Abstract
The consensus of the Asia Pacific Heart Rhythm Society (APHRS) on stroke prevention in atrial fibrillation (AF) has been published in 2017 which provided useful clinical guidance for cardiologists, neurologists, geriatricians, and general practitioners in the Asia-Pacific region. In these years, many important new data regarding stroke prevention in AF were reported. The practice guidelines subcommittee members comprehensively reviewed updated information on stroke prevention in AF, and summarized them in this 2021 focused update of the 2017 consensus guidelines of the APHRS on stroke prevention in AF. We highlighted and focused on several issues, including the importance of the AF Better Care pathway, the advantages of non-vitamin K antagonist oral anticoagulants (NOACs) for Asians, the considerations of use of NOACs for Asian AF patients with single one stroke risk factor beyond gender, the role of lifestyle factors on stroke risk, the use of oral anticoagulants during the “coronavirus disease 2019” pandemic, etc. We fully realize that there are gaps, unaddressed questions, and many areas of uncertainty and debate in the current knowledge of AF, and the physician's decision remains the most important factor in the management of AF.
Keywords: APHRS, atrial fibrillation, stroke prevention, consensus guidelines, executive summary
Epidemiology of AF and Risk of AF-Related Stroke
Atrial fibrillation (AF) is a global problem, with an increasing incidence and prevalence with an aging population. 1 Similar to Western countries, the prevalence rates of AF will continuously increase in the following decades, which are projected to be 4.0% in Taiwan and 5.4% in South Korea in year 2050 ( Fig. 1 ). 2 3
Fig. 1.

Projected prevalence of AF in Taiwan and South Korea. Data used in the figure were adapted from Chao et al and Kim et al. 2 3 AF, atrial fibrillation.
For Asian AF patients, the annual risk of ischemic stroke is around 3.0% (1.60–4.95%) based on the pooled analysis of eight studies. 4 Importantly, the 1-year risk of ischemic stroke after newly diagnosed AF was similar from year 2000 (4.45%) to 2010 (3.95%), 2 and gradually decreasing in the era of non-vitamin K antagonist (non-VKA) oral anticoagulants (NOACs). 5 The observed reduction in stroke risk may be contributed to the increasing initiation rates of oral anticoagulants (OACs) in newly diagnosed AF patients, which significantly increased from 13.6 to 35.6%, contemporaneous with the introduction of NOACs ( Fig. 2 ). 5
Fig. 2.

Temporal trend of prescriptions of OACs and risks of clinical events in newly diagnosed AF patients. The figure was redrawn and data were adapted from Chao et al. 5 AF, atrial fibrillation; OACs, oral anticoagulants.
This is an executive summary of the 2021 focused update of the 2017 consensus guidelines of the Asia-Pacific Heart Rhythm Society (APHRS) on stroke prevention in AF. The full document has been published in Journal of Arrhythmia 6 and includes further details of the evidence/data pertaining to the recommendations made in these guidelines.
The Importance of Integrated or Holistic Care in Managing Patients with AF: Impact on Stroke Risk Reduction and Adverse Outcomes in AF
Since AF patients usually had multiple comorbidities, a more holistic and integrated approach to AF management has been proposed to improve clinical outcomes in patients with AF. 7
This integrated approach is directed at stroke prevention, better symptom management, and to tackle other cardiovascular risk factors/comorbidities (e.g., hypertension) aimed to reduce AF-related mortality, morbidity, and hospitalizations. This can streamline decision-making for a holistic approach to AF management in an integrated manner, proposed as the ABC (Atrial fibrillation Better Care) pathway ( Fig. 3 ) 7 :
Fig. 3.

The ABC pathway of integrated care management. The figure was redrawn and modified from Lip et al. 7 ABC, Atrial fibrillation Better Care; NOAC, non-vitamin K antagonist oral anticoagulant; OAC, oral anticoagulant; TTR, time in therapeutic range; VKA, vitamin K antagonist.
“A”: Avoid stroke with anticoagulation, i.e., well-managed warfarin (time in therapeutic range [TTR] > 65–70%) or NOACs. NOACs are recommended in preference to warfarin for NOAC-eligible AF patients.
“B”: Better symptom management with patient-centered symptom-directed decisions for rate or rhythm control.
-
“C”: Cardiovascular risk and comorbidity management (blood pressure [BP] control, heart failure, cardiac ischemia, sleep apnea, etc.) as well as lifestyle changes (obesity reduction, regular exercise, reducing alcohol/stimulants, psychological morbidity, etc.).
With the focus on patient-centered management, explanation using the simple ABC concept can also lead to improved understanding and disease awareness amongst patients, better knowledge about their condition, and the priorities of management. Different health care professionals managing the AF patient can also discuss the management based on the A, B, and C pillars of the ABC pathway.
A systematic review and meta-analysis showed a lower risk of all-cause death (odds ratio [OR]: 0.42, 95% confidence interval [CI]: 0.31–0.56), cardiovascular death (OR: 0.37, 95% CI: 0.23–0.58), stroke (OR: 0.55, 95% CI: 0.37–0.82), and major bleeding (OR: 0.69, 95% CI: 0.51–0.94), with management adherent to the ABC pathway compared with noncompliance ( Fig. 4 ). 8
Fig. 4.

Impacts of adherence to the ABC pathway on clinical outcomes in AF patients. The figure was redrawn and modified from Romiti et al. 8 ABC, Atrial fibrillation Better Care; CI, confidence interval; OR, odds ratio.
The integrated care AF pathway approach (“simple as ABC…”) has been adopted and promoted in the Primary Care Clinical Pathway for AF Detection and Management ( https://bit.ly/2FhrwXQ ). The key feedback from multidisciplinary colleagues is the reassurance felt that a holistic approach to management can be streamlined across primary–secondary care, not being regarded as complex but is “simple as ABC…” The ABC pathway is now included within guidelines from American College of Chest Physicians, 9 the Korean national AF guidelines, 10 and the 2020 European AF guidelines, 11 and is therefore recommended in this guideline as part of the holistic approach to AF management. In this APHRS consensus document, we will particularly focus on the “A” domain and update data for stroke prevention in AF, but would highlight the importance of full compliance with the ABC pathway to improve outcomes in AF patients.
Recommendation
-
An integrated care or holistic management approach, based on the ABC pathway is recommended to improve outcome in the Asian AF population:
“A”: Avoid stroke with anticoagulation, i.e., well-managed warfarin (TTR > 65–70%) or NOAC.
“B”: Better symptom management with patient-centered symptom-directed decisions for rate or rhythm control.
“C”: Cardiovascular risk and comorbidity management (BP control, heart failure, cardiac ischemia, sleep apnea, etc.) as well as lifestyle changes (obesity reduction, regular exercise, reducing alcohol/stimulants, psychological morbidity, etc.).
Stroke Risk Assessment (and Re-assessment)
In our 2017 consensus document, we recommended the use of the CHA 2 DS 2 -VASc score for stroke risk assessment for Asian AF patients. 12
In this focused update, we still recommend the use of the CHA 2 DS 2 -VASc score as the stroke risk prediction scheme since it has been well validated in the Asian AF population. 13 14 15 16 17 18 We should acknowledge that all clinical risk stratification scores are simplifications to aid decision-making, and to recognize the limitations of such scores. For example, there are many stroke risk factors 19 and only the more common and validated ones have been included into risk scores, such as the CHA 2 DS 2 -VASc score.
The impact of individual stroke risk factors is not uniform, and for a single CHA 2 DS 2 -VASc risk factor in those aged <65, and assuming an ischemic stroke risk treatment threshold of ≥1% per year with NOACs, the tipping point with heart failure as a single risk was age 35 years, while for patients with hypertension, diabetes mellitus, and vascular diseases, the age thresholds for treatment were 50 years, 50 years, and 55 years, respectively. 20 21 Not all CHA 2 DS 2 -VASc risk factors carry equal weight, as event rates would be dependent on the population studied (e.g., hospitalized vs. community), study type (trial vs. real world), ethnicity, and study methodology. 22
Also, stroke risk is not static, given that aging and incident comorbidities would increase risk and the dynamic nature of stroke risk in AF would result in increments of their CHA 2 DS 2 -VASc scores. 23 For example, in a study from Taiwan which enrolled 31,039 AF patients without comorbidities of the CHA 2 DS 2 -VASc score except for age and sex at baseline, the mean CHA 2 DS 2 -VASc scores increased from 1.29 to 2.31 during a follow-up of 171,956 person-years ( Fig. 5 ). 23 24 25 Similar observations were reported in the Korean nationwide AF registry. 26
Fig. 5.

Cumulative incidences of increment of CHA 2 DS 2 -VASc score to ≥1 (males) or ≥2 (females). The figure was redrawn and data were adapted from Chang et al and Chao et al. 23 25 AF, atrial fibrillation.
Both the follow-up CHA 2 DS 2 -VASc score and change in stroke risk (“delta-CHA 2 DS 2 -VASc” score, i.e., the difference between the baseline and follow-up scores) had better predictive value for ischemic stroke compared with the baseline CHA 2 DS 2 -VASc score. 24 27 For initially low-risk (CHA 2 DS 2 -VASc score 0 for males or 1 for females) nonanticoagulated AF patients, the use of OACs once their CHA 2 DS 2 -VASc scores increased was associated with a lower risk of clinical events. 28
In summary, regular reassessment of stroke risk of AF patients and the timely prescriptions of OACs once the stroke risk of patients increased is important, given the increase in stroke risks with age and new comorbidities.
Frequency of Stroke Risk Reassessment
Data regarding the reasonable timing interval at which the stroke risk of AF patients should be reassessed are limited. In the study by Chao et al, which studied 14,606 AF patients with a baseline CHA 2 DS 2 -VASc score of 0 (males) or 1 (females), 6,188 patients acquired new risk factors with the acquisition of one or more new comorbidities approximately 4 to 5 months after their initial AF diagnosis; the most common incident comorbidity was hypertension, followed by heart failure, diabetes mellitus, and vascular disease; indeed, the onset of new comorbidities would depend on the type of comorbidity. Importantly, 596 of these original patients experienced ischemic stroke and the duration from the acquirement of incident comorbidities to the occurrence of ischemic stroke was an average of 4.4 months for 90% of the patients. 28 Based on these data, 4 months may be a reasonable timing interval at which the stroke risk of AF patients should be reassessed.
Recommendations
The CHA 2 DS 2 -VASc score is recommended for stroke risk assessment for Asian AF patients.
The stroke risk of AF patients is not static and should be reassessed regularly (at least annually and every 4 months if possible).
In patients with AF initially at low risk of stroke (CHA 2 DS 2 -VASc = 0 in men, or 1 in women), a reassessment of stroke risk should ideally be made at 4 months after the index evaluation and OACs should be prescribed in a timely manner once their CHA 2 DS 2 -VASc scores increase.
Bleeding Risk Assessment and Reassessment
As with the 2017 consensus document, the HAS-BLED score is recommended for bleeding risk assessment for Asian AF patients in this focused update. In a PCORI systematic review and evidence appraisal, the HAS-BLED score was found to be the best score for bleeding risk prediction. 29 In a recent analysis of ESC-EHRA EORP-AF General Long-Term Registry, the HAS-BLED score still performed better than the ORBIT score in the contemporary cohort of AF patients treated with NOACs. 30
The HAS-BLED score has been well validated in Asian cohorts, outperforming other bleeding risk scores (e.g., ATRIA, ORBIT, HEMORRH2AGES) and an approach simply focused only on modifiable bleeding risks. 31 The HAS-BLED score performs well even in contemporary AF patients taking NOACs. 30 Bleeding risk is also not static and may change among AF patients initially having a low HAS-BLED score (≤2). 32 In a previous study from Taiwan, the accuracy of the follow-up or delta HAS-BLED score in the prediction of major bleeding was significantly higher than that of the baseline HAS-BLED score; importantly, the bleeding risk is higher within several months after the increment of the HAS-BLED score. 32 The HAS-BLED score has also been validated in AF patients who are taking no antithrombotic therapy (e.g., when first diagnosed), antiplatelet therapy (e.g., when AF develops in patients on aspirin for vascular disease), and on anticoagulation (whether warfarin or NOACs). Thus, the HAS-BLED score would be applicable at all steps of the patient-management pathway.
Appropriate use of the HAS-BLED score has been tested in the mAFA-II trial, 33 which was a prospective cluster-randomized trial that compared an mHealth integrated care approach against usual care. The intervention arm used the HAS-BLED to identify and mitigate modifiable bleeding risks, and schedule high bleeding risk patients for regular review and follow-up; this led to lower major bleeding rates at 1 year and an increase in OAC use. 34 In contrast, the usual care arm has higher major bleeding and a decline in OAC use ( Fig. 6 ). A recent study from Taiwan further demonstrated that for anticoagulated AF patients with a baseline HAS-BLED score of 0 to 2 which increased to ≥3, the continuation of OACs was associated with better clinical outcomes. 35 A high HAS-BLED score is not a reason to withhold OACs even among AF patients with one non-sex risk factor (CHA 2 DS 2 -VASc score 1 for males and 2 for females) but a high bleeding risk (HAS-BLED score ≥ 3) as the use of OACs was still associated with a lower risk of composite adverse events of ischemic stroke, intracranial hemorrhage (ICH), or mortality (adjusted hazard ratio [aHR]: 0.781) in this population. 36
Fig. 6.

Use of OACs and risk of bleeding among patients who received integrated care approach and usual care. The figure was redrawn and modified from Guo et al. 34 AF, atrial fibrillation; BP, blood pressure; INR, international normalized ratio; NOAC, non-vitamin K antagonist oral anticoagulant; OACs, oral anticoagulants.
In summary, bleeding risk reassessment is important for anticoagulated AF patients, and the appropriate and responsible use of bleeding risk scores such as the HAS-BLED score is to identify and mitigate modifiable bleeding risk factors, and to identify high bleeding risk patients for early review and follow-up.
Recommendations
For bleeding risk assessment, a formal structured risk-score-based bleeding risk assessment with the HAS-BLED score is recommended to help identify nonmodifiable and address modifiable bleeding risk factors, and to identify patients potentially at high bleeding risk for early and more frequent clinical review and follow-up.
The bleeding risk of AF patients is not static, which should be reassessed regularly, and the identified modifiable bleeding risk factors should be corrected.
An increased HAS-BLED score in anticoagulated AF patients should not be the only reason to withhold OACs, but reminds physicians to correct modifiable bleeding risk factors and follow up patients more closely.
In this focused update, we emphasize the dynamic natures of CHA 2 DS 2 -VASc and HAS-BLED scores and highly emphasize the clinical importance of risk reassessment. The recommended clinical practice about stroke and bleeding risk assessments is summarized in Fig. 7 .
Fig. 7.

Stroke and bleeding risk assessment in AF. The figure was redrawn and modified from Chang et al. 23 AF, atrial fibrillation; NOAC, non-vitamin K antagonist oral anticoagulant; NSAIDs, nonsteroidal anti-inflammatory drugs; OACs, oral anticoagulants; TTR, time in therapeutic range.
Approach to Stroke Prevention in Asian AF Patients
Given the limitations of all stroke risk scores in predicting high stroke risk in AF patients and the dynamic nature of stroke risk, the artificial categorization into low, moderate, and high risk strata is discouraged. Thus, stroke prevention (which is oral anticoagulation) should be the default strategy, unless patients are at low risk (defined as CHA 2 DS 2 VASc score 0 in males or 1 in females). Fig. 8 shows our recommendations, which were consistent to other guidelines. 9
Fig. 8.

Three-step approach for the use of OACs for stroke prevention in AF. The flowchart was redrawn and modified from Lip et al. 9 AF, atrial fibrillation; INR, international normalized ratio; NOAC, non-vitamin K antagonist oral anticoagulant; OACs, oral anticoagulants; VKA, vitamin K antagonist.
Patients with AF and significant valvular heart disease (previously referred to as “valvular AF”), defined as prosthetic mechanical heart valves or moderate–severe mitral stenosis, should be offered warfarin, when oral anticoagulation is recommended. 37 Indeed, NOACs are contraindicated in such patients.
In other patients without significant valvular heart disease (so-called “nonvalvular AF” [NVAF]), the first step ( Step 1 ) is to identify low-risk patients (CHA 2 DS 2 VASc score 0 in males or 1 in females) where no antithrombotic therapy is recommended. The next step ( Step 2 ) is to offer stroke prevention (i.e., oral anticoagulation) to patients with ≥1 non-sex stroke risk factors (i.e., CHA 2 DS 2 VASc score ≥1 in males or ≥2 in females). Most of the randomized trials included patients with ≥2 non-sex stroke risk factors, but some clinical trials with warfarin (ACTIVE-W), dabigatran, and apixaban (RE-LY, ARISTOTLE, AVERROES) included patients with a single non-sex stroke risk factor. 38 39 40 41
Since the risk of stroke of each CHA 2 DS 2 -VASc risk component was not the same and age is an important driver, patients' ages and the comorbidities which contribute to the score 1 for males or 2 for females could be considered when making management decisions about the use of OACs or not 20 42 43 44 45 46 as summarized in Fig. 9 . As OAC is being started, bleeding risk assessment is recommended, using the HAS-BLED score to identify and mitigate modifiable bleeding risks, and to identify high bleeding risk patients for early review and follow-up.
Fig. 9.

Considerations about the use of NOACs for Asian AF patients with a CHA 2 DS 2 -VASc score of 1 (males) or 2 (females). AF, atrial fibrillation; NOAC, non-vitamin K antagonist oral anticoagulant.
Step 3 is to make the choice of OAC. We recommend the use of NOACs in preference to warfarin for stroke prevention. If NOACs are used, the recommended label dosing is important, given that the best outcomes are with label-adherent prescribing. 47 48 49 50 51 52 Apart from guideline-directed anticoagulation prescribing, adherence and persistence with therapy are important. 53 54 55
If warfarin is considered, we recommend a target international normalized ratio (INR) of 2.0 to 3.0 with an average TTR ≥65% (ideally ≥70%). We do not recommend low-intensity anticoagulation or lower target INRs, given the higher risk of thromboembolism although bleeding risk is lower. 56 Of note, a “one off” INR reading gives no indication of the quality of anticoagulation control, and many serious bleeds occur when the INR is between 2.0 and 3.0. 57 A high TTR is associated with low rates of stroke and bleeding, 58 but many factors influence the quality of anticoagulation control. The more common and validated factors associated with poor labile INRs have been used to formulate clinical risk scores such as the SAMe-TT 2 R 2 scores. A high SAMe-TT 2 R 2 score (>2) is associated with a likelihood of poor TTR, and such patients should be flagged up for more attention to ensure good-quality anticoagulation (e.g., education and counseling, more frequent INR checks) or to reconsider the decision to prescribe NOACs (if suitable). 59 60 61 62 63 One ongoing prospective randomized trial, TREAT-AF, is examining the impact of an educational intervention versus usual care on anticoagulation therapy control based on a SAMe-TT 2 R 2 score-guided management strategy amongst anticoagulant-naïve Thai patients with AF. 64
Recommendations
In AF patients with mechanical heart valves or moderate-to-severe mitral stenosis, warfarin is recommended.
For stroke prevention in AF patients without significant valvular heart disease (i.e., mechanical heart valves or moderate-to-severe mitral stenosis; so-called “valvular AF”) who are eligible for OAC, NOACs are recommended in preference to VKAs.
Clinical pattern of AF (i.e., whether first detected, paroxysmal, persistent, long-standing persistent, permanent) should not condition the indication to thromboprophylaxis, if stroke risk factors are present.
For stroke risk assessment, a risk-factor-based approach is recommended, using the CHA 2 DS 2 -VASc stroke risk score to initially identify patients at “low stroke risk” (CHA 2 DS 2 -VASc = 0 in men, or 1 in women) who should not be offered antithrombotic therapy.
In AF patients with CHA 2 DS 2 -VASc score ≥2 in men or ≥3 in women, OAC is recommended for stroke prevention.
In AF patients with a CHA 2 DS 2 -VASc score of 1 in men or 2 in women, OAC should be considered for stroke prevention. Different age thresholds for different comorbidities may help guide NOAC use (e.g., age 35 years for heart failure, 50 years for hypertension or diabetes mellitus, and 55 for vascular diseases).
-
If a VKA is used, a target INR of 2.0 to 3.0 is recommended, with individual TTR ≥65% (ideally ≥70%).
- A high SAMe-TT 2 R 2 score (>2) is associated with a likelihood of poor TTR, and such patients have more attention to ensure good-quality anticoagulation (e.g., education and counseling, more frequent INR checks) or to reconsider the decision to prescribe NOACs (if suitable).
-
In patients on VKAs with low time in INR therapeutic range (e.g., TTR < 70%), recommended options are:
- Switching to a NOAC but ensuring good adherence and persistence with therapy.
- Efforts to improve TTR (e.g., education/counseling and more frequent INR checks).
Antiplatelet therapy alone (monotherapy or aspirin in combination with clopidogrel) is not recommended for stroke prevention in AF patients.
Estimated bleeding risk, in the absence of absolute contraindications to OAC, or patients at high risk of falls, should not in itself guide treatment decisions to use OAC for stroke prevention.
Review Update Data Regarding Warfarin (Including INR Range) in Asia
When OAC is being considered, NOACs are the preferred option for stroke prevention in AF, because the benefits of NOAC on efficacy and safety compared with the VKAs are more profound in Asian than non-Asian population. 65 In some settings, the use of VKA is still needed because of the high cost of NOACs or in patients with specific indications including moderate to severe mitral stenosis and mechanical heart valves. Maintenance of a high TTR has been shown to reduce the risk of ischemic and bleeding events and should be the primary goal in the treatment of these patients independent of the type of management approach. Conversely, a change in the approach to these patients needs to be considered if a low TTR is consistently observed.
Several observational studies suggested that low-intensity warfarin therapy can reduce hemorrhage without increasing thromboembolism for East-Asian patients with NVAF receiving warfarin therapy, but the evidence is weak and no focus on quality of anticoagulation control, as reflected by TTR. 66 67 In a systematic review and evidence appraisal, low-intensity anticoagulation or lower target INRs are associated with a higher risk of thromboembolism although bleeding risk may be lower. 56 Of note, a “one off” INR reading does not reflect the quality of anticoagulation control, especially since many serious bleeds actually occur when the INR is between 2.0 and 3.0. 57 Hence, we strongly recommend evidence-based management, with the strongest data currently for INR 2.0 to 3.0 and TTR ideally ≥65% (or even 70%) in Asian patients. 68 We should ensure TTR is ≥65% (optimal ≥70%), with appropriate education and counseling, or more frequent INR checks. Efforts to improve OAC uptake, adherence, and persistence with therapy are also crucial, as are efforts to improve service provisions. 69 70 71
Recommendations
The use of VKA is recommended in patients with moderate to severe mitral stenosis and mechanical heart valve.
For the optimal management of VKA therapy, INR of 2.0 to 3.0 is recommended in Asian AF patients, with attention to ensure TTR is ≥65%.
Updates of the subanalyses of trials in Asia:
The results of the four pivotal phase III NOAC trials showed that all NOACs were at least noninferior to warfarin in prevention of stroke/thromboembolism, and NOACs were associated with lower rates of intracranial bleeding than was warfarin. In the meta-analysis of four NOACs, 72 NOACs significantly reduced stroke or systemic embolic events by 19% compared with warfarin (relative risk [RR]: 0.81, 95% CI: 0.73–0.91; p < 0.0001), mainly driven by a reduction in hemorrhagic stroke (RR: 0.49, 95% CI: 0.38–0.64; p < 0.0001). NOACs also significantly reduced all-cause mortality (RR: 0.90, 95% CI: 0.85–0.95; p = 0.0003) and ICH (RR: 0.48, 95% CI: 0.39–0.59; p < 0.0001), but increased gastrointestinal (GI) bleeding (RR: 1.25, 95% CI: 1.01–1.55; p = 0.04). There was a greater RR reduction in major bleeding with NOACs when the TTR was less than 66% than when it was 66% or more (RR: 0.69, 95% CI: 0.59–0.81 vs. RR: 0.93, 95% CI: 0.76–1.13; p for interaction = 0.022).
The efficacy and safety of NOACs was more profound in the Asian population than in non-Asian population. 65 Comparing with VKAs, standard-dose NOACs reduced stroke or systemic embolism (SE; OR = 0.65 vs. 0.85, p interaction = 0.045) more in Asians than in non-Asians and were safer in Asians than in non-Asians for major bleeding (OR = 0.57 vs. 0.89, p interaction = 0.004) and hemorrhagic stroke (OR = 0.32 vs. 0.56, p interaction = 0.046). There was no excess of GI bleeds in Asians, whereas GI bleeding was significantly increased in non-Asians (OR = 0.79 vs. 1.44, p interaction = 0.041). Generally, reduced-dose NOACs were safer than VKAs without heterogeneity in efficacy and safety between Asians and non-Asians, except for ischemic stroke, major bleeding, and GI bleeding. 65 In the recent subanalysis of ENGAGE AF-TIMI 48 trial comparing patients of Asian and non-Asian races, Asians treated with warfarin had a higher adjusted risk of ICH (aHR: 1.71, p = 0.03) compared with non-Asians. 73 Compared with warfarin, higher dose edoxaban significantly reduced ICH while preserving the efficacy of stroke prevention in both Asians and non-Asians. Two of three net clinical outcomes appeared to be more favorably reduced with edoxaban in Asians compared with non-Asians ( p int = 0.063 for primary, 0.037 for secondary, and 0.032 for third net clinical outcomes, respectively).
Real-World Data about NOACs in Asia
In a systematic review and meta-analysis of real-world comparisons of NOACs for stroke prevention in Asian patients with AF, 74 the NOACs were associated with lower risks of thromboembolism (HR: 0.70; [95% CI: 0.63–0.78]), acute myocardial infarction (0.67; [0.57–0.79]), all-cause mortality (0.62; [0.56–0.69]), major bleeding (0.59; [0.50–0.69]), ICH (0.50; [0.40–0.62]), GI bleeding (0.66; [0.46–0.95]), and any bleeding (0.82; [0.73–0.92]) than warfarin. While real-world data are no substitute for randomized trials, this meta-analysis shows that the NOACs had greater effectiveness and safety compared with warfarin in real-world practice for stroke prevention, among Asian patients with NVAF. 74
NOACs also showed better effectiveness and safety than warfarin in “high risk” real-world Asian AF populations including the very elderly, those with low body weight or liver disease. 45 75 76 77 78 79 80
The Importance of On-Label Dosing of NOACs in Asians
Varying degrees of renal function require recommendations for reduced dosing regimens of NOACs; however, different cut-off values for age, body weight, or interacting drugs also require consideration for appropriate dose selection. In routine clinical practice in Asia, prescribed NOAC doses are often inconsistent with drug labeling. 47 48 49 50 52 These prescribing patterns may be associated with worse safety profiles with no benefit in effectiveness in patients with severe kidney disease and worse effectiveness with no benefit in safety in apixaban-treated patients with normal or mildly impaired renal function. 81 82
In meta-analysis of four NOAC trials, low-dose NOAC regimens showed similar overall reductions in stroke or systemic embolic events to warfarin (RR: 1.03, 95% CI: 0.84–1.27; p = 0.74), and a more favorable bleeding profile (RR: 0.65, 95% CI: 0.43–1.00; p = 0.05), but significantly more ischemic strokes (RR: 1.28, 95% CI: 1.02–1.60; p = 0.045). 72
In patients eligible for reduced-dose NOACs, effects of reduced-dose NOACs compared with warfarin on stroke or SE (RR 0.84, 95% CI 0.69–1.03) and on major bleeding (RR: 0.70, 95% CI: 0.50–0.97) were consistent with those of full-dose NOACs relative to warfarin (RR: 0.86, 95% CI: 0.77–0.96 for stroke or SE and RR: 0.87, 95% CI: 0.70–1.08 for major bleeding; interaction p -values of 0.89 and 0.26, respectively). In addition, NOACs were associated with reduced risks of hemorrhagic stroke, ICH, fatal bleeding, and death regardless of patients' eligibilities for NOAC dose reduction (interaction p > 0.05 for each). 83
When checking the eligibility and determining the dosages of NOACs, it should be emphasized that the creatinine clearance (CCr) of AF patients should be calculated using the Cockcroft–Gault (CG) equation which was adopted in four pivotal randomized clinical trials. 84 Compared with the CG formula, modified diet in renal disease (MDRD) or Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equations would overestimate the renal functions of AF patients, especially for the elderly (≥75 years) and those with a low body weight (<50 kg). 85 The overestimations of the estimated glomerular filtration rates (eGFRs) would potentially result in inappropriate dosing of NOACs (mainly overdoing), and may therefore, attenuate the advantages of NOACs compared with warfarin. 85
A dose reduction of rivaroxaban in Asian patients might be necessary, but lacks the confirmation in large adequately powered prospective randomized clinical trials. Pharmacokinetic modeling data indicated that, at steady state, the distribution of both the maximum concentration and area under the curve (AUC) of rivaroxaban in Japanese patients with AF who received a 15 mg o.d. (once daily) dose of rivaroxaban would be comparable to the C max and AUC 0 to 24, in Caucasian patients with AF who received a 20 mg o.d. dose. Accordingly, instead of the 20 and 15 mg o.d. dose, the 15 and 10 mg o.d. doses of rivaroxaban were selected in Japan. The Korean AF guidelines recommend the use of 15 mg o.d. dose of rivaroxaban in very elderly (≥80 years) AF patients. 10 Another recent study from Taiwan which compared the clinical outcomes of AF patients receiving rivaroxaban following ROCKET-AF and J-ROCKET AF dosing regimens demonstrated that the risks of stroke/systemic and major bleeding did not differ significantly between the two groups. 86 However, a lower risk of major bleeding was observed for J-ROCKET AF dosing among patients with an eGFR <50 mL/min with a borderline p -value of 0.0445. 86 Of note, off-label underdosing rivaroxaban (10 mg/d for patients with an eGFR >50 mL/min) should be avoided since it was associated with a 2.75-fold higher risk of ischemic stroke. 49
Recommendations
Because NOACs are more effective and safer than warfarin in Asian AF patients, NOACs are the recommended choice of oral anticoagulation in Asian AF patients.
The CG equation should be adopted to calculate CCr to determine the dosing of NOACs.
On-label or guideline-adherent dosing of NOACs is recommended in Asian patients.
AF Complicating Acute Coronary Syndrome/Percutaneous Coronary Intervention
AF often occurs in patients with coronary artery disease (CAD). It has been reported that 5 to 8% of patients who undergo percutaneous coronary intervention (PCI) have AF. 87 88 Importantly, patients with CAD and AF are at high risk of stroke.
In the warfarin era, a major concern in Asian patients with AF was the risk of serious bleeding by combining OAC with antiplatelets; however, temporal trends of patients with AF undergoing PCI after introduction of NOAC show increasing use of OAC and combination therapy with antiplatelets, especially in the NOAC era ( Fig. 10 ). 89
Fig. 10.

Increasing use of OACs (especially NOACs) and combination therapy with antiplatelet agents among AF patients undergoing percutaneous coronary intervention. The figure was redrawn and data were adapted from Kwon et al. 89 AF, atrial fibrillation; DAPT, dual antiplatelet therapy; NOAC, non-vitamin K antagonist oral anticoagulant.
Patients with CAD and AF are not only at risk of stroke, but also at risk of bleeding due to associated comorbidities, and decision making should balance ischemic and bleeding risks when considering the duration, type, and treatment regime especially given the potential sensitivity of Asians to bleeding risks on OAC ( Fig. 11 ). 90 91
Fig. 11.

Factors tipping the balance between ischemic and bleeding risk in AF patients presenting with ACS and/or undergoing PCI. The figure was redrawn and modified from Vitolo et al. 90 ACS, acute coronary syndrome; AF, atrial fibrillation; BMI, body mass index; BRS, bioresorbable scaffold; CKD, chronic kidney disease; CTO, chronic total occlusion; DAT, dual antithrombotic therapy; DES, drug-eluting stent; ESRD, end-stage renal disease; LAD, left anterior descending artery; MI, myocardial infarction; NSAID, nonsteroidal anti-inflammatory drug; PCI, percutaneous coronary intervention; TAT, triple antithrombotic therapy.
In the warfarin era, the WOEST study demonstrated a higher bleeding risk of triple therapy compared with double therapy of OACs and clopidogrel. 92 More recently, the safety and efficacy of NOACs in combination with antiplatelet drugs in patients with CAD and AF have been reported in the PIONEER AF-PCI, 93 RE-DUAL PCI, 94 AUGUSTUS, 95 and ENTRUST-AF PCI trials. 96 The summary of those trials is presented in Table 1 .
Table 1. Summary of four randomized clinical trials in patients with coronary artery disease and atrial fibrillation 93 94 95 96 .
| PIONEER-PCI | RE-DUAL PCI | AUGUSTUS | ENTRUST-AF PCI | |
|---|---|---|---|---|
| No. of participating patients (Asian patients, %) | 2,124 (4.0%) |
2,725 (NA) |
4,614 (3.1%) |
1,506 (11.2%) |
| Randomization | • Rivaroxaban 15 mg + a P2Y12 inhibitor (group 1) • Rivaroxaban 2.5 mg + DAPT (group 2) • VKA + DAPT (group 3) |
• Dabigatran 110 mg + a P2Y12 inhibitor • Dabigatran 150 mg + a P2Y12 inhibitor • VKA + DAPT (except United States, dabigatran 110 mg + a P2Y12 inhibitor or VKA + DAPT for elderly patients) |
A 2 × 2 factorial design • Apixaban 5 mg vs. VKA • Aspirin vs. placebo |
• Edoxaban 60 mg + a P2Y12 inhibitor vs. VKA + DAPT |
| Duration from the PCI to randomization | Within 72 hours | Within 120 hours | Within 14 days | 4 hours to 5 days |
| Primary endpoint | Major or minor bleeding | Major or minor bleeding | Major or minor bleeding | Major or minor bleeding |
| Hazard ratio for the primary endpoint | Group 1 vs. group 3: 0.59 (0.47–0.76) Group 2 vs. group 3: 0.63 (0.50–0.80) |
Dabigatran 110 mg vs. VKA + DAPT: 0.52 (0.42–0.63) Dabigatran 150 mg vs. VKA + DAPT: 0.72 (0.58–0.88) |
Apixaban 5 mg vs. VKA: 0.69 (0.58–0.81) Aspirin vs. placebo: 1.89 (1.59–2.24) |
Edoxaban + a P2Y12 inhibitor vs. VKA + DAPT: 0.83 (0.65–1.05) |
Abbreviations: DAPT, dual antiplatelet therapy; PCI, percutaneous coronary intervention; VKA, vitamin K antagonist.
In the PIONEER AF-PCI, RE-DUAL PCI, and ENTRUST-AF PCI trials, dual therapy with a NOAC and a P2Y12 inhibitor was compared with a triple therapy with warfarin plus a dual antiplatelet therapy (DAPT). In the RE-DUAL PCI trial, elderly patients (≥80 years; age ≥ 70 years in Japan) were given 110 mg of dabigatran when assigned to the dual therapy group. The PIONEER AF-PCI and RE-DUAL PCI trials demonstrated that dual therapy decreased bleeding and did not increase thrombotic events, as compared with triple therapy. In the ENTRUST-AF PCI trial, dual therapy was noninferior to triple therapy for bleeding. The RE-DUAL PCI trial was also adequately powered to investigate a comparison of the combined dabigatran arms against warfarin for the composite thrombotic outcomes, and no significant difference was seen. The highest ticagrelor use was in RE-DUAL PCI, where 12% of the trial cohort used ticagrelor instead of clopidogrel; no significant interaction was evident. 97 Based on these trials, a NOAC-based anticoagulation strategy was safer than a warfarin-based strategy in terms of bleeding.
The role of aspirin was tested in the AUGUSTUS trial using a two-by-two factorial design. 95 In the AUGUSTUS trial, the use of apixaban reduced bleeding by 31% as compared with VKAs, and the use of aspirin resulted in an increase in bleeding by 47%, i.e., dual therapy with apixaban and a P2Y12 inhibitor was associated with a lower rate of bleeding than triple therapy or dual therapy with warfarin. Furthermore, patients taking apixaban had a lower incidence of death or hospitalization than those taking VKAs, mainly driven by a reduction in the incidence of hospitalizations. The incidence of death or ischemic events did not differ significantly between aspirin and a placebo or between apixaban and VKAs, but was numerically greater in the placebo-treated patients compared with aspirin. The incidence of stroke decreased by 50% in patients with apixaban as compared those with VKAs.
In all four trials, randomization was performed after the PCI, and all patients were treated by triple therapy during the periprocedural period, in which stent thromboses were most likely to occur. Thus, this consensus recommends an initial period of triple therapy with OAC plus a DAPT during the PCI and the following 7 to 28 days, depending on the balance between thrombotic and bleeding risks ( Fig. 12 ), as recommended by 2021 European Heart Rhythm Association (EHRA) Practical Guide on the Use of NOACs in Patients with AF. 98 Indeed, in patients at very high bleeding risks and acceptable thrombotic risk, aspirin may be dropped much earlier. In contrast, where patients have a high thrombotic risk (e.g., post-acute coronary syndrome [post-ACS]) but acceptable bleeding risks, the period of triple therapy should be continued for at least 4 weeks.
Fig. 12.
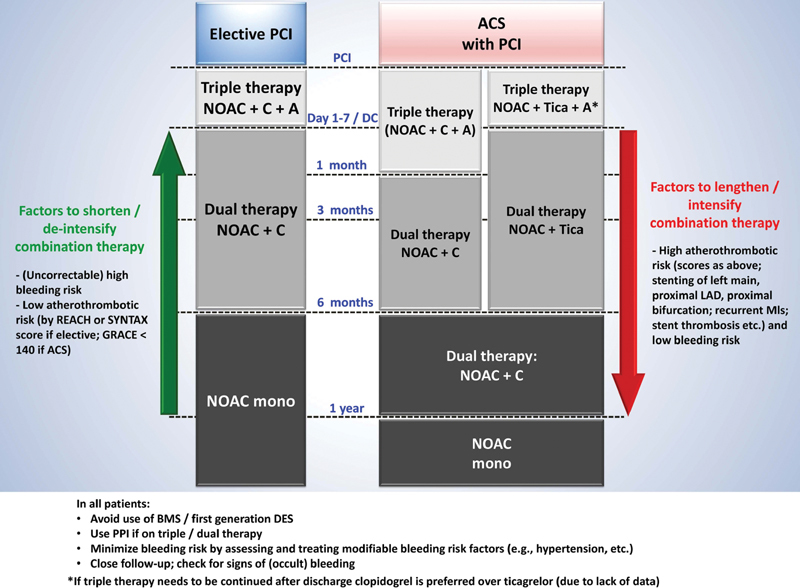
Anticoagulation therapy after elective PCI or ACS in AF patients. A, aspirin 75–100 mg QD; C, clopidogrel 75 mg QD; Tica, ticagrelor 90 mg BID. The figure was redrawn and modified from the 2021 European Heart Rhythm Association Practical Guide on the use of NOACs in patients with AF by Steffel et al. 98 ACS, acute coronary syndrome; AF, atrial fibrillation; BID, twice daily; BMS, bare metal stent; DES, drug-eluting stent; LAD, left anterior descending artery; MI, myocardial infarction; NOAC, non-vitamin K antagonist oral anticoagulant; PCI, percutaneous coronary intervention; PPI, proton pump inhibitor; QD, once daily.
Following the period of triple therapy, patients should be managed with an OAC plus a P2Y12 inhibitor, usually clopidogrel. After 1 year, the patient should be managed with OAC alone. The OAC strategy should be a NOAC (ideally with the potential for less bleeding) or if on warfarin, with good-quality anticoagulation control (TTR ≥ 70%)
Beyond 1 year, the evidence suggests that OAC monotherapy is the preferred option, given similar or worse major adverse cardiac events and more bleeding with combining NOAC and antiplatelets. 99 The AFIRE trial included AF patients who underwent PCI or coronary artery bypass grafting (CABG) more than 1 year earlier or did not require revascularization. 100 The patients were assigned to receive monotherapy with rivaroxaban (10 mg o.d. for patients with an eGFR of 15 to 49 mL/min or 15 mg o.d. for patients with an eGFR ≥50 mL/min) or a combination of rivaroxaban plus a single antiplatelet drug. The incidence of both cardiovascular and noncardiovascular death was lower in the rivaroxaban monotherapy group. For the primary efficacy endpoint (a composite of stroke, SE, myocardial infarction, unstable angina requiring revascularization, or death from any cause), monotherapy was noninferior to dual therapy (HR: 0.72, 95% CI: 0.55–0.95). Additionally, monotherapy decreased major bleeding by 41%. Therefore, monotherapy with rivaroxaban is recommended rather than a combination of rivaroxaban with an antiplatelet drug in AF patients with stable CAD at more than 1 year after a PCI or CABG. Although the AFIRE trial only investigated rivaroxaban at the J-ROCKET AF dosing, it suggests that monotherapy with a NOAC at the stroke prevention dosing without a combination of an antiplatelet drug is favored for AF patients with stable CAD.
Recommendations
In AF patients eligible for NOACs, it is recommended to use a NOAC in preference to a VKA in combination with antiplatelet therapy.
In patients at high bleeding risk (HAS-BLED ≥ 3), rivaroxaban 15 mg o.d. should be considered in preference to rivaroxaban 20 mg o.d. for the duration of concomitant single or DAPT, to mitigate bleeding risk.
In patients at high bleeding risk (HAS-BLED ≥ 3), dabigatran 110 mg b.i.d. (twice daily) should be considered in preference to dabigatran 150 mg b.i.d. for the duration of concomitant single or DAPT, to mitigate bleeding risk.
In AF patients with an indication for a VKA in combination with antiplatelet therapy, the VKA dosing should be carefully regulated with a target INR of 2.0 to 2.5 and TTR >70%.
Patients with ACS
In AF patients with ACS undergoing an uncomplicated PCI, early cessation (≤1 week) of aspirin and continuation of dual therapy with an OAC and a P2Y12 inhibitor (preferably clopidogrel) for up to 12 months is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns about risk of stent thrombosis.
Triple therapy with aspirin, clopidogrel, and an OAC for longer than 1 week after an ACS should be considered when risk of stent thrombosis outweighs the bleeding risk, with the total duration (≤1 month) decided according to assessment of these risks.
Elective PCI
After uncomplicated PCI for stable CAD, early cessation (≤1 week) of aspirin and continuation of dual therapy with OAC for up to 6 months and clopidogrel is recommended if the risk of stent thrombosis is low or if concerns about bleeding risk prevail over concerns about risk of stent thrombosis, irrespective of the type of stent used.
After uncomplicated PCI for stable CAD, triple therapy with aspirin, clopidogrel, and an OAC for longer than 1 week should be considered when risk of stent thrombosis outweighs the bleeding risk, with the total duration (≤1 month) decided according to assessment of these risks.
Stable CAD : In patients with stable CAD, such as more than 1 year after the PCI or CABG, a standard dose of NOAC monotherapy is recommended.
Footnotes
Risk of stent thrombosis encompasses: (1) risk of thrombosis occurring, and (2) risk of death should stent thrombosis occur, both of which relate to anatomical, procedural, and clinical characteristics. Risk factors for stable CAD (chronic coronary syndrome) patients include: stenting of left main stem or last remaining patent artery; suboptimal stent deployment; stent length >60 mm; diabetes mellitus; chronic kidney disease; bifurcation with two stents implanted; treatment of chronic total occlusion; and previous stent thrombosis on adequate antithrombotic therapy.
Management of OACs before, during, and after AF Ablation
Catheter ablation procedures for AF are associated with both prothromboembolic and bleeding risks, and appropriate anticoagulation managements before, during, and after the procedure are quite important. Since the COMPARE randomized study demonstrated lower risks of both thromboembolism and bleeding complications under uninterrupted VKA compared with interrupted VKA with heparin bridging, 101 it is generally accepted that the procedure should be performed without interrupting VKA, when anticoagulation control is appropriate. 102
NOACs are currently used in many patients even in those undergoing AF ablation. The Japanese Catheter Ablation Registry of AF (J-CARAF) during 2011 to 2016 showed that of the 9,048 patients with periprocedural oral anticoagulation, 3,231 (35.7%) were treated with VKA, whereas the other 5,817 (64.3%) were managed with NOACs. 103 A meta-analysis of nonrandomized studies showed that interrupted dabigatran for a minimum period (12–24 hours) before the procedure was associated with similar thromboembolism and bleeding complication rates to uninterrupted VKA. 104
Several randomized, prospective clinical trials on uninterrupted NOACs versus uninterrupted VKA have been conducted ( Table 2 ). These trials include VENTURE-AF study for rivaroxaban versus VKA 105 ; RE-CIRCUIT study for dabigatran versus VKA 106 ; AXAFA-AFNET 5 study for apixaban versus VKA 107 ; and ELIMINATE-AF study for edoxaban versus VKA. 108 In these studies, therapeutic doses of NOACs and VKA with target prothrombin time-INR between 2.0 and 3.0 were generally administered for >3 weeks before ablation, with exception of short-period administration in some cases in which transesophageal or intracardiac echocardiography confirmed the absence of intra-atrial thrombus. After the ablation procedure, the drugs were continued for >30 days. During the procedure, heparin was given to maintain activated clotting time >300 seconds in all studies. The RE-CIRCUIT, 106 AXAFA-AFNET 5, 107 and ELIMINATE-AF 108 studies included patients enrolled from the Asian countries. The incidences of major complications in uninterrupted NOACs versus uninterrupted VKA groups in each study are shown in Table 2 .
Table 2. Outlines and major outcomes of four randomized trials on NOACs versus VKA for AF ablations 105 106 107 108 .
| VENTURE-AF | RE-CIRCUIT | AXAFA-AFNET | ELIMINATE-AF | |||||
|---|---|---|---|---|---|---|---|---|
| NOAC | Rivaroxaban 20 mg QD (evening) |
Dabigatran 150 mg BID |
Apixaban 5 mg BID a |
Edoxaban 60 mg QD a (evening) |
||||
| Comparator | VKA (INR, 2.0–3.0) |
VKA (INR, 2.0–3.0) |
VKA (INR, 2.0–3.0) |
VKA (INR, 2.0–3.0) |
||||
| Study design | Open-label, randomized | Open-label, randomized | Open-label, randomized | Open-label, randomized | ||||
| No. of patients (NOAC vs. VKA) | 124 vs. 124 | 317 vs. 318 | 318 vs. 315 | 375 vs. 178 | ||||
| Enrollment from Asian countries | No | Yes | Yes | Yes | ||||
| Duration of administration before ablation | >3 wk | 4–8 wk | >30 days | 3–4 wk | ||||
| Follow-up period after ablation | >30 days | 8 weeks | >30 days | 90 days | ||||
| Patient characteristics | ||||||||
| Mean or median age (y) | 59.6 ± 10.2 | 59.1 ± 10.4 | 64 (58, 70) | 60.5 (53–67) | ||||
| Percentage of male patients | 71.0% | 74.8% | 67.0% | 71.5% | ||||
| Percentage of paroxysmal AF | 73.4% | 67.6% | 58.0% | 67.6% | ||||
| Mean CHA 2 DS 2 -VASc score | 1.6 | 2.1 | 2.4 | 0/1 in 49.8% | ||||
| Primary endpoints | ISTH/GUSTO/TIMI major bleeding | ISTH major bleeding | All-cause death, stroke, or major bleeding | All-cause death, stroke (ischemic, hemorrhagic, or undetermined), or ISTH major bleeding | ||||
| Major complication rates | Rivaroxaban | VKA | Dabigatran | VKA | Apixaban | VKA | Edoxaban | VKA |
| ISTH major bleeding | 0% | 0.8% | 1.6% | 6.9% | 3.1% | 4.4% | 2.4% | 1.7% |
| Ischemic stroke | 0% | 0.8% | 0% | 0.3% | 0.6% | 0% | 0.3% | 0% |
| Death | 0% | 0.8% | 0% | 0% | 0.3% | 0.3% | 0% | 0% |
| Composite | 0% | 2.4% | 1.6% | 7.2% | 4.0% | 4.7% | 2.7% | 1.7% |
Abbreviations: AF, atrial fibrillation; BID, twice daily; INR, international normalized ratio; NOACs, non-vitamin K antagonist oral anticoagulants; QD, once daily; VKA, vitamin K antagonist.
Dose reduced when dose reduction criteria were met.
In a meta-analysis of these four trials comparing NOACs versus VKA, 108 the rate of death was 0.1 versus 0.2%; ischemic stroke, 0.2 versus 0.2%; major bleeding, 2.1 versus 4.2%; and the composite outcome, 2.4 versus 4.6%, respectively. Another meta-analysis of six randomized studies 109 on uninterrupted NOACs (dabigatran, rivaroxaban, and apixaban) versus uninterrupted VKA revealed that the incidence of major bleeding was significantly lower in the NOAC group (1.68%) than in the VKA group (3.80%) (OR = 0.45, 95% CI: 0.26–0.81, p = 0.007); while the incidence of ischemic stroke or transient ischemic attack (TIA) was low and similar between the NOAC (0.21%) and VKA groups (0.21%). Further, the incidence of silent cerebral thromboembolic events (in three studies) was similar between NOAC (14.0%) and VKA groups (13.3%). Similar results were reported by another meta-analysis. 110
Interrupted NOAC protocols versus uninterrupted regimes have been tested by prospective, randomized studies done in Asian countries. 111 112 113 114 Notwithstanding the small-size study cohorts which may be underpowered for the thromboembolic outcomes, an ablation strategy with minimally interrupted periprocedural NOACs may be an option.
Recommendations
We recommend a preferential use of NOACs over VKA because of their safety profile relative to VKA in addition to their ease of management before and after ablation.
-
NOAC dosing protocols, uninterrupted or minimally interrupted, should be determined in each institution, depending on the volume of AF ablation done, experience of the operator, back-up system in case of life-threatening complications, baseline renal function and thromboembolism and bleeding risks of each patient, time of administration of once-daily NOACs (morning or evening), preparation of specific antidotes to NOACs, etc. ( Fig. 13 ).
- For most patients, an uninterrupted NOAC strategy may be the preferred option.
When VKA is used, it should be controlled within a therapeutic range and uninterrupted throughout the periprocedural period unless bleeding events preclude its continuous use.
In general, OAC therapy is continued for 2 months following ablation in all patients. Beyond this time, a decision to continue OAC long term is determined primarily by the presence of CHA 2 DS 2 -VASc stroke risk factors rather than the rhythm status.
Fig. 13.

A flow chart about the general recommendation for NOACs in the periprocedural period of catheter ablation. NOACs, non-vitamin K antagonist oral anticoagulants; TEE, transesophageal echocardiography.
Reversal Agents
The general principles of managements of bleeding are summarized in Fig. 14 . For severe bleeding or life-threatening bleeding, reversal agents could be considered to reverse the anticoagulant effects of NOACs.
Fig. 14.

General principles of managements of bleeding for anticoagulated AF patients. AF, atrial fibrillation; FFP, fresh frozen plasma; NOACs, non-vitamin K antagonist oral anticoagulants; OACs, oral anticoagulants.
Idarucizumab is a monoclonal antibody fragment and binds dabigatran with an affinity that is 350 times as high as that observed with thrombin. 115 In the RE-VERSE AD study, the efficacy and safety of idarucizumab was tested in patients who had serious bleeding or required urgent procedures. In an interim analysis of the first 90 patients, idarucizumab reversed the anticoagulant effect of dabigatran within minutes in 88 to 98% of patients. 116 In the whole cohort of 503 patients, the median time to cessation of bleeding was 2.5 hours in those with uncontrolled bleeding who could be assessed. 117 For the periprocedural group, the median time to the initiation of the intended procedure was 1.6 hours. Periprocedural hemostasis was assessed as normal in 93.4% of the patients, mildly abnormal in 5.1%, and moderately abnormal in 1.5%. At 90 days, thrombotic events had occurred in 6.3% of the patients in the uncontrolled bleeding group and in 7.4% in the periprocedural group, while the mortality rate was 18.8 and 18.9%, respectively. No serious adverse safety signals were noted. More recently, it was found that although both dabigatran and idarucizumab were renally cleared, impaired renal function did not affect the reversal of anticoagulation. 118 The REVERSE-AD study results were consistent and supported by observations from a post-approval global registry (RE-VECTO), which also showed that off-label use was minimal. 119 Idarucizumab is approved in many countries for patients treated with dabigatran when reversal of the anticoagulant effects of dabigatran is needed for emergency surgery/urgent procedures and in life-threatening or uncontrolled bleeding.
Andexanet alfa is a recombinant modified human factor Xa decoy protein that is catalytically inactive but which retains the ability to bind factor Xa inhibitors in the active site with high affinity. 120 In a clinical study of older healthy volunteers, andexanet reversed the anticoagulant activity of apixaban and rivaroxaban within minutes after administration and for the duration of infusion, without clinical evidence of toxic effects. 121 In the multicenter, open label, single-arm ANNEXA-4 trial, 352 patients with acute major bleeding associated with factor Xa inhibitors (mostly on rivaroxaban and apixaban) were given an initial bolus and subsequent 2-hour infusion of andexanet alfa. This substantially reduced anti-factor Xa activity after the bolus (75–92%) and this effect persisted till the end of the infusion. Good or excellent hemostatic efficacy was achieved in 82%, 12 hours after the infusion. 122 During 30 days of follow-up, 49 patients (14%) died and 34 (10%) experienced a thrombotic event. Similar data are based on an earlier interim analysis of this study, 121 and andexanet alfa was granted accelerated approval by the Food and Drug Administration for the reversal of anticoagulation if needed due to life-threatening or uncontrolled bleeding in patients treated with apixaban or rivaroxaban.
When managing OAC-related bleeding, it is important to survey for occult malignancies that are the cause/origin of the bleeding, e.g., GI tract cancer in patients with GI bleeding. 84 In a nationwide study from Taiwan, incident GI cancers were diagnosed in 1 of 37 AF patients at 1 year after OAC-related GI bleeding, and were more common among patients treated with NOACs (1/26) compared with warfarin (1/41). 123 Interestingly, the risk of mortality after GI tract cancers were diagnosed was lower in patients treated with NOACs than in those treated with warfarin (23.5 vs. 51.8%; aHR: 0.441; p < .001), and more patients treated with NOACs (33.8%) underwent surgery than those treated with warfarin (18.9%), suggesting that NOACs may serve as a stronger “screening test” than warfarin and may be able to disclose GI cancers at an earlier stage when operation is possible, therefore leading to a better prognosis. 123 Similar findings have been reported for anticoagulated patients presenting with hematuria among whom the possibility of underlying bladder cancers should be kept in mind. 124
Recommendations
Idarucizumab is indicated for the reversal of dabigatran in patients with serious bleeding or requiring urgent procedures.
Andexanet alfa can be useful for reversing anticoagulation in patients treated with factor Xa inhibitors with life-threatening or uncontrolled bleeding.
The possibility of occult malignancies that are the cause/origin of the bleeding should be kept in mind when managing OAC-related bleeding.
Stroke Prevention in Special Patient Groups
Issues about stroke prevention in special patient groups are discussed in the Supplementary Material (available in the online version).
Left Atrial Appendage Occlusion
The efficacy, safety, and procedural aspects, as well as the limitations of current data on left atrial appendage (LAA) occlusion have recently been the subject of a detailed expert consensus statement: EHRA/EAPCI (European Association of Percutaneous Cardiovascular Interventions) on catheter-based LAA occlusion. 125 More recently, the role of surgical occlusion of the LAA in AF patients undergoing cardiac surgery has gained prominence with publication of the LAAOS III trial. 126 The latter showed that stroke/SE occurred in 4.8% in the LAA occlusion group and in 7.0% in the no-occlusion group (HR: 0.67; 95% CI: 0.53–0.85; p = 0.001). The incidence of perioperative bleeding, heart failure, or death did not differ significantly between the trial groups. Thus, among participants with AF who had undergone cardiac surgery, the risk of ischemic stroke or SE was lower with concomitant LAA occlusion performed during the surgery than without it.
Catheter-Based LAA Occlusion
Efficacy
There are two randomized controlled trials (RCTs) comparing percutaneous LAA occlusion with the Watchman device to warfarin in patients with NVAF and high risk of stroke. 127 128 Data from these and their associated registries 129 130 demonstrate noninferiority to warfarin for prevention of ischemic stroke or SE >7 days postprocedure. There were more ischemic strokes in the device group (1.6 vs. 0.9 events/100 patient-years, p = 0.05), largely driven by procedure-related strokes, and a significant reduction in hemorrhagic stroke (0.15 vs. 0.96/100 patient-years, p = 0.004). 130 To date, there are limited data comparing LAA occlusion devices with NOACs. Noninferiority to NOACs has been examined in the PRAGUE-17 trial, ClinicalTrials.gov identifier NCT02426944, 131 which showed that in AF patients at high risk for stroke (CHA 2 DS 2 -VASc: 4.7 ± 1.5) and increased risk of bleeding, LAAO was noninferior to NOACs in preventing major AF-related cardiovascular, neurological, and bleeding events. There were no differences between groups for the components of the composite endpoint: all-stroke/TIA (subdistribution HR [sHR]: 1.00; 95% CI: 0.40–2.51), clinically significant bleeding (sHR: 0.81; 95% CI: 0.44–1.52), and cardiovascular death (sHR: 0.75; 95% CI: 0.34–1.62). Major LAAC-related complications occurred in 9 (4.5%) patients. 132
Safety
Safety data are available from the RCTs 127 128 and several registries, 129 133 134 135 including two conducted in the Asia-Pacific region. 136 137 In modern practice, there is high implantation success of 95 to 98.5%. 128 133 137
Procedure- and device-related complications in the first 7 days were high in the earlier PROTECT AF trial 127 at 8.7% but lower at 4.2% in the subsequent PREVAIL trial. 128 Similar reduction in complication rate has been seen over time in registries, with early data showing a high complication rate of 8.6%, 138 reducing to 2.2 to 3% for more contemporaneous registries. 128 133 137 However, trials and registries have selection bias and real-world data suggest that the complication rate may be significantly higher. 139
The rates of early device thrombosis in meta-analysis and registry data are 3.7 to 3.9%, 135 140 and there are no RCTs to guide the duration of anticoagulation and number, and type and duration of antiplatelet agents, although registry data suggest safety of a single antiplatelet agent. Other “real-world” reports of device-related thrombus (DRT) suggest incidence rates as high as 7.2% per year, 141 as well as high annual rates of mortality (7.4%), ischemic strokes (4.3%), and major hemorrhages (4.5%). 142 The EUROC-DRT registry reported that substantial proportion of DRT (18%) was detected >6 months after LAA closure, highlighting the need for imaging follow-up, especially since such patients were at high risk for stroke and mortality (13.8 and 20.0%, respectively). 143
Although there are registry data on safety of LAA occlusion in patients with a contraindication to anticoagulation, 135 there are no published RCT data on efficacy and safety of LAA occlusion devices in this cohort, although ongoing studies may address this. 125 144
Issues Specific to the Asia-Pacific Region
Asians are significantly underrepresented in clinical trials and registries of LAA occlusion devices with <1% of patients in the PROTECT-AF and PREVAIL trials and associated registries being of Asian ethnicity. 130 However, evidence for safety and efficacy in Asian patients come from two small registries from the Asia-Pacific region—the WASP registry 137 performed in South-East Asia and Australia with 106/203 patients being of Asian ethnicity and the SALUTE registry of 54 patients in Japan. 136 The WASP registry suggested important differences in anatomy and need for larger device sizes in Asian patients. 136
The lack of comparative data to NOACs may be especially pertinent in the Asia-Pacific region given the more profound benefits of NOACs in Asian populations, especially with respect to reduced incidence of intracranial hemorrhage. 65
Finally, cost-effectiveness analysis has been performed utilizing health care costs from the United States, 145 146 which may not be applicable in the Asia-Pacific region, especially when one considers the diverse health care systems, costs, and funding models across the region.
Recommendations
LAA occlusion may be considered for stroke prevention in patients with AF and clear contraindications for long-term anticoagulant treatment (e.g., intracranial bleeding without a reversible cause).
Surgical occlusion or exclusion of the LAA is recommended for stroke prevention in patients with AF undergoing cardiac surgery.
Role of Environmental and Lifestyle Factors in AF
Cardiovascular risk factors, including lifestyle factors and comorbidities, affect the risk and prognosis of AF. Management of these risk factors, unhealthy lifestyle behaviors and practices, and comorbidities is important for stroke prevention and to control the burden of AF and symptoms associated with AF. This strategy constitutes the “C” component of the ABC pathway. 11 Lifestyle modifications, including weight loss, physical activity, alcohol abstinence, and risk factor modifications including BP control, have been shown to reduce AF burden. 147 148 149 150 151 152 153 154
Unhealthy lifestyle factors tend to cluster together, and increased numbers of unhealthy lifestyle factors (current smoking, heavy drinking [>30 g/day], and lack of regular exercise) have been associated with a higher risk of incident AF. 155 156 Overall, the promotion of a healthy lifestyle to lower the risk of new-onset AF and AF-related complications is recommended.
Body Weight: Role of Obesity and Low Body Weight
Obesity is an important and potentially modifiable risk factor for AF and can affect the incidence and persistence of AF. 157 158 Obesity is also associated with other cardiovascular disease risks, including hypertension, sleep apnea, impaired glucose tolerance, and diabetes, which are all associated with incident AF and AF-related complications.
Aggressive weight reduction and risk factor modification have been shown to reduce AF recurrences and arrhythmia burden, as well as AF symptom burden; thus, there is improved maintenance of sinus rhythm and beneficial effects on cardiac remodeling compared with conventional therapy in patients with obesity. 148 149 159 160 For example, in patients diagnosed with overweight or obesity concomitant with AF, >10% weight reduction was associated with reduction in the AF burden and reversal of AF type and natural progression. 149 161 Underweight patients are not uncommon in the Asian population, and these patients show an increased risk of AF. 162 Moreover, fluctuations in body weight were associated with an increased risk of AF, particularly amongst those with low body weight. 163
With regard to clinical outcomes, the risk of the composite outcome of ischemic stroke, thromboembolism, or death is higher in those with overweight and obesity, even after adjustment for CHA 2 DS 2 -VASc scores. 164 However, in a systematic review and meta-analysis, an obesity paradox was observed in patients with AF taking anticoagulation therapy, particularly with regard to all-cause and cardiovascular death in subgroup analyses of randomized trial cohorts. 165 Another study showed that the risk of ischemic stroke, major bleeding, and mortality was lower in Asian patients with AF, who showed a high body mass index and received OACs compared with those with normal weight, whereas underweight patients had an increased risk of mortality and composite outcome compared with those with normal weight. 166 For stroke prevention, NOACs are generally associated with better outcomes than those with warfarin administration in Asians across patients of different body weights, particularly in underweight patients. 76 Given the observed obesity paradox in AF patients, keeping a normal body weight is recommended.
Alcohol
Excessive alcohol consumption is a well-known risk factor and trigger for AF. 167 Excessive alcohol consumption acts synergistically with other lifestyle risk factors for AF, including hypertension, obesity, obstructive sleep apnea, and cardiomyopathy to magnify their effects. Excessive alcohol consumption is a known clinical risk factor for bleeding during anticoagulation therapy, and is included in the HAS-BLED score. 168 High alcohol consumption is also associated with an increased risk of thromboembolism and death in patients with incident AF. 169 Asian data have shown that high alcohol consumption was associated with a high ischemic stroke risk. 170
One recent randomized trial has reported that alcohol abstinence reduced the risk of recurrent AF in those with heavy alcohol consumption patterns. 171 Alcohol abstinence was also associated with a low risk of incident AF in patients with newly diagnosed type 2 diabetes, 172 and alcohol abstinence after a diagnosis of AF was associated with a low risk of ischemic stroke. 170
Smoking
Smoking is associated with an increased risk of incident AF, 173 174 and smoking cessation seems to lower the risk of AF compared with current smokers. 173 174 In Asian AF patients with a low CHA 2 DS 2 -VASc score, smoking was identified as a risk factor for ischemic stroke. 175 Furthermore, quitting smoke after incident AF was associated with a low risk of ischemic stroke, lower stroke severity, and death from cerebrovascular events. 176
Air pollution
Epidemiological studies have suggested that elevated ambient particulate matter (PM) <2.5μμm (PM 2.5 ) or <10μμm (PM 10 ) in aerodynamic diameter is consistently associated with adverse cardiac events. In the Asian general population, long-term exposure of PM2.5 is associated with the increased incidence of new-onset AF. 177 178
Physical Activity
Moderate-intensity exercise (150 min/week) or vigorous-intensity exercise (75 min/week) recommended by the 2018 Physical Activity Guidelines Advisory Committee is known to improve cardiovascular health. Physical inactivity is associated with an increased risk of incident AF, 179 and regular exercise could reduce AF burden and improve AF-related symptoms and patients' quality of life. 180 181 182 183 However, the risk of AF increased in those who participate in extreme endurance exercise that far exceeds the levels recommended by the Physical Activity Guidelines Advisory Committee report. 184 Cardiorespiratory fitness generally reduces the AF burden and symptom severity in patients with obesity and concomitant AF, which may be attributable to the beneficial effects of weight loss. 147
One recent observational study in Asian patient with incident AF reported that regular exercise was associated with low risks of heart failure, mortality, and dementia in addition to a marginal benefit on ischemic stroke. 185 186 Regular moderate exercise (170–240 min/week) showed maximal cardiovascular benefits in patients who initiated exercise after diagnosis of AF. Patients who initiated or continued regular exercise after diagnosis of AF were associated with a lower risk of dementia than persistent non-exercisers, with no risk reduction associated with exercise cessation. 186
Recommendations
The promotion of a healthy lifestyle (smoking cessation, reduced alcohol consumption, regular exercise) is recommended to lower the risk of new-onset AF and AF-related complications.
Appropriate weight control is an important strategy to improve outcomes in patients with AF.
Reduced consumption or alcohol abstinence is recommended in AF patients with moderate-to-high levels of alcohol use to minimize AF burden and stroke risk.
Smoking cessation is recommended in patients with AF to reduce the stroke risk, even in those categorized as low-risk patients based on the CHA 2 DS 2 -VASc score.
Regular exercise based on the recommendations of the 2018 Physical Activity Guidelines Advisory Committee (150 min/week of moderate-intensity exercise or 75 min/week of vigorous-intensity exercise) can improve cardiovascular outcomes in patients with AF ( Fig. 15 ).
Fig. 15.

The integration of lifestyle management in patients with AF. AF, atrial fibrillation.
OAC Use in AF Patients during the COVID-19 Pandemic
AF is a common clinical manifestation in hospitalized patients with coronavirus disease 2019 (COVID-19) infection and is associated with a higher risk of mortality and/or requirement for intensive care. 187 188 189 190 The latter is perhaps unsurprising given the higher risk of adverse outcomes in COVID-19 with associated cardiovascular comorbidities. 190
During the COVID-19 pandemic, TTR values associated with VKA (e.g., warfarin) treatment may be suboptimal with the lack of INR monitoring, and in appropriate patients, a switch to NOACs may be appropriate. 191 Furthermore, the anticoagulated AF patients may not seek medical help even in the case of bleeding. 192 Thus, for the outpatients during the COVID-19 pandemic (during the lockdown phase or discharge after recovery from COVID-19 infection), NOAC therapy in replacement of VKA (except for the absolute contraindications of NOACs like prosthetic mechanical valve or moderate-to-severe mitral stenosis) is recommended to minimize the necessity for frequent clinic/office visits for INR monitoring and contact with health care workers. 193 Remote anticoagulation management/monitoring for elderly patients with NVAF receiving NOACs during the COVID-19 pandemic was associated with a reduction in bleeding complications and delays in the first outpatient revisit after discharge. 194
COVID-19 is associated with a prothrombotic state, perhaps due to cytokines and immunothrombosis. 195 For patients already treated with NOACs or VKA and infected with COVID-19 and particularly in the case of severe infection requiring hospitalization, patients should ideally continue their anticoagulation rather than discontinue, although outcome data are conflicting. 196 197 198 199
Conversion from NOAC or VKA into low-molecular-weight heparin (LMWH) during the hospitalization course (especially if severely affected, requiring intensive care unit admission) may be preferable due to less drug interaction with antiviral drugs (e.g., remdesivir) or immunomodulating drugs (e.g., dexamethasone, baricitinib, or tocilizumab), and a higher risk of clinical deterioration due to severe COVID-19 infection (particularly of coagulation and renal function). 193 195 It would therefore be reasonable to shift NOACs into alternative LMWH for patients with severe COVID-19 infection as long as antiviral agents are deemed necessary and until discharge. LMWH regimes have been tested in recent clinical trials of hospitalized COVID-19 patients but showed conflicting results. 200 201 202 203 204 For example, in noncritically ill patients with COVID-19, the ATTACC, ACTIV-4a, and REMAP-CAP investigators found that an initial strategy of therapeutic-dose anticoagulation with heparin increased the probability of survival to hospital discharge with reduced use of cardiovascular or respiratory organ support as compared with usual-care thromboprophylaxis. 201 However, in patients hospitalized with COVID-19 and elevated D-dimer concentration, in-hospital therapeutic anticoagulation with rivaroxaban or enoxaparin followed by rivaroxaban to day 30 did not improve clinical outcomes and increased bleeding compared with prophylactic anticoagulation in the ACTION trial. 204 Besides, these studies did not specifically enroll AF patients, and therefore, data about the optimal dosage of LMWH for hospitalized AF COVID-19 patients were very limited.
COVID-19 vaccines are usually administered by intramuscular injection, and are an important part of our pandemic response. 205 An opportunity to screen for AF amongst attendees for vaccination has been promoted. 206 In AF patients treated with NOACs, it is advisable to follow the scheme for “minor risk” interventions, and therefore, it is not necessary to withhold any NOAC dosage before and after the injection procedure. 207 However, it is recommended to use a fine-gauge needle for injection, and apply firm pressure for 5 to 10 minutes after the injection. If the scheduled NOAC dosage is close to the injection time before, the scheduled NOAC dosage may be postponed until after the injection if no progression of local hematoma noted.
Recommendations
For outpatients with AF during the COVID-19 pandemic, NOAC therapy as a replacement of VKA (unless contraindicated) may be considered.
For AF patients already treated with NOACs or VKA and infected with COVID-19 and particularly in case of severe infection requiring hospitalization or critical care, conversion from NOAC or VKA into LMWH during the hospitalization course of COVID-19 infection may be considered.
In AF patients taking NOACs and planned to receive COVID-19 vaccine injection, it is advisable to follow the scheme for “minor risk” interventions, and therefore, it is not necessary to withhold any NOAC dosage before and after the injection procedure.
Conflict of Interest B.J.: Served as a speaker for Bayer, BMS/Pfizer, Medtronic, and Daiichi-Sankyo and received research funds from Samjin, Medtronic, and Abbott. No fees have been received directly or personally. Y.T.: Research grants from Medtronic Japan, Boston Scientific, Japan Lifeline, WIN International, Abbott and Biosense-Webster, and speaker honoraria from Abbott and Biosense-Webster. G.Y. H. L.: Consultant and speaker for BMS/Pfizer, Boehringer Ingelheim, and Daiichi-Sankyo. No fees are received personally. The other authors report no conflict of interest.
This is an executive summary of the full consensus guideline, which is published in Journal of Arrhythmia by Chao et al. 6
Note: The review process for this paper was fully handled by Christian Weber, Editor-in-Chief .
Supplementary Material
References
- 1.Zhang J, Johnsen S P, Guo Y, Lip G YH. Epidemiology of atrial fibrillation: geographic/ecological risk factors, age, sex, genetics. Card Electrophysiol Clin. 2021;13(01):1–23. doi: 10.1016/j.ccep.2020.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Chao T F, Liu C J, Tuan T C. Lifetime risks, projected numbers, and adverse outcomes in Asian patients with atrial fibrillation: a report from the Taiwan nationwide AF cohort study. Chest. 2018;153(02):453–466. doi: 10.1016/j.chest.2017.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Kim D, Yang P S, Jang E. 10-year nationwide trends of the incidence, prevalence, and adverse outcomes of non-valvular atrial fibrillation nationwide health insurance data covering the entire Korean population. Am Heart J. 2018;202:20–26. doi: 10.1016/j.ahj.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Bai Y, Wang Y L, Shantsila A, Lip G YH. The global burden of atrial fibrillation and stroke: a systematic review of the clinical epidemiology of atrial fibrillation in Asia. Chest. 2017;152(04):810–820. doi: 10.1016/j.chest.2017.03.048. [DOI] [PubMed] [Google Scholar]
- 5.Chao T F, Chiang C E, Lin Y J. Evolving changes of the use of oral anticoagulants and outcomes in patients with newly diagnosed atrial fibrillation in Taiwan. Circulation. 2018;138(14):1485–1487. doi: 10.1161/CIRCULATIONAHA.118.036046. [DOI] [PubMed] [Google Scholar]
- 6.Chao T F, Joung B, Takahashi Y. 2021 Focused update of the 2017 consensus guidelines of the Asia Pacific Heart Rhythm Society (APHRS) on stroke prevention in atrial fibrillation. J Arrhythm. 2021 doi: 10.1016/j.ijid.2021.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lip G YH. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. 2017;14(11):627–628. doi: 10.1038/nrcardio.2017.153. [DOI] [PubMed] [Google Scholar]
- 8.Romiti G F, Pastori D, Rivera-Caravaca J M. Adherence to the ‘Atrial Fibrillation Better Care’ pathway in patients with atrial fibrillation: impact on clinical outcomes-a systematic review and meta-analysis of 285,000 patients. Thromb Haemost. 2021 doi: 10.1055/a-1515-9630. [DOI] [PubMed] [Google Scholar]
- 9.Lip G YH, Banerjee A, Boriani G. Antithrombotic therapy for atrial fibrillation: CHEST guideline and expert panel report. Chest. 2018;154(05):1121–1201. doi: 10.1016/j.chest.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 10.KHRS Atrial Fibrillation Guideline Working Group . Joung B, Lee J M, Lee K H. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018;48(12):1033–1080. doi: 10.4070/kcj.2018.0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ESC Scientific Document Group . Hindricks G, Potpara T, Dagres N. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(05):373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 12.Chiang C E, Okumura K, Zhang S. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017;33(04):345–367. doi: 10.1016/j.joa.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chao T F, Liu C J, Wang K L. Using the CHA2DS2-VASc score for refining stroke risk stratification in ‘low-risk’ Asian patients with atrial fibrillation. J Am Coll Cardiol. 2014;64(16):1658–1665. doi: 10.1016/j.jacc.2014.06.1203. [DOI] [PubMed] [Google Scholar]
- 14.Xiong Q, Chen S, Senoo K, Proietti M, Hong K, Lip G Y. The CHADS2 and CHA2DS2-VASc scores for predicting ischemic stroke among East Asian patients with atrial fibrillation: a systemic review and meta-analysis. Int J Cardiol. 2015;195:237–242. doi: 10.1016/j.ijcard.2015.05.115. [DOI] [PubMed] [Google Scholar]
- 15.Chao T F, Liu C J, Tuan T C. Comparisons of CHADS2 and CHA2DS2-VASc scores for stroke risk stratification in atrial fibrillation: which scoring system should be used for Asians? Heart Rhythm. 2016;13(01):46–53. doi: 10.1016/j.hrthm.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Kang S H, Choi E K, Han K D. Risk of ischemic stroke in patients with non-valvular atrial fibrillation not receiving oral anticoagulants - Korean nationwide population-based study. Circ J. 2017;81(08):1158–1164. doi: 10.1253/circj.CJ-16-1267. [DOI] [PubMed] [Google Scholar]
- 17.Kim T H, Yang P S, Uhm J S. CHA 2 DS 2 -VASc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65-74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study . Stroke. 2017;48(06):1524–1530. doi: 10.1161/STROKEAHA.117.016926. [DOI] [PubMed] [Google Scholar]
- 18.Kim T H, Yang P S, Kim D. CHA 2 DS 2 -VASc score for identifying truly low-risk atrial fibrillation for stroke: a Korean nationwide cohort study . Stroke. 2017;48(11):2984–2990. doi: 10.1161/STROKEAHA.117.018551. [DOI] [PubMed] [Google Scholar]
- 19.Noubiap J J, Feteh V F, Middeldorp M E. A meta-analysis of clinical risk factors for stroke in anticoagulant-naïve patients with atrial fibrillation. Europace. 2021;23(10):1528–1538. doi: 10.1093/europace/euab087. [DOI] [PubMed] [Google Scholar]
- 20.Chao T F, Lip G YH, Lin Y J. Age threshold for the use of non-vitamin K antagonist oral anticoagulants for stroke prevention in patients with atrial fibrillation: insights into the optimal assessment of age and incident comorbidities. Eur Heart J. 2019;40(19):1504–1514. doi: 10.1093/eurheartj/ehy837. [DOI] [PubMed] [Google Scholar]
- 21.Kim T H, Yang P S, Yu H T. Age threshold for ischemic stroke risk in atrial fibrillation. Stroke. 2018;49(08):1872–1879. doi: 10.1161/STROKEAHA.118.021047. [DOI] [PubMed] [Google Scholar]
- 22.Nielsen P B, Larsen T B, Skjøth F, Overvad T F, Lip G Y. Stroke and thromboembolic event rates in atrial fibrillation according to different guideline treatment thresholds: a nationwide cohort study. Sci Rep. 2016;6:27410. doi: 10.1038/srep27410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang T Y, Lip G YH, Chen S A, Chao T F. Importance of risk reassessment in patients with atrial fibrillation in guidelines: assessing risk as a dynamic process. Can J Cardiol. 2019;35(05):611–618. doi: 10.1016/j.cjca.2019.01.018. [DOI] [PubMed] [Google Scholar]
- 24.Chao T F, Lip G YH, Liu C J. Relationship of aging and incident comorbidities to stroke risk in patients with atrial fibrillation. J Am Coll Cardiol. 2018;71(02):122–132. doi: 10.1016/j.jacc.2017.10.085. [DOI] [PubMed] [Google Scholar]
- 25.Chao T F, Chiang C E, Chen T J, Lip G YH, Chen S A. Reassessment of risk for stroke during follow-up of patients with atrial fibrillation. Ann Intern Med. 2019;170(09):663–664. doi: 10.7326/M18-1177. [DOI] [PubMed] [Google Scholar]
- 26.Yoon M, Yang P S, Jang E. Dynamic changes of CHA2DS2-VASc score and the risk of ischaemic stroke in asian patients with atrial fibrillation: a nationwide cohort study. Thromb Haemost. 2018;118(07):1296–1304. doi: 10.1055/s-0038-1651482. [DOI] [PubMed] [Google Scholar]
- 27.Fauchier L, Bodin A, Bisson A. Incident comorbidities, aging and the risk of stroke in 608,108 patients with atrial fibrillation: a nationwide analysis. J Clin Med. 2020;9(04):9. doi: 10.3390/jcm9041234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chao T F, Liao J N, Tuan T C. Incident co-morbidities in patients with atrial fibrillation initially with a CHA2DS2-VASc score of 0 (males) or 1 (females): implications for reassessment of stroke risk in initially ‘low-risk’ patients. Thromb Haemost. 2019;119(07):1162–1170. doi: 10.1055/s-0039-1683933. [DOI] [PubMed] [Google Scholar]
- 29.Borre E D, Goode A, Raitz G. Predicting thromboembolic and bleeding event risk in patients with non-valvular atrial fibrillation: a systematic review. Thromb Haemost. 2018;118(12):2171–2187. doi: 10.1055/s-0038-1675400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Proietti M, Romiti G F, Vitolo M, Potpara T S, Boriani G, Lip G YH. Comparison of HAS-BLED and ORBIT bleeding risk scores in AF patients treated with NOACs: a report from the ESC-EHRA EORP-AF general long-term registry. Eur Heart J Qual Care Clin Outcomes. 2021 doi: 10.1093/ehjqcco/qcab069. [DOI] [PubMed] [Google Scholar]
- 31.Guo Y, Zhu H, Chen Y, Lip G YH. Comparing bleeding risk assessment focused on modifiable risk factors only versus validated bleeding risk scores in atrial fibrillation. Am J Med. 2018;131(02):185–192. doi: 10.1016/j.amjmed.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 32.Chao T F, Lip G YH, Lin Y J. Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta HAS-BLED scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost. 2018;118(04):768–777. doi: 10.1055/s-0038-1636534. [DOI] [PubMed] [Google Scholar]
- 33.mAF-App II Trial Investigators . Guo Y, Lane D A, Wang L. Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol. 2020;75(13):1523–1534. doi: 10.1016/j.jacc.2020.01.052. [DOI] [PubMed] [Google Scholar]
- 34.mAF-App II Trial investigators . Guo Y, Lane D A, Chen Y, Lip G YH. Regular bleeding risk assessment associated with reduction in bleeding outcomes: the mAFA-II randomized trial. Am J Med. 2020;133(10):119500–120200. doi: 10.1016/j.amjmed.2020.03.019. [DOI] [PubMed] [Google Scholar]
- 35.Chao T F, Chan Y H, Chiang C E. Continuation or discontinuation of oral anticoagulants after HAS-BLED scores increase in patients with atrial fibrillation. Clin Res Cardiol. 2021 doi: 10.1007/s00392-021-01816-z. [DOI] [PubMed] [Google Scholar]
- 36.Chao T F, Chan Y H, Tuan T C. Should oral anticoagulants still be prescribed to patients with atrial fibrillation with a single stroke risk factor but at high bleeding risk? a nationwide cohort study. Eur Heart J Qual Care Clin Outcomes. 2021 doi: 10.1093/ehjqcco/qcab050. [DOI] [PubMed] [Google Scholar]
- 37.Lip G YH, Collet J P, de Caterina R. Antithrombotic therapy in atrial fibrillation associated with valvular heart disease: executive summary of a joint consensus document from the European Heart Rhythm Association (EHRA) and European Society of Cardiology Working Group on Thrombosis, Endorsed by the ESC Working Group on Valvular Heart Disease, Cardiac Arrhythmia Society of Southern Africa (CASSA), Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), South African Heart (SA Heart) Association and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE) Thromb Haemost. 2017;117(12):2215–2236. doi: 10.1160/TH-17-10-0709. [DOI] [PubMed] [Google Scholar]
- 38.ACTIVE Writing Group of the ACTIVE Investigators Connolly S, Pogue J, Hart R.Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial Lancet 2006367(9526):1903–1912. [DOI] [PubMed] [Google Scholar]
- 39.RE-LY Steering Committee and Investigators . Connolly S J, Ezekowitz M D, Yusuf S. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 40.AVERROES Steering Committee and Investigators . Connolly S J, Eikelboom J, Joyner C. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(09):806–817. doi: 10.1056/NEJMoa1007432. [DOI] [PubMed] [Google Scholar]
- 41.ARISTOTLE Committees and Investigators . Granger C B, Alexander J H, McMurray J J. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 42.Chao T F, Chen S A, Lip G YH. Recommendations on stroke prevention for patients having a CHA 2 DS 2 -VASc score of 1 (males) or 2 (females) in 2019 atrial fibrillation guidelines . Trends Cardiovasc Med. 2019;29(07):427–428. doi: 10.1016/j.tcm.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 43.Chao T F, Liu C J, Wang K L. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J Am Coll Cardiol. 2015;65(07):635–642. doi: 10.1016/j.jacc.2014.11.046. [DOI] [PubMed] [Google Scholar]
- 44.Chao T F, Wang K L, Liu C J. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015;66(12):1339–1347. doi: 10.1016/j.jacc.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 45.Chao T F, Chiang C E, Liao J N, Chen T J, Lip G YH, Chen S A. Comparing the effectiveness and safety of nonvitamin K antagonist oral anticoagulants and warfarin in elderly asian patients with atrial fibrillation: a nationwide cohort study. Chest. 2020;157(05):1266–1277. doi: 10.1016/j.chest.2019.11.025. [DOI] [PubMed] [Google Scholar]
- 46.Kuo L, Chan Y H, Liao J N, Chen S A, Chao T F. Stroke and bleeding risk assessment in atrial fibrillation: where are we now? Korean Circ J. 2021;51(08):668–680. doi: 10.4070/kcj.2021.0170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lee S R, Lee Y S, Park J S. Label adherence for non-vitamin K antagonist oral anticoagulants in a prospective cohort of Asian patients with atrial fibrillation. Yonsei Med J. 2019;60(03):277–284. doi: 10.3349/ymj.2019.60.3.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee S R, Choi E K, Han K D, Jung J H, Oh S, Lip G YH. Optimal rivaroxaban dose in Asian patients with atrial fibrillation and normal or mildly impaired renal function. Stroke. 2019;50(05):1140–1148. doi: 10.1161/STROKEAHA.118.024210. [DOI] [PubMed] [Google Scholar]
- 49.Cheng W H, Chao T F, Lin Y J. Low-dose rivaroxaban and risks of adverse events in patients with atrial fibrillation. Stroke. 2019;50(09):2574–2577. doi: 10.1161/STROKEAHA.119.025623. [DOI] [PubMed] [Google Scholar]
- 50.Chan Y H, Chao T F, Chen S W. Off-label dosing of non-vitamin K antagonist oral anticoagulants and clinical outcomes in Asian patients with atrial fibrillation. Heart Rhythm. 2020;17(12):2102–2110. doi: 10.1016/j.hrthm.2020.07.022. [DOI] [PubMed] [Google Scholar]
- 51.Yu H T, Yang P S, Jang E. Label adherence of direct oral anticoagulants dosing and clinical outcomes in patients with atrial fibrillation. J Am Heart Assoc. 2020;9(12):e014177. doi: 10.1161/JAHA.119.014177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee S R, Choi E K, Park S H. Off-label underdosed apixaban use in Asian patients with non-valvular atrial fibrillation. Eur Heart J Cardiovasc Pharmacother. 2021;7(05):415–423. doi: 10.1093/ehjcvp/pvab004. [DOI] [PubMed] [Google Scholar]
- 53.Kim D, Yang P S, Jang E. The optimal drug adherence to maximize the efficacy and safety of non-vitamin K antagonist oral anticoagulant in real-world atrial fibrillation patients. Europace. 2020;22(04):547–557. doi: 10.1093/europace/euz273. [DOI] [PubMed] [Google Scholar]
- 54.Kim H, Lee Y S, Kim T H. A prospective survey of the persistence of warfarin or NOAC in nonvalvular atrial fibrillation: a COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Korean J Intern Med (Korean Assoc Intern Med) 2020;35(01):99–108. doi: 10.3904/kjim.2017.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guo Y, Kotalczyk A, Imberti J F, Wang Y, Lip G YH. Quality indicators in the management of elderly Chinese patients with atrial fibrillation: a report from the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. Eur Heart J Qual Care Clin Outcomes. 2021 doi: 10.1093/ehjqcco/qcab057. [DOI] [PubMed] [Google Scholar]
- 56.Pandey A K, Xu K, Zhang L. Lower versus standard INR targets in atrial fibrillation: a systematic review and meta-analysis of randomized controlled trials. Thromb Haemost. 2020;120(03):484–494. doi: 10.1055/s-0039-3401823. [DOI] [PubMed] [Google Scholar]
- 57.Berwaerts J, Dijkhuizen R S, Robb O J, Webster J. Prediction of functional outcome and in-hospital mortality after admission with oral anticoagulant-related intracerebral hemorrhage. Stroke. 2000;31(11):2558–2562. doi: 10.1161/01.str.31.11.2558. [DOI] [PubMed] [Google Scholar]
- 58.Wan Y, Heneghan C, Perera R. Anticoagulation control and prediction of adverse events in patients with atrial fibrillation: a systematic review. Circ Cardiovasc Qual Outcomes. 2008;1(02):84–91. doi: 10.1161/CIRCOUTCOMES.108.796185. [DOI] [PubMed] [Google Scholar]
- 59.Proietti M, Lane D A, Lip G Y. Relation of the SAMe-TT2R2 score to quality of anticoagulation control and thromboembolic events in atrial fibrillation patients: observations from the SPORTIF trials. Int J Cardiol. 2016;216:168–172. doi: 10.1016/j.ijcard.2016.04.131. [DOI] [PubMed] [Google Scholar]
- 60.Chan P H, Hai J J, Chan E W. Use of the SAMe-TT2R2 score to predict good anticoagulation control with warfarin in chinese patients with atrial fibrillation: relationship to ischemic stroke incidence. PLoS One. 2016;11(03):e0150674. doi: 10.1371/journal.pone.0150674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Roldán V, Cancio S, Gálvez J. The SAMe-TT2R2 score predicts poor anticoagulation control in AF patients: a prospective ‘real-world’ inception cohort study. Am J Med. 2015;128(11):1237–1243. doi: 10.1016/j.amjmed.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 62.Gallego P, Roldán V, Marin F. SAMe-TT2R2 score, time in therapeutic range, and outcomes in anticoagulated patients with atrial fibrillation. Am J Med. 2014;127(11):1083–1088. doi: 10.1016/j.amjmed.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 63.Apostolakis S, Sullivan R M, Olshansky B, Lip G YH. Factors affecting quality of anticoagulation control among patients with atrial fibrillation on warfarin: the SAMe-TT 2 R 2 score . Chest. 2013;144(05):1555–1563. doi: 10.1378/chest.13-0054. [DOI] [PubMed] [Google Scholar]
- 64.TREATS-AF Study Group . Phrommintikul A, Nathisuwan S, Gunaparn S. Prospective randomised trial examining the impact of an educational intervention versus usual care on anticoagulation therapy control based on an SAMe-TT 2 R 2 score-guided strategy in anticoagulant-naïve Thai patients with atrial fibrillation (TREATS-AF): a study protocol . BMJ Open. 2021;11(10):e051987. doi: 10.1136/bmjopen-2021-051987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang K L, Lip G Y, Lin S J, Chiang C E. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015;46(09):2555–2561. doi: 10.1161/STROKEAHA.115.009947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu T, Hui J, Hou Y Y. Meta-analysis of efficacy and safety of low-intensity warfarin therapy for East Asian patients with nonvalvular atrial fibrillation. Am J Cardiol. 2017;120(09):1562–1567. doi: 10.1016/j.amjcard.2017.07.050. [DOI] [PubMed] [Google Scholar]
- 67.J-RHYTHM Registry Investigators . Kodani E, Atarashi H, Inoue H, Okumura K, Yamashita T. Target intensity of anticoagulation with warfarin in Japanese patients with valvular atrial fibrillation – subanalysis of the J-RHYTHM registry. Circ J. 2015;79(02):325–330. doi: 10.1253/circj.CJ-14-1057. [DOI] [PubMed] [Google Scholar]
- 68.Chao T F, Guo Y. Should we adopt a standard international normalized ratio range of 2.0 to 3.0 for Asian patients with atrial fibrillation? An appeal for evidence-based management, not eminence-based recommendations. Thromb Haemost. 2020;120(03):366–368. doi: 10.1055/s-0040-1702230. [DOI] [PubMed] [Google Scholar]
- 69.Pritchett R V, Bem D, Turner G M. Improving the prescription of oral anticoagulants in atrial fibrillation: a systematic review. Thromb Haemost. 2019;119(02):294–307. doi: 10.1055/s-0038-1676835. [DOI] [PubMed] [Google Scholar]
- 70.Hwang J, Han S, Bae H J. NOAC adherence of patients with atrial fibrillation in the real world: dosing frequency matters? Thromb Haemost. 2020;120(02):306–313. doi: 10.1055/s-0039-1697954. [DOI] [PubMed] [Google Scholar]
- 71.Jones N R, Crawford W, Yang Y, Hobbs F DR, Taylor C J, Petrou S.A systematic review of economic aspects of service interventions to increase anticoagulation use in atrial fibrillationThromb Haemost2021 [DOI] [PubMed]
- 72.Ruff C T, Giugliano R P, Braunwald E.Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials Lancet 2014383(9921):955–962. [DOI] [PubMed] [Google Scholar]
- 73.Chao T F, Chen S A, Ruff C T. Clinical outcomes, edoxaban concentration, and anti-factor Xa activity of Asian patients with atrial fibrillation compared with non-Asians in the ENGAGE AF-TIMI 48 trial. Eur Heart J. 2019;40(19):1518–1527. doi: 10.1093/eurheartj/ehy807. [DOI] [PubMed] [Google Scholar]
- 74.Chan Y H, Lee H F, Chao T F. Real-world comparisons of direct oral anticoagulants for stroke prevention in asian patients with non-valvular atrial fibrillation: a systematic review and meta-analysis. Cardiovasc Drugs Ther. 2019;33(06):701–710. doi: 10.1007/s10557-019-06910-z. [DOI] [PubMed] [Google Scholar]
- 75.Chao T F, Liu C J, Lin Y J. Oral anticoagulation in very elderly patients with atrial fibrillation: a nationwide cohort study. Circulation. 2018;138(01):37–47. doi: 10.1161/CIRCULATIONAHA.117.031658. [DOI] [PubMed] [Google Scholar]
- 76.Lee S R, Choi E K, Park C S. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019;73(08):919–931. doi: 10.1016/j.jacc.2018.11.051. [DOI] [PubMed] [Google Scholar]
- 77.Lee S R, Lee H J, Choi E K. Direct oral anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll Cardiol. 2019;73(25):3295–3308. doi: 10.1016/j.jacc.2019.04.052. [DOI] [PubMed] [Google Scholar]
- 78.Kuo L, Chao T F, Liu C J. Liver cirrhosis in patients with atrial fibrillation: would oral anticoagulation have a net clinical benefit for stroke prevention? J Am Heart Assoc. 2017;6(06):6. doi: 10.1161/JAHA.116.005307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kwon S, Lee S R, Choi E K. Non-vitamin K antagonist oral anticoagulants in very elderly east Asians with atrial fibrillation: a nationwide population-based study. Am Heart J. 2020;229:81–91. doi: 10.1016/j.ahj.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 80.Tsai C T, Liao J N, Chen S J, Jiang Y R, Chen T J, Chao T F. Non-vitamin K antagonist oral anticoagulants versus warfarin in AF patients ≥ 85 years. Eur J Clin Invest. 2021;51(06):e13488. doi: 10.1111/eci.13488. [DOI] [PubMed] [Google Scholar]
- 81.Yao X, Shah N D, Sangaralingham L R, Gersh B J, Noseworthy P A. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69(23):2779–2790. doi: 10.1016/j.jacc.2017.03.600. [DOI] [PubMed] [Google Scholar]
- 82.Pokorney S D, Peterson E D, Piccini J P. When less is not more. J Am Coll Cardiol. 2017;69:2791–2793. doi: 10.1016/j.jacc.2017.04.045. [DOI] [PubMed] [Google Scholar]
- 83.Wang K L, Lopes R D, Patel M R. Efficacy and safety of reduced-dose non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation: a meta-analysis of randomized controlled trials. Eur Heart J. 2019;40(19):1492–1500. doi: 10.1093/eurheartj/ehy802. [DOI] [PubMed] [Google Scholar]
- 84.Cheng W H, Chan Y H, Liao J N, Kuo L, Chen S A, Chao T F. Optimal management of anticoagulation therapy in Asian patients with atrial fibrillation. Circ J. 2021;85(08):1245–1253. doi: 10.1253/circj.CJ-21-0399. [DOI] [PubMed] [Google Scholar]
- 85.Chan Y H, Chao T F, Lee H F. Impacts of different renal function estimation formulas on dosing of DOACs and clinical outcomes. J Am Coll Cardiol. 2020;76(15):1808–1810. doi: 10.1016/j.jacc.2020.08.025. [DOI] [PubMed] [Google Scholar]
- 86.Chan Y H, Lee H F, Wang C L. Comparisons of rivaroxaban following different dosage criteria (ROCKET AF or J-ROCKET AF trials) in Asian patients with atrial fibrillation. J Am Heart Assoc. 2019;8(21):e013053. doi: 10.1161/JAHA.119.013053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Angiolillo D J, Goodman S G, Bhatt D L. Antithrombotic therapy in patients with atrial fibrillation undergoing percutaneous coronary intervention: a North American Perspective-2016 update. Circ Cardiovasc Interv. 2016;9(11):9. doi: 10.1161/CIRCINTERVENTIONS.116.004395. [DOI] [PubMed] [Google Scholar]
- 88.Park J, Choi E K, Han K D. Temporal trends in prevalence and antithrombotic treatment among Asians with atrial fibrillation undergoing percutaneous coronary intervention: a nationwide Korean population-based study. PLoS One. 2019;14(01):e0209593. doi: 10.1371/journal.pone.0209593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kwon S, Jung J H, Choi E K. Impact of non-vitamin K antagonist oral anticoagulants on the change of antithrombotic regimens in patients with atrial fibrillation undergoing percutaneous coronary intervention. Korean Circ J. 2021;51(05):409–422. doi: 10.4070/kcj.2020.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Vitolo M, Javed S, Capodanno D, Rubboli A, Boriani G, Lip G YH. Antithrombotic treatment in atrial fibrillation patients undergoing percutaneous coronary interventions: focus on stent thrombosis. Expert Rev Cardiovasc Ther. 2020;18(09):587–600. doi: 10.1080/14779072.2020.1808463. [DOI] [PubMed] [Google Scholar]
- 91.Kim H K, Tantry U S, Smith S C., Jr The East Asian paradox: an updated position statement on the challenges to the current antithrombotic strategy in patients with cardiovascular disease. Thromb Haemost. 2021;121(04):422–432. doi: 10.1055/s-0040-1718729. [DOI] [PubMed] [Google Scholar]
- 92.WOEST study investigators Dewilde W J, Oirbans T, Verheugt F W.Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial Lancet 2013381(9872):1107–1115. [DOI] [PubMed] [Google Scholar]
- 93.Gibson C M, Mehran R, Bode C. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016;375(25):2423–2434. doi: 10.1056/NEJMoa1611594. [DOI] [PubMed] [Google Scholar]
- 94.RE-DUAL PCI Steering Committee and Investigators . Cannon C P, Bhatt D L, Oldgren J. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017;377(16):1513–1524. doi: 10.1056/NEJMoa1708454. [DOI] [PubMed] [Google Scholar]
- 95.AUGUSTUS Investigators . Lopes R D, Heizer G, Aronson R. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019;380(16):1509–1524. doi: 10.1056/NEJMoa1817083. [DOI] [PubMed] [Google Scholar]
- 96.Vranckx P, Valgimigli M, Eckardt L.Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial Lancet 2019394(10206):1335–1343. [DOI] [PubMed] [Google Scholar]
- 97.Oldgren J, Steg P G, Hohnloser S H. Dabigatran dual therapy with ticagrelor or clopidogrel after percutaneous coronary intervention in atrial fibrillation patients with or without acute coronary syndrome: a subgroup analysis from the RE-DUAL PCI trial. Eur Heart J. 2019;40(19):1553–1562. doi: 10.1093/eurheartj/ehz059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Steffel J, Collins R, Antz M. 2021 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Europace. 2021;23(10):1612–1676. doi: 10.1093/europace/euab065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lee S R, Rhee T M, Kang D Y, Choi E K, Oh S, Lip G YH. Meta-analysis of oral anticoagulant monotherapy as an antithrombotic strategy in patients with stable coronary artery disease and nonvalvular atrial fibrillation. Am J Cardiol. 2019;124(06):879–885. doi: 10.1016/j.amjcard.2019.05.072. [DOI] [PubMed] [Google Scholar]
- 100.AFIRE Investigators . Yasuda S, Kaikita K, Akao M. Antithrombotic therapy for atrial fibrillation with stable coronary disease. N Engl J Med. 2019;381(12):1103–1113. doi: 10.1056/NEJMoa1904143. [DOI] [PubMed] [Google Scholar]
- 101.Di Biase L, Burkhardt J D, Santangeli P. Periprocedural stroke and bleeding complications in patients undergoing catheter ablation of atrial fibrillation with different anticoagulation management: results from the Role of Coumadin in Preventing Thromboembolism in Atrial Fibrillation (AF) Patients Undergoing Catheter Ablation (COMPARE) randomized trial. Circulation. 2014;129(25):2638–2644. doi: 10.1161/CIRCULATIONAHA.113.006426. [DOI] [PubMed] [Google Scholar]
- 102.Calkins H, Hindricks G, Cappato R. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–e444. doi: 10.1016/j.hrthm.2017.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Japanese Heart Rhythm Society Members . Murakawa Y, Yamane T, Goya M. Influence of substrate modification in catheter ablation of atrial fibrillation on the incidence of acute complications: analysis of 10 795 procedures in J-CARAF Study 2011-2016. J Arrhythm. 2018;34(04):435–440. doi: 10.1002/joa3.12081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hohnloser S H, Camm A J. Safety and efficacy of dabigatran etexilate during catheter ablation of atrial fibrillation: a meta-analysis of the literature. Europace. 2013;15(10):1407–1411. doi: 10.1093/europace/eut241. [DOI] [PubMed] [Google Scholar]
- 105.VENTURE-AF Investigators . Cappato R, Marchlinski F E, Hohnloser S H. Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J. 2015;36(28):1805–1811. doi: 10.1093/eurheartj/ehv177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.RE-CIRCUIT Investigators . Calkins H, Willems S, Gerstenfeld E P. Uninterrupted dabigatran versus warfarin for ablation in atrial fibrillation. N Engl J Med. 2017;376(17):1627–1636. doi: 10.1056/NEJMoa1701005. [DOI] [PubMed] [Google Scholar]
- 107.Kirchhof P, Haeusler K G, Blank B. Apixaban in patients at risk of stroke undergoing atrial fibrillation ablation. Eur Heart J. 2018;39(32):2942–2955. doi: 10.1093/eurheartj/ehy176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hohnloser S H, Camm J, Cappato R. Uninterrupted edoxaban vs. vitamin K antagonists for ablation of atrial fibrillation: the ELIMINATE-AF trial. Eur Heart J. 2019;40(36):3013–3021. doi: 10.1093/eurheartj/ehz190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhao Y, Lu Y, Qin Y. A meta-analysis of randomized controlled trials of uninterrupted periprocedural anticoagulation strategy in patients undergoing atrial fibrillation catheter ablation. Int J Cardiol. 2018;270:167–171. doi: 10.1016/j.ijcard.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 110.Cardoso R, Knijnik L, Bhonsale A. An updated meta-analysis of novel oral anticoagulants versus vitamin K antagonists for uninterrupted anticoagulation in atrial fibrillation catheter ablation. Heart Rhythm. 2018;15(01):107–115. doi: 10.1016/j.hrthm.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 111.Nakamura K, Naito S, Sasaki T. Uninterrupted vs. interrupted periprocedural direct oral anticoagulants for catheter ablation of atrial fibrillation: a prospective randomized single-centre study on post-ablation thrombo-embolic and haemorrhagic events. Europace. 2019;21(02):259–267. doi: 10.1093/europace/euy148. [DOI] [PubMed] [Google Scholar]
- 112.Yu H T, Shim J, Park J. When is it appropriate to stop non-vitamin K antagonist oral anticoagulants before catheter ablation of atrial fibrillation? A multicentre prospective randomized study. Eur Heart J. 2019;40(19):1531–1537. doi: 10.1093/eurheartj/ehy870. [DOI] [PubMed] [Google Scholar]
- 113.ABRIDGE-J (ABlation peRIoperative DabiGatran in use Envisioning in Japan) Investigators . Nogami A, Harada T, Sekiguchi Y. Safety and efficacy of minimally interrupted dabigatran vs uninterrupted warfarin therapy in adults undergoing atrial fibrillation catheter ablation: a randomized clinical trial. JAMA Netw Open. 2019;2(04):e191994. doi: 10.1001/jamanetworkopen.2019.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.KYU-RABLE Investigators . Takahashi N, Mukai Y, Kimura T. Efficacy and safety of uninterrupted periprocedural edoxaban in patients undergoing catheter ablation for atrial fibrillation - the prospective KYU-RABLE study. Circ J. 2019;83(10):2017–2024. doi: 10.1253/circj.CJ-19-0535. [DOI] [PubMed] [Google Scholar]
- 115.Schiele F, van Ryn J, Canada K. A specific antidote for dabigatran: functional and structural characterization. Blood. 2013;121(18):3554–3562. doi: 10.1182/blood-2012-11-468207. [DOI] [PubMed] [Google Scholar]
- 116.Pollack C V, Jr, Reilly P A, Eikelboom J. Idarucizumab for dabigatran reversal. N Engl J Med. 2015;373(06):511–520. doi: 10.1056/NEJMoa1502000. [DOI] [PubMed] [Google Scholar]
- 117.Pollack C V, Jr, Reilly P A, van Ryn J. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377(05):431–441. doi: 10.1056/NEJMoa1707278. [DOI] [PubMed] [Google Scholar]
- 118.Eikelboom J W, van Ryn J, Reilly P. Dabigatran reversal with idarucizumab in patients with renal impairment. J Am Coll Cardiol. 2019;74(14):1760–1768. doi: 10.1016/j.jacc.2019.07.070. [DOI] [PubMed] [Google Scholar]
- 119.Fanikos J, Murwin D, Gruenenfelder F. Global use of idarucizumab in clinical practice: outcomes of the RE-VECTO surveillance program. Thromb Haemost. 2020;120(01):27–35. doi: 10.1055/s-0039-1695771. [DOI] [PubMed] [Google Scholar]
- 120.Lu G, DeGuzman F R, Hollenbach S J. A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa. Nat Med. 2013;19(04):446–451. doi: 10.1038/nm.3102. [DOI] [PubMed] [Google Scholar]
- 121.Siegal D M, Curnutte J T, Connolly S J. Andexanet alfa for the reversal of factor Xa inhibitor activity. N Engl J Med. 2015;373(25):2413–2424. doi: 10.1056/NEJMoa1510991. [DOI] [PubMed] [Google Scholar]
- 122.ANNEXA-4 Investigators . Connolly S J, Crowther M, Eikelboom J W. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380(14):1326–1335. doi: 10.1056/NEJMoa1814051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chang T Y, Chan Y H, Chiang C E. Risks and outcomes of gastrointestinal malignancies in anticoagulated atrial fibrillation patients experiencing gastrointestinal bleeding: a nationwide cohort study. Heart Rhythm. 2020;17(10):1745–1751. doi: 10.1016/j.hrthm.2020.05.026. [DOI] [PubMed] [Google Scholar]
- 124.Yu H T, Kim T H, Uhm J S. Clinical significance of hematuria in atrial fibrillation with oral anticoagulation therapy. Circ J. 2017;81(02):158–164. doi: 10.1253/circj.CJ-16-0917. [DOI] [PubMed] [Google Scholar]
- 125.ESC Scientific Document Group . Glikson M, Wolff R, Hindricks G. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion - an update. Europace. 2019 doi: 10.1093/europace/euz258. [DOI] [Google Scholar]
- 126.LAAOS III Investigators . Whitlock R P, Belley-Cote E P, Paparella D. Left atrial appendage occlusion during cardiac surgery to prevent stroke. N Engl J Med. 2021;384(22):2081–2091. doi: 10.1056/NEJMoa2101897. [DOI] [PubMed] [Google Scholar]
- 127.PROTECT AF Investigators Holmes D R, Reddy V Y, Turi Z G.Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial Lancet 2009374(9689):534–542. [DOI] [PubMed] [Google Scholar]
- 128.Holmes D R, Jr, Kar S, Price M J. Prospective randomized evaluation of the Watchman Left Atrial Appendage Closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. J Am Coll Cardiol. 2014;64(01):1–12. doi: 10.1016/j.jacc.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 129.Reddy V Y, Holmes D, Doshi S K, Neuzil P, Kar S. Safety of percutaneous left atrial appendage closure: results from the Watchman Left Atrial Appendage System for Embolic Protection in Patients with AF (PROTECT AF) clinical trial and the Continued Access Registry. Circulation. 2011;123(04):417–424. doi: 10.1161/CIRCULATIONAHA.110.976449. [DOI] [PubMed] [Google Scholar]
- 130.Holmes D R, Jr, Doshi S K, Kar S. Left atrial appendage closure as an alternative to warfarin for stroke prevention in atrial fibrillation: a patient-level meta-analysis. J Am Coll Cardiol. 2015;65(24):2614–2623. doi: 10.1016/j.jacc.2015.04.025. [DOI] [PubMed] [Google Scholar]
- 131.PRAGUE-17 Investigators . Osmancik P, Tousek P, Herman D. Interventional left atrial appendage closure vs novel anticoagulation agents in patients with atrial fibrillation indicated for long-term anticoagulation (PRAGUE-17 study) Am Heart J. 2017;183:108–114. doi: 10.1016/j.ahj.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 132.PRAGUE-17 Trial Investigators . Osmancik P, Herman D, Neuzil P. Left atrial appendage closure versus direct oral anticoagulants in high-risk patients with atrial fibrillation. J Am Coll Cardiol. 2020;75(25):3122–3135. doi: 10.1016/j.jacc.2020.04.067. [DOI] [PubMed] [Google Scholar]
- 133.EWOLUTION Investigators . Boersma L V, Ince H, Kische S. Efficacy and safety of left atrial appendage closure with WATCHMAN in patients with or without contraindication to oral anticoagulation: 1-year follow-up outcome data of the EWOLUTION trial. Heart Rhythm. 2017;14(09):1302–1308. doi: 10.1016/j.hrthm.2017.05.038. [DOI] [PubMed] [Google Scholar]
- 134.Mazzone P, D'Angelo G, Regazzoli D. Percutaneous left atrial appendage closure with WATCHMAN™ device: peri-procedural and mid-term outcomes from the TRAPS registry. J Interv Card Electrophysiol. 2018;52(01):47–52. doi: 10.1007/s10840-018-0351-1. [DOI] [PubMed] [Google Scholar]
- 135.following investigators and institutions participated in the EWOLUTION study . Boersma L V, Ince H, Kische S. Evaluating real-world clinical outcomes in atrial fibrillation patients receiving the WATCHMAN left atrial appendage closure technology: final 2-year outcome data of the EWOLUTION trial focusing on history of stroke and hemorrhage. Circ Arrhythm Electrophysiol. 2019;12(04):e006841. doi: 10.1161/CIRCEP.118.006841. [DOI] [PubMed] [Google Scholar]
- 136.Aonuma K, Yamasaki H, Nakamura M. Percutaneous WATCHMAN left atrial appendage closure for Japanese patients with nonvalvular atrial fibrillation at increased risk of thromboembolism - first results from the SALUTE trial. Circ J. 2018;82(12):2946–2953. doi: 10.1253/circj.CJ-18-0222. [DOI] [PubMed] [Google Scholar]
- 137.Phillips K P, Santoso T, Sanders P. Left atrial appendage closure with WATCHMAN in Asian patients: 2μyear outcomes from the WASP registry. Int J Cardiol Heart Vasc. 2019;23:100358. doi: 10.1016/j.ijcha.2019.100358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bajaj N S, Parashar A, Agarwal S. Percutaneous left atrial appendage occlusion for stroke prophylaxis in nonvalvular atrial fibrillation: a systematic review and analysis of observational studies. JACC Cardiovasc Interv. 2014;7(03):296–304. doi: 10.1016/j.jcin.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 139.Badheka A O, Chothani A, Mehta K. Utilization and adverse outcomes of percutaneous left atrial appendage closure for stroke prevention in atrial fibrillation in the United States: influence of hospital volume. Circ Arrhythm Electrophysiol. 2015;8(01):42–48. doi: 10.1161/CIRCEP.114.001413. [DOI] [PubMed] [Google Scholar]
- 140.Lempereur M, Aminian A, Freixa X. Device-associated thrombus formation after left atrial appendage occlusion: a systematic review of events reported with the Watchman, the Amplatzer Cardiac Plug and the Amulet. Catheter Cardiovasc Interv. 2017;90(05):E111–E121. doi: 10.1002/ccd.26903. [DOI] [PubMed] [Google Scholar]
- 141.Fauchier L, Cinaud A, Brigadeau F. Device-related thrombosis after percutaneous left atrial appendage occlusion for atrial fibrillation. J Am Coll Cardiol. 2018;71(14):1528–1536. doi: 10.1016/j.jacc.2018.01.076. [DOI] [PubMed] [Google Scholar]
- 142.Fauchier L, Cinaud A, Brigadeau F. Major adverse events with percutaneous left atrial appendage closure in patients with atrial fibrillation. J Am Coll Cardiol. 2019;73(20):2638–2640. doi: 10.1016/j.jacc.2019.03.468. [DOI] [PubMed] [Google Scholar]
- 143.Sedaghat A, Vij V, Al-Kassou B. Device-related thrombus after left atrial appendage closure: data on thrombus characteristics, treatment strategies, and clinical outcomes from the EUROC-DRT-registry. Circ Cardiovasc Interv. 2021;14(05):e010195. doi: 10.1161/CIRCINTERVENTIONS.120.010195. [DOI] [PubMed] [Google Scholar]
- 144.Holmes D R, Reddy V Y, Buchbinder M. The Assessment of the Watchman Device in Patients Unsuitable for Oral Anticoagulation (ASAP-TOO) trial. Am Heart J. 2017;189:68–74. doi: 10.1016/j.ahj.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 145.Reddy V Y, Akehurst R L, Armstrong S O, Amorosi S L, Beard S M, Holmes D R., Jr Time to cost-effectiveness following stroke reduction strategies in AF: warfarin versus NOACs versus LAA closure. J Am Coll Cardiol. 2015;66(24):2728–2739. doi: 10.1016/j.jacc.2015.09.084. [DOI] [PubMed] [Google Scholar]
- 146.Reddy V Y, Akehurst R L, Gavaghan M B, Amorosi S L, Holmes D R., Jr Cost-effectiveness of left atrial appendage closure for stroke reduction in atrial fibrillation: analysis of pooled, 5-year, long-term data. J Am Heart Assoc. 2019;8(13):e011577. doi: 10.1161/JAHA.118.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Pathak R K, Elliott A, Middeldorp M E. Impact of CARDIOrespiratory FITness on arrhythmia recurrence in obese individuals with atrial fibrillation: the CARDIO-FIT study. J Am Coll Cardiol. 2015;66(09):985–996. doi: 10.1016/j.jacc.2015.06.488. [DOI] [PubMed] [Google Scholar]
- 148.Pathak R K, Middeldorp M E, Lau D H. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J Am Coll Cardiol. 2014;64(21):2222–2231. doi: 10.1016/j.jacc.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 149.Pathak R K, Middeldorp M E, Meredith M. Long-term effect of goal-directed weight management in an atrial fibrillation cohort: a long-term follow-up study (LEGACY) J Am Coll Cardiol. 2015;65(20):2159–2169. doi: 10.1016/j.jacc.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 150.Lim C, Kim T H, Yu H T. Effect of alcohol consumption on the risk of adverse events in atrial fibrillation: from the COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) registry. Europace. 2021;23(04):548–556. doi: 10.1093/europace/euaa340. [DOI] [PubMed] [Google Scholar]
- 151.Joung B. Risk factor management for atrial fibrillation. Korean Circ J. 2019;49(09):794–807. doi: 10.4070/kcj.2019.0212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Kim T H, Yang P S, Yu H T. Effect of hypertension duration and blood pressure level on ischaemic stroke risk in atrial fibrillation: nationwide data covering the entire Korean population. Eur Heart J. 2019;40(10):809–819. doi: 10.1093/eurheartj/ehy877. [DOI] [PubMed] [Google Scholar]
- 153.Kim D, Yang P S, Kim T H. Ideal blood pressure in patients with atrial fibrillation. J Am Coll Cardiol. 2018;72(11):1233–1245. doi: 10.1016/j.jacc.2018.05.076. [DOI] [PubMed] [Google Scholar]
- 154.Lee S S, Ae Kong K, Kim D. Clinical implication of an impaired fasting glucose and prehypertension related to new onset atrial fibrillation in a healthy Asian population without underlying disease: a nationwide cohort study in Korea. Eur Heart J. 2017;38(34):2599–2607. doi: 10.1093/eurheartj/ehx316. [DOI] [PubMed] [Google Scholar]
- 155.Lee S R, Choi E K, Ahn H J, Han K D, Oh S, Lip G YH. Association between clustering of unhealthy lifestyle factors and risk of new-onset atrial fibrillation: a nationwide population-based study. Sci Rep. 2020;10(01):19224. doi: 10.1038/s41598-020-75822-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Lee J H, Yang P S, Yu H T. Association of cardiovascular health and incident atrial fibrillation in elderly population. Heart. 2021 doi: 10.1136/heartjnl-2020-318858. [DOI] [PubMed] [Google Scholar]
- 157.Wang T J, Parise H, Levy D. Obesity and the risk of new-onset atrial fibrillation. JAMA. 2004;292(20):2471–2477. doi: 10.1001/jama.292.20.2471. [DOI] [PubMed] [Google Scholar]
- 158.Baek Y S, Yang P S, Kim T H. Associations of abdominal obesity and new-onset atrial fibrillation in the general population. J Am Heart Assoc. 2017;6(06):6. doi: 10.1161/JAHA.116.004705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Abed H S, Wittert G A, Leong D P. Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trial. JAMA. 2013;310(19):2050–2060. doi: 10.1001/jama.2013.280521. [DOI] [PubMed] [Google Scholar]
- 160.Lim Y M, Yang P S, Jang E. Body mass index variability and long-term risk of new-onset atrial fibrillation in the general population: a Korean nationwide cohort study. Mayo Clin Proc. 2019;94(02):225–235. doi: 10.1016/j.mayocp.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 161.Middeldorp M E, Pathak R K, Meredith M. PREVEntion and regReSsive Effect of weight-loss and risk factor modification on Atrial Fibrillation: the REVERSE-AF study. Europace. 2018;20(12):1929–1935. doi: 10.1093/europace/euy117. [DOI] [PubMed] [Google Scholar]
- 162.Kang S H, Choi E K, Han K D. Underweight is a risk factor for atrial fibrillation: a nationwide population-based study. Int J Cardiol. 2016;215:449–456. doi: 10.1016/j.ijcard.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 163.Lee H J, Choi E K, Han K D. Bodyweight fluctuation is associated with increased risk of incident atrial fibrillation. Heart Rhythm. 2020;17(03):365–371. doi: 10.1016/j.hrthm.2019.09.029. [DOI] [PubMed] [Google Scholar]
- 164.Overvad T F, Rasmussen L H, Skjøth F, Overvad K, Lip G Y, Larsen T B. Body mass index and adverse events in patients with incident atrial fibrillation. Am J Med. 2013;126(07):6.4E11–6.4E19. doi: 10.1016/j.amjmed.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 165.Proietti M, Guiducci E, Cheli P, Lip G Y. Is there an obesity paradox for outcomes in atrial fibrillation? A systematic review and meta-analysis of non-vitamin K antagonist oral anticoagulant trials. Stroke. 2017;48(04):857–866. doi: 10.1161/STROKEAHA.116.015984. [DOI] [PubMed] [Google Scholar]
- 166.Lee S R, Choi E K, Jung J H. Body mass index and clinical outcomes in asian patients with atrial fibrillation receiving oral anticoagulation. Stroke. 2021;52(02):521–530. doi: 10.1161/STROKEAHA.120.030356. [DOI] [PubMed] [Google Scholar]
- 167.Larsson S C, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol. 2014;64(03):281–289. doi: 10.1016/j.jacc.2014.03.048. [DOI] [PubMed] [Google Scholar]
- 168.Pisters R, Lane D A, Nieuwlaat R, de Vos C B, Crijns H J, Lip G Y. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(05):1093–1100. doi: 10.1378/chest.10-0134. [DOI] [PubMed] [Google Scholar]
- 169.Overvad T F, Rasmussen L H, Skjøth F. Alcohol intake and prognosis of atrial fibrillation. Heart. 2013;99(15):1093–1099. doi: 10.1136/heartjnl-2013-304036. [DOI] [PubMed] [Google Scholar]
- 170.Lee S R, Choi E K, Jung J H, Han K D, Oh S, Lip G YH. Lower risk of stroke after alcohol abstinence in patients with incident atrial fibrillation: a nationwide population-based cohort study. Eur Heart J. 2021 doi: 10.1093/eurheartj/ehab315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Voskoboinik A, Kalman J M, De Silva A. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382(01):20–28. doi: 10.1056/NEJMoa1817591. [DOI] [PubMed] [Google Scholar]
- 172.Choi Y J, Han K D, Choi E K. Alcohol abstinence and the risk of atrial fibrillation in patients with newly diagnosed type 2 diabetes mellitus: a nationwide population-based study. Diabetes Care. 2021;44:1393–1401. doi: 10.2337/dc20-2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Chamberlain A M, Agarwal S K, Folsom A R. Smoking and incidence of atrial fibrillation: results from the Atherosclerosis Risk in Communities (ARIC) study. Heart Rhythm. 2011;8(08):1160–1166. doi: 10.1016/j.hrthm.2011.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhu W, Yuan P, Shen Y, Wan R, Hong K. Association of smoking with the risk of incident atrial fibrillation: a meta-analysis of prospective studies. Int J Cardiol. 2016;218:259–266. doi: 10.1016/j.ijcard.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 175.Kwon S, Kim T J, Choi E K. Predictors of ischemic stroke for low-risk patients with atrial fibrillation: a matched case-control study. Heart Rhythm. 2021;18(05):702–708. doi: 10.1016/j.hrthm.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 176.Lee S R, Choi E K, Jung J H, Han K D, Oh S, Lip G YH. Smoking cessation after diagnosis of new-onset atrial fibrillation and the risk of stroke and death. J Clin Med. 2021;10(11):10. doi: 10.3390/jcm10112238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kim I S, Yang P S, Lee J. Long-term exposure of fine particulate matter air pollution and incident atrial fibrillation in the general population: a nationwide cohort study. Int J Cardiol. 2019;283:178–183. doi: 10.1016/j.ijcard.2018.12.048. [DOI] [PubMed] [Google Scholar]
- 178.Kim I S, Yang P S, Jang E. Long-term PM 2.5 exposure and the clinical application of machine learning for predicting incident atrial fibrillation . Sci Rep. 2020;10(01):16324. doi: 10.1038/s41598-020-73537-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mozaffarian D, Furberg C D, Psaty B M, Siscovick D. Physical activity and incidence of atrial fibrillation in older adults: the cardiovascular health study. Circulation. 2008;118(08):800–807. doi: 10.1161/CIRCULATIONAHA.108.785626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Hegbom F, Stavem K, Sire S, Heldal M, Orning O M, Gjesdal K. Effects of short-term exercise training on symptoms and quality of life in patients with chronic atrial fibrillation. Int J Cardiol. 2007;116(01):86–92. doi: 10.1016/j.ijcard.2006.03.034. [DOI] [PubMed] [Google Scholar]
- 181.Osbak P S, Mourier M, Kjaer A, Henriksen J H, Kofoed K F, Jensen G B. A randomized study of the effects of exercise training on patients with atrial fibrillation. Am Heart J. 2011;162(06):1080–1087. doi: 10.1016/j.ahj.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 182.Faselis C, Kokkinos P, Tsimploulis A. Exercise capacity and atrial fibrillation risk in veterans: a cohort study. Mayo Clin Proc. 2016;91(05):558–566. doi: 10.1016/j.mayocp.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 183.Jin M N, Yang P S, Song C. Physical activity and risk of atrial fibrillation: a nationwide cohort study in general population. Sci Rep. 2019;9(01):13270. doi: 10.1038/s41598-019-49686-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Abdulla J, Nielsen J R. Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis. Europace. 2009;11(09):1156–1159. doi: 10.1093/europace/eup197. [DOI] [PubMed] [Google Scholar]
- 185.Ahn H J, Lee S R, Choi E K. Association between exercise habits and stroke, heart failure, and mortality in Korean patients with incident atrial fibrillation: a nationwide population-based cohort study. PLoS Med. 2021;18(06):e1003659. doi: 10.1371/journal.pmed.1003659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Lim J, Lee S R, Choi E K. Exercise and the risk of dementia in patients with newly diagnosed atrial fibrillation: a nationwide population-based study. J Clin Med. 2021;10(14):10. doi: 10.3390/jcm10143126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Elias P, Poterucha T J, Jain S S. The prognostic value of electrocardiogram at presentation to emergency department in patients with COVID-19. Mayo Clin Proc. 2020;95(10):2099–2109. doi: 10.1016/j.mayocp.2020.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Musikantow D R, Turagam M K, Sartori S. Atrial fibrillation in patients hospitalized with COVID-19: incidence, predictors, outcomes, and comparison to influenza. JACC Clin Electrophysiol. 2021;7(09):1120–1130. doi: 10.1016/j.jacep.2021.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lip G YH, Genaidy A, Tran G, Marroquin P, Estes C. Incident atrial fibrillation and its risk prediction in patients developing COVID-19: a machine learning based algorithm approach. Eur J Intern Med. 2021;91:53–58. doi: 10.1016/j.ejim.2021.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Romiti G F, Corica B, Lip G YH, Proietti M. Prevalence and impact of atrial fibrillation in hospitalized patients with COVID-19: a systematic review and meta-analysis. J Clin Med. 2021;10(11):10. doi: 10.3390/jcm10112490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function . Bikdeli B, Madhavan M V, Jimenez D. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75(23):2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Emren Z Y, Şenöz O, Erseçgin A, Emren S V.Evaluation of bleeding rate and time in therapeutic range in patients using warfarin before and during the COVID-19 pandemic-warfarin treatment in COVID-19Clin Appl Thromb Hemost 2021;27:10760296211021495 [DOI] [PMC free article] [PubMed]
- 193.Papakonstantinou P E, Borovac J A, Gąsecka A. Anticoagulation therapy in non-valvular atrial fibrillation in the COVID-19 era: is it time to reconsider our therapeutic strategy? Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Li X, Zuo C, Lu W. Evaluation of Remote pharmacist-led outpatient service for geriatric patients on rivaroxaban for nonvalvular atrial fibrillation during the COVID-19 pandemic. Front Pharmacol. 2020;11:1275. doi: 10.3389/fphar.2020.01275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Global COVID-19 Thrombosis Collaborative Group . Bikdeli B, Madhavan M V, Gupta A. Pharmacological agents targeting thromboinflammation in COVID-19: review and implications for future research. Thromb Haemost. 2020;120(07):1004–1024. doi: 10.1055/s-0040-1713152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.GeroCovid Working Group Fumagalli S, Trevisan C, Del Signore S.COVID-19 and atrial fibrillation in older patients: does oral anticoagulant therapy provide a survival benefit?-An insight from the GeroCovid RegistryThromb Haemost2021 [DOI] [PubMed]
- 197.Denas G, Gennaro N, Ferroni E. Reduction in all-cause mortality in COVID-19 patients on chronic oral anticoagulation: a population-based propensity score matched study. Int J Cardiol. 2021;329:266–269. doi: 10.1016/j.ijcard.2020.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Nadkarni G N, Lala A, Bagiella E. Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol. 2020;76(16):1815–1826. doi: 10.1016/j.jacc.2020.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Rivera-Caravaca J M, Buckley B JR, Harrison S L. Direct-acting oral anticoagulants use prior to COVID-19 diagnosis and associations with 30-day clinical outcomes. Thromb Res. 2021;205:1–7. doi: 10.1016/j.thromres.2021.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Talasaz A H, Sadeghipour P, Kakavand H. Recent randomized trials of antithrombotic therapy for patients with COVID-19: JACC state-of-the-art review. J Am Coll Cardiol. 2021;77(15):1903–1921. doi: 10.1016/j.jacc.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.ATTACC Investigators ; ACTIV-4a Investigators ; REMAP-CAP Investigators . Lawler P R, Goligher E C, Berger J S. Therapeutic anticoagulation with heparin in noncritically ill patients with Covid-19. N Engl J Med. 2021;385(09):790–802. doi: 10.1056/NEJMoa2105911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Bikdeli B, Talasaz A H, Rashidi F.Intermediate-dose versus standard-dose prophylactic anticoagulation in patients with COVID-19 admitted to the intensive care unit: 90-day results from the INSPIRATION randomized trialThromb Haemost2021 [DOI] [PubMed]
- 203.INSPIRATION Investigators . Sadeghipour P, Talasaz A H, Rashidi F. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021;325(16):1620–1630. doi: 10.1001/jama.2021.4152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.ACTION Coalition COVID-19 Brazil IV Investigators Lopes R D, de Barros E Silva P GM, Furtado R HM.Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial Lancet 2021397(10291):2253–2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Scientific Reviewer Committee . Gerotziafas G T, Catalano M, Theodorou Y. The COVID-19 pandemic and the need for an integrated and equitable approach: an international expert consensus paper. Thromb Haemost. 2021;121(08):992–1007. doi: 10.1055/a-1535-8807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Ford G A, Hargroves D, Lowe D. Targeted atrial fibrillation (AF) detection in COVID-19 vaccination clinics. Eur Heart J Qual Care Clin Outcomes. 2021;7(06):526–528. doi: 10.1093/ehjqcco/qcab061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Scientific Reviewer Committee . Elalamy I, Gerotziafas G, Alamowitch S. SARS-CoV-2 vaccine and thrombosis: an expert consensus on vaccine-induced immune thrombotic thrombocytopenia. Thromb Haemost. 2021;121(08):982–991. doi: 10.1055/a-1499-0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


