Abstract
Introduction
Previously, incisionless plication (IP) for correction of congenital penile curvature (CPC) has been performed after penile degloving via a circumscribing incision.
Aim
To describe our experience with non-degloving incisionless penile plication (NDIP) for correction of CPC and compare these outcomes with those of men who underwent degloving incisionless penile plication (DIP).
Methods
We conducted a retrospective review of men ≤ 45 years of age who underwent incisionless penile plication for correction of CPC between 2008 and 2020 at two adult tertiary hospitals. Patients underwent either NDIP, performed through a 2-3 cm longitudinal incision along the proximal-to-mid shaft opposite the point of maximum penile curvature, or DIP via a sub-coronal circumscribing incision.
Main Outcome Measures
Surgical and patient-reported outcomes were compared between the non-degloving and degloving groups.
Results
Among the 38 men (mean age, 26 years) who met the inclusion criteria, 25 underwent NDIP, including 6 patients with biplanar curvature (2 Ventral, 4 Dorsal, 6 Lateral). Thirteen patients underwent DIP, including 1 patient with biplanar curvature (1 ventral, 1 lateral). Curvature reduction was 50 ± 23 degrees for the NDIP group and 36 ± 10 degrees for the DIP group (P = .04). Five (20%) patients in the NDIP group and nine (69%) patients in the DIP group experienced a reduction in stretched penile length following plication (SPL) (P = .01). One patient in the NDIP group underwent an additional plication for recurrent curvature.
Conclusion
Both NDIP and DIP are safe and highly efficacious techniques for the correction of CPC.
Kusin SB, Khouri RK, Dropkin BM, et al., Plication for Correction of Congenital Penile Curvature: With or Without Degloving?. Sex Med 2021;9:100462.
Key Words: Congenital Penile Curvature, Plication, Surgical Outcomes, Non-Degloving
INTRODUCTION
Congenital penile curvature (CPC) is defined as curvature of the erect penis without associated hypospadias or Peyronie's disease.1 CPC often comes to clinical attention in young adulthood when erections accentuate the penile curvature. While the overall incidence of CPC is estimated to be between 0.5% and 10%, the incidence of clinically significant CPC is likely much lower.2, 3, 4
CPC has been postulated to originate by differential development of the tunica albuginea of the corpora cavernosa.5 Disorganization of collagen fibers within the tunica albuginea on the convex side of the curvature may result in increased elasticity of the tunica albuginea and ultimately curvature of the penis.5 Treatment for CPC is considered if the patient or their partner experiences difficulties during intercourse due to penile curvature.
Plication and corporoplasty of the tunica albuginea are the established, safe, and effective mainstay techniques for correction of CPC.5,6 Corporoplasty can be performed with (eg, Nesbit or Yachia) or without excision of tunica albuginea.7 Tunical plication is performed in an incisionless fashion (IP). Access to the tunica albuginea for either corporoplasty or plication can be achieved either via a circumcising incision with penile degloving or via a 2-3 cm incision over the penile shaft opposite the point of maximum curvature without penile degloving.7
Degloving and incisionless plication (DIP) has been well established as an effective treatment option for CPC by multiple prior studies.5,7 Two large case series have also reported highly successful outcomes following Nesbit-style excisional corporoplasty via a non-degloving approach for CPC correction.8,9 We have previously demonstrated the safety and efficacy of non-degloving incisionless penile plication (NDIP) used in several hundred men with Peyronie's disease.10 Are comparable benefits realized when NDIP is utilized in the CPC population? Herein we present the largest reported series of men with CPC treated with NDIP and compare these outcomes with those of men who underwent DIP.
MATERIAL AND METHODS
After institutional review board approval (IRB # STU-2019-1354), a retrospective review was conducted of all men ≤ 45 years old who underwent penile plication for correction of CPC between January 2008 and June 2020 at two adult tertiary hospitals. Patients were identified from the electronic medical record based on a diagnosis of CPC documented during the initial office visit. Patient data was abstracted and reviewed by the study authors and recorded in a secure database.
Surgery was offered to men with at least 15 degrees of curvature and bother, regardless of direction of deformity. During this period, Hospital A and Hospital B, each had one fellowship-trained reconstructive urologist who performed all plications using the same surgical techniques. Each reconstructive urologist was continuously employed by their institution during the study period. Patients with evidence of Peyronie's disease or hypospadias as well as patients with a history of penile trauma or fracture were excluded. All other patients whose histories and physical exams were consistent with CPC and whose medical records included documented follow-up were included in this analysis. Documented follow up was performed by the attending surgeon and consisted of a wound evaluation as well as patient-reported assessment of deformity correction, sexual function, and satisfaction with the procedure. Complications were classified according to the Clavien-Dindo classification system. All complications observed or communicated to the medical team were documented in the EMR. They were then reviewed by the study authors and recorded in the database.
Both SPL and penile curvature were documented pre- and post-operatively according to the procedure documented in the surgical technique. Patients with biplanar curvature had each plane of curvature analyzed as a separate case.
Surgical Technique
Following a thorough pre-operative discussion and obtainment of informed consent, the patient is prepped using sterile technique and general anesthesia is induced. Preoperative stretched penile length (SPL) is measured with a metal ruler by compressing the suprapubic fat pad and measuring the dorsal distance between the pubic symphysis and the tip of the glans while the penis is maximally stretched. An artificial erection is induced via an intracorporal injection of 10 μg of alprostadil. If the initial erectile response is poor, a second dose of 20 μg of alprostadil is administered to ensure that an erection sufficient for curvature evaluation is achieved. Intraoperative photographs are obtained to document the angle of deformity before and after plication. Angles are measured to the nearest degree between a line drawn from the base of the penis along the proximal shaft intersecting another line extending from the urethral meatus along the distal shaft.
DIP is performed via a circumscribing sub-coronal incision and the penis is degloved to the base of the penis. NDIP is performed through a 2-3 cm longitudinal incision along the proximal or mid shaft opposite the point of maximum curvature (Figure 1). The technique for NDIP has been described in previous literature in the context of Peyronie's disease.10, 11, 12, 13, 14, 15 For both DIP and NDIP the initial dissection is carried through the Dartos and Buck's fascia down onto the tunica albuginea. Senn retractors and/or vein retractors are then used to facilitate exposure of the tunica albuginea throughout the length of the penis. Starting proximally, the tunica albuginea is plicated using permanent 2-0 Ethibond (Ethicon Inc, Sommerville, NJ, USA) in a buried, interrupted fashion(Figure 2).11,14 The penis is straightened and the incision is centered over the plication stitch prior to tying down each knot.
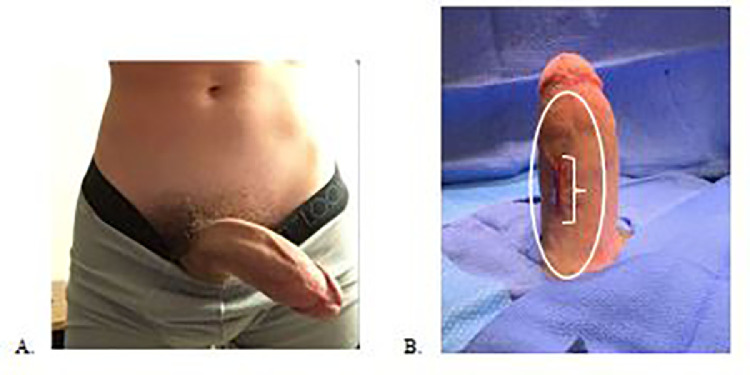
Figure 1.
(A) Preoperative photograph of a 17 year old patient with 60 degrees of left lateral CPC with torsion. (B) Postoperative photograph of same patient following NDIP performed with 7 plication sutures placed via a 2.5 cm right paramedian incision (white bracket). White oval demonstrates areas of tunica albuginea easily accessible through this incision.
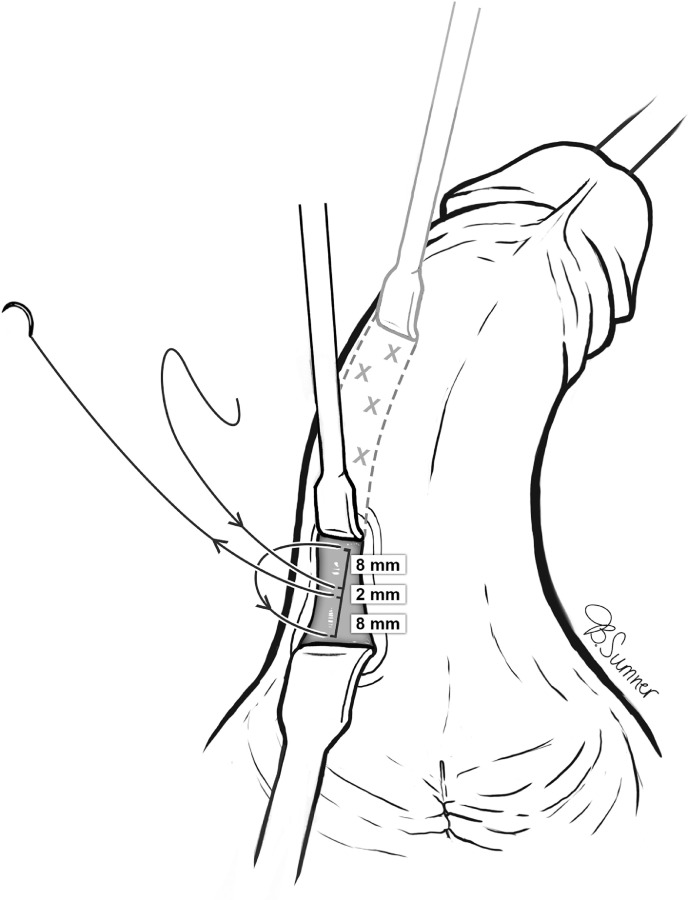
Figure 2.
Incisionless plication suture, placed in “near to far, far to near” format in longitudinal orientation over 18 mm opposite to the side of curvature. X's indicate additional plication sites for correction of a left-dorsal curvature (Morey).
For ventral curvature, the neurovascular bundle is identified to avoid injury from suture placement. The dorsal plication sutures are placed in a thin sulcus made by dissecting lateral to the dorsal penile vein and medial to the dorsal nerves. Following each suture, penile curvature is reassessed by manually compressing the proximal corporal bodies against the pubic symphysis to simulate an erection. Additional sutures are placed until adequate correction of the curvature is achieved.
Following correction, the incision is closed in three layers. First, Buck's and Dartos fascia are closed in two layers with 4-0 Monocryl (Ethicon Inc). The skin is then closed in a subcuticular manner with 4-0 Monocryl, and Dermabond skin glue is applied (Ethicon Inc). Following closure, measurement of the angle of deformity and SPL are repeated. The total number of plication sutures used for each plane is also recorded. A penile ring block is performed using 0.25% plain Bupivacaine. A lightly compressive Coban (3M Company, Maplewood, MN, USA) dressing is applied. All patients are discharged home after surgery. Upon discharge, patients are directed to replace the Coban dressing daily for a week and to abstain from sexual activity for four weeks post-operatively.
Follow-up visits are conducted 5 to 6 weeks after plication. Patients are instructed to engage in sexual activity in the week prior to their post-operative visit. Patients receive a wound evaluation as well as an assessment of SPL, deformity correction, sexual function, and satisfaction with the procedure. After the initial post-operative visit, patients are seen on an as-needed basis.
Statistical Methods
Data were collected in Microsoft Excel (Microsoft, Redmond, WA). For men with biplanar curvature each plane was analyzed as a separate case. Wilcoxon Signed-Rank tests were performed to test for normality. Mean and standard deviation (SD) were reported for normally distributed data, and median and interquartile ranges (IQR) were reported for non-normally distributed data. Mean, median, standard deviation, and interquartile ranges were formulated using Microsoft Excel. Groups were compared with Pearson correlation coefficient for linear correlation, chi-squared tests for categorical variables, t-tests for normally distributed continuous variables and Mann-U Whitney tests for non-normal distributions using PRISM 8.42 (Graph Pad Software, La Jolla, CA, USA). All statistical tests performed were two-sided with P < .05 considered statistically significant.
RESULTS
Surgical Outcomes
Between January 2008 and June 2020, 42 adult men with CPC underwent NDIP or DIP. Pre and postoperative data were available for 38 (90%) of the patients (mean age 26 ± 7.6). Among patients receiving care at hospital A, 25 were treated with NDIP and 3 (who requested simultaneous circumcision) were treated with DIP. All patients receiving care at hospital B were treated with DIP. Of the 25 men who underwent NDIP, six patients had biplanar curvature (2 Ventral, 4 Dorsal, 6 Lateral). Thirteen patients underwent DIP, including one patient who had biplanar curvature (1 ventral, 1 lateral). Ventral curvature was the most common direction of curvature in the cohort (49%). Table 1 provides an overview of curvatures in the study population.
Table 1.
Surgical and patient-reported outcomes. for patients with biplanar curvature, each plain is counted separately
| Penile Plication Approach | Non-degloving (n = 25) | Penile Degloving (n = 13) | P value |
|---|---|---|---|
| Age | 28 ± 8.3 | 23 ± 4.8 | 0.06 |
| Direction of Curvature, count (Directions) | 31 (5 D, 15 V, 11 L) | 14 (3 D, 7 V, 4 L) | 0.86 |
| Preoperative Curvature, degrees | 52 ± 21 | 43 ± 13 | 0.15 |
| Postoperative Curvature, degrees | 2 ± 5 | 6 ± 10 | 0.05 |
| Reduction in Curvature, degrees | 50 ± 23 | 36 ± 10 | 0.04 |
| Number of Sutures, count | 6.8 ± 4.1 | 4.4 ± 2.2 | 0.04 |
| Correction Per Suture, degrees | 9 ± 5 | 10 ± 4 | 0.40 |
| Pre-Operative SPL, cm | 16.1 ± 1.4 | 14.2 ± 2.9 | < 0.01 |
| Post-Operative SPL, cm | 16.0 ± 1.6 | 12.8 ± 2.9 | < 0.01 |
| Decrease in SPL, cm | 0.1 ± 0.2 | 1.1 ± 0.8 | < 0.01 |
Data are presented as mean ± standard deviation.
D = dorsal; V = ventral; L = lateral; SPL = stretched penile length
Mean pre-operative curvature was 52 ± 21 degrees for NDIP patients and 43 ± 13 degrees for DIP patients (P = .15). Mean curvature reduction was 50 ± 23 degrees after NDIP and 36 ± 10 degrees after DIP (P = .04). Final postoperative curvature was less after NDIP (2 ± 5 vs 6 ± 10 degrees, P = .05). An average of 6.8 ± 4.1 sutures were used per NDIP patient with 9 ± 5 degrees of correction per suture compared to an average of 4.4 ± 2.2 sutures and 10 ± 4 degrees of correction per patient with DIP (P = .04 and P = .40, respectively).
We found no significant change in SPL in the cohort overall (p = 0.46). Average preoperative SPL was 15.4 ± 2.3 cm across this cohort, roughly 1 cm longer than SPL in a large cohort of Peyronie's disease patients.12 Five (20%) patients in the NDIP group and nine (69%) patients in the DIP group experienced a reduction in SPL (P = .01).
Of the five NDIP patients who experienced a decrease in SPL, none had a decrease ≥ 1.5 cm. All five of these NDIP patients had a loss of 0.5 cm. Of the nine DIP patients with a decrease in SPL, one patient had a decrease of 0.5 cm, three patients had a decrease of 1 cm, one patient had a decrease of 1.5 cm, two patients had a decrease of 2 cm, and one patient had a decrease of 2.5 cm. Four of the DIP patients had a decrease in SPL ≥1.5 cm. The average SPL loss in these nine patients was 1.4 cm (range 0.5-2.5 cm).
Penile shortening was not associated with degree of preoperative curvature across the two groups (r = 0.18). No patient with a decrease in SPL after surgery reported a change in sexual function.
Perioperative Outcomes
Postoperative complications were rare. One Clavien-Dindo Grade II complication (3.7%) was noted in a NDIP patient; the patient had a wound infection and was successfully treated with a short course of oral antibiotics. One Clavien-Dindo Grade III complication (7.7%) was noted in a DIP patient; the patient required a circumcision revision due to ventral lymphedema. Mild pain with erections was common immediately following surgery. Two (8%) NDIP patients and two (15%) DIP patients continued to have de-novo penile pain with erections 4-6 weeks following surgery. The pain was not severe enough to limit sexual activity or function and improved over time in all cases.
Patient-Reported Outcomes
Median follow up was similar for NDIP and DIP patients 40 (IQR 33-81) vs 46 (IQR 32-102) days, P = .98. At the 4 to 6 week follow up visit, 25 (100%) NDIP patients had satisfactory results, defined as curvature < 20 degrees with erection and reported satisfaction. Twelve (92%) DIP patients were satisfied and one patient was unsatisfied due to persistent curvature > 20 degrees. One NDIP patient reported new onset erectile dysfunction post-operatively and was successfully managed with a PDE-5 inhibitor. No patients reported bothersome penile shortening or loss of sensation. One patient in the NDIP group who initially presented with a 70 degree ventral curvature underwent an additional plication for recurrent 30 degree ventral curvature that was first noticed three months after the initial plication.
DISCUSSION
This is the largest series to report on the use of non-degloving incisionless penile plication for the correction of CPC. The existing literature on NDIP for CPC is limited to two reports of men included within larger pooled analyses that did not report on outcomes specifically related to NDIP for CPC (n =2 and n = unspecified/12, respectively).16,17 Robust literature has shown low complication rates and high patient satisfaction both when using degloving incisionless penile plication to correct CPC and when using NDIP for Peyronie's disease.5,7,10,18, 19, 20, 21 The results of the present study now add support for NDIP for correction of CPC, with 24/25 (96%) reporting satisfaction after undergoing this treatment and only one patient requiring a repeat plication.
Surgical correction with Nesbit-style excisional corporoplasty, Yachia-style incisional corporoplasty, or incisionless penile plication is considered the gold standard for correction of CPC.6,7 All of these strategies have been demonstrated in multiple studies to yield success rates of > 90%. Alternative options such as incision and grafting are less frequently utilized due to higher complication rates and low concern over penile shortening given the long penile length typically observed with CPC.7 Selection of surgical technique appears to be largely determined by surgeon experience and preference.
We observed several differences in outcomes of NDIP and DIP in this study, including differences in the number of sutures placed per case and the overall degree of correction per case. We believe that incisionless penile plication is the most attractive treatment option for CPC because it completely preserves the tunica albuginea and is completed efficiently and reproducibly. Combining this technique with a non-degloving approach minimizes devascularization of the penile skin and tunica dartos and provides improved access to the proximal corporal bodies, which has previously been demonstrated to decrease the failure rate of NDIP for Peyronie's disease.9,15 We have not found any patient complaints which would justify the additional surgical time and trauma required for incisional and excisional techniques. Using residual curvature ≤ 20 degrees to define success, NIDP and DIP yielded a combined success rate of 95% (36/38) across the two cohorts in the present study.
A common concern with penile plication is post-operative penile shortening and change in sexual function. We found no significant change in SPL in our cohort overall (P = .46). NDIP resulted in a mean SPL decrease of just 0.1 ± 0.2 cm, with no NDIP patients having had a decrease ≥1.5 cm. These findings are consistent with prior studies that have shown that penile plication does not significantly reduce stretched penile lenth.12,13,19 New onset sexual dysfunction was also seen at low rates, with 2.6% (1/38) of our patients reporting new onset dysfunction. This is similar to findings by Cantoro et al. who reported worsening onset of erectile function in 3.3% of their study population of 60 CPC patients who underwent degloving penile plication.18 Of course, preoperative counseling regarding all possible complications is required prior to proceeding with penile plication.
Previous surgical algorithms suggested that penile plication be utilized mainly for mild-to-moderate curvature.22 Recent studies have shown penile plication to be successful in the correction of a wide range of deformities.11,14,18,23 In the present study, of the 12 patients with curvature ≥ 60 degrees, only one patient (8.3%) had residual curvature > 20 degrees. One patient with NDIP had residual curvature > 20 degrees and elected for a second NDIP. Our experience further suggests that penile plication is effective for all severities of curvatures, with NDIP specifically facilitating highly successful straightening.
Several additional theoretical benefits of NDIP deserve mention. The vasculature to the penile skin and underlying dartos run longitudinally along the penile shaft. A longitudinal, but not circumscribing, incision allows for preservation of the majority of these vessels.9 Proximal suture placement minimizes the risk of sensory complications with the glans. Previous studies have reported glans sensation decrease in up to 37% of degloving plication patients.19 No NDIP patients in our series reported a decrease in glans sensation. By avoiding a circumscribing incision the risk of complications due to mobilization of the foreskin, such as distal ischemia or lymphatic complications, are also avoided.11,24
Limitations
The retrospective nature of our study includes inherent biases. Postoperative follow up was limited. We used straightening, rigidity, stretched penile length, and overall satisfaction as measures to assess patient satisfaction. In the future, prospective use of standardized questionnaires, such as the Patient Global Impression of Improvement Index and International Index of Erectile Function, could help standardize results.25 The differences between NDIP and DIP outcomes could be confounded by differences between Hospitals A and B. In addition, it is possible that differences between the surgeons performing the procedures may have contributed to variability in outcomes. However, all procedures were done by fellowship trained reconstructive urologists utilizing standardized techniques, and all data points were measured and recorded according to standard protocols.
CONCLUSIONS
NDIP and DIP are safe and effective techniques that can be used to correct a wide variety of CPC malformations with few complications and minimal penile shortening. NDIP spares men the discomfort and requisite recovery associated with circumscribing incisions and complete penile degloving. These findings support the broad use of NDIP for correction of CPC.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of Interest: Dr. Allen Morey receives honoraria for being a guest lecturer and/or meeting participant for Boston Scientific and Coloplast Corp. No other authors have a disclosure to report.
Statement of Authorship: Conceptualization, S.B.K., R.K.K., P.N.D., A.S.B., J.K.K., A.I.G., and A.F.M.; Methodology, S.B.K., R.K.K., P.N.D., B.M.D., E.E.W., A.S.B., J.K.K., A.I.G., and A.F.M.; Formal Analysis, S.B.K., R.K.K., P.N.D., B.M.D., E.E.W., A.S.B., J.K.K., A.I.G., and A.F.M; Investigation, S.B.K., R.K.K., P.N.D., E.E.W., A.S.B., and J.K.K; Data Curation, S.B.K., R.K.K., P.N.D., E.E.W., and J.K.K; Writing – Original Draft, S.B.K., R.K.K., P.N.D., A.S.B., J.K.K., A.I.G., and A.F.M; Writing-Review & Editing, S.B.K., R.K.K., P.N.D., A.S.B., J.K.K., A.I.G., and A.F.M; Supervision, A.I.G. and A.F.M.; Project Administration, E.E.W.
REFERENCES
- 1.Devine CJ, Blackley SK, Horton CE, et al. The surgical treatment of chordee without hypospadias in Men. The Journal of Urology. 1991;146:325–329. doi: 10.1016/S0022-5347(17)37783-2. [DOI] [PubMed] [Google Scholar]
- 2.Baskin LS, Duckett JW, Lue TF. Penile curvature. Urology. 1996;48:347–356. doi: 10.1016/s0090-4295(96)00213-0. [DOI] [PubMed] [Google Scholar]
- 3.Montag S, Palmer LS. Abnormalities of penile curvature: chordee and penile torsion. ScientificWorldJournal. 2011;11:1470–1478. doi: 10.1100/tsw.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yachia D. Our experience with penile deformations: incidence, operative techniques, and results. J Androl. 1994;15:63s–68s. [PubMed] [Google Scholar]
- 5.Makovey I, Higuchi TT, Montague DK, et al. Congenital penile curvature: update and management. Curr Urol Rep. 2012;13:290–297. doi: 10.1007/s11934-012-0257-x. [DOI] [PubMed] [Google Scholar]
- 6.Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: AUA Guideline. Journal of Urology. 2015;194:745–753. doi: 10.1016/j.juro.2015.05.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sokolakis I, Hatzichristodoulou G. Current trends in the surgical treatment of congenital penile curvature. Int J Impot Res. 2020;32:64–74. doi: 10.1038/s41443-019-0177-0. [DOI] [PubMed] [Google Scholar]
- 8.Popken G, Wetterauer U, Schultze-Seemann W, et al. A modified corporoplasty for treating congenital penile curvature and reducing the incidence of palpable indurations. BJU Int. 1999;83:71–75. doi: 10.1046/j.1464-410x.1999.00887.x. [DOI] [PubMed] [Google Scholar]
- 9.Perdzyński W, Adamek M. Three anatomical levels: possibilities to decrease invasiveness of reconstructive surgery for congenital penile curvature. Cent European J Urol. 2017;70:280–288. doi: 10.5173/ceju.2017.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reddy RS, McKibben MJ, Fuchs JS, et al. Plication for Severe Peyronie's Deformities Has Similar Long-Term Outcomes to Milder Cases. J Sex Med. 2018;15:1498–1505. doi: 10.1016/j.jsxm.2018.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Dugi DD, 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int. 2010;105:1440–1444. doi: 10.1111/j.1464-410X.2009.08991.x. [DOI] [PubMed] [Google Scholar]
- 12.Hudak SJ, Morey AF, Adibi M, et al. Favorable patient reported outcomes after penile plication for wide array of peyronie disease abnormalities. J Urol. 2013;189:1019–1024. doi: 10.1016/j.juro.2012.09.085. [DOI] [PubMed] [Google Scholar]
- 13.Adibi M, Hudak SJ, Morey AF. Penile plication without degloving enables effective correction of complex Peyronie's deformities. Urology. 2012;79:831–835. doi: 10.1016/j.urology.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 14.Chung PH, Tausch TJ, Simhan J, et al. Dorsal plication without degloving is safe and effective for correcting ventral penile deformities. Urology. 2014;84:1228–1233. doi: 10.1016/j.urology.2014.05.064. [DOI] [PubMed] [Google Scholar]
- 15.Reddy RS, Yi YA, Fuentes J, et al. Preventing the need for revision surgery after penile plication reconstruction of Peyronie's deformities. Transl Androl Urol. 2020;9:82–86. doi: 10.21037/tau.2019.07.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chien GW, Aboseif SR. Corporeal plication for the treatment of congenital penile curvature. J Urol. 2003;169:599–602. doi: 10.1097/01.ju.0000046638.36848.a7. [DOI] [PubMed] [Google Scholar]
- 17.Kadirov R, Coskun B, Kaygisiz O, et al. Penile plication with or without degloving of the penis results in similar outcomes. Sex Med. 2017;5:e142–e147. doi: 10.1016/j.esxm.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cantoro U, Polito M, Lacetera V, et al. Plication corporoplasty for congenital penile curvature: our results with long-term follow-up. Int Urol Nephrol. 2014;46:1741–1746. doi: 10.1007/s11255-014-0728-8. [DOI] [PubMed] [Google Scholar]
- 19.Leonardo C, De Nunzio C, Michetti P, et al. Plication corporoplasty versus Nesbit operation for the correction of congenital penile curvature. A long-term follow-up. Int Urol Nephrol. 2012;44:55–60. doi: 10.1007/s11255-011-9976-z. [DOI] [PubMed] [Google Scholar]
- 20.Basiri A, Sarhangnejad R, Ghahestani SM, et al. Comparing absorbable and nonabsorbable sutures in corporeal plication for treatment of congenital penile curvature. Urol J. 2011;8:302–306. [PubMed] [Google Scholar]
- 21.Hsieh JT, Liu SP, Chen Y, et al. Correction of congenital penile curvature using modified tunical plication with absorbable sutures: the long-term outcome and patient satisfaction. Eur Urol. 2007;52:261–266. doi: 10.1016/j.eururo.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 22.Levine LA, Lenting EL. A surgical algorithm for the treatment of Peyronie's disease. J Urol. 1997;158:2149–2152. doi: 10.1016/s0022-5347(01)68184-9. [DOI] [PubMed] [Google Scholar]
- 23.Chung PH, Scott JF, Morey AF. High patient satisfaction of inflatable penile prosthesis insertion with synchronous penile plication for erectile dysfunction and Peyronie's disease. J Sex Med. 2014;11:1593–1598. doi: 10.1111/jsm.12530. [DOI] [PubMed] [Google Scholar]
- 24.Garaffa G, Sacca A, Christopher AN, et al. Circumcision is not mandatory in penile surgery. BJU Int. 2010;105:222–224. doi: 10.1111/j.1464-410X.2009.08763.x. [DOI] [PubMed] [Google Scholar]
- 25.Hellstrom WJ, Feldman R, Rosen RC, et al. Bother and distress associated with Peyronie's disease: validation of the Peyronie's disease questionnaire. J Urol. 2013;190:627–634. doi: 10.1016/j.juro.2013.01.090. [DOI] [PubMed] [Google Scholar]