Abstract
Orbital myositis in systemic lupus erythematosus (SLE) is a rare entity with risk of serious complications. Timely treatment with effective immunosuppressors is desirable.
We report a case of a 32-year-old female patient with SLE who presented with an acute ocular pain and extraorbital muscle thickening, consistent with orbital myositis.
Association with SLE was made after exclusion of other aetiologies. Due to refractoriness to steroids, off-label rituximab was initiated with clinical and imaging parameter improvement.
LEARNING POINTS
Orbital myositis is a rare entity that can be present in some autoimmune diseases or mimic other common ocular conditions, such as orbital cellulitis or thyroid orbitopathy.
In SLE, it may be the form of presentation of the disease or the only manifestation of active disease, even without elevation of inflammatory biomarkers.
Generally, patients with orbital myositis have an excellent response to high-dose corticosteroid therapy, but the risk of recurrence or refractoriness is not negligible.
Keywords: Orbital myositis, systemic lupus erythematosus, corticosteroid, rituximab
CASE DESCRIPTION
A 32-year-old Caucasian female sought the emergency department because of acute monocular pain.
She had a history of psoriasis and a 7-year-old systemic lupus erythematosus (SLE). This diagnosis was based on clinical – malar rash and arthritis, and immunological – positive antinuclear antibodies, high anti-dsDNA, low C3 serum levels and positive IgG anti-cardiolipin/IgG anti-β2-glycoprotein criteria. The patient had no past history of thrombosis. The Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) was 4 due to moderate arthritis. She was on standard of care therapy and steroids (dose equivalent to 10 mg of prednisolone).
She referred an acute and increasing right orbital pain accompained by diplopia and marked lid swelling. There was no history of trauma or infection. A full ophthalmic examination excluded proptosis, ptosis, changes in the anterior chamber and vitreous as well as retinal and optic nerve dysfunction. Visual acuity was preserved. Computed tomography (CT) and magnetic resonance imaging (MRI) of the orbits revealed thickening of the right medial, lateral and inferior rectus muscles and soft tissues in the right periorbital region (Figs. 1A and 1B).
Figure 1.
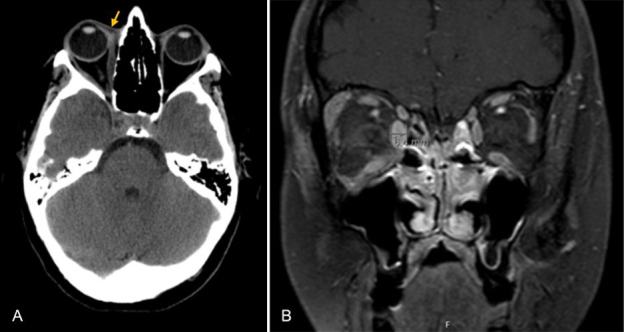
CT scan (A) and MRI of the orbit (B) showing thickening of the right medial, lateral and inferior rectus muscles and soft tissues in the right periorbital region (depicted by yellow arrow)
The blood cell count and biochemical analysis were within the normal ranges. The erythrocyte sedimentation rate was similar to previous determinations. No immunological activity of SLE was identified. All the thyroid hormone and antibody tests were normal (Table 1). No other signs suggestive of systemic diseases (sarcoidosis, vasculitis) or neoplasms were found.
Table 1.
Biochemical work-up values
| Laboratory parameter | Value | Reference range |
|---|---|---|
| Haemoglobin | 14.4 g/dl | 12.0–16.0 g/dl |
| Leucocytes | 8.24×10 3 /μl | 4.00–11.00×10 3 /μl |
| Erythrocyte sedimentation rate | 28 mm | 0–19 mm |
| Anti-dsDNA | 2.4 IU/ml | <15 U/ml |
| C3 | 150.8 mg/dl | 81–167 mg/dl |
| C4 | 30.8 mg/dl | 11–42 mg/dl |
| Thyroid stimulating hormone | 2.31 pIU/ml | 0.30–3.94 pIU/ml |
| Thyrotropin receptor antibodies | 0.49 U/l | <1.22 U/l |
| Thyroid peroxidase | 10.2 IU/ml | <34 IU/ml |
| Anti-thyroglobulin antibodies | <10 IU/ml | <115 IU/ml |
| Creatinine | 0.6 mg/dl | 0.5–0.9 mg/dl |
| Calcium | 2.30 mmol/l | 2.15–2.50 mmol/l |
Given the absence of a diagnosis, an eyelid and medial rectus biopsy was performed, showing an inflammatory infiltrate (predominance of lymphoplasmacytic cells without atypia) with perivascular and periadnexal distribution, without findings suggesting vasculitis, lymphoproliferative disease or IgG4-related disease (IgG4+/IgG+ was less than 5%). A diagnosis of exclusion, periorbital myositis due to SLE, was made.
A high dose of oral prednisolone was started (60 mg per day), without clinical or imaging response. Given the extension of the disease and the risk of amaurosis, off-label therapy with rituximab was initiated – after the first treatment cycle there was clinical improvement (resolution of pain and oedema, with residual diplopia in extreme dextroversion) and the follow-up CT scan showed a decrease in muscle thickening (Fig. 2).
Figure 2.
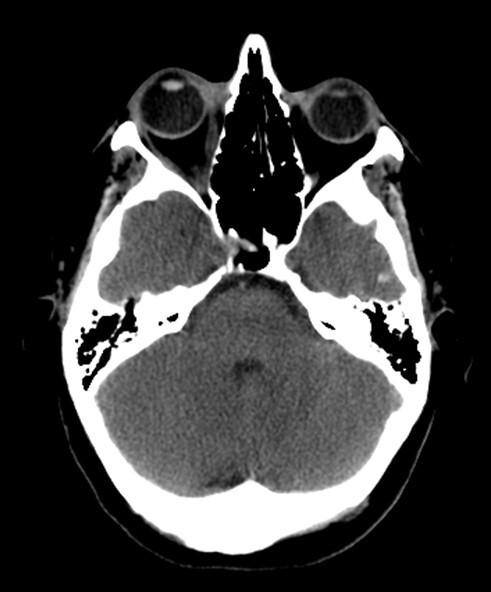
CT scan axial view of orbits showing a decrease in thickening of the right medial rectus muscle
DISCUSSION
SLE as a connective tissue disorder can affect multiple organ systems, including any eye structures. Ocular manifestations may develop in at least one-third of patients with SLE, with significant associated morbidity. The most frequent manifestations are keratoconjunctivitis sicca or ocular complications secondary to systemic therapy used, such as maculopathy in the context of hydroxychloroquine toxicity and cataracts or glaucoma resulting from corticosteroid therapy [1, 2].
Orbital myositis in SLE is an entity rarely described in the literature. To our knowledge, only 7 cases have been reported [3]. It is characterized by inflammation of the extraocular muscles with risk of developing amaurosis [2, 4]. Clinical manifestations are similar in all reported cases – unilateral or bilateral ocular pain, oedema, diplopia and limitation in extraocular movement [3].
Diagnosis is challenging, as clinical manifestations are nonspecific and mimic other (more common) entities, which should be excluded. It is important to exclude infectious causes (orbital cellulitis usually presents with fever, elevation of inflammatory parameters, history of trauma or an extension of other head and neck infections), endocrinological causes (Graves’ ophthalmopathy, easily ruled out with thyroid antibody testing and thyroid function tests), infiltrative (sarcoidosis) and neoplastic causes (for example, lymphoma, uveal melanoma) [3].
Orbital myositis is not a specific finding of SLE. It may be present in other autoimmune diseases such as rheumatoid arthritis, inflammatory myopathies or vasculitis. The pathological basis is not fully understood, but most evidence implicates an immune-mediated process [5].
Orbital myositis can be the first or the solitary manifestation of SLE. In the case reported, the patient had no involvement of other organs, neither elevation of inflammatory or immunologic markers, similar to the description of other case reports. Although the risk of serious complications is low, progression to ocular ischaemia and subsequent amaurosis can occur. A biopsy for histological confirmation is essential, but it should not delay treatment [3, 5].
High doses of systemic corticosteroid is the first choice for the treatment of orbital myositis leading usually to a quick clinical improvement, although recurrences have been documented [5].
To our knowledge this is the first case report of corticosteroid-unresponsive orbital myositis. Given the proven efficacy of rituximab in cases of refractory orbital myositis and, as it is the most used off-label drug in SLE, it was our choice for the treatment in the case reported.
The authors emphasize the importance of maintaining a high level of suspicion so that a timely diagnosis and treatment can be established.
Footnotes
Conflicts of Interests: The authors declare there are no competing interests.
REFERENCES
- 1.Serop S, Vianna RNG, Claeys M, De Laey JJ. Orbital myositis secondary to systemic lupus erythematosus. Acta Ophthalmol. 1994;72(4):520–523. doi: 10.1111/j.1755-3768.1994.tb02807.x. [DOI] [PubMed] [Google Scholar]
- 2.Silpa-archa S, Lee JJ, Foster CS. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2016;100:135–141. doi: 10.1136/bjophthalmol-2015-306629. [DOI] [PubMed] [Google Scholar]
- 3.Chan AJ, Rai AS, Lake S. Orbital myositis in systemic lupus erythematosus: a case report and literature review. Eur J Rheumatol. 2020;7(3):135–137. doi: 10.5152/eurjrheum.2020.19217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palejwala NV, Walia HS, Yeh S. Ocular manifestations of systemic lupus erythematosus: a review of the literature. Autoimmune Dis. 2012;2012:290898. doi: 10.1155/2012/290898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Espinoza GM. Orbital inflammatory pseudotumors: etiology, differential diagnosis, and management. Curr Rheumatol Rep. 2010;12:443–447. doi: 10.1007/s11926-010-0128-8. [DOI] [PubMed] [Google Scholar]


