Abstract
Background:
Most healthcare providers are unaware of the extraordinary opportunities for implementation in healthcare which can be enabled by 5G wireless networks. 5G created enormous opportunities for a myriad of new technologies, resulting in an integrated through 5G ‘ecosystem’. Although the new opportunities in healthcare are immense, medicine is slow to change, as manifest by the paucity of new, innovative applications based upon this ecosystem. Thus, emerges the need to “avoid technology surprise” - both laparoscopic and robotic assisted minimally invasive surgery were delayed for years because the surgical community was either unaware or unaccepting of a new technology.
Database:
PubMed (Medline) and Scopus (Elsevier) databases were searched and all published studies regarding clinical applications of 5G were retrieved. From a total of 40 articles, 13 were finally included in our review.
Discussion:
The important transformational properties of 5G communications and other innovative technologies are described and compared to healthcare needs, looking for opportunities, limitations, and challenges to implementation of 5G and the ecosystem it has spawned. Furthermore, the needs in the clinical applications, education and research in medicine and surgery, in addition to the administrative infrastructure are addressed. Additionally, we explore the nontechnical challenges, that either support or oppose this new healthcare renovation. Based upon proven advantages of these innovative technologies, current scientific evidence is analyzed for future trends for the transformation of healthcare. By providing awareness of these opportunities and their advantages for patients, it will be possible to decrease the prolonged timeframe for acceptance and implementation for patients.
Keywords: 5G, Telecommunications, Healthcare, Artificial intelligence, Internet of Things
INTRODUCTION
Today, the explosion of several information and communications technologies radically changes and creates an extraordinary ecosystem for new opportunities in an unprecedented rate. Every sector and industry, including healthcare, has been impacted by digital transformation. Digital innovations including the further expansion of telehealth, the development of fifth generation wireless networks (5G), artificial intelligence (AI) approaches such as machine learning and deep learning, Big Data (BD) and supercomputing, and the Internet of Things (IoT), as well as digital security capabilities such as blockchain, have created an extraordinary opportunity to create an integrated ecosystem for new opportunities in healthcare and other industries.1 These developments could potentially address some of the most urgent challenges facing health service providers and policy makers, including universal, equitable, sustainable healthcare service.
Together, these integrated technologies can fundamentally change screening, diagnosis and monitoring of diseases, enable more accurate profiling of disease progression and further refine and/or personalize treatments. Nascent technologies for therapy, such as next generation communications, AI, IoT, telesurgery, to name a few, will be addressed.
The fifth generation wireless networks (5G) have an extremely low latency (less than one millisecond (ms) of delay compared to about 70 milliseconds on the 4G network), together with higher data transmission speed (about 100-fold from the current 10 megabit per second on 4G) by using higher frequency millimeter waves compared to existing networks.2,3 All this increase in function occurs while it simultaneously reduces energy consumption by all the connected devices4 by having low power requirements. However, because 5G transmits at higher frequencies, signal degradation becomes a greater challenge, and “base stations” need to be densely populated (approximately every 250 m).5 Yet, such deployment provides unique opportunity to bring all those technologies locally to the point of care – and in real time.
However, a word of caution is needed. There are critical biological and physiologic factors of basic science that must be taken into consideration in developing and applying the new opportunities which the 5G ecosystem provides, especially for telemedicine – not all the capabilities of 5G can be leveraged at this moment, especially the huge number of healthcare related instruments and devices which are available on the IoT. Likewise, there are unique requirements within the domain of human interface technology (HIT) that must be investigated in order to optimize human use of the new communication capabilities; in addition, there are limitations and challenges in exploiting the communications spectrum. Finally, there are other technologies in addition to the Internet, such as AI, BD repositories, computational analytics (CA), supercomputers (including soon to be commercialized quantum computers) and factors involved in accessing and storage in ‘the cloud’ which dramatically impact the opportunities to exploit the new communications systems.
An existing and special use case is telemedicine, which is now well established and can be advantageous as it can provide more efficient and equitable distribution of healthcare when limited resources are available and patients’ transportation challenges might exist, all of which reduces unnecessary visits and exposure risks. Evidence of the effectiveness of this ecosystem will be presented in the review of the COVID-19 pandemic (below).
Finally, the sheer capacity of 5G combined with AI, and the capability to transfer data in order to accumulate and analyze BD, can be valuable in understanding the development of disease progression and improving forecasting capabilities.5 Due to all of the above, 5G has been already adopted by a few centers across the world.1,6–8
Although, telemedicine has been widely applied under different circumstances and applications, it faced several difficulties stemming from the limited latency and speed, especially in telesurgery applications which are reviewed below.
Therefore, this report is limited to reviewing the literature of healthcare application of the 5G which already exists and, after presenting the communication basic principles, to discuss future applications in the context of the other critical supporting infrastructures and biologic principles.
METHODS
Search Strategy and Article Selection
All published studies regarding clinical applications of 5G were retrieved. The present study was conducted in accordance with the protocol agreed on by all authors was the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.9,10 PubMed (Medline), and Scopus (Elsevier) databases (last search: December 3, 2020) were searched using the following medical subject heading (MeSH) terms and text words based on the following search strategy:
Group A terms: “5G” OR “high bandwidth telecommunications”
Group B terms: “telemedicine” OR “telepresence”
Group C terms: “telesurgery” OR “teleradiology” OR “telepathology” OR “teleophthalmology” OR “teledermatology”
Group’s A, B, C and D terms were combined. Therefore, our search algorithm was as follows: (((((((5G)) OR (()))) AND ((((((((((((5G)) AND (telemedicine))) OR ((telemedicine))) OR ((telepresence))) OR ((telesurgery))) OR ((teleradiology))) OR ((telepathology))) OR ((teleophthalmology))) OR ((teledermatology)))))).
Inclusion- Exclusion Criteria
Of the articles retrieved through the above-described search strategy only those that met the following criteria were included to this systematic review:
Original papers were only included. Review papers that met the inclusion criteria were not included; However, their reference lists were used to retrieve any relevant study of any publishing date.
All articles should report at least one clinical example of 5G.
Articles conducted in the last 5 years.
Articles written in English language.
Additional limits were applied to restrict manuscripts to those related to human subjects.
Article Selection
Articles were retrieved when their abstract were judged to possibly meet the inclusion criteria by two independent reviewers (EG, RS). If either author suggested retention, the study was included. The process was repeated for abstract review and, again, if either reviewer suggested retention, the study was included. All the retrieved article titles and abstracts were screened for relevant manuscripts. A full text review of the selected relevant articles was made in order to detect the studies included in this systematic review. Moreover, relevant full text review and/or systematic review manuscripts were used to retrieve articles of any publishing date from their reference list and include them to this systematic review.
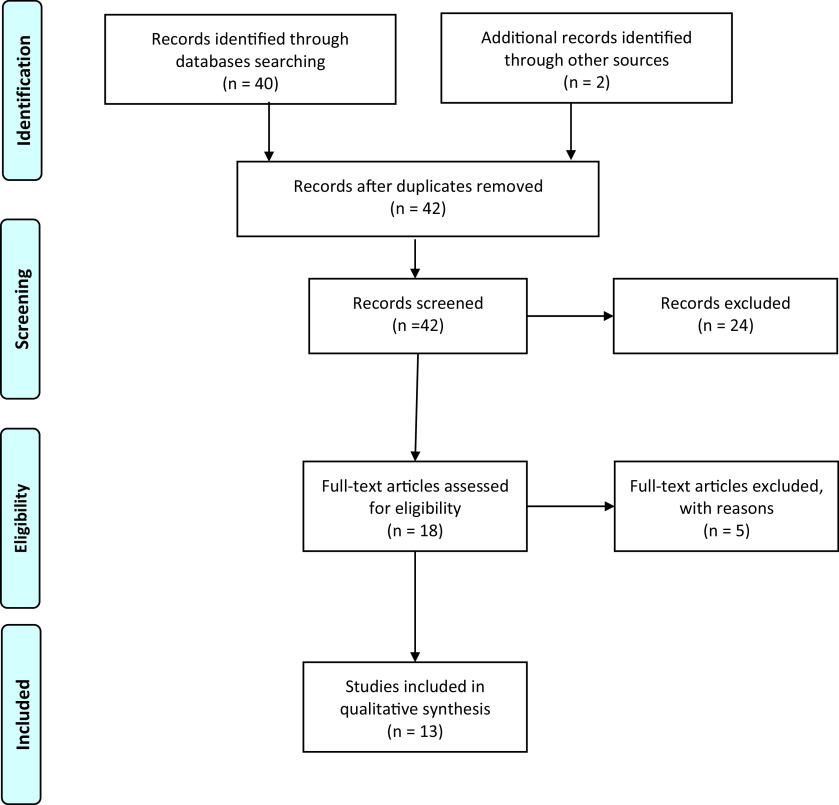
The PRISMA flow diagram of the search strategy is presented in the Figure. Note: Many other articles that supported the discussion and remainder portion of the manuscript were included.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram.
RESULTS
Data Extraction
A total of 40 articles were retrieved and screened (title/abstract) and two more were retrieved from other sources and their abstracts were assessed for eligibility. Twenty-four of those were unanimously considered as nonrelevant and were excluded from further analysis. From a total of 18 full text articles which were evaluated, five were excluded with other reasons and therefore 13 articles are included in this systematic review. The limited number of relevant publications emphasizes the lack of knowledge of and attention to these revolutionary technologies, and the opportunities for future implementation in healthcare.
The following data were extracted from each study: Author, publication year, Country, Type of study, Primary specialty, Participants, Results/Conclusion, and Remarks (Table 1). As can be seen in Table 1, the geographical location of the studies was mainly from China (8/13). Ten of the studies were clinical applications or at least had a clinical component using 5G technology.
Table 1.
Summary of Studies of 5G Medical Applications and Their Variables of Interest
| Study | Year | Country | Type of Study* | Primary Specialty Clinical/Research/Both | No. of Participants | Results/Conclusion | Remarks |
|---|---|---|---|---|---|---|---|
| Diagnostic applications | |||||||
| Naruse et al.38 | 2020 | Japan | Cardiotocograph Lab testing | Ob/GynClinical | - | Successful transmission via 5G | |
| Angelucci et al.22 | 2020 | Italy | Observational | Pneumonology Both | 18 volunteers | Better than traditional telemedicine systems | Home monitor chronic obstructive pulmonary disease via smartphone 5G application |
| Ye et al.33 | 2019 | China | Tele-ultrasound in COVID-19 | Radiology/ Internal medicine Clinical | 23 patients | 5G robot-assisted remote ultrasound effectively allows cardiopulmonary assessment of COVID-19 patients | Larger studies and resolving technical obstacles are required before widespread |
| Zhou et al.55 | 2020 | China | Observational | Cabin hospital for COVID-19. Engineer common healthcare profile | Engineering Research only | Prospect of 5G software wireless network better than wired conventionally | 1 – 2 days to setup.Software designed network |
| Surgical applications | |||||||
| Zheng et al.48 | 2020 | China | Preclinical Research lab latency time by distance | Robotic Laparoscopy surgery Clinical | 4 swine nephrectomy part hepatic cholecystectomy | Ultraremote distance 300 km, latency 164 ms round trip 114 ms packet loss 1.2% | Remaining obstacles for clinical use are discussed |
| Tian et al.52 | 2020 | China | Clinical | Orthopedics Clinical only | 12 patients. 62 pedicle screw implanted | 5G telerobotic spinal surgery is safe, efficacious, and feasible | Newer systems for bone grinding nerve decompression required. |
| Jell et al.40 | 2019 | Germany | Telesurgery & Surgery Education | General Surgery & engineers Both clinical and basic research | N = 5 pigs Surgeons and engineers | 5G data 95 – 106 MB/sec, 75% data in 30 ms. Latency 146 – 202 ms allows telesurgery | 2 patients – 1– 6 km distance Need more research, especially clinical |
| Lacy et al.41 | 2019 | Spain | Clinical | Surgery Clinical only | 2 patients underwent lap operation | 5G-assisted telementored surgery is safe, and feasible | It would be an optimal resource for underdeveloped areas and/or scarcity of experienced surgeons |
| Imaging applications | |||||||
| Wu et al.31 | 2020 | China | Tele-ultrasound COVID-19 | Radiology & Internal medicine Clinical | 4 patients | Teleultrasound protocol allows early diagnosis and reassessment available in the isolation ward | For early imaging assessment of COVID-19 |
| Madder et al.35 | 2020 | USA | Preclinical | Transcontinental Interventional Cardiology Both | Telestenting. 2 percutaneous coronary intervention ex vivo models (36 lesions) | Transcontinental robotic percutaneous coronary intervention is feasible in ex-vivo models @ 3500 mi latency = 162 ms | Easy to perform percutaneous coronary intervention lesion with 5G |
| Ye et al.60 | 2020 | China | Research Engineer stats | Engineers Community research | COVID-19. Health information technology community and decision makers | China’s shows health info tech has pivotal role in COVID-19 pandemic | Ηealth information technology has much more work facing the global pandemic of COVID-19 |
| Hong et al.54 | 2020 | China | COVID-19 Observational. 5G multimodal telemedicine network functionality research | Various healthcare professionals Engineers Community research | 152 remote computed tomography scans. Focus on resource management for telemedicine | The COVID-19 telemedicine system increases diagnostic accuracy of difficult cases and improves treatment of severe/critical case | Additionally, 1094 patients received telephone consultations or interventions from 137 clinicians |
| Yu et al.32 | 2020 | China | Tele-ultrasound COVID-19 | Radiology/ Internal medicine Clinical only | 2 patients ultrasound clinical trial | Tele-ultrasound for early diagnosis 700 km teleradiology diagnosis | 5G robotic ultrasound is easy to perform at bedside remotely |
DISCUSSION
1. Communication Basic Principles
5G technical Parameters
Currently, mobile data transmission is mainly based on 4G/LTE or on Wi-Fi. The 4G/Long-Term Evolution (LTE) offers a minimum signal delay of 20 ms mainly designed for internet (e.g., browsing and video streaming) which is well below that required for real-time integration of sensor data. Furthermore, Wi-Fi solutions are an alternative, but they can be interrupted by other users at any time due to unprotected radio bands.11
The new 5G telecommunication standard offers high bandwidths as compared to the current mobile transmission standard 4G/LTE: 5G is a 100 times higher data transmission rate (up to 10GB/s), and, at the same time, an extremely low latency time (<1ms), and 1000 times higher capacity (bandwidth) with a high quality of service which is almost equal to the zero data response time in the real world.12 Millimeter wave telecommunication is such an advantageous technology for 5G networks because it allows extremely high data transfer speeds (several gigabits per second). However, a large number of small cells with limited radius deployment must be used to achieve seamless and efficient coverage and form a 5G ultradense cellular network. The cells may be of different size, and they are classified as Femtocells, Picocells or Microcells. The massive multi-input, multioutput is an evolving technology capable to transmit multiple data beams at a time, thus increasing the throughput and spectrum effectiveness in both uplink and downlink.13
Additionally, 5G requires up to 10 times less energy than the previous 4G/LTE mobile communications standard.12 It is expected that the 5G network will have a 1,000-fold rise in traffic in the coming decade, although the energy usage of the whole infrastructure will be just half of today’s system's consumption. Therefore, this is a crucial factor for reducing the total cost of ownership, including the environmental impact of the networks.13
The above mentioned qualifications meet the requirements imposed by many new digital applications like the interconnection between physical and virtual objects, the IoT, autonomous driving,14 machine-to machine connection in industrial production,15 as well as different medical applications that were previously technically impossible to implement.16 The latter systems conform to the Ultrareliable low-latency communication protocol where a sub-millisecond latency with a response rate smaller than 1 packet loss in 105 packets is required for patient safety.17
To achieve their goals, the industry reached a consensus to use emerging major technologies like network function virtualization (NFV) and software-defined networking (SDN). The most remarkable technology to simplify a healthcare network management is SDN, which takes apart the network control from the data forwarding plane. Thus, the control plane oversees the entire network below as well as the network resources by using a programmable Application Programming Interface (API) .17
As 5G is expected to greatly influence our lives, its security is even more important than before. Two types of 5G network security are implemented:
Security using software such as firewall applications installed in the perimeter of any network, based on need.
AI-based security as it can sensibly identify the terminal actions and requirements on time to avoid service interruptions.
In order to further enhance the security one can also use security automation and Blockchain security assessment techniques.17
The 5G network requires more complex antenna design and distribution in the space needed to be covered in order to achieve faster speeds and low latency. Therefore, specific antennas are proposed for the 5G network, also known as active antennas (in contrast to passive antennas used in 4G) which differentiate 5G network in terms of speed, latency, and security.
Recently, big international telecommunication companies have taken the lead in the competition for the upcoming 5G cellular technology, as it is thought to be their most important future source of revenue. It is expected that the 5G network will be broadly introduced as a simple framework for hyperconnected mobile devices and will ultimately evolve into a modern 5G platform. It should be noted, however, that there is currently no uniform 5G standard. For a detailed technical review of the architecture and security of 5G Technology, the reader can refer to reference.17
Looking beyond 5G, the future generation of telecommunications (6G), is already in the late research and development (R&D) phases (Technology Readiness Levels - TRL 3–5), with an exponential increase in bandwidth and capabilities that will allow implementation of applications that even 5G cannot fulfil (Table 2). This is especially important in the area of network security/privacy and maintaining Healthcare Insurance Portability and Accountability Act (HIPAA)5 compliance.
Table 2.
Parameters of Current and Next Generations of Telecommunications*
| Generation | Bandwidth | Speed | Latency |
|---|---|---|---|
| Current 4G | 5–200 MHz | 10–50 megabits per second | 50–60 ms |
| 2020–2030 5G | 1 –23 GHz | 10–200 gigabits per second | 1–10 ms |
| 2030–2040 6G | 1–7 THz | 1–7 terabits per second | 1–10 ms |
Due to multiple companies and each company’s versions, these are estimates of the averages of generations.
With the current full life cycle development of a technology product from concept to commercialization at 10–15 years, it is likely that the 6G may be available within that time period, or perhaps slightly sooner. With integration of other advanced technologies, such as smart devices, composed of micro-electro-mechanical-systems (MEMS) sensors, AI and computational analytics on a single chip, automatic diagnosis can be immediately generated at the point of care (edge computing) and transmitted to a waiting consulting physician or directly to the electronic medical record. Another emerging area of 6G, will support virtual reality (VR), where a simulated presence is generated by computer graphics and allows users to interact with the simulated elements in a seemingly real way. Augmented reality (AR), where computer-aided information is generated and graphically augmented (overlayed) to the display real-time, can also have broad implications for healthcare. Counselling patients and preoperative consent can likely be enhanced with augmented reality, and nonclinical functions in hospitals such as navigation, in particular for visually impaired patients.5 Both humans and machines will use 6G which will allow for truly immersive extended reality (XR) and high-fidelity mobile hologram which could have enormous implications for healthcare; but although the 6G networking will provide ample potential for VR/AR or even XR, the immersive experience of these alternative realities has yet to find a practical application within the clinical healthcare field.
Telemedicine
The most use of 5G networks in healthcare is currently Telemedicine, and when the world emerges from global COVID-19 pandemic, healthcare will become a hybrid medical practice of live’ face-to-face’ clinical care and telemedicine-based care.
The World Health Organization (WHO) has announced COVID-19 was a “pandemic” (World Health Organization,2020). With the nonlinear rapid disease expansion, COVID-19 has caused widespread healthcare, socio-political and economic impact.18–20 Countries and healthcare systems around the world have been forced to rapidly adapt to telehealth and digital innovations to mitigate the impact of the risk of virus transmission to what is widely regarded as the “new normal”. The clinical adoption of telemedicine has been much slower (usually only used for special-use opportunities), however with this COVID-19 pandemic, there has been a surge in all digital communications.
Healthcare applications, especially telemedicine, has finally rapidly expanded, mainly because it enables physicians to remotely evaluate their patients. This can be advantageous for several reasons:
Telemedicine can assist to more efficient and reasonable distribution of constrained healthcare assets, by delivering support with innovative service design that already exists, to distant areas where there is a shortage of physicians and other healthcare professionals, by reducing travel transport challenges and the associated carbon footprint. Furthermore, in acute cases patients could receive immediate specialist input even if one is not available locally and access to care for both chronic and acute disease patients could be reduced while maximizing the quality of the telemedicine consultation.
During the COVID-19 pandemic, telemedicine is no more focused on only targeting remote regions, but it is rapidly becoming a new standard of care adopted by multiple centers across the world, as it enables triaging prior to patients’ arrival into hospital to avoid unnecessary visits and exposure risks.1, 6–8
Finally, the collection, storage and transmission of data offer the potential of combining telemedicine with AI and many other innovative technologies. When used prospectively with longitudinal data, vast swathes of new knowledge such as disease progression and real world, real-time incidence calculation could be harnessed. Moreover, this could grow into a consistent source of longitudinal data which would be valuable in the development of disease progression forecasting capabilities by training and incorporating AI.
2. Other Critical Supporting Infrastructures
Even as the Internet has been exponentially growing, and the communication systems (cabled and wireless) have likewise logarithmically increased, there are other parallel information-based technologies that have rapidly grown as well. In most cases, these technologies have developed in their own silo, usually due to inadequate communication systems to unite them. The emerging 5G wireless networks are finally providing the bandwidth, speed, and low-latency to act as a force to begin integrating these parallel technologies into an ‘information ecosystem’. What enables this huge increase is the change of the networking from connections by physical ‘wires’ (cables), to wirelessly distributing the network using software (software designed networks – SDN) and “network slicing”: an analogy of instead of ‘laying another wire or cable’, the software instead ‘slices’ the wireless network into different frequencies when a new connection is needed. This allows the integration of ‘other’ technologies, and most importantly the IoT which also supports robotics and sensor technology, BD acquisition, data repositories, AI, computational analytics, and supercomputing (Appendix 1).
The new telecommunications networks are not only connecting human to humans but also connecting ‘smart devices’ (especially the 8 billion smart phones) of the IoT total of 14.2 billion devices now, with projections of 25 billion by 2025 and 60 billion by 2030. In addition, there is massive data acquisition continuously monitoring by microsensors from machines (devices, equipment, systems) or living systems including humans, most of which is machine to machine communication for maintenance and/or autonomous control – and all linked together using Global Positioning System (GPS) for precise geolocation.
Careful attention must be paid to the interface between the HIT that provides the final connection of the communication system with a person, be it the current video technologies, or any of the forms of VR, or possible future interfaces such as wearable contact lens displays, or the ultimate brain-machine interface. After all, this information ecosystem is a ‘system-of-systems’, with each link in the chain dependent upon the success of all others, that decisively results in success.
3. Fundamental Biologic Principles
When integrating any two systems, there are points of ‘connection’ (interface). With systems that are alike (for example machine or electronic connections), their interfaces are similar (physical systems) and the solution is relatively straight forward since both systems obey physical laws. However, when integrating two dissimilar systems (machine and human), the connection (interface) becomes much more intricate, since both the laws of physics and biology (which are radically different) must be accommodated. This integration is defined as HIT: a means or place of interaction between two systems; especially, the interface between people (users) and computers or devices.21
The new advanced technologies, such as telecommunications, computers, imaging, etc., work at microsecond speeds; humans perceive and react milliseconds, so an interface must be built such that the human systems can be accommodated and enhanced (see Table 3) for the effect of how telecommunication latency can affect human performance). For example, the recent developments of 5G telecommunications that results in huge increase in bandwidth and speed with extraordinary low latency (∼ 1 ms) has the potential to extend the distance for safely performance of remote surgery (telesurgery). Conversely, there are human ‘systems’ which are extraordinarily complex such as the human neurosensory system (with 23 different types of nerve endings for sensing, at a density of 1000 nerve endings per cubic millimeter, in an average hand surface area of 4000 mm, each sending stimuluses at 1000 times/second), such that even recent exponential advances in microtechnologies and computation power are woefully insufficient to currently create high-fidelity haptics to provide the sense of touch for a safe robotic system for surgery. Examples of many other mismatches between human (especially the 5 major senses and the neuromuscular responses) and ‘machine’ are in Appendix 2, thus emphasizing the need for greater attention (and research) in human interface technologies.
Table 3.
Human Performance (Laparoscopic Knot Tying) Compensation Under Conditions of Latency
| Latency (ms) | Errors | Perception of Delay | Compensation |
|---|---|---|---|
| 0 ms | 0 | None | None |
| 50 ms | 0 | None perceived | Automatically subconsciously |
| 100 ms | 0 – 1 | Aware of a ‘difference’, Unclear of cause | Automatically and deliberately |
| 150 ms | 0 – 1 | Aware of delay | Consciously takes action – e.g., move-and-wait |
| 200 ms | > 2 | Very aware of delay | Attempts various methods, mostly successful |
| > 300 ms | critical | Very concerned of delay | Frustrated, often unsuccessful |
4. Clinical Applications Using 5-G Wireless Networking
The current capacity of 5G telecommunications provide the perfect ecosystem to reassess care delivery and to adopt the synergistic and complementary digital technologies discussed above, incorporating AI utilization, and facilitated by 5G networks, IoT and BD and computational analysis. Below are some clinical applications of using 5G:
The following examples illustrate the large breadth of healthcare clinical services that can now be provided because of the emerging 5G networks.
Pulmonology
Up to now, there is conflicting evidence that telemedicine solutions help address chronic respiratory diseases.22
However, a recent paper (see Table 1), profiting from the capacity to parallel several IoT applications due to the coexistence of multiple streams by 5G connectivity, presented a home telemonitoring system designed for chronic respiratory patients.
All data were streamed to an iPad which was connected via Wi-Fi to a 5G router and thereafter to the 5G infrastructure. The authors could access the data by means of a dedicated dashboard. The whole system was tested on 18 healthy volunteers during nonsupervised recordings lasting at least 48 hours. Due to the 5G bandwidth, the results showed that the system provided more complete and clinically relevant and real-time information than other previously studied telemedicine systems.22
Medical Imaging and 5G
As a massive number of images accumulates and manual segmentation requires a lot of time, it becomes a big challenge for analyzing and diagnosing and furthermore, it may not meet the demand of analyzing big images data.23 This problem is attacked by using automatic methods for sectioning medical images (SMI) to obtain any viewing angle via multiplanar reconstruction (MPR) by using a plethora of various technologies, for example, region-based methods, clustering methods, threshold algorithms, machine learning, and deep learning.24
However, since each MPR’s interaction requires the reconstruction of the raw data, thus hundreds of megabytes of SMI data must be transferred, resulting in a higher requirement for network transmission via Internet without a bottleneck creation as well as a higher security risk of data leakage.25 This is an example of the advantages and opportunity for 5G communication with Software Designed Networks (SDN) and ‘network slicing’ to more flexibly, efficiently and cost effectively provide enhance Intranet and Internet capability and security.
Of course, this is not the case for less demanding imaging such as echocardiography or dermatology images transfer, where effective transmission of high-quality images can be accomplished either through low-cost transmission systems or with images/video from publicly available apps.26,27 The same applies to otolaryngologic exams, especially regarding remote of video-otoscopy images, as a recent review suggests that they can deliver adequate information suitable for diagnosis in most cases and results in high levels of user satisfaction.28
Diagnostic pathology is mainly depending upon image quality. The conventional cytological glass slide examination is time consuming as only one person can view it at a time. Beyond the use of the static images in telepathology, dynamic telepathology has recently been introduced, where the transmission of microscopic slide images to the recipient is done in real time via live telecommunication. Furthermore, through the implementation of remote robotic control of the microscope, the consulting pathologist can also control the magnification, a feature extremely useful for interoperative pathological analysis.29 The introduction of advanced, micro-miniaturized imagers, such as optical coherence tomography (OCT) and near infrared spectroscopy, are being introduced through gastrointestinal endoscopes, providing immediate ultrahigh-resolution images of intra-cellular structural pathology for the endoscopist,30 which can be streamed live to the consulting pathologist and/or archived for future reference.
Remote Ultrasonography
Much interest has been shown in robotic-assisted teleultrasound and expert remote consultation. During this procedure, the operator manipulates a simulated robotic hand to remotely control the robotic arm at the patient end. An ultrasound probe is fixed on the robotic arm to scan the patient. Up to 2GB of ultrasonic image data from a lung ultrasound scan lasting a few minutes is produced and transmitted at high speed with low latency. The robotic arm is movable and easy to use, allowing clinicians to collect lung images directly and monitor patients remotely.
From a technical point of view, the network download rate is 930 Mbps and the upload rate of 132 Mbps, maintaining a stable level with latency being at 23–30 ms and the network jitter at 1–2 ms, thus allowing a smooth scanning by the robotic arm and an undetected time delay. No package loss was detected during all the procedures and thus the images quality transmitted to the attending physician had no visual reduction compared with those obtained by traditional on-site examination. Therefore, it is concluded that by breaking the temporal and spatial limitations due to the high bandwidth network, robotic-assisted teleultrasound succeeds in bridging the gaps between specialists and patients from remote cities.31 This real-time image acquisition of robotic ultrasound across long distances has the following advantages:
Examiners can be protected from cross infection by remotely monitoring patients without any personal contact thus diminishing the number of those who come into contact with the patients.
Experts by using this technology can remotely perform real-time ultrasound scan on patients in distant locations, thus alleviating the pressure of shortages of medical resources.
The robotic ultrasound can be performed anywhere, at the patient’s bedside or even in the patient’s home.32
As can be seen from Table 1, there are three relevant articles using robotic teleultrasound lung scanning for suspected and/or declared COVID-19 patients, all originating from China:
The first article evaluated robot-assisted teleultrasound and expert remote consultation for early cardiopulmonary evaluation by performing lung ultrasound, brief echocardiography, and blood volume assessment in four patients hospitalized in isolation wards and the examination results were immediately delivered to the attending physicians. Furthermore, the authors report the use of this robot-assisted teleultrasound examination as a routine for evaluating acute abdominal diseases such as cholecystitis, appendicitis, pancreatitis, and urolithiasis. In addition, teleultrasound has been applied in focused assessment with sonograph for trauma (FAST) and extended FAST, musculoskeletal injuries, thyroid gland diseases, and subcutaneous soft tissue lesions.31
The second article used a robotic ultrasound system, integrating remote robotic control, audio-visual communication and ultrasound examination, and assessed its feasibility in 23 COVID-19 cases. Furthermore, they established a standard examination and evaluation protocol as follows: A cardiopulmonary assessment completed successfully for all patients lasting on average 10 to 20 min. An ultrasound image contained information regarding distribution characteristics, morphology of the lungs and surrounding tissue lesions, left ventricular ejection fraction, right/left ventricular end diastolic area, pericardial and/or pleural effusion, and lung ultrasound score. Although they had excellent results in COVID-19 detection, they admit that the 5G robotic-assisted remote ultrasound system is still in its infancy, has several limitations (i.e. restrictions of the examination position of critically ill patients, limited operating angle of the robotic arm, use of only one ultrasound probe) and requires further improvements as well as multicenter trials to establish its feasibility as a valuable tool for remote lung pathology detection.33
The third article of two cases discusses the advantages of using US versus chest CT for detection of lung abnormalities due to COVID-19, stating that limitations of CT are: a) difficult to perform on patients in critical condition who cannot be moved. b) CT is not available everywhere, and c) the enclosed environment of CT may contribute to the spread of the coronavirus. On the other hand, ultrasound has the advantages of repeatability, absence of radiation, and ease of use. Compared with ordinary ultrasound, 5G remote robotic ultrasound has the added advantages of protecting operators, alleviating the pressure of medical equipment shortages, and considerable portability. The authors conclude that 5G remote robotic ultrasound may become a suitable choice for diagnosis and monitoring patients with COVID-19 infection.32
Ophthalmology
An excellent review summarizes the digital technologies applied across different countries which are expected to increase the clinical workflow of ophthalmologists.5 It is exactly because the data-rich image requirements needed in Ophthalmology that 5G, IoT and AI are introduced for OCT and fundus cameras and algorithms which are changing ophthalmological service delivery. These technologies are expected to enhance the quality and continuity of eye care to all patients.
Recently, a 5G connected smartphone attached to a portable slit lamp provided a live streaming in real time of high enough quality to be used clinically, thus opening up even more potential for telemedicine and teleophthalmology in the future.34
The implementation of these technologies remains challenging, including the validation, patient acceptance, and education and the training of ophthalmologists on these technologies. It is imperative that they must collaborate with technology experts and data scientists to achieve universal quality and sustainable ophthalmic services and continue to adapt to the changing models of healthcare delivery.5
Interventional Cardiology
Robotic telestenting, in which percutaneous coronary intervention (PCI) is performed on a remotely located patient, availability of 5G could improve patient access to PCI, but has not been attempted over long distances likely required to reach many underserved regions.
In a recent study cited in Table 1, telestenting performance was compared in regional (206 miles) and transcontinental (3,085 miles) distances from the interventional cardiologist. Ex vivo models of telestenting were used, and robotic PCI on endovascular simulators was attempted over both wired and 5G wireless networks and audio and video communications between the cardiologist and the simulation laboratory personnel were established over the network. A total of 20 consecutive target lesions in the regional model and of 16 consecutive target lesions in the transcontinental model were successfully performed. Outcome measures included procedural success, procedural time, and perceived latency. Procedural success was achieved in all lesions in both models. Latency was imperceptible in all cases in both models and the greater distance of the transcontinental model had not significantly different procedural times compared to the regional model for cases performed over wired or 5G-wireless networks.35 This is the first study which demonstrates that remote robotic manipulation of coronary devices is now possible using wireless network connectivity.
Emergency Medicine
The emergency department (ED) is a good example for the widespread introduction of virtual triage via telemedicine, rather than coming directly to the ED in person. The patients benefit as they are not obliged to attend in person and can be treated with remotely delivered prescriptions. If they do need to attend, an appointment time can be scheduled more efficiently, being seen directly by the specialists rather than spending long hours in the ED waiting room. Additionally, with the maturation of chatbots, much of the patients counselling can be performed flawlessly through video consultation. Additionally, the healthcare providers benefit from the absence of physical attendance, the costs associated with additional time and space utilization, as well as the use of personal protective equipment. The healthcare personnel who can work from home can contribute to the efficient use of human resources at a time where sustainability must also be considered. Reduced in person ED visits also decrease the general workforce risk of COVID- 19, avoiding the highly undesirable scenario of transmission between clinicians and patients.36 The safety and efficiency of remote triaging and automated counselling need to be evaluated, and until then, clinicians need to oversee each consultation as is standard process prior to the pandemic.
Obstetrics
So far, in an attempt to make accurate diagnoses in emergencies, smartphones are used to take videos transmitted in real time to consultants located at a central hospital who then can assess the situation.37 One such emergency is to estimate in real time the status of a fetus in utero through a cardiotocogram (CTG). However, it is used in medical care clinics only, and there are few reports attempting to send CTG data via a mobile network from home or from an ambulance to a medical institution. Several problems could occur and only one successful case has been published so far.38 With the deployment of 5G this solution could be implemented as described in a recent publication, where the authors simulated the feasibility to concomitantly transmit not only CTG but also real time fetus US videos as well with excellent results. Thus, except CTG, the images during ultrasound examinations were high-quality videos on patient actors, which were transmitted without problems.38 Thus, home monitoring of a fetus with the 5G system is a particularly useful application, which could create a new future for obstetric care.
Surgery
While the practice of a surgeon is very much like the practice of general medical practitioner, the distinguishing feature is the amount of time committed to performing surgical procedures upon their patients. Surgeons do have the same clinical, educational, research and administrative requirements as all physicians, including the basics of history, physical, lab/imaging studies, outpatient and in-hospital care, discharge and follow-up. Likewise, in response to the COVID-19 pandemic, this includes the increased use of teleconsultation, teleconferences, etc., which is anticipated to be continued upon resolution of the pandemic. However, like all healthcare specialties, there are additional unique requirements and opportunities, which is the focus of the following surgical areas:
Pre-operative preparation
Intraoperative procedure, and
Postoperative follow-up (both in hospital and outpatient care).
1. Pre-operative Preparation
The surgeon meets the patient in the pre-anesthesia area and needs access to all the medical information from the medical record for review – which includes both medical data and medical images. If it is a complex procedure, many surgeons will not only have review of a full 3-D reconstruction of imaging studies (computed tomography [CT], magnetic resonance imaging [MRI], etc.), but may have also actually previously rehearsed the procedure using simulation, all of which requires real-time access to massive amounts of imaging data.
2. Intraoperative Procedure
More and more operations are being performed by minimally invasive surgery (MIS). Often, the video image is being captured, with the potential for sharing real-time with other surgeons or archiving. When used for educational purposes, high - bandwidth is needed for the transmission of the video image, along with audio for the surgeon to communicate with the learners in the ‘audience’. The archived video of the procedure can be used for many educational and administrative or legal purposes, including credentialling, privileging, or remediation. In addition, during surgery, the surgeon often will need to take a biopsy which is sent to a pathologist to be examined and reported back to the surgeon waiting for the results to complete the operation. New instruments now are able to capture the image of the pathology in real time and transmit the image directly to the pathologist for diagnosis, saving significant operative time. Telepathology can be in the same hospital, or literally anywhere around the world for consultation in difficult diagnostic cases. Another technology, data fusion, permits overlaying the live video image with additional images (CT, MRI, fluorescence markers, etc.) to guide surgeons with ‘X-ray vision’ to see structures and pathology within organs or lymph nodes (for cancer).
3. Postoperative Care (Including Outpatients)
The immediate postoperative care of a surgical patient has previously been done within an in-hospital stay, however the newer MIS procedures have allowed many patients with simple, uncomplicated surgical procedures to go home the same day. Teleconsultation to the patient’s home, especially during the COVID-19 pandemic, has exponentially increased. Not only is there the opportunity to speak to the patient by using a cell phone, but it is now possible to actually see the patient and use the phone (or any one of the many new ‘in-home’ medical devices to examine the site of the surgery, saving patients the need to come to the hospital for follow up. This capability for a visual examination is also in very high demand for many chronic nonsurgical diseases, especially for wound care and dressing changes.
Trauma and accident injury is a special needs surgical application because minutes to surgical care can be critical. Innovation in instruments, devices, procedures, and training, including the Advanced Trauma and Life Support (ATLS), has dramatically increased the lives saved. The new capabilities of communicating with an ATLS trained responder, especially in a telemedicine-enabled ambulance, can bring a sophisticated trauma surgeon’s consultation directly to a first responder anywhere. Because of the military’s need for (and research in) battlefield trauma care, it is anticipated that a significant increase in remote, telemedical care (including the possibility of remote telesurgical care) will be enabled by the scope of 5G communications.
Clinical Telesurgery
Telesurgery (or remote surgery) aims to break the obstacle of geographical boundaries in providing high quality healthcare in the most complex medical interventions and surgeries. High-qualified medical expertise will be transferred from the major hospitals to the decentralized ones with the use of remote-surgery, remote diagnostics and telemedicine resulting in significant cost reduction, and improved efficiency in health care services. Telesurgery, where parts of the procedure are controlled by a surgeon from a central site to a remote location, is the most demanding application among the remote healthcare services and thus by successfully validating this application, the validation of technology for the entire range of less demanding remote healthcare applications can be implied.39
The domain of applications of remote surgery, apart from decentralizing health care, are remote surgical operations under extreme conditions, such as at the battlefield and remote operations in extreme environments like in space missions. Telesurgery entails the use of a master-slave robotic surgical system. Currently, the only Robot-assisted Minimally Invasive Surgery (RAMIS) system with FDA approval is the da Vinci surgical system, which has offered to surgeons’ a greater visualization, enhanced dexterity, greater precision and greater comfort; to the patients it has offered shorter hospitalization times, reduced pain and discomfort and faster recovery time.
As can be seen from Table 1 there are very few clinical reports using 5G for telesurgery. For example Remote RAMIS (telesurgery) has already had investigational testing in various scenarios and conditions.40,41 The first true telesurgery on a patient was performed in 2001 between New York, USA and Strasbourg, France (∼6200 km apart); the so-called “Lindbergh Operation”.42 The authors used a dedicated trans-Atlantic fiber-optic cable. The average round-trip delay was 155 ms including delays in image transmission, which made delay of movements executed by the surgeon in NY, apparent but easily managed within the 155 ms. Telesurgery has since been performed by other researchers. Anvari and colleagues43 have reported the largest patient series with more than 30 remote operations between the central site located in Hamilton, Canada and the remote site in North Bay, Canada (∼400Km apart), over a virtual private network (VPN) on a nondedicated fiber-optic line. Reported average latency was 140 ms which was noticeable by the surgeon, who automatically compensated for the delay. It has been suggested that the ideal latency time for telesurgery should be less than 100 ms and that problems such as inaccurate manipulation could appear if the latency time is longer than 300 ms.44 All aforementioned research outcomes do not include haptic feedback, which severely increases latency. It has yet to be tested whether future telesurgery systems will be able to integrate haptic feedback that is accurate and precise enough to increase the surgeon’s performance without increasing latency.
In order to implement remote surgery, we should address the critical technical challenges of robotic telesurgery, which are the minimization of latency between master-slave and the maximization of reliability, availability and security of the communication channel. The desired specifications are:
Latency (end-to-end round trips) of ≤ 100ms depending on the application.
Ultrareliable communications (“seven nines”).
The term ultrareliable can be quantified in terms of fixed-line carrier-grade reliability of seven nines i.e., an outage probability of 10−7, which translates to microseconds of outage per day. These specifications cannot be provided today by existing 3G and 4G networks.
The hypothesis is that 5G infrastructure offers the desired reliability and latency and therefore is an enabler for safety-critical applications such that remote surgery, from a central major surgical hospital medical center can be matched to a specific patient’s medical needs in a remote hospital location. In the more distant future, when haptic technologies develop to a safe level of precision and accuracy, these technologies can be applied to RAMIS telesurgery systems. It should be noted that the same infrastructure of haptics for telesurgery could be applied to other remote healthcare applications such as telediagnostic tools, which could be available anywhere, anytime, allowing remote physical examination which could include palpation.45
As with all newly implemented emerging technologies like telesurgery, facilitation by the 5G network is a game changer. Highly delicate procedures like spinal surgery could benefit from high capacity, low latency. This also applies to other surgeries in other specialties like cardiac surgery, urology, and colorectal surgery. In short, the entire domain of surgical procedures could be enhanced with 5G enabled telesurgery.
Before 5G, only a few telesurgeries were reported which were carried out through a 4G network while mostly internet and satellite networks were previously used for telesurgery.46 Thus, Wirz et al.. performed robotic telesurgery to complete a pituitary tumor resection on a simulated model over the Internet with a bandwidth of 1 Gb/s in 2015.47 Regarding surgical applications our review revealed two preclinical studies: One article reporting 5G mediated nephrectomies in 4 swine, estimating the latency time due to long (300 Km) distance,48 and another one operating in 5 pigs in a shorter distance (1–6 Km) 40 Rayman et al. performed robotic telesurgery to perform a left internal mammary artery dissection in pigs through a satellite network with a maximum bandwidth of 10 Mb/s.49
Regarding remote telesurgeries, in USA, a surgeon from Texas, 1200 miles away from a Florida Hospital, remotely manipulated the da Vinci robot, performing operations on simulated patients through the Internet. In China, Hainan Hospital of Chinese PLA General Hospital and Beijing Jishuitan Hospital performed remote positioning for brain pacemaker implantation surgery and screw fixation surgery, respectively, through a 5G network. However, these surgeries do not require high demands on network latency and bandwidth of the 5G network as compared to the continuous manipulation and 3D video transmission in laparoscopic surgery.48,50
While the future for telesurgery looks bright, there are a number of challenges that need to be addressed. The following are suggestions for research studies:
Both the surgeon console and the patient side cart need to be more compact or portable. Ultimately, the surgeon console could be as portable as a laptop computer and the patient side cart should be compact so that it can be placed in an ambulance or a mobile ward (En-route ‘damage-control’ surgery).
Surgical robots need to be combined with AI, capable to alert of dangerous actions during the operation (error prediction and hazard avoidance).
Protocols and responsibilities need to be clearly defined to define whether causation of errors is from device (robotic and/or telecommunication system) or surgeon control.
Communication corporations need to take measures to assign and guarantee enough bandwidth and high priority for telesurgery.
With network security is still one of the major challenges to telesurgery, a security guard system for the 5G network has to be designed and implemented (anti-hacking).
Telerobotic Spinal Surgery
It is well known that robot-assisted spinal surgery has been a popular and reliable surgical procedure. Furthermore, a recent meta-analysis showed that the accuracy of robot-assisted pedicle screw placement was significantly higher than the freehand method.51
A recent study (Table 1) in which 6 hospitals participated from 6 different cities in China, 5G telerobotic spinal surgeries for 12 patients were performed and a total of 62 pedicle screws were successfully implanted using the 5G telerobotic surgery system.52 The operation time was 142.5 ± 46.7 minutes, and the mean guide wire insertion time was 41.3 ± 9.8 minutes without any intraoperative adverse events. They concluded that telerobotic spinal surgery based on the 5G network is accurate, safe, and reliable. The application of the 5G network in the clinical area has great potential and value in the future.
The authors also explored the new pattern of “one-to-many” remote surgery. Under this mode of remote surgery, one expert surgeon can simultaneously provide surgical care to more than one remotely located hospitals, something which previously was significantly restricted by the limit of network bandwidth. A “one-to-three” telerobotic surgery was successfully performed during this study, and it is believed that even more multicenter remote surgery is simultaneously possible, due to the vast potential of the 5G network.52
5. Medical Education and Healthcare Research
Attention must be paid to the unique needs of both medical education and biomedical research, especially in this era of ‘evidence-based medicine’. Obviously, the equivalents are evidence-based education (a complete paradigm shift for education) and evidence-based research (an opportunity to improve speed and quality of research).
5.1. Medical Education
In the surgical specialties, technical training has changed from subjective mentored ‘see one, do one, teach one’ in the operating room, to objective assessment of performance with proficiency-based progression (PBP) training53 in the simulation center. Assessment is enhanced by AI software, analysis of performance through computational analytics on the massive data acquired in the simulators and use for immediate, formative feedback. During the beginning weeks of the COVID-19 pandemic in Wuhan, China, there were over 800,000 accesses to the COVID-19 training database. After the pandemic, it is postulated that there will be increased emphasis on a new ‘hybrid model’ of medical education, with many of the advantages of just in time and remote learning enriching traditional educational models.
5.2. Healthcare Research
The new 5G information ecosystem greatly increases the productivity on both basic science and clinical research. First, the technologies greatly facilitate collaborative, multi-institutional studies and secondly through the access to massive data (BD), repositories, AI and computational analytic software. The data is frequently being fed autonomously from the billions of devices, equipment and instruments connected to the IoT.
Basic science research, especially at the cellular, molecular, genetic and “-omics” levels, produce vast amounts of raw data which previously was too large to share among institutions and researchers, let alone be processed by AI, computational analytics, and super computers. For clinical researchers, acquiring enough patients for large enough clinical trials to prove validity can now be accomplished through collaboration in near real-time because of available bandwidth inherent in the 5G telecommunications.
6. 5G and the COVID-19 Pandemic
When the COVID –19 pandemic broke out in Wuhan, China, the city’s healthcare system was rapidly overwhelmed. A disaster response was quickly established, including the new 5-G telecommunications networking.54 In the first 29 hours, 3 ‘shelter’ (fangcang) hospitals of 4000 beds were created in empty stadiums and auditoriums, including a complete intra-net within the hospital and internet connecting hospitals globally, especially giving access to the internet of the existing 5-G high bandwidth wireless networks throughout all the city’s hospitals.52 The intranet connected all the computers, smart devices (for example, Real-time Remote Computed Tomography (CT) Scanning on 152 patients with COVID-19), in addition to critical information systems (X rays, laboratory tests, Electronic Medical Record, maintenance, administration and wireless mobile phone) services immediately, without the need to spend weeks running cables throughout the hospitals.54 Over the remainder of the week, an additional 13,000 beds were created using ‘cabin hospitals’, essentially standard ‘shipping containers’ that had previously been outfitted as individual departments of the hospital for beds and services. Simply connecting the various containers (cabins) together and instituting 5G networking, each department was assigned their own VPN using a software technique called “network slicing”.25 The result of the huge 5G bandwidth was creating an additional 17,000 beds, all immediately connected (essentially no latency) throughout the city for standard telecommunications, teleconsultation for medical experts throughout the country, telereferrals for critical patients (a total of 425 emergency teleconsultations), and other healthcare services. In addition, AI was implemented in intelligent diagnosis of medical imaging and temperature measurement technology based on computer vision and infrared technology; while AI together with BD were used for epidemic situational analysis; tagging, contact tracing and monitoring of personnel movement as well as of positive cases; just-in-time logistics, inventory control, asset tracking and material allocation. In short, the availability of huge bandwidth significantly reduced the chaos of the disaster by providing real-time access and ‘visibility’ to all aspects of healthcare delivery.55 An abridged version of the Wuhan response is contained in Appendix 3.
7. Pitfalls of the Use of 5G in Healthcare
The technology of 5G communications bring great promise to significantly improve healthcare – from the technology standpoint. However, Medicine is as much an Art as it is a Science, and therefore what appears to be a very simple elegant technological opportunity, which healthcare providers really want and which will greatly benefit patients, there are often challenges from business, political, behavioral and other sources which can impede or thwart even the best of technologies.
Transforming an innovative idea to a commercial product is a long and arduous process, with about 10% of the ‘great new ideas’ being successful. During the 15–20 years (or longer) process there are numerous challenges and pitfalls. This is especially true in the high-risk, risk-averse conservative profession of healthcare, where resistance to change is uncompromising. Unfortunately, any innovation will usually be overhyped, and unable to meet expectations which is especially deleterious in the healthcare profession. Another critical pitfall along the way is, should the technology be completely successful, approval for reimbursement for using a device will be very difficult to establish, or will be established at an exorbitant cost.56 Other reasons for lack of success are that inability to raise enough funding to complete the prototype to a commercial product, a poor fit of the device for clinical application, inadequate return on investment (ROI) and many other financial considerations.5 Solutions to the technology transfer have been implemented at many academic and hospital institutions with establishment of “centers for Innovation” where dedicated Director, administrative staff, resources and funding, multidisciplinary teams with clinicians, engineers and other nonmedical fields work synergistically to complete the full life cycle develop of a new device or product.57
Future Directions
A reflection on the enormous number of advanced technologies rapidly occurring in this new ‘Information Age’ emboldens the authors to make certain ‘extrapolations of known advancements in science’ to suggest ‘forward-looking statements’ about likely technology outcomes for the future. However, It is apparent that some of the emerging technologies, such as, 5G communications, AI, telemedicine (and telesurgery), automatic image interpretations, genetics, proteomics58,59 and others are radically (and rapidly) changing the practice of medicine. Two areas need to be addressed: The core technologies in 5G communication, that are supporting most every industry and the healthcare specific technologies for medical needs.
The assumption is that the 5G and subsequent generations of wireless communication technologies will provide service now and in the future with exponentially increasing bandwidth (for data/information flow), decreasing latency (for real-time, near-real-time or just-in-time requirements) and with reliability/availability (the “seven nines” 99.99999% reliability), usability (simple human/machine interface), accuracy (received/delivered to the correct person/location), and especially security/privacy. The second assumption is that while the transmitting and receiving of information must obey physical laws, the interfaces (devices) for humans must obey both physical laws and biologic limitations [Note: machine-to-machine interfaces only obey physical laws].
Finally, attention must also be paid to the type of ‘supporting technology’ requirements, such as AI to enhance human intellectual performance in solving problems, supercomputers and BD repositories, sensors/actuators and MEMS on the IoT for data acquisition, etc., which are driving the need for better communication networks.
Surgery is in its fourth generation (Open surgery, endoluminal surgery, laparoscopic surgery, and now robotic surgery) with the emerging fifth generation of surgery being directed energy. The trend is for less invasive procedures (endoluminal) through natural body openings (mouth, nose, rectum, ears, etc.) to perform surgical procedures. This has been followed by and today the newest generation is robotic assisted minimally invasive surgery (RAMIS). Postoperative follow-up visits are being performed with teleconsultation. Until now, only a few “remote surgeries” (telesurgeries) have been performed because of the connecting cable between the surgeon console and robot arms. It is anticipated that the wireless 5G networks, with huge bandwidth and low latency, will lead to more implementation of telesurgery.
CONCLUSIONS
The newly emerging advanced healthcare ecosystem which is being totally integrated through the high bandwidth of 5G communications is truly disruptive. In spite of the limited deployment of 5G at this time, new clinical application examples clearly illustrate the opportunities across all healthcare specialties, including the administrative and nonclinical applications solutions for cost savings and improved efficiency. The larger the bandwidth and the lower the latency, the greater the number and size of the enabling technologies; in turn, this increases the demand for more telecommunication capabilities, thus creating an ever escalating upward spiral of growth.
This ecosystem of innovations has also created a milieu ripe for telemedicine to thrive and expand, as evidenced by the response to the COVID-19 pandemic, which has hastened the rapid increase of telemedicine and awareness of the importance of these digital technologies. Evidence from the pandemic has revealed the utility of telemedicine. Physicians must continue to adapt to the ever-changing models of care delivery and collaborate with broader teams involving technology experts and data scientists to achieve universal quality and sustainable healthcare services.
Two of the great innovations of 5G are software designed networks (SDN) and bandwidth “slicing”, especially for in-hospital networking. However, some of the technology limitations and challenges to be faced include mismatch between new communication capabilities with human limitations (solution: attention to human interface technologies), and the nontechnical limitations of behavior, politics, equity, cost, access and availability. Finally, two common technologies which are not ready (without revolutionary discoveries) are haptics and virtual reality, both of which are truly still in their infancy.
The good news is that this is still just the beginning of a great new revolution in digital healthcare with unlimited opportunities for growth.
APPENDIX 1. Other Critical Supporting Infrastructures
Although the 5G communications infrastructure is a major driver for healthcare innovation, it is the interaction among multiple other technologies that empower each other, well beyond the single contribution of each technology. It is the IoT - devices that are mobile, or location based, consisting of microchips of sensors, actuators, transmitters and/or receivers, other MEMS and (soon) nanotechnologies that provide the input or output at either end of the communication network.
Recall the beginning of modern remote communication systems (radio, telegraph, and telephone systems), that it was only when there was ubiquity of the transmitting and receiving devices that the telecommunication infrastructure flourished. So too, with 5G (and the follow-on generations of communication systems) that only with addition of IoT for the input/output, AI to make processes ‘smart’ and ‘autonomous’ (or semiautonomous), and BD repositories (the Cloud) with supercomputing (eventually quantum computing) running sophisticated algorithms with computational analytics, that created the need to innovate even more to keep up with the ever-increasing demand for more capable communication infrastructure.
It is the interdependence of this escalating upward spiral of innovation that continues to stimulate and challenge communication networks, and hence the need to interact with other technologies to sustain growth. But do not forget the interface between the human and the technology that provides the final connection of the communication system with a person, be it any of the forms of VR, wearable contact lens displays, or the ultimate brain-machine interface. After all, it is a ‘system-of-systems’, with each link in the chain dependent upon the success of all others, that decisively results in success. Below is a sampling of many (but not all) of such systems.
THE INTERNET OF THINGS
The internet of things (IoT) is composed of an estimated of number of 14.2 billion connected devices (of which 5.2 billion are unique cell phone users), with more than 21 billion connected devices by 2025, compared to the 8.2 billion global population as of Jan 2021.3 In addition, there an unknown number of machine-to-machine connections, many of which are used for autonomous machine/device maintenance. There are more devices and machines talking to each other than people communicating, machines that are sharing information and automatically adjusting themselves. Although many machines used by humans are used for human-to-human communication over the internet (e.g., computers, cell phones), the machines/devices with their sensors, and receivers/actuators, and data storage, are going about their ‘businesses” without human intervention. There is certainly oversight of these machine activities, however the overwhelming mass of data (BD) is beyond human comprehension and sophisticated software of computational analytics is needed to for humans to have all that data to be converted into information relative to a person’s needs. As people begin using more and more wearable or embedded microdevices for health monitoring, there will be a logarithmic increase in generated data which will eventually connect every aspect of an individual’s life. In addition, possessions such as automobiles, appliances (stove, refrigerator, etc.) and other aspects of the ‘smart home’ that are currently attaching to the IoT will be seamlessly integrated into IoT. The new 5G network can accommodate this initial increase data flow, with the expectation that 6 generation (6G) and later networks will also exponentially increase communication to accommodates needs. For example, the IoT is estimated to increase to about 500 billion new “things” by 2030 (about 60 times greater than the global population), which is about the same time that 6G network is expected to be commercialized.61
The integration of human and machine generated data will radically change healthcare services. In order to accommodate these healthcare needs, an entire communication infrastructure integrating the IoT, BD repositories, AI, supercomputing, innovative computational algorithms, edge computing (microsensors which include processing at point of data acquisition data, etc.) will be needed to form a ‘telecommunication ecosystem’, which not only be able to archive, monitor and optimize current activities, but also be used longitudinally to estimate future trends in personalized medicine, as well as overall healthcare services. The opportunities in telemedicine and telesurgery are reviewed in their sections. Additionally, the 5G networking will allow for reduced latency, and less dependence on network bandwidth and availability, and potentially enhanced security.5
At the moment there are research projects62 investigating such potential systems. In the distant future, there is the possibility that the bathroom will also become extensively populated with all types of sensors for automatic daily monitoring health status, providing a complete physical examination every day to update health status on a daily basis, while the person is simply performing the normal daily bathroom activities.
ARTIFICIAL INTELLIGENCE, MACHINE LEARNING, AND DEEP LEARNING
As a practical definition for this manuscript, AI is: “technology which mimics human behavior”.63 Two areas (subfields) of AI have drawn attention in healthcare:
Machine Learning: Algorithms which can automatically learn rather than be programmed, and is the principle source for predictive analytics, especially for clinical practice and speech translation;64
Deep Learning: The discovery of underlying ‘features’ and ‘meaning’ (such as cause and effect) in data from multiple processing layers using neural networks, mimicking the process used by the human brain.65
In healthcare, DL is the best infrastructure for speech recognition66 as well as in image recognition i.e. automatic presumptive diagnoses of known diseases from various imaging technologies, such as X-Rays, CT, MRI, OCT, etc.67,68 At this time, AI has not reached a point of being able to independently perform diagnose and manage patients without human input. Currently, human review of all AI image interpretations requires clinician review, which provides a clear difference between autonomous and assistive AI.
BIG DATA, QUANTUM COMPUTING, AND COMPUTATIONAL ANALYTICS
The original process for the internet was: INPUT (Raw data typed in from a computer); TRANSMIT (communication over dedicated land lines via local area network (LAN)/distant wide area network (WAN); OUTPUT to a receiving computer (for storage and processing). The present status is MULTIPLE TYPES of INPUTS of data acquisition (see IoT), TRANSMIT (massive data over lines and wireless communication) for MULTIPLE TYPES of OUTPUT (massive “Big Data, to storage, streaming, computing with sophisticated algorithms for AI, etc.). The result of the Input and Output sides is an explosion of data that requires very wide bandwidth with decreased latency, accuracy, reliability, privacy and security.
VIRTUAL REALITY (VR), AUGMENTED REALITY (AR), MIXED REALITY AND EXTENDED REALITY (XR)
The original mobile phone-based AR/VR game applications (like Pokémon) were among the first types of practical apps on 4G. Now 5G networks, and in time 6G, will be able to support fully immersive VR. Rather than a graphic overlay of a real image of AR, the entire display (mobile phone, computer, etc.,) are replaced by an entirely simulated computer-generated graphics which provides the sense of “presence” in an imaginary “world”. Through a variety of ‘interfaces” (input devices) users are able to interact within the simulated world in a somewhat natural way. In AR, a graphic image, which is then fused in real-time to the display, especially to provide useful healthcare information, such as blood pressure, oxygen levels, positions of tissues and organs during surgery, etc. As a generalization, full VR is implemented in simulation and training, whereas AR is most advantageous for clinical care. Important tasks, such as counselling patients and preoperative consent can likely be facilitated with AR, and nonclinical functions in hospitals such as navigation aids for visually impaired patients.9
These ‘realities’ still remain in their infancy and have only few applications in healthcare (principally in education and training, using online information or in training labs with simulations/simulators). [Note: There are currently over 100 certified ‘simulation centers’, in major hospitals and medical schools]. However, once their implementation of virtual worlds, simulations and applications become practical, reliable and of high visual quality, there will be significant demand for high bandwidth with minimal latency for remote learning and training.
APPENDIX 2: Fundamental Biologic Principles
One of the most overlooked issues in healthcare (and most other industries) is the capability of humans to adjust to a new technology – physically. While everyone is personally aware of ‘information overload’, there is scarce attention paid to the principal characteristics of the ‘biologic systems’ which humans use with technologies: Nervous and musculoskeletal system (brain/muscles), vision (eyes/imaging), hearing (ears/acoustics) and touch (hands/haptics); the senses of taste and smell play a relatively small/focused role, especially in interacting with technology.
The science of HIT is defined as “a means or place of interaction between two systems a means or place of interaction between two systems; especially, the interface between people (users) and computers or devices.21 In order to address important new technologies (such as rapidly expanding communication technologies), consideration to the capabilities and limitations of the ‘human’ systems’ is important in order to optimize the devices to enhance human capabilities. Table 2 gives an example of typical human capabilities in regard to human performance related to perception and adaptation to latency in communication systems (earlier unpublished data by the author [RMS] but consistent with the average robotic knot tying in ‘box trainer under varying amounts of latency) and within the same range as the data stated by Anvari 69 under conditions of real time patient surgery. Recent long distance telesurgery case reports using 5G have stated latency much less than 200 milliseconds (ms), indicating that safe telesurgery is likely to increase with the use of 5G networking; however, larger validation studies are required. Another different example of human capability limitation is, although most persons claim to multitask at many different cognitive tasks simultaneously,70 the literature indicates that the frontal lobe (the attention center) can only perform 3–4 tasks at once.71 The explanation of the difference is that some authors considered automated functions which are controlled by the cerebellum and system of reflexes (such as when riding a bicycle, a person does not focus their attention on each leg and pedal when riding) or situational awareness, as part of multitasking. In addition, performing more than 2 cognitive tasks simultaneously results in increase error and decrease efficiency. Thus, when a person multitasks, there will be a HIT mismatch of massive data input overwhelming focused cognitive ability of the brain to process it, thereby decreasing performance and safety.
For the vision systems, will more new devices be developed using nanochip technologies, such as the ‘smart contact lens’,72 that can receive massive data to extend human vision beyond the visible spectrum; and if so, what will be consequences of such capabilities?
Or perhaps the reverse is an important issue for the sense of touch: on a fingertip there are 23 different sensors, at a density of 1000 nerve endings per cubic millimeter, in an average hand surface area of 4000 mm, each sending stimuluses at 1000 hertz/second. Even with 5G or 6G (see Table 3), will there be enough bandwidth to transmit in real time that massive amount of data per second (in addition to all the other massive data flow from all the other systems in the milieu for surgery) and their interface to the input device (hand controller) for a robotic surgeon to precisely perform a complex surgical procedure?
Such examples beg the issue of defining accurate human performance measures to enable new technologies to accurately be designed and developed that match human needs. Such mismatches can result in too much data overload, or insufficient sensory input which results in loss of accuracy and precision and errors. The biologic complexity of human performance is well beyond the complexity of man-made systems, and therefore the regulation of data flow, even as large as the 5G systems, needs to be modulated to match the capabilities of the human. Therefore, HIT is an area of research that requires much more attention in order to optimize both the mechanical devices and the communication system.
APPENDIX 3. Use of 5G IN Wuhan China during COVID 19
As the restriction lockdown emerged globally due to Covid-19 pandemic, a sudden strain occurred on existing cellular networks: Healthcare, education, work, and most other human interactions were suddenly pushed onto the virtual arena. It has therefore been shown that telemedicine is not reserved only for the remote and underserved, but it can routinely serve the wider population as it has been shown to be safe, efficient, and inclusive, provided that measures to ensure security, robustness and capacity, particularly in densely populated regions with massive competing demands for bandwidth.54
While the COVID-19 disease, initially discovered in Wuhan, China in Dec 2019 is well known, what is of specific interest is that the pandemic is one of the earliest examples of emergency use of 5G technology for many of the important applications for healthcare, not only as a communication tool, but also as a fundamental infrastructure to provide the necessary systems integration among the multiple informatics technologies.
Telemedicine had been available for decades, however only used in a small number of specific medical applications, in part due to limited capabilities of the communication networks – everything changed with the Covid-19 pandemic. Lockdowns were initially instituted within China with such a resounding success in Wuhan, that as the pandemic spread globally, lockdown followed. Without 5G, the existing 4G networks were insufficient because businesses, education, research, healthcare and personal (especially family) communications all battled for a share of the limited bandwidth.5
The criticality of using multiple information-based technologies is documented by Ye, Zhou and Wu 60 in their report of the informatics technologies used and the experience gathered in responding to the COVID-19 epidemic in China through the perspective of health informatics. Due to the pandemic, the so called “5G+ Health” has moved from the experimental to the clinical phase. A plethora of technologies, including cloud computing, BD, the IoT, mobile internet, AI, and 5G mobile network, were used for epidemic prevention and control in China. Taking full advantage of mobile internet and 5G technologies active internet health care services provided by clinical experts from all over the country has been realized, both within the hospital as well to many essential supporting services outside of the hospital. More specific examples include the fact that citizens were able to access real-time epidemic situation dynamics and prevention knowledge through the mobile internet. BD were used for epidemic situational analysis; tagging, contact tracing and monitoring of personnel movement as well as of positive cases; just-in-time logistics, inventory control and material allocation. AI has been implemented in intelligent diagnosis of medical imaging and temperature measurement technology based on computer vision and infrared technology. By increasing bandwidth and reducing latency, telemedicine based on 5G technology has also played an important role in the consultations and treatment of patients with severe COVID-19 and in facilitating international cooperation.
The above-mentioned clinical information systems deployed have the following 3 advantages as described by Chen S. et al. 36 in the description of the physical and functional attributes of an entire emergency hospital network:
“A rapid deployment: The first three shelter-hospitals (called fangcang hospitals) in Wuhan with 4000 beds were built in 29 hours and their clinical information systems were deployed within this time framework.
An online information exchange among medical institutions in the external network (especially each fangcang hospital’s connection to their ‘host’ hospital)
A rapid response of electronic health records (EHRs) to specifically respond to COVID-19.
It is interesting to note that not only were the fangcang shelter-hospitals established within existing available large structures (e.g., stadiums, auditoriums, warehouses) within record time, but within the same time frame, an entire 5G wireless network was established throughout an entire fangcang shelter via software designed networks (SDN) with ubiquitous distribution and access through ‘network slicing’ of the massive 5G bandwidth, but was also linked to the nearest ‘host’ hospital for global access. Therefore, it is possible to use information technology over 5-G networking to increase the near instantaneous acquisition, communication and distribution of information for clinical purposes, but also as important, to provide transparency of information about an epidemic to reduce public panic and enhance public confidence.
Experience from a multimodal telemedicine network in Sichuan Province in Western China 55 using a newly established 5G service, a smartphone app, and an existing telemedicine system during the COVID-19 pandemic. Three applications were developed:
Physicians Tele-Education about COVID-19: More than 800,000 person-accesses have been implemented on prevention and control of the disease.
A 5G Dual Gigabit Network and a Multidisciplinary Medical Team: 424 remote consultations were conducted through a new real-time video telemedicine system for consultations focused on severe and critical COVID-19 patients.
A 5G Dual Gigabit Network and Real-time Remote CT Scanning on 152 patients with COVID-19 under the control and guidance of the host centrally located hospital. This commemorates the transition of telemedicine from the traditional consultation mode to a practical operation mode, ensuring high-quality CT even in areas with severe shortages of qualified personnel.
The authors comment that although telemedicine clearly has a wide range of potential benefits, it also has some disadvantages like the occurring breakdown in the human relationship among health professionals and their patients; and some issues concerning the quality of health information; and organizational and bureaucratic difficulties. However, the 5G technology and improvement in the management experience of telemedicine by policymakers, the abovementioned limitations can be minimized, and telemedicine may become a sustainable, mainstream solution for both public health emergencies and routine medicine.
In this case report,55 the experience of accomplishing the IT infrastructure of 20 cabin hospitals in in Wuhan, China, to receive patients with mild symptoms within 48 hours is described. The cabin hospitals were largely engaged in blood and PCR testing, mobile CT scanning, and oral medicines administration. In order to complete the IT system construction within 24 to 48 hours, it was necessary to interconnect the cabin hospital within an existing hospital’s information network. A 5G all-wireless solution to divide the overall network system of the cabin hospital into multiple network units (i.e. the electronic medical records, a picture archiving and communication system, the laboratory information, the maintenance system, and other management information systems) was implemented and each unit was independently connected to the host hospital’s data center over a VPN capable to accept authenticated connections built on the 5G wireless network. The network bandwidth was about 10 times faster than 4G, and that the intranet bandwidth exceeded 50 MB, thus successfully conforming to the prerequisites demand of the network. Thus, all data, plus the Internet-assisted medical system of the host hospital, were integrated and built a lightweight wireless information system for the cabin hospital.
The outcomes of this approach were: a rapid system construction (within 48 hours for the system functional integration with the host hospital), zero maintenance of network and terminal devices (as remote maintenance software was installed on each computer), reduced chance of cross infection (as the whole information circulation was all electronic and paper was rarely used) and this implementation allowed minimum physical interaction of the healthcare personnel with the patients.
This networking mode is suitable for any emergency scenarios where an intranet connection to the host organization is necessary to set up within a short time. There is a bright future of 5G wireless network to dwarf the conventional wired network. Additionally, the proposed solution can be used for the multihospital network interconnection and rapid network recovery during the failure of wired network.
Footnotes
Disclosure: none.
Funding sources: none.
Conflict of interests: none.
Contributor Information
Konstantinos E. Georgiou, 1st Department of Propaedeutic Surgery, Hippokration General Hospital of Athens, Athens Medical School, National and Kapodistrian University of Athens, Athens, Greece..
Evangelos Georgiou, Medical Physics Laboratory Simulation Center (MPLSC), Athens Medical School, National and Kapodistrian University of Athens, Athens, Greece..
Richard M. Satava, Professor Emeritus of Surgery, University of Washington, Seattle, WA..
References:
- 1.Ting DSW, Lin H, Ruamviboonsuk P, Wong TY, Sim DA. Artificial intelligence, the internet of things, and virtual clinics: ophthalmology at the digital translation forefront. The Lancet Digital Health. 2020;2(1):e8–e9. [DOI] [PubMed] [Google Scholar]
- 2.Nordrum A, Clark K. 5G bytes: small cells explained. Published August 19, 2017Accessed February 20, 2020. https://spectrum.ieee.org/video/telecom/ wireless/5g-bytes-small-cells-explained. [Google Scholar]
- 3.Simkó M. 5G Wireless communication and health effects—a pragmatic review based on available studies regarding 6 to 100 GHz. IJERPH. 2019;16(18):3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agiwal M, Roy A, Saxena N. Next generation 5G wireless networks: a comprehensive survey. IEEE Commun Surv Tutorials. 2016;18(3):1617–1655. [Google Scholar]
- 5.Li J-PO, Liu H, Ting DSJ, et al. Digital technology, tele-medicine and artificial intelligence in ophthalmology: a global perspective. Progress in Retinal and Eye Research. September 2020;82:100900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. [DOI] [PubMed] [Google Scholar]
- 7.Wickham L, Hay G, Hamilton R, et al. The impact of COVID policies on acute ophthalmology services—experiences from Moorfields Eye Hospital NHS Foundation Trust. Eye (Lond). 2020;34(7):1189–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourdon H, Jaillant R, Ballino A, et al. Teleconsultation in primary ophthalmic emergencies during the COVID-19 lockdown in Paris: experience with 500 patients in March and April 2020. J Fr Ophtalmol. 2020;43(7):577–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. jul211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535 jul211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sauter M. Long rerm evolution (LTE) und LTE-advanced. In: Grundkurs Mobile Kommunikationssysteme. Springer; Fachmedien Wiesbaden: 2018:205–294. [Google Scholar]
- 12.Andrews JG, Buzzi S, Choi W, et al. What will 5G be? IEEE J Select Areas Commun. 2014;32(6):1065–1082. [Google Scholar]
- 13.Wu Q, Li GY, Chen W, Ng DWK, Schober R. An overview of sustainable green 5G networks. IEEE Wireless Commun. 2017;24(4):72–80. [Google Scholar]
- 14.Chen S, Hu J, Shi Y, et al. Vehicle-to-everything (v2x) services supported by LTE-based systems and 5G. IEEE Comm Stand Mag. 2017;1(2):70–76. [Google Scholar]
- 15.Simsek M, Aijaz A, Dohler M, Sachs J, Fettweis G. 5G-enabled tactile internet. IEEE J Select Areas Commun. 2016;34(3):460–473. [Google Scholar]
- 16.Zhang Q, Liu J, Zhao G. Towards 5G enabled tactile robotic telesurgery. arXiv:180303586 [cs]. 2021. Published online March 9, 2018. Accessed January 26 http://arxiv.org/abs/1803.03586. [Google Scholar]
- 17.Noohani MZ, Magsi KU. A Review of 5G Technology: Architecture, Security and Wide Applications. 2020. Published online May 21. [Google Scholar]
- 18.Labiris G, Fanariotis M, Christoulakis C, et al. Tele-ophthalmology and conventional ophthalmology using a mobile medical unit in remote Greece. J Telemed Telecare. 2003;9(5):296–299. [DOI] [PubMed] [Google Scholar]
- 19.Ethan S. Why “Exponential Growth” Is So Scary For The COVID-19 Coronavirus. Forbes. Published March 17, 2020. Accessed January 29, 2021. https://www.forbes.com/sites/startswithabang/2020/03/17/why-exponential-growth-is-so-scary-for-the-covid-19-coronavirus/?sh=4a971dbe4e9b.
- 20.Berlinger J. WHO warns governments “this is not a drill” as coronavirus infections near 100,000 worldwide. CNN. Published March 6, 2020. Accessed January 292021https://edition.cnn.com/2020/03/06/asia/coronavirus-covid-19-update-who-intl-hnk/index.html.
- 21.Satava RM, Ellis SR. Human interface technology. Surg Endosc. 1994;8(7):817–820. [DOI] [PubMed] [Google Scholar]
- 22.Angelucci A, Kuller D, Aliverti A. A home telemedicine system for continuous respiratory monitoring. IEEE J Biomed Health Inform. Published Online. 2020:1–1. [DOI] [PubMed] [Google Scholar]
- 23.Abd Elaziz M,AA, Al-Qaness M, Abo Zaid EO, Lu S, Ali Ibrahim R,A, Ewees A. Automatic clustering method to segment COVID-19 CT images. PLoS One. 2021;16(1):e0244416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang W, Zhang X, Zhao J, Qiang Y, Tian Q, Tang X. A segmentation method for lung nodule image sequences based on superpixels and density-based spatial clustering of applications with noise. PLoS One. 2017;12(9):e0184290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiao L, Wu H, Wu Y, et al. A lightweight internet sharing scheme for sectional medical images according to existing hospital network facilities and basic information security rules. Journal of Healthcare Engineering. 2020;1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salerno A, Kuhn D, El Sibai R, Levine AR, McCurdy MT. Real-time remote tele-mentored echocardiography: a systematic review. Medicina. 2020;56(12):668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kiss N, Cantoresi F, Lampitelli S, et al. Emergency dermatology: three‐month experience from an Italian academic outpatient clinic during lockdown for COVID-19 pandemic. Dermatologic Therapy. 2020;33(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ning AY, Cabrera CI, D'Anza B. Telemedicine in otolaryngology: a systematic review of image quality, diagnostic concordance, and patient and provider satisfaction. Ann Otol Rhinol Laryngol. 2021;130(2):195–204. [DOI] [PubMed] [Google Scholar]
- 29.Feroz A, Mohammed Feroz T, Bastian T, Selvamani M. Telepathology: an update on applications, latest advances, and current status in Indian scenario. J Cancer Res Ther. 2020;16(4):703–707. [DOI] [PubMed] [Google Scholar]
- 30.Li Y, Zhu Z, Chen JJ, et al. Multimodal endoscopy for colorectal cancer detection by optical coherence tomography and near-infrared fluorescence imaging. Biomed Opt Express. 2019;10(5):2419–2429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu S, Wu D, Ye R, et al. Pilot study of robot-assisted teleultrasound based on 5G network: a new feasible strategy for early imaging assessment during COVID-19 pandemic. IEEE Trans Ultrason Ferroelectr Freq Control. 2020;67(11):2241–2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yu R-Z, Li Y-Q, Peng C-Z, Ye R-Z, He Q. Role of 5G-powered remote robotic ultrasound during the COVID-19 outbreak: insights from two cases. Eur Rev Med Pharmacol Sci. 2020;24(14):7796–7800. [DOI] [PubMed] [Google Scholar]
- 33.Ye R, Zhou X, Shao F, et al. Feasibility of a 5G-based robot-assisted remote ultrasound system for cardiopulmonary assessment of patients with coronavirus disease 2019. Chest. 2021;159(1):270–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giardini ME, Livingstone IAT. Extending the reach and task-shifting ophthalmology diagnostics through remote visualisation. In: Rea PM, ed. Biomedical Visualisation. Vol Advances in Experimental Medicine and Biology 1320. Springer International Publishing; 2020:161–174. [DOI] [PubMed] [Google Scholar]
- 35.Madder RD, VanOosterhout S, Parker J, et al. Robotic telestenting performance in transcontinental and regional pre‐clinical models. Catheter Cardiovasc Interv. 2021;97(3):E327– E332. [DOI] [PubMed] [Google Scholar]
- 36.Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. The Lancet. 2020;395(10232):1305–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yanagawa Y, Jitsuiki K, Nagasawa H, et al. A smartphone video transmission system for verification of transfusion. Air Med J. 2019;38(2):125–128. [DOI] [PubMed] [Google Scholar]
- 38.Naruse K, Yamashita T, Onishi Y, et al. High-quality transmission of cardiotocogram and fetal information using a 5G system: pilot Experiment. JMIR Med Inform. 2020;8(9):e19744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bethea BT, Okamura AM, Kitagawa M, et al. Application of haptic feedback to robotic surgery. J Laparoendosc Adv Surg Tech A. 2004;14(3):191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jell A, Vogel T, Ostler D, et al. 5th-generation mobile communication: data highway for surgery 4.0. Surg Technol Int. 2019;35:36–42. [PubMed] [Google Scholar]
- 41.Lacy AM, Bravo R, Otero, Piñeiro AM, et al. 5G‐assisted telementored surgery. Br J Surg. 2019;106(12):1576–1579. [DOI] [PubMed] [Google Scholar]
- 42.Marescaux J, Leroy J, Gagner M, et al. Transatlantic robot-assisted telesurgery. Nature. 2001;413(6854):379–380. [DOI] [PubMed] [Google Scholar]
- 43.Anvari M, McKinley C, Stein H. Establishment of the world’s first telerobotic remote surgical service: for provision of advanced laparoscopic surgery in a rural community. Ann Surg. 2005;241(3):460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xu S, Perez M, Yang K, Perrenot C, Felblinger J, Hubert J. Determination of the latency effects on surgical performance and the acceptable latency levels in telesurgery using the dV-Trainer® simulator. Surg Endosc. 2014;28(9):2569–2576. [DOI] [PubMed] [Google Scholar]
- 45.Lema MA, Laya A, Mahmoodi T, et al. Business case and technology analysis for 5G low latency applications. IEEE Access. 2017:1–1. [Google Scholar]
- 46.Haidegger T, Sándor J, Benyó Z. Surgery in space: the future of robotic telesurgery. Surg Endosc. 2011;25(3):681–690. [DOI] [PubMed] [Google Scholar]
- 47.Wirz R, Torres LG, Swaney PJ, et al. An experimental feasibility study on robotic endonasal telesurgery. Neurosurgery. 2015;76(4):479-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zheng J, Wang Y, Zhang J, et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc. 2020;34(11):5172–5180. [DOI] [PubMed] [Google Scholar]
- 49.Rayman R, Croome K, Galbraith N, et al. Robotic telesurgery: a real-world comparison of ground- and satellite-based internet performance. Int J Med Robotics Comput Assist Surg. 2007;3(2):111–116. [DOI] [PubMed] [Google Scholar]
- 50.Nguan CY, Morady R, Wang C, et al. Robotic pyeloplasty using internet protocol and satellite network-based telesurgery. Int J Med Robot. 2008;4(1):10–14. [DOI] [PubMed] [Google Scholar]
- 51.Li H-M, Zhang R-J, Shen C-L. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine (Phila Pa 1976). 2020;45(2)::E111–E119. [DOI] [PubMed] [Google Scholar]
- 52.Tian W, Fan M, Zeng C, Liu Y, He D, Zhang Q. Telerobotic spinal surgery based on 5G network: the first 12 cases. Neurospine. 2020;17(1):114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gallagher AG, O’Sullivan GC. Fundamentals of Surgical Simulation. Springer, London, 2012. [Google Scholar]
- 54.Hong Z, Li N, Li D, et al. Telemedicine during the COVID-19 pandemic: experiences from western China. J Med Internet Res. 2020;22(5):e19577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhou B, Wu Q, Zhao X, Zhang W, Wu W, Guo Z. Construction of 5G all-wireless network and information system for cabin hospitals. J Am Med Inform Assoc. 2020;27(6):934–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brennan S, Serle J, Clover B. Tariff set for sweeping change from next year. HSJ. Published October 9, 2018. https://www.hsj.co.uk/finance-and-efficiency/tariff-set-for-sweeping-change-from-next-year/7023543.article. [Google Scholar]
- 57.Aanestad M, Grisot M, Hanseth O, Vassilakopoulou P. Strategies for Building eHealth Infrastructures. In: Aanestad M, Grisot M, Hanseth O, Vassilakopoulou P, eds. Information Infrastructures within European Health Care: Working with the Installed Base. Springer, 2017. Accessed February 21, 2021.http://www.ncbi.nlm.nih.gov/books/NBK543690/. [Google Scholar]
- 58.Sakellaropoulos T, Vougas K, Narang S, et al. A deep learning framework for predicting response to therapy in cancer. Cell Rep. 2019;29(11):3367–3373.e4. [DOI] [PubMed] [Google Scholar]
- 59.Quang D, Xie X. DanQ: a hybrid convolutional and recurrent deep neural network for quantifying the function of DNA sequences. Nucleic Acids Res. 2016;44(11):e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ye Q, Zhou J, Wu H. Using information technology to manage the COVID-19 pandemic: development of a technical framework based on practical experience in China. JMIR Med Inform. 2020;8(6):e19515.e19515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Samsung. 6G the next hyper-connected experience for all. In: Samsung Research. Published 2020. http://refhub.elsevier.com/S1350-9462(20)30072-0/sref260.
- 62.Du Lim T. A novel human activity recognition and prediction in smart home based on interaction. Sensors. 2019;19(20):4474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McCarthy J, Minsky ML, Rochester N, Shannon CE. A proposal for the Dartmouth Summer Research Project on Artificial Intelligence, August 31, 1955. AI Mag. 2006;27(4):12. [Google Scholar]
- 64.Bengio Y, Courville A, Vincent P. Representation learning: a review and new perspectives. IEEE Trans Pattern Anal Mach Intell. 2013;35(8):1798–1828. [DOI] [PubMed] [Google Scholar]
- 65.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521(7553):436–444. [DOI] [PubMed] [Google Scholar]
- 66.Schmidhuber J. Deep learning in neural networks: an overview. Neural Netw. 2015;61:85–117. [DOI] [PubMed] [Google Scholar]
- 67.Lakhani P, Sundaram B. Deep learning at chest radiography: automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology. 2017;284(2):574–582. [DOI] [PubMed] [Google Scholar]
- 68.Medeiros FA, Jammal AA, Thompson AC. From machine to machine. Ophthalmology. 2019;126(4):513–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anvari M. Telesurgery: translation technology to clinical practice. In: Rosen J, Hannaford B, Satava RM, eds. Surgical Robotics. Springer US, 2011:653–660. [Google Scholar]
- 70.Douglas HE, Raban MZ, Walter SR, Westbrook JI. Improving our understanding of multi-tasking in healthcare: drawing together the cognitive psychology and healthcare literature. Appl Ergon. 2017;59(Pt A):45–55. [DOI] [PubMed] [Google Scholar]
- 71.Cowan N, Elliott EM, Scott Saults J, et al. On the capacity of attention: its estimation and its role in working memory and cognitive aptitudes. Cogn Psychol. 2005;51(1):42–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Park J, Kim J, Kim S-Y, et al. Soft, smart contact lenses with integrations of wireless circuits, glucose sensors, and displays. Sci Adv. 2018;4(1):eaap9841. [DOI] [PMC free article] [PubMed] [Google Scholar]