Abstract
Introduction
The age at which transgender women (TW) and men (TM) first experience gender dysphoria (GD) has not been reported in a U.S. population of adults seeking genital gender-affirming surgery (gGAS). Because gender is an innate part of identity, we hypothesized that untreated GD would be a part of individuals’ earliest memories. Understanding GD onset can help guide providers with when and how to focus care to patients not yet identified as “transgender
Aim
(i) Determine the age at which transgender adults seeking gGAS first experience GD
(ii) Determine the number of life-years that transgender adults spend living with untreated GD
Methods
During initial consultation for gGAS, we asked patients the earliest age at which they experienced GD and the age at which they had their earliest episodic memory. We also queried history of anxiety, depression, and suicide attempt.
Main Outcome Measures
Patients self-reported their earliest recollections of experiencing GD, earliest memories in general, and history of anxiety, depression, and suicide attempt.
Results
Data from 155 TW (mean age 41.3; SD 16.3) and 55 TM (mean age 35.4; SD 10.8) were collected. Most patients (TM: 78%; TW: 73%) reported experiencing GD for the first time between ages 3 and 7 years. For TM the mean age of onset was 6.17 years; for TW it was 6.71 years. A total of 81% of TW and 80% of TM described their first recollection of GD as one of their earliest memories. Mean years of persistent GD before the start of gender transition were 22.9 (TM) and 27.1 (TW). Rates of depression, anxiety, and suicide ideation decreased following gender transition.
Conclusion
Our findings suggest that GD typically manifests in early childhood and persists untreated for many years before individuals commence gender transition. Diagnosis and early management during childhood and adolescence can improve quality of life and survival.
Zaliznyak M, Yuan N, Bresee C, et al. How Early in Life do Transgender Adults Begin to Experience Gender Dysphoria? Why This Matters for Patients, Providers, and for Our Healthcare System. Sex Med 2021;9:100448.
KEY WORDS: Transgender, Gender Dysphoria, Gender Affirming Hormone Therapy (GAHT), Gender Affirming Surgery (GAS), Sex Reassignment Surgery (SRS)
INTRODUCTION
“Gender dysphoria (GD)” refers to psychological anguish due to incongruence between an individual's gender assigned at birth and perceived gender identity.1 As public awareness and societal acceptance of GD increase, the transgender population is expected to continue to grow. In 2016, the Williams Institute estimated the US transgender population to be 1.4 million adults (0.6% of the total population), representing a 100% growth from 15 years earlier.2 Social stigma surrounding transgender identification likely makes these statistics an underestimate of the true transgender population.
Though robust studies are limited, the prevalence of GD in childhood and adolescence is believed to range from 0.5-1.3%3 and varies in severity. Studies have shown that childhood GD persists into adulthood in 10–27% of cases.4, 5, 6 Persistent GD carries with it serious comorbidities.7, 8 A 2015 national survey on transgender individuals9 found that 39% of transgender adults experienced serious psychological distress, compared with only 5% of the US population. 40% of transgender adults had attempted suicide at least once in their lives, nearly nine times the overall U.S. suicide rate of 4.6%; and 1.4% of transgender adults reported living with HIV, nearly 5 times the HIV-positive rate of 0.3% in the overall U.S. population. Rates of depression and anxiety are also higher among transgender adults. Studies evaluating mental health disparities of transgender adults have found that 44–65% of transgender adults reported suffering from depression10, 11, 12 and 35–48% reported suffering from anxiety12, 13, compared with the U.S. population average for depression and anxiety of 7% and 18%, respectively14.
With improved availability of transgender youth health clinics15, rates of children/adolescents referred for care will likely increase. This highlights the importance of understanding how early GD arises within individuals16. Most of our patients referring for genital gender affirming surgery (gGAS) report “knowing” that their gender identities did not match their bodies, and have had GD for “most of” their “entire life,” “starting in childhood.” This suggests that many transgender individuals may live with GD prior to seeking care. Our study aimed to answer the following questions: What is the age at which transgender adults seeking gGAS first experience GD, and how many life-years do transgender adults spend living with untreated GD? Prior studies have examined the age of onset of persistent GD and have shown that many patients report “gender dysphoria” during early adolescence.17, 18, 19, 20, 21 However, the mean earliest age at which adult transgender women (TW) (assigned male sex at birth; AMAB) and men (TM) (assigned female sex at birth; AFAB) first experience GD has not been reported in a United States population of adults seeking gGAS. Data on the length of time transgender people might live with GD and its associated morbidities helps direct patient care and resources. With improved understanding of the typical age of onset of GD, family members, care providers, and teachers can better support young individuals that may have GD. As with other challenging human conditions, early detection of GD, accompanied by early intervention and support, may reduce morbidity and lead to improvements in patient health, quality of life, and survival.
METHODS
Data Collection
The Cedars-Sinai Medical Center Institutional Review Board reviewed and approved this study (IRB #00055933). We performed a retrospective review of consecutive patients that presented to our institution for gGAS consultation between September 2016 and November 2018. Only patients who were presenting for gGAS consultation were included in this study. Patients who were not presenting for gGAS were excluded from this study. All participants were previously diagnosed with GD (per DSM 5 criteria) by 2 mental-health specialists. All patients in this study had both socially transitioned (living full-time as their identified gender) and had undergone gender-affirming hormone therapy (GAHT) for at least a year.
For each patient, the following variables were recorded: gender identity, earliest age at which persistent GD was experienced, age at time of earliest episodic memory, age at start of GAHT, age at start of social transition, past and present mental-health therapy history, past and current suicide ideation and suicide attempts (if any), medical history, surgical history, and other demographic information. We also recorded patients’ statements indicating that the experience of GD was among their earliest memories: for example, we recorded statements such as “I have known all my life,” and “for as long as I can remember.” All data were self-reported by patients and analyzed exactly as stated by patients, without modification or adjustment.
Statistical Analysis
Pearson correlation coefficients were computed to test correlations between variables. Age at earliest memory of GD or first memory, as well as years between first GD and gender transition, were tested with linear regression modeling to covary for both age and gender. Data are presented as means +/- standard deviations (SD). Differences were considered significant where 2-tailed P-values were <.05. All analysis were performed using SAS v9.4 software by SAS Institute Inc. (Cary, NC, USA).
RESULTS
Demographics of the patients in our study are shown in Table 1. A total of 155 transgender women (TW) and 55 transgender men (TM) were included.
Table 1.
Demographic data, sexual orientation details, and mental health comorbidities of patient subjects (n)
| Transgender men |
Transgender women |
|||
|---|---|---|---|---|
| Age (years) at consultation for surgery | n = 55 | % of n | n = 155 | % of n |
| Age (y) 16, and 17-20 | 0 | (0%) | 8 | (5%) |
| 20-29 | 19 | (35%) | 38 | (25%) |
| 30-39 | 13 | (24%) | 29 | (19%) |
| 40-49 | 15 | (27%) | 22 | (14%) |
| 50-59 | 6 | (11%) | 30 | (19%) |
| 60+ | 2 | (4%) | 28 | (18%) |
| Mean (SD) | 35.4 (10.8) | 41.3 (16.3) | ||
| Race | n = 55 | % of n | n = 155 | % of n |
| White (Non-Hispanic) | 26 | (47%) | 84 | (54%) |
| Hispanic | 10 | (18%) | 30 | (19%) |
| Black or African American | 7 | (13%) | 12 | (8%) |
| Asian or Pacific Islander | 4 | (7%) | 19 | (12%) |
| Not Disclosed | 8 | (15%) | 10 | (6%) |
| Sex of sexual partners | n = 52 | % of n | n = 153 | % of n |
| Men | 6 | (12%) | 71 | (46%) |
| Women | 38 | (73%) | 50 | (33%) |
| Both | 8 | (15%) | 32 | (21%) |
| Mental Health Comorbidities | n = 55 | % of n | n = 155 | % of n |
| Depression | 7 | (13%) | 17 | (11%) |
| Anxiety | 5 | (9%) | 10 | (6%) |
| Both | 17 | (31%) | 45 | (29%) |
| Neither | 26 | (47%) | 83 | (54%) |
| Reported History of Suicide Attempt? | n = 48 | % of n | n = 149 | % of n |
| Yes | 10 | (21%) | 45 | (30%) |
| No | 38 | (79%) | 104 | (70%) |
| Mean # of Suicide Attempts (SD) | 1.9 (1.3) | 1.8 (1.7) | ||
| Range | 1-5 | 1-10 | ||
| Reported Current Feelings of Suicide Ideation? | n = 48 | % of n | n = 149 | % of n |
| Yes | 1 | (2%) | 12 | (8%) |
| No | 47 | (98%) | 137 | (92%) |
| Medical HIV Comorbidities, No. of patients | n = 55 | % of n | n = 155 | % of n |
| HIV + | 0 | (0%) | 11 | (7%) |
| HIV - | 55 | (100%) | 144 | (93%) |
Transgender Men
Gender dysphoria history: Of the 55 TM patients included in our study, 41 (75%) reported feeling GD for the first time by age 7, and 53 (96%) reported first experiencing GD by age 13 (Table 2). A total of 80% of patients reported that feelings of GD were among their earliest childhood memories. TM reported remembering their earliest memories at a mean age of 4.70 years. Meanwhile, mean age of GD onset was 6.17 years, with a mode and median of 5 years. The mean number of years that these patients lived with GD prior to beginning gender affirming transition (either surgery, GAHT, or social transition) was 22.90 years. Two of these patients (4%) reported living over fifty years with GD before attempting any gender transition (Table 2).
Table 2.
Earliest age of first memory of gender dysphoria among patient subjects (n) in our study
| Transgender men | Transgender women | |||
|---|---|---|---|---|
| Mean age (y) at time of earliest memory | # of patients n = 30 | # of patients n = 101 | ||
| 4.7 (2.3) | 4.5 (2.0) | |||
| Mean age (y) at first gender dysphoria (GD) | # of patients n = 52 | # of patients n = 155 | ||
| 6.2 (3.1) | 6.7 (3.6) | |||
| Age (y) at first memory of GD, clustered by age group | n = 52 | % of n | n = 155 | % of n |
| Age 2-4 | 16 | (30%) | 38 | (25%) |
| 5-7 | 25 | (48%) | 74 | (48%) |
| 8-10 | 4 | (8%) | 19 | (12%) |
| 11-13 | 5 | (10%) | 17 | (11%) |
| 13+ (max age: 24 years) | 2 | (4%) | 7 | (5%) |
| Reported their earliest memory of GD as amongst their earliest life-memories | n = 30 | % of n | n = 101 | % of n |
| Yes | 24 | (80%) | 82 | (81%) |
| No | 6 | (20%) | 19 | (19%) |
| Number of years patients lived with GD prior to commencing gender transition (nonsurgical) | n = 50 | % of n | n = 150 | % of n |
| < 10 | 7 | (14%) | 20 | (13%) |
| 10-19 | 17 | (34%) | 40 | (27%) |
| 20-29 | 13 | (26%) | 33 | (22%) |
| 30-39 | 6 | (12%) | 23 | (15%) |
| 40-49 | 5 | (10%) | 16 | (11%) |
| 50+ | 2 | (4%) | 18 | (12%) |
| Mean: | 22.9 (12.6) | 27.1 (16.4) | ||
| Range: | 3–58 | 1-68 | ||
Mental-health history: Of the 55 TM patients in our study (Table 1), over 90% of patients reported a history of depression, anxiety, or both; 29 (53%) reported currently suffering from either depression, anxiety or a combination of both. Ten (18%) patients indicated a history of one or more suicide attempts (Table 1). Mean number of lifetime suicide attempts was 1.90 (range: 1–5). Of patients with suicide attempts, only one (10%) reported continued suicidal ideation after initiating either GAHT or social transition. No patients had further suicide attempts after starting transition.
Transgender Women Results
Gender dysphoria history: Of 155 TW patients, 112 (72%) reported feeling GD for the first time by age 7 (Table 2). Eighty-one percent reported that feelings of GD were among their earliest childhood memories. Patients reported that their earliest episodic memories occurred at a mean age of 4.53 years. The mean age of the first onset of GD was 6.71 years, with a mode and median of 5. The mean number of years that these patients lived with GD prior to beginning gender-affirming transition (either surgery, GAHT, or social transition) was 27.14 years (Table 2). Eighteen (12%) patients reported living over 50 years with GD before attempting any form of transition.
Mental health history: Of 155 TW patients, over 90% reported a history of depression, anxiety, or both, with 72 (46%) reporting current depression, anxiety or both. History of one or more suicide attempts was found in 45 (30%) patients (Table 1). The mean number of suicide attempts was 1.81 (range: 1–6). Of patients with prior suicide attempts, 12 (27%) reported continued suicide ideation following commencement of GAHT or social transition, but there were no further suicide attempts after transition. Eleven patients (7%) indicated being HIV+ during their primary visitation (Table 3).
Table 3.
Generational and gender differences related to reported age of earliest recollection of gender dysphoria, and, age of first memory
| Under 40 | 40 and older | P-value | |
|---|---|---|---|
| (n = 109) | (n = 101) | ||
| Age at earliest memory of GD | 6.8 (3.6) | 6.4 (3.4) | 0.182 |
| Age at reported first memory | 4.4 (1.9) | 4.8 (2.2) | 0.356 |
| Years from earliest memory of GD to undergoing gender transition (GAHT or social transition) | 16.0 (7.0) | 37.0 (15.1) | <0.001 |
| Transgender Men | Transgender Women | P-value | |
| (n = 55) | (n = 155) | ||
| Age at earliest memory of GD | 6.2 (3.1) | 6.7 (3.6) | .245 |
| Age at reported first memory | 4.7 (2.3) | 4.5 (2.0) | .653 |
| Years from earliest memory of GD to undergoing gender transition (GAHT or social transition) | 22.9 (12.6) | 27.1 (16.4) | .706 |
Generational Analysis
There was no significant association between current age and age of earliest recollection of GD (r = -0.044, P = .527), suggesting no “generational effect” between older and younger subjects with regards to age of GD onset. (Table 3). Patients that were 40 years and older had an average age of GD onset at 6.4 +/- 3.4 years, which was similar to patients under 40 years old, who had an average age of GD onset at 6.8 +/- 3.6 (P = .182) years.
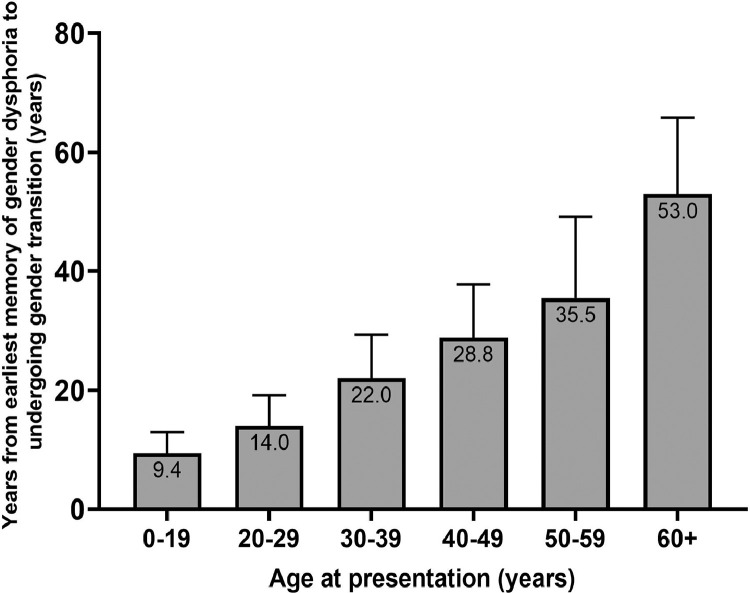
However, there was a significant generational effect with the number of years from GD onset to the start of gender transition (Table 1; Figure 1).: when compared to patients younger than 40 years old, older patients above age 40 reported living over twice as many years with GD before starting gender transition (P < .001).
Figure 1.
Average number of years from earliest memory of gender dysphoria to start of gender transition 338 x 190 mm (300 x 300 DPI).
The TM in this study was significantly younger than the TW. Nonetheless, no significant differences were observed between genders when comparing age of GD onset, age at reported first memory, or the number of years between GD onset and start of gender transition (Table 3) and no significant interaction of age with gender was observed.
DISCUSSION
Age of Earliest Childhood Memories and Age of GD Onset
This study aimed to identify, among a large sample of TM and TW, the age at which adult patients recall their first experience of GD. We were motivated to investigate the age of GD onset, as our patients have consistently reported “knowing” that they are transgender, and have experienced the discomfort of GD, “most of” their “entire life.” As most adults’ earliest complex (episodic) memories are from ages, 22, 23, 24, 25 we also asked our patients the ages at which they had their earliest complex memories. By comparing the earliest age of episodic memory and mean age of GD onset, we sought to estimate the proportion of our adult patient's lives that had been spent with GD and that were subject to recallable memories. This study finds that GD has, on average, an early onset and is experienced prior to age 7 by the majority of TM and TW. Birth sex, age at start of gender transition, sexual orientation, and age at time of gGAS consultation were not independent predictors of the age of GD onset (Table 2, Table 4). Both TM and TW reported a gap of about 2 years between their earliest memories and the age of GD onset.
Table 4.
Sexual orientation differences related to reported age of earliest recollection of gender dysphoria, and, age of first memory. Data presented as means (SD)
| Transgender men |
Transgender women |
|||||
|---|---|---|---|---|---|---|
| Preferred Gender of Sexual Partners | Men | Women | Both | Men | Women | Both |
| (n = 6) | (n = 38) | (n = 8) | (n = 71) | (n = 50) | (n = 32) | |
| Age at presentation | 39.7 (8.9) | 36.5 (11.4) | 29.0 (7.3) | 39.0 (15.5) | 45.0 (16.7) | 41.8 (16.6) |
| Age at earliest memory of GD | 9.8 (3.3) | 5.2 (2.3) | 8.0 (3.8) | 6.6 (3.5) | 6.8 (3.8) | 6.3 (2.9) |
| Years from earliest memory of GD to undergoing gender transition (GAHT or social transition) | 17.0 (5.1) | 25.6 (13.4) | 15.6 (8.2) | 21.7 (12.7) | 34.3 (17.3) | 29.6 (17.2) |
Our data aligns well with studies from the field of memory research, where Oliver Sacks and others have found that for most adults, episodic memories from the first 1–3 years of life cannot be recalled and that memories from ages 3 to 7 are low in number and quality.24, 25, 26 The average age of an adult's earliest recallable memories is age 3.5.22, 23 Our data also aligns with gender identity research, which has found that most children understand gender permanence (ie, fixed identity as a “girl” or “boy”) between 5 and 7 years of age.27 Most of our patients first experienced GD at this age when children naturally grasp the concept of gender. Our findings suggest that those who experience GD tend to experience it close to their entire (recallable) life. Interestingly, despite the approximately two-year gap between earliest memory and earliest experience of GD, nearly identical proportions of TM (80%) and TW (81%) in our study described feelings of GD as among their “earliest memories,” highlighting the impact of GD on their lives.
Impact of GD on Mental Health
Our findings confirm that, for nearly all patients in our series, GD affected childhood and adolescence as much as adulthood. While we did not assess the severity of GD experienced by these patients as children, several studies have reported that untreated GD in childhood has adverse mental and physical health effects, as it does in adulthood.28, 29, 30, 31 Although gender incongruence does not persist for most children that experience it,32 it should be noted that, for the minority of children whose GD persists into adulthood, lack of awareness of the child's experience and symptoms of GD increases the risk that GD will continue untreated throughout early childhood and early adulthood, increasing the risk to delay an adequate support and referral to specialized gender clinics. Given the well-defined morbidity of untreated GD, its cumulative morbidity can clearly be significant.
The transgender adult patients in this study showed elevated incidences of depression, anxiety, and suicidality in comparison with national averages. These findings corroborate numerous studies showing that transgender individuals are at greater risk of mental-health conditions compared to the general population.33, 34, 35 Suicidality in our patients was assessed not only before and after gGAS, but throughout gender transition preceding surgery (ie, after social transition and after commencing GAHT). Our data shows a considerable decrease in suicidal ideation following commencement of gender-affirming treatment (Table 1). Poor mental health often stems from discrimination and rejection from individuals’ families and communities.36, 37 Support and education of youth with early GD have been shown to significantly improve development and quality of life: gender-dysphoric children that are supported in their transition by their families have normative levels of depression and decreased or minimal elevations in anxiety.38 Given the high prevalence of suicidality, depression, and anxiety among transgender communities, it follows that proper measures should be taken to address the underlying condition– untreated GD.
Association of GD With HIV Positivity
In our cohort, 7% of TW patients were HIV-positive (Table 1). This is considerably higher than the national average of 0.3%9. Psychological conditions of depression and anxiety are linked to elevated HIV risk, particularly among young TW.39 Fear of being outed may cause gender dysphoric youths to hide their conditions from family members, primary care physicians, and social workers, thus creating a barrier to proper healthcare and treatment.40 The earlier that children are identified as being gender dysphoric, the earlier that preventative measures can be implemented to reduce psychological comorbidities that contribute to unsafe sexual practices. Currently, health services available to transgender youth are relatively limited as compared to adult services.41 Greater efforts should be made to make youth services more available nationwide.
Years of Untreated GD Before Gender Transition
This study highlights how transgender adults tend to live many years with untreated GD before starting any form of gender-affirming transition (social, hormonal, or surgical). When we consider that life-years of any untreated condition are a robust predictor for morbidity and decreased quality of life,42 the number of life-years associated with GD and its associated morbidities is striking and serves as a compelling reason for intervention. Many studies have confirmed that gender-affirming treatments lead to significantly improved quality of life and mental health.7, 8, 21, 43, 44
Relevance to Healthcare Access and Public Policy
When we compared the ages at which patients first experienced GD, we found no significant difference between younger patients (< age 40) and older patients (> age 40) (Table 3). However, we did find that older patients waited a significantly longer time before starting gender transition (ie, with social transition or GAHT) (Table 3; Figure 1). This generational trend suggests that, with increased societal acceptance of transgender people and increased access to transgender-related health services, patients have been starting gender transition (including surgery) earlier in life. Nonetheless, transgender youth and adults still face considerable barriers to healthcare access. Studies have shown that compared to cis-gender lesbian, gay, or bisexual patients, transgender adults were more likely to be uninsured, experience discrimination in healthcare settings, and postpone care due to discrimination.45 Despite the 2014 announcement that federal Medicare will cover gGAS for patients who meet WPATH Standards of Care guidelines (V. 7, 2011)43, 46 many U.S. states continue to deny coverage for gender-affirming related care under their State Medicaid Insurance plans.47
As healthcare reforms and societal acceptance for transgender individuals continue to improve, it is increasingly important that the public has access to healthcare professionals who, at minimum, can interact effectively with transgender youth, and who ideally are properly trained to address fully the needs of this growing population. A 2010 study of 464 physicians and residents at a United States medical school found that most physicians did not believe they had proper training to address issues surrounding sexual orientation and gender identity among pediatric patients.48 Additionally, if an adolescent stated that he or she was not sexually active, 41% of physicians in this study reported that they would not ask additional sexual health-related questions; the majority of physicians also reported that they would not ask patients about sexual orientation or gender identity if an adolescent presented with depression, suicidal thoughts, or had attempted suicide.48
The well-documented possibility of childhood GD persisting into adulthood4, 5, 6 highlights the need to educate medical and childcare providers in child/gender development and transgender-health needs. Domains that merit attention include sensitivity to questions about gender identity from children and adolescents, understanding of how children may express struggles with gender incongruence (eg, anxiety, depression and self-harm), and skills to constructively invite discussion with children/adolescents to better ascertain their needs.
Lastly, it should be noted that the results of this study demonstrate that TM and TW suffer from the morbidities commonly associated with GD nearly equally. In our work, for example, both genders reported similar rates of depression and anxiety. Ages of GD onset were similar between both genders, and patients of both genders reported that their experiences with GD were their earliest memories. Both genders reported similar rates of suicidality and decreases in suicidal ideation following treatment. The commonality of these findings across both genders supports both the importance and value of early access to care to transgender youth.
LIMITATIONS
Potential limitations of this study include a possible lack of generalizability. As this study only included patients presenting for gGAS, our findings might not be representative of transgender people who do not seek gGAS. Another potential limitation of this study is that patients were not queried as to the severity of their GD during early childhood. Therefore, the full morbidity of GD experienced during childhood was not studied directly. Finally, although we gathered data on patients’ history of mental-health comorbidities, we did not gather information on timing of these respective diagnoses and thus we are unable to definitively link these conditions to the diagnoses of GD.
CONCLUSION
Our findings suggest that GD first manifests in early childhood for the majority of adult transgender patients and that GD is a part of patients’ earliest memories, spanning the majority of patients’ recallable lives. Patients often spend many years living with untreated GD, which is associated with depression, anxiety, suicidality, and HIV. GD is a condition of childhood as much as adulthood. Access to gender-transition-related care is warranted and significantly improves quality of life.
Our findings are not meant to advocate for the early treatment of all children who report GD, but rather to highlight that, for the subset of children with GD that persists into adulthood, untreated GD can cause a significant impact on quality of life. Children may hide GD from their parents and healthcare providers, so providers treating children and adolescents should be sensitive both to patients who openly report GD, as well as to those that display other potential signs of GD such as anxiety, depression, and self-harm. Early intervention to help youth navigate their gender identities and gender transitions will likely reduce morbidity and improve quality of life.
Footnotes
Conflict of Interest: The authors report no conflicts of interest.
Funding: None.
STATEMENT OF AUTHORSHIP
Conceptualization, M.Z., N.Y., C.B., A.F., M.M.G.; Methodology, M.Z., N.Y., C.B., A.F., M.M.G.; Formal Analysis, M.Z., N.Y., C.B., A.F., M.M.G.; Investigation, M.Z., N.Y., C.B., A.F., M.M.G.; Resources, M.Z., N.Y., C.B., A.F., M.M.G.; Data Curation, M.Z., N.Y., C.B., A.F., M.M.G.; Writing – Original Draft, M.Z., N.Y., C.B., A.F., M.M.G.; Writing – Review & Editing, M.Z., N.Y., C.B., A.F., M.M.G.; Project Administration, M.Z., N.Y., C.B., A.F., M.M.G.
REFERENCES
- 1.American Psychiatry Association. What is gender dysphoria?; Available at: https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria. Accessed May 14, 2021.
- 2.Flores AR, Herman J, Gates GJ, et al. The Williams Institute, UCLA School of Law; Los Angeles, CA: 2016. How many adults identify as transgender in the United States? p. 1. online resource. [Google Scholar]
- 3.Zucker K.J. Epidemiology of gender dysphoria and transgender identity. Sex Health. 2017;14:404–411. doi: 10.1071/SH17067. [DOI] [PubMed] [Google Scholar]
- 4.Drummond KD, Bradley SJ, Peterson-Badali M, et al. A follow-up study of girls with gender identity disorder. Dev Psychol. 2008;44:34–45. doi: 10.1037/0012-1649.44.1.34. [DOI] [PubMed] [Google Scholar]
- 5.Steensma TD, McGuire JK, Kreukels BP, et al. Factors associated with desistence and persistence of childhood gender dysphoria: A quantitative follow-up study. J Am Acad Child Adolesc Psychiatry. 2013;52:582–590. doi: 10.1016/j.jaac.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 6.Wallien M.S., Cohen-Kettenis P.T. Psychosexual outcome of gender-dysphoric children. J Am Acad Child Adolesc Psychiatry. 2008;47:1413–1423. doi: 10.1097/CHI.0b013e31818956b9. [DOI] [PubMed] [Google Scholar]
- 7.Padula W.V., Heru S., Campbell J.D. Societal implications of health insurance coverage for medically necessary services in the U.S. transgender population: A cost-effectiveness analysis. J Gen Intern Med. 2016;31:394–401. doi: 10.1007/s11606-015-3529-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Costa R., Colizzi M. The effect of cross-sex hormonal treatment on gender dysphoria individuals' mental health: a systematic review. Neuropsychiatr Dis Treat. 2016;12:1953–1966. doi: 10.2147/NDT.S95310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James S.E., Herman J.L., Rankin S., Keisling M., Mottet L., Anafi M. National Center for Transgender Equality; Washington, DC: 2016. The report of the 2015 U.S. transgender survey. [Google Scholar]
- 10.Tan KKH, Ellis SJ, Schmidt JM, et al. Mental health inequities among transgender people in Aotearoa New Zealand: Findings from the Counting Ourselves Survey. Int J Environ Res Public Health. 2020;17 doi: 10.3390/ijerph17082862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becerra-Culqui TA, Liu Y, Nash R, et al. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141 doi: 10.1542/peds.2017-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bockting WO, Miner MH, Romine RES, et al. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103:943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Budge S.L., Adelson J.L., Howard K.A. Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. J Consult Clin Psychol. 2013;81:545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- 14.Anxiety and Depression Association of America. Anxiety and Depression Facts & Statistics. 2020 https://adaa.org/understanding-anxiety/facts-statistics Available from. Accessed May 14, 2021. [Google Scholar]
- 15.Hsieh S., Leininger J. Resource list: Clinical care programs for gender-nonconforming children and adolescents. Pediatr Ann. 2014;43:238–244. doi: 10.3928/00904481-20140522-11. [DOI] [PubMed] [Google Scholar]
- 16.Lawlis SM, Donkin HR, Bates JR, et al. Health concerns of transgender and gender nonconforming youth and their parents upon presentation to a transgender clinic. J Adolesc Health. 2017;61:642–648. doi: 10.1016/j.jadohealth.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 17.Simonsen R, Hald GM, Giraldi A, et al. sociodemographic study of danish individuals diagnosed with transsexualism. Sex Med. 2015;3:109–117. doi: 10.1002/sm2.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okabe N, Sato T, Matsumoto Y, et al. Clinical characteristics of patients with gender identity disorder at a Japanese gender identity disorder clinic. Psychiatry Res. 2008;157:315–318. doi: 10.1016/j.psychres.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 19.Nieder TO, Herff M, Cerwenka S, et al. Age of onset and sexual orientation in transsexual males and females. J Sex Med. 2011;8:783–791. doi: 10.1111/j.1743-6109.2010.02142.x. [DOI] [PubMed] [Google Scholar]
- 20.Kreukels BP, Haraldsen IR, De Cuypere G, et al. A European network for the investigation of gender incongruence: The ENIGI initiative. Eur Psychiatry. 2012;27:445–450. doi: 10.1016/j.eurpsy.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Heylens G, Elaut E, Kreukels BP, et al. Psychiatric characteristics in transsexual individuals: Multicentre study in four European countries. Br J Psychiatry. 2014;204:151–156. doi: 10.1192/bjp.bp.112.121954. [DOI] [PubMed] [Google Scholar]
- 22.West T.A., Bauer P.J. Assumptions of infantile amnesia: Are there differences between early and later memories? Memory. 1999;7:257–278. doi: 10.1080/096582199387913. [DOI] [PubMed] [Google Scholar]
- 23.Tustin K., Hayne H. Defining the boundary: Age-related changes in childhood amnesia. Dev Psychol. 2010;46:1049–1061. doi: 10.1037/a0020105. [DOI] [PubMed] [Google Scholar]
- 24.Rubin D.C. The distribution of early childhood memories. Memory. 2000;8:265–269. doi: 10.1080/096582100406810. [DOI] [PubMed] [Google Scholar]
- 25.Josselyn S.A., Frankland P.W. Infantile amnesia: A neurogenic hypothesis. Learn Mem. 2012;19:423–433. doi: 10.1101/lm.021311.110. [DOI] [PubMed] [Google Scholar]
- 26.Sacks O. The power of music. Brain. 2006;129(Pt 10):2528–2532. doi: 10.1093/brain/awl234. [DOI] [PubMed] [Google Scholar]
- 27.Ruble DN, Taylor LJ, Cyphers L, et al. The role of gender constancy in early gender development. Child Dev. 2007;78:1121–1136. doi: 10.1111/j.1467-8624.2007.01056.x. [DOI] [PubMed] [Google Scholar]
- 28.Spack NP, Edwards-Leeper L, Feldman HA, et al. Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics. 2012;129:418–425. doi: 10.1542/peds.2011-0907. [DOI] [PubMed] [Google Scholar]
- 29.Reisner S.L., Biello KB, Hughto JMW, et al. Psychiatric diagnoses and comorbidities in a diverse, multicity cohort of young transgender women: Baseline findings from project lifeskills. JAMA Pediatr. 2016;170:481–486. doi: 10.1001/jamapediatrics.2016.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Veale JF, Watson RJ, Peter T, et al. Mental health disparities among canadian transgender youth. J Adolesc Health. 2017;60:44–49. doi: 10.1016/j.jadohealth.2016.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Vries AL, Doreleijers TA, Steensma TD, et al. Psychiatric comorbidity in gender dysphoric adolescents. J Child Psychol Psychiatry. 2011;52:1195–1202. doi: 10.1111/j.1469-7610.2011.02426.x. [DOI] [PubMed] [Google Scholar]
- 32.Steensma TD, Biemond R, Boer FD, et al. Desisting and persisting gender dysphoria after childhood: A qualitative follow-up study. Clin Child Psychol Psychiatry. 2011;16:499–516. doi: 10.1177/1359104510378303. [DOI] [PubMed] [Google Scholar]
- 33.Clements-Nolle K., Marx R., Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. J Homosex. 2006;51:53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 34.Colizzi M., Costa R., Todarello O. Transsexual patients' psychiatric comorbidity and positive effect of cross-sex hormonal treatment on mental health: Results from a longitudinal study. Psychoneuroendocrinology. 2014;39:65–73. doi: 10.1016/j.psyneuen.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 35.Adams N.J., Vincent B. Suicidal thoughts and behaviors among transgender adults in relation to education, ethnicity, and income: A systematic review. Transgend Health. 2019;4:226–246. doi: 10.1089/trgh.2019.0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koken J.A., Bimbi D.S., Parsons J.T. Experiences of familial acceptance-rejection among transwomen of color. J Fam Psychol. 2009;23:853–860. doi: 10.1037/a0017198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russell ST, Ryan C, Toomey RB, et al. Lesbian, gay, bisexual, and transgender adolescent school victimization: Implications for young adult health and adjustment. J Sch Health. 2011;81:223–230. doi: 10.1111/j.1746-1561.2011.00583.x. [DOI] [PubMed] [Google Scholar]
- 38.Olson KR, Durwood L, DeMeules M, et al. Mental health of transgender children who are supported in their identities. Pediatrics. 2016;137 doi: 10.1542/peds.2015-3223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: The role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102:1751–1757. doi: 10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fisher CB, Fried AL, Desmond M, et al. Perceived barriers to HIV prevention services for transgender youth. LGBT Health. 2018;5:350–358. doi: 10.1089/lgbt.2017.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Puckett JA, Cleary P, Rossman K, et al. Barriers to gender-affirming care for transgender and gender nonconforming individuals. Sex Res Social Policy. 2018;15:48–59. doi: 10.1007/s13178-017-0295-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nobili A., Glazebrook C., Arcelus J. Quality of life of treatment-seeking transgender adults: A systematic review and meta-analysis. Rev Endocr Metab Disord. 2018;19:199–220. doi: 10.1007/s11154-018-9459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13:165–232. [Google Scholar]
- 44.Wierckx K., Caenegem EV, Elaut E, et al. Quality of life and sexual health after sex reassignment surgery in transsexual men. J Sex Med. 2011;8:3379–3388. doi: 10.1111/j.1743-6109.2011.02348.x. [DOI] [PubMed] [Google Scholar]
- 45.Macapagal K., Bhatia R., Greene G.J. Differences in healthcare access, use, and experiences within a community sample of racially diverse lesbian, gay, bisexual, transgender, and questioning emerging adults. LGBT Health. 2016;3:434–442. doi: 10.1089/lgbt.2015.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garcia M.C., N, Thomas P, Ralph D. Vol. 36. American Urologic Association; Linthicum, MD: 2017. Genital gender affirming surgery for transgender patients. AUA Update Series 2017. [Google Scholar]
- 47.Zaliznyak M, Jung EE, Bresee C, et al. Which U.S. States’ medicaid programs provide coverage for gender-affirming hormone therapy and gender-affirming genital surgery for transgender patients?: A state-by-state review, and a study detailing the patient experience to confirm coverage of services. J Sex Med. 2021;18:410–422. doi: 10.1016/j.jsxm.2020.11.016. [DOI] [PubMed] [Google Scholar]
- 48.Kitts R.L. Barriers to optimal care between physicians and lesbian, gay, bisexual, transgender, and questioning adolescent patients. J Homosex. 2010;57:730–747. doi: 10.1080/00918369.2010.485872. [DOI] [PubMed] [Google Scholar]