Abstract
Unhealthy dietary choices are associated with poor sleep in children through adults. Yet, how diet and sleep are related in early childhood, when diet is reliant on parent choices around food availability, is unknown. We aimed to explore how frequency of fruit, vegetable, fast food, and soda consumption are associated with preschool children’s sleep quality. We also considered how parenting factors may impact the relationship between children’s sleep and diet. Actigraphy data was collected from 383 children aged 33–70 months. Caregivers reported on child food and beverage frequency, demographics, and health items. Parenting strategies were assessed using the Parenting Scale. Multiple linear regression was used to examine associations between sleep and dietary measures with socioeconomic status, race/ethnicity, physical activity, and body mass index as covariates. Shorter nap duration was associated with more frequent consumption of fruits and vegetables (B=−3.6, p =.03). Shorter nighttime and 24-hour sleep durations were associated with more frequent consumption of fast food (B=−6.5, p=.01; B=−5.8, p=.01). Shorter nighttime sleep and later sleep onset were associated with more frequent soda consumption (B=−9.2, p=.01; B=0.23, p=.001). Use of ineffective parenting strategies was negatively associated with fruit and vegetable consumption (r=−.29, p=.01) and positively associated with soda consumption (r=.25, p=.02) but unrelated to sleep measures. Thus, ineffective parenting strategies may underlie child access to unhealthy foods, which, in turn, contributes to poor sleep. Encouraging healthier dietary habits, and educating caregivers on how to reinforce such practices, may lead to better sleep outcomes in early childhood.
Keywords: sleep, diet, early childhood, parenting, actigraphy
INTRODUCTION
Sleep and nutrition are integral to children’s overall development and well-being. Poor sleep quality and poor dietary habits are risk factors for obesity and other cardiometabolic health consequences in children (Chen, Beydoun, & Wang, 2008; Knutson, 2013). As such, it is important to understand relations between sleep and diet in early childhood. A recent meta-analysis exploring the bi-directional relationships between sleep and diet from ages 0–5 years found little available data in the preschool years (3–5 years), particularly with objectively measured sleep (Ward et al., 2019). Gaining a better understanding of how sleep and diet are connected is critical for science-based pediatric guidelines and for developing interventions, particularly for early childhood, when lifelong sleep and eating habits are established (Iglowstein, Jenni, Molinari, & Largo, 2003; Magarey, Daniels, Boulton, & Cockington, 2003).
Various aspects of children’s sleep have been associated with dietary choices. In children 6–9 years old, those with longer sleep durations tended to consume diets rich in more nutritious foods, such as fruits, vegetables, and lean proteins (Börnhorst et al., 2015; Tatone-Tokuda et al., 2012). Likewise, in older children (10–13 years old), longer sleep durations were associated with greater consumption of fruits and vegetables, even when controlling for confounding factors such as socioeconomic status (SES) or body mass index (BMI; Franckle et al., 2015). More generally, in a sample of 1.5–2 year old children, longer sleep duration was associated with higher intakes of carbohydrates at evening meals (Diethelm, Remer, Jilani, Kunz, & Buyken, 2011), though these findings do not directly indicate fruits and vegetables. Sleep timing is also related to healthier dietary choices in children. In a sample of 9–16 year olds, earlier bed time was associated with higher fruit and vegetable intake (Golley, Maher, Matricciani, & Olds, 2013). Similarly, in a low-income preschool population, earlier sleep mid-point (mid-point between sleep onset and wake onset) based on parent-reported sleep variables was associated with a higher consumption of vegetables and healthy proteins (Jansen et al., 2019).
While healthier dietary choices appear linked to more positive sleep trends, a number of studies have found that less healthy options, such as fast food or high-sugar snacks, are associated with poorer sleep quality. Shorter sleep duration in 7–11 year old children was associated with higher consumption of fast foods, “energy-dense” (as opposed to nutrient-dense) foods, and processed snacks (Córdova, Barja, & Brockmann, 2018; Kjeldsen et al., 2014). In 9–11 year old children, later bedtimes and higher reported fatigue in the morning were related to greater consumption frequency of less nutritious foods, such as fast food or sweets (Chaput et al., 2015; Westerlund, Ray, & Roos, 2009).
Few studies have explored the relationship between preschool-aged children’s sleep and fast food consumption, though the existing literature suggests similar findings as those seen in older children. In a sample of 3–5 year old children, Jansen et al. (2019) found that greater social jet lag (difference between weekday and weekend mid-sleep point) is associated with higher consumption of fried, processed foods. Additionally, in a longitudinal study, shorter sleep durations (<10h) at 2, 3 and 5 years of age were related to more frequent consumption of processed and fast foods at age 2 (Plancoulaine et al., 2018). These studies in early childhood, however, both relied on caregiver-reported sleep measures, which can be less reliable than objective measures such as actigraphy, with caregivers often overestimating night time sleep durations and morning wake times (Lam, Mahone, Mason, & Scharf, 2011a).
Children’s beverage consumption provides another potential source of added sugars. Whereas many studies have not found relationships between sleep quality and fruit juice consumption, overnight sleep duration in 6–9 year old girls (Tatone-Tokuda et al., 2012) and 6–13 year old boys (Hitze et al., 2009) was negatively associated with intake of soda regardless of caffeine content. In later childhood through adolescence, shorter sleep duration as well as greater variability in night-to-night sleep duration were related to increased intake of soda (Franckle et al., 2015; Kjeldsen et al., 2014). Interestingly, no studies to our knowledge have investigated the impact that soda intake may have on sleep in early childhood, in spite of a reported 23% of children in this age range being frequent consumers of soda (Bleich, Vercammen, Koma, & Li, 2018).
Parenting factors may influence these associations between sleep and diet in children. Young children are impacted by routines, or lack thereof, particularly with establishing bedtime habits (Mindell & Williamson, 2018). Additionally, young children may not make as many independent food choices as older children and rely more on parental guidance, or preferences, when making decisions about dietary options (Moreira et al., 2016). The role that parental discipline strategies may play in the relationship between sleep quality and dietary habits has not yet been considered in early childhood.
Finally, additional key factors such as SES, race/ethnicity, physical activity, and BMI are related to both sleep quality and dietary habits. SES is known to be associated with sleep disparities in children and adolescents, with those from lower SES households often experiencing poorer sleep quality (Bagley, Kelly, Buckhalt, & El-Sheikh, 2015; El-Sheikh et al., 2013). Lower SES is also known to be associated with poorer dietary patterns in young children (Rashid et al., 2018). Sleep differences also exist between racial and ethnic groups with Hispanic/Latino children often displaying poorer sleep quality compared to their non-Hispanic peers (Peña, Rifas-Shiman, Gillman, Redline, & Taveras, 2016). Black children have also been found to have shorter overnight sleep durations than their White peers, but are more likely to nap at preschool or daycare (Parsons, Ollberding, Smith, & Copeland, 2018). Additionally, physical activity is related to both children’s sleep and dietary habits. For example, shorter sleep duration is associated with increased moderate-to-vigorous activity bouts in school-age children, whereas poorer dietary quality is associated with lower activity levels (Harrington, 2013; Tremblay, et al., 2010). Lastly, BMI has well-evidenced links to sleep quality, particularly due to the association between obesity and obstructive sleep apnea (Tauman & Gozal, 2006). Mutually, BMI and dietary quality are closely linked across development (Gingras, Rifas-Shiman, Taveras, Oken, & Hivert, 2018). Although the above factors should be considered in research on sleep and diet, previous studies in early childhood have controlled for some, but not all, of these measures.
Thus, the purpose of our study was to explore the relation among dietary options, objectively measured sleep quality, and parenting factors in a diverse sample of preschool children. First, we examined the relations between distinct dietary options and sleep quality. We hypothesized that children who ate fruits and vegetables more frequently would have higher quality sleep as evidenced by earlier sleep onset, longer sleep durations, and shorter nap durations. Conversely, we hypothesized that children who ate fast food and/or drank soda more frequently would have poorer sleep quality, as evidenced by later sleep onset, shorter sleep durations, and longer nap duration, due to the sometimes compensatory nature of napping in this age range (Spencer et al., 2016; Ward, Gay, Anders, Alkon, & Lee, 2008). Second, we explored the associations between different parenting styles and consumption of food groups that were found to be significantly associated with sleep quality measures. We hypothesized that caregivers of children who more frequently consume fast food and soda make use of more ineffective parenting strategies, such as being too relaxed with rule-setting. We considered the role of numerous social and health factors that are known to influence sleep and dietary habits in childhood, including SES, race/ethnicity, physical activity, and BMI.
METHODS
Participants
Children were recruited from preschools in western Massachusetts as part of a larger study on memory and sleep in young children. To be eligible, children had to meet the following criteria: 1) between 33–71 months of age (typical age range for preschool enrollment), 2) no diagnosis of a sleep disorder or developmental disability, 3) not using sleep-affecting or psychotropic medications, 4) normal or corrected-to-normal vision and hearing, and 5) no recent illness or travel across time zones. Additionally, testing was scheduled to avoid daylight savings time.
Primary caregivers were asked to complete a series of surveys containing questions relating to demographics and health along with a sleep diary to corroborate actigraphy-defined sleep intervals. Additionally, to be included in the analysis, a minimum of three full days and nights of usable actigraphy data was required (Acebo & LeBourgeois, 2006; Penpraze et al., 2006). Of the 885 children enrolled, 383 children (45% female) met the minimum inclusion criteria for actigraphy and had sufficient questionnaire data completed by their caregiver.
Measures
Actigraphy
Children wore actigraph watches (Actiwatch Spectrum, Philips Respironics, Bend, OR) on their non-dominant wrist continuously for up to 16 days and 15 nights (M = 9.3 days, SD = 3.6, range: 3–16 days; M = 9.7 nights, SD = 3.3, range: 3–15 nights). Caregivers and children were instructed to press an event marker button at the start and end of nap and overnight sleep bouts. Activity data was sampled by the watch in 15-second epochs, with a sampling rate of 32 Hz and a sensitivity of <.01g. Actigraphy is considered a reliable method for objective sleep detection in children relative to polysomnography (Hyde et al., 2007).
Caregivers completed daily sleep diaries, recording daily bed time, wake time, sleep latency, and sleeping arrangements as well as if/when the watch was removed during the day. Preschool classroom teachers for enrolled children completed nap diaries, noting when enrolled children slept in the classroom during the 16-day measurement period.
Demographic and Health Questionnaires
Caregivers completed a series of questionnaires on demographics and health relating to both themselves and their child. Questions pertained to basic demographic and household information, home environment, eating habits, TV viewing habits, and physical health of both the child and caregiver.
Dietary habits were assessed using a caregiver-reported child food frequency questionnaire (FFQ), which has been shown to be a valid method for documenting children’s consumption habits (Huybrechts et al., 2010; Zheng, Campbell, Scanlan, & McNaughton, 2020). Questions about consumption of foods and beverages were posed as: “Thinking about the past month, on average, how often has your child eaten each of the foods or beverages listed” with reference to fruits, vegetables, and soda. Response categories included: never, less than once per week, 2–4 times per week, approximately daily, 2–4 times per day, and more than 4 times per day. A separate item probing frequency of fast food consumption was phrased as: “On average, how often does your child eat something from a fast food restaurant (McDonald’s, Burger King, Taco Bell, etc.)?”. Response options included: less than once per month, 1–3 meals per month, 1 meal per week, 2–4 meals per week, 5–6 meals per week, and more than 6 meals per week.
Parenting Scale
A sub-sample of caregivers (n = 89) also completed the 30-item Parenting Scale (Arnold, O’Leary, Wolff, & Acker, 1993), a questionnaire which measures ineffective or dysfunctional parenting strategies used by parents of young children. This scale gives an overall score of a caregiver’s tendency to use ineffective practices, as well as three subscales: laxness, over-reactivity, and verbosity.
BMI
Researchers measured children’s weight (in pounds) and height (in inches) during in-classroom visits.
Procedure
All procedures were reviewed and approved by the Institutional Review Board at the University of Massachusetts, Amherst. Caregivers consented to their children’s participation prior to data collection and child assent was sought before fitting the child with the actigraph watch. Caregivers were given the duration of the 16-day study to complete questionnaire materials.
Data Analysis
Responses to the fruit and vegetable categories were summed and averaged to determine consumption of produce as a whole, which will be referred to as “fruits and vegetables”. The reported scores ranged from 0 to 5. Soda and fast food responses ranged from 0 to 3, with no caregivers reporting frequency greater than daily for soda nor greater than 2–4 meals per week for fast food.
Actigraphy data was scored using Actiware software (Oakley, 1997) and standard scoring protocols (Acebo & LeBourgeois, 2006). Sleep diaries and event markers were used to corroborate sleep intervals. If there was a significant discrepancy between sources, consensus was sought between trained researchers. Sleep onset was defined as the first consecutive three minutes of sleep and wake onset as the last consecutive five minutes of sleep. Both sleep and nap duration were determined as the interval between sleep onset and wake onset. Total 24-hour sleep duration was the sum of nap duration plus the subsequent evening’s sleep duration. Actigraphy data was combined and averaged across all usable days for each participant. Due to these data deriving from a larger study in which naps were promoted or discouraged on two days, these experimental days were excluded from the overall analysis.
Physical activity was included as a covariate. Using scored actigraphy data, physical activity counts per minute were determined by summing activity counts across all epochs classified as wake intervals and dividing by minutes of wear time for that day. Counts were then averaged across all included days. Children were required to have 480 minutes (8 hours) of usable daytime activity for at least 3 days to be included in analyses.
Child race/ethnicity, household SES, and BMI were found to correlate with one or more sleep or dietary measures of interest (see Table S1), thus further warranting their inclusion as covariates. Caregivers reported child race and ethnicity. For the sake of our regression analyses, reported child race/ethnicity was recategorized as Hispanic/Latino of any race, non-Hispanic/Latino White, non-Hispanic/Latino Black, and other non-Hispanic/Latino.
SES was constructed as a composite variable, using responses from caregivers on income, education, and employment (Berzofsky, Smiley-McDonald, Moore, & Krebs, 2014). To determine household income, caregivers were asked “During the past year, what was the total income of your household before taxes?” with possible responses of $5000 or less, $5001 to 10,000, $10,001 to 20,000, $20,001 to 40,000, $40,001 to 70,000, $70,001 to 100,000, $100,001 to 150,000, or more than $150,000. Using additional questions about household size, we determined average household income (selected income range divided by household size) and compared that against the most current Federal Poverty Level (FPL) report available from the U.S. Department of Health and Human Services. Income was then matched into one of four categories and scored. To determine the education component, primary caregivers reported their education level (“What is the highest level of school you have completed?”) based on six responses: less than 12th grade, high school or GED, some college, Associate degree, Bachelor’s degree, Master’s or Doctorate. Lastly, employment was determined based on the question “What is your employment status?” with the responses full-time, part-time, or on temporary leave being considered affirmative. Scores from all three categories were summed to estimate SES. This range is 0 to 7, with higher scores representing higher socioeconomic status.
BMI was determined using the US imperial formula ([lbs x 703]/inches2) and adjusted into z-scores based on age and gender (Kuczmarski, Ogden, & Guo, 2002). BMI scores were then designated as overweight/obese (≥ 85th percentile) or not (< 85th percentile).
Parenting Scale scores were computed based on established scoring guidelines (Arnold et al., 1993). A global index of ineffective parenting strategies was determined as the average of responses to all items. Subscales (laxness, over-reactivity, verbosity) were determined as the average of responses on items relating to each factor.
All statistical analyses were run using SPSS Version 27.0. Multiple linear regression models were used to evaluate associations between sleep duration and timing measures with dietary frequency measures described above. One model was run for each sleep measure and dietary frequency pairing and adjusted for age, sex, race/ethnicity, SES, physical activity, and BMI.
Post-hoc analyses explored relationships between significant sleep and diet measures and ineffective parenting strategies using the sub-sample of respondents who received and completed the Parenting Scale survey. Partial Pearson’s correlations were run to determine associations between sleep measures and Parenting Scale scores. Partial Spearman’s correlations were run between food frequency measures and Parenting Scale scores. We controlled for both age and SES in these analyses, as the latter was found to be correlated with most of our sleep and dietary frequency measures (rs >.20; see Table S1).
RESULTS
Sample characteristics
Participant characteristics are provided in Table 1. The mean age was 51.6 months (SD = 9.5), with a range of 33–70 months. The sample was 55.5% non-Hispanic/Latino White and a quarter were defined as overweight (26.4%). The average SES score was 4.52 (SD = 1.98), defined as middle SES. Twenty percent of our population were defined as lower SES, and 19.1% of households were estimated to be at or below the federal poverty level.
TABLE 1.
Sample Demographic Characteristics, Sleep and Dietary Measures (N = 383)
| Variables | M ± SD or % |
|---|---|
| Child characteristics | |
| Female | 44.1 |
| Age, months | 51.6 ± 9.5 |
| Child Race/Ethnicity | |
| Hispanic/Latino | 26.3 |
| White, Non-Hispanic | 55.5 |
| Black, Non-Hispanic | 6.3 |
| Other, Non-Hispanic | 11.8 |
| Overweight (>85th percentile) | 26.4 |
| SES Score (0–7) | 4.5 ± 1.9 |
| Physical Activity Counts (avg per min) | 567.2 ± 97.4 |
| Sleep Measures | |
| Overnight Duration (min) | 577.7 ± 39.3 |
| Nap Duration (min) | 90.2 ± 24.6 |
| 24hr Total Duration (min) | 617.1 ± 36.5 |
| Sleep Onset (PM) | 9:20 ± 0:52 |
| Wake Onset (AM) | 6:58 ± 0:43 |
| Actigraphy Data (days) | 9.7 ± 3.3 |
| Food Frequency Measures (range) | |
| Fruits and Vegetables (0–5) | 3.1 ± 0.8 |
| Soda (0–3) | 0.3 ± 0.6 |
| Fast Food (0–3) | 0.7 ± 0.8 |
| Parenting Scale Scores a | |
| Overall | 3.0 ± 0.6 |
| Laxness | 3.0 ± 0.8 |
| Over-reactivity | 2.5 ± 0.7 |
| Verbosity | 3.9 ± 0.8 |
n = 89
On average, children slept 10.3 hours (SD = 0.6) in a 24-hour period, and 9.6 hours (SD = 0.7) overnight. Average nap duration was 90.2 minutes (SD = 24.6). Average nap frequency was 4.1 days per week, with 52% of children defined as habitual nappers (napping 5 days or more per week). Only children who napped on at least 2 days in the study timeframe (n = 339) were included in nap-related analyses. The average nighttime sleep onset was 9:20 PM (SD = 52 mins) and the average wake onset was 6:58 AM (SD = 43 mins).
Relations between fruits and vegetables, fast food, soda consumption, and sleep
Linear regression model results, reporting standardized beta coefficients are presented in Figures 1, 2, and 3. For ease of interpretation, all statistics presented in-text are unstandardized beta coefficients.
FIGURE 1.
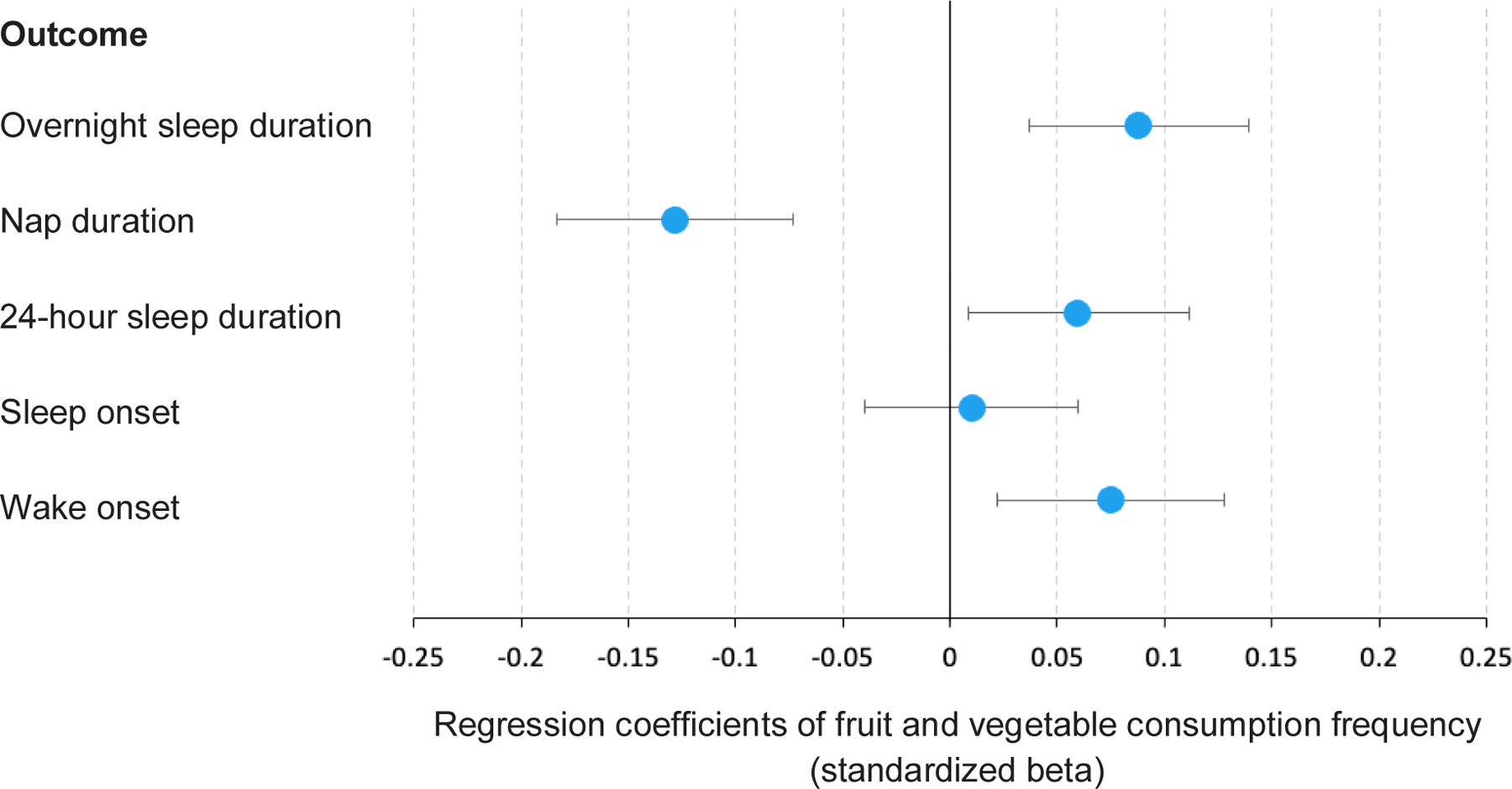
Regression coefficients for fruit and vegetable consumption frequency with sleep measures. Nap duration was significantly associated with consumption of fruits and vegetables (ß =−.13). Overnight sleep duration (ß =.08, p =.09), 24-hour sleep duration (ß =.06, p =.24), sleep onset (ß =.01, p =.89), and wake onset (ß =.08, p =.14) were non-significant. Error bars represent standard error.
FIGURE 2.
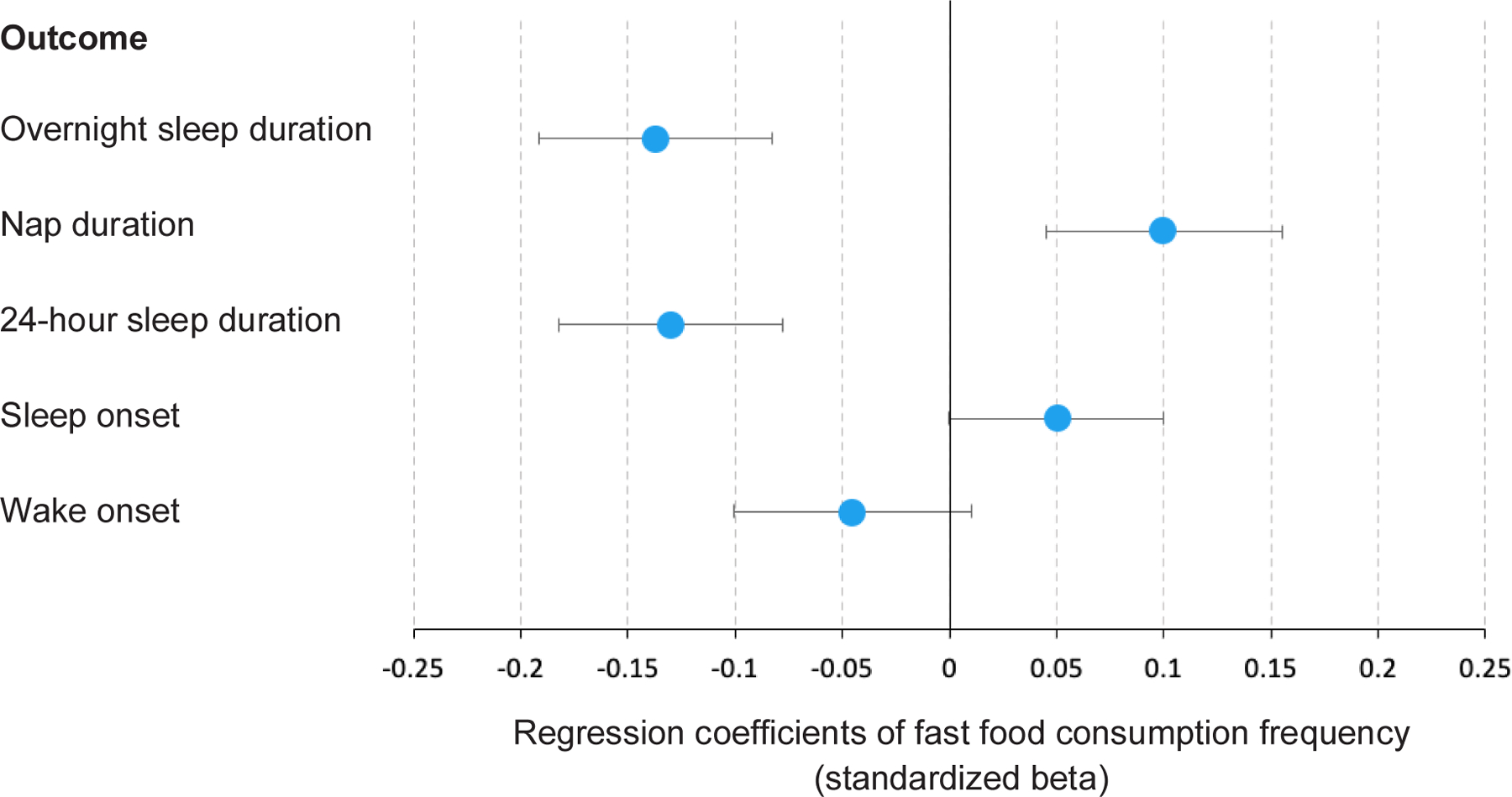
Regression coefficients for fast food consumption frequency with sleep measures. Overnight sleep duration (ß =−.14) and 24-hour sleep duration (ß =−.13) were associated with fast food consumption. Nap duration (ß =.10), sleep onset (ß =.05, p =.25), and wake onset (ß =−.05, p =.42) were non-significant. Error bars represent standard error.
FIGURE 3.
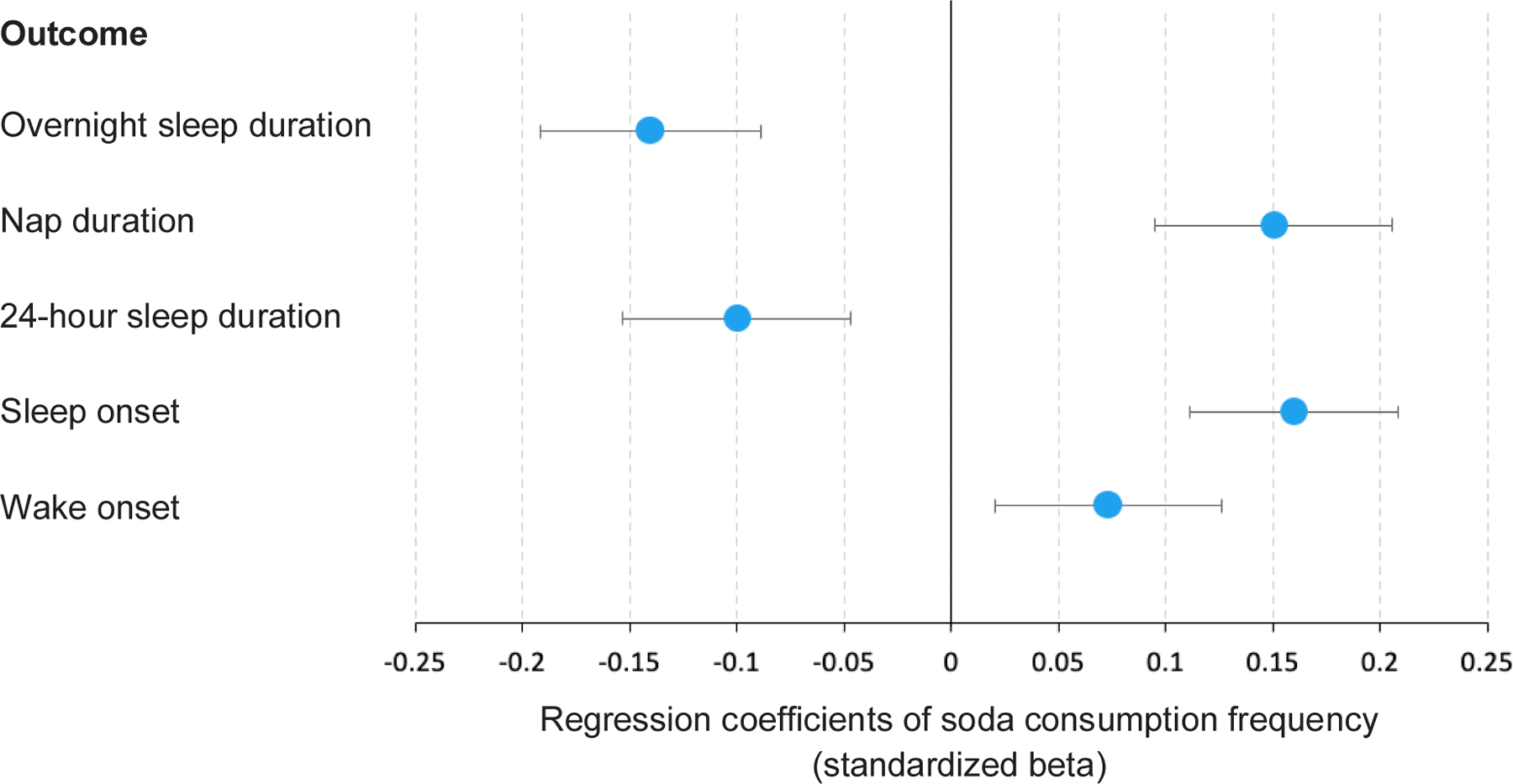
Regression coefficients for soda consumption frequency with sleep measures. Overnight sleep duration (ß =−.14), nap duration (ß =.15), and sleep onset (ß =.16) were associated with soda consumption. 24-hour sleep duration was marginally associated with fast food consumption (ß =−.10). Wake onset was non-significant (ß =.07, p =.15). Error bars represent standard error.
Consumption frequency of fruits and vegetables was associated with nap duration (B = −3.60, 95% CI −6.80 to −0.40, p = .03). For every one unit increase in the consumption of fruits and vegetables, nap duration decreased by 3.6 minutes. At the higher end of the frequency scale, this predicts an 18-minute reduction in nap duration. No other sleep duration or timing measures were associated with fruit and vegetable intake.
Fast food consumption was found to be associated with overnight sleep duration (B = −6.48, 95% CI −11.53 to −1.43, p = .01). For each unit increase in frequency of fast food intake, there was a 6.5-minute decrease in overnight sleep duration. Similarly, total 24-hour sleep duration was negatively associated with fast food consumption (B = −5.80, 95% CI −10.40 to −1.20, p = .01). At the higher end of fast food consumption, this predicts a 17.3-minute reduction in daily sleep. Nap duration, however, was not significantly associated with fast food consumption (B = 2.81, 95% CI −0.68 to 6.31, p = .11) nor any sleep timing measures.
Child soda consumption was significantly associated with overnight sleep duration (B = −9.21, 95% CI −15.83 to −2.59, p = .007). Each unit increase in frequency of consumption of soda was associated with a loss of 9.2 minutes of overnight sleep. Conversely, soda has an opposite effect on nap duration (B = 5.98, 95% CI 1.63 to 10.33, p = .01) with a 6-minute increase in nap duration for every unit increase in soda consumption frequency. Child soda consumption was also marginally associated with 24-hour sleep duration (B = −5.89, 95% CI −11.98 to 0.19, p = .058), suggesting that every unit increase in soda consumption predicted a 5.9-minute decrease in total daily sleep duration. Lastly, soda was positively associated with timing of sleep onset (B = 0.23, 95% CI 0.10 to 0.04, p = .001), with each unit increase in soda consumption predicting a sleep onset timing of 13.8 minutes later (decimalized time: 0.23*60 minutes).
Role of parenting
We considered whether relations between sleep and diet may reflect parenting factors. For instance, it is possible that caregiver laxness may underlie both unregulated dietary consumption and unregulated bed or wake times. Frequency of soda consumption correlated with overall ineffective parenting scores (rs(87) = .25, p = .02) and fruits and vegetables negatively correlated overall parenting scores (rs(87) = −.29, p =.01). Fruits and vegetables were also negatively associated with use of lax strategies (rs(87) = −.29, p =.01) as well as verbosity (rs(87) = −.23, p =.03). However, no other diet measures (fast food) nor any sleep measures correlated with parenting scale scores (see Tables 2 and 3).
TABLE 2.
Partial Pearson’s Correlations Between Sleep Measures and Parenting Scale Scores (n = 89)
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Overnight sleep duration | - | ||||||
| 2. Nap duration a | −.16 | - | |||||
| 3. 24-hr sleep duration | .72*** | .30** | - | ||||
| 4. Sleep onset | −.58*** | .04 | −.42*** | - | |||
| 5. Parenting Scale (Overall) | .17 | −.09 | .09 | −.06 | - | ||
| 6. Laxness Score | .17 | −.07 | .08 | −.04 | .89*** | - | |
| 7. Over-reactivity Score | .05 | −.11 | −.03 | −.03 | .74*** | .48*** | - |
| 8. Verbosity Score | .10 | .05 | .07 | −.06 | .47*** | .32** | .22 |
Note. All correlations control for age and socioeconomic status (SES).
indicates p <.01.
indicates p<.001.
n = 76
TABLE 3.
Partial Spearman’s Correlations Between Dietary Measures and Parenting Scale Scores (n = 89)
| Variables | 1 | 2 | 3 |
|---|---|---|---|
| 1. Fruits and vegetables | - | ||
| 2. Fast food | −.30** | - | |
| 3. Soda | −.02 | .30** | - |
| 4. Parenting Scale (Overall) | −.32** | .15 | .25* |
| 5. Laxness Score | −.29** | .10 | .20 |
| 6. Over-reactivity Score | −.13 | .17 | .21 |
| 7. Verbosity Score | −.23* | −.03 | −.05 |
Note. All correlations control for age and socioeconomic status (SES).
indicates p <.05.
indicates p <.01
DISCUSSION
Using objective sleep measures, we found that preschool children’s sleep duration and timing is predicted by consumption frequency of specific food categories. Consumption of fruits and vegetables was associated with reduced nap duration. Conversely, consumption of fast food and soda were associated with reduced overnight sleep. Those who consumed soda had increased nap duration, but this did not make up for sleep lost at night as 24-hr sleep duration was marginally lower in those with high soda consumption. Importantly, these associations controlled for the influence of age, SES, race/ethnicity, physical activity, and BMI. Furthermore, we found that use of ineffective parenting strategies is related to dietary consumption frequencies (fruits and vegetables, soda) but not sleep quality.
Fast food consumption was a strong predictor of poor sleep at night and this was not compensated for with daytime napping. Daytime naps in preschool children may sometimes be prolonged, seemingly to compensate for insufficient overnight sleep (Ward et al., 2008). However, children who ate more fast food did not show an increase in their nap duration. One possible explanation is that older children, who may be growing out of naps, are also more likely to eat fast food, as caregivers may be more comfortable with offering such options to a 5-year old vs. a 3-year old. Our analyses, however, controlled for age. Notably, there was also no association between measures of parenting and fast food intake or sleep. Thus, we interpret the relationship between fast food consumption and reduced sleep time to reflect the possible impact of increased consumption of dietary fats on sleep duration. Similar findings have been reported in both children and adults, whereby greater intake of dietary fats is associated with decreased sleep duration (Ferrer et al., 2019; Grandner, Kripke, Naidoo, & Langer, 2010). Evidence suggests that digestion of dietary fats, as opposed to protein, may require less energy expenditure (Petzke & Klaus, 2008). This, in turn, could lead to a reduced (perceived) sleep need via a decrease in endogenous sleep signals (Grandner et al., 2010).
Associations between children’s soda consumption and sleep were particularly interesting in that soda frequency predicted nearly 30 minutes less of overnight sleep in children who consume it 2–4 times/week, and those same children were predicted to nap for 24 minutes longer than their peers. A marginal association with 24-hour duration suggests that even with compensatory napping, many of these children are likely not meeting their individual sleep requirements. This may be due to later bedtimes. Soda consumption frequency was the only dietary measure that predicted sleep onset. This seems intuitive, as most sodas contain high amounts of sugar and some caffeine, both of which can impact sleep onset timing (Chaput et al., 2018; Clark & Landolt, 2017). Alternatively, the dietary content of food choices may not be the direct cause of later sleep onset, but rather parenting choices. Counterproductive parenting strategies, such as providing less structure around bed time or allowing snacking later in the evenings, are known to be detrimental towards encouraging sleep (Mindell & Williamson, 2018; Spaeth et al., 2019). Indeed, caregivers of children who consumed more soda scored higher on the Parenting Scale, which measured the use of ineffective strategies.
Fruits and vegetables predicted shorter nap durations, but not overnight sleep duration or timing measures. This is contrary to other reports in children, as greater fruit and vegetable intake often associated with superior sleep quality (Börnhorst et al., 2015; Golley et al., 2013; Tatone-Tokuda et al., 2012). Although, few studies in preschool-aged children, specifically, found associations between sleep and fruit and vegetable intake, but rather between sleep and carbohydrates or overall healthier dietary profiles (Diethelm et al., 2011; Jansen et al., 2019). Nonetheless, our findings could indicate that children who more frequently consume fruits and vegetables are achieving adequate overnight sleep and therefore do not require longer daytime naps to meet their total sleep need. This may reflect healthier development in children who eat fruits and vegetables. Fruits and vegetables are good sources of iron and B-vitamins, both of which are known to support healthy brain development in infancy and early childhood (Prado & Dewey, 2014). Moreover, reduced nap length (Lam, Mahone, Mason, & Scharf, 2011b) and frequency (Kurdziel, Duclos, & Spencer, 2013; Riggins & Spencer, 2020) are thought to reflect greater brain development. However, brain development is also associated with greater 24-hour sleep duration which was inconsistent with our results. Fruit and vegetable consumption was unrelated to overnight and 24-hour sleep duration. Thus, a more likely explanation is that parenting factors underlie access to fruits and vegetables.
Parenting Scale scores correlated with consumption of fruits and vegetables. Caregivers of children who frequently consumed fruits and vegetables were less apt to use ineffective parenting strategies, particularly lax strategies. This indicates that higher consumption of fruits and vegetables may be linked to parenting and that, more broadly, use of more effective strategies is beneficial towards encouraging healthy habits. While our sleep measures did not correlate with any Parenting Scale scores, prior research suggests that positive health behaviors tend to co-occur in families and households (Niermann, Spengler, & Gubbels, 2018). Thus, we cannot rule out that more disciplined parenting underlies both structured bedtimes/waketime as well as fruit and vegetable access.
Our findings, however, are contrary to previous literature that has reported associations between negative parenting styles (laxness, over-reactivity) and greater child sleep problems. Lax parenting has been shown to predict sleep problems such as shorter nighttime and 24-hr sleep durations in 3-year old children (Hall, Zubrick, Silburn, Parsons, & Kurinczuk, 2007; Staples, Bates, & Petersen, 2015). Greater parental over-reactivity has also been suggested to delay sleep onset, as it may increase child arousal (Newton, Honaker, & Reid, 2020). However, parenting style may impact children differently, depending on temperament (Reid, Hong, & Wade, 2009).
Due to the delayed introduction of the Parenting Scale in our data collection, we were only able to examine this relationship in a subset of children. Thus, we may not have had a sufficient sample to identify such effects. Additionally, parental reports were provided by one caregiver in a family unit and therefore could not address lack of consistency or agreement between caregivers, issues that can lead to greater child sleep problems (Hall et al., 2007).
Based on our findings, more frequent consumption of nutritious foods does not appear to encourage better sleep in preschool children per se. Rather, more frequent consumption of less nutritious foods (fast food, soda) appears to more strongly link to poorer sleep outcomes. This may be due to unhealthy fluctuations in sleep-related hormones. Consuming greater quantities of processed, sugary foods influences insulin and leptin levels, which in turn can impact behavioral and circadian cycles, leading to (or sustaining) irregular sleep/wake patterns (Scheer, Hilton, Mantzoros, & Shea, 2009). With circadian misalignment in mind, later timing of meals has been found to be associated with later bedtimes and shorter sleep durations in children (Spaeth et al., 2019). The structure of family meals may also influence sleep habits, as Khan et al. (2017) found that eating at fast food restaurants or in front of the TV was associated with poorer sleep quality.
For the present study, we worked from a conceptual model that dietary choices may impact sleep quality. Experimental support of this directionality has been shown in adult literature. Most notably, St-Onge and colleagues (2016) found that greater sugar consumption was associated with more nighttime arousals and greater saturated fat consumption predicted less slow-wave sleep. However, it is likely a bidirectional relationship, with sleep deficits also potentially contributing to poorer dietary choices (Lundahl & Nelson, 2015). Using an experimental paradigm, Mullins et al. (2017) found that preschool-aged children consumed 21% more calories and 25% more sugar following sleep restriction. This is to say, the associations found between sleep and diet in our data could conversely be interpreted as sleep’s influence on diet. Though, considering the age range, we believe that young children likely have less independence in their food choices and more autonomy surrounding their sleep tendencies. Therefore, we chose to interpret our findings primarily as dietary choices influencing sleep.
The current study used objective sleep measures to determine associations between sleep quality and dietary measures in preschool-aged children, while accounting for many variables known to influence both health factors. Food frequency questionnaires are useful towards gaining a general sense of an individual’s diet, but our results are limited by the lack of detailed food diaries. Future studies could include more detailed caregiver reports of children’s food consumption along with timing of meals, paired with actigraphic recordings. Furthermore, our actigraphy data was averaged across all available days of data, primarily owing to the fact that our caregiver-reported diet measures did not distinguish between weekday vs. weekend consumption. Exploring how sleep and dietary habits may change between weekdays and weekends, and the related associations between both, is worth investigation. Lastly, to more accurately assess the relationship between parenting and sleep, a more relevant measure of parenting, such as a survey on bedtime routines or beliefs around child sleep needs, could better capture this relationship.
CONCLUSIONS
Overall, our results indicate that sleep duration and timing are related to dietary habits in preschool-aged children. Most notably, poorer sleep quality is linked to poorer dietary choices. Parenting factors, such as using more relaxed discipline strategies, appear to influence dietary habits, but not sleep quality. Encouraging healthier dietary choices, and educating caregivers on ways to reinforce such habits, may be means to improve child sleep quality. Future research should investigate timing of meals or consistency in household schedules to better understand these connections between sleep and diet quality.
Supplementary Material
Acknowledgments:
We would like to thank Chloe Andre, Olivia Hanron, and Nora Roscoe for their assistance with data collection and preparation.
Biography
Jennifer Holmes earned her master’s degree from the Harvard Graduate School of Education in 2015. She is currently a research coordinator under Dr. Rebecca Spencer at the University of Massachusetts, Amherst.
Footnotes
Declaration of Interest: No conflicts of interest to disclose.
Data Availability: The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Acebo C, & LeBourgeois MK (2006). Actigraphy. Respiratory Care Clinics of North America, 12(1), 23–30. 10.1016/j.rcc.2005.11.010 [DOI] [PubMed] [Google Scholar]
- Arnold DS, O’Leary SG, Wolff LS, & Acker MM (1993). The parenting scale: A measure of dysfunctional parenting in discipline situations. Psychological Assessment, 5(2), 137–144. 10.1037/1040-3590.5.2.137 [DOI] [Google Scholar]
- Bagley EJ, Kelly RJ, Buckhalt JA, & El-Sheikh M (2015). What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Medicine, 16(4), 496–502. 10.1016/j.sleep.2014.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzofsky M, Smiley-McDonald H, Moore A, & Krebs C (2014). Measuring socioeconomic status (SES) in the NCVS: Background, options, and recommendations. Bureau of Justice Statistics, U.S. Department of Justice, (0213170), 65. 10.1007/BF03061070 [DOI] [Google Scholar]
- Bleich SN, Vercammen KA, Koma JW, & Li Z (2018). Trends in beverage consumption among children and adults, 2003–2014. Obesity, 26(2), 432–441. 10.1002/oby.22056 [DOI] [PubMed] [Google Scholar]
- Börnhorst C, Wijnhoven TMA, Kunešová M, Yngve A, Rito AI, Lissner L, … Breda J (2015). WHO European Childhood Obesity Surveillance Initiative: Associations between sleep duration, screen time and food consumption frequencies. BMC Public Health, 15(1). 10.1186/s12889-015-1793-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Katzmarzyk PT, LeBlanc AG, Tremblay MS, Barreira TV, Broyles ST, … Olds T (2015). Associations between sleep patterns and lifestyle behaviors in children: an international comparison. International Journal of Obesity Supplements, 5(S2), S59–S65. 10.1038/ijosup.2015.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput Jean Philippe, Tremblay MS, Katzmarzyk PT, Fogelholm M, Hu G, Maher C, … Sampasa-Kanyinga H (2018). Sleep patterns and sugar-sweetened beverage consumption among children from around the world. Public Health Nutrition, 21(13), 2385–2393. 10.1017/S1368980018000976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Beydoun MA, & Wang Y (2008). Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity, 16(2), 265–274. 10.1038/oby.2007.63 [DOI] [PubMed] [Google Scholar]
- Clark I, & Landolt HP (2017). Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials. Sleep Medicine Reviews, 31, 70–78. 10.1016/j.smrv.2016.01.006 [DOI] [PubMed] [Google Scholar]
- Córdova FV, Barja S, & Brockmann PE (2018). Consequences of short sleep duration on the dietary intake in children: A systematic review and metanalysis. Sleep Medicine Reviews, 42, 68–84. 10.1016/j.smrv.2018.05.006 [DOI] [PubMed] [Google Scholar]
- Coronado Ferrer S, Peraita-Costa I, Llopis-Morales A, Picó Y, Soriano JM, Nieto FJ, … Morales-Suárez-Varela M (2019). Actigraphic sleep and dietary macronutrient intake. Nutrients, 11, 1–19. Retrieved from https://www.mdpi.com/2072-6643/11/11/2568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diethelm K, Remer T, Jilani H, Kunz C, & Buyken AE (2011). Associations between the macronutrient composition of the evening meal and average daily sleep duration in early childhood. Clinical Nutrition, 30(5), 640–646. 10.1016/j.clnu.2011.05.004 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, & Buckhalt JA (2013). Economic adversity and children’s sleep problems: Multiple indicators and moderation of effects. Health Psychology, 32(8), 849–859. 10.1037/a0030413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franckle RL, Falbe J, Gortmaker S, Ganter C, Taveras EM, Land T, & Davison KK (2015). Insufficient sleep among elementary and middle school students is linked with elevated soda consumption and other unhealthy dietary behaviors. Preventive Medicine, 74, 36–41. 10.1016/j.ypmed.2015.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gingras V, Rifas-Shiman SL, Taveras EM, Oken E, & Hivert MF (2018). Dietary behaviors throughout childhood are associated with adiposity and estimated insulin resistance in early adolescence: A longitudinal study. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 1–12. 10.1186/s12966-018-0759-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golley RK, Maher CA, Matricciani L, & Olds TS (2013). Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. International Journal of Obesity, 37(4), 546–551. 10.1038/ijo.2012.212 [DOI] [PubMed] [Google Scholar]
- Grandner MA, Kripke DF, Naidoo N, & Langer RD (2010). Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Medicine, 11(2), 180–184. 10.1016/j.sleep.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall WA, Zubrick SR, Silburn SR, Parsons DE, & Kurinczuk JJ (2007). A model for predicting behavioural sleep problems in a random sample of Australian pre-schoolers. Infant and Child Development, 16, 509–523. 10.1002/icd [DOI] [Google Scholar]
- Hitze B, Bosy-Westphal A, Bielfeldt F, Settler U, Plachta-Danielzik S, Pfeuffer M, … Müller MJ (2009). Determinants and impact of sleep duration in children and adolescents: Data of the Kiel Obesity Prevention Study. European Journal of Clinical Nutrition, 63(6), 739–746. 10.1038/ejcn.2008.41 [DOI] [PubMed] [Google Scholar]
- Huybrechts I, Vereecken C, De Bacquer D, Vandevijvere S, Van Oyen H, Maes L, … De Henauw S (2010). Reproducibility and validity of a diet quality index for children assessed using a FFQ. British Journal of Nutrition, 104(1), 135–144. 10.1017/S0007114510000231 [DOI] [PubMed] [Google Scholar]
- Hyde M, O’Driscoll DM, Binette S, Galang C, Tan SK, Verginis N, … Horne RSC (2007). Validation of actigraphy for determining sleep and wake in children with sleep disordered breathing. Journal of Sleep Research, 16(2), 213–216. 10.1111/j.1365-2869.2007.00588.x [DOI] [PubMed] [Google Scholar]
- Iglowstein I, Jenni OG, Molinari L, & Largo RH (2003). Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics, 111(2), 302–307. 10.1542/peds.111.2.302 [DOI] [PubMed] [Google Scholar]
- Jansen EC, Peterson KE, Lumeng JC, Kaciroti N, LeBourgeois MK, Chen K, & Miller AL (2019). Associations between Sleep and Dietary Patterns among Low-Income Children Attending Preschool. Journal of the Academy of Nutrition and Dietetics, 119(7), 1176–1187. 10.1016/j.jand.2019.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MKA, Faught EL, Chu YL, Ekwaru JP, Storey KE, & Veugelers PJ (2017). Is it nutrients, food items, diet quality or eating behaviours that are responsible for the association of children’s diet with sleep? Journal of Sleep Research, 26(4), 468–476. 10.1111/jsr.12466 [DOI] [PubMed] [Google Scholar]
- Kjeldsen JS, Hjorth MF, Andersen R, Michaelsen KF, Tetens I, Astrup A, … Sjödin A (2014). Short sleep duration and large variability in sleep duration are independently associated with dietary risk factors for obesity in Danish school children. International Journal of Obesity, 38(1), 32–39. 10.1038/ijo.2013.147 [DOI] [PubMed] [Google Scholar]
- Knutson KL (2013). Sociodemographic and cultural determinants of sleep deficiency: Implications for cardiometabolic disease risk. Social Science and Medicine, 79(1), 7–15. 10.1016/j.socscimed.2012.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, & Guo SS (2002). 2000 CDC growth charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stats, 10(246). [PubMed] [Google Scholar]
- Kurdziel L, Duclos K, & Spencer RMC (2013). Sleep spindles in midday naps enhance learning in preschool children. Proceedings of the National Academy of Sciences of the United States of America, 110(43), 17267–17272. 10.1073/pnas.1306418110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam JC, Mahone EM, Mason TBA, & Scharf SM (2011a). Defining the roles of actigraphy and parent logs for assessing sleep variables in preschool children. Behavioral Sleep Medicine, 9(3), 184–193. 10.1080/15402002.2011.583906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam JC, Mahone EM, Mason T, & Scharf SM (2011b). The effects of napping on cognitive function in preschoolers. Journal of Developmental and Behavioral Pediatrics, 32(2), 90–97. 10.1097/DBP.0b013e318207ecc7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundahl A, & Nelson TD (2015). Sleep and food intake: A multisystem review of mechanisms in children and adults. Journal of Health Psychology, 20(6), 794–805. 10.1177/1359105315573427 [DOI] [PubMed] [Google Scholar]
- Magarey AM, Daniels LA, Boulton TJ, & Cockington RA (2003). Predicting obesity in early adulthood from childhood and parental obesity. International Journal of Obesity, 27(4), 505–513. 10.1038/sj.ijo.0802251 [DOI] [PubMed] [Google Scholar]
- Mindell JA, & Williamson AA (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews, 40, 93–108. 10.1016/j.smrv.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira I, Severo M, Oliveira A, Durão C, Moreira P, Barros H, & Lopes C (2016). Social and health behavioural determinants of maternal child-feeding patterns in preschool-aged children. Maternal and Child Nutrition, 12(2), 314–325. 10.1111/mcn.12132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullins EN, Miller AL, Cherian SS, Lumeng JC, Wright KP, Kurth S, & LeBourgeois MK (2017). Acute sleep restriction increases dietary intake in preschool-aged children. Journal of Sleep Research, 26(1), 48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton AT, Honaker SM, & Reid GJ (2020). Risk and protective factors and processes for behavioral sleep problems among preschool and early school-aged children: A systematic review. Sleep Medicine Reviews, 52, 101303. 10.1016/j.smrv.2020.101303 [DOI] [PubMed] [Google Scholar]
- Niermann CYN, Spengler S, & Gubbels JS (2018). Physical Activity, Screen Time, and Dietary Intake in Families: A Cluster-Analysis With Mother-Father-Child Triads. Frontiers in Public Health, 6(9), 1–12. 10.3389/fpubh.2018.00276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakley NR (1997). Validation with polysomnography of the Sleepwatch sleep/wake scoring algorithm used by the Actiwatch activity monitoring system. Bend: Mini Mitter, Cambridge, Neurotechnology [Google Scholar]
- Parsons AA, Ollberding NJ, Smith L, & Copeland KA (2018). Sleep matters: The association of race, bedtime, outdoor time, and physical activity with preschoolers’ sleep. Preventive Medicine Reports, 12(1), 54–59. 10.1016/j.pmedr.2018.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña MM, Rifas-Shiman SL, Gillman MW, Redline S, & Taveras EM (2016). Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood. Sleep, 39(9), 1653–1661. 10.5665/sleep.6086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penpraze V, Reilly JJ, MacLean CM, Montgomery C, Kelly LA, Paton JY, … Grant S (2006). Monitoring of physical activity in young children: How much is enough? Pediatric Exercise Science, 18(4), 483–491. 10.1123/pes.18.4.483 [DOI] [PubMed] [Google Scholar]
- Petzke KJ, & Klaus S (2008). Reduced postprandial energy expenditure and increased exogenous fat oxidation in young woman after ingestion of test meals with a low protein content. Nutrition and Metabolism, 5(1), 1–9. 10.1186/1743-7075-5-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plancoulaine S, Reynaud E, Forhan A, Lioret S, Heude B, Charles MA, … Thiebaugeorges O (2018). Night sleep duration trajectories and associated factors among preschool children from the EDEN cohort. Sleep Medicine, 48, 194–201. 10.1016/j.sleep.2018.03.030 [DOI] [PubMed] [Google Scholar]
- Prado EL, & Dewey KG (2014). Nutrition and brain development in early life. Nutrition Reviews, 72(4), 267–284. 10.1111/nure.12102 [DOI] [PubMed] [Google Scholar]
- Rashid V, Engberink MF, Van Eijsden M, Nicolaou M, Dekker LH, Verhoeff AP, & Weijs PJM (2018). Ethnicity and socioeconomic status are related to dietary patterns at age 5 in the Amsterdam born children and their development (ABCD) cohort. BMC Public Health, 18(1), 1–11. 10.1186/s12889-017-5014-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid GJ, Hong RY, & Wade TJ (2009). The relation between common sleep problems and emotional and behavioral problems among 2- and 3-year-olds in the context of known risk factors for psychopathology: Sleep in toddlers. Journal of Sleep Research, 18(1), 49–59. 10.1111/j.1365-2869.2008.00692.x [DOI] [PubMed] [Google Scholar]
- Riggins T, & Spencer RMC (2020). Habitual sleep is associated with both source memory and hippocampal subfield volume during early childhood. Scientific Reports, 10(1), 1–9. 10.1038/s41598-020-72231-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer FAJL, Hilton MF, Mantzoros CS, & Shea SA (2009). Adverse metabolic and cardiovascular consequences of circadian misalignment. Proceedings of the National Academy of Sciences of the United States of America, 106(11), 4453–4458. 10.1073/pnas.0808180106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spaeth AM, Hawley NL, Raynor HA, Jelalian E, Greer A, Crouter SE, … Hart CN (2019). Sleep, energy balance, and meal timing in school-aged children. Sleep Medicine, 60, 139–144. 10.1016/j.sleep.2019.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer RMC, Campanella C, de Jong DM, Desrochers P, Root H, Cremone A, & Kurdziel LBF (2016). Sleep and behavior of preschool children under typical and nap-promoted conditions. Sleep Health, 2(1), 35–41. 10.1016/j.sleh.2015.12.009 [DOI] [PubMed] [Google Scholar]
- St-Onge MP, Roberts A, Shechter A, & Choudhury AR (2016). Fiber and saturated fat are associated with sleep arousals and slow wave sleep. Journal of Clinical Sleep Medicine, 12(1), 19–24. 10.5664/jcsm.5384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staples AD, Bates JE, & Petersen IT (2015). Bedtime routines in toddlerhood: Prevalence, consistency, and associations with nighttime sleep. Monographs of the Society for Research in Child Development, 80(1), 141–159. 10.1111/mono.12149.Chapter [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tatone-Tokuda F, Dubois L, Ramsay T, Girard M, Touchette E, Petit D, & Montplaisir JY (2012). Sex differences in the association between sleep duration, diet and body mass index: A birth cohort study. Journal of Sleep Research, 21(4), 448–460. 10.1111/j.1365-2869.2011.00989.x [DOI] [PubMed] [Google Scholar]
- Tauman R, & Gozal D (2006). Obesity and obstructive sleep apnea in children. Paediatric Respiratory Reviews, 7(4), 247–259. 10.1016/j.prrv.2006.08.003 [DOI] [PubMed] [Google Scholar]
- Ward AL, Reynolds AN, Kuroko S, Fangupo LJ, Galland BC, & Taylor RW (2019). Bidirectional associations between sleep and dietary intake in 0–5 year old children: A systematic review with evidence mapping. Sleep Medicine Reviews, 49, 101231. 10.1016/j.smrv.2019.101231 [DOI] [PubMed] [Google Scholar]
- Ward TM, Gay C, Anders TF, Alkon A, & Lee KA (2008). Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. Journal of Pediatric Psychology, 33(6), 666–672. 10.1093/jpepsy/jsm102 [DOI] [PubMed] [Google Scholar]
- Westerlund L, Ray C, & Roos E (2009). Associations between sleeping habits and food consumption patterns among 1011-year-old children in Finland. British Journal of Nutrition, 102(10), 1531–1537. 10.1017/S0007114509990730 [DOI] [PubMed] [Google Scholar]
- Zheng M, Campbell KJ, Scanlan E, & McNaughton SA (2020). Development and evaluation of a food frequency questionnaire for use among young children. PLoS ONE, 15(3), 1–16. 10.1371/journal.pone.0230669 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


