Abstract
Objective:
To measure the forces delivered by thermoplastic appliances made from three materials and investigate effects of mechanical properties, material thickness, and amount of activation on orthodontic forces.
Materials and Methods:
Three thermoplastic materials, Duran (Scheu Dental), Erkodur (Erkodent Erich Kopp GmbH), and Hardcast (Scheu Dental), with two different thicknesses were selected. Values of elastic modulus and hardness were obtained from nanoindentation measurements at 28°C. A custom-fabricated system with a force sensor was employed to obtain measurements of in vitro force delivered by the thermoplastic appliances for 0.5-mm and 1.0-mm activation for bodily tooth movement. Experimental results were subjected to several statistical analyses.
Results:
Hardcast had significantly lower elastic modulus and hardness than Duran and Erkodur, whose properties were not significantly different. Appliances fabricated from thicker material (0.75 mm or 0.8 mm) always produced significantly greater force than those fabricated from thinner material (0.4 mm or 0.5 mm). Appliances with 1.0-mm activation produced significantly lower force than those with 0.5-mm activation, except for 0.4-mm thick Hardcast appliances. A strong correlation was found between mechanical properties of the thermoplastic materials and force produced by the appliances.
Conclusions:
Orthodontic forces delivered by thermoplastic appliances depend on the material, thickness, and amount of activation. Mechanical properties of the polymers obtained by nanoindentation testing are predictive of force delivery by these appliances.
Keywords: Thermoplastic appliances, Esthetic appliances, Orthodontic force, Nanoindentation testing, Polymer mechanical properties
INTRODUCTION
Improved esthetic orthodontic appliances, especially for adult patients, are highly desirable to alternative conventional fixed appliances. Various esthetic brackets and wires have been developed for clinical orthodontics.1,2 Recently, transparent thermoplastic removable appliances have been introduced, such as Invisalign, ClearSmile, and Clear Aligner, which are used sequentially by patients and are made from CAD/CAM technology or a stepwise setup model.3–5 Jeremiah et al.6 investigated the social perceptions of young adults wearing orthodontic appliances and reported that such thermoplastic appliances tended to be more attractive than conventional fixed appliances.
Recent clinical studies have investigated the treatment results for thermoplastic appliances.7–10 Djeu et al.7 compared results from the Invisalign and conventional fixed appliances, using an objective grading system (OGS), and found that cases treated with the Invisalign appliance showed lower OGS passing rate than cases treated with conventional fixed appliances. Kuncio et al.8 investigated postretention dental changes and reported that cases treated with thermoplastic appliances relapsed more than those treated with conventional fixed appliances. Baldwin et al.9 investigated the teeth adjacent to premolar extraction spaces during space closure with thermoplastic appliances and reported that treatment with thermoplastic appliances resulted in significant tipping of the teeth adjacent to premolar extraction sites. Some patients can be treated with thermoplastic appliances alone; however, in many cases, these appliances must be modified, or used with auxiliaries or fixed appliances.7,8 Thermoplastic appliances may be not recommended for treatment of extraction cases, uprighting severely tipped teeth, severe deep bites, and more extensive anteroposterior corrections.7
Only a few studies have investigated the force delivery properties of thermoplastic appliances.5,11–13 Barbagallo et al.5 investigated the force imparted by thermoplastic appliances to maxillary first premolars in vivo using a pressure film approach. A German research group has quantitatively investigated the force delivery properties of thermoplastic appliances during tipping and intrusive forces, and reported the effects from different materials and their thickness.11–13 In order to expand the clinical indications of thermoplastic appliances, it is important to understand the relevance of the orthodontic forces from these appliances, as well as the mechanical properties such as hardness and elastic modulus of the materials used in their fabrication. Little is presently known about the orthodontic forces and mechanical properties of thermoplastic materials. Only one recent study14 investigated the relevant force delivery properties and mechanical properties of thermoplastic materials, utilizing a three-point bending test and Vickers hardness measurement. The purpose of this in vitro study was to measure the forces delivered by thermoplastic appliances made from three different materials and to investigate the factors, such as the mechanical properties (hardness and elastic modulus), thickness of the thermoplastic materials, and amounts of activation affecting the orthodontic forces produced by the appliances. It was hypothesized that the mechanical properties of the thermoplastic materials affect the orthodontic forces.
MATERIALS AND METHODS
Materials
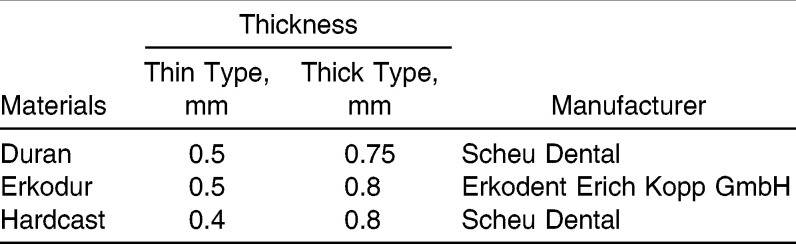
Three thermoplastic materials, Duran (Scheu Dental, Iserlohn, Germany), Erkodur (Erkodent Erich Kopp GmbH, Pfalzgrafenweiler, Germany), and Hardcast (Scheu Dental), with two different thicknesses were selected for this study (Table 1).
Table 1.
Thermoplastic Materials Used in the Present Study
Nanoindentation Test
Approximately 1 cm2 specimens were carefully cut from the thermoplastic materials, using a water-cooled diamond-saw (Isomet 11-1280, Buehler, Lake Bluff, Ill), and fixed on the specimen stage with adhesive resin (Superbond Orthomite, Sun Medical, Shiga, Japan). All nanoindentation testing (ENT-1100a, Elionix, Tokyo, Japan) was carried out at 28°C with a peak load of 10 mN using a Berkovich indenter.15–17 Each test consisted of three parts: 10 seconds for loading to the peak value, 1 second of holding at the peak load, and 10 seconds for unloading. Ten indentations were made for each material. Linear extrapolation methods (ISO Standard 14577) were used for the unloading curve between 95% and 70% of the maximum test force to calculate the elastic modulus.18 The hardness and elastic modulus were calculated using software available with the nanoindentation apparatus.
Measurement of Orthodontic Force
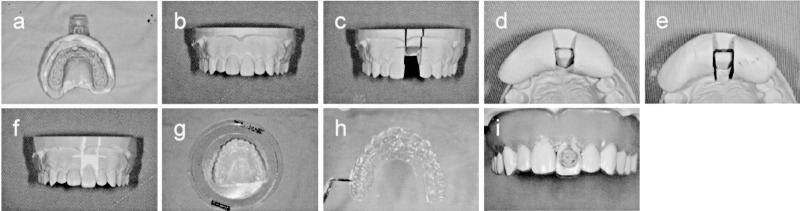
The in vitro force-measuring system consisted of a custom-made epoxy model with a small force sensor (PS-20KC, Kyowa, Tokyo, Japan) embedded in the left maxillary central incisor on the same level with the labial surface (Figure 1) and a sensor interface (PCD-300A, Kyowa), which was described in detail recently.19 An impression of the maxillary teeth was taken using a silicone rubber impression material (Dent Silicone V, Shofu, Kyoto, Japan) (Figure 2a). The casts were poured immediately with a vacuum-spatulated high-quality dental stone and allowed to dry overnight (Figure 2b). This model was trimmed to a height of 25 mm parallel to the occlusal plane, and two identical dental plaster copies of the model were made using a silicone rubber impression material (Duplicone, Shofu). To make the setup model, the left maxillary central incisor was dissected with a diamond disk (Figure 2c). The amounts of activation (0.5 mm or 1.0 mm) for bodily movement were adjusted using the silicone rubber impression material and spacers (small pieces of the thermoplastic materials with 0.5-mm and 1.0-mm thickness) placed between labial surface of the impression and dissected central incisor, attached to the impression with glue (Figure 2d,e), and finally fixed with high-quality dental stone (Figure 2f). Using a pressure-molding machine (BIOSTAR, Scheu Dental), 10 thermoplastic appliances of three different materials with two different thicknesses were carefully made (Figure 2g,h). Measurements were carried out at room temperature (25°C) in the dry condition after the sensitivity of the sensor was calibrated (Figure 2i) and repeated five times for each thermoplastic appliance. The force was stable within 5 seconds, and the average force between 10 and 20 seconds was considered in this study.
Figure 1.
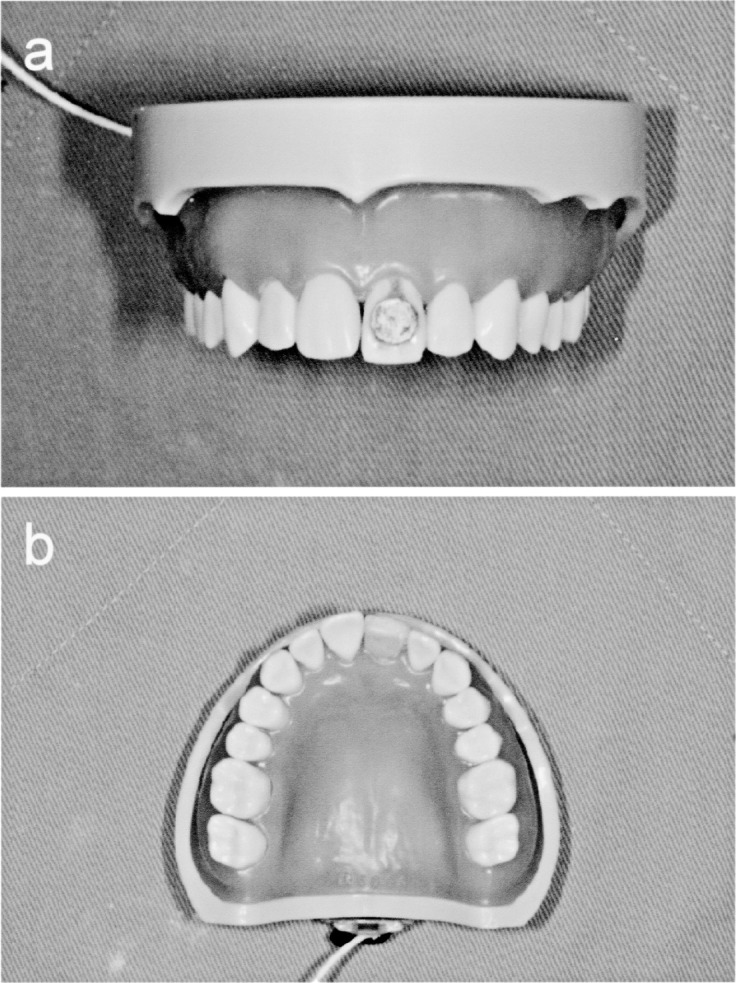
Custom-made epoxy model with small force sensor at left maxillary central incisor: (a) frontal view; (b) occlusal view.
Figure 2.
Fabrication of setup model and thermoplastic appliance for measuring orthodontic force. (a) Impression of maxillary teeth by silicone rubber impression material. (b) Trimmed cast made from high-quality stone. (c) Left maxillary central incisor dissected with diamond disk. (d and f) Adjusted activation (0.5 mm or 1.0 mm) using silicone rubber impression material and fixed with high-quality stone. (g and h) Thermoplastic appliance made with pressure-molding machine. (i) Placement of thermoplastic appliance.
Statistical Analysis
The experimental results were analyzed using SPSS Statistics software (version 19.0J for Windows, IBM, Armonk, NY). The mean hardness and elastic modulus obtained from each thermoplastic appliance, along with the standard deviation, were compared by one-way analysis of variance (ANOVA), followed by the Tukey-Kramer honestly significant difference (HSD) test with a significance level of 5%. The forces obtained from each thermoplastic material were compared by one-way (materials) and two-way (material thickness and amount of activation) ANOVA. Post-hoc multiple comparisons were made by the Tukey-Kramer HSD test, with a significance level of 5%. Additionally, Student's t-test, with a significance level of 5%, was used to examine two different thicknesses and for two different activations for each material. The relationships among mechanical properties (hardness, elastic modulus) and force for the thermoplastic appliances were investigated by the Pearson correlation coefficient test.
RESULTS
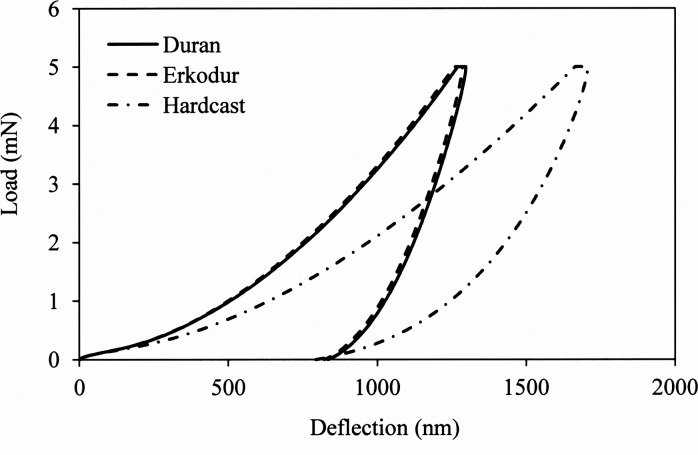
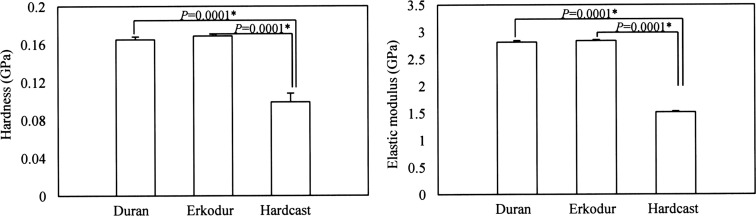
Representative loading-unloading curves for the three thermoplastic materials are shown in Figure 3, and the mean values of hardness and elastic modulus with standard deviations are shown in Figure 4. Based on the results of one-way ANOVA, significant differences in hardness (P = .0001) and elastic modulus (P = .00001) were found among the three specimens groups. Hardcast showed a significantly lower mean hardness (0.099 GPa) and elastic modulus (1.517 GPa) than the other two thermoplastic materials (Duran: 0.165 GPa for hardness, 2.811 GPa for elastic modulus; Erkodur: 0.169 GPa for hardness, 2.835 GPa for elastic modulus). There were no significant differences in hardness and elastic modulus for Duran and Erkodur.
Figure 3.
Representative loading-unloading curves for three thermoplastic materials: Duran, continuous line; Erkodur, dashed line; and Hardcast, dashed-dotted line.
Figure 4.
Mean hardness and elastic modulus for thermoplastic appliances with standard deviations. Comparisons are presented for each material. Left side, Duran; middle, Erkodur; and right side, Hardcast. * P < .05 by Tukey test. Hardcast showed significantly lower hardness and elastic modulus than the other two thermoplastic materials.
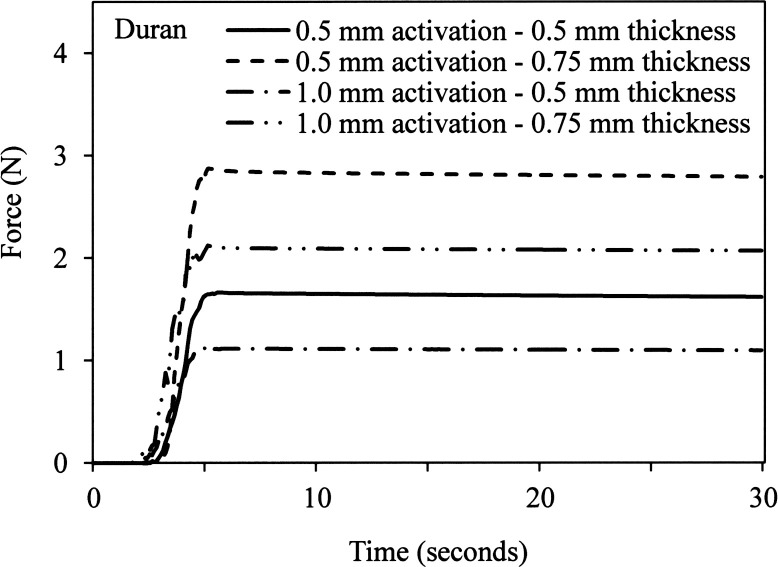
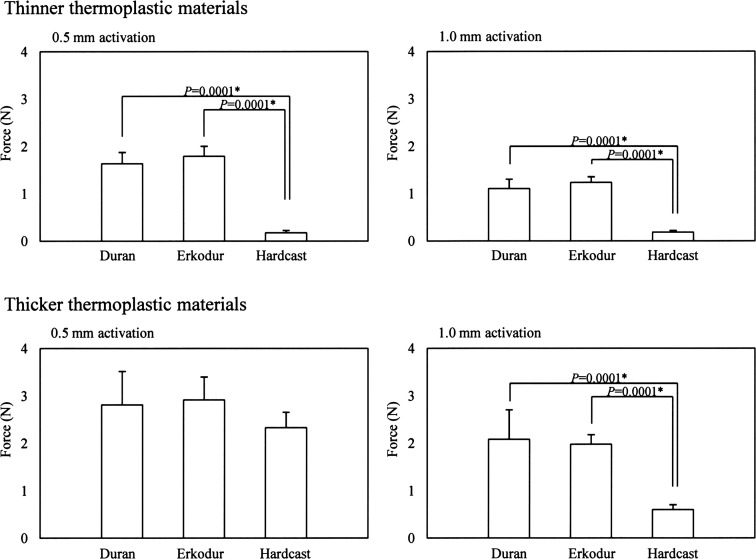
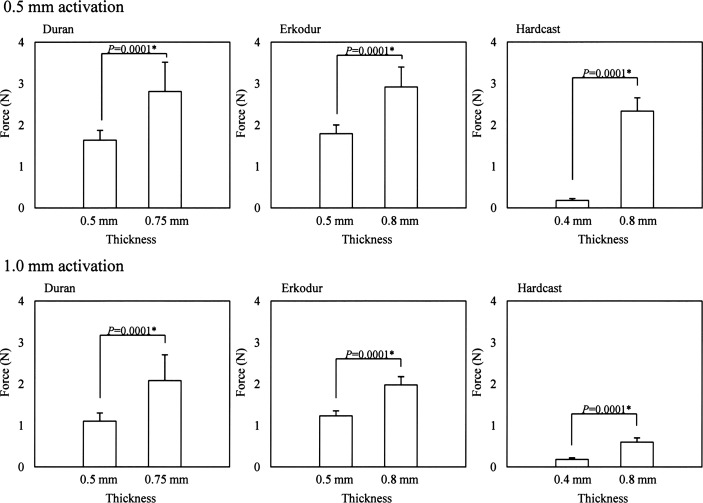
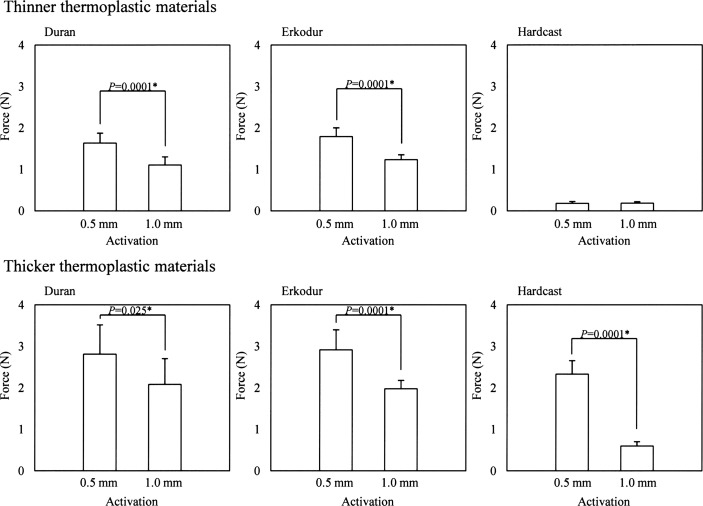
Representative measurements of orthodontic force obtained with the Duran thermoplastic appliances are shown in Figure 5, and the mean forces and standard deviations for the three thermoplastic appliances are compared for three different materials, two different thicknesses of the materials, and two different activations in Figures 6, 7, and 8, respectively. Hardcast showed a significantly lower orthodontic force than the other two thermoplastic materials (Duran and Erkodur) in all conditions except an activation of 0.5 mm (Figure 5). Two-way ANOVA showed that the material thickness (P = .0001) and amount of activation (P = .0001) were statistically significant factors. For each of the three thermoplastic materials, appliances fabricated from the thicker material showed significantly greater orthodontic force than those fabricated from the thinner material. Moreover, for all three thermoplastic materials, appliances with the greater amount of activation showed significantly lower orthodontic force than those with the smaller amount of activation, except for appliances made with the thinner (0.4-mm thick) Hardcast material.
Figure 5.
Representative results for measuring orthodontic force obtained from Duran thermoplastic appliances: 0.5-mm thickness and 0.5-mm activation, continuous line; 0.75-mm thickness and 0.5-mm activation, dashed line; 0.5-mm thickness and 1.0-mm activation, dashed-dotted line; and 0.75-mm thickness and 1.0-mm activation, double-dotted line.
Figure 6.
Mean forces from thermoplastic appliances with standard deviations. Comparisons are presented for each material at two different thicknesses. Left side shows results for activation of 0.5 mm; right side shows results for activation of 1.0 mm. Left bar, Duran; middle bar, Erkodur; and right bar, Hardcast. * P < .05 by Tukey test. Hardcast showed significantly lower orthodontic force than the other two thermoplastic materials.
Figure 7.
Mean forces from thermoplastic appliances with standard deviations. Comparisons are presented for each material at two different thicknesses. Upper row shows results for 0.5-mm activation; lower row shows results for 1.0-mm activation (Table 1). * P < .05 by Student's t-test. Appliances fabricated from thicker materials delivered greater forces.
Figure 8.
Mean forces from thermoplastic appliances with standard deviations. Comparisons are presented for each material at two different activations. Upper row shows results for thinner thermoplastic materials; lower row shows results for thicker thermoplastic materials (Table 1). Left side, Duran; middle, Erkodur; and right side, Hardcast. * P < .05 by Student's t-test. Appliances receiving greater activation generally delivered lower forces.
DISCUSSION
A previous systematic review article20 showed that human studies dealing with the relation between force magnitude and rate of tooth movement used various initial forces (18–1500 cN) and that there is no evidence-based force level for the optimal efficiency in clinical orthodontics. In the present study, the orthodontic force magnitudes produced by the thermoplastic appliances ranged from 0.18–2.91 N, which are of a similar level to those reported in a study21 of the in vitro force from nickel-titanium orthodontic wires (0–4.1 N). On the other hand, a recent study10 investigating the initial force from thermoplastic appliances reported a mean value of 5.1 N for an activation of 0.5 mm, using the Erkodur material with 0.8-mm thickness; this value is higher than that obtained (2.91 N) in the present study for the same material. However, it is difficult to compare these values because our study attempted to investigate the force exerted by supposedly bodily tooth movement, although the mode of tooth movement in the referenced study was tipping movement.
In the present study, Duran and Erkodur showed similar mechanical properties, and Hardcast showed significantly lower mean hardness and elastic modulus. A strong correlation (P < .0001) was observed between the hardness (r = 0.654) and elastic modulus (r = 0.642) values for orthodontic force produced by thermoplastic appliances fabricated from the three materials, suggesting that nanoindentation testing is a worthwhile method for evaluating materials used to fabricate thermoplastic appliances and that the test results may enable prediction of the resulting orthodontic force.
In the present study, the thickness of the materials had a highly significant influence on the forces delivered by the thermoplastic appliances, and this trend is in agreement with a recent finding from another study.11 The two amounts of activation (0.5 mm and 1.0 mm) for bodily tooth movement used in the present study were in accordance with recent publications on the Clear Aligner4 and ClearSmile5 materials.
In general, two types of thermoforming procedures are employed for these materials—vacuum and high-pressure—and it was previously found that high-pressure thermoformed appliances deliver significantly higher forces than those produced by vacuum forming because of better fitting.12 In the present study, most appliances with greater amount of activation showed significantly lower orthodontic force than those produced by the appliances with smaller amount of activation, except for the appliances made by Hardcast with 0.4-mm thickness. High-pressure thermoforming was used for making all of the appliances in this study, and it is plausible that some permanent deformation occurred during the fabrication process. Otherwise, it may be considered that permanent deformation was introduced when the thermoplastic appliance was worn on the custom-made epoxy model. This is an area for further investigation.
Recent in vitro studies11–13 measuring the force produced by thermoplastic appliances, as well as the present study, have not simulated the effect of the periodontal ligament that occurs in vivo. Moreover, while Ryokawa et al.22 found that water sorption of the thermoplastic materials increased with time in a simulated intraoral environment, the extent of this behavior is unknown for true in vivo conditions. In addition, Vardimon et al.23 investigated in vivo von Mises (IVM) strains during Invisalign treatment and found that peak IVM strains developed on the first day after intraoral placement and decreased on the second day and maintained a plateau thereafter to the 15th day; consequently, most tooth movement occurred during the first 24 hours. Since degradation of the polymer molecular structure by water sorption is well known to occur in the oral environment, the actual orthodontic forces delivered by the thermoplastic appliances may clinically decrease with time.14,22,23 Further research is necessary to elucidate the changes after clinical use of these thermoplastic appliances, which involve degradation of the mechanical properties and alteration of their molecular structure. Studies are in progress to obtain this information, utilizing nanoindentation testing15–17 and differential scanning calorimetry.24 Additional information about the structure of these thermoplastic polymers can be acquired by Fourier transform infrared spectroscopy.
CONCLUSIONS
Under the conditions of this study:
The orthodontic force by thermoplastic appliances has strong correlation with the hardness and elastic modulus of the materials.
The thickness of the materials had a highly significant influence on the forces delivered by thermoplastic appliances, with appliances fabricated from thicker materials delivering greater forces.
The amount of activation also affected the forces delivered by the thermoplastic appliances, with appliances receiving greater activation generally delivering lower forces. The one exception was the 0.4-mm thick Hardcast appliances.
REFERENCES
- 1.Eliades T, Eliades G, Brantley WA. Orthodontic brackets. In: Brantley WA, Eliades T, editors. Orthodontic Materials Scientific and Clinical Aspects. Stuttgart, Germany: Thieme; 2001. pp. 143–172. [Google Scholar]
- 2.Iijima M, Muguruma T, Brantley W, Choe HC, Nakagaki S, Alapati SB, Mizoguchi I. Effect of coating on properties of esthetic orthodontic nickel-titanium wires. Angle Orthod. 2012;82:319–325. doi: 10.2319/021511-112.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyd R, Miller RJ, Vlaskalic V. The Invisalign system in adult orthodontics: mild crowding and space closure cases. J Clin Orthod. 2000;34:13–15. [Google Scholar]
- 4.Kim TW, Echarri P. Clear aligner: an efficient, esthetic, and comfortable option for an adult patient. World J Orthod. 2007;8:13–18. [PubMed] [Google Scholar]
- 5.Barbagallo LJ, Shen G, Jones AS, Swain V, Petocz P, Darendeliler MA. A novel pressure film approach for determining the force imparted by clear removable thermoplastic appliances. Ann Biomed Eng. 2008;36:335–341. doi: 10.1007/s10439-007-9424-5. [DOI] [PubMed] [Google Scholar]
- 6.Jeremiah HG, Bister D, Newton JT. Social perceptions of adults wearing orthodontic appliances: a cross-sectional study. Eur J Orthod. 2011;33:476–482. doi: 10.1093/ejo/cjq069. [DOI] [PubMed] [Google Scholar]
- 7.Djeu G, Shelton C, Maganzini A. Outcome assessment of Invisalign and traditional orthodontic treatment compared with the American Board of Orthodontics objective grading system. Am J Orthod Dentofacial Orthop. 2005;128:292–298. doi: 10.1016/j.ajodo.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Kuncio D, Maganzini A, Shelton C, Freeman K. Invisalign and traditional orthodontic treatment postretention outcome compared using the American Board of Orthodontics objective grading system. Angle Orthod. 2007;77:864–869. doi: 10.2319/100106-398.1. [DOI] [PubMed] [Google Scholar]
- 9.Baldwin DK, King G, Ramsay DS, Huang G, Bollen AM. Activation time and material stiffness of sequential removable orthodontic appliances. Part 3: Premolar extraction patients. Am J Orthod Dentofacial Orthop. 2008;133:837–845. doi: 10.1016/j.ajodo.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 10.Kravitz ND, Kusnoto B, BeGole E, Obrez A, Agran B. How well does Invisalign work? A prospective clinical study evaluating the efficacy of tooth movement with Invisalign. Am J Orthod Dentofacial Orthop. 2009;135:27–35. doi: 10.1016/j.ajodo.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 11.Hahn W, Dathe H, Fialka-Fricke J, Fricke-Zech S, Zapf A, Kubein-Meesenburg D, Sadat-Khonsari R. Influence of thermoplastic appliance thickness on the magnitude of force delivered to a maxillary central incisor during tipping. Am J Orthod Dentofacial Orthop. 2009;136:12.e1–e7. doi: 10.1016/j.ajodo.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Hahn W, Fialka-Fricke J, Dathe H, Fricke-Zech S, Zapf A, Gruber R, Kubein-Meesenburg D, Sadat-Khonsari R. Initial forces generated by three types of thermoplastic appliances on an upper central incisor during tipping. Eur J Orthod. 2009;31:625–631. doi: 10.1093/ejo/cjp047. [DOI] [PubMed] [Google Scholar]
- 13.Hahn W, Engelke B, Jung K, Dathe H, Fialka-Fricke J, Kubein-Meesenburg D, Sadat-Khonsari R. Initial forces and moments delivered by removable thermoplastic appliances during rotation of an upper central incisor. Angle Orthod. 2010;80:239–246. doi: 10.2319/033009-181.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kwon JS, Lee YK, Lim BS, Lim YK. Force delivery properties of thermoplastic orthodontic materials. Am J Orthod Dentofacial Orthop. 2008;133:228–234. doi: 10.1016/j.ajodo.2006.03.034. [DOI] [PubMed] [Google Scholar]
- 15.Pharr GM, Oliver WC. Nanoindentation of silver-relations between hardness and dislocation structure. J Mater Res. 1989;4:94–101. [Google Scholar]
- 16.Oliver WC, Pharr GM. An improved technique for determining hardness and elastic modulus using load and displacement sensing indentation experiments. J Mater Res. 1992;7:1564–1583. [Google Scholar]
- 17.Iijima M, Muguruma T, Brantley WA, Mizoguchi I. Comparisons of nanoindentation, 3-point bending, and tension tests for orthodontic wires. Am J Orthod Dentofacial Orthop. 2011;140:65–71. doi: 10.1016/j.ajodo.2009.11.015. [DOI] [PubMed] [Google Scholar]
- 18.ISO 14577-1 Metallic Materials—Instrumented Indentation Test for Hardness and Materials Parameters—Part 1: Test Method. 1st ed. 2002 International Organization for Standardization; [Google Scholar]
- 19.Muguruma T, Yasuda Y, Iijima M, Kohda N, Mizoguchi I. Force and amount of resin composite paste used in direct and indirect bonding. Angle Orthod. 2010;80:1089–1094. doi: 10.2319/031910-41.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ren Y, Maltha JC, Kuijpers-Jagtman AM. Optimum force magnitude for orthodontic tooth movement: a systematic literature review. Angle Orthod. 2003;73:86–92. doi: 10.1043/0003-3219(2003)073<0086:OFMFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Iijima M, Ohno H, Kawashima I, Endo K, Mizoguchi I. Mechanical behavior at different temperatures and stresses for superelastic nickel-titanium orthodontic wires having different transformation temperatures. Dent Mater. 2002;18:88–93. doi: 10.1016/s0109-5641(01)00025-2. [DOI] [PubMed] [Google Scholar]
- 22.Ryokawa H, Miyazaki Y, Fujishima A, Miyazaki T, Maki K. The mechanical properties of dental thermoplastic materials in a simulated intraoral environment. Orthodontic Waves. 2006;65:64–72. [Google Scholar]
- 23.Vardimon AD, Robbins D, Brosh T. In-vivo von Mises strains during Invisalign treatment. Am J Orthod Dentofacial Orthop. 2010;138:399–409. doi: 10.1016/j.ajodo.2008.11.027. [DOI] [PubMed] [Google Scholar]
- 24.Brown ME. Differential thermal analysis (DTA) and differential scanning calorimetry (DSC) In: Brown ME, editor. Introduction to Thermal Analysis Techniques and Applications 2nd ed. Dordrecht, Netherlands: Kluwer Academic Publishers; 2001. pp. 55–90. [Google Scholar]