contributing to the outcome. bDowngraded ‐1 for risk of bias due to moderate or major concerns about the structural assumptions and input parameters. cDowngraded ‐1 for indirectness due to moderate or major concerns about the external validation of the model. dDowngraded ‐1 for inconsistency due to mixed or inconsistent effects in the studies contributing to the outcome. eDowngraded ‐1 for imprecision due to only one study contributing to the outcome. fDowngraded ‐1 for imprecision due to moderate or major concerns about the assessment of uncertainty in the studies in the majority of studies contributing to the outcome.
Summary of findings 3. Summary of findings: surveillance and response measures.
| Intervention subcategory: surveillance and response measures ‐ mass testing and isolation | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 7 modelling studies (Cohen 2020; Di Domenico 2020a; Head 2020; Lyng 2020; Panovska‐Griffiths 2020a; Tupper 2020; Williams 2020) | The seven studies that looked at the impact of mass testing and isolation interventions on the number or proportion of cases all found positive results. Cohen 2020 found that measures that limit transmission and detect, trace, and quarantine cases within schools could lead to reductions in the cumulative COVID‐19 infection rate among students, teachers, and staff by over 14‐fold. However, these measures were implemented alongside classroom cohorting, face masks, physical distancing, and handwashing protocols in schools, so it is not possible to comment on the impact of these measures alone. Head 2020 suggested that although testing and isolation strategies could lead to reductions in transmission, their effectiveness on their own was low, and when combined with strict social‐distancing measures, and a reduction in community transmission, they could be more effective. | Very lowb,c,f ⨁◯◯◯ |
| Number of cases detected | 1 observational/experimental study (Hoehl 2020) | One observational study looked at the impact of mass testing strategies on the number of cases detected due to the intervention. The main goal of the study was to evaluate the practical application of a self‐performed, high‐frequency antigen test in a school setting and 10,768 of these tests (99.37%) were recorded to have been valid and 113 negative, 47 (0.43%) were recorded as invalid and 21 (0.19%) as positive (either true or false). The study found that 0.15% of all antigen tests (16 tests) gave false‐positive results. | Very lowa,c,e ⨁◯◯◯ |
| Reproduction number | 1 modelling study (Panovska‐Griffiths 2020a) | One study looked at two different testing strategies and found that test–trace–isolate strategies would need to test a sufficiently large proportion of the population with COVID‐19 symptomatic infection and trace their contacts with sufficiently large coverage, for R to diminish below 1. | Very lowa,c,e ⨁◯◯◯ |
| Number or proportion of deaths | 2 modelling studies (Head 2020; Panovska‐Griffiths 2020a) | Two studies assessed the impact of testing and isolation strategies on the number and proportion of deaths. They showed positive results overall. One study only showed results in a graphical way and suggested that more intense testing and isolation measures would lead to fewer deaths than less intense measures (Panovska‐Griffiths 2020a). The other study found that, under a testing strategy, the excess proportion of deaths in teachers would be 8.12 (95% CI 0.00 to 47.85), compared to 0 for students and 0.5 (95% CI ‐2.72 to 3.68) in the community (Head 2020). The effect sizes are moderated by the model parameters such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. | Very lowb,c,f ⨁◯◯◯ |
| Shift in pandemic development | 4 modelling studies (Landeros 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Williams 2020) | The four studies that assessed the impact of mass testing and isolation strategies on the timing and progression of the epidemic found that testing and isolation could slow or prevent a second wave of the epidemic. The studies suggest that the timing of the epidemic depends on the degree to which testing and isolation strategies are being implemented and the combination of testing and tracing. | Very lowb,c,f ⨁◯◯◯ |
| Outcome category: healthcare utilisation | |||
| Number or proportion of hospitalisations | 1 modelling study (Head 2020) | One study found that reopening schools with a weekly or monthly testing strategy for teachers and students would lead to a higher number of hospitalisations compared to reopening under strategies to reduce contacts. The excess proportion of hospitalisations in teachers under a testing strategy would be 162.47 (95% CI 0.00 to 588.24), compared to students 0.58 (95% CI 0.00 to 15.27), and the community 3.68 (95% CI ‐7.27 to 15.54). The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. | Very lowa,c,e ⨁◯◯◯ |
| Outcome category: societal, economic and ecological outcomes | |||
| Numbers of days spent in school | 1 modelling study (Gill 2020) | One study found that policies that close the school when infections are detected substantially reduce the total number of days that students can attend in person. These effects are larger in schools operating full‐time than in schools using hybrid approaches. In secondary schools where students are attending daily and the community infection rate is at a moderate level, closing the school for 14 days for each detected infection would be highly disruptive. Even in the absence of a school closure policy, quarantines of the classmates and bus mates of infected students are likely to reduce in‐person attendance for the typical student. | Very lowa,c,e ⨁◯◯◯ |
| Resource costs | 3 modelling studies (Campbell 2020b; Lyng 2020; Williams 2020) | Three studies looked at the cost of testing interventions and showed mixed results. One study used health economic modelling to look at the human resource costs of testing strategies. The study found that testing students and employees in primary and secondary schools over 1.5 months would cost CAD 816.0 million, compared to no intervention. Another study identified one high‐performing strategy of community‐based testing with a per person per day cost as low as USD 1.32. | Very lowb,c,f ⨁◯◯◯ |
| Intervention subcategory: symptom‐based screening and isolation | |||
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 2 modelling studies (Bershteyn 2020; Burns A 2020) | Two studies found that policies that screen and isolate suspected cases can, overall, decrease the attack rate. The most effective testing and isolation strategies used a combination of early testing together with symptom screening and isolation of symptomatic cases. These strategies were often implemented alongside other transmission mitigation measures, such as physical distancing and cohorting, so it is not possible to assess the impact of symptom screening and quarantine measures alone. | Very lowb,c,f ⨁◯◯◯ |
| Shift in pandemic development | 1 modelling study (Burns A 2020) | One study found that implementing a policy of two days of home isolation following the last episode of fever, predicted a reduction in all outcome categories would reduce the peak number of infected people from 148 (interquartile range (IQR) 82 to 213) to 124 (IQR 58 to 184)). The interval between the first and last day with at least two cases would increase to 145 (IQR 127 to 157) from 139 (IQR 120 to 154). The effects varied according to the rate of detecting fever. | Very lowa,c,e ⨁◯◯◯ |
CAD: Canadian Dollars; CI: confidence interval; IQR: interquartile range; USD: US Dollars.
aDowngraded ‐2 for risk of bias due to major concerns about the structural assumptions and input parameters in the majority of studies contributing to the outcome. bDowngraded ‐1 for risk of bias due to moderate or major concerns about the structural assumptions and input parameters. cDowngraded ‐1 for indirectness due to moderate or major concerns about the external validation of the model. dDowngraded ‐1 for inconsistency due to mixed or inconsistent effects in the studies contributing to the outcome. eDowngraded ‐1 for imprecision due to only one study contributing to the outcome. fDowngraded ‐1 for imprecision due to moderate or major concerns about the assessment of uncertainty in the studies in the majority of studies contributing to the outcome.
Summary of findings 4. Summary of findings: multicomponent measures.
| Outcome | Number of studies | Summary of findings | Certainty of evidence |
| Outcome category: transmission‐related outcomes | |||
| Number or proportion of cases | 2 observational/experimental studies (Isphording 2020; Vlachos 2020) | These two studies showed mixed results on the effectiveness of multicomponent interventions to make contacts safer on the number or proportion of cases. One study found that the intervention reduced cumulative infection rate by 0.55 or 27% of a standard deviation (Isphording 2020), while the other found that exposure to open rather than closed schools resulted in a small to moderate increase in the number of infections among parents and teachers, and their partners (Vlachos 2020). | Lowa,b ⨁⨁◯◯ |
| Number or proportion of cases | 1 modelling study (Naimark 2020) | One study compared a multicomponent intervention consisting of: i) reducing the number of students; ii) reducing the number of contacts; iii) universal masking; iv) alternating attendance schedules in high schools; and v) symptom‐based isolation, to full school closures. The study found that there was an increase in the predicted number of infections when reopening with measures compared to a full school closure scenario. | Very lowc,d,e ⨁◯◯◯ |
aDowngraded ‐1 for risk of bias due to ROBINS‐I rating being moderate. bDowngraded ‐1 for inconsistency due to inconsistent effects in studies contributing to the outcome. cDowngraded ‐1 for risk of bias due to major concerns about the structural assumptions and input parameters. dDowngraded ‐1 for inconsistency due to only one study contributing to the outcome. eDowngraded ‐1 for imprecision due to only one study contributing to the outcome.
The certainty of evidence is defined in GRADE as the extent to which one can be confident that the true effect of an intervention lies on one side of a specified threshold, or within a chosen range (Hultcrantz 2017). In this rapid review, we considered 'difference from the null' as the most relevant threshold, assuming that even small effect sizes may be relevant for school measures applied to large populations.
The certainty of evidence rating in GRADE yields four possible levels of evidence: high certainty (i.e. the estimated effect lies close to the true effect), moderate certainty (i.e. the estimated effect is probably close to the true effect), low certainty (i.e. the estimated effect might substantially differ from the true effect), and very low certainty (i.e. the estimated effect is probably substantially different from the true effect) (Hultcrantz 2017).
We rated bodies of evidence from quasi‐experimental/observational and modelling studies separately.
In GRADE, evidence from RCTs enters the rating as high certainty, as does evidence from observational studies whose risk of bias has been assessed using ROBINS‐I (Sterne 2016). Five domains are then used to further downgrade evidence, including study limitations, inconsistency, indirectness, imprecision, and publication bias, and three domains are used to upgrade evidence, including plausible confounding, large estimates of effect, and presence of a dose‐response relationship. The ROBINS‐I judgements for empirical studies informed the GRADE criterion on study limitations.
To apply GRADE in the specific context of modelling studies, we used the recent guidance developed by the GRADE Working Group (Brozek 2021). Evidence from modelling studies also entered the assessment as high certainty, and all the GRADE domains described above were then used to assess certainty of the model outputs. The quality assessment of the studies using the bespoke tool informed our GRADE assessment of modelling studies. With regards to the study limitations domain of GRADE, the quality assessment ratings for the model structure and input data were used to downgrade bodies of evidence if studies raised concerns in either of these aspects. This was partially operationalised by considering major concerns in input data or structure as a definite indicator for downgrading. If the decision about downgrading once or twice or not downgrading at all was on the edge, we used the external validation category as a tiebreaker. To assess the imprecision in the bodies of evidence from modelling studies, we rated the analyses conducted to assess the variability and uncertainty of the outcomes and critically examined these against the aspects of uncertainty that should have been considered in the models. Where only one study contributed to the body of evidence, we downgraded the evidence for imprecision. A modelling study might for example report tight confidence intervals, which arise from an incomplete consideration of all the important underlying sources of uncertainty. To assess indirectness, we focused on the external validity of the model as an important indicator for a credible model. We assessed inconsistency based on a consistent or inconsistent direction of effect across studies for any given outcome category.
Results
Description of studies
Results of the search
We identified 2687 unique records from database searches and identified 4043 additional records from snowball searches. Of these, 152 studies entered full‐text screening. After a comprehensive screening process, detailed in the PRISMA flow diagram (Figure 4), we included 38 studies in the rapid review, comprising 31 preprints, four peer‐reviewed studies (Campbell 2020b; Lee 2020; Panovska‐Griffiths 2020a; Simonsen 2020), and three reports (Alvarez 2020; Gill 2020; Isphording 2020). Of these preprints, 16 studies have been published after the analysis had been completed. A comparison of the differences between the preprint and the peer‐reviewed publication can be found in Appendix 6. While we do not include a list of ongoing studies in this review, this is available upon request by contacting the study authors. We excluded 114 studies from this review. We have provided a list of 20 of these studies which we felt would be of most interest/relevance to readers and have provided reasons for exclusion at the full‐text level in Excluded studies. Broad reasons for exclusions (i.e. population, disease, outcome) are provided in Figure 4.
4.
PRISMA flow chart
Based on our findings, we adapted the a priori logic model that informed the development of the rapid review protocol (Krishnaratne 2021).
Given the delay between the initial search and the publication of this review, we conducted a top‐up search on the Cochrane Covid‐19 Study Register in August 2021 in order to identify studies published since the original search. The goal of this search was to identify eligible studies, and not to conduct any data extraction or quality assessment. The search was conducted exactly as it had been run in December 2020 but with search dates from 9 December 2020 to 5 August 2021. The search identified 1379 unique records. Of these, 118 studies entered full‐text screening. After a comprehensive screening process, we added 16 novel study reports to Studies awaiting classification. A detailed PRISMA flow diagram documenting this top‐up search can be found in Figure 5.
5.
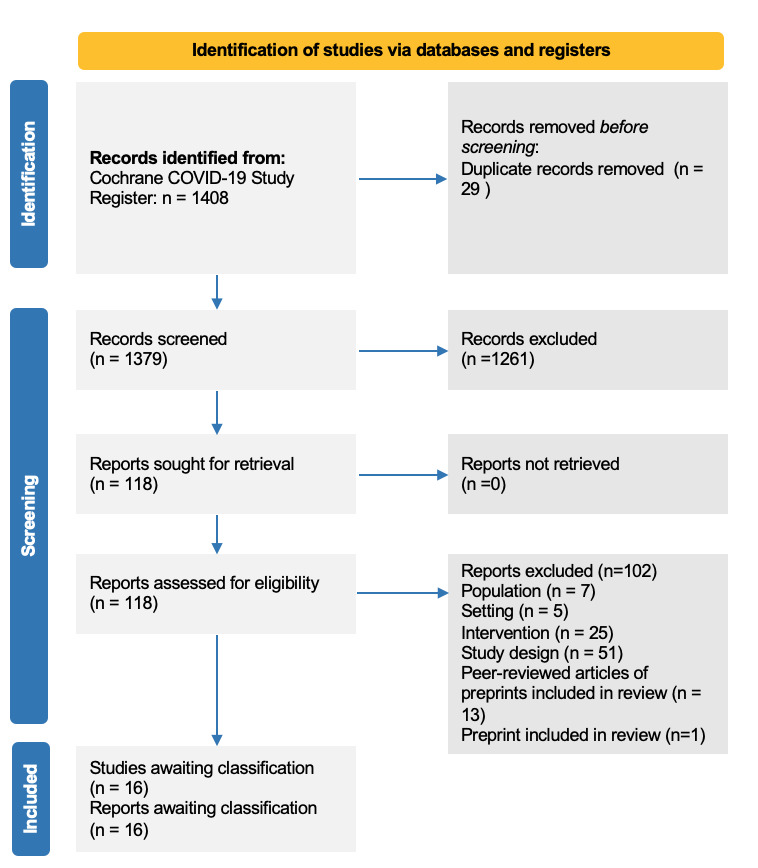
PRISMA flow chart: top‐up search
Included studies
The characteristics of each of the included studies are described in the characteristics of included studies table (Table 6). In the following, summary information is provided according to their setting, population, intervention, comparison, outcome(s), and study design. The evidence gap map summarises the distribution of studies related to the study types, intervention and outcome categories (Figure 3).
2. Characteristics of included studies .
| Study ID | Study design | Population (populations; school type; age group) | Country implementing the measure | School measure | Comparison | Outcome(s) | Notes ‐ funding source as reported in the study |
| Alvarez 2020 | Compartmental SEIR model | Population in which intervention is implemented: general school population; all school types Population in which outcome is assessed: general population; unspecified school types; unspecified age group | Chile | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students and contacts: 100%, 75%, 50% and 25% *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: shift in pandemic development Healthcare utilisation outcome: number or proportion of cases requiring intensive care Follow‐up: 1 month (May to Jun 2020) | Not reported |
| Aspinall 2020 | Bayesian Belief Network (stochastic uncertainty modelling tool ‐Unitet) | Population in which intervention is implemented: general school population; primary schools; age groups: 20 to 60 years (teachers, school staff); students Population in which outcome is assessed: general school population; primary schools; age groups: 20 to 60 years (teachers, school staff); student | UK | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students and contacts (35% to 41%/49% capacity; phased reopening for specific grades) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: number or proportion of infected schools Follow‐up: unclear | The study was part of the RAMP initiative of the Royal Society. |
| Baxter 2020 | Agent‐based modelling study | Population in which intervention is implemented: general school population; kindergarten, primary school and K‐12; unspecified age group (cut‐off for younger children at 10 years) Population in which outcome is assessed: general population | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students in school (phased reopening of primary schools; 50% capacity) *Reduction of contacts: alternating attendance schedule (daily) | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths Follow‐up: ~5 months (Jul to Nov 2020) | Supported by the William W George and by the Virginia C and Joseph C Mello endowments at Georgia Tech. This research was supported in part by NSF grant MRI 1828187 and research cyberinfrastructure resources and services provided by the Partnership for an Advanced Computing Environment (PACE) at the Georgia Institute of Technology. |
| Bershteyn 2020 | Simulation model | Population in which intervention is implemented: general school population; Kindergarten, primary school and K‐12; unspecified age group Population in which outcome is assessed: student population; unspecified school type; unspecified age group | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students in school (50% capacity in schools) *Reduction of number of students in class (9 versus 13 students per class) *Reduction of contacts: alternating attendance schedule (daily, weekly) Surveillance and response measures: symptom‐based screening and quarantine measures | Least intense measure | Transmission‐related outcome: number or proportion of cases Follow‐up: not specified | Not reported |
| Burns A 2020 | Determinstic SEIR modification | Population in which intervention is implemented: general school population; unspecified school type; unspecified age group Population in which outcome is assessed: general school population; unspecified school types; unspecified age group | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: alternating attendance schedule Surveillance and response measures: symptom‐based screening and quarantine measures | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; shift in pandemic development Follow‐up: 8 months (Jan to Aug 2020) | One author was sponsored by US NIH grant R01GM121600. |
| Campbell 2020b | Health economic model | Population in which intervention is implemented: general school population; primary and secondary schools; unspecified school types; unspecified age group Population in which outcome is assessed: general school population; unspecified school types; unspecified age group | Canada | Surveillance and response measures: mass testing and isolation | Least intense measure | Societal, economic and ecological outcome: resources Follow‐up: 42 days (1 complete round of testing) | Directly funded by an operating grant (ECRF‐R1‐30) from the McGill Interdisciplinary Initiative in Infection and Immunity (MI4), a philanthropic scientific‐granting organisation with peer‐reviewed competition; Dick Menzies was the Principal Investigator and Jonathon Campbell the co‐Principal Investigator. The grant also supports the salaries of Aashna Uppal and Mercedes Yanes‐Lane. Jonathon Campbell (Award #258907, Award #287869) and Stephanie Law (Award #258467) are funded by a postdoctoral fellowship from the Fonds de Recherche du Québec—Santé. Nicholas Winters (Award #284837) is funded by a doctoral fellowship from the Fonds de Recherche du Québec, Santé. W Alton Russell is funded by a Stanford Interdisciplinary Graduate Fellowship. Mayara Bastos, Federica Fregonese, Nicholas Winters, Jonathon Campbell and Olivia Oxlade are funded through a Canadian Institutes of Health Research grant (#FRD143350). Giorgia Sulis is funded by a Richard H Tomlinson Doctoral Fellowship. |
| Cohen 2020 | Agent‐based model (Covasim) | Population in which intervention is implemented: general school population; primary, middle, and high schools; students of 5 to 18 years old Population in which outcome is assessed: general population; unspecified age group | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: alternating attendance schedule Making contacts safer: combined measures to make contacts safer Surveillance and response measures: mass testing and isolation | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; reproduction number; risk of infection Societal, economic and ecological outcome: numbers of days spent in school Follow‐up: 3 months (Sep to Dec 2020) | Not reported |
| Curtius 2020 | Experimental study with modelling component | Population in which intervention is implemented: general school population; high school; unspecified age group (note: typical high school students in Germany are 10 to 19 years) Population in which outcome is assessed: general school population; high school; unspecified age group (note: typical high school students in Germany are 10 to 19 years) | Germany | Making contacts safer: ventilation | Full opening of schools with no measures in place | Transmission‐related outcomes: other (inhaled dose) Follow‐up: 2 hours | Conducted without external financial support |
| Di Domenico 2020a | Stochastic discrete age‐structured epidemic model | Population in which intervention is implemented: general school population; primary schools, middle schools, high schools; unspecified age group Population in which outcome is assessed: general population; unspecified age group | France | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (75%, 50%, 25% capacity) *Reduction of contacts: implicit Surveillance and response measures: mass testing and isolation | Full opening of schools with no measures in place | Transmission‐related outcome: number or proportion of cases Healthcare utilisation outcome: number or proportion of cases requiring intensive care Follow‐up: 2 months (May to Jun 2020) | Partially funded by: ANR projects SPHINX (ANR‐17‐CE36‐0008‐05) and DATAREDUX (ANR‐19‐CE46‐0008‐03); EU H2020 grants RECOVER (H2020‐101003589) and MOOD (H2020‐874850); REACTing COVID‐19 modelling grant |
| España 2020 | Meta‐population model *based on FRED | Population in which intervention is implemented: school students, staff and parents; elementary, middle and high; 5 to 18 years Population in which outcome is assessed: schools and general population; elementary, middle and high; all ages | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (75%, 50% capacity) *Reduction of contacts: implicit Making contacts safer: face masks | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths; risk of infection; risk of death Follow‐up: 4 months (Aug to Dec 2020) | Supported by a NSF RAPID grant (DEB 2027718), an Arthur J Schmitt 313 Fellowship and Eck Institute for Global Health Fellowship, and a Richard and Peggy 314 Notabaert Premier Fellowship |
| Germann 2020 | Agent‐based community simulation | Population in which intervention is implemented: students, teachers and staff; elementary, middle and high schools; 5 to 18 years Population in which outcome is assessed: general population | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (80% capacity) * Reduction of contacts: alternating attendance schedule (weekly, 2 days) Making contacts safer: combined measures to make contacts safer *Face masks *Hand‐hygiene policy *Other 'distancing measures' | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths; shift in pandemic development Healthcare utilisation outcome: number or proportion of hospitalisations Follow‐up: 8 months | Sponsored by the United States Centers for Disease Control and Prevention. Los Alamos National Laboratory, an affirmative action/equal opportunity employer, is operated by Triad National Security, LLC, for the National Nuclear Security Administration of the United States Department of Energy under contract # 19FED1916814CKC. Approved for public release: LA‐UR‐20‐27982 |
| Gill 2020 | Agent‐based model | Population in which intervention is implemented: students, teachers and school staff; primary and secondary schools; 5 to 18 years Population in which outcome is assessed: students, teachers and school staff; elementary, middle and high school population | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: alternating attendance schedule (1 to 4 days per week) Making contacts safer: combined measures to make contacts safer *Face masks in school and on school bus *Lunch is eaten in classroom *Elementary students remain with the same class all day, while older students take six classes during the day Surveillance and response measures: mass testing and isolation *Testing and quarantine | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcome: number or proportion of cases Societal, economic and ecological outcome: numbers of days spent in school Follow‐up: not specified | Not reported |
| Head 2020 | Meta‐population model | Population in which intervention is implemented: students, staff and teachers; elementary, middle and high schools; 5 to 18 years Population in which outcome is assessed: students, staff and teachers; household members; community members; elementary, middle and high schools; all age groups | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity in class (high school: 10 students; 20 students in elementary schools)) *Reduction of contacts: alternating attendance schedule Making contacts safer: face masks Surveillance and response measures: mass testing and isolation | Full opening of schools with no measures in place Single intervention component Least intense measure |
Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths Healthcare utilisation outcome: number or proportion of hospitalisations Follow‐up: 12 months (Jan to Dec 2020) | JVR, JRH, QC, PAC, SP, AKH, CMH, and KC were supported in part by National Science Foundation grant no. 2032210, National Institutes of Health grants nos. R01AI125842, R01TW010286 and R01AI148336, and by the University of California Multicampus Research Programs and Initiatives award # 17‐446315. JAL received support from the Berkeley Population Center (grant number P2CHD073964 from the National Institute of Child Health & Human Development, National Institutes of Health). |
| Hoehl 2020 | Observational test accuracy study | Unspecified | Germany | Surveillance and response measures: mass testing and isolation | Least intense measure | Transmission‐related outcome: number of cases detected due to measure Follow‐up: 7 weeks | The study was commissioned and funded by the Hessian Ministry of Education and the Hessian Ministry of Integration and Social Affairs. |
| Isphording 2020 | Quasi‐experimental study | Population in which intervention is implemented: students and teachers; primary and secondary schools; 6 to 18 years Population in which outcome is assessed: general population; age groups: 0 to 14, 15 to 34 and 35 to 59, 60 to 79, 80+ years | Germany | Multicomponent measures *Reduction of contacts: alternating attendance schedule; staggered arrival and departure *Face masks *Testing and quarantine | School closures | Transmission‐related outcome: number or proportion of cases Follow‐up: 3 Aug to 14 Sep 2020 | Discussion paper published by the IZA Institute of Labor Economics (an independent economic research institute that conducts research in labor economics and offers evidence‐based policy advice on labor market issues). Supported by the Deutsche Post Foundation |
| Jones 2020 | Poisson regression model | Population in which intervention is implemented: students and staff at primary, middle and high school Population in which outcome is assessed: students and staff at primary, middle and high school; all age groups | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (55% capacity) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: number or proportion of cases Follow‐up: ~3 months (Aug to Oct 2020) | No funding was secured for this study. |
| Kaiser 2020 | Network model: simulating the transmission of COVID‐19 in classrooms | Population in which intervention is implemented: general school population; all school types; contact data from 14 to 15 year‐olds Population in which outcome is assessed: general school population; all school types; all age groups | UK, Germany, the Netherlands, Sweden | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: alternating attendance schedule | Least intense measure | Transmission‐related outcome: number or proportion of cases Follow‐up: 7 weeks | Supported by the state of Baden‐Württemberg through bwHPC and the German Research Foundation (DFG) through grant INST 35/1134‐1 FUGG. CILS4EU research project funded in the NORFACE ERA NET Plus Migration in Europe‐programme |
| Keeling 2020 | Complex SEIR‐based ordinary differential equation model | Population in which intervention is implemented: general school population; all school types; 0 to 19 year olds Population in which outcome is assessed: general population; unspecified school types; unspecified age group | UK | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths; reproduction number Healthcare utilisation outcome: number or proportion of cases requiring intensive care Follow‐up: 3 weeks (Jun 2020) | This work was funded by the Engineering and Physical Sciences Research Council through the 423 MathSys CDT (grant number EP/S022244/1) and by the Medical Research Council through the 424 COVID‐19 Rapid Response Rolling Call (grant number MR/V009761/1). |
| Kraay 2020 | SIR‐based modelling study | Population in which intervention is implemented: school staff (cleaning); unspecified school types; unspecified age group Population in which outcome is assessed: general population; unspecified school types; unspecified age group | USA | Making contacts safer: cleaning Making contacts safer: handwashing | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcome: reproduction number Follow‐up: not specified | Not reported |
| Landeros 2020 | SEIR‐based ordinary differential equation model | Population in which intervention is implemented: general school population; K‐12; K‐12 age (5 to 18 years) Population in which outcome is assessed: general school population; K‐12; K‐12 age (5 to 18 years) | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% and 33% capacity) *Reduction of contacts: alternating attendance (parallel and rotating cohorts) Making contacts safer: combined measures to make contacts safer *Masks *Desk shields *Frequent surface cleaning *Outdoor instruction Surveillance and response measures: mass testing and isolation | Full opening of schools with no measures in place | Transmission‐related outcomes: reproduction number; shift in pandemic development Follow‐up: 6 months | KLL and JSS are supported by the National Institute of General Medical Sciences of the National Institutes of Health under award number R01GM053275. MES is supported by the Susan G Komen Career Catalyst Award CCR16380478. JX is supported by the National Science Foundation under grant number DMS‐2030355. |
| Lazebnik 2020 | Hybrid model: SIRD type temporal dynamics and spatial dynamics for home, school, workplace (Additional compartments: age classes children (< 13 years) and adults) | Population in which intervention is implemented: general school population; not specified; average age 13 years Population in which outcome is assessed: general population; unspecified school types; unspecified age group | Israel | Making contacts safer: modification of activities | Least intense measure | Transmission‐related outcome: reproduction number Follow‐up: two weeks | No external funding was received. |
| Lee 2020 | Age‐stratified estimation for R0 based on assumed SIR‐model | Population in which intervention is implemented: general school population; not specified; 0 to 14 years Population in which outcome is assessed: general population; unspecified school types; unspecified age group | China | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (33% capacity in high schools) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: reproduction number Follow‐up: not specified | None |
| Lyng 2020 | SIR model analysing different test/suveillance strategies | Population in which intervention is implemented: general school population; unspecified school types; unspecified age group Population in which outcome is assessed: general population; unspecified school types; unspecified age group | USA | Surveillance and response measures: mass testing and isolation | Least intense measure | Transmission‐related outcome: number or proportion of cases Societal, economic and ecological outcome: resources Follow‐up: not specified | Not reported |
| Mauras 2020 | Agent‐based SEIR with contact networks | Population in which intervention is implemented: general school population; primary and high school; unspecified age group Population in which outcome is assessed: general population; unspecified school types; unspecified age group | France | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; shift in pandemic development Follow‐up: not specified | LO received research funding from Pfizer (through her research unit) on research related to meningococcal epidemiology and antimicrobial resistance. |
| Monod 2020 | Bayesian model for transmission dynamics in the USA | Population in which intervention is implemented: school students and staff; kindergarten and elementary schools; 0 to 11 years Population in which outcome is assessed: students; kindergarten and elementary schools; 0 to 11 years | USA | Making contacts safer: combined measures to make contacts safer *Masks *Other NPIs | Full opening of schools with no measures in place | Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths Follow‐up: 90 days | This study was supported by the Imperial College COVID‐19 Response Fund, the Imperial College Research Computing Service DOI:10.14469/hpc/2232, the Bill & Melinda Gates Foundation, and the EPSRC through the EPSRC Centre for Doctoral Training in Modern Statistics and Statistical Machine Learning at Imperial and Oxford, the UK Medical Research Council under a concordat with the UK Department for International Development, the NIHR Health Protection Research Unit in Modelling Methodology and Community Jameel. |
| Munday 2020 | Network model describing transmission between schools | Population in which intervention is implemented: general school population; school type; 4 to 18 years Population in which outcome is assessed: schools; all school types; 4 to 18 years | UK | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (phased reopening of primary schools; grades) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: risk of transmission to other schools Follow‐up: not specified | This project received funding from the European Union's Horizon 2020 research and innovation programme ‐ project EpiPose (101003688: WJE). This research was partly funded by the National Institute for Health Research (NIHR) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK Department of Health and Social Care (PR‐OD‐1017‐20002: WJE). Health Protection Research Unit for Immunisation NIHR200929: AJvH, JDM, KEA. UK MRC (MC_PC_19065: WJE). Wellcome Trust (210758/Z/18/Z: JDM, JH, KS, NIB, SA, SFunk, SRM). Nakajima Foundation (AE). DFID/Wellcome Trust (Epidemic Preparedness Coronavirus research programme 221303/Z/20/Z: CABP). This research was partly funded by the Bill & Melinda Gates Foundation (INV‐001754: MQ; INV‐003174: KP, MJ, YL; NTD Modelling Consortium OPP1184344: CABP). NTD Modelling Consortium OPP1184344: CABP. No funding (JW) |
| Naimark 2020 | Agent‐based SEIR‐based simulation model | Population in which intervention is implemented: general school population; daycare, primary, elementary and high school; 2 to 17 years Population in which outcome is assessed: school and general population; daycare, primary, elementary and high school; all age groups | Canada | Multicomponent measures *Reduction of number of students (15 to 23 students per class) *Face masks | School closure | Transmission‐related outcome: number or proportion of cases Follow‐up: 2 months (Sep to Oct 2020) | This research was supported by COVID‐19 Rapid Research Funding (C‐291‐2431272‐SANDER through the Ontario Ministry of Health, Ontario Together grant. This research was supported, in part, by a Canada Research Chair in Economics of Infectious Diseases held by Beate Sander (CRC‐950‐232429). Sharmistha Mishra is supported by a Tier 2 Canada Research Chair in Mathematical Modelling and Programme Science. |
| Panovska‐Griffiths 2020a | Agent‐based SEIR‐model (Covasim) | Population in which intervention is implemented: general school population; all school types; 4 to 18 years Population in which outcome is assessed: general population; unspecified school types; unspecified age group | UK | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% capacity) *Reduction of contacts: 20 contacts per day Surveillance and response measures: mass testing and isolation | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcomes: number or proportion of cases; number or proportion of deaths; reproduction number; shift in pandemic development Follow‐up: 2 years (Dec 2019 to Dec 2021) | None |
| Panovska‐Griffiths 2020b | Agent‐based model (based on Covasim) | Population in which intervention is implemented: school population; secondary school; 12 to 19 years Population in which outcome is assessed: general population; secondary school; all age groups | UK | Making contacts safer: face masks Surveillance and response measures: mass testing and isolation | Least intense measure | Transmission‐related outcomes: number or proportion of cases; shift in pandemic development Follow‐up: 9 months (Jul 2020 to Mar 2021) | Not reported |
| Phillips 2020 | Agent‐based simulation of one school/child care facility embedded in the community | Population in which intervention is implemented: students, teachers, school staff; primary schools; 0 to 9 years; 25 to 44 years Population in which outcome is assessed: general population; unspecified school types; unspecified age group | Canada | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (30 versus 15 versus 8 students per class) *Reduction of contacts: alternating attendance schedule (weekly) Making contacts safer: combined measures to make contacts safer *Face masks *Social distancing *Disinfection protocols | Least intense measure Full opening of schools with no measures in place |
Transmission‐related outcomes: reproduction number: shift in pandemic development Societal, economic and ecological outcome: numbers of days spent in school Follow‐up: 120 days | Not reported |
| Rozhnova 2020 | Model for the Netherlands (effect of opening/closing schools on informative epidemic data) |
Population in which intervention is implemented: students; all school types; 0 to 20 years (0 to 5; 5 to 10; 10 to 20) Population in which outcome is assessed: general population; unspecified school types; unspecified age group | the Netherlands | Reducing the opportunity for contacts: reducing the number of contacts *Reduction of contacts between students (100% to 0%) | Full opening of schools with no measures in place | Transmission‐related outcome: reproduction number Follow‐up: 1 month (Dec 2020) | Did not report on cases without symptoms. The contribution of CHvD was under the auspices of the US Department of Energy (contract number 89233218CNA000001) and supported by the National Institutes of Health (grant number R01‐OD011095). MEK was supported by ZonMw grant number 10430022010001, ZonMw grant number 91216062, and H2020 project 101003480 (CORESMA). MJMB and PB‐V were supported by H2020 project 101003589 (RECOVER). GR was supported by FCT project 131_596787873. |
| Shelley 2020 | Deterministic SEIR model stratified into town and different cohorts within a school | Population in which intervention is implemented: general school population; unspecified school types; unspecified age group Population in which outcome is assessed: general population; all school types; all age groups | USA | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (50% and 25% capacity) *Reduction of contacts: alternating attendance schedule | Full opening of schools with no measures in place | Transmission‐related outcome: number or proportion of cases Follow‐up: 10 weeks | Not reported |
| Simonsen 2020 | Uncontrolled before‐after study | Population in which intervention is implemented: students; primary schools; 5 to 13 years Population in which outcome is assessed: students; primary schools; 5 to 13 years | Denmark | Making contacts safer: handwashing | Full opening of schools with no measures in place | Other health outcomes: physical health Follow‐up: not specified | None |
| Sruthi 2020 | Machine Learning algorithm to disentangle effects of different NPIs | Population in which intervention is implemented: general school population; secondary school; 11 to 18 years Population in which outcome is assessed: general population; not specified; all age groups | Switzerland | Making contacts safer: face masks | Full opening of schools with no measures in place | Transmission‐related outcome: reproduction number Follow‐up: 26 weeks (Mar to Sep 2020) | Not reported |
| Tupper 2020 | Stochastic individual‐based model with the states susceptible (S), exposed (E), presymptomatic (P), symptomatic (Sym), and recovered (R) | Population in which intervention is implemented: students; elementary and high school; age groups: elementary and high school students Population in which outcome is assessed: students; elementary and high school; age groups: elementary and high school students | Canada | Surveillance and response measures: mass testing and isolation; testing and quarantine *Weekly or every three days testing or environmental monitoring covering all individuals in the class *Isolation/quarantine | Least intense measure | Transmission‐related outcome: number or proportion of cases Follow‐up: 50 days | Funding from the Natural Sciences and Engineering Research Council of Canada (NSERC) grant RGPIN‐2019‐06911 and from Genome British Columbia (COV‐142) |
| Vlachos 2020 | Difference‐in‐difference study | Population in which intervention is implemented: general school population; lower secondary school (school years 7 to 9, typical age 14 to 16). Authors focus on final year; upper secondary school (school years 10 to 12, typical age 17 to 19) Population in which outcome is assessed: general population; unspecified school types; unspecified age group | Sweden | Multicomponent measures *Handwashing policy *Physical distance *Modification of activities (open house, parental meetings, outdoor activities, large gatherings cancellation) *Cleaning protocols | School closure | Transmission‐related outcome: number or proportion of cases Follow‐up: not specified | Financial support from Handelsbankens forskningssiftelser |
| Williams 2020 | COVID agent‐based model | Population in which intervention is implemented: general school population; unspecified school types; unspecified age group Population in which outcome is assessed: general population; unspecified school types; unspecified age group | USA | Surveillance and response measures: mass testing and isolation *Testing: sampling (simple random sampling, cluster sampling, and pooled sampling strategies) *Quarantine (isolation of positive cases) | Least intense measure | Transmission‐related outcomes: number or proportion of cases; shift in pandemic development Societal, economic and ecological outcome: resources Follow‐up: ~8 months | Department of Sociology at the University of Washington funded support programming efforts for this study |
| Zhang 2020 | SIR model and with contact matrices based on diaries/questionaires via phone | Population in which intervention is implemented: general school population; all school types; age groups: 0 to 6 yrs; 7 to 19 yrs Population in which outcome is assessed: general population; unspecified school types; unspecified age group | China | Reducing the opportunity for contacts: reducing the number of students and reducing the number of contacts *Reduction of number of students (phased reopening of high schools) *Reduction of contacts: implicit | Full opening of schools with no measures in place | Transmission‐related outcome: reproduction number Follow‐up: not specified | Not reported |
FRED: framework for reconstructing epidemic dynamics; NPI: non‐pharmaceutical intervention; R0: basic reproduction number; SEIR: Susceptible‐Exposed‐Infectious‐Removed; SIR: susceptible, infectious‐asymptomatic, infectious‐symptomatic, removed; SIRD: Susceptible‐Infectious‐Recovered‐Deceased model
Setting
While the majority of studies either did not differentiate between different school types or assess measures in any school type, four studies specifically assessed the implementation of measures within a secondary school setting (Curtius 2020; Panovska‐Griffiths 2020b; Sruthi 2020; Vlachos 2020), while four assessed measures implemented in the primary school setting (Aspinall 2020; Monod 2020; Phillips 2020; Simonsen 2020).
Context
Studies were carried out in a range of countries: 15 studies in the USA (Baxter 2020; Bershteyn 2020; Burns A 2020; Cohen 2020; España 2020; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kraay 2020; Landeros 2020; Lyng 2020; Monod 2020; Shelley 2020; Williams 2020), four in Canada (Campbell 2020b; Naimark 2020; Phillips 2020; Tupper 2020), three in Germany (Curtius 2020; Hoehl 2020; Isphording 2020), five in the UK (Aspinall 2020; Keeling 2020; Munday 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b), two in France (Di Domenico 2020a; Mauras 2020), two in China (Lee 2020; Zhang 2020), one in Chile (Alvarez 2020), one in Denmark (Simonsen 2020), one in Israel (Lazebnik 2020), one in the Netherlands (Rozhnova 2020), one in Sweden (Vlachos 2020), and one in Switzerland (Sruthi 2020). One study referred to multiple countries (Kaiser 2020). Studies assessed measures implemented both in primary and secondary school settings. Therefore, 20 studies have been conducted in the WHO Region of the Americas (AMR), 16 in the WHO European region (EUR) and two in the WHO Western Pacific Region (WPR) (Figure 6).
6.
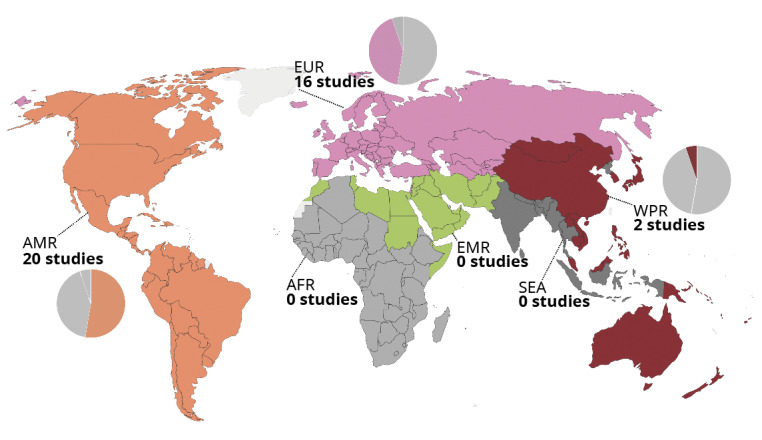
Geographical distribution of included studies
As in the scoping review, reporting on other contextual aspects was scarce. One study outlined that the economic consequences, such as an increase in unemployment and a decrease of gross domestic product may have led to a relaxation of multiple measures in Canada, including the reopening of schools (Campbell 2020b). Weather conditions, such as temperate and precipitation, were mentioned as a factor affecting sufficient ventilation in Germany, with warmer temperatures and less precipitation being mentioned as a beneficial factor (Isphording 2020).
Population
We differentiated between populations targeted by the intervention and populations in which outcomes were assessed. Most studies focused on outcomes among populations in the school setting (i.e. students and teachers); in some instances, outcomes were also assessed among parents and carers as well as the wider community.
Study designs
Overall, included studies comprised 33 modelling studies, two observational studies (Simonsen 2020; Vlachos 2020), one observational screening study (Hoehl 2020), one quasi‐experimental study (Isphording 2020), and one experimental study with modelling components (only the modelling component was assessed in this review) (Curtius 2020). Modelling studies varied in the employed modelling approaches, including compartmental models, agent‐based models, and Susceptible‐Exposed‐Infectious‐Removed (SEIR) models. Details are presented in the characteristics of included studies table (Table 6). As indicated above (Methods), when assessing observational studies which reported adjusted and unadjusted outcomes, our aim was to assess adjusted outcomes as much as possible.
Interventions
We identified a wide range of interventions across four broad intervention categories: (i) measures reducing the opportunity for contacts; (ii) measures making contacts safer; (iii) surveillance and response measures; and (iv) multicomponent measures.
Measures reducing the opportunity for contacts
We identified 23 modelling studies on measures reducing opportunity for contacts (Alvarez 2020; Aspinall 2020; Baxter 2020; Bershteyn 2020; Burns A 2020; Cohen 2020; Di Domenico 2020a; España 2020; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Landeros 2020; Lee 2020; Mauras 2020; Munday 2020; Panovska‐Griffiths 2020a; Phillips 2020; Rozhnova 2020; Shelley 2020; Zhang 2020). We differentiate between measures reducing the number of students and contacts (i.e. reducing the number of students on school premises automatically reduces the number of contacts with or without additional contact‐reducing measures being implemented) andmeasures reducing contacts (i.e. contacts between students as well as between students and school staff can also be reduced through forming cohorts with all students present on school premises).
We identified 22 modelling studies addressing measures reducing the number of students and contacts (Alvarez 2020; Aspinall 2020; Baxter 2020; Bershteyn 2020; Burns A 2020; Cohen 2020; Di Domenico 2020a; España 2020; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Landeros 2020; Lee 2020; Mauras 2020; Munday 2020; Panovska‐Griffiths 2020a; Phillips 2020; Shelley 2020; Zhang 2020). Measures reducing the number of students can be implemented on a macro level (phased reopening of certain school types), school level (in‐schooling of certain classes), or class level (reduction of number of students per class). With modelling studies mostly simulating a percentage reduction in the total number of students (i.e. 0 to 100% of students attending school in person), some studies reported how this reduction was achieved: by implementing a phased reopening of certain school types (Baxter 2020; Munday 2020; Zhang 2020), in‐schooling of certain classes only (Aspinall 2020; Lee 2020; Munday 2020), or a reduction of the number of students per class (Bershteyn 2020; Head 2020; Phillips 2020). Where models reported on how this reduction in student numbers was achieved, they referred to implementing an alternating attendance schedule (e.g. one cohort attends school in week one; another cohort attends school in week two) (Baxter 2020; Bershteyn 2020; Burns A 2020; Cohen 2020; Germann 2020; Gill 2020; Head 2020; Jones 2020; Phillips 2020; Shelley 2020).
Among these studies, six allowed for a separate assessment of measures that onlyreduced contacts while maintaining the same number of students (Cohen 2020; Germann 2020; Gill 2020; Head 2020; Landeros 2020; Phillips 2020). In all six studies, a reduction in contacts was achieved by simulating alternating attendance of cohorts without reducing the number of students.
One study exclusively looked at the reduction of contacts (simulating a range of contact reduction between 0 to 100%) without assessing a scenario in which the number of students was also reduced (Rozhnova 2020).
Measures making contacts safer
We identified 12 studies examining the impact of interventions aimed at making contacts safer (Cohen 2020; Curtius 2020; España 2020; Germann 2020; Gill 2020; Head 2020; Kraay 2020; Lazebnik 2020; Monod 2020; Panovska‐Griffiths 2020b; Sruthi 2020; Simonsen 2020). All but one study (Simonsen 2020), used modelling to assess the effects of the measures. Among these, studies focused on interventions promoting mask wearing in schools (España 2020; Head 2020; Panovska‐Griffiths 2020b; Sruthi 2020), handwashing interventions (Kraay 2020; Simonsen 2020), cleaning interventions (Kraay 2020), modifying activities in the school setting (Lazebnik 2020), and ventilation interventions (Curtius 2020). Five studies assessed combined measures to make contacts safer, where it was not possible to disaggregate the effects of each individual intervention (Cohen 2020; Germann 2020; Gill 2020; Monod 2020; Phillips 2020).
Surveillance and response measures
Fourteen modelling studies reported outcomes on interventions of mass testing and isolation measures, and symptom‐based screening and quarantine measures (Bershteyn 2020; Burns A 2020; Campbell 2020b; Cohen 2020; Di Domenico 2020a; Gill 2020; Head 2020; Hoehl 2020; Landeros 2020; Lyng 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Tupper 2020; Williams 2020). Twelve studies looked at measures involving mass testing and isolation (Campbell 2020b; Cohen 2020; Di Domenico 2020a; Gill 2020; Head 2020; Hoehl 2020; Landeros 2020; Lyng 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Tupper 2020; Williams 2020), while two studies looked specifically at symptom‐based screening and isolation (Bershteyn 2020; Burns A 2020). The distinction between these two categories is that testing and isolation measures refer to mass/routine testing (i.e. testing all students or teachers), whereas symptom‐based screening involves screening symptomatic cases only.
Multicomponent measures
We identified three additional studies that reported outcomes relating to multicomponent measures (Isphording 2020; Naimark 2020; Vlachos 2020), where it was not possible to disaggregate the effects of each individual intervention. One modelling study assessed a multicomponent measure consisting of reducing the number of students, reducing the number of contacts, universal masking, alternating attendance schedules in high schools, and symptom‐based isolation (Naimark 2020). One quasi‐experimental study assessed an intervention consisting of mask wearing, fixed cohorts, testing, quarantine measures, modification of sports and music classes, isolation of at‐risk students, reduced cohort size, ventilation, staggered school hours, and spacing in the school yard (Isphording 2020). One observational study assessed an intervention including a handwashing policy, physical distancing measures, increased outdoor activities, cancellation of large gatherings, and enhanced cleaning protocols (Vlachos 2020).
A breakdown of the different broad intervention categories and the specific interventions within them is presented in Table 5.
Comparisons
We encountered the following comparisons.
Measures to safely open schools versus keeping schools closed. Here, authors compared scenarios in which schools were opened with various measures in place to scenarios in which schools were closed completely. While reporting on the comparator was often suboptimal, authors usually made a reference to substituting face‐to‐face teaching with virtual teaching.
Measures to safely open schools versus opening schools with no measures in place. Here, authors compared a scenario with various measures in place to a scenario in which schools were open without any measures in place (e.g. prepandemic status).
Intense versus least intense measures under which schools are opened. Here, authors compared interventions that were implemented more or less intensely (i.e. testing all versus only some students) with schools open.
Single‐component measure versus multicomponent measures. Here, a single measure (i.e. schools opening with a testing strategy only) was compared with multiple measures (i.e. schools opening with testing, mask wearing and measures to reduce contacts).
In the modelling studies ‐ 33 studies constituting the majority of our evidence base ‐ the interventions and comparisons were conceptualised as scenarios. Many studies included more than two scenarios. In most modelling studies, the comparison was a scenario in which no measure was implemented (i.e. schools open without any measures in place or prepandemic status), which we considered to be the main comparison. Therefore, we used only one summary of findings table per intervention category and used this main comparator as a basis for developing narrative summaries and GRADE ratings. If the study only allowed for comparing operating schools with measures in place to school closures, we used this comparison as a basis for the evidence synthesis and signalled this clearly.
In the observational studies ‐ three studies only ‐ two studies compared measures to a scenario in which schools were closed completely. One study compared more intense measures to the least intense measures. In the experimental study with a modelling component, the comparison was made with full school reopening with no measures in place. In the observational screening study, the comparison was made with the least intense measure.
Outcomes
We included studies that assessed outcomes in four broad categories:
transmission‐related outcomes;
healthcare utilisation outcomes;
other health outcomes;
societal, economic and ecological outcomes.
Within category 1, we identified outcomes, such as the number or proportion of cases in the school or general population, the number of cases detected by a measure, the number of schools having one infected student present, the number or proportion of deaths, the progression of the pandemic, and the reproduction number.
Within category 2, we identified outcomes related to the utilisation of the healthcare system. This might have been the number or proportion of cases requiring intensive care.
In category 3, we identified outcomes related to health beyond transmission‐related outcomes. This refers to outcomes such as hand eczema.
Category 4 was rarely addressed in the included studies. The only outcome we identified was the number of days spent in school. The number of days spent in school differs across the studies for two reasons. First, the number of days in school is affected by the design of the measure, i.e. with measures to reduce the number of students in school, a proportion of students stay home, thus reducing planned days on school premises. Second, the number of days in school is affected in an unplanned manner by isolation or quarantine measures of individuals, classes or whole schools.
Risk of bias and quality of included studies
The quality of modelling studies (including the experimental study with a modelling component), the risk of bias in observational/quasi‐experimental studies, as well as the quality of the observational screening study are summarised in Table 7, Table 8 and Table 9.
3. Summary of quality appraisal for modelling studies.
| Study ID | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 |
| Alvarez 2020 | Yes | No/minor concerns | Moderate concerns | Major concerns | Partial | Moderate concerns | No | Moderate concerns | Major concerns | Moderate concerns |
| Aspinall 2020 | Partial | Moderate concerns | No/minor concerns | No/minor concerns | No | Major concerns | Partial | No/minor concerns | No/minor concerns | No/minor concerns |
| Baxter 2020 | Partial | Moderate concerns | No/minor concerns | Moderate concerns | No | Major concerns | Partial | Moderate concerns | Major concerns | Major concerns |
| Bershteyn 2020 | No | Major concerns | Major concerns | Major concerns | No | Major concerns | No | Major concerns | Major concerns | Major concerns |
| Burns A 2020 | Partial | Major concerns | Moderate concerns | Major concerns | Partial | Major concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
| Campbell 2020b | Yes | No/minor concerns | No/minor concerns | No/minor concerns | No | Major concerns | No | Moderate concerns | No/minor concerns | No/minor concerns |
| Cohen 2020 | Partial | Moderate concerns | Moderate concerns | Moderate concerns | No | Major concerns | Partial | Moderate concerns | Moderate concerns | Major concerns |
| Curtius 2020 | Partial | Major concerns | Moderate concerns | Moderate concerns | Partial | Moderate concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
| Di Domenico 2020a | Partial | Moderate concerns | No/minor concerns | Moderate concerns | Partial | Moderate concerns | Partial | Moderate concerns | Moderate concerns | Major concerns |
| España 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | Yes | Moderate concerns | Partial | Moderate concerns | Moderate concerns | Moderate concerns |
| Germann 2020 | Partial | No/minor concerns | Moderate concerns | No/minor concerns | No | Major concerns | Partial | Moderate concerns | Major concerns | Major concerns |
| Gill 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | No | Major concerns | Partial | Moderate concerns | Moderate concerns | No/minor concerns |
| Head 2020 | Yes | No/minor concerns | Moderate concerns | Moderate concerns | Yes | Moderate concerns | No | Moderate concerns | Moderate concerns | Major concerns |
| Jones 2020 | Partial | No/minor concerns | No/minor concerns | Major concerns | Partial | Moderate concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
| Kaiser 2020 | Yes | No/minor concerns | No/minor concerns | Moderate concerns | No | Major concerns | No | Moderate concerns | No/minor concerns | Moderate concerns |
| Keeling 2020 | Partial | No/minor concerns | Moderate concerns | No/minor concerns | Partial | Moderate concerns | Partial | Moderate concerns | Moderate concerns | Major concerns |
| Kraay 2020 | Partial | Moderate concerns | No/minor concerns | Moderate concerns | No | Major concerns | No | Moderate concerns | Major concerns | Moderate concerns |
| Landeros 2020 | Yes | Major concerns | No/minor concerns | Major concerns | No | Major concerns | No | Moderate concerns | Moderate concerns | No/minor concerns |
| Lazebnik 2020 | Partial | Moderate concerns | No/minor concerns | Major concerns | Yes | Moderate concerns | Partial | Moderate concerns | Major concerns | Major concerns |
| Lee 2020 | Yes | Moderate concerns | Moderate concerns | Moderate concerns | No | Major concerns | No | Moderate concerns | Moderate concerns | No/minor concerns |
| Lyng 2020 | Yes | Major concerns | No/minor concerns | Major concerns | No | Major concerns | Partial | Moderate concerns | Major concerns | No/minor concerns |
| Mauras 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | Partial | No/minor concerns | Partial | No/minor concerns | No/minor concerns | No/minor concerns |
| Monod 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | Yes | Moderate concerns | No | Moderate concerns | No/minor concerns | No/minor concerns |
| Munday 2020 | Yes | Major concerns | No/minor concerns | No/minor concerns | No | Major concerns | No | Moderate concerns | Moderate concerns | Major concerns |
| Naimark 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | Partial | Moderate concerns | No | Moderate concerns | Moderate concerns | No/minor concerns |
| Panovska‐Griffiths 2020a | Yes | Moderate concerns | No/minor concerns | Moderate concerns | Partial | Moderate concerns | Partial | Moderate concerns | Moderate concerns | No/minor concerns |
| Panovska‐Griffiths 2020b | Yes | Moderate concerns | No/minor concerns | Moderate concerns | Partial | Moderate concerns | Partial | Moderate concerns | Moderate concerns | No/minor concerns |
| Phillips 2020 | Yes | Major concerns | No/minor concerns | Moderate concerns | No | Major concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
| Rozhnova 2020 | Yes | No/minor concerns | No/minor concerns | No/minor concerns | No | Moderate concerns | No | Moderate concerns | No/minor concerns | No/minor concerns |
| Shelley 2020 | Partial | Major concerns | Moderate concerns | Major concerns | No | Major concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
| Sruthi 2020 | Partial | Major concerns | No/minor concerns | No/minor concerns | Yes | Moderate concerns | Partial | Moderate concerns | Moderate concerns | No/minor concerns |
| Tupper 2020 | Partial | Moderate concerns | No/minor concerns | Moderate concerns | No | Major concerns | No | Moderate concerns | Major concerns | Moderate concerns |
| Williams 2020 | Partial | Moderate concerns | Major concerns | Moderate concerns | No | Major concerns | Partial | Major concerns | Major concerns | No/minor concerns |
| Zhang 2020 | Yes | Moderate concerns | No/minor concerns | Major concerns | Partial | Major concerns | No | Moderate concerns | Moderate concerns | Moderate concerns |
4. Summary of assessment using the ROBINS‐I tool.
| Study | Bias due to confounding | Bias in selection of participants into the study | Bias in classification of interventions | Bias due to deviations from the intended intervention | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of the reported result | Overall risk of bias |
| Curtius 2020 | Moderate | Low | Low | Low | Low | Low | Moderate | Moderate |
| Low risk of bias due to appropriate analysis methods to control for confounding domains | N/A | N/A | N/A | Outcome data available for nearly all participants. Other outcomes N/A | Outcome assessors were aware of the intervention received by participants. Methods of outcome assessment N/A | Results unlikely to be selected from multiple measurements. Results unlikely to be selected from different subgroups | Two domains at moderate risk of bias. No domains at serious risk of bias | |
| Isphording 2020 | Low | Low | Low | Moderate | Moderate | Moderate | Low | Moderate |
| Low risk of bias due to appropriate analysis methods to control for confounding domains and reliable measurement of confounding domains | Low risk of bias due to selection based on participants characteristics observed after the start of the intervention and most participants followed from the start of the intervention | Intervention groups clearly defined | Deviations from intended interventions unclear. Unclear whether deviations were unbalanced between groups. Unclear if co‐interventions were balanced across groups | Outcome data available for nearly all participants but exclusion of/missing participants unclear | Outcome assessors were aware of the intervention received by participants. Methods of outcome assessment comparable across groups | Results likely to be selected from multiple measurements. Results likely to be selected from different subgroups | Three domains at moderate risk of bias. No domains at serious risk of bias. | |
| Simonsen 2020 | Moderate | Low | Low | Moderate | Serious | Low | Low | Moderate |
| Low risk of bias due to appropriate analysis methods to control for confounding domains | Low risk of bias due to selection based on participants characteristics observed after the start of the intervention and most participants followed from the start of the intervention | Intervention groups clearly defined | Deviations from intended interventions unclear. Unclear whether deviations were unbalanced between groups. Unclear if co‐interventions were balanced across groups | Unclear if outcome data available for nearly all participants; exclusion of/missing participants unclear | N/A | Results likely to be selected from multiple measurements. Results likely to be selected from different subgroups | One domain at serious risk of bias. Two domains at moderate risk of bias | |
| Vlachos 2020 | Serious | Moderate | Low | Moderate | Moderate | Low | Low | Serious |
| Low risk of bias due to appropriate analysis methods to control for confounding domains and confounding domains not measured reliably | Participant selection procedures unclear | Intervention groups clearly defined | Deviations from intended interventions unclear. Unclear whether deviations were unbalanced between groups. Unclear if co‐interventions were balanced across groups | Outcome data available for nearly all participants but exclusion of/missing participants unclear | Knowledge of outcome assessors of the intervention received by participants N/A. Methods of outcome assessment comparable across groups | Results likely to be selected from multiple measurements. Results likely to be selected from different subgroups | One domain at serious risk of bias. Three domains at moderate risk of bias |
N/A: not applicable
5. Summary of assessment using the QUADAS‐2 tool.
| Study information | Domain 1: patient selection | Domain 2: index test(s) | Domain 3: reference test | Domain 4: flow and timing |
| Hoehl 2020 | High | Unclear | Low/high: high for positive, low for negative | High |
The ratings for modelling studies according to our bespoke quality assessment tool can be found in Table 7 and Appendix 7. We observed a general lack of external and internal validation across studies. Internal validity describes whether the model calculations and results are consistent with the model’s specifications, i.e. whether it works as intended. Although this is necessary for the model results to be reliable, it was often not explicitly checked or reported, but is likely given due to the iterative model‐building process. External validity is an important aspect of a model pertaining to the agreement of model predictions and real‐world data. Successful validation on independent data awards a large amount of credibility to any model predictions. However, in the context of measures implemented in schools, external validation is often only possible to a very limited extent, given the short time frame in which COVID‐19‐related data have been gathered, and sometimes even impossible, given a specific model structure or scope. Due to this lack of external validation, credibility of the models was difficult to compare based only on their structure and input data, as there was no true or best reference model. However, a wide range of ratings of the structure and input data aspects allowed for detection of problematic studies, which led to downgrading for risk of bias in such instances. Only a few studies achieved a rating of minor concerns for their uncertainty analysis, arising from the fact that many studies did not address all crucial sources of uncertainty, which likely would impact the model results and lead to an overestimation of the accuracy of the outcomes.
All quasi‐experimental or observational studies had one or several moderate or serious risk of bias ratings in important domains, notably due to potential confounding, deviations from intended interventions, and missing data (Table 8).
Using the QUADAS‐2 tool, we assessed the one observational screening study as having a high risk of bias (Hoehl 2020; Table 9). This study assessed the effect of screening and intervention with respect to the number of cases detected as well as diagnostic accuracy.
Effects of interventions/results of the synthesis
In the following, we provide a narrative summary of the impact of the four categories of measures implemented in the school setting. Within each intervention category, we distinguish between different types of specific measures (Table 5) and report on each of the four predefined outcome categories (i.e. transmission‐related outcomes; healthcare utilisation outcomes; other health outcomes; societal, economic and ecological outcomes). Where we describe effects as ‘positive,’ we mean that the direction of the point estimate of the effect favours the intervention(s); ‘negative’ effects do not favour the intervention(s). ‘Mixed effects’ are when there is evidence in favour of and against the intervention(s).
For each intervention‐outcome combination we present 'Summary of findings' tables (Table 1; Table 2; Table 3; Table 4), including a narrative summary of the effects, potential effect moderators as derived from the individual studies, as well as certainty of evidence ratings, and a more concise description and synthesis of these findings. A study‐by‐study overview of the individual studies informing these summaries can be found in the corresponding appendices (Appendix 8; Appendix 9; Appendix 10; Appendix 11; Appendix 12; Appendix 13; Appendix 14; Appendix 15).
Given that potential effect moderators were generally only assessed in individual studies (for modelling studies) or were based on limited data (for observational studies), these data should be interpreted with caution. Although we could not explicitly assess how methodological and contextual differences across studies impacted the results, we consider these very important, and they should be kept in mind when interpreting the results described below.
Measures reducing the opportunity for contacts
For all studies in this category, an overview of the study‐by‐study evidence can be found in Appendix 8; Table 1 presents the GRADE summary of findings for this body of evidence. The studies were largely consistent in predicting positive effects on transmission‐related outcomes (e.g. a reduction in the number or proportion of cases, reproduction number) and healthcare utilisation outcomes (i.e. fewer hospitalisations) and mixed or negative effects on societal, economic and ecological outcomes (i.e. fewer number of days spent in school). We assessed the certainty of evidence for all outcomes as very low due to risk of bias/study quality, indirectness and imprecision encountered in the body of evidence.
Measures reducing the number of students and contacts
Among the 22 modelling studies examining measures reducing the number of students and contacts (Alvarez 2020; Aspinall 2020; Baxter 2020; Bershteyn 2020; Burns A 2020; Cohen 2020; Di Domenico 2020a; España 2020;Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Landeros 2020; Lee 2020; Mauras 2020; Munday 2020; Panovska‐Griffiths 2020a; Phillips 2020; Shelley 2020; Zhang 2020), the percentage of students attending school was reduced to 80% (Germann 2020), 55% (Jones 2020), 50% (Baxter 2020; Bershteyn 2020; Burns A 2020; Di Domenico 2020a; Gill 2020; Head 2020; Kaiser 2020; Keeling 2020; Mauras 2020; Panovska‐Griffiths 2020a; Shelley 2020), 40% (Germann 2020), and 20% (Shelley 2020). All of these studies assessed at least one transmission‐related outcome. Five studies assessed outcomes with regards to healthcare utilisation (Alvarez 2020; Di Domenico 2020a; Germann 2020; Head 2020; Keeling 2020), and three studies assessed a societal outcome (Cohen 2020; Gill 2020; Phillips 2020).
Transmission‐related outcomes
Number or proportion of cases
Thirteen modelling studies reported on the number or proportion of cases (Baxter 2020; Bershteyn 2020; Burns A 2020; Di Domenico 2020a; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Mauras 2020; Panovska‐Griffiths 2020a; Shelley 2020). Two of the studies contributing to this outcome compared implementation of more intense with less intense measures (Bershteyn 2020; Kaiser 2020), while the others compared a reduced number of students and contacts with schools being fully open with no measures in place. Twelve of these studies showed reductions in the number or proportion of cases. One study showed inconsistent results with two scenarios (2‐day alternating attendance schedule; morning ‐ afternoon shift alternating attendance schedule), associated with more cases than fully opening schools, and with full attendance associated with fewer cases than if 100% of the students did distance learning (Shelley 2020). The findings of these studies suggested potential influencing factors, such as the level of community transmission (Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Mauras 2020; Panovska‐Griffiths 2020a; Shelley 2020), co‐interventions implemented in the community (Bershteyn 2020; Germann 2020; Panovska‐Griffiths 2020a), susceptibility or transmission probabilities (Di Domenico 2020a; Head 2020; Shelley 2020), as well as the age of students (Baxter 2020; Di Domenico 2020a; Gill 2020; Keeling 2020; Mauras 2020). We assessed the certainty of evidence for this outcome as very low.
Risk of infection
Two modelling studies reported on the risk of infection with SARS‐CoV‐2 (Cohen 2020; España 2020). Reducing the number of students to 50% by introducing alternating attendance schedules and enforcing measures, such as face masks, would lead to a predicted reduction in the risk of infection. In one study (Cohen 2020), the risk of infection in students varied between 0.2% and 3.1% and in teachers and school staff between 0.4% and 4.3%, when the measures were applied. In contrast, when operating schools without any measures, the risk of infection ranged between 6.4% and 17.2% for students and between 9.5% and 24.6% for teachers and school staff, depending on the level of community transmission. The same study predicted that the lowest risk of infection can be achieved by reducing attendance in primary schools to 50% (Cohen 2020), while keeping secondary schools in remote learning (risk of infection in teachers: 0.2% to 0.7%; risk of infection in students: 0.1% to 1.0%). In another study, relative to a scenario with operating schools at full capacity and without face masks, a reduction in students led to a proportional reduction in the risk of infection across all populations (students, teachers, general population) (España 2020). The variation in the effect estimates within studies might be explained by varying levels of adherence to wearing face masks (España 2020), susceptibility of individuals to a SARS‐CoV‐2 infection, age of the students targeted by the intervention (primary versus secondary school students), as well as the level of community transmission (Cohen 2020). We assessed the certainty of evidence for this outcome as very low.
Reproduction number
Six modelling studies reported on the reproduction number (Cohen 2020; Keeling 2020; Landeros 2020; Lee 2020; Phillips 2020; Zhang 2020). All but one study predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the reproduction number when compared to operating schools with no measures in place. The discrepant study (Cohen 2020), which presented results on the effective reproduction number in a graphical way, predicted no consistent trend across different scenarios of alternating schedules and reduction of students. The variation in the magnitude of effect within studies might be explained by the level of community transmission (Cohen 2020; Keeling 2020; Landeros 2020; Lee 2020; Phillips 2020), co‐interventions implemented in the community (Zhang 2020), as well as the age of students targeted by the intervention (Cohen 2020; Keeling 2020). We assessed the certainty of evidence for this outcome as very low.
Number or proportion of deaths
Five modelling studies reported on the number or proportion of deaths (Baxter 2020; Germann 2020; Head 2020; Keeling 2020; Panovska‐Griffiths 2020a). All studies predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the number or proportion of deaths (among students, teachers and staff, and the general population) when compared to schools operating without measures in place. The variation in the magnitude of effect within studies might be explained by the level of community transmission (Keeling 2020), age of students (Baxter 2020; Head 2020; Keeling 2020), susceptibility of children to a SARS‐CoV‐2 infection (Head 2020), as well as implementation of community‐based interventions (Germann 2020; Head 2020; Panovska‐Griffiths 2020a). We assessed the certainty of evidence for this outcome as very low.
Risk of death
One modelling study reported on the risk of death (España 2020). The study predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the risk of death in various populations when compared to operating schools without measures. If only 50% of all students attended school, the risk of death could be reduced to 3.0% (3.0% to 4.0%) in teachers, 0.4% (0.4% to 0.5%) in family members, and 4.0% (4.0% to 5.0%) in the general population if measures, such as face masks, were also in place. The study assesses the variation in effect dependent on the level of adherence to co‐interventions such as mask adherence. We assessed the certainty of evidence for this outcome as very low.
Shift in pandemic development
Five modelling studies assessed six different outcomes describing potential shifts in pandemic development (Alvarez 2020; Germann 2020; Landeros 2020; Mauras 2020; Phillips 2020). Specific outcomes assessed by these studies were time to peak intensive care unit (ICU) occupancy (Alvarez 2020), time to peak incidence (Germann 2020), time to peak prevalence (Germann 2020), time to stopping rule (i.e. a rule that urges schools to close fully when prevalence among students reaches a certain number; Landeros 2020), time to outbreak (Mauras 2020), and outbreak length (Phillips 2020). All studies predicted that reducing the number of students, and thus reducing the number of contacts between students, would slow pandemic development when compared to schools operating without measures in place. The variation in the magnitude of effect might be explained by the implementation of community‐based interventions (Alvarez 2020; Germann 2020), transmissibility (Landeros 2020), the level of community transmission (Landeros 2020), as well as the age of students targeted by the intervention (Mauras 2020; Phillips 2020). We assessed the certainty of evidence for this outcome as very low.
Number or proportion of infected schools
One modelling study assessed the proportion of primary schools with at least one infected person on the premises (Aspinall 2020). The study predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in this outcome when compared to all students attending. With all students attending, the proportion of primary schools with at least one infected individual on the premises would range between 4% and 20% (661 to 3310 schools); if only one‐third of all students were attending, the risk could be reduced to between 1% and 6% of primary schools (178 to 924 schools). Besides, the magnitude of effects varied by time point of opening, which may serve as a proxy for the level of community transmission; with increasing levels of community transmission, effect estimates are assumed to increase. We assessed the certainty of evidence for this outcome as very low.
Risk of transmission to other schools
One modelling study assessed the risk of transmission from one school to other schools (Munday 2020). When compared to operating schools without measures in place, the study predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the risk of transmission to another school. For 100% attendance, the risk ranged between 0.42% and 3.6%; it was lowest if only certain grades of primary school students attended school, with the risk ranging between 0.01% and 0.09%. The level of community transmission appeared to influence the risk of transmission from one school to another. We assessed the certainty of evidence for this outcome as very low.
Healthcare utilisation outcomes
Number or proportion of hospitalisations
Two modelling studies reported on the number or proportion of cases requiring hospitalisation (Germann 2020; Head 2020). While Germann 2020 reported on the number of cases, Head 2020 reported on the excess hospitalisations per 10,000 students, teachers and staff, household members and community members. Both studies predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the number or proportion of hospitalisations when compared to operating schools without measures in place. Factors influencing the effect were co‐interventions implemented in the community (Germann 2020), the level of community transmission, as well as varying degrees of susceptibility (Head 2020). We assessed the certainty of evidence for this outcome as very low.
Number or proportion of cases requiring intensive care
Three modelling studies reported on the number or proportion of cases requiring intensive care (Alvarez 2020; Di Domenico 2020a; Keeling 2020). All studies predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the number or proportion of cases requiring intensive care when compared to operating schools without any measures. Factors that might influence the range of predicted effects are the level of community transmission (Keeling 2020), the age of students targeted by the intervention (Di Domenico 2020a; Keeling 2020), as well as co‐interventions implemented in the community (Alvarez 2020). We assessed the certainty of evidence for this outcome as very low.
Societal, economic and ecological outcomes
Number of days spent in school
Three modelling studies assessed these outcomes (Cohen 2020; Gill 2020; Phillips 2020). Cohen 2020 and Gill 2020 assessed the number of days spent in school, while Phillips 2020 assessed the number of student days lost to classroom closure. Two studies predicted that reducing the number of students, and thus reducing the number of contacts between students, would lead to a reduction in the number of planned days spent in school when compared to operating schools without measures in place. However, the interventions would increase the number of intended days spent in school due to their ability to prevent school days lost to classroom closures due to quarantine or isolation. In one study, the number of days spent in school increased due to a reduction of students leading to a lower number of days lost to classroom closures. For a ratio of students to teachers of 8:1, the number of school days lost was standard deviation (SD) 76.0 ± 59.5 and for a ratio of 30:1 SD 1157.7 ± 684.3. Factors that might influence the variation in the effects assessed in the studies were the level of community transmission (Cohen 2020; Gill 2020; Phillips 2020), as well as the age of students targeted by the intervention (Cohen 2020). We assessed the certainty of evidence for this outcome as very low.
Measures reducing contacts
Seven modelling studies assessed measures that reduced the number of contacts between individuals (Cohen 2020; Germann 2020; Gill 2020; Head 2020; Landeros 2020; Phillips 2020; Rozhnova 2020). Six of these studies assessed a transmission‐related outcome (Cohen 2020; Gill 2020; Head 2020; Landeros 2020; Phillips 2020; Rozhnova 2020). Two studies assessed outcomes with regards to healthcare utilisation (Germann 2020; Head 2020), and three studies assessed a societal outcome (Cohen 2020; Gill 2020; Phillips 2020).
Transmission‐related outcomes
Number or proportion of cases
Three modelling studies reported on the number or proportion of cases (Cohen 2020; Gill 2020; Head 2020). All studies predicted that reducing the number of contacts between students would lead to a reduction in the number or proportion of cases when compared to operating schools without measures. One study reported a reduction in the cumulative infection rate for teachers and school staff from between 9.5% and 24.6% to between 0.8% to 5.5%, and a reduction for students from between 6.4% and 17.2% to between 0.6% to 4.1% (Cohen 2020). The magnitude of effects varied according to the level of community transmission (Gill 2020; Head 2020), and susceptibility of individuals to a SARS‐CoV‐2 infection (Cohen 2020). We assessed the certainty of evidence for this outcome as very low.
Reproduction number
Three modelling studies assessed the reproduction number (Cohen 2020; Phillips 2020; Rozhnova 2020). Two studies predicted that compared to operating schools without reducing the number of contacts, a reduction in the number of contacts between students would lead to a reduction in the reproduction number. One study graphically predicted that reducing the number of contacts, while maintaining the number of students at 100%, did not have a large impact on the reproduction number (Phillips 2020). The magnitude and direction of effects varied according to the susceptibility of individuals to a SARS‐CoV‐2 infection (Cohen 2020). We assessed the certainty of evidence for this outcome as very low.
Shift in pandemic development
Two modelling studies assessed outcomes related to a shift in pandemic development (Landeros 2020; Phillips 2020). One study reported on the time to a stopping rule (Landeros 2020), and one study reported on the outcome length (Phillips 2020). One study predicted that reducing the number of contacts between students would lead to a positive shift in pandemic development (Landeros 2020). Implementing an alternating attendance schedule by creating rotating cohorts with a weekly rotating schedule, the model predicts a longer period of instruction (18 to 22 weeks) compared to a simulation in which all students attended at once (10 to 12 weeks) until reaching the stopping rule at a cumulative prevalence of 5%. With regards to the length of an outbreak, one study predicts that an alternating attendance schedule, while maintaining the number of students, performs slightly better with regards to mean and median outbreak lengths than a non‐alternating attendance schedule (Phillips 2020), but probably not in a significant way (results presented graphically). We assessed the certainty of evidence for this outcome as very low.
Healthcare utilisation outcomes
Number or proportion of hospitalisations
Two modelling studies reported on the number or proportion of individuals requiring hospitalisation due to a SARS‐CoV‐2 infection (Germann 2020; Head 2020). Both studies reported that the number or proportion of cases requiring hospitalisation was reduced by reducing the contacts between students through implementing an alternating attendance schedule. In one study (Germann 2020), the model predicts that if schools reopened without measures in place, the cumulative number of hospitalisations during the peak four weeks of the pandemic would be 1,798,188 in the USA. Implementing a weekly alternating attendance schedule, while maintaining the number of students at 40%, predicted a number of hospitalisations of 67,090 in the USA. Implementing a two‐day alternating attendance schedule, while maintaining the number of students at 40%, the number could be further reduced to 59,056. The second study predicts that with a reduction of contacts (Head 2020), the number of hospitalisations would decrease. Compared to a baseline scenario in which the excess rate of hospitalisations per 10,000 subpopulation would be 40.5 (95% confidence interval (CI) ‐46.95 to 146.64) in teachers; 0.08 (0.00 to 0.08) in students; 6.86 (95% CI ‐14.32 to 30.11) in household members; and 4.2 (95% CI ‐7.33 to 16.32) in community members, these numbers can be reduced to 2.14 (95% CI ‐47.39 to 47.85) in teachers; 0.00 (95% CI 0.00 to 0.00) for students; 0.73 (95% CI ‐17.97 to 18.49) in household members and to 0.49 (95% CI ‐9.94 to 10.04) in the general population, when contacts are reduced by 75%. The magnitude of effects varied according to the level of community transmission (Head 2020), co‐interventions implemented in the community (Germann 2020), and susceptibility of individuals to a SARS‐CoV‐2 infection (Head 2020). We assessed the certainty of evidence for this outcome as very low.
Societal, economic and ecological outcomes
Numbers of days spent in school
Three modelling studies assessed the number of days spent in school (Cohen 2020; Gill 2020; Phillips 2020). The studies reported mixed effects. Two studies predicted that reducing the number of contacts by implementing an alternating attendance schedule, or enforcing that students remain within their classroom, would lead to more days spent in school than when the number of contacts was not reduced (Gill 2020; Phillips 2020). One study predicted no effect: reducing the number of contacts between cohorts alongside other countermeasures (non‐pharmaceutical interventions; screening) predictably led to an equal percentage of school days spent at home as if no measures were in place (~5% to 10%) (Cohen 2020). Effects varied according to the level of community transmission (Cohen 2020; Gill 2020; Phillips 2020), and co‐interventions implemented in the community (Baxter 2020). We assessed the certainty of evidence for this outcome as very low.
Measures making contacts safer
For all studies in this category, an overview of the study‐by‐study evidence can be found in Appendix 9 and Appendix 10; Table 2 presents the GRADE summary of findings for this body of evidence. Here we have separated bodies of evidence that reported on the different measures and outcomes. While we observed a mostly consistent and positive direction of effect, we assessed the overall certainty of evidence for all outcomes as either low or very low due to risk of bias/study quality, indirectness and imprecision encountered in the body of evidence.
Measures making contacts safer ‐ wearing masks in school
Four modelling studies were concerned with wearing masks in school (España 2020; Head 2020; Panovska‐Griffiths 2020a; Sruthi 2020). Overall, studies considering masks did not define or specify the type of mask they were referring to, i.e. cloth masks or medical‐grade masks. Three studies reported on the number of cases avoided due to the measure (España 2020; Head 2020; Panovska‐Griffiths 2020a), two studies reported on the number or proportion of deaths (España 2020; Head 2020), and one study looked at the reproduction number (Sruthi 2020). Additionally, one study looked at the number and proportion of hospitalisations (Head 2020).
Transmission‐related outcomes
Number or proportion of cases
Three modelling studies examined cases avoided due to the intervention (España 2020; Head 2020; Panovska‐Griffiths 2020b). The comparators in these studies varied, with two comparing outcomes to the least intense measure (España 2020; Panovska‐Griffiths 2020b), and one comparing outcomes to schools being fully open with no measures. Overall, studies showed reductions in the number or proportion of cases resulting from mandatory mask policies. This included a reduction from 81.7 times to 3.0 times the number of infections in the community (España 2020), and a reduction from 57% to 46% of those with symptomatic infections needing to be tested in the community under 30% effective coverage of masks (i.e. high mask adherence and proper face coverage with masks) (Panovska‐Griffiths 2020b). A further study found a reduction in the excess proportion of infections in the school setting at a moderate level of community transmission with mandatory masks among teachers and staff (1.73, 95% CI 2.32 to 6.29), as well as students (2.51, 95% CI 0.05 to 6.95), compared to reopening with no countermeasures (teachers and staff: 14.83, 95% CI 0.93 to 29.25), students: 14.18, 95% CI 1.63 to 26.77) (Head 2020). Factors influencing the effect were the level of community transmission as well as varying degrees of susceptibility (Head 2020). We assessed the certainty of evidence for this outcome as very low.
Reproduction number
One modelling study examined the reproduction number (R) (Sruthi 2020). The study found that opening schools with mask requirements led to a reduction in R, with an estimated reduction in the general population of R by 0.01 (95% CI 0.00 to 0.01) (Sruthi 2020). We assessed the certainty of evidence for this outcome as very low.
Number or proportion of deaths
Two modelling studies examined the number or proportion of deaths (España 2020; Head 2020), finding consistent reductions in the outcome. Head 2020 found that at a moderate level of community transmission, school reopening with mandatory mask wearing and assuming children were 50% as susceptible to COVID‐19 as adults, predicted reductions in excess proportion of deaths among students and school staff and teachers compared with school reopening with no countermeasures. With schools opening at full capacity with no measures in place, at a moderate level of community transmission, with children assumed to be half as susceptible as adults, the study predicts that the excess number of deaths per 10,000 of the subpopulation would be 10.3 (95% CI 0.47 to 20.66) for teachers/staff and 2.98 (95% CI 0.33 to 5.83) for students. España 2020 focused on the general population, finding that, under a scenario with high capacity and high face‐mask adherence, there would be a decrease in the ratio of the cumulative number of deaths in the overall population of 1.5 (95% CI 1.5 to 1.6). Factors influencing the effect were the level of community transmission as well as varying degrees of susceptibility (Head 2020). We assessed the certainty of evidence for this outcome as very low.
Healthcare utilisation outcomes
Number or proportion of hospitalisations
One modelling study examined the number of hospitalisations (Head 2020). It predicts that with schools opening at full capacity with no measures in place, at a moderate level of community transmission, with children assumed to be half as susceptible as adults, the excess rate of hospitalisations per 10,000 of the subpopulation among students would be 0.08 (95% CI 0.00 to 0.08) and school staff and teachers would be 40.5 (95% CI ‐46.95 to 146.64), compared to the intervention scenarios. The study predicts that mandatory mask wearing in schools when reopening all schools would lead to reduced hospitalisations among students, staff, household members and community members. Factors influencing the effect were the level of community transmission as well as varying degrees of susceptibility. We assessed the certainty of evidence for this outcome as very low.
Measures making contacts safer ‐ cleaning
Transmission‐related outcomes
Reproduction number
One modelling study assessed the impact of an enhanced cleaning policy on the reproduction number (Kraay 2020). The study found that compared to the least intense measure of eight‐hourly and four‐hourly surface cleaning and disinfection, hourly cleaning and disinfection alone could bring the fomite R below 1 in some office settings, particularly combined with reduced shedding, but would be inadequate in schools. This study did not take into account direct transmission through droplet spray, aerosols and hand‐to‐hand contact. We assessed the certainty of evidence for this outcome as very low.
Measures making contacts safer ‐ handwashing
We identified two studies that assessed the impact of handwashing (Kraay 2020; Simonsen 2020). One used a modelling design (Kraay 2020), the other was observational (Simonsen 2020).
Transmission‐related outcomes
Reproduction number
One modelling study assessed the impact of handwashing on the reproduction number and suggested that the intervention had no impact when compared to full school reopening with no measures in place (Kraay 2020). While results are only presented in a graphical way, it predicted that handwashing (hourly with 100% effectiveness) compared to no handwashing showed no effect with regards to the projected reproduction number from fomite transmission. We assessed the certainty of evidence for this outcome as very low.
Other health outcomes
Incidence of hand eczema
One study (Simonsen 2020), using an observational design, found an increase in the prevalence of hand eczema among students in reopened schools with a handwashing intervention. The comparator in this study was full school reopening with no measures in place. We assessed the certainty of evidence for this outcome as low.
Measures making contacts safer ‐ modification of activities
Transmission‐related outcomes
Reproduction number
One modelling study assessed the impact of changing the length of the school day (Lazebnik 2020), and found that increasing the school day to between 8 and 9 hours each day for five days would reduce R by 0.83 compared to the least intense measure of a policy in which children go to school every other day for five hours. We assessed the certainty of evidence for this outcome as very low.
Measures making contacts safer ‐ ventilation
Transmission‐related outcomes
Inhaled dose of aerosol particles containing RNA virus in the room and inhaled dose of RNA virus for a susceptible person
One modelling study assessed the effect of four air purifiers with an air exchange rate of 5.7 L/h and equipped with HEPA filters in a single high school classroom (Curtius 2020). Using air purifiers, for a person spending two hours in a room with an infectious person, the inhaled dose of particles containing RNA virus is predicted to be reduced by a factor of six, compared to a closed classroom with no air purifiers. We assessed the certainty of evidence for this outcome as very low.
Measures making contacts safer ‐ combined measures to make contacts safer
We identified five modelling studies assessing multicomponent interventions aimed at making contacts safer (Cohen 2020; Germann 2020; Gill 2020; Monod 2020; Phillips 2020), where it was not possible to disaggregate the effects of each individual intervention. These studies employed different combinations of mask wearing, hand hygiene, respiratory etiquette, enhanced cleaning, modification of activities, physical distancing, and exclusion of high‐risk students from attending school. Findings showed a reduction in the number of cases, but there were mixed effects regarding changes to the reproduction number and the number of hospitalisations. Three of the studies used full school reopening with no measures in place as the comparator (Cohen 2020; Gill 2020; Monod 2020), and two studies used the least intense measure (Germann 2020; Phillips 2020).
Transmission‐related outcomes
Number or proportion of cases
Four modelling studies looked at cases avoided (Cohen 2020; Germann 2020; Gill 2020; Monod 2020). Three studies reported the (cumulative) number of cases or the attack rate. All but one of the studies predicted that multicomponent interventions reduced the number of cases in the community (Gill 2020; Germann 2020), and in the school (Cohen 2020; Gill 2020). For the study that reported on community‐level transmission, it was found that implementing a variety of infection control measures would lead to a reduction in the total number of infections, although specific figures were not reported (Gill 2020). Studies also showed a reduction in the number of cases in scenarios where schools reopened with partial online learning and 'ideal social distancing' (assumed 50% reduction in contacts due to face masks, hygiene, and distancing measures) compared to scenarios with no countermeasures (Germann 2020). Studies that reported on school‐level outcomes found that implementing a variety of infection control measures led to a four‐fold reduction in the cumulative COVID‐19 infection rate among students, teachers, and staff (Cohen 2020), and a reduction in the total number of infections, although specific figures were not reported (Gill 2020). For one study, the direction of effect was unclear due to reporting (Monod 2020). We assessed the certainty of evidence for this outcome as very low.
Reproduction number
Two modelling studies examined the reproduction number (Cohen 2020; Phillips 2020). Both studies found a reduction in R, however, results were only presented graphically, making it difficult to determine effect sizes. Findings from one study showed that implementing countermeasures that limit transmission and detect, trace, and quarantine cases within schools, compared to reopening with no countermeasures, reduces the effective reproduction number to < 1 (Cohen 2020). The other study only presented results pertaining to the reproduction number in a graphical way. With this limited evidence, the study implied that the effective reproduction number would be lower in low‐transmission settings. We assessed the certainty of evidence for this outcome as very low.
Number or proportion of deaths
Two modelling studies examined the number or proportion of deaths (Germann 2020; Monod 2020), finding mixed results. One study found that when fewer workplaces were open, all four 40% partial online learning scenarios with alternating days or weeks of attendance, were found to reduce deaths (Germann 2020). Full school reopening with no countermeasures was predicted to result in 230,451 deaths. In contrast, this decreased to 25,474 deaths where a 50% reduction in contacts due to mask wearing was modelled and to 27,874 deaths with reduced social distancing with minimal mask use. The other study estimated a 12.6% (95% CI 7.4% to 22.7%) increase in deaths among children and the general population as a result of schools reopening with countermeasures, compared to keeping schools closed (Monod 2020). We assessed the certainty of evidence for this outcome as very low.
Shift in pandemic development
One modelling study examined the shift in pandemic development (Germann 2020), reporting positive results. Findings showed that when fewer workplaces were open, 40% partial online learning scenarios, with 'ideal social distancing' (a 50% reduction in contacts due to face masks, hygiene, and distancing measures) increased the time to peak prevalence from 66 days when schools were fully reopened with no countermeasures in place to 178 days. The study found the results of its simulations to be highly dependent on the number of workplaces assumed to be open for in‐person business, as well as the initial COVID‐19 incidence within the community. We assessed the certainty of evidence for this outcome as very low.
Healthcare utilisation outcomes
Number or proportion of cases requiring hospitalisation
One modelling study examined the number or proportion of cases requiring hospitalisation (Germann 2020). The study predicted that when fewer workplaces were open, all four 40% partial online learning scenarios, with ideal social distancing (defined as a 50% reduction in contacts due to physical distancing, hygiene and masks), were found to avert between 543,977 and 1,708,197 hospitalisations. Moreover, for these scenarios, hospitalised cases during the peak four weeks ranged from 59,056 to 354,878 compared to a baseline scenario of 685,747 with schools reopening with full attendance and no measures in place. We assessed the certainty of evidence for this outcome as very low.
Societal, economic and ecological outcomes
Numbers of days spent in school
Two modelling studies examined the impact of the intervention on the number of days spent in school (Gill 2020; Phillips 2020). One study found that at very low community infection rates (10 reported infections per 100,000 population over the last seven days), most students can expect to attend nearly every day even in schools operating full‐time, as long as schools implement multiple interventions. It is not possible to determine effect size due to lack of reporting (Gill 2020). The other study compared high with low transmission settings in primary schools. Except for a ratio of 30:1, the number of student days lost to closure was consistently higher in low transmission settings (Phillips 2020).
Surveillance and response measures
For all studies in this category, an overview of the study‐by‐study evidence can be found in Appendix 11, Appendix 12 and Appendix 13; Table 3 presents the GRADE summary of findings for this body of evidence. Here, we have separated bodies of evidence that reported on the different measures and outcomes. While we observed a mostly consistent and positive direction of effect, we assessed the overall certainty of evidence for all outcomes as very low due to risk of bias/study quality, indirectness and imprecision encountered in the body of evidence.
Mass testing and isolation measures
Among studies looking at mass testing and isolation, 11 studies used modelling study designs (Campbell 2020b; Cohen 2020; Di Domenico 2020a; Gill 2020; Head 2020; Landeros 2020; Lyng 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Tupper 2020; Williams 2020), and one study used an observational design (Hoehl 2020). Nine studies assessed transmission‐related outcomes (Cohen 2020; Di Domenico 2020a; Head 2020; Landeros 2020; Lyng 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Tupper 2020; Williams 2020), one study assessed healthcare utilisation outcomes (Head 2020), and four studies examined societal outcomes (Campbell 2020b; Gill 2020; Lyng 2020; Williams 2020). One study assessed the number of cases detected (Hoehl 2020). Overall, the studies yielded positive outcomes. However, these measures were often implemented alongside other transmission mitigation measures, such as physical distancing and cohorting strategies which may have moderated the effects of the testing and isolation strategies. Furthermore, the effectiveness of measures was also dependent on the level of community transmission. Outcome measures were also not reported consistently, making it difficult to pool estimates of effect sizes across studies.
Transmission‐related outcomes
Number or proportion of cases
Seven modelling studies looked at the number or proportion of cases (Cohen 2020; Di Domenico 2020a; Head 2020; Lyng 2020; Panovska‐Griffiths 2020a; Tupper 2020; Williams 2020). All studies showed positive results, however all studies assessed testing and isolation strategies alongside other countermeasures. For example, Cohen 2020 found that measures that limit transmission and detect, trace and quarantine cases within schools could lead to reductions in the cumulative COVID‐19 infection rate among students, teachers and staff by over 14‐fold. However, these measures were implemented alongside classroom cohorting, face masks, physical distancing and handwashing protocols in schools, so it is not possible to comment on the impact of these measures alone. Head 2020 suggested that although testing and isolation strategies could lead to reductions in transmission, their effectiveness on their own was low, and when combined with strict social‐distancing measures and a reduction in community transmission, they could be more effective. Di Domenico 2020a assessed the impact of several different reopening strategies from partial, progressive, or full school reopening coupled with moderate social‐distancing interventions and large‐scale testing, tracing, and isolation measures. It is therefore impossible to comment on the effectiveness of testing and isolation strategies alone in this study.
The comparators used for these studies varied, with two studies comparing outcomes to full school reopening with no measures in place (Cohen 2020; Di Domenico 2020a), four studies comparing outcomes to the least intense measure (Lyng 2020; Panovska‐Griffiths 2020a; Tupper 2020; Williams 2020), and one study comparing outcomes to a single intervention component (Lyng 2020). Moderating factors for the impact of outcomes included relative susceptibility and infectiousness of children and extent of community transmission amid opening (Head 2020; Lyng 2020). We assessed the certainty of evidence for this outcome as very low.
Number of cases detected
One observational study looked at the impact of testing strategies on the number of cases detected due to the intervention (Hoehl 2020). The study evaluated the application of a self‐testing strategy. Compared to the least intense measure of no testing, the strategy found an increase in detected cases. It also found that 10,768 (99.4%) antigen tests were recorded to have been valid, 47 (0.43%) were recorded as invalid, and 16 (0.15%) gave false‐positive results. We assessed the certainty of evidence for this outcome as very low.
Reproduction number
One modelling study looked at the impact of two different testing strategies on the reproduction number in schools (Panovska‐Griffiths 2020a), and found that test–trace–isolate strategies would need to test a sufficiently large proportion of the population with symptomatic COVID‐19 infection and trace their contacts with sufficiently large coverage, for R to diminish below 1. The comparator used in this study was the least intense measure or the least intense testing strategy. We assessed the certainty of evidence for this outcome as very low.
Number or proportion of deaths
Two modelling studies assessed the impact of testing and isolation strategies on the number and proportion of deaths and found positive results overall (Head 2020; Panovska‐Griffiths 2020a). One study only showed results in a graphical way and suggested that more intense testing and isolation measures would lead to fewer deaths than less intense measures (Panovska‐Griffiths 2020a). The other study predicted that there would be a lower proportion of deaths for teachers, students, and in the community, if a testing strategy was implemented, compared to full school reopening with no measures in place (Head 2020). The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. We assessed the certainty of evidence for this outcome as very low.
Shift in pandemic development
The four modelling studies that assessed the impact of testing and isolation strategies on the timing and progression of the epidemic (Landeros 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020b; Williams 2020), found that testing and isolation could slow or prevent a second wave of the epidemic compared to full reopening with no measures in place, or to a less intense testing and isolation intervention. The studies suggest that the timing of the epidemic depends on the degree to which testing and isolation strategies are being implemented and the combination of testing and tracing, with one study suggesting that daily testing levels of between 8% and 11% would be required in order to avoid a second wave of the pandemic (Panovska‐Griffiths 2020b). Landeros 2020 demonstrated that reopening schools with a surveillance programme in place may provide 10 to 12 weeks of continuous instruction with low infection risk. Infections after the closure of schools are driven by a lack of interventions outside of school. It was therefore suggested that testing and isolation in this context, can curtail this growth within schools, in order to counter the lack of interventions in the community.
Across studies, the level of community transmission of SARS‐CoV‐2 seemed to impact the magnitude of the effect of the testing and isolation strategies employed. Further, measures such as masks, and hygiene policies, and compliance with these measures, also seemed to influence outcomes. We assessed the certainty of evidence for this outcome as very low.
Healthcare utilisation outcomes
Number or proportion of hospitalisations
One modelling study found that reopening schools with a weekly or monthly testing strategy for teachers and students would lead to a higher number of hospitalisations compared to reopening under strategies to reduce contacts (Head 2020). The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopenings. We assessed the certainty of evidence for this outcome as very low.
Societal, economic and ecological outcomes
Number of days spent in school
One modelling study looked at the number of days spent in the classroom in scenarios where testing and isolation measures were implemented (Gill 2020), and found that policies closing the school (for 3 days or 14 days) upon detection of infections, substantially reduced the total number of days that students can attend in person compared to fully reopening schools with no measures in place. These effects are larger in schools operating full‐time than in schools using hybrid approaches because schools using hybrid approaches experienced fewer infections that led to quarantines or closures. Therefore, although isolation measures will inevitably lead to days lost in school, the number of days will be influenced by other countermeasures that are being implemented at the same time, as well as the length of quarantine/school closure upon detection of cases. We assessed the certainty of evidence for this outcome as very low.
Resource costs
Three modelling studies looked at the impact of testing and isolation strategies on resources and found mixed effects (Campbell 2020b; Lyng 2020; Williams 2020). The studies all compared the impact of the intervention as compared to the least intense testing strategy. One study used health economic modelling to look at the human resource costs of testing strategies (Campbell 2020b). The study found that testing of at‐risk groups, in particular testing all 6,012,144 students and employees in primary and secondary schools over 1.5 months would require an additional 20,956 healthcare professionals, 22,950 administrative staff and 22,462 laboratory staff, costing CAD 816.0 million, compared to no intervention, demonstrating that the intervention had an overall negative impact on resources. One study found that frequent testing strategies can reduce the rate of new infections compared to scenarios where there is no testing at all (Lyng 2020). The study found that a 98% sensitive test, with no delay in results, administered every three days with pooling, and no confirmatory test offered by the institution costs less than USD 1.50 per person per day, with high performance. Another study looking at different testing strategies found no effect on resources. It is difficult to compare or synthesise findings across these studies due to the fact that they all assess different strategies in terms of intensity and type of testing. We assessed the certainty of evidence for this outcome as very low.
Symptom‐based screening and quarantine measures
Two modelling studies looked at symptom‐based screening and quarantine measures and showed a reduction in the number of cases due to the intervention (Bershteyn 2020; Burns A 2020). These studies found that policies that screen and isolate suspected cases can, overall, decrease the attack rate compared to fully reopening schools with no measures in place. As predicted by the studies, the most effective testing and isolation strategies used a combination of early testing together with symptom screening and isolation of symptomatic cases. Bershteyn 2020 assessed the proportion of cases that could be reduced due to the intervention, and found an overall reduction of in‐school transmission from 26% to 71.1%, depending on the level and timing of testing. Burns A 2020 assessed the impact of symptom‐based testing and isolation on the attack rate and found that symptom‐based detection and isolation could reduce the attack rate by up to 15%.
Transmission‐related outcomes
Number or proportion of cases
The two studies that looked at symptom‐based screening and quarantine found that policies that screen and isolate suspected cases can, overall, decrease the attack rate compared to full school reopening with no measures in place (Bershteyn 2020; Burns A 2020). The studies found that the most effective testing and isolation strategies used a combination of early testing, together with symptom screening and isolation of symptomatic cases. These strategies were often implemented alongside other transmission mitigation measures, such as physical distancing and cohorting, so it is not possible to assess the impact of symptom screening and quarantine measures alone. We assessed the certainty of evidence for this outcome as very low.
Shift in pandemic development
One modelling study found that with no testing policy in place (Burns A 2020), the peak number of infected school staff and students is assumed to be 148 (interquartile range (IQR) 82 to 213), and the interval between the first and last day, with at least two cases, would be 139 (IQR 120 to 154). Implementing a policy of two days of home isolation, following the last episode of fever, predicted a reduction in all outcome categories: the peak number of infected people is predicted to sink to 124 (IQR 58 to 184). The interval between the first and last day, with at least two cases, would increase to 145 (IQR 127 to 157). The study measured a strategy that was implemented alongside other transmission mitigation interventions, such as cohorting and physical distancing, so it is not possible to assess the impact of symptom‐based screening and quarantine measures alone. We assessed the certainty of evidence for this outcome as very low.
Multicomponent measures
For all studies in this category, an overview of the study‐by‐study evidence can be found in Appendix 14 and Appendix 15; Table 4 presents the GRADE summary of findings for this body of evidence. Here, we have separated bodies of evidence that reported on the different measures and outcomes. While we observed a mostly consistent and positive direction of effect, we assessed the overall certainty of evidence for all outcomes as very low due to risk of bias/study quality, indirectness and imprecision encountered in the body of evidence.
Transmission‐related outcomes
Number or proportion of cases
Three studies assessed the number or proportion of cases (Isphording 2020; Naimark 2020; Vlachos 2020).
One experimental study showed a positive effect that multicomponent measures reduced the number of cases (Isphording 2020), and found that implementing a variety of infection control measures led to a reduced cumulative infection rate (Isphording 2020). The observational study showed a negative effect (Vlachos 2020), finding that exposure to open rather than closed schools resulted in a small increase in PCR‐confirmed infections. We assessed the certainty of evidence for this outcome as low.
One modelling study compared a multicomponent measure consisting of: i) reducing the number of students; ii) reducing the number of contacts; iii) universal masking; iv) alternating attendance schedules in high schools; and v) symptom‐based isolation, to full school closures. The study found that there was an increase in the predicted number of infections when reopening with measures compared to a full school closure scenario. We assessed the certainty of evidence for this outcome as very low.
Implementation
With regards to context, reporting on implementation of the respective measures has been scarce. Some studies accounted for adherence to the intervention in their models (e.g. España 2020; Keeling 2020; Lee 2020; Panovska‐Griffiths 2020b; Rozhnova 2020), or was referred to as a relevant aspect influencing the effectiveness of measures implemented in the school setting.
As implementation agents, actors at multiple levels have been referred to as: agents at the national or subnational level (e.g. health authorities; Simonsen 2020); agents at the school level (e.g. teachers conducting self‐testing; Hoehl 2020); household members (e.g. parents); as well as actors outside of the school setting (e.g. healthcare professionals; Campbell 2020b).
As in the scoping review, we identified very little information on exactly how these measures are implemented within the school setting or the strategies used to implement an intervention (e.g. enforcement). One study reported enforcement and facilitating strategies for surveillance measures. These included remote monitoring of isolation, penalty for non‐compliance, help in maintaining home isolation, as well as provision of thermometers for screening (Burns A 2020). One study reported training of teachers conducting self‐testing (Hoehl 2020). In another study, the strictness of measures implemented in the community was described as mild (Vlachos 2020).
Discussion
Summary of main results
Our primary objective was to assess the effectiveness of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic. This rapid review found studies that focused on the effectiveness of school measures on several SARS‐CoV‐2/COVID‐19‐related outcomes across four broad intervention categories including: i) measures reducing the opportunity for contacts; ii) measures making contacts safer; iii) surveillance and response measures; and iv) multicomponent measures. While studies used various study designs, the majority of them used modelling. Overall, while studies showed variable reductions in transmission and healthcare utilisation‐related outcomes, the evidence available at the time the searches were conducted was of limited quality. Thus, there is much uncertainty regarding the true effect of most measures. Thus, it is likely that the true effects of most measures remain unknown. Most studies, regardless of the intervention category in which they were included, assessed the effects of a combination of interventions, which could not be disentangled to examine individual effects, making the interpretation of the results, and the ability to comment on the effectiveness of individual measures difficult. Across all intervention types and outcome measures, there were a number of factors that could potentially explain the variation in the direction and/or magnitude of results, including the level of community transmission, the susceptibility of target populations, and type of schooling (i.e. primary versus secondary). Below, we describe studies identified within the four broad intervention categories.
In measures reducing the opportunityfor contacts, we summarised measures to reduce contacts between individuals, or cohorts, or both, as well as measures to reduce the number of students in attendance, which ultimately lead to a reduction of contacts by design. Overall, the studies included in this category consistently predicted outcomes in a positive direction with regards to transmission‐related outcomes and healthcare utilisation outcomes; they also showed a reduction in the number of days spent in school due to the intervention, but in some cases, the initial reduction in days spent in school was offset by an increase the number of intended days spent in school due to their ability to prevent days lost due to quarantine or isolation. There were some differences in the direction of the effect for different types of interventions to reduce the opportunity for contacts (i.e. alternating attendance schedules, staggered start/finish times). Overall, very low‐certainty evidence showed a reduction in the number of cases, reproductive number, hospitalisations, and ICU admissions, as well as days of school missed.
Under measures making contacts safer, we summarised findings with regards to policies and practices ensuring safe contacts between individuals. These include measures such as mask‐wearing policies, handwashing policies, and enhanced cleaning and ventilation procedures and systems. We found several modelling studies and one observational study that fit into this category. Overall, the evidence showed a reduction in the number of cases, reproduction number, hospitalisations, and ICU admissions, as well as days of school missed, but the certainty of evidence was very low for studies assessing mask‐wearing policies, modification of activities, and cleaning and ventilation procedures and systems. Two studies assessing handwashing policies showed either negative or no effects, with one study of low certainty showing an increase in hand eczema due to a handwashing policy introduced once schools reopened and another study of very low certainty showing no effect, although results were only presented graphically. Evidence on interventions combining multiple measures to make contacts safer was of very low certainty and showed mixed results in terms of a reduction in the number of cases, reduction in the number of deaths, shift in pandemic development, as well as days of school missed, however, they did show a reduction in the reproduction number and the number or proportion of hospitalisations.
We identified several modelling studies, one quasi‐experimental and one observational study focused on surveillance and response measures, including testing and isolation, and symptomatic screening and isolation. Overall, very low‐certainty evidence showed that implementing measures to detect, trace, and quarantine cases within schools could lead to reductions in the COVID‐19 infection/transmission rate among students, teachers, and staff, and could also slow or prevent a second wave of the epidemic, and reduce the reproduction number and number or proportion of deaths. The most effective testing and isolation strategies used a combination of early testing together with symptom screening and isolation of symptomatic cases, with one study finding that opening schools was likely to more rapidly increase the death count if asymptomatic testing and tracing strategies were not implemented. There was mixed evidence on the costs and human resource costs of surveillance measures, but there was generally evidence that surveillance and response measures could reduce the number of hospitalisations and the number of school days missed. Studies that assess symptom‐based screening and isolation measures also showed some evidence to suggest that such measures could reduce the number or proportion of infections and could reduce the peak number of people infected during the pandemic, however the certainty of evidence was very low.
We found three additional studies assessing multicomponent measuresthat combined measures to make contacts safer or reduce the opportunity for contacts with measures reducing the number of contacts and surveillance and response measures. Two observational/quasi‐experimental studies with very low‐certainty evidence, showed mixed results on the impact of these measures on reducing the number or proportion of cases, but this is likely due to the fact that the comparator used in both studies was full school closure. One modelling study with very low‐certainty evidence, showed that reopening schools with such measures in place would still lead to a higher number or proportion of cases as compared to when schools were closed.
Overall completeness and applicability of the evidence
Consistent with the scoping review on which this rapid review is based (Krishnaratne 2020), we identified studies assessing a broad range of measures implemented in the school setting to safely reopen schools, or keep schools open, or both, during the COVID‐19 pandemic. We identified studies examining outcomes across all categories identified in the scoping review. To that end, we identified sufficient studies to address the objectives of this review. Our findings within this rapid review mostly aligned with the scoping review (Krishnaratne 2020). As in Krishnaratne 2020, we identified some gaps in the evidence base relating to setting, socioeconomic inequality, study design, and outcomes. Additionally, it should be noted that in modelling the population, setting, context and interventions, modelling studies all make a series of assumptions; some of these are closer to real‐world conditions than others. Our evidence gap map visualises the areas in which more evidence is needed (Figure 3).
While we used the logic model resulting from the scoping review to inform the protocol for this rapid review (Krishnaratne 2021), we adapted the logic model based on what we found in our analysis (Figure 2). The major change was the restructuring of the intervention categories: while analysing the pathways between measure and effect, we felt that the intervention categories did not fully grasp the mechanisms of interest. We also removed the levels of interventions because our analyses showed that the line between intervention levels was often blurry, in particular with regards to measures which were only modelled and not implemented in a real‐world setting. Lastly, we updated the outcome box of the logic model integrating the outcomes we encountered during data extraction.
Population
Regarding the populations assessed, most modelling studies across all intervention categories considered outcomes in the general population, but not always within the population in which the measure was implemented, that is students and school staff. Observational and quasi‐experimental studies used data on the populations being targeted by the intervention, including teachers and students.
Setting
We identified evidence from several different countries, however most of these were high‐income countries in North America and Europe, with limited evidence from Asia, Australia, and South America, and no evidence from Africa. This is likely to have implications with regards to the transferability and generalisability of these findings to other countries, in particular with regards to low‐ and middle‐income settings. In terms of the actual school setting, studies assessed measures implemented both in primary and secondary school settings but also looked at outcomes in the wider community. Most studies did not differentiate between different school types (i.e. primary and secondary) and if they did, they focused on the primary school setting. There are various differences in contextual conditions between school types, such as changing classrooms, size of the buildings, commuting styles, and children’s age, whereby studies have reported lower levels of transmission among younger compared to older children (Cohen 2020; Gill 2020; Lazebnik 2020). Thus, evidence which separates findings according to school type would be useful to inform decision‐making. Given the publication dates of the studies included, much of the identified evidence relates to early stages of the pandemic. Therefore, there is a need for more data from the later stages of the pandemic.
Intervention
We found a range of different interventions which all aligned with the three main categories described in the a posteriori model of our scoping review. Most included studies assessed measures to reduce the opportunity for contacts in schools, followed by surveillance and response measures to make contacts safer, and lastly multicomponent measures. With regards to reducing the opportunity for contacts, the way in which the number of contacts was reduced differed across the included studies, comprising reduction of students on the level of an entire school versus reduction of students on the level of a single class. As stated, the majority of studies identified used modelling designs which is why the reporting on the components of the measures was mostly scarce. Interestingly, the category on multicomponent measures includes two real‐world studies and only one modelling study. While the real‐world studies would have offered valuable insight on the impact of measures such as masks, the way in which the measures were reported and presented, made it impossible to draw conclusions with regards to single intervention components. While we did identify more observational and quasi‐experimental studies in the rapid review than in the scoping review, the vast majority of studies used modelling. Further, as will be discussed in more detail below, the certainty of the evidence was often very low, so the ability for interpretation of findings from these studies is limited. Also, the evidence in some intervention categories was sparse and did not allow for a comprehensive or robust synthesis. This was particularly the case for interventions aimed at making contacts safer, including mask‐wearing and handwashing policies, modification of activities, and enhanced cleaning and ventilation policies. Therefore, the current synthesis is mainly focused on interventions to reduce the opportunity for contacts and surveillance and response measures.
Outcomes
Studies presented findings across four broad outcome categories including: i) transmission‐related outcomes; ii) healthcare utilisation outcomes; iii) other health outcomes; and (iv) societal, economic and ecological outcomes. As with the scoping review (Krishnaratne 2020), most studies identified in this rapid review focused on transmission‐related outcomes, including the number or proportion of cases, number of detected cases, the reproduction number, the size or timing of the epidemic, or the number or proportion of deaths. Less commonly reported outcomes included healthcare utilisation outcomes, such as the number or proportion of hospitalisations or ICU beds needed. Other health outcomes included physical health, namely hand eczema as a result of increased handwashing. Societal, economic and ecological outcomes included human resource costs and financial costs of the intervention, as well as the intended and unintended number of days spent in school or the number of school days lost due to the intervention. No included studies assessed unintended outcomes concerned with potential adverse effects in terms of psychosocial health (e.g. isolation and lack of social interaction), educational outcomes (e.g. school grades, passing of final exams, graduation to next grade, learning outcomes, scores on standardised tests) or broader societal implications (e.g. employment). This represents a major limitation regarding the completeness of the evidence, as this information is important to assess the benefits and harms of the measures.
Context and implementation
There were some gaps in the evidence in terms of context, specifically regarding the geographic focus of the studies. Overall, studies fell short in reporting on contextual aspects, such as cultural, legal or socioeconomic factors. When it comes to transferring these measures to other contexts, the lack of reporting on these aspects has implications on the assessment of feasibility, acceptability and transferability of measures, as well as the need for their adaptation. Further, as the majority of studies included in the review were modelling studies, there is a lack of empirical, real‐world data, which means that there are very little data on the actual implementation of interventions ‐ one of the key objectives of this review. Some included studies acknowledged that adherence to or compliance with interventions might influence implementation (Bershteyn 2020; Burns A 2020; Landeros 2020; Panovska‐Griffiths 2020b). The one study that assessed a ventilation intervention mentioned cost, noise, size, and position of the ventilation device as factors influencing implementation (Curtius 2020), and one study suggested that intervention fidelity may have influenced the effect of the intervention (Simonsen 2020).
Study design
Most included studies used modelling study designs (N = 33). Modelling studies become necessary to address the complex phenomena investigated and there are no generally agreed‐upon principles of how such studies need to be conducted, although several studies have offered guidance in this regard (Ramos 2015). Consequently, various study designs and types of models have been encountered, ranging from simple deterministic compartmental models described by ordinary differential equations or highly detailed agent‐based simulations. The quality of each model has been assessed case‐by‐case, but some general concerns with regards to the usefulness of models emerged in this review. Most studies investigated combined interventions that could not be disentangled to examine individual effects, such that results are difficult to apply in the context of this review. Also, the way in which measures have been implemented in a model differs. For example, the way in which the measure "mask" is implemented in a model can express itself in the same way as the measure "contact reduction". While this makes no difference to the equation, this has implications with regards to the transferability of these findings to the real world, the design of the measure as well as its actual implementation. Additionally, results are difficult to compare across the included modelling studies as these assumed a heterogeneous set of settings and scopes, which is only directly applicable within the well‐defined context of the respective model, hindering generalisation of the results. Furthermore, there are appreciable quality concerns in some studies, which limits their usefulness in contributing to the body of evidence established in this review. This highlights the importance of generating more high‐quality modelling studies in order to contribute to the body of evidence in a meaningful way. Whilst modelling studies do have their merits in predicting complex outcomes, it is especially important that primary data are collected and reported going forwards.
Sources of heterogeneity
As part of the narrative synthesis, we carefully documented and assessed potential sources of heterogeneity. In both the modelling and observational studies, assumptions with regards to co‐interventions in place, level of community transmission, context, as well as implementation, differed widely. Measures likely varied in effectiveness according to the stage of the pandemic, the number and type of co‐interventions in place in the community, school contextual differences, and the level of community transmission. Whilst co‐interventions and the level of community transmission were reported in most studies, this allowed the results to be interpreted according to context but not to be systematically compared through subgroup analysis. Modelling studies across all intervention categories differed in the methodologies they employed and assessed a broad range of potential factors, generally relating to properties of the pandemic, the broader community context, and the presence or absence of other measures being implemented in the communities, such as:
COVID‐19 pandemic: studies suggest that the level of community transmission and the proportion of asymptomatic cases play a role;
susceptibility of the target population: studies suggest that the susceptibility of the target population of the intervention to the pandemic may influence the effectiveness of the intervention (i.e. younger students being less susceptible than older students);
other public health measures: whether other public health measures, such as a stay‐at‐home order and testing and contact tracing, are in place in the communities where school measures are implemented;
implementation of the intervention: factors related to the earlier or later timing of implementation of the intervention, and compliance with the measures influenced effectiveness.
Certainty of the evidence
Overall, the GRADE process found the certainty of evidence to be low or very low for each intervention category and outcome combination; we can therefore not be confident in the findings. The true effects may be or are likely to be substantially different from the estimates of effect described in the studies. Across all outcomes, we downgraded the evidence to 'very low' mainly due to risk of bias and indirectness. We also downgraded some outcomes due to inconsistencies and imprecision.
In observational studies, we downgraded for risk of bias if we assessed any of the studies contributing to a body of evidence as having an overall rating of moderate or serious risk of bias in ROBINS‐I (Sterne 2016). Across all observational studies, risk of bias was most often introduced due to deviations from intended interventions or due to missing data. We assessed one study using QUADAS‐2 (Whiting 2011), as it assessed the effect of screening and intervention with respect to how many cases could be identified. We also downgraded this study for risk of bias due to lack of clarity about strategies to mitigate bias in the study.
Modelling studies contributed evidence to all four intervention categories. Although modelling studies differed in quality, we downgraded most bodies of evidence comprising modelling studies due to serious concerns about the quality of the modelling in at least some aspects. The frequent lack of external validation procedures warranted concerns about the validity of predictions in most studies. Other quality concerns varied across studies, but most often had to do with the inappropriate or unrealistic assumptions related to structural elements of the model or the model input data, and an inappropriate or insufficient assessment of uncertainty.
Further, across modelling studies, we consistently downgraded the evidence for imprecision if only a single study contributed to one outcome, as this limited our confidence that the predictions in that study were a precise estimate of true effects. We also downgraded for imprecision when models had high levels of uncertainty, and when multiple studies showed unclear effects. Some of the modelling studies provided no estimates of effect (e.g. data presented in a graphical way), and many studies provided estimates of effect (e.g. number of deaths avoided) with insufficient information on the precision (e.g. confidence intervals). Given the nature of the data and models, it is plausible that the uncertainty in estimates is wide, and such information would be necessary for an appropriate interpretation of the study findings. We therefore downgraded for imprecision as well. We also downgraded studies for indirectness due to concerns about the external validation of the model. Specifically, we downgraded evidence for indirectness when there was no external validation of the model(s), as it created uncertainties in assessing how directly the model outputs relate to our review question. Despite the challenges of external validation, particularly within the context of an ongoing pandemic, it is important that findings are generalisable to a wider population; the lack of external validity reduced our confidence. In some cases, we downgraded for inconsistency due to inconsistent effects in the studies contributing to the outcome (i.e. when effect estimates across studies varied).
Potential biases in the review process
There are several limitations to this review. We followed transparent and systematic rapid review conduct throughout the review process, whilst keeping to a tight timeline. The protocol was approved by Cochrane in January 2021 (Krishnaratne 2021). The search, according to the approved search strategy was conducted in December 2020. We only included the data from studies published before 8 December 2020 in this review. We conducted a search of the Cochrane COVID‐19 Study Register in August 2021; however, we did not conduct data extraction or risk of bias assessment on the 16 studies awaiting classification (Studies awaiting classification). This constitutes a potential source of bias. We will, however, consider these studies in a future update of this rapid review.
Whilst most aspects of the review were completed in accordance with systematic reviewing according to Cochrane standards, we followed the Cochrane guidance on conducting rapid reviews (Garritty 2020). Potential biases related to the rapid nature of the review were mitigated through regular team meetings, piloting and calibration at each screening and the data extraction stages, and maintaining a list of rolling questions to ensure consistency. This rapid review also built upon a preceding scoping review (Krishnaratne 2020).
In order to mitigate bias in decision‐making and interpretation and synthesis of findings, the inclusion criteria covered a large range of study designs and included preprint publications due to the novel nature of the COVID‐19 challenges and the associated young and rapidly growing body of literature. We also applied GRADE to assess the certainty of evidence according to each potential category of intervention and outcome, and assessed studies for risk of bias/quality using appropriate risk of bias assessment tools according to study design. This included an adapted tool for modelling studies which was recently designed for a rapid review of international travel‐related control measures to contain COVID‐19 (Burns J 2021).
Our comprehensive search strategy was designed and undertaken by an information specialist in line with Cochrane guidance for rapid reviews. The search incorporated databases to capture preprints. Inclusion of more databases may have captured further relevant studies but may also have lengthened the time needed to carry out the review, whereas the current situation demands timely evidence to inform policy‐makers’ decisions around school measures.
The dominance of modelling studies is a potential source of bias within this rapid review. As most of the included studies handle complex questions and phenomena, mathematical models make use of a combination of epidemiological knowledge and modelling assumptions in an attempt to answer these questions. Such modelling studies are prone to introducing risk of bias due to many implicit or explicit assumptions and a usually considerable amount of input data or parameters that have to be specified. However, it is typical of a global pandemic that evidence is needed rapidly, and data collection is often difficult and complex, such that modelling studies are used as a method of prediction to inform policy decisions in lieu of primary data. A further issue is that many modelling studies did not clearly describe the hypothetical interventions implemented and did not allow for the separate analysis of how individual intervention components of multicomponent or combined interventions exerted effects on the respective outcomes. Further, the assumptions made within the models varied across studies, adding another source of heterogeneity.
As mentioned previously, many of the studies that we identified assessed the impact of measures implemented within the school setting on outcomes within the broader community, even if they did not have any direct connection with the school setting. This was a limitation that we identified in the scoping review (Krishnaratne 2020), and we were thus aware of it ahead of conducting this review. Allowing for extraction of data pertaining to the general population allowed us to capture studies looking at broader population impacts, and to assess whether or not they also looked at impacts on populations directly affected by the school setting.
A key limitation to this review was the lack of focus on the unintended consequences of measures implemented in the school setting to control the COVID‐19 pandemic. When we developed the protocol for this review (Krishnaratne 2021), we decided that the most pressing question was the effectiveness of measures implemented in the school setting and that this review should thus focus primarily on studies assessing the effectiveness of measures; if included studies also reported on harms, we decided we would also examine these data, but that would not be a primary focus of the review. A separate scoping review of the unintended consequences of school measures and potential adverse health effects and broader social harms of school measures is currently ongoing (Kratzer 2021).
Another potential limitation to this review is that we limited the setting to primary and secondary schools, and did not consider early childhood or university settings. These settings are important in their own right, however, given the differences in the ages of these target groups and the non‐compulsory nature of childcare and education in these settings, we anticipated that the measures implemented in these settings would be very different from those implemented in the school setting, as defined in the protocol for this review.
A further limitation to this review is that the risk of bias assessment was conducted by a single review author, with a second review author verifying the ratings. While this is in accordance with the Cochrane interim guidance on rapid reviews (Garritty 2020), it has to be acknowledged that this is prone to more subjectivity than an assessment in duplicate.
In terms of language, we did not consider databases in other languages, and might therefore have missed some studies. Lastly, most of the studies included in this review are preprints, which did not undergo peer review. While we endeavoured to mitigate this through thorough quality appraisal by the review authors, these studies may nevertheless be more prone to bias and quality concerns than peer‐reviewed studies.
Finally, a major limitation of this review is the fact that we identified all the included studies in December 2020, almost one year ago. We conducted a top‐up search in August 2021 and identified 16 new studies (Characteristics of studies awaiting classification), but we have not carried out data extraction on these studies. Therefore, this review reflects the state of the literature in December 2020, and it is highly likely that the effects of these interventions would be very different now, especially given the rapid and widespread advancements in prevention and containment measures, most notably, the COVID‐19 vaccines and increases in testing capacity, as well as the rise of more transmissible variants of the virus. An update to this review is imminent and will include those studies identified in the top‐up search, as well as additional studies identified through a newer search.
Agreements and disagreements with other studies or reviews
Overall, this review, whilst mainly comprising modelling studies, suggests that measures to reduce transmission in schools can have a positive impact on a number of outcomes. This is supported by primary quantitative data in Wales (Thompson 2021), which has shown that with mitigation strategies in place, the occurrence of positive COVID‐19 cases was shown to not increase the risk of staff to subsequently test positive. The occurrence of positive cases in a students' year group also did not lead to an increased risk for these students. However, the specific measures in place in the schools studied have not been investigated; further investigation is called for (Thompson 2021). The safe reopening of schools is particularly important due to the well‐documented adverse effect of school closures, including impacts on nutrition, physical activity, mental health and overall well‐being (Engzell 2021; Golberstein 2020; UNESCO 2021). There is also evidence that vulnerable children are more at risk without the safety net of the school setting, and that health and educational inequalities are widened (Viner 2020).
Authors' conclusions
Implications for practice
While there are some limitations with the evidence that we identified, and the overall certainty of evidence was generally very low, our review suggests that many measures implemented in the school setting can have positive impacts on the transmission of SARS‐CoV‐2, and on healthcare utilisation outcomes related to COVID‐19. We identified a range of different interventions that worked in different ways to achieve intended outcomes.
The most commonly assessed measure in this review was reducing the opportunity for contacts in and on the way to schools. While showing largely positive effects with regards to transmission‐related outcomes, none of the included studies in the review reported on adverse effects in terms of psychosocial health, educational outcomes or socioeconomic inequality. For studies that focused on phased reopening, this was a key strategy to reduce cases, transmission number and hospitalisations. A key detail for the implementation of this is distinguishing by age groups, with opening/reopening of primary schools consistently showing a smaller impact on these outcomes, thus suggesting it may be safer to open primary, versus secondary schools. We are unable to draw conclusions on the practicalities of such measures as most studies fell short of providing any insights into the reality of implementing such measures.
Studies focusing on measures to make contacts safer provided less clear evidence. Whilst studies that focused on the effect of masks were often multicomponent interventions, results suggested that mask wearing may be an important strategy for facilitating reopening of schools going forwards. A recent review has concluded that the benefit of public mask wearing is highest when compliance is high (Howard 2021), and that public compliance to mask wearing was associated with lower SARS‐CoV‐2/COVID‐19 rates (Fischer 2021). However, these studies did not look specifically at the school setting. There were insufficient studies in this review to draw conclusions with regards to the effectiveness of ventilation interventions. Whilst it was shown within one study that air purifiers do reduce the dose of particles containing RNA virus in an experimental scenario (Curtius 2020), the quality of this evidence was low. Installing air purifiers in schools might entail significant costs and resources (e.g. energy, disposal of used filters), whilst at the same time contributing to widening inequalities with regards to some districts, states or nations being unable to afford ventilators/air purifiers.
Among studies looking at measures to detect, trace, and quarantine cases within schools it was found that such interventions could lead to reductions in the COVID‐19 infection/transmission rate among students, teachers, and staff. The most effective testing and isolation strategies used a combination of early testing together with symptom screening and isolation of symptomatic cases. Students attending schools employing a hybrid approach were found to miss fewer days of school due to quarantines. This suggests that surveillance and isolation measures may need to be tailored to the specific context in which they are implemented and should take community‐level factors into account in their design. There were also important findings relating to cost, and days lost in the classroom, which will need to be considered within future policy decisions, suggesting that surveillance testing of at‐risk populations is cheaper than universal testing.
The 16 studies in the 'Studies awaiting classification' category may alter the conclusions of the review once assessed. There are a number of studies that we have identified, but that have not yet been incorporated in this review. If these studies are deemed to be important in terms of sample size or direction of effect, there may be a degree of change in the results and conclusions of this review. This is particularly important given the rapid and widespread advancements in prevention and containment measures, such as the COVID‐19 vaccines and increases in testing capacity, as well as the rise of more transmissible variants of the virus. Like the current review, the majority of the studies awaiting classification used modelling study designs (n=8), followed by observational studies (n=7); one study used a randomized controlled study design. Nine studies were based in the USA and two were in Canada, with one study each in Belgium, Brazil, Italy, Israel, and the United Kingdom.
Implications for research
Future research should continue to refine the assessment of interventions and the factors that influence their effectiveness, such as the level of community transmission and adherence to measures. For example, while studies focused on reducing contacts within schools found that a smaller cohort was consistently associated with a lower level of transmission and fewer days of education lost, further primary research is required to be conducted in real‐world settings to help to determine the exact effect of this measure, as well as the extent to which it is practical within schools in various countries where resources, such as teaching staff and classroom space are varied and finite. In regards to mental and social health, and educational outcomes, these need to be at the forefront of future research to ensure that interventions aimed at reducing transmission do not do so to the detriment of these other important outcomes for students. The previously mentioned scoping review on unintended consequences of measures implemented in the school setting will address this to some extent (Kratzer 2021).
A major gap in the evidence that we identified is the fact that very few of the studies included here accounted for contextual factors in their assessment of intervention effectiveness. The largest intervention category we identified was 'measures to reduce contacts'. This often meant that interventions required only some students to attend school on certain days while others stayed at home and studied online. It also often meant that there needed to be significant space between students in classrooms. This is important, as many of the interventions described would require financial resources to provide virtual learning tools and infrastructure, and the availability of space for effective implementation. Indeed, most of the studies we identified either used data from, or were focused on, high‐income countries, but regional differences, or even school‐level differences relating to socioeconomic status, might influence how interventions are implemented and taken up, and this was rarely examined within the identified studies.
Also, while we acknowledge the challenge of collecting real‐world data in the context of a pandemic, and the benefits of using modelling studies to provide insight into situations where empirical data collection is not easy, future research should employ observational and/or experimental and quasi‐experimental study designs. This is essential for understanding how these interventions work, for whom, and in what contexts. Despite the strengths and value of modelling studies, real‐world data will best be able to answer these key research questions, and the pandemic presents an opportunity to use internally valid experimental or quasi‐experimental approaches to understand a complex and rapidly changing situation.
Further, many of the studies we identified described interventions that were multifaceted, and employed different types of measures at the same time. In future research, it would be helpful to go beyond presenting findings about multiple measures together and to pull apart the effects of individual intervention components. This will also have implications for practice as it will allow decision makers to understand which components of the interventions are most effective. Also, importantly, when we ran the original search for this rapid review, no vaccines against SARS‐CoV‐2 had been developed. The development and subsequent implementation of these vaccines will have greatly changed the evolution of the pandemic, particularly in the school setting, and especially now as use of the vaccines in younger populations is not yet widely approved. The implications of the vaccine on future practices surrounding the control of the pandemic in the school setting will need to be evaluated in future research.
With the evidence base on COVID‐19 and the impact of measures implemented in the school setting to control the pandemic rapidly expanding and constantly changing, and with the anticipation that modelling studies will continue to form the bulk of the evidence base, it is critical that future modelling studies improve reporting and technical documentation to allow for adequate assessment of their quality. Finally, to ensure that the best available evidence informs decision‐making about safely keeping schools open in the context of the pandemic, future research should employ a range of epidemiological designs and assessment tools to assess the broad impacts of these measures, including all potential benefits and harms in terms of education, and social and mental health. Given the growing evidence base and the developments in the control of the pandemic, particularly the introduction of vaccines, as well as in anticipation of new studies that will be published in the near future, we plan to update this review again in 2022.
The majority of studies were conducted or based in high‐income countries. This may have implications for low‐ and middle‐income countries, which have been shown to have more varied and expansive detrimental effects linked to school closures, such as widening inequalities, children missing out on vaccinations, parents losing vital income and children dropping out of school entirely (Viner 2021b). Thus, there is a need for further research to investigate the effect of non‐pharmaceutical interventions on safe school reopening within low‐ and middle‐income countries.
It is important to note that this is a fast‐moving research field. Since December 2020, when we conducted our searches, 16 more studies examining school measures have been published (Asgary 2021; Bilinski 2021; Bosslet 2021; Cruz 2021; Ertem 2021; Gandini 2021; Lessler 2021; Liu 2021; Miller 2021; Pavilonis 2021; Reinbold 2021; Somekh 2021; van den Berg 2021; Willem 2021; Young 2021; Yuan 2021). They highlight, however, that the evidence base is growing further, and that a future update to this review will be important.
What's new
| Date | Event | Description |
|---|---|---|
| 31 January 2022 | Amended | Minor edits to title |
History
Review first published: Issue 1, 2022
Acknowledgements
We would like to thank Robin Featherstone for designing and running the searches in the databases. Moreover, several of the co‐authors with children were only able to accomplish this review under ongoing pandemic circumstances due to continuous support through their support networks.
Cochrane Public Health supported the development of this review. The following people conducted the editorial process for this review:
Sign‐off Editor (final editorial decision): Luke Wolfenden, The University of Newcastle
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Joey Kwong, Cochrane Editorial & Methods Department
Editorial Assistant (conducted editorial policy checks and supported editorial team): Leticia Rodrigues, Cochrane Editorial & Methods Department
Copy Editor (copy‐editing and production): Clare Dooley, c/o Cochrane Copy Edit Support
Peer‐reviewers (provided comments and recommended an editorial decision*): Archana Koirala, National Centre for Immunisation Research and Surveillance, Sydney, Australia (clinical review); Emma Dobson, School of Education at Durham University (clinical review); Sebastian Walsh, Cambridge Public Health, University of Cambridge (clinical review); Ian Shemilt, EPPI Centre, University College London (UCL), UK (methods review); Gautham Suresh, Baylor College of Medicine; Texas Children's Hospital, Houston, Texas (DTA review); Robert Walton, Cochrane UK (summary versions review); Jennifer Hilgart, Cochrane Editorial & Methods Department (methods review); Theresa Moore, Cochrane Editorial & Methods Department; the National Institute for Health Research Applied Research Collaboration West (NIHR ARC West), University Hospitals Bristol NHS Foundation Trust; Population Health Sciences, Bristol Medical School, University of Bristol, UK (methods review); Ruth Foxlee, Cochrane Editorial & Methods Department (search review). One additional peer reviewer provided consumer peer review but chose not to be publicly acknowledged. *Lisa Bero, Senior Editor of Cochrane Public Health and Health Systems, provided comments on this review, but was not otherwise involved in the editorial process or decision‐making for this review.
Appendices
Appendix 1. List of existing (systematic) reviews and guidelines for forward and backward searches
D'Angelo D, Coclite D, Napoletano A, Fauci AJ, Latina R, Iacorossi L, et al. Strategies for exiting COVID‐19 lockdown for workplace and school: a scoping review protocol. medRxiv. 2020:2020.09.04.20187971.
Chinese Center for Disease Control and Prevention. Health protection guideline of schools and other educational institutions during COVID‐19 outbreak. 2020 Apr 6;54(4):348‐350.
Strategy and Policy Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. Interim guidelines for prevention and control of COVID‐19 for students back to school. Pubmed.gov. 2020.08.10;41(8):1195‐1196.
Araújo LA, Veloso CF, Souza MC, Azevedo JM, Tarro G. The potential impact of the COVID‐19 pandemic on child growth and development: a systematic review. J Pediatr (Rio J). 2020 Sep 23: 10.1016/j.jped.2020.08.008.
Cohena R, Delacourtb C, Gras‐Le Guenc C, Launayc E. COVID‐19 and schools. Guidelines of the French Pediatric Society. ScienceDirect. j.arcped.2020.09.001.
Fardin MA. COVID‐19 and anxiety: a review of psychological impacts of infectious disease outbreaks. Archives Clinical Infectious Disease. 10.5812/archcid.102779.
Kneale D, O'Mara‐Eves A, Rees R, Thomas J. School closure in response to epidemic outbreaks: systems‐based logic model of downstream impacts. F1000Res. 2020;9:352. 10.12688/f1000research.23631.1.
Nussbaumer‐Streit B, Mayr V, Dobrescu AI, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID‐19: a rapid review. Cochrane Database Syst Rev. 2020;4(4):CD013574. 10.1002/14651858.CD013574.
Abadio de Oliveira W, Luiz da Silva J, Monezi Andrade AL, De Micheli D, Carlos DM, Silva MA, et al. Adolescents’ health in times of COVID‐19: a scoping review. Cad. Saúde Pública. 2020, vol.36, n.8, 10.1590/0102‐311x00150020.
Viner RM, Mytton OT, Bonell C. Susceptibility to SARS‐CoV‐2 infection among children and adolescents compared with adults: a systematic review and meta‐analysis. JAMA Pediatrics. 2020;e204573. 10.1001/jamapediatrics.2020.4573.
Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID‐19: a rapid systematic review. The Lancet Child & Adolescent Health. Vol 4, Issue 5. 2020:10.1016/S2352‐4642(20)30095‐X.
WHO. Considerations for school‐related public health measures in the context of COVID‐19. 202.09.14. WHO/2019‐nCoV/Adjusting_PH_measures/Schools/2020.2.
Juneau CE, Pueyo T, Bell M, Gee G, Collazzo P, Potvin L. Evidence‐based, cost‐effective interventions to suppress the COVID‐19 pandemic: a systematic review. medRxiv. 2020.04.20.20054726.
Brooks SK, Smith LE, Webster RK, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children's social contact: rapid evidence review. Euro Surveillance. 2020;25(13):2000188. 10.2807/1560‐7917.ES.2020.25.13.2000188.
New York State Education Department. Recovering, Rebuilding, and renewing: the spirit of New York’s schools ‐ reopening guidance.
Simon A, Huebner J, Berner R, Munro AP, Exner M, Huppertz H‐I, et al. Measures to maintain regular operations and prevent outbreaks of SARS‐CoV‐2 in childcare facilities or schools under pandemic conditions and co‐circulation of other respiratory pathogens. GMS Hyg Infect Control. 2020;15:Doc22. Published 2020 Sep 15. 10.3205/dgkh000357.
Walger P, Heininger U, Knuf M, Exner M, Popp W, Fischbach T, et al. Children and adolescents in the CoVid‐19 pandemic: Schools and daycare centers are to be opened again without restrictions. The protection of teachers, educators, carers and parents and the general hygiene rules do not conflict with this. GMS Hygiene and Infection Control. 2020;15:Doc11. Published 2020 May 28. 10.3205/dgkh000346.
CDC www.cdc.gov/coronavirus/2019‐ncov/community/schools‐childcare/schools.html
CDC www.cdc.gov/coronavirus/2019‐ncov/community/schools‐childcare/k‐12‐testing.html
Leclerc QJ, Fuller NM, Knight LE, Funk S, Knight GM. What settings have been linked to SARS‐CoV‐2 transmission clusters? Wellcome Open Research. 2020;5:83. 5 June 2020. 10.12688/wellcomeopenres.15889.2.
National Collaborating Centre for Methods and Tools. Rapid Evidence Review: What is the specific role of daycares and schools in COVID‐19 transmission? Update 8. 5 October 2020.
Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID‐19: a rapid systematic review. Lancet Child Adolescent Health. 2020;4(5):397‐404. 10.1016/S2352‐4642(20)30095‐X.
Viner RM, Mytton OT, Bonell C, Melendez‐Torres GJ, Ward JL, Hudson L, et al. Susceptibility to and transmission of COVID‐19 amongst children and adolescents compared with adults: a systematic review and meta‐analysis. medRxiv. 2020.05.20.20108126.
Appendix 2. Search strategies
Database: Ovid MEDLINE(R) ALL 1946 to December 08, 2020
Date search conducted: 9 December 2020
Strategy:
1 Coronavirus/ (4179)
2 Coronavirus Infections/ (44000)
3 COVID‐19/ [MeSH 2021 ‐ Included for future updates] (0)
4 SARS‐CoV‐2/ [MeSH 2021 ‐ Included for future updates] (0)
5 COVID‐19.rs. (39029)
6 severe acute respiratory syndrome coronavirus 2.os. (33023)
7 (2019 nCoV or 2019nCoV or 2019‐novel CoV).tw,kf. (1365)
8 (corona vir* or coronavir* or neocorona vir* or neocoronavir*).tw,kf. (45701)
9 COVID.mp. (78541)
10 COVID19.tw,kf. (937)
11 (nCov 2019 or nCov 19).tw,kf. (99)
12 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").mp. (26538)
13 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").mp. (37903)
14 or/1‐13 [Set 1: SARS‐CoV‐2] (96498)
15 School Teachers/ (1606)
16 Schools/ (39273)
17 Students/ (60547)
18 ((campus* or class* or employee* or pupil* or staff* or student$1 or teacher$1) adj3 (college$1 or elementary or junior or middle* or primary or secondary)).tw,kf. (54031)
19 educational setting$1.tw,kf. (1544)
20 (gradeschool* or highschool* or kindergarten* or school* or schoolbus*).tw,kf. (296102)
21 or/15‐20 [Set 2: Primary or secondary school settings] (368794)
22 and/14,21 [Sets 1 & 2] (1530)
23 ((clos* or open* or re entry or re open* or re start* or reopen* or restart* or resum* or suspen*) and (highschool$1 or kindergarten* or school$1)).ti. (854)
24 22 or 23 [Concept searches combined with specific title search] (2256)
25 limit 24 to "humans only (removes records about animals)" (2251)
26 limit 25 to yr="2020‐Current" (1521)
27 remove duplicates from 26 (1476)
Database: Ovid Embase 1974 to 2020 December 07
Date search conducted: 9 December 2020
Strategy:
1 coronaviridae/ (1064)
2 exp coronavirinae/ (22562)
3 exp coronavirus infection/ (24193)
4 (2019 nCoV or 2019nCoV or 2019‐novel CoV).ti,ab,kw. (1353)
5 (corona vir* or coronavir* or neocorona vir* or neocoronavir*).ti,ab,kw. (44994)
6 COVID.af. (72428)
7 COVID19.ti,ab,kw. (947)
8 (nCov 2019 or nCov 19).ti,ab,kw. (68)
9 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2").af. (25308)
10 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2").af. (22762)
11 or/1‐10 [Set 1: SARS‐CoV‐2] (105031)
12 elementary student/ (1557)
13 high school/ (21166)
14 high school student/ (8046)
15 kindergarten/ (2934)
16 middle school/ (1838)
17 middle school student/ (1405)
18 primary school/ (13129)
19 *school/ (17931)
20 school teacher/ (1646)
21 *student/ (26634)
22 ((campus* or class* or employee* or pupil* or staff* or student$1 or teacher$1) adj3 (college$1 or elementary or junior or middle* or primary or secondary)).ti,ab,kw. (67575)
23 educational setting$1.ti,ab,kw. (1801)
24 (gradeschool* or highschool* or kindergarten* or school* or schoolbus*).ti,ab,kw. (360655)
25 or/12‐24 [Set 2: Primary or secondary school settings] (431646)
26 and/11,25 [Sets 1 & 2] (1341)
27 ((clos* or open* or re entry or re open* or re start* or reopen* or restart* or resum* or suspen*) and (highschool$1 or kindergarten* or school$1)).ti. (646)
28 26 or 27 [Concept searches combined with specific title search] (1872)
29 (animal experiment/ or exp animal/) not exp human/ (5055006)
30 28 not 29 (1863)
31 limit 30 to yr="2020‐Current" (1238)
32 remove duplicates from 31 (1216)
Database: Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 11) in the Cochrane Library
Date search conducted: 9 December 2020
Strategy:
#1 [mh ^Coronavirus] 2
#2 [mh ^"Coronavirus Infections"] 506
#3 [mh ^"COVID‐19"] 0
#4 [mh ^"SARS‐CoV‐2"] 0
#5 ("2019 nCoV" or 2019nCoV or "2019 novel CoV"):ti,ab,kw 10
#6 ((corona next vir*) or coronavir* or (neocorona next vir*) or neocoronavir*):ti,ab,kw 2093
#7 COVID:ti,ab,kw 3420
#8 COVID19:ti,ab,kw 228
#9 ("SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2"):ti,ab,kw 1317
#10 ("SARS coronavirus 2" or "SARS‐like coronavirus" or "Severe Acute Respiratory Syndrome Coronavirus‐2"):ti,ab,kw 250
#11 {or #1‐#10} 3696
#12 [mh ^"School Teachers"] 118
#13 [mh ^Schools] 1994
#14 [mh ^Students] 2686
#15 ((campus* or class* or employee* or pupil* or staff* or student* or teacher*) near/2 (college* or elementary or junior or middle* or primary or secondary)):ti,kw 2968
#16 (educational next setting*):ti,ab,kw 116
#17 (gradeschool* or highschool* or kindergarten* or school* or schoolbus*):ti,kw 20924
#18 {or #12‐#17} 24604
#19 #11 and #18 15
#20 ((clos* or open* or "re entry" or (re next open*) or (re next start)* or reopen* or restart* or resum* or suspen*) and (highschool* or kindergarten* or school*)):ti,ab 390
#21 #19 or #20 405
#22 #19 or #20 in Trials 180
#23 #19 or #20 with Publication Year from 2020 to 2020, in Trials 26
Database: Cochrane COVID‐19 Study Register
URL:https://covid-19.cochrane.org/ (searched via the Cochrane Register of Studies: https://crsweb.cochrane.org/)
Date search conducted: 9 December 2020
Strategy:
1 ((campus* OR class* OR employee* OR pupil* OR staff* OR student* OR teacher*) ADJ3 (college* or elementary OR junior OR middle* OR primary OR secondary)):TI,AB AND INREGISTER 148
2 (educational NEXT setting*):TI,AB AND INREGISTER 2
3 (gradeschool* OR highschool* OR kindergarten* OR school* OR schoolbus*):TI,AB AND INREGISTER 597
4 #1 OR #2 OR #3 708
Contents note: The Cochrane COVID‐19 Study Register contains study references from ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), PubMed, Embase.com, medRxiv and other hand‐search articles from publishers' websites.
Database: Ovid ERIC 1965 to September 2020
Date search conducted: 9 December 2020
Strategy:
1 ("2019 nCoV" or 2019nCoV or "2019 novel CoV" or coronavirus or COVID or COVID19 or "nCov 2019" or "nCov 19" or "SARS‐CoV‐2" or "SARS‐CoV2" or SARSCoV2 or "SARSCoV‐2" or "SARS coronavirus 2" or "SARS‐like coronavirus").ti,ab. (134)
2 limit 1 to yr="2020‐Current" (133)
Database: WHO COVID‐19 Global literature on coronavirus disease
URL:https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/
Date search conducted: December 09, 2020
Strategy:
(tw:(school* AND (elementary OR grade* OR high* OR junior OR kindergarten* OR middle* OR primary OR secondary))) OR (tw:(highschool*)) (1629)
Source: Google
Date search conducted: 10 December 2020
Strategy: (coronavirus | covid | SARS‐CoV‐2) (children | pupil | staff | student | teacher) ("educational setting" | "educational settings" | gradeschool | highschool | kindergarten | school)
Searched the first 10 pages of results (n=100)
Kept 53
Top up Search conducted in August 2021
Database: Cochrane COVID‐19 Study Register
URL:https://covid-19.cochrane.org/ (searched via the Cochrane Register of Studies: https://crsweb.cochrane.org/)
Date search conducted: 5 August 2021
Strategy:
1 ((campus* OR class* OR employee* OR pupil* OR staff* OR student* OR teacher*) ADJ3 (college* or elementary OR junior OR middle* OR primary OR secondary)):TI,AB AND 09/12/2020_TO_05/08/2021:CRSCREATED AND INREGISTER 360
2 (educational NEXT setting*):TI,AB AND 09/12/2020_TO_05/08/2021:CRSCREATED AND INREGISTER 15
3 (gradeschool* OR highschool* OR kindergarten* OR school* OR schoolbus*):TI,AB AND 09/12/2020_TO_05/08/2021:CRSCREATED AND INREGISTER 1163
4 #1 OR #2 OR #3 1431
Contents note: The Cochrane COVID‐19 Study Register contains study references from ClinicalTrials.gov, WHO International Clinical Trials Registry Platform (ICTRP), PubMed, Embase.com, medRxiv and other hand‐search articles from publishers' websites.
Appendix 3. Data extraction form
Study information
Study ID
Study title
Publication year
Study source (journal, report, preprint publication)
For preprint publication only: date of publication
Study design
Study type (e.g. modelling study, cross‐sectional study, econometric study)
Data type (e.g. modelling versus observational data)
Verbal summary of study (e.g, stochastic discrete event simulation model)
Comments
Population and setting
-
Population group targeted by intervention (students, teaching staff, school staff, parents, other family members, other individuals outside school)
Type of population (i.e. students versus teachers versus school staff)
Age
Risk profile (e.g. elevated risk of infection, adverse health effects due to COVID‐19, students with special learning needs, students from disadvantaged families)
Characteristics of school (e.g. socioeconomic status of school location or student’s families, catchment area)
Study setting (e.g. primary school, high school, other school forms)
Comments
Intervention
Broad measure category
Measures reducing the opportunity for contacts
Measures making contacts safer
Surveillance and response measures
Multicomponent intervention
Verbal summary of the measures
Duration of the intervention
Level of intervention (i.e. individual, cohort, school, macro, multiple)
Comments
Outcomes (repeated for each outcome) and results
-
Outcome category
Transmission‐related outcomes,
Healthcare utilisation,
Other health outcomes and
Societal, economic and ecological implications.
Description of outcome
Outcome attributable to measures (yes/no)
Level on which outcome is assessed (i.e. students, teachers, staff, wider community, general population)
Length of follow‐up
Estimate related to the impact of measure(s) implemented in the school setting
Summary of overall impact of measure(s) implemented in the school setting
Comments
Implementation
Implementation outcomes (e.g. adherence, fidelity)
Implementation strategies (e.g. enforcement, communication and feedback)
Implementation agents (e.g. parents, teachers, bus drivers)
Context
Country in which measure is implemented
Co‐interventions
Other relevant contextual factors (geographical, sociocultural, socioeconomic, ethical, political, legal, and epidemiological context on the macro (e.g. international, national or state level) and meso level (e.g. community)
Comments
Appendix 4. QUADAS‐2 domains as applied in the rapid review
| Domain | Signalling question | Application in this review | |
| Domain 1: participant selection | A. Risk of bias | 1.1 Was a consecutive or random sample of participants enrolled? | Assess how the individuals screened and/or quarantined as part of the study were determined; where all individuals were screened (e.g. as part of a blanket screening) or where a random sample was selected, a risk of bias is not likely. |
| 1.2 Was a case‐control design avoided? | If disease status was used to determine the sample, a risk of bias should be considered. | ||
| 1.3 Did the study avoid inappropriate exclusions? | Any exclusions to screening/quarantine programmes should be justified; however even with justification, exclusions could lead to bias, especially where the screening and disease status of those excluded are unknown. Thus, if no exclusion criteria were applied, the risk of bias is low. | ||
| Comments | ‐ | ||
| 1. Could the selection of participants have introduced bias? | Consider whether bias may have arisen from 1.1 to 1.3 | ||
| B. Concerns regarding applicability | Describe included participants (prior testing, presentation, intended use of index test and setting) | Consider those individuals screened, and whether they are representative of individuals likely to be screened during the COVID‐19 pandemic. These studies should be therefore regarded as having a low external validity. | |
| Is there concern that the included participants do not match the review question? | See above | ||
| Domain 2: index test(s) | A. Risk of bias | 2.1 Can we be sure that those identified in index test (true and false positive screening results) were identified by the index test (e.g. automated fever scanner) rather than any other means (e.g. self‐reporting)? | Consider how those screened positive were determined – all ‘positives’ should stem from the symptom screening and not from any other procedures (e.g. self‐reporting of cases missed by the screening intervention; based on respiratory symptoms). |
| 2.2 Were the index test results interpreted without knowledge of the results of the reference standard? | Consider whether, for example, the results of the PCR test were known when symptom or fever screening was applied to individuals. | ||
| 2.3 If a threshold was used, was it prespecified? | Consider for temperature screening, whether the cut‐off for determining acceptable/high temperature was predefined; for symptom screening, consider whether any symptom or a certain threshold of symptoms was used in defining whether an individual was symptomatic and whether this was predefined. | ||
| Comments on risk of bias | ‐ | ||
| 2. Could the conduct or interpretation of the index test have introduced bias? | Consider whether bias may have arisen from 2.1 to 2.3 | ||
| B. Concerns regarding applicability | Describe the index test and how it was conducted and interpreted | Consider the screening/quarantine programme assessed, and whether it is representative of one likely to be applied as part of screening programmes during the COVID‐19 pandemic. | |
| Is there concern that the index test, its conduct, or interpretation differ from the review question? | See above | ||
| Domain 3: approach to identify cases and timing | A. Risk of bias | 3.1 Is the reference standard (the approach to identify and classify 'cases') likely to correctly classify the target condition (is there active infection with SARS‐CoV‐2)? | Consider whether the approach to identify cases may have missed relevant cases or classified individuals not infected with SARS‐CoV‐2 as a case. Any method other than positive PCR test results can be considered at high risk of bias. |
| For the studies using a case‐classification based on a positive PCR test, we assumed the risk of bias due to false positives as low due to the high specificity of the PCR test (in particular if the population is assumed to have a high risk of infection). | |||
| However, there is a considerable risk of false negatives for the PCR test, primarily due to the course of infection (e.g. very low probability of detection in the first days after infection), but also due to inadequate procedures for specimen collection, handling, transportation, or storage (e.g. if only a single test shortly after an infection is applied to a swab sample, the viral load in the individual may not have been high enough for detection, leading to a false‐negative test). | |||
| We therefore assume a high risk of bias in studies, where asymptomatic individuals do not receive at least two PCR tests and symptomatic individuals did not receive at least two PCR tests after symptom onset. | |||
| 3.2. Were the reference standard results interpreted without knowledge of the results of the index test? | Consider whether, for example, the results of the symptom screening were known when the classification was conducted. For PCR tests, where the risk of subjective judgements to have led to a risk of erroneously classifying a test result as negative or positive is regarded as low, this knowledge of the outcome of the index test is still regarded as leading to a low risk of bias. | ||
| Comments on risk of bias | ‐ | ||
| 3. Could the reference standard, its conduct, or its interpretation have introduced bias? | Consider whether bias may have arisen from 3.1 to 3.2 | ||
| Describe the reference standard and how it was conducted and interpreted | Consider the procedure for determining who receives the reference standard (the PCR test used to identify cases), and whether it is representative of that likely to be applied as part of screening programmes during the COVID‐19 pandemic. | ||
| B. Concerns regarding applicability | Is there concern that the target condition as defined by the reference standard does not match the review question? | See above | |
| Domain 4: flow and timing | 4.1. Did all participants receive the reference standard? | Consider whether all individuals received the reference test (the respective approach to identify and classify ‘cases’; in most cases likely the PCR test). | |
| For example, if only those who were screened positive (positive index test) and those who developed symptoms during a quarantine observational period were given a PCR test, as this would have led to a high risk of bias due to cases being missed). | |||
| If individuals declined to or for other reasons receive the reference standard (e.g. PCR test), this could lead to cases being missed, which puts the study at a high risk of bias. | |||
| Note: this is independent from 3.1, which evaluates the appropriateness of the approach to classify individuals as cases. | |||
| A. Risk of bias | 4.2. Did all participants receive the same reference standard? | Consider whether the procedure for identifying cases was the same across all individuals or whether it was applied differently without an adequate justification (e.g. individuals with symptoms receiving a different testing procedure). | |
| Studies, which used different approaches for classifying cases (e.g. some cases defined based on chest computer tomography and some based on PCR) would be classified as high risk of bias. | |||
| Studies in which the classification of cases is based on multiple PCR tests, we consider a high risk of bias if some symptomatic individuals were treated differently from other symptomatic individuals (e.g. some received more PCR tests than others) and if some of the asymptomatic individuals were treated differently from asymptomatic individuals. | |||
| 4.3. Were all participants included in the analysis? | Consider whether some individuals may have been excluded from the analysis; this would lead to a high risk of bias. | ||
| Is there likely no or a very low risk of attrition bias? | |||
| 4.4. Is it possible that the true disease status could have changed between the application of the index test and the reference standard? | Consider whether individuals may have become infected after the initial screening, e.g. if being quarantined among other infected individuals led to some initially non‐infected individuals becoming infected. If there is a high risk that individuals who were classified as cases were not cases (i.e. not infected with SARS‐CoV‐2) at the time when the index test was applied, this would lead to a high risk of bias. | ||
| Comments on risk of bias | ‐ | ||
| 4. Could the participants flow have introduced bias? | Consider whether bias may have arisen from 4.1 to 4.4 | ||
Appendix 5. Tool for criteria used for assessing the quality of individual modelling studies, developed from Burns J 2021
| Aspect | Source | Questions | Application in this review | Examples |
| Model structure | Philips 2006 | 1. Are the structural assumptions transparent and justified? | 1. Assess whether all structural model assumptions are explicitly stated and whether the authors substantiate these assumptions, either through theoretical reasoning or through prior knowledge from the literature. | Description of model type and defining equations |
| Comprehensible explanation of model variables and equations | ||||
| Description of features of the disease captured by the model, e.g. a randomly distributed incubation time | ||||
| Explanations of model structure implications by text or graphical representations visualising the simulation pathway, e.g. a scheme of the context being modelled | ||||
| Description of model limitations and simplifying assumptions | ||||
| 2. Are the structural assumptions reasonable, given the overall objective, perspective and scope of the model? | 2. Consider whether the structural assumptions are consistent with what is known about the phenomenon of interest in the literature. In case of disagreement, assess to what extent these discrepancies undermine the overall validity of results and conclusions. | |||
| Input data | Caro 2014 | 3. Are the input parameters transparent and justified? | 3. Assess whether the values of all input parameters are explicitly stated and whether the authors substantiate these values, either through theoretical reasoning or through prior knowledge from the literature. | Epidemiological characteristics known from other studies |
| Inputs to data calibration algorithms | ||||
| Table with input parameters and probability distributions used for probabilistic modelling | ||||
| Explanation and discussion of choice of parameter values with appropriate citations | ||||
| 4. Are the input parameters reasonable? | 4. Consider whether the input parameter values are consistent with what is known about the phenomenon of interest in the literature. In case of disagreement, assess to what extent these discrepancies undermine the overall validity of results and conclusions. | |||
| Validation (external) | Caro 2014 | 5. Has the external validation process been described? | 5. Assess whether there was a formal process of comparing the predictions of the model with: i) the data source that was used to build the model (dependent validation); ii) a data source that was not used to build the model, e.g. an independent country (independent validation); or iii) future values that did not intervene in model building (predictive validation). | Calibration of SEIR model to case data (dependent validation) |
| Prediction of a subset of observed data points based on training data set and comparison with validation data set (dependent validation) | ||||
| Prediction of data points of country/region that was not part of the model fitting and calibration process and comparison with observed data (independent validation) | ||||
| 6. Has the model been shown to be externally valid? | 6. Consider the extent to which model predictions agree with the data sources that were selected for the external validation process. | Prediction of future values that were not used in model building (predictive validation) | ||
| Validation (internal) | Caro 2014 | 7. Has the internal validation process been described? | 7. Assess whether there was a formal process of verifying the extent to which the mathematical calculations are consistent with the model’s specifications, e.g. in the form of a simulation study in which the mathematical calculations are applied to data that were simulated according to the model with known parameter values. | Application of the model on simulated data to establish that analyses work as intended |
| Code review process conducted by authors or by an independent source to ensure correct implementation of mathematical structure | ||||
| 8. Has the model been shown to be internally valid? | 8. Consider the extent to which the results of the internal validation process indicate that the mathematical calculations are consistent with the model’s specifications. | Independent replication of model | ||
| Uncertainty | Caro 2014 | 9. Was there an adequate assessment of the effects of uncertainty? | 9. Consider whether the robustness of results to alternative input parameter values or model assumptions was assessed, either by reporting the results of specific sensitivity analyses or through an app in which readers can themselves explore the effects of varying these model assumptions and input parameter values. | Structural and parameter sensitivity analyses |
| Inherent stochasticity due to simulation nature of model | ||||
| Reporting of an app in which effects of input changes can be tracked | ||||
| Propagation of present uncertainties to outcomes | ||||
| Was the model probabilistic, i.e. were parameter values fixed or sampled from a distribution? | ||||
| Is uncertainty transparently reported, described and justified? | ||||
| Transparency | Caro 2014 | 10. Was technical documentation, in sufficient detail to allow (potentially) for replication, made available openly or under agreements that protect intellectual property? | 10. Assess whether the description of the analyses (including model structure, input parameters, data sources and methods) is sufficiently detailed to allow for the replication of results. In particular, consider whether the code that was used to obtain the results is freely available and well documented. | Description of model which is qualitatively extensive enough to allow for scrutiny of other researchers (e.g. supplementary material) |
| Do authors encourage replication by clarifying a procedure to obtain code? | ||||
| Do the authors only refer to other, similar models for justification and detailed methodological description or do they provide their own documentation? |
Appendix 6. Comparison between preprints and published peer‐reviewed articles
| Preprint ID | Full publication ID | Differences |
| Burns A 2020 | Burns A 2021 | Title: changed Methods: more details on model, its validation and parameters Results: The authors focus on the two outcomes: outbreak duration and attack rate (less outcomes as presented in the preprint); results have been restructured to reduction in attack rate. The results do not seem to correspond to the ones reported in the preprint. The figure axes have been adapted to make the graphs more comparable. Discussion: in the first paragraph, the results are reported differently now (preprint: "For influenza, a 15% and 25% reduction in the attack rate is expected with one and two days of isolation" versus peer‐reviewed article: "For influenza, requiring isolation for fever is expected to reduce the typical attack rate by 29 (13–59)% and 70 (55–85)% with 1 and 2 days of post‐fever isolation, respectively."); for covid‐19, it is the same (preprint: "For COVID‐19, we find that one day of post‐fever isolation would reduce the attack rate by 8% in the conservative scenario where only 50% of the cases detect fever" versus peer‐reviewed article: "Indeed, we found that a 1‐day post‐fever isolation policy would reduce the attack rate in schools by 7 (5–14)%, and with 14 days of fever isolation we estimated that the attack rate would change by 14 (5–26)%." |
| Curtius 2020 | Curtius 2021 | Title: not changed Methods: one additional section in methods, some sections moved from results (Curtius 2020) to methods (Curtius 2021); number of particles emitted per hour changed from 68.400 to 198.000; estimated risk of one infection in the classroom 70% (Curtius 2021), instead of 33% (Curtius 2020); no implication for results (unless we misunderstood) Results: few smaller new sections (i.e. p9: "from the average...", "The OPS total number..."; added comparison with venting a room (p.10 and supplements); no change in overall results/conclusion: the overall conclusion "inhaled dose via airborne transmission is reduced by a factor of six when using air purifiers with an air exchange rate of 5.7/h" remains the same but there is one changed measurement in the results section: total aerosol mass (p.9, upper right): "56 mg/m3 at the beginning of the lesson to about 9 mg/m3" instead of reduction from 35 mg/m³ to 6 mg/m³ (Curtius 2020) Discussion: minor changes |
| Di Domenico 2020a | Di Domenico 2021 |
Title: not changed Background/intro: appears to be differences because of additional data that became available after the preprint was written: "This study was conducted in the lockdown phase, before its end in May, and was therefore based on a scenario analysis. Here, we also provide an ex‐post assessment of the epidemic situation reported by data that became available after the initial submission." Methods: different parameters described in preprint versus peer‐reviewed:
Results: major differences in numerical findings, probably because of different dates/parameters used to construct model. Examples:
Discussion: no major changes |
| Head 2020 | Head 2021 | Title: changed Abstract: While the results remain the same, the authors add one important sentence: "However, we found that reopening policies for elementary schools that combine universal masking with classroom cohorts could result in few within school transmissions, while high schools may require masking plus a staggered hybrid schedule." Methods: no major changes Results: no major changes Discussion: stronger focus on effectiveness of reopening strategies "Some reopening strategies can result in few in‐school transmissions among students and teachers alike, according to our findings. Most notably, our model found that reducing in‐school mixing via classroom cohorts or hybrid scheduling is an effective means of reducing the risk of school‐attributable illness across all levels of education, especially when combined with universal masking. These findings concur with observations of schools that reopened with universal masking, social distancing and a hybrid or cohort approach and avoided large outbreaks" |
| Kaiser 2020 | Kaiser 2021 | Title: changed Abstract: substantially condensed Background: substantially shortened Methods: mean of out‐of‐school student contacts as per CILS4EU data cited 3.58 in preprint and 3.15 in peer‐reviewed version; no implications for model as average number of out‐of‐school interactions still 4.2 in both preprint and peer‐reviewed version (daily/weekly contact probabilities) Model parameters: baseline probabilities of infection: same (modelled for 5%, 15%, 25%); proportion of subclinical infections modelled for 20%, 40%, 60% and 80% in preprint and 20%, 50%, 80% in peer‐reviewed version Results: section on the superiority of cohorting versus not cohorting shortened (fig 3 adapted, fig 4 removed in the peer‐reviewed version); reductions of cross‐cohort ties for different cohorting strategies: same (preprint versus peer‐reviewed); figure 6 (preprint) simplified (= fig 5 in peer‐reviewed version); performance of different cohorting strategies: same in preprint versus peer‐reviewed version, however, the numbers cited in the example on page 7, line 6 onwards differ slightly in peer‐reviewed version; sensitivity analyses reported in supplements; short section added that reports on performance of the gender‐split versus other models in individual classrooms (as opposed to aggregated results) – while network‐chain cohorting performs better than gender‐split cohorting in the majority of classrooms, gender‐split cohorting performs better in a minority of classrooms (e.g. in very gender‐segregated in‐school and out‐of‐school cohorts); short section added reporting on another cohorting model: attendance for one cohort on Monday/Tuesday and for the other on Wednesday/Thursday – more effective when overall transmission is low (due to less time spent in school overall), less effective compared to weekly rotation when transmission is high (less “cool‐down”/natural quarantine time) Discussion: minor changes |
| Keeling 2020 | Keeling 2021 | Title: not changed Abstract: not changed Methods: no major changes (just rearrangement of presentation of figures) Results: no major changes Discussion: no changes to the Discussion but the authors have added an 'In context' section which puts the paper into context of simulated versus actual reopening. The authors acknowledge that the Delta variant has changed the context in which schools have reopened. The authors state that in their simulations, return to schools was unlikely to push R above 1, but that the Delta variant may cause R to go above 1 upon reopening. The authors also conducted a retrospective analysis and found that in many regions, there was a positive correlation between cases in the community and cases in schools, with weak evidence suggesting that cases in schools lag behind cases in the surrounding community. Ultimately, the authors conclude that reopening schools (especially secondary schools) is associated with an increased risk of transmission both within the school‐aged pupils and in the wider community. The scale of this increase will inherently depend on the strength of control measures within the classroom and the compliance with mass testing as well as measures in the local community. |
| Landeros 2020 | Landeros 2021 |
Title: not changed Abstract: slightly changed, more details on methods, results and implications Methods: method section more detailed, e.g. more details on the simulation of prevalence tresholds; they also conduct an analysis of different test sensitivities Results: the way the results are presented graphically was revised; the assessment of test sensititivity which was only a parameter in the preprint is now specifically reported ("Compared to this ideal scenario, an imperfect test with 50% detection leads to a slightly later stopping time owing to infections spread by undetected cases and greater overall paediatric infections. The effect is less pronounced in the adult population due to high adult‐adult transmission." They adapted the natural transmission rates and reran the model, resulting in different results for the reproduction number:
Discussion: in the conclusion, the authors now conclude: "We find that measures reducing class density by rotating cohorts between in‐person and remote schooling are likely to have greater impact in reducing the spread of SARS‐CoV‐2 than policies such as mask wearing, handwashing, and physical distancing in the classroom. Nevertheless, the latter policies combined with a reduction in class density are still quite effective in reducing effective transmission" versus "As already mentioned, our simulations suggest that measures that reduce class density by rotating cohorts between in‐person and online schooling are likely to have the greatest impact in reducing the spread of SARS‐CoV‐2 brought on by the resumption of in‐person instruction." |
| Lazebnik 2020 | Lazebnik 2021 | Title: not changed Abstract: shortened; message remains the same Methods: minor changes Results: 3.3. Lockdown policies ‐ added paragraph: "The lockdown policy is similar to the schooling‐working hours policy in the manner that both modify the spatial dynamics of the population. Nevertheless, the schooling‐working hours policy defined the number of hours all the children and working adults populations go to school and work, respectively, while the lockdown policy keeps part (or all) the population at home all day long alongside the remain part of the population keeps the regular working and schooling hours. In addition, the lockdown policy isolates individuals at home, which is expressed by the fact that individuals can contact with them but they can not initial an contact with other individuals while this constraint does not take place in the working‐schooling hours policy." Discussion: minor changes |
| Lyng 2020 | Lyng 2021 |
Title: not changed Methods: refer more specifically to classical epidemiological susceptible, infectious‐asymptomatic, infectious‐symptomatic, removed (SIR) model in their peer‐reviewed version. In the peer‐reviewed version, they justify why they did not add the exposed category to the model ("We do not include an “exposed” category as is often done for compartmental models but account for the shorter time a person is infectious rather than the longer period of time they are infected."); add justification about choice of Miami‐Dade as one scenario for their forcing ("It should be noted that the case counts in Miami‐Dade County over this time period are outliers compared to case counts in other counties across the US over the past ten months. These cases are chosen for illustration to show the widest array of possible scenarios.") Results: peer‐reviewed paper: "At the most lenient frequency considered, every 14 days, the number of infections is reduced approximately 21‐56% (versus 31% to 98% in preprint) compared to no testing at all."
Discussion: peer‐reviewed paper: additional information: "Even with a highly specific (99.5%) test such as a PCR, in a low prevalence community with large pools, false positives may still become an issue. The previous example results in 253 false positives over 100 days, highlighting the importance of confirmatory testing." |
| Munday 2020 | Munday 2021 |
Title: not changed Methods: minor changes Results: peer‐reviewed paper ‐ added information:
Discussion: peer‐reviewed paper ‐ added paragraphs:
|
| Naimark 2020 | Naimark 2021 | Title: changed Abstract: no major changes Methods: no major changes Results: authors have added a paragraph about a sensitivity analysis stating that when NPIs were implemented and their effectiveness held at the base case value, as the effectiveness of mitigation efforts within schools diminished, the difference in mean estimated cumulative case numbers by October 31, 2020, between keeping schools closed or reopening them increased. When school mitigation effectiveness was held at the base case value, as the effectiveness of community‐based NPIs decreased, the difference in mean estimated cumulative case numbers between keeping schools closed vs reopening them did not increase. Discussion: no major changes ‐ authors add a bit more detail about how their study compares to other similar studies and what it adds to the evidence base |
| Panovska‐Griffiths 2020b | Panovska‐Griffiths 2021 | Title: not changed Abstract: slightly changed Methods: not changed Results: no major changes Discussion: no major changes |
| Phillips 2020 | Phillips 2021 |
Title: not changed
Methods: minor changes
Results: peer‐reviewed paper: the maximum mean level of exposure (E) is 5.03% in the 15:2 RA scenario (on average) 12 days into the the simulation, with peak 3.18% presymptomatic (P) and 1.63% asympto‐matic (A) proportions of attendees at days 12 and 19 respectively. Meanwhile, peak mean exposure in scenario 7:3 ST occurs on day 2, with 2% attendees exposed to the disease and presymptomatic cases never exceeding that of the start of any simulation; very detailed sensitivity analyses added to main paper (suppose that was in supplementary material before parameter a is now αC (foot c)
Discussion: peer‐reviewed paper: In the most unfavorable scenario (15:2 RA), there were cumulatively 539 and 324 student‐days missed in high versus low‐transmission settings, respectively. Conversely, in the best scenario (7:3, siblings together), there were only 62 and 51 student‐days missed.
|
| Rozhnova 2020 | Rozhnova 2021 |
Title: not changed Methods: minor changes Results: peer‐reviewed paper:
Discussion: peer‐reviewed paper:
|
| Vlachos 2020 | Vlachos 2021 |
Title: changed Methods: minor changes Results:
Discussion: minor changes |
| Zhang 2020 | Zhang 2021 | Title: not changed Abstract: minor changes Methods: minor changes Results: more info added here but no change to numerical results Discussion: they added some limitations to their modelling approach ("In particular, it is possible that the difference in mixing patterns observed in the prepandemic, outbreak, and post‐lockdown phase would be less marked for symptomatic individuals (especially for severe ones). Therefore, our estimates of SARS‐CoV‐2 transmission in the post‐lockdown phase may be slightly underestimated.") |
Appendix 7. Detailed quality assessment of modelling studies
| Study ID | Study design | 1. Are the structural assumptions transparent and justified? | 2. Are the structural assumptions reasonable given the overall objective, perspective and scope of the model? | 3. Are the input parameters transparent and justified? | 4. Are the input parameters reasonable? | 5. Has an external validation process been described? | 6. Has the model been shown to be externally valid? | 7. Has an internal validation process been described? | 8. Has the model been shown to be internally valid? | 9. Was there an adequate assessment of the effects of uncertainty? | 10. Was technical documentation, in sufficient detail to allow (potentially) for replication, made available openly or under agreements that protect intellectual property? | Further comments concerning bias and evidence |
| Alvarez 2020 | Compartmental SEIR model with additional states * Model is extended by mild symptoms, presymptomatic transmission, hospitalised cases, ICU cases and deaths * Age‐stratification by context‐dependent contact matrices * Includes contact tracing and symptom‐based isolation * Models Chilean Population |
Yes Model equations are clearly stated and scheme is visualised; one of multiple reports with similar methodology, but sufficiently explained in this report (but references to other reports which may contain further justifications); structure is mostly motivated by intuitive reasoning |
No/minor concerns The model structure as employed is generally sensible |
Moderate concerns Most input parameters are not stated explicitly or explained, but instead with reference to other reports. Not entirely clearly laid out which parameters were used, especially with respect to parameters which have been calibrated; calibration data have been given with source and also visualised |
Major concerns There are concerns with regards to some important parameters employed, as found in their report #3 (e.g. symptomatic contact rate, relative infectiousness between compartments have been assumed). Contact matrices are critical |
Partial Calibrated predictions to case data and death data and similar data sets |
Moderate concerns Calibrated curve fits the data, but only weak dependent validation as there are only two rather simple data sets independent of each other |
No No internal validation |
Moderate concerns No internal validation |
Major concerns There have been no uncertainty analyses reported; only analysis for different scenarios |
Moderate concerns Code has not been reported, but replication might be feasible |
|
| Aspinall 2020 | Bayesian Belief Network (BBN) *Primary schools in England *Focus on number of schools with ≥ 1 infection depending on prevalence |
Partial There is a justification, however not convincing; no argument why BBN is appropriate |
Moderate concerns BBN/hazard model cannot track individuals |
No/minor concerns They are transparent and justified rather well |
No/minor concerns Population parameters are known or distributions including uncertainties were assumed |
No No external validation |
Major concerns No external validation |
Partial Authors refer to a well‐established tool (UNINET) |
No/minor concerns UNINET should be well tested |
No/minor concerns Comprehensive Monte‐Carlo approach, partly expert judgement |
No/minor concerns Comprehensive information, reference to an unpublished programming code file |
|
| Baxter 2020 | Agent‐based modelling study * Outcome at population level in Georgia, USA |
Partial Only reference to previous publications which do not seem relevant |
Moderate concerns Justification in references seems rather convincing, but based on previous models for influenza |
No/minor concerns Only reference to previous publications which do not seem relevant |
Moderate concerns Justification in references seems rather convincing, but based on previous models for influenza, decline because of missing susceptibles seem unrealistic |
No No external validation |
Major concerns No external validation; Decline (it seems to occur because of limited number of susceptibles which is unrealistic. |
Partial No internal validation described. However major parts seem to be based on an established framework. |
Moderate concerns No internal validation |
Major concerns Not reported |
Major concerns No code, description only via references, it is unclear which parts are from with reference. Unclear how many times model was run. Paper written in the style of a quick tech report |
Limited number of susceptibles ≥ unrealistic |
| Bershteyn 2020 | Some kind of simulation model, but not really clear what was done * Some parts may be purely observational results without use of model, which may be applicable |
No Some mathematical model details are scattered around the paper, but the general model structure is mainly unclear |
Major concerns Lack of model structure descriptions justifies major concerns |
Major concerns Input parameters are described every now and then, but their role in the model is mainly unclear |
Major concerns As it is unclear how model parameters are used in the model, there are major concerns to whether they are reasonable. The secondary attack rate seems to be an important parameter, but unclear how it is used. |
No No external validation |
Major concerns No external validation |
No No internal validation |
Major concerns No internal validation. Major concerns due to lack of transparency of approach |
Major concerns There are some uncertainty analyses on the simulation parts, but unclear which uncertainties are covered by these analyses |
Major concerns Replication is impossible given the available descriptions |
|
| Burns A 2020 | Deterministic SEIR‐Modification * Accounts for cohorts (age groups) * Investigates symptom‐based isolation strategies * Time‐dependent infectiousness |
Partial Model is roughly justified with reference to previous studies in the same field. Special properties of this model are justified on base of reasoning. The exact structure of cohorting is mentioned, but never elucidated in detail. Relationships of parameters and states might benefit from more visual representations |
Major concerns State equations seem questionable, for example: "Return to isolation" parameter controls flux out of and into isolation. Although not really mechanistic, model makes a lot of detailed but not well‐founded assumptions which, for example, are based on influenza behaviour; model seems a bit over‐parametrised. A deterministic model can be problematic in the context of smaller systems like schools with rather small age cohorts, since stochastic effects may become important (superspreading and similar occurrences) |
Moderate concerns There is a table of input parameters with some references to sources and if they were calibrated. The transparency of input parameter values is of some concern, as not all are clearly stated in the manuscript (e.g. relative contact rate), some with reference to a repository which has not been checked further. |
Major concerns There are major concerns of the validity of inputs as there are a lot of different parameters needed in the model, but their values and their appearance in the model are not always clear. A 30‐day period of infectiousness for COVID‐19 is at least questionable. As some inputs have been supposedly calibrated from influenza data, the validity of values is compromised. Sources and reporting do not award enough credibility to the many input parameters needed for the model. |
Partial The authors mentioned "validation", but data were only calibrated. |
Major concerns Description of calibration process and the illustration barely sufficient to establish that calibration is successful |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns There is a hint to some kind of parameter uncertainty analysis, but the details are hidden in a repository which was not accessed, should be reported in document due to its importance; results have been presented with uncertainty which arises from uncertain parameters |
Moderate concerns There are links to some repositories with reference to data, but it is not entirely clear whether they contain the study code |
|
| Campbell 2020b | Simple health economic model to calculate the cost of passive and active surveillance testing * Considers Canadian population * Comprises a testing scenario for schools |
Yes Structural assumptions are mechanistic and well explained |
No/minor concerns The study structure is mostly clear and its assumptions are reasonable; partial surveillance scenario with some questionable assumptions (e.g. about test frequency and necessity). Study covers PCR, point‐of‐care tests that are increasingly more relevant |
No/minor concerns Input parameters are all stated with plenty of sources |
No/minor concerns No concerns about validity of input parameters |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
No/minor concerns Most parameters (especially important ones) have been analysed in one‐way sensitivity analyses and visualised in Tornado Plot |
No/minor concerns Model is well described and some code is given in the appendix |
|
| Cohen 2020 | Agent‐based model (COVASIM) for COVID‐19 transmission * Combination with model of school network structure for King County, USA, * Seven school reopening strategies and three different values for infectious cases in the two weeks prior to school reopening are simulated |
Partial Model structure is based on COVASIM which is roughly described. There is not enough information to understand the school network model |
Moderate concerns Majority of model assumptions seem reasonable; school network: only qualitative information provided to understand the assumptions; reference to COVASIM is given, but not enough information is provided concerning COVASIM |
Moderate concerns Parameter values are not stated explicitly but with reference to the methodological paper (COVASIM). Parameter table would have been helpful, some parameters obtained by calibration |
Moderate concerns In general input parameters seem reasonable, but hard to verify with large Agent‐Based Model. R=0.9 is set as an input parameter before school reopening, explanation: schools reopen after slow decrease in infectivity, variation in this parameter would have been good |
No No external validation |
Major concerns No external validation |
Partial COVASIM is an established framework; no internal validation for the student network model |
Moderate concerns Besides the use of COVASIM no internal validation |
Moderate concerns Many assumptions based on COVASIM are not checked by uncertainty analysis; parametre uncertainties: sensitivity analysis for the infectivity of children, susceptibility of children; stochastic uncertainty is presented for the effective reproductive number |
Major concerns Code for COVASIM is available, no code for the school network model, replication seems impossible |
|
| Curtius 2020 | Measurement of the aerosol concentration in two different classrooms: * first classroom without air purifiers * second classroom with air purifiers In order to calculate the risk of onward infection in the two different classrooms and comparison the infection risk model by Lelieveld 2020 is used as a base for the model |
Partial Two parts of the model: 1. model by Lelieveld 2020: model seems reasonable but based on questionable assumptions; 2. measurement of aerosol in the two classrooms: clearly described. For the modelling part, they just take the model of Lelieveld 2020 |
Major concerns Many assumptions based on Lelieveld's model (Lelieveld 2020) but not described in detail; some figures are not comprehensible |
Moderate concerns Input parameters are stated with their respective sources but just one source for almost all parameters, a reduced viral load by the factor ten for children is stated without any source |
Moderate concerns Questionable input parameters, especially parameters concerning the infection risk |
Partial Experimental approach in order to assess their assumptions of the particle concentration levels; no external valdiation for the other part of the model |
Moderate concerns The conducted experiment suggests some external validity for a part of the model |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Uncertainty of measurement devices of purifiers is given, no sensitivity analysis and no parameter uncertainty analysis |
Moderate concerns No code available, with the data available replication of results seems feasible |
It is rather an experimental approach, the modelling part is small and based on references. |
| Di Domenico 2020a | Author description: stochastic discrete age‐structured epidemic model * In its core, the structure is a bit unclear * Models possible Ile‐de‐France school opening scenarios from May to summer holidays |
Partial Although there are many details about the model described, the core of the utilised mathematical model is seemingly never described explicitly, making assessment of quality difficult. There seemingly is another paper from the author in which the same approach is utilised, but also complete descriptions are seemingly missing. Quantitative results and methods from other paper are probably used, but mostly not explicitly stated in this context |
Moderate concerns With the available model descriptions and justifications the model seems to make reasonable and justified assumptions. But as the core model structure is unclear, there is a possible risk of bias as some parts cannot be scrutinised |
No/minor concerns Necessary parameters presumably stated with referenced sources and by a parameter table; some parameters are calibrated. Contact matrices would have been nice to have in the paper. Calibration data are not presented in paper, but presumably in other paper. |
Moderate concerns Parameter values are mostly not a direct cause of concern. Speculation about R value during lockdown phase questionable but probably important. Due to obscured structure, it is unclear if all inputs are stated. |
Partial Model calibration successful for some data, but no true external validation in this paper |
Moderate concerns No true external validation reported |
Partial No internal validation |
Moderate concerns No internal validation |
Moderate concerns Uncertainties and sensitivity analyses of results generally reported. Sensitivity to parameter values was analysed for the relative infectiousness of young children, effectiveness of case isolation and the expected R value during lockdown. Stochastic uncertainties have been considered and visualised. Structural uncertainties presumably not considered and also unclear structure. |
Major concerns Code has not been made available and it might not be possible to replicate results given the descriptions |
|
| España 2020 | Meta‐population model * Based on FRED (Framework for Reconstructing Epidemic Dynamics) * Models population of Indiana * Adjusted for properties of COVID‐19 * Investigates effects of face‐mask adherence and school operating capacity |
Yes Although based on an existing tool, there is a detailed summary of model structure and modifications to account for COVID‐19. Structural assumptions are mostly reasonable as the model is mechanistic. Not fully clear how face masks and school operating capacity are incorporated structurally. |
No/minor concerns Overall, model structure is reasonable. There are some minor concerns due to inexplicit description of incorporation of face mask and school operating capacity effect. Assuming that community level reproduction number does not change is questionable, but appropriate assumption if only school effect should be assessed. |
No/minor concerns COVID‐19 relevant parameters are described in paper and referenced with sources. For other parameters FRED is referenced, but they are mostly not explicitly stated. Data used for calibration is clearly stated and referenced. |
No/minor concerns Stated inputs are mostly reasonable. Authors make use of age‐dependent susceptibility, may be questionable given the extent of justification and its importance. |
Yes Data calibrations are visualised. Results were validated on serological results of cumulative proportions of infected individuals and also stratified for different age groups. |
Moderate concerns Although there are independent assessments of external validity presented, the extent of validation is still rather small with regards to their quality and their agreement. Data calibrations were mostly successful within the presented uncertainties, although there are some concerns. |
Partial Established tool has been used |
Moderate concerns Authors used an established tool, but no specific internal validation |
Moderate concerns Results were presented with credible intervals in all instances and uncertainty has also been visualised. However, due to inherent complexity of the model many structural/parameter uncertainties are not considered which raises concerns about the adequateness of presented credible intervals. |
Moderate concerns Study‐specific code has not been made available. But structure and methods are otherwise described in sufficient detail to possibly replicate results by modifying the base FRED |
|
| Germann 2020 | Agent‐based community simulation of USA * Two levels of working, nine levels of schooling * Some scenarios only for the Chicago region |
Partial Major parts of the model structure are taken from literature, however the description is incomplete |
No/minor concerns There are no obvious problematic assumptions, however assumptions not completely listed |
Moderate concerns Information incomplete, no list of all parameters |
No/minor concerns Information incomplete but no obvious problems |
No No external validation |
Major concerns No external validation |
Partial No internal validation described. However, major parts are based on an established framework |
Moderate concerns No internal validation described. However, major parts are based on an established framework |
Major concerns No uncertainty analyses performed |
Major concerns No code available, description is incomplete |
|
| Gill 2020 | Agent‐based model of schools (children + others) and transport of children |
Yes No concerns |
No/minor concerns No specific concerns |
No/minor concerns Comprehensive justification |
No/minor concerns |
No No external validation |
Major concerns No external validation |
Partial No external validation |
Moderate concerns No internal validation described. However, major parts are based on an established framework. In addition, the simulation results seem more smooth than expected |
Moderate concerns Some sensitivity analyses conducted. They refer to a previous similar study where robustness has been shown |
No/minor concerns No code available, description is comprehensive |
|
| Head 2020 | Meta‐population model for San Francisco Bay area * Especially concerned with effectiveness of school measures * Describes time‐discrete stochastic transmission dynamics * Models relations between pairs of individuals by classifying household/school/grade/class/work/community * Survey to obtain age‐dependent community transmission |
Yes Structural assumptions are well described and mostly justified or at least documented |
No/minor concerns Structure is mostly acceptable; stochastic courses of disease rightfully included; force of infection reasonable; assumptions about interventions are acceptable. Not clear if simulating 1 meta‐individual = 25 real individuals introduces a bias |
Moderate concerns Critical assumption about children susceptibility is well justified by literature. Other parameters are also stated with sources and in table. Important parameter "mean transmission rate" not entirely clear in derivation and value has not been stated. Community contact matrix is not explicitly stated. |
Moderate concerns There are some concerns about the general mean transmission rate and the relative differences between the different transmission classes (work/school/household etc.) as they are critical. Many intervention effectiveness parameters have just been assumed. |
Yes Model has been validated in various instances: * comparison with case data after interventions * comparison with seroprevalence data * household attack rate has been compared to literature * composition of synthetic population has been validated |
Moderate concerns Although external validation is given, the quality and extent of validation is not sufficient to confidently validate model outputs |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Uncertainty in the susceptibility of children and the transmission context during the evaluated scenarios has been assessed. Stochastic uncertainty due to the simulation nature has been assessed by generating 1000 simulation runs. Uncertainties to results are given but they are quite large. Still, due to the many parameters and assumptions in the model there are concerns as to how reliable results are. |
Major concerns Code has not been made available but would likely be necessary to replicate analysis due to its complexity |
|
| Jones 2020 | Poisson regression model * Models total cases in Florida school districts * Covariates: prevalence, percent in‐person enrolment, total district enrolment |
Partial The structural assumptions are stated transparently, but it has not been well justified (although model is simple); almost no references |
No/minor concerns Model seems mostly reasonable, but choice of Poisson regression could have been better justified. Results confirm that predictors all have significant impact |
No/minor concerns Many data sets are mentioned, but which data has been used for regression is not entirely clear. There are references to data repositories. |
Major concerns Besides the minor concerns about the description of employed data, it seems like data for schools with no outbreaks have not been considered. This might introduce major bias. |
Partial By virtue of the model structure, calibration is necessary part of model |
Moderate concerns No rigorous quality of fit measure has been described, but standard errors and significance values for parameters suggest reasonability of structure |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Regression parameters are given with z‐values, two similar data sets have been used. No alternative predictors have been assessed |
Moderate concerns Code has not been made available. Data is supposedly stored in repository and the model is described in sufficient detail to replicate analysis. |
|
| Kaiser 2020 | Network model: simulating the transmission of COVID‐19 in classrooms:
* dividing each class in two cohorts which are taught separately;
* four different cohorting strategies: randomly splitting, splitting by gender, separation optimised by minimising intercohort‐contact out of school, network‐based chains for the out‐of‐school contact as a basis of the separation |
Yes Model structure seems reasonable |
No/minor concerns Out‐of‐school interaction of children is based on a different model and seems realistic; information about the mathematical reasoning for the model is missing |
No/minor concerns Sample: 507 classrooms in England, Germany, the Netherlands and Sweden, data for student interaction by a model of 2010/11 (CILS4EU), this data might be outdated; most of the data with reference to literature; just one source for important parameters Davies 2020 |
Moderate concerns Input parameters seem mostly reasonable, some parameter values are stated through literature, others through theoretical reasoning. Assumed fraction of high‐risk contacts and reduced infectivity of low‐risk contacts. |
No No external validation |
Major concerns No external validation |
No No external validation |
Moderate concerns No internal validation |
No/minor concerns Stochastic uncertainty: 300 simulations for each classroom were performed and the average result is given, no further evaluation of stochastic uncertainty; parameter uncertainties are checked for transmission, out‐of‐school interaction and proportion of infections by using different plausible values; uncertainties for parameters concerning the infection are not assessed; structural uncertainties are not assessed but network plausible |
Moderate concerns No code available, description rather comprehensive, replication of model might be difficult |
|
| Keeling 2020 | Complex SEIR‐based ODE model for UK with: *fine‐grained age stratification *school/work/household transmission *undetected/detected cases *compliance‐dependent effect on contact matrices |
Partial Larger ODE model makes it difficult to examine the complete dynamics, visualisation would have been helpful. It is not always clear how analyses exactly have been conducted. There are references to a previous paper with more detailed methodology, but also not perfectly detailed. |
No/minor concerns No direct concerns about specific points. Generally, an overwhelming amount of implicit assumptions to consider due to complexity of model and some lack of descriptions |
Moderate concerns Sources of data and parameters seem to be mostly stated. Parameter table is given, mixing matrices and age‐dependent parameters as figures. Many parameters calibrated from data, but calibration data are not shown and not entirely clear. |
No/minor concerns There are some concerns since it is not clear which data fitting calibrated the parameters (there are some descriptions, but lack of reporting). |
Partial There is dependent validation due to model calibration, but there is limited information about how well model is calibrated to data. The model calibration is done in another paper. |
Moderate concerns Calibration in referenced paper by same author |
Partial There is some validation by authors reported at the end of paper, but no processes reported |
Moderate concerns No internal validation conducted, but model is complex so it would be necessary to check |
Moderate concerns Uncertainties have been partially reported from parameter posterior distributions, covering stochastic and parameter uncertainties. However, uncertainty for some parameters seem rather small. There are some instances in which possibly important values are assumed to be fixed (age‐dependent mixing matrix, effect of lockdown on mixing matrices). Due to its specific model structure, study would have benefited from an analysis by use of a different model structure |
Major concerns Code has not been made available and the way data that are presented will presumably complicate replication attempts |
|
| Kraay 2020 | SIR‐based modelling study *Focus on transmissions via hands and fomite (surface) touching |
Partial Stated "previously described" but no reference provided |
Moderate concerns Only deterministic, very simplified structure |
No/minor concerns Mainly justified by influenza and rhinovirus values |
Moderate concerns Partly taken from influenza/rhinovirus |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
Major concerns Sensitivity analysis for only a few parameters |
Moderate concerns No code available, description rather comprehensive |
|
| Landeros 2020 | SEIR‐based ODE model for the USA * Three different school opening scenarios: reopening at full capacity, allowing half of the students to attend school, rotating cohort (students are divided into 3 cohorts and 2 of them are allowed to attend school at the same time) * Effect on the reproduction number (R) and prevalence is simulated under these three possibilities and compared to the impact of people > 18 years on R and cumulative prevalence of COVID‐19 |
Yes Model structure is clearly stated and justified; equations are based on mathematical reasoning |
Major concerns Model assumptions are simplistic; cohorting strategies for children because of school reopening strategies, but it is unreasonable to have different cohorts in the model for adults as well; model is stated to apply to school communities rather than states |
No/minor concerns Input parameters are justified, literature is given for most of them; child‐to‐child contact rate at school is given without any source |
Major concerns Latent, infectious and incubation period are justified by literature. Weak justification for other parameters such as same values for children and adults for transmission and their latent and infectious period and no source for the multiplier for increased child‐to‐child‐contact c = 10. Input parameters for the transmission rate are highly unspecific, they have a wide range. |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Parameter uncertainty for transmission rate is assessed by large range of different values for said rate. Structural uncertainties are not discussed, although probably important |
No/minor concerns Code available from the author by request; description is comprehensive |
Wide range for the input parameters ≥ no significant result |
| Lazebnik 2020 | Hybrid model: SIRD type temporal dynamics and spatial dynamics for home, school, workplace * Additional compartments: age ‐ children (< 13 years) and adults |
Partial There is a good overview of other studies and their results, motivating the approach. ODE part is described extensively and transparently. Spatial part seems to be a stochastic simulation, but description lacks depth to understand the mechanics involved. |
Moderate concerns Generally, the model adopts features which possibly could produce sensible results due to age stratification and differences in mixing patterns due to different physical locations. But according to the model, children above 13 years would have the properties of adults, i.e. go to work, 2 class age stratification might not be enough. Model is just a forward simulation of input parameters, which requires great care concerning the inputs and their applicability as well as a reliable model structure. Regarding this aspect, there are concerns about the validity of the model. Spatial part can not really be fully assessed with the available information. |
No/minor concerns Input parameters are stated with their respective sources in most cases. The number of meeting events is set to one per hour, without further commentary. |
Major concerns There are significant concerns about the model inputs due to their significance in generating the model results. The inputs are mainly parameters from other studies, such that their reliability in this study are not guaranteed as they are not calibrated against data. Some parameters seem odd: why would children not be able to infect other adults, but other children? (beta_ac,beta_cc) This should presumably be property of the spatial structure, not of the transmission parameter. The derivation of beta_ca as reported is questionable, since beta incorporates infection as well as contact probability, but the derivation only covers infection probability reliably |
Yes Daily R0 from data was compared with R0 from model for a two‐week span before and after school closure. |
Moderate concerns It was shown that the model can in some way approximately reproduce the case numbers in a small time frame. It is not reported to which extent this is really an independent validation. Although better than simple calibration, this is still a weak validation. There have been some comparisons to other modellers' results. |
Partial There are some sanity‐check type analysis from a mathematical standpoint concerning the equations, but from a computational standpoint it is unclear whether the implementation is right |
Moderate concerns Not convincingly validated |
Major concerns Uncertainty has mostly not been assessed, even if it would have been important due to nature of the forward simulation type model. Stochastic Uncertainty was partially assessed as some R2values for result fits have been specified. Parameter uncertainty has not been assessed. Structural uncertainties were not considered, although there has been a discussion of other model structures. |
Major concerns Code has not been made available. Description of spatial stochastic model part lacks in‐depth explanation such that it might not be possible to reproduce model |
|
| Lee 2020 | Simple age‐stratified estimation for basic reproduction number (R0) based on assumed SIR model * Considering different frequencies of contacts among age groups * Impact of different susceptibilities among age groups is assessed |
Yes Model clearly described. |
Moderate concerns Within the limits of SEIR model |
Moderate concerns Sparse details. |
Moderate concerns Sparse details. |
No No description of external validation. |
Major concerns No description and based on hypothetical situation, not a particular context. |
No Not described |
Moderate concerns Not described. |
Moderate concerns Tested 5 different scenarios of children's % susceptibility from 35 to 60% |
No/minor concerns Model available on Github. |
Simple model, but large influence of the contact matrix on the outcome. Contact matrix just roughly described |
| Lyng 2020 | SIR model analysing different test/surveillance strategies * Linked to two observed prevalences in population * No stochasticity, no agents, basic reproduction number (R0) = 2.5, institution = subset of 1500 people |
Yes Information in paper and supplement seem to be complete |
Major concerns Deterministic with fixed R0, very simplified model structure, scope: one initial condition (1.35 infections) and two prevalence scenarios |
No/minor concerns Justification sufficient, however only very few parameters required |
Major concerns Decrease due to limited number of susceptibles, R0=2.5 |
No No external validation |
Major concerns No external validation |
Partial No internal validation described, but code (partly) and online simulator available for testing validity |
Moderate concerns No internal validation described, but code (partly) and online simulator available for testing validity |
Major concerns The weakest part of the study is missing analysis of uncertainty. Predicting costs and effectiveness at an absolute level without uncertainty or sensitivity analysis poses a serious risk. |
No/minor concerns Code is partly available, online simulator available |
Limited number of susceptibles ≥ unrealistic |
| Mauras 2020 | Agent‐based SEIR with contact networks: * investigates probabilities of outbreaks after one index case |
Yes Good and convincing |
No/minor concerns Comprehensive justification, realistic structure |
No/minor concerns Justification sufficient |
No/minor concerns |
Partial Comparison with some specific findings in other studies |
No/minor concerns External validation as good as possible done by comparing with literature |
Partial No explicit internal validation procedure but a very comprehensive set of analyses were done that indicate validity |
No/minor concerns No explicit internal validation procedure but a very comprehensive set of analyses were done that indicate validity |
No/minor concerns Sufficient analyses by evaluating parameter sensitivity and dependency on model assumptions |
No/minor concerns Code available on github, results seem reproducible |
The model focus is on temporal evolution of single index cases within school/workplace. They consider the probability of getting an outbreak (≥ 5 secondary cases). The effect to the population is not the primary scope of the model. |
| Monod 2020 | Bayesian model for transmission dynamics in the USA * Age‐stratified contact‐and‐infection model, * Impact of different age groups to infection dynamics is estimated * Interaction for different age groups is based on mobile phone data, then SARS‐CoV‐2 transmission, infections and deaths are estimated |
Yes Relative mobility levels for the different age groups: mobility between February and August compared to a baseline; mobility is attributed to mortality data to fit the model; mathematical approach is clearly described |
No/minor concerns Model assumptions are justified; limitations: population structure except age is not completely accounted for, young children without phone cannot be followed up, but source for their mobility input data is given; mobility of population depends on a lot of external factors |
No/minor concerns Reference for input parameters is given; two sources for network data are given |
No/minor concerns Input parameters seem reasonable for the US, but strongly depending on the population structure |
Yes Validation for the interaction of individuals by data of a second mobile phone provider; predictions of the model are compared to reported cases of COVID‐19; calibration for the cumulative number of deaths seems reasonable |
Moderate concerns Age‐stratified death data closely matches the model predictions; number of reported COVID‐19 cases compared to the prediction of the model increases, but explanation is given (increased testing); calibration as kind of dependent validation |
No No internal validation |
Moderate concerns No internal validation |
No/minor concerns Credible intervals for key outcomes are given (e.g. R0, onward spread, contribution to infection transmission); parameter uncertainties: sensitivity analysis for the age‐stratified infection fatality ratio; one reference to a similar model, besides that no assessment of structural uncertainties |
No/minor concerns Code available on Github, MIT license is needed |
|
| Munday 2020 | Network model describing transmission between schools * Transmission probability model showing the interaction of schools and households in England * Outbreak probability for six different school reopening scenarios is modelled |
Yes Majority of model assumptions are stated through equations, visualisations might have been helpful |
Major concerns Model assumptions seem idealistic, because the network is simplistic: it accounts for household and schools, other population structures are neglected. Spread between schools is seemingly mediated by infection between siblings in households which seems questionable |
No/minor concerns Source of information for the network of schools in England is given. Parameters are complete, but only a small amount of input parameters are used. |
No/minor concerns Input parameters are reasonable |
No No external validation, but reference to other studies who came to similar qualitative results |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Parameter uncertainty: sensitivity analysis for the reproductive number (R) and for the within‐household transmission probability; stochastic uncertainty: credible intervals are given, 100 simulations in order to account for stochastic uncertainty; no structural uncertainty analysis, although this is needed to justify the structure |
Major concerns No code available, with the data available replication of results might be difficult |
|
| Naimark 2020 | Agent‐based SEIR‐based simulation model * Model to calculate cumulative COVID‐19 cases for six different scenarios: schools remaining closed and schools being reopened in combination with three different non‐pharmacological intervention (NPI) measures; * Hypothetical population of one million individuals based on the characteristics of the population of Ontario, Canada, calibrated for the first and second COVID‐19 wave |
Yes Model structure is stated with reference to the supplementary material; clear visualisation in the supplementary material; reference to a similar model in another study |
No/minor concerns In general it seems reasonable to combine school reopening and schools remaining closed with different NPI measurements; infectiousness of children might be different to adult's infectiousness |
No/minor concerns Input parameters are transparent and justified, table for key parameters with sources is given |
No/minor concerns Input parameters seem to be reasonable, parameters are calibrated or with reference to literature |
Partial Calibration and recalibration for the first and second wave of COVID‐19 (dependent validation) |
Moderate concerns Besides the data used for calibration, no proof that the model fits to external data as well |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Stochastic uncertainties are checked by several simulations, credible intervals are given for stochastic uncertainties; parameter uncertainties are checked by the different scenarios, besides that they are not checked |
No/minor concerns No code available, description rather comprehensive |
|
| Panovska‐Griffiths 2020a | Agent‐based SEIR‐model (COVASIM) * Analysed impact of two different school opening scenarios and three ways of testing on reproduction number (R), incidence and death of COVID‐19 * Second simulation with 50% infectiousness of children compared to older ages * Two possible strategies for reopening schools: full‐ and part‐time with 50% attendance, combined with three types of testing |
Yes Model structure is clearly stated and justified, used COVASIM as a basis of model (briefly described) |
Moderate concerns It is reasonable that reopening of schools is proportional to return to workplaces, effect of decisions of policy makers on this topic is neglected; 14‐days complete isolation of people tested positive might be idealistic; prediction until end of 2021 questionable |
No/minor concerns Input data are stated and source is publicly available for confirmed cases and deaths, referring to COVA for other model parameters; updates of COVASIM are integrated into the model |
Moderate concerns In general the input parameters are reasonable; it is referred to the UK Government's COVID19 dashboard; calibration of some parameters; some concerns because model has a lot of parameter inputs |
Partial Dependent validation for the confirmed cases and deaths, with data of UK Government's COVID‐19 dashboard; but these data were also used to build the model, no other external validation |
Moderate concerns Apart from the dependent validation no external validation described |
Partial COVASIM is an established framework |
Moderate concerns COVASIM is an established framework, no other internal validation |
Moderate concerns Assessment for the effects of uncertainties for deaths, R and incidence of COVID‐19; several simulations in order to account for stochastic errors, shown by 10% and 90% quantiles (but only 10 simulations); different scenarios for test‐tracing and school reopening seem reasonable; parameter uncertainties: two different parameters for children's infectiousness, besides that parameter uncertainties are not assessed; structural uncertainties are not further assessed |
No/minor concerns With the given data, replication of results seems possible, Code for COVASIM is available |
|
| Panovska‐Griffiths 2020b | Agent‐based model based on COVASIM, evaluating the impact of face coverings in the UK, number of new infections for different scenarios: * no mask wearing at schools but community mask wearing * mask wearing at secondary schools and community mask wearing Considered two different levels of effective mask coverage |
Yes Model structure seems reasonable, extensions to COVASIM sufficiently described; not enough information about COVASIM |
Moderate concerns It might not be reasonable to predict a pandemic until 12/2021, only one mask‐wearing scenario at school is modelled and compared to no mask‐wearing at school |
No/minor concerns Illustrative table for the input parameters, COVASIM‐based parameters and calibrated parameters are stated |
Moderate concerns Some concerns because of the many input parameters of COVASIM |
Partial There is no external validation but model calibration for the COVID‐19 cases with case data and death data for the UK |
Moderate concerns Data have been calibrated; calibration c |
Partial COVASIM is an established framework |
Moderate concerns COVASIM is an established framework, no other internal validation |
Moderate concerns Stochastic uncertainties: several simulations are done and 10%/90% quantiles are given, stochastic uncertainty is extremely large; uncertainty of input parameters: different values for effectiveness of mask wearing; no assessment of structural uncertainty |
No/minor concerns Code for COVASIM is available, code for the rest of the model is available on github |
|
| Phillips 2020 | Agent‐based simulation of one school/childcare facility embedded in the community * Basic simulation approach, homogeneous mixing based on household/class/school * Investigates allocation of children and educators to classes |
Yes The model structure is documented and justified in most instances. Unclear whether transmission probability is understood correctly, beta as well as contact matrices have been described as the probability of transmission. |
Major concerns Model assumptions might be too simplistic as small scale of model highlights importance of network effects. Homogeneous mixing is argued by aerosol transmission, however this would contradict the assumption of strongly age‐dependent transmission probabilities. As understood by reviewer: transmission probability approximately proportional to class size, might not be expected as contacts of children might not increase proportionally with larger class size. Immediate detection of symptomatic individuals and perfect compliance with no household transmission in isolation is questionable (only 5 classrooms and 1 school) |
No/minor concerns Input parameters have been stated with sources and some were additionally clarified with explanations. For community transmission an under‐ascertainment factor of 8.45 has been assumed without justification. Although hinted at in the text, different infectiousness of children compared to adults has seemingly not been analysed. |
Moderate concerns Transmission probabilities were calibrated to produce a household attack rate of 15% based on only one study, for the class/school the transmission rate has been scaled down somewhat arbitrarily or at least not convincing |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns There were several sensitivity analyses on important parameters. Uncertainties have been generally visualised, in some instances it is not clear whether standard error of the mean or standard deviation of results is given. Error bands which lead to negative proportions of infected individuals indicate flawed uncertainty analysis. Uncertainties generally large, indicates that choice of outcome variables is not perfect (fractions between strategies more relevant than absolute values) |
Moderate concerns Code not available, but data and method might be sufficiently described to allow for replication |
|
| Rozhnova 2020 | Model for the Netherlands, effect of opening/closing schools on effective reproduction number (Re), informative epidemic data (random cross‐ section, not reported cases with symptoms) |
Yes Justification is comprehensive |
No/minor concerns The assumptions are reasonable |
No/minor concerns Justification is sufficient |
No/minor concerns Estimation of parameters using Bayesian approach (priors seems reasonable), reliable methodology, negative binomial observations assumed |
No No external validation, some literature mentioned |
Moderate concerns No independent external validation, but real and very informative data used for parameter fitting, agreement of model and data shown |
No No internal validation |
Moderate concerns No internal validation, but the methodology was applied previously |
No/minor concerns Reliable methodology for uncertainty analyses applied |
No/minor concerns Code available on github, reproducibility seems given |
|
| Shelley 2020 | Deterministic SEIR model stratified into town and different cohorts within a school * Adds preclinical and subclinical infectious states |
Partial Model structure is mostly clear, some lack of justifications. Exact implementation of testing and quarantine in the model not totally clear and neglected in results/discussion |
Major concerns It is doubtful if this deterministic model of such a non‐closed system starting from one seed infection can properly describe infection dynamics; mass testing fraction is randomly drawn between 0 and 1; high sensitivity of results to the first seeded infection implies practical lack of robustness of deterministic approach; beta has seemingly not been adjusted for the change of magnitude introduced by transmission matrices |
Moderate concerns Epidemiological parameters have been set to Centers for Disease Control (CDC). Effect of cohorting has been chosen without quantitative justification |
Major concerns It is conceivable that form of transmission matrices which have not been sufficiently justified have a major impact on results. Role of mass testing which is chosen to random degrees is unclear |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation |
Moderate concerns Parameter uncertainty has been investigated probabilistically. Transmission matrices have not been subject to uncertainty analyses. There are concerns that the simple model structure can not describe the real dynamics, so an analysis of alternative model structure would have been adequate. |
Moderate concerns Code has not been made available but model is comparably simple. Given information might enable replication of model, but unclear implementation of testing and quarantine. |
|
| Sruthi 2020 | Machine‐learning algorithm to disentangle effects of different non‐pharmacological interventions (NPIs) in Switzerland cantons |
Partial Much of the structure is hidden away in an AI‐type algorithm |
Major concerns As far as it can be addressed the assumed structure seems reasonable. Many of the assumptions are impossible to assess given the information in the study. |
No/minor concerns Algorithm parameters are specified; not many more parameters as it seems. |
No/minor concerns Since model inputs are fairly straightforward, there are barely any problems. A minor concern would be the input of recovery time which scales the reproduction rate. |
Yes Five‐fold cross validation |
Moderate concerns Cross‐validity seems to suggest that weekly infection rates can be predicted well if case numbers are high enough. No other forms of validation reported. |
Partial No internal validation, but cross‐validation |
Moderate concerns Functionality of cross‐validation suggests that model is functional in some sense |
Moderate concerns Uncertainties were reported, but they likely do not span varying structural assumptions which may have significant impact on the reproduction rate contributions. |
No/minor concerns Code and source data available |
|
| Tupper 2020 | Agent‐based/stochastic SEIR model of in‐class transmissions: * focus on large clusters (super‐spreading events) |
Partial Weakly justified, but based on a rather widely used model structure |
Moderate concerns Only children, only within classroom considered |
No/minor concerns Mostly justified by literature |
Moderate concerns No obvious issues, but weak justifications for many parameters |
No No external validation |
Major concerns No external validation |
No No internal validation |
Moderate concerns No internal validation done, results look plausible |
Major concerns Only sensitivity analysis for few parameters. These show large impact on results. |
Moderate concerns No code available, description rather comprehensive |
|
| Williams 2020 | COVID meta‐population model for Seattle * Based on CORVID which is based on FluTe which simulated influenza * Analysis of different test and isolation strategies |
Partial Justifications are shifted to the method papers, but mostly understandable there. Descriptions could have been more technical and detailed. Unclear how tests/symptomatic cases averted was calculated |
Moderate concerns There are some concerns as structure is ultimately based on influenza model, with some natural history of disease modifications introduced for COVID‐19. Because model is meta‐population model, it is difficult to verify that structure is reasonable, mechanistic to a high degree. Simulation of results until end of epidemic is rather unreasonable for assessing outcomes, as this creates a large degree of uncertainty. |
Major concerns It is difficult to gather all model inputs, as most of it is not contained in this paper. Additionally, it is difficult to see how much of up‐to‐date parameter knowledge was used in the simulations |
Moderate concerns There are no obvious flaws, but given the paper information this is impossible to assess without looking into code files |
No No external validation |
Major concerns No external validation |
Partial Model is based on existing published framework |
Major concerns Model is based on existing published framework. But the given outputs are not explicitly validated. The almost equal infection peaks for different simulations are atypical for agent‐based models. |
Major concerns Minimal assessments were provided, some instances of different seeds and different R0 analysed. But model still contains a great deal of uncertainties with respect to structural assumptions and implicit model parameters which are hidden. |
No/minor concerns Code and data are available in repository |
|
| Zhang 2020 | Modelling of four Chinese cities; SIR model and with contact matrices based on diaries/questionnaires via phone; analysis only based on reported contacts; most of the information is from reported contacts not from modelling; only "schools open without any containment measures" versus "schools closed" considered |
Yes Justification is sufficient |
Moderate concerns Self‐reported contacts of study participants play a major role in the model |
No/minor concerns Contact matrices are justified, SIR model parameters only partly justified (it seems to be used only for calculation of R0 not for simulating the epidemics) |
Major concerns Self‐reported contact matrices might be strongly biased, estimation of some parameters of SIR model is not described |
Partial Comparison with mobility |
Major concerns No external validation for the important results, i.e. prediction of R0 or reported infections |
No No internal validation |
Moderate concerns No internal validation, but comprehensive analyses that partly indicate reliability, no comparison of SIR model with data about infections |
Moderate concerns Uncertainty of count matrices is reliable, uncertainty from SIR model not considered |
Moderate concerns No code available, role of SIR model not entirely clear, other parts are sufficiently described |
Transfer of results from China to Western countries unclear. Most information is from reported contacts. These reported contacts (via phone calls) might be unreliable. |
Appendix 8. Measures reducing the opportunity for contacts: study‐by‐study overview of the evidence contributing to each outcome (modelling studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Intervention subcategory: reducing opportunity for contacts ‐ reducing the number of students and reducing the number of contacts | ||||
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 13 modelling studies (Baxter 2020; Bershteyn 2020; Burns A 2020; Di Domenico 2020a; Germann 2020; Gill 2020; Head 2020; Jones 2020; Kaiser 2020; Keeling 2020; Mauras 2020; Panovska‐Griffiths 2020a; Shelley 2020) | Baxter 2020: under a regular schedule, the predicted number of cases in adults would be 3,600,338 (1,491,000 cases in children). When implementing an alternating attendance schedule in primary schools with 50% attendance only, the number of infections in adults would be 3,098,000 and 1,072,000 in children. When implementing the same schedule on all school levels, the number of infections in adults would be 3,166,000 and 1,134,000 in children. If only primary school children (< 10 years) attend school, the predicted cumulative number of infections in adults would be 3,242,000 and 1,183,000 in children. | Full opening of schools with no measures in place | Positive ▲ |
| Bershteyn 2020: among other measures, the study assessed the effect of reducing the number of students per class as well as an alternating attendance schedule compared to a remote learning option, widespread testing at the beginning of the work week, and daily symptom screening and self‐isolation. Reducing the number of students by 50% predicted a 75% reduction in the secondary attack rate. If there are several choices for schools for how to schedule rotating cohorts, the decision for smaller cohorts (e.g. 9 students per group attending one‐third of days instead of 13 students attending one‐half of days) reduces transmission risk as well (results presented in a graphical way only). The effectiveness of the measure was assessed alongside other measures (e.g. testing, symptom screening and subsequent isolation). | Least intense measure | Positive ▲ | ||
| Burns A 2020: compared to reopening under symptom‐based isolation and full capacity, reducing the number of students by 50% was predicted to lead to a reduction in the attack rate by 16%. | Full opening of schools with no measures in place | Positive ▲ | ||
| Di Domenico 2020a: across all scenarios, opening schools fully (100% capacity) on 11 May 2020 would lead to the largest increase in new daily cases. With results presented in a graphical way only, they imply that all measures assessed lead to benefits, and these are generally similar across measures. However, for some scenarios progressive reopening of schools over four weeks (with 25%, 50%, 75% and 100% capacity in weeks 1, 2, 3 and 4) is less beneficial than both the partial reopening of schools to 50% capacity immediately and progressive reopening over two weeks (with 25% and 50% capacity in weeks 1 and 2). The magnitude of the effect depends strongly on what types of schools are involved in reopening: if only pre‐schools and primary schools are reopened much fewer cases occur than if middle and high schools or all schools are reopened. Additionally, the effect is moderated by the relative transmissibility of pre‐school and primary school children: in scenarios with lower transmissibility in these younger children, fewer cases occur with each measure in place. | Full opening of schools with no measures in place | Positive ▲ | ||
| Germann 2020: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study asesses the impact of reducing the number of students (80%, 40%) and introducing alternating attendance schedules (weekly, 2 days). With schools opening at full capacity with no measures in place, the study predicts that the cumulative number of cases during the peak four weeks of the pandemic would be 59,664,577 in the USA. Reducing the number of students by 20% decreases the number of cases to 12,346,146 during this period. Further reducing the number of students to 40% and implementing an alternating attendance schedule further decreases the number of deaths in this period: with a weekly alternating schedule the number of deaths would be 2,263,045, while it would be 1,997,647 for a two‐day alternating schedule. With more workplaces open, the numbers of cases was consistently higher across all scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that strategies that reduce the number of students in schools (rotating 2 days per week; weekly 4‐day rotation; rotating 1 day per week) all lead to reduced cumulative infections among students and staff. This includes both strategies based on alternating attendance (rotating 1 to 4 days per week) as well as strategies based on in‐school cohorting (class cohorting; class cohorting and block scheduling for older students; complete class podding). The size of this effect is moderated by school type, with the rate in primary schools the lowest across scenarios, followed by typical secondary schools then large secondary schools. While all of the strategies are effective, those built on alternating attendance are more effective and rotating one day per week may be slightly more effective than other alternating attendance strategies at a higher community incidence. The size of this effect is moderated by community incidence, with a higher community incidence leading to a higher number of cumulative infections across scenarios. It is not possible to disaggregate effects or determine effect size due to co‐interventions and lack of reporting. | Full opening of schools with no measures in place | Positive ▲ | ||
| Head 2020: the study predicts that strategies that reduce the number of students and thus reducing contacts between students lead to reduced excess proportion of infected students, teachers and staff, household members and community members. This includes strategies based on alternating attendance (reduction of number of students on school or on class level). With schools reopening at full capacity with no measures in place, at a moderate level of community transmission and with children being half susceptible as compared to adults, the study predicts an excess proportion of infected teachers of 14.83 (95% CI 0.93 to 29.25), 14.18 ( 95% CI 1.63 to 26.77) of students, 2.04 (95% CI ‐0.77 to 5.07) of household members and 1.16 ( 95% CI ‐0.9 to 3.28) of community members. When reducing the number of students on the school level (maintaining class sizes, half the school attends two staggered days each week according to grade groups), the proportion of cases can be reduced. For teachers, the excess proportion of cases per 10,000 is reduced to between 0.68 (95% CI ‐2.78 to 4.13); for students, this decreases to 0.55 (95% CI ‐0.32 to 1.66); for family members, the proportion decreases to 0.15 (95% CI ‐1.65 to 1.92). For the general population, the excess rate would be reduced to 00.09 (95% CI ‐1.48 to 1.46). When reducing the number of students on the class level (50% or 10 students; each half attends 2 different days each week), the proportion of cases can be further reduced in students, family members and the general population. For teachers, the excess proportion of cases per 10,000 is slightly higher than for the strategy that reduced the number of students on the school level to 0.7 (95% CI ‐2.38 to 3.85); for students, the proportion decreases to 0.4 (95% CI ‐0.44 to 1.31); for family members, to 0.09 (95% CI ‐1.59 to 1.8) and for the general population, the excess rate would be reduced to 0.04 (95% CI ‐1.42 to 1.55). In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Jones 2020: this is an observational study that observed a reduced cohort, with 55% of all students in the counties returning to in‐person instruction, with 45% enrolling in virtual learning programmes. A one percentage‐point increase of in‐person students (e.g. 60% to 61%) would have an estimated increase in district‐wide student and staff case rates of about 2.1%. School staff appear to be more affected than students in all school types except high schools. Regarding levels of community transmission, each increase in one case per 1000 per week in the community leads to an increase in the average rate within schools by more than 41%. | Full opening of schools with no measures in place | Positive ▲ | ||
| Kaiser 2020: compared to opening schools with no measures in place, forming random cohorts to reduce the number of students by 50% predicts a ~50% reduction in classroom‐level proportion of infections (results only presented graphically). Cohorting that considers out‐of‐school contact between classmates can lower the frequency of spread by 39% to 79% relative to random cohorting. The average proportion of infections at the same time falls from 11% (random cohorting) to about 10% in gender split (where separate cohorts are based on gender), network chain (where cohorts are based on reported social networks, accounting for out‐of‐school contacts) and optimised cohorting (where 2 equal cohorts are formed), with reductions of 4% (gender split strategy), 5% (network chain strategy) and 7% (optimisation strategy). Consistently through all studies, weekly alternating attendance schedules always reduces infections relative to same‐day instruction. The results of the simulations are highly dependent on the level of community transmission and out‐of‐school interaction. | Least intense measure | Positive ▲ | ||
| Keeling 2020: the study assessed the impact of certain grades attending school on the increase in number of cases. With results being presented in a graphical way only they predict that the increase in number of cases can be reduced if only certain grades attend school. The effect is predicted to be largest when only the years 1, 2 and 6 attend school. The increase in cases is predicted to be larger when only secondary school students attend compared to when only primary school students attend. Implementing an alternating attendance schedule and having only 50% of the students attend class leads to a reduction in the increase in cases when compared to having 100% of the respective year groups attending school. The effects are moderated by the level of community transmission, with higher levels of community transmission leading to a larger increase in cases. | Full opening of schools with no measures in place | Positive ▲ | ||
| Mauras 2020: in a primary school, with a baseline reproduction number of 1.25, no specific measure implemented would lead to 50 cases (SD = 1.6); implementing an alternating attendance schedule and an on‐off model (presence versus absence of all students) is predicted to lead to a reduction in the number of cases. The cumulative number of cases in the population according to this strategy would reduce the number of cases to 19.2 (SD = 0.9) in an on‐off daily scenario; 16.8 (SD = 0.7) in an on‐off weekly scenario; 12.7 (SD = 0.6) in a rotating daily scenario and 11.9 (SD = 0.6) in a rotating weekly scenario. In the long run, weekly alternation is predicted to perform better than daily alternation, both for on‐off (15.6 versus 17.4) and for rotating (12.0 versus 12.4) strategies. Although the magnitude varies compared to a primary school, similar effects are seen in a high school. | Full opening of schools with no measures in place | Positive ▲ | ||
| Panovska‐Griffiths 2020a: while results are only presented in a graphical way they imply that under different testing/tracing scenarios, an alternating attendance schedule compared to full reopening leads to fewer new infections. With improved testing and tracing in place, the number of infections can be reduced in both cases. The study also assumed that reopening of schools would correspond to increases in workplace and community transmission probabilities, to account for increased social mixing with reopening of schools and relaxation of the physical distancing restrictions that have applied to work, leisure, and community activities. | Full opening of schools with no measures in place | Positive ▲ | ||
| Shelley 2020: opening schools with 100% of the students attending school five days in a row is predicted to lead to a total of 56,009 (95% CI 47,295 to 64,723) cases in the general population and 5263 (95% CI 3565 to 6961) cases in children in a community of 100,000 individuals. Reducing the number of students by 50% and implementing alternating attendance schedules leads to inconsistent effects: when implementing an A/B daily alternating attendance schedule (50% students attending school in the morning; 50% students attending school in the afternoon), this is predicted to lead to 59,948 (95% CI 51,118 to 68,777) cases in the general population and 8994 (95% CI 7654 to 10,333) cases in children; when implementing a two‐day per week alternating attendance schedule (50% of students attending Monday and Tuesday; Wednesday off; 50% of students attending Thursday and Friday), this is predicted to lead to 59,917 (95% CI 53,182 to 66,653) of cases in the general population and 8985 (95% CI 7927 to 10,044) of cases in children. The lowest number of cases is predicted for a scenario when a weekly alternating attendance schedule is implemented (50% of students attending one week; 50% of students attending the other week), this is predicted to lead to 16.72 (95% CI 8.31 to 33.63) cases in the general population and 1.42 (95% CI 0.77 to 2.63) cases in children. When reducing the number of students to 20%, this is predicted to lead to 176.90 (95% CI 48.02 to 651.68) cases in the general population and 26.33 (95% CI 7.08 to 97.94) cases in children. With 100% of the students being in distance learning, number of predicted cases would be 59,942.76 (95% CI 50,767.00 to 69,118.52) in the general population and 8958.00 (95% CI 6808.34 to 11,107.66) in children. These numbers vary according to level of community transmission as well as co‐interventions in place: with mitigation measures in place that lead to a reduced R of 1.01 to 1.40 compared to R0 of 2.5 to 3.0, the numbers are consistently lower. | Full opening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ | ||
| Risk of infection | 2 modelling studies (Cohen 2020; España 2020) | España 2020: the study compares schools operating with 50% 75%, and 100% of students attending school in person and under different levels of face‐mask adherence (50%, 75%, 100% adherence) and its effect on the proportional reduction in risk of infection when compared to operating schools at full capacity and without face masks. When compared to operating schools at 100% capacity and no face masks, the risk of infection in all population groups is predicted to decrease if fewer students attend school. With 75% of students attending, the risk of infection in teachers decreases by 7.9% (95% CI 7.5% to 8.3%) under a low‐mask adherence (high adherence: 0.7% (95% CI 0.6% to 0.7%) compared to the baseline scenario; with only 50% of students attending, the risk decreases by 0.6% (0.6% to 0.7%) (high‐mask adherence: 0.4 (95% CI0.4% to 0.4%)). In students, the risk is reduced by 8.5% (95% CI8.1% to 8.8%) (high adherence: 0.4% (95% CI0.4% to 0.4%)) in a 75% attendance scenario and 0.5% (95% CI0.4% to 0.5%) (high adherence: 0.2% (95% CI0.2% to 0.2%)) in a 50% capacity scenario. In the general population, the risk of infection can be reduced by 10% (9% to 10%) (high adherence: 1% (95% CI1.0% to 1.0%)) if only 75% of students attend school, and by 1% (95% CI1.0% to 1.0%) (high adherence: 1% (95% CI1.0% to 1.0%)) when only 50% attend school. | Full opening of schools with no measures in place | Positive ▲ |
| Cohen 2020: if schools open at full capacity and no countermeasures in place, the cumulative risk of an infection for individuals in schools would range between 9.5% and 24.6% for teachers and school staff and between 6.4% and 17.2% for students, depending on the level of community transmission. Reducing the number of students predictably leads to a reduction in the cumulative infection rate for individuals in schools. The lowest risk of an infection is predictably achieved by implementing an alternating attendance schedule in primary schools (thus reducing the number of students by 50%) while keeping middle and high schools remote. The risk of infection for school teachers and staff is predicted to range between 0.2% and 0.7% and the risk for students between 0.1% and 1.0%, depending on the level of community transmission. Teaching all primary school students in person with countermeasures in place (non‐pharmaceutical interventions, cohorting, screening) and middle and high school students remotely leads to a predicted increase in risk of an infection (teachers/school staff = 0.3% to 2.1%; students 0.2% to 1.2%). Keeping high school students remote while teaching primary and middle school students in person further increases the predicted cumulative infection rates (teachers/school staff = 0.5% to 3.4%; students 0.3% to 2.4%). Teaching all students in person with countermeasures in place and implementing an alternating attendance schedule leads to predicted risk of an infection of 0.6% to 4.3% in teachers/school staff while increasing the rate in students to 0.4% to 3.1%. Teaching all students in person with countermeasures in place without implementing an alternating attendance schedule leads to predicted risk of an infection of 0.8% to 5.5% in teachers/school staff while increasing the rate in students to 0.6% to 4.1%. A sensitivity analysis showed that an increasing susceptibility of children had a significant impact on the infection rate for people in schools. The effect varies according to the level of transmission in the community. | Full opening of schools with no measures in place | Positive ▲ | ||
| Reproduction number | 6 modelling studies (Cohen 2020; Keeling 2020; Landeros 2020; Lee 2020; Phillips 2020; Zhang 2020) | Cohen 2020: compared to schools opening with full capacity and no countermeasures, reducing the number of students in schools by opening primary and middle schools only as well as implementing an alternating attendance schedule is predicted to reduce the effective reproduction number to below 1 (results presented graphically). The results vary according to the level of community transmission, with no consistent trend across the different scenarios. | Full opening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ |
| Keeling 2020: the study assessed the impact of certain grades attending school on the reproduction number in four regions of the UK. With results being presented in a graphical way only they predict that the increase in R can be reduced if only certain grades attend school. The effect is predicted to be largest when only years 1, 2 and 6 attend school. The increase in R is predicted to be larger when only secondary school students attend compared to when only primary school students attend. Implementing an alternating attendance schedule and having only 50% of the students attend class leads to a reduction in the increase in R when compared to having 100% of the respective year groups attending school. The effects are moderated by the level of community transmission, with higher levels of community transmission leading to a larger increase in R. | Full opening of schools with no measures in place | Positive ▲ | ||
| Landeros 2020: splitting a school community into two or three even rotating cohorts substantially reduces R0 under a wide range of parameter values, and slows viral spread in cases of moderate transmissibility. Moving from full capacity to two cohorts reduces R0 by 50%, using three cohorts further reduces R0, by an unspecified amount. | Full opening of schools with no measures in place | Positive ▲ | ||
| Lee 2020: the study found that reopening schools for all children would return postintervention transmission levels to baseline R0, despite strict physical distancing in the rest of the community. Compared to this, reopening schools only for children < 10 years, even without reduction in daily contacts, is predicted to maintain postintervention R0 < 1 up to a baseline R0 of ~4.5. The addition of school reopening with reduction in daily contacts for children aged 10 to 19 years to 33% of baseline is predicted to keep postintervention R0 < 1 up to a baseline R0 of ~3.3. | Full opening of schools with no measures in place | Positive ▲ | ||
| Phillips 2020: while results are only presented in a graphical way, decreasing the number of students in the classroom decreases the effective reproductive rate (Re) for both low and high rates of transmission, with numbers being lower under a low‐transmission setting. | Full opening of schools with no measures in place | positive ▲ | ||
| Zhang 2020: with very strict community measures in place where very little workplace and community contacts take place (e.g. lockdown), opening high schools would lead to an R(t) of just above 1, compared to an R(t) of approximately 1.75 if schools were completely open. This is moderated strongly by the proportion of 'normal' contacts taking place in the workplace and community: as this proportion approaches 100%, the R(t) value becomes very similar regardless of whether only high schools or all schools are open. | Full opening of schools with no measures in place | Positive ▲ | ||
| Number or proportion of deaths | 5 modelling studies (Baxter 2020; Germann 2020; Head 2020; Keeling 2020; Panovska‐Griffiths 2020a) | Baxter 2020: under a regular schedule, the predicted number of deaths would be 21,980 in the general population of the state of Georgia, USA. If only primary school children (< 10 years) attend school, the predicted cumulative number of deaths would be 18,977. When implementing an alternating attendance schedule with 50% attendance on all school levels, the number of deaths would be reduced to 18,385. When implementing an alternating attendance schedule in primary schools, the number of deaths would be further reduced to 18,075. If all students receive online instruction, the number of deaths would be 17,417. | Full opening of schools with no measures in place | Positive ▲ |
| Germann 2020: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study assessed the impact of reducing the number of students (80%, 40%) and introducing alternating attendance schedules (weekly, 2 days). With schools opening with full attendance and no measures in place, the study predicts that the number of deaths during the peak four weeks of the pandemic would be 107,322 in the general population of the USA. Reducing the number of students by 20% decreases the number of deaths to 20,900 during this period. Further reducing the number of students to 40% and implementing an alternating attendance schedule further decreases the number of deaths in this period: with a weekly alternating schedule the number of deaths would be 4108, while it would be 3624 for a two‐day alternating schedule. With more workplaces open, the number of deaths was consistently higher across all scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Head 2020: with schools reopening at full capacity with no measures in place, at a moderate level of community transmission and with children being half susceptible as compared to adults, the study predicts an excess total death rate of 0.56 (95% CI ‐1.88 to 3.13) per 10,000, corresponding to 434 (95% CI ‐1451 to 2418) deaths across the Bay area, of which 287 would be among the general population (0.54, 95% CI ‐2.73 to 3.66), 114 among household members of students (0.87, 95% CI ‐3.8 to 7.48), and 31 among teachers (2.97, 95% CI 0.00 to 47.17); only one death was expected among students (0.01, 95% CI 0.00 to 0.01). The study predicts that strategies that reduce the number of students, and thus reduce contacts between students, lead to reduced excess rate of deaths in students, teachers and staff, household members and community members. This includes strategies based on alternating attendance (reduction of number of students on school or on class level). The study predicts that strategies that reduce the number of students lead to reduced proportion of deaths among students, staff and teachers, household members and community members. This includes both strategies based on alternating attendance (reduction of number of students on class level, reduction of number of students on school level). When reducing the number of students on the school level (maintaining class sizes, half the school attends 2 staggered days each week according to grade groups), the proportion of deaths can be reduced. For teachers, the excess proportion of cases per 10,000 is reduced to ‐0.05 (95% CI ‐0.05 to 0.00); for students, this would be reduced to 0.00 (95% CI 0.00 to 0.00); for household members, the proportion decreases to 0.12 (95% CI ‐3.79 to 7.24). For the general population, the excess rate would be reduced to 0.04 (95% CI ‐2.76 to 3.6). When reducing the number of students on the class level (10 students per class, 2‐day attendance per week), the excess rate of deaths in teachers per 10,000 is further reduced to ‐0.18 (95% CI ‐0.18 to 0.00). For students, this remains unchanged at 0.00 (95% CI 0.00 to 0.00). For household members, it decreases to 0.06 (95% CI ‐3.8 to 4.01). For the general population, the excess rate would be reduced to 0.01 (95% CI ‐2.74 to 2.75). In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Keeling 2020: the study assessed the impact of certain grades attending school on the increase in number of deaths in the general population of England. With results being presented in a graphical way, they predict that the increase in number of deaths can be reduced if only certain grades attend school. The effect is predicted to be largest when only grades 1, 2 and 6 attend school. The increase in deaths is predicted to be larger when only secondary school students attend compared to when only primary school students attend. Implementing an alternating attendance schedule and having only 50% of the students attend class leads to a reduction in the increase in deaths when compared to having 100% of the respective year groups attending school. The effects are moderated by the level of community transmission, with higher levels of community transmission leading to a larger increase in deaths. | Full opening of schools with no measures in place | Positive ▲ | ||
| Panovska‐Griffiths 2020a: with results presented in a graphical way, they imply that under different testing/tracing scenarios, an alternating attendance schedule compared to a full reopening (assuming that 90% of the students attend) leads to an equal number of deaths in the general population of the UK. With improved testing and tracing in place, the number of deaths can be decreased in both cases. The study also assumed that reopening of schools would correspond to increases in workplace and community transmission probabilities, to account for increased social mixing with reopening of schools and relaxation of the physical distancing restrictions that have applied to work, leisure, and community activities. | Full opening of schools with no measures in place | Positive ▲ | ||
| Risk of death | 1 modelling study (España 2020) | España 2020: the study compares schools operating at 50%, 75%, and 100% capacity under different assumptions of adherence to wearing face masks (50%, 75%, 100% adherence) compared to operating schools at full capacity and without face masks and its effect on risk of death. In teachers, the risk of death can be reduced by reducing capacity to 75% (high adherence: 4.0% (4.0% to 5.0%); low adherence: 3.8% (3.6% to 4.0%) or 50% (high: 3.0% (3.0% to 3.0%); low: 4.0% (4.0% to 4.0%). In the family, the risk of death can be reduced to 0.4% (0.4 to 0.5%) (low adherence: 4.2% (3.9% to 4.4%)) if only 75% of students attend school, and 0.3% (0.3% to 0.3%) (low adherence: 0.4% (0.4% to 0.5%)) when only 50% attend school. In the general population, the risk of death can be reduced to a 5.0% (5.0% to ‐5.0%) (low adherence: 11.0% (11.0% to 11.0%)) if only 75% of students attend school, and 4.0% (4.0% to 5.0%) (low adherence: 5.0% (5.0% to 5.0%)) when only 50% attend school. | Full opening of schools with no measures in place | Positive ▲ |
| Shift in pandemic development | 5 modelling studies (Alvarez 2020; Germann 2020; Landeros 2020; Mauras 2020; Phillips 2020) | Alvarez 2020: when reducing the capacity of students attending school, the peaks in ICU capacity occurred later compared with higher rates of student attendance (results presented in graphical way). The effects varied based on the intensity of the contact tracing and isolation strategy that was in place | Full opening of schools with no measures in place | Positive ▲ |
| Germann 2020a: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study assessed the impact of reducing the number of students (80%, 40%) and introducing alternating attendance schedules (weekly, 2 days). With schools opening at full capacity with no measures in place, the study predicts that the time to peak incidence would be 62 days in the USA. Reducing the number of students by 20% increases the number of days to peak incidence in the USA to 118. Further reducing the number of students to 40% and implementing an alternating attendance schedule further increases the number of days to peak incidence to 174 days. There was no difference between the two alternating attendance schedules (174 days for both weekly versus 2 days alternating attendance). With more workplaces open, the time to peak incidence would be consistently shorter, with also no difference shown for the two different alternating attendance schedules. | Full opening of schools with no measures in place | Positive ▲ | ||
| Germann 2020b: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study assessed the impact of reducing the number of students (80%, 40%) and introducing alternating attendance schedules (weekly, 2 days). For time to peak prevalence the effects are similar. With schools opening at full capacity with no measures in place, the study predicts that the time to peak prevalence would be 66 days in the USA. Reducing the number of students by 20% increases the number of days to peak prevalence in the USA to 122. Further reducing the number of students to 40% and implementing an alternating attendance schedule further increases the number of days to peak prevalence to 178 days. There was no difference between the two alternating attendance schedules (178 days for both weekly versus 2 days alternating attendance). With more workplaces open, the time to peak prevalence would be consistently shorter, with also no difference shown for the two different alternating attendance schedules. | Full opening of schools with no measures in place | Positive ▲ | ||
| Landeros 2020: using a stopping rule on cumulative prevalence of 5%, the model predicts closures within a month if all students attend school in person and with no mitigation. With results being presented in a graphical way only, they show that reducing the number of students predictably increases the time until the stopping rule is reached. Reducing the number of students to 50% by implementing alternating attendance schedules (2 parallel cohorts versus 2 rotating cohorts) is predicted to lead to 6 to 8 weeks to reach the stopping point (2 rotating cohorts) or 8 to 10 weeks under two parallel cohorts. Reducing the number of students to 33% by implementing an alternating attendance schedule (3 cohorts) further extends the period of time (length not reported). Effects vary according to the assumed transmission rate in children and adults. | Full opening of schools with no measures in place | Positive ▲ | ||
| Mauras 2020: in a primary school, with a baseline reproduction number of 1.25, no specific measure implemented would mean 12.7 days (SD = 0.3) until an outbreak (≥ 5 secondary cases); all measures are effective in reducing the time to outbreak: on‐off daily: 13.6 days (SD = 0.4); on‐off weekly: 13.4 days (SD = 0.4); rotating daily: 14.5 days (SD = 0.5); rotating weekly: 14.6 (SD = 0.5). Although the magnitude varies compared to a primary school, similar effects are seen in a high school. | Full opening of schools with no measures in place | Positive ▲ | ||
| Phillips 2020: with results presented in a graphical way, they imply that a ratio of 15:1 (student‐educator) also results in shorter mean and median outbreak lengths in the entire population in both low‐ and high‐transmission cases in primary schools. Higher student‐educator ratios facilitate faster disease spread through the school than smaller ones. | Full opening of schools with no measures in place | positive ▲ | ||
| Number or proportion of infected schools | 1 modelling study (Aspinall 2020) | Aspinall 2020: if all schools are open to 100% in‐person teaching, the percentage of primary schools with at least one infected person on the premises was predicted to be between 4% and 20% (661 to 3310 primary schools); with certain grades returning to school, the percentage was predicted to range between 2% and 11% (336 to 1873 primary schools), while for ~33% of all primary school students returning to schools, between 1% and 5.5% of primary schools (178 to 924 schools) would have at least one infected person on the premises. The effects varied by time point of school reopening. If all primary schools return to 100% in‐person teaching three months later, the percentage of schools with at least one infected person on the premises would be between 3.6% and 19.8% of schools (612 to 3310 schools). With increasing levels of community transmission, effect estimates are assumed to increase by 30%. | Full opening of schools with no measures in place | Positive ▲ |
| Risk of transmission to other school | 1 modelling study (Munday 2020) | Munday 2020: with all students attending school, the risk of transmission to other schools varied between 0.42 and 3.6 depending on the level of community transmission. With certain grades returning to primary school (reception (children aged 4 to 5); year 1 (children aged 5 to 6) and year 6 (children aged 10 to 11), the predicted risk of transmission between schools was lowest (0.01 to 0.09, depending on the level of community transmission). The additional attendance of Year 10 students (14 to 15 and 16 to 17‐year olds) resulted in an increase in the risk of transmission between schools to 0.03 to 0.34. When letting Year 12 students return, the number increased to 0.01 to 0.15. With both Year 10 and 12 students returning, the number would be 0.04 to 0.44. when all secondary school students attended school the predicted number was highest 0.26 to 2.6). With all primary school students attending school, the number was 0.05 to 0.45. The effect varied by level of community transmission (R = 1.1 to R = 1.5) | Full opening of schools with no measures in place | Positive ▲ |
| Outcome category: healthcare utilisation | ||||
| Number or proportion of hospitalisations | 2 modelling studies (Germann 2020; Head 2020) | Germann 2020: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study assessed the impact of reducing the number of students (80%, 40%) and introducing alternating attendance schedules (weekly, 2 days). With schools opening at full capacity with no measures in place (prepandemic scenario), the study predicted a cumulative number of hospitalisations during the peak four weeks of the pandemic of 1,798,188 in the USA. With community interventions in place, the number of hospitalisations in that period is predicted to be 685,746. Reducing the number of students by 20% reduced the number of hospitalisations to 354,878 during this period. Further reducing the number of students to 40% and implementing an alternating attendance schedule further decreases the number of deaths in this period: with a weekly alternating schedule the number of deaths would be 67,090, while it would be 59,056 for a two‐day alternating schedule. With more workplaces open, the numbers of cases was consistently higher across all scenarios. | Full opening of schools with no measures in place | Positive ▲ |
| Head 2020: the study predicts that strategies that reduce the number of students and thus reducing contacts between students lead to reduced excess hospitalisations per 10,000 students, teachers and staff, household members and community members. This includes strategies based on alternating attendance (reduction of number of students on school or on class level). With no measures in place, the excess rate of hospitalisations per 10,000 subpopulation would be 40.5 (95% CI ‐46.95 to 146.64) for teachers, 0.08 (95% C I0.00 to 0.08) for students, 6.86 (95% CI‐ 14.32 to 30.11) for household members and 4.2 (95% CI‐ 7.33 to 16.32) for community members. When reducing the number of students on the class level (50% or 10 students; each half attends 2 different days each week), the proportion of hospitalisations can be further reduced. For teachers, the excess proportion of hospitalisations per 10,000 is reduced to 2.12 (95% CI‐ 47.62 to 47.85, 47.85); for students, this decreases to 0.01 (0.00 to 0.01); for household members, the proportion decreases to 0.9 (95% CI‐18.34 to 18.7); for the general population the rate of hospitalisations decreases to 0.18 (95% CI ‐9.98 to 9.96). When reducing the number of students on the school level (maintaining class sizes, half the school attends 2 staggered days each week according to grade groups), the proportion of hospitalisations can be reduced. For teachers, the excess proportion of hospitalisations per 10,000 is reduced to 2.12 (95% CI ‐47.62 to 47.85; for students, this decreases to 0.01 (95% CI 0.00 to 0.01); for household members, the proportion decreases to ‐0.9 (95% CI ‐18.34 to 18.7); for the general population the rate of hospitalisations decreases to ‐0.03 (95% CI ‐10.03 to 9.87). In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Number or proportion of cases requiring intensive care | 3 modelling studies (Alvarez 2020; Di Domenico 2020a; Keeling 2020) | Alvarez 2020: compared with opening schools with full attendance (100%), opening schools with decreased attendance (25%) predicted reductions in demands on ICU beds, with effects varying due to concurrent contract tracing and isolation. Compared to a scenario in which 0% of the students attended school (baseline ICU demand in metropolitan region: n = 2013 ; Antofogasta region n = 1362; Valparaiso region n = 70), the demand for ICU beds increased by 121% to 1221% when 100% of students attended school (metropolitan region: n = 4452 (increase of 121%); Antofogasta region n = 708 (increase of 165%); Valparaiso region n = 925 (increase of 1221%)). The effects varied according to the intensity level of contact tracing and isolation strategies outside of the school setting: with increased contact tracing and isolation, the demand for ICU beds was consistently lower across all scenarios. | Full opening of schools with no measures in place | Positive ▲ |
| Di Domenico 2020a: reopening schools fully on 11 May 2020 with no measures in place predicted the largest demand in ICU occupancy. Reopening of schools over four weeks (with 25%, 50%, 75% and 100% capacity in weeks 1, 2, 3 and 4, respectively) was found less beneficial than both the partial reopening of schools to 50% capacity immediately and progressive reopening over two weeks (with 25% and 50% capacity in weeks 1 and 2, respectively). The magnitude of effect varied depending on the types of schools operated: if only pre‐schools and primary schools are operated, the overall ICU occupancy remains under capacity and lower than if secondary schools or all schools are operated. Additionally, the effect varied by the relative transmissibility of pre‐school and primary school children: in scenarios with lower transmissibility in these younger children, ICU occupancy was generally lower. | Full opening of schools with no measures in place | Positive ▲ | ||
| Keeling 2020: the study assessed the impact of certain grades attending school on the increase in ICU admissions. With results being presented in a graphical way only they predict that ICU admissions increase can be reduced if only certain grades attend school. The effect is largest when only years 1, 2 and 6 attend school. The increase in ICU admission is predicted to be larger when only secondary school students attend compared to when only primary school students attend. Implementing an alternating attendance schedule and having only 50% of the students attend class leads to a lower increase ICU admissions when compared to having 100% of the respective year groups attending school. The effects are moderated by the level of community transmission, with higher levels of community transmission leading to a larger increase in ICU admissions. | Full opening of schools with no measures in place | Positive ▲ | ||
| Outcome category: societal, economic and ecological outcomes | ||||
| Numbers of days spent in school | 3 modelling studies (Cohen 2020; Gill 2020; Phillips 2020) | Cohen 2020: while numbers are only reported in a graphical way, reducing the number of students would reduce the number of days spent at school to 17% to 40% due to planned school closure or a SARS‐CoV‐2 infection, depending on the cumulative infection rate. The lowest number of days spent at school (~17%) is under a measure which only teaches primary students in person and with an alternating attendance schedule (i.e. middle and high school students are taught remotely). When either (i) teaching primary school students in person with countermeasures in place (non‐pharmaceutical interventions, cohorting, screening) and middle and high school students remotely or (ii) teaching all students in person with countermeasures in place and implementing an alternating attendance schedule, the percentage of days spent at school would be around 40%. Teaching primary and middle school students in person with countermeasures in place while teaching high school students remotely would lead to ~65% of school days spent at home. With all students being taught in person with no countermeasures in place, the percentage of days spent at school would predictably be at around 90% to 95%. The results vary according to the level of community transmission, with higher levels of community transmission leading to a higher percentage of school days lost. | Full opening of schools with no measures in place | Negative ▼ |
| Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that strategies that reduce the number of students in schools (rotating 2 days per week; weekly 4‐day rotation; rotating 1 day per week) all lead to a lower proportion of school days attended in person by design. With results presented in a graphical way only, they imply that the number of unplanned days spent at home is larger in schools operating full‐time than in schools using hybrid approaches because schools using hybrid approaches experience fewer infections that lead to quarantines or closures. The number of days attended in person remains constant for all strategies that reduce the number of students in schools, regardless of the community incidence. | Full opening of schools with no measures in place | Negative ▼ | ||
| Phillips 2020: the study results imply that for reducing the class size from 30 to 15 and 8 reduced the predicted number of student days lost to closure, thus increasing the number of days spent in school. The predicted number of student days lost was 76.0 ± 59.5 for a ratio of 8:1, 270.2 ± 195.6 for a ratio of 15:1 and 1157.7 ± 684.3 for a ratio of 30:1. These effects were moderated by the level of community transmission. For all but the ratio 30:1, the number of student days lost to closure were consistently higher in a higher transmission setting. | Full opening of schools with no measures in place | Positive ▲ | ||
| Intervention subcategory: reducing opportunity for contacts ‐ reducing number of contacts | ||||
| Outcome | Number of studies | Summary of findings | Certainty of evidence | Comments |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 3 modelling studies (Cohen 2020; Gill 2020; Head 2020) | Cohen 2020: if schools operate under full capacity and no countermeasures are in place, the predicted cumulative infection rate for individuals in schools would range between 9.5 and 24.6 for teachers and school staff and between 6.4 and 17.2 for students, depending on the level of community transmission. Implementing countermeasures such as mask wearing, detecting, tracing, and quarantining cases within schools alongside a reduction of contacts between cohorts is predicted to decrease the cumulative infection rates to 0.8 to 5.5 in teachers/school staff and 0.6 to 4.1 in students. A sensitivity analysis showed that an increasing susceptibility of children had a significant impact on the infection rate for people in schools. | Full opening of schools with no measures in place | Positive ▲ |
| Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that strategies that employ precautions, including mask wearing for students and staff on the bus and throughout the school day, as well as reduce the number of contacts between students in schools (class cohorting; class cohorting and block scheduling for older students; complete class podding) all lead to reduced cumulative infections among students and staff (results presented graphically). The size of this effect is moderated by community incidence, with a higher community incidence leading to a higher number of cumulative infections across scenarios. While all the strategies that reduce the number of contacts in schools are similarly effective, class cohorting may be slightly more effective at higher community incidence. | Full opening of schools with no measures in place | Positive ▲ | ||
| Head 2020: the study predicts that strategies that reduce contacts (by 50% and by 75%) between students lead to reduced excess proportion of infected students, teachers and staff, household members and community members. With schools reopening at full capacity with no measures in place, at a moderate level of community transmission and with children being half susceptible as compared to adults, the study predicts an excess proportion of infected teachers of 14.83 (95% CI 0.93 to 29.25), 14.18 (1.63 to 26.77) of students, 2.04 (‐0.77 to 5.07) of household members and 1.16 (‐0.9 to 3.28) of community members. When reducing the number of contacts by 50%, the proportion of cases can be reduced. For teachers, the excess proportion of cases per 10,000 is reduced to between 3.16 (‐1.42 to 8.74); for students, this decreases to 2.92 (0.19, 6.96); for household members, the proportion decreases to 0.5 (‐1.23 to 2.5). For the general population, the excess rate would be reduced to 0.29 (‐1.18 to 1.8). When reducing the number of contacts by 75%, the proportion of cases can be further reduced in all subpopulations. For teachers, the excess proportion of cases per 10,000 is reduced to 1.25 (‐2.77 to 5.16); for students, the proportion decreases to 1.3 (0.05 to 3.41); for household members, to 0.22 (‐1.55 to 2.08) and for the general population, the excess rate would be reduced to 0.15 (‐1.33 to 1.54). In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Reproduction number | 3 modelling studies (Cohen 2020; Phillips 2020; Rozhnova 2020) | Cohen 2020: the study found that implementing countermeasures that limit transmission and detect, trace, and quarantine cases within schools, compared to reopening with no countermeasures, reduces the effective reproduction number to below 1 (results presented graphically). However, these measures were implemented alongside classroom cohorting, symptomatic screening, testing and tracing in schools, so it is not possible to assess the effect size of the reduction of contacts separately. The results vary according to the assumptions made in the model, such as susceptibility and transmission in children. | Full opening of schools with no measures in place | Positive ▲ |
| Phillips 2020: while results are only presented in a graphical way, they imply that an alternating attendance schedule while keeping the number of students in the classroom unchanged leads to a small effect with regards to changes to the reproduction number | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
| Rozhnova 2020: based on different values for Re as a function of the reduction of school contacts in different age groups (0 to 20‐year olds), the study varied the number of school contacts in one age group while keeping the number of school contacts in the other two age groups constant. The model predicts a maximum impact on Re from reducing contacts of 10‐ to 20‐year old children. The level of community transmission is assumed to mirror the pandemic situation in the Netherlands in November (R = 1, 95% CrI 0.94 to 1.33) | Full opening of schools with no measures in place | Positive ▲ | ||
| Shift in pandemic development | 2 modelling studies (Landeros 2020; Phillips 2020) | Landeros 2020: implementing an alternating attendance schedule by creating rotating cohorts with a weekly rotating schedule, the model predicts a longer period of instruction (18 to 22 weeks) with the parallel strategy compared to the previous simulation with all students attending at once (10 to 12 weeks) until reaching the stopping rule on cumulative prevalence of 5%. | Least intense measure | Positive ▲ |
| Phillips 2020: the study compared different student to teacher ratios (15:1 and 8:1) and the difference between alternating and non‐alternating attendance schedules in primary schools. With results presented in a graphical way, they imply that an alternating attendance schedule performs slightly better with regards to mean and median outbreak lengths than non‐alternating schedules, however probably not in a significant way. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
| Outcome category: healthcare utilisation | ||||
| Number or proportion of hospitalisations | 2 modelling studies (Germann 2020; Head 2020) | Germann 2020: alongside measures to make contacts safer (face masks, hygiene, and distancing measures), the study assessed the impact of reducing the number of students (40%) and introducing alternating attendance schedules (weekly, 2 days). With schools opening at full capacity with no measures in place (prepandemic scenario), the study predicted a cumulative number of hospitalisations during the peak four weeks of the pandemic of 1,798,188 in the USA. With community interventions in place, the number of hospitalisations in that period is predicted to be 685,746. When implementing a weekly alternating attendance schedule while maintaining the number of students at 40%, the number of hospitalisations would be 67,090. Implementing a two‐day alternating attendance schedule while maintaining the number of students at 40%, the expected number of hospitalisations would be 59,056. With more workplaces open, the numbers of cases was consistently higher across all scenarios. | Least intense measure | Positive ▲ |
| Head 2020: the study predicts that strategies that reduce contacts (by 50% and 75%) between students lead to a reduction in excess hospitalisations per 10,000 of the respective subpopulation. With schools reopening at full capacity with no measures in place, at a moderate level of community transmission and with children being half susceptible as compared to adults, the study predicts an excess rate of hospitalisations per 10,000 subpopulation would be 40.5 (95% CI ‐46.95 to 146.64) in teachers; 0.08 (95% CI 0.00 to 0.08) in students; 6.86 (95% CI ‐14.32 to 30.11) in household members; and 4.2 (95% CI ‐7.33 to 16.32) in community members. When reducing the number of contacts by 50%, the excess hospitalisations can be reduced across all populations. For teachers, the excess proportion of hospitalisations per 10,000 is reduced to 8.46 (95% CI ‐47.39 to 91.76); for students, this decreases to 0.03 (95% CI 0.00 to 0.03); for household members, the proportion decreases to 2.19 (95% CI ‐15.29 to 22.34). For the general population, the excess rate would be reduced to 0.92 (95% CI ‐9.08 to 11.86). When reducing the number of contacts by 75%, the proportion of cases can be further reduced in all subpopulations. For teachers, the excess proportion of hospitalisations per 10,000 is reduced to 2.14 (‐47.39 to 47.85); for students, this decreases to 0.00 (0.00 to 0.00); for household members, the proportion decreases to 0.73 (95% CI ‐17.97 to 18.49). For the general population, the excess rate would be reduced to 0.49 (95% CI ‐9.94 to 10.04). In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Least intense measure | Positive ▲ | ||
| Outcome category: societal, economic and ecological outcomes | ||||
| Numbers of days spent in school | 3 modelling studies (Cohen 2020; Gill 2020; Phillips 2020) | Cohen 2020: while numbers are only reported in a graphical way, reducing the number of contacts between cohorts alongside other countermeasures (non‐pharmaceutical interventions; screening) predictably leads to an equal percentage of school days spent at home as if no measures would be in place (~5% to 10%). The results vary according to the level of community transmission, with higher levels of community transmission leading to a higher percentage of school days lost. | Full opening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ |
| Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that strategies that reduce the contacts between students by limiting interaction to classmates only ("podding"), and providing lunch in the classroom negative impact on the number of days spent in school in a secondary school in Pennsylvania. Compared to the school operating without any measures in place, the proportion of school days attended in person by a typical student in a typical Pennsylvania secondary school is consistently higher under various closure policies (0 day closure after positive case in class; 3‐day closure; 14‐day closure). The typical student in a secondary school open full‐time with measures reducing contacts might be sent home for about 15% of possible days due to quarantines. Even without a closing policy, the number of days spent in school when measures reducing contacts are implemented are reduced by about 10% due to quarantines of the classmates and bus mates of infected students. The size of this effect is moderated by community incidence, with a higher community incidence leading to a higher number of cumulative infections across scenarios. At 100 reported community infections per 100,000 per week, the typical student in a secondary school open full‐time with precautions (scenario B) might be sent home for about 15% of possible days due to quarantines. | Full opening of schools with no measures in place | Positive ▲ | ||
| Phillips 2020: the study results imply that introducing an alternating attendance schedule leads to less student days lost to closure. When implementing an alternating attendance schedule in the 8:1 scenario, the predicted number of student days lost was 73.3 ± 65.7 compared to 76.0 ± 59.5. For a ratio of 15:1, the number of days lost to closure was 264.6 ± 204.9 when an alternating attendance schedule was introduced as compared to 270.2 ± 195.6 for a ratio of 15:1. These effects were moderated by potential co‐interventions implemented (low versus high transmission setting), with number of student days lost to closure being consistently higher in high transmission settings. | Least intense measure | Positive ▲ | ||
Appendix 9. Measures making contacts safer: study‐by‐study overview of the evidence contributing to each outcome (modelling studies)
| Intervention subcategory: making contacts safer ‐ masks | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 3 modelling studies (España 2020; Head 2020; Panovska‐Griffiths 2020a) | España 2020: with schools open at full capacity (100% of students) with low‐face‐mask adherence, the study predicts an increase of 81.7 times the number of infections in the general population. With schools reopening at full capacity with high‐face‐mask adherence there would be a predicted proportional increase of 3.0 times the number of infections. With schools reopening at reduced capacity (75% and 50% of all students) with high‐face‐mask adherence there would be an increase of 1.4 and 2.6 times the number of infections for 50% and 75% capacity, respectively. | Least intense measure | Positive ▲ |
| Head 2020: at a moderate level of community, school reopening with mandatory mask wearing and assuming children were 50% as susceptible to SARS‐CoV‐2 as adults, predicted reductions in excess proportion of infections and symptomatic infections among students and school staff and teachers compared with school reopening with no countermeasures. With schools opening at full capacity with no measures in place, at a moderate level of community transmission, with children assumed to be half as susceptible as adults, the study predicts that the excess percentage of teachers experiencing symptomatic illness would be 10.27% (95% CI 0.47 to 20.66) for teachers/staff and 2.98% (95% CI 0.33 to 5.83) for students. The study predicts that mandatory mask wearing in schools when reopening, all lead to reduced percentage of symptomatic infections among students, staff, household members and community members. For teachers/staff, the percentage experiencing symptomatic illness, the magnitude of effect varied based on model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. | Full opening of schools with no measures in place | Positive ▲ | ||
| Panovska‐Griffiths 2020a: under current testing and tracing levels (24% testing, 47% tracing) and masks’ effective coverage of 30%, the predicted second SARS‐CoV‐2 wave in the general population would be less than half of the original wave if masks were mandatory in secondary schools, as well as used in community settings. The minimum testing levels necessary to avoid a second wave, under scaled up testing, tracing, and isolating, is 8% to 11% less when masks are mandatory in schools than if they are not, depending on the effective coverage of masks (76% and 57% compared to 68% and 46%). If masks were mandatory in secondary schools, assuming that current tracing levels of 47% continue, 68% or 46% of those with symptomatic infection would need to be tested, respectively under scenarios of 15% and 30% mask effective coverage. If masks were not mandatory at secondary schools, the respective numbers would be 76% and 57% for 15% and 30% effective coverage of masks in the relevant community settings. | Least intense measure | Positive ▲ | ||
| Reproduction number | 1 modelling study (Sruthi 2020) | Sruthi 2020: mask requirements led to a reduction of R in the general population of R 0.01 (95% CI 0.01 to 0.01), compared to school opening with no mask requirements. Compared to the no‐mask requirement from the prelockdown period, a mandatory mask in public transport contributed to a reduction of 0.0139 (95% CI 0.0132 to 0.0144). An additional requirement of wearing masks in shops when a requirement in public transport is already mandated did not reduce Rt further. The combined effect of the use of masks in public transport and at schools is thus a reduction in Rt of 0.025 (95% CI 0.018 to 0.030). | Full opening of schools with no measures in place | Positive ▲ |
| Number or proportion of deaths | 2 modelling studies (España 2020; Head 2020) | España 2020: under a scenario with 100% of students and low‐face‐mask adherence, the study predicts an increase in the ratio of the cumulative number of deaths in the overall population by 13.4 (95% CrI 12.8 to 14.0). Under a scenario with 100% of students in school and high‐face‐mask adherence, there would be a predicted decrease in the ratio of the cumulative number of deaths in the overall population of 1.5 (95% CrI 1.5 to 1.6). Due to their older ages, teachers and families experienced a much higher risk of death under scenarios with 100% of students in school and moderate or low‐face‐mask adherence, as compared with a scenario with remote instruction. | Least intense measure | Positive ▲ |
| Head 2020: with schools opening at full capacity with no measures in place, at a moderate level of community transmission, with children assumed to be half as susceptible as adults, the study predicts that the excess rate of deaths compared to school closure would be 2.97 (95% CI 0.00 to 47.17) for teachers/staff and 0.01 (95% CI 0.00 to 0.01) for students. The study predicts that mandatory mask wearing in schools when reopening all lead to reduced deaths among students, staff, household members and community members. For teachers/staff, the excess rate of deaths per 10,000 of the subpopulation is reduced to 0.44 (95% CI 0.oo to 0.44). For students this decreases to 0.00 (95% CI 0.00 to 0.00). The size of this effect is moderated by level of community transmission, type of school and whether children are considered half or equally susceptible as adults. In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ | ||
| Outcome category: healthcare utilisation | ||||
| Number or proportion of hospitalisations | 1 modelling study (Head 2020) | Head 2020: with schools opening at full capacity with no measures in place, at a moderate level of community transmission, with children assumed to be half as susceptible as adults, the study predicts an excess proportion of hospitalisations among students (0.08, 95% CI 0.00 to 0.08) and school staff and teachers (40.5, 95% CI ‐46.95 to 146.64). The study predicts that mandatory mask wearing in schools when reopening will lead to reduced hospitalisations among students, staff, household members and community members. For teachers/staff, the excess rate of hospitalisations per 10,000 of the subpopulation is reduced to 4.2 (95% CI ‐47.39 to 48.09) For students this decreases to 0.07 (95% CI 0.00 to 0.01). The size of this effect is moderated by level of community transmission, type of school and whether children are considered half or equally susceptible as adults. In general, higher transmission, high schools, and increased relative susceptibility of children lead to a higher number of cumulative infections across scenarios. | Full opening of schools with no measures in place | Positive ▲ |
| Intervention subcategory: making contacts safer ‐ cleaning | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Reproduction number | 1 modelling study (Kraay 2020) | Kraay 2020: compared to 8‐hourly and 4‐hourly surface cleaning and disinfection, hourly cleaning and disinfection alone could bring the fomite R0 below 1 in some office settings, particularly combined with reduced shedding, but would be inadequate in child daycares and schools. This study does not take into account direct transmission through droplet spray, aerosols and hand‐to‐hand contact. | Least intense measure | Positive ▲ |
| Intervention subcategory: making contacts safer ‐ handwashing | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Reproduction number | 1 modelling study (Kraay 2020) | Kraay 2020: while results are only presented in a graphical way, it predicts that handwashing (hourly with 100% effectiveness) compared to no handwashing did not make a difference with regards to the projected reproduction number from fomite transmission. | Full reopening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ |
| Outcome category: other health outcomes | ||||
| Physical health | 1 observational study (Simonsen 2020) | Simonsen 2020: this study found that 6.5% (2000 of 30,907, 95% CI 6.2 to 6.8) of children had hand eczema prior to school closures, 14.1% (4363 of 30,907, 95% CI 13.7 to 14.5) of students had hand eczema before reopening of schools on 15 April 2020. This prevalence increased to 50.5% (15,595 of 30,907, 95% CI 49.9 to 51.0) after children returned to school and the strict hand hygiene regimen (handwashing for 45 to 60 seconds every 2 hours; after arrival, before and after meals, after toilet visits, after coughing or sneezing or whenever hands were visibly dirty) was implemented, which was a statistically significant increase of 36.3% (P < 0001). | Full opening of schools with no measures in place | Negative ▼ |
| Intervention subcategory: making contacts safer ‐ modification of activities | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Reproduction number | 1 modelling study (Lazebnik 2020) | Lazebnik 2020: keeping schools open while preventing the infection rate from increasing significantly is possible if schooling hours are longer (8 to 9 hours each day). The influence of this policy in Israel during school opening on 1 September, shows that the R0 can be reduced by 0.83 in comparison to a policy in which children go to school every other day for five hours. Also, if at least half of the adult population will be in lockdown, the influence of schools on the infection rate will be relatively small. | Least intense measure | Positive ▲ |
| Intervention subcategory: making contacts safer ‐ ventilation | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Concentration of aerosol particles containing RNA virus in the room and inhaled dose of RNA virus for a susceptible person | 1 experimental study with modelling component (Curtius 2020) | Curtius 2020: this study comprised an experimental design, combined with elements of modelling to test the efficiency and practicability of operating four air purifiers equipped with HEPA filters in a high school classroom in Germany while regular classes were taking place. Using air purifiers with an air exchange rate of 5.7 h‐1 and equipped with HEPA filters (H13 or H14), for a person spending two hours in a room with an infectious person, the inhaled dose of particles containing RNA virus is predicted to be reduced by a factor of six, compared to a closed classroom with no air purifiers. Other factors which need to be considered include noise levels of the air purifiers and their maintenance, such as regular cleaning. | Full opening of schools with no measures in place | Positive ▲ |
| Intervention subcategory: making contacts safer ‐ combined measures to make contacts safer | ||||
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 4 modelling studies (Cohen 2020; Germann 2020; Gill 2020; Monod 2020) | Cohen 2020: if schools open at full capacity and no countermeasures in place, the cumulative infection rate for individuals in schools would range between 9.5% and 24.6% for teachers and school staff and between 6.4% and 17.2% for students, depending on the level of community transmission. Implementing countermeasures such as mask wearing, detecting, tracing, and quarantining cases within schools alongside a reduction of contacts between cohorts is predicted to decrease the cumulative infection rates to 0.8% to 5.5% in teachers/school staff and 0.6% to 4.1% in students. The results vary according to the level of community transmission, with higher levels of community transmission leading to a higher percentage of school days lost. | Full opening of schools with no measures in place | Positive ▲ |
| Germann 2020: alongside reducing the number of students (80%, 40%) and alternating attendance schedules (weekly, 2 days), the authors compare two different degrees of intensity of measures such as masks, hygiene and physical distancing for the Chicago area during the peak four weeks of the pandemic. More intense measures consistently predicted a reduction in the number of cases: with 80%, 40% (weekly alternating schedule) and 40% (2‐day alternating schedule), the number of cases were 527,005, 82,602 and 70,226, respectively. With less intense measures, the number of cases would be 660,681 (80% attendance), 134,122 (40% attendance, weekly alternating attendance) and 119,614 (40% attendance, 2‐day alternating attendance). With more workplaces open, the number of cases was consistently higher across all scenarios. | Least intense measure | Positive ▲ | ||
| Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that strategies that employ precautions such as mask wearing and lunch in classrooms substantially reduce total infections in the school population. It is not possible to determine effect size due to lack of reporting. | Full opening of schools with no measures in place | Positive ▲ | ||
| Monod 2020: the study compares different levels of transmission reduction obtained through masks and other non‐pharmaceutical interventions (reduction of transmission by 0 to 80%) across all 37 states and metropolitan areas. Compared to a scenario in which schools were closed, reopening the school without masks or other non‐pharmaceutical interventions lead to an increase in infections in children from 0 to 11 years by 1788.5% (95% CrI 994.9% to 3401.1%). With masks and other measures leading to a reduction of transmission of 80%, the increase was 39.6% in infections in children (95% CrI 33.5% to 49.5%). Compared to a scenario in which schools were closed, infections in the general population increased by 248.3% (95% CrI 112.3% to 571.9%) if schools were reopened with no measures in place. With masks and other measures leading to a reduction of transmission of 80%, the increase was 5.6% (95% CrI 3.4% to 9.4%). | Full opening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ | ||
| Reproduction number | 2 modelling studies (Cohen 2020; Phillips 2020) | Cohen 2020: the study found that implementing countermeasures that limit transmission and detect, trace, and quarantine cases within schools, compared to reopening with no countermeasures, reduces the effective reproduction number to below 1 (results presented graphically). However, these measures were implemented alongside classroom cohorting, symptomatic screening, testing and tracing in schools so it is not possible to comment on the effect size of these measures alone. The results vary according to the assumptions made in the model, such as susceptibility and transmission in children. | Full opening of schools with no measures in place | Positive ▲ |
| Phillips 2020: the study compared high with low‐transmission settings in primary schools. With results presented in a graphical way, they imply that the effective reproduction number is consistently lower in a low‐transmission setting. | Least intense measure | Positive ▲ | ||
| Number or proportion of deaths | 2 modelling studies (Germann 2020; Monod 2020) | Germann 2020: alongside reducing the number of students (80%, 40%) and alternating attendance schedules (weekly, 2 days), the authors compare two different degrees of intensity of measures such as masks, hygiene and physical distancing for the Chicago area during the peak four weeks of the pandemic. More intense measures consistently predicted a reduction in the number of deaths: with 80%, 40% (weekly alternating schedule) and 40% (2‐day alternating schedule), the number of cases were 787, 138 and 117 respectively. With less intense measures, the predicted number of deaths would be 965 (80% attendance), 220 (40% attendance, weekly alternating attendance) and 185 (40% attendance, 2‐day alternating attendance). With more workplaces open, the number of deaths was consistently higher across all scenarios. | Least intense measure | Positive ▲ |
| Monod 2020: the study compares different levels of transmission reduction obtained through masks and other non‐pharmaceutical interventions (reduction of transmission by 0 to 80%) across all 37 states and metropolitan areas. When no measures were in place, the excess COVID‐19 attributable deaths in children aged 0 to 11 years would be 137 (65; 287). With 66% reduction in transmission, excess COVID‐19 attributable deaths in children would be 10 (5; 17) excess deaths and with 80% reduction excess deaths would be 4 (2; 7). | Full opening of schools with no measures in place | No change/mixed effects/conflicting findings ◀▶ | ||
| Shift in pandemic development | 2 modelling studies (Germann 2020; Phillips 2020) | Germann 2020a: alongside reducing the number of students (80%, 40%) and alternating attendance schedules (weekly, 2 days), the authors compare two different degrees of intensity of measures such as masks, hygiene and physical distancing for the Chicago area. More intense measures predicted mixed effects with regards to the time to peak incidence: with 80%, 40% (weekly alternating schedule) and 40% attendance (2‐day alternating schedule), the time to peak incidence would be 129, 205 and 206 days, respectively. With less intense measures, the predicted number of days to peak incidence would be 118 (80% attendance), 188 (40% attendance, weekly alternating attendance) and 188 days (40% attendance, 2‐day alternating attendance). With more workplaces open, the effects were also mixed. There was no difference in time to peak incidence for the scenarios of 80% and 40% attendance with weekly alternating attendance, while more intense measures lead to 117 days to peak incidence as compared to 110 with less intense measures. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ |
| Germann 2020b: alongside reducing the number of students (80%, 40%) and alternating attendance schedules (weekly, 2 days), the authors compare two different degrees of intensity of measures such as masks, hygiene and physical distancing for the Chicago area. With regards to time to peak prevalence, more intense measures predicted a longer time to peak prevalence: with 80%, 40% (weekly alternating schedule) and 40% (2‐day alternating schedule), the time to peak incidence would be 129, 205 and 206 days, respectively. With less intense measures, the predicted number of days to peak prevalence would be 122 (80% attendance), 192 (40% attendance, weekly alternating attendance) and 192 days (40% attendance, 2‐day alternating attendance). With more workplaces open, the effects were mixed. There was no difference in time to peak prevalence for the scenarios of 80% and 40% attendance with weekly alternating attendance, while more intense measures lead to 119 days to peak incidence as compared to 115 with less intense measures. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
| Phillips 2020: the study compared high‐ with low‐transmission settings in primary schools. With results presented in a graphical way, they imply that the mean duration of the outbreak is shorter in low‐transmission than high‐transmission settings in all student to teacher ratios except for the 30:1 ratio. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
| Outcome category: healthcare utilisation | ||||
| Number or proportion of hospitalisations | 1 modelling study (Germann 2020) | Germann 2020: alongside reducing the number of students (80%, 40%) and alternating attendance schedules (weekly, 2 days), the authors compare two different degrees of intensity of measures such as masks, hygiene and physical distancing for the Chicago area. With regards to the number of people hospitalised, more intense measures predicted a reduction in the number of people hospitalised. With 80%, 40% (weekly alternating schedule) and 40% (2‐day alternating schedule), the number of people hospitalised would be 14,501, 2348 and 1990, respectively. With less intense measures, the predicted number of people hospitalised would be 18,117 (80% attendance), 3773 (40% attendance, weekly alternating attendance) and 3392 (40% attendance, 2‐day alternating attendance). With more workplaces open, the predicted number of hospitalised persons was consistently higher. | Least intense measure | Positive ▲ |
| Outcome category: societal, economic and ecological outcomes | ||||
| Numbers of days spent in school | 2 modelling studies (Gill 2020; Phillips 2020) | Gill 2020: compared with schools reopening at full capacity with no measures in place, the study predicts that at very low community infection rates (10 reported infections per 100,000 population over the last 7 days), most students can expect to attend nearly every day, even in schools operating full‐time, as long as schools implement precautions such as mask wearing. It is not possible to disaggregate effects or determine effect size due to co‐interventions and lack of reporting. |
Full opening of schools with no measures in place |
Positive ▲ |
| Phillips 2020: the study compared high‐ with low‐transmission settings in primary schools. Except for a ratio of 30:1, the number of student days lost to closure was consistently higher in low‐transmission settings. The predicted number of student days lost was 76.0 ± 59.5 for a ratio of 8:1, 270.2 ± 195.6 for a ratio of 15:1 and 1157.7 ± 684.3 for a ratio of 30:1 in a low‐transmission setting while it was 111.2 ± 72.8; 389.9 ± 202.0 and 1093.9 ± 396.1 for a high‐transmission setting. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
Appendix 10. Measures making contacts safer: study‐by‐study overview of the evidence contributing to each outcome (observational/experimental studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 2 observational/experimental study (Isphording 2020; Vlachos 2020) | Isphording 2020: compared to school closures, three weeks after school openings, cases per 100,000 people decreased by 0.55 or 27% of a SD within the experimental group where co‐interventions included mask wearing, hand‐hygiene policy, respiratory etiquette, general physical distancing policy, modification of activities and exemption of high‐risk students. These were implemented alongside testing and quarantine and cohorting measures. The effect is strongest in the youngest age group of 0 to 14 year‐old cases where the end of summer break is associated with a significant reduction in cases per 100,000 population of about 1.4 cases after 3 weeks for individuals up to 14 years (42% of a SD). Reductions for older age groups are smaller and insignificant: 0.82 cases in the group of 15 to 34 years (21% of a SD) and 0.43 cases in the group of 35 to 59 years (16% of a SD). The more vulnerable population of 60+ years appears to be unaffected by the school openings. Levels of community transmission were relatively low at the time point at which schools were reopened, while compliance and agreement with social distance measures decreased strongly. It was not possible to disaggregate the effect of co‐interventions. | School closure | Positive ▲ |
| Vlachos 2020: among parents, exposure to open rather than closed schools resulted in a small increase in PCR‐confirmed infections (odds ratio (OR) 1.17, 95% CI 1.03 to 1.32). Among lower secondary teachers the infection rate doubled relative to upper secondary teachers (OR 2.01, 95% CI 1.52 to 2.67). This spilled over to the partners of lower secondary teachers who had a higher infection rate than their upper secondary counterparts (OR 1.29, 95% CI 1.00 to 1.67). When analysing COVID‐19 diagnoses from healthcare visits and the incidence of severe health outcomes, results are similar for teachers but weaker for parents and teachers’ partners. The results for parents indicate that keeping lower secondary schools open had minor consequences for the overall transmission of SARS‐CoV‐2 in society. The results for teachers suggest that measures to protect teachers could be considered. | School closure | Negative ▼ | ||
Appendix 11. Surveillance and response measures ‐ mass testing and isolation: study‐by‐study overview of the evidence contributing to each outcome (modelling studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 7 modelling studies (Cohen 2020; Di Domenico 2020a; Head 2020; Lyng 2020; Panovska‐Griffiths 2020a; Tupper 2020; Williams 2020) | Cohen 2020: in the absence of any countermeasures in schools, 6% to 25% of teaching and non‐teaching staff and 4% to 20% of students would be infected with COVID in the first three months of school, depending upon the case detection rate. Implementing countermeasures that limit transmission and detect, trace, and quarantine cases within schools would lead to reductions in the cumulative SARS‐CoV‐2 infection rate among students, teachers, and staff over 14‐fold. Surveillance measures were implemented alongside classroom cohorting, face masks, physical distancing, and handwashing protocols in schools, so it is not possible to comment on the impact of these measures alone. | Full opening of schools with no measures in place | Positive ▲ |
| Di Domenico 2020a: the authors provide no effect estimates for testing, tracing and isolation, but provide results in a graphical way for both assumptions (25% and 50% case isolation through a 90% reduction of their contacts, simulating the result of rapid and efficient tracing and testing of cases). A sensitivity analysis performed indicates that a 25% case isolation compared to a 50% case isolation leads to a reduction in the daily number of new clinical cases under moderate social‐distancing interventions in all scenarios, except for the 100% reopening with no measures in place. Additionally, the effect is moderated by the relative transmissibility of pre‐school and primary school children: in scenarios with lower transmissibility in these younger children, fewer cases occur with each measure in place. | Full opening of schools with no measures in place | Positive ▲ | ||
| Head 2020: when faculty and/or students are tested (85% sensitivity, 100% specificity) on a weekly or monthly basis, with positive cases isolated, and their class quarantined for 14 days, the study predicted that in the absence of other interventions, testing and isolation/quarantine strategies have low effectiveness. When combined with strict social‐distancing measures, a modest reduction in community cases is possible as infectious individuals and their contacts identified in the school environment are quarantined (i.e. have their community contacts reduced by 75% for 14 days). The excess proportion of infections in teachers when only testing is employed is 37.77 (95% CI 10.64 to 53.31) compared to a scenario in which testing is combined with cohorting and mask wearing 1.45 (95% CI ‐2.36 to 5.69), compared to students where it is 52.07 (16.82 to 69.12) and 3.18 (95% CI 0.2 to 7.16), respectively. The excess proportion of infections in the community is 1.01 (95% CI ‐0.78 to 2.97). The effect sizes are moderated by the model parameters such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. For weekly versus monthly testing, results are presented only in graphical form, but indicate that there would be a higher proportion of students with symptomatic infection with a monthly testing strategy than with a weekly testing strategy. | Single intervention component | Positive ▲ | ||
| Lyng 2020: at sensitivities of 98%, the models predict that a 2‐day delay in results will result in a just a 59% reduction in infections experienced at a 14‐day testing frequency. As the testing frequency is increased, the number of missed infections reduces rapidly by > 99% from no testing at all to a daily testing frequency, even with the 2‐day delay. Increasing testing frequency was associated with a non‐linear positive effect on cases averted over 100 days. While precise reductions in cumulative number of infections depended on community disease prevalence, testing every 3 days versus every 14 days (even with a lower sensitivity test) reduces the disease burden substantially. | Least intense measure | Positive ▲ | ||
| Panovska‐Griffiths 2020a: the study suggests that it might be possible to avoid a second pandemic wave if enough people with symptomatic infection can be tested, and contacts of those diagnosed can be traced and effectively isolated. Assuming 68% of contacts could be traced, the study estimates that 75% of those with symptomatic infection would need to be tested and isolated if schools return full time in September, or 65% if a part‐time rota system were used. If only 40% of contacts could be traced, these figures would increase to 87% and 75%, respectively. | Least intense measure | Positive ▲ | ||
| Tupper 2020: in all scenarios, if individuals have not already been identified through the relevant protocol, transmission stops when symptoms begin, as symptomatic individuals do not attend (or they leave when symptoms arise). In scenario 4, the mean cluster size was reduced from 11.9 to 6.5 in the asymptomatic case, whereas the group and two group protocols reduce it to 8.3 and 7.5 students, respectively. Over all the scenarios, the whole class protocol reduced cluster sizes roughly in half, with the contact and two‐group protocols performing slightly worse. | Least intense measure | Positive ▲ | ||
| Williams 2020: isolating household members of individuals who experience symptoms is estimating to avert 2.22 times more symptomatic cases than not isolating them. The multiplicative effect is slightly higher for surveillance/test/quarantine scenarios and highest for cluster sampling on schools, where 3.37 times more symptomatic cases are averted by isolating household members. | Least intense measure | Positive ▲ | ||
| Reproduction number | 1 modelling study (Panovska‐Griffiths 2020a) | Panovska‐Griffiths 2020a: across two scenarios of school reopening and different tracing levels, the test–trace–isolate strategy would need to test a sufficiently large proportion of the population with COVID‐19 symptomatic infection and trace their contacts with sufficiently large coverage, for R to diminish below 1. | Least intense measure | Positive ▲ |
| Number or proportion of deaths | 2 modelling studies (Head 2020; Panovska‐Griffiths 2020a) | Head 2020: the excess proportion of deaths in teachers when only testing is employed is 8.12 (95% CI 0.00 to 47.85), compared to 0 for students and 0.5 (95% CI ‐2.72 to 3.68) in the community. The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. | Full opening of schools with no measures in place | Positive ▲ |
| Panovska‐Griffiths 2020a: while results are only presented in a graphical way, they imply that more intense test, trace, and isolate strategies would lead to lower death rates than less intense strategies. | Least intense measure | Positive ▲ | ||
| Shift in pandemic development | 4 modelling studies (Landeros 2020; Panovska‐Griffiths 2020a; Panovska‐Griffiths 2020a (Preprint); Williams 2020) | Landeros 2020: the study found that reopening with a surveillance programme in place may provide 10 to 12 weeks of continuous instruction with low‐infection risk. Infections after closing are driven by a lack of interventions outside of school; testing and isolation in this context can curtail this growth. In general, the results support the importance of testing and complete school closure in preventing a major disease outbreak after reopening. Overall, this model also shows that reduction of class density and the implementation of rapid viral testing, even with imperfect detection, have greater impact than moderate measures for transmission mitigation. | Full opening of schools with no measures in place | Positive ▲ |
| Panovska‐Griffiths 2020a: the time point at which R diminishes depends on the degree to which the test–trace–isolate strategy had been implemented and the combination of testing and tracing. | Least intense measure | Positive ▲ | ||
| Panovska‐Griffiths 2020a: test–trace–isolate models, combined with mask wearing in the community and secondary schools were modelled. Results suggest that there is a greater benefit of mandatory masks in secondary schools if the effective coverage of masks is high (30%). Under current testing and tracing levels (24% testing, 47% tracing) and masks’ effective coverage of 30%, the predicted second COVID‐19 wave would be less than half of the original wave if masks were mandatory in secondary schools, as well as used in community settings. The minimum testing levels necessary to avoid a second wave, under scaled up test–trace–isolate strategies is 8% to 11% less when masks are mandatory in schools than if they are not, depending on the effective coverage of masks. The simulations suggest that the time point at which R diminishes depends on the degree to which the test–trace–isolate strategy had been implemented and the combination of testing and tracing. | Least intense measure | Positive ▲ | ||
| Williams 2020: isolation of symptomatic, asymptomatic individuals, and their household members can delay the peak prevalence. As with numbers of cases, the largest delays in peak prevalence occur when household members are isolated along with symptomatic and known asymptomatic cases. When all known infected cases and their household members are isolated, this delays the peak prevalence by 74 days. | Least intense measure | Positive ▲ | ||
| Outcome category: healthcare utilisation | ||||
| Number or proportion of hospitalizations | 1 modelling study (Head 2020) | Head 2020: reopening schools with a weekly or monthly testing strategy for teachers and students would lead to a higher number of hospitalisations than reopening under strategies to reduce contacts, such as stable cohorts or alternating attendance. The excess proportion of hospitalisations in teachers when only testing is employed is 162.47 (95% CI 0.00 to 588.24), compared to students 0.58 (95% CI 0.00 to 15.27), and the community 3.68 (95% CI ‐7.27 to 15.54). The effect sizes are moderated by the model parameters, such as relative susceptibility and infectiousness of children, and extent of community transmission amid reopening. | Full opening of schools with no measures in place | Positive ▲ |
| Outcome category: societal, economic and ecological outcomes | ||||
| Numbers of days spent in school | 1 modelling study (Gill 2020) | Gill 2020: in the absence of a school closure policy, quarantine of classmates and bus mates of infected students are likely to reduce in‐person attendance for the typical student by about 10% in a school open full‐time with precautions. High‐community infection rates were predicted to be more disruptive to schools operating full‐time in person than to schools using hybrid approaches. Even at 100 reported community infections per 100,000 per week, the typical student in a hybrid secondary school can expect to miss only a very few days due to quarantine, while the typical student in a secondary school open full‐time with precautions might be sent home for about 15% of possible days due to quarantine. Delays in testing would have large effects in schools implementing no precautions: as testing turnaround time increases from zero to 10 days. Policies that close the school (for 3 days or 14 days) when infections are detected substantially reduce the total number of days that students can attend in person. These effects are larger in schools operating full‐time than in schools using hybrid approaches because schools using hybrid approaches experience fewer infections that lead to quarantines or closures. In secondary schools where students attend daily, and the community infection rate is at a moderate level (50 per 100,000 per week), closing the school for 14 days for each detected infection would be highly disruptive, such that the typical student would be able to attend only about half of all school days. | Least intense measure | Negative ▼ |
| Resources | 3 modelling studies (Campbell 2020b; Lyng 2020; Williams 2020) | Campbell 2020b: the study predicts that universal testing for at‐risk populations would cost CAD 1.3 billion for each round of testing. The status quo testing approach from 8 to 17 July 2020 was predicted to require 41,751 tests per day and required 755 nurses, 213 nursing assistants, 172 other healthcare professionals, 3261 clerical and nonclinical staff, and 721 laboratory staff (5122 personnel total). Testing of at‐risk groups, in particular testing all 6,012,144 students and employees in primary and secondary schools over 1.5 months would require an added 20,956 healthcare professionals, 22,950 clerical staff and 2462 laboratory staff, costing CAD 816.0 million. A strategy of actively testing large population groups who are at increased risk of acquiring SARS‐CoV‐2 is feasible and affordable in Canada. | Least intense measure | Negative ▼ |
| Lyng 2020: frequent testing strategies can reduce the rate of new infections compared to scenarios where there is no testing at all. A 98% sensitive test with no delay in results administered every 3 days with pooling, and no confirmatory test offered by the institution costs less than USD 1.50 per person per day, with high performance. The model demonstrates that frequency of testing, test sensitivity, turn‐around time, and the external community prevalence are all important factors to consider, and there is often more than one testing strategy to achieve the desired level of performance. | Least intense measure | Positive ▲ | ||
| Williams 2020: if household members of symptomatic cases are also isolated (without testing them), a much lower eight tests are required to avert each one symptomatic case. Moving to the symptomatic testing and quarantine (STQ) scenarios, using simple random sampling and isolating only the cases that test positive with STQ, results in 145 tests required to avert one symptomatic case. This decreases to a low of 16 tests to avert one symptomatic case for pooled sampling of 5‐person pools and seven tests for pooled sampling of 5‐person pools if household members are also isolated. Notably, the STQ scenario of pooled sampling of 5‐person pools is slightly more efficient than the current status quo of testing and isolating symptomatic cases. All other STQ scenarios are less efficient than the status quo. However, instituting even these less efficient STQ scenarios is likely to avert a substantial number of cases (as described above) and could be more cost‐effective than the emergency room visits, long‐term care, lost labour, and other economic costs of symptomatic cases and deaths. | Least intense measure | No change/mixed effects/conflicting findings ◀▶ | ||
Appendix 12. Surveillance and response measures ‐ mass testing and isolation: study‐by‐study overview of the evidence contributing to each outcome (observational/experimental studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission outcomes | ||||
| Number of cases detected | 1 observational screening study (Hoehl 2020) | Hoehl 2020: the study aims to evaluate the practical application of self‐performed high‐frequency antigen tests in a school setting. 10,768 of these tests (99.4%) were recorded to have been valid and 113 negative, 47 (0.43%) were recorded as invalid and 21 (0.19%) as positive (either true or false). The study found that 0.15% of all antigen tests (16 tests) gave false‐positive results. False‐positive results were seen predominantly when the local incidence in the general population was low. In four cases, the study participant reported that a PCR had detected a SARS‐CoV‐2 infection, but the antigen test was negative, indicating a false negative. No asymptomatic infection was detected in this study. | Least intense measure | Negative ▼ |
Appendix 13. Surveillance and response measures ‐ symptom‐based screening and quarantine: study‐by‐study overview of the evidence contributing to each outcome (modelling studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 2 modelling studies (Bershteyn 2020; Burns A 2020) | Bershteyn 2020: policies include daily symptom screening, and monthly or weekly testing of 10%, 20%, or 100% of attendees, with testing occurring either on the most optimal day (the first week day of a 5‐day work week, which is Monday for USA public schools) or the least optimal day (the last week day of a 5‐day week, which is Friday for USA public schools). Compared to no testing or isolation, a policy requiring index cases to self‐isolate if they develop symptoms, in‐school transmission is predicted to occur during presymptomatic infection (days 1 through 4) and asymptomatic infection (26% to 39% of index cases). In the absence of additional testing for asymptomatic individuals, this policy predictably reduced transmission by 34.8% to 41.8% relative to no isolation. The impact of weekly testing varied according to the day of the week in which testing was deployed, due to the lack of in‐school transmission over the two‐day weekend. The first week day (Monday) was the most optimal day for testing, while the last weekday (Friday) was the least optimal. Testing on Monday averted 27.1% to 34.0% more infections than testing on Friday, and could reduce transmission by 61.8% to 64.2% without symptom‐based isolation. The most effective testing and isolation strategy used a combination of testing 100% of attendees on the first week day together with symptom screening and isolation of all those who are symptomatic, for an overall transmission reduction of 68.6% to 71.1% relative to no testing or symptom‐based screening. | Full opening of schools with no measures in place | Positive ▲ |
| Burns A 2020: in the baseline scenario of no intervention, the study predicted a median attack rate of 0.79 (IQR 0.56 to 0.9). The estimated attack rates were 0.79 (IQR 0.56 to 0.9), 0.71 (IQR 0.43 to 0.86), and 0.72 (IQR 0.43 to 0.86) at 1 and 2 days of isolation following fever in the scenario of 50% fever detection. The effects varied according to the rate of detecting fever. Applying an 88% detection rate compared to a 50% detection rate, implementing a one fever‐free day predicts an 8% reduction in the attack rate. At this higher rate of symptom detection, increasing the isolation to 6 days predicts a 15% reduction in the median attack rate to 0.43 (0.03 to 0.82) compared to no policy. | Full opening of schools with no measures in place | Positive ▲ | ||
| Shift in pandemic development | 1 modelling study (Burns A 2020) | Burns A 2020: with no policy in place, the peak number of infected people is assumed to be 148 (IQR 82 to 213) and the interval between the first and last day with at least two cases would be 139 (IQR 120 to 154). Implementing a policy of two days of home isolation following the last episode of fever predicted a reduction in all outcome categories: peak number of infected people is predicted to sink to 124 (IQR 58 to 184). The interval between the first and last day with at least two cases would increase to 145 (IQR 127 to 157). The effects varied according to the rate of detecting fever. If the rate of detecting fever is a higher rate of 88%, implementing a 1 fever‐free day achieves a 20% reduction in the peak concurrently infected and a 7‐day increase in the interval between the first and last day with at least two cases. | Full opening of schools with no measures in place | Positive ▲ |
Appendix 14. Multicomponent measures: study‐by‐study overview of the evidence contributing to each outcome (modelling studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 1 modelling study (Naimark 2020) | Naimark 2020: the study assesses the effect of multiple interventions on the cumulative number of confirmed COVID‐19 cases after 2 months. The measures are: i) reducing the number of students (primary and elementary class sizes were capped at 23, and high school classes were capped at 15 students); ii) reduction of contacts (students remained in their assigned classrooms for the school day rather than moving among classrooms); iii) universal masking; iv) alternating attendance schedules in high schools; and v) if more than two confirmed cases of COVID‐19 occurred in a daycare or classroom less than two weeks apart, the daycare or classroom was closed for 14 days with the children in the class excluded from school rather than moved to another classroom. These measures were implemented alongside community‐based interventions. With no community‐based interventions being implemented, the cumulative number of confirmed COVID‐19 cases after 2 months with schools opening without co‐interventions in place would be 82,379 if schools are closed and 86,507 when schools are open. With community‐based interventions being implemented, the cumulative number of confirmed COVID‐19 cases after 2 months with schools opening without co‐interventions in place would be 45,112 if schools are closed and 45,068 when schools are open. The study found a large impact of co‐interventions: The mean difference in cumulative COVID‐19 cases by 31 October 2020, for the scenarios in which community‐based co‐interventions were not implemented versus scenarios in which they were implemented was 39,355 cases. In contrast, the mean difference in cumulative COVID‐19 cases for the scenarios in which schools were reopened versus scenarios in which they were not was 2040 cases. | School closure | Negative ▼ |
Appendix 15. Multicomponent measures: study‐by‐study overview of the evidence contributing to each outcome (observational/experimental studies)
| Outcome | Number of studies | Overview of effect by study | Comparison used in each study | Effect direction per study (positive ▲; negative ▼; no change/mixed effects/conflicting findings ◀▶) |
| Outcome category: transmission‐related outcomes | ||||
| Number or proportion of cases | 2 observational/experimental studies (Isphording 2020; Vlachos 2020) | Isphording 2020: compared to school closures, three weeks after school openings, cases per 100,000 people decreased by 0.55 or 27% of a SD within the experimental group where co‐interventions included mask wearing, hand‐hygiene policy, respiratory etiquette, general physical distancing policy, modification of activities and exemption of high‐risk students. These were implemented alongside testing and quarantine and cohorting measures. The effect is strongest in the youngest age group of 0 to 14‐year‐old cases where the end of summer break is associated with a significant reduction in cases per 100,000 population of about 1.4 cases after 3 weeks for individuals up to 14 years (42% of a SD). Reductions for older age groups are smaller and insignificant: 0.82 cases in the group of 15 to 34 years (21% of a SD) and 0.43 cases in the group of 35 to 59 years (16% of a SD). The more vulnerable population of 60+ years appears to be unaffected by school openings. Levels of community transmission were relatively low at the time point at which schools were reopened, while compliance and agreement with social distance measures decreased strongly. It was not possible to disaggregate the effect of co‐interventions. | School closure | Positive ▲ |
| Vlachos 2020: among parents, exposure to open rather than closed schools resulted in a small increase in PCR‐confirmed infections (odds ratio (OR) 1.17, 95% CI 1.03 to 1.32]. Among lower secondary teachers the infection rate doubled relative to upper secondary teachers (OR 2.01, 95% CI 1.52 to 2.67). This spilled over to the partners of lower secondary teachers who had a higher infection rate than their upper secondary counterparts (OR 1.29, 95% CI 1.00 to 1.67). When analysing COVID‐19 diagnoses from healthcare visits and the incidence of severe health outcomes, results are similar for teachers but weaker for parents and teachers’ partners. The results for parents indicate that keeping lower secondary schools open had minor consequences for the overall transmission of SARS‐CoV‐2 in society. The results for teachers suggest that measures to protect teachers could be considered. | School closure | Negative ▼ | ||
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alvarez 2020.
| Study characteristics | ||
| Notes | ||
Aspinall 2020.
| Study characteristics | ||
| Notes | ||
Baxter 2020.
| Study characteristics | ||
| Notes | ||
Bershteyn 2020.
| Study characteristics | ||
| Notes | ||
Burns A 2020.
| Study characteristics | ||
| Notes | ||
Campbell 2020b.
| Study characteristics | ||
| Notes | ||
Cohen 2020.
| Study characteristics | ||
| Notes | ||
Curtius 2020.
| Study characteristics | ||
| Notes | ||
Di Domenico 2020a.
| Study characteristics | ||
| Notes | ||
España 2020.
| Study characteristics | ||
| Notes | ||
Germann 2020.
| Study characteristics | ||
| Notes | ||
Gill 2020.
| Study characteristics | ||
| Notes | ||
Head 2020.
| Study characteristics | ||
| Notes | ||
Hoehl 2020.
| Study characteristics | ||
| Notes | ||
Isphording 2020.
| Study characteristics | ||
| Notes | ||
Jones 2020.
| Study characteristics | ||
| Notes | ||
Kaiser 2020.
| Study characteristics | ||
| Notes | ||
Keeling 2020.
| Study characteristics | ||
| Notes | ||
Kraay 2020.
| Study characteristics | ||
| Notes | ||
Landeros 2020.
| Study characteristics | ||
| Notes | ||
Lazebnik 2020.
| Study characteristics | ||
| Notes | ||
Lee 2020.
| Study characteristics | ||
| Notes | ||
Lyng 2020.
| Study characteristics | ||
| Notes | ||
Mauras 2020.
| Study characteristics | ||
| Notes | ||
Monod 2020.
| Study characteristics | ||
| Notes | ||
Munday 2020.
| Study characteristics | ||
| Notes | ||
Naimark 2020.
| Study characteristics | ||
| Notes | ||
Panovska‐Griffiths 2020a.
| Study characteristics | ||
| Notes | ||
Panovska‐Griffiths 2020b.
| Study characteristics | ||
| Notes | ||
Phillips 2020.
| Study characteristics | ||
| Notes | ||
Rozhnova 2020.
| Study characteristics | ||
| Notes | ||
Shelley 2020.
| Study characteristics | ||
| Notes | ||
Simonsen 2020.
| Study characteristics | ||
| Notes | ||
Sruthi 2020.
| Study characteristics | ||
| Notes | ||
Tupper 2020.
| Study characteristics | ||
| Notes | ||
Vlachos 2020.
| Study characteristics | ||
| Notes | ||
Williams 2020.
| Study characteristics | ||
| Notes | ||
Zhang 2020.
| Study characteristics | ||
| Notes | ||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anchordoqui 2020 | Irrelevant intervention |
| Balabdaoui 2020 | Irrelevant study design |
| Bracis 2020 | Irrelevant setting |
| Brooks‐Pollock 2021 | Irrelevant study design |
| Buonsenso 2020 | Irrelevant study design |
| Coletti 2020 | Irrelevant study design |
| Di Domenico 2020b | Irrelevant intervention |
| Ehrhardt 2020 | Irrelevant study design |
| Gandolfi 2021 | Irrelevant intervention |
| Garchitorena 2020 | Irrelevant intervention |
| Johnson 2020 | Irrelevant intervention |
| Kim 2020 | Irrelevant intervention |
| Macartney 2020 | Irrelevant study design |
| McBride 2020 | Irrelevant intervention |
| McBryde 2020 | Irrelevant intervention |
| Sneppen 2020 | Irrelevant intervention |
| Stage 2021 | Irrelevant intervention |
| Stein‐Zamir 2020 | Irrelevant study design |
| Wibbens 2020 | Irrelevant intervention |
| Yoon 2020 | Irrelevant study design |
Characteristics of studies awaiting classification [ordered by study ID]
Asgary 2021.
| Notes | Objectives: to develop an agent‐based model and simulation tool to evaluate testing strategies and scenarios in schools with various number of classrooms and class sizes in the Province of Ontario, Canada. |
Bilinski 2021.
| Notes | Objectives: to develop an agent‐based network model, simulating transmission in elementary and high school communities, including home, school, and interhousehold interactions, for assessment of transmission risk in elementary and high school communities in the US. |
Bosslet 2021.
| Notes | Objectives: to determine the county‐level effect of in‐person primary and secondary school reopening on daily cases of SARS‐CoV‐2 in Indiana, USA, by a panel data regression analysis of the proportion of in‐person learning |
Cruz 2021.
| Notes | Objectives: to analyse different strategies to reopen schools in the São Paulo Metropolitan Area, including one similar to the official reopening plan, through a computer simulation based on a stochastic compartmental model |
Ertem 2021.
| Notes | Aims: a national, retrospective cohort study to evaluate the impact of school mode and opening to in‐person education on subsequent changes in community incidence of SARS‐CoV‐2 in the USA. |
Gandini 2021.
| Notes | Aims: a cross‐sectional and prospective cohort study to investigate the overall incidence of SARS‐CoV‐2 infection among students and teachers and to explore if there is an association between the increase in transmissibility of SARS‐CoV‐2 and dates of school openings in different Italian Regions. |
Lessler 2021.
| Notes | Aims: to investigate how different mitigation measures influenced COVID‐19 transmission rates in the wider community in the US using data from the COVID‐19 Symptom Survey, which collects and analyses data on schooling behaviours and SARS‐CoV‐2–related outcomes from households throughout the US. |
Liu 2021.
| Notes | Aims: a retrospective cohort study based on a crowdsourcing data set from the National Education Association (NEA) of reopened K‐12 public schools in the US to assess the spread of COVID‐19 cases among the 3 reopening models (remote, hybrid, and in person) at the school district level. |
Miller 2021.
| Notes | Objectives: using the COVIDTracer Advanced tool to model the transmission of SARS‐CoV‐2 in a school of 596 individuals, a scenario‐based analysis to investigate the risk of transmission and adherence to mitigation measures. |
Pavilonis 2021.
| Notes | Objectives: to estimate the risk of potential aerosol transmission of SARS‐CoV‐2 transmission among New York City public school students and teachers under steady‐state conditions using previously collected classroom CO2 concentrations (from a large indoor air quality survey). |
Reinbold 2021.
| Notes | Aims: to determine whether differences in K‐12 instruction types at the beginning of the 2020‐2021 school year in Illinois school districts were related to differences in COVID‐19 cases, hospitalizations, and deaths in Illinois counties. |
Somekh 2021.
| Notes | Aims: to investigate the effects of school reopening and easing of social‐distancing restrictions on severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) infections in Israel. |
van den Berg 2021.
| Notes | Objectives: to conduct a retrospective analysis of data from traditional public schools in Massachusetts that opened with any in‐person learning in order to evaluate the effectiveness of different physical distancing policies on the incidence of SARS‐CoV‐2 infections among students and school staff after school reopening. |
Willem 2021.
| Notes | Objectives: a stochastic individual‐based model to analyse the effect of repetitive leisure contacts in extended household settings on the transmission of SARS‐Cov‐2 and explore contact tracing strategies based on the open‐source IBM “STRIDE”, fitted to COVID‐19 data from Belgium. |
Young 2021.
| Notes | Aims: an open‐label cluster RCT in students and staff from secondary schools and further education colleges in England to investigate the effects of self‐isolation vs. voluntary daily lateral flow device (LFD) testing for control of COVID‐19 transmission. |
Yuan 2021.
| Notes | Objectives: a Susceptible‐Exposed‐Asymptomatic‐Infectious‐Recovered‐Hospitalised‐Isolated model to explore school reopening scenarios using data from the city of Toronto. |
Differences between protocol and review
There were no differences between the protocol and the review in terms of the search for, and inclusion of studies, however, given the time between the initial search and the publication of this review, the authors were advised by Cochrane to run a top‐up search for studies in August 2021 using the Cochrane Covid‐19 Study Register. The search was performed exactly as it had been conducted in December 2020 but with search dates from 9 December 2020 to 5 August 2021. The studies identified through this search are listed in Characteristics of studies awaiting classification. We have not performed any quality assessment nor data extraction on these studies.
The protocol stated that we would use the Cochrane RoB 2 tool (Higgins 2021), adapted for cluster‐RCTs, to assess risk of bias in RCTs. However, as we did not identify any RCTs, we did not use this tool. The protocol also stated that where appropriate, we would use the synthesis without meta‐analysis (SWiM) guidance as a basis for the reporting of results when exploring heterogeneity between studies (Campbell 2020a). However, we did not use this guidance as the majority of studies included in this review are modelling studies that do not lend themselves to using the SWiM guidance.
Contributions of authors
Co‐ordination of review process: ShK, HL, LMP
Protocol development: ShK, HL, ER, LMP
Citation searches: LMP
Title and abstract screening: ShK, HL, KS, JB, JR, MC, KG, SuK, CaK, SV, LMP
Full‐text screening: ShK, HL, KS, JB, JR, MC, KG, SuK, RB, SV, LMP
Data extraction: ShK, HL, KS, JR, MC, KG, SuK, CaK, RB, SV, LMP
Risk of bias/quality assessment: ShK, HL, KS, JB, JS, AB, TL, CK, LMP
GRADE assessment: ShK, HL, JB, JS, AB, TL, ClK, AM, LMP
Evidence synthesis: ShK, HL, JB, AM, LMP
Title and abstract screening of updated searches: ShK, LMP
Full‐text screening of updated searches: ShK, KS, MC, BV, LMP,
Comparison of preprints and peer‐reviewed articles: ShK, KS, KW, BV, LMP
Development of figures and tables: ShK, HL, KW, BS, LMP
Manuscript preparation: ShK, HL, KS, JB, JR, AB, TL, ClK, AM, BS, ER, LMP
Manuscript approval: ShK, HL, KS, JB, JR, JS, AB, TL, MC, KG, ClK, AM, SuK, CaK, KW, BS, BV, ER, RB, SV, CJS, LMP
Sources of support
Internal sources
No sources of support provided
External sources
-
Ministry of Education and Research, Germany
This review was undertaken in the context of the COVID‐19 Evidence Ecosystem project, funded by the German Ministry of Education and Research.
Declarations of interest
RB: grant/contract from Bundesministerium für Bildung und Forschung
AB: none
JB: grant/contract from German Federal Ministry of Education and Research
MC: grant/contract from Bundesministerium für Bildung und Forschung
KG: grant/contract from German Federal Ministry of Education and Research; Board Member of the German Public Health Association
CJS: German Federal Ministry of Education and Research; I work as a physician (primary tasks: education and research) at the Chair of Public Health, LMU Munich
CaK: grant/contract from German Federal Ministry of Education and Research SuK: grant/contract from Bundesministerium für Bildung und Forschung ClK: none ShK: grant/contract from German Federal Ministry of Education and Research HL: none TL: grant/contract from German Federal Ministry of Education AM: grant/contract from German Federal Ministry of Education and Research LMP: grant/contract from German Federal Ministry of Education and Research JR: grant/contract from German Federal Ministry of Education and Research; I declare being first author of a study on the psychosocial burden in parents of school‐aged children during different phases of the Covid‐19 pandemic in Germany, that was submitted to, but is not yet published by the Journal “Bundesgesundheitsblatt” and might be eligible in future updates of the review. Data for this study were derived from the Covid‐19 Snapshot Monitoring (COSMO) project (https://projekte.uni-erfurt.de/cosmo2020/web/). COSMO is a joint project by the University of Erfurt, the Robert‐Koch‐Institute, the German Federal Agency for Health Education (BZgA), the Leibniz Institute for Psychology, the Science Media Centre, the Bernhard Nocht Institute for Tropical Medicine and the Yale Institute for Public Health. Besides funding from these institutions, funding of the COSMO project derives from the Klaus Tschira Foundation, the Ministry of Economy, Research and Digital Society of Thuringia as well as the state chancellery of Thuringia. ER: grant/contract from Bundesministerium für Bildung und Forschung; a member of the scientific advisory board of the Robert Koch Institute and the Bavarian Health and Food Safety Authority that have both issued guidance on schooling during COVID‐19, but have not been involved with developing this guidance; a member of the WHO Regional Office for Europe’s Technical Advisory Group on Schooling during COVID‐19 and, in this role, is involved with advising the WHO Regional Office for Europe on the issue KS:grant/contract from German Federal Ministry of Education and Research BS: grant/contract from German Federal Ministry of Education and Research JS: grant/contract from Bundesministerium für Bildung und Forschung BV: grant/contract from German Federal Ministry of Education and Research SV: grant/contract from German Federal Ministry of Education and Research KW: grant/contract from German Federal Ministry for Education and Research
RB, KG, CaK, SuK, AM, LMP, JR, ER, KS, BS, JS, BV, SV, KW declare being part of the scientific secretariat that supports the development of a living interdisciplinary, evidence‐based and consensus‐based guideline on measures to prevent and control SARS‐CoV‐2 transmission in schools, registered with the Association of the Scientific Medical Societies (AWMF) in Germany (www.awmf.org/en/clinical-practice-guidelines/detail/anmeldung/1/ll/027-076.html).
CJS, AM and ER are involved in the conduct of an ongoing study that, after completion, is likely to be eligible for inclusion in the review (COVID Kids Bavaria, funded by the State of Bavaria, Germany).
Edited (no change to conclusions)
References
References to studies included in this review
Alvarez 2020 {published data only}
- Álvarez C, Cancino A, Castillo C, Wolff T, Gajardo P, Lecaros R, et al.Report #5: Scenarios for the opening schools during the Chilean COVID-19 outbreak; 7 May 2020. covid-19.cmm.uchile.cl/wp-content/uploads/2020/04/Reporte5_CMM_AM2V_CEPS-VF.pdf.
Aspinall 2020 {published data only}
- Aspinall WP, Sparks RS, Cooke RM, Scarrow J.Quantifying threat from COVID-19 infection hazard in primary schools in England. medRxiv 2020. [DOI: 10.1101/2020.08.07.20170035] [DOI] [Google Scholar]
Baxter 2020 {published data only}
- Baxter A, Oruc BE, Keskinocak P, Asplund J, Serban N.Evaluating scenarios for school reopening under COVID19. medRxiv 2020. [DOI: 10.1101/2020.07.22.20160036] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bershteyn 2020 {published data only}
- Bershteyn A, Kim H-Y, McGillen J, Braithwaite RS.Which policies most effectively reduce SARS-CoV-2 transmission in schools? medRxiv 2020. [DOI: 10.1101/2020.11.24.20237305] [DOI]
Burns A 2020 {published data only}
- Burns AA, Gutfraind A.Effectiveness of isolation policies in schools: evidence from a mathematical model of influenza and COVID-19. medRxiv 2020. [DOI: 10.1101/2020.03.26.20044750] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020b {published data only}
- Campbell JR, Uppal A, Oxlade O, Fregonese F, Bastos ML, Lan Z, et al.Active testing of groups at increased risk of acquiring SARS-CoV-2 in Canada: costs and human resource needs. CMAJ 2020;192(40):E1146-55. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2020 {published data only}
- Cohen JA, Mistry D, Kerr CC, Klein DJ.Schools are not islands: Balancing COVID-19 risk and educational benefits using structural and temporal countermeasures. medRxiv 2020. [DOI: 10.1101/2020.09.08.20190942] [DOI] [Google Scholar]
Curtius 2020 {published data only}
- Curtius J, Granzin M, Schrod J.Testing mobile air purifiers in a school classroom: Reducing the airborne transmission risk for SARS-CoV-2. medRxiv 2020. [DOI: 10.1101/2020.10.02.20205633] [DOI] [Google Scholar]
Di Domenico 2020a {published data only}
- Di Domenico L, Pullano G, Sabbatini CE, Boëlle P-Y, Colizza V.Modelling safe protocols for reopening schools during the COVID-19 pandemic in France. medRxiv 2020. [DOI: 10.1101/2020.05.08.20095521] [DOI] [PMC free article] [PubMed] [Google Scholar]
España 2020 {published data only}
- España G, Cavany S, Oidtman R, Barbera C, Costello A, Lerch A, et al.Impacts of K-12 school reopening on the COVID-19 epidemic in Indiana, USA. medRxiv 2020. [DOI: 10.1101/2020.08.22.20179960] [DOI] [PMC free article] [PubMed] [Google Scholar]
Germann 2020 {published data only}
- Germann TC, Smith MZ, Dauelsberg L, Fairchild G, Turton TL, Gorris ME, et al.Using an agent-based model to assess K-12 School reopenings under different COVID-19 spread scenarios – United States, school year 2020/21. medRxiv 2020. [DOI: 10.1101/2020.10.09.20208876] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gill 2020 {published data only}
- Gill BP, Goyal R, Hotchkiss J.Operating schools in a pandemic: predicted effects of opening, quarantining, and closing strategies; 16 September 2020. Available at https://www.mathematica.org/publications/operating-schools-in-a-pandemic-predicted-effects-of-opening-and-quarantining-strategies.
Head 2020 {published data only}
- Head JR, Andrejko KL, Cheng Q, Collender PA, Phillips S, Boser A, et al.The effect of school closures and reopening strategies on COVID-19 infection dynamics in the San Francisco Bay Area: a cross-sectional survey and modeling analysis. medRxiv 2020. [DOI: 10.1101/2020.08.06.20169797] [DOI] [Google Scholar]
Hoehl 2020 {published data only}
- Hoehl S, Schenk B, Rudych O, Göttig S, Foppa I, Kohmer N, et al.At-home self-testing of teachers with a SARS-CoV-2 rapid antigen test to reduce potential transmissions in schools. medRxiv 2020. [DOI: 10.1101/2020.12.04.20243410] [DOI] [Google Scholar]
Isphording 2020 {published data only}
- Isphording IE, Lipfert M, Pestel N.IZA DP No. 13790: School re-openings after summer breaks in Germany did not increase SARS-CoV-2 cases; October 2020. Available at www.iza.org/publications/dp/13790/school-re-openings-after-summer-breaks-in-germany-did-not-increase-sars-cov-2-cases.
Jones 2020 {published data only}
- Jones RD.COVID-19 trends in Florida K-12 schools, August 10 – November 14, 2020. medRxiv 2020. [DOI: 10.1101/2020.11.30.20241224] [DOI] [Google Scholar]
Kaiser 2020 {published data only}
- Kaiser A, Kretschmer D, Leszczensky L.Social network-based strategies for classroom size reduction can help limit outbreaks of SARS-CoV-2 in high schools. A simulation study in classrooms of four European countries. medRxiv 2020. [DOI: 10.1101/2020.11.30.20241166] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keeling 2020 {published data only}
- Keeling MJ, Tildesley MJ, Atkins BD, Penman B, Southall E, Guyver-Fletcher G, et al.The impact of school reopening on the spread of COVID-19 in England. medRxiv 2020. [DOI: 10.1101/2020.06.04.20121434] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kraay 2020 {published data only}
- Kraay AN, Hayashi MA, Berendes DM, Sobolik JS, Leon JS, Lopman BA.Risk of fomite-mediated transmission of SARS-CoV-2 in child daycares, schools, and offices: a modeling study. medRxiv 2020. [DOI: 10.1101/2020.08.10.20171629] [DOI] [PMC free article] [PubMed] [Google Scholar]
Landeros 2020 {published data only}
- Landeros A, Ji X, Lange K, Stutz TC, Xu J, Sehl ME, et al.An examination of school reopening strategies during the SARS-CoV-2 pandemic. medRxiv 2020. [DOI: 10.1101/2020.08.05.20169086] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lazebnik 2020 {published data only}
- Lazebnik T, Bunimovich-Mendrazitsky S.The signature features of COVID-19 pandemic in a hybrid mathematical model - implications for optimal work-school lockdown policy. medRxiv 2020. [DOI: 10.1101/2020.11.02.20224584] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2020 {published data only}
- Lee B, Hanley JP, Nowak S, Bates JH, Hébert-Dufresne L.Modeling the impact of school reopening on SARS-CoV-2 transmission using contact structure data from Shanghai. BMC Public Health 2020;20(1):1713. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyng 2020 {published data only}
- Lyng GD, Sheils NE, Kennedy CJ, Griffin D, Berke EM.Identifying optimal COVID-19 testing strategies for schools and businesses: balancing testing frequency, individual test technology, and cost. medRxiv 2020. [DOI: 10.1101/2020.10.11.20211011] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mauras 2020 {published data only}
- Mauras S, Cohen-Addad V, Duboc G, Dupré la Tour M, Frasca P, Mathieu C, et al.Mitigating COVID-19 outbreaks in workplaces and schools by hybrid telecommuting. medRxiv 2020. [DOI: 10.1101/2020.11.09.20228007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monod 2020 {published data only}
- Monod M, Blenkinsop A, Xi X, Hebert D, Bershan S, Tietze S, et al.Report 32: Age groups that sustain resurging COVID-19 epidemics in the United States. medRxiv 2020. [DOI: 10.1101/2020.09.18.20197376] [DOI] [PMC free article] [PubMed] [Google Scholar]
Munday 2020 {published data only}
- Munday JD, Sherratt K, Meakin S, Endo A, Pearson CA, Hellewell J, et al.Implications of the school-household network structure on SARS-CoV-2 transmission under different school reopening strategies in England. medRxiv 2020. [DOI: 10.1101/2020.08.21.20167965] [DOI] [PMC free article] [PubMed] [Google Scholar]
Naimark 2020 {published data only}
- Naimark D, Mishra S, Barrett K, Khan YA, Mac S, Ximenes R, et al.The potential impact of school closure relative to community-based non-pharmaceutical interventions on COVID-19 cases in Ontario, Canada. medRxiv 2020. [DOI: 10.1101/2020.11.18.20234351] [DOI] [Google Scholar]
Panovska‐Griffiths 2020a {published data only}
- Panovska-Griffiths J, Kerr CC, Stuart RM, Mistry D, Klein DJ, Viner RM, et al.Determining the optimal strategy for reopening schools, the impact of test and trace interventions, and the risk of occurrence of a second COVID-19 epidemic wave in the UK: a modelling study. Lancet Child & Adolescent Health 2020;4(11):817-27. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Panovska‐Griffiths 2020b {published data only}
- Panovska-Griffiths J, Kerr CC, Waites W, Stuart RM, Mistry D, Foster D, et al.Modelling the potential impact of mask use in schools and society on COVID-19 control in the UK. medRxiv 2020. [DOI: 10.1101/2020.09.28.20202937] [DOI] [PMC free article] [PubMed] [Google Scholar]
Phillips 2020 {published data only}
- Phillips B, Browne DT, Anand M, Bauch CT.Model-based projections for COVID-19 outbreak size and student-days lost to closure in Ontario childcare centers and primary schools. medRxiv 2020. [DOI: 10.1101/2020.08.07.20170407] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rozhnova 2020 {published data only}
- Rozhnova G, Dorp CH, Bruijning-Verhagen P, Bootsma MC, de Wijgert JH, Bonten MJ, et al.Model-based evaluation of school- and non-school-related measures to control the COVID-19 pandemic. medRxiv 2020. [DOI: 10.1101/2020.12.07.20245506] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shelley 2020 {published data only}
- Shelley CD, Chadwick PS, Manore C, Del Valle SY.Safely reopening K-12 schools during the COVID-19 pandemic. medRxiv 2020. [DOI: 10.1101/2020.10.07.20208710] [DOI] [Google Scholar]
Simonsen 2020 {published data only}
- Simonsen AB, Ruge IF, Quaade AS, Johansen JD, Thyssen JP, Zachariae C.High incidence of hand eczema in Danish schoolchildren following intensive hand hygiene during the COVID-19 pandemic: a nationwide questionnaire study. British Journal of Dermatology 2020;183(5):975-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sruthi 2020 {published data only}
- Sruthi CK, Biswal MR, Saraswat B, Joshi H, Prakash MK.How policies on restaurants, bars, nightclubs, masks, schools, and travel influenced Swiss COVID-19 reproduction ratios. medRxiv 2020. [DOI: 10.1101/2020.10.11.20210641] [DOI] [Google Scholar]
Tupper 2020 {published data only}
- Tupper P, Colijn C.COVID-19’s unfortunate events in schools: mitigating classroom clusters in the context of variable transmission. medRxiv 2020. [DOI: 10.1101/2020.10.20.20216267] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vlachos 2020 {published data only}
- Vlachos J, Hertegård E, Svaleryd H.School closures and SARS-CoV-2. Evidence from Sweden’s partial school closure. medRxiv 2020. [DOI: 10.1101/2020.10.13.20211359] [DOI] [Google Scholar]
Williams 2020 {published data only}
- Williams NE, Yao X, Pal A, Qian X, Rathod M, Xu C, et al.An innovative non-pharmaceutical intervention to mitigate SARS-CoV-2 spread: probability sampling to identify and isolate asymptomatic cases. medRxiv 2020. [DOI: 10.1101/2020.10.07.20208686] [DOI] [Google Scholar]
Zhang 2020 {published data only}
- Zhang J, Litvinova M, Liang Y, Zheng W, Shi H, Vespignani A, et al.The impact of relaxing interventions on human contact patterns and SARS- CoV-2 transmission in China. medRxiv 2020. [DOI: 10.1101/2020.08.03.20167056] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Anchordoqui 2020 {published data only}
- Anchordoqui LA, Chudnovsky EM, Paul TC.Risk assessment of COVID-19 airborne infection during hybrid learning. medRxiv 2020. [DOI: 10.1101/2020.09.24.20200782] [DOI] [Google Scholar]
Balabdaoui 2020 {published data only}
- Balabdaoui F, Mohr D.Age-stratified discrete compartment model of the COVID-19 epidemic with application to Switzerland. Scientific Reports 2020;10(1):21306. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bracis 2020 {published data only}
- Bracis C, Burns E, Moore M, Swan D, Reeves DB, Schiffer JT, et al.Widespread testing, case isolation and contact tracing may allow safe school reopening with continued moderate physical distancing: a modeling analysis of King County, WA data. medRxiv 2020. [DOI: 10.1101/2020.08.14.20174649] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks‐Pollock 2021 {published data only}
- Brooks-Pollock E, Read JM, McLean AR, Keeling MJ, Danon L.Mapping social distancing measures to the reproduction number for COVID-19. Philosophical Transactions of the Royal Society B: Biological Sciences 2021;376(1829):20200276. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buonsenso 2020 {published data only}
- Buonsenso D, De Rose C, Moroni R, Valentini P.SARS-CoV-2 infections in Italian schools: preliminary findings after one month of school opening during the second wave of the pandemic. medRxiv 2020. [DOI: 10.1101/2020.10.10.20210328] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coletti 2020 {published data only}
- Coletti P, Libin P, Petrof O, Willem L, Abrams S, Herzog SA, et al.A data-driven metapopulation model for the Belgian COVID-19 epidemic: assessing the impact of lockdown and exit strategies. medRxiv 2020. [DOI: 10.1101/2020.07.20.20157933] [DOI] [PMC free article] [PubMed] [Google Scholar]
Di Domenico 2020b {published data only}
- Di Domenico L, Pullano G, Sabbatini CE, Boëlle PY, Colizza V.Impact of lockdown on COVID-19 epidemic in Île-de-France and possible exit strategies. BMC Medicine 2020;18(1):240. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ehrhardt 2020 {published data only}
- Ehrhardt J, Ekinci A, Krehl H, Meincke M, Finci I, Klein J, et al.Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Württemberg, Germany. Eurosurveillance 2020;25(36):2001587. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gandolfi 2021 {published data only}
- Gandolfi A.Planning of school teaching during Covid-19. Physica D 2021;415:132753. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Garchitorena 2020 {published data only}
- Garchitorena A, Gruson H, Cazelles B, Karki T, Sudre B, Roche B.Integrated packages of non-pharmaceutical interventions increased public health response efficiency against COVID-19 during the first European wave: evidence from 32 European countries. medRxiv 2020. [DOI: 10.1101/2020.08.17.20174821] [DOI] [Google Scholar]
Johnson 2020 {published data only}
- Johnson KE, Stoddard M, Nolan RP, White DE, Hochberg NS, Chakravarty A.In the long shadow of our best intentions: model-based assessment of the consequences of school reopening during the COVID-19 pandemic. medRxiv 2020. [DOI: 10.1101/2020.09.18.20197400] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2020 {published data only}
- Kim S, Kim YJ, Peck KR, Jung E.School opening delay effect on transmission dynamics of coronavirus disease 2019 in Korea: based on mathematical modeling and simulation study. Journal of Korean Medical Science 2020;35(13):e143. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macartney 2020 {published data only}
- Macartney K, Quinn HE, Pillsbury AJ, Koirala A, Deng L, Winkler N, et al.Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child & Adolescent Health 2020;4(11):807-16. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McBride 2020 {published data only}
- McBride JA, Eickhoff J, Wald ER.Impact of COVID-19 quarantine and school cancelation on other common infectious diseases. Pediatric Infectious Disease Journal 2020;39(12):e449-52. [PMID: ] [DOI] [PubMed] [Google Scholar]
McBryde 2020 {published data only}
- McBryde ES, Trauer JM, Adekunle A, Ragonnet R, Meehan MT.Stepping out of lockdown should start with school re-openings while maintaining distancing measures. Insights from mixing matrices and mathematical models. medRxiv 2020. [DOI: 10.1101/2020.05.12.20099036] [DOI] [Google Scholar]
Sneppen 2020 {published data only}
- Sneppen K, Taylor RJ, Simonsen L.Impact of superspreaders on dissemination and mitigation of COVID-19. medRxiv 2020. [DOI: 10.1101/2020.05.17.20104745] [DOI] [Google Scholar]
Stage 2021 {published data only}
- Stage HB, Shingleton J, Ghosh S, Scarabel F, Pellis L, Finnie T.Shut and re-open: the role of schools in the spread of COVID-19 in Europe. medRxiv 2020. [DOI: 10.1101/2020.06.24.20139634] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stein‐Zamir 2020 {published data only}
- Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al.A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Eurosurveillance 2020;25(29):2001352. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wibbens 2020 {published data only}
- Wibbens P, Koo WW, McGahan AM.Which COVID policies are most effective? A Bayesian analysis of COVID-19 by jurisdiction. medRxiv 2020. [DOI: 10.1101/2020.12.01.20241695] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yoon 2020 {published data only}
- Yoon Y, Kim KH, Park H, Kim SY, Kim YJ.Stepwise school opening online and off-line and an impact on the epidemiology of COVID-19 in the pediatric population. medRxiv 2020. [DOI: 10.1101/2020.08.03.20165589] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Asgary 2021 {published data only}
- Asgary A, Cojocaru MG, Najafabadi MM, Wu J.Simulating preventative testing of SARS-CoV-2 in schools: policy implications. BMC Public Health 2021;21(1):125. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bilinski 2021 {published data only}
- Bilinski A, Salomon JA, Giardina J, Ciaranello A, Fitzpatrick MC.Passing the test: a model-based analysis of safe school-reopening strategies. Annals of Internal Medicine 2021;174(8):1090-100. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bosslet 2021 {published data only}
- Bosslet GT, Pollak M, Jang JH, Roll R, Sperling M, Khan B.The effect of in-person primary and secondary school instruction on county-level SARS-CoV-2 spread in Indiana. medRxiv 2021. [DOI: 10.1101/2021.03.17.21250449] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cruz 2021 {published data only}
- Cruz EH, Maciel JM, Clozato CL, Serpa MS, Navaux PO, Meneses E, et al.Simulation-based evaluation of school reopening strategies during COVID-19: a case study of São Paulo, Brazil. Epidemiology and Infection 2021;149:e118. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ertem 2021 {published data only}
- Ertem Z, Schechter-Perkins E, Oster E, den Berg P, Epshtein I, Chaiyakunapruk N, et al.The impact of school opening model on SARS-CoV-2 community incidence and mortality: a nationwide cohort study; 27 October 2021. Available at www.nature.com/articles/s41591-021-01563-8.pdf. [DOI: 10.1038/s41591-021-01563-8] [DOI] [PubMed]
Gandini 2021 {published data only}
- Gandini S, Rainisio M, Iannuzzo ML, Bellerba F, Cecconi F, Scorrano L.A cross-sectional and prospective cohort study of the role of schools in the SARS-CoV-2 second wave in Italy. Lancet Regional Health - Europe 2021;5:100092. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lessler 2021 {published data only}
- Lessler J, Grabowski MK, Grantz KH, Badillo-Goicoechea E, Metcalf CJ, Lupton-Smith C, et al.Household COVID-19 risk and in-person schooling. Science 2021;372(6546):1092-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2021 {published data only}
- Liu D, Lin G, Sun X, Du Y, Liu H, Qu M.Different school reopening plans on Coronavirus Disease 2019 case growth rates in the school setting in the United States. Journal of School Health 2021;91(5):370-5. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller 2021 {published data only}
- Miller GF, Greening B Jr, Rice KL, Arifkhanova A, Meltzer MI, Coronado F.Modeling the transmission of Covid-19: impact of mitigation strategies in prekindergarten-grade 12 public schools, United States, 2021. Journal of Public Health Management and Practice 2021 Apr 30 [Epub ahead of print]. [DOI: 10.1097/PHH.0000000000001373] [DOI] [PMC free article] [PubMed]
Pavilonis 2021 {published data only}
- Pavilonis B, Ierardi AM, Levine L, Mirer F, Kelvin EA.Estimating aerosol transmission risk of SARS-CoV-2 in New York City public schools during reopening. Environmental Research 2021;195:110805. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reinbold 2021 {published data only}
- Reinbold GW.Effect of Fall 2020 K-12 instruction types on COVID-19 cases, hospital admissions, and deaths in Illinois counties. American Journal of Infection Control 2021;49(9):1146-51. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Somekh 2021 {published data only}
- Somekh I, Shohat T, Boker LK, Simões EA, Somekh E.Reopening schools and the dynamics of SARS-CoV-2 infections in Israel: a nationwide study. Clinical Infectious Diseases 2021 Jan 18 [Epub ahead of print]. [DOI: 10.1093/cid/ciab035] [DOI] [PMC free article] [PubMed]
van den Berg 2021 {published data only}
- den Berg P, Schechter-Perkins EM, Jack RS, Epshtein I, Nelson R, Oster E, et al.Effectiveness of three versus six feet of physical distancing for controlling spread of COVID-19 among primary and secondary students and staff: a retrospective, state-wide cohort study. Clinical Infectious Diseases 2021;73(10):1871–88. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Willem 2021 {published data only}
- Willem L, Abrams S, Libin PJ, Coletti P, Kuylen E, Petrof O, et al.The impact of contact tracing and household bubbles on deconfinement strategies for COVID-19. Nature Communications 2021;12(1):1524. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2021 {published data only}
- Young BC, Eyre DW, Kendrick S, White C, Smith S, Beveridge G, et al.A cluster randomised trial of the impact of a policy of daily testing for contacts of COVID-19 cases on attendance and COVID-19 transmission in English secondary schools and colleges. medRxiv 2020. [DOI: 10.1101/2021.07.23.21260992] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yuan 2021 {published data only}
- Yuan P, Aruffo E, Ogden N, Tan Y, Gatov E, Gournis E, et al.School and community reopening during the COVID-19 pandemic: a mathematical modeling study (preprint). medRxiv 2020. [DOI: 10.1101/2021.01.13.21249753] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Aleta 2020
- Aleta A, Moreno Y.Age differential analysis of COVID-19 second wave in Europe reveals highest incidence among young adults. medRxiv 2020. [DOI: 10.1101/2020.11.11.20230177] [DOI] [Google Scholar]
Bin Nafisah 2018
- Bin Nafisah S, Alamery AH, Al Nafesa A, Aleid B, Brazanji NA.School closure during novel influenza: A systematic review. Journal of Infection and Public Health 2018;11(5):657-61. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bonell 2020
- Bonell C, Melendez-Torres GJ, Viner RM, Rogers MB, Whitworth M, Rutter H, et al.An evidence-based theory of change for reducing SARS-CoV-2 transmission in reopened schools. Health & Place 2020;64:102398. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brozek 2021
- Brozek JL, Canelo-Aybar C, Akl EA, Bowen JM, Bucher J, Chiu WA, et al.GRADE Guidelines 30: the GRADE approach to assessing the certainty of modeled evidence—An overview in the context of health decision-making. Journal of Clinical Epidemiology 2021;129:138-50. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buonsenso 2021
- Buonsenso D, Munblit D, De Rose C, Sinatti D, Ricchiuto A, Carfi A, et al.Preliminary evidence on long COVID in children. Acta Paediatrica 2021;110(7):2208-11. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns A 2021
- Burns AA, Gutfraind A.Effectiveness of isolation policies in schools: evidence from a mathematical model of influenza and COVID-19. PeerJ 2021;9:e11211. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burns J 2021
- Burns J, Movsisyan A, Stratil JM, Biallas RL, Coenen M, Emmert-Fees KM, et al.International travel‐related control measures to contain the COVID‐19 pandemic: a rapid review. Cochrane Database of Systematic Reviews 2021, Issue 3. Art. No: CD013717. [DOI: 10.1002/14651858.CD013717.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020a
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al.Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:l6890. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Castagnoli 2020
- Castagnoli R, Votto M, Licari A, Brambilla I, Bruno R, Perlini S, et al.Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatrics 2020;174(9):882-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Choi 2020
- Choi SH, Kim HW, Kang JM, Kim DH, Cho EY.Epidemiology and clinical features of coronavirus disease 2019 in children. Clinical and Experimental Pediatrics 2020;63(4):125-32. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chowell 2011
- Chowell G, Viboud C, Simonsen L, Miller MA.Measuring the benefits of school closure interventions to mitigate influenza. Expert Review of Respiratory Medicine 2011;5(5):597-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Christakis 2020
- Christakis DA.School reopening - the pandemic issue that is not getting its due. JAMA Pediatrics 2020;174(10):928. [PMID: ] [DOI] [PubMed] [Google Scholar]
Couzin‐Frankel 2020
- Couzin-Frankel J, Vogel G.Not open and shut: School openings across globe suggest ways to keep coronavirus at bay, despite outbreaks; 7 July 2020. Available at www.science.org/content/article/school-openings-across-globe-suggest-ways-keep-coronavirus-bay-despite-outbreaks. [DOI: 10.1126/science.abd7107] [DOI]
Curtius 2021
- Curtius J, Granzin M, Schrod J.Testing mobile air purifiers in a school classroom: Reducing the airborne transmission risk for SARS-CoV-2. Aerosol Science and Technology 2021;55(5):586-99. [DOI: 10.1080/02786826.2021.1877257] [DOI] [Google Scholar]
Dattner 2020
- Dattner I, Goldberg Y, Katriel G, Yaari R, Gal N, Miron Y, et al.The role of children in the spread of COVID-19: Using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. medRxiv 2020. [DOI: 10.1101/2020.06.03.20121145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Davies 2020
- Davies NG, Klepac P, Liu Y, Prem K, Jit M, CMMID COVID-19 working group, et al.Age-dependent effects in the transmission and control of COVID-19 epidemics. Nature Medicine 2020;26(8):1205-11. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dibner 2020
- Dibner KA, Schweingruber HA, Christakis DA.Reopening k-12 schools during the covid-19 pandemic: A report from the national academies of sciences, engineering, and medicine. JAMA 2020;324(9):833-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Di Domenico 2021
- Di Domenico L, Pullano G, Sabbatini CE, Boëlle PY, Colizza V.Modelling safe protocols for reopening schools during the COVID-19 pandemic in France. Nature Communications 2021;12(1):1073. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dong 2020
- Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al.Epidemiology of COVID-19 among children in China. Pediatrics 2020;145(6):e20200702. [PMID: ] [DOI] [PubMed] [Google Scholar]
EndNote X9 [Computer program]
- EndNote X9.Clarivate, 2013.
Engzell 2021
- Engzell P, Frey A, Verhagen MD.Learning loss due to school closures during the COVID-19 pandemic. Proceedings of the National Academy of Sciences 2021;118(17):e2022376118. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fadlallah 2020
- Fadlallah R, Jamal D, Daher N, Masri R, Hemadi N.K2P COVID-19 Series: supplement on school reopening (2 of 3): impact of school closure/reopening and school management practices on COVID-19 pandemic. Knowledge to Policy (K2P) Center, Beirut, Lebanon, 18 September 2020. Available at www.aub.edu.lb/k2p/Documents/K2P%20COVID19%20Supplement%20on%20School%20Re-opening%20%282%20of%203%29%20Impact%20of%20School%20Closure%20Reopening%20and%20School%20Management%20Practices%20on%20COVID19%20Pandemic.pdf.
Fischer 2021
- Fischer CB, Adrien N, Silguero JJ, Hopper JJ, Chowdhury AI, Werler MM.Mask adherence and rate of COVID-19 across the United States. PLoS One 2021;16(4):e0249891. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fontanet 2020
- Fontanet A, Tondeur L, Madec Y, Grant R, Besombes C, Jolly N, et al.Cluster of COVID-19 in northern France: A retrospective closed cohort study. medRxiv 2020. [DOI: 10.1101/2020.04.18.20071134] [DOI] [Google Scholar]
Fung 2015
- Fung IC, Gambhir M, Glasser JW, Gao H, Washington ML, Uzicanin A, et al.Modeling the effect of school closures in a pandemic scenario: exploring two different contact matrices. Clinical Infectious Diseases 2015;60 Suppl 1:S58-63. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gandini 2021
- Gandini S, Rainisio M, Iannuzzo ML, Bellerba F, Cecconi F, Scorrano L.No evidence of association between schools and SARS-CoV-2 second wave in Italy. medRxiv 2020. [DOI: 10.1101/2020.12.16.20248134] [DOI] [Google Scholar]
Garritty 2020
- Garritty C, Gartlehner G, Kamel C, King VJ, Nussbaumer-Streit B, Stevens A, et al.Cochrane Rapid Reviews. Interim Guidance from the Cochrane Rapid Reviews Methods Group; March 2020. Available at methods.cochrane.org/rapidreviews/sites/methods.cochrane.org.rapidreviews/files/public/uploads/cochrane_rr_-_guidance-23mar2020-final.pdf.
Golberstein 2020
- Golberstein E, Wen H, Miller BF.Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics 2020;174(9):819-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
Götzinger 2020
- Götzinger F, Santiago-García B, Noguera-Julián A, Lanaspa M, Lancella L, Calò Carducci FI, et al.COVID-19 in children and adolescents in Europe: a multinational, multicentre cohort study. Lancet Child & Adolescent Health 2020;4(9):653-61. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Han 2021
- Han X, Li X, Xiao Y, Yang R, Wang Y, Wei X.Distinct characteristics of COVID-19 infection in children. Frontiers in Pediatrics 2021;9:619738. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Head 2021
- Head JR, Andrejko KL, Cheng Q, Collender PA, Phillips S, Boser A, et al.School closures reduced social mixing of children during COVID-19 with implications for transmission risk and school reopening policies. Journal of the Royal Society Interface 2021;18(177):20200970. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2021
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA.Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Howard 2021
- Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, Westhuizen HM, et al.An evidence review of face masks against COVID-19. Proceedings of the National Academy of Sciences 2021;118(4):e2014564118. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hultcrantz 2017
- Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al.The GRADE Working Group clarifies the construct of certainty of evidence. Journal of Clinical Epidemiology 2017;87:4-13. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Isfeld‐Kiely 2014
- Isfeld-Kiely H, Moghadas S.Effectiveness of school closure for the control of influenza: a review of recent evidence. Available at nccid.ca/publications/effectiveness-of-school-closure-for-the-control-of-influenza/ 2014.
Ismail 2021
- Ismail SA, Saliba V, Lopez Bernal J, Ramsay ME, Ladhani SN.SARS-CoV-2 infection and transmission in educational settings: a prospective, cross-sectional analysis of infection clusters and outbreaks in England. Lancet Infectious Diseases 2021;21(3):344-53. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kaiser 2021
- Kaiser AK, Kretschmer D, Leszczensky L.Social network-based cohorting to reduce the spread of SARS-CoV-2 in secondary schools: A simulation study in classrooms of four European countries. Lancet Regional Health - Europe 2021;8:100166. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keeling 2021
- Keeling MJ, Tildesley MJ, Atkins BD, Penman B, Southall E, Guyver-Fletcher G, et al.The impact of school reopening on the spread of COVID-19 in England. Philosophical Transactions of the Royal Society B: Biological Sciences 2021;376(1829):20200261. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kneale 2020
- Kneale D, O'Mara-Eves A, Rees R, Thomas J.School closure in response to epidemic outbreaks: Systems-based logic model of downstream impacts. F1000Research 2020;9:352. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Koh 2020
- Koh WC, Naing L, Chaw L, Rosledzana MA, Alikhan MF, Jamaludin SA, et al.What do we know about SARS-CoV-2 transmission? A systematic review and meta-analysis of the secondary attack rate and associated risk factors. PLoS One 2020;15(10):e0240205. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kratzer 2021
- Kratzer S, Verboom B, Biallas R, Featherstone R, Klinger C, Movsisyan A, et al.Unintended consequences of measures implemented in the school setting to contain the COVID-19 pandemic: a scoping review protocol; 25 March 2021. Available at osf.io/6kqpx/. [DOI] [PMC free article] [PubMed]
Landeros 2021
- Landeros A, Ji X, Lange K, Stutz TC, Xu J, Sehl ME, et al.An examination of school reopening strategies during the SARS-CoV-2 pandemic. PLOS ONE 2021;16(5):e0251242. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Laws 2021
- Laws RL, Chancey RJ, Rabold EM, Chu VT, Lewis NM, Fajans M, et al.Symptoms and transmission of SARS-CoV-2 among children - Utah and Wisconsin, March-May 2020. Pediatrics 2021;147(1):e2020027268. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lazebnik 2021
- Lazebnik T, Bunimovich-Mendrazitsky S.The signature features of COVID-19 pandemic in a hybrid mathematical model-implications for optimal work-school lockdown policy. Advanced Theory and Simulations 2021;4(5):2000298. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2010
- Lee BY, Brown ST, Cooley P, Potter MA, Wheaton WD, Voorhees RE, et al.Simulating school closure strategies to mitigate an influenza epidemic. Journal of Public Health Management and Practice 2010;16(3):252-61. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2021
- Lee B, Raszka WV Jr.COVID-19 in children: looking forward, not back. Pediatrics 2021;147(1):e2020029736. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lelieveld 2020
- Lelieveld J, Helleis F, Borrmann S, Cheng Y, Drewnick F, Haug G, et al.Model calculations of aerosol transmission and infection risk of COVID-19 in indoor environments. International Journal of Environmental Resesarch in Public Health 2020;17(21):8114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyng 2021
- Lyng GD, Sheils NE, Kennedy CJ, Griffin DO, Berke EM.Identifying optimal COVID-19 testing strategies for schools and businesses: Balancing testing frequency, individual test technology, and cost. PLoS One 2021;16(3):e0248783. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Macartney 2020
- Macartney K, Quinn HE, Pillsbury AJ, Koirala A, Deng L, Winkler N, et al.Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child & Adolescent Health 2020;4(11):807-16. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Microsoft 2018 [Computer program]
- Microsoft Excel.Microsoft Corporation, 2018.
Munday 2021
- Munday JD, Sherratt K, Meakin S, Endo A, Pearson CA, Hellewell J, et al.Implications of the school-household network structure on SARS-CoV-2 transmission under school reopening strategies in England. Nature Communications 2021;12(1):1942. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Naimark 2021
- Naimark D, Mishra S, Barrett K, Khan YA, Mac S, Ximenes R, et al.Simulation-based estimation of SARS-CoV-2 infections associated with school closures and community-based nonpharmaceutical interventions in Ontario, Canada. JAMA Network Open 2021;4(3):e213793. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCCMT 2021
- National Collaborating Centre for Methods and Tools.Living Rapid Review Update 17: What is the specific role of daycares and schools in COVID-19 transmission? 12 August 2021. Available at res.nccmt.ca/res-schools-daycares-EN.
NCIRS 2020
- National Centre for Immunisation Research and Surveillance (NCIRS).COVID-19 in schools and early childhood education and care services - the Term 2 experience in NSW; 31 July 2020. Available at ncirs.org.au/sites/default/files/2020-08/COVID-19%20Transmission%20in%20educational%20settings%20in%20NSW%20Term%202%20report_0.pdf.
Otte im Kampe 2020
- Otte Im Kampe E, Lehfeld AS, Buda S, Buchholz U, Haas W.Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Eurosurveillance 2020;25(38):2001645. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ouzzani 2016
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A.Rayyan - a web and mobile app for systematic reviews. Systematic Reviews 2016;5(1):210. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Panovska‐Griffiths 2021
- Panovska-Griffiths J, Kerr CC, Waites W, Stuart RM, Mistry D, Foster D, et al.Modelling the potential impact of mask use in schools and society on COVID-19 control in the UK. Scientific Reports 2021;11(1):8747. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2020
- Park YJ, Choe YJ, Park O, Park SY, Kim YM, Kim J, et al.Contact tracing during coronavirus disease outbreak, South Korea, 2020. Emerging Infectious Disease 2020;26(10):2465-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pfadenhauer 2017
- Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, et al.Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implementation Science 2017;12(1):21. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Phillips 2021
- Phillips B, Browne DT, Anand M, Bauch CT.Model-based projections for COVID-19 outbreak size and student-days lost to closure in Ontario childcare centres and primary schools. Scientific Reports 2021;11(1):6402. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Prem 2020
- Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al.The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health 2020;5(5):e261-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Public Health Ontario 2020
- Ontario Agency for Health Protection and Promotion (Public Health Ontario).COVID-19 pandemic school closure and reopening impacts; 27 July 2020. Available at www.publichealthontario.ca/-/media/documents/ncov/main/2020/08/covid-19-school-closure-reopening-impacts.pdf?la=en.
Ramos 2015
- Ramos MC, Barton P, Jowett S, Sutton AJ.A systematic review of research guidelines in decision-analytic modeling. Value in Health 2015;18(4):512-29. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rashid 2015
- Rashid H, Ridda I, King C, Begun M, Tekin H, Wood JG, et al.Evidence compendium and advice on social distancing and other related measures for response to an influenza pandemic. Paediatric Respiratory Reviews 2015;16(2):119-26. [PMID: ] [DOI] [PubMed] [Google Scholar]
Rozhnova 2021
- Rozhnova G, Dorp CH, Bruijning-Verhagen P, Bootsma MC, de Wijgert JH, Bonten MJ, et al.Model-based evaluation of school- and non-school-related measures to control the COVID-19 pandemic. Nature Communications 2021;12(1):1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2020
- Smith WC.Potential long-term consequences of school closures: Lessons from the 2013-2016 Ebola pandemic. Available at www.researchsquare.com/article/rs-51400/v1 (accessed prior to 20 November 2021). [DOI: 10.21203/rs.3.rs-51400/v1] [DOI] [PMC free article] [PubMed]
Stein‐Zamir 2020
- Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al.A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Eurosurveillance 2020;25(29):2001352. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2016
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al.ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2021
- Sterne JA, Hernán MA, McAleenan A, Reeves BC, Higgins JP.Chapter 25: Assessing risk of bias in a non-randomized study. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Thompson 2021
- Thompson DA, Abbasizanjani H, Fry R, Marchant E, Griffiths L, Akbari A, et al.Staff-pupil SARS-CoV-2 infection pathways in schools in Wales: a population-level linked data approach. BMJ Paediatrics Open 2021;5(1):e001049. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
UNESCO 2021
- UNESCO.Education: From disruption to recovery. Available at en.unesco.org/covid19/educationresponse (accessed prior to 20 November 2021).
Viner 2020
- Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al.School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child & Adolescent Health 2020;4(5):397-404. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viner 2021a
- Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, et al.Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: a systematic review and meta-analysis. JAMA Pediatrics 2021;175(2):143-56. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viner 2021b
- Viner RM, Bonell C, Drake L, Jourdan D, Davies N, Baltag V, et al.Reopening schools during the COVID-19 pandemic: governments must balance the uncertainty and risks of reopening schools against the clear harms associated with prolonged closure. Archives of Disease in Childhood 2021;106(2):111-3. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vlachos 2021
- Vlachos J, Hertegård E, Svaleryd HB.The effects of school closures on SARS-CoV-2 among parents and teachers. Proceedings of the National Academy of Sciences 2021;118(9):e2020834118. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walsh 2021
- Walsh S, Chowdhury A, Braithwaite V, Russell S, Birch JM, Ward JL, et al.Do school closures and school reopenings affect community transmission of COVID-19? A systematic review of observational studies. BMJ Open 2021;11(8):e053371. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al.QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529-36. [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2019
- World Health Organization.Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza: annex: report of systematic literature reviews. Available at apps.who.int/iris/handle/10665/329439 2019.
WHO 2020a
- World Health Organization.WHO Director-General's opening remarks at the media briefing on COVID-19; 11 March 2020. Available at www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
WHO 2020b
- World Health Organization.WHO, UNICEF urge safe school reopening in Africa; 20 August 2020. Available at www.who.int/news-room/feature-stories/detail/who-unicef-urge-safe-school-reopening-in-africa.
Zhang 2021
- Zhang J, Litvinova M, Liang Y, Zheng W, Shi H, Vespignani A, et al.The impact of relaxing interventions on human contact patterns and SARS-CoV-2 transmission in China. Science Advances 2021;7(19):eabe2584. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zimmermann 2021
- Zimmermann P, Curtis N.Why is COVID-19 less severe in children? A review of the proposed mechanisms underlying the age-related difference in severity of SARS-CoV-2 infections. Archives of Disease in Childhood 2021;106:429-39. [PMID: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Krishnaratne 2020
- Krishnaratne S, Pfadenhauer LM, Coenen M, Geffert K, Jung-Sievers C, Klinger C, et al.Measures implemented in the school setting to contain the COVID‐19 pandemic: a rapid scoping review. Cochrane Database of Systematic Reviews 2020, Issue 12. Art. No: CD013812. [DOI: 10.1002/14651858.CD013812] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krishnaratne 2021
- Krishnaratne S, Littlecott H, Coenen M, Geffert K, Jung-Sievers C, Kratzer S, et al.Measures implemented in the school setting to contain the COVID-19 pandemic: a rapid review protocol; 8 October 2021. Available at osf.io/vepzf/?view_only=1c15168a1f7f420f9388cdf102fc99a1. [DOI: 10.17605/OSF.IO/VEPZF] [DOI]
Pfadenhauer 2020
- Pfadenhauer LM, Krishnaratne S, Burns J, Coenen M, Geffert K, Jung-Sievers C, et al.Measures implemented in the school setting to contain the COVID-19 pandemic: a scoping review protocol; 14 October 2020. Available at osf.io/bm2xu. [DOI: 10.17605/OSF.IO/BM2XU] [DOI] [PMC free article] [PubMed]