Abstract
Objectives:
To analyze the scientific literature and compare in the results of conventional orthopedic appliances with those obtained from recent bone-anchored orthopedics for Class III malocclusion.
Materials and Methods:
The literature was systematically reviewed using PubMed/Medline, Scopus, and Scirus databases up to January 2012. Articles were selected by two different researchers (kappa index = 0.83), based on established inclusion/exclusion criteria. Methodologic quality was classified as high, medium, or low quality.
Results:
The search strategy identified 1020 titles. Thirty studies were selected after applying the criteria (high quality = 9, medium quality = 21). Protraction rates differed within a range of one- to twofold between bone-anchored and dentoalveolar therapies (P < .001). All studies noted the effect of clockwise rotation on the mandible and an increase in inferior-anterior and total facial height; this was more obvious in dentoalveolar therapy than in bone-anchored orthopedics (P < .001).
Conclusions:
Dental parameters like overjet increased significantly with both sets of groups, ranging from 1.7 to 7.9 mm with dentoalveolar therapy and from 2.7 to 7.6 mm with bone-anchored orthopedics.
Keywords: Dentofacial orthopedics, Orthodontics, Bone-anchored orthopedics
INTRODUCTION
Treating Class III malocclusion is one of the most complex problems arising in orthodontic practice because the growth patterns in such patients are unpredictable and unfavorable. The components of a Class III malocclusion include dental compensation and skeletal problems. Maxillary retrusion (hypoplasia), mandibular protrusion (hyperplasia), or a combination of the two may form the skeletal origin of malocclusion,1 leading to an anterior crossbite and a concave profile.2
The traditional orthopedic treatment for skeletal Class III malocclusion in children who have not yet reached the period of pubertal growth spurt involved correcting skeletal deficiencies.3 The introduction of the new orthopedics based on bone-anchored systems has made it necessary to revise all of these previous concepts.4 In modern orthodontic practice, it appears possible to apply pure bone-borne orthopedic forces between the maxilla and the mandible for 24 hours per day, avoiding dentoalveolar compensations.5
The aim of the present study is to compile and analyze the various possibilities of orthopedic treatment for Class III malocclusion in the scientific literature and to compare the results of conventional orthopedic appliances with those obtained from recent bone-anchored orthopedics.
MATERIALS AND METHODS
Search Strategy
A literature search was carried out using the Medline (PubMed, www.ncbi.nlm.nih.gov), Scirus, and Scopus databases. The search strategy covered the period October 2001 to January 2012 and used the following MeSH (Medical Subject Heading) terms: “Malocclusion, Angle Class III” AND (“Extraoral Traction Appliances” OR “orthodontics, interceptive” OR “orthodontics, corrective” OR “Malocclusion, Angle Class III/therapy” OR “Orthodontics, Corrective/methods”) NOT surgery.
Selection Criteria
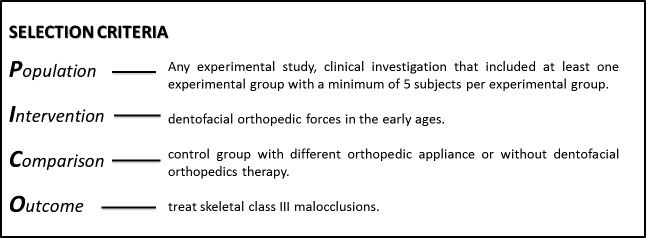
Articles selected for this study fulfilled the following criteria for inclusion, according to PICO (Figure 1). We excluded case reports, case series, descriptive studies, technical descriptions, review articles, opinion articles, letters, and articles that did not correspond to the objectives of the review.
Figure 1.
Criteria for inclusion in the review.
Data Collection and Analysis
The initial selection of articles was based on the title and abstract, the complete article being reviewed whenever there was doubt as to whether it should be included or not. Two reviewers independently applied the inclusion and exclusion criteria to every article, and good concordance was shown (kappa index = 0.83).
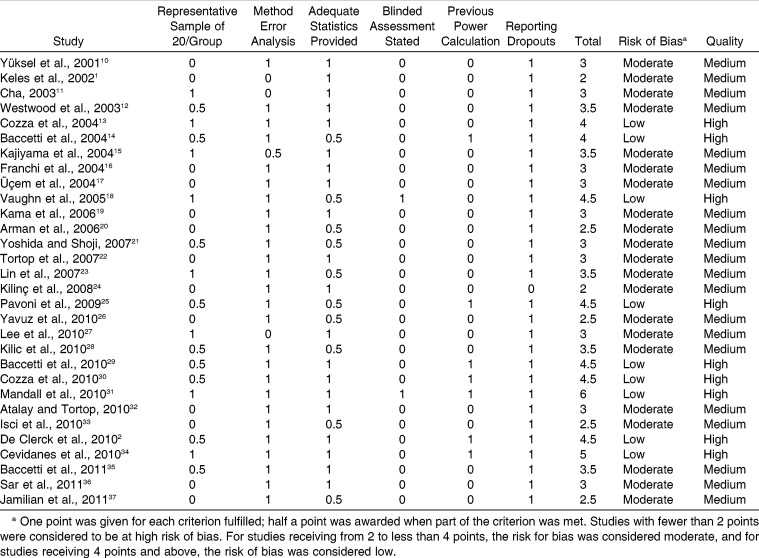
The methodologic quality of the selected articles was assessed using a modified version of the method reported by Antczak et al.6 and Jadad et al.7 Two investigators made independent quality assessments of the included studies using a modified Newcastle-Ottawa Scale. The variables were analyzed on the basis of Chen et al.8 Based on this checkpoint analysis, the risk of bias and quality of each article was scored as low, medium, or high, as detailed in Table 1. Quality was classified as low, medium, and high as previously defined by others.9
Table 1.
Quality assesment of the included articles
RESULTS
Search and Quality Assessment Results
The search strategy yielded 1020 titles/abstracts: 726 from PubMed, 146 from Scopus, and 148 from Scirus. After applying the criteria for inclusion/exclusion, 984 articles were removed, largely because they were descriptive articles, case reports, or articles that did not correspond to the objectives of this review. The remaining 36 articles were then read in full, and a further 6 articles were excluded: 2 because there was no cephalometric study, 2 because no control group was used, 1 because no protraction device was fitted, and 1 because it did not correspond with the objectives of this study. Only 30 articles1,2,10–37 therefore matched all the criteria for inclusion in the review.
All selected articles were based on human studies. Of the 30 articles, 9 were considered to be of high methodologic quality, and the remaining 21 articles were rated as medium quality (Table 1). The main quality defects were inadequate size of study-sample subgroups, absence of blinding in measurements, and no previous power calculation.
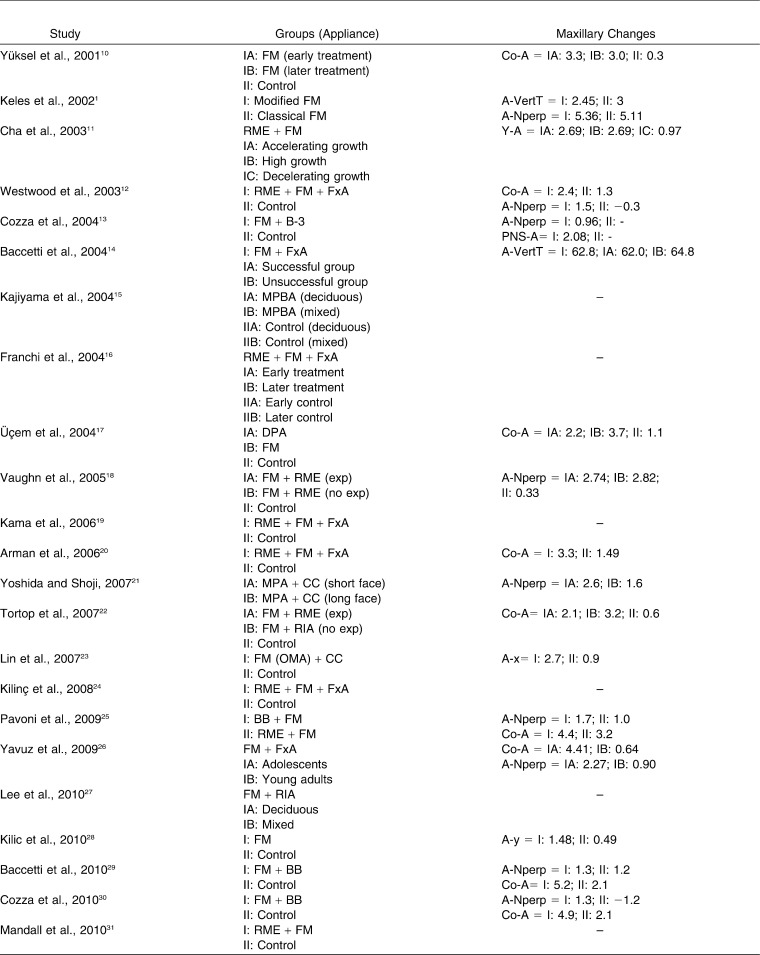
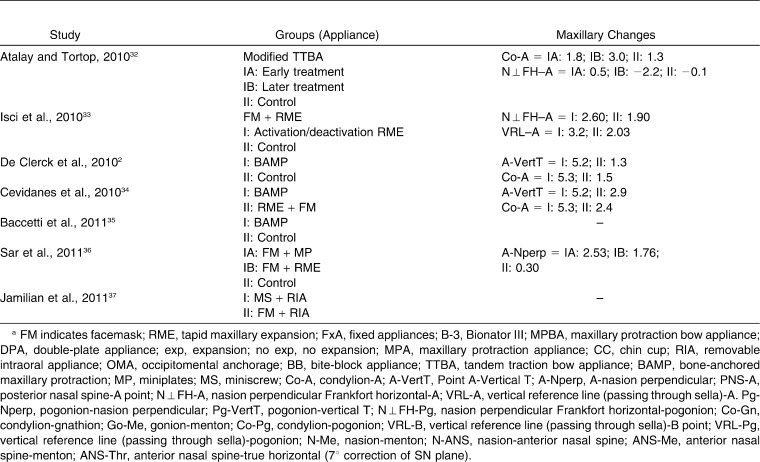
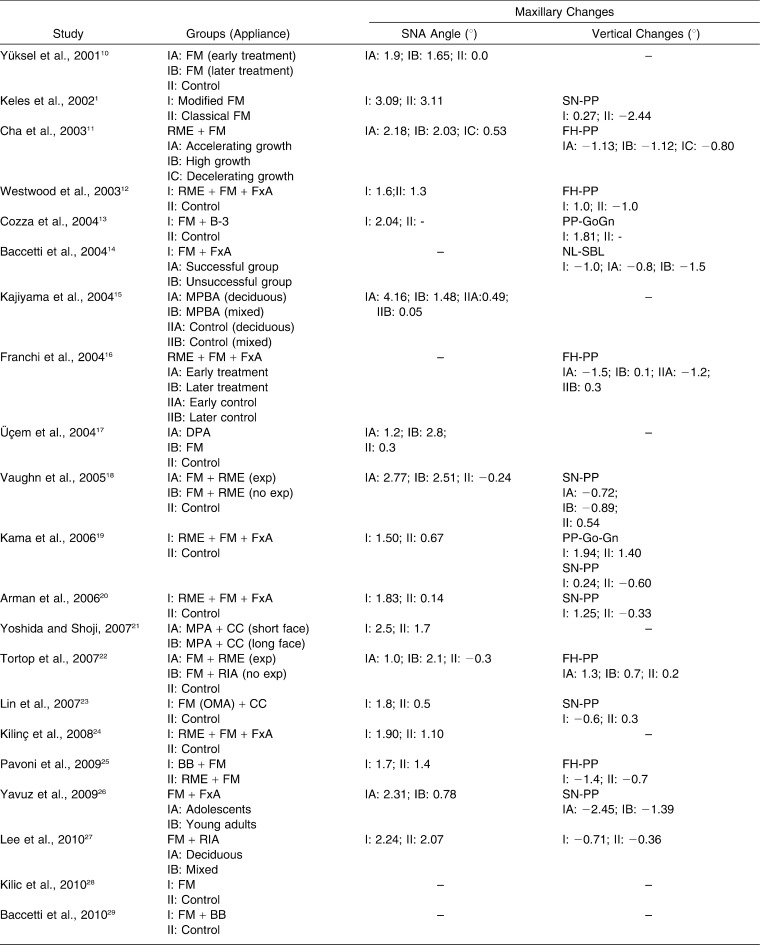
Skeletal Effects on the Upper Jaw
In spite of differences between treatment protocols and experimental design among the studies, a common trend was observed in the similar results for A-point advancement in the horizontal plane as a result of dentoalveolar or bone-anchored orthopedic treatment. Forward movement in the horizontal plane was noted in every study (Table 2), with a mean A-point advancement of around 0.81 mm with dentoalveolar therapy and 5.2 mm with bone-anchored orthopedics (Table 2), independent of whether or not there was maxillary expansion before the protraction facemask (Table 2).
Table 2.
Linear measurements performed in the included studiesa
Table 2.
Extended
Table 2.
Continued
Table 2.
Continued Extended
Some comparative studies have claimed that protraction rates differ within a range of 0.45 and 0.24 mm/month (P < .001)36 between bone-anchored and dentoalveolar therapies, respectively, so less treatment time (6.78 and 9.45 months, respectively) is required to move the maxilla forward 2.3 mm and 1.83 mm, respectively, in each group (P < .001).
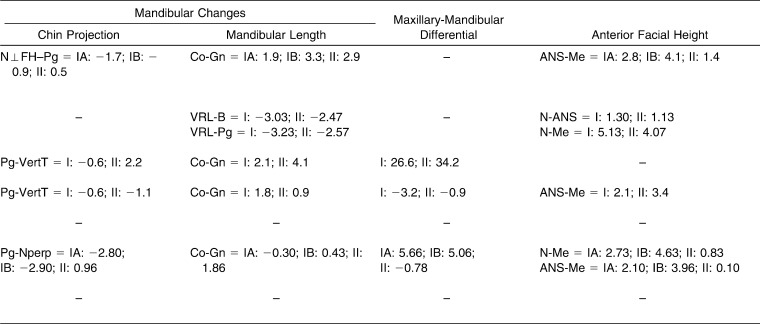
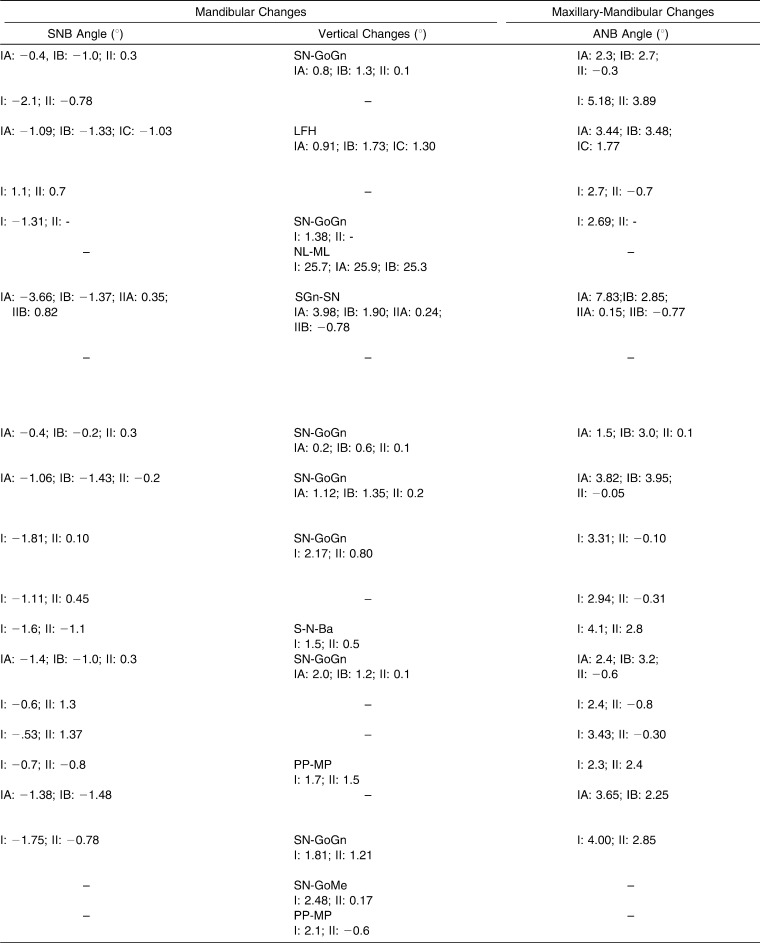
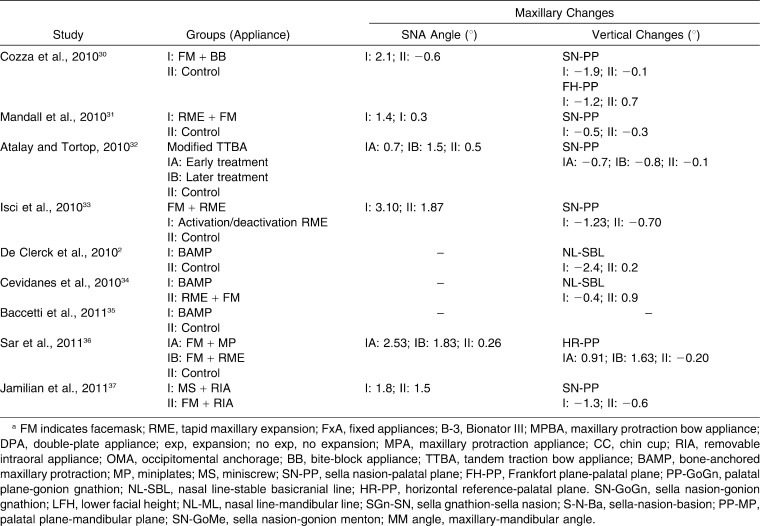
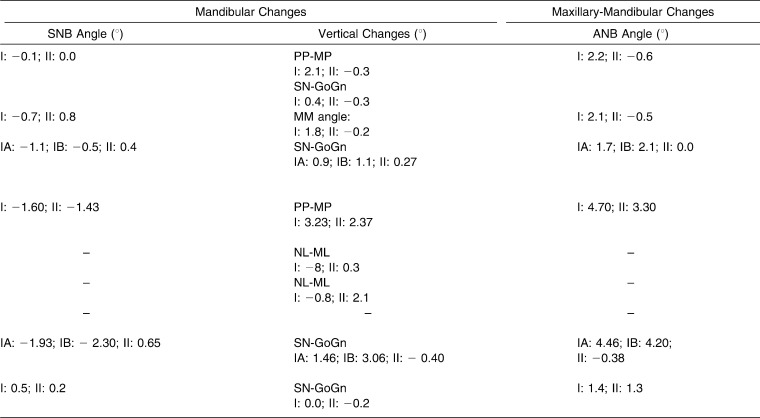
In summary, despite the differences, shown in Table 3, the included studies indicated an increase in SNA angle of 1° to 3.09° with dentoalveolar traction. Of the studies analyzed here, the only study to date that reported SNA measurements for bone-anchored orthopedics registered an increase of 2.53°, compared to a 1.83° increase in the internal control group (dentoalveolar-anchored therapy).
Table 3.
Angular measurements performed in the included studies a
Table 3.
Extended
Table 3.
Continued
Table 3.
Continued Extended
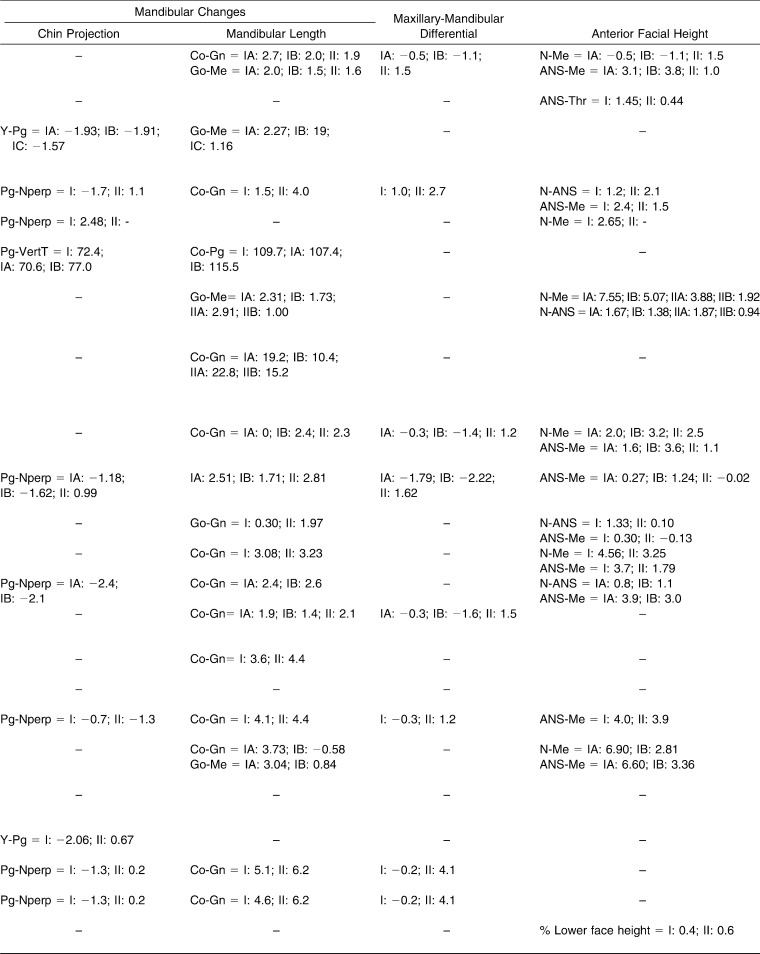
Skeletal Effects on the Mandible
All studies noted the effect of clockwise rotation on the mandible and a subsequent increase in facial height with mandibular protraction; this was more obvious in dentoalveolar therapy than bone-anchored orthopedics (Table 3). Both the maxilla and the mandible moved forward significantly in the control group of every study (Table 2). However, the protrusion and mesialization of maxillary teeth with dentoalveolar therapy appears to have been eliminated in bone-anchored groups where these parameters were analyzed (Table 4).
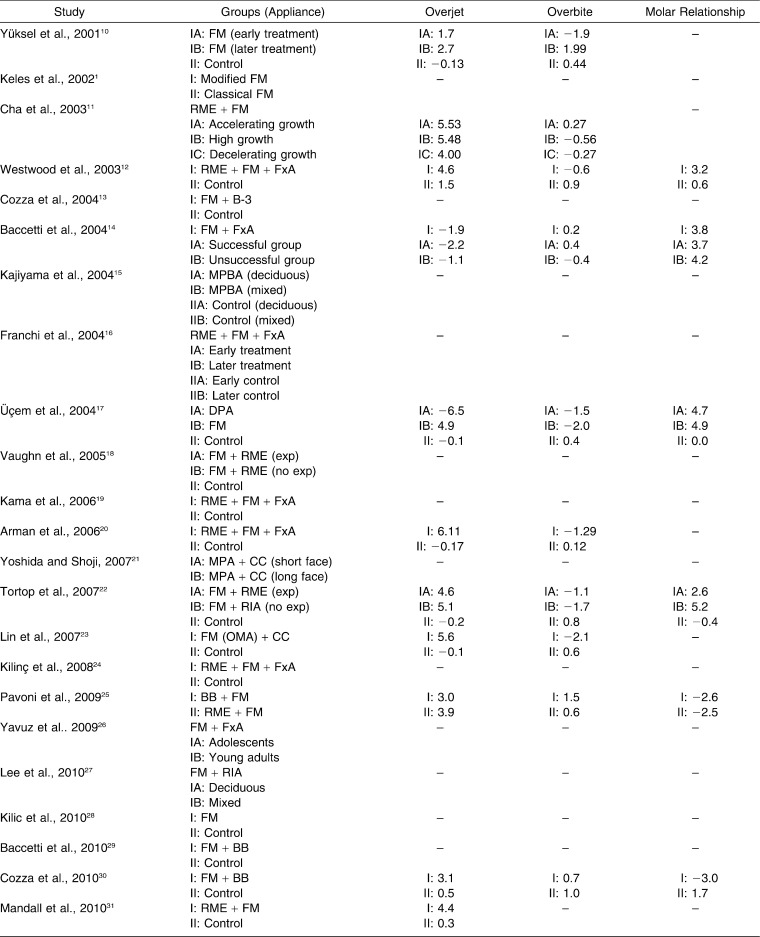
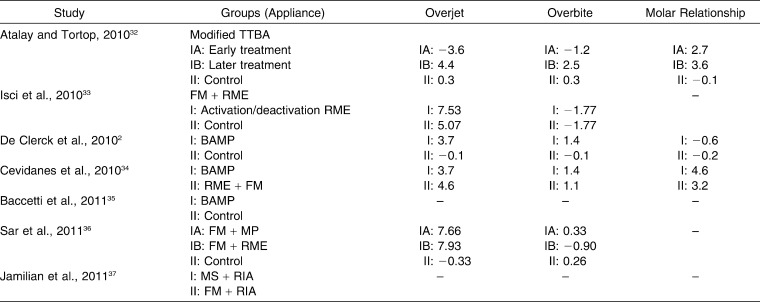
Table 4.
Dental parameters measured in the included studies
Table 4.
Continued
Interestingly, although the main orthopedic effect was directed toward correcting maxillary deficiency, the studies noted substantial changes in angular and linear mandibular parameters during bone-anchored and orthopedic treatment (Tables 2 and 3). The backward movement of point B and the increase in angular parameters corresponding to facial height were observed in both treatments.
Despite the marked differences in upper jaw correction shown for dentoalveolar and bone-anchored orthopedics in Class III treatment, some studies36 found no differences between groups for the results of final intermaxillary skeletal variables, such as Wits appraisal, ANB, and the like (Table 3).
Effect on Dental and Dentoalveolar Parameters
Bone-anchored orthopedic treatment at an early age was observed to lead not to compensation for upper incisor inclination but to their effectively protruding along the upper jaw bone. Dental parameters like overjet increased significantly with both sets of groups using bone- and dentoalveolar-anchored treatment (Table 4); considerable increases were reported with the use of bone-anchored orthopedics, between +2.7 mm2 and +7.6 mm,36 and substantial variations in changes in overjet, ranging from 1.7 mm to 7.9 mm, were also described for dentoalveolar therapy. Analyses of maxillary incisor position and angulation, however, showed significant differences between the two types of anchoring treatment. Some studies36 noted statistically significant differences of maxillary incisor position (P < .001) between the treatment groups, with a notable protrusion in the dentoalveolar group and even retrusion in the bone-anchored group (P < .05).36 Other authors found a slight upper incisor proclination of +0.6° with bone-anchored therapy.34 The effects on the maxillary molars followed the same trend, with significant mesialization from dentoalveolar therapy (P < .05) and no changes of significance in the bone-anchored group.36
Some studies using a conventional orthopedic approach found a reduced horizontal position for the lower incisors, which meant that the lower incisors were significantly retruded and tipped lingually.20,32,33 So, at the end of the observation period, some authors recorded differences of lower incisor inclination and found significant retroinclination of these in the treated group compared with the control group.12,31 In the literature, therefore, conventional orthopedic treatment has sought to reduce dentoalveolar effects, making corresponding changes in the appliance to minimize the side effects.30 This study also found that the mandibular incisors were significantly retracted with both bone and dentoalveolar orthopedic treatment, while the other studies of bone-anchored therapy that were included found a slight proclination of the mandibular incisors.2,34,37 Surprisingly, it was reported that bone-anchored orthopedic treatment had a slight compensatory effect on the inferior incisors, although the effect was in the opposite direction to what was expected, with proclination of the lower incisors, which might be defined as decompensation in a Class III malocclusion (Table 4).
Effects on the Vertical Dimension
Vertical analysis of changes in the lower third of the face highlights the fact that both bone- and dentoalveolar-anchored therapies increased the facial angle of the lower facial height (Table 3). The increase in the vertical dimension was brought about by posterior rotation of the mandible, which was more marked in the dentoalveolar-anchored group (Table 3). When other orthopedic methods were used, such as the chin cup or a Class III functional appliance, a slight +1.8° increase, and even a decrease of −0.4°, was reported associated with this therapy. Similarly, significant changes in inferior anterior and total facial height, ranging between −0.5 mm10 and +4.9 mm were found in most studies on dentoalveolar-anchored therapy10,26; the situation was similar for bone-anchored orthopedic therapy, with ranges of between 2 and 3 mm (Table 2).34,36 However, studies that compared the two groups in parallel36 also found statistically significant differences (P < .001) between the two types of therapy, with increased measurements for dentoalveolar-anchored therapy.36
DISCUSSION
Because of the high degree of maxillary retrusion in skeletal Class III malocclusion, several studies dealt with maxillary protraction using a facemask combined with a functional appliance (Bionator III),13 with a bite-block appliance,30 or after rapid maxillary expansion.20 These studies reported forward movement of the maxilla, maxillary incisor advancement, increased measurements for vertical parameters, and posterior movement of the mandible.
Dentofacial orthopedics using chin-cup therapy for a Class III malocclusion has also been studied in the literature, although its effects are not reported as orthopedic therapy as such. This treatment may be used to make improvements to both jaws by inhibiting mandibular growth and inducing remodeling the mandible with closure of the gonial angle or posterior rotation and distal displacement of the mandible.38,39
The basis of chin-cup therapy consists of applying a force to the temporomandibular joint in order to inhibit or redirect condylar growth, which causes morphologic changes at this region.40
In recent times, orthopedic therapy with bone anchoring has become the new paradigm for early treatment of skeletal Class III malocclusions. In some studies, orthopedic treatment was initiated with bone anchoring, using an extraoral appliance for maxillary protraction.41,42 Later, a new orthopedic protocol appeared using bone anchoring and intermaxillary elastics applied from four miniplates in each patient to maintain a constant pull force.43 Cevidanes et al.34 compared the bone-anchored maxillary protraction (BAMP) and rapid maxillary expansion and facemask protocols, reporting that the BAMP protocol produced greater maxillary advancement and fewer vertical changes. Also, this group of patients did not show clockwise rotation of the mandible or dental compensation.
Although the timing of treatment for facemask therapy is a subject that is not fully clarified in the articles included in the present study, because the permanent incisors continue erupting until 10 years of age maxillary protraction can be prescribed.44 On the other hand, the BAMP protocol should be performed on late mixed or permanent dentition because there is no alveolar bone development or inferior canine eruption.34,43
There is substantial variability regarding the magnitude of force used to obtain orthopedic results. In an overview of the literature, the force magnitude applied to each side is usually between 300g and 600g for the maxilla and 300–500g per side for the mandible. De Clerck et al.,43 using the bone-anchored maxillary protraction protocol, used 150g on each side in the initial phase, 200g after 1 month of treatment, and 250g after 3 months to avoid possible clinical failure. This new orthopedic approach produced significant skeletal changes.34,43
Different protocols are used in the literature according to whether or not there was previous expansion or disjunction of the upper jaw combined with facemask therapy. The literature describes various benefits of maxillary expansion combined with a protraction appliance. Maxillary expansion also corrected crossbite and Class III malocclusion, and the orthopedic effect was increased by splinting the maxillary arch and separating the circumaxillary sutures.45
Some clinicians have suggested that expansion and a protraction facemask leads to more of an anteroposterior skeletal effect, which is intensified depending on the timing, and less dental change.44 Others have found a backward and downward rotation of the mandible, as well as an increase in lower facial height and a positive overjet, a reduced overbite, and an improvement in the sagittal lip relationship.20 However, rapid palatal expansion before maxillary protraction should only be performed if there is a transversal problem.
CONCLUSIONS
Based on the findings of the 30 selected articles:
The recent orthopedic approach using temporary bone anchoring on late mixed or early permanent dentition results in effective skeletal changes with minimal dental compensation. The lack of long-term studies, however, means that further research, using well-designed studies and better clinical evidence, is necessary to assess the stability of orthopedic therapy in skeletal Class III malocclusions.
Although all such studies ought to be compared quantitatively, there is wide variability and heterogeneity in the methodologies of the scientific literature in the field. There are also various limitations, such as malocclusion variants among patients, different growth patterns, different levels of patient cooperation, duration of treatment, time spent wearing the appliance daily, and the diverse nature of the appliances used.
Differences in the efficiency parameters of bone- and dentoalveolar-anchored orthopedics were found, with a reduced treatment time using the bone-anchored approach.
REFERENCES
- 1.Keles A, Tokmak EC, Erverdi N, Nanda R. Effect of varying the force direction on maxillary orthopedic protraction. Angle Orthod. 2002;72:387–396. doi: 10.1043/0003-3219(2002)072<0387:EOVTFD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofac Orthop. 2010;138:577–581. doi: 10.1016/j.ajodo.2009.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Toffol LD, Pavoni C, Baccetti T, Franchi L, Cozza P. Orthopedic treatment outcomes in Class III malocclusion. Angle Orthod. 2008;78:561–573. doi: 10.2319/030207-108.1. [DOI] [PubMed] [Google Scholar]
- 4.Cornelis MA, Scheffler NR, Mahy P, Siciliano S, De Clerck HJ, Tulloch JF. Modified miniplates for temporary skeletal anchorage in orthodontics: placement and removal surgeries. J Oral Maxillofac Surg. 2008;66:1439–1445. doi: 10.1016/j.joms.2008.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67:2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Antczak AA, Tang J, Chalmers TC. Quality assessment of randomized control trials in dental research. 1. Methods. J Period Res. 1986;21:315–321. doi: 10.1111/j.1600-0765.1986.tb01465.x. [DOI] [PubMed] [Google Scholar]
- 7.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Controlled Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 8.Chen SS, Greenlee GM, Kim JE, Smith CL, Huang GJ. Systematic review of self-ligating brackets. Am J Orthod Dentofacial Orthop. 2010;137:726.e1–726.e18. doi: 10.1016/j.ajodo.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Feldmann I, Bondemark L. Orthodontic anchorage: a systematic review. Angle Orthod. 2006;76:493–501. doi: 10.1043/0003-3219(2006)076[0493:OA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Yüksel S, Uçem TT, Keykubat A. Early and late facemask therapy. Eur J Orthod. 2001;23:559–568. doi: 10.1093/ejo/23.5.559. [DOI] [PubMed] [Google Scholar]
- 11.Cha KS. Skeletal changes of maxillary protraction in patients exhibiting skeletal Class III malocclusion: a comparison of three skeletal maturation groups. Angle Orthod. 2003;73:26–35. doi: 10.1043/0003-3219(2003)073<0026:SCOMPI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Westwood PV, McNamara JA, Jr, Baccetti T, Franchi L, Sarver DM. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123:306–320. doi: 10.1067/mod.2003.44. [DOI] [PubMed] [Google Scholar]
- 13.Cozza P, Marino A, Mucedero M. An orthopaedic approach to the treatment of Class III malocclusions in the early mixed dentition. Eur J Orthod. 2004;26:191–199. doi: 10.1093/ejo/26.2.191. [DOI] [PubMed] [Google Scholar]
- 14.Baccetti T, Franchi L, McNamara JA., Jr Cephalometric variables predicting the long-term success or failure of combined rapid maxillary expansion and facial mask therapy. Am J Orthod Dentofac Orthop. 2004;126:16–22. doi: 10.1016/j.ajodo.2003.06.010. [DOI] [PubMed] [Google Scholar]
- 15.Kajiyama K, Murakami T, Suzuki A. Comparison of orthodontic and orthopedic effects of a modified maxillary protractor between deciduous and early mixed dentitions. Am J Orthod Dentofacial Orthop. 2004;126:23–32. doi: 10.1016/j.ajodo.2003.04.014. [DOI] [PubMed] [Google Scholar]
- 16.Franchi L, Baccetti T, McNamara JA. Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2004;126:555–568. doi: 10.1016/j.ajodo.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 17.Üçem TT, Ucuncu N, Yüksel S. Comparison of double-plate appliance and facemask therapy in treating Class III malocclusions. Am J Orthod Dentofacial Orthop. 2004;126:672–679. doi: 10.1016/S088954060400561X. [DOI] [PubMed] [Google Scholar]
- 18.Vaughn GA, Mason B, Moon HB, Turley PK. The effects of maxillary protraction therapy with or without rapid palatal expansion: a prospective, randomized clinical trial. Am J Orthod Dentofacial Orthop. 2005;128:299–309. doi: 10.1016/j.ajodo.2005.04.030. [DOI] [PubMed] [Google Scholar]
- 19.Kama JD, Ozer T, Baran S. Orthodontic and orthopaedic changes associated with treatment in subjects with Class III malocclusions. Eur J Orthod. 2006;28:496–502. doi: 10.1093/ejo/cjl011. [DOI] [PubMed] [Google Scholar]
- 20.Arman A, Ufuk Toygar T, Abuhijleh E. Evaluation of maxillary protraction and fixed appliance therapy in Class III patients. Eur J Orthod. 2006;28:383–392. doi: 10.1093/ejo/cjl008. [DOI] [PubMed] [Google Scholar]
- 21.Yoshida I, Shoji T, Mizoguchi I. Effects of treatment with a combined maxillary protraction and chincap appliance in skeletal Class III patients with different vertical skeletal morphologies. Eur J Orthod. 2007;29:126–133. doi: 10.1093/ejo/cjl087. [DOI] [PubMed] [Google Scholar]
- 22.Tortop T, Keykubat A, Yuksel S. Facemask therapy with and without expansion. Am J Orthod Dentofacial Orthop. 2007;132:467–474. doi: 10.1016/j.ajodo.2006.09.047. [DOI] [PubMed] [Google Scholar]
- 23.Lin HC, Chang HP, Chang HF. Treatment effects of occipitomental anchorage appliance of maxillary protraction combined with chincup traction in children with Class III malocclusion. J Formos Med Assoc. 2007;106:380–391. doi: 10.1016/S0929-6646(09)60323-5. [DOI] [PubMed] [Google Scholar]
- 24.Kilinç AS, Arslan SG, Kama JD, Ozer T, Dari O. Effects on the sagittal pharyngeal dimensions of protraction and rapid palatal expansion in Class III malocclusion subjects. Eur J Orthod. 2008;30:61–66. doi: 10.1093/ejo/cjm076. [DOI] [PubMed] [Google Scholar]
- 25.Pavoni C, Mucedero M, Baccetti T, Franchi L, Polimeni A, Cozza P. The effects of facial mask/bite block therapy with or without rapid palatal expansion. Prog Orthod. 2009;10:20–28. [PubMed] [Google Scholar]
- 26.Yavuz I, Halicioğlu K, Ceylan I. Face mask therapy effects in two skeletal maturation groups of female subjects with skeletal Class III malocclusions. Angle Orthod. 2009;79:842–848. doi: 10.2319/090308-462.1. [DOI] [PubMed] [Google Scholar]
- 27.Lee KJ, Park YC, Park JY, Hwang WS. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 2010;137:830–839. doi: 10.1016/j.ajodo.2007.10.065. [DOI] [PubMed] [Google Scholar]
- 28.Kilic N, Catal G, Kiki A, Oktay H. Soft tissue profile changes following maxillary protraction in Class III subjects. Eur J Orthod. 2010;32:419–424. doi: 10.1093/ejo/cjp119. [DOI] [PubMed] [Google Scholar]
- 29.Baccetti T, Franchi L, Mucedero M, Cozza P. Treatment and post-treatment effects of facemask therapy on the sagittal pharyngeal dimensions in Class III subjects. Eur J Orthod. 2010;32:346–350. doi: 10.1093/ejo/cjp092. [DOI] [PubMed] [Google Scholar]
- 30.Cozza P, Baccetti T, Mucedero M, Pavoni C, Franchi L. Treatment and posttreatment effects of a facial mask combined with a bite-block appliance in Class III malocclusion. Am J Orthod Dentofacial Orthop. 2010;138:300–310. doi: 10.1016/j.ajodo.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Mandall N, DiBiase A, Littlewood S, et al. et al. Is early Class III protraction facemask treatment effective? A multicentre, randomized, controlled trial: 15-month follow-up. J Orthod. 2010;37:149–161. doi: 10.1179/14653121043056. [DOI] [PubMed] [Google Scholar]
- 32.Atalay Z, Tortop T. Dentofacial effects of a modified tandem traction bow appliance. Eur J Orthod. 2010;32:655–661. doi: 10.1093/ejo/cjp153. [DOI] [PubMed] [Google Scholar]
- 33.Isci D, Turk T, Elekdag-Turk S. Activation-deactivation rapid palatal expansion and reverse headgear in Class III cases. Eur J Orthod. 2010;32:706–715. doi: 10.1093/ejo/cjq006. [DOI] [PubMed] [Google Scholar]
- 34.Cevidanes L, Baccetti T, Franchi L, McNamara JA, Jr, De Clerck H. Comparison of two protocols for maxillary protraction: bone anchors versus facemask with rapid maxillary expansion. Angle Orthod. 2010;80:799–806. doi: 10.2319/111709-651.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baccetti T, De Clerck HJ, Cevidanes LH, Franchi L. Morphometric analysis of treatment effects of bone-anchored maxillary protraction in growing Class III patients. Eur J Orthod. 2011;33:121–125. doi: 10.1093/ejo/cjq170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sar C, Arman-Özçırpıcı A, Uçkan S, Yazıcı AC. Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 2011;139:636–649. doi: 10.1016/j.ajodo.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 37.Jamilian A, Haraji A, Showkatbakhsh R, Valaee N. The effects of miniscrew with Class III traction in growing patients with maxillary deficiency. Int J Orthod. 2011;22:25–30. [PubMed] [Google Scholar]
- 38.Graber LW. Chin cup therapy for mandibular prognathism. Am J Orthod. 1997;72:23–41. doi: 10.1016/0002-9416(77)90122-1. [DOI] [PubMed] [Google Scholar]
- 39.Sugawara J, Asano T, Endo N, Mitani H. Long-term effects of chincap therapy on skeletal profile in mandibular prognathism. Am J Orthod Dentofacial Orthop. 1990;98:127–133. doi: 10.1016/0889-5406(90)70006-X. [DOI] [PubMed] [Google Scholar]
- 40.Gokalp H, Kurt G. Magnetic resonance imaging of the condylar growth pattern and disk position after chin cup therapy: a preliminary study. Angle Orthod. 2005;75:568–575. doi: 10.1043/0003-3219(2005)75[568:MRIOTC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 41.Liu C, Hou M, Liang L, Huang X, Zhang T, Zhang H, Ma X, Song R. Sutural distraction osteogenesis (SDO) versus osteotomy distraction osteogenesis (ODO) for midfacial advancement: A new technique and primary clinical report. J Craniofac Surg. 2005;16:537–548. doi: 10.1097/01.scs.0000159083.21931.c5. [DOI] [PubMed] [Google Scholar]
- 42.Kircelli BH, Pektas ZO. Midfacial protraction with skeletally anchored face mask therapy: a novel approach and preliminary results. Am J Orthod Dentofacial Orthop. 2008;133:440–449. doi: 10.1016/j.ajodo.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 43.De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ. Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 2009;67:2123–2129. doi: 10.1016/j.joms.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115:675–685. doi: 10.1016/s0889-5406(99)70294-5. [DOI] [PubMed] [Google Scholar]
- 45.Baccetti T, Franchi L, McNamara JA. Treatment and posttreatment craniofacial changes after rapid maxillary expansion and facemask therapy. Am J Orthod Dentofacial Orthop. 2000;118:404–413. doi: 10.1067/mod.2000.109840. [DOI] [PubMed] [Google Scholar]