Abstract
Background
Major efforts are being made to control the spread and impacts of the coronavirus pandemic using vaccines. Ethiopia began on March 13, 2021, to vaccinate healthcare workers (HCWs) for COVID-19 with the AstraZeneca vaccine. However, willingness to be vaccinated depends to a large extent on factors beyond the availability of vaccines. This study aimed to determine the rate of intention to refuse COVID-19 vaccination and associated factors among HCWs in northeastern Ethiopia. northeastern, Ethiopia.
Method
An institution-based cross-sectional study was employed among 404 HCWs in Dessie City, northeastern Ethiopia in May, 2021. Data were collected, checked, coded, entered into EpiData Version 4.6 and exported to Statistical Package of Social Sciences (SPSS) Version 25.0 for cleaning and analysis. The dependent variable was refuse to receive COVID-19 vaccination and the independent variables included socio-demographic factors, knowledge, attitudes and perceptions. A Binary logistic regression model was used to determine the association between vaccine refusal and the independent variables. From bivariate analysis, variables with p-values < 0.25 were retained for multivariable analysis. From multivariable analysis, variables with adjusted odds ratio (AOR), p-values <0.05 at 95% confidence interval (CI) were declared as factors significantly associated with refusal to be vaccinated among HCWs in Dessie City, northeastern Ethiopia.
Results
The proportion of HCWs with overall good knowledge, good perception, and positive attitudes about COVID-19 vaccination were 62.5%, 60.5%, and 52.3%, respectively; 64.0% of the HCWs wanted to be vaccinated while 36.0% said that they would refuse to do so. Multivariable analysis identified negative attitudes (AOR: 3.057; 95%CI [1.860 - 5.026]) and poor perceptions (AOR: 4.73; 95%CI [2.911 - 7.684]) about COVID-19 vaccines were significantly associated with refusal to be vaccinated for COVID-19. Nearly half (46.9%) of the HCWs stated that vaccines could worsen any pre-existing medical conditions and 39.5% of them thought that vaccines could cause COVID-19 infections.
Conclusion
The willingness of HCWs to get vaccinated against COVID-19 was relatively high among HCWs. Negative attitudes and poor perceptions towards the anticipated COVID-19 vaccination were significant factors to refuse to be vaccinated. Our findings may provide information for the management authorities and stakeholders to promote and improve attitudes, knowledge and perceptions towards COVID-19 vaccination uptake among HCWs.
Keywords: attitudes, COVID-19 vaccine, healthcare workers, knowledge, perceptions, vaccine refusal, Ethiopia
Background
COVID-19 infection rates are accelerating in Africa, including in Ethiopia. By October 24, 2021, Ethiopia had reported 362,088 COVID-19 cases and 6,347 deaths [1]. Many countries, including Ethiopia have implemented various strategies to control COVID-19, including declaring a state of emergency, issuing restrictions on mass gathering, enforcing stay-at-home orders, and promoting the use of personal protective equipment [2]. As part of the worldwide strategy, efforts have been made to develop and distribute vaccines. The COVAX program, backed by the World Health Organization (WHO) and other multilateral bodies, aims to supply 600 million doses to Africa, enough to vaccinate at least 20% of the population. However, by April 2021, only 18 million doses, representing 2% of all vaccine doses administered globally, had been administered by 41 African countries [3]. An additional 400 million doses of the Johnson & Johnson vaccine are scheduled to be shipped to the African Union starting in the third quarter of 2021 [4]. The first large shipment (2.2 million doses) of the AstraZeneca vaccine was received by Ethiopia in early March 2021 through the COVAX program. The country expected to receive an additional 5.4 million doses by May 2021 [5]. In addition, the African Vaccine Acquisition Trust (AVAT) announced the first monthly shipment of 108,000 doses of Johnson & Johnson vaccine to Ethiopia [6]. By April 2021, Ethiopia had administered only 430,000 doses of COVID vaccines, covering 0.2% of the country’s population with 2-shot vaccinations [7], but expected to cover 20% of the population by the end of 2021 [5, 8]. As of October 26, 2021, while more than 3.84 billion people worldwide had received one dose of a COVID-19 vaccine (equal to about 50% of the world population), 24 African countries had vaccinated less than 3% of their populations and only 0.9% of Ethiopia’s population had been fully vaccinated [9].
Ethiopia began on March 13, 2021, to vaccinate HCWs for COVID-19 with the AstraZeneca vaccine. Healthcare workers include medical doctors, laboratory technicians, nurses, midwives, pharmacists, radiographers, anesthesiologists, public health and environmental health officers, any any other professionals including non-medical auxiliary staff who work in a healthcare facility. Non-medical auxiliary staff are other than health professionals such as financial workers, human resource workers, janitors, card room and documentation workers, porters, guardians and others.
Elderly people above the age of 60 and those above 50 years who have chronic diseases are also prioritized by the Ethiopian Ministry of Health. The launch of the vaccine program was attended by the WHO country representative Boueri Hama Sambo, who urged "communities and community leaders to build trust" as well as "demand for the vaccine" and to "promptly address "misinformation” [8]. During that event, one health worker was not convinced, saying "I don't believe in this vaccine. The virus is a sign of God’s wrath upon us, so I prefer to pray” [8]. Negative attitudes and mistrust towards COVID-19 vaccines are major barriers to increasing vaccine coverage worldwide [10].
Despite the scarcity of COVID-19 vaccines in Africa, several countries including Sierra Leone and Malawi have discarded large numbers of vaccines doses that expired before they were used due to low demand in the population, a situation also anticipated in Uganda [11]. In addition to the low accessibility of COVID-19 vaccines and hesitancy to be vaccinated for COVID-19, a preference for traditional medicines may constitute another barrier to vaccine acceptance in African countries, including Ethiopia. Indigenous medicines have been used to treat COVID-19 in Tanzania and Madagascar without meeting safety and efficacy standards [12]. The use of these plant products to treat COVID-19 carries safety risks and may hinder use of scientifically proven COVID-19 vaccinations. A study in Nepal revealed that the use of medicinal plants has increased since the outbreak of the COVID-19 pandemic [13]. The use of traditional medicine for COVID-19 and its impact on vaccination rates has not been investigated in Ethiopia. However, it is known that some plant extracts have traditionally been used to treat influenza [14], and people may prefer using them rather than accepting COVID-19 vaccines in the absence of diagnostic tests.
Willingness to receive a COVID-19 vaccine is a challenge in many countries [15]. COVID-19 vaccine acceptance rates in the general population were highest in Vietnam (98%), India (91%), China (91%), Denmark (87%), and South Korea (87%) and lowest in Serbia (38%), Croatia (41%), France (44%), Lebanon (44%), and Paraguay (51%) [16]. High hesitancy rates were also reported worldwide among HCWs, who play a central role in reducing the burden of the pandemic through their role in modeling preventive behavior and administering vaccinations. A review of 35 studies revealed that vaccination hesitancy rates varied from 4.3% to 72% worldwide [17]. Major concerns of health workers were vaccine safety, efficacy, and potential side effects. Higher socioeconomic status, directly working with patients, perceived risk and fear of COVID-19, and a history of influenza vaccination were associated with higher vaccine uptake [17].
Reluctance of HCWs to accept COVID-19 vaccination may not only increase the risk of virus transmission to their patients but also reduce the likelihood that HCWs will encourage patients to be vaccinated [17]. There is no documented evidence regarding attitudes and perceptions of Ethiopian health workers towards COVID-19 vaccination. This study examines knowledge, attitudes, perceptions towards the COVID-19 vaccine, level of refusal and associated factors of COVID-19 vaccination among HCWs in Dessie City, Ethiopia.
Methods
Study design, period and setting
This institution-based cross-sectional study was conducted in Dessie City in May, 2021. Dessie is the capital of South Wollo Zone, located about 400 km from Addis Ababa. The city is located at an altitude of 2,470 to 2,550 meters. According to Dessie City administration health office, the city has 8 health centers, 2 government hospitals, 3 private hospitals and 15 clinics.
Source population, inclusion and exclusion criteria
The source population for the study included all HCWs in Dessie City. The study population was all HCWs in the selected health facilities. All HCWs present at the selected health institutions during the survey were included in the study. Those who were absent (on sick leave, annual leave, or maternity leave) were excluded and not considered in sampling procedure (interval calculation) based on payroll lists.
Sample size determination and sampling procedure
A total of 404 study participants were identified by using the single population proportion formula and considering the following assumptions:
where: n: is the minimum sample size required, Zα/2 is the standard normal variable at (1-α) % confidence level (α is 0.05 with 95% CI, Zα/2 = 1.96), P is an estimate of the attitude towards COVID-19 vaccine (50%) and d is the margin of error (5%). Based on these assumptions, 384 individuals were estimated. Then 5% of the sample size contingency was added to minimize errors arising from the likelihood of non-compliance, giving a final sample size of 404.
To select study subjects, 11 health institutions (2 government hospitals, 2 private hospitals, 4 health centers, and 3 private clinics) were randomly selected. For the selected healthcare facilities, study subjects’ proportional allocation was made based on their number regardless of the profession. Then each institution's payroll for all professions and systematic random sampling was used to identify study participants. The first participant was selected by the simple lottery method. Professions represented in the study included medical doctors, laboratory technicians, nurses, midwives, ophthalmologists, pharmacists, public health officers, radiographers, environmental health specialists, anesthesiologists, porters, medical record workers, administrative staff, cleaners, laundry workers, and guards.
Outcome measurement and explanatory variables
The independent variables were socio-demographic factors, knowledge, attitudes, and perceptions and the dependent variable was refusalof to receive COVID-19 vaccination. To compute the three outcome variables of knowledge (good or poor), attitude (positive or negative), and perception (good or poor), we used the mean score of responses to 9 questions about knowledge and perceptions and 8 questions about attitudes. A score of 1 was assigned for poor knowledge, negative attitude and poor perception and a score of 2 for good knowledge, positive attitude and good perception. Scores above the mean value for each category were considered as good knowledge, positive attitude, and good perception. In addition, refusal to receive the COVID-19 vaccine was correlated as an outcome variable with socio-demographic, knowledge, attitude, and perception as independent variables.
Data collection and quality assurance
The data were collected using a structured questionnaire adapted from relevant literature. Data were collected both through a self-administered questionnaire and interviews with selected professionals. Ten nurses with BSc degrees and 5 environmental health professionals with BSc degrees were employed as data collectors and supervisors. To ensure the acquisition of reliable data, both data collectors and supervisors were trained by the principal investigator for one day on the objectives of the study, the content of the questionnaire, ethical issues, and methods of data collection. We also pre-tested the questionnaire on 5% of the sample size among HCWs in nearby Haik Town before actual data collection and made adjustments in the questionnaire where necessary. The collected data were checked daily by the supervisors for completeness. To ensure accurate and reliable data, the reliability of the questionnaire was assessed using the Cronbach alpha test, giving values of 0.82, 0.79, and 0.87 for knowledge, attitude and perception questions, respectively. We also assessed the validity of this questionnaire by recruiting experts to evaluate the content of the questionnaire using face validity, resulting in the experts agreeing that the test was a valid measure of the concept being measured. This means that they evaluated whether each of the measured items matched any given domain of the concept.
Data management and statistical analysis
The collected data were checked, coded, and entered into EpiData Version 4.6 and exported to Statistical Package for Social Sciences (SPSS) Version 25.0 for data cleaning and analysis. Descriptive statistics, such as frequency distribution (n) and proportions (%) were computed. We ran a logistic regression analysis using socio-demographic, knowledge, attitudes and perceptions as independent variables and refusal of vaccination as the dependent variable. First, bivariate logistic regression analysis (crude odds ratio [COR] at 95% confidence interval [CI]) was performed and then variables with p< 0.25 were retained for multivariablelogistic regression analysis.
From the multivariable analysis, variables with a significance level of p< 0.05 with adjusted odds ratio (AOR) at 95% CI were taken as statistically significant factors that were independently associated with the refusal of vaccination.
Model goodness of fit was checked using the Hosmer and Lemeshow test; P-values greater than 0.05 showed a value of 0.27, indicating the model was fit. Multi-collinearity between independent variables was also checked using the standard error of the coefficient of the model with a cut off value of 2. A maximum standard error value of 0.683 was reported from our model indicating the absence of multi-collinearity between independent variables.
Results
Socio-demographic characteristics of respondents
Of the 404 study participant HCWs, the response rate was 97.0%. The mean age of the respondents was 34.37 years (standard deviation [SD] = ± 7.785) and 198 were male (50.5%) and 194 female (49.5%). The study participants included 34 (8.7%) medical doctors, 46 (11.7%) laboratory technicians, 130 (33.2%) nurses and midwives, 50 (12.7%) pharmacists, 18 (4.6%) radiographers, 21 (5.4%) anesthesiologists, 36 (9.2%) public health officers and environmental health officers, and 57 (14.5%) non-medical auxiliary staff. The majority were university degree holders 257 (65.6%), 315 (80.4%) did not have health insurance, and more than one-third 157(40.1%) had received training or orientation about COVID-19 vaccination. The great majority (91.3%) of respondents did not have any chronic condition while 3.6% had hypertension, 2.3% asthma, 1.8% diabetes, and 0.5% each had HIV/AIDS and/or kidney disease (Table 1).
Table 1.
Socio-demographic characteristics among healthcare workers in Dessie City, Ethiopia, May 2021
| Questions | Frequency (n) | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 198 | 50.5 |
| Female | 194 | 49.5 |
| Age (years) | ||
| 20-30 | 157 | 40.1 |
| 31-40 | 156 | 39.8 |
| 41-50 | 16 | 16.8 |
| 51-60 | 13 | 3.3 |
| Education status | ||
| Primary level | 7 | 1.8 |
| Secondary level | 9 | 2.3 |
| Diploma | 119 | 30.3 |
| University degree | 257 | 65.6 |
| Profession | ||
| Medical doctor | 34 | 8.7 |
| Laboratory technician | 46 | 11.7 |
| Nurse and midwive | 130 | 33.2 |
| Pharmacist | 50 | 12.7 |
| Radiographer | 18 | 4.6 |
| Anesthesiologist | 21 | 5.4 |
| Public health officer | 36 | 9.2 |
| Nonmedical auxiliary staff | 57 | 14.5 |
| Religion | ||
| Orthodox Christian | 213 | 54.3 |
| Protestant | 29 | 7.4 |
| Muslim | 150 | 38.3 |
| Marital status | ||
| Single | 144 | 36.7 |
| Married | 214 | 54.6 |
| Divorced, widowed or separated | 34 | 8.6 |
| Where did you grow up? | ||
| Rural | 151 | 38.5 |
| Semi-urban | 77 | 19.6 |
| Urban | 164 | 41.8 |
| Household size (persons) | ||
| ≤5 | 277 | 70.7 |
| >5 | 115 | 29.3 |
| Years worked in a healthcare facility | ||
| 10 or less | 306 | 78.1 |
| >10 | 86 | 21.9 |
| Do you have health insurance? | ||
| No | 315 | 80.4 |
| Yes | 77 | 19.6 |
| Has anyone in your family or of your colleagues or friends had COVID-19? | ||
| Yes | 129 | 32.9 |
| No | 263 | 67.1 |
| Have you been tested for COVID-19? | ||
| Yes | 132 | 33.7 |
| No | 260 | 66.3 |
| If “yes”, were you positive? (N = 132) | ||
| Yes | 25 | 18.9 |
| No | 107 | 81.1 |
| Do you have any chronic diseases? | ||
| Yes | 34 | 8.7 |
| No | 358 | 91.3 |
| Smoking status | ||
| Current smoker | 12 | 3.1 |
| Ex-smoker | 33 | 8.4 |
| Never smoked | 347 | 88.5 |
| Have you received any training or orientation about COVID-19 vaccination? | ||
| Yes | 157 | 40.1 |
| No | 235 | 59.9 |
| How many times have you received training/orientation? | ||
| Once | 116 | 29.6 |
| More than once | 41 | 10.4 |
| Source of information about COVID-19 vaccine (multiple responses possible) | ||
| Television | 326 | 83.2 |
| Internet | 263 | 67.1 |
| Radio | 230 | 58.7 |
| Scientific literature | 159 | 40.6 |
| Relatives and friends | 127 | 32.4 |
HCWs knowledge about COVID-19 vaccines
The mean score of the knowledge was 14.97, with a standard deviation of 1.881. The overall good knowledge rate of the HCWs about COVID-19 and its vaccine was 62.5% with 95% CI (57.4-66.8%). Of those who had good knowledge of COVID-19 and its vaccine, 171 (69.79%) were planning to be vaccinated as soon as a vaccine becomes available. One hundred twenty-eight (64.65%) males and 117 (60.3%) females had good knowledge whereas 70 (35.35%) males and 77 (39.69%) females had poor knowledge about COVID-19 and its vaccines. Similarly, 20 (58.8%) doctors, 31 (67.4%) laboratory technicians, 84 (64.6%) nurses, and midwives and 31 (54.38%) non-medical axillary staff had good knowledge. Among those who had a chronic disease, 22 (64.7%) had good knowledge. The majority (340, 86.7%) responded that COVID-19 is a serious disease and 329 (83.9%) stated that it could result in many health complications. One hundred fifty (38.3%) HCWs considered the differences in the effectiveness among the Pfizer, Moderna, and Astra Zeneca COVID-19 vaccines to be large. More than three-quarters (77.6%) of the HCWs considered the major mode of COVID-19 transmission to be touching contaminated surfaces and touching one’s eyes, nose, and mouth, followed by shaking hands, hugging, and kissing (70.4%) and inhaling the virus (69.9%) (Table 2).
Table 2.
Knowledge about COVID-19 and COVID-19 vaccines among healthcare workers in Dessie City, Ethiopia, May 2021
| Questions | Frequency (n) | Percentage (%) |
|---|---|---|
| Is COVID-19 a serious disease? * | ||
| Yes | 340 | 86.7 |
| No | 29 | 7.4 |
| I don't know δ | 23 | 5.9 |
| Do you know that COVID-19 can result in complications? * | ||
| Yes | 329 | 83.9 |
| No | 63 | 16.1 |
| Can vaccines effectively prevent COVID-19? * | ||
| Yes | 161 | 41.1 |
| No | 112 | 28.6 |
| I don't know δ | 119 | 30.4 |
| Can COVID-19 be acquired after full vaccination? * | ||
| Yes | 132 | 33.7 |
| No | 111 | 28.3 |
| I don’t know δ | 149 | 38.0 |
| Do you know where you can be vaccinated when a COVID-19 vaccine becomes available? * | ||
| Yes | 255 | 65.1 |
| No | 137 | 34.9 |
| Are there large differences in the effectiveness of the Pfizer, Moderna, and Astra Zeneca COVID-19 vaccines? * | ||
| Yes | 150 | 38.3 |
| No | 242 | 61.7 |
| Does the effectiveness of the major COVID-19 vaccines vary between about 50% and 95%? (N = 150) | ||
| Yes | 103 | 68.7 |
| No | 17 | 13.3 |
| I don’t know | 30 | 20.0 |
| Do COVID-19 vaccines have side effects? * | ||
| Yes | 279 | 71.2 |
| No | 48 | 12.2 |
| I don’t know δ | 65 | 16.6 |
| Are older people and chronic disease patients most likely to experience severe illness and death from COVID-19 infection?* | ||
| Yes | 354 | 90.3 |
| No | 38 | 9.7 |
| Are HCWs more vulnerable to COVID-19 infection than the general public? * | ||
| Yes | 340 | 86.7 |
| No | 25 | 6.4 |
| I don’t know δ | 27 | 6.9 |
| Knowledge of HCWs about the mode of transmission of COVID-19 (multiple responses possible) | ||
| Poor hygiene | 218 | 55.6 |
| Inhalation of the virus | 274 | 69.9 |
| Touching contaminated surfaces, eyes, nose or mouth | 304 | 77.6 |
| Shaking hands, hugging, and kissing | 276 | 70.4 |
*These questions are used to compute the overall score of knowledge
δThe third choice “I don’t know” in some questions was included in the “No” category for the analysis
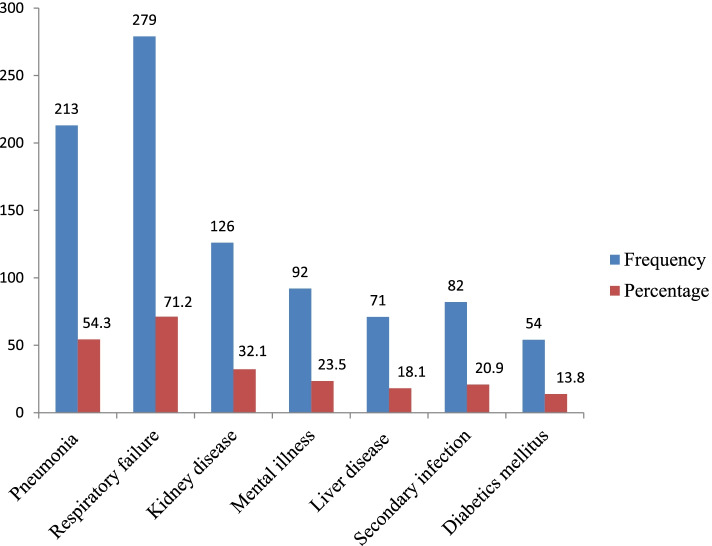
COVID-19 disease was associated with untreated infections. Two hundred thirteen (54.3%) of the respondents stated that it could result in pneumonia and 279 (71.2%) in respiratory failure (Fig. 1).
Fig. 1.
Respondents’ knowledge about complication of COVID-19
HCWs attitudes towards COVID-19 vaccines
The mean score of attitudes was 13.31, with a standard deviation of 1.529. The overall positive attitude rate about the COVID-19 vaccine was 52.3% with 95% CI (47.7 – 57.4%). Of those who had a positive attitude towards the COVID-19 vaccine, 189 (79.75%) were planning to get vaccinated when a vaccine becomes available. One hundred-nine (55.05%) males and 96 (49.5%), females had a positive attitude while 89 (44.95%) of males and 98 (50.5%) of females had a negative attitude towards COVID-19 vaccines.
Fifteen (44.12%) of the medical doctors, 30 (65.23%) laboratory technicians, 66 (50.77%) nurses and midwives, and 32 (56.14%) non-medical auxiliary staff had a positive attitude towards the COVID-19 vaccine. Of those who had a chronic disease, 19 (55.9%) had a positive attitude towards COVID-19 vaccines. Two-fifths (40.6%) of the HCWs were confident that the Ministry of Health can control COVID-19 in Ethiopia but 55.4% of them expressed a general mistrust/uncertainty about the effectiveness of COVID-19 vaccines (Table 3).
Table 3.
Attitudes towards COVID-19 vaccines among healthcare workers in Dessie City, Ethiopia, May 2021
| Questions | Frequency (n) | Percentage (%) |
|---|---|---|
| Are you confident that the Ministry of Health can control COVID-19 in Ethiopia? * | ||
| Yes | 159 | 40.6 |
| No | 233 | 59.4 |
| Do you have general mistrust/uncertainty about COVID-19 vaccine effectiveness? * | ||
| Yes | 217 | 55.4 |
| No | 175 | 44.6 |
| Do you fear COVID-19 vaccines? * | ||
| Yes | 221 | 56.4 |
| No | 171 | 43.6 |
| Reasons for fearing COVID-19 vaccines (N = 221) | ||
| Infertility | 55 | 24.9 |
| Severe allergic reactions | 72 | 32.6 |
| Unknown long-term effects | 94 | 42.5 |
| Are you planning to be vaccinated for COVID-19? | ||
| Yes | 251 | 64.0 |
| No | 141 | 36.0 |
| Do you refuse to get vaccinated because only God/Allah can prevent COVID-19?* | ||
| Yes | 137 | 34.9 |
| No | 255 | 65.1 |
| What alternative preventive measures did you use to prevent COVID-19 | ||
| Traditional medicine | 15 | 3.8 |
| Praying | 48 | 12.2 |
| Physical exercise | 43 | 11.0 |
| Should people with chronic and severe diseases get priority for COVID-19 vaccination? * | ||
| Yes | 341 | 87.0 |
| No | 51 | 13.0 |
| Should HCWs get priority in COVID-19 vaccination? * | ||
| Yes | 340 | 86.7 |
| No | 52 | 13.3 |
| Should all HCWs be vaccinated to protect the public? * | ||
| Yes | 276 | 70.4 |
| No | 62 | 15.8 |
| I don't know δ | 54 | 13.8 |
| To protect the public, HCWs should follow government guidelines about vaccines * | ||
| Agree | 322 | 82.1 |
| Disagree | 70 | 17.9 |
*These questions are used to compute the overall score of attitude
δTo compute the overall score of Attitude, the third choice “I do not know” in some questions were included in the “No” category for analysis
Perceptions of HCWs about COVID-19 vaccines
The mean score of perceptions was 14.66, with a standard deviation of 1.866. The overall rate of good perception about the COVID-19 vaccine was 60.5% with 95% CI (55.6–65.3%). Of those who had a good perception about COVID-19 vaccine, only 189 (79.75%) were planning to be vaccinated. Nearly two-thirds 125 (63.13%) of the male and 112 (57.73%) of the female HCWs had a good perception whereas 73 (36.87%) of the males and 82 (42.3%) of the females had a poor perception of COVID-19 vaccines.
Nineteen (55.9%) doctors, 32 (69.57%) laboratory technicians, 86 (66.15%) nurses and midwives, 24 (48%) pharmacists, and 33 (57.9%) non-medical auxiliary staff had a good perception about COVID-19 vaccines. One hundred twenty-six (59.15%) of the Orthodox Christians, 16(55.17%) of the Protestants, and 95(63.3%) Muslims had a good perception about COVID-19 vaccines. Eighty-nine (58.9%), 44 (57.14%) and 104 (63.41%) HCWs who grew up in rural, semi-urban and urban areas, respectively, had a good perception of the COVID-19 vaccines. Among those who had a chronic disease, 23 (67.65%) had good perceptions.
Three-quarters (292, 74.5%) of the HCWs considered themselves to be at high risk of becoming infected with COVID-19 and 39.5% of them thought that they could get infected with COVID-19 through vaccination. Of these, 56 (14.3%) in the 20-30 age group, 67 (17.1%) aged 31-40, 26 (6.6%) aged 41-50 and 6 (1.5%) in the 51-60 age group linked vaccines to COVID-19 infection. With regard to educational level, 6 (1.5%) HCWs with secondary education and below (grades 12 and below), 49 (12.5%) with diplomas, and 100 (25.5%) with university degrees associated vaccines with infection. Among the different occupational categories, 16 (4.1%) medical doctor, 21 (5.4%) medical laboratory technician, 50 (12.6%) nurse and midwive, 18 (4.6%) pharmacist,15 (3.8%) public health officer, 9 (2.3%) anesthesiologist, 10 (2.6%) radiographer and 16 (4.1%) non-medical auxiliary staff believed that they could get infected with COVID-19 through vaccination. Similarly, nearly half (184, 46.9%) of the HCWs thought that vaccines could worsen any pre-existing medical conditions. On the other hand, 173 (44.1%) of the respondents thought that it may not be possible to reduce the incidence of COVID-19 without vaccination (Table 4).
Table 4.
Perception towards COVID-19 vaccine among healthcare workers in Dessie City, Ethiopia, May 2021
| Questions | Frequency (n) | Percentage (%) |
|---|---|---|
| Do you think you are at high risk of becoming infected with COVID-19? | ||
| Yes | 292 | 74.5 |
| No | 73 | 18.6 |
| I don’t know δ | 27 | 6.9 |
| Do you think that you could get infected with COVID-19 through vaccination? | ||
| Yes | 155 | 39.5 |
| No | 165 | 42.1 |
| I don’t know δ | 72 | 18.4 |
| Is it possible to reduce and control the incidence of covid-19 without vaccination? | ||
| Yes | 173 | 44.1 |
| No | 174 | 44.4 |
| I don’t know δ | 45 | 11.5 |
| Do most of my colleagues appear to think that getting vaccinated is a good idea? | ||
| Yes | 272 | 69.4 |
| No | 72 | 18.4 |
| I don’t know δ | 48 | 12.2 |
| Is getting yourself vaccinated for COVID-19 a good way to protect your family and other people against infection? | ||
| Yes | 274 | 69.9 |
| No | 83 | 21.2 |
| I don’t know δ | 35 | 8.9 |
| My family and friends think that getting vaccinated for COVID-19 is a good idea | ||
| Agree | 285 | 72.7 |
| Disagree | 60 | 15.3 |
| Neutral δ | 47 | 12.0 |
| Do you think that the COVID-19 vaccine can worsen any health conditions you have? | ||
| Yes | 184 | 46.9 |
| No | 140 | 35.7 |
| I don’t know δ | 68 | 17.4 |
| Do you believe that you can get proper medical care if you contract COVID-19? | ||
| Yes | 197 | 50.3 |
| No | 131 | 33.4 |
| I don’t know δ | 64 | 16.3 |
| Do you think that the development of COVID-19 vaccines was properly carried out to make them safe? | ||
| Yes | 282 | 71.9 |
| No | 110 | 28.1 |
δThese questions are included to compute the overall score of perception, the third choice “I don’t know/ neutral” in some questions was categorized into the “No/disagree” category for the analysis
Nearly two-thirds 251 (64.0%) with 95%CI (59.4-68.6%) of the HCWs were planning to be vaccinated and 141 (36.0%) with 95% CI (31.4-40.6%) refused to be vaccinated for COVID-19 (Table 3). Bivariate analysis identified the following factors in the refusal to be vaccinated: absence of COVID-19 in the family or among colleagues and friends, failure to be tested for COVID-19, failure to obtain training or orientation about COVID-19 vaccination, negative attitude, and poor knowledge and perception (Table 5).
Table 5.
Bivariate analysis of factors associated with refusal of COVID-19 vaccine among healthcare workers in Dessie City, Ethiopia, May 2021
| Variables | Refusal of vaccination | COR (95% CI) | |
|---|---|---|---|
| Yes | No | ||
| Sex | |||
| Male | 68 | 130 | 0.87(0.57-1.31) |
| Female | 73 | 121 | Ref |
| Age (years) | |||
| 20-30 | 59 | 98 | 1.36(0.39-4.59) |
| 31-40 | 57 | 99 | 1.29(0.38-4.39) |
| 41-50 | 21 | 45 | 1.05(0.29-3.80) |
| 51-60 | 4 | 9 | Ref |
| Educational status * | |||
| Secondary or below level | 4 | 12 | 0.65(0.20-2.08) |
| Diploma | 50 | 69 | 1.42(0.91-2.21) |
| University degree | 87 | 170 | Ref |
| Religion * | |||
| Christian | 96 | 146 | 1.53(0.99-2.37) |
| Muslim | 45 | 105 | Ref |
| Marital status | |||
| Currently single | 67 | 111 | 1.14(0.76-1.73) |
| Married | 74 | 140 | Ref |
| Place of residence where you grew up | |||
| Rural | 58 | 93 | 1.24(0.78-1.96) |
| Semi-urban | 28 | 49 | 1.13(0.64-1.99) |
| Urban | 55 | 109 | Ref |
| Household size (persons) | |||
| Five or less | 103 | 174 | 1.19(0.76-1.89) |
| More than five | 38 | 77 | Ref |
| Duration of work as HCW | |||
| 10 years or less | 114 | 192 | 1.29(0.78-2.16) |
| >10 years | 27 | 59 | Ref |
| Have health insurance | |||
| No | 117 | 198 | 1.31(0.77-2.23) |
| Yes | 24 | 53 | Ref |
| Anyone in your family or colleague or friend had COVID-19 * | |||
| No | 107 | 156 | 1.92(1.21-3.04) |
| Yes | 34 | 95 | Ref |
| Tested for COVID-19 * | |||
| No | 104 | 156 | 1.71(1.09-2.69) |
| Yes | 37 | 95 | Ref |
| Have a chronic disease | |||
| No | 130 | 228 | 1.19(0.56-2.52) |
| Yes | 11 | 23 | Ref |
| Smoking status | |||
| Currently smoke | 2 | 10 | 0.34(0.07-1.57) |
| Ex-smoker | 10 | 23 | 0.74(0.34-1.59) |
| Never smoked | 129 | 218 | Ref |
| Profession * | |||
| Medical doctor | 15 | 19 | Ref |
| Laboratory technician | 16 | 30 | 0.68(0.27-1.68) |
| Nurse and midwive | 32 | 98 | 0.41(0.19-.91) |
| Pharmacist | 29 | 21 | 1.75(0.73-4.22) |
| Radiographer | 7 | 11 | 0.81(0.25-2.58) |
| Anesthesiologist | 10 | 11 | 1.15(0.39-3.43) |
| Public health officer | 8 | 28 | 0.36(0.13-1.02) |
| Non-medical auxiliary staff | 24 | 33 | 0.92(0.39-2.17) |
| Received training or orientation about COVID-19 vaccination * | |||
| No | 99 | 136 | 1.99(1.29-3.09) |
| Yes | 42 | 115 | Ref |
| Knowledge level about COVID-19 vaccine* | |||
| Poor | 67 | 80 | 1.94(1.27-2.96) |
| Good | 74 | 171 | Ref |
| Attitude towards COVID-19 vaccine* | |||
| Negative | 97 | 90 | 3.94(2.54-6.12) |
| Positive | 44 | 161 | Ref |
| Perceptions of COVID-19 vaccine* | |||
| Poor | 93 | 62 | 5.91(3.76-9.27) |
| Good | 48 | 189 | Ref |
*Indicates variables included in the multivariable logistic regression analysis; Ref, reference category
Proportion of refusal to be vaccinated for COVID-19
One hundred forty-one (36.0%, 95% CI [31.4-40.6%]) refused to be vaccinated for COVID-19 when vaccines become available and 251 (64.0%, 95% CI [59.4- 68.6%]) said that they wanted to be vaccinated.
Factors associated with refusal to be vaccinated
In multivariable analysis, refusal to be vaccinated for COVID-19 vaccine was significantly associated with a negative attitude (AOR: 3.06; 95% CI [1.86-5.03]) and poor perception (AOR: 4.73; 95% CI [2.91-7.68]). HCWs who had negative attitude about COVID-19 vaccines were 3.06 times refused to be vaccinated compared to those who had positive attitude towards COVID-19 vaccines. Furthermore, HCWs who had poor perception about COVID-19 vaccines were 4.73 times refused to be vaccinated compared to those who had good perception towards COVID-19 vaccines. However, being nurses and midwives (AOR: 0.38; 95% CI [0.15-0.97]) was significantly associated with to be vaccinated for COVID-19 vaccine compared to other HCWs. Also, most pharmacists refused to be vaccinated but this association was not statistically significant (Table 6).
Table 6.
Multivariable analysis of factors significantly associated with refusal to be vaccinated for COVID-19 vaccine among healthcare workers in Dessie City, Ethiopia, May 2021
| Variables | Refusal of vaccinations | COR (95% CI) | AOR (95% CI) |
P-value (adjusted model) |
|
|---|---|---|---|---|---|
| Yes | No | ||||
| Profession | |||||
| Medical doctor | 15 | 19 | Ref | Ref | |
| Laboratory technician | 16 | 30 | 0.68(0.27-1.68) | 0.98(0.34-2.83) | 0.973 |
| Nurse and midwive | 32 | 98 | 0.41(0.19-.91) | 0.38(0.15-.97) | 0.042 |
| Pharmacist | 29 | 21 | 1.75(0.73-4.22) | 1.50(0.53-4.25) | 0.445 |
| Radiographer | 7 | 11 | 0.81(0.25-2.58) | 0.66(0.16-2.33) | 0.470 |
| Anesthesiologist | 10 | 11 | 1.15(0.39-3.43) | 0.72(0.20-2.60) | 0.617 |
| Public health officer | 8 | 28 | 0.36(0.13-1.02) | 0.46(0.14-1.50) | 0.197 |
| Non-medical auxiliary staff | 24 | 33 | 0.92(0.39-2.17) | 0.97(0.36-2.66) | 0.955 |
| Attitude towards COVID-19 vaccine | |||||
| Negative | 97 | 90 | 3.94(2.54-6.12) | 3.06(1.86-5.03) | < 0.001 |
| Positive | 44 | 161 | Ref | Ref | |
| Perception of COVID-19 vaccine | |||||
| Poor | 93 | 62 | 5.91(3.76-9.27) | 4.73(2.91-7.68) | < 0.001 |
| Good | 48 | 189 | Ref | Ref | |
Discussion
On-going efforts are been made to end the COVID-19 pandemic. Various COVID-19 vaccines have been distributed in many countries, including Ethiopia. The overall good knowledge, good perception, and positive attitude rates of the HCWs about COVID-19 vaccines were 62.5%, 60.5%, and 52.3%, respectively.
In our study, 64.0% of the HCWs planned to be vaccinated and 36.0% refused to do so. A similar vaccine acceptance rate was reported by a study in Iraq (61.7%) [18], which was higher than in two studies in the USA, where more than half of all HCWs were undecided and delayed the decision to be vaccinated [19, 20]. Low acceptance rates were also reported among healthcare workers in Ghana (39.3%) [21]), the Democratic Republic of Congo (27.7%) [22]), Egypt (21%) [23]), and Nepal (38.3%) [24]). Studies in Nigeria and Saudi Arabia reported intended vaccine uptake rates of 50.2% [25] and 50.52%, respectively [26]. Low rates may be due to earlier study dates (when prospects of the vaccine rollout were uncertain), HCWs limited knowledge about vaccines, lack of trust in government management capacity, and concerns about vaccine safety.
Some of the highest vaccine acceptance rates (above 95%) were reported from South and Southeast Asia, where HCWs were willing to be vaccinated because as they perceived the pandemic to be severe, considered the vaccines to be safe, experienced few financial constraints and little stigmatization of being vaccinated, and trusted the health authorities [27]. Studies in China and Vietnam reported intended vaccine uptakes of 76.63% [28] and 76.10%, respectively [29], slightly higher than our findings. These high rates were associated with good knowledge regarding the severity of COVID-19, HCWs’ trust in the vaccines, and earlier study dates than in our study.
In this study, high rates of not intending to be vaccinated when vaccines become available were associated with negative attitude and low perception about COVID-19 vaccine. Our study also showed that being a nurse and midwife was significantly associated with acceptance to be vaccinated for COVID-19. Consistent with our findings, a study in India found vaccine acceptance to be highest among nurses [30]. However, in a study in the Democratic Republic of the Congo, the highest acceptance rates among HCWs were reported for medical doctors [22] and in Debre Tabor Hospital in northern Ethiopia, nurses had the lowest acceptance rates [31].
Our findings corroborate a study from the Democratic Republic of the Congo that reported that having a positive attitude towards COVID-19 vaccines was significantly associated with the willingness to receive a vaccine [22]. A study among HCWs of an inner-city hospital in New York [32] reported similar results. A study in Libya indicated that having a family member or friend infected with COVID-19 was positively associated with the likelihood of vaccine acceptance [33]. A community-based study in Wolaita Zone, Ethiopia, showed that family members and friends who had been tested for COVID-19 were significantly associated with the acceptance of COVID-19 vaccine [34]. In our study, having COVID-19-infected family members, colleagues, or friends was associated with increased vaccine uptake intention only in the bivariate analysis but not in the final adjusted logistic model (Table 5). In addition, as indicated in Table 4, 39.5% of the HCWs associated vaccines with possible COVID-19 infections and 46.9% of them thought that vaccines could worsen any pre-existing medical conditions. This is very concerning, as it indicates that HCWs are not convinced about the safety of COVID-19 vaccines and are also misinformed. The reason for this widespread misinformation is not known but the public health agencies in Ethiopia may need to increase their efforts to educate HCWs about the safety of these vaccines.
Limitation of the study
Bias may have affected the result of our study. Social desirability bias in which HCWs answered questions in a manner that would be viewed favorably by others may have resulted in over-reporting of good attitudes and perceptions as well as intended uptake of vaccines. Moreover, causal inferences cannot be drawn from this study due to the nature of the study design.
Conclusion
The willingness to get vaccinated against COVID-19 was moderately high among healthcare workers in Dessie City. Negative attitudes and poor perceptions of HCWs towards COVID-19 vaccines were the most significant factors in the refusal to accept vaccines. Because HCWs are scheduled to be among the first to receive vaccines and play a central role in their administration in the population, key factors in their decision-making process, such as knowledge about the safety of vaccines, must be addressed as early as possible. Our findings may inform health planners and administrators in developing relevant interventions that promote COVID-19 vaccination uptake among healthcare workers in Ethiopia. In particular, the large proportions of HCWs who considered vaccines to worsen any pre-existing medical conditions or cause COVID-19 is very concerning, as it seems that HCWs are not convinced about the safety of the vaccines and are also misinformed. These issues need to be urgently addressed by the public health agencies in Ethiopia. Working on behavioral change communication and social mobilization towards COVID-19 vaccines using culturally appropriate manner might increase the attitudes and perceptions, which in turn increasing the rate of COVID-19 vaccination. We also recommend studies in urban and rural communities to investigate the religious conspiracy about COVID-19 vaccines that may ensure increasing the vaccination rate of COVID-19.
Implication of the study
The information on attitudes, knowledge and perceptions pertaining to the refusal of COVID-19 vaccine among HCWs can inform policy makers and administrators about opportunities and constraints in distributing vaccines among HCWs in Dessie and other Ethiopian cites. The findings may thus contribute to developing a strategy for controlling the pandemic by addressing factors significantly affecting vaccination uptake.
Acknowledgments
We gratefully acknowledge Wollo University for providing the ethical clearance letter, which allowed us to do this study. We also express our thanks to Dessie City health bureau for giving permission to conduct this study. We also acknowledge the managers of the public and private healthcare facilities in Dessie City for their permission to conduct this study and for the information we received when needed. We thank the data collectors and supervisors for their assistance and all study participants for their participation and valuable information.
Abbreviations
- AOR
adjusted odds ratio
- CI
confidence interval
- COR
crude odds ratio
- HCWs
healthcare workers
Authors’ contributions
AA and MA conceptualized, designed, analyzed, and interpreted the data, prepared a draft manuscript and edited the manuscript. HK conceptualized, designed, and edited the manuscript. AA and MA contributed equally to this work. All authors read and approved the final manuscript.
Funding
No funding was obtained from institution. However, data collection budget was covered by Dr Helmut Kloos, who is a co-author for this study.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval was obtained from the Institutional Ethical Review Committee of the College of Medicine and Health Sciences of Wollo University. Informed written consent was obtained from study subjects after explaining the purpose of the study and assurance that their information would not be used for purposes other than scientific research. Confidentiality was ensured by using code numbers rather than names. All the methods used comply with the principles and ethical standards of the declaration of Helsinki.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Metadel Adane and Ayechew Ademas contributed equally to this work.
References
- 1.Worldometer. Coronavirus Cases: deaths: recovered : [Internet]. 2021 [cited 2 Jul 20, 2020], Available from: https://www.worldometers.info/coronavirus.
- 2.FDRE (Federal Democratic Repuplic of Ethiopia). COVID-19 state of emergency. Addis Ababa; 2020.
- 3.BBC. Covid-19 Africa : what is happening with vaccines ? Which countries are using up [Internet]. 2021. Available from: https://www.bbc.com/news/56100076.
- 4.Reuters. Ethiopia to get 300, 000 doses of Sinopharm COVID-19 shot , health minister says [Internet]. 2021. Available from: https://www.reuters.com/article/uk-healthcare-coronavirus-ethiopia-id USKBN2BL1TE.
- 5.WHO. Ethiopia introduces COVID-19 vaccine in a national launching ceremony [Internet]. 2021. Available from: https://www.afro.who.int/news/ethiopia-introduces-covid-19-vaccine-national-launching-ceremony.
- 6.African Vaccine Acquisition Trust delivers 108,000 doses of COVID-19 vaccine to Ethiopia – Africa CDC [Internet]. 2021. Available from: https://africacdc.org/news-item/african-vaccine-acquisition-trust-delivers-108,000-doses-of-covid-19-vaccine-to-ethiopia.
- 7.Reuters. Ethiopia, COVID-19 tracker [Internet]. 2021 [cited Apr 27, 2021]. Available from: https://graphics.reuters.com/world-coronavirus-tracker-and-maps/countries-and-territories/ethiopia.
- 8.Africanews. NEWS Ethiopia launches Covid vaccination in Addis Ababa. 2021; Available from: https://www.africanews.com/2021/03/14/ethiopia-launches-covid-vaccinations-in-addis-ababa.
- 9.Holder Josh. Covid World Vaccination Tracker - The New York Times [Internet]. The New York Times. 2021. Available from: https://www.nytimes.com/interactive/2021/world/covid-vaccinations-tracker.html.`
- 10.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: Implications for public health communications. Lancet Reg Health - Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muhumuza R. vaccine hesitancy adds to slow rollout of doses. Associated Press, Kampala. [Internet]. 2021. Available from: Available at: http:www.wkr.com/news/in-africa-vaccine.
- 12.Materu B. Tanzanians urged to use traditional medicine for Covid-19 [Internet]. 2021. Available from: https://www.theeastafrican.co.ke/tea/news/east-africa/tanzania-traditional-medicine-covid-19-3276402.
- 13.Khadka D, Dhamala MK, Li F, Aryal PC, Magar PR, Bhatta S, et al. The use of medicinal plants to prevent COVID-19 in Nepal. J Ethnobiol Ethnomed. 2021;17(1):1–17. doi: 10.1186/s13002-021-00449-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Worku AM. A review on significant of traditional medicinal plants for human use in case of Ethiopia. J Plant Pathol Microbiol. 2019;10(6):1–12. [Google Scholar]
- 15.WHO. WHO issues its first emergency use validation for a COVID-19 vaccine and emphasizes need for equitable global access [Internet]. 2020. Available from: https://www.who.int/news/item.
- 16.Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet [Internet]. 2021;397(10278):1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health [Internet]. 2021;(0123456789). Available from: http://www.ncbi.nlm.nih.gov/pubmed/33877534. [DOI] [PMC free article] [PubMed]
- 18.Al-Metwali BZ, Al-Jumaili AA, Al-Alag ZA, Sorofman B. Exploring the acceptance of COVID-19 vaccine among healthcare workers and general population using health belief model. J Eval Clin Pract. 2021(April):1–11. [DOI] [PMC free article] [PubMed]
- 19.Gadoth A, Halbrook M, Matine-Blais R, Gray A, Tobin NH, Ferbas KG, Adrovandi GM RA. Cross-sectional assessment of COVID-19 vaccine acceptance among healthcare workers in Los Angeles. Ann Internal Med. 2021; Available from: https://doi.org/10.7326/M20-7580. [DOI] [PMC free article] [PubMed]
- 20.Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9(2):1–18. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Agyekum MW, Afrifa-Anane GF, Kyei-Arthur F, Addo B. Acceptability of COVID-19 vaccination among healthcare workers in Ghana. Adv Public Health. 2021. 10.1155/2021/9998176.
- 22.Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmatic Obs Res. 2020;11:103–109. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 vaccination perception and attitude among healthcare workers in Egypt. J Prim Care Community Health. 2021;12. [DOI] [PMC free article] [PubMed]
- 24.Paudel S, Palaian S, Subedi N. Risk perception and hesitancy toward COVID-19 vaccination among healthcare workers and staff at a medical college in Nepal. Risk Manag. Health Policy. 2021:2253–61. [DOI] [PMC free article] [PubMed]
- 25.Tobin EA, Okonofua M, Azeke A, Ajekweneh V, Akpede G. Willingness to acceptance a covid-19 vaccine in nigeria: a population-based cross-sectional study. J Med Res [Internet]. 2021;5(2):1–6. Available from: https://www.alliedacademies.org/allied-journal-of-medical-research.
- 26.Qattan AMN, Alshareef N, Alsharqi O, Al Rahahleh N, Chirwa GC, Al-Hanawi MK. Acceptability of a COVID-19 vaccine among healthcare workers in the Kingdom of Saudi Arabia. Front Med. 2021;8(March):1–12. doi: 10.3389/fmed.2021.644300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew NWS, Cheong C, Kong G, Phua K, Ngiam JN, Tan BYQ, et al. An Asia-Pacific study on healthcare worker’s perception and willingness to receive COVID-19 vaccination. Int J Infect Dis [Internet]. 2021;106:52–60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33781902. [DOI] [PMC free article] [PubMed]
- 28.Sun Y, Chen X, Cao M, Xiang T, Zhang J, Wang P, et al. Will healthcare workers accept a COVID-19 vaccine when it becomes available? A cross-sectional study in China. Front Public Health. 2021;9(May):1–8. doi: 10.3389/fpubh.2021.664905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huynh G, Tran TT, Nguyen HTN, Pham LA. COVID-19 vaccination intention among healthcare workers in Vietnam. Asian Pac J Trop Med. 2021;14(4):159–164. doi: 10.4103/1995-7645.312513. [DOI] [Google Scholar]
- 30.Singhania N, Kathiravan S, Pannu AK. Acceptance of coronavirus disease 2019 vaccine among health-care personnel in India: a cross-sectional survey during the initial phase of vaccination. Clin Microbiol Infect [Internet]. 2021;2019–21. Available from: https://doi.org/10.1016/j.cmi.2021.03.008. [DOI] [PMC free article] [PubMed]
- 31.Alle YF, Oumer KE. Attitude and associated factors of COVID-19 vaccine acceptance among health professionals in Debre Tabor Comprehensive Specialized Hospital, North Central Ethiopia; 2021: cross-sectional study. Virus Disease [Internet]. 2021; Available from: https://doi.org/10.1007/s13337-021-00708-0. [DOI] [PMC free article] [PubMed]
- 32.Ciardi F, Menon V, Jensen JL, Shariff M a, Pillai A, Venugopal U, et al. knowledge, attitudes and perceptions of COVID-19 vaccination among healthcare workers of an inner-city hospital in New York. Vaccines. 2021;9(5):516. doi: 10.3390/vaccines9050516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elhadi M, Alsoufi A, Alhadi A, Hmeida A, Alshareea E, Dokali M, et al. Knowledge , attitude , and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross- sectional study. BMC Public Health. 2021;1–21. [DOI] [PMC free article] [PubMed]
- 34.Mesele M. COVID-19 Vaccination acceptance and its associated factors in Sodo Town , Wolaita Zone, Southern Ethiopia: cross-sectional study. Infect Drug Resist. 2021;2361–7. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.