Abstract
Objective
To understand whether the Comprehensive Care for Joint Replacement (CJR) program induces participating hospitals to (1) preferentially select lower risk patients, (2) reduce 90‐day episode‐of‐care costs, (3) improve quality of care, and (4) achieve greater cost reduction during its second year, when downside financial risk was applied.
Data sources
We identified beneficiaries of age 65 years or older undergoing hip or knee joint replacement in the 100% sample of Medicare fee‐for‐service inpatient (Part A) claims from January 1, 2013 to August 31, 2017. Cases were linked to subsequent outpatient, Part B, home health agency, and skilled nursing facility claims, as well as publicly available participation status for CJR.
Study design
We estimated the effect of CJR for hospitals in the 67 metropolitan statistical areas (MSA) selected to participate in CJR (785 hospitals), compared to those in 104 non‐CJR MSAs (962 hospitals; maintaining fee‐for‐service). A difference‐in‐differences approach was used to detect patient selection, as well as to compare 90‐day episode‐of‐care costs and quality of care between CJR and non‐CJR hospitals over the first two performance years.
Data collection
We excluded 172 hospitals from our analysis due to their preexisting BPCI participation. We focused on elective admissions in the main analysis.
Principal findings
While reductions in 90‐day episode‐of‐care costs were greater among CJR hospitals (−$902, 95% CI: −$1305, −$499), largely driven by a 16.8% (p < 0.01) decline in 90‐day spending in skilled nursing facilities, CJR hospitals significantly reduced the 90‐day readmission rate (−3.9%; p < 0.05) and preferentially avoided patients aged 85 years or older (−5.9%; p < 0.01) and Black (−7.0%; p < 0.01). Cost reduction was greater in 2017 than in 2016, corresponding to the start of downside risk.
Conclusions
Participation in CJR was associated with a modest cost reduction and a reduction in 90‐day readmission rates; however, we also observed evidence of preferential avoidance of older patients perceived as being higher risk among CJR hospitals.
Keywords: bundled payment program, Centers for Medicare and Medicaid Services, Comprehensive Care for Joint Replacement model, Medicare, patient selection
What is known on this topic
The Comprehensive Care for Joint Replacement model (CJR) modestly reduces Medicare spending without harming quality.
There is sparse evidence of the effect of CJR on patient selection.
What this study adds
Focusing on elective admission, for which providers might have more discretion to select a healthier patient, we found that CJR hospitals avoided older patients who are more likely to be perceived as being a higher risk.
Compared to non‐CJR hospitals, CJR hospitals preferentially selected fewer Black patients for elective admissions, which may reflect racial disparities in health and access to health care.
1. INTRODUCTION
The Center for Medicare and Medicaid Innovation (CMMI), under the Centers for Medicare and Medicaid Services (CMS), launched the Comprehensive Care for Joint Replacement model (CJR), a mandatory 90‐day bundled payment program for lower extremity joint replacement (LEJR), on April 1, 2016. 1 CMS mandated that all hospitals paid under the Inpatient Prospective Payment System (IPPS) in 67 randomly selected metropolitan statistical areas (MSA; defined as having at least one urbanized area with a minimum population of 50,000) adopt episode‐based bundled payments for LEJR, except for some already participating in the voluntary bundled payment for care improvement (BPCI) program for LEJR. 2
Through an annual reconciliation, CJR provides a financial incentive for participating hospitals to reduce fee‐for‐service (FFS) spending and to improve quality. 3 Specifically, over 5 years, participating hospitals receive a reconciliation payment if the sum of their actual LEJR‐related episode‐of‐care spending (extending through the 90 days following discharge) is less than a contracted target price. The target price is established by CMS based on a weighting of each hospital's own historical spending and a regional spending target. In addition, hospitals must maintain a certain level of quality. If they fail to meet a minimum of 5.0 on a composite quality score based on a complication (50%), a patient satisfaction survey (40%), and a patient reported outcome (PRO) (10%), they would not be able to receive a reconciliation payment. On the other hand, hospitals with actual episode payments that exceed the target price must pay the difference back to Medicare. Stop‐loss/stop‐gain provisions cap the amount that hospitals can gain or lose. During the first two performance years, stop‐gain was 5% of the target price. Stop‐loss was 5% of the target price during the second year, without downside risk in the first year.
This form of an incentive allows CJR participant hospitals to achieve greater cost reduction compared to non‐CJR hospitals. According to the Lewin Group, after accounting for the reconciliation payment to hospitals, CJR episode payments decreased by $17.4 million or 0.5% (compared to the baseline mean) without compromising patient care in the first two performance years. 4 However, this also raised concerns about unintended consequences. Specifically, under a bundled payment model, some hospitals might avoid treating patients who are older, frailer, have greater comorbidity, and represent more complex pathology because they represent greater financial risk (“lemon dropping”), or they might want to treat only younger and healthier patients in order to maximize their revenue (“cherry picking”). 5 , 6 Sparse evidence of these concerns exists in early evaluations. 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 Most studies show that CJR reduced Medicare spending without evidence of harm to quality, 7 , 8 , 9 , 10 , 11 and there is little or no evidence of unintended effects such as preferential patient selection. 5 , 6 , 7
However, previous studies ignored the fact that the type of admission (elective vs. emergency department [ED]) could affect providers' decision to admit a patient and manage the corresponding financial risk in a bundled payment. For example, the Emergency Medical Treatment and Active Labor Act (EMTALA) requires hospitals to provide emergency medical care to all patients regardless of their ability to pay, 12 while with elective admissions, providers have more discretion to select patients. In addition, compared to ED or urgent admissions, patients admitted through elective admission often have fewer comorbidities, 13 so that providers might have more ability to select healthier patients. Thus, in order to find the causal relationships between CJR and patient selection, our analysis focused on elective admission.
In this study, we sought to provide empirical evidence of CJR's impact not only on patient selection but also on costs and quality of care during the first 2 years of the program, particularly focusing on elective admissions. We hypothesized that CJR would induce participating hospitals to (1) preferentially select lower risk patients, (2) reduce 90‐day episode‐of‐care costs, (3) improve quality of care, and (4) achieve greater cost reduction during the second year, when downside financial risk was applied.
2. METHODS
2.1. Study design
We performed a retrospective analysis of Medicare beneficiaries undergoing LEJR (diagnosis‐related group [DRG] 469 or DRG 470) using Medicare claims from 2013 to 2017. In July 2015, CMS initially announced that 75 MSAs were randomly selected to the reimbursement model, and 121 MSAs would serve as a control (maintaining FFS). However, on November 2015, CMS further excluded 25 MSAs due to BPCI participation.
The remaining 171 MSAs were eligible for CJR, and CMS randomly selected 67 to participate in the CJR model, with 104 MSAs designated as controls. Importantly, the random selection of CJR participant and nonparticipant MSA occurred after the exclusion of the 25 MSAs. 14 Unlike previous studies, 7 , 8 , 9 , 10 we based our analysis on the final MSA list (171 MSAs), applying the revised criteria to exactly identify those subject to the policy. 2 Thus, we estimated the average treatment on the treated effect (ATT), the average effect of CJR for hospitals in the 67 MSAs selected to participate in CJR, compared to those in 104 non‐CJR MSAs. 15
Initially we focused on elective admission, which excluded “emergency” and “urgent” cases. Then, we employed a difference‐in‐differences method (DID) to detect patient selection, as well as to compare overall 90‐day episode‐of‐care cost and quality of care between CJR participant and nonparticipant hospitals over the first two performance years. We also estimated the effects by year to see if they change over time since in 2017; CJR hospitals were exposed to downside risk, in which hospitals whose actual episode payments exceeded the target price had to pay the difference, up to 5% of the target price, back to Medicare. Finally, we performed a subgroup analysis to understand the effect among ED/urgent admissions.
CMS conducted a randomized block design by dividing eligible MSAs into eight strata based on median MSA population and historical spending for LEJR before the implementation of the CJR model. 2 MSAs within each stratum have the same probability of being selected for the CJR policy, while MSAs across strata have a different probability of treatment. By mandating hospital participation, CJR overcame the problem of noncompliance common in randomized trials. 15
Although randomization and mandatory participation help reduce selection in participation bias under CJR, subsequent changes in CJR could influence CJR hospitals' behavior that might be correlated with the outcomes. Since a DID analysis cannot remove bias caused by this sort of time‐varying factors, we excluded two intervening periods to account for these idiosyncratic temporary shocks 16 (known as “Ashenfelter's dip”). First, we omitted the period from July 2015 to April 2016, corresponding to the time that CJR hospitals may have changed practices after the policy was announced in July 2015 but prior to risk bearing. Second, because CMS announced a revision of CJR in September 2017 and in order to ensure 90 days of surveillance, we excluded the period following September 2017. In summary, preintervention period was from January 2013 through June 2015 and our policy period extended from May 2016 through August 2017.
2.2. Data and outcomes
Medicare claims were accessed through the Virtual Research Data Center (VRDC). 17 We identified beneficiaries aged 65 years or older undergoing major joint replacement of the lower extremity (DRG 469 or DRG 470) using 100% sample of Medicare FFS inpatient claims, excluding beneficiaries eligible for Medicare via end‐stage renal disease (ESRD), or who had Medicare Health Maintenance Organizations (HMO) (e.g., Advantage). Social Security Disability Insurance (SSDI) was also excluded except where it was used to examine patient selection. We further restricted the analytical data to each beneficiary's first instance of LEJR during the study period so that each beneficiary is only represented once in the analysis. For each index case thus observed, we then summed the costs for the index admission, along with all subsequent hospital inpatient, hospital outpatient, Part B, home health agency, skilled nursing facility (SNF), and durable medical equipment claims occurring with 90‐days of discharge. We did not include pharmacy or out‐of‐pocket expenditures. All costs were adjusted to their 2017 equivalents using the Implicit Price GDP Deflator. 18
We collected information of each patient's age, gender, and race as well as quality measures, such as 90‐day readmission in each hospital from Medicare claims. In addition, we used the International Classification of Diseases version 9 or 10 (ICD‐9/10) to create variables reflecting comorbidity (Charlson Comorbidity Index [CCI]) and surgical complications (pulmonary embolism (PE), and deep vein thrombosis (DVT)).
The primary outcomes of selection were patients' characteristics (age, race, and gender), comorbidity (e.g., CCI), and disability entitlement (e.g., SSDI). Economic outcomes includes 90‐day episode‐of‐care costs (total 90‐day episode costs, postacute care costs), and 90‐day all‐cause readmission. Secondary outcomes included length of stay, LEJR procedure volume (a monthly rate), 30/90‐day mortality, and surgical complication rate as measured by PE and DVT.
The Annual Survey of the American Hospital Association (AHA) was used to describe hospital volume and geographical information.
2.3. Statistical analysis
In order to compare pre‐versus‐post patient characteristics as well as 90‐day episode‐of‐care cost and quality of care between CJR participant and nonparticipant hospitals, we performed a DID analysis at the MSA level. For continuous outcome variables such as cost, length of stay, or procedure volume, ordinary least square (OLS) models were used, 19 while probit models were employed for binary dependent variables such as age group indicators, race, gender, 90‐day readmission, 30‐/90‐day mortality, or surgical complications (e.g., PE and DVT). For cost outcomes, we also performed a generalized linear model (GLM) since the cost data were positively skewed. 20 Because the results produced from OLS and GLM were similar, we ultimately decided to report OLS since it is a more efficient approach to predict the mean cost. 21
The DID estimator can be obtained from the estimated coefficient on the interaction of two indicator variables: (1) whether the MSA is in the mandated policy group (67 MSAs) and (2) whether the index case occurred after April 2016, when CJR was initiated. In our regression models, we included hospital and MSA‐fixed effects to control for time‐invariant differences that might be correlated with the outcome variables, and we added year‐fixed effects to account for macroeconomic changes that could also be correlated with the outcomes. All regressions included strata‐specific fixed effects since, as described in the Study Design section, each stratum has a different probability of being selected. In additional analysis, we added variables to identify the effect of CJR in 2017 separately from that in 2016. This allowed us to estimate the effect of CJR by year (e.g., the effect of CJR in 2016 and in 2017). All regressions except for those estimating patient selection included patient‐level covariates for age, gender, race, and comorbidity because these covariates might be correlated with our outcomes of interest (see Appendix A for details). All standard errors were clustered by MSAs. 22
Stata version 16.1‐MP (StataCorp) was used to conduct analysis. All results are reported with 2‐tailed tests with a statistical significance threshold of p < 0.05. This study was approved by the institutional review board of the University of Utah.
3. RESULTS
3.1. Primary analysis of elective admissions
3.1.1. Study population
Our primary analysis of elective admissions included 785 CJR participant hospitals in 67 MSAs and a non‐CJR comparison group of 962 hospitals in 104 MSAs. Among 1747 hospitals, we excluded 172 hospitals from our analysis due to their preexisting BPCI participation. There were 694,275 eligible beneficiaries undergoing LEJR from January 1, 2013, to August 31, 2017. Specifically, there are 471,651 patients during the preintervention period of January 2013 through June 2015 and 222,624 in the postpolicy period from May 2016 to August 2017.
3.1.2. Influence of patient selection
Table 1 shows descriptive statistics for elective admission by hospital CJR participation status, before and after the implementation of CJR, respectively. Overall, the average age of LEJR patients in prepolicy era was older than the post policy.
TABLE 1.
Descriptive statistics for elective admissions
| Variables | Prepolicy periods | Postpolicy periods | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| All admissions | CJR | Non‐CJR | p value | All admissions | CJR | Non‐CJR | p value | |
| Total 90‐day episode costs | $24,717 | $25,492 | $24,150 | <0.001 | $21,430 | $21,659 | $21,271 | <0.001 |
| SNF 90‐day costs | $3445 | $3663 | $3285 | <0.001 | $2117 | $2089 | $2137 | <0.001 |
| Inpatient costs (index procedures) | $13,324 | $13,589 | $13,130 | <0.001 | $12,352 | $12,540 | $12,220 | 0.039 |
| Outpatient 90‐day costs | $635 | $624 | $643 | <0.001 | $657 | $651 | $662 | 0.097 |
| Durable medical equipment | $124 | $128 | $120 | <0.001 | $92 | $91 | $92 | 0.759 |
| Home health agency | $2195 | $2242 | $2160 | <0.001 | $2042 | $2122 | $1986 | <0.001 |
| BPCI inpatient 90‐day costs | $1034 | $1070 | $1007 | <0.001 | $961 | $989 | $940 | 0.038 |
| BPCI Part B 90‐day costs | $2983 | $3040 | $2941 | <0.001 | $2748 | $2793 | $2717 | <0.001 |
| Length of stay (days) | 3.67 | 3.66 | 3.68 | 0.180 | 3.31 | 3.17 | 3.41 | <0.001 |
| Number of episode a | 361 | 326 | 385 | <0.001 | 380 | 328 | 416 | <0.001 |
| Mortality (30 days) | 0.23% | 0.25% | 0.22% | 0.045 | 0.20% | 0.20% | 0.19% | 0.869 |
| Mortality (90 days) | 0.48% | 0.50% | 0.47% | 0.130 | 0.40% | 0.40% | 0.40% | 0.870 |
| 90‐day readmission (any reasons) | 9.74% | 9.69% | 9.77% | 0.330 | 9.29% | 9.10% | 9.42% | 0.010 |
| PE | 2.43% | 2.34% | 2.49% | 0.001 | 2.04% | 1.97% | 2.09% | 0.060 |
| DVT | 5.01% | 5.01% | 5.01% | 0.975 | 4.50% | 4.51% | 4.49% | 0.762 |
| Age | 74.08 | 74.17 | 74.02 | <0.001 | 73.71 | 73.75 | 73.69 | 0.023 |
| Female | 62.82% | 63.16% | 62.58% | <0.001 | 61.99% | 62.37% | 61.73% | 0.002 |
| White | 91.19% | 90.54% | 91.66% | <0.001 | 90.32% | 89.79% | 90.70% | <0.001 |
| Black | 4.78% | 4.83% | 4.74% | 0.184 | 4.70% | 4.58% | 4.78% | 0.026 |
| Disabled | 0.70% | 0.68% | 0.71% | 0.445 | 0.63% | 0.61% | 0.65% | 0.349 |
| CCI of 0 | 55.4% | 55.4% | 55.3% | 0.553 | 55.5% | 55.0% | 55.9% | <0.001 |
| CCI of 1 | 26.7% | 26.5% | 26.8% | 0.024 | 25.4% | 25.5% | 25.3% | 0.170 |
| CCI of 2 or higher | 17.9% | 18.1% | 17.9% | 0.067 | 19.1% | 19.4% | 18.9% | <0.001 |
| Age 65–69 years | 28.8% | 28.5% | 29.0% | <0.001 | 30.4% | 30.4% | 30.4% | 0.713 |
| Age 70–74 years | 28.4% | 28.1% | 28.6% | <0.001 | 29.5% | 29.1% | 29.8% | <0.001 |
| Age 75–79 years | 22.1% | 22.3% | 22.0% | 0.038 | 21.6% | 21.7% | 21.5% | 0.425 |
| Age 80–84 years | 13.6% | 13.9% | 13.4% | <0.001 | 12.3% | 12.6% | 12.1% | 0.002 |
| Age 85 years or older | 7.1% | 7.2% | 6.9% | <0.001 | 6.2% | 6.3% | 6.2% | 0.554 |
| Dual eligibility | 6.5% | 7.3% | 6.0% | <0.001 | 5.9% | 6.7% | 5.3% | <0.001 |
| DRG 469 | 2.5% | 2.7% | 2.4% | <0.001 | 2.2% | 2.3% | 2.0% | <0.001 |
| DRG 470 | 97.5% | 97.3% | 97.6% | <0.001 | 97.8% | 97.7% | 98.0% | <0.001 |
| N | 471,651 | 199,251 | 272,400 | 222,624 | 91,554 | 131,070 | ||
Note: Only prepolicy periods included (January 2013–June 2015). Cost variables were adjusted for inflation (2017 dollar value). DRG 469 represents major joint replacement with major complication and DRG 470 represents major joint replacement without major complication.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DRG, diagnosis‐related group; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
The mean volume in each prepolicy and postpolicy was calculated using an identical length of time and accounted for seasonality.
Table 2 provides estimated coefficients from our DID analysis. CJR hospitals significantly selected younger (−0.13 years or −0.17% compared to mean, 95% CI: −0.23, −0.026 years; p = 0.0140), more White (0.35 percentage points [ppts] or 0.38% compared to mean, 95% CI: 0.06, 0.64 ppts; p = 0.0178), and fewer Black patients (−0.34 ppts or −6.98% compared to mean, 95% CI: −0.57, −0.11 ppts; p = 0.0039), while there is no statistical difference in patient selection based on gender (female, 0.10 ppts or 0.16% compared to mean, 95% CI: −0.48, 0.6 ppts; p = 0.7252), CCI (1.1 or 1.5% compared to mean, 95% CI: −0.14, 0.36; p = 0.3827), or disability status (−0.22 ppts or −31.9% compared to mean, 95% CI: −0.54, 0.09 ppts; p = 0.1683) between CJR participant and nonparticipant hospitals. We also explored heterogeneity across age groups. We found that the decrease in average age of patients in CJR hospitals was achieved through reducing the volume of procedures for those 85 years or older (the probability of being treated decreased by 0.41 ppts or by 5.9% compared to mean, 95% CI: −0.72, −0.10 ppts; p = 0.0098). If these CJR selection effects were extrapolated to all hospitals, more than 6600 fewer patients per year would undergo LEJR due to avoidance of 85+‐year‐olds. 23
TABLE 2.
Overall effect of CJR for elective admissions and the effects by years
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | −0.13* (0.0140) | −0.12* (0.0380) | −0.14* (0.0218) |
| Female | 0.0010 (0.7252) | 0.0026 (0.4537) | −0.0061 (0.8783) |
| White | 0.0035* (0.0178) | 0.0047* (0.0100) | 0.0024 (0.1952) |
| Black | −0.0034** (0.0039) | −0.0040* (0.0130) | −0.0029* (0.0339) |
| Disabled | −0.0022 (0.1683) | 0.00044 (0.8534) | −0.0037* (0.0373) |
| CCI (mean) | 0.011 (0.3827) | 0.013 (0.3187) | 0.008 (0.6018) |
| CCI of 0 | −0.0036 (0.3889) | −0.0040 (0.4203) | −0.0033 (0.4745) |
| CCI of 1 | 0.0025 (0.3771) | 0.0023 (0.5060) | 0.0028 (0.3910) |
| CCI of 2 or higher | 0.00058 (0.8754) | 0.0012 (0.7632) | −0.00011 (0.9950) |
| Age 65–69 years | 0.0066 (0.0619) | 0.0066 (0.0684) | 0.0067 (0.1267) |
| Age 70–74 years | −0.00052 (0.8601) | −0.00031 (0.9293) | −0.00074 (0.8355) |
| Age 75–79 years | −0.00029 (0.9173) | −0.0015 (0.6327) | 0.00088 (0.8048) |
| Age 80–84 years | −0.0011 (0.5725) | −0.00077 (0.7426) | −0.0013 (0.5668) |
| Age 85 years or older | −0.0041** (0.0098) | −0.0035 (0.0674) | −0.0049* (0.0116) |
| Cost outcomes | |||
| Total 90‐day episode costs | −902*** (0.0000) | −785*** (0.0000) | −1017*** (0.0000) |
| SNF 90‐day costs | −499** (0.0037) | −431** (0.0061) | −565** (0.0030) |
| Inpatient costs (index procedure) | −151 (0.0578) | −116 (0.1712) | −185* (0.0200) |
| Outpatient 90‐day costs | 14.7 (0.1871) | 4.6 (0.7132) | 24.9 (0.0575) |
| Durable medical equipment 90‐day costs | −4.7 (0.3514) | −6.0 (0.2284) | −3.2 (0.5801) |
| Home health agency 90‐day costs | 28.5 (0.8061) | 54.7 (0.6139) | 2.9 (0.9818) |
| BPCI inpatient 90‐day costs | −8.8 (0.7570) | −6.2 (0.8777) | −11.4 (0.7599) |
| BPCI Part B 90‐day costs | −20.9 (0.4653) | −20.3 (0.4798) | −20.3 (0.5059) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.0037* (0.0294) | −0.0036 (0.0911) | −0.0037 (0.1036) |
| Mortality (30 days) | −0.00025 (0.4824) | −0.00018 (0.7024) | −0.00034 (0.4270) |
| Mortality (90 days) | −0.00022 (0.5651) | −0.00022 (0.6734) | −0.00021 (0.6938) |
| PE | 0.00052 (0.6267) | 0.00039 (0.7337) | 0.00073 (0.5905) |
| DVT | 0.00084 (0.6080) | −0.000081 (0.9646) | 0.00175 (0.3549) |
| Volume | |||
| Length of stay (day) | −0.20 (0.3223) | −0.27 (0.1745) | −0.14 (0.5442) |
| Number of episode | −0.65 (0.2042) | −0.51 (0.4893) | −0.79 (0.2045) |
| SNF utilization | |||
| Discharge to SNF | −0.021* (0.0281) | −0.018* (0.0492) | −0.024* (0.0240) |
| SNF duration (day) | −0.58** (0.0051) | −0.51** (0.0083) | −0.64** (0.0042) |
Note: Column 1 represents difference in differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference‐in‐differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
3.1.3. Influence of costs
Costs were greater in nearly all categories during the pre‐CJR versus post‐CJR years. Compared to non‐CJR hospitals, CJR hospitals had greater cost before the implementation and greater reductions in costs after the policy (Table 1). Compared to non‐CJR hospitals, CJR was associated with a significant decrease in 90‐day episode costs (−$902, −3.8% compared to mean, 95% CI: −$1305, −$499; p < 0.001). The differential reduction was largely driven by a 16.8% decline in 90‐day SNFs (−$499 or −16.8% compared to mean, 95% CI: −$833, −$164; p = 0.0037). We found that CJR was not associated with service‐specific cost reductions for 90‐day hospital inpatient (−$51 or −3.7% compared to mean, 95% CI: −$116, $13; p = 0.1183), hospital outpatient (−$15 or −2.3% compared to mean, 95% CI: −$7.2, $36.6; p = 0.1871), Part B (−$21 or −0.7% compared to mean, 95% CI: −$77, $36; p = 0.4653), home health agency ($29 or 1.4% compared to mean, 95% CI: −$200, $258; p = 0.8061), and durable medical equipment (−$5 or −4.5% compared to mean, 95% CI: −$15, $5; p = 0.3514) (Table 2).
3.1.4. Influence of quality
While 90‐day all‐cause readmission rate was decreased in both CJR and non‐CJR hospitals after implementing the CJR program, the magnitude of reduction was greater in CJR hospitals compared to non‐CJR hospitals (Table 1). Table 2 shows no significant differences attributed to CJR were found in hospital length of stay (−0.20 days or −5.4% compared to mean, 95% CI: −0.60, 0.20 days; p = 0.3223), PE (0.05 ppts or 2.3% compared to mean, 95% CI: −0.16, 0.26 ppts; p = 0.6267), DVT (0.08 ppts or 1.7% compared to mean, 95% CI: −0.14, 0.28 ppts; p = 0.6080), 30‐day mortality (0.024 ppts or 9.9% compared to mean, 95% CI: −0.092, 0.043 ppts; p = 0.7014), 90‐day mortality (0.022 ppts or 4.9% compared to mean, 95% CI: −0.099, 0.054 ppts; p = 0.5651), and procedure volume (−0.65 or 2.8% compared to mean, 95% CI: −1.88, 0.57; p = 0.2042). However, CJR hospitals significantly reduced the 90‐day readmission rate (decrease by 0.37 ppts or by 3.9% compared to mean, 95% CI: −0.71, −0.038 ppts; p = 0.0294).
3.1.5. Influence of downside risk
Compared to 2016, the relative reduction in 90‐day costs among CJR hospitals was greater in 2017, the year that downside risk was initiated. The relative reduction in 90‐day episode‐of‐care costs for CJR participants was −$785 (95% CI: −$1152, −$419; p < 0.001) in 2016 and −$1017 (95% CI: −$1490, −$545; p < 0.001) in 2017, and for SNF costs, the reduction was −$431 (95% CI: −$737, −$125; p = 0.0061) in 2016 and −$565 (95% CI: −$936, −$195; p = 0.0030) in 2017. We also found that CJR hospitals likely avoided patients with disability compared to non‐CJR hospitals in 2017 (−0.37 ppts or 55.0% compared to mean, 95% CI: −0.72, 0.02 ppts; p = 0.0373).
3.1.6. Patient selection and cost saving
Because reduction in 90‐day episode costs among CJR hospitals was largely driven by a cost reduction in SNF utilization, we conducted an additional analysis to further investigate whether avoiding old patients (aged 85 years or above) was associated with cost reductions. We first confirmed a significant reduction in SNF use (−2.1 ppts or 6.8% compared to mean, 95% CI: −3.9, −0.2 ppts; p = 0.0276) and in SNF duration (−0.58 day or 12.2% compared to mean, 95% CI: −0.97, −0.18 day; p = 0.0046) (Table 2). We then confirmed that a moderate correlation (0.20) between hospitals' pre–post cost reduction in SNF cost and pre–post reduction in treating older patient (85 years or above). Finally, we used a two‐part regression model to describe the relationship between avoidance of older patients and SNF utilization. Table 3 shows the results from our two‐part model. The probability of being discharged to SNF significantly increased with age. For example, compared to patients whose ages are between 65 and 69, older patients (age 85 years or older) are five times more likely to be discharged to SNF (OR = 5.76; 95% CI: 5.17, 6.42; p < 0.001). The second part of the model reports the average 90‐day cost for SNF use conditioned on being discharged to SNF. The mean adjusted SNF costs for older patients (age 85 years or above) was $4291 higher (p < 0.001) compared to younger patients (age 65–69 years). The model suggests substantial savings for CJR hospitals from avoiding older patients who were much more likely to be discharged to SNF and much more likely to have a higher SNF cost once they were discharged to SNF.
TABLE 3.
Results from two‐part model to show the relationship between patient selection and SNF utilization and cost
| Part 1: SNF (logistics) | Part 2: SNF (GLM) | Average adjusted cost | |
|---|---|---|---|
| Age group, years (ref = 65–69) | |||
| 70–74 | 1.45 (p < 0.001) | 0.04 (p < 0.001) | $781 (p < 0.001) |
| 75–79 | 2.23 (p < 0.001) | 0.12 (p < 0.001) | $1798 (p < 0.001) |
| 80–84 | 3.71 (p < 0.001) | 0.22 (p < 0.001) | $3005 (p < 0.001) |
| 85+ | 5.76 (p < 0.001) | 0.38 (p < 0.001) | $4291 (p < 0.001) |
| Year (ref = 2013) | |||
| 2014 | 0.93 (p < 0.001) | −0.02 (p = 0.007) | −$227 (p < 0.001) |
| 2015 | 0.82 (p < 0.001) | −0.03 (p = 0.002) | −$507 (p < 0.001) |
| 2016 | 0.58 (p < 0.001) | −0.11 (p < 0.001) | −$1264 (p < 0.001) |
| 2017 | 0.49 (p < 0.001) | −0.13 (p < 0.001) | −$1603 (p < 0.001) |
| Sex (ref = male) | |||
| Female | 1.97 (p < 0.001) | 0.06 (p < 0.001) | $1393 (p < 0.001) |
| Race (ref = White) | |||
| Black | 1.60 (p < 0.001) | 0.17 (p < 0.001) | $1356 (p < 0.001) |
| Other | 1.23 (p = 0.006) | 0.22 (p < 0.001) | $1044 (p < 0.001) |
| Comorbidity (ref = none) | |||
| One | 1.40 (p < 0.001) | 0.09 (p < 0.001) | $870 (p < 0.001) |
| Two or more | 1.90 (p < 0.001) | 0.19 (p < 0.001) | $1728 (p < 0.001) |
| Constant | 0.15 (p < 0.001) | 8.92 (p < 0.001) | $3021 (p < 0.001) |
Note: “SNF (logistics)” represents the probability of observing a positive SNF cost (e.g., discharge to SNF), “SNF (GLM)” represents the amount of SNF spending conditional on discharge to SNF, and “average adjusted cost” represents the marginal effects for the combined logit and GLM version of the two‐part model.
Abbreviations: Comorbidity, Charlson Comorbidity Index; ref, reference group; SNF, skilled nursing facilities.
3.2. Secondary analysis of all admissions (ED + urgent + elective)
We repeated the primary analysis after including those undergoing LEJR via ED or an urgent admission (see Appendix B for study population and descriptive statistics). With the analysis including elective, urgent, and emergency visits, we found no evidence of preferential patient selection among CJR hospitals. Table A1, A2, A3 shows that there is no significant difference in the changes in mean age, gender, race, CCI, and disability status by hospitals' CJR status from pre‐to‐post CJR.
Following implementation of CJR, there was a greater reduction in 90‐day episode‐of‐care costs among those treated by CJR hospitals (Table A2). We estimated a −$957 (95% CI: −$1384, −$552) or 3.6% (compared to mean; p < 0.001) decrease in the mean 90‐day episode‐of‐care costs relative to non‐CJR hospitals. As with the elective only analysis, the differential reduction was largely driven by a −$436 (95% CI: −$759, −$129) or 9.6% (compared to mean; p = 0.0064) decline in 90‐day SNFs. There were no changes in hospital length of stay, PE, DVT, 30/90‐day mortality, and procedure volume between CJR and non‐CJR hospitals. In addition, unlike what we found in primary analysis, we found no significant effect on 90‐day readmission and SNF use among CJR hospitals (Table A2).
Similar to the elective only analysis, we also estimated the effect of CJR by year. Columns 2 and 3 in Table A2 indicate that the relative reduction in 90‐day episode‐of‐care costs (−$886 in 2016 and −$1029 in 2017; p < 0.001) and in SNF costs (−$353 in 2016; p = 0.0185 and −$519 in 2017; p = 0.0030) increased in the more recent year among CJR hospitals, suggesting there are the same patterns between elective admissions and all admissions analyses.
In summary, adding the ED and urgent case to our primary analysis, there are no differences in patient selection by age, race, comorbidity, or SSDI status. The results with the added ED cases are broadly consistent with previous findings. 7 , 8 , 9 , 10 , 11
3.3. Secondary analysis of ED/urgent‐only admissions
When we only focused on ED and urgent admissions, we found that CJR hospitals significantly selected patients who are older (age 85 years or above) and have greater comorbidity (CCI of 2 or higher), compared to non‐CJR hospitals (Table A4). We estimated a −$1052 (95% CI: −$1454, −$612) or 2.6% (compared to mean; p < 0.001) reduction in the mean 90‐day episode‐of‐care costs among CJR hospitals, while no significant differences were detected in outcomes related to quality, volume, and SNF. Also, unlike previous analyses, costs reduction was greater in 2016 than in 2017 (see Appendix C for details).
3.4. Robustness check
Several tests were performed to check the robustness of our model. First, we plotted pretrend graphs to test whether CJR hospitals and non‐CJR hospitals faced similar trends during the period before the policy implementation. Figure 1 shows that both CJR and non‐CJR hospitals had very similar trend of outcomes before the policy implementation.
FIGURE 1.
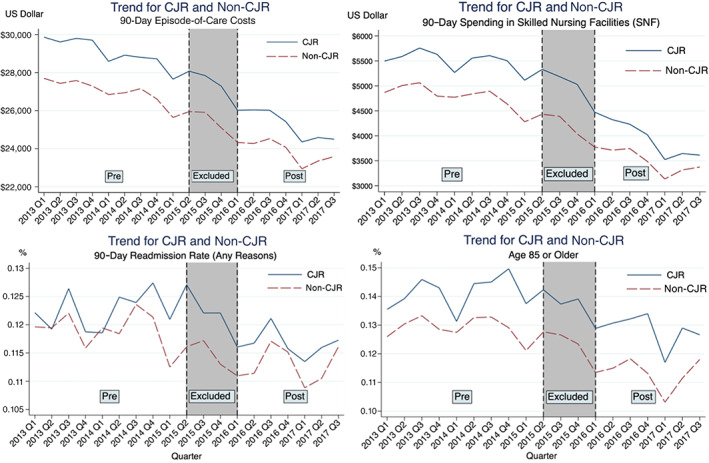
Pretrend graph between CJR hospitals and non‐CJR hospitals on 90‐day episode‐of‐care costs, 90‐day spending in skilled nursing facilities, 90‐day readmission rate for any reasons, and age 85 years or older. “Pre” means prepolicy periods and “post” means postpolicy periods. “Excluded” represent the periods from July 2015 to April 2016. The US dollar value is adjusted to 2017‐dollar value [Color figure can be viewed at wileyonlinelibrary.com]
As an alternative check for DID robustness, we included MSA‐specific linear time trends, which is a linear year variable (from 2013 to 2017) interacted with indicators for each of the 171 MSA to allow any underlying trends in unobservable to vary in a linear fashion for different MSAs. If there exist different trends in outcome variables, then adding MSA‐specific linear time trend would substantially alter the estimated coefficients. Columns 1–3 in Table 4 show that our findings are not sensitive to the inclusion of MSA‐specific linear time trends, suggesting that there were no underlying trends to produce a biased estimate of the policy effect.
TABLE 4.
Several robustness checks
| Outcomes | MSA‐specific linear time trends | Falsification test | ||
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| CJR (overall) | CJR (2016) | CJR (2017) | CJR (overall) | |
| All admissions (ED + urgent + non‐ED) | ||||
| Total 90‐day episode costs | −882*** (0.0001) | −880*** (0.0001) | −996*** (0.0001) | −67.36 (0.5504) |
| SNF 90‐day costs | −492** (0.0041) | −487** (0.0043) | −693** (0.0024) | 25.49 (0.7251) |
| Age | −0.0465 (0.6188) | −0.0453 (0.6276) | −0.0993 (0.3930) | −0.0690 (0.1550) |
| 90‐day readmission (any reasons) | −0.0075* (0.0173) | −0.0076* (0.0172) | −0.0074 (0.0760) | −0.0006 (0.7333) |
| Elective admissions only | ||||
| Total 90‐day episode costs | −813*** (0.0001) | −809*** (0.0001) | −1022*** (0.0007) | −40.78 (0.7175) |
| SNF 90‐day costs | −558** (0.0020) | −554** (0.0020) | −739** (0.0021) | 40.08 (0.5186) |
| Age | −0.0880 (0.2953) | −0.0872 (0.2983) | −0.1301 (0.2264) | −0.0557 (0.1999) |
| 90‐day readmission (any reasons) | −0.0064* (0.0377) | −0.0064* (0.0381) | −0.0071 (0.0980) | −0.0011 (0.5516) |
| Age 85 years or older | −0.0046 (0.1031) | −0.0045 (0.1113) | −0.0076* (0.0300) | −0.00051 (0.7347) |
| White | 0.00096 (0.7484) | 0.00092 (0.7574) | −0.00293 (0.4898) | 0.00215 (0.2597) |
| ED and urgent admissions only | ||||
| Total 90‐day episode costs | −1346* (0.0130) | −1350* (0.0127) | −1243 (0.0574) | −11.38 (0.9637) |
| Age | 0.1945 (0.4680) | 0.1993 (0.4565) | 0.091 (0.8550) | −0.0344 (0.7855) |
| CCI of 2 or higher | 0.0122 (0.3171) | 0.0123 (0.3117) | 0.0100 (0.5776) | 0.00092 (0.1850) |
| Age 85 years or older | 0.0151 (0.2758) | 0.0152 (0.2724) | 0.0120 (0.4706) | −0.0031 (0.6461) |
Note: Inclusion of MSA‐specific linear time trends for testing whether there exists different trends in outcome variables. Falsification test to evaluate the validity of our findings. Estimated coefficients represent a change in each unit for continuous outcomes (costs and age). For binary outcomes (90‐day readmission rate, White, Black, and age older than 85 years), they represent a percentage point change.
Abbreviations: CJR, Comprehensive Care for Joint Replacement; SNF, skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
In order to test whether the observed treatment effect was spurious, we performed a falsification test using a sample that is not affected by the CJR policy. Specifically, we tested the effects of CJR only using sample before the program implementation (2013–2014). If we find any evidence of between‐group differences in this subsample, then it would indicate that the policy effects we report are spurious. Column 4 in Table 4 indicates that estimated coefficients from the falsification test are small compared to those found in Tables 2, A2, and A4, and none of them are different from zero. This confirms that our identification strategy is reliable, and the effects of the policy we estimated in the main analysis (elective admissions only) and the secondary analyses (all and ED/urgent admissions) are credible.
One concern of using year‐fixed effects is that year‐fixed effects may provide biased estimates if there exists seasonality correlated with outcome variables. So, in order to account for seasonality observed in pretrend time series plots, we added year‐quarter‐fixed effects in both analyses. Results were reported in Tables A5, A6, A7. Overall, estimates from the specification with year‐quarter‐fixed effects are very similar to those found in Tables 2, A2, and A4, suggesting that there was no unobserved seasonal shock correlated with outcomes of interest such as patient selection, costs, and quality in both analyses.
4. DISCUSSION
Hip and knee replacement is one of the most common and expensive procedures in the United States and is expected to rapidly increase in the near future. 24 Thus, it is crucial to understand how bundled payment programs affect LEJR procedures, and whether the programs can achieve cost reduction without compromising the quality of care. We evaluated the effect of CJR on patient selection, costs, and quality using a sample period from January 2013 to August 2017, the first 2 years of its implementation.
In our main analysis (elective admissions), we found that CJR was associated with a 3.8% decrease in 90‐day episode cost largely driven by a reduction in SNF costs and were greater in 2017 than in 2016. 10 , 11 We also found that CJR was associated with a 3.9% reduction in 90‐day all cause readmission rates. However, we further observed that CJR was significantly associated with patient selection. For example, CJR hospitals seemingly avoided older, more disabled, and Black patients who are more likely to be perceived as being a higher risk. 25 , 26 Previous research failed to find this, perhaps, because they ignored the fact that individual providers have more discretion in deciding which patient should be treated in elective setting. This is because selection differences were not observed when ED and urgent admissions were included in the analysis. Specifically, in the all admission analysis, we found significant cost reductions in CJR hospitals without harming quality and patient selection, which is generally consistent with prior studies. 7 , 8 , 9 , 10 , 11 In a subgroup analysis restricted to ED/urgent cases only, we found that CJR hospitals treated LEJR patients who were older and had higher comorbidity and did not achieve similar levels of cost reductions, which might suggest that CJR hospitals have less ability to select and manage financial risk in LEJR.
Broadly, the magnitude of the policy effects in 2017 was greater than in 2016. This might be explained by several reasons. First, hospitals required time to ramp up their clinical pathway changes. Secondly, there was no downside risk in 2016, so hospitals were not faced with financial penalties if they did not achieve price targets. In other words, during the first performance year, CJR hospitals would receive the financial gain if they achieved cost reductions but were not penalized for failing to maintain cost efficiencies.
There are several limitations in this study. First, among CJR hospitals, although we found evidence of patient selection in elective admissions, it is not clear why providers choose fewer Black patients. Health disparities and social determinants of health across racial groups in the CJR model have been well documented, 27 , 28 and are a persistent systematic issue in health care. 29 , 30 However, it is unknown whether providers' decisions to admit patients are due to racial disparities in health and access or partially based on racial discrimination and/or implicit bias. Second, while this study only presents the average effect of CJR, there may be substantial heterogeneity in this effect across hospitals. Recent ongoing analysis shows that the effect of CJR varies based on surgical volume and historic episode‐of‐care costs [not shown]. If the effect concentrated on a certain type of CJR hospitals, then, from the perspective of social planner, bundled payment programs may not be an efficient strategy to reduce Medicare spending. Also, even though we found moderate savings in CJR hospitals, we do not know if the savings will be sustained or just a one‐time reduction. It is also unclear whether patient selection was associated with saving in costs and improvement in quality. If CJR hospitals primarily reduce the mean episode‐of‐care by patient selection, then new concerns about avoiding recommended care and inducing disparities could emerge. Another limitation is that Medicare claims do not have information regarding functional status of patients. Thus, we do not know whether reduction in the costs or SNF utilization is associated with worse functional outcomes.
Although we performed rigorous statistical analysis to capture causal effect of CJR, and CJR assignment to MSAs was conducted through a random allocation, unobservable time‐varying factors may still lead to biased estimates. For example, factors that affect providers' behavior coinciding with implementation of CJR could bias our estimates. Finally, there is likely a delayed impact of changes made to care pathways and the reporting of data available for hospitals to act on. Indeed, because of the delay in reconciliations and data reporting, it may well be that the true impacts of CJR will be better demonstrated in future year, and as such, we recognize the need for ongoing study of CJR.
CJR is associated with modest cost reductions; however, we also found evidence of preferential patient avoidance among elective admissions at CJR hospitals. Because providers have more selective control among elective admissions, hospitals with a higher proportion of elective cases may have better success at managing financial risk of LEJR patients and achieving pricing target. Conversely, hospitals with greater rates of ED/urgent cases have an inherent disadvantage in a bundled payment model. Consequently, these hospitals and health system might strive to integrate ED/urgent patients into their efficient LEJR pathways that are developed within Orthopedics departments at CJR hospitals. Policy makers might consider accounting for elective vs. nonelective admission in developing target prices under bundled payment models.
ACKNOWLEDGMENT
This study was funded by grant R01HS024714, from the Agency for Healthcare Research and Quality (AHRQ). The study sponsors had no role in the design or conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, or approval of the manuscript. The statements in this article are solely the responsibility of the authors and do not necessarily represent the views of AHRQ.
Appendix A. ECONOMETRIC SPECIFICATIONS USED IN THE ANALYSIS
We used the following regression model for continuous outcomes.
is an outcome values for patient “i” in hospital “h” in MSA “m” in stratum “s” in year “t.”
is a constant term.
- is equal to one if the MSA is in the treated group (67 MSAs) and the year is after April 2016 and is 0 otherwise
- To identify the effect of CJR over time, we added and instead of
- is patient level covariates.
- We included dummy for race (White and Black), age (60–64, 65–69, 70–74, 75–79, 80–84 years), CCI (CCI of 0, CCI of 1), and sex (female).
- In order to avoid dummy variable trap, race (other), age (85+), CCI (CCI of 2+), and sex (male) were excluded.
is strata‐fixed effects.
is hospital‐fixed effects.
is MSA‐fixed effects.
- is year‐fixed effects.
- We excluded two intervening periods (July 2015–April 2016, and periods following September 2017).
is an error term.
- 2. For binary outcome variables, model specification was the following:
is a dummy for being each binary outcome.
- is patient level covariates.
- When one of race, age, CCI, and sex dummy was an outcome, the corresponding dummy variables were excluded from patient‐level covariates, for example, when age 85+ was an outcome, age dummy variables were excluded from the patient‐level covariates.
The other variables are the same as above.
Appendix B. STUDY POPULATION FOR ALL ANALYSIS (ED + URGENT + ELECTIVE)
We included both elective and emergency visits of 846,147 beneficiaries undergoing LEJR from January 1, 2013 to August 31, 2017. CJR was targeted to 804 hospitals in 67 MSAs, and the nonparticipation group consisted of 996 hospitals in 104 MSAs. Before the policy implementation, the overall mean 90‐day episode‐of‐care costs was $27,925, and the mean age of the cohort was 75.5 years, with 64.0% female and 91.3% White (column 1 in Table 1), while the overall mean 90‐day episode‐of‐care costs and the mean age of the cohort declined to $24,424 and 75.0, respectively, with lower proportion of female (63.0%) and White (90.5%) after the policy implementation (column 5 in Table 1). As we expected, patients from this all admissions analysis were more expensive, older, and had greater comorbidity compared those in the elective analysis.
Appendix C. ED/URGENT‐ONLY ADMISSION ANALYSIS
C.1. Study population
In ED/urgent only admission analysis, we included 151,912 beneficiaries who underwent LEJR from January 1, 2013, to August 31, 2017. There were 775 CJR hospitals in 67 MSAs and 940 non‐CJR hospitals in 104 MSAs. During the preintervention period of January 2013 through June 2015, the average 90‐day episode‐of‐care costs was $42,096. The average age of the cohort was 81.8 years, with 91.7% White and 38.1% of patients had CCI of 2 or higher (column 1 in Table 3). After the policy implementation (April 2016), while the mean 90‐day episode‐of‐care costs and the mean age of the cohort decreased to $39,194 and 81.5, respectively, the proportion of patients with severe comorbidity increased to 42.8% (column 5 in Table 3). Table 3 also show that after the policy implementation, CJR hospitals experienced a relative increase in patients with high comorbidity, while non‐CJR hospitals had a greater relative reduction in selecting patients with age 85 years or older and patients with dual eligibility status for Medicare and Medicaid.
C.2. Influence of patient selection, costs, quality, and downside risk
Including only ED and urgent admissions, we found evidence of patient selection among CJR hospitals. Table 4 shows that CJR hospital significantly selected older (0.26 years or 0.32% compared to mean, p = 0.042), more female (−1.3 ppt or −1.9% compared to mean, p = 0.030), and patients with higher comorbidity (1.9 ppts or 4.8% compared to mean, p = 0.004) compared to non‐CJR hospitals. Specifically, increase in average age resulted from increasing the volume of procedures for an age group whose age is at least 85 years (1.4 ppts or 3.4% compared to mean, p = 0.040). This is exactly the opposite pattern to what we observed in the main analysis (elective admission analysis).
We found that CJR is associated with modest cost reduction in 90‐day episode‐of‐care costs (−$1052 or −2.6% compared to mean, p < 0.001), BPCI inpatient 90‐day costs (−$752 or −15.2% compared to mean, p = 0.001), and BPCI Part B 90‐day costs (−$86 or −2.1% compared to mean, p = 0.031), while we found no evidence that CJR is associated with postacute care costs (Table 4). Similar to all admission analysis, we found no significant effect of CJR on hospital length of stay, PE, DVT, 30/90‐day mortality, 90‐day mortality, procedure volume, 90‐day readmission rate, and SNF use (Table 4).
Unlike previous elective only admission or all admission analyses, we found no evidence that the effect of CJR increases over time. We observed that cost reduction was greater in 2016 than in 2017. Specifically, in 2016, CJR hospitals reduced the mean 90‐day episode‐of‐care costs by $1145, while they reduced it by $954 in 2017.
Overall, when we focused only on ED/urgent cases, we found that CJR hospitals selected patients who are older and have higher comorbidity, which is very opposite to our findings from the main analysis.
TABLE A1.
Descriptive statistics for all admissions (ED + urgent + elective)
| Variables | Prepolicy periods | Postpolicy periods | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| All admissions | CJR | Non‐CJR | p value | All admissions | CJR | Non‐CJR | p value | |
| Total 90‐day episode costs | $27,925 | $29,018 | $27,105 | <0.001 | $24,424 | $25,100 | $23,940 | <0.001 |
| SNF 90‐day costs | $5075 | $5471 | $4778 | <0.001 | $3610 | $3853 | $3435 | <0.001 |
| Inpatient costs (index procedures) | $13,676 | $13,982 | $13,446 | <0.001 | $12,689 | $12,947 | $12,504 | <0.001 |
| Outpatient 90‐day costs | $651 | $644 | $656 | 0.002 | $685 | $685 | $685 | 0.948 |
| Durable medical equipment | $121 | $125 | $118 | <0.001 | $90 | $91 | $90 | 0.748 |
| Home health agency | $2220 | $2275 | $2180 | <0.001 | $2095 | $2169 | $2042 | <0.001 |
| BPCI inpatient 90‐day costs | $1488 | $1577 | $1421 | <0.001 | $1388 | $1471 | $1328 | <0.001 |
| BPCI Part B 90‐day costs | $3221 | $3310 | $3154 | <0.001 | $2965 | $3046 | $2908 | <0.001 |
| Length of stay (days) | 4.02 | 4.06 | 3.98 | <0.001 | 3.70 | 3.62 | 3.77 | <0.001 |
| Number of episode a | 408 | 366 | 436 | <0.001 | 434 | 372 | 473 | <0.001 |
| Mortality (30 days) | 312.48 | 309.70 | 314.57 | <0.001 | 216.02 | 187.48 | 236.50 | <0.001 |
| Mortality (90 days) | 1.20% | 1.25% | 1.15% | <0.001 | 1.05% | 1.10% | 1.01% | 0.019 |
| 90‐day readmission (any reasons) | 2.49% | 2.63% | 2.39% | <0.001 | 2.21% | 2.38% | 2.09% | <0.001 |
| PE | 12.07% | 12.25% | 11.94% | <0.001 | 11.46% | 11.63% | 11.34% | 0.022 |
| DVT | 2.58% | 2.51% | 2.64% | 0.001 | 2.11% | 2.04% | 2.16% | 0.045 |
| Age | 75.51 | 75.70 | 75.38 | <0.001 | 75.03 | 75.23 | 74.88 | <0.001 |
| Female | 64.03% | 64.44% | 63.73% | <0.001 | 62.98% | 63.31% | 62.75% | 0.003 |
| White | 91.28% | 90.65% | 91.76% | <0.001 | 90.48% | 89.88% | 90.91% | <0.001 |
| Black | 4.73% | 4.76% | 4.71% | 0.463 | 4.70% | 4.64% | 4.74% | 0.243 |
| Disabled | 0.64% | 0.62% | 0.65% | 0.155 | 0.59% | 0.57% | 0.60% | 0.277 |
| CCI of 0 | 51.7% | 51.5% | 51.8% | 0.091 | 51.1% | 50.1% | 51.8% | <0.001 |
| CCI of 1 | 26.7% | 26.6% | 26.8% | 0.049 | 25.8% | 25.9% | 25.7% | 0.174 |
| CCI of 2 or higher | 21.7% | 21.9% | 21.5% | <0.001 | 23.1% | 23.9% | 22.5% | <0.001 |
| Age 65–69 years | 25.3% | 24.8% | 25.7% | <0.001 | 27.1% | 26.7% | 27.4% | 0.001 |
| Age 70–74 years | 25.6% | 25.1% | 25.9% | <0.001 | 26.9% | 26.2% | 27.4% | <0.001 |
| Age 75–79 years | 20.9% | 21.0% | 20.9% | 0.580 | 20.6% | 20.6% | 20.7% | 0.709 |
| Age 80–84 years | 14.6% | 14.9% | 14.4% | <0.001 | 13.3% | 13.6% | 13.1% | <0.001 |
| Age 85 years or older | 13.6% | 14.2% | 13.1% | <0.001 | 12.0% | 12.8% | 11.4% | <0.001 |
| Dual eligibility | 8.2% | 9.1% | 7.5% | <0.001 | 7.4% | 8.5% | 6.6% | <0.001 |
| DRG 469 | 5.6% | 6.0% | 5.3% | <0.001 | 5.3% | 5.9% | 4.8% | <0.001 |
| DRG 470 | 94.4% | 94.0% | 94.7% | <0.001 | 94.7% | 94.1% | 95.2% | <0.001 |
| N | 578,452 | 247,932 | 330,520 | 267,735 | 111,798 | 155,937 | ||
Note: Only prepolicy periods included (January 2013–June 2015). Cost variables were adjusted for inflation (2017 dollar value). DRG 469 represents major joint replacement with major complication, and DRG 470 represents major joint replacement without major complication.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DRG, diagnosis‐related group; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
The mean volume in each prepolicy and postpolicy was calculated using an identical length of time and accounted for seasonality.
TABLE A2.
Overall effect of CJR for all admissions (ED + urgent + elective)
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | −0.092 (0.0944) | −0.076 (0.1865) | −0.107 (0.1125) |
| Female | −0.0016 (0.5509) | −0.00063 (0.8343) | −0.0025 (0.4878) |
| White | 0.0027 (0.0887) | 0.0036 (0.0656) | 0.0018 (0.2953) |
| Black | −0.0022 (0.0629) | −0.0025 (0.1064) | −0.0019 (0.1680) |
| Disabled | −0.0019 (0.2331) | −0.00044 (0.8464) | −0.0028 (0.0978) |
| CCI (mean) | 0.019 (0.1333) | 0.021 (0.1177) | 0.017 (0.2461) |
| CCI of 0 | −0.0066 (0.1006) | −0.0058 (0.2044) | −0.0074 (0.0958) |
| CCI of 1 | 0.0017 (0.5000) | 0.0004 (0.8997) | 0.0091 (0.3176) |
| CCI of 2 or higher | 0.0040 (0.2604) | 0.0045 (0.2405) | 0.0035 (0.3887) |
| Age 65–69 years | 0.0058 (0.0699) | 0.0053 (0.1091) | 0.0063 (0.1137) |
| Age 70–74 years | −0.00046 (0.8724) | −0.00022 (0.9472) | −0.00070 (0.8308) |
| Age 75–79 years | 0.000038 (0.9879) | −0.0016 (0.5853) | 0.0017 (0.5662) |
| Age 80–84 years | −0.0015 (0.3775) | −0.00065 (0.7761) | −0.0024 (0.2563) |
| Age 85 years or older | −0.0018 (0.3657) | −0.0011 (0.6692) | −0.0026 (0.2651) |
| Cost outcomes | |||
| Total 90‐day episode costs | −957*** (0.0000) | −886*** (0.0000) | −1029*** (0.0001) |
| SNF 90‐day costs | −436** (0.0064) | −353* (0.0185) | −519** (0.0030) |
| Inpatient costs (index procedure) | −137 (0.0683) | −112 (0.1701) | −162* (0.0326) |
| Outpatient 90‐day costs | 15.0 (0.1838) | 3.0 (0.8602) | 27.0* (0.0475) |
| Durable medical equipment 90‐day costs | −3.7 (0.4311) | −5.5 (0.2452) | −1.9 (0.7170) |
| Home health agency 90‐day costs | 13.1 (0.8972) | 32.2 (0.7347) | −6.0 (0.9563) |
| BPCI inpatient 90‐day costs | −375* (0.0200) | −417** (0.0061) | −334 (0.0634) |
| BPCI Part B 90‐day costs | −32.6 (0.2799) | −33.2 (0.2659) | −32.0 (0.3287) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.0031 (0.0648) | −0.0036 (0.0901) | −0.0025 (0.2360) |
| Mortality (30 days) | −0.00080 (0.1511) | −0.00077 (0.2455) | −0.00082 (0.2542) |
| Mortality (90 days) | −0.00063 (0.4563) | −0.00088 (0.4010) | −0.00035 (0.7321) |
| PE | 0.00014 (0.8918) | 0.000093 (0.9373) | 0.00019 (0.8786) |
| DVT | 0.00018 (0.8935) | −0.00067 (0.6846) | 0.00104 (0.4862) |
| Volume | |||
| Length of stay (day) | −0.23 (0.1936) | −0.28 (0.1151) | −0.19 (0.3504) |
| Number of episode | −0.88 (0.1994) | −0.86 (0.2995) | −0.90 (0.1532) |
| SNF utilization | |||
| Discharge to SNF | −0.0093 (0.2740) | −0.0070 (0.3866) | −0.0116 (0.2243) |
| SNF duration (day) | −0.46* (0.0156) | −0.37* (0.0408) | −0.55** (0.0075) |
Note: Column 1 represents difference‐in‐differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference‐in‐differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
TABLE A3.
Descriptive statistics for ED‐/urgent‐only admissions (ED + urgent)
| Variables | Prepolicy periods | Postpolicy periods | ||||||
|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| All admissions | CJR | Non‐CJR | p value | All admissions | CJR | Non‐CJR | p value | |
| Total 90‐day episode costs | $42,096 | $43,456 | $40,956 | <0.001 | $39,194 | $40,656 | $38,003 | <0.001 |
| SNF 90‐day costs | $12,276 | $12,868 | $11,780 | <0.001 | $10,978 | $11,833 | $10,282 | <0.001 |
| Inpatient costs (index procedures) | $15,234 | $15,599 | $14,928 | <0.001 | $14,354 | $14,786 | $14,002 | <0.001 |
| Outpatient 90‐day costs | $720 | $725 | $717 | 0.459 | $822 | $838 | $809 | 0.216 |
| Durable medical equipment | $110 | $114 | $108 | 0.014 | $83 | $87 | $80 | 0.082 |
| Home health agency | $2334 | $2408 | $2272 | <0.001 | $2357 | $2380 | $2337 | 0.062 |
| BPCI inpatient 90‐day costs | $7149 | $7327 | $7000 | <0.001 | $6562 | $6542 | $6579 | 0.767 |
| BPCI Part B 90‐day costs | $4272 | $4415 | $4152 | <0.001 | $4038 | $4191 | $3914 | <0.001 |
| Length of stay (days) | 5.53 | 5.69 | 5.40 | <0.001 | 5.66 | 5.65 | 5.66 | 0.944 |
| Number of episode a | 96 | 111 | 84 | <0.001 | 97 | 101 | 94 | <0.001 |
| Mortality (30 days) | 5.45% | 5.37% | 5.51% | 0.329 | 5.25% | 5.19% | 5.29% | 0.623 |
| Mortality (90 days) | 11.37% | 11.34% | 11.40% | 0.782 | 11.13% | 11.29% | 10.99% | 0.315 |
| 90‐day readmission (any reasons) | 22.39% | 22.73% | 22.10% | 0.015 | 22.19% | 23.07% | 21.48% | <0.001 |
| PE | 3.28% | 3.17% | 3.37% | 0.076 | 2.46% | 2.37% | 2.53% | 0.286 |
| DVT | 6.47% | 6.67% | 6.29% | 0.012 | 6.27% | 6.44% | 6.13% | 0.173 |
| Age | 81.83 | 81.97 | 81.72 | <0.001 | 81.51 | 81.94 | 81.17 | <0.001 |
| Female | 69.35% | 69.64% | 69.11% | 0.062 | 67.86% | 67.57% | 68.10% | 0.223 |
| White | 91.70% | 91.06% | 92.24% | <0.001 | 91.26% | 90.28% | 92.05% | <0.001 |
| Black | 4.53% | 4.47% | 4.59% | 0.383 | 4.70% | 4.92% | 4.51% | 0.040 |
| Disabled | 0.37% | 0.34% | 0.38% | 0.254 | 0.38% | 0.38% | 0.39% | 0.988 |
| CCI of 0 | 35.22% | 35.57% | 34.93% | 0.030 | 29.39% | 28.07% | 30.46% | <0.001 |
| CCI of 1 | 26.71% | 26.73% | 26.69% | 0.907 | 27.80% | 27.70% | 27.88% | 0.660 |
| CCI of 2 or higher | 38.07% | 37.70% | 38.37% | 0.025 | 42.81% | 44.23% | 41.65% | <0.001 |
| Age 65–69 years | 9.98% | 9.61% | 10.29% | <0.001 | 10.89% | 9.91% | 11.68% | <0.001 |
| Age 70–74 years | 13.02% | 12.77% | 13.24% | 0.023 | 14.04% | 13.28% | 14.66% | <0.001 |
| Age 75–79 years | 15.69% | 15.65% | 15.72% | 0.770 | 16.05% | 15.87% | 16.19% | 0.356 |
| Age 80–84 years | 19.04% | 19.24% | 18.88% | 0.135 | 18.40% | 18.44% | 18.36% | 0.837 |
| Age 85 years or older | 42.27% | 42.73% | 41.88% | 0.005 | 40.63% | 42.51% | 39.10% | <0.001 |
| Dual eligibility | 15.50% | 16.75% | 14.45% | <0.001 | 14.77% | 16.87% | 13.06% | <0.001 |
| DRG 469 | 19.28% | 19.66% | 18.96% | 0.004 | 20.67% | 21.88% | 19.68% | <0.001 |
| DRG 470 | 80.72% | 80.34% | 81.04% | 0.004 | 79.33% | 78.12% | 80.32% | <0.001 |
| N | 106,801 | 48,681 | 58,120 | 45,111 | 20,244 | 24,867 | ||
Note: Only pre policy periods included (January 2013–June 2015). Cost variables were adjusted for inflation (2017 dollar value). DRG 469 represents major joint replacement with major complication, and DRG 470 represents major joint replacement without major complication.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DRG, diagnosis‐related group; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
The mean volume in each prepolicy and postpolicy was calculated using an identical length of time and accounted for seasonality.
TABLE A4.
Overall effect of CJR for ED/urgent admissions and the effects by years
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | 0.26* (0.0423) | 0.31* (0.0313) | 0.20 (0.2095) |
| Female | −0.013* (0.0298) | −0.014 (0.0549) | −0.011 (0.1534) |
| White | −0.0014 (0.6947) | −0.00064 (0.8839) | −0.0023 (0.5884) |
| Black | 0.0041 (0.2500) | 0.0043 (0.2897) | 0.0038 (0.3900) |
| Disabled | 0.0041 (0.7231) | −0.015 (0.4656) | 0.0165 (0.1579) |
| CCI (mean) | 0.051 (0.1083) | 0.054 (0.1160) | 0.047 (0.2280) |
| CCI of 0 | −0.015* (0.0403) | −0.011 (0.1764) | −0.020* (0.0298) |
| CCI of 1 | −0.0044 (0.4132) | −0.0086 (0.1482) | −0.00012 (0.9882) |
| CCI of 2 or higher | 0.019** (0.0041) | 0.020** (0.0077) | 0.019* (0.0228) |
| Age 65–69 years | −0.0030 (0.4636) | −0.0055 (0.2846) | −0.0002 (0.9688) |
| Age 70–74 years | −0.0035 (0.4470) | −0.0038 (0.4783) | −0.0032 (0.5764) |
| Age 75–79 years | 0.00010 (0.9799) | −0.0041 (0.4691) | 0.0046 (0.3351) |
| Age 80–84 years | −0.0052 (0.2564) | −0.00058 (0.9243) | −0.010 (0.0818) |
| Age 85 years or older | 0.014* (0.0402) | 0.016 (0.0540) | 0.012 (0.1439) |
| Cost outcomes | |||
| Total 90‐day episode costs | −1052*** (0.0003) | −1145*** (0.0008) | −954** (0.0037) |
| SNF 90‐day costs | −75 (0.6720) | 62 (0.7447) | −221 (0.3047) |
| Inpatient costs (index procedure) | −82 (0.4150) | −87 (0.4443) | −77 (0.5206) |
| Outpatient 90‐day costs | 14.4 (0.6656) | −1.61 (0.9590) | 31.6 (0.5035) |
| Durable medical equipment 90‐day costs | 1.26 (0.8358) | −2.48 (0.7465) | 5.26 (0.4538) |
| Home health agency 90‐day costs | −72.0 (0.3002) | −73.3 (0.3136) | −70.5 (0.3436) |
| BPCI inpatient 90‐day costs | −752** (0.0011) | −959*** (0.0004) | −534* (0.0269) |
| BPCI Part B 90‐day costs | −86* (0.0312) | −84 (0.0679) | −88* (0.0470) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.00042 (0.9208) | −0.0022 (0.7150) | 0.0015 (0.7841) |
| Mortality (30 days) | −0.0034 (0.2240) | −0.0033 (0.2912) | −0.0034 (0.3878) |
| Mortality (90 days) | −0.0033 (0.4608) | −0.0040 (0.4209) | −0.0025 (0.6631) |
| PE | −0.00038 (0.8864) | −0.000024 (0.9949) | −0.00077 (0.8136) |
| DVT | −0.0017 (0.6146) | −0.0024 (0.5562) | −0.00086 (0.8162) |
| Volume | |||
| Length of stay (day) | −0.31 (0.1784) | −0.25 (0.2699) | −0.38 (0.1617) |
| Number of episode | −1.69 (0.2042) | −2.29 (0.2322) | −1.06 (0.1712) |
| SNF utilization | |||
| Discharge to SNF | 0.014 (0.2191) | 0.016 (0.3002) | 0.013 (0.2343) |
| SNF duration (day) | 0.042 (0.8564) | 0.217 (0.3841) | −0.144 (0.6009) |
Note: Column 1 represents difference in differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference‐in‐differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
TABLE A5.
Overall effect of CJR for elective admissions (with year‐quarter‐fixed effects)
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | −0.1269* (0.0132) | −0.1171* (0.0356) | −0.1365* (0.0222) |
| Female | 0.00087 (0.7706) | 0.00234 (0.5002) | −0.00059 (0.8882) |
| White | 0.00352* (0.0178) | 0.00469** (0.0098) | 0.00235 (0.1941) |
| Black | −0.00346** (0.0034) | −0.00398* (0.0129) | −0.00292* (0.0341) |
| Disabled | −0.00225 (0.1575) | 0.00038 (0.8711) | −0.00372* (0.0324) |
| CCI (mean) | 0.0105 (0.4041) | 0.0130 (0.3280) | 0.0080 (0.5981) |
| CCI of 0 | −0.00359 (0.3945) | −0.00389 (0.4346) | −0.00329 (0.4701) |
| CCI of 1 | 0.00252 (0.3809) | 0.00223 (0.5150) | 0.00280 (0.3899) |
| CCI of 2 or higher | 0.00056 (0.8805) | 0.00113 (0.7786) | −0.000001 (0.9999) |
| Age 65–69 years | 0.00670 (0.0589) | 0.00669 (0.0657) | 0.00671 (0.1259) |
| Age 70–74 years | −0.00050 (0.9589) | −0.00027 (0.9379) | −0.00074 (0.8351) |
| Age 75–79 years | −0.00031 (0.9116) | −0.00154 (0.6200) | 0.00089 (0.8012) |
| Age 80–84 years | −0.00108 (0.5632) | −0.00084 (0.7192) | −0.00131 (0.5730) |
| Age 85 years or older | −0.00418** (0.0087) | −0.00355 (0.0611) | −0.00483* (0.0107) |
| Cost outcomes | |||
| Total 90‐day episode costs | −906*** (0.0000) | −788*** (0.0000) | −1024*** (0.0000) |
| SNF 90‐day costs | −500** (0.0036) | −432** (0.0060) | −567** (0.0029) |
| Inpatient costs (index procedure) | −150 (0.0576) | −115 (0.1713) | −185* (0.0200) |
| Outpatient 90‐day costs | 14.75 (0.1842) | 4.43 (0.7237) | 24.95 (0.0569) |
| Durable medical equipment 90‐day costs | −4.59 (0.3622) | −6.08 (0.2254) | −3.18 (0.5811) |
| Home health agency 90‐day costs | 28.52 (0.8059) | 54.58 (0.6140) | 2.77 (0.9823) |
| BPCI inpatient 90‐day costs | −8.94 (0.7573) | −6.34 (0.8754) | −11.52 (0.7568) |
| BPCI Part B 90‐day costs | −20.54 (0.4725) | −20.86 (0.4678) | −20.22 (0.5066) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.00365* (0.0335) | −0.00366 (0.0889) | −0.00365 (0.1048) |
| Mortality (30 days) | −0.000261 (0.4504) | −0.000188 (0.6903) | −0.000339 (0.4257) |
| Mortality (90 days) | −0.000216 (0.5793) | −0.000221 (0.6680) | −0.000210 (0.6961) |
| PE | 0.00055 (0.6058) | 0.00039 (0.7366) | 0.00072 (0.5981) |
| DVT | 0.00089 (0.6105) | −0.000086 (0.9259) | 0.00177 (0.3444) |
| Volume | |||
| Length of stay (day) | −0.2055 (0.3123) | −0.2722 (0.1742) | −0.1397 (0.5423) |
| Number of episode | −0.67 (0.2169) | −0.52 (0.5123) | −0.81 (0.2098) |
| SNF utilization | |||
| Discharge to SNF | −0.0207* (0.0301) | −0.0176* (0.0473) | −0.0242* (0.0241) |
| SNF duration (day) | −0.586** (0.0043) | −0.513** (0.0077) | −0.642** (0.0059) |
Note: Column 1 represents difference in differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference in differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR: Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF: skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
TABLE A6.
Overall effect of CJR for all admissions (with year‐quarter‐fixed effects)
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | −0.0924 (0.0917) | −0.0785 (0.1709) | −0.1063 (0.1161) |
| Female | −0.00155 (0.5534) | −0.00077 (0.7964) | −0.00232 (0.5162) |
| White | 0.00280 (0.0741) | 0.00372 (0.0554) | 0.00188 (0.2657) |
| Black | −0.00221 (0.0638) | −0.00252 (0.1083) | −0.00188 (0.1705) |
| Disabled | −0.0021 (0.1945) | 0.00048 (0.8112) | −0.00351 (0.0824) |
| CCI (mean) | 0.0196 (0.1251) | 0.0215 (0.1125) | 0.0177 (0.2309) |
| CCI of 0 | −0.00688 (0.0860) | −0.00604 (0.1875) | −0.00773 (0.0801) |
| CCI of 1 | 0.00171 (0.4885) | 0.00038 (0.8966) | 0.00305 (0.3050) |
| CCI of 2 or higher | 0.00426 (0.2280) | 0.00474 (0.2169) | 0.00378 (0.3446) |
| Age 65–69 years | 0.00591 (0.0643) | 0.00548 (0.0989) | 0.00633 (0.1100) |
| Age 70–74 years | −0.00043 (0.8823) | −0.00011 (0.9731) | −0.00074 (0.8226) |
| Age 75–79 years | −0.00011 (0.9644) | −0.00183 (0.5376) | 0.00160 (0.5876) |
| Age 80–84 years | −0.00159 (0.3616) | −0.00075 (0.7418) | −0.00245 (0.2565) |
| Age 85 years or older | −0.00172 (0.3950) | −0.00106 (0.6751) | −0.00239 (0.3012) |
| Cost outcomes | |||
| Total 90‐day episode costs | −954*** (0.0000) | −883*** (0.0000) | −1025*** (0.0000) |
| SNF 90‐day costs | −434** (0.0066) | −352* (0.0198) | −516** (0.0031) |
| Inpatient costs (index procedure) | −134 (0.0742) | −109 (0.1811) | −160* (0.0358) |
| Outpatient 90‐day costs | 14.74 (0.1922) | 2.88 (0.8153) | 26.58 (0.0508) |
| Durable medical equipment 90‐day costs | −3.84 (0.4110) | −5.63 (0.2337) | −2.05 (0.6909) |
| Home health agency 90‐day costs | 13.00 (0.8979) | 32.12 (0.7352) | −6.10 (0.9553) |
| BPCI inpatient 90‐day costs | −375* (0.0202) | −417** (0.0062) | −334 (0.0637) |
| BPCI Part B 90‐day costs | −34.17 (0.2592) | −34.84 (0.2451) | −33.50 (0.3080) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.00323 (0.0537) | −0.00377 (0.0779) | −0.00267 (0.2134) |
| Mortality (30 days) | −0.000800 (0.1488) | −0.000778 (0.2423) | −0.000823 (0.2525) |
| Mortality (90 days) | −0.000647 (0.4429) | −0.000866 (0.4140) | −0.000412 (0.6858) |
| PE | 0.000102 (0.9230) | 0.000054 (0.9633) | 0.000149 (0.9061) |
| DVT | 0.00024 (0.8587) | −0.00046 (0.7841) | 0.00094 (0.5210) |
| Volume | |||
| Length of stay (day) | −0.2314 (0.1998) | −0.2763 (0.1180) | −0.1866 (0.3617) |
| Number of episode | −0.89 (0.2001) | −0.87 (0.2976) | −0.91 (0.1643) |
| SNF utilization | |||
| Discharge to SNF | −0.0087 (0.2653) | −0.0069 (0.3763) | −0.0108 (0.2122) |
| SNF duration (day) | −0.47* (0.0163) | −0.38* (0.0412) | −0.55** (0.0081) |
Note: Column 1 represents difference‐in‐differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference‐in‐differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
p < 0.05; **p < 0.01; ***p < 0.001; p value in parenthesis.
TABLE A7.
Overall effect of CJR for ED/urgent only admissions (with year‐quarter‐fixed effects)
| Outcomes | (1) | (2) | (3) |
|---|---|---|---|
| CJR (overall) | CJR (2016) | CJR (2017) | |
| Patient selection | |||
| Age | 0.26* (0.0435) | 0.31* (0.0318) | 0.20 (0.2136) |
| Female | −0.013* (0.0277) | −0.015 (0.0520) | −0.011 (0.1480) |
| White | −0.0014 (0.7041) | −0.00061 (0.5998) | −0.0022 (0.5998) |
| Black | 0.0040 (0.2537) | 0.0042 (0.2932) | 0.0038 (0.3959) |
| Disabled | 0.0048 (0.6984) | −0.015 (0.4819) | 0.0177 (0.1527) |
| CCI (mean) | 0.051 (0.1096) | 0.054 (0.1174) | 0.047 (0.2294) |
| CCI of 0 | −0.015* (0.0404) | −0.011 (0.1794) | −0.020* (0.0298) |
| CCI of 1 | −0.0044 (0.4235) | −0.0086 (0.1485) | 0.000051 (0.9950) |
| CCI of 2 or higher | 0.0193** (0.0043) | 0.0194** (0.0082) | 0.0192* (0.0238) |
| Age 65–69 years | −0.0029 (0.4731) | −0.0055 (0.2911) | −0.00015 (0.9773) |
| Age 70–74 years | −0.0035 (0.4475) | −0.0038 (0.4762) | −0.0032 (0.5774) |
| Age 75–79 years | 0.00010 (0.9901) | −0.0042 (0.4628) | 0.0046 (0.3385) |
| Age 80–84 years | −0.0053 (0.2509) | −0.00060 (0.9203) | −0.010 (0.0796) |
| Age 85 years or older | 0.014* (0.0410) | 0.016 (0.0543) | 0.013 (0.1464) |
| Cost outcomes | |||
| Total 90‐day episode costs | −1052*** (0.0003) | −1147*** (0.0008) | −950** (0.0039) |
| SNF 90‐day costs | −75 (0.6724) | 61 (0.7194) | −219 (0.3073) |
| Inpatient costs (index procedure) | −82 (0.4195) | −86 (0.4486) | −76 (0.5242) |
| Outpatient 90‐day costs | 14.3 (0.6678) | −1.99 (0.9492) | 31.7 (0.5002) |
| Durable medical equipment 90‐day costs | 1.31 (0.8298) | −2.48 (0.7472) | 5.36 (0.4455) |
| Home health agency 90‐day costs | −72 (0.2976) | −74 (0.3132) | −70 (0.3407) |
| BPCI inpatient 90‐day costs | −753** (0.0011) | −959*** (0.0004) | −532* (0.0273) |
| BPCI Part B 90‐day costs | −86* (0.0310) | −85 (0.0662) | −87* (0.4810) |
| Quality outcomes | |||
| 90‐day readmission (any reasons) | −0.00039 (0.9346) | −0.0022 (0.7178) | 0.0015 (0.7784) |
| Mortality (30 days) | −0.0034 (0.2205) | −0.0033 (0.2898) | −0.0035 (0.3817) |
| Mortality (90 days) | −0.0034 (0.4508) | −0.0040 (0.4138) | −0.0026 (0.6526) |
| PE | −0.00039 (0.8838) | −0.000019 (0.996) | −0.00080 (0.8078) |
| DVT | −0.0016 (0.6213) | −0.0024 (0.5604) | −0.00083 (0.8230) |
| Volume | |||
| Length of stay (day) | −0.31 (0.1798) | −0.24 (0.2719) | −0.38 (0.1623) |
| Number of episode | −1.69 (0.2081) | −2.28 (0.2322) | −1.06 (0.1823) |
Note: Column 1 represents difference in differences estimates during the first 2 years of the CJR program. Columns 2 and 3 represent difference‐in‐differences estimates during the first year (2016) of the CJR program and the second year (2017) of the CJR program, respectively. For continuous variables (costs, length of stay, number of episodes, and Charlson Comorbidity Index [mean]), estimated coefficients represent a change in each unit. For binary outcomes (30‐day mortality, 90‐day mortality, 90‐day readmission rate, PE, DVT, female, White, Black, disabled, Charlson Comorbidity Index of 0, 1, and 2+, age between 65 and 69 years, age between 70 and 74 years, age between 75 and 79 years, age between 80 and 84 years, and age older than 85 years), they represent a percentage point (ppts) change.
Abbreviations: BPCI, bundled payment for care improvement; CCI, Charlson Comorbidity Index; CJR, Comprehensive Care for Joint Replacement; DVT, deep vein thrombosis; PE, pulmonary embolism; SNF, skilled nursing facilities.
p < 0.05 **p < 0.01 ***p < 0.001; p value in parenthesis.
Ko H, Martin BI, Nelson RE, Pelt CE. Patient selection in the Comprehensive Care for Joint Replacement model. Health Serv Res. 2022;57(1):72‐90. doi: 10.1111/1475-6773.13880
Funding information Agency for Healthcare Research and Quality, Grant/Award Number: R01HS024714
REFERENCES
- 1. Centers for Medicare & Medicaid Services (CMS), HHS . Medicare program; Comprehensive Care for Joint Replacement Payment Model for acute care hospitals furnishing lower extremity joint replacement services. Final rule. Fed Regist. 2015;80(226):73273. https://www.federalregister.gov/documents/2015/11/24/2015-29438/medicare-program-comprehensive-care-for-joint-replacement-payment-model-for-acute-care-hospitals [PubMed] [Google Scholar]
- 2. Lewin Group, CMS Comprehensive Care for Joint Replacement Model: Performance Year 1 Evaluation Report. Appendices. 2018. Accessed October 29, 2020. https://innovation.cms.gov/Files/reports/cjr-firstannrptapp.pdf
- 3. Centers for Medicare & Medicaid Services . Comprehensive Care for Joint Replacement model. Accessed December 23, 2020 https://innovation.cms.gov/initiatives/cjr
- 4. Lewin Group, CMS Comprehensive Care for Joint Replacement Model: Performance Year 2 Evaluation Report. 2019. Accessed November 07, 2020. https://innovation.cms.gov/Files/reports/cjr-secondannrpt.pdf
- 5. Humbyrd CJ, Wu SS, Trujillo AJ, Socal MP, Anderson GF. Patient selection after mandatory bundled payments for hip and knee replacement: limited evidence of lemon‐dropping or cherry‐picking. J Bone Joint Surg Am. 2020;102(4):325‐331. [DOI] [PubMed] [Google Scholar]
- 6. Bernstein DN, Reitblat C, van de Graaf VA, et al. Is there an association between bundled payments and “cherry picking” and “lemon dropping” in orthopaedic surgery? A systematic review. Clin Orthop Relat Res. 2021; Publish Ahead of Print. 10.1097/corr.0000000000001792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agarwal R, Liao JM, Gupta A, Navathe AS. The impact of bundled payment on health care spending, utilization, and quality: a systematic review: a systematic review of the impact on spending, utilization, and quality outcomes from three Centers for Medicare and Medicaid Services bundled payment programs. Health Aff. 2020;39(1):50‐57. [DOI] [PubMed] [Google Scholar]
- 8. Finkelstein A, Ji Y, Mahoney N, Skinner J. Mandatory Medicare bundled payment program for lower extremity joint replacement and discharge to institutional postacute care: interim analysis of the first year of a 5‐year randomized trial. JAMA. 2018;320(9):892‐900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gray CF, Prieto HA, Duncan AT, Parvataneni HK. Arthroplasty care redesign related to the Comprehensive Care for Joint Replacement Model: results at a tertiary academic medical center. Arthroplasty Today. 2018;4(2):221‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barnett ML, Wilcock A, McWilliams JM, et al. Two‐year evaluation of mandatory bundled payments for joint replacement. N Engl J Med. 2019;380(3):252‐262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Haas DA, Zhang X, Kaplan RS, Song Z. Evaluation of economic and clinical outcomes under centers for Medicare & Medicaid Services mandatory bundled payments for joint replacements. JAMA Intern Med. 2019;179(7):924‐931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zibulewsky J. The emergency medical treatment and active labor act (EMTALA): what it is and what it means for physicians. Bayl Univ Med Cent Proc. 2001;14:339‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. American Hospital Association . Sicker, more complex patients are driving up intensity of ED care. Issue Brief. 2013;13(1). http://www.aha.org/content/13/13issuebrief-ed.pdf [Google Scholar]
- 14. Lewin Group, CMS Comprehensive Care for Joint Replacement Model: Performance Year 1 Evaluation Report. 2018. Accessed July 01, 2021. https://innovation.cms.gov/files/reports/cjr-firstannrpt.pdf
- 15. Angrist JD, Pischke JS. Mostly Harmless Econometrics: An Empiricist's Companion. Princeton University Press; 2008. [Google Scholar]
- 16. Heckman JJ, Smith JA. The pre‐programme earnings dip and the determinants of participation in a social programme. Implications for simple programme evaluation strategies. Econ J. 1999;109(457):313‐348. [Google Scholar]
- 17. CMS Virtual Research Data Center . https://www.resdac.org/cms-virtual-research-data-center-vrdc
- 18. The Bureau of Economic Analysis . Accessed September 8, 2020. https://apps.bea.gov/iTable/iTable.cfm?reqid=19&step=3&isuri=1&1921=survey&1903=13#reqid=19&step=3&isuri=1&1921=survey&1903=13
- 19. Mihaylova B, Briggs A, O'Hagan A, Thompson SG. Review of statistical methods for analysing healthcare resources and costs. Health Econ. 2011;20(8):897‐916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461‐494. [DOI] [PubMed] [Google Scholar]
- 21. Buntin MB, Zaslavsky AM. Too much ado about two‐part models and transformation?: comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23(3):525‐542. [DOI] [PubMed] [Google Scholar]
- 22. Bertrand M, Duflo E, Mullainathan S. How much should we trust differences‐in‐differences estimates? Q J Econ. 2004;119(1):249‐275. [Google Scholar]
- 23. Centers for Medicare & Medicaid Services . Chronic conditions data warehouse. ‘Medicare Beneficiary Counts’. Accessed September 21, 2020. https://www2.ccwdata.org/web/guest/medicare-tables-reports
- 24. Mayfield CK, Haglin JM, Levine B, Della Valle C, Lieberman JR, Heckmann N. Medicare reimbursement for hip and knee arthroplasty from 2000 to 2019: an unsustainable trend. J Arthroplasty. 2020;35(5):1174‐1178. [DOI] [PubMed] [Google Scholar]
- 25. Murphy BPD'S, Dowsey MM, Choong PFM. The impact of advanced age on the outcomes of primary total hip and knee arthroplasty for osteoarthritis: a systematic review. JBJS Rev. 2018;6(2):e6. [DOI] [PubMed] [Google Scholar]
- 26. Amen TB, Varady NH, Rajaee S, Chen AF. Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the US: a comprehensive analysis of trends from 2006 to 2015. J Bone Joint Surg Am. 2020;102(9):811‐820. [DOI] [PubMed] [Google Scholar]
- 27. Kim H, Meath THA, Quiñones AR, McConnell KJ, Ibrahim SA. Association of Medicare mandatory bundled payment program with the receipt of elective hip and knee replacement in White, Black, and Hispanic beneficiaries. JAMA Netw Open. 2021;4(3):e211772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thirukumaran CP, Kim Y, Cai X, et al. Association of the comprehensive care for joint replacement model with disparities in the use of total hip and total knee replacement. JAMA Netw Open. 2021;4(5):e2111858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hinman AD, Chan PH, Prentice HA, Paxton EW, Okike KM, Navarro RA. The association of race/ethnicity and total knee arthroplasty outcomes in a universally insured population. J Arthroplasty. 2020;35(6):1474‐1479. [DOI] [PubMed] [Google Scholar]
- 30. Thirukumaran CP, Cai X, Glance LG, et al. Geographic variation and disparities in Total joint replacement use for Medicare beneficiaries: 2009 to 2017. J Bone Joint Surg Am. 2020;102(24):2120‐2128. [DOI] [PMC free article] [PubMed] [Google Scholar]


