Abstract
Objectives
Knowledge is lacking on the interaction between fear of movement (FOM) and work‐related physical and psychosocial factors in the development and persistence of musculoskeletal disorders (MSDs).
Methods
In this cross‐sectional study, 305 healthcare workers from several Belgian hospitals filled out a questionnaire including sociodemographic factors, work‐related factors (social support, autonomy at work, workload, and physical job demands), FOM, and MSDs for different body regions during the past year. Path analysis was performed to investigate (1) the association between the work‐related factors, FOM and MSDs, and (2) the moderating role of FOM on the association between the work‐related factors and MSDs among healthcare workers.
Results
Complaints were most frequently located at the neck–shoulder region (79.5%) and lower back (72.4%). Physical job demands (odds ratio [OR] 2.38 and 95% confidence interval [CI] 1.52–3.74), autonomy at work (OR 1.64 CI [1.07–2.49]) and FOM (OR 1.07 CI [1.01–1.14] and OR 1.12 CI [1.06–1.19]) were positively associated with MSDs. Healthcare workers who experienced high social support at work (OR 0.61 CI [0.39–0.94]) were less likely to have MSDs. Fear of movement interacted negatively with workload (OR 0.92 CI [0.87–0.97]) and autonomy at work (OR 0.94 CI [0.88–1.00]) on MSDs.
Conclusions
Work‐related physical and psychosocial factors as well as FOM are related to MSDs in healthcare workers. FOM is an important moderator of this relationship and should be assessed in healthcare workers in addition to work‐related physical and psychosocial factors to prevent or address MSDs.
Keywords: fear avoidance, fear of movement, pain beliefs, pain cognitions, physical job demands, work‐related psychosocial factors
1. INTRODUCTION
Musculoskeletal disorders (MSDs) are one of the major concerns in Europe. More than half the workers with MSDs are absent at work due to their complaints. 1 The economic consequences are substantial for employees, employers, and society. 1 The healthcare sector is one of the occupational settings that is frequently confronted with MSDs. 1 The one‐year prevalence of MSDs among nurses ranges between 33% and 88%, with the lower back, neck, shoulders, and knees being the most commonly affected areas. 2 Similar prevalence rates have been found for other healthcare professionals. 3
Healthcare workers are exposed to high physical job demands. 2 , 4 They must transfer patients, handle heavy objects, stand for a prolonged period, repeatedly execute movements, and adopt uncomfortable postures. 2 , 4 These tasks have been related to MSDs in the lower back, knees, shoulders, and wrists or hands. 2 , 3 , 5 , 6 , 7 , 8 , 9 , 10 In addition, psychosocial stressors at work could be involved in the occurrence and persistence of MSDs in healthcare workers. 2 , 4 Research suggests that high demands (e.g., high workload, time pressure, mental and emotional stress), low job control, and a lack of social support are associated with pain in different regions of the body. 2 , 3 , 5 , 7 , 8 , 9 , 10 , 11 However, evidence on physical and psychosocial stressors at work remains inconclusive.
With respect to MSDs, pain‐related cognitions and perceptions such as fear of movement (FOM), which is the belief that certain movements or activities will cause damage to the body, must also be taken into account. 12 , 13 , 14 , 15 Multiple underlying mechanisms have been proposed to explain how FOM contributes to MSDs. 12 , 13 , 14 , 15 First, FOM may lead to overestimation of perceived sensations and amplification of the cognitive response to pain. 14 Due to this altered functioning of the central nervous system, normal bodily sensations are perceived as painful and the pain experience is amplified. 14 Second, cognitions about pain can alter behavior and thereby influence the risk of MSDs. 15 An individual might develop FOM if an activity has caused pain, or even if the individual believes that certain movements can harm the body. 15 In this situation, it seems logical to avoid specific activities. Although short‐term avoidance may prevent or decrease MSDs, long‐term avoidance interferes with valuable work activities and puts the individual at risk of disuse, disability, and prolonged pain. 13 , 15
To date, only a few studies have evaluated the role of FOM in healthy individuals. Research indicates that FOM is related to MSDs in different body regions, both in healthcare workers and the general population. 6 , 7 , 16 , 17 Specifically, FOM is related to new as well as ongoing MSDs. 6 However, there is little knowledge on the interaction between FOM and work‐related physical and psychosocial factors in the development and persistence of MSDs. Only Jensen et al. evaluated whether the relationship between physical job demands and lower back pain depends on FOM. 6 They were not able to demonstrate a significant effect. Nevertheless, the hypothesis that high FOM levels lead to an increased risk of MSDs in combination with specific work‐related factors is worth exploring. Such interactions might contribute to the literature on the role of work‐related physical and psychosocial factors in MSDs.
Therefore, this study aimed to investigate (1) the association between work‐related physical and psychosocial factors, FOM, and MSDs in different body regions among healthcare workers, and (2) the moderating role of FOM on the association between work‐related factors and MSDs.
2. METHODS
2.1. Study design
Between September 2017 and January 2018, Belgian healthcare workers (Dutch‐ or French‐speaking) were asked to complete a self‐reported questionnaire and drop them in a sealed box while waiting for their periodical health examination by occupational physicians at several locations of a Belgian Occupational Service for Prevention and Protection at work. The target locations were geographically spread across the country to obtain a representative sample of the Belgian working population.
2.2. Measures
The self‐reported questionnaire consisted of questions on MSDs, sociodemographic factors, work‐related physical and psychosocial factors, and FOM.
Musculoskeletal disorders were assessed using items from the validated Dutch Musculoskeletal Questionnaire. 18 The participants were asked to indicate how frequently they experienced pain or discomfort in different parts of the body during the previous year using four options. The body parts were grouped as follows: neck–shoulder (neck, shoulders, and upper back), lower back, upper extremities (elbows, wrists, and hands), and lower extremities (hips, knees, ankles, and feet). Previous studies have used the same subdivision. 17 The participants were categorized as having musculoskeletal complaints when they answered “Yes, on a regular basis,” or “Yes, long‐lasting” on at least one part of the body in one region.
To measure fear of movement, the Tampa Scale for Kinesiophobia was used. 19 This scale was developed to measure the fear of getting (re)injured during exercise or other physical activities. The scores range from 13 to 52, with high scores indicating high FOM levels. Previous studies have shown support for the validity and reliability of the TSK. 20 Several authors preferred removing the four reverse‐scored items from the original 17‐items scale since this improved the psychometric parameters. 21 Therefore, the 13‐items Tampa Scale for Kinesiophobia (TSK‐13) was used in this study; it showed good reliability (Cronbach's α = 0.85).
The work‐related factors assessed in this study were physical job demands, workload, autonomy at work, and social support. Physical job demands were measured using five items from the Dutch Musculoskeletal Questionnaire. 18 The participants rated the extent to which they performed each of several tasks at work. Originally, this scale consisted of 11 items. The five selected items have high factor loadings on the first factor, and the scale had good reliability (Cronbach's α = 0.82). High scores represented physically demanding jobs. The scales for workload (three items) and social support from colleagues and direct supervisor (four items) were derived from the Short Inventory to Monitor Psychosocial Hazards (SIMPH). 22 The SIMPH is a validated and reliable questionnaire that surveys major psychosocial hazards at work through 11 different scales. 22 Both scales for workload (Cronbach's α = 0.88) and social support (Cronbach's α = 0.75) had good to acceptable reliabilities. Autonomy at work was measured using four items from the Questionnaire on the Experience and Evaluation of Work, a validated Dutch questionnaire measuring psychosocial well‐being and work‐related stress. 23 The scale for autonomy had acceptable reliability (Cronbach's α = 0.77). High scores indicated unfavorable outcomes on the scale for workload and favorable outcomes on the scales for social support and autonomy.
2.3. Statistical analysis
Univariate descriptive statistical analyses were performed using SPSS 23.0 statistical software package (SPSS Inc., Chicago, IL). All other analyses were performed using the MPlus 7.4 statistical software package (Muthén & Muthén, Los Angeles, CA). Figure 1 gives an overview of the relations that were examined in this study. Path analysis was performed in MPlus on a model with FOM, social support, autonomy at work, workload and physical job demands as independent variables, with age and gender as control variables and with the different types of MSDs (neck–shoulder, lower back, upper extremities, and lower extremities) as dependent variables. Interactions between FOM and each of the other independent variables (resulting in four interaction terms for each type of MSD) were also included in the model. First, the entire model was tested. Then, the interaction effects that contributed least to the model were removed in a step‐by‐step approach. The final model, next to the main effects of the independent and control variables, only included these interaction effects with a p‐value of .05 or lower. To include as much information as possible (given missing data), maximum likelihood estimation with robust standard errors (MLR‐estimation) and Monte Carlo integration were used, and the variances of the covariates were introduced into the model. 24 To interpret the possible interaction effects, all continuous variables were centered when testing the model.
FIGURE 1.
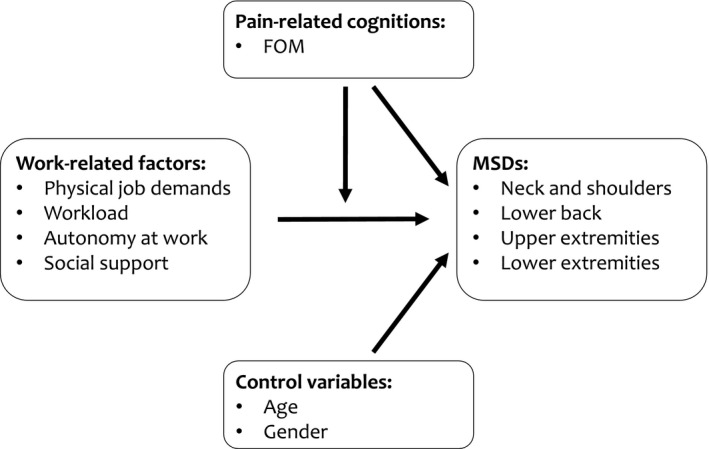
Theoretical model of relationships between work‐related factors, FOM and MSDs. FOM, fear of movement; MSDs, musculoskeletal disorders
3. RESULTS
3.1. Group characteristics
In total, 305 healthcare workers (95% Dutch‐speaking and 5% French‐speaking) completed the questionnaire. Table 1 presents the sociodemographic characteristics and the prevalence of MSDs during the past year. These data are in line with the distribution of age and gender within a Belgian population of healthcare workers, studied by the Belgian Statistical Office. 25 Complaints were most frequently related to the neck–shoulder region (79.5%) and lower back (72.4%). The mean score on the TSK‐13 was 24.74 (±6.76). The distribution of scores on TSK‐13 is presented in Figure 2.
TABLE 1.
Descriptive characteristics of the study population
| n (%) | |
|---|---|
| Occupation | n = 305 |
| Nurse | 102 (33.4%) |
| Nursing assistant | 146 (47.9%) |
| Paramedic | 57 (18.7%) |
| Age | n = 298 |
| Younger than 25 years | 50 (16.8%) |
| 25–34 years | 78 (26.2%) |
| 35–44 years | 78 (26.2%) |
| 45 years or older | 92 (30.9%) |
| Gender | n = 300 |
| Women | 264 (88%) |
| Men | 36 (12%) |
| Work regime | n = 288 |
| Full‐time | 90 (31.3%) |
| Between full‐time and half‐time | 133 (46.2%) |
| Half‐time (or less) | 65 (22.5%) |
| Education | n = 301 |
| Lower secondary school | 33 (10.9%) |
| Higher secondary school | 127 (42.2%) |
| College of higher education or university | 141 (46.9%) |
| Tenure in function | n = 264 |
| 0–4 years | 91 (34.5%) |
| 5–9 years | 61 (23.1%) |
| 10–14 years | 32 (12.1%) |
| (+) 15 years | 80 (30.3%) |
| Musculoskeletal disorders over the past year | |
| Neck and shoulders | 225/283 (79.5%) |
| Lower back | 202/279 (72.4%) |
| Upper extremities | 112/261 (42.9%) |
| Lower extremities | 170/266 (63.9%) |
| Minimum one region with complaints | 271/290 (93.4%) |
FIGURE 2.
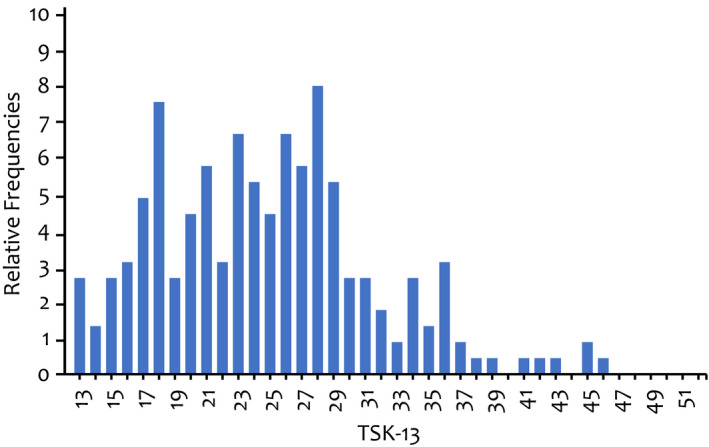
Fear of Movement: distribution of scores on TSK‐13 (n = 225). High scores on TSK‐13 indicate high Fear of Movement levels. TSK‐13, Tampa scale of kinesiophobia‐13 items version
3.2. Effect of FOM and work‐related physical and psychosocial factors on MSDs
Figure 3 presents the model with the significant main and interaction effects of the associations between work‐related factors, FOM and MSDs. Both FOM and work‐related physical and psychosocial factors were significantly associated with MSDs in healthcare workers (see Table 2). FOM was positively associated with pain in the neck–shoulder region and lower extremities. Furthermore, autonomy at work was positively related to lower back pain and physical job demands to MSD in the upper extremities. Social support was shown to be a protective factor of MSDs: the higher the social support at work, the lower the risk of lower back pain. A similar trend was observed in the upper and lower extremities. Age was positively associated with MSD in the upper extremities.
FIGURE 3.
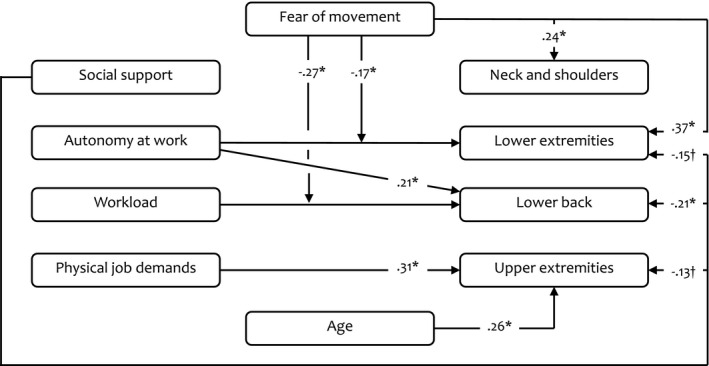
Main and interaction effect of the associations between work‐related factors, FOM and MSDs. This model presents only the significant effects with standardized beta coefficients. Other estimated effects were not included. *p < .05; †p < .10. FOM, fear of movement; MSDs, musculoskeletal disorders
TABLE 2.
Effect of FOM and work‐related physical and psychosocial factors on MSDs and the moderating role of FOM on this relationship
| Neck and shoulders | Lower back | Upper extremities | Lower extremities | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Stand. B‐coeff | OR [CI] | Stand. B‐coeff | OR [CI] | Stand. B‐coeff | OR [CI] | Stand. B‐coeff | OR [CI] | ||
| Main effects | |||||||||
| FOM | 0.24 a | 1.07 [1.01–1.14] | −0.02 | 0.99 [0.94–1.05] | 0.09 | 1.03 [0.98–1.08] | 0.37 a | 1.12 [1.06–1.19] | |
| Social support | −0.12 | 0.75 [0.46–1.22] | −0.21 a | 0.60 [0.39–0.94] | −0.13 b | 0.71 [0.49–1.05] | −0.15 b | 0.70 [0.43–1.04] | |
| Autonomy at work | −0.02 | 0.95 [0.60–1.51] | 0.21 a | 1.64 [1.07–2.49] | 0.07 | 1.18 [0.82–1.71] | 0.02 | 1.04 [0.70–1.53] | |
| Workload | 0.06 | 1.13 [0.79–1.62] | 0.04 | 1.09 [0.80–1.48] | 0.00 | 1.01 [0.74–1.37] | −0.01 | 0.97 [0.70–1.35] | |
| Physical job demands | 0.12 | 1.38 [0.86–2.22] | 0.10 | 1.29 [0.83–2.02] | 0.31 a | 2.38 [1.52–3.74] | 0.10 | 1.33 [0.88–2.01] | |
| Control variables | |||||||||
| Gender | 0.09 | 1.67 [0.71–3.97] | −0.01 | 1.04 [0.44–2.46] | −0.06 | 0.70 [0.28–1.70] | 0.01 | 1.09 [0.44–2.69] | |
| Age | −0.07 | 0.99 [0.96–1.02] | −0.04 | 0.99 [0.97–1.02] | 0.26 a | 1.05 [1.02–1.07] | 0.07 | 1.01 [0.99–1.04] | |
| Moderation effects of FOM | |||||||||
| Social support | ns | ns | ns | ns | |||||
| Autonomy at work | ns | ns | ns | −0.17 a | 0.94 [0.88–1.00] | ||||
| Workload | ns | −0.27 a | 0.92 [0.87–0.97] | ns | ns | ||||
| Physical job demands | ns | ns | ns | ns | |||||
Abbreviations: CI, confidence interval around the odds ratio; FOM, fear of movement; MSDs, musculoskeletal disorders; ns, not significant; OR, odds ratio; Stand. B‐coeff, standardized beta coefficients.
p < .05.
p < .10.
3.3. Impact of FOM on the relation between work‐related physical and psychosocial factors and MSDs
The results are summarized in the lower part of Table 2. Fear of movement had a negative interaction effect on the relationship between autonomy at work and MSD in the lower extremities (see Figure 4A). Healthcare workers with higher FOM levels but lower levels of autonomy at work were at higher risk of MSD in the lower extremities than those with higher levels of autonomy at work. For healthcare workers with lower FOM levels, they were more likely to experience MSD in the lower extremities when they had higher levels of autonomy at work compared to lower levels of autonomy at work. Additionally, workers with higher FOM levels reported MSD in the lower extremities more frequently than workers with lower FOM levels. This difference in risk between healthcare workers with higher and lower levels of FOM was especially true in the case of lower levels of autonomy at work, but decreased when healthcare workers experienced more autonomy. Further, FOM negatively interacted with workload in the prediction of lower back pain (see Figure 4B). Healthcare workers with higher FOM levels but lower workloads were at higher risk of MSD in the lower back than those with higher workloads. Fear of movement was associated with lower odds of pain in the lower back among healthcare workers with higher workloads and higher odds of pain in the lower back among healthcare workers with lower workloads.
FIGURE 4.
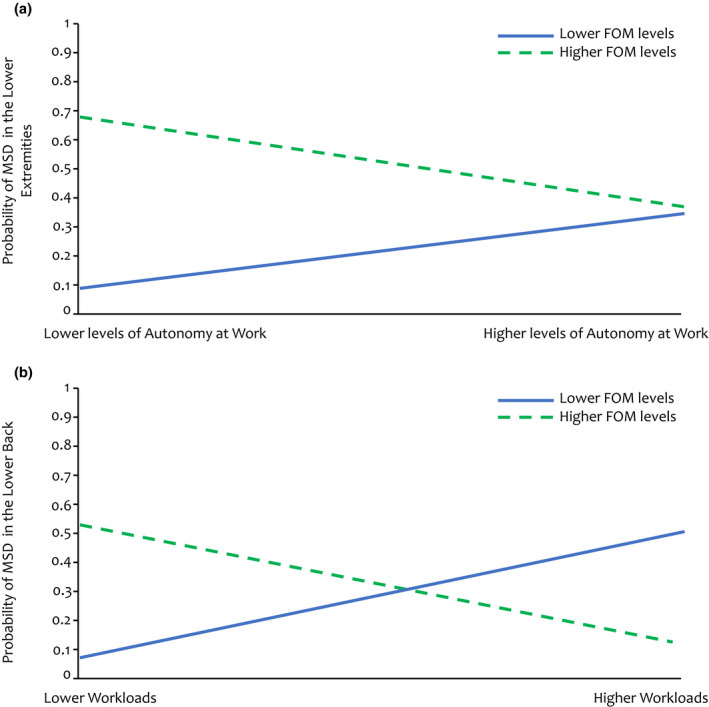
Interaction effects between FOM and work‐related factors in the prediction of MSDs in healthcare workers. (A) Interaction of FOM on the relationship between autonomy and MSDs in the lower extremities; (B) interaction of FOM on the relationship between workload and MSDs in the lower back. FOM, fear of movement; MSDs, musculoskeletal disorders
4. DISCUSSION
This study aimed to investigate (1) the association between work‐related physical and psychosocial factors, FOM and MSDs in different body regions among healthcare workers, and (2) the moderating role of FOM on the association between work‐related factors and MSDs.
The results indicate a high prevalence of MSDs in the past year in different body regions, with 93.4% of the healthcare workers reporting pain in at least one of the regions. These prevalence rates are in line with those reported in previous studies. 2 , 3
Concerning the main effects, this study found that FOM is an independent predictor of MSD in the neck–shoulder region and lower extremities. Previous studies have found similar results. 7 , 17 In contrast to other studies, we found no significant relationship between FOM and MSDs in other regions such as the lower back. 6 , 16 This can be explained as follows: The mean TSK‐13 score in our study was rather low (24.74), which indicates that most healthcare workers do not struggle with FOM. 26 Since FOM is related to absenteeism and forms a barrier for return to work, it is reasonable that some healthcare workers with FOM are on sick leave. 27 , 28 Therefore, they were not included in the analysis. Regardless, our results support the hypothesis that FOM plays an important role in the development or maintenance of MSDs in healthcare workers. Next, the results show that physical job demands are related to MSDs of the upper extremities. Healthcare workers frequently lift and perform recurrent movements engaging the elbows, wrists, and fingers, which might contribute to this risk. 2 Previous research found similar results but linked transferring patients, lifting heavy objects, and standing in uncomfortable positions to MSDs in other regions such as the lower back. 2 , 3 , 5 , 6 , 7 , 8 , 9 , 10 For psychosocial factors, social support is a protective factor for pain in the lower back, and similar trends were noted for other regions. Good collaboration and support at work can prevent MSDs. 2 , 7 , 8 , 9 , 10 , 11 A supportive environment might help with physical job demands and reduce distress by dividing the work or completing difficult tasks together. 9 Furthermore, a strong team might cope better with a suddenly increased workload (e.g., when a colleague is on sick leave). In the case of poor social support, workers might be afraid to ask colleagues for help. Consequently, they force themselves to work in suboptimal conditions. Our results show that autonomy at work contributes to lower back pain. The positive association between autonomy at work and work engagement could support these findings. 29 It is possible that healthcare workers with autonomy at work put in extra effort to perform their jobs. Therefore, they could be exposed to higher physical and mental demands. However, previous studies have shown a protective role of job control and autonomy at work on the occurrence of MSDs. 2 , 3 , 7 , 9 , 10 , 11 Finally, workload did not predict MSDs in the current study. It seems that personal and contextual factors play a role in the relationship between work‐related physical and psychosocial factors and MSDs. A study in Europe showed that nurses who are dissatisfied with their physical job demands are at a higher risk of MSDs than those who are satisfied. 8 The lack of ergonomic devices to assist with physical job demands has been linked to MSDs as well. 8 , 9 Another study reported that nurses who participate in regular recreational physical activity are at low risk of MSDs. 30 These nurses might cope better with physical work demands. Finally, research has shown an improvement in perceived stress at work due to stress management interventions. 31 Healthcare workers with adequate stress management skills might cope better with psychosocial stressors, such as high workloads. Future studies should consider personal and contextual factors when evaluating the relationship between work‐related physical and psychosocial factors and MSDs in healthcare workers.
Further, this study demonstrates that the relationship between work‐related physical and psychosocial factors and MSDs in healthcare workers depends on FOM. First, FOM moderates the association between autonomy at work and pain in the lower extremities. FOM was associated with higher odds of MSDs among the healthcare workers with lower levels of autonomy at work. These workers might be fearful when performing certain activities and lack influence in the planning or execution of their tasks. Consequently, they may experience increased muscle tone or engage in altered movement patterns and focus on sensory input related to pain, all of which increase the risk of MSDs. 12 , 14 On the other hand, healthcare workers with higher FOM levels and higher levels of autonomy at work were less at risk of MSDs than those with lower levels of autonomy at work. Autonomy at work might create opportunities to avoid fearful activities and, hence, reduce painful experiences. 15 In the case of high levels of autonomy at work, the difference in risk of MSDs in the lower extremities decreased substantially between healthcare workers with higher and lower levels of FOM. Due to the association between autonomy and work engagement, healthcare workers with lower levels of FOM might be more willing to expose themselves to physically demanding tasks to provide better care for their patients. 29 This would probably not be the case for healthcare workers with higher levels of FOM. Due to long‐lasting avoidance, these workers might have decreased physical capacity and be less prepared (e.g., suboptimal movement patterns or exaggerated bracing) when confronted with physically demanding tasks, still placing them at risk of MSDs. 13 , 15 Second, the relationship between workload and MSD of the lower back depends on FOM. Healthcare workers with lower FOM levels but higher workloads were at higher risk of MSD in the lower back than those with lower workloads. High workloads might be associated with high physical job demands (e.g., increased number and hasty execution of tasks and long time in uncomfortable positions). 32 Surprisingly, FOM was associated with lower odds of pain in the lower back among healthcare workers with higher workloads. The underlying mechanism is unclear in this situation. Finally, and contrary to our expectations, there was no significant effect of FOM on the relationship between physical job demands and MSDs. Although these results are in agreement with those of Jensen and colleagues, we believe that suboptimal movement patterns and overestimation of bodily sensations place healthcare workers with high physical demands at a high risk of developing MSDs. 6 , 12 , 14 Possibly, this group was already on sick leave and, therefore, not included in this study. 27 , 28 This is the second study to evaluate the moderating role of FOM on the relationship between work‐related physical and psychosocial factors and MSDs, so further research is needed. 6 Nevertheless, our results suggest that FOM should be considered when evaluating the relationship between work‐related physical and psychosocial factors and MSDs.
This study adds value to the current literature and has important strengths. First, the results show that FOM as well as physical and psychosocial factors at work are related to MSDs in different body regions among healthcare workers. We suggest that the occupational assessment for the risk of MSDs should include pain‐related cognitions besides work‐related physical and psychosocial factors. Consequently, a personalized and multifactorial intervention trajectory can be implemented. A review by Van Hoof and colleagues showed insufficient evidence for interventions that focus on isolated work‐related factors. 33 Most of the included studies focused on stress management and ergonomic training, where interventions such as exercise and advice to stay active showed promising results. The curative sector uses, for example, pain education and graded activity to target FOM and improve physical functioning. 34 , 35 , 36 It might be worthwhile to provide pain education in the management of MSDs at work to employees who struggle with FOM as well as to gradually increase their work activities. Next, our results show that FOM can influence the relationship between work‐related physical and psychosocial factors and MSDs. This interaction might explain the inconclusive results in the literature on the role of work‐related physical and psychosocial factors in MSDs and should be considered in future studies along with other personal and contextual factors. Based on the interactions between FOM and work‐related factors, it appears to be more beneficial to prioritize FOM optimization. For example: increasing autonomy at work in healthcare workers with higher FOM levels might lead to opportunities to avoid fearful activities, which could deteriorate the condition of the healthcare worker in the long run. 13 , 15 Studies have shown that maladaptive pain‐related cognitions must be targeted before activity‐based interventions. 36 People who are convinced that certain activities are truly harmful to the body could be less eager to engage in treatments focusing on exercise, physical activity, or ergonomic advice than those who are not. Future studies must evaluate whether the strategies that prioritize targeting unhelpful cognitions or perceptions about pain, such as FOM, are useful at the workplace.
The study limitations merit attention as well. First, this was a cross‐sectional study, which made it impossible to demonstrate causal relationships. Since the impact of FOM on MSDs in employees is a relatively new research focus, longitudinal studies are needed to investigate the causal relationship between FOM and work‐related MSDs. Next, only healthcare workers who had their periodical health examination were recruited in this study, and the assessment of risk factors was based on self‐report. This may have caused selection bias and reporting bias due to selective recall, social desirability, or negative affectivity. However, every healthcare worker, independent of health status, undergoes periodical health examinations, and the questionnaires to measure work‐related physical and psychosocial risk factors, FOM, and MSDs have been validated in epidemiological studies. 18 , 19 , 20 , 22 , 23 Finally, this study only evaluated fear avoidance as a maladaptive response to pain. There has been increasing interest in other responses such as an endurance response. 37 , 38 , 39 , 40 Avoidance is characterized by fear of pain, fear of movement, and catastrophizing, while an endurance‐based response is characterized by thought suppression, distraction from pain and pain minimization. These individuals will persist in executing their daily activities despite pain. Without paying the necessary attention to recovery, they might put themselves at increased risk of overloading and, consequently, increased and prolonged pain. An endurance‐based pain response is also associated with disability and a depressive mood. 38 Future research should evaluate the interaction between other pain coping strategies and factors at work in the development and persistence of MSDs as this might have consequences for treatment.
5. CONCLUSION
Work‐related physical and psychosocial factors as well as FOM are related to MSDs in healthcare workers. The influence of personal and contextual factors could explain the inconclusive results in the literature on the relationship between work‐related physical and psychosocial factors and MSDs. This study demonstrated that FOM is an important moderator of this relationship. The occupational evaluation of healthcare workers should consider work‐related physical and psychosocial factors as well as FOM. Consequently, a personalized intervention that targets all factors contributing to MSDs can be implemented. Based on the interaction between FOM and work‐related physical and psychosocial factors, it might be worthwhile to prioritize FOM optimization. Future studies are needed to corroborate our findings and evaluate if the relation between factors at work and MSDs is influenced by other pain response strategies. Furthermore, it is needed to explore the additional benefits of including modalities that target FOM in workplace interventions to prevent or address MSDs in healthcare workers.
DISCLOSURE
Approval of research protocol: This study was approved by the Social Ethics Commission of the KU Leuven (dd 17‐08‐2017) and carried out according to Belgian and international privacy and ethical legislation. Informed consent: N/A. Competing interests: None declared. Registry and registration no. of the study/trial: N/A. Animal studies: N/A. Conflict of interest: The authors declare that there is no conflict of interest.
AUTHOR CONTRIBUTION
L.D. designed the study and scientific model; E.D. carried out the statistical analyses; S.K. drafted the manuscript; all authors interpreted the study results and contributed with manuscript revisions and approved the final version of the manuscript.
ACKNOWLEDGEMENTS
The authors have not received a specific grant for this research from any funding agency in the public or commercial sectors.
Keyaerts S, Godderis L, Delvaux E, Daenen L. The association between work‐related physical and psychosocial factors and musculoskeletal disorders in healthcare workers: Moderating role of fear of movement. J Occup Health. 2022;64:e12314. doi: 10.1002/1348-9585.12314
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. De Kok J, Vroonhof P, Snijders J. Work‐Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU. European Agency for Safety and Health at Work (EU‐OSHA); 2019. https://data.europa.eu/doi/10.2802/66947 [Google Scholar]
- 2. Soylar P, Ozer A. Evaluation of the prevalence of musculoskeletal disorders in nurses: a systematic review. Med Sci. 2018;7:1. [Google Scholar]
- 3. Anderson SP, Oakman J. Allied health professionals and work‐related musculoskeletal disorders: a systematic review. Saf Health Work. 2016;7(4):259‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. De Jong T, Bos E, Pawlowska‐Cyprysiak K, et al. Current and emerging occupational safety and health (OSH) issues in the healthcare sector, including home and community care. EU‐OSHA; 2014. https://osha.europa.eu/en/publications/current‐and‐emerging‐occupational‐safety‐and‐health‐osh‐issues‐healthcare‐sector‐including‐home‐and‐community‐care [Google Scholar]
- 5. Freimann T, Coggon D, Merisalu E, Animägi L, Pääsuke M. Risk factors for musculoskeletal pain amongst nurses in Estonia: a cross‐sectional study. BMC Musculoskelet Disord. 2013;14:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jensen JN, Albertsen K, Borg V, Nabe‐Nielsen K. The predictive effect of fear‐avoidance beliefs on low back pain among newly qualified health care workers with and without previous low back pain: a prospective cohort study. BMC Musculoskelet Disord. 2009;10:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hoe VC, Kelsall HL, Urquhart DM, Sim MR. Risk factors for musculoskeletal symptoms of the neck or shoulder alone or neck and shoulder among hospital nurses. Occup Environ Med. 2012;69(3):198‐204. [DOI] [PubMed] [Google Scholar]
- 8. Heijden BV, Estryn‐Béhar M, Heerkens H. Prevalence of, and risk factors for, physical disability among nurses in Europe. Open J Soc Sci. 2019;7:(11):147‐173. doi: 10.4236/jss.2019.711012 [DOI] [Google Scholar]
- 9. Andersen LL, Vinstrup J, Villadsen E, Jay K, Jakobsen MD. Physical and psychosocial work environmental risk factors for back injury among healthcare workers: prospective cohort study. Int J Environ Res Public Health. 2019;16(22):4528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ando S, Ono Y, Shimaoka M, et al. Associations of self estimated workloads with musculoskeletal symptoms among hospital nurses. Occup Environ Med. 2000;57(3):211‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bernal D, Campos‐Serna J, Tobias A, Vargas‐Prada S, Benavides FG, Serra C. Work‐related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: a systematic review and meta‐analysis. Int J Nurs Stud. 2015;52(2):635‐648. [DOI] [PubMed] [Google Scholar]
- 12. Hodges PW, Tucker K. Moving differently in pain: a new theory to explain the adaptation to pain. Pain. 2011;152(suppl 3):S90‐S98. [DOI] [PubMed] [Google Scholar]
- 13. Vlaeyen JW, Linton SJ. Fear‐avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317‐332. [DOI] [PubMed] [Google Scholar]
- 14. Zaman J, Vlaeyen JW, Van Oudenhove L, Wiech K, Van Diest I. Associative fear learning and perceptual discrimination: a perceptual pathway in the development of chronic pain. Neurosci Biobehav Rev. 2015;51:118‐125. [DOI] [PubMed] [Google Scholar]
- 15. Bunzli S, Smith A, Schutze R, Lin I, O'Sullivan P. Making sense of low back pain and pain‐related fear. J Orthop Sports Phys Ther. 2017;47(9):628‐636. [DOI] [PubMed] [Google Scholar]
- 16. Yoshimoto T, Oka H, Ishikawa S, Kokaze A, Muranaga S, Matsudaira K. Factors associated with disabling low back pain among nursing personnel at a medical centre in Japan: a comparative cross‐sectional survey. BMJ Open. 2019;9(9):e032297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andersen JH, Haahr JP, Frost P. Risk factors for more severe regional musculoskeletal symptoms: a two‐year prospective study of a general working population. Arthritis Rheum. 2007;56(4):1355‐1364. [DOI] [PubMed] [Google Scholar]
- 18. Hildebrandt VH, Bongers PM, van Dijk FJ, Kemper HC, Dul J. Dutch musculoskeletal questionnaire: description and basic qualities. Ergonomics. 2001;44(12):1038‐1055. [DOI] [PubMed] [Google Scholar]
- 19. Kori S, Miller R, Todd D. Kinesiophobia: a new view of chronic pain behavior. Pain Manag. 1990;3:35‐43. [Google Scholar]
- 20. Roelofs J, Goubert L, Peters ML, Vlaeyen JW, Crombez G. The Tampa scale for kinesiophobia: further examination of psychometric properties in patients with chronic low back pain and fibromyalgia. Eur J Pain (London, England). 2004;8(5):495‐502. [DOI] [PubMed] [Google Scholar]
- 21. Goubert L, Crombez G, Van Damme S, Vlaeyen JW, Bijttebier P, Roelofs J. Confirmatory factor analysis of the Tampa scale for kinesiophobia: invariant two‐factor model across low back pain patients and fibromyalgia patients. Clin J Pain. 2004;20(2):103‐110. [DOI] [PubMed] [Google Scholar]
- 22. Notelaers G, De Witte H, Van Veldhoven M, Vermunt J. Construction and validation of the short inventory to monitor psychosocial hazards. Arbeidsgezondheidzorg En Ergonomie. 2007;44:11‐17. https://research.tilburguniversity.edu/en/publications/construction‐and‐validation‐of‐the‐short‐inventory‐to‐monitor‐psy [Google Scholar]
- 23. Veldhoven M, Meijman TF. Het Meten Van Psychosociale Arbeidsbelasting Met Een Vragenlijst: De Vragenlijst Beleving En Beoordeling Van De Arbeid (VBBA) (zie VBBA2.0 voor nieuwe versie). NIA; 1994. http://resolver.tudelft.nl/uuid:d231f2f3‐8574‐4e77‐862b‐4abe1ebd4df5 [Google Scholar]
- 24. Lee T, Shi D. A comparison of full information maximum likelihood and multiple imputation in structural equation modeling with missing data. Psychol Methods. 2021;26(4):466‐485. [DOI] [PubMed] [Google Scholar]
- 25. Statbel . Professionals in Health Care. 2020. Accessed November 25, 2021. https://statbel.fgov.be/en/themes/datalab/professionals‐health‐care
- 26. Neblett R, Hartzell MM, Mayer TG, Bradford EM, Gatchel RJ. Establishing clinically meaningful severity levels for the Tampa scale for kinesiophobia (TSK‐13). Eur J Pain (London, England). 2016;20(5):701‐710. [DOI] [PubMed] [Google Scholar]
- 27. Jensen JN, Karpatschof B, Labriola M, Albertsen K. Do fear‐avoidance beliefs play a role on the association between low back pain and sickness absence? A prospective cohort study among female health care workers. J Occup Environ Med. 2010;52(1):85‐90. [DOI] [PubMed] [Google Scholar]
- 28. Carriere JS, Thibault P, Milioto M, Sullivan MJL. Expectancies mediate the relations among pain catastrophizing, fear of movement, and return to work outcomes after whiplash injury. J Pain. 2015;16(12):1280‐1287. [DOI] [PubMed] [Google Scholar]
- 29. Malinowska D, Tokarz A, Wardzichowska A. Job autonomy in relation to work engagement and workaholism: mediation of autonomous and controlled work motivation. Int J Occup Med Environ Health. 2018;31(4):445‐458. [DOI] [PubMed] [Google Scholar]
- 30. Mynarski W, Grabara M, Nawrocka A, Niestrój‐Jaworska M, Wołkowycka B, Cholewa J. Physical recreational activity and musculoskeletal disorders in nurses. Med Pr. 2014;65(2):181‐188. [PubMed] [Google Scholar]
- 31. Nowrouzi B, Lightfoot N, Larivière M, et al. Occupational stress management and burnout interventions in nursing and their implications for healthy work environments: a literature review. Workplace Health Saf. 2015;63(7):308‐315. [DOI] [PubMed] [Google Scholar]
- 32. Bongers PM, de Winter CR, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health. 1993;19(5):297‐312. [DOI] [PubMed] [Google Scholar]
- 33. Van Hoof W, O'Sullivan K, O'Keeffe M, Verschueren S, O'Sullivan P, Dankaerts W. The efficacy of interventions for low back pain in nurses: a systematic review. Int J Nurs Stud. 2018;77:222‐231. [DOI] [PubMed] [Google Scholar]
- 34. Watson JA, Ryan CG, Cooper L, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed‐methods systematic review and meta‐analysis. J Pain. 2019;20(10):1140.e1‐1140.e22. [DOI] [PubMed] [Google Scholar]
- 35. Blickenstaff C, Pearson N. Reconciling movement and exercise with pain neuroscience education: a case for consistent education. Physiother Theor Pract. 2016;32(5):396‐407. [DOI] [PubMed] [Google Scholar]
- 36. Meeus M, Nijs J, Van Wilgen P, Noten P, Goubert D, Huijnen I. Moving on to mevement with chronic joint pain. Pain: Clin Updates. 2016;24(1):1‐8. http://hdl.handle.net/1854/LU‐7161646 [Google Scholar]
- 37. Hasenbring MI, Hallner D, Rusu AC. Fear‐avoidance‐ and endurance‐related responses to pain: development and validation of the avoidance‐endurance questionnaire (AEQ). Eur J Pain (London, England). 2009;13(6):620‐628. [DOI] [PubMed] [Google Scholar]
- 38. Hasenbring MI, Verbunt JA. Fear‐avoidance and endurance‐related responses to pain: new models of behavior and their consequences for clinical practice. Clin J Pain. 2010;26(9):747‐753. [DOI] [PubMed] [Google Scholar]
- 39. Parker R, Bergman E, Mntambo A, Stubbs S, Wills M. Levels of physical activity in people with chronic pain. S Afr J Physiother. 2017;73(1):323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rovner G, Johansson F, Gillanders D. Cutoff scores for the 8‐item version of the chronic pain acceptance questionnaire (CPAQ‐8) to identify different profiles of pain acceptance patterns, levels of function and behavioral flexibility. J Contextual Behav Sci. 2019;14:146‐156. doi: 10.1016/j.jcbs.2019.07.006 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


