Abstract
Objective
To systematically evaluate the effect and safety of compound Kushen injection (CKI) as an add-on treatment on the treatment for breast cancer.
Methods
We searched eight major electronic databases from their inception to November 1, 2021, for randomized clinical trials (RCTs) comparing CKI plus chemotherapy with chemotherapy alone. Primary outcomes included objective response rate (ORR) and disease control rate (DCR), health-related quality of life (HRQoL), progression-free survival (PFS), and overall survival (OS). Secondary outcomes included adverse drug reactions (ADRs) and tumor marker level. We used Cochrane's RevMan 5.3 for data analysis. The GRADEpro was used to appraise the certainty of evidence. Trial sequential analysis (TSA) was applied to estimate the required sample size in a meta-analysis and test the robustness of the current results.
Results
Thirty RCTs with 2556 participants were totally included. CKI plus chemotherapy showed significant effects in increasing ORR (RR 1.30, 95%CI [1.18, 1.43], I2 = 27%, n = 1694), increasing DCR (RR 1.21, 95%CI [1.15, 1.28], I2 = 16%, n = 1627), increasing HRQol as measured by Karnofsky Performance Scale (KPS) score improvement rate (RR 1.42, 95% CI [1.26, 1.61], I2 = 37%, n = 1172), increasing the PFS (MD 2.24 months, 95%CI [1.26, 3.22], n = 94) and the OS (MD 2.24 months, 95%CI [1.45, 3.43], n = 94), compared to chemotherapy alone. The results showed that CKI plus chemotherapy had a lower risk of ADRs than that of chemotherapy alone group. The certainty of evidence of the included trials was generally low to very low. TSA for ORR and KPS score improvement rate demonstrated that the current results reached a sufficient power regarding both numbers of trials and participants.
Conclusions
Low certainty of evidence suggested that the combination of CKI and conventional chemotherapy appeared to improve ORR, DCR, and KPS score in breast cancer patients. Conclusions about PFS and OS could not be drawn due to lack of evidence. Additionally, CKI appeared to relieve the risk of ADRs in patients with breast cancer receiving chemotherapies. However, due to weak evidence, the findings should be further confirmed in large and rigorous trials.
1. Introduction
Breast cancer is one of the most common cancers experienced by women and is reported as the leading cause of cancer-related death in women around the world [1, 2]. The incidence rate increased significantly in the last decade, with more than 1 million women newly diagnosed with breast cancer every year [3]. Therefore, breast cancer has been a serious burden for societies in the world. Current treatments for breast cancer mainly included surgery, chemotherapy, radiotherapy, hormone, and immunological therapy [4]. However, it was reported that these treatments usually bring about significant side effects, including cardiac toxicity, gastrointestinal toxicity, and other multiple adverse drug reactions [5–7]. All these seriously affected the patients' quality of life, work, and other health outcomes. Therefore, finding alternative options to alleviate the side effects of conventional therapies and improve the clinical efficacy are needed and expected.
Traditional Chinese medicine (TCM), as an add-on treatment, has been increasingly used for the treatment of tumors [8, 9]. Among TCM treatments, compound Kushen injection (CKI) (drug approval number: Z14021231, China food and Drug Administration), an important Chinese herb injection, is used extensively for multiple malignant tumors in China nowadays. Especially in the treatment of breast cancer, it has become increasingly popular TCM injection [10, 11]. CKI is composed of the extracts from Kushen (Radix Sophorae Flavescentis) and Baituling (Rhizoma Smilacis Glabrae). Their main active ingredients are matrine, oxymatrine, sophocarpine, and sophoridine, which have been reported to exhibit a variety of pharmacological activities such as a good synergistic antitumor effect [11, 12]. Furthermore, previous studies have revealed that CKI can inhibit the proliferation, invasion, and migration of breast cancer cells through different mechanisms [12, 13].
Some clinical trials have been conducted to investigate the effect of CKI on treating breast cancer. The systematic reviews in 2018 and 2019 [14, 15] involving 24 trials and 18 trials, respectively, showed that CKI had a beneficial effect on improving the working status of patients with breast cancer, and the combination therapy also had a lower risk of adverse drug reactions (ADR) (such as neutropenia, thrombocytopenia, and nausea/vomiting). However, some nonrandomized controlled trials were mistakenly included for analysis, and the results demonstrated that the available data provided insufficient evidence to support the use of CKI for the treatment of breast cancer. On the other hand, the studies included in the systematic review did not report on important outcomes such as the disease control rate (DCR) and long-term survival, which increased the limitation of interpretation and application of the findings. Another recent systematic review [16] involving 16 trials published in 2019 summarized evidence of CKI for breast cancer. The pooled results indicated that the combination of CKI and chemotherapy might improve performance status and reduce ADRs among postoperative patients with breast cancer, but might not improve clinical response rate. In addition, the review finally included trials from 2009 to 2017 and has not been updated since relevant databases were searched from their inception to 2017. Since then, there have been many studies on the effect of CKI on breast cancer. Therefore, this review aims to systematically collect all relevant RCTs to further confirm whether CKI combined with chemotherapy can improve the tumor responses and survivals and reveal its safety.
2. Methods
The protocol of this study has been registered at PROSPERO (NO: CRD42020216652). This systematic review was reported in accordance with PRISMA guidelines [17], and we followed the methods of Cochrane methodological guidelines and a previous study published by B.Y. Lai et al. [18, 19].
2.1. Inclusion Criteria
2.1.1. Type of Study
This review included randomized clinical trials (RCTs) enrolling participants with breast cancer.
2.1.2. Type of Participants
Type of participants included women who were diagnosed with breast cancer by histopathological and cytological diagnostic criteria, regardless of their age, race, and disease TNM stage.
2.1.3. Type of Interventions
The experimental groups were treated with CKI plus chemotherapy, and the control groups were treated with chemotherapy alone.
2.1.4. Type of Outcomes
Primary outcomes were tumor response (including objective response rate (ORR) and disease control rate (DCR)), health-related quality of life (HRQoL) and long-term survival. For the review, tumor response should be measured using standard evaluation criteria (WHO guidelines or RECIST) and reported as either complete response, partial response, or stable disease or progressive disease [20, 21]. ORR includes participants measured by complete response and partial response. DCR includes participants measured by complete response, partial response, and stable disease. HRQoL could be measured by any recognized evaluation tool. We also considered “Karnofsky Performance Scale (KPS) score improvement” defined as KPS score of more than 10 points increase after treatment as an indicator of HRQoL [16, 21]. Long-term survival was measured by overall survival (OS) or progression-free survival (PFS). Secondary outcomes included adverse drug reactions (ADRs) and tumor marker level. ADRs were summarized according to common terminology criteria for adverse events version (CTCAE) (i.e., the hematotoxicity, liver or renal injury, nausea and vomiting, oral mucositis, and alopecia) [22]. The decrease of tumor marker level' was defined as the tumor marker level decreased more than 25%, or the result recovered from abnormal range to normal range.
Studies were excluded if (1) data could not be extracted; (2) studies where the outcome assessment was not clearly stated; and (3) duplicates.
2.2. Search Strategy
We systematically searched major electronic databases (including PubMed, Embase Database, Cochrane library, Web of science, Chinese Biomedical Literature Database (SinoMed), China National Knowledge Infrastructure (CNKI), Wanfang Database and China Science Technology Journal Database (VIP)) from their inception to November 1, 2021. Clinical trial registration platforms (including ClinicalTrials.gov (http://www.clinicaltrials.gov) and Chinese Clinical Trial Registry (http://www.chictr.org/cn)) were also searched for potentially eligible studies. The search terms included “matrine injection,” “compound Kushen injection,” “yan shu injection,” “radix sophorae flavescentis injection,” and “breast cancer.” For example, PubMed was searched with the following search strategy: ((((compound kushen injection [Title/Abstract]) OR (matrine injection [Title/Abstract])) OR (yan shu injection [Title/Abstract])) OR (radix sophorae flavescentis injection [Title/Abstract])) AND (breast cancer [Title/Abstract]). English and Chinese language publications were included.
2.3. Study Selection and Data Extraction
Two authors independently selected the studies according to the eligibility criteria. We conducted data extraction using a self-developed data extraction form, and the extracted data mainly included first authors and year of publication, sample size, characteristics of participants, information of randomization, details of intervention, and outcome assessments. If the necessary data were not available in the publication papers, further information was obtained by contacting the first or corresponding author. Any disagreement regarding study selection and data extraction was resolved through discussion.
2.4. Assessment of Risk of Bias
The risk of bias of eligible trials was assessed according to the criteria from the Cochrane Handbook for Systematic Reviews of Interventions [18]. Criteria included the following seven domains: random sequence generation, allocation concealment, blinding (including blinding of participants, personnel, and outcome assessors), incomplete outcome data, selective reporting, and other bias (e.g., the comparison of the baseline information). The trials were categorized to high risk of bias when at least one of the items being assessed as “high.” A judgment of low risk of bias of trials was made when all the items met the criteria, and the trial was categorized to unclear risk of bias if insufficient information was obtained for assessment. Any disagreements were resolved by discussion. Finally, the certainty of evidence across studies of each important outcome in this review was appraised using the GRADEpro tool (https://gradepro.org/).
2.5. Data Analysis
We used RevMan software 5.3 provided by the Cochrane collaboration to perform statistical analyses. The binary outcomes were expressed as risk ratio (RR) with 95% confidence interval (CI), and the continuous outcomes were expressed as mean difference (MD) with 95% CI. We used the I2 test to detect statistical heterogeneity in effect sizes between studies, and an I2 >50% indicated the possibility of statistical heterogeneity among the studies [23]. Meta-analysis was performed only when there was no significant difference between participants and had acceptable statistical heterogeneity (I2≤75%). Considering potential sources of clinical heterogeneity, the random-effect model (REM) was adopted for meta-analysis in this review. When I2 >75%, meta-analysis would not be conducted, and individual study results were given, respectively [23]. Then subgroup analysis was performed by disease TNM stage or tumor responses criteria if enough randomized trials were identified and data were available. Furthermore, to estimate the required sample size in a meta-analysis and to test the robustness of the current results, the trial sequential analysis (TSA) was performed if there were more than eight studies in a meta-analysis [24].
3. Results
3.1. Study Selection
A total of 413 studies were identified from eight electronic databases. First, 165 duplicates were excluded, and then 248 were excluded by abstracts reading. Full texts of 54 articles were screened according to the eligibility criteria. Thirty RCTs were included finally. The study searching and selecting process is shown in Figure 1.
Figure 1.
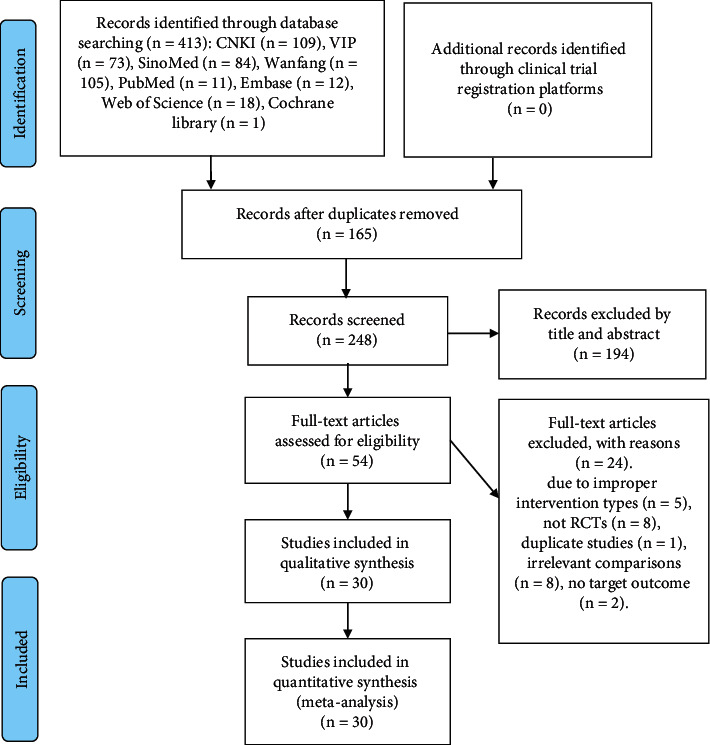
Study selection flow diagram.
3.2. Study Characteristics
Thirty RCTs [25–54] involving 2556 participants were included in this review. The sample size varied from 24 to 130 participants, with an average of 85 patients per trial. The mean age of participants was 46.48 ± 6.67 years old based on 14 trials [31, 32, 35, 37, 39, 42, 43, 46, 48–53] reporting age. The dose of CKI was 12–30 ml each time. The treatment time per cycle was from 6 days to 21 days, and the treatment cycle was 2–8 cycles of intravenous injection. None of the trials specified the calculation of sample size. All trials were carried out in China from 2007 to 2020. The characteristics of the included trials are shown in Table 1.
Table 1.
Characteristics of included RCTs on compound Kushen injection for breast cancer.
| Study ID | Sample (T/C) | Age (y) | Course of disease (months) | Stage | Control/chemotherapies | Intervention (CKI) | Duration | Tumor responses criteria | Outcome measures |
|---|---|---|---|---|---|---|---|---|---|
| Adlt YS 2016 [25] | T:56 | T:34–68 | NR | I∼II | AC1 | CT + CKI 20 mL, qd,21d | 6 cycles | Unclear | PFS, OS, CEA/CA153 level |
| C:62 | C:30–65 | ||||||||
|
| |||||||||
| Cao W 2012 [26] | T:52 | T:42–70 | NR | II∼III | C1AF | CT + CKI 20 mL, qd,10d | 6 cycles | Unclear | ADRs |
| C:52 | C:45–68 | ||||||||
|
| |||||||||
| Chen LJ 2010 [27] | T:35 | T: 39–71 | NR | II∼III | TC1A | CT + CKI 20 mL, qd,14d | 6 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:32 | C: 35–68 | ||||||||
|
| |||||||||
| Dai YN 2019 [28] | T:44 | T:30–67 | NR | II∼III | TC1A | CT + CKI 20 mL, qd,6d | 8 cycles | Unclear | ORR, DCR, HRQoL-KPS, ADRs, CEA/CA153 level |
| C:44 | C:30–67 | ||||||||
|
| |||||||||
| Dai YN 2020 [29] | T:50 | T:31–67 | NR | II∼III | TC1A | CT + CKI 20 mL, qd,6d | 8 cycles | Unclear | ORR, DCR |
| C:50 | C:30–66 | ||||||||
|
| |||||||||
| Huang YH 2012 [30] | T:20 | T:33–75 | NR | III∼IV | TA | CT + CKI 20 mL, qd,14d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:20 | C:33–75 | ||||||||
|
| |||||||||
| Li LY 2016 [31] | T:34 | T:45.6 ± 4.2 | T:5.2 ± 2.1 y | III∼IV | TA | CT + CKI 20 mL, qd,14d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:34 | C:46.5 ± 3.1 | C:6.2 ± 3.1 y | |||||||
|
| |||||||||
| Li YX 2012 [32] | T:30 | T:49.3 ± 0.9 | NR | II∼IV | C1EF | CT + CKI 15 mL, qd,14d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:30 | C:49.3 ± 0.9 | ||||||||
|
| |||||||||
| Ma YQ 2011 [33] | T:32 | T:28–63 | T:10m | III∼IV | TC1A | CT + CKI 20 mL, qd,21d | 3 cycles | Unclear | HRQoL-KPS, ADRs |
| C:31 | C:30–62 | C:11m | |||||||
|
| |||||||||
| Mao WJ 2018 [34] | T:39 | T:40–70 | NR | NR | TC1A | CT + CKI 15 mL, qd,12d | 8 cycles | RECIST | ORR, DCR, ADRs, CEA/CA153 level |
| C:39 | C:40–70 | ||||||||
|
| |||||||||
| Niu YL 2017 [35] | T:40 | T:50.02 ± 12.11 | NR | NR | GP | CT + CKI 20 mL, qd,14d | 3 cycles | Unclear | HRQoL-KPS |
| C:40 | C:48.35 ± 12.23 | ||||||||
|
| |||||||||
| Qi JH 2012 [36] | T:57 | T:35–75 | NR | IV | TP | CT + CKI 20 mL, qd,14d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:52 | C:35–75 | ||||||||
|
| |||||||||
| Qian XY 2017 [37] | T:23 | T:46.6 ± 5.2 | NR | IV | GP | CT + CKI 20 mL, qd,10d | 2 cycles | RECIST | ORR, DCR, HRQoL-KPS, ADRs |
| C:23 | C:47.3 ± 5.9 | ||||||||
|
| |||||||||
| Ren JH 2010 [38] | T:62 | T:39–65 | NR | II∼III | C1AF | CT + CKI 30 mL, qd,15d | 6 cycles | Unclear | HRQoL-KPS, ADRs, CEA/CA153 level |
| C:60 | C:39–65 | ||||||||
|
| |||||||||
| Ren MY 2016 [39] | T:50 | T:50.34 ± 5.13 | NR | IV | TE | CT + CKI 20 mL, qd,10d | 2 cycles | WHO | ORR, DCR, ADRs |
| C:50 | C:50.19 ± 5.24 | ||||||||
|
| |||||||||
| Song RF 2009 [40] | T:64 | T:22–65 | NR | IV | NG | CT + CKI 20 mL, qd,20d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS |
| C:54 | C:24–63 | ||||||||
|
| |||||||||
| Sun X 2008 [41] | T:38 | T:28–69 | NR | IV | TA | CT + CKI 20 mL, qd,10d | 2 cycles | Unclear | ORR, DCR, HRQoL-KPS, ADRs |
| C:32 | C:28–69 | ||||||||
|
| |||||||||
| Sun XH 2019 [42] | T:41 | T:49.05 ± 7.29 | NR | II∼III | TEC1 | CT + CKI 20 mL, qd,7d | 3 cycles | WHO | ORR, DCR, ADRs, CEA/CA153 level |
| C:39 | C:49.69 ± 6.11 | ||||||||
| Wang J 2019 [43] | T:47 | T:47.2 ± 5.3 | NR | II∼III | TE | CT + CKI 20 mL, qd,10d | 2 cycles | UICC | ORR, DCR, HRQoL-BREF, PFS, OS, ADRs, CEA/CA153 level |
| C:47 | C:45.3 ± 4.9 | ||||||||
|
| |||||||||
| Wang L 2007 [44] | T:30 | T:28–65 | NR | NR | C1EF | CT + CKI 20 mL, qd,10d | 2–3 cycles | WHO | ORR, DCR, ADRs |
| C:30 | C:28–65 | ||||||||
|
| |||||||||
| Wei YH 2010 [45] | T:12 | T:35–65 | NR | NR | C1AF | CT + CKI 20 mL, qd,15d | 2 cycles | Unclear | HRQoL-KPS, ADRs |
| C:12 | C:35–65 | ||||||||
|
| |||||||||
| Xu N 2017 [46] | T:52 | T:42.4 ± 4.5 | NR | II∼III | C1AF | CT + CKI 20 mL, qd,21d | 6 cycles | RECIST | ORR, DCR, ADRs |
| C:52 | C:43.7 ± 5.3 | ||||||||
|
| |||||||||
| Xu HJ 2017 [47] | T:49 | T:28–75 | NR | II∼III | TC1A | CT + CKI 12 mL, qd,10d | 4 cycles | Unclear | HRQoL-KPS, ADRs |
| C:49 | C:26–76 | ||||||||
|
| |||||||||
| Yan J 2015 [48] | T:40 | T:52.3 ± 4.6 | NR | II∼III | TE | CT + CKI 12 mL, qd,14d | 2 cycles | WHO | ORR, DCR, HRQoL-KPS, ADRs |
| C:40 | C:52.5 ± 4.5 | ||||||||
|
| |||||||||
| Yang X 2013 [49] | T:30 | T:41.5 ± 10.29 | NR | III∼IV | TE | CT + CKI 20 mL, qd,21d | NR | RECIST | ORR, DCR, HRQoL-KPS, ADRs |
| C:30 | C:41.5 ± 10.29 | ||||||||
|
| |||||||||
| Yang H 2019 [50] | T:55 | T:44.1 ± 4.5 | NR | II∼III | TA | CT + CKI 20 mL, qd,7d | 6 cycles | WHO | ORR, DCR, ADRs |
| C:55 | C:43.5 ± 4.7 | ||||||||
|
| |||||||||
| Zhai XJ 2014 [51] | T:61 | T:42.7 ± 10.5 | NR | I∼III | C1AF | CT + CKI 20 mL, qd,21d | 6 cycles | Unclear | ADRs |
| C:62 | C:43.5 ± 11.2 | ||||||||
|
| |||||||||
| Zhang ZJ 2015 [52] | T:65 | T:43.2 ± 17.9 | NR | I∼II | AC1 | CT + CKI 12 mL,21d | 6 cycles | Unclear | HRQoL-KPS, ADRs |
| C:65 | C:43.2 ± 17.9 | ||||||||
|
| |||||||||
| Zhang GY 2014 [53] | T:36 | T:46.25 ± 5.29 | T:8.25 ± 2.28 | NR | TC1A | CT + CKI 30 mL, qd,14d | 6 cycles | RECIST | ORR, DCR, HRQoL-KPS, ADRs |
| C:36 | C:46.36 ± 5.41 | C:8.16 ± 2.3 | |||||||
|
| |||||||||
| Zhang JZN 2018 [54] | T:45 | T:34–72 | NR | IV | GC2 | CT + CKI 20 mL, qd,10d | 4 cycles | RECIST | ORR, DCR, HRQoL-KPS, ADRs, CEA/CA153 level |
| C:45 | C:33–71 | ||||||||
Note. T: compound KuShen injection group; C: control group; d: day; y: year; NR: not reported. ∗: chemotherapy regimens: A: ADM (doxorubicin); F: 5-fluorouracil; C1: CTX (cyclophasphamide); T: docetaxel; E: EPI (epirupicin); G: GEM (gemcitabline); P: paclitaxel; N: NVB (vinorelbine); C2: CBP (carboplatin). HRQoL-KPS: health-related quality of life measured by Karnofsky Performance scale; HRQoL-BREF: health-related quality of life measured by QoL-BREF scale.
3.3. Methodological Quality in Included Trials
According to the Cochrane risk of bias tool, the included trials were found to be high risk of bias due to inadequate reporting of the methodological components. Only 9 trials [35–37, 42, 46, 50–53] described that the method of randomization used was assessed as having low risk of bias. It was not possible to blind the participants or personnel as CKI was only used in the experimental group. No trials reported the information of allocation concealment and the blinding of outcome assessment, so the risk of bias on them was judged as “unclear.” Two trials [37, 42] reported participant dropout rate, and the reasons were regarded as low risk of attrition bias. The other trials did not specify the dropout and were all judged as unclear risk of attrition bias. For selective outcome reporting bias, one trial [25] was assessed as high risk of selective reporting bias since it reported primary outcome of long-term survival but failed to report the detailed information. The remaining trials were assessed as having unclear risk of selective reporting bias due to unavailable trial registry. Other bias was assessed by comparability between groups on baseline data, and all trials had baseline comparability. The methodological quality of the included studies is presented in Figures 2 and 3.
Figure 2.
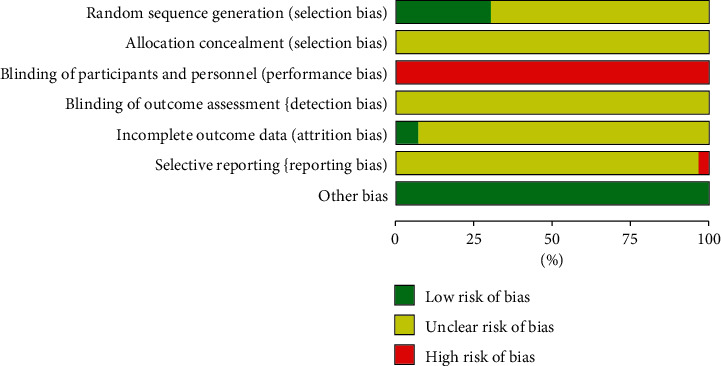
Risk of bias graph.
Figure 3.
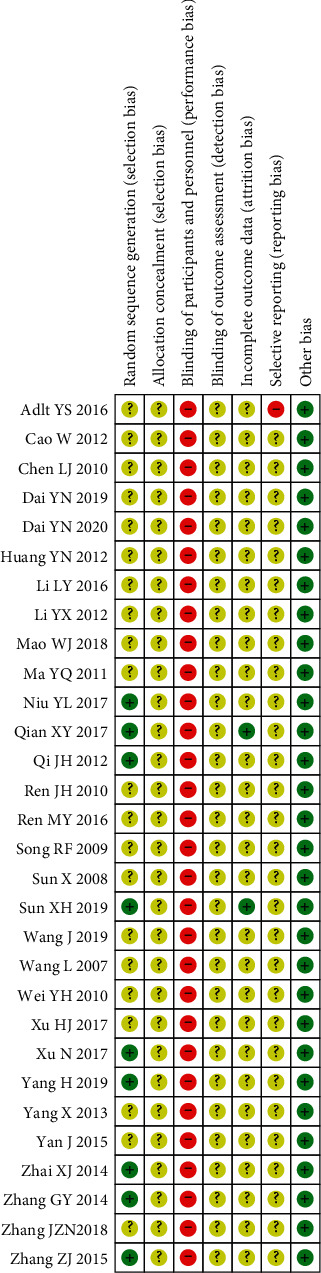
Risk of bias summary.
3.4. Effect Estimates
3.4.1. Primary Outcomes
(1) The Tumor Responses. The pooled data of 21 trials [27–32, 34, 36, 37, 39–44, 46, 48–50, 53, 54] showed a higher ORR and DCR in CKI plus chemotherapy group than that of chemotherapy alone, and the difference was statistically significant (RR 1.30, 95%CI [1.18, 1.43], I2 = 27%, n = 1694, 21 trials, Figure 4) and (RR 1.21, 95%CI [1.12, 1.31], I2 = 71%, n = 1694, 21trials). To explore potential causes of the statistical heterogeneity in outcomes of DCR (I2 = 71%), we excluded one trial [27] that reported the same DCR result (100%) in CKI plus chemotherapy group and chemotherapy group, and the remaining trials showed that CKI could increase the DCR (RR 1.21, 95%CI [1.15, 1.28], I2 = 16%, n = 1627, 20 trials, Figure 5), but the I2 value was reduced to 16%. Thus, we think heterogeneity in this outcome might be caused by participants' baseline conditions or reporting bias.
Figure 4.
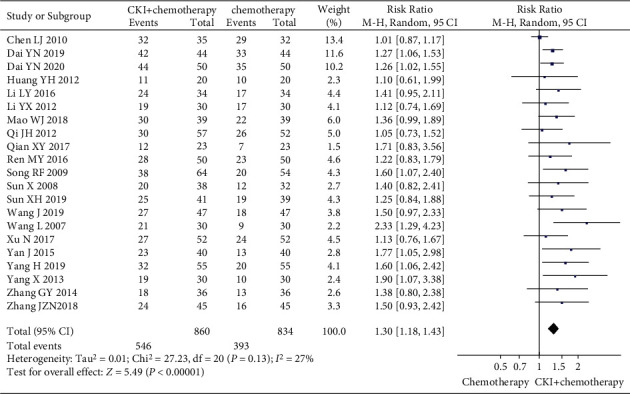
Meta-analysis of ORR of CKI plus chemotherapy for the treatment of breast cancer.
Figure 5.
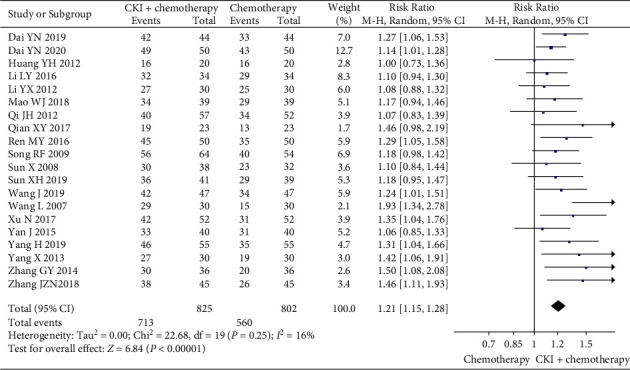
Meta-analysis of DCR of CKI plus chemotherapy for the treatment of breast cancer.
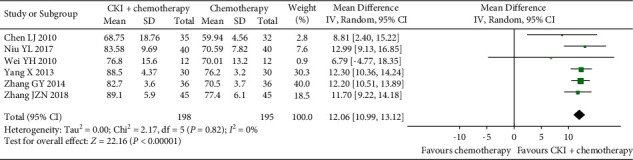
(2) HRQoL. According to the predefined criteria for KPS score improvement, HRQoL was reported as KPS score improvement in 14 trials [28, 30–33, 36–38, 40–42, 47, 48, 52]. A pooled analysis of 14 trials showed a higher KPS score improvement rate in the CKI plus chemotherapy group than that of chemotherapy group alone, and the difference was statistically significant (RR 1.42, 95% CI [1.26, 1.61], I2 = 37%, n = 1172, 14 trials, Figure 6). In addition, six trials compared CKI plus chemotherapy with chemotherapy alone [27, 35, 45, 49, 53, 54], and the combination therapy group showed the better effect in improving HRQoL as measured by the KPS score (MD 12.06 score, 95%CI [10.99, 13.12], I2 = 0%, n = 393, 6 trials, Figure 7). Similarly, the result from another one trial [43] also showed that CKI plus chemotherapy was superior in improving HRQoL as measured by the QoL-BREF scale (MD 18.11 score, 95%CI [16.50, 18 270 19.72], n = 94, Table 2). No other measure of HRQoL was reported in any of the included trials.
Figure 6.
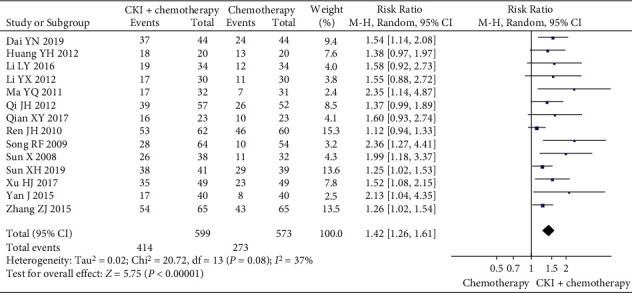
Meta-analysis of KPS score improvement rate of CKI plus chemotherapy for the treatment of breast cancer.
Figure 7.
Meta-analysis of KPS score of CKI plus chemotherapy for the treatment of breast cancer.
Table 2.
Effect estimates of compound Kushen injection for breast cancer.
| Outcomes and comparisons | Studies | Participants | Effect estimate (95%CI) REM | P value | Study ID references | |
|---|---|---|---|---|---|---|
| Compound Kushen injection plus chemotherapy versus chemotherapy alone | ||||||
| ORR | Stage II∼III | 7 | 656 | RR 1.31, [1.17, 1.46], I2 = 0% | P=0.002 | [28, 29, 42, 43, 46, 48, 50] |
| Stage IV | 6 | 533 | RR 1.33, [1.11, 1.60], I2 = 0% | P=0.002 | [36, 37, 39–41, 54] | |
|
| ||||||
| DCR | Stage II∼III | 7 | 656 | RR 1.20, [1.12, 1.28], I2 = 0% | P < 0.001 | [28, 29, 42, 43, 46, 48, 50] |
| Stage IV | 6 | 533 | RR 1.22, [1.11, 1.35], I2 = 0% | P < 0.001 | [36, 37, 39–41, 54] | |
|
| ||||||
| ORR | WHO criteria | 10 | 825 | RR 1.36, [1.18, 1.56], I2 = 2% | P < 0.001 | [30–32, 36, 39, 40, 42, 44, 48, 50] |
| RECIST criteria | 6 | 450 | RR 1.40, [1.16, 1.68], I2 = 0% | P < 0.001 | [34, 37, 46, 49, 53, 54] | |
|
| ||||||
| DCR | WHO criteria | 10 | 825 | RR 1.17, [1.08, 1.28], I2 = 30% | P < 0.001 | [30–32, 36, 39, 40, 42, 44, 48, 50] |
| RECIST criteria | 6 | 450 | RR 1.35, [1.21, 1.52], I2 = 0% | P < 0.001 | [34, 37, 46, 49, 53, 54] | |
|
| ||||||
| KPS score improvement rate | Stage II∼III | 5 | 468 | RR 2.93, [1.88, 4.56], I2 = 0% | P < 0.001 | [28, 38, 42, 47, 48] |
| Stage IV | 4 | 343 | RR 2.98, [1.88, 4.72], I2 = 0% | P < 0.001 | [36, 37, 40, 41] | |
|
| ||||||
| QoL-BREF score | 1 | 94 | MD 18.11, [16.50, 19.72] | P < 0.001 | [43] | |
| PFS | 1 | 94 | MD 2.24, [1.26, 3.22] | P < 0.001 | [43] | |
| OS | 1 | 94 | MD 2.24, [1.45, 3.43] | P < 0.001 | [43] | |
| ADRs | Leukocyte decrease | 15 | 1121 | RR 0.60, [0.5, 0.71], I2 = 40% | P < 0.001 | [27, 30–34, 36, 37, 39, 41, 42, 47, 48, 53, 54] |
| Platelet decrease | 9 | 750 | RR 0.41, [0.29, 0.58], I2 = 36% | P < 0.001 | [27, 28, 36, 37, 39, 42, 47, 53, 54] | |
| Liver injury | 13 | 1215 | RR 0.42, [0.31, 0.57], I2 = 26% | P < 0.001 | [26–28, 36, 37, 39, 42–44, 46, 50–52] | |
| Renal injury | 9 | 879 | RR 0.63, [0.46, 0.86], I2 = 0% | P=0.004 | [27, 28, 36, 37, 42, 46, 49–51] | |
| Nausea and vomiting | 14 | 1171 | RR 0.68, [0.59, 0.79], I2 = 43% | P < 0.001 | [26, 33, 34, 36, 37, 41, 43, 44, 46, 47, 49, 51, 53, 54] | |
| Diarrhea | 3 | 210 | RR 0.55, [0.35, 0.88], I2 = 0% | P < 0.001 | [26, 37, 49] | |
| Alopecia | 8 | 584 | RR 0.51, [0.39, 0.67], I2 = 32% | P < 0.001 | [27, 28, 33, 34, 36, 37, 49, 50, 53] | |
| Oral mucositis | 4 | 441 | RR 0.18, [0.07, 045], I2 = 0% | P < 0.001 | [26, 46, 50, 51] | |
| Tumor marker | Decrease rate of CEA | 3 | 336 | RR 1.19, [1.05, 1.35], I2 = 0% | P=0.007 | [25, 28, 52] |
| Decrease rate of CA153 | 2 | 206 | RR 1.15, [1.03, 1.27], I2 = 0% | P=0.009 | [25, 29] | |
Note: REM: random-effect models; CI: confidence intervals; MD: mean difference; RR: risk rate.
(3) Long-Term Survival. One trial [43] showed CKI plus chemotherapy was superior in increasing the PFS (MD 2.24 months, 95%CI [1.26, 3.22], n = 94, Table 2). Similarly, the result also showed CKI plus chemotherapy was superior in increasing the OS (MD 2.24 months, 95%CI [1.45, 3.43], n = 94, Table 2). The findings of another trial [25] were not finally summarized due to this trial reporting no detailed data on the PFS or the OS.
3.4.2. Secondary Outcomes
(1) Adverse Drug Reactions. The meta-analysis results showed that CKI plus chemotherapy group had a lower risk of leukocyte decrease (RR 0.60, 95%CI [0.5, 0.71], n = 1121, 15 trials), platelet decrease (RR 0.41, 95%CI [0.29, 0.58], n = 750, 9 trials), liver injury (RR 0.42, 95%CI [0.31, 0.57], n = 1215, 13 trials), renal injury (RR 0.59, 95%CI [0.43, 0.82], n = 879, 9 trials), nausea and vomiting (RR 0.68, 95%CI [0.59, 0.79], n = 1171, 14 trials), diarrhea (RR 0.55, 95%CI [0.35, 0.88], n = 210, 3 trials), alopecia (RR 0.51 [0.39, 0.67], n = 584, 8 trials), and oral mucositis (RR 0.18, 95%CI [0.07, 0.45], n = 441, 4 trials) than that of chemotherapy alone group. All differences were statistically significant, and the detailed results are shown in Table 2.
(2) Tumor Marker Level. The pooled result of three trials [25, 29, 52] showed a higher CEA decrease rate in the CKI plus chemotherapy group than that of the chemotherapy alone group (RR 1.19, 95%CI [1.05, 1.35], n = 336, 3 trials, Table 2). Additionally, the pooled data of two trials [25, 28] showed a higher CA15-3 decrease rate in CKI plus chemotherapy group than that of the chemotherapy group (RR 1.15, 95% CI [1.03, 1.27], 2 trials, Table 2).
3.4.3. Subgroup Analyses
Subgroup analyses were performed according to breast cancer TNM stage to reveal the sources of clinical heterogeneity and their influences on ORR, DCR, and KPS score improvement rate. Subgroup analysis indicated a higher ORR and DCR (TNM stage II∼III) in the CKI plus chemotherapy group than that of the chemotherapy alone group from eight trials (Table 2). Similarly, the subgroup analysis also showed a higher ORR and DCR (TNM stage IV) in the CKI plus chemotherapy group than that of the chemotherapy alone group (Table 2).
In addition, subgroup analysis demonstrated that CKI plus chemotherapy group was superior to the chemotherapy alone group in increasing KPS score improvement rate based on TNM stage II∼III or TNM stage IV (Table 2). Finally, tumor responses were evaluated by using WHO criteria or RECIST criteria. The subgroup analysis showed that CKI plus chemotherapy could both increase ORR and DCR according to the two criteria (Table 2).
3.4.4. Certainty of Evidence
We graded the overall certainty of evidence by the GRADE approach for each important outcome. In the comparison of all outcomes and interventions assessments, the certainty of evidence for all outcomes was downgraded to “low” or “very low” mainly due to the high risk of performance bias, the design of comparison and unclear risk of bias for not reporting blinding the outcome assessor. The details of results are shown in Table 3.
Table 3.
Summary of main findings of RCTs on compound Kushen injection for breast cancer.
| Outcomes | No. of participants (no. of RCTS) | Certainty of the evidence | Relative effect (95% CI) | Anticipated absolute effects | |
|---|---|---|---|---|---|
| Risk with control | Risk difference with intervention (95% CI) | ||||
| CKI plus chemotherapy versus chemotherapy | |||||
| ORR | 1694 (21) | ⊕⊕○○1,5 | RR 1.30, [1.18, 1.43] | 471 per 1000 | 141 more per 1000, (from 85 more to 203 more) |
| DCR | 1627 (20) | ⊕○○○1,2,5 | RR 1.21, [1.15, 1.28] | 698 per 1000 | 147 more per 1000, (from 105 more to 196 more) |
| KPS score improvement rate | 1172 (14) | ⊕⊕○○1,5 | RR 1.42, [1.26, 1.61] | 476 per 1000 | 200 more per 1000, (from 124 more to 291 more) |
| KPS score | 393 (6) | ⊕○○○1,4,5 | N/A | N/A | The KPS score improvement in the intervention groups was 12.81 higher (10.16 to 15.46 higher) |
| PFS | 94 (1) | ⊕○○○1,4,5 | N/A | N/A | The PFS in the intervention groups was 2.24 months higher (1.26 to 3.22 higher) |
| OS | 94 (1) | ⊕○○○1,4,5 | N/A | N/A | The OS in the intervention groups was 2.44 months higher (1.45 to 3.43 higher) |
| Leukocyte decrease | 1121 (15) | ⊕○○○1,2,5 | RR 0.60, [0.5, 0.71] | 572 per 1000 | 229 fewer per 1000, (from 286 fewer to 166 fewer) |
| Platelet decrease | 750 (9) | ⊕⊕○○1,5 | RR 0.41, [0.29, 0.58] | 397 per 1000 | 234 fewer per 1000, (from 282 fewer to 167 fewer) |
| Liver injury | 1215 (13) | ⊕⊕○○1,5 | RR 0.42, [0.31, 0.57] | 269 per 1000 | 156 fewer per 1000, (from 185 fewer to 116 fewer) |
| Renal injury | 879 (9) | ⊕⊕○○1,5 | RR 0.63, [0.46, 0.86] | 203 per 1000 | 83 fewer per 1000, (from 116 fewer to 37 fewer) |
| Nausea and vomiting | 1171 (14) | ⊕⊕○○1,5 | RR 0.68, [0.59, 0.79] | 578 per 1000 | 185 fewer per 1000, (from 237 fewer to 121 fewer) |
| Diarrhea | 210 (3) | ⊕○○○1,3,5 | RR 0.55, [0.35, 0.88] | 324 per 1000 | 146 fewer per 1000, (from 210 fewer to 39 fewer) |
| Alopecia | 584 (8) | ⊕○○○1,2,5 | RR 0.51, [0.39, 0.67] | 514 per 1000 | 252 fewer per 1000, (from 313 fewer to 170 fewer) |
| Oral mucositis | 441 (4) | ⊕⊕○○1,5 | RR 0.18, [0.07, 045] | 136 per 1000 | 111 fewer per 1000, (from 126 fewer to 75 fewer) |
| Decrease rate of CEA | 336 (3) | ⊕○○○1,3,5 | RR 1.19, [1.05, 1.35] | 468 per 1000 | 89 more per 1000, (from 23 more to 164 more) |
| Decrease rate of CA153 | 206 (2) | ⊕○○○1,3,5 | RR 1.15, [1.03, 1.27] | 821 per 1000 | 123 more per 1000, (from 25 more to 22 more) |
Note. (1) Risk of bias: methodological quality of these trials was graded as “high risk of bias” due to the design of comparison. The trials also had unclear risk of performance bias for not reporting blinding the outcome assessor. (2) Inconsistency: the significant heterogeneity with a large I2 value, an I2 >50% indicated the possibility of statistical heterogeneity among the studies. (3) Imprecision: for dichotomous outcomes, the total number of events is less than 300; or pooled results included no effects. (4) Imprecision: for continuous outcomes, the total population size is less than 400; or pooled results included no effects. (5) All the trials had high risk of performance bias for not blinding the participants. ∗The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; MD: mean difference. N/A: not applicable. RCT: randomized controlled trial. No.: number. ⨁: very low quality of the evidence; ⨁⨁: low quality of the evidence; GRADE Working Group grades of evidence. Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.
3.4.5. Trial Sequential Analysis
TSA was performed with the data from trials reporting the ORR [27–32, 34, 36, 37, 39–44, 46, 48–50, 53, 54]. A required information size was estimated based on Daris type I error = 5%, power = 80%, RRR = 15%, and a two-side graph [24, 51]. The result of TSA illustrated the cumulative Z-curve across the traditional boundary of 5% significance (horizontal red line) and also cross the monitoring boundaries (red inward sloping curves). These indicated that CKI plus chemotherapy for patients with breast cancer could draw an encouraging conclusion on ORR before acquired information size of 2677 participants (Figure 8). Similarly, the result from trials reporting the KPS score improvement rate [28, 30–33, 36–38, 40–42, 47, 48, 52] illustrated that the cumulative Z-curve across the traditional boundary of 5% significance and cross the monitoring boundaries as well, indicating that CKI plus chemotherapy for patients with breast cancer could draw an encouraging conclusion on KPS score improvement rate before acquired information size of 3072 participants [55] (Figure 9).
Figure 8.
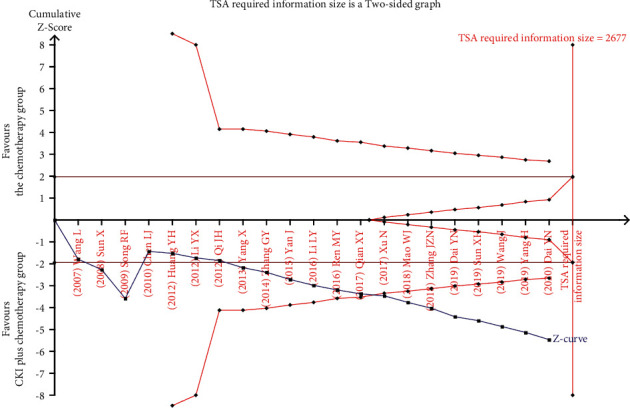
TSA on CKI plus chemotherapy versus chemotherapy for ORR in patients with breast cancer.
Figure 9.
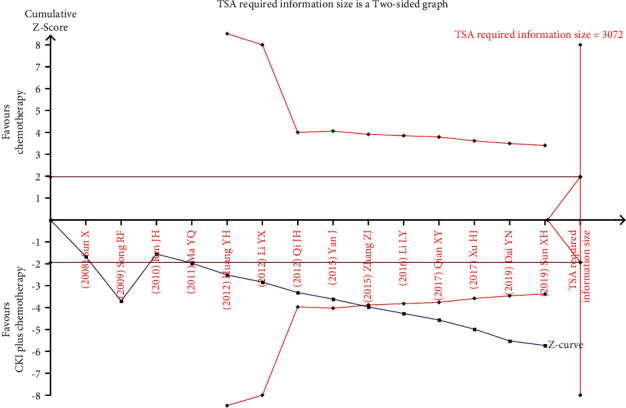
TSA on CKI plus chemotherapy versus chemotherapy for KPS score improvement rate in patients with breast cancer.
3.4.6. Publication Bias
The funnel plot was performed using RR and 1/(standard error: SE) values obtained from the trials measuring ORR and KPS score improvement rate. The funnel plots based on ORR and KPS score improvement rate appeared asymmetrical, suggesting the potential publication bias [56] (Figures 10 and 11).
Figure 10.
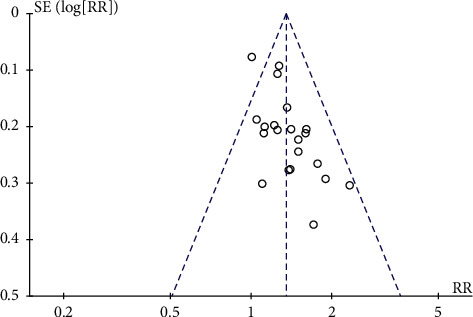
Funnel plot assessing publication bias (using ORR in 21 trials).
Figure 11.
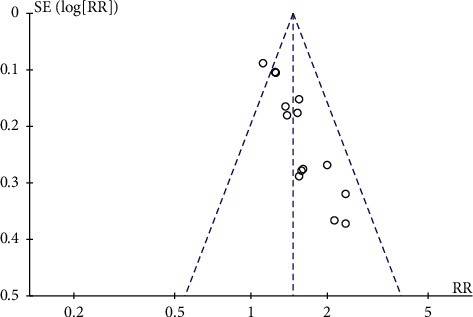
Funnel plot assessing publication bias (using KPS score improvement rate in 14 trials).
4. Discussion
4.1. Summary of the Main Results
Thirty trials involving 2556 participants were included in this review. Our results suggested that the combination of CKI and chemotherapy seems to demonstrate the beneficial effect of CKI as an add-on therapy for breast cancer. The tumor response rate (ORR and DCR) and HRQol measured by the KPS score improvement rate in CKI plus chemotherapy group were approximately 14% and 20% higher than that of the chemotherapy group, respectively. The KPS score improvement in CKI plus chemotherapy group was about 12 scores higher than that of the chemotherapy alone group. Long-term effectiveness of the combination of CKI and chemotherapy was insufficiently reported in terms of PFS or OS. CKI plus chemotherapy seemed to be more effective than chemotherapy alone in treating breast cancer. However, the certainty of evidence for all outcomes was mainly assessed as “low” or “very low” due to the risk of bias and statistical heterogeneity among the included studies. The results showed that CKI plus chemotherapy group had a lower risk of ADRs compared to the chemotherapy alone group, and CKI appeared to ease the toxic reaction induced by chemotherapy. However, we could not draw a powerful conclusion from the current evidence.
4.2. Strengths and Limitations
Three previous studies [14–16] have assessed the effectiveness of CKI for breast cancer, which demonstrated that CKI used in combined with conventional treatment of chemotherapy seemed more effective than conventional chemotherapy alone. The included trials of the three reviews applied CKI as add-on intervention, and the performance status and tumor response improvement were analyzed. Our findings supported the claims of previous reviews. In contrast, this updated review expanded the trials and sample size, which increased the reliability of synthesized results. Additionally, this review conducted a more rigorous inclusion criterion for participant and outcome assessment and covered additional outcome assessments (such as HRQol, PFS, and OS). Furthermore, we performed subgroup analysis based on the TNM stage and tumor response criteria to reveal the sources of clinical heterogeneity and their influences on primary outcomes such as ORR, DCR, and KPS score improvement rate. This review provided the latest evidence of CKI for treating breast cancer.
There are some limitations of this review. Firstly, all included trials had high risk of performance bias, most of which had unclear risk of selection and attrition bias, which contributed to compromising the trustworthiness and strength of the evidence. Thus, the findings of this review should be interpreted cautiously. Secondly, there were some differences among the dosage of CKI application and chemotherapy regimens in the included trials, which contributed to the increased clinical heterogeneity of the pooled results. Thirdly, our analysis failed to draw conclusions on the long-term survival (PFS or OS) of CKI for breast cancer because there was no evidence to support the effect of CKI for this important clinical outcome in patients with breast cancer. This result needs to be further investigated by new evidence.
4.3. Implications for the Clinical Practice
Although there are some potential biases and limitations in this review, the results suggested that CKI as an adjunctive treatment had potential effect in the treatment of breast cancer. According to the results, with the help of CKI, the number of patients with improved tumor response per thousand patients would be almost 140 more than those with the chemotherapy alone. Similarly, the number of patients with improved KPS score per thousand patients in the combination of CKI group would be 200 more than those with the chemotherapy group. Subgroup analysis did not find significant different results between stage II-III and Stage IV for all the concerned outcomes. According to this review, the common dosage of CKI in the treatment of breast cancer was 12–30 ml/time injected intravenously (the general dosage is 20 ml/time). The treatment durations per cycle were 6, 7, 10, 12, 14, 15, or 21 days, and treatment cycles varied from two to eight cycles. Overall, though the certainty of the evidence is “low” or “very low,” the combination of CKI and chemotherapy might be a choice in clinical practice for women with breast cancer because its estimate effect was significantly better than that of the chemotherapy alone. Considering the weak evidence of this intervention, practitioners may consider its use based on their clinical experience and the actual condition of patients.
4.4. Implications for Research
The methodological information was reported insufficiently in the included trials. Future trials are encouraged to design, conduct, and report according to the Consolidated Standards of Reporting Trials (CONSORT) statement [57], which is critical to control the risk of bias and improve the reliability of the evidence of CKI in the treatment of breast cancer. Additionally, study protocol should be prospectively registered on authoritative registration platforms before study implementation to ensure the research can be conducted according to the predefined standard [58]. Furthermore, in order to observe the long-term efficacy of CKI in the treatment of breast cancer and evaluate the survival time or progression time of patients, sufficient follow-up time should be considered and reported during the study period. Most importantly, to give conclusive evidence and influence clinical practice, we also suggest future studies report detailed information on PFS, OS, and ADRs, as well as tumor marker level, which are important data for further evaluation of the effectiveness of CKI.
Besides the effectiveness, safety issues related to CKI should not be overlooked. The results of this review indicated that CKI might have a protective effect on liver and kidney function. Based on the quality of current evidence and the related evidence, we believe that CKI could relieve the hematotoxicity and gastrointestinal reactions [10, 59, 60]. However, only about 53% of the included trial reported ADRs during treatment; thus, no firm conclusion on the safety of CKI could be drawn from this review.
5. Conclusions
Low certainty of evidence suggested potential effectiveness of the combination of CKI and chemotherapy regimens for treating breast cancer, especially on improving ORR, DCR, and KPS score in patients with breast cancer. The conclusions about PFS or OS could not be drawn according to this review due to lack of evidence. CKI appeared to relieve the risk of ADRs in patients with breast cancer receiving chemotherapies. However, due to weak evidence, the findings should be further confirmed in large and rigorous trials.
Acknowledgments
The authors would like to thank all authors of the primary studies included in this review. This work was supported by the fund from Guidelines on Clinical Application of Chinese Patent Medicines Standardized Program (no. SATCM-2015-BZ402).
Abbreviations
- ADRs:
Adverse drug reactions
- CKI:
Compound Kushen injection
- CONSORT:
Consolidated Standards of Reporting Trials
- CI:
Confidence interval
- CNKI:
China National Knowledge Infrastructure
- DCR:
Disease control rate
- HRQoL:
Health-related quality of life
- KPS:
Karnofsky Performance Scale
- MD:
Mean difference
- ORR:
Objective response rate
- OS:
Overall survival
- PFS:
Progression-free survival
- RCTs:
Randomized clinical trials
- RR:
Risk ratio
- REM:
The random-effect model
- SinoMed:
Chinese Biomedical Literature Database
- SE:
Standard error
- TSA:
Trial sequential analysis
- TCM:
Traditional Chinese medicine
- VIP:
China Science Technology Journal Database.
Contributor Information
Ying-Yi Fan, Email: fan38898901@126.com.
Xiao-Hua Pei, Email: pxh_127@163.com.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Disclosure
Bao-Yong Lai and Ai-Jing Chu are co-first authors.
Conflicts of Interest
All authors declare that they have no conflicts of interest.
Authors' Contributions
BY Lai conceptualized the study; AJ Chu and LY Jia were responsible for data curation; AJ Chu, BY Lai, and LY Jia were responsible for formal analysis; AJ Chu and LY Jia investigated the study; BY Lai, AJ Chu, and LYJ were responsible for methodology; BY Lai and AJ Chu took part in project administration; XH Pei supervised the study; BY Lai and AJ Chu wrote the original draft; BW Yu, YY Fan, JP Liu, and XH Pei reviewed and edited the manuscript. Bao-Yong Lai and Ai-Jing Chu contributed equally to this work.
References
- 1.Lewis D. R., Chen H.-S., Cockburn M. G., et al. Early estimates of cancer incidence for 2015: expanding to include estimates for white and black races. Cancer . 2018;124(10):2192–2204. doi: 10.1002/cncr.31315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fan L., Strasser-Weippl K., Li J.-J., et al. Breast cancer in China. The Lancet Oncology . 2014;15(7):e279–e289. doi: 10.1016/s1470-2045(13)70567-9. [DOI] [PubMed] [Google Scholar]
- 3.Ferlay J., Soerjomataram I., Dikshit R., et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. International Journal of Cancer . 2015;136(5):E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 4.Harbeck N., Gnant M. Breast cancer. The Lancet . 2017;389(10074):1134–1150. doi: 10.1016/s0140-6736(16)31891-8. [DOI] [PubMed] [Google Scholar]
- 5.Denegri A., Moccetti T., Moccetti M., Spallarossa P., Brunelli C., Ameri P. Cardiac toxicity of trastuzumab in elderly patients with breast cancer. Journal of geriatric cardiology: JGC . 2016;13(4):355–363. doi: 10.11909/j.issn.1671-5411.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valachis A., Nilsson C. Cardiac risk in the treatment of breast cancer. assessment and management. Breast Cancer . 2015;7:21–35. doi: 10.2147/BCTT.S47227.S47227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alcantara-Silva T. R., Freitas-Junior R., Freitas N. M., Machado G. D. Fatigue related to radiotherapy for breast and/or gynaecological cancer: a systematic review. Journal of Clinical Nursing . 2013;22(19-20):2679–2686. doi: 10.1111/jocn.12236. [DOI] [PubMed] [Google Scholar]
- 8.Ma Z., Fan Y., Wu Y., et al. Traditional Chinese medicine-combination therapies utilizing nanotechnology-based targeted delivery systems: a new strategy for antitumor treatment. International Journal of Nanomedicine . 2019;14:2029–2053. doi: 10.2147/ijn.s197889.S197889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C. Y., Bai X. Y., Wang C. H. Traditional Chinese medicine: a treasured natural resource of anticancer drug research and development. The American journal of Chinese medicine . 2014;42(3):543–559. doi: 10.1142/S0192415X14500359. [DOI] [PubMed] [Google Scholar]
- 10.Qu Z., Cui J., Harata-Lee Y., et al. Identification of candidate anti-cancer molecular mechanisms of Compound Kushen Injection using functional genomics. Oncotarget . 2016;7(40):66003–66019. doi: 10.18632/oncotarget.11788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cao X., He Q. Anti-tumor activities of bioactive phytochemicals in Sophora flavescens for breast cancer. Cancer Management and Research . 2020;12:1457–1467. doi: 10.2147/cmar.s243127.S243127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu S., Hu X., Fan X. A bioinformatics research on novel mechanism of compound kushen injection for treating breast cancer by network pharmacology and molecular docking verification. Evid Based Complement Alternat Med . 2020;2020 doi: 10.1155/2020/2758640.2758640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nourmohammadi S., Aung T. N., Cui J., et al. Effect of compound kushen injection, a natural compound mixture, and its identified chemical components on migration and invasion of colon, brain, and breast cancer cell lines. Frontiers in Oncology . 2019;9:p. 314. doi: 10.3389/fonc.2019.00314.00314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng J. W., Liu S. Y., Wang K. H., Wu J. R., Duan X. J., Ni M. W. Systematic review on compound Kushen injection in treatment of breast cancer based on Meta-Analysis. Evaluation and Analysis of Drug-Use in Hospitals of China . 2018;18(8):1015–1020. [Google Scholar]
- 15.Zhou Y. Q. Efficacy and Safety of Fu Fang Ku Shen Injection Combined with Chemotherapy for Patients with Breast Cancer after Surgery: A Meta-Analysis . Zhejiang, China: Zhe jiang University of Chinese Medicine; 2019. Master Dissertation. [Google Scholar]
- 16.Ao M., Xiao X., Li Q. Efficacy and safety of compound Kushen injection combined with chemotherapy on postoperative Patients with breast cancer. Medicine (Baltimore) . 2019;98(3) doi: 10.1097/md.0000000000014024.e14024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moher D., Liberati A., Tetzlaff J., Altman D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology . 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 18. J. Higgins, and S. Green, “Cochrane Handbook for Systematic Reviews of Interventions,” Version 5.1.0, updated march 2011.
- 19.Lai B.-Y., Jia L.-Y., Yu B.-W., et al. Chinese herbal medicine (Rupi Sanjie capsule) for the treatment of breast pain: a systematic review and meta-analysis of randomized clinical trials. Integrative Medicine Research . 2021;10(2) doi: 10.1016/j.imr.2020.100491.100491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park J. O., Lee S. I., Song S. Y. Measuring response in solid tumors: comparison of RECIST and WHO response criteria. Japanese Journal of Clinical Oncology . 2003;33(10):533–537. doi: 10.1093/jjco/hyg093. [DOI] [PubMed] [Google Scholar]
- 21.Xiao Z., Wang C., Zhou M., et al. Clinical efficacy and safety of Aidi injection plus paclitaxel-based chemotherapy for advanced non-small cell lung cancer: a meta-analysis of 31 randomized controlled trials following the PRISMA guidelines. Journal of Ethnopharmacology . 2019;228:110–122. doi: 10.1016/j.jep.2018.09.024. [DOI] [PubMed] [Google Scholar]
- 22.Trotti A., Colevas A., Setser A., et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Seminars in Radiation Oncology . 2003;13(3):176–181. doi: 10.1016/s1053-4296(03)00031-6. [DOI] [PubMed] [Google Scholar]
- 23.Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. Measuring inconsistency in meta-analyses. BMJ . 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wetterslev J., Jakobsen J. C., Gluud C. Trial Sequential Analysis in systematic reviews with meta-analysis. BMC Medical Research Methodology . 2017;17(1):39–41. doi: 10.1186/s12874-017-0315-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adlt Y. S., Ai X. Y., Zhang J. Z. N., Tong Y., Wu J., Zhao B. Toxic and side effects of compound matrine injection in breast cancer adjuvant chemotherapy. Liaoning Journal of Traditional Chinese Medicine . 2016;43(10):2101–2102. [Google Scholar]
- 26.Cao W. Clinical study of compound Kushen injection combined with chemotherapy in the treatment of breast cancer. Modern Journal of Integrated Traditional Chinese and Western Medicine . 2012;21(36):4044–4045. [Google Scholar]
- 27.Chen L. J. Efficacy analysis of compound kushen injection as adjunctive treatment for breast cancer. China Pharmacy . 2010;21(20):1866–1867. [Google Scholar]
- 28.Dai Y. N., Han J. J., Li J. M., Chen X. J., Feng X. X., Wang R. Clinical Observation on compound sophora flavescens injection combined with neoadjuvant chemotherapy on primary breast cancer. Liaoning Journal of Traditional Chinese Medicine . 2019;46(10):2121–2123. [Google Scholar]
- 29.Dai Y. N., Tian Y., Chen X. J., Sun S. G., Song Q. Q., Guo L. Efficiency observation of compound Kushen injection and neoadjuvant chemotherapy on breast cancer. Shanxi Journal of Traditional Chinese Medicine . 2020;36(04):23–24. [Google Scholar]
- 30.Huang Y. H., Liao Z. Y., Fan C. H., Wang Y. F. The clinical observation combined com pound Kushen with paclitaxel plus amycin in treatment of advanced manmmary cancer. Medical Journal of West China . 2012;24(09):1699–1701. [Google Scholar]
- 31.Li L. Y. Clinical observation of Compound Kushen injection combined with paclitaxel and adriamycin in the treatment of advanced breast cancer. Journal of New Chinese Medicine . 2016;48(01):158–159. [Google Scholar]
- 32.Li Y. X. Clinical observation on 60 cases of advanced breast cancer treated with Compound Kushen injection combined with chemotherapy. Guide of China Medicine . 2012;10(36):302–303. [Google Scholar]
- 33.Ma Y. Q., Yang M. C., Wang H., Du F. Clinical observation of compound Kushen injection combined with chemotherapy in the treatment of advanced breast cancer. Yi Yao Qian Yan . 2011;01(21):90–91. [Google Scholar]
- 34.Mao W. J., Me Y. Me Impacts on the safety to the ACT scheme after breast cancer operation by administration of compound Kushen injection. Liaoning Journal of Traditional Chinese Medicine . 2018;45(04):760–762. [Google Scholar]
- 35.Niu Y. L. Effect of gemcitabine and cisplatin chemotherapy combined with compound Kushen injection on serum T cell subsets and quality of life in patients with breast cancer after operation. Modern Diagnosis and Treatment . 2017;28(24):4582–4583. [Google Scholar]
- 36.Qi J. H., Liang Y. N. Clinical study of compound Kushen injection combined with chemotherapy in the treatment of advanced breast cancer. World Health Digest . 2012;9(34):401–402. [Google Scholar]
- 37.Qian X. Y., Zho M. Y., Lin H. F., Zhou A. X. Clinical observation of compound Kushen injection combined with platinum and gemcitabine chemotherapy for triple negative breast cancer. The Practical Journal of Cancer . 2017;32(02):305–316. [Google Scholar]
- 38.Ren J. H., Wang H., Liu L. M., Li X. H., Zhang F. M., Zhang X. Q. “Clinical observation on Kushen injection combined with “CAF” chemotherapy for one hundred and twenty --three patients with early breast carcinoma underwent modified radical mastectomy. Evaluation and Analysis of Drug-Use in Hospitals of China . 2010;10(08):736–739. [Google Scholar]
- 39.Ren M. Y., Zhang Y., Yang S. L., Zhang H. R., Gao X., Xu Z. Q. Efficacy and recurrence of compound Kushen injection combined with ET chemotherapy in the treatment of advanced breast cancer. Chinese Journal of Modern Drug Application . 2016;10(22):128–129. [Google Scholar]
- 40.Song R. F., Wan Y. Y., Chen C. Clinical observation of compound Kushen injection combined with chemotherapy in the treatment of advanced breast cancer. Jiangxi Medical Journal . 2009;44(04):343–344. [Google Scholar]
- 41.Sun X., Pei F. Z., Qu Z. Y. Clinical observation of compound Kushen injection (Yanshu injection) combined with chemotherapy in the treatment of advanced breast cancer. China & Foreign Medical Treatment . 2008;22:p. 67. [Google Scholar]
- 42.Sun X. H., You R. L., Li Z. Y., Zhao Y., Yang M. H., Yang Y. Clinical efficacy, serum tumor markers, toxic and side reactions on advanced breast cancer by compound sophora flavescens combined with heoadjuvant chemotherapy. Liaoning Journal of Traditional Chinese Medicine . 2019;46(08):1670–1673. [Google Scholar]
- 43.Wang J., Ren Y. Clinical study on compound Kushen injection combined with ET regimen in treatment of breast cancer. Drugs & Clinic . 2019;34(07):2137–2141. [Google Scholar]
- 44.Wang L., Liu J. Clinical observation of CTF regimen combined with Yanshu injection in neoadjuvant chemotherapy of breast cancer. China Medical Herald . 2007;4(24):55–97. [Google Scholar]
- 45.Wei Y. H. Compound Kushen injection combined with postoperative adjuvant chemotherapy for breast cancer: a report of 24 cases. Chinese Medicine Modern Distance Education of China . 2010;8(08):100–101. [Google Scholar]
- 46.Xu N. Clinical efficacy of compound Kushen injection in the treatment of breast cancer patients with postoperative chemotherapy and its influence on peripheral blood T cell subsets. Medical Journal of Chinese People’s Health . 2017;29(07):16–18. [Google Scholar]
- 47.Xu H. J. Clinical observation on treating breast cancer after surgery with the Kushen injection plus chemotherapy. Clinical Journal of Chinese Medicine . 2017;9(08):120–121. [Google Scholar]
- 48.Yan J., Chen B., Yuan J. H., Guo Y. W., Liu Z. Y., Wu J. Application effect of compound Kushen injection in chemotherapy of breast invasive ductal carcinoma. Women’s Health Research . 2015;12:p. 173. [Google Scholar]
- 49.Yang X. Observation on the effects of compound matrine injection on the toxic and side effects in chemotherapy of breast cancer. Journal of Clinical Medicine in Practice . 2013;17(05):105–107. [Google Scholar]
- 50.Yang H. Application value of compound Kushen injection in postoperative chemotherapy of breast cancer patients. Shenzhen Journal of Integrated Traditional Chinese and Western Medicine . 2019;29(01):28–30. [Google Scholar]
- 51.Zhai X. J. Effect of compound Kushen injection on side effects and immune function of breast cancer patients after chemotherapy. Journal of Basic Chinese Medicine . 2014;20(06):829–831. [Google Scholar]
- 52.Zhang Z. J. Clinical observation of compound Kushen injection combined with AC regimen in the treatment of patients with early breast cancer after modified radical mastectomy. Guangming Journal of Chinese Medicine . 2015;30(09):1963–1965. [Google Scholar]
- 53.Zhang G. Y., Yu X. L., Li C. L., Meng R. Q., Zhou G. Y. Efficacy of matrine injection on chemotherapy in patients with breast cancer after operation. Guiding Journal of Traditional Chinese Medicine and Pharmacy . 2014;20(05):38–40. [Google Scholar]
- 54.Zhang J. Z. N., Adlt Y. S., Ai X. Y., Tong Y., Zhao B. Efficacy of Compound Kushen injection combined with gemcitabine and carboplatin for metastatic triple negative breast cancer. Liaoning Journal of Traditional Chinese Medicine . 2018;45(10):2123–2125. [Google Scholar]
- 55.Xia Y., Sun Y., Liu Z. L., Liu J. P. Estimation of sample size in systematic review and Meta-analysis: trial sequential analysis. Clinical Medical Image . 2013;20(05):31–33. [Google Scholar]
- 56.Sedgwick P., Marston L. How to read a funnel plot in a meta-analysis. BMJ . 2015;16:p. 351. doi: 10.1136/bmj.h4718.h4718 [DOI] [PubMed] [Google Scholar]
- 57.Moher D., Hopewell S., Schulz K. F., et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. International Journal of Surgery . 2012;10(1):28–55. doi: 10.1016/j.ijsu.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 58.Laine C., Horton R., DeAngelis C. D., et al. Clinical trial registration - looking back and moving ahead. New England Journal of Medicine . 2007;356(26):2734–2736. doi: 10.1056/nejme078110. [DOI] [PubMed] [Google Scholar]
- 59.Yu L., Zhou Y., Yang Y., Lu F., Fan Y. Efficacy and safety of compound kushen injection on patients with advanced colon cancer: a meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med . 2017;12 doi: 10.1155/2017/7102514.7102514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen H., Yao X., Li T., et al. Compound Kushen injection combined with platinum-based chemotherapy for stage III/IV non-small cell lung cancer: a meta-analysis of 37 RCTs following the PRISMA guidelines. Journal of Cancer . 2020;11(7):1883–1898. doi: 10.7150/jca.40267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.


