Abstract
Objective:
To compare the changes in incisor inclination between two compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions.
Materials and Methods:
Among Class II malocclusion patients a total of 38 consecutive patients treated with the Xbow appliance and later with full brackets (XB) were compared to 36 consecutive patients treated with Forsus connected to the archwire while on full brackets (FO). Evaluated cephalometric variables were overjet, overbite, skeletal Class II, lower incisor inclination, and upper incisor inclination. Factors that were analyzed were gender, treatment type, age at start of treatment (T1), and treatment length. Independent t-tests, χ2, multiple analysis of variance, and Pearson correlations were applied.
Results:
No differences in incisor inclination between both treatment protocols were identified. At T1 no statistical difference for any cephalometric variable was demonstrated with regard to gender and treatment type. Gender was also not associated with a different treatment time or age at T1. The mean treatment time was 24.2 months for XB and 30.2 months for the FO group (P = .037). XB patients averaged 10 fewer months of fixed edgewise appliances compared to FO patients. Neither gender nor treatment type had any influence on the changes of the evaluated dependent variables between T1 and the end of treatment. Lower incisors proclined more the longer the treatment (P = .005). Both overjet and upper incisor inclination were affected by age at T1 (P = .001 and P = .014, respectively).
Conclusions:
Both compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions appear to generate the same amount of incisor inclination. Large variability was identified.
Keywords: Xbow, Forsus, Incisor inclination
INTRODUCTION
The controversy over lower incisor proclination from treating the Class II nonextraction patient persists today. While some authors1–3 claim that the gingival/periodontal condition is worsened in patients who undergo incisor proclination, others4,5 have found no association between Class II mechanics and gingival recession or bone loss. In this regard Herbst™ appliances, the most popular “bite jumping” Class II correctors, have been studied,6 and no before increase in gingival recession was found in treated adolescents and children. Even considering this, some authors7,8 have suggested avoiding proclining incisors in adults because of a lack of resiliency of these tissues. To consolidate this controversy two systematic reviews9,10 have explored all of the available evidence. Both concluded that there is no strong clinically important association between the degree of incisor proclination and increased gingival recession. The authors of these studies hypothesized that it is the combination of thin attached gingival coverage, poor oral hygiene, and inflammation that facilitates incisal gingival recession when proclining teeth.
In a systematic review11 evaluating treatment changes resulting from Herbst therapy, it was determined that dental changes were more significant than skeletal changes in the final occlusal results. Since most of the correction is dento-alveolar, auxiliary devices that are mainly believed to produce dentoalveolar changes, such as the Forsus™ device, may serve as a good alternative. The Fatigue Resistant Device, more commonly known by its trade name “Forsus,” has gained widespread acceptance in recent years as a replacement for other Class II treatment alternatives while in full fixed edgewise appliances. This device was developed by 3M Unitek (3M Unitek, Monrovia, Calif). Since its introduction in 2001 several modifications12 have been made by the manufacturer to enhance fatigue resistance and improve patient comfort. The development of the Forsus evolved through a combination of trial and error and CAD/CAM technology. When fully compressed, the spring force is approximately 200 g and was designed to correct a Class II malocclusion in 6 months while simultaneously enduring the demanding oral environment. It is mentioned that the available attachment variations makes it universally appealing, easily modified to adapt to various oral sizes and shapes.
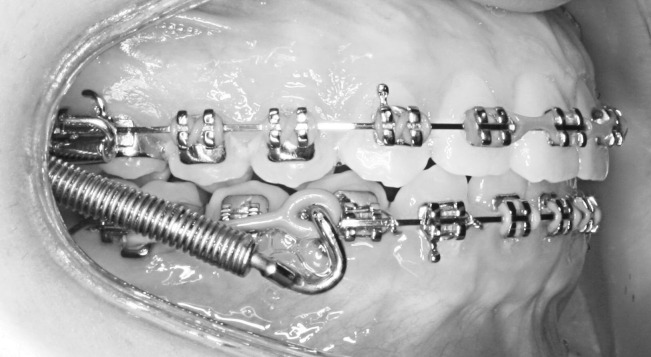
Lately the Forsus spring has been used as the mechanism of force for the Xbow™ Class II corrector (Xbow). The Xbow (pronounced crossbow) is a patented appliance that uses the Forsus springs as a phase 1 appliance for treatment in the late mixed or early permanent dentition.13 In a recent study,14 the Xbow was shown to correct dentally a mild to moderate Class II malocclusion in approximately 4.5 months; then it was removed to allow some musculoskeletal and dental relapse to occur prior to initiation of full fixed edgewise appliances. This result has shown to compare quite favorably with the reported Herbst effects.15 Some control of the lower incisors inclination is believed to be achieved by a low position of the lingual arch and a higher position of the labial arch of the lower framework. Brackets, when indicated, are only used on the maxillary incisors to decompensate the maxillary incisors for the Class II correction by increasing the available OJ (Figure 1), a clinical concept described in the past16 in conjunction with Herbst therapy.
Figure 1.
XBow with brackets on maxillary anterior teeth to decompensate incisors during Class II correction.
The purpose of this study was to compare changes in the incisor inclination between two compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions. The hypothesis of this study was that there is no difference between the two treatment approaches, as measured by five representative cephalometric variables.
MATERIALS AND METHODS
The Human Ethics Research Office at the University of Alberta granted authorization (Pro00023805) for this study. A collection of consecutive treated patients (who were treated with two Forsus methodologies) was available from a private orthodontic practice. These methodologies consisted of a Xbow (Figures 2 through 4) followed by full edgewise appliances or a Forsus used in combination with full brackets for the treatment of mild to moderate Class II nonextraction patients before growth cessation (Figures 5 through 7). A total of 74 patients were used; all were treated by the same experienced orthodontist (with 15 years of experience). This was a retrospective study of 40 consecutively treated Xbow (XB) patients and 40 consecutively cases in which Forsus was connected to the archwire (FO). A total of four patients were later excluded from the FO group and two were excluded from the XB group because they did not meet the age criteria or had missing records, reducing the total sample size in this study to 36 FO patients and 38 XB patients. Both groups had the same brackets (0.022-inch slot, −6° torque in the lower incisors; and 0.019 × 0.025–inch stainless steel (SS) archwire while Forsus was connected in the FO group) and finished with the same finishing occlusal and esthetic objectives.
Figure 2.
XBow maxillary occlusal 4 banded Rapid Palatal Expander with Forsus connected to the Headgear Tube.
Figure 3.
XBow mandibular occlusal view of a lingual arch and labial rail to support the pushrod and the Forsus spring.
Figure 4.
XBow view with Forsus springs fully compressed in a nonpropulsive CR relationship.
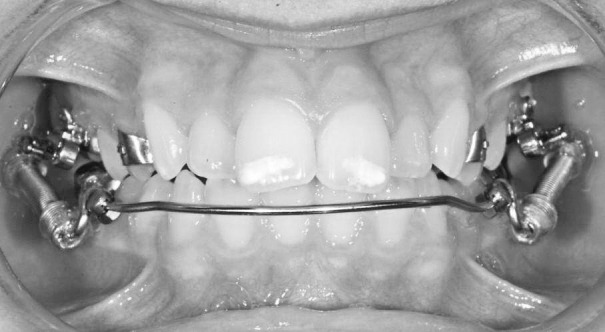
Figure 5.
Forsus connected to the archwire, with modifications for less breakage and improved patient comfort (frontal view).
Figure 6.
Forsus connected to the archwire, with modifications for less breakage and improved patient comfort (lateral view).
Figure 7.
Forsus connected to the archwire, with modifications for less breakage and improved patient comfort (lateral view).
For the XB group, the initial posterior Class II occlusion was overcorrected into a Class III occlusion. Forsus springs were then removed, and a relapse period of approximately 2 to 4 months was followed. No active Class II mechanics were instituted during this period. After this relapse period full edgewise appliance treatment was initiated. If required, intraoral elastics were utilized. If second molars were present a tendency to start as soon as possible applied. In cases in which some significant Class II relapse occurred, the Forsus springs were activated again until satisfactory posterior occlusal correction was attained. For the FO group, the Forsus appliances were inserted after a full-dimensional 0.019 × 0.025–inch SS archwire did express itself. Once 2 mm to 3 mm of Class III overcorrection was attained the springs were removed, and intraoral elastics were used, when indicated. For both groups negative torque was added if clinically required during the finishing stages.
All patients were under the age of 17 years, and their pretreatment (T1) and posttreatment (T2) cephalometric radiographs were taken on the same cephalometric machine (T1 prior to appliance placement and T2 6–8 weeks after all fixed appliances were removed). The cephalometric radiographs were taken on an Instrumentarium OP 100D direct digital radiograph and stored in Dolphin Imaging. All T1 and T2 cephalometric radiographs were coded and transferred via a digital file to an author who realized the measurements. Data for only a few key variables were collected, such as identified as T1 or T2, age at the time of radiograph, concurrent use of a 2 × 4 device, and gender. All cephalometric radiographs were hand-traced with a customized analysis measuring five variables. Cephalometric variables were overjet (OJ), overbite (OB), skeletal Class II (ANB), lower incisor inclination (L1MP), and upper incisor inclination (U1PP). One author digitized all cephalograms used in this study.
Statistics
A reliability study was done whereby a randomly selected sample of 10 radiographs were traced three times with a week between tracings. Distribution of data was shown to be normally distributed. Therefore, parametric tests were used.
An independent Student's t-test was used to determine if treatment length (number of months in orthodontic treatment) and age at start of treatment were different based on treatment groups and gender. A χ2 test was applied to determine if gender distribution was even among treatment groups.
A multiple analysis of variance (MANOVA) was used to assess the differences between and within the cephalometric variables and the evaluated factors (gender, treatment type, age at T1, and treatment time) and their interactions. Finally, Pearson correlations were calculated to further explore the strength of the association when there was a significant difference in the evaluated variables based on the MANOVA.
RESULTS
Reliability results (Intraclass Coefficient) were acceptable, as all were higher than 0.82 (OJ: 0.95; OB: 0.88; L1MP: 0.82; U1PP: 0.97; ANB: 0.84). As a result of the small number of cases (eight cases) that required maxillary incisor decompensation, the initial use of a 2 × 4 appliance in the upper incisors variable was excluded from the analysis.
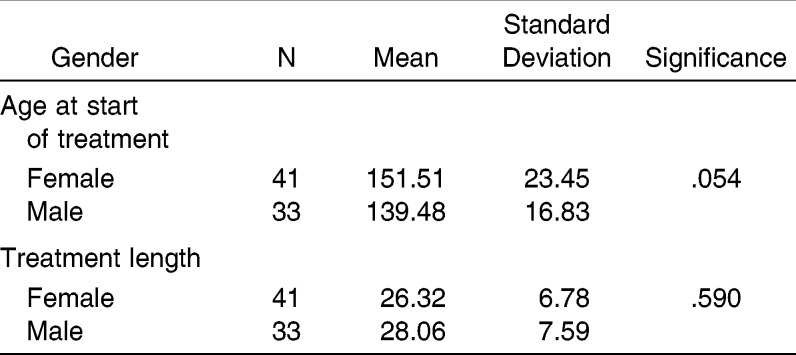
There was no difference in age at the start of treatment based on treatment group (P = .152), but the XB treatment time was around 6 months shorter than the FO treatment time (P = .037) (Table 1). Based on these results, the actual time difference (not between records, as in the statistical analysis) with fixed edgewise appliances on each patient was calculated. The average difference was 10 more months in the FO group (26.75 months FO group vs 16.68 months in the XB group).
Table 1.
Independent t-Test of Treatment Length and Age at Start of Treatment (Months) Between Xbow Appliance and Full Brackets (XB) and Forsus Connected to the Archwire While on Full Brackets (FO) Groups
Gender distribution was even among treatment groups (P = .242). There was no difference in treatment length (P = .590) or age at the start of treatment (P = .054) based on gender (Table 2). Table 3 summarizes the descriptive values of the analyzed cephalometric variables at T1 and at T2 based on treatment type. Differences between T1 and T2 are also reported.
Table 2.
Independent t-Test of Treatment Length and Age at Start of Treatment (Months) Based on Gender
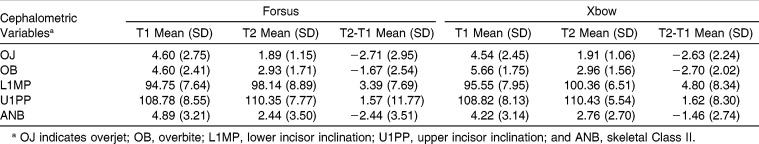
Table 3.
Cephalometric Variables of Pretreatment (T1), Posttreatment (T2), and T2-T1 for Patients in Both Treatment Groups
There were no gender (all P-values greater than .388) or treatment type (all P-values greater than .098) differences in the cephalometric variables at T1. Treatment length only influences L1MP (P = .005). Age at T1 (in months) only influences OJ (P = 0.001) and U1PP (P = .014). Lower incisors procline more the longer the treatment (r = 0.279). Reduction of OJ is greater the younger the patient (r = 0.375). Maxillary incisor inclination is reduced the younger the patient (r = 0.259). The similar trend between these two variables is expected, as they are interrelated.
DISCUSSION
Although many appliance systems that correct a nonextraction Class II malocclusion using dental anchorage exist, one common side effect is proclination of the lower incisors. In this study, we looked at two treatment methods, with the common variable of the Forsus bite jumping spring as the device of force application. Although one clinician treated all of these patients, and despite the fact that all cephalometric radiographs were taken on the same machine, large variability in the cephalometric values was demonstrated. Therefore, the predictability of the treatment results is limited.
The treatment times were shorter for the Xbow patients, by an average of 6 or 10 months, depending how treatment time is measured. With regard to the longer treatment times in the FO group, one explanation is that too many treatment outcomes were tried to be solved at the same time, rendering this approach less efficient than first solving the Class II posterior occlusion and then aligning the teeth, as well as settling the occlusion. These results are similar for the XB group even when considering the 4–6-month relapse period allocated between the Xbow correction and the initiation of full brace treatment.
This study confirms the null hypothesis that the final cephalometric results are not significantly different between both approaches. Therefore, the decision to go with one treatment approach or the other is really a practice management decision. This may support the use of a phase I device that corrects the Class II discrepancy prior to initiation of full fixed edgewise appliances, because the overall treatment is reduced in this sample. This may not be the case for every Class II corrector. In this study, it was reduced by 6 months (the XB group had full brackets for 10 months less than did the FO group). A main expected side effect, lower incisor proclination, happened in both treatment groups, without the change being statistically significant.
The lower incisors procline to about the same degree (XB, 4.8° vs FO, 3.4°), with similar variability (standard deviation = 8°). When in full brackets some17 have suggested that negative torque (−6°) in mandibular incisor brackets will give added resistance to proclination of the lower incisors. Perhaps the longer treatment time with lower incisor negative-torque brackets allows for a better non–statistically significant control of the proclination. L1MP is not only the measure of lower incisor inclination but it could also be considered a measure of torque control in the FO group. As a limitation, it does not measure the bodily movement of the lower incisors. In this sample it could be hypothesized that the negative torque in brackets or archwires to lower anterior teeth influences final incisor position no differently than does the labial/lingual archwire of the XBow, followed by a period of relapse prior to initiation of fixed edgewise appliances.
The XB group did finish with the same type of brackets as the FO group, but the short treatment Xbow phase did not seem to create more treatment from the larger incisor proclination (untoward effect), if it indeed did exist. This can be explained by dento-alveolar rebound prior to the application of fixed edgewise appliances. In both treatment groups the mandibular dento-alveolus moves mesially and the lower incisors procline and then rebound after spring removal, as found previously.18 This pattern has also been shown for the Herbst.6,19 Leveling the Curve of Spee is another explanation, as it often flares the lower incisors. In a recent study20 it was shown that lower incisors flare 4° for each millimeter of ‘flattening’ of the Curve of Spee. There are two clinical side effects in the FO group that did not occur in the XB group. They include occlusal plane canting when used unilaterally and buccal flaring of the upper molars. This could possibly explain the longer treatment times in the FO group. This was not specifically quantified in this study and should be a topic of future studies.
There are a few published reports14,21 evaluating lower incisor changes using the Forsus device, and they report changes in the 3°–5° range. Similar lower incisor proclination changes have been shown with Class II elastics,22 where it was claimed that the overall differences were clinically insignificant when compared to those of the Forsus device. In a recent study23 the Twin Block, MARA, Herbst, and bionator devices were compared, and although short-term incisor proclination was worse for the Twin Block group, no significant long-term changes were observed between the four treatment groups. Other studies show similar short-term results when observing lower incisor changes. With the cantilever Herbst design17 was used the mandibular incisors proclined an average of 6.6°. Furthermore, the authors stated that mandibular growth was in the 1-mm range, consistent with the findings in a published systemic review11 on changes from Herbst therapy. Favorable skeletal and dental changes from Forsus to the archwire group have been reported24 when compared to an untreated control, but these results exhibited a large amount of proclination (5.2°) and forward movement (2.5 mm). The treated group also used similar −6° torque lower incisor brackets and a 0.019 × 0.025–inch SS archwire, which were the same clinical criteria used in our study.
CONCLUSIONS
Both compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions appear to generate the same amount of incisor inclination. Large variability was identified.
The older the patient, the more overjet and upper incisor inclination remains at the conclusion of treatment.
The longer the treatment time, the more the lower incisors procline.
The Xbow protocol averaged 6 fewer months of overall treatment and 10 fewer months of fixed edgewise appliances compared to the Forsus protocol.
REFERENCES
- 1.Årtun J, Krogsyad O. Periodontal status of mandibular incisors following excessive proclination: a study in adults with surgically treated mandibular prognathism. Am J Orthod Dentofacial Orthop. 1987;91:225–232. doi: 10.1016/0889-5406(87)90450-1. [DOI] [PubMed] [Google Scholar]
- 2.Coatoam GW, Behrents RG, Bissada NF. The width of keratinized gingiva during orthodontic treatment. Its significance and impact on periodontal status. J Periodontol. 1981;52:307–313. doi: 10.1902/jop.1981.52.6.307. [DOI] [PubMed] [Google Scholar]
- 3.Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod. 1978;74:286–297. doi: 10.1016/0002-9416(78)90204-x. [DOI] [PubMed] [Google Scholar]
- 4.Kloehn JS, Pfeifer JS. The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44:127–134. doi: 10.1043/0003-3219(1974)044<0127:TEOOTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Busschop JL, Van Vleirberghe M, De Boever J, Dermaut L. The width of the attached gingiva during orthodontic treatment: a clinical study in human patients. Am J Orthod. 1985;87:224–229. doi: 10.1016/0002-9416(85)90043-0. [DOI] [PubMed] [Google Scholar]
- 6.Ruf S, Hansen K, Pancherz H. Does orthodontic proclination of lower incisors in children and adolescents cause gingival recession. Am J Orthod Dentofacial Orthop. 1998;114:100–106. doi: 10.1016/s0889-5406(98)70244-6. [DOI] [PubMed] [Google Scholar]
- 7.Maynard JG, Jr, Ochsenbein C. Mucogingival problems: prevalence and therapy in children. J Periodontol. 1975;46:543–552. doi: 10.1902/jop.1975.46.9.543. [DOI] [PubMed] [Google Scholar]
- 8.Andlin-Sobocki A, Persson M. The association between spontaneous reversal of gingival recession in mandibular incisors and dentofacial changes in children: a 3-year longitudinal study. Eur J Orthod. 1994;16:229–239. doi: 10.1093/ejo/16.3.229. [DOI] [PubMed] [Google Scholar]
- 9.Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. Orthod Craniofac Res. 2010;13:127–141. doi: 10.1111/j.1601-6343.2010.01491.x. [DOI] [PubMed] [Google Scholar]
- 10.Aziz T, Flores-Mir C. A systematic review of the association between appliance-induced labial movement of mandibular incisors and gingival recession. Aust Orthod J. 2011;27:33–39. [PubMed] [Google Scholar]
- 11.Flores-Mir C, Ayehc A, Goswanic A, Charkhandehc S. Skeletal and dental changes in Class II Division 1 malocclusions treated with splint-type Herbst appliances: a systematic review. Angle Orthod. 2007;77:376–380. doi: 10.2319/0003-3219(2007)077[0376:SADCIC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Cleary J. The Forsus™ Fatigue Resistant Device 10 years at hard labor (and still going strong) Orthod Perspect. 2011;18:11–12. [Google Scholar]
- 13.Higgins DW. Xbow™. Available at: http://www.crossboworthodontic.com Accessed June 27, 2012.
- 14.Flores-Mir C, Barnett G, Higgins DW, Heo G, Major PW. Short-term skeletal and dental effects of the Xbow appliance as measured on lateral cephalograms. Am J Orthod Dentofacial Orthop. 2009;136:822–832. doi: 10.1016/j.ajodo.2008.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Pancherz H. The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Semin Orthod. 1997;3:232–243. doi: 10.1016/s1073-8746(97)80056-4. [DOI] [PubMed] [Google Scholar]
- 16.Obijou C, Pancherz H. Herbst appliance treatment of Class II, Division 2 malocclusions. Am J Orthod Dentofacial Orthop. 1997;112:287–291. doi: 10.1016/S0889-5406(97)70258-0. [DOI] [PubMed] [Google Scholar]
- 17.Vogt W. The Forsus Fatigue Resistant Device. J Clin Orthod. 2006;40:368–377. [PubMed] [Google Scholar]
- 18.Barnett G, Higgins D, Major P, Flores-Mir C. Immediate skeletal and dentoalveolar effects of the crown- or banded type Herbst appliance on Class II Division 1 malocclusion. Angle Orthod. 2008;78:361–369. doi: 10.2319/031107-123.1. [DOI] [PubMed] [Google Scholar]
- 19.Moro A, Janson G, de Freitas MR, Henriques JF, Petrelli NE, Lauris JP. Class II correction with the Cantilever Bite Jumper. Angle Orthod. 2009;79:221–229. doi: 10.2319/121807-591.1. [DOI] [PubMed] [Google Scholar]
- 20.Pandis N, Polychronopoulou A, Sifakakis I, Makou M, Eliades T. Effects of levelling of the Curve of Spee on the proclination of mandibular incisors and expansion of dental arches: a prospective clinical trial. Aust Orthod J. 2010;26:61–65. [PubMed] [Google Scholar]
- 21.Aziz T, Nassar U, Flores-Mir C. Prediction of lower incisor proclination during Xbow treatment based on initial cephalometric variables. Angle Orthod. 2012;82:472–479. doi: 10.2319/072311-465.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 23.Siara-Olds N, Pagrazio-Kulbersh V, Berger J, Bayirli B. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthod. 2010;80:18–29. doi: 10.2319/020109-11.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franchia L, Alvetro L, Giuntinic V, Masuccid C, Defraiae E, Baccetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]