Abstract
Objective:
To examine skeletal, dental, and soft tissue effects of the Miniscrew Implant Supported Distalization System (MISDS) and the Bone-Anchored Pendulum Appliance (BAPA).
Materials and Methods:
Among 28 patients displaying Angle Class II malocclusion, 14 patients with a mean age of 14.8 ± 3.6 years treated with MISDS were included in the first group, and 14 patients with a mean age of 14.5 ± 1.5 years treated with BAPA were included in the second group. The pretreatment and posttreatment lateral cephalograms were analyzed. Statistical evaluation was carried out using the paired Shapiro-Wilk test, the paired-sample t-test, and the unpaired t-test.
Results:
Upper posterior teeth were distalized successfully in both groups. Nearly bodily distalization was seen in the MISDS group, whereas significant distal tipping of the upper first molars was observed in the BAPA group (P < .001). There were no statistically significant changes in the sagittal position of the maxilla and mandible and in the position of the upper incisors as a result of treatment in either group.
Conclusions:
Both methods provided absolute anchorage for distalization of posterior teeth; however, almost translatory distal movement was encountered in the MISDS group, and substantial distal tipping of the maxillary molars accompanied distalization in the BAPA group.
Keywords: Distalization, Miniscrews, Class II, Intraoral distalization appliances
INTRODUCTION
Distalization of the maxillary molars can be achieved either extraorally or intraorally. Intraoral distalization appliances typically do not require patient cooperation, but they may have undesired side effects.1–8 Because these appliances usually derive their anchorage from maxillary premolars, mesialization of premolars and protrusion of incisors accompany maxillary molar distalization. In order to eliminate anchorage loss and maximize anchorage, these appliances can be used with implant anchorage. Recently, an ever-increasing number of reports9–19 regarding implant-supported distalization systems have been introduced in the literature. They usually derive their anchorage from orthodontic screws placed in the anterior palate. Accordingly, Kircelli et al.,13 Escobar et al.,15 Onçağ et al.,16 and Polat-Ozsoy et al.17 used pendulum appliances supported with two miniscrews placed in the anterior palate for molar distalization.
Papadopoulos20 introduced the Miniscrew Implant Supported Distalization System (MISDS) in 2008. The anchorage unit of this appliance comprised two miniscrew implants in the paramedian region of the palate. The distalization force was applied by the palatally positioned open nickel-titanium coil springs, which pass through the center of resistance of the maxillary molars. Squeezing the coil springs and screwing the anteriorly positioned stop screws following cementation activate the appliance.
Some unwanted side effects might occur with implant-supported molar distalization appliances, such as distal crown tipping accompanying molar distalization. The point of force application passes below the center of resistance of the maxillary molars in pendulum appliances, whereas it passes through the center of resistance in MISDS, which might cause clinically significant differences in the overall distalization procedure.
In this study, we compared the skeletal, dentoalveolar, and soft tissue effects of two implant-supported distalization systems—the MISDS and the Bone-Anchored Pendulum Appliance (BAPA)—for maxillary molar distalization and evaluated the efficacy of two distalizing forces, one from the apex level and the other from the crown level of the maxillary molars.
MATERIALS AND METHODS
This study was approved by the Baskent University Insitutional Review Board. The power analysis revealed that a total sample size of 24 (12 per group) was needed to detect clinically meaningful differences between the groups at a power of 85% and at the .05 significance level. Sample size estimation was performed using NCSS and PASS software (Number Cruncher Statistical Systems, Version 2000; Kaysville, Utah).
The study consisted of 28 patients and was ethically approved by the Başkent University Research and Ethical Committee for all orthodontic, cephalometric, and surgical stages. The inclusion criteria for the study are shown below:
Skeletal Class I or Class II, dental Class II (half-unit) molar relationship;
All permanent teeth present and erupted except for the third molars;
Absence of supernumerary teeth;
Crowding in the upper dental arch and/or increased overjet;
Minimal or no crowding in the lower dental arch; and
Presence of high-quality and standard lateral cephalometric radiographs.
Exclusion criteria included past orthodontic treatment, severe caries lesions, poor oral hygiene, increased vertical growth pattern, and poor quality of cephalometric radiographs.
The study was conducted on 56 lateral cephalometric radiographs obtained from 28 patients. All patients and parents were informed about the surgical and orthodontic procedures that would be applied throughout the study and signed a consent form after they received detailed information about the planned clinical trial. Two intermaxillary fixation (IMF) screws (Stryker, Leibinger, Germany) were used as skeletal anchorage. The screws measured 2.0 mm in diameter and 8 mm in length. In each group, IMF screws were placed in the anterior paramedian region of the midpalatal suture, 4–5 mm posterior to the foramen incisivum and 3–4 mm lateral to the median line. Following insertion of the screws, impressions were taken, and stone model casts were obtained with the screws. Appliances were constructed on the model casts.
The first group was designed prospectively of 14 patients (eight girls, six boys; mean age: 14.8 years) who were suitable candidates for maxillary molar distalization, met the inclusion criteria, and were consecutively included in this group. The MISDS appliance described by Papadopoulos20 was used for distalization of the upper molars for patients in this group. A bihelix palatal appliance with two loops at the anterior part was bent with 0.036-inch wire, and 0.045-inch tubes were soldered onto the palatal side of the maxillary molar bands. After placement of the miniscrews, the MISDS was cemented with multicure glass ionomer cement (3M Unitek, Monrovia, Calif), and the loops of the appliance were inserted on the heads of the miniscrews. A 0.036-inch wire passed through the tubes; it was crucial that the wire passed parallel to the occlusal plane. The appliance was connected and fixed to the miniscrews with the help of metallic ligatures. Activation of MISDS was performed by squeezing the open coil springs and screwing the anteriorly positioned stop screws, which produced an average distalization force of 230 g, as measured by a force gauge. The patients were scheduled for visits every 4 weeks, and the force was activated if needed.
The first group was compared with the second group (nine girls, five boys; mean age: 14.5 years), selected retrospectively among 22 patients who had been treated with a BAPA at the Başkent University Faculty of Dentistry Department of Orthodontics between the years 2005 and 2007. The records of these 22 patients had also been used in another study.17 Eight patients within this group who failed to meet the inclusion criteria (three patients with poor-quality or nonstandard radiographs; five patients who did not match for gender, age, or skeletal characteristics) for this study were excluded. The remaining 14 patients composed the second group.
In this group, screw heads were blocked out on a stone cast and the pendulum appliance was constructed as described by Hilgers,21 excluding the occlusal rests on the premolars. Before placement and cementation of the appliance, 0.032-inch TMA springs (TMA; Ormco, Glendora, Calif) were bent 70° posteriorly for activation. The force applied was approximately 230 g, which was identical to that applied in the first group.
One week following screw insertion and after checking the stability of the screws, the acrylic part of the appliance was cemented to the screw heads with cold-cure, methyl methacrylate free acrylic resin (Ufi Gel Hard; Voco GmbH, Cuxhaven, Germany). At the same time the molar bands were cemented with multicure glass ionomer cement (3M Unitek). The springs were placed into the lingual sheaths of the molar bands, and 230 g of force was applied. Accordingly, the patients were instructed to maintain good oral hygiene and were scheduled for visits once per month. The activation of the springs was checked during these appointments. If reactivation was needed, the springs were removed from the sheaths and reactivated in the mouth.
Both the BAPA and MISDS appliances were applied by the authors of the study in the same clinic. Lateral cephalograms were taken on the day of the insertion of the appliance (T0) and immediately after the distalization was achieved (T1) with a Planmeca Cephalometer (PM2002EC; Proline, Helsinki, Finland). The distalization was continued until Class II molar relationship was corrected to a super–Class I molar relationship in both groups. The appliances were then left in place for retention. All cephalograms were hand-traced on orthodontic tracing paper on a conventional sight box using 0.3-mm lead pencil and were measured by the same investigator. For measurements on the radiographs, the horizontal reference plane was constructed with a 7° angle to the sella-nasion plane, and the vertical reference plane was constructed perpendicular to the horizontal reference plane at the Sella point. The cephalometric analysis involved 21 landmarks (Figure 1).
Figure 1.
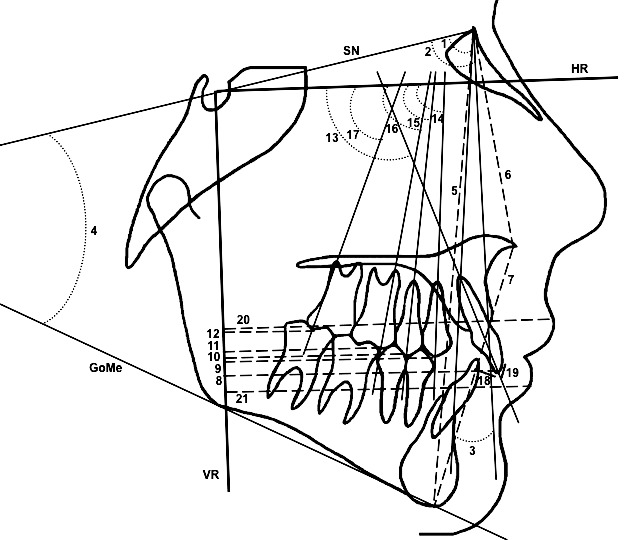
Cephalometric measurements used in the study: 1: SNA, °; 2: SNB, °; 3: ANB, °; 4: SN/GoMe, °; 5: N-Me, mm; 6: N-ANS, mm; 7: ANS-Me, mm; 8: U1-VR, mm; 9: U4-VR, mm; 10: U5-VR, mm; 11: U6-VR, mm; 12: U7-VR, mm; 13: U1/HR, °; 14: U4/HR, °; 15: U5/HR, °; 16: U6/HR, ° 17: U7/HR, °; 18: Overjet, mm; 19: Overbite, mm; 20: ULip-VR, mm; and 21: LLip-VR, mm.
Statistical Analysis
Data analysis was performed using SPSS for Windows, version 11.5 (SPSS Inc, Chicago, Ill). The Shapiro-Wilk test was used to check whether the continuous variables were normally distributed. Data were shown as mean ± standard deviation for continuous variables. The mean differences between pre- and postdistalization measurements were analyzed by Bonferroni-adjusted, paired-sample t-test, and a P-value of <.025 was considered statistically significant. The mean differences between groups were compared by unpaired t-test, and a P-value of <.05 was considered statistically significant.
Method Error
Three weeks after the first measurements, 20 lateral cephalometric films from 10 randomly selected patients were analyzed, and the measurements were repeated by the same examiner. Intraclass correlation coefficients (r) were calculated on pretreatment and posttreatment cephalometric films for evaluation of reliability. Confidence intervals of 95% were considered statistically reliable, and the r values calculated for each variable ranged between the limits of 0.950 and 1.000. In addition to the correlation coefficients, Dahlberg's formula was used for the assessment of random error, and the measurement error was between 0.112 and 0.274.
RESULTS
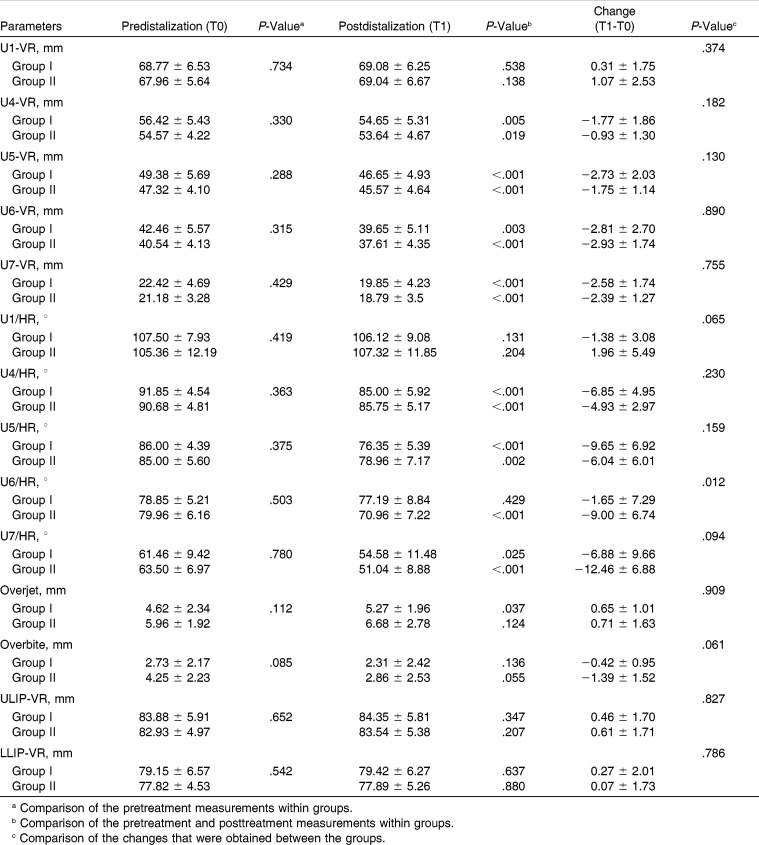
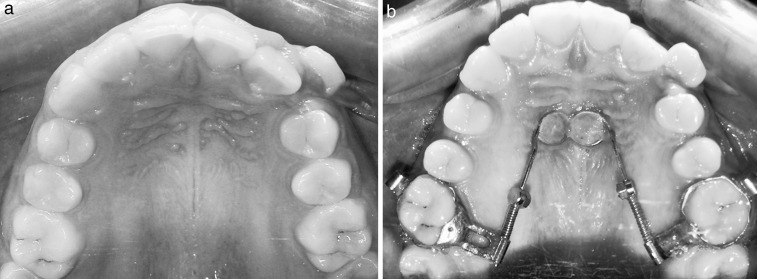
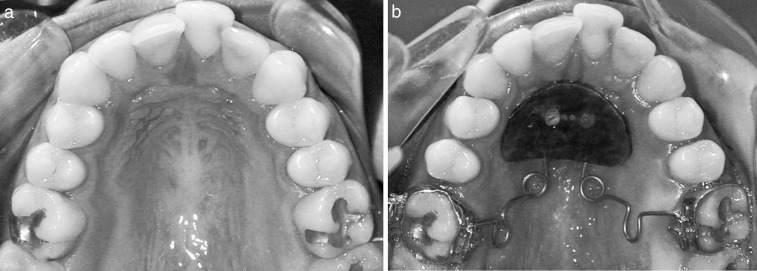
There were no significant differences for all parameters between two groups at T0. Table 1 demonstrates the demographic distribution of the groups. The differences between changes through T0 to T1 in the MISDS and BAPA groups are demonstrated in Tables 2 and 3. Pretreatment and posttreatment occlusal photographs of two cases in the MISDS and BAPA groups are shown in Figures 2 and 3.
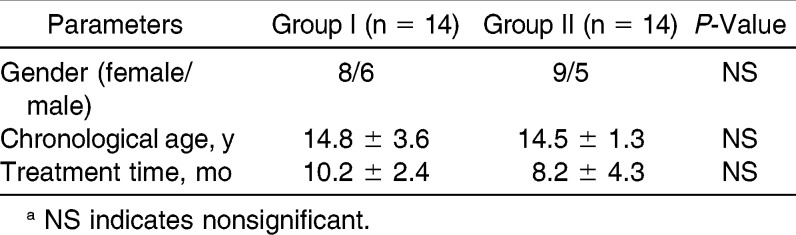
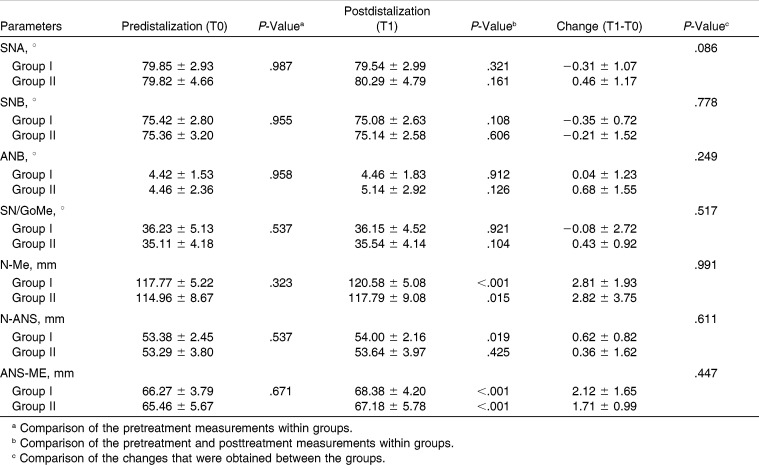
Table 1.
Demographic Assessment of the Samplea
Table 2.
Skeletal Comparisons Within and Between the Groups
Table 3.
Dental and Soft Tissue Comparisons Within and Between the Groups
Figure 2.
(a) Occlusal pretreatment photograph of a patient in the Miniscrew Implant Supported Distalization System (MISDS) group; (b) Occlusal posttreatment photograph of a patient and the MISDS appliance.
Figure 3.
(a) Occlusal pretreatment photograph of a patient in the Bone-Anchored Pendulum Appliance (BAPA) group; (b) Occlusal posttreatment photograph of a patient and the BAPA appliance.
The mean maxillary first molar distalization was 2.8 mm (P < .025) in the first group, whereas 2.9 mm (P < .001) was found in the second group. The difference between the two groups was not significant.
The average distalization duration was 8.2 months in the MISDS group and 10.2 months in the BAPA group. Accordingly, the amount of distal tipping for the maxillary first molars measured 1.65° (P = .42) in the MISDS group and 9° (P < .001) in the BAPA group. The difference between the two groups was statistically significant (P < .05). The distalization rate was 0.2 mm/mo in the first group and 0.3 mm/mo in the second group. Moreover, significant distalization of maxillary second molars was found in both of the groups.
Regarding the sagittal movement of maxillary second premolars, an average of 2.7 mm (P < .001) of distalization in the MISDS group and 1.7 mm (P < .001) of distalization in the BAPA group was seen. Accordingly, distal tipping of 9.6° (P < .001) in the MISDS group and of 6.0° (P < .025) in the BAPA group accompanied premolar distalization. Significant distalization and distal tipping of maxillary first premolars was observed as well.
Sagittal movement of the maxillary incisors was not statistically significant for either group. However, significant extrusion of maxillary incisors was found in the MISDS group (P < .001). Moreover, the maxillary incisors were slightly retroclined in the MISDS group and slightly proclined in the BAPA group. These findings were not statistically significant.
There was no significant treatment-related change in the sagittal position of the maxilla and the mandible in either group. Significant vertical changes in N-Me, N-ANS, and ANS-Me were found in both groups. However, no significant differences were found between the groups.
DISCUSSION
The major objective of this study was to evaluate the efficacy of two equal distalizing forces, one from the crown level and one from the approximate center of resistance of the maxillary molars, and to compare the effects of these two force application levels. In the MISDS group, the force was applied through the apex level of the maxillary first molar, and in the BAPA group the force was applied through the crown of the maxillary first molar. This second group was constructed retrospectively, in contrast to the prospectively designed first group, which is a drawback of the study.
Previous studies have shown that the pendulum appliance causes distal tipping of the maxillary molars together with distalization. Escobar et al.15 showed 6 mm of distalization and 11.3° of tipping; Önçağ et al.16 demonstrated 3.4–4.5 mm of distalization and 10–14° of tipping; Kircelli et al.13 found 6.4 mm of distalization and 10.9° of tipping, and Polat-Ozsoy et al.17 showed 4.8 mm of distalization and 9.1° of tipping in their studies, which used implant-supported pendulum appliances. In this study, in the MISDS group, since the force was applied close to the center of resistance of the maxillary first molars, distal tipping was not statistically significant, and the amount of distalization was 2.81 mm.
Papadopoulos,20 who introduced the MISDS appliance, stated that when the MISDS is used, the force vector is positioned 10–13 mm apical to the occlusal surface of the maxillary molar and passes through or close to its center of resistance; therefore, when the appliance is used, almost pure bodily movement and no distal tipping are expected to occur. The findings of this study corroborate the statement of Papadopoulos. The amount of distalization in the BAPA group was 2.93 mm, and 9° of distal tipping accompanied distalization. As the distalization force was generated with 60–70° posterior activation of the pendulum springs from the crown level and because no control mechanism related to tipping of the upper molars was present in the BAPA group, distal tipping at the maxillary molars was inevitable.
According to a systematic review22 that examined the effects of distalizing appliances reinforced with temporary skeletal anchorage devices, the mean distal movement of the maxillary molars ranged from 3.5 to 6.4 mm, and concomitant distal tipping ranged from 0.8° to 12.2°. The mean distal movement was 0.7 mm/mo (range, 0.2–1.2 mm/mo). However, the design of the appliances and the quality of the studies varied. The amounts of distalization in this study are slightly less than that identified in the studies in the literature. This may be the result of the smaller amount of required distalization for Class II correction, as almost all patients had a half-unit Class II molar relationship before treatment.
The average distalization period was 10.2 months in the MISDS group and 8.2 months in the BAPA group. This period was longer in the MISDS group; however, the difference was not statistically significant. Even though the treatment durations cannot be directly compared as a result of the differences in the appliance mechanics, the main reason for this result might be applying force vector from the apex level of the first molars in the MISDS group and trying to achieve bodily movement. Although the distalization time in the pendulum group was smaller, total treatment time would be longer than in the MISDS group because of the need for molar uprighting in the second phase of the treatment.
The rate of molar distalization is calculated as millimeters of molar distal movement per month. When considered clinically, evaluating the distalization rate would be more important than evaluating the amount of distalization. The distalization rate was 0.27 mm/mo in the MISDS group and 0.35 mm/mo in the BAPA group. According to a systematic review, distalization rate varies from 0.2 mm/mo to 1.2 mm/mo in studies using implant-supported distalization systems.
As reported in previous studies12–19 with implant-supported intraoral distalization systems, spontaneous distalization of maxillary premolars was seen in both groups. During distalization of the maxillary first molars, the maxillary second premolars and maxillary first premolars move distally with the help of transeptal fibers as well. In our study, in the MISDS group, the second premolars were distalized an average of 2.73 mm, with an inclination of 9.65°, and an average of 1.75 mm of distalization was found, with 6° of distal tipping, in the BAPA group. The difference in the amounts of distalization of the maxillary second premolars might be due to the bodily movement of the maxillary first molars in the MISDS group. Likewise, the distal tipping of the maxillary second premolars was more prominent in the MISDS group depending not only on the tensile force of the transeptal fibers but also on the absence of any mechanics that could control the tipping movement accompanying distalization.
Upper incisors were slightly retroclined in the first group and slightly proclined in the second group. The reason for this slight proclination of the upper incisors in the BAPA group might be the reactive force, which pushes the acrylic plate and the screws to the anterior palate. In the MISDS group, a slight retroclination of the upper incisors, which is advantageous, especially in Class II division 1 cases, was seen as a result of the effects of the transeptal fibers. In both groups, molar distalization was achieved without any significant change in the inclination of the mandibular plane. No change was seen in mandibular plane in the MISDS group, and in the BAPA group the mandibular plane rotated 0.43° clockwise, which was not statistically significant.
Following molar distalization, the screws and the appliances were left in place in both groups. Even though spontaneous distalization of premolars was seen, additional distalization was needed. Premolars and canines were distalized with molar anchorage which were connected and stabilized to the miniscrew-supported appliance.
With regard to comparing the clinical advantages and disadvantages of the two systems, fabrication of both appliances is simple. Insertion of the BAPA is easier; however, activation of the appliance is harder, and breakages might be seen during activation of TMA springs and during insertion of the lingual sheaths to the molar bands. On the other hand, the MISDS is more hygienic, as it is smaller and does not have an acrylic body, and activation of the appliance is easy.
CONCLUSIONS
Distalization of the maxillary first molars was successfully achieved in both groups, and the mean maxillary first molar distalization was 2.81 mm in the MISDS group, while it was 2.93 mm in the BAPA group.
An almost translatory distal movement was seen in the MISDS group, and substantial distal tipping of the maxillary molars accompanied distalization in the BAPA group.
No significant changes in the mandible in the vertical plane and in the inclination of the upper incisors were observed in either group.
REFERENCES
- 1.Gianelly AA, Vaitas AS, Thomas WM. The use of magnets to move molars distally. Am J Orthod Dentofacial Orthop. 1989;96:161–167. doi: 10.1016/0889-5406(89)90257-6. [DOI] [PubMed] [Google Scholar]
- 2.Bondemark L, Kurol J, Bernhold M. Repelling magnets versus superelastic NiTi simultaneous distal movement of maxillary first and second molars. Angle Orthod. 1994;64:189–198. doi: 10.1043/0003-3219(1994)064<0189:RMVSNC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Carano A, Testa M. The distal jet for upper molar distalization. J Clin Orthod. 1996;30:374–380. [PubMed] [Google Scholar]
- 4.Ghosh J, Nanda RS. Evaluation of an intraoral maxillary molar distalization technique. Am J Orthod Dentofacial Orthop. 1996;110:639–646. doi: 10.1016/s0889-5406(96)80041-2. [DOI] [PubMed] [Google Scholar]
- 5.Brickman D, Sinha PK, Nanda RS. Evaluation of the Jones jig appliance for distal molar movement. Am J Orthod Dentofacial Orthop. 2000;118:526–534. doi: 10.1067/mod.2000.110332. [DOI] [PubMed] [Google Scholar]
- 6.Bussick T, McNamara JA., Jr Dentoalveolar and skeletal changes associated with the pendulum appliance. Am J Orthod Dentofacial Orthop. 2000;117:333–343. doi: 10.1016/s0889-5406(00)70238-1. [DOI] [PubMed] [Google Scholar]
- 7.Chiu PP, McNamara JA, Jr, Franchi L. A comparison of two intraoral molar distalization appliances: distal jet versus pendulum. Am J Orthod Dentofacial Orthop. 2005;128:353–365. doi: 10.1016/j.ajodo.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 8.Antonarakis GS, Kiliaridis S. Maxillary molar distalization with noncompliance intramaxillary appliances in Class II malocclusion. A systematic review. Angle Orthod. 2008;78:1133–1140. doi: 10.2319/101507-406.1. [DOI] [PubMed] [Google Scholar]
- 9.Byloff FK, Kärcher H, Clar E, Stoff F. An implant to eliminate anchorage loss during molar distalization: a case report involving the Graz implant-supported pendulum. Int J Adult Orthod Orthognath Surg. 2000;15:129–137. [PubMed] [Google Scholar]
- 10.Karaman AI, Basciftci FA, Polat O. Unilateral distal molar movement with an implant-supported distal jet appliance. Angle Orthod. 2002;72:167–174. doi: 10.1043/0003-3219(2002)072<0167:UDMMWA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Keles A, Erverdi N, Sezen S. Bodily distalization of molars with absolute anchorage. Angle Orthod. 2003;73:471–482. doi: 10.1043/0003-3219(2003)073<0471:BDOMWA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Gelgör IE, Büyükyilmaz T, Karaman AI, Dolanmaz D, Kalayci A. Intraosseous screw-supported upper molar distalization. Angle Orthod. 2004;74:838–850. doi: 10.1043/0003-3219(2004)074<0838:ISUMD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Kircelli BH, Pektaş ZO, Kircelli C. Maxillary molar distalization with a bone-anchored pendulum appliance. Angle Orthod. 2006;76:650–659. doi: 10.1043/0003-3219(2006)076[0650:MMDWAB]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Gelgör IE, Karaman AI, Büyükyilmaz T. Comparison of 2 distalization systems supported by intraosseous screws. Am J Orthod Dentofacial Orthop. 2007;131:161.e1–161.e8. doi: 10.1016/j.ajodo.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 15.Escobar SA, Tellez PA, Moncada CA, Villegas CA, Latorre CM, Oberti G. Distalization of maxillary molars with the bone-supported-pendulum: a clinical study. Am J Orthod Dentofacial Orthop. 2007;131:545–549. doi: 10.1016/j.ajodo.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Onçağ G, Seçkin O, Dinçer B, Arikan F. Osseointegrated implants with pendulum springs for maxillary molar distalization: a cephalometric study. Am J Orthod Dentofacial Orthop. 2007;131:16–26. doi: 10.1016/j.ajodo.2005.02.034. [DOI] [PubMed] [Google Scholar]
- 17.Polat-Ozsoy O, Kircelli BH, Arman-Ozçirpici A, Pektas ZO, Uçkan S. Pendulum appliances with 2 anchorage designs: conventional anchorage vs. bone anchorage. Am J Orthod Dentofacial Orthop. 2008;133:339.e9–339.e17. doi: 10.1016/j.ajodo.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 18.Kinzinger GS, Gülden N, Yildizhan F, Diedrich PR. Efficiency of a skeletonized distal jet appliance supported by miniscrew anchorage for noncompliance maxillary molar distalization. Am J Orthod Dentofacial Orthop. 2009;136:578–586. doi: 10.1016/j.ajodo.2007.10.049. [DOI] [PubMed] [Google Scholar]
- 19.Oberti G, Villegas C, Ealo M, Palacio JC, Baccetti T. Maxillary molar distalization with the dual-force distalizer supported by mini-implants: a clinical study. Am J Orthod Dentofacial Orthop. 2009;135:282.e1–282.e5. doi: 10.1016/j.ajodo.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Papadopoulos MA. Orthodontic treatment of Class II malocclusion with miniscrew implants. Am J Orthod Dentofacial Orthop. 2008;134:604.e1–604.e16. doi: 10.1016/j.ajodo.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Hilgers JJ. The pendulum appliance for Class II non-compliance therapy. J Clin Orthod. 1992;26:706–714. [PubMed] [Google Scholar]
- 22.Fudalej P, Antoszewska J. Are orthodontic distalizers reinforced with the temporary skeletal anchorage devices effective. Am J Orthod Dentofacial Orthop. 2011;139:722–729. doi: 10.1016/j.ajodo.2011.01.019. [DOI] [PubMed] [Google Scholar]