Abstract
Complex perianal Crohn's disease (CD) remains a challenging problem. Fecal stream is thought to be a trigger of disease progression in patients with CD. In patients with refractory perianal CD, diversion of fecal stream is sometimes required to alleviate clinical symptoms when medical and local surgical management are unsuccessful. Several studies evaluated the outcomes of fecal diversion for complex perianal CD. After fecal diversion, the majority of patients achieved early clinical response, but the prospect of restoring bowel continuity was low (approximately 20%). Nearly half of the patients eventually required proctectomy. A number of studies attempted to identify predictive factors for the outcomes of fecal diversion. Only rectal involvement was associated with unsuccessful restoration of bowel continuity. Biologic therapy did not seem to improve the efficacy of fecal diversion, although the evidence level was low because of insufficient data or methodological limitations. Based on these results, fecal diversion may be useful in alleviating clinical symptoms related to severe perianal CD and avoiding immediate proctectomy. The impact of biologic therapy on the outcomes of fecal diversion should be further investigated.
Keywords: Crohn's disease, perianal Crohn's disease, fecal diversion, proctectomy, biologic therapy
Severe perianal Crohn's disease (CD) remains a challenging problem. Management of perianal CD requires a multidisciplinary approach with a combination of medical therapy including antibiotics, immunosuppressants or biologics, and surgery. 1 Fecal stream is thought to be a trigger of disease progression in CD and, therefore, diversion of fecal stream is sometimes required to control disease when all other medical and local surgical management are unsuccessful. 2 A proportion of patients with complex perianal CD undergo fecal diversion with the hope that diversion of fecal stream may improve clinical symptoms and avoid the need for a major surgical intervention such as proctectomy. Fecal diversion can also be useful in patients with recurrent perianal sepsis or cases with perineal destruction and fecal incontinence, despite disease activity. The advantage of fecal diversion alone is that it is a relatively minor procedure, and after fecal diversion there is no risk of fecal incontinence or complications of proctectomy, such as dysuria, impotence, or a persistent perineal sinus. 3 Therefore, fecal diversion may be an attractive alternative to resectional surgery in selected patients. Several studies reported the outcomes of fecal diversion for refractory perianal CD. 4 5 6 7 8 9 10 11 12 13 14 15 16
In this review, we evaluated the outcomes of fecal diversion for complex perianal CD, including the rate of early response and restoration of bowel continuity after diversion, and the need for proctectomy. Further, predictive factors for the efficacy of fecal diversion were identified. To evaluate the impact of biologic therapy on the outcomes of fecal diversion, we separately reviewed the studies in the prebiological and biological era.
The Efficacy of Fecal Diversion for Complex Perianal CD
Studies in the Prebiological Era
A number of studies were conducted for the assessment of the outcomes of fecal diversion for refractory perianal CD before the era of biologics. 4 5 6 7 8 9 10 11 Yamamoto et al 10 reviewed 31 patients who underwent fecal diversion alone for complex perianal CD in the University of Birmingham between 1970 and 1997. The characteristics of the 31 patients are shown in Table 1 . The outcomes of fecal diversion are summarized in Fig. 1 . One patient died from Fournier's gangrene 1 month after fecal diversion. Twenty-five patients (81%) achieved early remission, and the other 6 patients (19%) failed to respond. Among the 25 early responders, 8 patients (26%) achieved complete remission and required no further surgery for perianal disease at a median duration of 81 months after fecal diversion. In contrast, 17 relapsed at a median duration of 23 months after the fecal diversion. Twenty-two patients required surgery at a median duration of 20 months after fecal diversion (2 patients after stoma closure): proctectomy in 21 and repeated drainage of anal sepsis in 1. At the end of the study, intestinal continuity has been restored in only 3 patients (10%). Stoma closure was performed at a median duration of 41 months after fecal diversion.
Table 1. Characteristics of 31 patients undergoing fecal diversion alone for complex perianal Crohn's disease (CD).
| Median (range) age at fecal diversion | 29 (14–80) y |
| Male:female | 14:17 |
| Median (range) duration of CD before fecal diversion | 12 (0–144) mo |
| The principal indications for fecal diversion | |
| Severe perianal sepsis | 13 patients (42%) |
| Recurrent deep anal ulcer | 3 patients (10%) |
| Complex anorectal fistula | 9 patients (29%) |
| Rectovaginal fistula | 6 patients (19%) |
| Surgery for perianal CD before fecal diversion | |
| Drainage of perianal sepsis | 12 patients (39%) |
| Seton fistulotomy | 6 patients (19%) |
| Medication at fecal diversion | |
| Corticosteroids | 13 patients (42%) |
| Site of concomitant CD | |
| Ileum alone | 3 patients (10%) |
| Ileocolonic region | 2 patients (6%) |
| Ileum and total colon | 1 patient (3%) |
| Total colon and rectum | 7 patients (23%) |
| Segmental colon and rectum | 10 patients (32%) |
| Type of fecal diversion | |
| Loop ileostomy | 27 patients (87%) |
| Loop colostomy | 4 patients (13%) |
Fig. 1.
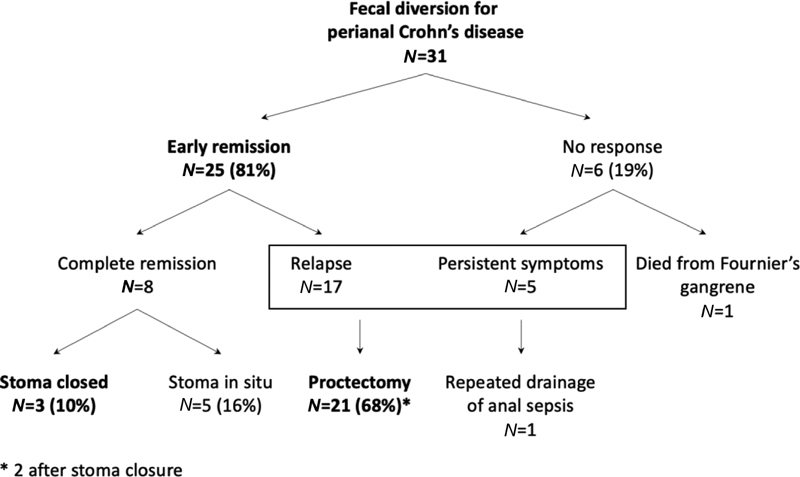
The outcomes of fecal diversion for refractory perianal Crohn's disease in the Birmingham study.
Harper et al 7 evaluated the outcomes of 32 split ileostomies on 29 patients with severe perianal CD. Perianal CD improved or healed in 23 patients with split ileostomies (72%), although it relapsed while diverted in 2 patients and after closure of split ileostomy in 6 patients. Seven of 12 rectovaginal fistulas healed initially but only remained healed in those patients without rectal involvement. Overall, 6 patients (21%) have normal bowel continuity, 8 (28%) have had proctocolectomies, and 15 (52%) are still defunctioned. The authors concluded that split ileostomy should be considered as an initial step in the management of intractable perianal CD. In the study by Régimbeau et al, 11 among 136 patients who were operated for refractory perianal CD over an 18-year period, 17 underwent fecal diversion. Mean follow-up duration after fecal diversion was 135 months (range, 20–328 months). Initial healing of perianal CD was observed in 11 patients (65%), and subsequently the stomas were closed after a mean duration of 14 months. The other 6 patients underwent proctectomy for persistent perianal CD. Three of the 11 patients with normal bowel continuity required secondary proctectomy for recurrence of perianal CD. Overall, 8 patients (47%) continued to have normal bowel continuity with a mean follow-up term of 124 months after stoma closure. In contrast, 9 patients (53%) underwent proctectomy with a permanent stoma.
Studies in the Era of Biologics
Several studies included patients receiving biologic therapy in the perioperative period of fecal diversion for perianal CD. 12 13 14 15 16 Uzzan et al 12 reported 3 cases of acute Crohn's colitis with severe endoscopic lesions and active perineal disease treated with an intensive medico-surgical strategy combining a defunctioning stoma with anti-tumor necrosis factor (TNF) treatment. All the patients were naive to anti-TNF agents. None could benefit from the intensive medico-surgical strategy to subsequently restore intestinal continuity. Hong et al 13 reviewed 21 patients who underwent fecal diversion for refractory perianal CD. At a median follow-up time of 22 months (range, 4–121 months), 4 patients (19%) had undergone stoma closure, 11 (52%) had had proctocolectomy, and 6 (29%) had a stoma in situ. Eleven patients (52%) were treated with infliximab. In this group with infliximab therapy, 4 patients (36%) underwent proctocolectomy and 2 (18%) had intestinal continuity restored.
In the study by Sauk et al, 14 49 patients underwent fecal diversion for perianal CD between 1991 and 2011 at a tertiary referral center. Forty-three (88%) of the 49 patients received biologic therapy before and after fecal diversion. Fifteen patients (31%) restored bowel continuity during the study follow-up period. Ten (67%) of the 15 patients who had restored bowel continuity required an additional procedure to divert the fecal stream. Of 5 patients maintaining bowel continuity, 3 patients required further procedures to alleviate sepsis. Gu et al 15 reported the outcomes of 138 patients who underwent fecal diversion for severe perianal CD between 1994 and 2012. Seventy-seven patients (56%) received anti-TNF therapy. Thirty patients (22%) achieved stoma closure, 45 (33%) had a stoma with the rectum left in situ, and 63 (45%) required proctectomy with a permanent stoma with a mean follow-up of 5.7 years. In the study by Martí-Gallostra et al, 16 76 patients underwent fecal diversion (57 patients with biologic therapy) for colonic and perianal CD between 2003 and 2011. Fifteen (20%) of the 76 patients achieved early clinical response, and 31 (41%) overall response. At the end of the study, restoration of bowel continuity was achieved in 20 patients (27%).
Overall Outcomes of Fecal Diversion
The summary of the main studies investigating the outcomes of fecal diversion for complex perineal CD is presented in Table 2 . Based on these results in both studies during the prebiological and biological era, 4 5 6 7 8 9 10 11 12 13 14 15 16 we can conclude that fecal diversion improves clinical symptoms in the majority of patients with complex perianal CD, but the prospect of bowel restoration after diversion is low (around 20%). Further, nearly half of the patients eventually required proctectomy with a permanent stoma for severe perianal disease. Biologic therapy did not seem to improve the outcomes (restoration of bowel continuity) of fecal diversion, although the level of evidence obtained from the previous studies was low because of insufficient data or methodological limitations. 12 13 14 15 16
Table 2. The outcomes of fecal diversion for complex perianal Crohn's disease in major studies.
| Author (Year) | Location of study | No. of patients | Follow-up duration (mo) | Clinical response | Restoration of bowel continuity | Proctectomy | Predictive factors for the outcomes |
|---|---|---|---|---|---|---|---|
| Studies in the prebiological era | |||||||
| Yamamoto et al 10 (2000) | Birmingham, UK | 31 | 103 | 81% | 10% | 68% | None |
| Harper et al 7 (1982) | Oxford | 29 | 12-18 | 72% | 21% | 28% | Rectal involvement, intestinal activity |
| Régimbeau et al 11 (2001) | Paris | 17 | 135 | 65% | 47% | 53% | Rectal involvement |
| Studies in the era of biologics | |||||||
| Hong et al 13 (2011) | Melbourne | 21 (11 with infliximab) | 22 | 81% | 19% | 52% | None |
| Gu et al 15 (2015) | Cleveland | 138 (77 with biologics) | 68 | Not recorded | 22% | 45% | Rectal involvement, frequency of loose seton placement |
| Martí-Gallostra et al 16 (2017) | Oxford | 76 (57 with biologics) | 48 | 61% | 27% | 46% | Endoscopic or histological improvement in the colon |
Predictive Factors for the Outcomes of Fecal Diversion
Several studies attempted to identify predictive factors for the outcomes of fecal diversion for refractory perianal CD. 10 11 13 15 16 In the study by Yamamoto et al, 10 the following parameters were compared in patients with and without complete clinical remission after fecal diversion: age, sex, duration of CD, use of corticosteroids, smoking habit, concomitant CD, preoperative blood indices, and CD activity index. None of these parameters affected the outcomes. Régimbeau et al 11 found that only the presence of rectal involvement was the predictive factor for poor outcomes: 8/9 (89%) patients with rectal involvement versus 1/8 (13%) patients without rectal involvement required subsequent proctectomy (statistically significant).
Regarding the impact of biologic therapy on the outcomes, Hong et al 13 reported that the rate of restoration of bowel continuity after fecal diversion was not significantly different between patients treated with and without infliximab therapy. In the study by Gu et al, 15 univariate analysis indicated that concomitant colonic or rectal involvement, and an increased frequency of loose seton placement were significantly associated with unsuccessful outcomes (without restoration of bowel continuity). Multivariate analysis showed a significant association between the poor outcomes and concomitant rectal involvement (odds ratio [OR] 7.5, 95% confidence interval [CI] 2.4–33.4), one or two placements of a loose seton (OR 3.3, 95% CI 1.4–8.8), and more than two placements (OR 6.9, 95% CI 1.2–132.5). No specific medical therapy including biologic agents was associated with the outcomes (restoration of bowel continuity) after fecal diversion. Martí-Gallostra et al 16 found that patients with endoscopic or histological improvement in the colon after fecal diversion were associated with a higher rate of restoring bowel continuity compared with those without improvement (63% vs. 27%, p = 0.05). The chance of restoration of bowel continuity was identical (26%) in patients treated with and without biologic therapy.
In summary, only rectal involvement was associated with unsuccessful restoration of subsequent bowel continuity after diversion. Biologic therapy did not seem to a significant predictive factor, although further investigation is needed because of insufficient data or methodological limitations in the previous studies.
Meta-Analysis Evaluating the Efficacies of Fecal Diversion
Singh et al 17 analyzed 16 cohort studies (556 patients) evaluating the outcomes of fecal diversion for complex perianal CD. This meta-analysis found that 64% (95% CI 54–73%) of patients had early response after fecal diversion. Restoration of bowel continuity was attempted in 35% (95% CI 27–43%) of patients, and it was successful in only 17% (95% CI 12–23%). Of patients in whom intestinal restoration was attempted, 27% (95% CI 14–44%) required repeat diversion due to relapse of severe perianal CD. Overall, 42% (95% CI 33–51%) of patients required proctectomy after failure of fecal diversion. The authors also identified factors associated with the outcomes of fecal diversion (restoration of intestinal continuity). 17 There was no difference in the successful restoration of bowel continuity after fecal diversion in the prebiological or biological era (14% vs. 18%, not significant). The use of anti-TNF agents did not appear to be associated with the outcomes of fecal diversion. Absence of rectal involvement was the most consistent factor associated with successful restoration of bowel continuity.
Conclusion and Future Perspectives
Based on the results of previous studies, 4 5 6 7 8 9 10 11 12 13 14 15 16 after fecal diversion for refractory perianal CD, the majority of patients achieve early clinical response, but the prospect of restoring intestinal continuity is low (approximately 10–25%) in the long term. Many patients have a stoma in situ after fecal diversion or require proctectomy with a permanent stoma. It was reported that approximately half of the patients eventually required proctectomy for relapse of severe perianal CD. However, in previous studies, the number of included patients was small, and type and severity of perianal disease and follow-up duration are not consistent between the studies. Further large prospective studies are required to rigorously assess the efficacy of fecal diversion. At the moment, we do believe that fecal diversion may be useful in alleviating clinical symptoms related to severe perianal CD and avoiding immediate proctectomy. When proctectomy is eventually needed, the incidence of complication may be reduced by prior fecal diversion.
Regarding predictive factors for the efficacy of fecal diversion, only the presence of rectal involvement appeared to be a significant predictor. Rectal involvement with CD was associated with a lower chance of restoring bowel continuity. Biologic therapy did not seem to improve the outcomes of fecal diversion. But further research is warranted to evaluate the efficacy of biologic agents since it was not rigorously tested in the setting of the previous studies. Additionally, the efficacy of early combination therapy with immunosuppressive and biologic agents should be also evaluated. With appropriate medical treatment, restoration of bowel continuity may be more frequently achieved, and the need for proctectomy may be decreased after fecal diversion.
It appeared that patients rarely developed malignancy in the defunctioned large bowel including perianal region in the previous studies. 4 5 6 7 8 9 10 11 12 13 14 15 16 There is a theoretical risk of malignancy in the defunctioned intestine, particularly in the rectum and perianal region. 18 Although in our clinical practice its occurrence is not high, surveillance of the defunctioned anorectal region after fecal diversion is necessary. Patients with a high risk of malignancy from persistent perianal fistulas and strictures are advised to undergo subsequent proctectomy after fecal diversion. However, if medical therapy including biologic agents is markedly useful for alleviating inflammation of anorectal CD, the risk of developing malignancy may be decreased. Further research on this topic is warranted.
Acknowledgments
None.
Funding Statement
Funding The authors do not have any financial disclosures or conflict of interest. This research was not supported by any funding agency.
Footnotes
Conflict of Interest None declared.
References
- 1.Crohn's & Colitis Foundation of America, Inc . Schwartz D A, Ghazi L J, Regueiro M. Guidelines for the multidisciplinary management of Crohn's perianal fistulas: summary statement. Inflamm Bowel Dis. 2015;21(04):723–730. doi: 10.1097/MIB.0000000000000315. [DOI] [PubMed] [Google Scholar]
- 2.Burke J P. Role of fecal diversion in complex Crohn's disease. Clin Colon Rectal Surg. 2019;32(04):273–279. doi: 10.1055/s-0039-1683916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamamoto T, Bain I M, Allan R N, Keighley M R. Persistent perineal sinus after proctocolectomy for Crohn's disease. Dis Colon Rectum. 1999;42(01):96–101. doi: 10.1007/BF02235190. [DOI] [PubMed] [Google Scholar]
- 4.McIlrath D C. Diverting ileostomy or colostomy in the management of Crohn's disease of the colon. Arch Surg. 1971;103(02):308–310. doi: 10.1001/archsurg.1971.01350080224035. [DOI] [PubMed] [Google Scholar]
- 5.Burman J H, Thompson H, Cooke W T, Williams J A. The effects of diversion of intestinal contents on the progress of Crohn's disease of the large bowel. Gut. 1971;12(01):11–15. doi: 10.1136/gut.12.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Orkin B A, Telander R L. The effect of intra-abdominal resection or fecal diversion on perianal disease in pediatric Crohn's disease. J Pediatr Surg. 1985;20(04):343–347. doi: 10.1016/s0022-3468(85)80216-5. [DOI] [PubMed] [Google Scholar]
- 7.Harper P H, Kettlewell M G, Lee E C. The effect of split ileostomy on perianal Crohn's disease. Br J Surg. 1982;69(10):608–610. doi: 10.1002/bjs.1800691017. [DOI] [PubMed] [Google Scholar]
- 8.Grant D R, Cohen Z, McLeod R S. Loop ileostomy for anorectal Crohn's disease. Can J Surg. 1986;29(01):32–35. [PubMed] [Google Scholar]
- 9.Edwards C M, George B D, Jewell D P, Warren B F, Mortensen N J, Kettlewell M G. Role of a defunctioning stoma in the management of large bowel Crohn's disease. Br J Surg. 2000;87(08):1063–1066. doi: 10.1046/j.1365-2168.2000.01467.x. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto T, Allan R N, Keighley M R.Effect of fecal diversion alone on perianal Crohn's disease World J Surg 200024101258–1262., discussion 1262–1263 [DOI] [PubMed] [Google Scholar]
- 11.Régimbeau J M, Panis Y, Cazaban L. Long-term results of faecal diversion for refractory perianal Crohn's disease. Colorectal Dis. 2001;3(04):232–237. doi: 10.1046/j.1463-1318.2001.00250.x. [DOI] [PubMed] [Google Scholar]
- 12.Uzzan M, Stefanescu C, Maggiori L, Panis Y, Bouhnik Y, Treton X. Case series: does a combination of anti-TNF antibodies and transient ileal fecal stream diversion in severe Crohn's colitis with perianal fistula prevent definitive stoma? Am J Gastroenterol. 2013;108(10):1666–1668. doi: 10.1038/ajg.2013.188. [DOI] [PubMed] [Google Scholar]
- 13.Hong M K, Craig Lynch A, Bell S. Faecal diversion in the management of perianal Crohn's disease. Colorectal Dis. 2011;13(02):171–176. doi: 10.1111/j.1463-1318.2009.02092.x. [DOI] [PubMed] [Google Scholar]
- 14.Sauk J, Nguyen D, Yajnik V. Natural history of perianal Crohn's disease after fecal diversion. Inflamm Bowel Dis. 2014;20(12):2260–2265. doi: 10.1097/MIB.0000000000000216. [DOI] [PubMed] [Google Scholar]
- 15.Gu J, Valente M A, Remzi F H, Stocchi L. Factors affecting the fate of faecal diversion in patients with perianal Crohn's disease. Colorectal Dis. 2015;17(01):66–72. doi: 10.1111/codi.12796. [DOI] [PubMed] [Google Scholar]
- 16.Martí-Gallostra M, Myrelid P, Mortensen N, Keshav S, Travis S P, George B. The role of a defunctioning stoma for colonic and perianal Crohn's disease in the biological era. Scand J Gastroenterol. 2017;52(03):251–256. doi: 10.1080/00365521.2016.1205127. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Ding N S, Mathis K L. Systematic review with meta-analysis: faecal diversion for management of perianal Crohn's disease. Aliment Pharmacol Ther. 2015;42(07):783–792. doi: 10.1111/apt.13356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yamamoto T, Kotze P G, Spinelli A, Panaccione R. Fistula-associated anal carcinoma in Crohn's disease. Expert Rev Gastroenterol Hepatol. 2018;12(09):917–925. doi: 10.1080/17474124.2018.1500175. [DOI] [PubMed] [Google Scholar]


