Abstract
Background and objectives:
Studies have shown that COVID-19 school closures negatively impacted children’s well-being. We assessed the impact of school closures on children in Japan. We postulated that screen time and sleep habits during school closure would be associated with children’s mental health status.
Methods:
A cross-sectional study was conducted with 959 children in four public elementary schools. Parents completed an original questionnaire in which we enquired about children’s behavioral problems, screen time (duration of watching TV/videos and duration of playing video games), sleep habits, and bodyweight change during school closure. Logistic regression analyses were performed to investigate the relationships between behavioral problems, bodyweight gain, and screen time.
Results:
It was found that 50.3% of children exhibited some behavioral problems during school closure; fewer children exhibited such problems after schools reopened. Moreover, children’s behavioral problems during school closure were associated with longer total screen time (odds ratio [OR]: 1.2, 95% confidence interval [CI]: 1.14–1.28, p < .001). Sleep habits were not different between children with behavioral problems and those without. Of the children, 16.7% experienced bodyweight gain during school closure, which was associated with behavioral problems (OR: 2.0, 95% CI: 1.43–2.92, p < .001) and time spent watching TV/videos (OR: 1.2, 95% CI: 1.08–1.28, p < .001) during closure.
Conclusions:
COVID-19 school closure negatively impacted school children physically and psychologically. Screen time was associated with both physical and mental health status. Therefore, children should not engage in arbitrary screen time during school closures and should be supported in their daily routines.
Keywords: COVID-19, school closure, psychological impact, children, screen time, sleep habits
Introduction
Pediatricians report that patients’ physical and psychological complaints increase after long periods of school closures in Japan, such as summer vacations. It has been reported that the number of children who commit suicide is greatest in September in Japan (1); therefore, the Japanese government has alerted pediatricians and parents to pay attention to subtle changes in children when they are due to return to school. Hence, long school closures seem to affect children’s physical and psychological status.
Owing to the coronavirus disease 2019 (COVID-19), schools were unexpectedly and abruptly closed in many countries as part of physical distancing policy. The Japanese government ordered the closure of all schools on February 27, 2020, and a state of emergency was declared nationwide on April 16. The period of the school closure varied by region; however, people were requested to remain at home and have restricted contact with non-family members. Given this unusual school closure with these severe restrictions, children’s lives were more severely affected than by conventional annual closures (2). In Saga, Japan, the state of emergency was lifted on May 14, 2020; subsequently, schools gradually reopened, and all schools in this area were open as usual by June 1, 2020.
These unusual conditions prompted us to investigate how this school closure affected schoolchildren. Studies have revealed that COVID-19 school closures exerted profound negative impacts on schoolchildren physically (3) and psychologically (4-7); however, thus far, no extensive study has been conducted of the precise mechanisms affecting children’s mental health. Therefore, this work was driven by the following research questions:
1) How did the incidence of physical and mental problems change during and after the COVID-19 school closure in Japan? 2) What factors were associated with children experiencing these problems? We hypothesized that there would be a relationship between increased screen time and the incidence of such problems. We also assessed the connection between sleep habits and children’s problems.
Methods
Participants
This was a cross-sectional study conducted in July 2020, which enrolled students from all four public elementary schools in Miyaki-Machi, a suburban town in Saga prefecture, Japan. Parents received a letter describing the study and a questionnaire to be returned to the school by July 30 after completion. Participants were offered no financial incentive. The Regional Research Ethics Committee approved the study (approval number: 02-19) before its commencement.
Measures
All data were anonymously reported by parents or guardians. Five main types of questions were created for this study. Specifically, parents and guardians were asked to identify the characteristics of the participants such as gender and grades, time spent watching TV and/or videos and playing video games, sleep habits (wakeup time and bedtime) during school closure and after school reopened, and behavior related questions, which addressed behavioral problems (irritability, inability to stop playing video games, frequent fights with siblings, excessive dependence on parents, and refusal to sleep independently) during school closure and after school reopened (using binary responses). Total screen time was defined as the sum of the time spent watching TV and/or videos and playing video games. Data on bodyweight change before and after school reopened were also collected (by binary response).
Statistical analyses
All statistical analyses were performed using JMP® Pro version 14 (SAS Institute Inc., Cary, NC, USA). Demographic characteristics were expressed as means and standard deviations for continuous variables and as frequencies and percentages for categorical variables. Chi-squared and Wilcoxon rank sum tests were used to compare differences between groups. Logistic regression analyses were performed to calculate the adjusted odds ratio (OR) with 95% confidence interval (CI) for evaluating the relationships between exhibiting behavioral problems or experiencing bodyweight gain and screen time (total screen time, time spent watching TV and/or videos and playing video games during school closure), respectively. Furthermore, we also analyzed the relationship between exhibiting behavioral problems and experiencing bodyweight gain during school closure. Confounding variables of gender and grades were adjusted for logistic regression analyses. Statistical significance was defined at the .05 level.
Results
Sample characteristics
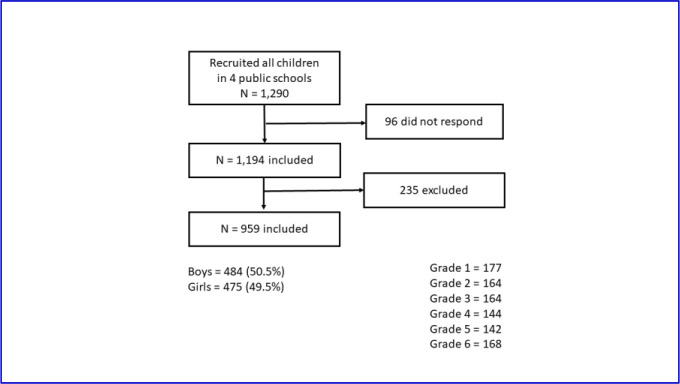
Figure 1 shows the sample characteristics. A total of 1,290 schoolchildren were enrolled in this study. The response rate was 92.6%. Of the students enrolled, 235 were excluded because of incomplete responses. Overall, 959 children were assessed in this study. In Japan, students in Grade 1 are typically 6 to 7 years old.
FIGURE 1.
Sample Characteristics
Changes in children with behavioral problems
During school closure, 50.3% of children exhibited some problematic behaviors; percentage decreased to 38.0% after schools reopened (-12.3%, p < .001; Table 1). Neither gender nor grades were significantly associated with exhibiting behavioral problems during school closure (Table 2).
TABLE 1.
Frequency of children with behavioral problems during school closures and after schools reopened
| During school closures n (%) |
After schools reopened n (%) |
During vs. after p |
|
|---|---|---|---|
| Children with at least one of the following problems: | 482 (50.3) | 364 (38.0) | < .001 |
| Irritability | 186 (19.3) | 152 (15.8) | < .001 |
| Inability to stop playing video games | 260 (27.1) | 158 (16.5) | < .001 |
| Frequent fights with siblings | 265 (27.6) | 189 (19.7) | < .001 |
| Excessive dependence on parents | 73 (7.6) | 72 (7.5) | .93 |
| Refusal to sleep independently | 14 (1.5) | 18 (2.5) | < .001 |
Note. Chi-squared tests were used to compare groups
TABLE 2.
Characteristics of children with behavioral problems during school closure
| Children with behavioral problems during school closure (n = 482) | Children without behavioral problems during school closure (n = 477) | With problems vs. Without problems p | ||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | |||||
| Gender | 253/482 | 229/482 | 231/477 | 246/477 | 0.220 † | |||
| p = 1.00 *† | p = 1.00 *† | |||||||
| 1 | 83 | 94 | ||||||
| 2 | 85 | 79 | ||||||
| Grade | 3 | 85 | 79 | 0.675 † | ||||
| 4 | 79 | 65 | ||||||
| 5 | 66 | 76 | ||||||
| 6 | 84 | 84 | ||||||
| Mean duration of watching TV/video (SD) | 3.3 h (1.9) | 2.8 h (1.8) | < .001 ‡ | |||||
| Mean duration of playing video games (SD) | 2.1 h (1.9) | 1.4 h (1.6) | < .001 ‡ | |||||
| Total screen time (SD) | 5.4 h (2.7) | 4.2 h (2.5) | < .001 ‡ | |||||
| Mean sleep duration (SD) | 9.4 h (0.9) | 9.4 h (0.8) | 0.653 ‡ | |||||
| Mean wakeup time (SD) | 7:28 (1.0 h) | 7:21 (1.0 h) | 0.109 ‡ | |||||
| Mean bedtime (SD) | 21:54 (1.2 h) | 21:54 (0.9 h) | 0.357 ‡ | |||||
| Bodyweight gain during school closure | 105/482 | 56/477 | < .001 † | |||||
Note. SD = standard deviation; h = hours;
*: p compares proportion of boys and that of girls;
†: Chi-squared tests were used to compare groups;
‡: Wilcoxon rank sum tests were used to compare groups
Relationship between screen time and behavioral problems
In general, schoolchildren watched TV and/or video and played video games significantly longer during school closure than after school reopened (TV/video: Mean [M] = 3.0 h, Standard Deviation [SD] =1.9 h versus M = 1.5 h, SD = 1.0 h; video games: M = 1.8 h, SD =1.8 h versus M = 0.8 h, SD = 0.8 h, respectively; p < .001). Total screen time during school closure was significantly higher in children with behavioral problems (+1.2 h; p < .001; Table 2) than in those without. During school closure, children with behavioral problems watched TV and/or videos, and played video games significantly longer than children without such problems (+0.5 h, +0.7 h, respectively; p < .001; Table 2). The logistic regression analysis revealed that both the time spent watching TV/video and playing video games were risk factors for behavioral problems during school closure (Table 3).
TABLE 3.
Odds ratios and 95% confidence intervals of exhibiting behavioral problems during school closure
| Crude | Adjusted | |||||
|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | P value | OR | 95% CI | P value |
| Time spent watching TV/video | 1.1 | 1.07 – 1.22 | < .001 | 1.2 | 1.07 – 1.24 | < .001 |
| Time spent playing video games | 1.3 | 1.2 – 1.4 | < .001 | 1.3 | 1.18 – 1.41 | < .001 |
| Total screen time | 1.2 | 1.14 – 1.28 | < .001 | 1.2 | 1.14 – 1.28 | < .001 |
| Bodyweight gain | 2.1 | 1.47 – 2.98 | < .001 | 2.0 | 1.43 – 2.92 | < .001 |
Note. Logistic regression analyses were performed to calculate the adjusted odds ratio (OR) with 95% confidence interval (CI) for the relationship between exhibiting behavioral problems and screen time (time spent watching TV and/or videos, time spent playing video games and total screen time during school closure) and experiencing bodyweight gain during school closure, respectively. Controls are gender and grades
Association between sleep habits and behavioral problems
We examined children’s sleep habits during school closure and after schools reopened. In general, children slept longer during school closure than after schools reopened (M = 9.4 h, SD = 0.8 h versus M = 8.8 h, SD = 0.7 h; p < .001). Mean sleep duration during school closure did not differ between children with and without behavioral problems (Table 2). Moreover, bedtime and wakeup time during school closure were almost identical between these children (Table 2).
Bodyweight change
Overall, 16.7% of the children reported bodyweight gain (n = 161; 79 boys, 82 girls), and 0.3% reported bodyweight loss (n = 3, all boys) during school closure (Table 4). We assessed the relationship between bodyweight gain and screen time during school closure. Children with bodyweight gain reported higher total screen time, which was attributed to longer duration of watching TV/video, but not that of playing video games (Table 4). Thus, time spent watching TV/video was a risk factor for bodyweight gain and not time spent playing video games (Table 5). Sleep habits did not differ between these children (Table 4).
TABLE 4.
Characteristics of children with experiencing bodyweight gain
| Children with bodyweight gain (n = 161) | Children no bodyweight gain (n = 798) | With bodyweight gain vs. no bodyweight gain p | ||||||
|---|---|---|---|---|---|---|---|---|
| Boys | Girls | Boys | Girls | |||||
| Gender | 79/161 | 82/161 | 405/798 | 393/798 | 0.730 † | |||
| p = 1.00 *† | p = 1.00 *† | |||||||
| 1 | 83 | 94 | ||||||
| 2 | 85 | 79 | ||||||
| Grade | 3 | 85 | 79 | 0.675 † | ||||
| 4 | 79 | 65 | ||||||
| 5 | 66 | 76 | ||||||
| 6 | 84 | 84 | ||||||
| Mean duration of watching TV/video (SD) | 3.6 h (2.3) | 2.9 h (1.8) | < .001 ‡ | |||||
| Mean duration of playing video games (SD) | 1.9 h (2.0) | 1.7 h (1.7) | < .674 ‡ | |||||
| Total screen time (SD) | 5.2 h (3.0) | 4.7 h (2.5) | < .001 ‡ | |||||
| Mean sleep duration (SD) | 9.5 h (0.8) | 9.4 h (0.8) | 0.234 ‡ | |||||
| Mean wakeup time (SD) | 7:28 (1.0 h) | 7:21 (1.0 h) | 0.402 ‡ | |||||
| Mean bedtime (SD) | 21:54 (0.9 h) | 21:54 (0.9 h) | 0.490 ‡ | |||||
| Bodyweight gain during school closure | 105/161 | 377/798 | < .001 † | |||||
Note. SD = standard deviation; h = hours;
*: p compares proportion of boys and that of girls;
†: Chi-squared tests were used to compare groups;
‡: Wilcoxon rank sum tests were used to compare groups
TABLE 5.
Odds ratio and 95% confidence intervals of children experiencing body weight gain during school closure
| Crude | Adjusted | |||||
|---|---|---|---|---|---|---|
| Variable | OR | 95% CI | P value | OR | 95% CI | P value |
| Time spent watching TV/video | 1.2 | 1.10 – 1.30 | < .001 | 1.2 | 1.08 – 1.28 | < .001 |
| Time spent playing video games | 1.1 | 0.96 – 1.15 | 0.317 | 1.0 | 0.91 – 1.12 | 0.845 |
| Total screen time | 1.1 | 1.05 – 1.19 | < .001 | 1.1 | 1.02 – 1.16 | < .001 |
| Behavioral problems | 2.1 | 1.47 – 2.98 | < .001 | 2.0 | 1.43 – 2.92 | < .001 |
Note. Logistic regression analyses were performed to calculate the adjusted odds ratio (OR) with 95% confidence interval (CI) for the relationship between experiencing body weight gain during school closure and screen time (time spent watching TV and/or videos, time spent playing video games and total screen time during school closure) and exhibiting behavioral problems during school closure, respectively. Controls are gender and grades
The interrelationship between behavioral problems and bodyweight gain
Lastly, we assessed the relationship between bodyweight gain and behavioral problems during school closure. The proportion of children experiencing bodyweight gain during school closure was significantly higher among those with behavioral problems than those without (Table 2). Similarly, children with bodyweight gain reported a significantly higher proportion of behavioral problems than those with no bodyweight gain (Table 4). Logistic regression analyses revealed that exhibiting behavioral problems during school closure and experiencing bodyweight gain were mutual risk factors (Tables 3 and 5).
Discussion
In the current study, we revealed that more than half of schoolchildren in Miyaki-Machi, Japan, exhibited some behavioral problems during COVID-19 school closure, which decreased after schools reopened. School closure due to COVID-19 poses an imminent threat to children’s health and wellbeing worldwide, in educational (8), nutritional (9), and economic terms (9). This study also reinforces the results of prior reports (2-9) demonstrating negative impacts of school closure on children, especially children’s mental health.
School closure due to COVID-19 were unique in some respects. In Japan, only 5% of all public elementary schools provided interactive online classes in April, 2020 (10). The remaining schoolchildren were given paper-based homework (10) without time constraints. These children might have lacked direct connections with teachers and schools for approximately three months, which was longer than usual annual school closures. The four elementary schools examined in this study had no remote learning systems. Additionally, it was reported that only 20.8% of elementary schoolchildren in Japan used daycare in 2020 (11). The remaining children were ordered to stay at home and were prohibited to contact their friends, indicating that they could not engage in enjoyable activities with their friends. Although teachers in these elementary schools sometimes visited their students, compared with the usual annual closures, most children were likely placed in an environment in which they could spend time on their own terms, without an appropriate educational connection to school. Thus, children likely both feared infection and experienced distress due to experiencing unstructured days, frustration, boredom (12-15), and isolation (15) for longer periods than during regular annual school closures. This was one of the possible factors causing schoolchildren in this area to experience negative impacts due to school closure.
A national survey in the US revealed that 14% parents reported worsening behavior in their children (4) and increases in their children’s irritability, inattention, and clinging since the pandemic began (7), regardless of age (16). A survey in China showed that 22.6% of students (from Grade 2 to Grade 6) reported depressive symptoms, and 18.9% reported anxiety during in-home confinement (17). Our study showed that more than 50% of schoolchildren, regardless of their gender and grades, exhibited behavioral problems during school closure, and the percentage decreased significantly after schools reopened. This indicates that these children exhibited behavioral problems in response to the stress experienced during school closure. Reopening schools might have relieved children of these stressors through school-based peer interactions and reestablishment of their daily routines (18). A significant increase in the body mass index of youths during COVID-19 lockdown has been reported (3). Notably, 16.7% of children experienced bodyweight gain during school closure in this study. Delayed access to healthcare (19), delayed illness presentation (19, 20), and dropping vaccination rates (21) have been reported as the indirect physical effects of the COVID-19 pandemic in children. In this study, we demonstrated that children exhibiting behavioral problems during school closure had a high risk of bodyweight gain. Mental burden originating from this COVID-19 school closure might have affected children’s physical status. Thus, school closure exerted profound negative impacts on children, both psychologically and physically.
Although media entertainment has become a tool for coping with distress, boredom, and lack of social interaction caused by the pandemic (16, 22), digital technology has demonstrated potentially harmful effects on the developing brain (23). Moreover, total screen time is associated with unfavorable temperament (24), such as irritability, anxiety, clinginess, and inattention (23, 25). Therefore, we examined screen time during this COVID-19 school closure. Children’s screen time in this study was longer than that reported in previous studies (3). In addition, children with behavioral problems during school closure had a longer total screen time than those without such problems. This suggests that children with behavioral problems experienced the additional distress of excessive usage of screen media in addition to the distress of the quarantine.
Media use, especially TV viewing (26), is associated with the risk of becoming overweight (27). The current study results are consistent with those of previous studies (26, 27). The bodyweight gain during school closure reported in this study may have resulted from longer screen time and less physical activity due to the quarantine (27, 28). The type of screen time has been shown to affect physical and psychological health; moreover, the magnitude of the effect depends on how children use screens—passively (e.g., watching TV) or interactively (e.g., playing video games) (24). The former exerts negative impacts on schoolchildren (24). Consistent with these findings, the current study demonstrated that passive use, and not interactive use, of screen media affected schoolchildren physically. However, both the passive and interactive use of screen media were significantly associated with children exhibiting behavioral problems during school closure. Despite the lack of investigation of the video game genre played by children during school closure in the current study, some violent games profoundly affected children’s psychological status (29, 30). Although gaming alone and gaming in groups were not associated with depressive symptoms in adolescents (31), it might be better for children to watch TV with other people rather than watch it alone (32). As children were prohibited from contacting non-family members amidst the COVID-19 school closure, it might be possible that screen time exerted more profound effects then in comparison to during the annual school closure (33). Research suggests that educational efficacy in remote learning systems is higher with interactive communication than one way communication (34). This may indicate the need to nurture human connection—families and friends—even in screen media usage for mental health (35), especially among children. Therefore, our study highlights the importance of precisely how children interact with screen media during long school closures, such as summer vacations and COVID-19 quarantine.
We further investigated other physical and psychological factors affecting children’s sleep habits. Sleep plays a critical role in children’s physical and mental development; shorter sleep duration is a risk factor for behavioral issues (36). The American Academy of Sleep Medicine recommends that children between 6 and 12 years of age should sleep for more than 9 hours per night (37). Japan has been reported to be the most sleepless country in the world (38); sleep duration among most schoolchildren in Japan is less than 9 hours per night (36). Children in our study appeared to sleep sufficiently to satisfy their physiological needs during school closure. Before implementing this study, we speculated that children with behavioral problems would stay up late at night and engage in longer screen time than those without such problems. However, sleep duration in children with behavioral problems did not differ from that in those without behavioral problems. Bedtime and wakeup time were almost identical in both types of children. Furthermore, sleep habits were not associated with bodyweight gain during school closure. These observations indicate that shorter sleep duration was not the only factor associated with the physical and mental health of children in this study. Although this study did not examine to what degree parents could supervise their children’s screen time and sleep habits during school closure, it may be necessary for children to be assigned a daily routine by their parents or guardians (26, 27, 39, 40).
The strength of our study is that it was conducted with participants from public elementary schools. Compared to online surveys, our study was not affected by Internet access or access to devices. In contrast, the primary limitation of this study was that the questionnaire was originally developed by the authors; thus, the study lacked standardized and validated instruments. This caused potential differences in interpretation of variable meaning across respondents and made it difficult to generalize our findings globally. The second limitation was a lack of information about each child’s environment, such as family member or parents’ job, which may influence the results (5). The third limitation was the potential inadequacy of the methods and items used to assess children exhibiting behavioral problems. Moreover, the questionnaires did not include items on psychosomatic symptoms or psychological symptoms such as depression and inattention. Lastly, to investigate and compare the long-term mental impact of school closures on children due to this global pandemic, especially as it relates to screen usage, we must use well-generalized instruments designed to investigate the mental health status of children and evaluate regional differences in quarantine-sternness while considering the influences of gender and grades.
Clinical significance
The school closure due to COVID-19 had negative physical and psychological impacts on schoolchildren in Japan, which were closely associated with each other and with children’s screen media usage. Accordingly, parents should restrict children’s arbitrary use of screen media; in addition, they should provide children with the opportunity to use screen media interactively and spend enjoyable screen time together with their children to establish human connection. For future school closures, we suggest that parents and caregivers cooperate with teachers to generate daily routines for children, which enable the latter to feel connected to friends and schools, rather than allow children to engage in arbitrary screen time.
Acknowledgements
We would like to thank all of the parents and guardians who took part in our study, the Board of Education in Miyaki-Machi and all of the public elementary schools that cooperated with us. We also thank Ms. Ayako Takamori, Ph.D. and M.M.Sc for her advice on the statistical technique.
Footnotes
Conflict of interest disclosures:
The authors have no conflict of interest relevant to this article to disclose.
References
- 1.The analysis of suicides among school children [Internet]. Japan Support Center for Suicide Countermeasures. 2018. [cited 2020, Dec. 1]. Available from: https://jssc.ncnp.go.jp/file/pdf/2018-0807-report. [Google Scholar]
- 2.Masonbrink AR, Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics 2020;146(3):e20201440. [DOI] [PubMed] [Google Scholar]
- 3.Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes 2020c;10(6):e12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, et al. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics 2020;146(4):e2020016824. [DOI] [PubMed] [Google Scholar]
- 5.Gassman-Pines A, Ananat EO, Fitz-Henley J 2nd. COVID-19 and parent-child psychological well-being. Pediatrics 2020;146(4):e2020007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coller RJ, Webber S. COVID-19 and the well-being of children and families. Pediatrics 2020;146(4):e2020022079. [DOI] [PubMed] [Google Scholar]
- 7.Orgilés M, Morales A, Delvecchio E, Mazzeschi C, Espada JP. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front Psychol 2020;11:579038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hefferon C, Taylor C, Bennett D, Falconer C, Campbell M, Williams JG, et al. Priorities for the child public health response to the COVID-19 pandemic recovery in England. Arch Dis Child 2021;106(6):533-8. [DOI] [PubMed] [Google Scholar]
- 9.Carroll N, Sadowski A, Laila A, Hruska V, Nixon M, Ma DWL, et al. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income canadian families with young children. Nutrients 2020;12(8):2352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fumiko T. Survey on how students spent time off school during the COVID-19 pandemic school closure. Center for Educational Research and Training, Faculty of Education Kumamoto University. 2021;38:27-35. [Google Scholar]
- 11.The report of after-school child activities [Internet]. Ministry of Health, Labour and Welfare, Japan. 2020. [cited 2020, Dec. 1]. Available from: https://www.mhlw.go.jp/content/11921000/000708397.pdf. [Google Scholar]
- 12.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395(10227):912-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Giorgio E, Di Riso D, Mioni G, Cellini N. The interplay between mothers’ and children behavioral and psychological factors during COVID-19: an Italian study. Eur Child Adolesc Psychiatry 2021;30(9):1401-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh S, Roy D, Sinha K, Parveen S, Sharma G, Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res 2020;293:113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry 2020;59(11):1218-39.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr 2020;221:264-6.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr 2020;174(9):898-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bahn GH. Coronavirus disease 2019, school closures, and children’s mental health. Soa Chongsonyon Chongsin Uihak 2020;31(2):74-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chanchlani N, Buchanan F, Gill PJ. Addressing the indirect effects of COVID-19 on the health of children and young people. CMAJ 2020;192(32):E921-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lynn RM, Avis JL, Lenton S, Amin-Chowdhury Z, Ladhani SN. Delayed access to care and late presentations in children during the COVID-19 pandemic: a snapshot survey of 4075 paediatricians in the UK and Ireland. Arch Dis Child 2021;106(2):e8. [DOI] [PubMed] [Google Scholar]
- 21.Crawley E, Loades M, Feder G, Logan S, Redwood S, Macleod J. Wider collateral damage to children in the UK because of the social distancing measures designed to reduce the impact of COVID-19 in adults. BMJ Paediatr Open 2020;4(1):e000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marques de Miranda D, da Silva Athanasio B, Sena Oliveira AC, Simoes-E-Silva AC. How is COVID-19 pandemic impacting mental health of children and adolescents? Int J Disaster Risk Reduct 2020;51:101845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoehe MR, Thibaut F. Going digital: how technology use may influence human brains and behavior. Dialogues Clin Neurosci 2020;22(2):93-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sanders T, Parker PD, Del Pozo-Cruz B, Noetel M, Lonsdale C. Type of screen time moderates effects on outcomes in 4013 children: evidence from the Longitudinal Study of Australian Children. Int J Behav Nutr Phys Act 2019;16(1):117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imran N, Aamer I, Sharif MI, Bodla ZH, Naveed S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci 2020;36(5):1106-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Jong E, Visscher TL, HiraSing RA, Heymans MW, Seidell JC, Renders CM. Association between TV viewing, computer use and overweight, determinants and competing activities of screen time in 4- to 13-year-old children. Int J Obes (Lond) 2013;37(1):47-53. [DOI] [PubMed] [Google Scholar]
- 27.Council on Communications and Media . Media use in school-aged children and adolescents. Pediatrics 2016;138(5):e20162592. [DOI] [PubMed] [Google Scholar]
- 28.López-Bueno R, López-Sánchez GF, Casajús JA, Calatayud J, Gil-Salmerón A, Grabovac I, et al. Health-related behaviors mong school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr 2020;8:573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Anderson CA, Sakamoto A, Gentile DA, Ihori N, Shibuya A, Yukawa S, et al. Longitudinal effects of violent video games on aggression in Japan and the United States. Pediatrics 2008;122(5):e1067-72. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Q, Cao Y, Tian J. Effects of violent video games on aggressive cognition and aggressive behavior. Cyberpsychol Behav Soc Netw 2021;24(1):5-10. [DOI] [PubMed] [Google Scholar]
- 31.Ma L, Evans B, Kleppang AL, Hagquist C. The association between screen time and reported depressive symptoms among adolescents in Sweden. Fam Pract 2021;38(6):773-9. [DOI] [PubMed] [Google Scholar]
- 32.Vokacova J, Badura P, Pavelka J, Kalman M, Hanus R. Brief report: Changes in parent-adolescent joint activities between 2002 and 2014 in the Czech Republic, Health Behaviour in School-aged Children (HBSC) study. J Adolesc 2016;51:1-5. [DOI] [PubMed] [Google Scholar]
- 33.Marchi J, Johansson N, Sarkadi A, Warner G. The impact of the COVID-19 pandemic and societal infection control measures on children and adolescents’ mental health: A scoping review. Front Psychiatry 2021;12:711791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sinclair P, Kable A, Levett-Jones T. The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: a systematic review protocol. JBI Database System Rev Implement Rep 2015;13(1):52-64. [DOI] [PubMed] [Google Scholar]
- 35.Bhaskara NV, Nandanur BS, Chakraborty A, Ghosh S. The effect of social media usage on the mental well-being of medical college students in Bangalore, Karnataka. J Family Med Prim Care 2020;9(11):5731-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sakamoto N, Gozal D, Smith DL, Yang L, Morimoto N, Wada H, et al. Sleep duration, snoring prevalence, obesity, and behavioral problems in a large cohort of primary school students in Japan. Sleep 2017;40(3). [DOI] [PubMed] [Google Scholar]
- 37.Paruthi S, Brooks LJ, D’Ambrosio C, Hall WA, Kotagal S, Lloyd RM, et al. Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: methodology and discussion. J Clin Sleep Med 2016;12(11):1549-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Special focus: Measuring leisure in OECD countries [Internet]. Organisation for Economic Co-operation and Development. 2020. [cited 2020, Dec. 1]. Available from: https://www.oecd.org/berlin/42675407.pdf. [Google Scholar]
- 39.Jago R, Sebire SJ, Edwards MJ, Thompson JL. Parental TV viewing, parental self-efficacy, media equipment and TV viewing among preschool children. Eur J Pediatr 2013;172(11):1543-5. [DOI] [PubMed] [Google Scholar]
- 40.Brindova D, Pavelka J, Ševčikova A, Žežula I, van Dijk JP, Reijneveld SA, et al. How parents can affect excessive spending of time on screen-based activities. BMC Public Health 2014;14:1261. [DOI] [PMC free article] [PubMed] [Google Scholar]