Hypertension affects almost half of US adults, and blood pressure (BP) control is a national public health priority.1 The coronavirus disease 2019 (COVID-19) pandemic has disrupted both daily life and routine medical care, including the treatment of chronic diseases such as hypertension. Given the unknown impact of the pandemic on BP, this study investigated changes in BP during the pandemic among participants in a US employer-sponsored wellness program.
This longitudinal study included employees and their spouses/partners, from all 50 states and the District of Columbia, participating in an annual employer-sponsored wellness program operated by Quest Diagnostics. Participants were required to have BP measured by trained personnel in all 3 years analyzed (2018–2020). The annual BP changes for 2019 versus 2018, January to March 2020 versus 2019, and April to December 2020 versus 2019 were estimated for comparisons between prepandemic (January 2019–March 2020) and pandemic (April–December 2020) periods. Most US jurisdictions put in place COVID-19 stay-at-home orders between mid-March and the start of April 2020, thus establishing prepandemic and pandemic time periods. The mixed model for repeated measures was fitted to assess the adjusted effects of time (pandemic versus prepandemic), sex, and age on changes in BP. Data analyses were performed using SAS Studio 3.6 on SAS version 9.4.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for reporting cross-sectional studies2 and was deemed exempt by the Western Institutional Review Board in accordance with 45 CFR §160 and §164. Inquiries for data and collaboration inquiries may be directed to healthtrends@questdiagnostics.com or to harvey.w.kaufman@questdiagnostics.com.
Of 533 645 potential participants in 2018, after applying data exclusions, 464 585 (87%) study participants remained for evaluation with valid data for each of the 3 calendar years analyzed. The cohort included 53.5% women, with a mean (SD) age of 45.7 (11.1) years in 2018.
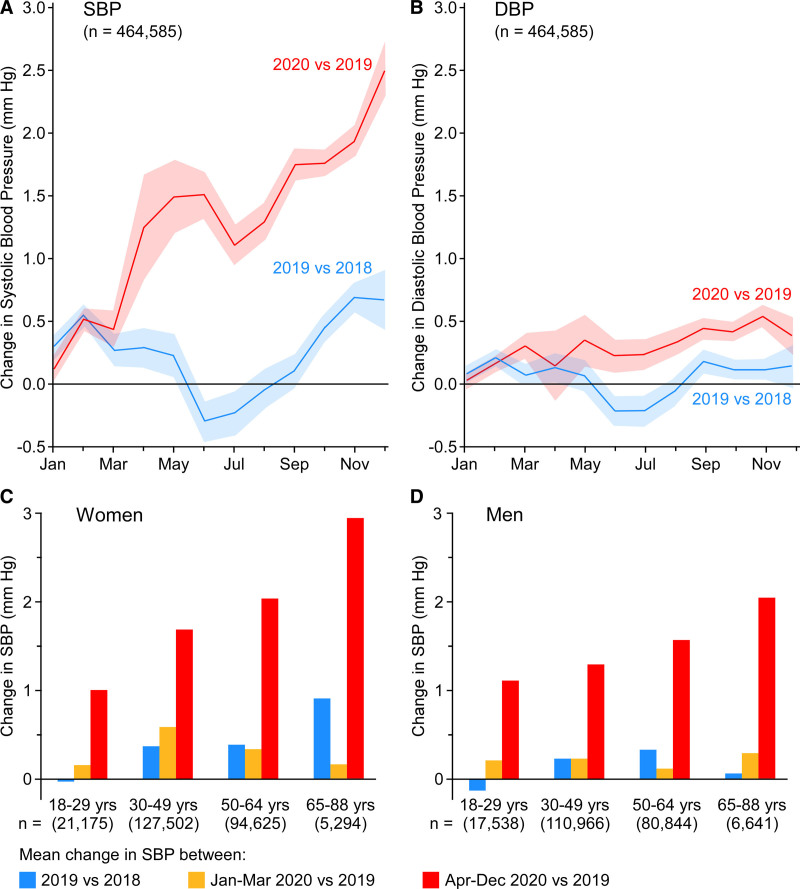
Changes from the preceding year in both systolic and diastolic BP showed no differences between 2019 and January to March 2020 (P=0.8 for systolic and P=0.3 for diastolic BP; Figure). In contrast, annual BP increase was significantly higher in April to December 2020 than 2019 (P<0.0001 for systolic and diastolic BP). During the pandemic period, mean changes each month, compared with the previous year, ranged from 1.10 to 2.50 mm Hg for systolic BP and 0.14 to 0.53 mm Hg for diastolic BP; systolic and diastolic BP increases held true for men and women and across age groups; larger increases were seen in women for both systolic and diastolic BP, in older participants for systolic BP, and in younger participants for diastolic BP (all P<0.0001).
Figure.
Blood pressure changes during the COVID-19 pandemic. Mean changes (with 95% CIs) in systolic and diastolic blood pressure (mm Hg) from the preceding year, by most recent month of participation, among all participants (A and B) and categorized by time period, age group, and sex (C, women; D, men). P<0.0001 for comparisons of annual changes in systolic blood pressure (mm Hg) between 2019/2018 and April to December 2020/2019 (larger), women (larger), and men, younger and older (larger), respectively; estimate of each of time period, sex, and age group in multivariate mixed model while adjusting for the other 2 factors. P=0.8 for comparisons of changes in systolic blood pressure (mm Hg) between 2019/2018 and January to March 2020/2019. P<0.0001 for comparisons of annual changes in diastolic blood pressure (mm Hg) between 2019/2018 and April to December 2020/2019 (larger), women (larger), and men, younger (larger) and older, respectively; estimate of each of time period, sex, and age group in multivariate mixed model while adjusting for the other 2 factors. P=0.3 for comparisons of changes in diastolic blood pressure (mm Hg) between 2019/2018 and January to March 2020/2019.
Participants were next categorized as outlined in the 2017 American BP guidelines (normal, elevated, stage 1 hypertension, and stage 2 hypertension). In the 15-month prepandemic period, compared with the previous year, participant recategorization to a higher versus lower BP category was equivalent (chi-square test, P=0.1; 2019: 24.4% higher/23.6% lower; January–March 2020: 24.9% higher/23.8% lower). In April to December 2020, compared with the prepandemic period, a greater proportion of participants were upcategorized (26.8%) than downcategorized (22.0%; chi-square test, P<0.0001).
Weight gain was not the apparent reason for the observed rise in BP during the pandemic, because an average reduction in weight in men was seen in the pandemic period (–0.2 ± 12.4 lb) and the increase in weight of women (0.6 ± 12.2 lb) was the same as the prepandemic period, in 400 067 (86%) participants with weight data in all 3 years.
Small population-level increases in BP are associated with increased long-term incidence of major adverse cardiovascular events. For example, a 2-mm Hg higher systolic BP is associated with significant increases in mortality from stroke and ischemic heart disease among middle-aged adults.3 Thus, the increase in systolic BP among US adults during the COVID-19 pandemic could signal a forthcoming increase in incident cardiovascular disease mortality. Reasons for pandemic-associated BP elevations are likely multifactorial, and although weight gain was not the reason, other possible reasons could include increased alcohol consumption, less physical activity, emotional stress, and less ongoing medical care (including reduced medication adherence).4 The finding of greater BP increases in women, compared with men, provides more evidence of the outsized burden that pandemics place on women.5 Although the current cohort is large and includes adults, primarily of middle age, from all 50 states, whether it serves as a representative of US adults is unknown.
Continued surveillance of BP among US adults after the pandemic is needed to assess the permanence of the increases noted here. Public health interventions reinforcing the need to address chronic medical problems, even during a pandemic, remain crucial.
Article Information
Acknowledgments
L.J.L. and H.W.K. had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The authors made the following contributions: concept and design, L.J.L., H.W.K., and S.L.H.; acquisition, analysis, or interpretation of data, L.J.L., H.W.K., S.L.H., J.K.N., Z.C., A.R.A., and L.A.B.; drafting of the article, L.J.L. and H.W.K.; critical revision of the article for important intellectual content, all authors; statistical analysis, Z.C., A.R.A., and J.K.N.; and administrative, technical, or material support, H.W.K. and S.L.H.
Sources of Funding
S.L.H. is supported by grant P01 HL147823 from the National Institutes of Health and the Office of Dietary Supplements. The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit the article for publication.
Disclosures
Dr Hazen reports having received royalty payments for inventions or discoveries related to cardiovascular diagnostics or therapeutics from Cleveland Heart Laboratory, a fully owned subsidiary of Quest Diagnostics, and Procter & Gamble. Dr Hazen is a paid consultant for Procter & Gamble and Zehna Therapeutics and has received research funds from Proctor & Gamble, Zehna Therapeutics, Pfizer Inc, and Roche Diagnostics. Dr Laffin is a paid consultant for Medtronic and medical advisor for LucidAct Health. Dr Kaufman, J.K. Niles, Z. Chen, Dr Bare, and A.R. Arellano are employees of Quest Diagnostics, and Dr Kaufman, Z. Chen, Dr Bare, and A.R. Arellano own stock in Quest Diagnostics.
Footnotes
L.J. Laffin and H.W. Kaufman contributed equally.
For Sources of Funding and Disclosures, see page 237.
Contributor Information
Harvey W. Kaufman, Email: harvey.w.kaufman@questdiagnostics.com.
Zhen Chen, Email: Zhen.X.Chen@questdiagnostics.com.
Justin K. Niles, Email: Justin.K.Niles@questdiagnostics.com.
Andre R. Arellano, Email: Andre.R.Arellano@questdiagnostics.com.
Lance A. Bare, Email: lance.a.bare@questdiagnostics.com.
Stanley L. Hazen, Email: hazens@ccf.org.
References
- 1.Adams JM, Wright JS. A national commitment to improve the care of patients with hypertension in the US. JAMA. 2020;324:1825–1826. doi: 10.1001/jama.2020.20356 [DOI] [PubMed] [Google Scholar]
- 2.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8 [DOI] [PubMed] [Google Scholar]
- 4.Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wenham C, Smith J, Davies SE, Feng H, Grépin KA, Harman S, Herten-Crabb A, Morgan R. Women are most affected by pandemics - lessons from past outbreaks. Nature. 2020;583:194–198. doi: 10.1038/d41586-020-02006-z [DOI] [PubMed] [Google Scholar]