Abstract
Multidisciplinary treatment and multimodal analgesia are the approach to reduce mortality and morbidity of breast cancer. Pectoral nerve block (PECS I and II) is one of the modes of analgesia advocated. The primary aim is to find the risks and benefits of the block in providing analgesia for intraoperative and immediate postoperative cancer-related breast surgery and total morphine consumption. The secondary aim is to evaluate, any additional knowledge acquired, in the reduction of persistent chronic pain state and cancer recurrence, during the time frame studied. The study was conducted after the approval of the ethics committee and National Registry, and included patients of ASA I and II undergoing mastectomy surgery with axillary clearance, under general anesthesia, during the period of 2017 to 2018. A total of 60 patients were recruited, randomizing them into two groups: group 1 (n = 30): ultrasound-guided PECS I (0.2 ml/kg) and PECS II (0.4 ml/kg) block, post-induction with 0.25% levobupivacaine, maximum dose of 2 mg/kg; group 2 (n = 30): no block, only general anesthesia. Intraoperatively, vitals were monitored at regular intervals and analgesics given as per response. Postoperatively, pain was assessed using the numerical pain score and arm abduction score, until discharge. Data collected was analyzed and interpreted using statistical methods. Patients were followed up telephonically, until six months for any chronic pain and cancer recurrence instances. The PECS block group used less morphine intra and postoperatively, which was statistically significant (p = 0.0001). Group 1- Had a significant decrease in the mean intraoperative systolic blood pressure (p = 0.03). There was significant improvement in the arm abduction in the test group as compared to that in the control group (p = 0.001). The average time for block performance was 7.9 min and no complications were observed. No patients in the study groups reported chronic pain or cancer recurrence issues. The two-level PECS block is safe, effective, reliable, and easy to perform.
Clinical Trial Registration Number: CTRI/2017/11/010630
Keywords: Pecs block, Breast analgesia, Postoperative pain, Chronic pain management, Opioid-sparing analgesia
Introduction
Among the overall incidence of cancers, including both sexes, all ages, and specifically in women, breast cancer is the most common. The global cancer burden has escalated to 19.3 million new cases and 10 million cancer deaths in 2020, according to the GLOBOCAN 2020 report. For the first time female breast cancer has surpassed lung cancer as the most often diagnosed cancer, one of every four malignancies, with 2.3 million new cases worldwide and the leading cause of cancer deaths in women, owing to its high incidence in low and middle-income nations (LMICs), with the prediction to further increase by 2040 [1]. India accounts for 25% of the world population and, depending upon the socioeconomic status, is categorized as medium, under the 4‐tier Human Development Index (HDI) based on the United Nation's 2019 Human Development Report [2]. Indian data shows breast cancer as the commonest in women with an incidence of 13.5% of new cases in both sexes and all ages and 26% in females of all ages with the death rate of 10.6% [ 1]. Among several conventional therapies, a multidisciplinary team approach, early identification and excision of localized lesions, such as, lumpectomy or partial mastectomy, are more favorable for long-term survival. Breast cancer treatment has evolved since the eighteenth century, when William Halsted pioneered radical mastectomy, which came with a slew of sequelae, including paraesthesia, lymphedema, and a loss of upper-limb mobility. The modifications proposed by Madden, in the late nineteenth century, have been implemented. This ranged from radical mastectomy, with or without breast reconstruction to sentinel node biopsy with or without axillary lymph node dissection, keeping both the pectoral muscles which produced the best results. The combinations of advances in adjuvants like chemotherapy, radiotherapy, plastic, and robotic surgery have offered several advantages in the clinical management of breast oncosurgery [3]. More recently, immunotherapy has been added to the armamentarium of breast oncotherapy [4]. Despite the improved efficiency in the surgical treatment, complications still occur, such as peri-mastectomy pain syndrome (PPBCS), which accounts to an incidence of 20–50%. General anesthesia with multimodal analgesia is the standard of perioperative care [5]. There is growing evidence of cancer recurrence with the use of morphine [6]. Previously considered as the “gold standard,” thoracic epidural and paravertebral block were commonly used, but associated with several side effects [7]. The pioneering work by Blanco R, in 2011, illustrated the effectiveness of pectoral nerve (PECS) block in reducing pain over the breast and axillary. This was demonstrated by injecting a local anesthetic between the pectoral muscles and serratus anterior, warranting more randomized studies to further authenticate this technique [8]. At the start of this study, only three randomized controlled trials (RCT) were available in the scientific literature.
Inadequately treated acute pain will lead to chronic pain state [9]. Our aim was to investigate the possible benefits and drawbacks of an ultrasound-guided pectoralis nerve block and the amount of morphine consumed, as well as the quality of analgesia, intraoperatively and postoperatively, in order to add to the growing body of research supporting opioid-sparing analgesia and the safety of this block for postoperative analgesia.
Methods
This study was conducted, at the Department of Anaesthesia, in collaboration with Endocrine Surgery, at our quaternary-level hospital and research institution. Following ethics committee approval, and registration in the National Registry, the study design was a randomized control trial (parallel arms). The acute phase studied was within one week postoperatively or up to discharge and the long-term follow-up until six months after the surgery. Independent data and safety monitoring board were in place to review periodically the efficacy and safety of the data collection, which was completed without interim analysis within the stipulated time period.
Inclusion Criteria
All ASA I and II consenting patients with breast cancer aged between 18 years and above undergoing radical mastectomy with axillary clearance.
Exclusion Criteria
Non-consenting patients, ASA III and IV physical status, bilateral mastectomy, allergy to local and general anesthetic drugs, chest wall anatomical abnormality, presence of infection, patients on anticoagulants or antiplatelet drugs or coagulopathy.
Method of Randomization
Block randomization was performed using computer-generated random numbers used to ensure equality of numbers in the two groups studied.
Blinding
This was blinded by using concealed opaque envelopes until time of recruitment. However, intervention was not blinded. Evaluation of the outcome was performed by an independent pain nurse in the ward who was unaware of the intervention received by the patient.
Recruitment
The study included patients who fulfilled the inclusion criteria. Patients underwent routine preanesthetic evaluation, and written and informed consent was obtained. The same was explained to their closest relative. The confidentiality of the patient was maintained. Following routine fasting protocols, patients were reassessed on the day of surgery. All safety precautions, for standard monitoring and anesthetic care; the patients were induced and maintained with oxygen, and opioids (fentanyl 2–3 μg·kg−1, morphine 0.1 mg·kg−1), propofol 2–3 mg·kg−1, and vecuronium bromide 0.1 mg·kg−1 were used to facilitate endotracheal, inhalational agent (isoflurane-MAC = 0.8·1), additionally, paracetamol (15 mg·kg−1).
Intervention
Group 1 (study arm), Group 2 (control arm).
Group 1 (n = 30): Received ultrasound-guided PECS-I (0.2 ml·kg−1) and PECS-II (0.4 ml·kg−1) block with 0.25% levobupivacaine (maximum dose 2 mg·kg−1).
Group 2 (n = 30): Received only general anesthesia and no block.
The block was performed under strict aseptic precautions with the Sonosite ultrasound machine (US), using high-frequency linear (8–12 MHz) probe, ultrasound gel, and SonoPlex (Pajunk) locating and stimulating needle. However, we did not use the nerve stimulation option. Slightly rotating the transducer allowing the in-plane needle trajectory from the medical to lateral side was the approach adopted. At all times, the shaft of the needle along with the tip of the needle was visualized. The landmarks identified under USG, for PECSI, at the level of myofascial plane between the pectoralis major and pectoralis minor, within which is also the pectoral branch of the thoracoacromial artery. A further deeper level is between the serratus anterior and pectoralis minor, for PECS-II. Confirming the plane by hydro-dissection with saline to open the space and only then administer the drug.
Outcome Measurements
Intraoperative Period: Any increase in heart rate and blood pressure to more than 20% of the baseline was treated as a pain response after the patient was under the adequate plane of anesthesia and supplemented with morphine as required. Intraoperative vitals were monitored on intervals of 5, 10,15 30, 45, 60, 90, 120, 160, and 180. Heart rate (HR), and systolic, diastolic, mean blood pressure (BP) along with EtCO2 and SpO2 were recorded. After completion of surgery, neuromuscular blockade was reversed with neostigmine (0.05 mg·kg−1 and glycopyrrolate 0.01 mg·kg−1) and patients were extubated once the criteria for extubation were met. Total morphine and fentanyl consumptions were noted.
Postoperative Period: After surgery, patients were transferred to the postanaesthesia care unit (PACU), monitored for vitals, and discharged to ward when stable. Pain score was documented against Numeric Rating Scale score (NRS, 0 “no pain at all” whereas 10 “the worst pain possible”) every 2 h for the initial 24 h and every 6 h for the next 24 h until discharge. Functional activity score (arm abduction score) was used to assess ability for arm abduction postoperative (Table 1) [10].
Table 1.
Functional Activity Score (arm abduction score)
| No | Comment | Score |
|---|---|---|
| 1 | No limitation of relevant activity | A |
| 2 | Mild limitation of relevant activity | B |
| 3 | Severe limitation of relevant activity | C |
Note: The Score is assessed relative to the patient’s baseline functional ability and based on activity that is relevant to the cause of acute pain
Statistical Methods
The sample size varied from 28 to 63 for various potential differences in standard deviation to detect differences of 2 mg and 3 mg between two groups intraoperatively. The various sample sizes for potential differences in two groups with possible standard deviations of the dose of morphine.
Postoperative pain was taken as the main outcome. The amount of morphine consumed was noted as one of the primary outcomes. One of the RCT suggests one unit difference in NRS scale to be significant, among PECS and control group [11]. So, if we consider one unit difference, we need 20 samples in each arm with a power of 80% and error of 5%. The following formula was used:
For the present study, it was decided to choose 30 subjects per group. This addition is reserved, in the event of any dropouts.
Analytical Methods
SPSS software was used for analysis of data. Baseline data was described using frequency, mean, and 95% confidence interval in the two study groups. Continuous variables in the data were compared between two treatment groups for outcome variables measured at different times using “Mixed Model Analysis of Co-Variance” with “Group” as between group variable and “Time” as repeated measures. Baseline data was used as the “Co-variate.” Since most of the surgery took less than 180 min, ANOVA measurement included only periods (Time) with outcomes where more than 50% of patients were available. Total dose of morphine and fentanyl were compared using Student’s t test. p-value of less than 0.05 was considered significant [12].
Results
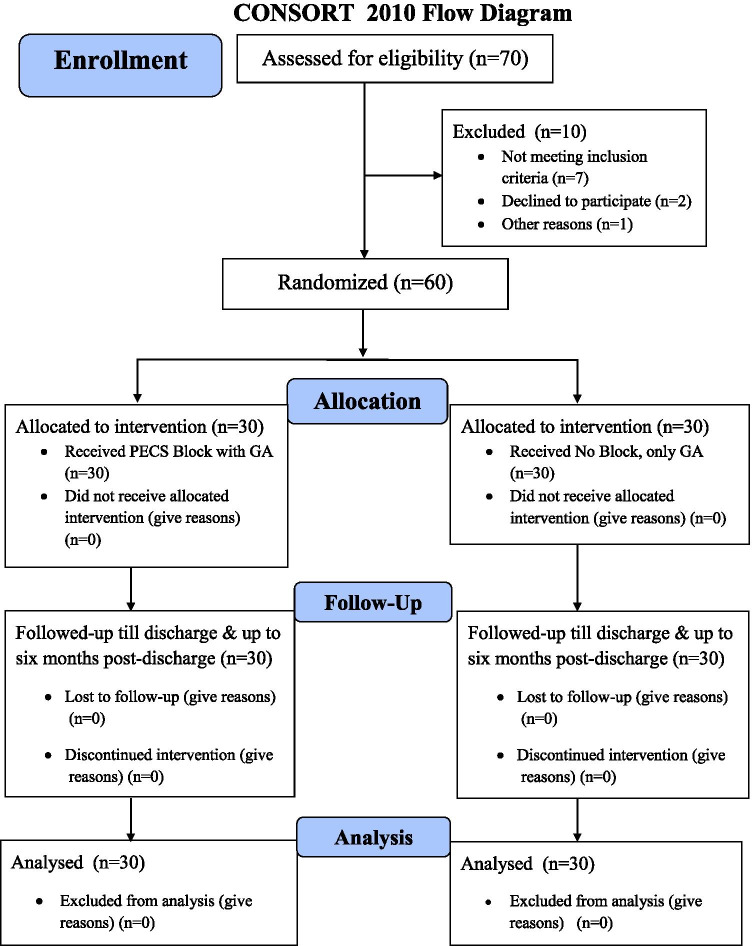
There were 60 patients recruited as per inclusion and exclusion criteria during the study period. There were 30 patients in each arm, allocated to group-1, the intervention arm (PECS block with GA), and group-2, the control arm (GA alone). There were 1 male and 59 females. The mean age in the study was 49 + 10 years. There was no statistically significant difference noted in the sex, age, weight, and ASA grade in the test and control groups (Fig. 1, Table 2).
Fig. 1.
CONSORT flow diagram
Table 2.
Overall relevant data findings
| Category | Parameter | Group 1 (Block + GA) N = 30 |
Group 2 (GA alone) N = 30 |
p value |
|---|---|---|---|---|
| Demographic | Sex (male:female) | 0:30 | 1:29 | 0.5 |
| Mean age | 51 | 47 | 0.14 | |
| Mean weight | 59 | 63 | 0.1 | |
| ASA grade (1:2) | 11:19 | 17:13 | 0.12 | |
| Type of surgery | Modified radical/simple mastectomy | 29/1 | 27/3 | 0.28 |
| Intra-op systolic blood pressure | Mean | 119.361 | 130.458 | 0.03 |
| Total morphine consumption | Mean | 3.07 | 5.63 | 0.0001 |
| SD | 1.388 | 1.426 | ||
| Arm abduction score | Mean | 1.178 | 1.528 | 0.001 |
Intraoperative Data
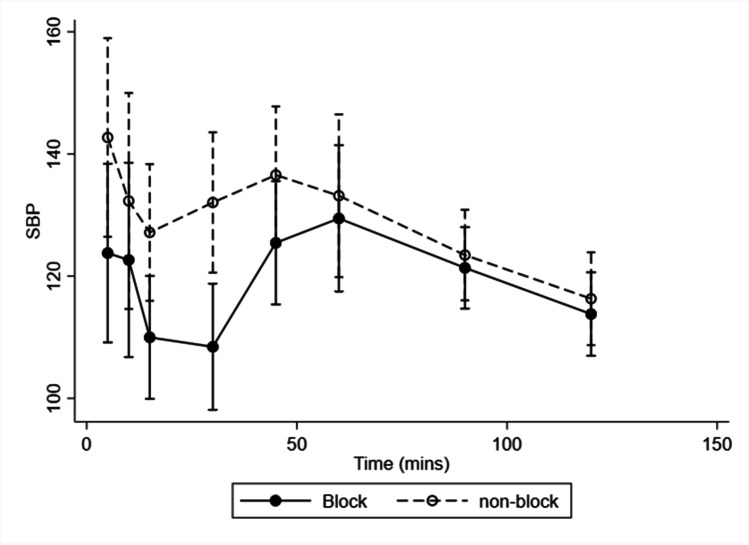
The duration of surgical time ranged from 60 to 180 min, with a mean of 115 min with standard deviation of 27 min. The time to performing the block varied from 3 to 26 min with mean value of 7.9 min and standard deviation of 4.4 min. Heart rate (HR): Heart rate in both the test and control groups decreased marginally (mean of 3 beats), which did not reach statistical significance (p = 0.36). Systolic blood pressure (SBP): There was a statistically significant reduction in the SBP in group-1 (p = 0.03) (Fig. 2). Diastolic and mean blood pressure (DBP/MBP): Did not show any clinical or statistical significance in both groups.
Fig. 2.
Systolic blood pressure
Postoperative Data
Pain Score: None of the patients required rescue analgesia with morphine in the ward, as the NRS score did not cross 4/10 in both the groups and did not show any statistical difference (p = 0.56) between both the groups in the first 18 h. Paracetamol was continued every 6 h as per protocol.
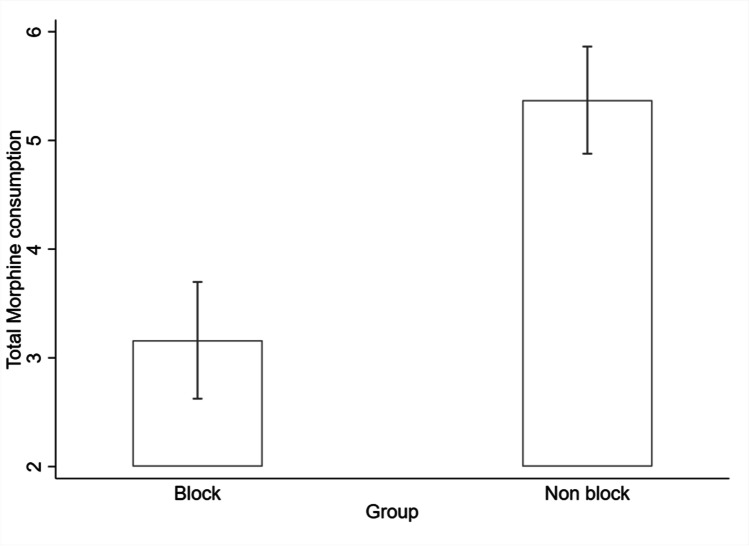
Total Morphine Consumption: The study showed that the mean total morphine dose given to test group was significantly lesser than that of the control group (p = 0.0001). However, there was no difference in fentanyl consumption. Figure 3 shows a significant reduction in the consumption of morphine, in the block group, than the control group, during the initial 18 h postoperatively (p = 0.001).
Fig. 3.
Total morphine consumption
The postoperative HR and SBP were not significant.
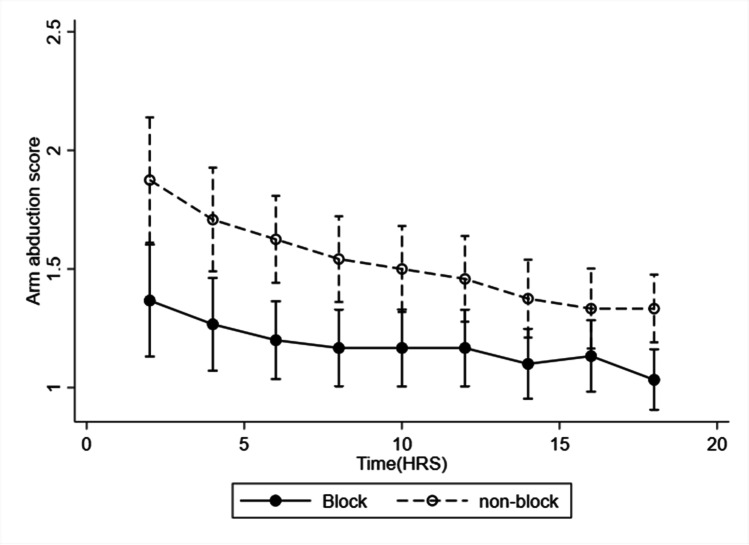
Arm Abduction Score (Fig. 4): p value for group 1 = 0.001. p value time = 0.0001: Interaction P G × T = 0.13.
Fig. 4.
Arm abduction score
Although the arm abduction score is assessed as A, B, and C, for the purpose of calculating the statistical significance, it was marked as 1, 2, and 3, respectively. Mean and confidence interval were measured for systolic blood pressure and arm abduction score and median and confidence interval for total morphine consumption. None of the patients reported symptoms of chronic pain or cancer recurrence in the stipulated time of six months follow-up [12].
Discussion
Although, by definition, cancer patients should be categorized as ASA II, as they have a systemic illness, for practical clinical practice and research purposes, this non-specific preoperative risk assessment tool is still utilized. First introduced in 1941, the American Society of Anesthesiologists Physical Status (ASA-PS) cannot serve as a direct indicator of perioperative risk indicator for most cancer patients and should be combined with other preoperative classification systems, depending on the stage of cancer, associated comorbidities, and surgical dissection [13]. With the advent of ultrasound in regional anesthesia and several cadaveric studies, new myofascial plane blocks have emerged, with promising evidence for safer, effective, and satisfying outcomes, one of which is the PECS block [14]. With emphasis on enhanced recovery protocols, the shift in the perioperative care is to provide multi-modal opioid-sparing analgesia, minimally invasive surgical techniques, quicker mobility, and lower levels of intravenous fluid administration. Furthermore, there is growing evidence anesthetic techniques play a role in cancer recurrence through immunological and stress-related mechanisms; nevertheless, more research is warranted in these areas [15].
Paravertebral block is well studied and utilized, however, they may result in serious complications, such as, vascular puncture (3.8%), hypotension (4.6%), pleural puncture (1.1%) and pneumothorax (0.5%), Horner’s syndrome, epidural spread and spinal cord trauma [16]. Nevertheless, it is still advocated for its advantages [17]. Cadaveric dissection along with contrast study has demonstrated the spread of the local anesthetic into the axilla [18]. While the first-level PECS-I block targets the medial and lateral pectoral nerves, the second-level PECS-II block covers one to six thoracic intercostal nerves, mainly the lateral cutaneous branches as the anterior cutaneous branches of the same cannot be approached by the local anesthetic with the barrier of the external and internal intercostal muscles. Additionally, there is sparing of the supraclavicular nerve, which is a branch of the superficial cervical plexus. These nerves will need a separate approach to the injection. This accounts for the drawbacks of PECS block [19]. Notably, in our study, there were only minor, not significant differences in the heart rate (mean of 3 beats). Heart rate and blood pressure are the most relevant indicators of pain and can reflect intraoperative pain. Warrén et al. had concluded that although these variables may be frequent indicators to pain they are not necessarily precise, due to other changes in sympathetic responses, such as, inadequate depth of anesthesia, intraoperative blood loss, or patients on beta blockers [20]. Yet in outweighing the risk of post-traumatic stress disorder, these indirect variables must be treated accordingly [21]. There was a statistically significant (p = 0.03) reduction in systolic blood pressure in group-1. There was no significant change noted in the diastolic blood pressure or mean arterial pressure in the two groups. This is in line with the study reported by Manzoor et al. [22]. Their study patients were under general anesthesia with PEC-I and II, one group got bupivacaine versus bupivacaine with dexmedetomidine for the other group, which recorded no statistical difference in intraoperative blood pressure or heart rate at baseline, at surgical incision, and at 10-min interval until completion of surgery. This may be related to the dexmedetomidine used for block. Postoperatively, the NRS has shown high correlations as compared to other pain assessment tools [23]. Furthermore, our study demonstrated that none of the patients required rescue morphine in the postoperative ward, as the scores were well within 4/10, even up to the first 18 h, in both groups. This could be due to patients in both groups receiving adequate paracetamol, as per protocol. Bashandy et al. [11], who studied the beneficial effects of PECS block versus general anesthesia, documented that VAS scores and morphine-fentanyl consumption in the PECS group stayed significantly lower than that in the control group, at 3 h and 24 h postoperatively. Postoperative arm abduction is considered as reflecting persistent postoperative pain particularly in breast surgery. Our study showed a statistically significant difference in the range of arm abduction in PECS group as compared to control group for 18 h postoperatively. This result was similar to the RCT done by Kim et al., GA and PEC-II [19]. We used the Functional Activity Score, which is categorized as A, B, and C, to measure as the arm abduction score, inferred as 1, 2, and 3, to depict statistical information [10]. Median NRS of the axillary pain during abduction was significantly lower than the control group between groups (p ≤ 0.001), for the first 24 h. In the RCT of Wang et al., the PECS group showed favorable shoulder abduction during the recovery period [24]. Our study demonstrated a mean time taken for the block was only 7.9 min and it was technically simple to perform. The PECS block did not record any complications, and was safe, with a potential to reduce persistent pain after breast surgery, which has an incidence of up to 60% following poorly treated acute pain and 10% for up to one year [25]. A single blocking method would not provide adequate analgesia in the entire breast area, which would require combination of blocks, due to the multiple innervation of the breast [26].
Recent Advances
The utility of this newly developed block is increasingly supported by the scientific evidence in favor of its use due to its safety and simplicity [27]. It has demonstrated significant opioid-sparing effects when administered for breast surgery, both intraoperatively and up to 24 h postoperatively [28]. Precautions should be taken as for any regional anesthetic procedure, due to the risk of hematoma formation, especially for patients on anticoagulant and antiplatelet drugs [29]. Systematic reviews and meta-analysis guidance with procedure-specific postoperative pain management (PROSPECT), demonstrating recommendations for optimal pain management after oncological breast surgery, suggest preoperative gabapentin, dexamethasone, intraoperative paravertebral or PECS block, or wound infiltration, along with basic analgesics, such as paracetamol and non-steroidal anti-inflammatory drugs and opioids only as rescue analgesia in the postoperative period [30].
The limitations in this study are as follows: Firstly, the intervention arm is not blinded and hence the outcome measurements have been influenced by the observer (measurement bias), as the same person gave the block and also measured intraoperative outcomes. However, postoperative measurements were taken by a different observer (pain nurses), who was unaware of the allocation into test and control groups. Secondly, PECS was performed under general anesthesia. Hence, dermatome distribution or quality of block could not be assessed before surgery. Thirdly, the shoulder range of motion was not assessed by a standardized method using universal full circle manual goniometer under the guidance of dedicated physiotherapist and hence inter-observer variation could have occurred in the measurement.
Conclusion
Our research backs up current thinking in perioperative medicine, regional anesthesia, and pain management. The findings showed that a two-level PECS block is safe, effective, dependable and simple to perform in breast cancer surgery, reducing morphine consumption, improving postoperative pain and increasing patient satisfaction, thereby, achieving the primary outcome. As with the secondary outcome, there were no reported cases with symptoms of chronic pain or cancer recurrence, therefore, no conclusive inference but certainly contributing to the evidence towards the same.
Author Contribution
All the authors contributed to the conduct of the study, collection, compiling of data, literature search, and writing of the paper. The manuscript has not been published and is not under consideration for publication in any other journal. All the authors approved the manuscript and its submission to the journal, and the authors have not published or submitted any related papers from the same study.
Funding
As per institutional provision approved by the review board.
Declarations
Consent to Participate
taken from all patients.
Consent for Publication
agreed by all the authors.
Institutional Review Board Approval Number
IRB Min. No:10390[INTERVEN] dated 30.11.2016.
Conflict of Interest
The authors declared no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Importance of the Study and Research Question Answered
Advances in Knowledge This original study was conducted in one of the premiere, over a century old, medical educational and research institutions of the country. It adds to the evidence of ongoing quest to determine ideal breast analgesia, with the use of PECS block, by reduction in opioid consumption, lower pain scores, early functionality, and discharge in the time period studied. Our study proved the safety and efficacy of this easily usable block, which advocates many practitioners, in perioperative care, to use it under the set safety guidelines.
Application to Patient Care There is significant incidence of acute and chronic postoperative pain with oncological breast surgery. Providing clinicians with an evidence-based approach, for better patient care to improve perioperative outcome and patient satisfaction, is certainly beneficial with the use of PECS block, among other modalities for analgesia.
Contributor Information
Roshan K. Kurien, Email: roshan.kurien@gmail.com
Serina Ruth Salins, Email: serinaruthsalins@gmail.com.
Paul Mazhuvanchary Jacob, Email: mjpaul@cmcvellore.ac.in.
Kurien Thomas, Email: kurien123@gmail.com.
References
- 1.GLOBOCAN 2020: New Global Cancer Data | UICC [Internet]. [cited 2021 Jul 17]. Available from: https://www.uicc.org/news/globocan-2020-new-global-cancer-data
- 2.Human Development Report (2020) internet, hdr2019.pdf [Internet]. [cited 2021 Jul 20]. Available from: http://hdr.undp.org/sites/default/files/hdr2019.pdf
- 3.Plesca M, Bordea C, El Houcheimi B, Ichim E, Blidaru A. Evolution of radical mastectomy for breast cancer. J Med Life. 2016;9(2):183–186. [PMC free article] [PubMed] [Google Scholar]
- 4.Thakur V, Kutty RV. Recent advances in nanotheranostics for triple negative breast cancer treatment. J Exp Clin Cancer Res CR. 2019;38(1):430. doi: 10.1186/s13046-019-1443-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tait RC, Zoberi K, Ferguson M, Levenhagen K, Luebbert RA, Rowland K, et al. Persistent post-mastectomy pain: risk factors and current approaches to treatment. J Pain Off J Am Pain Soc. 2018;19(12):1367–1383. doi: 10.1016/j.jpain.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun Y, Li T, Gan TJ. The effects of perioperative regional anesthesia and analgesia on cancer recurrence and survival after oncology surgery: a systematic review and meta-analysis. Reg Anesth Pain Med. 2015;40(5):589–598. doi: 10.1097/AAP.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 7.Calì Cassi L, Biffoli F, Francesconi D, Petrella G, Buonomo O. Anesthesia and analgesia in breast surgery: the benefits of peripheral nerve block. Eur Rev Med Pharmacol Sci. 2017;21(6):1341–1345. [PubMed] [Google Scholar]
- 8.Blanco R. The ‘pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66(9):847–848. doi: 10.1111/j.1365-2044.2011.06838.x. [DOI] [PubMed] [Google Scholar]
- 9.Andersen KG, Duriaud HM, Kehlet H, Aasvang EK. The relationship between sensory loss and persistent pain 1 year after breast cancer surgery. J Pain Off J Am Pain Soc. 2017;18(9):1129–1138. doi: 10.1016/j.jpain.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 10.Macintyre PE, Schug SA. Acute pain management: a practical guide. 2015
- 11.Bashandy GMN, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015;40(1):68–74. doi: 10.1097/AAP.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 12.Items where Subject is ‘MEDICAL > Anaesthesiology’ - EPrints@Tamil Nadu Dr MGR Medical University [Internet]. [cited 2020 Nov 3]. Available from: http://repository-tnmgrmu.ac.in/view/subjects/MEDICAL26.html#group_R
- 13.F R, Ap T, G Q, F G, C F, L S, et al. The impact of preoperative ASA-physical Status on postoperative complications and long-term survival outcomes in gastric cancer patients [Internet]. Vol. 23, European review for medical and pharmacological sciences. Eur Rev Med Pharmacol Sci; 2019 [cited 2020 May 29]. Available from: https://pubmed.ncbi.nlm.nih.gov/31539125/ [DOI] [PubMed]
- 14.Garg R, Bhan S, Vig S. Newer regional analgesia interventions (fascial plane blocks) for breast surgeries: review of literature. Indian J Anaesth [Internet]. 2018 Jan 4 [cited 2020 Jul 18];62(4):254. Available from: http://www.ijaweb.org/article.asp?issn=0019-5049;year=2018;volume=62;issue=4;spage=254;epage=262;aulast=Garg;type=0 [DOI] [PMC free article] [PubMed]
- 15.Cata JP. Outcomes of regional anesthesia in cancer patients. Curr Opin Anaesthesiol. 2018;31(5):593–600. doi: 10.1097/ACO.0000000000000636. [DOI] [PubMed] [Google Scholar]
- 16.Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postoperative analgesia after radical mastectomy: a randomized controlled trial†. Br J Anaesth [Internet]. 2016 Sep 1 [cited 2020 May 31];117(3):382–6. Available from: http://www.sciencedirect.com/science/article/pii/S000709121733800X [DOI] [PubMed]
- 17.Syal K, Chandel A. Comparison of the post-operative analgesic effect of paravertebral block, pectoral nerve block and local infiltration in patients undergoing modified radical mastectomy: a randomised double-blind trial. Indian J Anaesth. 2017;61(8):643–648. doi: 10.4103/ija.IJA_81_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de la Torre PA, Jones JW, Álvarez SL, Garcia PD, de Miguel FJG, Rubio EMM, et al. Axillary local anesthetic spread after the thoracic interfacial ultrasound block - a cadaveric and radiological evaluation. Rev Bras Anestesiol. 2017;67(6):555–564. doi: 10.1016/j.bjan.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Kim D-H, Kim S, Kim CS, Lee S, Lee I-G, Kim HJ, et al. Efficacy of pectoral nerve block type ii for breast-conserving surgery and sentinel lymph node biopsy: a prospective randomized controlled study. Pain Res Manag. 2018;2018:4315931. doi: 10.1155/2018/4315931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stomberg MW, Sjöström B, Haljamäe H. Assessing pain responses during general anesthesia. AANA J. 2001;69(3):218–222. [PubMed] [Google Scholar]
- 21.Fiedler MA. Assessing pain responses during general anesthesia. AANA J. 2001;69(5):361. [PubMed] [Google Scholar]
- 22.Manzoor S, Taneja R, Sood N, Puri A, Kadayaprath G. Comparative study to assess the quality of analgesia of bupivacaine and bupivacaine with dexmedetomidine in ultrasound-guided pectoral nerve block type I and II in breast surgeries. J Anaesthesiol Clin Pharmacol [Internet]. 2018 [cited 2020 May 31];34(2):227–31. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6066886/ [DOI] [PMC free article] [PubMed]
- 23.Closs SJ, Barr B, Briggs M, Cash K, Seers K. A comparison of five pain assessment scales for nursing home residents with varying degrees of cognitive impairment. J Pain Symptom Manage. 2004;27(3):196–205. doi: 10.1016/j.jpainsymman.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 24.Wang K, Zhang X, Zhang T, Yue H, Sun S, Zhao H, et al. The Efficacy of ultrasound-guided type II pectoral nerve blocks in perioperative pain management for immediate reconstruction after modified radical mastectomy: a prospective, randomized study. Clin J Pain. 2018;34(3):231–236. doi: 10.1097/AJP.0000000000000529. [DOI] [PubMed] [Google Scholar]
- 25.Fecho K, Miller NR, Merritt SA, Klauber-Demore N, Hultman CS, Blau WS. Acute and persistent postoperative pain after breast surgery. Pain Med Malden Mass. 2009;10(4):708–715. doi: 10.1111/j.1526-4637.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- 26.Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: a qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017;42(5):609–631. doi: 10.1097/AAP.0000000000000641. [DOI] [PubMed] [Google Scholar]
- 27.Bartakke DAA, Varma DMK (2019) Analgesia for breast surgery — a brief overview 7
- 28.Singh PM, Borle A, Kaur M, Trikha A, Sinha A. Opioid-sparing effects of the thoracic interfascial plane blocks: a meta-analysis of randomized controlled trials. Saudi J Anaesth [Internet]. 2018 Jan 1 [cited 2020 Jul 18];12(1):103. Available from: http://www.saudija.org/article.asp?issn=1658-354X;year=2018;volume=12;issue=1;spage=103;epage=111;aulast=Singh;type=0 [DOI] [PMC free article] [PubMed]
- 29.Ueshima H, Otake H. Ultrasound-guided pectoral nerves (PECS) block: complications observed in 498 consecutive cases. J Clin Anesth. 2017;42:46. doi: 10.1016/j.jclinane.2017.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Jacobs A, Lemoine A, Joshi GP, Van de Velde M, Bonnet F. PROSPECT guideline for oncological breast surgery: a systematic review and procedure‐specific postoperative pain management recommendations. Anaesthesia [Internet]. 2020 May [cited 2021 Feb 13];75(5):664–73. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7187257/ [DOI] [PMC free article] [PubMed]