Abstract
The posterior cruciate ligament (PCL) is the primary stabilizer to posterior tibial translation of the knee. PCL injuries classically occur as the result of a posteriorly directed force against the anterior part of the tibia. They frequently occur as multiligament injuries or with concomitant cartilage or meniscal injuries. The posterior drawer test is highly sensitive and specific for PCL injuries. Posterior stress radiography is critical for objective assessment of posterior tibial translation and grading of PCL injuries. Grade I and II injuries may be treated nonoperatively, but in general isolated grade III injuries and multiligament injuries require surgical intervention due to the inevitable development of osteoarthritis. Anatomical and biomechanical studies have led to the development of an anatomic double-bundle reconstruction, which has been reported in clinical outcome studies to result in better functional and objective outcomes than single-bundle reconstructions. This article focuses on the clinically and surgically relevant anatomy and biomechanics of the PCL, diagnosis and treatment of PCL injuries, and a description of the anatomic double-bundle PCL reconstruction technique.
Key Words: Posterior Cruciate Ligament, Reconstruction, Meniscus Root
Introduction
The posterior cruciate ligament (PCL) is a large intraarticular, extrasynovial knee ligament. It functions to resist against posterior translation of the tibia in relation to the femur, as well as to provide rotational stability beyond 90o of knee flexion. Isolated PCL injuries occur less frequently than tears in combination with other ligament tears (combined PCL injuries), or with concomitant meniscal or chondral injuries. PCL injuries are common in sports and motor vehicle accidents (MVA), with reported incidences of combined PCL injuries of 58.5% with sports injuries and 71.7% in MVAs (1). Treatment decisions for PCL injuries are often made based on the grade of injury, chronicity, activity levels of patients, and symptoms, such as pain and instability. Typically, grade I and II isolated PCL injuries are treated nonoperatively, whereas most isolated grade III and combined PCL injuries require surgical reconstruction.
PCL deficiency alters the kinematics of the knee, especially by causing increased loads on the medial and patellofemoral compartments, which may be responsible for the increased incidence of articular cartilage degeneration in those compartments (2, 3). In patients with chronic PCL tears, the medial femoral condyle is anteriorly displaced throughout all ranges of motion in relation to the medial tibial plateau (3). This displacement affects load distribution in the medial compartment and helps explain the increased incidence of medial compartment cartilage degeneration in PCL deficient knees. After 5 years of PCL deficiency, the incidence of articular cartilage degeneration is reported to be 77.8% of the medial femoral condyle, and 46.7% of the patella (3, 4). Therefore, surgical reconstruction is recommended in patients with grade III PCL deficiency to restore native knee kinematics and improve patient outcomes. While historically the outcomes of PCL reconstructions were less than optimal with frequent recurrence of knee joint laxity, recent in-depth surgically relevant anatomic and biomechanical studies have helped to turn the corner and lead to better subjective and objective outcomes for PCL reconstruction [Table 1].
Table 1.
Key Points – Effects of Posterior Cruciate Ligament (PCL) Deficiency on the Knee Joint
| The medial and patellofemoral joint compartments have increased compression forces |
| The medial tibial plateau is posteriorly subluxed at all flexion angles |
| The PCL has intrinsic healing ability, but can often heal in a lax position, leading to altered knee kinematics over time |
| PCL deficiency can lead to progressive degeneration of the articular cartilage of the medial femoral condyle and patella |
Recently, anatomical and biomechanical studies have improved our understanding of the PCL and the effects of PCL injury on knee kinematics. These studies have also
provided guidance for more anatomical methods of PCL
reconstructions, with outcomes now being noted to be comparable to outcomes in anterior cruciate ligament (ACL) reconstruction. The purpose of this article is to review the current concepts of posterior cruciate ligament anatomy, biomechanics, diagnosis, treatment options, surgical technique, and clinical outcomes where surgical treatment of PCL tears has been validated to have improved outcomes.
Anatomy
The PCL is composed of two bundles, the larger anterolateral bundle (ALB), and the smaller posteromedial bundle (PMB). The femoral and tibial attachments of the PCL are approximately three times larger than the midsubstance cross-sectional area (5). Attempts to quantify and describe the femoral and tibial attachment areas of the ALB and PMB have been conducted with the purpose of improving tunnel placement during double-bundle PCL reconstruction (DB PCLR) (6).
The femoral attachments of the ALB, which lies on the roof, and PMB, which lies along the medial wall, have been described in relationship to arthroscopically pertinent bony landmarks of the intercondylar notch. The proximal borders of the ALB and PMB lie along the medial intercondylar ridge, and the separation between the two bundles is identified as a structure along the intercondylar ridge termed the medial bifurcate prominence. The ALB femoral attachment distal border lies almost at the articular cartilage margin (noted to be “distal” biomechanically), at a mean of 1.5 mm proximal to the articular cartilage margin. Along this cartilage border, the lateral and medial margins of the ALB lie at the trochlear point and the medial arch point, respectively. The ALB femoral center is a mean of 7.4 mm from the trochlear point and 11.0 mm from the medial arch point. The PMB femoral center is located a mean of 11.1 mm from the medial arch point, 10.8 mm from the posterior point, and 8.6 mm proximal to the articular cartilage margin. The mean distance between the ALB and PMB centers is 12.1 mm (6). Using this data to guide the placement of the femoral tunnels during PCL reconstruction, it is recommended that the ALB tunnel be triangulated using the trochlear point, medial arch point, and medial bifurcate prominence. The distal edge should be placed directly adjacent to the articular cartilage. The PMB should be placed just distal to the medial intercondylar ridge, equidistance between the posterior point and the medial arch point, and 8.6 mm proximal to the articular cartilage margin (6).
The tibial attachment of the PCL is much more compact and centered along the bundle ridge. The PMB envelops the ALB attachment on its posteromedial aspect, and the functional centers of each bundle are only a mean of 8.9 mm apart (6). Based on these considerations, it is recommended that a single tunnel be used to replicate the tibial attachment of the PCL center. Placement of the tibial tunnel too anteriorly risks injury to the posterior root of the medial meniscus (7), and too posteriorly risks injury to neurovascular structures. LaPrade et al reported that drilling of the tibial tunnel in the anatomic center of the ALB, 5 mm anterior to the overall tibial center, resulted in decreased ultimate failure strength and attachment area of the posterior root attachment of the medial meniscus (8). The overall tibial center of the PCL, and recommended tunnel posterior exit point, is just anterosuperior to the bundle ridge, which consistently marks the border between the ALB and PMB attachments. The overall PCL center is a mean of 9.8 mm medial to the lateral cartilage point, 7.8 mm posterior to the shiny white fiber point, and 5.0 mm lateral to the medial groove (6). [Figure 1 and 2] illustrate the anatomy of the posterior cruciate ligament, its individual bundles, and other associated structures of the knee. [Table 2] indicates the key arthroscopically relevant anatomical landmarks of the posterior cruciate ligament bundle attachments (6).
Figure 1.
Posterior view of a dissected cadaveric knee showing the anatomy of the posterior cruciate ligament and associated structures. MFC – medial femoral condyle; LFC – lateral femoral condyle; MM – medial meniscus; LM – lateral meniscus; pMFL – posterior meniscofemoral ligament; ALB – anterolateral bundle; PMB – posteromedial bundle; CGD – champagne-glass drop-off
Figure 2.
Hemisected distal femur visualizing the anterolateral bundle (ALB) on the intercondylar roof and posteromedial bundle (PMB) on the intercondylar wall of the medial femoral condyle (MFC). LM – lateral meniscus
Table 2.
Surgically relevant landmarks of the posterior cruciate ligament ALB and PMB attachment areas
| Femoral PCL attachment landmarks | |
|---|---|
| Trochlear point | Along the articular cartilage border, medial to the most distal aspect of the trochlear groove, the articular cartilage makes a distinct turn medially |
| Medial arch point | Continuing along the articular cartilage border from the trochlear point, the articular cartilage is curved until the medial arch point, where it abruptly turns and continues directly posteriorly |
| Medial intercondylar ridge | Consistently marks the proximal border of both the ALB and the PMB |
| Tibial PCL attachment landmarks | |
| Bundle ridge | Lies between the ALB and PMB tibial attachment sites |
| Shiny white fiber point | Shiny white fibers of the posterior horn of the medial meniscus are a mean of 7.8 mm anterior to the whole PCL tibial attachment center |
PCL – posterior cruciate ligament; ALB – anterolateral bundle; PMB – posteromedial bundle
The anterior and posterior meniscofemoral ligaments are part of the PCL complex. At least one of these ligaments is present in up to 95% of knees, and both ligaments are present in up to 60% of knees (6). These ligaments stabilize the lateral meniscus, which redistributes forces in the lateral compartment during loading and range of motion (ROM) (9). Additionally, the posterior oblique ligament and the posteromedial capsule are secondary stabilizers to posterior tibial translation in PCL deficient knees (10).
Accurate radiographic measurements of the PCL and its bundle centers can assist in correct anatomic placement of femoral and tibial tunnels during surgical reconstruction (11, 12). On lateral views of the femur, the anterior cortex line can be drawn perpendicular to the Blumensaat line, and the distal condyle line can be drawn perpendicular to the posterior cortex line of the femur. The ALB center is a mean of 17.4 mm posteroproximal to the anterior cortex line, 4.7 mm posteroinferior to the Blumensaat line, and 14.1 mm proximal to the distal condyle line (12). The PMB center is a mean of 23.9 mm posteroproximal to the anterior cortex line, 10.7 mm posteroinferior to the Blumensaat line, and 15.8 mm proximal to the distal condyle line (12). These measurements can be used to verify proper tunnel placement on day-one postoperatively, which is consistent with the author’s practice.
On lateral views of the tibia, a reference line at the level of the champagne glass drop-off point (CGD line) should be drawn perpendicular to the long axis of the tibia. The PCL tibial attachment center is a reported mean 5.5 mm proximal to the CGD line (12), which is the most clinically important intraoperative radiographic measurement. A line drawn at a 45o angle to the long axis of the tibia through the PCL tibial attachment center is meant to represent the placement of the tibial guide pin during PCL reconstruction. This line should be a mean of 7.0 mm from the posterior cortex of the tibia (12). It is recommended that an intraoperative lateral view radiograph of the tibia be obtained at all times prior to reaming a tibial PCL reconstruction tunnel to ensure the tunnel is positioned correctly. A more detailed understanding of the arthroscopically and radiographically relevant anatomy of the PCL has the potential to improve anatomic double-bundle posterior cruciate ligament reconstruction (DB PCLR) (6, 11-13).
Biomechanics
The ALB and PMB function synergistically throughout knee motion to resist against posterior tibial translation (PTT) and internal/external rotation beyond 90o of flexion. Using human cadaveric knees and robotics to study kinematics, Kennedy et al found that a completely sectioned PCL displays a mean of 11.7 mm of increased posterior tibial translation at 90o of flexion compared to the intact knee, which is indicative of a grade III tear (14). When the ALB or PMB are sectioned in isolation, the increase in PTT at 90o of flexion is reported to be a mean of 2.6 mm and 0.9 mm, respectively compared to the intact PCL state (14). This demonstrates that each bundle has a codominant role in restricting PTT. Using similar methods, Wijdicks et al demonstrated that an anatomic DB PCLR had significantly less PTT at 90o of flexion than an anatomic SB PCLR (13). Additionally, there is increased internal and external rotation following anatomic SB PCLR compared to an intact PCL (13). [Figures 3 and 4] are graphical representations of these findings (13). In fact, the amount of PTT seen of 4-5 mm at 90o of flexion is very similar to what has been reported for SB PCLR in clinical studies (15). At flexion angles greater than 90o, there is a significant increase in internal rotation in a SB PCLR compared to a DB PCLR (13). These findings suggest that a SB PCLR is not sufficient at restoring knee kinematics and stability throughout all ranges of motion and support the use of an anatomic DB PCLR.
Figures 3 and 4.
Increases in posterior tibial translation and internal rotation at various flexion angles after complete sectioning of posterior cruciat Reproduced with permission from AJSM Vol. 41 Issue 12, pp. 2839–2848. e ligament (PCL), anatomic single-bundle PCL reconstruction, and anatomic double-bundle PCL reconstruction
It is clinically important to understand the relationship between posterior tibial slope, PTT stability, and PCL graft tension forces. As demonstrated in [Figure 5], Utzschneider et al described a method for calculating posterior tibial slope (16). First, decreased posterior tibial slope is associated with an increased risk of PCL injury (17). Studying cadaveric knees, Bernhardson et al reported that as posterior tibial slope increased, PCL graft forces decreased, exhibiting an inverse relationship (18). Increased posterior tibial slope reduces forces on the PCL by directing weightbearing forces anteriorly on the tibia throughout all ranges of motion. As the posterior tibial slope decreases, both the tendency of the tibia to shift posteriorly and the force in the PCL to prevent PTT necessarily increase. A decreased posterior tibial slope should be considered as a possible cause of graft failure in PCL reconstruction due to the resultant increase in graft forces (18). Thus, in chronic cases with medial compartment cartilage wear or in revision PCL reconstruction cases with a flat tibial slope, an opening wedge osteotomy may be considered as a first-stage or concurrent procedure to increase posterior tibial slope prior to PCL reconstruction (18).
Figure 5.

Sagittal XR of a right knee with 9o of posterior tibial slope
Diagnosis
Injury to the PCL is commonly caused by a posteriorly directed force on the anterior proximal tibia, as is seen in the classically described “dashboard injury” or after a fall on a flexed knee with the foot in plantar flexion (19, 20). PCL tears are common in sports injuries and road traffic accidents, often in combination with other injuries, especially with high energy mechanisms (1, 19, 20). Eliciting the mechanism of injury can be helpful in diagnosing PCL tears. Rubinstein et al found in a randomized, blinded control study that the accuracy of clinical evaluation for PCL injury diagnosis and grading was 96% and 81%, respectively (21).
The posterior drawer test is reported to be highly sensitive and specific for PCL tears, 90% and 99%, respectively (21, 22). When evaluating PCL laxity using the posterior drawer test, grade I laxity is defined as increased posterior tibial displacement compared to the uninjured side, with the anterior tibial aspect remaining anterior to the femoral condyles. In grade II PCL laxity, the anterior tibial aspect will displace posteriorly until it is flush with the femoral condyles. In grade III PCL laxity, the anterior tibial aspect will be subluxated posterior to the femoral condyles (21).
The posterior sag test is performed with the patient supine, with the hip and knee flexed to 90o and the leg being supported by the examiner. The test is positive if the proximal tibia sags or displaces posteriorly on the femur (20).
The quadriceps active test is performed with the patient supine, hip flexed to 45o, and knee flexed to 90o. With the foot stabilized, the patient is instructed to isometrically contract their quadriceps. If quadriceps activation causes anterior translation of the tibia, this is considered a positive sign. The quadriceps active test is reported to be 97% specific for an isolated chronic PCL injury (21).
In addition to the value of a thorough history and physical examination in detecting PCL tears, MRI and posterior stress radiographs have proven to be objectively reliable. MRI has been found to be up to 99% accurate in diagnosing acute PCL tears, when the diagnosis was verified arthroscopically (23). However, in the case of chronic PCL tears, healing of the ligament in continuity may result in significant posterior laxity with an apparently intact PCL. Servant et al found a mean accuracy of 57% in the diagnosis of a chronic PCL tear by experienced musculoskeletal radiologists (24). Recently, increased PTT in the medial compartment on MRI has been found to be an accurate tool for assessment of a chronic PCL tear or PCL graft tear on MRI. Posterior tibial translation in the medial compartment can be measured on MRI by comparing the posterior-most aspect of the medial femoral condyle with the posterior-most aspect of the medial tibial plateau, as demonstrated in [Figure 6]. Posteromedial tibial subluxation of 2.0 mm in cases of chronic PCL injury, and 3.6 mm in revision cases have a reported sensitivity of 80% and 92% for PCL insufficiency, respectively (25). The sensitivity of MRI for diagnosing chronic PCL tears and PCL graft failure is increased using this technique.
Figure 6.
MRI of medial compartment showing 3.3 mm of posteromedial tibial subluxation. The posterior-most aspect of the MFC is measured in relationship to the posterior-most aspect of the MTP. MFC – medial femoral condyle, MTP – medial tibial plateau
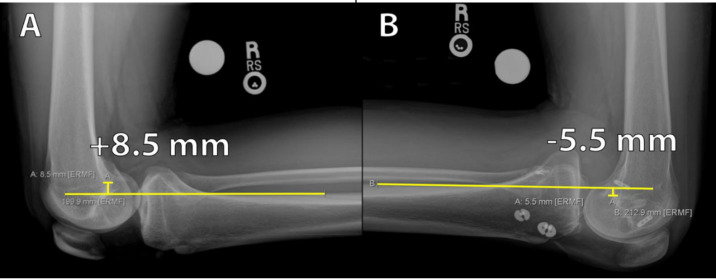
The kneeling technique of stress radiography has proven to be inexpensive and reliable in quantifying posterior knee laxity (26). With the knee flexed to 90o, the patient kneels on a padded support with the femoral condyles overhanging the edge of the support. The patient’s weight should be supported by the anterior aspect of the tibia, which applies posterior stress to the proximal tibia. Bilateral stress radiographs should be taken for side-to-side comparison. [Table 3] illustrates the grading of PCL insufficiency based on the side-to-side difference (in mm) of posterior tibial translation. [Figures 7 and 8] demonstrate the calculation of PTT using kneeling stress radiographs and a patient demonstrating the positioning for kneeling stress radiography, respectively.
Table 3.
Grading of PCL injuries based on the degree of posterior tibial translation as found on posterior drawer exam and kneeling stress radiograph measurement of side to side difference
| Grade | Clinical finding with posterior drawer exam | Kneeling stress radiograph measurement SSD |
| I | 0-5 mm PTT | 0-7 mm PTT |
| II | 5-10 mm PTT | ◊ |
| III | >10 mm PTT; MTP posterior to MFC; posterior sag | ◊ |
PCL – posterior cruciate ligament; SSD – side-to-side difference; PTT – posterior tibial translation; MTP – medial tibial plateau; MFC – medial femoral condyle
Figure 7.
Posterior tibial stress radiographs to measure PTT. Identify a point on the PTC about 15 cm distal to the joint line and draw a line parallel to the PTC. Perpendicular to this line, find the distance between the PTC and the posterior-most aspect of Blumensaat’s line. A SSD of 14.0 mm is shown above in a patient who also presented with a concomitant PLC injury. PTT – posterior tibial translation; PTC – posterior tibial cortex; SSD – side-to-side difference; PLC – posterolateral corner
Figure 9.
Arthroscopic images of the medial femoral condylar roof and wall in a right knee. Top left – trochlear point. Top right – medial arch point. Bottom left – ALB tunnel reamed and passing suture, acorn reamer in location of PMB tunnel. Bottom right – 2 mm bone bridge between ALB tunnel and PMB tunnel location
In acute injuries, pain and discomfort may restrict a patient’s ability to completely support their weight on the injured knee. In these instances, Holliday et al have described an alternative method termed “weighted gravity stress radiographs” which has the potential benefit of improved patient comfort (27).
PCL tears commonly occur with combined ligamentous and meniscal injures. Schlumberger et al studied a cohort of 1,000 patients with PCL tears and found that 63.3% presented with a combined injury (1). Injury to the posterolateral corner (PLC) can accentuate posterior tibial subluxation on clinical examination and radiographic stress testing, and therefore additional tests to exclude PLC injury is crucial to obtain an accurate diagnosis (28, 29). When the mechanism of injury is high-energy, and/or involves rotational or varus/valgus forces, further ligamentous injury is more likely (19). The integrity of all knee ligaments and menisci should be evaluated in the setting of a PCL injury. Accurate assessment of the grading of PCL injuries and chronicity are clinically important in determining the most efficacious course of treatment.
Surgical Reconstruction
Double bundle PCL reconstruction technique
Surgical reconstruction is indicated in isolated symptomatic grade III PCL injuries and combined PCL injuries to restore stability and function to improve patient outcomes. Under anesthesia, the diagnosis should be confirmed and the normal amount of tibiofemoral step-off at 90o of flexion of the contralateral normal knee should be determined to guide later tibiofemoral positioning during graft fixation (11). The author’s preferred reconstruction technique utilizes allografts, with an Achilles tendon allograft for the ALB and semitendinosus (ST) or tibialis anterior (TA) allograft for the PMB. The Achilles tendon ALB graft should be 11 mm in diameter with a 25 mm long calcaneal bone plug. The distal soft tissue of the graft should be tubularized with a number-2 nonabsorbable suture. Similarly, the ST/TA PMB graft should be prepared to be 7 mm in diameter, tubularizing each end of the graft (11).
If allografts are not available for use, Ponzo et al have published a technique for an autograft anatomic DB PCLR (30). Recently, a systematic review by Ansari et al reported that there were no significant differences in functional outcomes for autograft versus allograft in PCL reconstruction (31). For the ALB, a quadriceps tendon autograft is harvested from a 12- to 15-cm vertical incision over the quadriceps to about the mid-patella. A 20 x 11-mm diameter bone plug is harvested from the patella, and the graft should be at least 10 cm long and nearly full thickness (30). For the PMB, a semitendinosus tendon is harvested from an incision made over the proximal anteromedial tibia, about 6 cm distal to the joint line. The pes anserinus tendons are dissected, and the ST tendon is surgically released from the tibia. Next, the end of the ST tendon is whipstitched, and the tendon is harvested up to the musculotendinous junction using an open hamstring harvester (30). To prepare the autografts, the distal soft tissue end of the quadriceps tendon is tubularized with number-5 nonabsorbable sutures. Both ends of the ST tendon are whipstitched with a number-5 nonabsorbable suture (30).
After diagnostic arthroscopy through anterolateral and anteromedial portals, the first surgical step involves identification of the PCL femoral attachments of the ALB and PMB and outlining them with an arthroscopic coagulator. The ALB tunnel should be placed as distal as possible, adjacent to the edge of the articular cartilage (11). The PMB center is a mean of 8.6 mm distal to the articular cartilage, and the tunnel should be placed slightly posterior to the ALB (6, 11). The diameters of the ALB and PMB tunnels should be 11 mm and 7 mm, respectively, and each closed socket tunnel should be reamed to a depth of 25 mm. A notch is made on the posteroinferior aspect of the PMB tunnel to facilitate later screw fixation because the bone is quite dense at this location. A bone bridge of 2 mm between the femoral tunnels should be maintained (11) [Figure 9]. shows arthroscopic images which demonstrate these pertinent anatomic landmarks of the medial femoral condyle and the appropriate locations for reaming of the femoral tunnels.
After passing sutures have been placed through each tunnel for future graft passage, the tibial tunnel placement should be identified. Due to the compact nature of the tibial PCL attachment, a single 12 mm tunnel is recommended. The anatomic center of the PCL tibial attachment is slightly proximal to the bundle ridge, 5.0 mm lateral to the medial groove, 9.8 mm medial to the lateral cartilage point, and 7.8 mm posterior to the shiny white fiber point (6). A tibial guide pin should be drilled entering the tibia approximately 6 cm distal to the joint line, in between the medial tibial border and anterior tibial crest (11). As shown in [Figure 10], the guide pin should exit posteriorly at the center of the PCL tibial attachment site. Radiographic or fluoroscopic confirmation of tibial guide pin placement should be performed intraoperatively. There should be approximately 7 mm between the guide pin and the champagne glass drop off on intraoperative lateral radiographs (11). Next, with a 12 mm acorn reamer under arthroscopic visualization, the tibial tunnel should be reamed to a depth of 60%. Reaming is completed by hand with a large curette positioned to protect the neurovascular structures as the reamer penetrates the posterior tibial cortex (11). A smoother or other passing device should be passed and cycled proximally up the tibial tunnel to prevent obstruction at the tibial tunnel aperture and unnecessary difficulty during graft passage.
Figure 10.
Lateral tibia radiograph taken with intraoperative C-arm. The guide pin should be approximately 7.0 mm from the posterior cortex, and it should be exiting the posterior tibial cortex at the PCL attachment site
Graft fixation
First, the PMB graft is passed into the femoral tunnel and fixed with a 7x20 mm bioabsorbable interference screw, positioned posteroinferiorly in the tunnel (11). The ALB bone plug, cortical side up, should then be passed into the femoral tunnel and anchored with a 7x20 mm titanium interference screw positioned anteriorly and superiorly in the tunnel (11).
Now fixed in the femoral tunnels, the grafts are passed through the transtibial tunnel and out of the anteromedial aspect of the tibia by placing the ends of the graft sutures through the end on the smoother or passing device and pulling them down the tibia. This graft passing technique has been proven to simplify PCL graft passage and takes 5-10 seconds. Kennedy et al have showed that fixation of the PMB at 0o and 15o of flexion and ALB fixation at 75o, 90o, and 105o resulted in significantly reduced PTT, but fixation of the PMB at 15o and the ALB at 75o resulted in significantly increased graft forces (32). It is therefore recommended that the
ALB be fixated at 90o of flexion, and then subsequently the PMB be fixated at 0o of flexion to reduce the risk of graft attenuation or failure (32).
SB vs DB PCL Reconstruction
Clinical outcome studies following SB vs DB PCL reconstruction can be difficult to compare based on differences in operative techniques, graft choices, graft fixation angles, tunnel placement, rehabilitation protocol, etc. In a systematic review of 441 patients at a minimum of 2 years follow up, Chahla et al reported improvements from baseline in subjective outcomes and knee stability in both SB an DB PCLR (33). Objective PTT measured with a Telos device was found to be significantly lower for the DB group than the SB group (33). This is in agreement with biomechanical findings that demonstrated an anatomic DB PCLR is superior to an SB PCLR for restoring native knee kinematics (13). [Table 4] highlights some pearls and pitfalls of anatomic double-bundle PCL reconstruction. Historically, PCLR outcomes have been worse than outcomes for isolated anterior cruciate ligament (ACL) reconstruction. In 2018, LaPrade et al showed that functional and objective outcomes after anatomic DB PCLR at a mean of 3 years follow-up were comparable with an isolated ACL reconstruction control cohort (34).
Table 4.
Pearls and Pitfalls of Anatomic Double-Bundle PCL Reconstruction
| Surgical Pearls | Surgical Pitfalls |
|---|---|
|
|
PCL – posterior cruciate ligament; ALB – anterolateral bundle; PMB – posterolateral bundle
Rehabilitation
Grade I and II isolated PCL injuries can usually be treated nonoperatively (22, 28). Isolated grade III PCL injuries require surgical reconstruction in most cases (35). Functional nonoperative and postoperative rehabilitation programs have been recommended by Pierce et al (36). Dynamic bracing is an important part of PCL rehabilitation. A dynamic force PCL brace (Rebound PCL brace, Össur Inc., Foothill Ranch, CA, USA) has been reported to apply a dynamically increasing anteriorly directed force as flexion angle increases, replicating the tensioning patterns of the native PCL (37). Jacobi et al found that the use of a dynamic (static force) anterior drawer brace reduces posterior sag from a mean of 7.1 mm initially to a mean of 2.3 mm after 12 months, and 3.2 mm after 24 months (38). The dynamic force PCL brace has been reported to be biomechanically superior to a static force brace, because it is capable of applying greater anterior forces than the static force brace at higher angles of flexion, when tension in the PCL is higher (37). These findings suggest that rehabilitation with a dynamic force PCL brace may improve clinical outcomes by helping to restore knee stability. Further studies should be done comparing clinical outcomes between static force and dynamic force PCL braces in the acute treatment of isolated grade I and II PCL injury.
General rehabilitation protocols, whether postoperative or after PCL injury, follow a similar set of guidelines. Initially, the main priority of treatment is protection of the healing ligament or graft. This is accomplished by using a dynamic force PCL brace, avoiding hyperextension, and preventing PTT by gravity or hamstrings contraction. Alternatively, using a knee immobilizer with a bolster to prevent PTT can be used to attempt to overcome the negative effect of gravity. The PCL brace is worn at all times, except during grooming and passive prone ROM exercises for up to the first 6 months postoperatively. Biomechanical studies have shown that sheer forces in the PCL are increased beyond 90o of flexion, so passive prone ROM is initially limited from 0-90o. Progressive mobility is important to recovery. Passive prone ROM exercises begin day one post-operatively or after injury. Immediately following PCLR, keeping the patient non-weightbearing is important to prevent straining the graft. During nonoperative rehabilitation, it is recommended that patients be partial weightbearing with crutches, and eventually wean off the crutches and progress to weight bearing once they can ambulate without a limp. Quadriceps activation and strengthening are a focus of early rehabilitation. Eventually, progressive strengthening of the lower limb musculature becomes a primary objective. Four months after injury, or 6 months post-operatively, the patient is objectively evaluated for graft/ligament healing with posterior stress radiographs. Then the patient can begin to wean out of the dynamic force PCL brace. Once the patient has demonstrated sufficient strength and stability, running can be reintroduced. When the patient is ready, sport-specific
agility and power exercises can begin. Once greater than 90% function on return-to-sport testing is achieved with good objective PCL stress radiographic results, and the patient is mentally prepared to return to sport, return to competition may be allowed.
Discussion
The treatment of PCL tears has been greatly advanced over the past decade. While in the past, PCLR often resulted in recurrent posterior laxity, which often resulted in surgeons abandoning PCLR or reporting that PCLR did not work well, outcomes similar to ACL reconstructions can now be expected when PCL tears are treated with an anatomic reconstruction, a dynamic PCL brace, and guided physical therapy protocols. It is now well understood that PCL deficiency leads to altered knee kinematics and instability, results in increased forces in the medial and patellofemoral compartments and is associated with an increased development of osteoarthritis (3, 4, 14, 28). Grade I and II PCL injuries have a probability to heal in the acute phase (within 6 weeks) if treated with functional rehabilitation and a dynamic force PCL brace to protect the healing ligament by keeping the tibia in a reduced position (36, 37). In the setting of chronic PCL instability, isolated grade III PCL injuries, or combined other ligamentous or meniscal injuries involving the PCL, surgery is indicated to restore knee stability and kinematics and to improve patient outcomes. To evaluate for indications for surgery, the posterior drawer clinical test is highly specific and sensitive to PCL injuries (21, 22). Posterior tibial stress radiographs are the gold standard for objective assessment of PCL laxity (26).
When surgery is indicated, it has been reported that double-bundle PCL reconstructions result in better objective IKDC (International Knee Documentation Committee) knee scores, with increased stability marked by increased resistance to PTT and rotation beyond 90o
of flexion when compared with single-bundle PCL reconstructions (33). Additionally, DB PCLR have been reported to be biomechanically superior to SB PCLR for stabilizing the knee to resist PTT and internal/external rotation beyond 90o of flexion, and for nearly achieving full restoration of native knee kinematics (13).
Intraoperatively, anatomic identification of the PCL attachments and placement of the femoral and tibial tunnels is critical. The use of an arthroscopic coagulator to outline the location of each bundle will ensure more accurate placement of the tunnels. When drilling the ALB femoral tunnel, the 11-mm reamer should be placed as distal as possible, adjacent to the articular cartilage of the roof of the medial femoral condyle, and the center of the tunnel should be 7.4 mm from trochlear point and 11.0 mm from the medial arch point (6, 11). The PMB femoral tunnel should be roughly 8.6 mm proximal to the articular cartilage margin, and equidistance between the medial arch point and the posterior point, along the wall of the notch (6). Notching the posteroinferior aspect of the PMB tunnel will facilitate screw fixation. Prior to drilling the single tibial tunnel, locate the shiny white fibers and the bundle ridge. The use of intraoperative radiographs or fluoroscopy help ensure that the guide pin is exiting the posterior tibial cortex at the crest of the bundle ridge while also ensuring there is approximately 7 mm between the pin and the champagne glass drop-off (11). The ALB graft should be fixated while the knee is flexed to 90o, with the tibia reduced, and distal traction applied to the graft to ensure proper graft tensioning. The PMB graft should be fixated next with the knee in full extension with distal traction applied to the graft (32).
Postoperatively, immediate immobilization and eventual bracing with a dynamic force PCL brace should be used to prevent graft attenuation or failure. Rehabilitation should focus on protection of the graft, quadriceps activation, and progressive weight-bearing (11, 36, 37). At 6 months post-op, posterior tibial stress radiographs should be performed to objectively assess graft healing, and to begin weaning out of the dynamic PCL brace. In the setting of grade 3 and combined PCL tears, double-bundle PCLR followed by functional rehabilitation, graft protection, and dynamic bracing has demonstrated outcomes comparable to ACL reconstruction (34).
Figure 8.
Patient demonstrating a posterior stress radiograph of the right knee. The patient is instructed to bear their full weight on the anterior aspect of the tibia with femoral condyles overhanging the padded support
Financial Disclosures:
None
References
- 1.Schlumberger M, Schuster P, Eichinger M, Mayer P, Mayr R, Immendörfer M, et al. Posterior cruciate ligament lesions are mainly present as combined lesions even in sports injuries. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(7):2091–8. doi: 10.1007/s00167-020-05919-4. [DOI] [PubMed] [Google Scholar]
- 2.Skyhar MJ, Warren RF, Ortiz GJ, Schwartz E, Otis JC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. JBJS. 1993;75(5):694–9. doi: 10.2106/00004623-199305000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Logan M, Williams A, Lavelle J, Gedroyc W, Freeman M. The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med. 2004;32(8):1915–22. doi: 10.1177/0363546504265005. [DOI] [PubMed] [Google Scholar]
- 4.Strobel MJ, Weiler A, Schulz MS, Russe K, Eichhorn HJ. Arthroscopic evaluation of articular cartilage lesions in posterior cruciate ligament—Deficient knees. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003;19(3):262–8. doi: 10.1053/jars.2003.50037. [DOI] [PubMed] [Google Scholar]
- 5.Harner CD, Baek GH, Vogrin TM, Carlin GJ, Kashiwaguchi S, Woo SL. Quantitative analysis of human cruciate ligament insertions. Arthroscopy the journal of arthroscopic related surgery : official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 1999;15(7):741–9. doi: 10.1016/s0749-8063(99)70006-x. [DOI] [PubMed] [Google Scholar]
- 6.Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically Pertinent Anatomy of the Anterolateral and Posteromedial Bundles of the Posterior Cruciate Ligament. JBJS. 2012;94(21):1936–45. doi: 10.2106/JBJS.K.01710. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy NI, Michalski MP, Engebretsen L, LaPrade RF. Iatrogenic Meniscus Posterior Root Injury Following Reconstruction of the Posterior Cruciate Ligament: A Report of Three Cases. JBJS Case Connector. 2014;4:1. doi: 10.2106/JBJS.CC.M.00175. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade CM, Smith SD, Rasmussen MT, Hamming MG, Wijdicks CA, Engebretsen L, et al. Consequences of Tibial Tunnel Reaming on the Meniscal Roots During Cruciate Ligament Reconstruction in a Cadaveric Model, Part 2: The Posterior Cruciate Ligament. The American Journal of Sports Medicine. 2014;43(1):207–12. doi: 10.1177/0363546514554771. [DOI] [PubMed] [Google Scholar]
- 9.Knapik DM, Salata MJ, Voos JE, Greis PE, Karns MR. Role of the Meniscofemoral Ligaments in the Stability of the Posterior Lateral Meniscus Root After Injury in the ACL-Deficient Knee. JBJS Reviews. 2020;8(1):e0071. doi: 10.2106/JBJS.RVW.19.00071. [DOI] [PubMed] [Google Scholar]
- 10.Petersen W, Loerch S, Schanz S, Raschke M, Zantop T. The Role of the Posterior Oblique Ligament in Controlling Posterior Tibial Translation in the Posterior Cruciate Ligament-Deficient Knee. The American Journal of Sports Medicine. 2008;36(3):495–501. doi: 10.1177/0363546507310077. [DOI] [PubMed] [Google Scholar]
- 11.Chahla J, von Bormann R, Engebretsen L, LaPrade RF. Anatomic posterior cruciate ligament reconstruction: State of the Art. oint Disorders & Orthopaedic Sports Medicine. 2016;1(5):292. [Google Scholar]
- 12.Johannsen AM, Anderson CJ, Wijdicks CA, Engebretsen L, LaPrade RF. Radiographic Landmarks for Tunnel Positioning in Posterior Cruciate Ligament Reconstructions. The American Journal of Sports Medicine. 2012;41(1):35–42. doi: 10.1177/0363546512465072. [DOI] [PubMed] [Google Scholar]
- 13.Wijdicks CA, Kennedy NI, Goldsmith MT, Devitt BM, Michalski MP, Årøen A, et al. Kinematic Analysis of the Posterior Cruciate Ligament, Part 2: A Comparison of Anatomic Single- Versus Double-Bundle Reconstruction. The American Journal of Sports Medicine. 2013;41(12):2839–48. doi: 10.1177/0363546513504384. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Årøen A, et al. Kinematic Analysis of the Posterior Cruciate Ligament, Part 1: The Individual and Collective Function of the Anterolateral and Posteromedial Bundles. The American Journal of Sports Medicine. 2013;41(12):2828–38. doi: 10.1177/0363546513504287. [DOI] [PubMed] [Google Scholar]
- 15.Kim SJ, Kim TE, Jo SB, Kung YP. Comparison of the clinical results of three posterior cruciate ligament reconstruction techniques. J Bone Joint Surg Am. 2009;91(11):2543–9. doi: 10.2106/JBJS.H.01819. [DOI] [PubMed] [Google Scholar]
- 16.Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, et al. Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surgery, Sports Traumatology, Arthroscopy. 2011;19(10):1643–8. doi: 10.1007/s00167-011-1414-3. [DOI] [PubMed] [Google Scholar]
- 17.Bernhardson A, DePhillipo N, Daney B, Kennedy M, Aman Z, LaPrade R. Posterior Tibial Slope and Risk of Posterior Cruciate Ligament Injury. The American Journal of Sports Medicine. 2019;47:036354651881917. doi: 10.1177/0363546518819176. [DOI] [PubMed] [Google Scholar]
- 18.Bernhardson AS, Aman ZS, DePhillipo NN, Dornan GJ, Storaci HW, Brady AW, et al. Tibial Slope and Its Effect on Graft Force in Posterior Cruciate Ligament Reconstructions. The American Journal of Sports Medicine. 2019;47(5):1168–74. doi: 10.1177/0363546519827958. [DOI] [PubMed] [Google Scholar]
- 19.Owesen C, Sandven-Thrane S, Lind M, Forssblad M, Granan L-P, Årøen A. Epidemiology of surgically treated posterior cruciate ligament injuries in Scandinavia. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(8):2384–91. doi: 10.1007/s00167-015-3786-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verhulst FV, MacDonald P. Diagnosing PCL Injuries: History, Physical Examination, Imaging Studies, Arthroscopic Evaluation. Sports Medicine and Arthroscopy Review. 2020;28(1):2–7. doi: 10.1097/JSA.0000000000000251. [DOI] [PubMed] [Google Scholar]
- 21.Rubinstein RA, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The Accuracy of the Clinical Examination in the Setting of Posterior Cruciate Ligament Injuries. The American Journal of Sports Medicine. 1994;22(4):550–7. doi: 10.1177/036354659402200419. [DOI] [PubMed] [Google Scholar]
- 22.Feltham GT, Albright JP. The diagnosis of PCL injury: literature review and introduction of two novel tests. Iowa Orthop J. 2001;21:36–42. [PMC free article] [PubMed] [Google Scholar]
- 23.Fischer SP, Fox JM, Del Pizzo W, Friedman MJ, Snyder SJ, Ferkel RD. Accuracy of diagnoses from magnetic resonance imaging of the knee A multi-center analysis of one thousand and fourteen patients. J Bone Joint Surg Am. 1991;73(1):2–10. [PubMed] [Google Scholar]
- 24.Servant CTJ, Ramos JP, Thomas NP. The accuracy of magnetic resonance imaging in diagnosing chronic posterior cruciate ligament injury. The Knee. 2004;11(4):265–70. doi: 10.1016/j.knee.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 25.DePhillipo NN, Cinque ME, Godin JA, Moatshe G, Chahla J, LaPrade RF. Posterior Tibial Translation Measurements on Magnetic Resonance Imaging Improve Diagnostic Sensitivity for Chronic Posterior Cruciate Ligament Injuries and Graft Tears. The American Journal of Sports Medicine. 2017;46(2):341–7. doi: 10.1177/0363546517734201. [DOI] [PubMed] [Google Scholar]
- 26.Jackman T, LaPrade RF, Pontinen T, Lender PA. Intraobserver and Interobserver Reliability of the Kneeling Technique of Stress Radiography for the Evaluation of Posterior Knee Laxity. The American Journal of Sports Medicine. 2008;36(8):1571–6. doi: 10.1177/0363546508315897. [DOI] [PubMed] [Google Scholar]
- 27.Holliday CL, Martin R, Grant JA. Comparing the Efficacy of Kneeling Stress Radiographs and Weighted Gravity Stress Radiographs to Assess Posterior Cruciate Ligament Insufficiency. The American Journal of Sports Medicine. 2021;49(4):1017–22. doi: 10.1177/0363546520988114. [DOI] [PubMed] [Google Scholar]
- 28.Bedi A, Musahl V, Cowan JB. Management of Posterior Cruciate Ligament Injuries: An Evidence-Based Review. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2016;24(5):277–89. doi: 10.5435/JAAOS-D-14-00326. [DOI] [PubMed] [Google Scholar]
- 29.Margheritini F, Mancini L, Mauro CS, Mariani PP. Stress radiography for quantifying posterior cruciate ligament deficiency. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003;19(7):706–11. doi: 10.1016/s0749-8063(03)00399-2. [DOI] [PubMed] [Google Scholar]
- 30.Ponzo N, Del Castillo J, Fregeiro J, Kennedy MI, LaPrade RF. Autograft Anatomic, Double-Bundle Posterior Cruciate Ligament Reconstruction. Arthrosc Tech. 2018;7(9):e957–e62. doi: 10.1016/j.eats.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ansari AS, Dennis BB, Horner NS, Zhu M, Brookes C, Khan M, et al. Influence of Graft Source on Postoperative Activity and Joint Laxity in Posterior Cruciate Ligament Reconstruction: A Systematic Review. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2019;35(1):262–74. doi: 10.1016/j.arthro.2018.07.027. [DOI] [PubMed] [Google Scholar]
- 32.Kennedy NI, LaPrade RF, Goldsmith MT, Faucett SC, Rasmussen MT, Coatney GA, et al. Posterior Cruciate Ligament Graft Fixation Angles, Part 2: Biomechanical Evaluation for Anatomic Double-Bundle Reconstruction. The American Journal of Sports Medicine. 2014;42(10):2346–55. doi: 10.1177/0363546514541226. [DOI] [PubMed] [Google Scholar]
- 33.Chahla J, Moatshe G, Cinque ME, Dornan GJ, Mitchell JJ, Ridley TJ, et al. Single-Bundle and Double-Bundle Posterior Cruciate Ligament Reconstructions: A Systematic Review and Meta-analysis of 441 Patients at a Minimum 2 Years' Follow-up. Arthroscopy. 2017;33(11):2066–80. doi: 10.1016/j.arthro.2017.06.049. [DOI] [PubMed] [Google Scholar]
- 34.LaPrade RF, Cinque ME, Dornan GJ, DePhillipo NN, Geeslin AG, Moatshe G, et al. Double-Bundle Posterior Cruciate Ligament Reconstruction in 100 Patients at a Mean 3 Years’ Follow-up: Outcomes Were Comparable to Anterior Cruciate Ligament Reconstructions. The American Journal of Sports Medicine. 2018;46(8):1809–18. doi: 10.1177/0363546517750855. [DOI] [PubMed] [Google Scholar]
- 35.Ittivej K, Prompaet S, Rojanasthien S. Factors influencing the treatment of posterior cruciate ligament injury. J Med Assoc Thai. 2005;88 Suppl 5:S84–8. [PubMed] [Google Scholar]
- 36.Pierce CM, O'Brien L, Griffin LW, Laprade RF. Posterior cruciate ligament tears: functional and postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21(5):1071–84. doi: 10.1007/s00167-012-1970-1. [DOI] [PubMed] [Google Scholar]
- 37.LaPrade R, Smith S, Wilson K, Wijdicks C. Quantification of functional brace forces for posterior cruciate ligament injuries on the knee joint: an in vivo investigation. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2014:23. doi: 10.1007/s00167-014-3238-4. [DOI] [PubMed] [Google Scholar]
- 38.Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace. The Journal of Bone and Joint Surgery British volume. 2010;92-B(10):1381–4. doi: 10.1302/0301-620X.92B10.24807. [DOI] [PubMed] [Google Scholar]