Abstract
Introduction
Despite the success of antiretroviral therapy (ART) in transforming HIV disease into a chronic infection, people living with HIV (PLWH) remain at risk for various non-AIDS inflammatory comorbidities. Risk of non-AIDS comorbidities is associated with gut dysbiosis, epithelial gut damage and subsequent microbial translocation, and increased activation of both circulating CD4+ and CD8+ T-cells. Therefore, in addition to ART, novel gut microbiota-modulating therapies could aid in reducing inflammation and immune activation, gut damage, and microbial translocation. Among various gut-modulation strategies under investigation, the Amazonian fruit Camu Camu (CC) presents itself as a prebiotic candidate based on its anti-inflammatory and antioxidant properties in animal models and tobacco smokers.
Method and analysis
A total of 22 PLWH on ART for more than 2 years, with a viral load <50 copies/mL, a CD4 +count >200 and a CD4+/CD8 +ratio <1 (suggesting increased inflammation and risk for non-AIDS comorbidities), will be recruited in a single arm, non-randomised, interventional pilot trial. We will assess tolerance and effect of supplementation with CC in ART-treated PLWH on reducing gut damage, microbial translocation, inflammation and HIV latent reservoir by various assays.
Ethics and dissemination
The Canadian Institutes of Health Research (CIHR)/Canadian HIV Trials Network (CTN) pilot trial protocol CTNPT032 was approved by the Natural and Non-prescription Health Products Directorate of Health Canada and the research ethics board of the McGill university Health Centre committee (number 2020-5903). Results will be made available as free access through publications in peer-reviewed journals and through the CIHR/CTN website.
Trial registration number
Keywords: HIV & AIDS, inflammatory bowel disease, nutritional support, immunology
Strengths and limitations of this study.
Camu camu (CC) is an Amazonian rainforest fruit which has been shown to have anti-inflammatory and gut microbiota-modulating properties in mice.
The CC study seeks to confirm mouse model findings on systemic inflammation and immune activation, gut dysbiosis and damage, and subsequent microbial translocation in antiretroviral therapy (ART)-treated people living with HIV (PLWH).
We hypothesise that treatment with CC will beneficially impact ART-treated PLWH by improving their gut microbiota composition, reducing microbial translocation, reducing inflammation to potentially decreasing latent HIV reservoir size and the risk to develop non-AIDS comorbidities.
Changes induced by CC treatment will be assessed by plasma markers of gut damage, microbial translocation, inflammation, percentage of activated T-cells, HIV reservoir size and gut bacterial taxa.
This pilot trial with 22 ART-treated PLWH, will provide sufficient data for future sample size calculations to confirm the effect of CC in more definitive larger studies.
Introduction
Antiretroviral therapy inhibits viral replication without eradication
Antiretroviral therapy (ART) successfully controls HIV infection by inhibiting viral replication and has significantly improved the life expectancy of people living with HIV (PLWH) while eliminating transmission to others. However, ART-treated PLWH remain at risk for developing inflammatory non-AIDS comorbidities such as cardiovascular diseases, fatty liver, neurocognition dysfunction and cancer.1 2 These non-AIDS comorbidities are associated with persistent immune activation and increase with ageing, coinfections like cytomegalovirus and viral hepatitis as well as microbial translocation. It has been observed in HIV infection and inflammatory bowel disease (IBD) that abnormal composition of the gut microbiota called ‘dysbiosis’, alteration of the gut barrier, T-helper (Th) 17 cell dysfunction and microbial translocation lead to systemic inflammation and immune activation contributing to non-AIDS comorbidities.3–9 Long-term HIV control by ART appears to only partially reduce inflammation and poorly replenishes Th17 protective mucosal function, highlighting the importance of research on gut microbiota and the epithelial barrier. Furthermore, despite control of HIV replication, persistent HIV infection in long-lived memory CD4+ T-cells and likely macrophages also contribute to inflammation and microbial translocation, creating a vicious cycle nurturing inflammation. Importantly, the size of the HIV reservoir has been linked to the level of inflammation and immune activation measured in CD8+ T-cells and macrophages.3 10 Conversely, it remains unknown whether the reduction of inflammation can lead to a decrease in the size of the HIV reservoir.
Gut damage and immune activation
As HIV is not cleared with ART, persistent viral products and inflammation subsequently impair antigen-specific T-cell responses. This overall activation leads to the exhaustion of the immune system, including T-cells. This distinctive feature from other chronic viral infections is relevant as HIV replicates preferentially in Th17 CD4+ T-cells residing in the gut, leading to cell death and mucosa damage.11–13 Microbial products penetrate the damaged gut barrier and pass into the systemic circulation. Such microbial translocation contributes to systemic immune activation, disease progression, and development of non-AIDS comorbidities.14–17 Markers of bacterial translocation, including lipopolysaccharide (LPS), LPS binding protein, and soluble CD14 (sCD14) have been correlated with immune activation and disease progression.3 11 18 19 While bacterial translocation is thought to be a major cause of immune activation, we have shown that circulating beta-D-glucan (BDG), a marker of fungal translocation, also contributes to immune activation in an LPS-independent manner.20 21
Although ART suppresses HIV replication to undetectable levels, microbial translocation and Th17 damage remain, contributing to persistent immune activation. Local gut inflammation has been associated with HIV reservoir size.22 Monocytes/macrophages, dendritic cells and natural killer cells detect microbial products in the mesenteric lymph nodes and in systemic circulation, secreting pro-inflammatory cytokines (interleukin (IL)-1β, IL-8, tumour necrosis factor (TNF)-α). These cytokines drive CD4+ T-cell activation, leading to elevated expression of the HIV coreceptor C-C chemokine receptor (CCR) 5 and the gut homing receptor CCR6 (23). Th17 measured by CD4+ T-cells expressing CCR6 have then been shown by our group to be preferentially infected by HIV.23 12 13 24
Gut microbiota, dysbiosis and immune regulation
The gut microbiota composition and metabolites play an important role in inflammation in obesity, diabetes, cancer and HIV infection. Its role includes food and metabolite processing, microbial regulation and immune regulation.25–28 PLWH, compared with uninfected controls, present with a dysbiosis characterised by a lower abundance of Firmicutes and more abundant Proteobacteria in their gut microbiota. In addition lack of Lactobacilli in stools is associated with lower CD4+ T-cell count and a higher levels of systemic immune activation.29 Moreover, lower levels of Akkermansia muciniphila have been observed in PLWH. Dysbiosis combined with microbial translocation has been linked to non-AIDS comorbidities in HIV-infected individuals and influences CD4+ T-cell recovery on ART as reported by our group and others.3 14 18 30 31
Akkermansia muciniphila in health and disease
A. muciniphila is a gram-negative, strict anaerobe and mucin-degrading bacterium that colonises the gut of humans and rodents. A. muciniphila represents 1%–5% of all intestinal bacteria. This bacterium acts as a shield on the gut epithelial barrier and has been shown to reduce insulin resistance in obese individuals.26 32–36 Lower abundance of A. muciniphila has been found in the faeces of patients with IBD and individuals with obesity, when compared with faeces of healthy individuals.25 26 Furthermore, oral administration of A. muciniphila to mice fed a high-fat diet alleviates obesity, reduces LPS in the circulation and alleviates insulin resistance.26 37 38
Additionally, patients with lung and renal cell carcinoma responding to anti-PD-1 treatment were more prone to have an elevated abundance of gut A. muciniphila compared with non-responders.28 To go beyond association, Routy et al transferred the microbiota from responders and non-responders into germ-free mice and observed a tumour response only in mice with a A. muciniphila rich human faecal microbiota from the responders.28 Both in vitro and in vivo, A. muciniphila has been shown to increase mucus secretion by goblet cells and gut epithelium integrity contributing to the prevention of other bacterial products from passing into the circulation.35 38 39 Moreover, oral administration A. muciniphila was shown to successfully elevate key anti-ageing and anticancer metabolites primarily in the gut and liver.40
Based on these encouraging results, different attempts have been made to increase A. muciniphila in the gut. Everard et al showed that pasteurised A. muciniphila increased mucus thickness, decreased LPS translocation, and reduced metabolic syndrome in obese mice. In contrast, heat-killed A. muciniphila did not protect mice from obesity.38 However, such pasteurised strains are costly, difficult to produce and may not last after oral administration.
The Amazonian fruit Camu Camu
Camu Camu (CC), also named Myriciaria dubia, is an Amazon rainforest fruit with antioxidant and anti-inflammatory properties. Anhê et al showed that polyphenol-rich cranberry and CC extracts protect mice from diet-induced obesity and intestinal inflammation in association with increased A. muciniphila in the gut microbiota.32–35 CC was more efficient at reducing the amount of LPS in plasma than cranberry extract in the diet-induced model of obesity, and it was also found to increase other beneficial microbes in addition to A. muciniphila. Other studies have shown that polyphenols could favour A. muciniphila in the gut.26 41 42 Importantly, CC extracts also decreased C reactive protein (CRP), IL-6 and IL-8 in the plasma of healthy tobacco smokers.43 CC is considered a ‘super fruit’ which is widely available in many Canadian health food stores in either powder or capsule form. CC products have been used as a nutritional supplement that is well tolerated in humans.44
CC is a fruit rich in polyphenols and has been shown in mouse model of inflammation-related diseases to reduce inflammation and improve gut microbiota with increased A. muciniphila and other beneficial bacteria.32–35 However, no studies have been performed to test CC in PLWH. Moreover, PLWH on ART have been shown to exhibit persistent dysbiosis, an altered gut microbiota composition, along with microbial translocation which can cause non-AIDS comorbidities and hamper CD4+ T-cell recovery.3 14 18 30 Therefore, we will evaluate if the polyphenol-rich CC can positively affect PLWH on ART in terms of reducing inflammation, improving gut microbiota and potentially decreasing HIV persistent reservoir.
Objective
To determine the feasibility and suitable design of a full-scale study on the effect of CC in ART-treated PLWH, we designed a non-randomised, single arm, interventional study.
Primary outcomes
The primary outcome of this study will be to evaluate the effect of CC on the reduction of the plasma marker of microbial translocation LPS, assessed using ELISA.
Secondary outcomes
The secondary outcomes of this study will be changes in the following before and after 12 weeks of CC intake, and after 8 weeks of CC discontinuation:
Safety and tolerability of CC measured by evaluating adverse events, haematology, and serum chemistries over the course of the study. These evaluations will include HIV viral load, glucose levels, a lipid profile and plasma levels of high sensitivity CRP and D-dimer.
Gut barrier integrity markers Intestinal-Fatty Acid Binding Protein (I-FABP) and Suppression of Tumourigenicity (sST2), measured by ELISA.
Microbial translocation marker1–3-BDG assessed using the Fungitell assay.
Proinflammatory markers (IL-1β, IL-6, IL-8, IL-18. IP-10, IL-17A and F, IL-22, and soluble CD14) and anti-inflammatory markers (IL-10) assessed by ELISA.
T-cell and monocyte activation levels assessed by flow cytometry using markers CD38, HLA-DR and PD-1.
A. muciniphila levels in stools using qPCR.
Microbiota composition and diversity in stools assessed using 16S rDNA sequencing.
HIV reservoir size in blood assessed by PCR.
Evaluate intrapatient variability using data from two baseline visits, approximately 2 weeks apart from each other to confirm reliability of baseline results.
Exploratory outcomes
The exploratory outcomes of this study will be the following:
Difference in HIV reservoir size from Baseline (visit 0) to 12 weeks post-CC treatment by Tat/rev Induced Limiting Dilution Assay (TILDA), performed on blood samples.
Changes in other markers of gut damage (including plasma REG3α45), microbial translocation (such as plasma 16S rDNA) and immune activation (T-cell activation, cytokines) in the blood and gut biopsies.
Substudy outcomes
The substudy outcomes will be the following:
Changes in gut mucosa architecture in a subset of participants who will consent to have colon biopsies before and at the end of the 12 weeks of CC treatment.
Changes in inflammation in gut mucosa biopsy assessed by myeloperoxidase staining before and at the end of the 12 weeks of CC treatment.
Changes in HIV reservoir size in biopsies using qPCR.
Association between baseline gut microbiota composition (16S rDNA sequencing), and markers of gut integrity (I-FABP, tissue staining) and inflammation (T-cell activation, inflammatory cytokines).
Methods and analysis
Study design, settings, sample size and recruitment strategy
Trial CTN PT032 is an open label, non-randomised, single arm interventional pilot study (Clinicaltrials.gov NCT04058392); protocol version # 1.3; February 12, 2021. The study sponsor is the Canadian Institutes of Health Research Canadian HIV Trials Network (CTN). The following study protocol fulfils the requirements of the 2013 Standard Protocol Items: Recommendations for Interventional Trials guidelines.46 47
Comparisons and assessment of outcomes will be made through various measures at baseline, during and after CC use (figure 1 and table 1).
Figure 1.
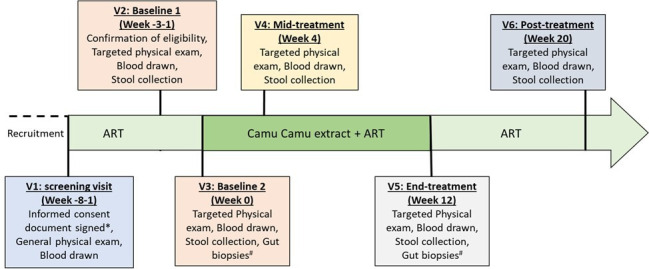
Study flow chart. Visit 1, the screening visit, will take place 1–8 weeks prior to the second baseline visit (week 0, visit 3). At the screening visit the informed consent document will be explained to the participant and will be signed prior to any screening and study activities. Two baseline visits will be conducted, the second one being at week 0 and all visits after that will be relative to this baseline week 0 visit (visit 3, day 0). Data collected at these two baseline visits will be directly compared with determine intrapatient variability. Camu Camu treatment will be a single daily dose of 1000 mg (2500 mg Camu C capsules*) taken with a meal, at the same time each day for 12 weeks. Treatment and post-treatment visit dates (visit 4, week four and visit 6, week 20) can vary ±7 days according to participant and/or research team availability. Visit 5 at week 12 can vary +7 days to ensure the participant has completed 12 weeks of Camu Camu treatment prior to the end-of-treatment visit. See section 8 schedule of events (table 1) to see more test details. *The consent form for the optional gut biopsy will also be explained, but consent for this will not be necessary to be part of the main study. The substudy is only available to participants at the Montreal site. #Optional gut biopsies will be taken for the sub-study at indicated time points. ART, antiretroviral therapy.
Table 1.
Schedule of events
| Visit type | Screening | Study visits | ||||
| Baseline 1 | Baseline 2 | Treatment | Follow-up | |||
| Visit window procedures: | −8 to −1 weeks | Week −2 (±7 days) | Week 0 (day 0) | Week 4 (±7 days) | Week 12 (+7 days) | Week 20 (±7 days) |
| Visit no | 1 | 2 | 3 | 4 | 5 | 6 |
| Informed consent | X | X | ||||
| Eligibility assessment | X | X | X | |||
| Concomitant medication | X | X | X | X | X | X |
| Medical history | X | |||||
| Complete physical exam and vital signs | X | |||||
| Targeted physical exam and vital signs | X | X | X | X | X | |
| Adverse event assessment | X | X | X | |||
| Serum pregnancy test | X | X | X | X | X | X |
| Haematology* | X | X† | X | X | X | X |
| Serum chemistry‡ | X | X† | X | X | X | X |
| Serology§ | X | X | ||||
| HIV-1 viral load§ | X | X† | X | X | X | X |
| Immune activation markers/cytokines (ELISA)¶ | X | X | X | X | X | |
| Monocyte and T-cell activation markers** | X | X | X | X | X | |
| Markers of gut barrier integrity, inflammation, and microbial translocation†† | X | X | X | X | X | |
| Size of HIV reservoir in latently infected CD4+T-cells‡‡ | X | X | X | X | X | |
| Stool sample collection and microbiota composition§§ | X | X | X | X | X | |
| Alcohol use questionnaire (AUDIT-Full) | X | |||||
| Alcohol use questionnaire (AUDIT-C) | X | X | X | X | X | |
| Study product dispensation | X | |||||
| Study product compliance | X | X | ||||
| Colon mucosal biopsies¶¶ | X | X | ||||
*CBC, CD4 and CD8 T-cell counts, erythrocyte sedimentation rate.
†Not required when the same tests have been performed at the screening visit within the past 14 days, with the exception of CBC, CD4, CD8 (and serum pregnancy test).
‡Alkaline phosphatase, ALT, amylase, AST, bilirubin (total), creatine kinase, creatinine, D-dimer, fasting blood glucose, HbA1c, high sensitivity C reactive protein, lipase, lipid profile (total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides), serum phosphate, urea.
§Serology measurements include: cytomegalovirus, hepatitis B virus, HCV and HIV viral load. Since HIV viral load will be measured at each visit, it was put as a separate line item.
¶Immune activation markers/cytokines include soluble CD14, proinflammatory cytokines (IL-1β, IL-6, IL-8, TNF-α) and anti-inflammatory cytokine IL-10. Measured in plasma by ELISA.
**Monocyte and T-cell activation markers include HLA-DR and CD38. T-cell exhaustion marker: PD-1. Measured by staining and flow cytometry.
††Markers of gut barrier integrity, microbial translocation, and inflammation: lipopolysaccharide, soluble ST2, I-FABP (measured in plasma by ELISA).
‡‡PBMCs will be isolated and then latent CD4 T-cells will be isolated by flow cytometry. HIV viral reservoir in the latent CD4 T-cell population will be measured by nested qPCR. More specific TILDA analysis will be performed on baseline week 0 and end-treatment week 12 samples to assess the HIV viral reservoir (exploratory analysis).
§§qPCR of Akkermansia muciniphila, 16S and 18S rDNA sequencing for other members of the microbiota.
¶¶Optional substudy procedure.
ALT, Alanine Aminotransferase; AST, Aspartate Aminotransferase; AUDIT, Alcohol Use Disorders Identification Test; HbA1c, Hemoglobin A1c; I-FABP, Intestinal-Fatty Acid Binding Protein; PBMCs, Peripheral Blood Mononuclear Cells; TILDA, Tat/rev Induced Limiting Dilution Assay.
A total of 22 ART-treated participants living with HIV will be enrolled at the Chronic Viral Illness Service at the McGill University Health Centre (MUHC), Glen Site, Montreal, QC and the Ottawa Hospital, General Campus, Infectious Diseases Clinic, Ottawa, Ontario, Canada. A convenient sample size of 22 participants was chosen without formal power calculations for this pilot study, based on the Lilac study design48 49 and the study by Inoue et al.43 This sample size accounts for an estimated loss to follow-up/non-completion of 10% for the study. It can therefore be estimated that two participants may not fully complete the study. There will be an optional colon biopsy sub-study. For logistical reasons, only participants recruited at the Montreal site will be given the option to participate in this substudy, after giving informed consent to participate in the main study and being shown to be eligible for the main study (after screening). The substudy will have a separate informed consent form. The obtained data from this study will be used for calculation of sample size for future larger studies.
Participants will be recruited at two above-mentioned centres in Canada. Both participating medical clinics provide care to more than 2000 HIV-infected persons. Teleconferences and face-to-face meetings will be organised between the qualified investigators and study staff to help promote patient recruitment and follow-up during the study.
At screening, a medical history and medication history will be recorded by study staff through chart review and/or patient interview. Date of diagnosis, date of ART initiation, nadir CD4 count, mode of HIV acquisition and previous AIDS defining illnesses will be recorded. Previous use of ART drugs and other medication will also be documented.
Recruitment started in November 2020 and is expected to end in January 2022.
Inclusion criteria
Participants will be eligible for the study if they meet the following criteria: (1) male or female adults ≥18 years of age; (2) documented HIV-1 infection by Western Blot, Enzyme Immuno Assay or viral load assay; (3) on ART for at least 2 years, and stable ART regimen (same prescription) for at least 3 months to ensure a stabilisation of inflammation markers; (4) persistent undetectable viral load <50 copies/mL for the past 2 years. One viral blip are allowed if preceded and followed by a HIV viraemia below 50 copies/mL; (5) CD4 +count >200 and a CD4+/CD8 +ratio <1, to recruit participants with increased inflammation and risk for non-AIDS comorbidities; (6) able to communicate adequately in either French or English; (7) able and willing to provide written informed consent prior to screening; (8) as the influence of CC on pregnant women is unknown, women of childbearing potential must have a negative serum pregnancy test; (9) women of childbearing potential must agree to use an approved methods of birth control while in the study and until 2 weeks after completion of the study; (10) women of non-child-bearing potential as defined as either postmenopausal (12 months of spontaneous amenorrhea and ≥45 years of age) or physically incapable of becoming pregnant with documented tubal ligation, hysterectomy or bilateral oophorectomy and (11) sexually active men with a female partner of childbearing potential must agree to use an approved methods of birth control.
Exclusion criteria
Participants will not be eligible to participate in the study if they meet any of the following conditions: (1) Known allergy/hypersensitivity to CC; (2) Current AIDS-related event or serious health condition including systemic infections in the last 3 months; (3) Severe systemic diseases (eg, uncontrolled hypertension, chronic renal failure) or active uncontrolled infections; (4) Coinfection with active Hepatitis B or C virus; (5) Current use or have used in the past 3 months: immune-modulatory agents, prophylactic antibiotics41/antibiotics, proton pump inhibitors, or Morphine as these drugs modulate gut microbiota; (6) Current use of aluminium containing phosphate binders, chemotherapeutics, niacin, anticoagulant and protease inhibitors (including in their ART-regimen) as increased vitamin C levels can prevent the activity of those molecules; (7) Diagnosis of diabetes mellitus (HbA1c≥6.5%) as defined by the Canadian Clinical Practice Guidelines for the Prevention and Management of Diabetes50; (8) Frequent use of probiotics or polyphenol-rich prebiotics (eg, cranberry and CC powders and/or capsules) in the last 12 months; (9) Recent changes in dietary habits, intermittent fasting, chronic constipation or laxative use as these can affect gut microbiota; (10) Psychiatric or cognitive disturbance or any illness that could preclude compliance with the study; (11) Current participation in an experimental therapy study or receipt of experimental therapy within the last 6 months; (12) Women who are planning to become or who are pregnant, or breast feeding and (13) A score of higher than eight on a full Alcohol Use Disorders Identification test (AUDITà questionnaire at the screening visit, suggesting an alcohol abuse problem.
Study intervention
Participants will be instructed to take 1000 mg of Camu C (provided by Natural Traditions, Canada) once daily administered as two 500 mg oral capsules for 12 weeks. Capsules will be taken at the same time each day with a meal, preferentially breakfast. Camu C can be taken with ART as no interactions are expected. The 1000 mg dose is based on the dose given to mice per mean body weight divided by 12.3 as per the Food and Drug Administration equation to determine equivalent dosing in human vs mice, and consistent with Health Canada’s recommendations of 1–3 capsules daily.51 52
The interaction between CC and other medication is unknown. CC has a high vitamin C concentration and therefore any drug with negative interactions with vitamin C were included in the exclusion criteria. The vitamin C in CC could interact with aluminium in phosphate binders (possible harmful to kidneys); chemotherapeutics (CC antioxidative properties could reduce the chemotherapeutic drug’s effect); protease inhibitors (vitamin C might reduce the effect of antiviral drugs containing protease inhibitors); niacins (vitamin C could reduce niacin’s effect); and anticoagulants since high doses of vitamin C can reduce responses to some anticoagulants. Hence, participants will be asked to refrain from using vitamin C supplements during the study.
Use of street drugs, cigarette smoking, non-prescription medications and marijuana/cannabis products use will be recorded in questionnaires by a research staff at each visit. Study continuation will be based on the Investigator’s judgement. In the 24 hours prior to a study visit participants will be instructed to refrain from using marijuana/cannabis products and limit alcohol to no more than one alcoholic beverage with dinner the night before the study visit as they could influence inflammation markers in blood and gut microbiota in stools.
Adverse events and toxicity management
During each follow-up visit with the participant, information on adverse events (AEs) will be gathered and documented accordingly. AEs will be graded as mild, moderate, severe or life-threatening and assessed by causality as probably related, possibly related, unlikely to be related or not related to Camu C. Stable chronic conditions which are present prior to clinical trial entry and do not worsen are not considered AEs and will be accounted for in the participant’s medical history.
Risk minimisation, management and assessment procedures have been implemented in the study to minimise and assess potential risks to participants who participate in this clinical study with Camu C. Components include specific study entry and exclusion criteria to ensure that participants who have underlying characteristics that potentially increase their risk for an adverse outcome are excluded; monitoring for adverse events for the duration of the study; overview surveillance by an Independent data safety monitoring Committee; risk identification and mitigation management over the course of the study (and the substudy).
When side effects are perceived to be related to Camu C, the investigator can use their clinical judgement regarding whether to continue or to discontinue the study medication. If Camu C treatment is discontinued, the participant will be scheduled for follow-up visit(s) as required to treat the symptoms or adverse event related to Camu C intake.
Clinical and laboratory assessments
Assessment of gut damage, microbial translocation and inflammation
To evaluate gut epithelial damage, we and others have validated markers that will be measured in the plasma by ELISA before, during and after CC intake.11 53–55 LPS, a common marker of bacterial translocation,56 soluble sST220 and I-FABP will be measured to assess gut barrier integrity. Immune activation markers (sCD14) and pro-(IL-1β, IL-6. IL-8, TNF-α) and anti-inflammatory (IL-10) cytokines will be quantified.57 58 Activation of monocytes and CD4+ and CD8+ T-cells will be assessed ex vivo by flow cytometry with HLA-DR and CD38 staining. CD4+and CD8+ T-cells will also be assessed for PD-1 expression as a marker of T-cell exhaustion. Plasma will be assayed for BDG as a marker of fungal infection.21 58 REG3α and 16S rDNA as well as other markers of microbial translocation and gut damage may be tested in plasma as well.45
Assessment of microbiota composition
qPCR for A. muciniphila will be performed on faecal DNA samples as previously described by our group.48 Gut microbiota composition will be further studied by 16S and 18S rDNA sequencing to determine the impact on other beneficial microbes (eg, Barnesiella and Turicibacter) known to respond to CC in the obesity mouse model.48
Assessment of HIV reservoir size
If differences in microbial translocation and/or inflammation are observed, HIV reservoirs will be quantified in blood and rectal biopsies. HIV DNA (total and integrated) and cell-associated HIV RNA (gag) will be measured in DNA and RNA obtained from isolated CD4+ T-cells from the blood (obtained by negative magnetic selection) and gut biopsies (sorted by flow cytometry). HIV DNA and cell-associated RNA measures will be performed using an ultrasensitive nested qPCR as described previously.59
In addition, the frequency of cells with inducible proviruses will be measured in isolated CD4+ T-cells from PBMCs using the TILDA in the laboratory of Dr. Chomont at Baseline Week 0 and End-treatment Week 12 timepoints.
In mucosal biopsies, HIV DNA and RNA will also be quantified and localised by DNA/RNAscope.24 60
Assessment of gut mucosa architecture (optional colon biopsy/sub-study)
Biopsies will be included in paraffin at the MUHC Histopathology core facility. Gut architecture will be monitored by immunochemistry and immunostaining of the epithelial tight junctions (Claudin-3/Occludin).56 If a diminution in inflammation is noted, myeloperoxidase staining will be performed to allow for the quantification of inflammatory myeloid cells in the gut.
For other analyses, gut cells will be separated from tissues by enzyme digestion using a collagenase-based method as reported previously.61 62 Briefly, fresh tissue biopsies will be incubated with type II collagenase for 30 min at 37°C in a shaking incubator. The resulting lymphocyte suspension will be stained with monoclonal Antibodies against CD3+, CD4+, CD8+ and myeloid markers. The total frequency of activated CD4+ and CD8+ T-cells will be determined by flow cytometry as described above.
Statistical analysis
To examine the change in plasma LPS and soluble CD14 levels relative to baseline, linear mixed effects regression will be used. Time will be considered as a categorical variable in the model to allow flexible modelling of the time trend. All five measurements (two for baseline and three for follow-up visits) will be included as outcome variable in the model. Log transformation of the outcome variable or generalised mixed effects regression will be employed if normality assumption is not satisfied. Changes in plasma markers, percentage of activated T-cells, HIV reservoir size and bacterial taxa by type in the stools samples relative to baselines will be assessed in the same fashion. Demographics including age, sex, sexual practice and HIV history data will be included in multivariable analyses as they have been shown to influence microbiota composition and immune activation in ART-treated PLWH.29 63
Patient and public involvement
Initial design of the study was presented to community groups.
Compliance questionnaires completed by participants throughout the study will allow for an assessment of their respective experiences.
Results generated by the study are expected to be published in both formal scientific and lay language; however, will not be directly disseminated to study participants.
Ethics and dissemination plan
All participants will be given detailed oral and written information about the study. Consent documents describing in detail the study medication and interventions, study procedures and risks will be given to each participant and written documentation of informed consent is required prior to starting study medication/intervention. Participants must sign an informed consent document that has been approved by a participating centre’s research ethics board (REB) prior to any procedures being done specifically for the trial. All potential protocol amendments will be submitted to Health Canada and the respective research ethics board of the participating centres. Protocol deviations must first receive ethics approval and be reported to the data safety and monitoring committee of the CTN by the investigator. The sole exception is when the suggested change intends to eliminate an immediate hazard to study participants.
Dissemination plan
The results of the trial will be disseminated through the traditional routes of scientific peer-reviewed publications, through international and national specialist conferences and through the press release by CTN. An open access journal will be chosen to ensure access to study results to all. Locally, results from the study will be shared with the McGill community. Study results will be submitted for publication in the Montréal LGBTQ+Community journal Fugues. Moreover, both the sponsor-investigator and qualified investigator will promote the CC study when attending or presenting at local, national and international meetings.
Conclusion
We hypothesise that treatment with CC will beneficially impact ART-treated PLWH by improving the gut microbiota composition, reducing systemic inflammation and immune action, reducing gut damage and microbial translocation, and potentially decreasing latent HIV reservoir size, thus decreasing the risk in developing non-AIDS comorbidities. This pilot trial with 22 ART-treated PLWH will provide sufficient data for future sample size calculations and set the foundation to assess the impact of CC in larger definitive studies.
Supplementary Material
Acknowledgments
The authors would like to thank Angie Massicotte, Josee Girouard, Hansi Peiris, Cynthia Dion and Cezar Iovi for their help with coordination. The authors are grateful to members of the CIHR/CTN who’s insights paramount in the development of the protocol: Dr Judy Needham, Dr Joanne McBane, as well as Dana Nohynek for her help with regulatory affairs. The authors thank William Chau for building the study database.
Footnotes
Collaborators: Group Authorship/Collaborating Author Names: SI, BF, JO, JL, LR, SB, NS, PL, TB, NS, MK, BL, CTC, BR, AM, and JPR, for the Camu Camu Study Group.
Contributors: J-PR and SI designed the study, with insights from JO, LR, JL, NS, NC, BR and AM. BF and SI wrote the manuscript. JL, LR, SB, PL, TB, NC, MK, BL, CTTC, BR and AM will participate in data collection and analysis. All authors critically reviewed the manuscript and approved the final version.
Funding: This study was funded by the Canadian Institutes of Health Research (CIHR) Canadian HIV trials Network (CTN) (CTN PT032 grant to SI and JPR), and by the Canadian HIV Cure Enterprise (CanCURE) (Team Grant HB-164064 to JPR). Authors who are CTN and/or CanCURE members were involved in the study design and in the writing of the manuscript, and will also be involved in data collection, analysis and interpretation.
Competing interests: J-PR has performed contract research and/or served on Advisory Boards for Gilead Sciences Canada, Merck Canada, Abbvie, ViiV Healthcare, Bristol Myers Squibb, Janssen, Argos Pharmaceuticals from InnaVirVax and has served on the Advisory Board of Theravectys. JBA has performed contract research and/or served on Advisory Boards for Gilead Sciences Canada, Merck Canada, Abbvie, ViiV Healthcare, Bristol Myers Squibb, Janssen and Argos Pharmaceuticals. NC has received research funding from EMD Serono and has served on the Advisory Board of Gilead Sciences Canada. SI is a post-doctoral fellow from the Fonds de recherche du Quebec en santé, and from the CIHR/CTN. BL is supported by a career award LE 250 from Quebec’s Ministry of Health for researchers in family medicine. BL has received consultancy fees and/or honoraria from Gilead, Merck, and ViiV, and research funds from Gilead, Merck, and ViiV, support to attend educational conferences from Viiv Healthcare and Gilead. LR is a postdoctoral fellow supported by the Swiss National Science Foundation.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Srinivasa S, Grinspoon SK. Metabolic and body composition effects of newer antiretrovirals in HIV-infected patients. Eur J Endocrinol 2014;170:R185–202. 10.1530/EJE-13-0967 [DOI] [PubMed] [Google Scholar]
- 2. Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet 2013;382:1525–33. 10.1016/S0140-6736(13)61809-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 2006;12:1365–71. 10.1038/nm1511 [DOI] [PubMed] [Google Scholar]
- 4. Douek DC. Immune activation, HIV persistence, and the cure. Top Antivir Med 2013;21:128–32. [PMC free article] [PubMed] [Google Scholar]
- 5. Monnig MA, Kahler CW, Cioe PA, et al. Markers of microbial translocation and immune activation predict cognitive processing speed in Heavy-Drinking men living with HIV. Microorganisms 2017;5. 10.3390/microorganisms5040064. [Epub ahead of print: 21 09 2017]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Neff CP, Krueger O, Xiong K, et al. Fecal microbiota composition drives immune activation in HIV-infected individuals. EBioMedicine 2018;30:192–202. 10.1016/j.ebiom.2018.03.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sui Y, Dzutsev A, Venzon D, et al. Influence of gut microbiome on mucosal immune activation and SHIV viral transmission in naive macaques. Mucosal Immunol 2018;11:1219–29. 10.1038/s41385-018-0029-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vázquez-Castellanos JF, Serrano-Villar S, Latorre A, et al. Altered metabolism of gut microbiota contributes to chronic immune activation in HIV-infected individuals. Mucosal Immunol 2015;8:760–72. 10.1038/mi.2014.107 [DOI] [PubMed] [Google Scholar]
- 9. Zevin AS, McKinnon L, Burgener A, et al. Microbial translocation and microbiome dysbiosis in HIV-associated immune activation. Curr Opin HIV AIDS 2016;11:182–90. 10.1097/COH.0000000000000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clayton KL, Garcia JV, Clements JE, et al. Hiv infection of macrophages: implications for pathogenesis and cure. Pathog Immun 2017;2:179–92. 10.20411/pai.v2i2.204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mehraj V, Jenabian M-A, Ponte R, et al. The plasma levels of soluble ST2 as a marker of gut mucosal damage in early HIV infection. AIDS 2016;30:1617–27. 10.1097/QAD.0000000000001105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gosselin A, Monteiro P, Chomont N, et al. Peripheral blood CCR4+CCR6+ and CXCR3+CCR6+CD4+ T cells are highly permissive to HIV-1 infection. J Immunol 2010;184:1604–16. 10.4049/jimmunol.0903058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gosselin A, Wiche Salinas TR, Planas D, et al. HIV persists in CCR6+CD4+ T cells from colon and blood during antiretroviral therapy. AIDS 2017;31:35–48. 10.1097/QAD.0000000000001309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tincati C, Douek DC, Marchetti G. Gut barrier structure, mucosal immunity and intestinal microbiota in the pathogenesis and treatment of HIV infection. AIDS Res Ther 2016;13:19. 10.1186/s12981-016-0103-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Deeks SG, Phillips AN. Hiv infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ 2009;338:a3172. 10.1136/bmj.a3172 [DOI] [PubMed] [Google Scholar]
- 16. Gandhi RT, McMahon DK, Bosch RJ, et al. Levels of HIV-1 persistence on antiretroviral therapy are not associated with markers of inflammation or activation. PLoS Pathog 2017;13:e1006285. 10.1371/journal.ppat.1006285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hoenigl M, Moser CB, Funderburg N, et al. Soluble urokinase plasminogen activator receptor is predictive of non-AIDS events during antiretroviral therapy-mediated viral suppression. Clin Infect Dis 2019;69:676–86. 10.1093/cid/ciy966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Marchetti G, Tincati C, Silvestri G. Microbial translocation in the pathogenesis of HIV infection and AIDS. Clin Microbiol Rev 2013;26:2–18. 10.1128/CMR.00050-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sandler NG, Douek DC. Microbial translocation in HIV infection: causes, consequences and treatment opportunities. Nat Rev Microbiol 2012;10:655–66. 10.1038/nrmicro2848 [DOI] [PubMed] [Google Scholar]
- 20. Mehraj V, Ramendra R, Isnard S. (1-3)-Beta-D-Glucan antigenimia contributes to 1 immune activation during HIV infection. Clin Infect Dis 2018. [Google Scholar]
- 21. Isnard S, Lin J, Bu S, et al. Gut leakage of Fungal-Related products: turning up the heat for HIV infection. Front Immunol 2021;12:656414. 10.3389/fimmu.2021.656414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Peng X, Isnard S, Lin J, et al. Differences in HIV burden in the inflamed and non-inflamed colon from a person living with HIV and ulcerative colitis. J Virus Erad 2021;7:100033. 10.1016/j.jve.2021.100033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stevenson M, Stanwick TL, Dempsey MP, et al. HIV-1 replication is controlled at the level of T cell activation and proviral integration. Embo J 1990;9:1551–60. 10.1002/j.1460-2075.1990.tb08274.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chomont N, El-Far M, Ancuta P, et al. HIV reservoir size and persistence are driven by T cell survival and homeostatic proliferation. Nat Med 2009;15:893–900. 10.1038/nm.1972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Anhê FF, Varin TV, Le Barz M, et al. Gut microbiota dysbiosis in obesity-linked metabolic diseases and prebiotic potential of polyphenol-rich extracts. Curr Obes Rep 2015;4:389–400. 10.1007/s13679-015-0172-9 [DOI] [PubMed] [Google Scholar]
- 26. Dao MC, Everard A, Aron-Wisnewsky J, et al. Akkermansia muciniphila and improved metabolic health during a dietary intervention in obesity: relationship with gut microbiome richness and ecology. Gut 2016;65:426–36. 10.1136/gutjnl-2014-308778 [DOI] [PubMed] [Google Scholar]
- 27. Sepich-Poore GD, Zitvogel L, Straussman R, et al. The microbiome and human cancer. Science 2021;371. 10.1126/science.abc4552. [Epub ahead of print: 26 03 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Routy B, Le Chatelier E, Derosa L, et al. Gut microbiome influences efficacy of PD-1-based immunotherapy against epithelial tumors. Science 2018;359:91–7. 10.1126/science.aan3706 [DOI] [PubMed] [Google Scholar]
- 29. Vujkovic-Cvijin I, Somsouk M. Hiv and the gut microbiota: composition, consequences, and avenues for amelioration. Curr HIV/AIDS Rep 2019;16:204–13. 10.1007/s11904-019-00441-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lu W, Feng Y, Jing F, et al. Association between gut microbiota and CD4 recovery in HIV-1 infected patients. Front Microbiol 2018;9:1451. 10.3389/fmicb.2018.01451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vujkovic-Cvijin I, Sortino O, Verheij E, et al. Hiv-Associated gut dysbiosis is independent of sexual practice and correlates with noncommunicable diseases. Nat Commun 2020;11:2448. 10.1038/s41467-020-16222-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Anhê FF, Roy D, Pilon G, et al. A polyphenol-rich cranberry extract protects from diet-induced obesity, insulin resistance and intestinal inflammation in association with increased Akkermansia spp. population in the gut microbiota of mice. Gut 2015;64:872–83. 10.1136/gutjnl-2014-307142 [DOI] [PubMed] [Google Scholar]
- 33. Anhê FF, Nachbar RT, Varin TV, et al. Treatment with camu camu (Myrciaria dubia) prevents obesity by altering the gut microbiota and increasing energy expenditure in diet-induced obese mice. Gut 2019;68:453–64. 10.1136/gutjnl-2017-315565 [DOI] [PubMed] [Google Scholar]
- 34. Anhê FF, Nachbar RT, Varin TV, et al. A polyphenol-rich cranberry extract reverses insulin resistance and hepatic steatosis independently of body weight loss. Mol Metab 2017;6:1563–73. 10.1016/j.molmet.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Anhê FF, Pilon G, Roy D, et al. Triggering Akkermansia with dietary polyphenols: A new weapon to combat the metabolic syndrome? Gut Microbes 2016;7:146–53. 10.1080/19490976.2016.1142036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ouyang J, Lin J, Isnard S, et al. The Bacterium Akkermansia muciniphila: A Sentinel for Gut Permeability and Its Relevance to HIV-Related Inflammation. Front Immunol 2020;11:645. 10.3389/fimmu.2020.00645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cani PD. Human gut microbiome: hopes, threats and promises. Gut 2018;67:1716–25. 10.1136/gutjnl-2018-316723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Everard A, Belzer C, Geurts L, et al. Cross-Talk between Akkermansia muciniphila and intestinal epithelium controls diet-induced obesity. Proc Natl Acad Sci U S A 2013;110:9066–71. 10.1073/pnas.1219451110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Reunanen J, Kainulainen V, Huuskonen L, et al. Akkermansia muciniphila adheres to enterocytes and strengthens the integrity of the epithelial cell layer. Appl Environ Microbiol 2015;81:3655–62. 10.1128/AEM.04050-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Grajeda-Iglesias C, Durand S, Daillère R, et al. Oral administration of Akkermansia muciniphila elevates systemic antiaging and anticancer metabolites. Aging 2021;13:6375–405. 10.18632/aging.202739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Etxeberria U, Arias N, Boqué N, et al. Reshaping faecal gut microbiota composition by the intake of trans-resveratrol and quercetin in high-fat sucrose diet-fed rats. J Nutr Biochem 2015;26:651–60. 10.1016/j.jnutbio.2015.01.002 [DOI] [PubMed] [Google Scholar]
- 42. Li Z, Henning SM, Lee R-P, et al. Pomegranate extract induces ellagitannin metabolite formation and changes stool microbiota in healthy volunteers. Food Funct 2015;6:2487–95. 10.1039/C5FO00669D [DOI] [PubMed] [Google Scholar]
- 43. Inoue T, Komoda H, Uchida T, et al. Tropical fruit camu-camu (Myrciaria dubia) has anti-oxidative and anti-inflammatory properties. J Cardiol 2008;52:127–32. 10.1016/j.jjcc.2008.06.004 [DOI] [PubMed] [Google Scholar]
- 44. Langley PC, Pergolizzi JV, Taylor R, et al. Antioxidant and associated capacities of Camu camu (Myrciaria dubia): a systematic review. J Altern Complement Med 2015;21:8–14. 10.1089/acm.2014.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Isnard S, Ramendra R, Dupuy FP, et al. Plasma levels of C-type lectin REG3α and gut damage in people with human immunodeficiency virus. J Infect Dis 2020;221:110–21. 10.1093/infdis/jiz423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Chan A-W, Tetzlaff JM, Altman DG, et al. Spirit 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Isnard S, Lin J, Fombuena B, et al. Repurposing metformin in nondiabetic people with HIV: influence on weight and gut microbiota. Open Forum Infect Dis 2020;7:ofaa338. 10.1093/ofid/ofaa338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Routy J-P, Isnard S, Mehraj V, et al. Effect of metformin on the size of the HIV reservoir in non-diabetic ART-treated individuals: single-arm non-randomised Lilac pilot study protocol. BMJ Open 2019;9:e028444. 10.1136/bmjopen-2018-028444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. CDACPE C, Canada D. Clinical practice guidelines for the prevention and management of diabetes in Canada. Canadian Journal of Diabetes 2018;2018:S1–325. [DOI] [PubMed] [Google Scholar]
- 51. Canada H, Camu C. Product information. Available: https://health-products.canada.ca/lnhpd-bdpsnh/info.do?licence=80042046 [Accessed 5 Dec 2018].
- 52. Nair AB, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm 2016;7:27–31. 10.4103/0976-0105.177703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mehraj V, Ramendra R, Isnard S. Circulating (1->3)-beta-D-Glucan is associated with immune activation during HIV infection. Clin Infect Dis 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ramendra R, Isnard S, Mehraj V, et al. Circulating LPS and (1→3)-β-D-Glucan: A Folie à Deux Contributing to HIV-Associated Immune Activation. Front Immunol 2019;10. 10.3389/fimmu.2019.00465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Younas M, Psomas C, Mehraj V, et al. Plasma level of soluble ST2 in chronically infected HIV-1 patients with suppressed viremia. Open AIDS J 2017;11:32–5. 10.2174/1874613601711010032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Ortiz AM, Flynn JK, DiNapoli SR, et al. Experimental microbial dysbiosis does not promote disease progression in SIV-infected macaques. Nat Med 2018;24:1313–6. 10.1038/s41591-018-0132-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mehraj V, Ramendra R, Isnard S, et al. Cxcl13 as a biomarker of immune activation during early and chronic HIV infection. Front Immunol 2019;10:289. 10.3389/fimmu.2019.00289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Mehraj V, Ramendra R, Isnard S, et al. Circulating (1→3)-β-D-glucan Is Associated With Immune Activation During Human Immunodeficiency Virus Infection. Clin Infect Dis 2020;70:232–41. 10.1093/cid/ciz212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Vandergeeten C, Fromentin R, Merlini E, et al. Cross-Clade ultrasensitive PCR-based assays to measure HIV persistence in large-cohort studies. J Virol 2014;88:12385–96. 10.1128/JVI.00609-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Procopio FA, Fromentin R, Kulpa DA, et al. A novel assay to measure the magnitude of the inducible viral reservoir in HIV-infected individuals. EBioMedicine 2015;2:874–83. 10.1016/j.ebiom.2015.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Shacklett BL, Critchfield JW, Ferre AL, et al. Mucosal T-cell responses to HIV: responding at the front lines. J Intern Med 2009;265:58–66. 10.1111/j.1365-2796.2008.02042.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Planas D, Pagliuzza A, Ponte R, et al. LILAC pilot study: effects of metformin on mTOR activation and HIV reservoir persistence during antiretroviral therapy. EBioMedicine 2021;65:103270. 10.1016/j.ebiom.2021.103270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Vujkovic-Cvijin I, Sortino O, Verheij E. Colonic microbiota is altered in treated HIV infection independently of sexual practice and correlates with HIV disease progression. Internation Workshop on Microbiome in HIV 2019;14. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


