Abstract
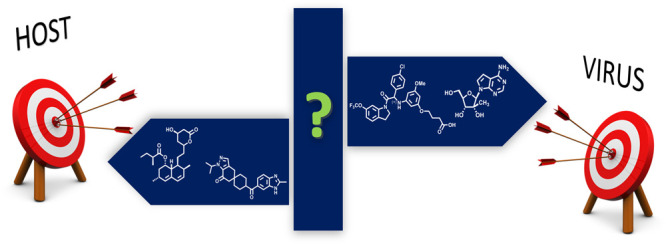
The COVID pandemic has evidenced how vulnerable we are to emerging infectious diseases and how short our current armamentarium is. Flavivirus, single stranded RNA viruses transmitted by arthropods, are considered a global health challenge. No drugs to treat these infections have been approved. In this Viewpoint, we analyze the advantages and disadvantages of two different, but probably also complementary, therapeutic approaches: virus-targeting antivirals and host-targeting drugs.
Keywords: flavivirus, virus-targeting, host-targeting, emerging virus
The current COVID-19 pandemic has evidenced our short armamentarium to fight emerging viral diseases. Moreover, it has raised false expectations feeding the idea that an effective antiviral against a new virus could be developed in a short time period. Fortunately, highly effective vaccines have been developed in an extraordinary short time interval, which has become a milestone in prevention. This historical situation should make us consider which approaches must be followed in order to develop antivirals against other life-threatening viruses and for which, so far, no effective vaccines or antivirals have been developed.
In Southern Europe and particularly the Iberian Peninsula (Spain and Portugal), (re)emerging flaviviruses represent a very serious threat transmitted by the bites of infected mosquitoes. Viruses in this group include Dengue virus (DENV1–4), Zika virus (ZIKV), Yellow Fever Virus (YFV), and West Nile virus (WNV). Their ability to emerge or re-emerge is the product of a variety of eco-epidemiological factors such as the expansion of competent vectors to new areas, global warming, changes in land use and/or urbanization, and globalization of travel and trade.1 Therefore, flaviviruses are considered “well-placed” candidates for the next viral pandemic.2 The particular relevance of the flaviviruses WNV and DENV to Southern Europe has become patent by the recent outbreak of West Nile encephalitis in Southeastern Spain in 20203 or the epidemic of dengue in Madeira (Portugal) in 2010.4 Whereas human vaccines against few mosquito-borne flaviviruses such as YFV and Japanese encephalitis virus are highly efficient, there is still a lack of vaccines or specific therapies against the majority of the mosquito-borne flaviviruses. It is not the objective of this Viewpoint to enumerate compounds and approaches described to fight against these viruses, but to use some recent illustrative examples to describe the current state of the art, the pros and cons of antivirals targeting the viral machinery or the host, together with some reflections for the close future.
Flaviviruses are single-stranded positive RNA viruses whose genome encodes three structural proteins (capsid (C), membrane (M), and envelope (E)) and seven nonstructural proteins, with the most studied for antiviral intervention being the NS3 protease with its cofactor NS2B and the NS5 that contains the methyltransferase/guanylyltransferase (MTase/GTase) domain for mRNA capping and the RNA-dependent RNA polymerase (RdRp). Interestingly, the high sequence and structural similarities among NS3/NS2B5 and NS54 from different flaviviruses has supported the idea that compounds inhibiting these enzymes may lead to pan-flavivirus antivirals. Indeed, most of the approved drugs against human immunodeficiency virus (HIV) or hepatitis C virus (HCV) target their respective proteases or polymerases. Excellent reviews describing direct antivirals have been recently published,6−9 so just a couple of illustrative examples are here included.
The N-terminal domain of NS3 contains the residues of the active site of the serine-protease and requires NS2B as a cofactor. Flavivirus protease shows a strong preference for cleaving peptide sequences after two basic residues. Peptide-based inhibitors, including those with a warhead to target the serine in the active site, have shown potent inhibition in enzymatic assays but have not led to significant antiviral activities in cell culture.10 The dibasic recognition moiety mimicking the substrate and the rather shallow binding site accounts for the poor druglike properties of the identified protease inhibitors.10 Alternatively, allosteric inhibitors sound more promising. Yao et al. described pyrazine derivatives (exemplified by 1, Figure 1) as allosteric inhibitors of ZIKV protease which exhibited antiviral activities at sub μM concentrations and protective effects in a mouse model of ZIKV infection.11 These compounds were also inhibitory to DENV-2, DENV-3, and WNV proteases while being inactive against several human serine-cysteine-, aspartic- and metallo-proteases.11 Compound 1 was proposed to bind to an allosteric hydrophobic pocket of NS3 keeping the protein in an open inactive conformation.11 However, there is some debate about this hypothetical binding site based on the insufficient electron density of the ligand.12 Other chemical classes are also being studied as allosteric inhibitors of NS3/NS2B including proline-based compounds meant to improve lipophilic ligand efficiency compared to previously identified 2-phenoxynaphthalene derivatives.12 Also a conformational switch assay has been developed to monitor the conformation of NS2B that may allow the characterization of new allosteric inhibitors.13 Thus, this area of allosteric inhibition of the viral protease is being nowadays explored with different chemical series, and represent an interesting approach for direct pan-antivirals against flavivirus.
Figure 1.
Chemical structures of relevant direct-targeting antivirals (1–8) and host-targeting drugs (9, 10) against flavivirus.
The viral NS5 contains the MTase/GTase activity at the N-terminus to cap the mRNA and the RNA-dependent RNA-polymerase (RdRp) activity at the C-terminus, which lacks proofreading activity, thus facilitating the rate of mutations. The availability of the X-ray structure of different flavivirus NS5 MTases, in complex with substrate analogues or inhibitors (i.e., Sinefugin, 2), has led to different virtual screening campaigns to identify potential inhibitors.9 The identified hits show activity against the MTase/GTase of different flaviviruses, but in most cases the inhibitory activity in enzymatic assays either has not been translated into potent antiviral effect in cell culture or has shown a low therapeutic window.
Compounds acting at the level of RdRps have provided one of the most successful approaches for the treatment of positive strand RNA virus infections such as HCV (i.e., sofosbuvir). The anti-influenza compound favipiravir (T-705, 3), a prodrug of the nucleotide triphosphate (T-705-RTP, 4), inhibits flaviviruses, including WNV in animal models14 through a dual mechanism of action: direct inhibition of the polymerase and lethal mutagenesis.15 Another interesting example is 7-deaza-2′-C-methyladenosine (5) that was able to protect WNV-infected mice from mortality if the treatment was initiated 3 days postinfection.16 Galidesivir (BCX4430, 6), a C-imino adenosine analogue, also reduces the replication of several flaviviruses in mouse models and diminishes viremia in ZIKV-infected rhesus macaques.17
Interestingly, recent reports on potent antivirals with pan-serotype dengue inhibition involve a novel target: the viral NS4B, a transmembrane protein forming part of the replication complex in the endoplasmic reticulum membrane. This is the case for JNJ-A07 (7) exhibiting nano- to picomolar potencies against a panel of 21 dengue clinical isolates from the four serotypes.18 JNJ-A07 seems to block the “de novo” formation of the NS3-NS4B complex and shows a high barrier to resistance, despite targeting a viral protein. Promising data have been obtained in DENV-2 infection mouse models, with a rapid and significant reduction in viral load. Also NITD-688 (8) has been described as a potent inhibitor of all four types of dengue serotypes, targeting NS4B.19 Pharmacokinetic and toxicological studies support the potential of this compound as a preclinical candidate. Remarkably, both compounds (7 and 8) are active against different DENV serotypes, but not against other flaviviruses.
A more recent approach for the development of broad-spectrum antivirals to combat current and future flavivirus targets host factors required for viral replication rather than viral proteins.20 Flaviviruses redirect cellular metabolism, and an increasing number of cellular factors and pathways essential for their replication are now being identified. In some cases, specific factors can be shared with other viruses, including SARS-CoV-2. For instance, cellular furin protease is required for SARS-CoV-2 entry but also for flavivirus maturation. Therefore, furin inhibitors will potentially be useful to combat both pathogens.21 Besides co-opting for isolated host factors, flaviviruses deeply rearrange major cellular pathways including host lipid metabolism.22 In this context, lovastatin (9), a cholesterol lowering agent, increased survival rates in mouse models of DENV infection.23 However, retrospective studies in patients treated with statins do not further support a positive impact of statins in dengue severity.24,25 Inhibition of lipid synthesis by targeting the acetyl-coA carboxylase using PF-05175157 (10) reduced viremia and virus load in the kidney of mice experimentally infected with WNV, although it was unable to block neuroinvasion.26 Additionally, pharmacological activation of adenosine monophosphate activated protein kinase (AMPK), a master regulator of cellular metabolism, appeared as an interesting strategy for antiviral intervention against WNV, DENV, and ZIKV.27 However, the results obtained with metformin, a first-line anti-diabetic drug and indirect AMPK activator, do not further support its therapeutic value for DENV infections.28,29 SARS-CoV-2 manipulation of host metabolism shares some similar metabolic requirements with flavivirus infection, but in this case both statins and metformin could have a positive effect on infection outcome.30,31 These differences may suggest that the efficacy of certain host-targeting antiviral approaches could be pathogen-dependent.
Both the virus-directed and host-directed antivirals have pros and cons that require a detailed analysis, summarized in Figure 2. Virus-directed antivirals are supported by their success based on approved drugs, particularly against HIV and HCV. These drugs have certainly changed the mortality and morbidity of patients and are characterized by wide therapeutic windows related to their selective mechanism of action. Their main disadvantages are the difficulties encountered to develop broad-spectrum antivirals due to the peculiarities of each virus or family of virus. Also relevant is the rapid development of virus-resistant strains, a limitation that has been successfully overpassed by combination therapies.
Figure 2.
Pros and cons of virus-targeting and host-targeting approaches.
On the other hand, host-targeted antivirals constitute a very interesting approach in the search for broad spectrum antivirals suitable to combat present or future unknown viral emergences since the same pathway can be altered by the infection of different viruses. Also very relevant is that compounds acting on host targets are expected to show a high barrier to resistance and this is particularly relevant for RNA viruses with a high tendency to mutate, such as flaviviruses. Lastly, host targets are also ideal for drug repositioning. On the disadvantages side, the most relevant limitation is the toxicity associated and side effects since we are dealing with a target or a pathway constitutively expressed in the host. Also, and particularly important for repositioning drugs, data from the clinic indicate that in many cases the doses required for a significant antiviral effect largely exceed those already approved for other therapeutic purposes. Along this line, the huge efforts to find new antivirals by drug repositioning (i.e., hydroxychloroquine or favipiravir) made during the COVID-19 pandemic have demonstrated that this approach is not always as successful as desired.32,33
It should be highlighted that more and more reports describe the interaction of nonstructural viral proteins with the host factors, which might shed light on how the virus manipulates the host and is able to interfere with the innate and adaptive immune response.34 Moreover, we are also starting to understand how the replication complexes for flavivirus are constructed at the endoplasmic reticulum.35 This opens new perspectives for antiviral intervention targeting virus-host interactions.
As for most anti-infective agents, an ideal compound for targeting flavivirus infection should be available for oral administration and with a wide therapeutic window so that it could even by applied as a prophylactic to try to reduce the viremia as soon as possible. Even more, for certain flaviviruses such as WNV, it should be able to cross the blood-brain barrier to fight neurotropic infections. Two additional desirable properties for the active principle, thinking in the developing countries where the incidence of these infectious is very high, are an accessible price and high stability to support the climate conditions. Even, it is claimed that a broad-spectrum antiviral targeting also other RNA viruses is what is needed. But is this really achievable? The reality, particularly relevant through the COVID pandemic, has shown that our armamentarium for viral diseases is really limited, so much more basic and applied research is required. Probably the solution will not come from a single agent, as already learned from other antiviral interventions. It might be that the right combination of an antiviral-directed agent and a host-targeting compound will unify the pros from both approaches. Drug repurposing, particularly for host-targeting agents, is indeed a straightforward way to jump into the clinic, but this should not be accompanied by a relaxation of what the development of an antiviral drug requires36,37 and should not rely exclusively on biochemical or cell culture assays.
Acknowledgments
Our own research in the search of antivirals against West Nile virus and other flaviviruses is financed by grants PID2019-105117RR-C22 and PID2019-105117RR-C21 funded by Ministerio de Ciencia e Innovación, Agencia Estatal de Investigación MCIN/AEI/10.13039/501100011033.
Views expressed in this viewpoint are those of the author and not necessarily the views of the ACS.
The authors declare no competing financial interest.
Special Issue
Published as part of the ACS Medicinal Chemistry Letters virtual special issue “Medicinal Chemistry in Portugal and Spain: A Strong Iberian Alliance”.
References
- Baker R. E.; Mahmud A. S.; Miller I. F.; Rajeev M.; Rasambainarivo F.; Rice B. L.; Takahashi S.; Tatem A. J.; Wagner C. E.; Wang L.-F.; Wesolowski A.; Metcalf C. J. E. Infectious Disease in an Era of Global Change. Nat. Rev. Microbiol. 2021, 1–13. 10.1038/s41579-021-00639-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierson T. C.; Diamond M. S. The Continued Threat of Emerging Flaviviruses. Nat. Microbiol. 2020, 5 (6), 796–812. 10.1038/s41564-020-0714-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García San Miguel Rodríguez-Alarcón L.; Fernández-Martínez B.; Sierra Moros M. J.; Vázquez A.; Julián Pachés P.; García Villacieros E.; Gómez Martín M. B.; Figuerola Borras J.; Lorusso N.; Ramos Aceitero J. M.; Moro E.; de Celis A.; Oyonarte S.; Mahillo B.; Romero González L. J.; Sánchez-Seco M. P.; Suárez Rodríguez B.; Ameyugo Catalán U.; Ruiz Contreras S.; Pérez-Olmeda M.; Simón Soria F. Unprecedented Increase of West Nile Virus Neuroinvasive Disease, Spain, Summer 2020. Eurosurveillance 2021, 26 (19), 2002010. 10.2807/1560-7917.ES.2021.26.19.2002010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaffner F.; Mathis A. Dengue and Dengue Vectors in the WHO European Region: Past, Present, and Scenarios for the Future. Lancet Infect. Dis. 2014, 14 (12), 1271–1280. 10.1016/S1473-3099(14)70834-5. [DOI] [PubMed] [Google Scholar]
- Nitsche C.Strategies Towards Protease Inhibitors for Emerging Flaviviruses BT - Dengue and Zika: Control and Antiviral Treatment Strategies. In Dengue and Zika: Control and Antiviral Treatment Strategies; Springer, 2018; Vol. 1062, pp 265–276. 10.1007/978-981-10-8727-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S. P. Dengue Drug Discovery: Progress, Challenges and Outlook. Antiviral Res. 2019, 163, 156–178. 10.1016/j.antiviral.2018.12.016. [DOI] [PubMed] [Google Scholar]
- Bernatchez J. A.; Tran L. T.; Li J.; Luan Y.; Siqueira-Neto J. L.; Li R. Drugs for the Treatment of Zika Virus Infection. J. Med. Chem. 2020, 63, 470. 10.1021/acs.jmedchem.9b00775. [DOI] [PubMed] [Google Scholar]
- Sinigaglia A.; Peta E.; Riccetti S.; Barzon L. New Avenues for Therapeutic Discovery against West Nile Virus. Expert Opin. Drug Discovery 2020, 15 (3), 333–348. 10.1080/17460441.2020.1714586. [DOI] [PubMed] [Google Scholar]
- Felicetti T.; Manfroni G.; Cecchetti V.; Cannalire R. Broad-Spectrum Flavivirus Inhibitors: A Medicinal Chemistry Point of View. ChemMedChem. 2020, 15, 2391–2419. 10.1002/cmdc.202000464. [DOI] [PubMed] [Google Scholar]
- Voss S.; Nitsche C. Targeting the Protease of West Nile Virus. RSC Med. Chem. 2021, 12 (8), 1262–1272. 10.1039/D1MD00080B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao Y.; Huo T.; Lin Y. L.; Nie S.; Wu F.; Hua Y.; Wu J.; Kneubehl A. R.; Vogt M. B.; Rico-Hesse R.; Song Y. Discovery, X-Ray Crystallography and Antiviral Activity of Allosteric Inhibitors of Flavivirus NS2B-NS3 Protease. J. Am. Chem. Soc. 2019, 141 (17), 6832–6836. 10.1021/jacs.9b02505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millies B.; Von Hammerstein F.; Gellert A.; Hammerschmidt S.; Barthels F.; Göppel U.; Immerheiser M.; Elgner F.; Jung N.; Basic M.; Kersten C.; Kiefer W.; Bodem J.; Hildt E.; Windbergs M.; Hellmich U. A.; Schirmeister T. Proline-Based Allosteric Inhibitors of Zika and Dengue Virus NS2B/NS3 Proteases. J. Med. Chem. 2019, 62 (24), 11359–11382. 10.1021/acs.jmedchem.9b01697. [DOI] [PubMed] [Google Scholar]
- Brecher M.; Li Z.; Liu B.; Zhang J.; Koetzner C. A.; Alifarag A.; Jones S. A.; Lin Q.; Kramer L. D.; Li H. A Conformational Switch High-Throughput Screening Assay and Allosteric Inhibition of the Flavivirus NS2B-NS3 Protease. PLoS Pathog. 2017, 13 (5), e1006411. 10.1371/journal.ppat.1006411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrey J. D.; Taro B. S.; Siddharthan V.; Wang H.; Smee D. F.; Christensen A. J.; Furuta Y. Efficacy of Orally Administered T-705 Pyrazine Analog on Lethal West Nile Virus Infection in Rodents. Antiviral Res. 2008, 80 (3), 377–379. 10.1016/j.antiviral.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escribano-Romero E.; Jimenez de Oya N.; Domingo E.; Saiz J. C. Extinction of West Nile Virus by Favipiravir through Lethal Mutagenesis. Antimicrob. Agents Chemother. 2017, 61 (11), e01400–17. 10.1128/AAC.01400-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyer L.; Fojtíková M.; Nencka R.; Rudolf I.; Hubálek Z.; Ruzek D. Viral RNA-Dependent RNA Polymerase Inhibitor 7-Deaza-2′- C -Methyladenosine Prevents Death in a Mouse Model of West Nile Virus Infection. Antimicrob. Agents Chemother. 2019, 63 (3), e02093–18. 10.1128/AAC.02093-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim S.-Y.; Osuna C. E.; Best K.; Taylor R.; Chen E.; Yoon G.; Kublin J. L.; Schalk D.; Schultz-Darken N.; Capuano S.; Safronetz D.; Luo M.; MacLennan S.; Mathis A.; Babu Y. S.; Sheridan W. P.; Perelson A. S.; Whitney J. B. A Direct-Acting Antiviral Drug Abrogates Viremia in Zika Virus–Infected Rhesus Macaques. Sci. Transl. Med. 2020, 12 (547), eaau9135. 10.1126/scitranslmed.aau9135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaptein S. J. F.; Goethals O.; Kiemel D.; Marchand A.; Kesteleyn B.; Bonfanti J.-F.; Bardiot D.; Stoops B.; Jonckers T. H. M.; Dallmeier K.; Geluykens P.; Thys K.; Crabbe M.; Chatel-Chaix L.; Münster M.; Querat G.; Touret F.; de Lamballerie X.; Raboisson P.; Simmen K.; Chaltin P.; Bartenschlager R.; Van Loock M.; Neyts J. A Pan-Serotype Dengue Virus Inhibitor Targeting the NS3–NS4B Interaction. Nature 2021, 598 (7881), 504–509. 10.1038/s41586-021-03990-6. [DOI] [PubMed] [Google Scholar]
- Moquin S. A.; Simon O.; Karuna R.; Lakshminarayana S. B.; Yokokawa F.; Wang F.; Saravanan C.; Zhang J.; Day C. W.; Chan K.; Wang Q. Y.; Lu S.; Dong H.; Wan K. F.; Lim S. P.; Liu W.; Seh C. C.; Chen Y. L.; Xu H.; Barkan D. T.; Kounde C. S.; Sim W. L. S.; Wang G.; Yeo H. Q.; Zou B.; Chan W. L.; Ding M.; Song J. G.; Li M.; Osborne C.; Blasco F.; Sarko C.; Beer D.; Bonamy G. M. C.; Sasseville V. G.; Shi P. Y.; Diagana T. T.; Yeung B. K. S.; Gu F. NITD-688, a Pan-Serotype Inhibitor Ofthe Dengue Virus NS4B Protein, Shows Favorable Pharmacokinetics and Efficacy in Preclinical Animal Models. Sci. Transl. Med. 2021, 13 (579), 1–13. 10.1126/scitranslmed.abb2181. [DOI] [PubMed] [Google Scholar]
- Boldescu V.; Behnam M. A. M.; Vasilakis N.; Klein C. D. Broad-Spectrum Agents for Flaviviral Infections: Dengue, Zika and Beyond. Nat. Rev. Drug Discovery 2017, 16 (8), 565–586. 10.1038/nrd.2017.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty C.; Bhattacharya M.; Mallick B.; Sharma A. R.; Lee S.-S.; Agoramoorthy G. SARS-CoV-2 Protein Drug Targets Landscape: A Potential Pharmacological Insight View for the New Drug Development. Expert Rev. Clin. Pharmacol. 2021, 14 (2), 225–237. 10.1080/17512433.2021.1874348. [DOI] [PubMed] [Google Scholar]
- Martín-Acebes M. A.; Vázquez-Calvo Á.; Saiz J.-C. Lipids and Flaviviruses, Present and Future Perspectives for the Control of Dengue, Zika, and West Nile Viruses. Prog. Lipid Res. 2016, 64, 123–137. 10.1016/j.plipres.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Martinez-Gutierrez M.; Correa-Londoño L. A.; Castellanos J. E.; Gallego-Gómez J. C.; Osorio J. E. Lovastatin Delays Infection and Increases Survival Rates in AG129 Mice Infected with Dengue Virus Serotype 2. PLoS One 2014, 9 (2), e87412. 10.1371/journal.pone.0087412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitehorn J.; Nguyen C. V. V.; Khanh L. P.; Kien D. T. H.; Quyen N. T. H.; Tran N. T. T.; Hang N. T.; Truong N. T.; Hue Tai L. T.; Cam Huong N. T.; Nhon V. T.; Van Tram T.; Farrar J.; Wolbers M.; Simmons C. P.; Wills B. Lovastatin for the Treatment of Adult Patients With Dengue: A Randomized, Double-Blind, Placebo-Controlled Trial. Clin. Infect. Dis. 2015, 62 (4), civ949. 10.1093/cid/civ949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia P. Y.; Htun H. L.; Ling W. P.; Leo Y. S.; Yeo T. W.; Lye D. C. B. Hyperlipidemia, Statin Use and Dengue Severity. Sci. Rep. 2018, 8 (1), 17147. 10.1038/s41598-018-35334-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez de Oya N.; Esler W. P.; Huard K.; El-Kattan A. F.; Karamanlidis G.; Blázquez A. B.; Ramos-Ibeas P.; Escribano-Romero E.; Louloudes-Lázaro A.; Casas J.; Sobrino F.; Hoehn K.; James D. E.; Gutiérrez-Adán A.; Saiz J. C.; Martín-Acebes M. A. Targeting Host Metabolism by Inhibition of Acetyl-Coenzyme A Carboxylase Reduces Flavivirus Infection in Mouse Models. Emerging Microbes Infect. 2019, 8 (1), 624–636. 10.1080/22221751.2019.1604084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiménez de Oya N.; Blázquez A.-B.; Casas J.; Saiz J.-C.; Martín-Acebes M. A. Direct Activation of Adenosine Monophosphate-Activated Protein Kinase (AMPK) by PF-06409577 Inhibits Flavivirus Infection through Modification of Host Cell Lipid Metabolism. Antimicrob. Agents Chemother. 2018, 62 (7), e00360–18. 10.1128/AAC.00360-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Htun H. L.; Yeo T. W.; Tam C. C.; Pang J.; Leo Y. S.; Lye D. C. Metformin Use and Severe Dengue in Diabetic Adults. Sci. Rep. 2018, 8 (1), 3344. 10.1038/s41598-018-21612-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheang Y. Z. N.; Ting H. R. D.; Koh H. Q. V.; Alonso S. In Vitro and in Vivo Efficacy of Metformin against Dengue. Antiviral Res. 2021, 195, 105186. 10.1016/j.antiviral.2021.105186. [DOI] [PubMed] [Google Scholar]
- Kifle Z. D.; Woldeyohanis A. E.; Demeke C. A. A Review on Protective Roles and Potential Mechanisms of Metformin in Diabetic Patients Diagnosed with COVID-19. Metab. Open 2021, 12, 100137. 10.1016/j.metop.2021.100137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memel Z. N.; Lee J. J.; Foulkes A. S.; Chung R. T.; Thaweethai T.; Bloom P. P. Association of Statins and 28-Day Mortality in Patients Hospitalized with SARS CoV-2 Infection. J. Infect. Dis. 2021, jiab539. 10.1093/infdis/jiab539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doi Y.; Hibino M.; Hase R.; Yamamoto M.; Kasamatsu Y.; Hirose M.; Mutoh Y.; Homma Y.; Terada M.; Ogawa T.; Kashizaki F.; Yokoyama T.; Koba H.; Kasahara H.; Yokota K.; Kato H.; Yoshida J.; Kita T.; Kato Y.; Kamio T.; Kodama N.; Uchida Y.; Ikeda N.; Shinoda M.; Nakagawa A.; Nakatsumi H.; Horiguchi T.; Iwata M.; Matsuyama A.; Banno S.; Koseki T.; Teramachi M.; Miyata M.; Tajima S.; Maeki T.; Nakayama E.; Taniguchi S.; Lim C. K.; Saijo M.; Imai T.; Yoshida H.; Kabata D.; Shintani A.; Yuzawa Y.; Kondo M. A Prospective, Randomized, Open-Label Trial of Early versus Late Favipiravir Therapy in Hospitalized Patients with COVID-19. Antimicrob. Agents Chemother. 2020, 64 (12), e01897–20. 10.1128/AAC.01897-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins-Filho P. R.; Ferreira L. C.; Heimfarth L.; Araújo A. A. de S.; Quintans-Júnior L. J. Efficacy and Safety of Hydroxychloroquine as Pre-and Post-Exposure Prophylaxis and Treatment of COVID-19: A Systematic Review and Meta-Analysis of Blinded, Placebo-Controlled, Randomized Clinical Trials. Lancet Reg. Heal. - Am. 2021, 2, 100062. 10.1016/j.lana.2021.100062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar P.; Sreekanth G. P.; Murali-Krishna K.; Chandele A.; Sitaraman R. Dengue Virus Non-Structural Protein 5 as a Versatile, Multi-Functional Effector in Host–Pathogen Interactions. Front. Cell. Infect. Microbiol. 2021, 11, 1–7. 10.3389/fcimb.2021.574067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan H. A.; Kumar M. Role of Endoplasmic Reticulum-Associated Proteins in Flavivirus Replication and Assembly Complexes. Pathogens 2019, 8 (3), 148. 10.3390/pathogens8030148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards A.; Hartung I. V. No Shortcuts to SARS-CoV-2 Antivirals. Science (Washington, DC, U. S.) 2021, 373 (6554), 488–489. 10.1126/science.abj9488. [DOI] [PubMed] [Google Scholar]
- Tummino T. A.; Rezelj V. V.; Fischer B.; Fischer A.; O’Meara M. J.; Monel B.; Vallet T.; White K. M.; Zhang Z.; Alon A.; Schadt H.; O’Donnell H. R.; Lyu J.; Rosales R.; McGovern B. L.; Rathnasinghe R.; Jangra S.; Schotsaert M.; Galarneau J.-R.; Krogan N. J.; Urban L.; Shokat K. M.; Kruse A. C.; García-Sastre A.; Schwartz O.; Moretti F.; Vignuzzi M.; Pognan F.; Shoichet B. K. Drug-Induced Phospholipidosis Confounds Drug Repurposing for SARS-CoV-2. Science (Washington, DC, U. S.) 2021, 373 (6554), 541–547. 10.1126/science.abi4708. [DOI] [PMC free article] [PubMed] [Google Scholar]




