Public health restrictions caused by the COVID-19 pandemic have disrupted routine physical activities.1 , 2 Little objective information is available on the extent to which physical activity (PA) has changed among patients with cardiovascular disease who are at high risk of adverse clinical outcomes from reduced activity. We sought to assess trends in PA levels among patients with pacemakers and implantable cardioverter-defibrillators, devices that provide reliable measurements of activity level,3 in New York City (NYC) and Minneapolis/Saint Paul (MSP) from 2019 to 2020. We hypothesized that COVID-19 restrictions were associated with a significant decrease in PA.
A deidentified dataset of individuals aged ≥18 years from NYC and MSP with pacemakers or implantable cardioverter-defibrillators transmitting between January 1, 2019, and December 31, 2020, was derived from Boston Scientific Corporation’s LATITUDE database. These 2 cities were chosen for their data availability and asynchronous COVID-19 case burdens. PA was measured through an accelerometer that detected the frequency and amplitude of patient motion. An algorithm specified whether the sensor exceeded a threshold of 25 milligravities, corresponding to a walking speed of 2 miles/hour, to determine a state of “active” or “not active” for a given minute. Daily activity level was defined as minutes spent in an active state per day. These measures have been used in previous studies.4
We assessed the trends in daily activity levels using the 7-day moving average of activity in 2020, overall and by age and sex. Data from 2019 were used as a comparator to account for seasonal variability. We considered 2-sided P values <0.05 as statistically significant. Analyses were performed using R version 4.0.2 (R Foundation). This study was approved by the Institutional Review Board at Yale University.
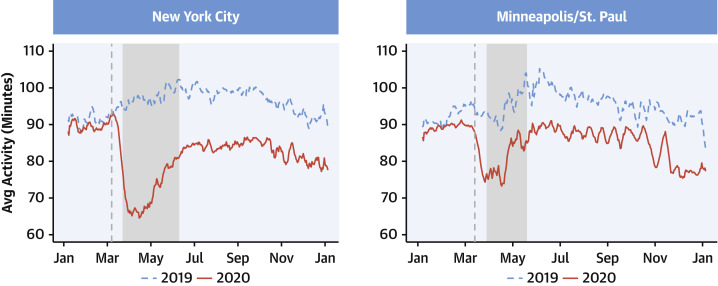
A total of 11,102 patients from NYC (n = 7,279) and MSP (n = 3,823) were included (median age 76 years [IQR: 67-84 years]; 42.4% women). Before COVID-19 restrictions began in 2020, the average daily PA was 89.7 ± 4.7 minutes in NYC and 89.1 ± 4.3 minutes in MSP. PA significantly declined during the lockdown period in each city (P < 0.001, Figure 1 ). Compared with data from the same period of 2019, the median reductions in PA were 26 minutes (26% reduction) in NYC and 14 minutes (15% reduction) in MSP. This represented a walking distance reduction of 1 and 0.5 miles daily for patients in NYC and MSP. In both cities, PA decreased the most during the first 2 weeks of the regional lockdown, and then increased slowly. However, 5 months after restrictions were lifted, activity levels had not returned to 2019 levels. The 2020 median daily activity level remained 14.5 minutes (84.5 minutes vs 99.0 minutes; P < 0.01) lower in NYC and 9.6 minutes (81.2 minutes vs 95.5 minutes; P < 0.01) lower in MSP. These trends were consistent by age and sex.
Figure 1.
Daily Activity Trends Among Patients With Intracardiac Remote Monitoring Devices
(Left) Daily activity trends among patients in New York City (NYC). (Right) Daily activity trends among patients in Minneapolis/Saint Paul (MSP). In both panels, daily activity levels were calculated using the 7-day moving average of activity in 2020 (solid line), and data from 2019 (dashed line) were used as a comparator to account for seasonal variability. The vertical dashed line is the date of regional emergency declaration (March 7, 2020, for NYC; March 13, 2020, for MSP) and the shaded area is the stay-at-home order (March 22 to June 8, 2020, for NYC; March 28 to May 18, 2020, for MSP). Marked declines in daily activity were observed during COVID-19 restrictions in both NYC and MSP, and activity levels did not return to prerestriction levels months after restrictions were eased.
In this large observational study, we found marked declines in PA during COVID-19 restrictions that were consistent across age and sex subgroups. Moreover, PA among these patients did not return to prerestriction levels months after restrictions were eased. These findings highlight the need to identify patients with significant activity reductions, support simple and safe ways to stay physically active within the limits of pandemic restrictions, and resume prior activities as restrictions are lifted.
Our results were consistent with a recent systematic review that showed decreases in PA during COVID-19 lockdowns across multiple populations.1 We extended prior studies by assessing postlockdown PA levels. Compared with NYC, the decline of PA in MSP was less dramatic; it coincided with the NYC emergency order but before the MSP emergency order. People in MSP may have adjusted behavior based on trends in other cities.2
Our study is limited by lacking detail information on medical history, sociodemographic characteristics, and type and intensity of activity. Therefore, we cannot assess populations most vulnerable to physical inactivity sequelae.
In conclusion, the public health restrictions for COVID-19 were associated with a persistent decrease in PA among patients with cardiovascular disease.
Footnotes
Dr Lu is supported by the National Heart, Lung, and Blood Institute (K12HL138037) and the Yale Center for Implementation Science; and was a recipient of a research agreement, through Yale University, from the Shenzhen Center for Health Information for work to advance intelligent disease prevention and health promotion. Mr Jones and Dr Ahmed are employees of the Boston Scientific Cooperation. Dr Murugiah works under contract with the Centers for Medicare & Medicaid Services to support quality measurement programs. Dr Krumholz has received expenses and/or personal fees from UnitedHealth, IBM Watson Health, Element Science, Aetna, Facebook, the Siegfried and Jensen Law Firm, Arnold and Porter Law Firm, Martin/Baughman Law Firm, F-Prime, Massachusetts Medical Society, and the National Center for Cardiovascular Diseases in Beijing; he is a co-founder of Refactor Health and HugoHealth; and has received grants and/or contracts from the Centers for Medicare & Medicaid Services, Medtronic, U.S. Food and Drug Administration, Johnson & Johnson, Foundation for a Smoke-Free World, State of Connecticut Department of Public Health, Agency for Healthcare Research and Quality, National Institutes of Health, American Heart Association, and the Shenzhen Center for Health Information. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
References
- 1.Stockwell S., Trott M., Tully M., et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ Open SEM. 2021;7 doi: 10.1136/bmjsem-2020-000960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hunter R.F., Garcia L., de Sa T.H., et al. Effect of COVID-19 response policies on walking behavior in US cities. Nat Commun. 2021;12:3652. doi: 10.1038/s41467-021-23937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parthiban N., Esterman A., Mahajan R., et al. Remote monitoring of implantable cardioverter-defibrillators: a systematic review and meta-analysis of clinical outcomes. J Am Coll Cardiol. 2015;65:2591–2600. doi: 10.1016/j.jacc.2015.04.029. [DOI] [PubMed] [Google Scholar]
- 4.Kramer D.B., Mitchell S.L., Monteiro J., et al. Patient activity and survival following implantable cardioverter-defibrillator implantation: the ALTITUDE activity study. J Am Heart Assoc. 2015;4 doi: 10.1161/JAHA.115.001775. [DOI] [PMC free article] [PubMed] [Google Scholar]