Abstract
A reverse transcription-PCR (RT-PCR)–enzyme-linked immunosorbent assay system that detects a relatively conserved region within the RNA genome of all seven serotypes of foot-and-mouth disease virus (FMDV) has been developed. The high specificity of the assay is achieved by including a rapid hybridization step with a biotin-labeled internal oligonucleotide. The assay is highly sensitive, fast, and easy to perform. A similar assay, based on a highly variable region of the FMDV genome and employing a single asymmetric RT-PCR and multiple hybridization oligonucleotides, was developed to demonstrate the method's ability to type FMDV. Based on our theoretical and practical knowledge of the methodology, we predict that similar assays are applicable to diagnosis and strain differentiation in any system amenable to PCR amplification.
Foot-and-mouth disease (FMD) is an Office International des Épizooties list A disease that can affect all cloven-hoofed animals. FMD virus (FMDV) belongs to the Aphthovirus genus (of the Picornaviridae family) (6) and is considered to be the most contagious agent of infection of domestic animals. FMDV infects many different species and is excreted at high levels. The virus can be transmitted by multiple routes, including contaminated fomites and infected animals and products as well as by wind-borne transmission (aerosol). An important factor in virus spread is the short generation time of FMDV (2, 15, 16).
FMDV can establish a persistent or carrier stage in ruminants, but for pigs, only acute infection has been described (36, 43). It appears that if pigs are infected using an appropriate isolate, dose, and route (i.e., around 104 to 105 50% tissue culture infective doses [TCID50s] by the oral route and perhaps as few as 100 TCID50s [depending on the strain of FMDV] by heel pad inoculation), the virus will replicate rapidly and to high titers (8, 38). Very young animals may die from FMDV-induced myocarditis; however, most animals will survive and, in pigs, the immune system will clear the infection within 1 to 3 weeks (7, 16, 17, 36, 41, 43).
Clinical diagnosis of FMD may be difficult, especially for sheep and goats, in which clinical signs are often mild (3, 12). Furthermore, several other vesicular virus infections, including those caused by swine vesicular disease (SVD) virus, vesicular stomatitis virus, and others, cannot be distinguished from FMDV infection by the clinical findings. Thus, definitive diagnosis must be carried out at specialized laboratories and, due to the rapid spread of the infection, diagnosis must be fast, sensitive, and specific. Traditionally, laboratory diagnosis is achieved by enzyme-linked immunosorbent assay (ELISA) detection of specific FMDV antigens from epithelial tissue suspensions, often accompanied by concurrent cell culture isolation (19, 20, 22, 34). ELISA is performed on epithelial suspensions and on tissue culture supernatants to determine the serotype of the virus. Recently, reverse transcription-PCR (RT-PCR) assays for diagnosis of FMDV infection have been developed. Although various protocols have been published, none seem to have sufficient sensitivity, specificity, and robustness for diagnostic work unless backed up by other techniques (30, 31). RT-PCR assays for serotyping of FMDV have been published, but the protocols are excessively labor-intensive (9, 25, 30, 31, 33, 40, 42).
The aim of this study was to develop a rapid, sensitive, and specific assay suitable for routine FMDV diagnosis. To achieve this, we improved the RT-PCR steps to increase sensitivity and, furthermore, included a novel simple and aqueous-phase (SNAP) hybridization step to obtain optimal specificity within an easy and fast assay. Additionally, we show an example of the adaptation of this assay to a more variable region of the virus [within VP1 (1D)] and used SNAP hybridization with multiple oligonucleotide probes to demonstrate “proof of concept” for a fast and focused method for preliminary typing of FMDV isolates.
MATERIALS AND METHODS
Cells and virus.
Primary bovine calf thyroid (BTY) cells and porcine cell line IB-RS-2 cells were used for virus isolation as described previously (31, 32). Virus isolates were either original suspensions from epithelial lesions or virus stocks submitted to and stored at the Office International des Épizooties/FAO World Reference Laboratory for Foot-and-Mouth Disease (WRL) at Pirbright. All virus-containing materials had previously been serotyped by antigen detection ELISA as previously described (19, 20, 22, 34).
RNA extraction.
RNA samples consisted of total RNA extracted from original epithelial suspensions or from cell culture supernatants. Total RNA was extracted by the TRIzol method as described previously (30, 31).
PCR amplification.
RT-PCR was performed using different combinations of primers. The sequences and locations of primers from within the 5′ untranslated region (UTR) as well as from the VP1 (1D) region of FMDV are shown in Table 1 and in Fig. 1A. Upstream primers were commercially labeled (MWG Biotech) with digoxigenin (DIG) or fluorescein isothiocyanate (FITC) at the 5′ end. Downstream primers were unlabeled or, in certain instances, were commercially 5′ end labeled with biotin (MWG Biotech). The specific primers used in the experiments, as well as any additional control combinations, are named in the Results section. The numbering system used for the primers specific for Internal Ribosome Entry Site (IRES) (6) and for the VP1 region (using primers P1 and P2 [1] and primers internal to these) is based on consensus alignment, full-length FMDV genomes using the published FMDV O1 Kaufbeuren (O1Kauf) sequence (5, 44) from GenBank (accession no. X00871) as the backbone and with an additional 387 bases added, of which 368 bases were at the extreme 5′ end, 1 base (nucleotide [nt] 512) was inserted in the 5′ region before the IRES region, 2 bases (nt 873 and 1007) were inserted in the IRES region, as were another 3 bases inserted at nt 2995 to 2997, 3 bases were inserted in the P1-P2 primer region (nt 3845 to 3847), and finally 10 A's were added to the extreme 3′ end (nt 8187 to 8196). These base additions and insertions were made to the consensus sequence on the basis of comparison to other FMDV sequences available in GenBank (accession no. X00871, AJ007347, AJ007572, X74812, AF154271, and M10975) in order to make it a universal FMDV numbering system. Thus, the consensus is in regards to the numbering of nucleotides, not the actual sequence.
TABLE 1.
Primers used for the RT-PCRa
| Primer | Sequence (5′ to 3′) | Location |
|---|---|---|
| P1 | CCTACCTCCTTCAACTACGG | Corresponds to FMDV nt 3737–3756 |
| P2 | GAAGGGCCCAGGGTTGGACTC | Complementary to FMDV nt 3955–3935 |
| IRES 1 | CCTGGTCTTTCCAGGTCTAGA | Corresponds to FMDV nt 667–687 |
| IRES 2 | CCTCCTTGGTAACAAGGACCC | Corresponds to FMDV nt 790–810 |
| IRES 3 | CCTTCTCAGATCCCGAGTGT | Complementary to FMDV nt 987–968 |
| IRES 4 | CCTATTCAGGCGTAGAAGCTT | Complementary to FMDV nt 1042–1022 |
Certain primers were also used as SNAP capture probes (see text).
FIG. 1.
(A) Schematic representation of the FMDV genome showing the principal features. The localization of the IRES region and the P1-P2 primer region as well as the areas used for SNAP probes are shaded. (B) Direct RT-PCR ELISA using dual labeling of the PCR product with either FITC (IRES1) or DIG (P1) together with biotin-labeled IRES4 or P2, respectively. RT-PCR products were directly bound to streptavidin plates and subjected to ELISA. OD readings are shown. Three FMDV-infected samples (O, C, and Asia 1) as well as a negative control were assayed. Nested PCR was performed as described in Materials and Methods. Negative-control samples yielding a spurious weak positive reaction in the ELISA are indicated (<).
The sensitivity of the RT-PCR based on the IRES region primers was maximal when using random hexamers and TaqMan Gold RT-PCR kit reagents (technical information; PE Applied Biosystems, Warrington, Cheshire, United Kingdom) together with FITC-labeled IRES2 upstream primer and unlabeled IRES4 downstream primer, both at 0.2 μM. After the reverse transcriptase step (50 mM KCl, 10 mM Tris [pH 8.3], 5.5 mM MgCl2, 0.5 mM concentrations of each deoxynucleoside triphosphate [dNTP], 2.5 μM random hexamers, and 4 U of RNase inhibitor and 25 U of Multiscribe RT per 10 μl of reaction mixture), the PCRs were set up in separate tubes using the cDNA corresponding to 1 to 5 μl of cDNA reaction mixture and TaqMan Gold reagents as described by the manufacturer (50 mM KCl, 10 mM Tris [pH 8.3], 5.5 mM MgCl2, 0.2 mM concentrations of each dNTP, 200 nM primers, and Amplitaq Gold enzyme [1.25 U per 50-μl reaction mixture]) (technical information; PE Applied Biosystems). After activation of the AmpliTaq Gold DNA polymerase, the PCRs were taken through a two-step amplification protocol at 95°C for 15 s and 60°C for 1 min for 40 cycles. Samples of amplified DNA were run on 1 or 2% agarose gels in Tris-borate-EDTA buffer.
In some experiments (indicated in Results), slightly different protocols were used, such as nested PCR performed for another 30 cycles on 1-μl samples from the first PCR amplification using internal primers and standard conditions. The amplification strategy for the P1-P2 primer region (VP1) was essentially as described previously (1, 30, 31) except that the upstream P1 primer was DIG labeled and the unlabeled downstream P2 primer was used at a 10- to 100-fold lower concentration (normal primer concentration was 200 nM, so downstream primer concentration was at 2 to 20 nM) to produce a primarily single-stranded (positive sense) PCR product (asymmetric PCR).
SNAP capture probes.
Oligonucleotides used as SNAP capture probes are shown in Table 2 and in Fig. 1A. For the IRES region, the highly conserved IRES3 oligonucleotide, 5′-end labeled with biotin, was used (Table 1). For typing of the VP1 region, a number of oligonucleotides were designed based on available data in public databases (GenBank). These oligonucleotide probes were produced as the negative sense strand and commercially labeled with biotin at the 5′ end (MWG Biotech).
TABLE 2.
5′-biotin-labeled (MWG Biotech) primers used for SNAP hybridization of the VP1 region
| Designation (short name) | Sequence (5′ to 3′) | Complementary to sequence (serotype): |
|---|---|---|
| O1Kauf3777 (O1K-1) | CCGGTAAAGCAACTCGGTGA | nt 3777–3796 (O1Kauf) |
| O Taiwan3777 (O Tai-1) | TCTGTAGAGTAGTTCAGTAA | nt 3777–3796 (O Taiwan) |
| A22-3777 (A22-1) | GCGCACGAGGAGCTCGTGGA | nt 3777–3796 (A22) |
| C3-3777 (C3-1) | GCGCACAAGCAGTTCTGTGA | nt 3777–3796 (C3) |
| Asia 1-3777 (Asia 1-1) | GCGGATCAACAGCTCCGTGA | nt 3777–3796 (Asia 1) |
| O1 Kauf3800 (O1K-2) | ACAGTATGTTTCGGCCCTCTT | nt 3800–3820 (O-Kauf) |
| C/A3800 (C/A-2) | GCAGTAGAGTTCAGCACGCTT | nt 3800–3820 (C and A) |
| Asia 1-3800 (Asia 1-2) | GCAGTATGTCTCCGCACGCTT | nt 3800–3820 (Asia 1) |
SNAP hybridization and ELISA procedure.
SNAP capture probes at a concentration of 10 pmol/μl of water were added to 200-μl 96-well PCR plates in a volume of 1 to 2 μl. For certain experiments, up to 5 μl of the probe was used or the concentrations of the probes were increased to 100 pmol/μl. However, the most consistent results were obtained using 2 μl (i.e., 20 pmol) per well. For the IRES-specific assay, the probe (IRES3-biotin) was added to all wells except blanks, while for the VP1 typing, each of the eight oligonucleotides was added to a single row (11 wells, the 12th well being a blank). Thus, the IRES detection assay could accommodate 88 samples per plate while the VP1 assay allowed the analysis of 11 samples with up to eight probes. After applying the capture probe to the wells, the plates were wrapped in tissue paper and kept at 4°C until used. The 2-μl aliquot dried out in 1 to 2 days, and the oligonucleotides remained stable for long periods when stored dry at 4°C. In the experiments described, plates were stored in this way for up to 2 weeks without any adverse effects. Aliquots of PCR products (2 to 10 μl, usually 3 μl) were directly added to the wells of the preloaded probe wells. The plates were then covered, placed in a thermocycler, and heated to 95°C for 5 min and then cooled to the annealing temperature for 5 min. The annealing temperature may differ for each capture probe, and the optimal temperature for the IRES assay was determined to be 55 to 60°C. The multiple capture probes for the VP1 area had variable melting temperatures and were tested at various temperatures. The optimal temperature for the series 3777 probes (Table 2) was 40 to 45°C while the optimal temperature for the 3800 series (Table 2) was 60 to 65°C. After the annealing step, ELISA diluent buffer (phosphate-buffered saline [PBS] without Ca++ and Mg++, with 0.05% Tween 20 and 0.1% bovine serum albumin; 200 μl) was immediately added to the wells and the material was transferred to streptavidin-coated ELISA plates (Boehringer). Plates were shaken at 37°C for 10 to 15 min and washed three times in PBS–0.1% Tween 20, and the captured product (biotinylated probe bound to the DIG- or FITC-labeled PCR product) was detected by adding a 1:2,000 dilution of anti-DIG-peroxidase (POD) or anti-FITC-POD conjugate (Boehringer) in ELISA diluent (200 μl) followed by incubation for up to 30 min at 37°C with shaking followed by three washes as above. ABTS [2,2′-azinobis(3-ethylbenzthiazolinesulfonic acid] substrate (Boehringer) was added, and incubation continued with shaking at 37°C for 5 to 60 min. Plates were read at 405 nm.
RESULTS
Direct RT-PCR ELISA for FMDV.
Initially, an RT-PCR–ELISA system was developed to be capable of detecting the RNA from all seven serotypes of FMDV using primers from conserved regions of the IRES region (within the 5′ UTR). The technique was sensitive, but the system was not sufficiently specific for routine application (21). The problem with this direct assay was that any product containing both 5′-(label)-end primer and 3′-(biotin)-end primer was bound and detected in the ELISA. This included any potential primer-dimer formation as well as any mispriming that linked the two primers during PCR. These problems are demonstrated in Fig. 1B, where, although the IRES primers apparently worked well in the direct PCR, the background reactivity could be high when sensitivity was increased by, in this example, performing a nested PCR assay. It was also apparent that the P1 and P2 primers produced a high background from negative samples even in the standard RT-PCR. Based on these findings, a specific hybridization step was introduced by using an internal oligonucleotide between the RT-PCR and the ELISA step in order to overcome any nonspecific reaction. Typically, such a hybridization step is performed by alkaline denaturation of the PCR product, followed by dilution and neutralization in a relatively large volume of hybridization solution containing the internal oligonucleotide probe. Furthermore, the hybridization is often performed on streptavidin-coated plates, which converts the assay into a solid-phase hybridization. Thus, the procedure using conventional methods is labor-intensive and slow (the hybridization step alone is around 3 h). Therefore, theoretical and practical considerations led us to develop a very simple and very efficient hybridization step, termed SNAP hybridization. A schematic outline of the method is shown in Fig. 2.
FIG. 2.
Schematic representation of the SNAP procedure. The primers used for the PCR step are indicated (●, DIG or FITC label), as is the SNAP oligonucleotide (■, biotin labeled) used for capture of the specific product onto the streptavidin (S)-coated ELISA plate. Final detection is in a standard ELISA format using peroxidase-labeled (POD) antibody.
Efficiency of SNAP hybridization.
The efficiency of hybridization in the SNAP procedure was estimated by performing RT-PCR amplification with DIG-labeled IRES1 primer and biotin-labeled IRES4 primer. The ELISA was then performed on aliquots of these PCRs and developed using anti-DIG antibody. Subsequently, a sample of the same PCR material was subjected to the SNAP hybridization using FITC-labeled IRES2 oligonucleotide. The ELISA was then performed using anti-FITC antibody. The ratio between the signals obtained using anti-DIG and anti-FITC antibodies was used to estimate the amount of product captured by the probe (both ELISAs were done at optimal antibody dilution). Three FMDV samples, of types O, C, and Asia 1, and one noninfected cell culture control as well as water were included in the experiment and were tested three times. The results indicated that the specific signal after hybridization was generally up to 90% of the total input signal. In contrast, the nonspecific signal (using negative controls or an unrelated primer) was less than 1%. After these initial experiments, other experiments (more than 20) confirmed that the nonspecific background signal was normally very low (i.e., one to two times that of background).
Optimization of the IRES RT-PCR.
The IRES RT-PCR assay described above produced a fragment with around 450 bases. In order to improve the sensitivity of the assay without a nested PCR system, an alternative primer set (IRES2 and IRES4) with relatively high and similar melting temperatures, making them useable in high temperature protocols, was used. PCR with these primers produced a fragment with around 250 bp and showed improved sensitivity when used in high-temperature hot-start PCR using RT and Amplitaq GOLD RT-PCR reagents (PE Applied Biosystems). The most consistent and sensitive system used these reagents and a two-step protocol for 40 cycles. These changes resulted in a sensitivity increase of around 100-fold greater than a preliminary protocol previously used in our laboratory (21), and thus, the final sensitivity of the combined RT-PCR oligo-ELISA was around 0.2 TCID50s (in BTY cells) or around 20 molecules of RNA, assuming approximately 100 genomes per TCID50 (S. Alexandersen, unpublished data).
The RT-PCR products on agarose gels and the SNAP ELISA readings obtained in representative assays with all seven serotypes of FMDV are shown in Fig. 3. The IRES primers were designed to be specific for regions of sequence that are highly conserved among different FMDV isolates. The primers used on cell culture samples in this study have previously been shown to work well with samples from experimentally infected animals (21), and data obtained using other IRES primers indicate that this part of the genome is very suitable for the RT-PCR diagnosis of FMDV from clinical samples submitted to the WRL (32a). Thus, this IRES-specific RT-PCR with SNAP hybridization-ELISA shows great promise as a fast, highly sensitive, and specific test useful for diagnostic work on clinical samples.
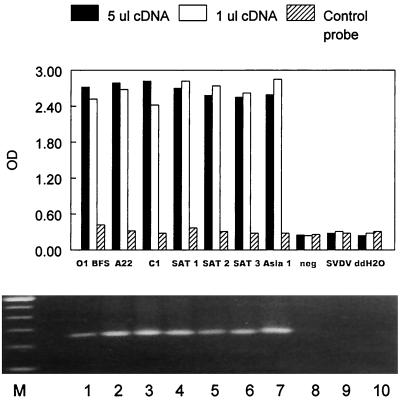
FIG. 3.
SNAP probing ELISA. RT-PCR amplification was performed using the optimized protocol on the IRES region with FITC-labeled IRES2 primer and unlabeled IRES4 primer. The SNAP capture probe was IRES3-biotin. As a control, capture probe P2-biotin was used. RNA samples were derived from cells infected with all seven FMDV serotypes (O, A, C, Asia 1, SAT 1, SAT 2, and SAT 3) and various negative controls (uninfected cells, SVD virus-infected cells, and ddH2O) were also included. Two samples from each isolate were analyzed using 1 or 5 μl of the cDNA reaction mixtures from total RNA isolated from cell cultures. The RT-PCR products of the 1-μl samples were also electrophoresed into agarose gels and stained with ethidium bromide. Lanes: M, size marker; 1 to 7, the seven serotypes of FMDV; 8, negative cell culture; 9, SVD virus in cell culture; 10, ddH2O negative control. The products are around 250 bp.
Development of an assay with the potential to type FMDV isolates.
The method described above used a highly conserved region of the FMDV genome and a single SNAP capture probe capable of binding to cDNA from all seven serotypes of FMDV. However, we reasoned that if we amplified and probed for a highly variable region, the method should theoretically be able to distinguish between FMDV isolates. For FMDV, the VP1 (1D) region is highly variable and is thought to play a major role in defining serogroup specificity and protective immunity. Furthermore, the region has been extensively sequenced and isolates have been classified based on their VP1 sequence (1, 5, 13, 23, 24, 26–28, 35, 37, 39). Primers designed for this region for RT-PCR assays to serotype FMDV isolates have had variable success (9, 31, 42). Thus, to show proof of concept we used the conserved primers P1 and P2, which amplify a 216-bp fragment of VP1 and which in regular RT-PCRs detect most types O, A, and Asia 1 isolates of FMDV (the most common types) as well as some C, SAT 1, SAT 2, and SAT 3 types (S. M. Reid, unpublished results) in conjunction with a set of selected internal hybridization probes designed to distinguish between certain virus isolates. Sequences of around 25 FMDV isolates that span this region and that are accessible in the public databases (GenBank) were grouped by serotype and were aligned. Most attention focused on serotype O, as it had the most available sequence information. Only a few sequences were available for serotypes A, C, and Asia 1. Furthermore, the SAT serotypes were excluded from the primer design due to lack of sufficient sequence information. However, the probes used here were sufficient to demonstrate the proof of concept for the methodology and indicate the path for further developments. The alignments of all sequences indicated that the 216-nt P1-P2 primer region contained two regions potentially useful for the mapping assay. The region at nt 3800 to 3820 (Table 2) was the most conserved, and thus a capture probe was designed to primarily detect FMDV type O, another was designed to detect types A or C (almost identical in this region), and a third probe was designed primarily to detect Asia 1 (Table 2). It should be noted that there was some degree of variability within the serotypes, but that the variabilities across serotypes were higher. This difference was used to make the assay more specific, by applying a single capture oligonucleotide in the presence of an excess of unlabeled competitor oligonucleotides from the other serotypes. The region between nt 3777 and 3796 (Table 2) was more variable between isolates and hence more specific for particular isolates. We thus designed capture probes able to distinguish between, for example, the Taiwan 97-like type O isolates from pigs (4, 14, 18) and Kaufbeuren-like type O isolates, as well as others able to identify isolates resembling A22, C3, and Asia 1 in this region.
Testing the assay for the VP1 region.
Initially, we tested the assay by using DIG-labeled P1 primer and unlabeled P2 primer. The RT-PCR step produced the expected products (as detected by agarose gel electrophoresis); however, SNAP capture ELISA with each of the eight oligonucleotides resulted in no signal (only background signal in all wells). From controlled experiments, it was apparent that in this instance, internal oligonucleotides could not hybridize to this double-stranded PCR product during the SNAP procedure. Consequently, we decided to test two specific methods to improve the efficiency of the SNAP hybridization to the P1-P2 primer region. Method A consisted of running a standard RT-PCR as before, followed by the SNAP procedure with denaturation at 95°C for 5 min. After this denaturation, the samples (in the plate) were immediately placed in a dry ice-ethanol bath for 5 min (replacing the annealing step at 40 to 60°C). Method B utilized asymmetric PCR in order to synthesize primarily single-stranded PCR product available for SNAP hybridization. This was achieved by lowering the concentration of the unlabeled downstream P2 primer by a factor of 10 to 100 (primer concentration at 2 to 20 nM). These PCR products were then subjected to the SNAP procedure as before by using three of the eight SNAP capture probes and a number of isolates. As can be seen from Fig. 4, hybridization was now detected and thus a strategy was designed for the testing of a larger number of samples.
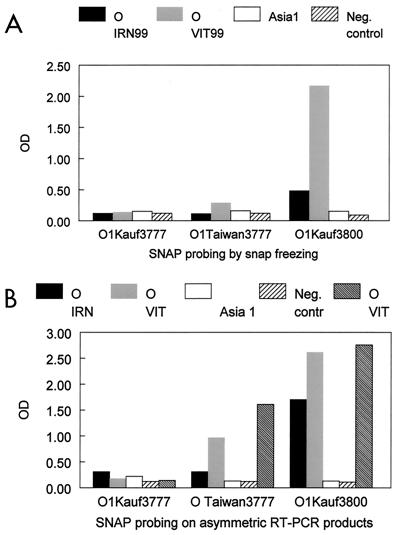
FIG. 4.
Adaptation of SNAP hybridization for genotyping. Samples were subjected to RT-PCR with the P1 and P2 primers and were SNAP probed following either denaturation and rapid freezing in dry ice (A) or asymmetric PCR (B). Three SNAP probes (O1Kauf3777, O Taiwan3777, and O1Kauf3800) were used with aliquots of individual RT-PCR samples as indicated.
A multiple-capture probe SNAP hybridization-ELISA to map the VP1 region.
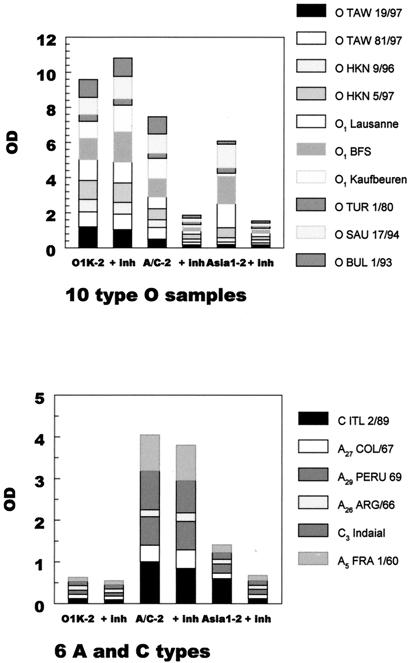
Since asymmetric PCR was technically easy and hybridization conditions could easily be varied, we used this procedure for the following experiments. The origins and nature of the virus-containing materials are shown in Table 3. The optimal dilution of the reverse P2 primer was found to be 1:50 (i.e., a concentration of 4 nM is equivalent to 0.2 pmol of the P2 primer per 50 μl of PCR mixture), which consistently yielded products detectable on agarose gels as well as in the SNAP procedure. A representative ELISA plate from the mapping of the samples is shown in Fig. 5. Individual SNAP capture probes were loaded in each row (as indicated), and RT-PCR aliquots were loaded into columns as indicated. The individual wells were read at 405 nm, and the optical density (OD) values were plotted to show specific features (Fig. 6 and 7). The results show that all type O isolates reacted well with the O1Kauf3800 (O1K-2) probe while the other serotypes did not react or reacted very weakly with this probe. The type O isolates also cross-reacted with the C/A3800 probe; however, because only type O reacted strongly with the O1Kauf3800 probe, this reaction was indicative of the sample being type O. In addition, A22-like isolates reacted with the A22-3777 and C/A3800 probes while the type C isolates reacted with the C probes. The Asia 1 isolate reacted weakly with the Asia 1-3777 and 3800 probes (not shown). Nevertheless, the reaction was measurable when reading the OD values (data not shown). As mentioned above, the capture probe O1Kauf3800 reacted with all FMDV type O sequences tested, while reaction with, for example, the O Taiwan3777 capture probe, as seen with the Vietnam (VIT) 99 samples (Fig. 4B), indicated relatedness to the O Taiwan 97 isolate of FMDV (confirmed by sequencing). Of the type O isolates from Taiwan and Hong Kong, the two isolates from Taiwan were, as expected, Taiwan-like, while four isolates from Hong Kong (including the Hong Kong 9/96 original suspension) were Taiwan-like. A sixth isolate from Hong Kong, i.e., Hong Kong 9/96 grown in cell culture, did not react significantly with the O Taiwan-like probe. Interestingly, the isolate Hong Kong 8/99 was apparently more related to Kauf-like sequences than to Taiwan-like sequences, and an isolate from Bahrain (BAR 7/99) also had this reaction (Table 3). Nevertheless, the data are consistent with the presence of Taiwan 97-like genotypes of FMDV in Hong Kong before 1997 (23). Furthermore, the presence in Hong Kong of at least three significantly different types of serotype O FMDV is consistent with sequence data (N. Knowles, personal communication). A single isolate from Vietnam also had a Taiwan-like reactivity while three well-characterized Kauf-like isolates (FMDV O1 BFS 1860, Lausanne and Kauf) reacted as expected. Regarding the typing reactivity, it should be noted that, due to an inherent low melting temperature of the Taiwan-like SNAP probe, full reactivity with the Taiwan-like probe is usually around 0.5 to 1 OD while full reactivity of the other probes may be higher than 2, everything else being equal. The reactivities of the isolates in regard to Taiwan-like or Kauf-like types were confirmed using additional SNAP probes (based on the full sequence from nt 3777 to 3820, i.e., a 43-mer Taiwan-like probe and a 43-mer Kauf-like SNAP probe using a 60°C annealing step [data not shown]).
TABLE 3.
Summary of RT-PCR SNAP mapping
| Isolate | Origin | Type of suspensiona | SNAP mapping |
|---|---|---|---|
| Type O | |||
| BAR 1/99 | Bahrain | T/C | O |
| BAR 7/99 | Bahrain | T/C | O1Kauf-like |
| ALG 4/99 | Algeria | T/C | Ob |
| UAE 2/99 | United Arab Emirates | OS | O |
| HKN 10/99 | Hong Kong | OS | O Taiwan 97-like |
| MYA 16/89 | Myanmar | OS | O |
| BAR2/96 | Bahrain | OS | O |
| HKN 9/96 | Hong Kong | OS | O Taiwan 97-like |
| NEP 7/96 | Nepal | OS | O |
| NEP 48/96 | Nepal | OS | O |
| BAR 1/96 | Bahrain | OS | O |
| MYA 15/89 | Myanmar | OS | O |
| IRN 1/99 | Iran | OS | O |
| VIT 3/99 | Vietnam | T/C | O Taiwan 97-like |
| TAW 19/97 | Taiwan | T/C | O Taiwan 97-like |
| TAW 81/97 | Taiwan | T/C | O Taiwan 97-like |
| HKN 9/96 | Hong Kong | T/C | O |
| HKN 8/99 | Hong Kong | OS | O1Kauf-like |
| HKN 9/99 | Hong Kong | OS | O Taiwan 97-like |
| HKN 5/97 | Hong Kong | T/C | O Taiwan 97-like |
| TUR 1/80 | Turkey | T/C | O |
| SAU 17/94 | Saudi Arabia | T/C | O |
| BUL 1/93 | Bulgaria | T/C | O |
| ISR 1/82 | Israel | T/C | O |
| O1 BFS 1860 | United Kingdom | VS | O1Kauf-like |
| O1 Kaufbeuren FRG/66 | Germany | T/C | O1Kauf-like |
| O1 Lausanne SW/65 | Switzerland | T/C | O1Kauf-like |
| Type A | |||
| SAU 47/93 | Saudi Arabia | T/C | Ac |
| IRN 3/96 | Iran | T/C | A or Cb |
| NEP 40/86 | Nepal | T/C | Ac |
| IND 1/78 | India | T/C | Ac |
| SEN 17/97 | Senegal | T/C | A or Cb |
| IRN 3/96 | Iran | T/C | A or C |
| A27 COL/67 | Germany | T/C | Ac |
| A29 PER/69 | Peru | T/C | Ac |
| A26 ARG/66 | Argentina | T/C | A or C |
| A5 Allier FRA/60 | France | T/C | Ac |
| Type C | |||
| SAU 1/84 | Saudi Arabia | OF | A or C |
| SAU 1/84 | Saudi Arabia | OF | A or C |
| SAU 1/84 | Saudi Arabia | OF | Negb |
| SRL 1/84 | Sri Lanka | T/C | A or C |
| IND 1/82 | India | T/C | A or Cb |
| ITL 3/89 | Italy | T/C | A or Cb |
| PHI 4/94 | Phillipines | T/C | A or Cb |
| ITL 2/89 | Italy | T/C | A or Cb |
| C3 Indaial BRA/71 | Brazil | T/C | A or Cb |
| Type Asia 1 | |||
| IRN 58/99 | Iran | T/C | Asia 1 |
| IRN 59/99 | Iran | T/C | Asia 1 |
| SAU 9/92 | Saudi Arabia | RT/C | Neg |
| CAM 1/88 | Cambodia | T/C | Asia 1 |
| CAM 9/80 | Cambodia | T/C | Asia 1 |
| ISR 3/63 | Israel | T/C | Asia 1 |
| OMN 21/89 | Oman | T/C | Asia 1bd |
| IND 16/76 | India | T/C | Asia 1 |
| Negative control | |||
| BTY neg. | Neg T/C | Neg | |
| SVDV 13/93 | Italy | T/C | Neg |
| BTY neg. | Neg T/C | Neg | |
| BTY neg. | Neg T/C | Neg | |
| Neg. tongue epithelium | Neg OS | Neg |
T/C, tissue culture; RT/C, received as a virus-inoculated cell culture; OS, original epithelial suspension; OF, original sample fluids were used in samples with limited or no epithelial tissue; VS, vaccine strain.
Isolate yielded a negative result by gel electrophoresis in the actual PCR, but had been positive in a previous PCR analysis. Type C isolates often yield an inconsistent result by gel electrophoresis of the RT-PCR product; however, the product could still be convincingly detected and typed as A or C by the SNAP ELISA.
Isolate reacted with the A22-3777 probe in addition to the C/A3800 probe.
Isolate had a borderline reaction with Asia 1 probes in the SNAP assay.
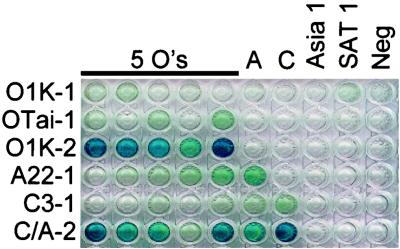
FIG. 5.
SNAP array ELISA for FMDV genotyping based on the P1-P2 region (VP1). Individual SNAP capture probes were loaded in each row (as indicated) and RT-PCR aliquots were loaded into wells as indicated, and SNAP ELISA was performed. For the identities of the capture probes used, see Table 2.
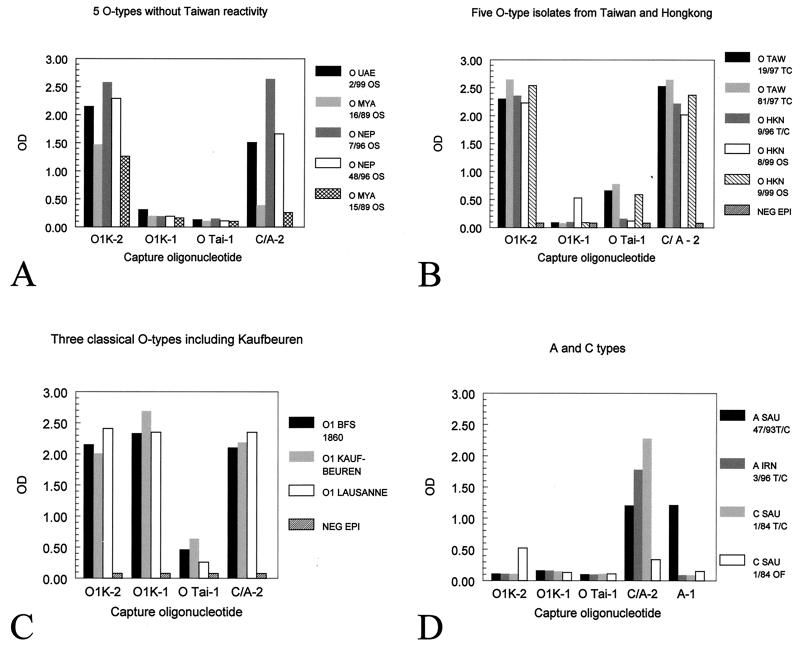
FIG. 6.
Characterization of FMDV isolates by SNAP hybridization ELISA. For the identities of the capture probes used, see Table 2. (A) The typical reaction of type O isolates without Taiwan-like reactivity is shown. Such isolates react with the O1Kauf3800 (O1K -2) probe as well as a cross-reaction with the C/A3800 (C/A-2) probe. (B) The typical reaction of type O isolates with Taiwan-like reactivity is shown. Such isolates react as described for panel A and, in addition, with the O Taiwan3777 (O Tai-1) probe. It should be noted that, due to an inherent low melting temperature of the Taiwan-like SNAP probe, full reactivity with the Taiwan-like probe is usually around 0.5 to 1 OD while full reactivity of the other probes may be higher than 2, everything else being equal. (C) Reactivity of Kauf-like isolates. The strong reactivity of Kauf-like isolates (O1 BFS 1860, O1 Lausanne, and O1 Kauf) with the O1Kauf3800 (O1K-2) probe (as all O isolates) as well as with the O1Kauf3777, specific for Kauf-like sequences, is evident. As is true for other type O isolates, such isolates also cross-react with the C/A3800 (C/A-2) probe. (D) Reactivities of selected types A and C FMDV. It can be seen that types A and C generally react well with the C/A3800 SNAP probe (a reactivity not blocked by unlabeled O1Kauf3800 and Asia 1-3800 competitors at 1.5× equimolar amounts [Fig. 7]). Most type A and C isolates react only weakly with the O1Kauf3800 probe, and any reactivity can easily be removed by unlabeled competitors. Of the isolates shown, one is A22-like (A SAU 47/93, which reacted with the A22-3777 probe) while the other three isolates shown, based on currently available SNAP probes, could be identified only as type A or C.
FIG. 7.
Increased specificity of SNAP hybridization by including unlabeled competitors. For the identities of the capture probes used, see Table 2. The FMDV serotypes O, A, C, and Asia 1 3800 series SNAP probes (biotin labeled) were mixed with unlabeled competitor oligonucleotides (at 1.5× the concentration of the capture probe for each of the serotypes to be inhibited [e.g., O1Kauf3800-biotin plus A/C3800-unlabeled and Asia 1-3800-unlabeled]) in the SNAP assay. The data are depicted as bars with stacked readings of each of 10 type O isolates, 4 type A isolates, and 2 type C isolates and are shown without and with inhibitors (+ inh).
A summary of the mapping data of 59 samples (previously mapped by ELISA) including controls mapped in the SNAP array method is shown in Table 3. Samples of 27 serotype O isolates were analyzed and all were classified as serotype O in the SNAP assay based on their strong reaction with the O1Kauf3800 probe. Samples from 10 type A isolates were analyzed, and 6 of these could be classified as type A (positive with the A22-3777 probe and the C/A3800 probe) while 4 samples were either type A or C (positive with the C/A3800 probe only). Nine type C samples were analyzed and all, except for a single negative, were classified as type A or C (positive with the C/A3800 probe only). Even type C isolates which did not produce visible bands in gel electrophoresis could be convincingly detected in this method. One isolate also had a weak type O reaction; however, this reaction could easily be removed by the inclusion of competitor oligonucleotides (see below). Eight type Asia 1 samples were analyzed; seven were characterized as type Asia 1 (weakly positive with the Asia 1-3777 and Asia 1-3800 probes, with one sample yielding a borderline reaction) and one sample was negative. The Asia 1 isolates reacted only weakly with the SNAP capture probes. However, albeit weak, the highest OD reading was consistent with the Asia 1-3777 and Asia 1-3800 SNAP probes and with low background signals (data not shown) when inhibitors were included (see below). Thus, the isolates could be typed as serotype Asia 1; however, the weak reaction with the Asia 1-3777 and Asia 1-3800 probes may indicate that the isolates tested are rather distant from the Asia 1-like sequences used for the probe design. In addition, although no specific primers were designed for this purpose (due to a lack of sequence information), seven SAT types were analyzed and the five samples were negative in the SNAP assay (consistent with no SAT-specific SNAP probes); however, two isolates (SAT 1 NIG 20/75 and SAT 2 RHO 10/80) showed a weak to medium type A or C reaction. Interestingly, this reaction could not be inhibited by unlabeled inhibitors (see below), and this indicated that these two isolates are highly related to types A and C isolates in this particular region (nt 3800 to 3820; data not shown). All negative-control preparations produced no significant reaction in the assay.
In summary, the assay could detect and identify type O isolates and could also place types A and C isolates in a single group, i.e., type A or C. However, additional SNAP probes are required for total serotype determination. The type O isolates could be further divided into Kauf-like or Taiwan-like groups or as isolates apparently unrelated to these strains. Likewise, certain type A isolates could be characterized as A22-like.
Several of the SNAP probes reacted with the expected serotype, and in addition, often also with other serotypes, but differentiation as indicated above and as shown in Table 3 could be achieved. However, the SNAP reaction could be made more specific by using competition probes (inhibitors) (Fig. 7). In this system, the specific probe, such as O1Kauf3800 (biotin labeled), was mixed with the A/C-3800 probe (unlabeled) and Asia 1-3800 probe (unlabeled), each at a concentration of 1.5 times the concentration of the labeled capture probe when loading the plates. Thus, these probes compete for binding to the target and only the probe with the best sequence similarity binds at high levels. Thus, when this mixture was mixed with a type O PCR product, the type O probe bound efficiently (specifically), leading to capture (through the biotin-streptavidin interaction), while A, C, or Asia 1 PCR products bound more efficiently to the unlabeled probes, which, lacking the biotin label, were not captured on the streptavidin-coated ELISA plate, and hence a serotype-specific signal was obtained. Examples of typing of serotype O, A, and C isolates of FMDV using the 3800 series probes and including competitor oligonucleotides are shown in Fig. 7.
DISCUSSION
We have developed RT-PCRs combined with SNAP probing with internal oligonucleotides in an ELISA format for use in diagnosis of FMD and for preliminary genotyping of the virus. The assays are highly sensitive and specific and do not have the nonspecific background problems seen in the sensitive RT-PCR ELISA without probing (21). Furthermore, the assays are easy and fast to perform. The single assay developed for detecting conserved sequences in the IRES region of the FMDV genome could detect all seven serotypes of FMDV with high sensitivity and specificity (the assay could detect as little as 0.2 TCID50s or around 20 molecules of FMDV RNA). Thus, this assay, capable of handling 88 samples per plate, shows great promise as a diagnostic method in any laboratory having the necessary equipment, i.e., standard equipment for running RT-PCR and ELISA.
A modified assay was based on a highly variable region of the FMDV genome, the VP1 (1D) region, using previously described primers for RT-PCR in conjunction with a selection of internal SNAP probes. Sequences of around 25 FMDV isolates that span this region and that are accessible in the public databases (GenBank) were grouped by serotype and aligned. The alignments of all sequences indicated that the 216-nt P1-P2 primer region contained two regions potentially useful for the mapping assay, and this was confirmed by the data obtained. The region at nt 3800 to 3820 (Table 2) seemed to be the most conserved, and a capture probe was designed to detect FMDV O types, another detected types A and C (almost identical in this region), and a third probe could detect Asia 1 (Table 2). Although SAT sequences were excluded from the analyses, the SNAP probes effectively demonstrated the proof of concept for the methodology and set the stage for future work. It should be mentioned that of the FMDV isolates from diagnostic samples sent to the WRL (Pirbright), about 90% of these are of type O or A, while only around 10% are of the other serotypes (Asia 1 or, rarely, C, SAT 1, SAT 2, or SAT 3) (http://www.iah.bbsrc.ac.uk/virus/Picornaviridae/Aphthovirus /fmdv.htm). It should be noted that isolates which yielded weak or no bands in gel electrophoresis of RT-PCR products (as, for example, many C isolates with the P1-P2 primers) could still be detected and typed in the SNAP ELISA assay. If required, the assay could be made even more specific for the selected serotype by including unlabeled competitor oligonucleotides. However, mapping could be consistently achieved even without these inhibitors. The other region (nt 3777 to 3796; Table 2) was more variable between isolates and hence more specific for particular isolates. As an example, we demonstrated that capture probes were able to distinguish Taiwan-like (1997) type O isolates from Kauf-like type O isolates. Furthermore, isolates resembling A22, C3, and Asia 1 isolates could be identified. In conclusion, the array-SNAP probing can quickly show preliminary typing characteristics of the isolate, characteristics that may be important in short-term control efforts or in efforts to control or reduce the spread of certain isolates like, for example, Taiwan 97 and similar isolates. However, more SNAP probes should be designed and tested.
RT-PCR ELISA assays have been described by others, both for general use (PCR Applications Manual, Boehringer GmbH, Mannheim, Germany) and for detection of FMDV and SVD virus (10–12). However, our SNAP assay significantly increased the speed of the hybridization step (hybridization time reduced from 3 h to 5 min) and at the same time resulted in high efficiency of captured product (up to 90% efficiency in a 5-minute SNAP hybridization). The explanation for the high speed and efficiency of the SNAP hybridization step is the use of solution hybridization at a relatively high temperature and the very high concentrations of both product and capture probe. This combination led to very fast hybridization, while the subsequent steps curtailed possible low-temperature, nonspecific probe binding by dilution of the reaction mixture (which reduced the concentration of both probe and product around 50-fold) and then binding of the capture probe to a solid phase (the microtiter plate surface). The amount of probe potentially hybridizing to PCR products subsequent to the hybridization step was estimated to be less than 0.1% of the amount bound during controlled hybridization at the annealing temperature.
The features of the SNAP assay, as described for FMDV in this study, may have the potential for development into a general assay. It can most likely be adapted for detection of other RNAs or DNA, derived from other viruses or other microorganisms, or cellular mRNAs (and even for spliced mRNA-specific assays), i.e., any system in which PCR amplification is possible and internal sequence information is known. We are currently attempting to develop assays that detect morbillivirus RNA and, potentially, differentiate between related morbilliviruses, for example, those responsible for rinderpest and peste des petits ruminants. Thus, the method should be able to contribute to fast, easy, and specific diagnoses as well as easy, preliminary typing of the pathogens received in the clinical microbiological laboratory. Preliminary SNAP typing data can then be used for selection of clinical isolates targeted for a more detailed analysis. Furthermore, the SNAP procedure facilitates the production of preloaded (with capture probes) 96-well plates, making direct immobilization of oligonucleotides (29) and other complicated, time-consuming procedures unnecessary.
The basic assay worked very well on the FMDV IRES region, but with the P1-P2 region primers, the hybridization assays had to rely on asymmetric PCR to generate single-stranded target DNA. Apparently, this property of the PCR fragment may be determined by the specific primers used for RT-PCR, because the use of another primer just downstream of the P2 primer resulted in products efficiently captured by the 3777 and 3800 SNAP probes without using asymmetric PCR (data not shown).
The potential advantages of this method using simultaneous analysis with multiple SNAP capture probes compared to the previously described serotype-specific PCRs (9, 31, 42) are that only a single set of PCR primers is needed, based on conserved sequences, and only a single PCR per sample is performed. Furthermore, the SNAP hybridization method relies on sequence homology, temperature, salt concentration, etc., making the assay very flexible. In contrast, PCR for strain differentiation is dependent on multiple PCR primers and produces more of an “all or nothing” phenomenon. However, each method has advantages and disadvantages, and thus they may complement each other. Furthermore, it should be mentioned that the SNAP assay does not replace sequencing for detailed analysis of FMDV. Sequence analysis can give much more detailed information, and moreover, current SNAP array testing will depend on knowledge of current sequences being available. Thus, the SNAP array is primarily intended for the rapid and easy initial mapping of isolates which, after selection based on the SNAP map, may be sequenced for final characterization.
In conclusion, we have established a fast and efficient SNAP hybridization step in conjunction with RT-PCR assays and an ELISA readout. The concept of the method is demonstrated by the detection of any serotype of FMDV, and furthermore, the assay can determine if the isolate in question is of type O, A or C, or Asia 1. Further work to identify other target sequences in the FMDV genome suitable for RT-PCR and SNAP probing assays as well as the characterization of additional type-specific SNAP oligonucleotide probes are required.
ACKNOWLEDGMENTS
We thank Geoff H. Hutchings and Nigel P. Ferris for assistance. Alex I. Donaldson and R. Paul Kitching made helpful comments to the work.
The research was supported in part by the UK Ministry of Agriculture, Fisheries and Food (Project No. SE1113) and the Danish Ministry of Food, Agriculture, and Fisheries.
REFERENCES
- 1.Amaral-Doel C M, Owen N E, Ferris N P, Kitching R P, Doel T R. Detection of foot-and-mouth disease viral sequences in clinical specimens and ethyleneimine-inactivated preparations by the polymerase chain reaction. Vaccine. 1993;11:415–421. doi: 10.1016/0264-410x(93)90281-2. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. Report of the Committee of Inquiry on Foot-and-Mouth Disease (1968) London, United Kingdom: Ministry of Agriculture, Fisheries & Food, Her Majesty's Stationery Office; 1969. pp. 56–57. [Google Scholar]
- 3.Barnett P V, Cox S J. The role of small ruminants in the epidemiology and transmission of foot-and-mouth disease. Vet J. 1999;158:6–13. doi: 10.1053/tvjl.1998.0338. [DOI] [PubMed] [Google Scholar]
- 4.Beard C W, Mason P W. Genetic determinants of altered virulence of Taiwanese foot-and-mouth disease virus. J Virol. 2000;74:987–991. doi: 10.1128/jvi.74.2.987-991.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beck E, Strohmaier K. Subtyping of European foot-and-mouth disease virus strains by nucleotide sequence determination. J Virol. 1987;61:1621–1629. doi: 10.1128/jvi.61.5.1621-1629.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belsham G J. Distinctive features of foot-and-mouth disease virus, a member of the picornavirus family; aspects of virus protein synthesis, protein processing and structure. Prog Biophys Mol Biol. 1993;60:241–260. doi: 10.1016/0079-6107(93)90016-D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown C C, Olander H J, Meyer R F. Pathogenesis of foot-and-mouth disease in swine, studied by in-situ hybridization. J Comp Pathol. 1995;113:51–58. doi: 10.1016/s0021-9975(05)80068-4. [DOI] [PubMed] [Google Scholar]
- 8.Burrows R. The infectivity assay of foot-and-mouth disease virus in pigs. J Hyg. 1966;64:419–429. doi: 10.1017/s0022172400040729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Callens M, De Clercq K. Differentiation of the seven serotypes of foot-and-mouth disease virus by reverse transcriptase polymerase chain reaction. J Virol Methods. 1997;67:35–44. doi: 10.1016/s0166-0934(97)00074-8. [DOI] [PubMed] [Google Scholar]
- 10.Callens M, De Clercq K. Highly sensitive detection of swine vesicular disease virus based on a single tube RT-PCR system and DIG-ELISA detection. J Virol Methods. 1999;77:87–99. doi: 10.1016/s0166-0934(98)00140-2. [DOI] [PubMed] [Google Scholar]
- 11.Callens M, De Clercq K, Danes M. Transmission of foot-and-mouth disease virus between contact sheep and contact pigs: detection of infected animals. Aldershot, United Kingdom: Session of the Research Group of the Standing Technical Committee, European Commission for the Control of Foot-and-Mouth Disease; 1998. pp. 129–138. . Food and Agricultural Organization of the United Nations, Rome, Italy. [Google Scholar]
- 12.Callens M, De Clercq K, Gruia M, Danes M. Detection of foot-and-mouth disease by reverse transcription polymerase chain reaction and virus isolation in contact sheep without clinical signs of foot-and-mouth disease. Vet Q. 1998;20(Suppl. 2):37–40. [PubMed] [Google Scholar]
- 13.Carrillo C, Wigdorovitz A, Oliveros J C, Zamorano P I, Sadir A M, Gomez N, Salinas J, Escribano J M, Borca M V. Protective immune response to foot-and-mouth disease virus with VP1 expressed in transgenic plants. J Virol. 1998;72:1688–1690. doi: 10.1128/jvi.72.2.1688-1690.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen B J, Sung W H, Shieh H K. Managing an animal health emergency in Taipei China: foot and mouth disease. Rev Sci Tech. 1999;18:186–192. doi: 10.20506/rst.18.1.1154. [DOI] [PubMed] [Google Scholar]
- 15.Donaldson A I. Aerobiology of foot-and-mouth disease (FMD): an outline and recent advances. Rev Sci Tech Off Int Epizoot. 1986;5:315–321. doi: 10.20506/rst.5.2.234. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson A I. Foot-and-mouth disease: the principal features. Irish Vet J. 1987;41:325–327. [Google Scholar]
- 17.Donaldson A I, Ferris N P, Wells G A. Experimental foot-and-mouth disease in fattening pigs, sows and piglets in relation to outbreaks in the field. Vet Rec. 1984;115:509–512. doi: 10.1136/vr.115.20.509. [DOI] [PubMed] [Google Scholar]
- 18.Dunn C S, Donaldson A I. Natural adaption to pigs of a Taiwanese isolate of foot-and-mouth disease virus. Vet Rec. 1997;141:174–175. doi: 10.1136/vr.141.7.174. [DOI] [PubMed] [Google Scholar]
- 19.Ferris N P, Dawson M. Routine application of enzyme-linked immunosorbent assay in comparison with complement fixation for the diagnosis of foot-and-mouth and swine vesicular diseases. Vet Microbiol. 1988;16:201–209. doi: 10.1016/0378-1135(88)90024-7. [DOI] [PubMed] [Google Scholar]
- 20.Ferris N P, Powell H, Donaldson A I. Use of pre-coated immunoplates and freeze-dried reagents for the diagnosis of foot-and-mouth disease and swine vesicular disease by enzyme-linked immunosorbent assay (ELISA) J Virol Methods. 1988;19:197–206. doi: 10.1016/0166-0934(88)90014-6. [DOI] [PubMed] [Google Scholar]
- 21.Forsyth M A, Belsham G J, Felipe E, Mackay D K. Detection of FMDV in nasal swabs and oesophago-pharyngeal fluids using a reverse-transcription polymerase chain reaction reaction. Aldershot, United Kingdom: Session of the Research Group of the Standing Technical Committee, European Commission for the Control of Foot-and-Mouth Disease; 1998. pp. 88–92. . Food and Agricultural Organization of the United Nations, Rome, Italy. [Google Scholar]
- 22.Hamblin C, Armstrong R M, Hedger R S. A rapid enzyme-linked immunosorbent assay for the detection of foot-and-mouth disease virus in epithelial tissues. Vet Microbiol. 1984;9:435–443. doi: 10.1016/0378-1135(84)90064-6. [DOI] [PubMed] [Google Scholar]
- 23.Kitching R P. A recent history of foot-and-mouth disease. J Comp Pathol. 1998;118:89–108. doi: 10.1016/s0021-9975(98)80002-9. [DOI] [PubMed] [Google Scholar]
- 24.Knowles N J, Samuel A R. Molecular techniques in foot-and-mouth disease epidemiology. IAEA-Proceedings. 1998;348:185–201. [Google Scholar]
- 25.Locher F, Suryanarayana V V, Tratschin J D. Rapid detection and characterization of foot-and-mouth disease virus by restriction enzyme and nucleotide sequence analysis of PCR products. J Clin Microbiol. 1995;33:440–444. doi: 10.1128/jcm.33.2.440-444.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marquardt O, Haas B. VP1-coding sequences of recent isolates of foot-and-mouth disease virus types A, O and Asia1. Virus Genes. 1998;16:185–193. doi: 10.1023/a:1007968007117. [DOI] [PubMed] [Google Scholar]
- 27.Martinez M A, Dopazo J, Hernandez J, Mateu M G, Sobrino F, Domingo E, Knowles N J. Evolution of the capsid protein genes of foot-and-mouth disease virus: antigenic variation without accumulation of amino acid substitutions over six decades. J Virol. 1992;66:3557–3565. doi: 10.1128/jvi.66.6.3557-3565.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piccone M E, Kaplan G, Giavedoni L, Domingo E, Palma E L. VP1 of serotype C foot-and-mouth disease viruses: long-term conservation of sequences. J Virol. 1988;62:1469–1473. doi: 10.1128/jvi.62.4.1469-1473.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rasmussen S R, Rasmussen H B, Larsen M R, Hoff-Jorgensen R, Cano R J. Combined polymerase chain reaction-hybridization microplate assay used to detect bovine leukemia virus and Salmonella. Clin Chem. 1994;40:200–205. [PubMed] [Google Scholar]
- 30.Reid S M, Forsyth M A, Hutchings G H, Ferris N P. Comparison of reverse transcription polymerase chain reaction, enzyme linked immunosorbent assay and virus isolation for the routine diagnosis of foot-and-mouth disease. J Virol Methods. 1998;70:213–217. doi: 10.1016/s0166-0934(97)00181-x. [DOI] [PubMed] [Google Scholar]
- 31.Reid S M, Hutchings G H, Ferris N P, De Clercq K. Diagnosis of foot-and-mouth disease by RT-PCR: evaluation of primers for serotypic characterisation of viral RNA in clinical samples. J Virol Methods. 1999;83:113–123. doi: 10.1016/s0166-0934(99)00113-5. [DOI] [PubMed] [Google Scholar]
- 32.Reid S M, Knowles N J, Hutchings G H, Ferris N P. Diagnosis of FMD by RT PCR: design and evaluation of alternative primers for the diagnosis of serotypes O and SAT2. Aldershot, United Kingdom: Session of the Research Group of the Standing Technical Committee, European Commission for the Control of Foot-and-Mouth Disease; 1998. pp. 109–116. . Food and Agricultural Organization of the United Nations, Rome, Italy. [Google Scholar]
- 32a.Reid S M, Ferris N P, Hutchings G H, Samuel A R, Knozoles N J. Primary diagnosis of food-and-mouth disease by reverse transcription polymerase chain reaction. J Virol Methods. 2000;89:167–176. doi: 10.1016/s0166-0934(00)00213-5. [DOI] [PubMed] [Google Scholar]
- 33.Rodriguez A, Martinez-Salas E, Dopazo J, Davila M, Saiz J C, Sobrino F. Primer design for specific diagnosis by PCR of highly variable RNA viruses: typing of foot-and-mouth disease virus. Virology. 1992;189:363–367. doi: 10.1016/0042-6822(92)90717-4. [DOI] [PubMed] [Google Scholar]
- 34.Roeder P L, Le Blanc Smith P M. Detection and typing of foot-and-mouth disease virus by enzyme-linked immunosorbent assay: a sensitive, rapid and reliable technique for primary diagnosis. Res Vet Sci. 1987;43:225–232. [PubMed] [Google Scholar]
- 35.Saiz J C, Sobrino F, Dopazo J. Molecular epidemiology of foot-and-mouth disease virus type O. J Gen Virol. 1993;74:2281–2285. doi: 10.1099/0022-1317-74-10-2281. [DOI] [PubMed] [Google Scholar]
- 36.Salt J S. The carrier state in foot and mouth disease—an immunological review. Br Vet J. 1993;149:207–223. doi: 10.1016/S0007-1935(05)80168-X. [DOI] [PubMed] [Google Scholar]
- 37.Samuel A R, Knowles N J, Mackay D K. Genetic analysis of type O viruses responsible for epidemics of foot-and-mouth disease in North Africa. Epidemiol Infect. 1999;122:529–538. doi: 10.1017/s0950268899002265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sellers R F. Quantitative aspects of the spread of foot and mouth disease. Vet Bull. 1971;41:431–439. [Google Scholar]
- 39.Stram Y, Molad T, Chai D, Gelman B, Yadin H. Detection and subtyping of foot-and-mouth disease virus in infected cattle by polymerase chain reaction and amplified VP1 sequencing. J Vet Diagn Investig. 1995;7:52–55. doi: 10.1177/104063879500700107. [DOI] [PubMed] [Google Scholar]
- 40.Suryanarayana V, Madanamohan B, Bist P, Natarajan C, Tratschin J D. Serotyping of foot-and-mouth disease virus by antigen capture reverse transcriptase/polymerase chain reaction. J Virol Methods. 1999;80:45–52. doi: 10.1016/s0166-0934(99)00029-4. [DOI] [PubMed] [Google Scholar]
- 41.Terpstra C. Pathogenesis of foot-and-mouth disease in experimentally infected pigs. Bull Off Int Epizoot. 1972;77:859–874. [PubMed] [Google Scholar]
- 42.Vangrysperre W, De Clercq K. Rapid and sensitive polymerase chain reaction based detection and typing of foot-and-mouth disease virus in clinical samples and cell culture isolates, combined with a simultaneous differentiation with other genomically and/or symptomatically related viruses. Arch Virol. 1996;141:331–344. doi: 10.1007/BF01718403. [DOI] [PubMed] [Google Scholar]
- 43.Woodbury E L. A review of the possible mechanisms for the persistence of foot-and-mouth disease virus. Epidemiol Infect. 1995;114:1–13. doi: 10.1017/s0950268800051864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zibert A, Maass G, Strebel K, Falk M M, Beck E. Infectious foot-and-mouth disease virus derived from a cloned full-length cDNA. J Virol. 1990;64:2467–2473. doi: 10.1128/jvi.64.6.2467-2473.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]