Abstract
Objective:
To investigate the factors related to changes in alveolar bone thickness during upper incisor retraction.
Materials and Methods:
The subjects consisted of 23 ongoing orthodontic patients (mean age 20.4 ± 2.7 years) whose upper incisors were bound for retraction. Changes in alveolar bone thickness in the retracted area were assessed using preretraction (T0) and postretraction (T1) cone-beam computed tomography images. Labial bone thickness (LBT), palatal bone thickness (PBT), and total bone thickness (TBT) were assessed at the crestal, midroot, and apical levels of the retracted incisors. Paired t-tests were used to compare T0 and T1 bone thickness measurements. Spearman's rank correlation analysis was performed to determine the relationship of changes in alveolar bone thickness with the rate of tooth movement, change in inclination, initial alveolar bone thickness, and the extent of intrusion.
Results:
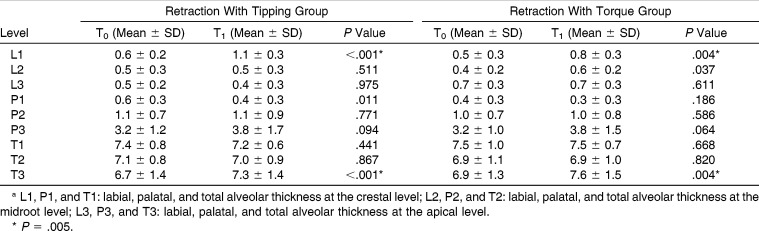
As the upper incisors were retracted, the LBT at the crestal level and TBT at the apical level significantly increased (P < .005). Changes in alveolar bone thickness were significantly associated with the rate of tooth movement, change in inclination, and extent of intrusion (P < .05) but not initial alveolar bone thickness (P > .05).
Conclusion:
Rate of tooth movement, change in inclination, and extent of intrusion are significant factors that may influence alveolar bone thickness during upper incisor retraction. These factors must be carefully monitored to avoid the undesirable thickening of alveolar bone.
Keywords: Alveolar bone, Bone remodeling, CBCT, Incisor inclination, Incisor intrusion
INTRODUCTION
Orthodontic tooth movement is a process whereby the application of a force induces bone resorption on the pressure side and bone apposition on the tension side. Controversy exists whether the changes occurring in anterior alveolar bone during orthodontic tooth movement always follow the direction and extent of tooth movement.1 A basic axiom in orthodontics is “bone traces tooth movement,” which suggests that whenever orthodontic tooth movement occurs, the bone around the alveolar socket will remodel to the same extent.2 However, sometimes there may not be coherence with this rule, and an unfavorable bone response may occur after incisor retraction. For example, the increased bone due to a labial cortical plate is usually greater than the tooth displacement, leading to visible bone exostosis, labial bone protuberance, and an irregular ridge of bone.3,4 Labial bone protuberance usually causes esthetic problems, and alveloplasty can be used to eliminate excess alveolar bone. Currently, the mechanisms leading to different alveolar bone responses are unclear; there is interest in determining the factors related to changes in alveolar bone thickness during incisor retraction.
Many studies have shown that cone-beam computed tomography (CBCT) can be used as a tool to qualitatively evaluate hard-tissue changes in the alveolar bone plates in three dimensions,5,6 as the technique has a one-to-one image-to-reality ratio7 and the measurements are not affected by changes in the orientation of the skull.8 The resulting images allow clinicians and researchers to quantitatively evaluate hard-tissue changes in three dimensions.6 CBCT images can also be used to determine the factors affecting buccal bone changes for the maxillary posterior teeth after rapid maxillary expansion.9 Therefore, this study was designed to evaluate bone thickness changes using CBCT.
The aims of this study were to evaluate the changes in alveolar bone thickness during upper incisor retraction and to investigate the factors related to changes in alveolar bone thickness during upper incisor retraction.
MATERIALS AND METHODS
The study was approved by the ethical committee of the Faculty of Dentistry, Prince of Songkla University. Adult patients receiving orthodontic treatment in the Orthodontic Clinic at the Dental Hospital, Faculty of Dentistry, Prince of Songkla University, were selected on the basis of the following inclusion criteria: (1) upper incisors bound for retraction with a space ≥4 mm between the lateral incisors and canines, (2) no significant medical history, (3) no use of anti-inflammatory drugs for at least 6 months before or during the study, (4) no evidence of periodontal or gingival problems at the beginning of orthodontic treatment, and (5) no history of trauma to the upper and lower anterior teeth.
To evaluate changes in alveolar bone and the factors potentially influencing alveolar bone thickness during upper incisor retraction, CBCT images and lateral cephalograms were taken preretraction (T0) and postretraction (T1). The parameters measured in this study included the rate of tooth movement; change in inclination and extent of intrusion, determined from lateral cephalograms; and alveolar bone thickness, measured from CBCT images. General information on each patient was collected from the patient's dental record, including the patient's sex, type of wire, type of mechanic, distance, and retraction time.
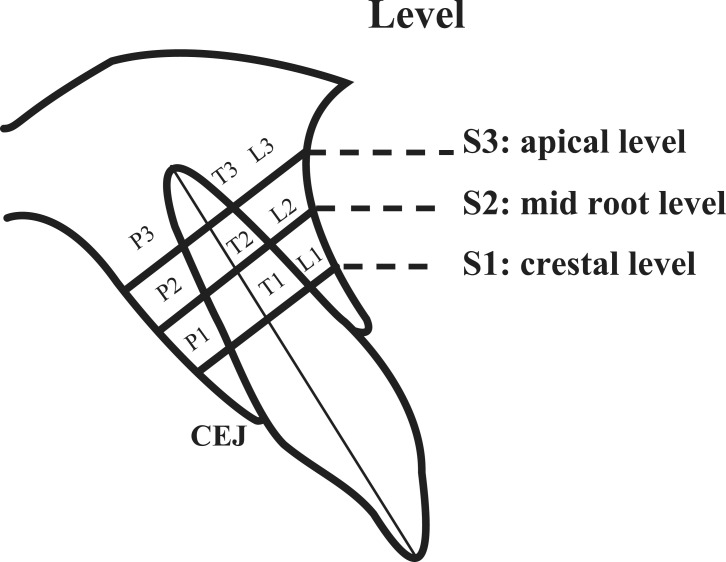
Changes in alveolar bone were evaluated using CT scans (80 kV, 5 mA, 7.5-second exposure time, 0.125 mm voxel resolution, and 80 × 40 mm field of view; Veraviewepocs J Morita MPG). The CBCT data from each patient were reconstructed at 0.125-mm increments. The Digital Imaging and Communications in Medicine images were assessed. The thickness of the labial and palatal alveolar plates was measured for each tooth, at the site adjacent to the widest point of the labiopalatal root, in three slices separated by 3 mm (S1, S2, and S3, respectively). Labial, palatal, and total alveolar bone thicknesses were assessed at the crestal level (S1; L1, P1, and T1), midroot level (S2; L2, P2, and T2), and apical level (S3; L3, P3, and T3) to evaluate bone thickness changes during retraction (Figures 1 and 2).
Figure 1.
Location of the pre- and postretraction bone thickness measurements.
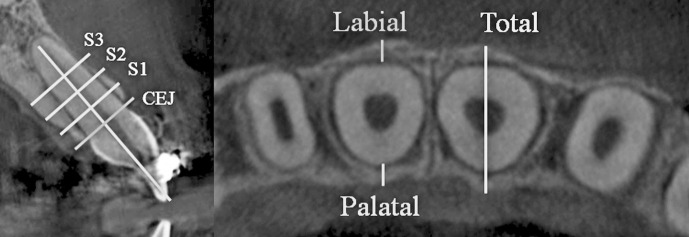
Figure 2.
Measurement of maxillary tooth bone plate thickness.
Preretraction (T0), nine measurements were taken for each tooth from the radiographs: three on the labial side, three on the palatal side, and three for the total thickness. The same measurements were repeated at 6 months postretraction or after incisor retraction was completed (T1). T1 measurements were taken at the same slice levels as the T0 measurements, using the first slice on the incisor edge of the tooth as a reference point. All measurements were determined by a single investigator.
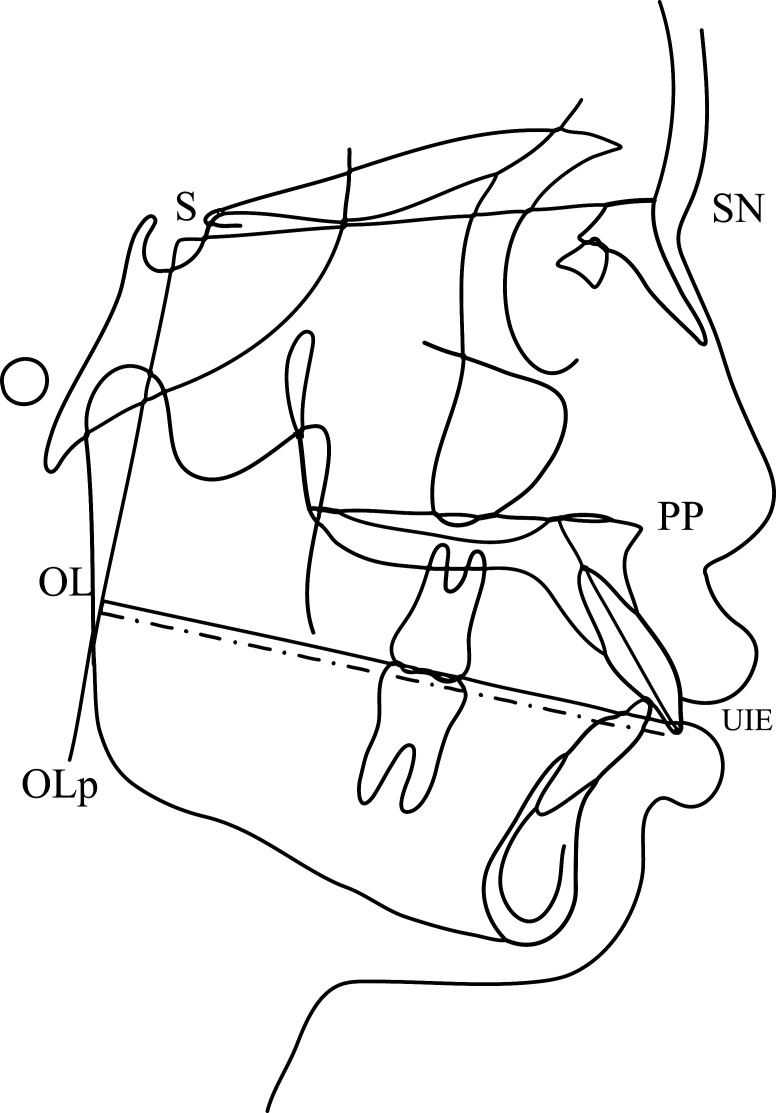
The retraction time was registered and the extent of space closure was evaluated as the change in distance between the U1 incisal edge (UIE) and the OLp pre– and post–incisor retraction, to determine the rate of tooth movement. Change in inclination was evaluated as the change in the angle between the UIE and palatal plane pre– and post–incisor retraction (Figure 3).
Figure 3.
Reference planes and angular measurements pre– and post–incisor retraction.
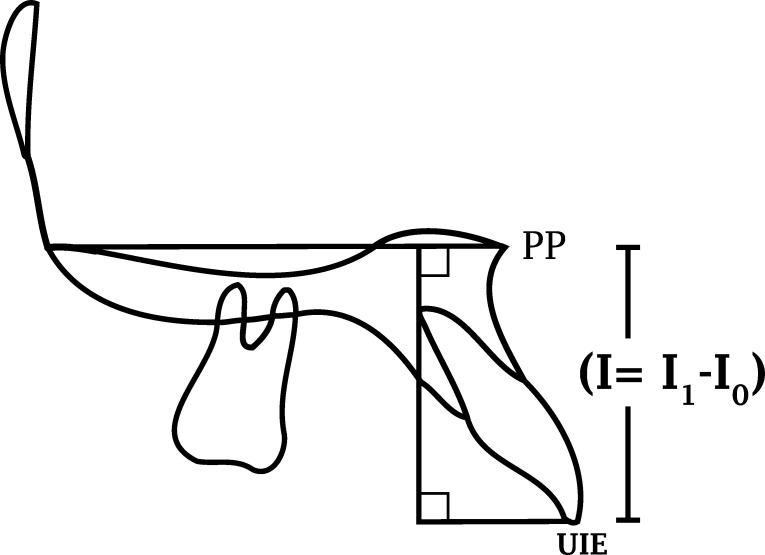
The extent of intrusion was evaluated using the change in distance between the UIE and the palatal plane pre– (I0) and post–incisor retraction (I1), as shown in Figure 4.
Figure 4.
Reference planes used to determine the extent of intrusion.
Statistical Analysis
Paired t-tests with a significance level of .05 were used to evaluate the bony changes that occurred as a result of incisor retraction. The Bonferroni adjustment was applied to avoid the chance of encountering a Type I error due to repeated measurements. The Bonferroni adjustment was used with an adjusted alpha level of .05 divided by the number of outcome measures (nine levels of alveolar bone thickness); therefore, the level of significance was adjusted to P < .005. Spearman's rank correlation analysis was applied to identify any correlations between potential influencing factors and changes in alveolar bone thickness with a significant level of .05.
The reproducibility of the bone thickness and bone level measurements was assessed by calculating the method error for two sets of measurements taken at least 4 weeks apart using the formula of Dahlberg.10 The reliability of the data was evaluated by calculating the intraclass correlation coefficient.11
RESULTS
Twenty-one female and two male patients (mean age, 20.4 ± 2.7 years; range, 18–27 years) were included in the study. Dahlberg's error was less than .5. Paired t-tests indicated no significant difference between the two series of measurements. The intraclass correlation coefficients for all measurements were higher than .90.
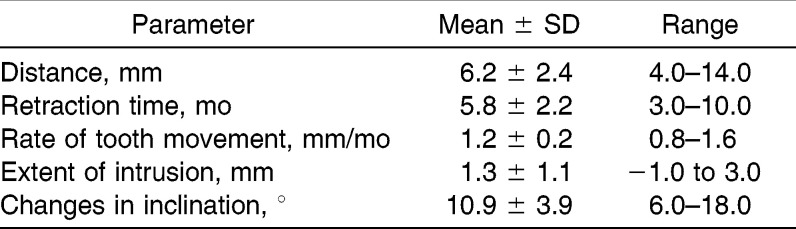
Thirteen patients were retracted with a loop mechanic, and 10 patients were retracted with sliding mechanics. Stainless-steel wire was used for 12 patients, and TMA wire was used for 11 patients. The mean distance, retraction time, rate of tooth movement, extent of intrusion, and change in inclination were 6.2 mm, 5.8 months, 1.2 mm per month, 1.3 mm, and 10.9°, respectively (Table 1).
Table 1.
Means, Standard Deviation, and Ranges of Distance, Retraction Time, Rate of Tooth Movement, Amount of Intrusion, and Changes in Inclination
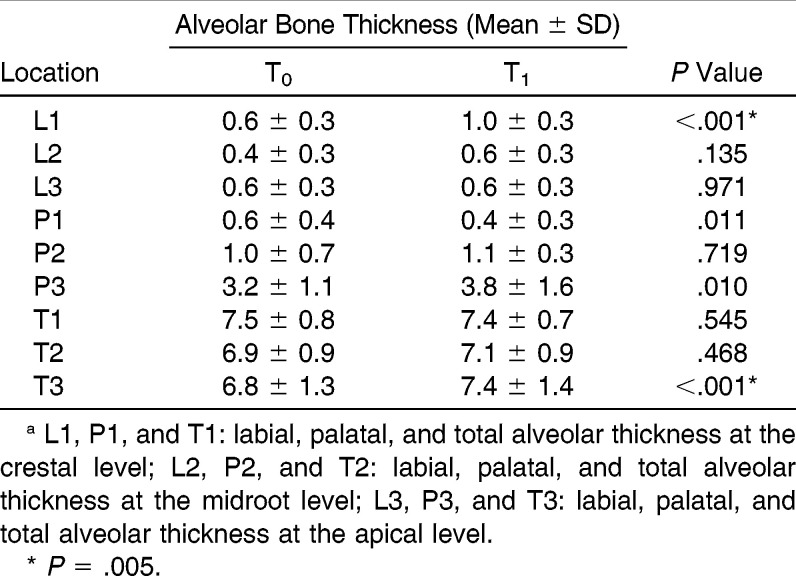
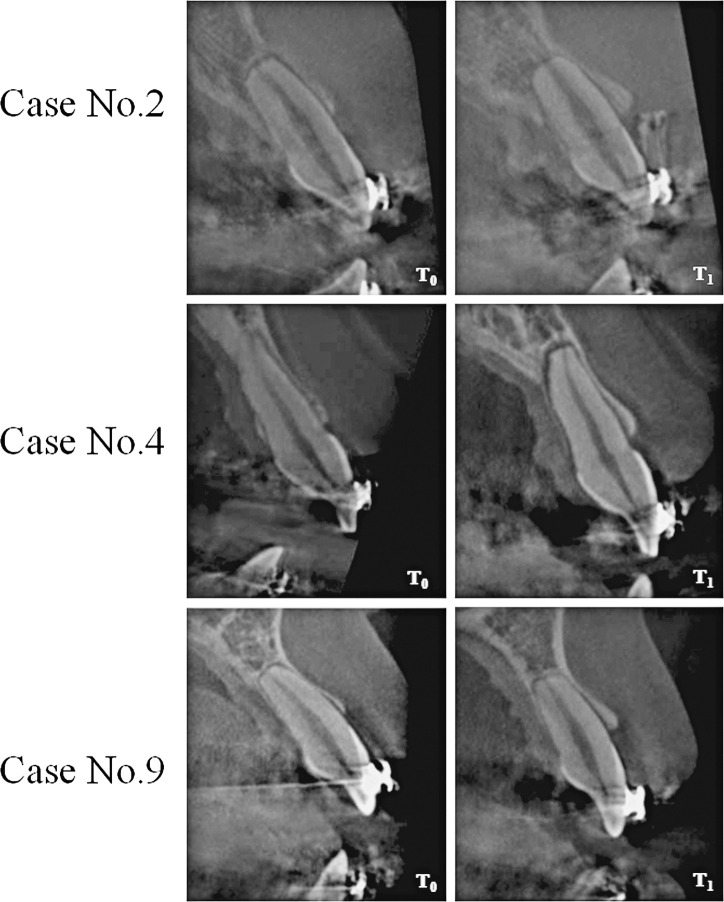
The Shapiro-Wilk test was used to test for normality and demonstrated that the mean alveolar bone thickness values were normally distributed. Paired t-tests were used to compare the difference in mean alveolar bone thickness preretraction (T0) and postretraction (T1). The mean change in alveolar bone thickness of the four upper incisors, as measured from CT scans at T0 to T1, is shown in Table 2 and Figure 5.
Table 2.
Comparison of Mean Alveolar Bone Thickness at T0 and T1 With Paired t-Testa
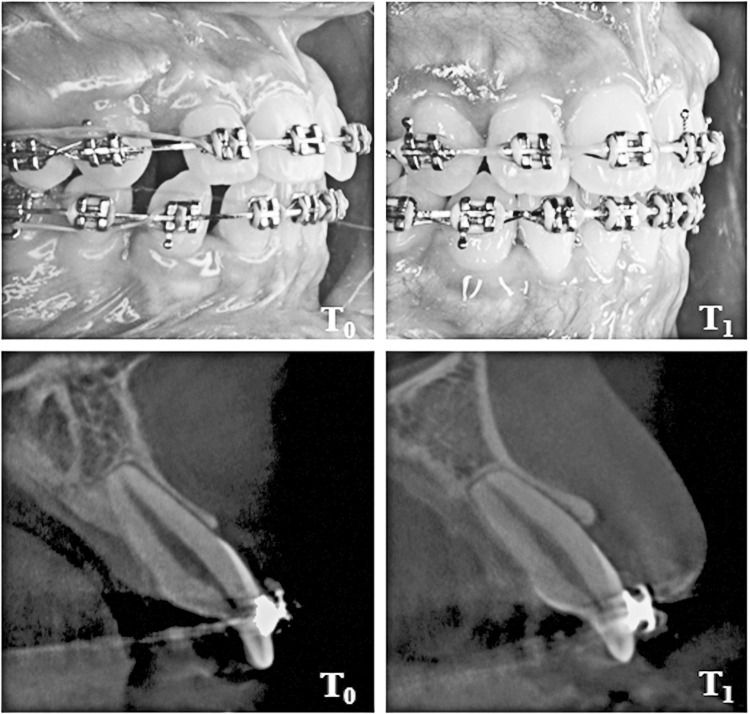
Figure 5.
Changes in alveolar bone thickness at L1 and T3 during incisor retraction.
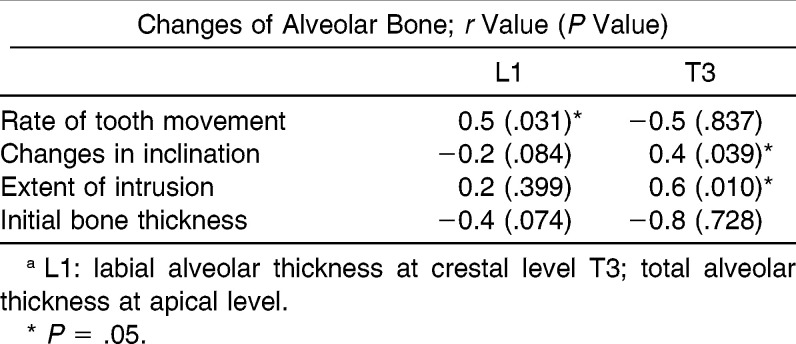
Spearman's rank correlation analysis was applied to identify relationships between the potential influencing factors and the mean alveolar bone changes of the four upper incisors (Table 3).
Table 3.
Correlation Between Mean Changes of Alveolar Bone Thickness and Potential Influencing Factorsa
Alveolar bone thickness changes at L1 demonstrated a strong correlation with the rate of tooth movement (r = .5; P = .031). Alveolar bone thickness changes at T3 showed a strong correlation with the change in inclination and extent of intrusion (r = .4 and .6; P = .039 and .010, respectively). Initial alveolar bone thickness was not significantly correlated with alveolar bone thickness changes (P > .05).
The type of root movement in all subjects could be categorized into two subgroups: retraction of the upper incisors with tipping (11 subjects) and retraction of the upper incisors with torque (12 subjects). Paired t-tests were used to compare the change in alveolar bone thickness between T0 and T1 in both subgroups and demonstrated that both the retraction with tipping group and the retraction with torque group had a significantly increased bone thickness at L1 and T3 during retraction (Table 4).
Table 4.
Comparison of Mean Alveolar Bone Thickness of Four Upper Incisors at T0 and T1 Measurements With Paired t-Test in Subgroupa
When these subgroups were taken into account during Spearman's rank correlation analysis, alveolar bone thickness change at L1 was strongly and positively correlated with the retraction with tipping group (r = .6; P = .006). Conversely, alveolar bone thickness change at L1 was strongly and negatively correlated with the retraction with torque group (r = −.3; P = .031). However, alveolar bone thickness changes at T3 were not significantly correlated with either subgroup (P > .05).
DISCUSSION
Several studies have indicated a lag in bone remodeling in response to tooth movement and reported that as the upper incisors are retracted, labial bone thickness at the crestal level and total alveolar bone thickness at the apical level significantly increase.2–4,12–14 This finding disputes that of De Angelis,1 who presented the bending capacity of alveolar bone. According to De Angelis, mechanotherapy induces alveolar distortion, which alters the electric environment via a process attributed to the piezoelectricity of bone. As a result, theory suggests that highly synchronized, coordinated changes are triggered, and the alveolar bone retains its structural characteristics and size as it moves due to coordinated apposition and resorption.
Our results demonstrated a significant increase in labial bone thickness at the crestal level during upper incisor retraction, in a similar manner to the study of Bimstein et al.,12 which reported that an increase in the amount of buccal alveolar bone may occur as a result of orthodontic treatment, which involves lingual positioning of the procumbent mandibular permanent central incisors. In this study, we observed that a non–statistically significant decrease in palatal bone thickness after upper incisor retraction may be from either shorter retraction time or small samples, in contrast to the results of Sarikaya et al.,2 Vardimon et al.,13 and Wehrbein et al.14
The aim of this study was to determine whether the change in inclination, rate of tooth movement, initial alveolar bone thickness, or the extent of intrusion were related to the change in alveolar bone thickness during upper incisor retraction. Significant correlations were observed between the change in inclination, rate of tooth movement, extent of intrusion, and change in alveolar bone thickness during upper incisor retraction. However, no significant correlation was found between the initial alveolar bone thickness and the change in alveolar bone thickness during upper incisor retraction.
The rate of tooth movement correlated strongly with changes in labial bone thickness at the crestal level L1 (r = .5; P = .031), indicating that the rate of tooth movement is related to alveolar bone thickness changes at L1. A similar finding was observed in the clinical examination of one subject, in whom a protuberance of alveolar bone could be observed close to the gingival margin postretraction (Figure 6). This result is similar to the reports of Mimura3 and Lin et al.4
Figure 6.
A protuberance of alveolar bone near the gingival margin could be observed on clinical examination of one patient during incisor retraction.
This study demonstrates that a rapid rate of incisor retraction increased bone thickness at the labial crestal level. The bone-remodeling process may not be able to keep up with rapid tooth movement; however, our results indicated that total alveolar bone thickness was maintained. It can be interpreted from this observation that the rate of resorption on the labial aspect is relatively slower than the rate of apposition on the lingual aspect (secondary bone remodeling), which may lead to bone prominence. A longitudinal follow-up study would be beneficial to explain the long-term response of alveolar bone to various rates of tooth movement.
Changes in inclination were strongly correlated with changes in total bone thickness at the apical level (T3; r = .4; P = .039), in agreement with the results of Abdwani et al.15 and Nimri et al.,16 who reported that incisal inclination changes during orthodontic treatment result in a change in the position of point A.
The extent of intrusion was strongly correlated with changes in total bone thickness at the apical level (T3; r = .6, P = .010). This observation could be explained by the fact that increased intrusion can be expected to lead to increased alveolar bone changes at the apical level during upper incisor retraction. Moreover, the case report by Mimura3 indicated that the maxillary alveolar process can fail to remodel as the upper anterior teeth are intruded and retracted, leaving behind a prominent labial ridge of bone.
Changes in the total alveolar bone thickness at the apical level were related to the change in inclination and extent of intrusion by the upper incisors. Similarly, Bimstein et al.12 suggested that the change in the alveolar bone height of protruded mandibular permanent incisors may be influenced by the change in angulation between the mandibular plane and the axis of the mandibular central incisors and also by orthodontic intrusion of the teeth. In agreement with this suggestion, a positive correlation was observed between the change in inclination and the extent of intrusion (r = .6; P = .010).
Patients with either tipping or retraction root movement of the upper incisors had a significant increase in both labial bone thickness at the crestal level and total bone thickness at the apical level during retraction. Spearman's rank correlation analysis demonstrated that labial bone thickness at the alveolar crestal level was strongly and positively correlated with the tipping group. Conversely, labial bone thickness at the alveolar crestal level was strongly and negatively correlated with the torque group. This observation could imply that different alveolar bone thickness changes occurred during the different types of root movement when the upper incisors were retracted. It is possible that the retraction forces applied to alveolar bone at the crestal level were different from the retraction forces at the labial and palatal bone in the tipping and torque groups. Moreover, in the retraction with tipping group, the results of orthodontic treatment involved lingual positioning of the incisor edge, which increased labial bone thickness at the alveolar crestal level. However, this technique varies from the guidelines of Vardimon et al.,13 who recommended that a 1∶2 bone remodeling/tooth movement ratio should be used to determine the biocompatible range of orthodontic tooth movements during maxillary incisor retraction with tip or torque movements.
Loop and sliding mechanics were used retract the upper incisors during orthodontic treatment in this study. Mechanics had no significant association with changes in alveolar bone thickness. Moreover, no significant correlation was observed between changes in alveolar bone thickness and the type of wire, retraction time, tooth movement distance, or the sex of the patient (P > .05).
In orthodontic treatment planning for cases requiring retraction of the anterior teeth, the extent of intrusion and change in inclination should be appropriately assessed to prevent a gummy smile or camouflaged cases. In cases at risk of undesirable side effects due to changes in the alveolar bone thickness, surgery may be a more appropriate choice of treatment.
In addition, if the upper incisors were retracted with a rapid rate of tooth movement, the labial alveolar bone thickness increased. The rate of tooth movement must be carefully monitored to avoid undesirable thickening of alveolar bone. Moreover, the risk of alveolar bone loss should be considered during incisor retraction, and the anatomical limitations of the labial and palatal bone on tooth movement should be greatly emphasized.
The limitations of this study should be considered. First, CBCT is unable to produce sufficiently high-resolution images for fine measurement of bone thickness, which questions the reliability and accuracy of the measurement tool itself. Second, bone thickness was evaluated cross-sectionally, whereas remodeling occurs continuously and may be unequal on the apposition and resorption sides. The results of this study cannot explain the continual changes observed in bone thickness during retraction. Finally, long-term changes in bone thickness after orthodontic treatment were not followed up. A longitudinal observation beyond debanding may provide further insight into alveolar bone remodeling throughout the treatment course.
CONCLUSION
Labial bone thickness at the crestal level (L1) and total alveolar bone thickness at the apical level (T3) significantly increased during upper incisor retraction.
The factors related to changes in alveolar bone thickness during incisor retraction were the rate of tooth movement, the degree of inclination change, and the extent of intrusion of the upper incisors.
Acknowledgments
We would like to thank the Graduate School, Faculty of Dentistry, Prince of Songkla University, for grant support and Assistant Professor Dr Udom Thongudomporn for statistical advice.
REFERENCES
- 1.De Angelis V. Observations on the response of alveolar bone to orthodontic force. Am J Orthod. 1970;58:284–294. doi: 10.1016/0002-9416(70)90092-8. [DOI] [PubMed] [Google Scholar]
- 2.Sarikaya S, Haydar B, Ciger S, Ariyurek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 3.Mimura H. Treatment of severe bimaxillary protrusion with miniscrew anchorage: treatment and complication. Aust Ortho J. 2008;24:156–163. [PubMed] [Google Scholar]
- 4.Lin J, Yeh C, Liou E, Bowman S. Treatment of skeletal-origin gummy smile with miniscrew anchorage. J Clin Orthod. 2008;5:285–296. [PubMed] [Google Scholar]
- 5.Fuhrmann RAW, Wehrbein H, Langen HJ, Diedrich PR. Assessment of the dentate alveolar process with high resolution computed tomography. Dentomaxillofac Radiol. 1995;24:50–54. doi: 10.1259/dmfr.24.1.8593909. [DOI] [PubMed] [Google Scholar]
- 6.Maki K, Inou N, Takanishi A, Miller AJ. Computer-assisted simulations in orthodontic diagnosis and the application of a new cone beam x-ray computed tomography. Orthod Craniofac Res. 2003;6(suppl 1):95–101. doi: 10.1034/j.1600-0544.2003.241.x. [DOI] [PubMed] [Google Scholar]
- 7.Lagravere M, Carey J, Toogood R, Major P. Three-dimensional accuracy of measurements made with software on cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2008;134:112–116. doi: 10.1016/j.ajodo.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 8.Hassan B, Setelt P, Sanderink G. Accuracy of three-dimensional measurements obtained from cone beam computed tomography surface-rendered images for cephalometric analysis: influence of patient scanning position. Eur J Orthod. 2008;23:1–6. doi: 10.1093/ejo/cjn088. [DOI] [PubMed] [Google Scholar]
- 9.Rungcharassaeng K, Caruso M, Kan J, et al. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–428.e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 10.Dahlberg G. Statistical Methods for Medical and Biological Students. London, UK: Allen and Unwin; 1940. [Google Scholar]
- 11.Donner A, Zou G. Testing the equality of dependent intraclass correlation coefficients. Statistician. 2002;51:367–379. [Google Scholar]
- 12.Bimstein E, Crevoisier RA, King DL. Changes in the morphology of the buccal alveolar bone of protruded permanent mandibular incisors secondary to orthodontic alignment. Am J Orthod Dentofacial Orthop. 1990;97:427–430. doi: 10.1016/0889-5406(90)70115-s. [DOI] [PubMed] [Google Scholar]
- 13.Vardimon AD, Basset B. Cortical bone remodeling/tooth movement ratio during maxillary incisor retraction with tip versus torque movements. Am J Orthod Dentofacial Orthop. 1998;114:520–529. doi: 10.1016/s0889-5406(98)70172-6. [DOI] [PubMed] [Google Scholar]
- 14.Wehrbein H, Bauer W, Diedrich PR. Mandibular incisors, alveolar bone, and symphysis after orthodontic tooth movement: a retrospective study. Am J Orthod Dentofacial Orthop. 1996;110:239–246. doi: 10.1016/s0889-5406(96)80006-0. [DOI] [PubMed] [Google Scholar]
- 15.Abdwani R, Moles D, Harold Noar J. Change of inclination effects on points A and B. Angle Orthod. 2009;79:462–467. doi: 10.2319/041708-218.1. [DOI] [PubMed] [Google Scholar]
- 16.Nimri K, Hazza A, Omari R. Maxillary incisor proclination effect on the position of point A in Class II division 2 malocclusion. Angle Orthod. 2009;79:880–884. doi: 10.2319/082408-447.1. [DOI] [PubMed] [Google Scholar]