Highlights
-
•
We can empower practitioners to lead quality improvement projects in LMICs.
-
•
Nurses can play a significant role in the improvement of burns services.
-
•
Interactive blended-learning courses can support nurses to lead on quality improvement.
-
•
The training and development must be designed to be context specific.
Keywords: Quality improvement, Service improvement, Nursing development, Low-middle income countries, Malawi, Ethiopia
Abstract
Background
There is an urgent need to empower practitioners to undertake quality improvement (QI) projects in burn services in low-middle income countries (LMICs). We piloted a course aimed to equip nurses working in these environments with the knowledge and skills to undertake such projects.
Methods
Eight nurses from five burns services across Malawi and Ethiopia took part in this pilot course, which was evaluated using a range of methods, including interviews and focus group discussions.
Results
Course evaluations reported that interactive activities were successful in supporting participants to devise QI projects. Appropriate online platforms were integral to creating a community of practice and maintaining engagement. Facilitators to a successful QI project were active individuals, supportive leadership, collaboration, effective knowledge sharing and demonstrable advantages of any proposed change. Barriers included: staff attitudes, poor leadership, negative culture towards training, resource limitations, staff rotation and poor access to information to guide practice.
Conclusions
The course demonstrated that by bringing nurses together, through interactive teaching and online forums, a supportive community of practice can be created. Future work will include investigating ways to scale up access to the course so staff can be supported to initiate and lead quality improvement in LMIC burn services.
1. Introduction
According to the World Health Organisation (WHO) the global health community faces challenges implementing proven health interventions into practice [1]. These issues are often associated with a lack of understanding or communication between those who are doing the research and those who are working in frontline healthcare. This lack of unity not only restricts progress but comes at a significant cost to both patients and health services. Consequently, there is an urgent need to ensure that frontline practitioners are consulted, supported and involved in research and quality improvement (QI) studies in order to identify and address potential issues which may affect the implementation of evidenced-based practice at the earliest opportunity [1]. This need is particularly evident in burns care in low-resourced countries where evidence has consistently demonstrated a significant difference in the outcomes for burns patients in comparison to resource rich countries [2]. Two -thirds of the estimated 180,000 annual deaths from burn injuries occur in African and South-East Asian region [3]. The tertiary care centre in Lilongwe, Malawi reported that the mortality from burns was 16% for children aged 0–18 years between June 2011 and December 2012 [4], while burns account for the second most common cause of paediatric injury in the country [5]. In Ethiopia data are particularly difficult to access, but a recent review indicated that burns account for about 1.5% to 9% of injuries over all age groups and between 4% and 15% of injuries in the paediatric population [6].
Nurses, particularly those working in low-middle income countries (LMICs), have often lacked the support to develop, undertake and lead their own research due to a lack of resources, insufficient education and training at an advanced level, poor leadership and an undervaluing of nursing’s contribution to research [7]. In a collaboration between the International Council of Nurses (ICN) and the World Health Organisation (WHO), the ‘Nursing Now’ global campaign was launched in 2018, to re-emphasise the importance of raising the profile and status of nurses worldwide [8]. The WHO named 2020 as the year of the Nurse and Midwife in recognition of the fact that nurses make up the largest occupation group in the health sector and, therefore, play a central role in achieving universal health coverage, sustainable development goals, economic growth and gender equality [7,9]. The WHO report calls for an acceleration in the provision of nurse education in low- and middle-income countries, where global skills partnerships can support skill development in health system strengthening activities, including service delivery and quality improvement.
In response to this need, the Centre for Global burn Injury Policy and Research (CGBIPR) and the NGO Interburns (International Network for Training, Education and Research in Burns) have been working together to build capacity in a range of skills related to burn prevention and treatment in LMICs [2]. A 5-day course on Implementation and Improvement science for healthcare professionals working in burn care and prevention in low resource environments, had already been delivered to senior staff. The idea of developing a similar programme specifically for nurses, based on problem solving in the ‘real’ world [10,11], grew from the desire to encourage leadership and skills development in this vital group of health professionals who are working on the front line of health service delivery. The pilot program outlined in this paper was designed to support nurses working in burn services in Malawi and Ethiopia and provide them with the skills to undertake useful quality improvement projects relevant to their clinical areas. These countries were selected as they were already part of a larger research programme undertaken by the CGBIPR and Interburns; our previous experience of working in these countries included undertaking a community survey of burn injuries and associated knowledge, attitudes and practices (papers submitted for publication) and delivery of Advanced Burn Care (Surgery) and Advanced Burn Care (Nursing) courses. These previous experiences ensured that we were fully conversant with the burn service provision in these countries and allowed us to build on relationships which helped with the logistics and planning aspects of the course.
More specifically this program aimed to investigate the following questions:
-
1)
Is it possible to provide effective training on improvement and implementation science, to nurses working in burns units, in Malawi and Ethiopia through a combination of face-to-face and online learning?
-
2)
What barriers and/or facilitators do nurses in Malawi and Ethiopia encounter in finding, reviewing, applying and changing practice in relation to current evidence?
Whilst this study was not a traditional scientific research project, the paper outlines the development of the course and the experiences of the participants while undertaking quality improvement projects within their clinical contexts to help us more fully understand the feasibility of this approach and allow others to build on these experiences.
2. Methods and materials
2.1. Developing the implementation and improvement science course for nurses
The content of the original 5-day course was further developed and refined in consultation with health professionals and academics from Malawi, Ethiopia, the UK, Tanzania, Palestine and South Africa to ensure that the content was both appropriate and contextually relevant [12,13]; these external experts contributed to the final version of the learning objectives for the course. In particular, the Malawian and Ethiopian perspective on expectations of teaching and adult learning were sought during the development and delivery of the course, with the aim of producing an effective teaching environment which was responsive to participants needs and expectations [8]. Nurses from these countries are most familiar with a didactic teaching method, but the context is now changing, and we wished to introduce a more experiential approach to learning [14] including a focus on problem solving [15], in line with the general principles of adult learning (developed from the work of Knowles 1968 [16]). A similar framework was used for the Advanced Burn Care course that all participants had already attended. There was a strong emphasis throughout the course on the importance of using evidence to inform clinical practice and the ways in which small scale, low-cost QI projects can make a big difference to patient outcomes.
The learning outcomes were developed and refined using Bloom’s (1956) taxonomy as an initial framework [17], ensuring that the outcomes would consider the application of cognitive, psychomotor and affective domains [18]. Using an iterative process with experts from LMICs, the final set of learning outcomes were agreed (see Table 1) and covered the following areas, all of which were applied to burn care:
-
●
Approaches to implementing quality and service improvements in practice
-
●
The principles related to undertaking implementation and quality improvement in practice
-
●
The logistical factors associated with planning and preparing an implementation and improvement science project
-
●
The methods used to measure quality improvement (QI) in practice
-
●
Approaches to monitoring, evaluating and disseminating quality improvement outcomes
-
●
Leadership, management and team working for quality improvement
Table 1.
Course aim and learning outcomes.
| Course aim |
| This course aims to prepare and equip nurses working within burns units with the theoretical and practical skills to plan, implement, monitor and communicate small scale quality and service improvement projects in their clinical area. |
| Approaches to improving quality and patient safety: |
| By the end of this course the participant should be able to: |
| Describe what implementation science is and how it can be applied to burn care |
| 1.1 Discuss key issues that affect the translation of evidence into practice within the context of burns care and treatment |
| 1.2 Identify the role of a nurse in implementation science research |
| 1.3 Explain the importance of implementation science for the development of quality burns services |
| 1.4 Systematically describe the steps required in an implementation science project, including models of change |
| 1.5 Identify strategies to analyse current processes and identify problems such as process mapping and root cause analysis |
| 1.6 To contextualise the physical, socio-economic and cultural context in relation to implementation science research and consider how these factors may affect proposed interventions |
| Foundations of research methods used in implementation and improvement science: |
| By the end of this course the participant should be able to: |
| 1.1 Describe the ethical principles related to implementation science and quality improvement |
| 1.2 Identify and describe research methods (qualitative, quantitative or mixed) that could be used to answer implementation science questions |
| 1.3 Explain how quality is maintained in implementation and improvement projects |
| 1.4 Describe a range of strategies to measure the outcomes of an implementation project |
| Practicalities of planning and preparing an implementation and improvement project: |
| By the end of this course the participant should be able to: |
| 3.1 Discuss key logistical factors in relation to planning an implementation and improvement project including data collection, analysis and ethical considerations |
| 3.2 Apply the factors outlined in outcome 3.1 to prepare, plan and undertake a small quality improvement project with the support of a mentor |
| 3.3 Discuss how different implementation science tools could be applied to different types of improvement challenges |
| 3.4 Identify an appropriate means for integrating stakeholders (including those beyond the healthcare professional and patient) into the planning, communication and dissemination of results from an implementation project |
| 3.5 Assess the strengths and limitations of key research methods currently used in implementation and improvement studies |
| 3.6 To demonstrate ways in which findings from implementation science projects can be disseminated through both written and oral presentation |
| Approaches to dissemination, monitoring and sustaining change: |
| By the end of this course the participant should be able to: |
| 4.1 Discuss the barriers and facilitators to knowledge transfer and the use of quality improvement in practice |
| 4.2 Recognise the value of disseminating information and quality improvement throughout the project cycles |
| 4.3 Identify methods to monitor, evaluate and sustain changes following an implementation project |
| Study skills |
| By the end of this course the participant should be able to: |
| 5.1 Identify a wide variety of information resources and search tools |
| 5.2 Demonstrate effective search strategies to source relevant materials |
| 5.3 Demonstrate critical thinking in relation to practice and analysis of information sources |
| 5.4 Demonstrate an awareness of academic conventions i.e. avoiding plagiarism, referencing etc. |
| 5.5 Prepare and deliver oral and written information to peers |
| 5.6 Use a number of different communication tools including e-mail, group chats and online classrooms |
| Leadership, management and teamwork |
| By the end of this course the participant should be able to: |
| 6.1 To reflect on the strengths, limitations, threats and opportunities faced in practice relating to implementing a quality improvement project and consider how these elements may be developed or overcome |
| 6.2 Discuss the role of a manager and a leader in relation to developing quality and service improvement in practice |
| 6.3 Engage in teamwork activities to plan, develop and evaluate methods to implement quality and service improvement in clinical practice |
| 6.4 Develop leadership skills though supporting and recognising how quality improvement and service development can be used to enhance healthcare delivery |
2.2. Course structure
From our previous experiences with courses overseas, we had learnt that the participants felt more engaged when involved in face-to-face format that allowed them to network with colleagues at a national and international level and develop a community of practice. This led us to develop a course that was a blend of face-to-face sessions and online support.
The course was designed to work around the clinical duties of the participants and allow them to complete a small-scale quality improvement project under supervision. The course included 3 blocks of 1-week face-to-face teaching, supported by a range of online and social media-based activities (see Fig. 1). The 3 face-to-face contact sessions were planned to be separated by a block of time in order to allow for the participants to identify an area to benefit fromto QI intervention and build support for their project in their places of work, particularly with their line managers. We aimed to achieve the course aims through the 3 weeks face-to face sessions, regular (usually every 2–3 weeks) online topic-driven tutorial sessions (via WhatsApp – which were transcribed, analysed, reviewed and a report sent to the participants), multiple focus group sessions and via their supervised QI project – thus providing multiple methods of input and support. The course was designed to be delivered over a 12-month period (May 2019–May 2020). Unfortunately, due to the COVID-19 epidemic, the final block was converted into an online learning experience with live streaming, recorded session and discussion groups using ZoomApp.
Fig. 1.
Teaching and learning activities.
2.3. Face to face training sessions
Each week was designed to incorporate a combination of taught and interactive workshops to allow participants the time to apply concepts to real world examples, with the support of each other and group facilitators. Each week included a range of methods such a pre-prepared and recorded presentations from a wide range of colleagues from the CGBIPR and Interburns, case study examples, problem-based discussion and both group and individual activities. Each participant was provided with an e-stick that contained all the documents related to the course and their participation, together with copies of presentations, handouts and templates. Each taught week was supported by two facilitators who attended the training, which was delivered in Malawi:
Week one (5 days – May 2019) provided an introduction to the theoretical principles and tools used in implementation and improvement science. Several sessions in week 1 (face-to-face) were discussions with the participants about the most appropriate way to support the participants between the contact weeks.
Week two (5 days – July/August 2019) considered more specifically the logistical factors relating to running a quality improvement project using the participants own project ideas. This included sessions on leadership and management, budgeting, timelines and measurement tools. During this block the participants presented their ongoing project work via a live stream to senior colleagues back at CGBIPR for critique and ideas for improvement.
Week three (3 days – February/March 2020) assisted participants to complete any additional analysis related to their individual QI projects, develop an oral presentation based on their completed project and consider how they might disseminate and sustain their work beyond the end of the course.
Each study block included multiple opportunities for feedback and evaluation of the course to ensure true partnership with the participants and ensure that course delivery was optimised. For example, via group discussion it became clear that our original intention to use a particular technology platform for online support was not going to work for everyone, whilst the use of WhatsApp was easily available and the preferred choice for the group.
2.4. Online forum
An online forum was set up to engage participants in discussion and feedback on their progress between each of the face-to-face weeks. The frequency, time and date of these sessions was agreed during the first training week; however, anticipating potential problems with wi-fi access, the timings were flexible with the option for a second session on the topic if problems occurred. Online group discussions were held every 2–3 weeks. The online sessions were conducted using WhatsApp, which was found to be the most convenient platform. The discussions based on topics proposed by the facilitator and supplemented by student questions and progress updates. The topics were selected to support the participants through their project and move from understanding a topic through to applying the concepts in practice and sharing a problem-solving approach when faced with difficulties in encouraging colleagues to change their behaviour in line with their QI projects. All participants had their own mobile phone, which was their preferred choice of accessing WhatsApp.
2.5. Individual projects
To bring theory to practice, participants were supported to design, develop, implement and monitor a small-scale QI project in their clinical area (burn care) during the course. Participants were assisted to develop their ideas; measurement tools and analysis plans individually by the course facilitators via e-mail and WhatsApp discussions. At the end of the course participants were encouraged to share their findings and disseminate their work to their wider professional networks. Seven of the participants had their own laptop or computer, whilst the remaining participant had access to a computer in their place of work. There was no requirement for work to be presented digitally, with some projects being submitted via scanned documents of handwritten accounts.
2.6. Assessment strategies
As the course was not graded, the assessment activities were formative in nature and used as an opportunity to reflect on course content and confirm understanding of key concepts [[19], [20], [21], [22]]. These activities included contributions to group discussion, peer presentations and workshop activities. Pre and post session quizzes and student presentations were also used to assess participant knowledge in relation to the learning outcomes. Each participant, either alone or in pairs, delivered a final presentation which outlined their QI project, including the results and ideas for future work. These were reviewed by 2 faculty members who provided individual feedback. Group feedback on each other’s presentations was encouraged as a means to increase engagement and critical reflection on both their own and their peers project ideas [23]. At the end of the course participants received a certificate of completion.
2.7. Course participants
Eight participants (Male: Female = 4:4), from 5 different burn services in Malawi and Ethiopia, took part in the course, following a selection process based on a written application. There are 2 main referral centres in Ethiopia dedicated to burn injuries, with a further 2 regional centres; Malawi has 2 dedicated centres. In both countries many patients are treated on surgical wards rather than a dedicated burn centre. The applications (n = 22) were independently graded by three members of staff based at the CGBIPR, using the following essential criteria:
-
•
They were a qualified (fully registered) nurse
-
•
Directly involved in burn care and regularly treated burn patients in Malawi or Ethiopia
-
•
Had previously attended an Advanced Burns Care (ABC) Nursing course delivered by Interburns1, ensuring that they had previous experience of an experiential approach to learning and were familiar with the evidence base for burn injury treatment.
-
•
Had the ability to communicate in written and spoken English.
-
•
Understood the importance of reliable wi-fi/internet connection to fully participate in the course
-
•
They had agreement/support from their hospital management staff to take part in all aspects of the course including a small quality improvement project in their clinical area
The above criteria ensured that applicants were in a strong position to undertake a relevant, small scale quality improvement project and had recently undertaken burn specific training to ensure they were up to date with best practice in burns care. Seven of the participants had a BSc qualification, so had already received an introduction to research, whilst the 8th participant had extensive experience in burn care and attended a number of post-registration burn care courses, having initially qualified in 1992; all participants had a minimum of 7 years clinical experience post initial registration. This course aimed to build on their advanced knowledge of burn care (from the ABC course) and give them the skills to change practice in their workplace. Participant numbers were kept small to allow the nurses to get more involved in their own learning, allow meaningful group work, engaged discussions and the development of a supportive community of practice.
2.8. Data collection
Course evaluations of content, delivery and materials were completed throughout the project, while focus groups were held at the start, middle and end of the program to capture the participant’s experience of undertaking a QI project.
Multiple methods of obtaining evaluative feedback (both quantitative and qualitative) were used [[23], [24], [25], [26]], including feedback from the participants, teaching faculty and self-reflection. The course participants were invited to complete a short questionnaire at the end of the teaching week, which included questions on the overall organisation, content and format of the week. At the end of the course participants were asked to rate their confidence in relation to each learning objective, using a 5-point scale. Course evaluations for Week 1 and 2 were completed as part of the block teaching week; the final questionnaire was completed online using Qualtrics online survey software (as the course was reconfigured due to COVID 19).
Peer evaluation was used informally to help evaluate the appropriateness of the teaching methods, session design and pace of delivery [25]. The observing facilitators provided feedback on student interaction with each other and the facilitator. This feedback formed part of a reflection and de-brief meeting which was held at the end of each teaching day. The main facilitator regularly monitored student responses in order to adapt content and pace in line with student levels of engagement [27].
Focus groups were conducted on the first day of each face-to-face teaching week by the first author, who already knew all the participants from their attendance on the ABC course. An initial discussion guide was developed in consultation with the project team, which was further refined as the course progressed. The Consolidated Framework for Implementation Research (CFIR) [28] was also used to capture different elements of the improvement process. With the permission of the participants, these discussions were audio recorded for later thematic analysis. Due to the COVID-19 epidemic the final focus group was unable to run in the same way; restrictions with mobile data, connectivity and participant availability prevented a virtual focus group. Instead the participants were invited to complete a final project review form which was returned via a secure e-mail.
2.9. Data management and analysis
All audio data and project reflections were transcribed verbatim into Microsoft Word. Due to the nature of recording focus groups, it was not always possible to identify the participant speaking on the audio. However, where identifiable information was provided this was anonymised at the point of transcription. Thematic analysis was used to systematically code the data for key features, repetitions, actions and beliefs, taking into account all comments which both agree and or disagree with the point under discussion [29,30]. To enhance validity the transcripts were independently analysed by two researchers (MH, CH) before meeting to agree codes, themes and sub-themes [30,31]. The final codes were then presented back to the course participants to ensure there had been no misinterpretation of their experiences and expand on any areas which had been unclear during the coding process. Data analysis was completed using NVivo (version 12) software.
2.10. Ethics and funding
Ethical approval was obtained from the University of Swansea, College of Human and Health Sciences Research Ethics Committee (190219d). All participants gave written informed consent at the start of the study, knowing that their all their data would be anonymised and held confidentially. This project was funded by the National Institute for Health Research (NIHR), NIHR Global health Research Group on Burn Trauma, Grant Reference 16/ 137/ 110. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
3. Results
The results are presented in two sections; the first section covers the course evaluation, while the second section covers the student experience of conducting a quality improvement project. The quotations included are taken verbatim from the student feedback.
3.1. Course evaluation
Qualitative feedback from the students suggested that the structure of the course was clear, the content was relevant, and the facilitators were praised for being supportive and helpful through the process, with group discussions singled out as an effective learning method multiple times:
“Group project participation allowed us to internalise what we have learned through the work and put them in practice”.
Previous experiences of QI projects in both Malawi and the West Bank were used as real life examples which the participants felt helped them contextualise what they were learning:
“The QI presentation of burn unit in West Bank and the maternal newborn health project in Malawi helped me to visualise on how best to implement the project.”
Participants noted their enjoyment of preparing and then giving their presentations, as a way to deepen their understanding of QI projects:
“Presenting the project proposal gave us a feel of reality of QI project.”
Participants were also asked specifically how they felt the course could be improved; many of the comments related to practical and logistical issues, such as the inconsistent power supply, which was disruptive to their learning, although they also acknowledged that this was not in the control of the facilitators:
“The venue was not well equipped with power back up as we experienced power interruptions several times that affected the lessons.”
Poor internet connection was raised multiple times as needing improvement and some also noted that the days were too long:
“It was so tiresome, and we finished a bit late. I would suggest we start earlier and finish in good time.”
This particular comment comes from Week 1 of the course and provides a concrete example of how we then amended the course to fit the times that best suited the participants; the times were all amended for Week 2. This would have applied to Week 3 as well, but this was overtaken by the changes associated with the epidemic.
Some felt that there was plenty of time to prepare the project proposals whilst others felt that more time would have been beneficial.
“We had enough time to prepare the project proposals and it was well organised.”
“I feel that more time could have been given for the development of the project.”
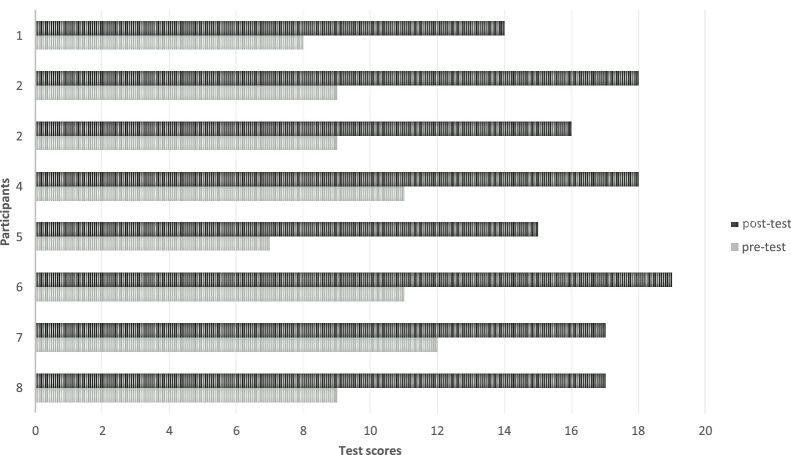
In Week 1, a pre- and post-course test was completed based on 20 questions that related to the content of the week which focused on the principles behind implementation science and the steps needed to complete a QI project. This was a knowledge-based test that allowed us to reflect on the amount of learning that had taken place during the week and start to formulate some of the topics for the online tutorials, to ensure that the participants were fully prepared to start their QI project. At the end of Week 1, each of the eight participants had a higher post- than pre-score, with an average 78% increase (see Fig. 2); although all participants had improved their overall scores it became clear that additional work was need on certain topics such as the reliability of measurement tools, the assumptions made in QI projects and when to collect and use QI information. These areas became the focus of online group discussions and the initial session in Week 2, before moving on to new topics.
Fig. 2.
Knowledge of QI processes at the beginning and end of week 1 for each participant.
An example of the end of course evaluation is included in Fig. 3. One participant had to leave early due to a family emergency, so only 7 participants are included. The data indicate that all the students either agreed or strongly agreed with the scaled items.
Fig. 3.
Teaching evaluation week 2.
3.2. Face-to-face and online learning
Participants were asked to comment on the combination of face-to-face and online learning: all respondents thought it was a good combination, and the spacing between each of the face-to-face blocks was appropriate although concerns about IT hardware and access to the network were raised:
“It’s very useful in conducting this kind of implemented project to discuss very unclear ideas in detail and sharing new ideas to improve changes from other members and it’s very nice but in the case of online meetings personally we faced problem like having bad network.”
“Very helpful, we had good time indeed, we only had a limitation in having a rim of paper and for me especially, I was challenged with having no laptop, made it difficult for me to do much work”
3.3. Online discussion groups
Online discussion groups were rated very positively highlighting how they were: convenient and efficient, helped keep learning active, were economical for data usage and were an enjoyable way to share ideas. In terms of timing between the online discussions, 67% felt it was adequate, 11% thought they should have been less frequent and 22% thought they should have been more frequent. Following a recurring theme for other aspects of the evaluation, poor connection at a national level was discussed as barrier to the utility of the discussion groups:
“There was good participation with an aspect of reality on the ground. Sharing ideas and progress. But it also helped not to relax on the project but put an extra effort”
3.4. Conducting quality improvement projects
Although the success of the course was not designed to be measured by the outcome of individual participant’s quality improvement projects per se, it is important to recognise the work undertaken by the students in developing a QI project in their clinical area. All the projects were successfully completed within the time frame and are presented in Table 2 (N.B., while there were eight participants four worked in pairs resulting in six projects overall).
Table 2.
Participant led quality improvement projects completed by the participants.
| Title | Problem | Aim | Outcome |
|---|---|---|---|
| Improving vital signs and fluid balance monitoring for HDU burns patients | Patient vital signs and fluids monitoring is not regularly done therefore patients do not always receive the right care or prescribed fluids | To improve vital signs and fluid administration documentation on patients that are in the burn HDU from 40%* to 90% from September 2019 to January 2020 | The project resulted in 78% of cases having complete documentation after 3 months, with nurse reporting an increase in their confidence and knowledge |
| Improving the decontamination process of surgical instruments | The steps of the decontamination process for cleaning surgical instruments are not followed or completely missed | To improve compliance with the decontamination processes for surgical instruments in main theatres by January 2020 | Compliance to the 11- step process rose from 77% to 90%. Improvement was seen for 10 steps, so an additional session of staff training was developed on ‘dipping instruments correctly’. |
| Improving pain control for burns patients during dressing changes | Patient do not regularly get pain relief before dressing changes causing anxiety, distress and lack of co-operation | To improve pain control in for burns patient during dressing changes from 10%* to 70% during dressing changes by December 2019 in the male and female surgical wards | After five months the number of patients reporting that they had sufficient pain control rose to 66% |
| Hand hygiene practice among health workers in the burn unit | There are poor hand hygiene practices amongst healthcare workers | To improve hand hygiene practice among healthcare workers in the burns unit from 5%* to 50%* by December 2019. | The project saw an increase in availability of hand washing facilities to 95.6% and hand hygiene practices increase to >80% within 6 months. |
| Improving documentation following dressing changes | Inadequate information was being documented in files leading to poor escalation of concerns follow-up. | To improve documentations in patient files amongst the staff following dressing changes in adult burn patients from 44% to 90% by February 2020. | After three months, an audit revealed that 85% of dressing changes were supported with accurate documentation. |
| Keeping the privacy of male and female patients | Dressings are done for male and female patients in the same room causing complaints from the patients and their attendants | To improve privacy and dignity among male and female burn patients who have been admitted to the ward at the time of dressing using a patient screen from 15%* to 50% by December 2019 | Data from the project convinced colleagues that this was an important topic; screens were introduced and are now used routinely. |
Focus group and project review data were categorised into barriers (see Table 3) and/or facilitators (see Table 4) associated with finding and reviewing current evidence, developing and conducting a QI project.
Table 3.
Barriers to change and providing evidence-based practice.
| Themes | Sub-themes |
|---|---|
| People | Lack of accountability and supervision |
| Staff rotation | |
| Unit culture and attitudes | |
| Inadequate leadership | |
| Burns not seen as a priority | |
| Negative attitudes towards training and lack of follow up | |
| Poor communication and information access | Limited access to devices and reliable connection |
| Costs associated with information access | |
| ICT competence | |
| Lack of resources | High workload and staff shortages |
| Inadequate equipment and stock shortages | |
| Lack of access to additional finances |
Table 4.
Facilitators to change and providing evidence-based practice.
| Themes | Sub-themes |
|---|---|
| People | Active individuals |
| Positive leadership | |
| Supportive and collaborative work environment | |
| Engagement of staff and patients in change | |
| Knowledge sharing | Access to appropriate training |
| Access to up-to-date information to guide practice | |
| Successful communication strategies | |
| Improved patient care | |
| Demonstrable advantages of the proposed change | Progress reports |
| Simplification of processes | |
The key barriers to providing evidence-based care and motivating change were grouped into the themes of people, poor communication and information access, and lack of resources.
3.5. People
This theme incorporates six sub-themes: (1) lack of accountability and supervision, (2) frequent staff movement and rotation of experienced staff to other areas, (3) negative unit culture and attitudes towards change, (4) lack of adequate leadership to champion for changes, (5) lack of attention given to burns care compared to other specialities and (6) attitudes towards those who attend additional training and a lack of follow up on behalf of the trainers.
Participants indicated that staff might “take short cuts” in order to complete a task in less time due to an increased workload. They also indicated that occasionally there was a lack of individual accountability coupled with a lack of supervision by senior staff:
“People don’t want to do things in the right way because of a lack of supportive supervision because if the supervisor is not there and s/he is not involved in the direct care of the patients the subordinates will do whatever they want and nobody will follow them up and no one takes them to task that is why they do that, that's why so I think that's what contributes for them not to do the right thing.”
Frequent staff movement and rotation out of the burns unit to work in other areas or specialities in the hospital resulted in a frequent loss of expertise and experience:
“If there is someone who knows more about burns and is moved to another unit most definitely the care will go down and we will still have more needs, we will need to train more nurses on the same, on an issue that someone has already learned so there will stall be a gap.”
They also reported that nursing staff avoided rotations to the burns units or tried to cut their time short within these areas’ due high workloads and a “fear” of working with burns wounds:
“I think most of the nurses they will say the wounds are so scary every day I should be seeing wounds from there I go and eat meat so it’s like an attitude so most of the nurses who work in burns they either maybe they have been in a surgical department for some time and they are used but you cannot move someone from the maternity wing to surgical department they won't allow that so it is an attitude thing.”
Negative attitudes towards burns patients and care were also described by participants to be hospital wide. For instance, it was reported that, in comparison with other specialities, burns were not seen as a priority. This lack of attention to the burns problem resulted in a feeling amongst participants that it would be very difficult to levy support to make changes in the unit that required hospital investment. Additionally, it was reported that these attitudes were possibly a result of senior management having little awareness or understanding of burns care and what this involves.
It was acknowledged that while training was viewed as an important factor to improve burns knowledge and bring about change, there were limitations to its effectiveness including dissemination of new knowledge:
“Whenever people have gone to training. Now those on the ground will say “because you went there it means you are responsible for that” the information can be there but they will never read or the references will be there but they will never, I mean never refer to them they will just expect the one who went for that training is the one who should be responsible for that part.”
3.6. Poor communication and information access
The main sources of information used to review and guide their practice included: journal databases, Google Scholar, library books, colleagues, symposiums, training, university webpages and generic internet sites. While local hospital guidelines exist to provide information about certain procedures, many were missing or out of date and therefore, they felt they needed to seek further information. Participants explained that they used personal mobile phones, hospital e-libraries, ward computer or, for those that had them, a personal laptop to access information. However, participants experienced: (1) limited access to computer equipment and reliable connections, (2) high costs associated with the purchase of journal records and (3) limited training on information searching and ICT competence:
“I think the main barrier is access to internet through like the Wi-Fi and also through the computers and if you have a phone the data is very expensive in our country so that is the main barrier.”
The participants report that as nurses they felt they had limited time to seek new information in comparison to other professions. For example, the nurses reported that for the doctors it was acceptable for them to use personal mobile devises during work time, on the unit, to access information. However, the use of mobile phones for nurses in this case was prohibited. Moreover, once the participants were able to access the internet and locate relevant papers they are faced with journal and access costs:
“Most of the articles they sell you see that the right article, maybe the right information you are looking for bur you need to buy it, so it is not easy to access it.”
Limited knowledge and competence with using the technology and relevant search engines was also noted as a barrier:
“there are some who don't know how to use the computer. I think on the type of people who likes using the computer is the I can say the youth and the young adults because of this technology but for elder nurses or yeah they don't like and they don't know how to use it so they can't even do it so it is only really for the young nurses who prefer checking the information on the internet” [Focus Group 2]
3.7. Lack of resources
Lack of resources, both human and physical, was a common theme. These challenges could be categorised within three sub-themes (1) High workload and staff shortages, (2) Inadequate equipment and stock shortages and (3) Lack of access to additional finances to precure new or replacement equipment.
The high workloads were considered to affect staff’s willingness to engage in change:
“Change is always difficult. Many nurses may have felt it was just increasing their work and when monitoring they thought you were being difficult.”
In other cases, having a shortage of specialities to assist with patient care was increasingly demotivating:
“if you are doing a process and you are stuck somewhere because there is no human resources, like what he said you might clean the wound and they are ready for skin grafting but after being scheduled you find that you don't have an anaesthetist or there are a pile of patients to go so you that you see that the patients are delayed in the hospital instead of being helped and going home early they stay a long time in the hospital so that demotivates me” [Focus Group 2]
Participants reported a lack of equipment was demotivating as they were unable to provide best practice resulting in increased suffering or deterioration for the patients:
“there are a number of times when you see that maybe the patient has developed a complication like in our instance toxic shock syndrome for children which indicates special antibiotics and you find there is no support from the pharmacy - they will always say that we don't, we don't have even maybe the patient him or herself or the guardian cannot manage to buy that and losing a patient because of that and you know that maybe you could have saved that patient it is very devastating and demotivating.”
In some cases, it was not that the hospital lacked the equipment or medication but the processes in which equipment was allocated to their unit was not fit for purpose:
“I become frustrated most of the time working in the burns unit or in the burn ward because of like as she said exactly there is less resource being located to the wards. Like for use for medical and also other wards the resources the gauze is allocated more but in for burn and also surgical wards the resources are allocated last.”
As participants began to undertake their own quality improvement projects, they reported that it was a challenge to access any significant finances to procure additional resources, especially where they were competing against different specialities. Moreover, while in some cases external agencies and non-governmental organisations could provide stock and equipment this did not always result in a consistent supply, or participants found that hospital policy could make accepting resources from outside organisations challenging:
“When you don’t have those things you have to go into other wards begging and stuff and sometimes asking outside the hospital and sometimes when you want to ask from outside the hospital you have to go through the hospital management the protocols and stuff and most people they don't like that they just want, if they want to donate something they just come in and donate.”
People were also seen as facilitators to supporting change (see Figure 5), which incorporated four sub-themes: (1) active and motivated individuals, (2) positive leadership, (3) a supportive and collaborative work environment and (4) engaging staff and patients in intervention development. Participants reported that best practice and changes were often encouraged by “active” individuals within their team who were particularly motivated to improve their work environment and the care of the patients:
“it also depends on how active the people who has the knowledge to disseminate otherwise if you just have the knowledge and you keep down nothing will change.”
The motivation to disseminate good practice and change was enhanced in units where nurses felt they were valued for their own expertise:
“When I see that there is a real gap a big gap in the knowledge not only to the nurses but also even the doctors so when I see that there is a gap and maybe I have the knowledge I have already said through this training and come in to the extent that maybe even the senior doctors are trusting you that the work that the doctors are supposed to do entrusting you that nurses, especially you people you have to do this, this, this I feel very motivated because I see that gap being filled by me! Myself as a nurse! So, it motivates me very much.”
Providing supportive supervision for staff, a culture of teamworking and receiving positive feedback was seen as very important:
“Motivation comes from everyone but normally from the stakeholders and administrators, doctors, patients and attendants if someone gives you thanks it is also motivation for me this is one part of motivation, so motivation is very important.”
Lastly, participants indicted that, through engaging relevant stakeholders early in their improvement project, they were able to overcome some of their initial concerns. They did this by creating project committees, enlisting QI champions and involving their team in project measurements and progress:
“A project committee was involved in the decision-making process. In the introduction of the project most of the stakeholders could not understand the project. With time they appreciated the change in burn care. By making the colleagues to own the project this eased communication. Teamwork also improved ownership.”
3.8. Knowledge sharing
The most effective means of sharing knowledge, developing practice and bringing about change, as reported by participants, could be categorised into the following three sub-themes: (1) access to training and (2) access to up to date information to guide practice and (3) local strategies to communicate information about practice development. They found training as an effective motivator to review their own practice and consider improvements:
“Before attending the (Interburns) ABC training I never thought a burn patient has a lot to go through but I have learnt that a burn patient you don't just look at the burn but you look at the patient as a whole all the systems in him or her they get affect […] So, after taking care of the patient I feel satisfied that I have received the patient who was severely burned and I have helped them and they are going home healed I become satisfied and I still like to work in the burns unit.”
Participants also noted the importance of having regular training within their unit teams to share knowledge and review their practice. Participants indicated that they have continued professional development (CPD) training within the hospital, and described this as a means to indirectly bring attention to a particular issue in practice without causing tension with colleagues:
“I think sometimes ignorance is a problem so they are very resistant to change if they don't know something so the right way to go with maybe implementation is to first of all, you have to provide the knowledge to them and then we have to work together don't just tell them, don't just say "we should do that" give the knowledge they should know what to do and then we can implement.”
Experiences of training were not consistent across participants and CPD could often be cancelled. In addition, participants indicated that the application of evidenced-based practice was reliant on having easily accessible and up-to date guidelines with many noting that existing protocols were often missing or out of date.
Effective communication strategies were considered crucial to the dissemination of up-to-date information to guide practice. Effective communication strategies described by the participants included: development of guidance documents, conference meetings, new staff orientation, team meetings, WhatsApp groups and video clips:
“The video clips showing how infections are spread through hands also encouraged many of the co-workers to embrace the changes. Not only that, but also sharing the lab investigation on MRSAs and pseudomonas infraction which was high on the ward played a role to encourage the team to do their best.”
E-mail was reported as a form of communication used for knowledge sharing but was not seen as effective as other strategies.
3.9. Demonstrable advantages of the proposed change
Participants reported that where it was possible to demonstrate the advantages of the proposed change in their QI project, they were able to convince colleagues, who may initially have been apprehensive, to adopt and sustain the improvement. Participants used: (1) improvements in patient care, (2) progress reporting and (3) the simplification of existing processes to convince colleagues to work as a team.
Improvements in patient care included reports by participants where their changes had, through improving patient experience, assisted staff in reviewing and redesigning their clinical tasks. For example, a participant designed and implemented a project to improve pain control during dressing changes where they aimed to encourage staff to offer analgesia to their patients at least 30 min prior to wound dressings. Staff reported that this resulted in a better experience for the patient but also allowed the practitioner to undertake their task without additional support and stress:
“Initially patients would be forcibly dressed, and this received extra human resource to restrain the patient. Now wound cleaning is done thoroughly as patients cooperative and this aids in wound healing hence reduced period of hospitalization […] patients were narrating to some nurses about improvement in terms of pain control during dressing changes and staff felt more comfortable as there was cooperation from the patients.”
Presenting their project data back to their unit allowed staff to observe both the extent of the initial problem and the impact of the subsequent changes. This data was then used to give recognition to staff, both individually and to groups, for their role in the improvement:
“Pasting the best documenters names on the wall encouraged others to also do well in documentation.”
Lastly, participants indicated that where a proposed change was seen to help simplify or make clear an existing process, their colleagues started to integrate the change into their own practice. For example, a project which introduced new documentation to be completed at dressing changes included creating a chart made up of a simple checklist for wound documentation and an accompanying guidance document:
“At first there was some resistance to get them on board, but after some orientation and involving them to come up with problems and solutions, things changed […] staff recommended that this was an easy way of documentation and the patients said they are not missed in wound management.”
4. Discussion
The results of the study demonstrate that it is possible to provide effective training on improvement and implementation science to nurses working in burns units, in Malawi and Ethiopia, through a combination of face-to-face and online learning. The study also highlights the wide range of barriers and facilitators experienced by the participants as they set up and conducted their projects, with issues relating to the high turn over of staff and limited resources resonating with an earlier study that focused on paediatric burn treatment education in Malawi [32]. While some of these will resonate with health professionals from all parts of the world [32,33], the results capture some of the particular challenges of working in an LMIC environment. The best testament to the quality of the projects completed by the participants can be found in an innovative open access educational resource in the form of an e-book (available at https://interburns.org/news/a-practical-guide-to-quality-improvement-in-burn-care or
https://online.flippingbook.com/view/792687/). This e-book focuses on the practical steps needed when undertaking a quality improvement project in an LMIC, celebrating the projects undertaken by the participants.
The arrival of the epidemic required the team to focus more directly on different methods of course delivery, increasing the emphasis on online methods in order to ensure that the participants completed the course. This work will lead to a new, interactive online resource in the form of an online module that will include an introduction to Implementation and Improvement Science and the tools that are available to undertake a QI project. The module, which will be free to access from www.interburns.org, will also include a step-by-step guide to the process of undertaking a QI project in a burns service in LMIC settings. While we should not underestimate the additional benefits of face-to-face interactions, the epidemic has refocused attention on the importance of providing alternative ways to scale up access to resources that do not rely on international travel.
The course was developed recognising that in Malawi authoritarian and teacher-centred styles tend to dominate the educational activities of nurse tutors and clinical learning [[34], [35], [36]], while staff in Malawi and Ethiopia have been less able to develop their approaches to pedagogy due to a lack of resources and opportunities [[37], [38], [39]]. However, more recently there has been an increase in examples of success (in both Malawi and Ethiopia) where participatory and active learning techniques have been used to build research capacity and implement post-graduate training curriculums [[40], [41], [42], [43]]. This course used interactive, scenario-based sessions to assist participants to make a connection between the theory which underpins QI methodology and reviewing and improving their current practice.
One element of the course that received constant reinforcement was that implementation and improvement science is different to “traditional” research approaches. There was a perception that all projects required a large budget with an injection of IT hardware (e.g., iPad, laptops). Using case studies of other quality improvement projects, led by nurses in similar contexts, proved invaluable in addressing this issue as participants were able to see examples relevant to their own experiences, many of which did not require injections of funding. The content of Week 2 was also amended to include more emphasis on an asset-based approach while participants were developing ideas for their own projects.
An unexpected consequence of the course has been the swift recognition of the skillset developed by the participants by senior staff in their places of work. Since the course ended a number of the participants have been invited to act as mentors for future initiatives, supporting other nurses working in burns care settings. This recognises that the participants are now in a position to share their own experiences as a means of demonstrating how QI can be both developed and led by nurses, without the need to access large financial investment or external stakeholders.
Although the use of WhatsApp was not our original plan, this platform was selected as the majority of the participants already had the application, found it easy to navigate, and knew they could share files and voice messages. The group found the WhatsApp discussions complimented the course delivery; if participants were unable to attend at the time of the discussion, they were able to review what had been said and provide their thoughts at a more convenient time. The informal nature of the application allowed participants the freedom to send quick, short messages without needing to spend too much time considering their use of language style while maintaining their support network despite being geographically separated. Similar effects have also been found when using WhatsApp as a means to support higher education teacher development courses [44].
4.1. Strengths and limitations
This pilot course has provided a wealth of information and lessons learned, from which future courses and educational resources on improvement and implementation science can be developed. However, while the participants represented five different hospital facilities, the sample was relatively small which allowed for significant individual attention and support. The group itself was a biased group in that motivation for participation was part of the selection process, the course was only available through the medium of English, and everyone had to have already attended an Interburns Advanced Burn Care (Nursing) course, demonstrating their commitment to ongoing self-improvement and life-long learning. The use of face-to-face focus groups allowed the facilitators to seek clarification on the understanding of key concepts and ask follow up questions to encourage in-depth discussions. Unfortunately, the final focus group was unable to go ahead as planned and instead participants were invited to complete a project review form to provide information about the implementation of their projects. Although the review forms provided valuable information about the projects, the depth of information was limited and, in some cases, superficial.
As is always the case with qualitative data, there is the potential for the researchers to emphasise those elements that support their own views. Indeed, it is possible that some of the qualitative content reflects a social desirability set within the participants, given the facilitators also ran the face-to-face elements of the course. The processes used to analyse the data (e.g., 2 independent researchers, and confirmation of thematic analysis with the participants) will have gone some way to ensure that these potential biases were kept to a minimum.
5. Conclusions and recommendations
This study has identified some of the key barriers (staff attitudes, poor leadership, negative culture towards training, resource limitations, staff rotation and poor access to information to guide practice) and facilitators (active individuals, supportive leadership, collaboration, effective knowledge sharing and demonstrable advantages of any proposed change) that nurses encounter in applying and motivating changes in Malawi and Ethiopia, particularly when undertaking a quality improvement project in a burns facility. An understanding of these issues will help support course refinement and prompt an exploration of new forms of course delivery. The changes imposed on the course members by the arrival of the COVID-19 epidemic, has provided an opportunity to consider a wider range of possible methods of delivery allowing for a faster approach to scale-up of course provision across a wide range of LMICs. An introductory, open-access online course is now available via registration on the Interburns website.
However, this pilot has demonstrated that by bringing nurses together for face-to-face sessions that include interactive teaching, case studies and a problem-solving approach increases the potential for the development of a successful community of practice whereby members can advise and support each other to overcome barriers to implementing change. The success of the projects undertaken by the participants has demonstrated that nurses can play a significant role in the improvement of burns services. It is important that nurse training on quality improvement is designed to be context specific and responsive to the barriers and facilitators identified. The course provided an understanding of implementation and improvement science, whereby these low cost but well-designed projects led to improved patient care whilst building sustainable skillsets leading to lasting change.
Conflicts of interest
There are no conflicts of interest for any of the authors.
Funding
This work was supported by the National Institute for Health Research (NIHR) UK [grant numbers HHR1013-10]. The views expressed are those of the authors and not necessarily those of the NIHR of the Department of Health and Social Care.
Author contributions
MH, PP and TP were responsible for the overall concept and planning of the programme; MH drafted the detailed planning and delivery of the programme, supported by EO, and supervised by PP and TP; MH and EO were the main facilitator for the face-to-face delivery component of the course; CH reviewed and analysed the qualitative data with MH. MH, PP and TP were responsible for the production of the paper which was supported by CH and reviewed by EO. All authors have agreed the final content.
Acknowledgements
The authors would like to thank all of the participants on the course for their positive approach to participation and their infectious enthusiasm for learning. Thanks are also due to all those members of Interburns and Swansea University who contributed to the course through organisational support or deliver of specialist podcasts, particularly Lucy Kynge (Interburns) for her support with the digital delivery of the program and issues related to internet access, and Jenine de Vries for all things logistics and administration.
Footnotes
ABC Nursing is a 5-day modular program designed for nurses who are working in burns care in resource-poor countries. ABC nursing is a highly practical course which focuses on group work, interactive case studies and problem solving. The course is delivered by Interburns using a combination of local instructors and international faculty.
References
- 1.Peters D.H., Tran T., Adam T. World Health Organization; Geneva, Switzerland: 2013. Implementation research in health: a practical guide. ISBN; 9789241506212. [Google Scholar]
- 2.Potokar T., Bendell R., Chamania S., Falder S., Nnabuko R., Price P.E. A comprehensive, integrated approach to quality improvement & capacity building in burn care and prevention in low & middle income countries: an overview. Burns. 2020;46:1756–1767. doi: 10.1016/j.burns.2020.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organisation Factsheet: https://www.who.int/news-room/fact-sheets/detail/burns. [Accessed 1 March 2021].
- 4.Tyson A.F., Boschini L.P., Kiser M.M., Samuel J.C., Mjuweni S.N., Cairns B.A., et al. Survival after burn in a Sub-Saharan burn unit: challenges and opportunities. Burns. 2013;31:1619–1625. doi: 10.1016/j.burns.2013.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiser M.M., Samuel J.C., Mclean S.E., Muyco A.P., Cairns B.A., Charles A.G. Epidemiology of pediatric injury in Malawi: burden of disease and implications for prevention. Int J Surg. 2012;10:611–617. doi: 10.1016/j.ijsu.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Ogada E.A., Gebreag A.H., Potokar T.S. Review of the epidemiology of burn injuries in Ethiopia; implications for study design and prevention. Burn Open. 2019;3(3):75–82. doi: 10.1016/j.burnso.2019.05.002. [DOI] [Google Scholar]
- 7.All-Party Parliamentary Group on Global Health . All-Party Parliamentary Group on Global Health; London: 2016. Triple Impact – how developing nursing will improve health, promote gender equality and support economic growth. [Google Scholar]
- 8.Nursing Now. Vision available. [Accessed 26 March 2018].
- 9.World Health Organisation . World Health Organization; Geneva: 2020. State of the world’s nursing 2020: investing in education, jobs and leadership. ISBN: 978-92-4-000327-000329. [Google Scholar]
- 10.Eccles M.P., Mittman B.S. Welcome to implementation science. Implement Sci. 2006;1:1. doi: 10.1186/1748-5908-1-1. [DOI] [Google Scholar]
- 11.Peters D.H., Adam T., Alonge O., Agyepong I.A., Tran N. Implementation research: what it is and how to do it. BMJ. 2013;347:f6753. doi: 10.1136/bmj.f6753. [DOI] [PubMed] [Google Scholar]
- 12.Murray J.P., Wenger A.F.Z., Downes E.A., Terrazas S. Springer Publishing Company; New York: 2011. Educating health professionals in Low-Resource countries: a global approach. [Google Scholar]
- 13.Eaves M. The relevance of learning styles for international pedagogy in higher education. Teach Teach Theory Pract. 2011;17(6):677–691. doi: 10.1080/13540602.2011.625143. [DOI] [Google Scholar]
- 14.Kolb D. Prentice-Hall; 1984. Experiential learning: experience as the source of learning and development. ISBN: 0132952610. [Google Scholar]
- 15.Medina M.S., Castleberry A.N., Persky A.M. Strategies for improving learner metacognition in health professional education. Am J Pharm Educ. 2017;81(4):78. doi: 10.5688/ajpe81478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knowles M. 4th edition. Gulf Publishing; Houston: 1990. The adult learner: a neglected species (building blocks of Huan potential) ISBN: 9780872010741. [Google Scholar]
- 17.Bloom B. Handbook one: cognitive domain. McKay; New York: 1956. Taxonomy of educational objectives: the classification of educational goals. [Google Scholar]
- 18.Quinn F.M., Hughes S.J. Nelson Thornes Ltd; Cheltenham: 2007. Principles and practice of nurse education. ISBN:978074879660. [Google Scholar]
- 19.Norton L. In: A handbook for teaching and learning in higher education: enhancing academic practice. 3rd edition. Fry H., Ketteridge S., Marshall S., editors. Routledge; New York: 2009. Assessing student learning; pp. 132–149. ISBN: 10:0-415-43464-5. [Google Scholar]
- 20.Race P. 2nd edition. Kogan Page; London: 2001. The lecturers toolkit. ISBN 13:978-0-415-40382-5. [Google Scholar]
- 21.Rushton A. Formative assessment: a key to deep learning? Med Teach. 2005;27(6):509–513. doi: 10.1080/01421590500129159. [DOI] [PubMed] [Google Scholar]
- 22.Cauley K.M., McMillan J.H. Formative assessment techniques to support student motivation and achievement. Clear House J Educ Strategies Issues Ideas. 2010;83(1):1–6. doi: 10.1080/00098650903267784. [DOI] [Google Scholar]
- 23.Liu N., Carless D. Peer feedback: the learning element of peer assessment. Teach High Educ. 2006;11(3):279–290. doi: 10.1080/13562510600680582. [DOI] [Google Scholar]
- 24.Biggs J. The reflective institution: assuring and enhancing the quality of teaching and learning. High Educ. 2001;41(3):221–238. doi: 10.1016/0969-5931(94)00033-1. [DOI] [Google Scholar]
- 25.Hounsell D. In: A handbook for teaching and learning in higher education: enhancing academic practice. 3rd edition. Fry H., Ketteridge S., Marshall S., editors. Routledge; New York: 2009. Evaluating courses and teaching; pp. 198–212. ISBN: 10:0-415-43464-5. [Google Scholar]
- 26.Parkinson B. Using evaluation to improve teaching. Nurs Times. 2016;112(7):8–10. http://www.nursingtimes.net/roles/nures-educators/using-evaluation-to-improve_teaching/7010065.article [Google Scholar]
- 27.Walsh D. 2nd edition. McGraw Hill; Maidenhead: 2014. The nurse mentor’s handbook. ISBN-10-0335263194. [Google Scholar]
- 28.Consolidated Framework for Implementation Research. Interview Guide Tool Available from: https://cfirguide.org/guide/app/#/. [Accessed 1 May].
- 29.Ryan G.W., Bernard H.R. Techniques to identify themes. Field Methods. 2003;15(1):85–109. doi: 10.1177/1525822X02239569. [DOI] [Google Scholar]
- 30.Braun V., Clarke V. SAGE Publications; London: 2013. Successful qualitative research. ISBN: 9781847875815. [Google Scholar]
- 31.Shenton A.K. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf. 2004;22(2):63–75. doi: 10.3233/EFI-2004022201. [DOI] [Google Scholar]
- 32.Harris L., Fioratou E., Broadis E. Paediatric burns in LMICs: an evaluation of the barriers and facilitators faced by staff involved in burns education training programmes in Blantyre, Malawi. Burns. 2016;42(5):1074–1081. doi: 10.1016/j.burns.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 33.Sommerbakk R., Hauhen D.F., Tjora A., Kaasa S., Hjermstad M.J. Barriers to and facilitators for implementing quality improvements in palliative care–results from a qualitative interview study in Norway. BMC Palliat Care. 2016;15(1):61. doi: 10.1186/s12904-016-0132-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chilemba E.B., Bruce J.C. Teaching styles used in Malawian BSN programmes: a survey of nurse educator preferences. Nurse Educ Today. 2015;35:55–60. doi: 10.1016/j.nedt.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 35.Mbirimtengerenji N.D., Adejumo O.N. Education challenges of student nurse tutor interactions in Malawi nursing colleges. Int J Sci Res. 2015;4(4):88–101. doi: 10.36106/ijsr. [DOI] [Google Scholar]
- 36.Solum E.M., Maluwa V.M., Tveit B., Severinsson E. Enhancing students’ moral competence in practice: challenges experienced by Malawian nurse teachers. Nurs Ethics. 2016;23(6):685–697. doi: 10.1177/0969733015580811. [DOI] [PubMed] [Google Scholar]
- 37.Biku T., Demas T., Woldehawarait N., Getahun M., Mekonnen A. The effect of teaching without pedagogical training in St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. Adv Med Educ Pract. 2018;9:893–904. doi: 10.2147/AMEP.S1677944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Middleton L., Howard A.A., Dohrn J., Von Zinkernagel D., Hopson D.A., Aranda-Naranjo B., et al. The nursing education partnership initiative (NEPI): innovations in nursing and midwifery education. Acad Med. 2014;89(8):24–28. doi: 10.1097/ACM.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 39.Bvumbwe T.M., Mtshali N.G. A middle-range model for improving quality of nursing education in Malawi. Curationis. 2018;41(1):1–11. doi: 10.4102/curationis.v41i1.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meshkat N., Teklu S., Hunchak C. Design and Implementation of a post graduate curriculum to support Ethiopia’s first emergency medicine residency training program: the Toronto Addis Ababa Academic Collaboration in Emergency Medicine (TAAAC-EM) BMC Med Educ. 2018;18(71):1–8. doi: 10.1186/s12909-018-1140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smythe T., Le G., Owen R., Ayana B., Hansen L., Lavy C. The development of a training course for clubfoot treatment in Africa: learning points for course development. BMC Med Educ. 2018;18(1):163. doi: 10.1186/s12090-018-1269-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haileamlak A., Hailu S., Nida H., Desta T., Tesema T. Evaluation of Pre-service training on integrated management of neonatal and childhood illnesses in Ethiopia. Ethiop J Health Sci. 2010;21(1):1–14. doi: 10.4314/ejhs.v20i1.69427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tveit B., Solum E., Simango M. Building research capacity in Malawian nursing education - a key to development and change. J Nurs Educ Pract. 2015;5(10):1–8. doi: 10.5430/jnep.v5n10p1. [DOI] [Google Scholar]
- 44.Tyrer C. Beyond social chit chat? Analysing the social practice of a mobile messaging service on a higher education teacher development course. Int J Educ Technol High Educ. 2019;16(1):13. doi: 10.1186/s41239-019-0143-4. [DOI] [Google Scholar]