Abstract
Background
Delayed diagnosis of cerebrovascular disease (CVD) among patients can result in substantial harm. If diagnostic process failures can be identified at Emergency Department (ED) visits that precede CVD hospitalization, interventions to improve diagnostic accuracy can be developed.
Methods
We conducted a nested case-control study using a cohort of adult ED patients discharged from a single medical center with a benign headache diagnosis from 10/1/2015-3/31/2018. Hospitalizations for CVD within 1 year of index ED visit were identified using a regional health information exchange. Patients with subsequent CVD hospitalization (cases) were individually matched to patients without subsequent hospitalization (controls) using patient’s age and visit date. Demographic, clinical, and ED processes characteristics were assessed via detailed chart review. McNemar’s test for categorical and paired t-test for continuous variables were used with statistical significance set at ≤0.05.
Results
Of the 9,157 patients with ED headache visits, 57 (0.6%; 95% CI:0.5-0.8) had a subsequent CVD hospitalization. Median time from ED visit to hospitalization was 107 days. In twenty-five patients (43.9%; 25/57) the CVD hospitalization and the index ED visit were at different hospitals. Fifty-three cases and 53 matched controls were included in the final study analysis. Cases and controls had similar baseline demographic and headache characteristics. Cases more often had a history of stroke (32.1% vs. 13.2%, p=0.02) and neurosurgery (13.2% vs. 1.9%, p=0.03) prior to the index ED visit. Cases more often had <2 components of the neurological exam documented (30.2% vs. 11.3%, p=0.03).
Conclusion
We found that 0.6% of patients with an ED headache visit had subsequent CVD hospitalization, often at another medical center. ED visits for headache complaints among patients with prior stroke or neurosurgical procedures may be important opportunities for CVD prevention. Documented neurological examinations were poorer among cases, which may represent an opportunity for ED process improvement.
Keywords: Diagnostic Error, Headache, Cerebrovascular disease, Emergency Medicine
Introduction
Delayed diagnosis of cerebrovascular disease (CVD) including acute ischemic stroke, intracerebral hemorrhage, transient ischemic attack (TIA), and subarachnoid hemorrhage (SAH) can preclude time sensitive treatments resulting in significant patient harms.1–4 Initial misdiagnosis in the emergency department (ED) occurs in approximately 9% of stroke patients;5 false-negative stroke patients who are discharged directly from the ED are often initially diagnosed with ‘benign’ neurological conditions, most frequently headache,6 whereas those that are admitted from the ED are often initially labeled as having altered mental status or acute confusional state.1,7 Although the incidence of dangerous diseases among patients evaluated for headache complaints in the ED is low,8 various types of CVD are associated with headache.9–11 Non-trivial rates of diagnostic error among patients discharged from the ED after headache diagnosis have been reported.6,12,13 Understanding sources of diagnostic error among ED patients with headache complaints is an important step towards reducing misdiagnosis related harms. To date, only the presence of vascular risk factors and having a head computed tomography performed at index ED visit have been associated with increased risk of subsequent cerebrovascular events among ED treat-and-release headache patients.14,15
In this paper, we first use administrative claims data from a regional health information exchange to measure the rate of potential CVD misdiagnosis among ED treat-and-release headache patients using Symptom-Disease Pair Analysis of Diagnostic Error (SPADE) methods.16 We then conduct a detailed review of the ED electronic medical record (EMR) for all included patients. We use this nested case-control design to evaluate for differences in demographic, clinical, diagnostic, and radiographic features between headache patients with (cases) versus without (controls) a subsequent CVD hospitalization. We hypothesized that evidence of diagnostic process failures would be more frequent in cases.
Methods
Study Design and Setting
We first identified a cohort of patients discharged home with a ‘benign’ headache diagnosis from any one of the four main EDs of John Hopkins Medicine (JHM) in the State of Maryland from 10/1/2015, when International Classification of Disease 10 Clinical Medicine (ICD-10-CM) codes were adopted in the US, until 3/31/2018. Of the four JHM EDs, one is a joint commission certified comprehensive stroke center and two were joint commission certified primary stroke centers during the study period.
We used ICD-10-CM primary discharge diagnosis codes for tension headache, migraine, cluster headache, cephalgia, or headache not otherwise specified to identify our study cohort of ‘benign’ headache patients (Supplement Table 1).14,15 Only index ED visits (first eligible visit per patient during the study period) that resulted in a discharge to home (ED treat-and-release visit) for patients age >18 years of age were included.
We defined all patients with a hospitalization for CVD within 365 days of their index JHM ED headache visit as potentially misdiagnosed cases; patients without a CVD hospitalization within 365 days of index ED visit were defined as controls. A research team member (AH), with expertise using large datasets, then matched all cases to controls in a one-to-one exact fashion with random selection of matched controls when there was more than one exact match. We used patients’ age at ED arrival as well as year and month of index ED visit to create case-control pairs.
The JHM Internal Review Board (IRB) approved this project and granted a waiver for patient consent. Access to the Chesapeake Regional Information System for our Patients (CRISP) hospitalization records had been granted to Johns Hopkins by the State of Maryland/Department of Health/ Health Service Cost Review Commission for quality improvement purposes, and this retrospective re-use of these data was approved by the JHM IRB as research.
Outcomes
To identify subsequent inpatient hospitalizations for CVD in our cohort, we used the CRISP regional health information exchange. CRISP contains data from 48 regional hospitals, including those that are part of JHM. Hospitals are located in the State of Maryland as well as adjacent areas in the State of Pennsylvania, Delaware, Northern Virginia, and Washington DC. CRISP’s data warehouse imports records from Epic, Cerner and Meditech electronic health record systems in these hospitals.17 We defined hospitalizations for CVD as those with an ICD-10-CM primary discharge diagnosis codes for ischemic stroke, TIA, intracerebral hemorrhage, and subarachnoid hemorrhage (Supplemental Table 2).18 We did not include outpatient or ED visits for CVD in our outcome measure.
Variables
Once case-control pairs were created using administrative claims data, we conducted a detailed review of the index JHM ED headache visit using the EMR for each included case and their matched control. We abstracted pre-specified demographic, clinical, and radiographic features. Record review was performed by a single board-certified vascular neurologist (ALL) who was completely masked to case-control assignment.
To fully describe all included headache patients, we abstracted documentation of red or orange flag clinical features included in the SNOOP10 list19 as well as additional high-risk features included in the Ottawa subarachnoid hemorrhage rule.20 This approach is consistent with the recommendations of the American College of Emergency Medicine Physicians guidelines.21
To evaluate diagnostic processes at the index ED visit, we abstracted information regarding provider’s documented differential diagnosis (including any mention of CVD), number of providers seeing the patient, medication response, documented neurological examination, and whether or not the patient was seen by an Emergency Medicine trainee. We used a modified version of the Safer Stroke-Dx Instrument to evaluate for missed diagnostic opportunities at the index ED headache visit (Supplemental Table 3); the board certified vascular neurologist who developed this tool applied it in this study. The Safer Stroke-Dx Instrument is a 16 item medical record review tool which includes the original 13 statements from the Revised Safer Dx Instrument and 3 additional statements focused on neurological disease;22–24 in a recent study of hospitalized patients with possible stroke misdiagnosis in the ED we found that the inter-rater reliability of Safer Stroke-Dx Instrument was high (κ=0.9 [SE=0.04]).25 For this study, we modified the Safer Stroke-Dx Instrument to a 12 item measure by eliminating the items that require knowledge of a “final diagnosis.” Modification of the Safer Stroke-Dx instrument was necessary since all chart review in this study was done by a reviewer masked to whether or not a subsequent CVD hospitalization occurred (Supplemental Table 3).
To identify instances of potential missed TIA diagnosis at index ED headache visit, a board certified vascular neurologist (ALL) applied the recently validated modified version of the explicit diagnostic criteria for TIA (EDCT).26 This tool consists of 5 criteria and was originally designed to differentiate migraine with aura patients from those with TIA.27 The modified EDCT has a sensitivity of 98% and specificity of 74% for the diagnosis of TIA.26
Medical Record Adequacy
Prior work using ED records to evaluate diagnostic accuracy in patients who complained of dizziness found poor documentation regarding essential elements of the patients’ chief complaints28 as well as their neurological exam.29 We therefore specified that if an ED record did not contain any mention of even one of the following: (1) headache onset characteristics (i.e., thunderclap, progressive), (2) headache pain quality, (3) headache triggers, or (4) associated headache features documented, then the record was deemed to be missing essential chief complaint information. We also categorized ED records as missing essential examination data if fewer than two components of a headache-focused neurological examination were not documented by any ED provider. We considered a headache-focused neurological examination to consist of 12 components: (1) fundoscopic evaluation (2) meningeal signs (3) mental status (4) otoscopic exam (5) pupils (6) visual fields (7) ocular motility (8) facial asymmetry (9) sensation (10) limb strength (11) coordination and (12) gait evaluation. Whether or not each component of the neurological examination was mentioned in the ED record was abstracted in addition to whether or not the findings were normal or abnormal.
We considered “inadequate” ED records to be ones where either essential chief complaint elements were missing or less than two components of the 12 component neurological examination were recorded. We included all eligible patients, regardless of medical record adequacy, in our primary study analysis.
Additional analysis
We conducted a pre-specified additional analysis comparing cases hospitalized for CVD within 30 days of index ED visit versus those that were hospitalized >30 days of their index ED visit to evaluate for factors associated with short-term CVD hospitalization. Using a 30-day time frame is in keeping with the known temporal patterns of cerebrovascular events after TIA/minor stroke where highest risk is in the days following the index event30 and this time frame has been previously used to identify potential misdiagnosis at index ED visit.6, 12
Based on the comments of an anonymous reviewer, we also report the number of patients with at least one interval ED headache treat-and-release visit to a JHM facility in the 365 days following their index ED visit and compare interval visits between cases and controls.
To evaluate the reliability of variables abstracted from the EMR, we randomly selected 12 patient charts (6 cases and 6 controls) and asked a second reviewer blinded to all other study data to abstract from the ED record: (1) history of stroke, (2) sudden onset of fully reversible neurological or retinal symptoms, the first component of EDCT, and (3) whether <2 components of the neurological exam were documented.
Statistical analysis
Standard descriptive statistics were used to characterize the study population, including means with standard deviations (SD) for normally distributed continuous variables and medians with interquartile range (IQR) for non-normally distributed ones. We used the modified Wald method to calculate 95% confidence intervals (CI) for proportions. We compared demographic, clinical, and radiographic features between case-control pairs using McNemar’s test for categorical variables and paired t-test for continuous variables. For our additional comparative analysis between cases who returned with CVD within 30 days of index ED visits and all other cases, we used chi-squared and Student’s t-test statistics. To compare the number of interval ED headache visits between cases and controls, we also used chi-squared. Inter-rater reliability for EMR data abstraction was assessed using percent agreement and Cohen’s kappa coefficient (κ). We did not impute any values for missing data. To depict rates of return with cerebrovascular disease, we used a histogram. The threshold for statistical significance was set as ≤0.05. All tests of comparison were two-sided. Analyses were performed using Stata/IC, version 16 (StataCorp, TX).
Results
We identified a total of 9,157 ED headache visits at JHM during the study period. The average age was 42 (SD 16.5) years and 67.5% were women. A total of 62 patients (0.7%; 95% CI:0.5-0.9) were initially identified as having an ED visit for headache followed by a CVD hospitalization. These 62 headache patients (cases) were matched to 62 headache patients who did not have a subsequent CVD hospitalization (controls). Detailed review of all initially identified cases and controls (n=124) revealed that 12 patients (5 cases and 7 controls) did not have a true ED treat-and-release visit and were therefore excluded (Figure 1).
Figure 1.
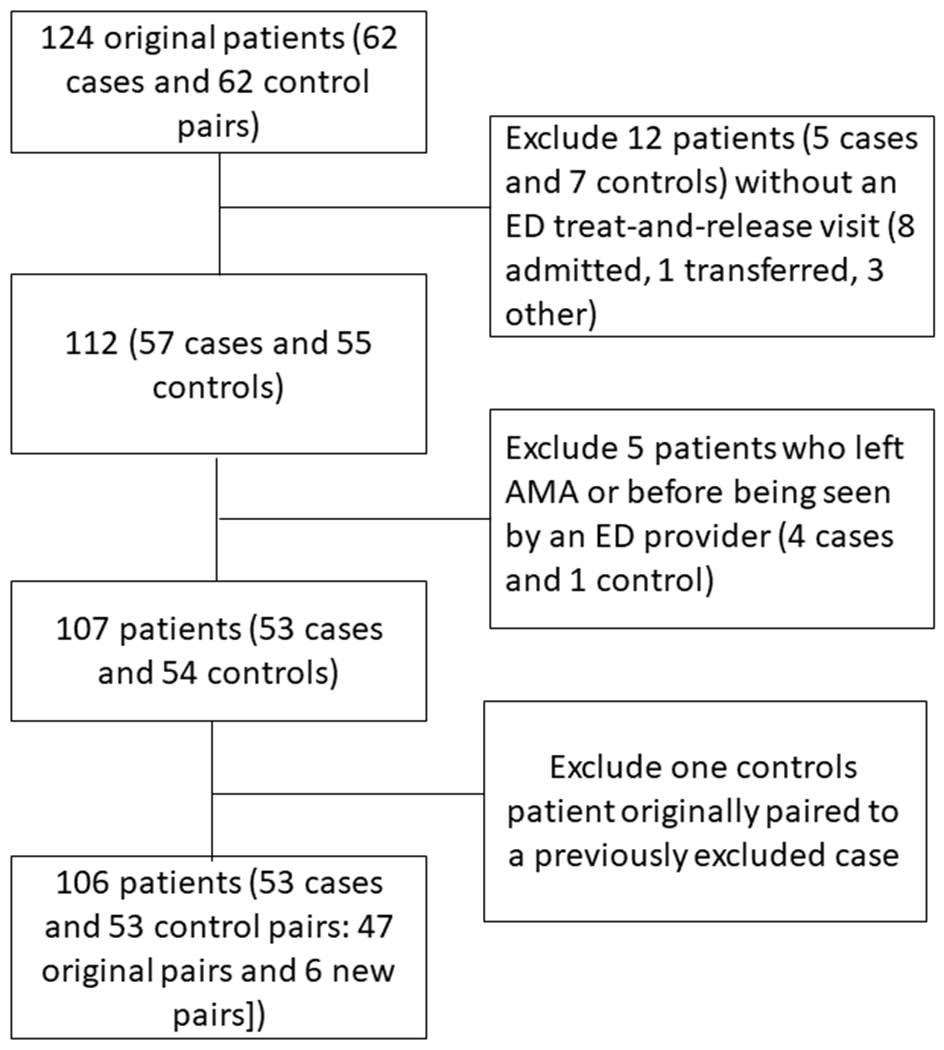
Study Flow
There were thus 57 (0.6%; 95% CI:0.5-0.8) patients with a confirmed ED treat-and-release visit from a JHM ED with a subsequent cerebrovascular disease hospitalization. A total of 25 cases (43.9%; 25/57) were hospitalized at a non-JHM hospital (health-system crossover). Median time from ED visit to CVD hospitalization was 107 days IQR (31-189).
A total of 106 patients (53 cases and 53 controls) were included in the final case-control analysis (Figure 1). Five patients in the original study cohort (4 cases and 1 control) were found on detailed EMR review to have left the ED against medical advice (AMA) or before being seen by a provider. After excluding these 5 patients, a total of 47 original case-control pairs remained. Six new case-control pairs were formed by matching the remaining unpaired cases to unpaired controls; three of these new case-control pairs were exactly matched for patient age, but three could not be (difference in age of 1, 16, and 17 years). A single control patient (n=1) originally paired to an excluded case was removed.
Primary Analysis
The included 53 cases-control pairs had similar baseline demographic and headache characteristics. Nearly two thirds of both groups had >1 red or orange flag headache feature at presentation. No thunderclap headaches were documented (Table 1). A total of 13 patients (24.5%, 13/53) were hospitalized within 30 days of their index ED visit (Figure 2). Among patients who were hospitalized within 30 days (n=13), the median time from index ED visit to hospitalization was 11 days (IQR: 6-13) among those who returned >30 days median time to hospitalization was 154 (IQR: 89-206) days. Only 2 patients were hospitalized within 72 hours of the index ED visit. Within 365 days of index ED visit, only 8 (15.1%) cases and 4 (7.5%) controls had at least one interval ED visit for headache (p= 0.22).
Table 1.
Baseline demographic and clinical features for cases and matched controls
| Cases (n=53) | Controls (n=53) | P-value | |
|---|---|---|---|
| Demographics | |||
| Female Sex, n(%) | 31 (58.5) | 30 (56.6) | 0.84 |
| Race/Ethnicity, n(%) | |||
| - Non-Hispanic White | 18 (34.0) | 19 (35.8) | |
| - Non-Hispanic Black | 32 (60.4) | 23 (43.4) | |
| - Hispanic | 0 | 0 | |
| - Asian | 2(3.8) | 9 (17.0) | |
| - Other | 1 (1.9) | 2(3.8) | |
| Translation services used | 0 | 5(9.4) | 0.08 |
| John Hopkins ED | |||
| - A | 14 (26.4) | 12(22.6) | |
| - B | 8 (15.1) | 17 32.1) | |
| - C | 23 43.4) | 13 24.5) | |
| - D | 8 (15.1) | 11 (20.8) | |
| Past Medical History | |||
| Hypertension | 38 (71.7) | 29 (54.7) | 0.07 |
| Hyperlipidemia | 20 (37.7) | 12 (22.6) | 0.17 |
| Diabetes | 15 (28.3) | 12(22.6) | 0.55 |
| Prior stroke | 17 (32.1) | 7 (13.2) | 0.02 |
| Atrial fibrillation | 5 (9.4) | 4(7.5) | 0.71 |
| Heart failure | 6 (11.3) | 2 (3.8) | 0.16 |
| Smoker | 20(37.7) | 20 (37.7) | 1.0 |
| Alcohol use | 4(7.5) | 6 (11.3) | 0.48 |
| Human Immunodeficiency Virus | 2 (3.8) | 2(3.8) | 1.0 |
| Cancer | 7(13.2) | 2(3.8) | 0.06 |
| Prior Neurosurgery | 7 (13.2) | 1(1.9) | 0.03 |
| Recent trauma | 4 (7.5) | 4 (7.5) | 1.0 |
| Psychiatric illness | 14 (26.4) | 14 (26.4) | 1.0 |
| Drug use | 4 (7.5) | 2 (3.8) | 0.41 |
| Pregnant or post-partum | 0 | 0 | |
| Home medications | |||
| Any antiplatelet agent* | 21 (39.6) | 10 (22.6) | 0.02 |
| Anticoagulation | 4 (7.5) | 5 (9.4) | 1.0 |
| Anti-hypertensive | 32 (60.4) | 23 (43.4) | 0.09 |
| Statin | 25 (47.2) | 11 (20.8) | 0.01 |
| Headache features | |||
| Presenting complaint in triage did not include headache** | 15 (28.3) | 9 (17.0) | 0.16 |
| Any prior headache disorder | 20 (37.7) | 20 (37.7) | 1.0 |
| Similar to prior headache | 7 (13.2) | 15 (28.3) | 0.07 |
| Thunderclap Quality | 0 | 0 | |
| Duration < 6 hours | 12 (22.6) | 7 (13.2) | 0.23 |
| Duration >24 hours | 28 (52.8) | 29 (54.7) | 0.86 |
| Associated neurological complaints (including blurry vision and dizziness) | 25 (47.2) | 22 (41.5) | 0.49 |
| SNOOP10 >1 | 34 (64.2) | 33 (62.2) | 0.82 |
| Improvement in headache pain while in the ED | 15 (28.3) | 20 (37.7) | 0.34 |
| Vitals at ED arrival | |||
| Temp > 100.4°F or < 96.8°F | 0 | 1 (1.9) | 0.32 |
| Mean systolic blood pressure (SD) | 153.5 (3.4) mm Hg | 145.4 (3.9) mm Hg | 0.09 |
| Mean diastolic blood pressure (SD) | 85.3 (2.0) mm Hg | 82.1 (1.8) mm Hg | 0.21 |
| Heart rate (SD) | 81.5 (2.1) | 77.5 (2.1) | 0.19 |
Two cases were prescribed dual antiplatelet therapy
No triage complaint was documented for two patients
Figure 2.
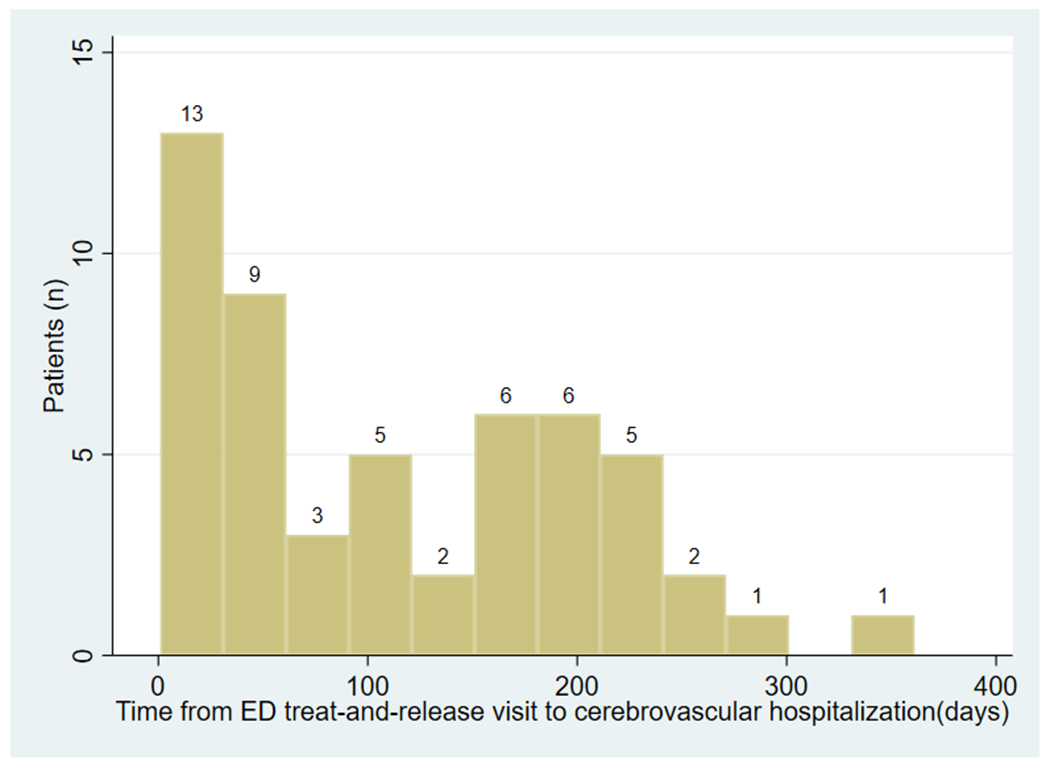
Histogram showing hospitalizations for cerebrovascular disease following index ED headache visit among all cases (n=53) (width of each bar = 30 days)
Table 2 shows the comparison of cases versus controls. Cases more often had a prior history of stroke (32.1% vs. 13.2%, p=0.02) and of a neurosurgical procedure (13.2% vs. 1.9%, p=0.03) compared to controls. Similarly, cases more often had radiographic evidence of a chronic infarct on imaging as compared to controls (28.3% vs. 9.4%, p=0.02) and were more likely to have been prescribed statins (47.2% vs. 20.8%; p=0.01) or antiplatelet agents (39.6% vs. 22.6%; p=0.02) than controls. Having a neurological consultation (18.9% vs. 7.5%, p=0.06) and being seen by multiple providers (11.3% vs. 3.8%, p=0.06) was also more frequent among cases than controls, but with borderline p-values.
Table 2.
Adequacy of record documentation and diagnostic process failures (other than neurologic exam) among cases versus controls
| Cases (n=53) | Controls (n=53) | P-value | |
|---|---|---|---|
| ED record documentation quality | |||
| Essential headache-related information not documented | 11(20.8) | 7 (13.2) | 0.32 |
| Inadequate record documentation | 22 (41.5) | 13 (24.5) | 0.08 |
| Any differential diagnosis documented | 35 (66.0) | 36 (67.9) | 0.83 |
| Differential diagnosis by any provider included mention of cerebrovascular disease | 25 (47.2) | 28 (52.8) | 0.53 |
| Providers and consultations | |||
| Seen by more than two providers | 6 (11.3) | 2 (3.8) | 0.06 |
| Stroke code | 1 (1.9) | 0 | 0.32 |
| Neurology consult | 10 (18.9) | 4 (7.5) | 0.06 |
| Other consult | 6 (11.3) | 3 (5.7) | 0.16 |
| Emergency Medicine trainee | 20 (37.7) | 13 (24.5) | 0.09 |
| Diagnostic testing done in the ED | |||
| Head CT | 36 (67.9) | 42 (79.2) | 0.10 |
| MRI brain | 3 (5.7) | 2(3.8) | 0.32 |
| Vessel imaging | 2(3.8) | 7 (13.2) | 0.10 |
| Lumbar puncture | 2(3.8) | 2(3.8) | 1.0 |
| Imaging results at index ED visit | |||
| Acute/subacute infarct | 2(3.8) | 0 | 0.16 |
| Chronic infarct | 15(28.3) | 5(9.4) | 0.02 |
| Markers of misdiagnosis | |||
| Missed diagnostic opportunity using modified Safer Stroke-Dx | 8 (15.1) | 5 (9.4) | 0.32 |
| Sudden onset of reversible neurological symptoms | 4 (7.5) | 1 (1.9) | 0.18 |
Using the modified Safer Stroke-Dx instrument, 13 instances of missed diagnostic opportunities were identified. A total of 8 cases and 5 controls were identified as having missed diagnostic opportunities (P=0.32; Table 2). In one of the 8 cases an acute infarct was seen on MR imaging and in another case a subacute infarct was seen; neither finding was clearly addressed by the ED care team despite the radiologists’ read of stroke (Supplemental Table 4).
No definitive missed TIA cases were identified at index ED visit using the modified EDCT. A total of 5 patients (5/106) had documentation of sudden onset of fully reversible neurological or retinal symptoms. Of those five patients, 4 were cases and 1 was a control (Table 2). Among the cases, one patient had symptoms of right sided numbness lasting for > 24 hours and was diagnosed with non-specific numbness after neurological consultation and an unremarkable MRI brain. The other 3 cases did not have enough information in the medical record to determine whether or not they satisfied the other EDCT criteria. The single control patient with documentation of sudden onset fully reversible neurological symptoms was unable to provide a detailed history or definite symptoms onset time due to delirium.
Abnormal neurological findings were reported in only 19% of included patients with no differences in the presence of abnormalities between cases and controls (Table 3). Documentation of individual components of neurological exam in the medical record by ED providers was similar between cases and controls except for facial asymmetry.
Table 3.
Headache-specific neurologic exam findings documented by ED providers among cases versus controls
| Cases (n=53) | Controls (n=53) | P-value | |
|---|---|---|---|
| Fundoscopic exam | 1 (1.9) | 0 | 0.32 |
| Meningeal signs | 11(20.8) | 13 (24.5) | 0.62 |
| Mental status | 50 (94.3) | 51 (96.2) | 0.56 |
| Otoscope | 4 (7.5) | 2 (3.8) | 0.41 |
| Visual fields | 27 (50.9) | 32 (60.4) | 0.28 |
| Pupillary exam | 31 (58.5) | 36 (67.9) | 0.32 |
| Ocular motility | 31 (58.5) | 37 (69.8) | 0.20 |
| Facial asymmetry | 32 (60.4) | 44 (83.0) | 0.01 |
| Sensation | 19 (35.8) | 19 (35.8) | 1.0 |
| Strength | 25 (47.2) | 26 (49.1) | 0.84 |
| Coordination | 22 (41.5) | 21 (39.6) | 0.85 |
| Gait evaluation | 11 (20.8) | 13 (24.5) | 0.67 |
| <2 components of the neurological examination documented | 16 (30.2) | 6 (11.3) | 0.03 |
| Any abnormality noted on neurological exam | 8 (15.1) | 12 (22.6) | 0.41 |
| Any abnormality noted on general medicine exam | 19 (35.8) | 27 (50.9) | 0.84 |
Medical Record Completeness
Cases were significantly more likely than controls to have < 2 components of the neurological exam documented in the EMR (30.2% vs. 11.3%, p=0.03). A total of 18 encounters (11 cases and 7 controls) lacked enough information regarding headache chief complaint without significant differences between cases and controls (20.8% vs. 13.2%; p=0.32). Inadequate records, lacking either essential headache chief complaint information or with <2 components of the neurological examination were more common among cases than controls with a large effect size (41.5% vs. 24.5%; P=0.08) that did not reach statistical significance.
Inter-rater reliability
There was 91.7% agreement on chart abstraction (by two independent raters masked to case versus control status) of history of stroke (κ=0.8), 91.7% agreement on whether or not <2 components of the neurological exam was missing (κ=0.7), and 83.3% on whether the patient had sudden onset of reversible neurological symptoms (κ=0.6) between the two raters.
Additional Analysis
Differences in diagnostic process markers between cases with return visit within 30 days (n=13) versus all other cases (n=40) were minimal (Table 4). Inadequate records lacking essential chief complaint or neurological exam documentation were more common in cases with CVD hospitalization >30 days from index event than those with CVD hospitalizations ≤ 30 (50% vs. 15.4%; p=0.03).
Table 4.
Comparison of cases with stroke occurring ≤30 versus >30 days of the index ED visit
| Case within 30 days (n=13) | Other cases (n=40) | P-value | |
|---|---|---|---|
| Headache not in triage complaint | 3 (23.1) | 12 (30) | 0.70 |
| Health-system Crossover | 5 (38.5) | 8 (20) | 0.57 |
| Missed diagnostic opportunity using modified Safer Stroke-Dx | 1 (7.7) | 7 (17.5) | 0.36 |
| Differential diagnosis documented | 7 (53.8) | 28 (70) | 0.29 |
| Stroke on differential diagnosis | 4 (30.8) | 21 (52.5) | 0.43 |
| SNOOP > 1 | 7 (53.8) | 27 (67.5) | 0.37 |
| Essential headache-related information not documented | 1 (7.7) | 10 (25) | 0.18 |
| Inadequate record documentation | 2(15.4) | 20 (50) | 0.03 |
| Seen by an Emergency Medicine trainee | 6 (46.2) | 14 (35) | 0.47 |
| Acute/subacute infarct | 0 | 2 (5) | 0.43 |
| Neuro consult | 2 (15.4) | 8 (20) | 0.84 |
| Neurological Examination | |||
| Fundoscopic exam | 0 | 1 (2.5) | 0.57 |
| Meningeal signs | 2 (15.4) | 9 (22.5) | 0.56 |
| Mental status | 13 (100) | 37 (92.5) | 0.31 |
| Otoscopy | 2 (15.4) | 2 (5) | 0.22 |
| Visual fields | 8 (61.5) | 19 (47.5) | 0.38 |
| Pupils | 10 (76.9) | 21 (52.5) | 0.12 |
| Ocular motility | 10 (76.9) | 21 (52.5) | 0.12 |
| Facial droop | 9 (69.2) | 23 (57.5) | 0.45 |
| Limb sensory | 4 (30.8) | 15 (37.5) | 0.66 |
| Motor strength | 7 (53.8) | 18 (45) | 0.58 |
| Coordination | 8 (32) | 14 (35) | 0.09 |
| Ambulates | 3 (23.1) | 8 (20) | 0.81 |
| < 2 components of the neurological exam documented | 2 (15.4) | 14 (35) | 0.18 |
Discussion
Using administrative claims data, we found that 0.6% of patients with an ED treat-and-release headache visit at JHM had a subsequent hospitalization for CVD within 1 year. After matching patients with versus without a subsequent hospitalization in a nested case-control design, detailed medical record review revealed that cases more often had a history and radiographic evidence of prior stroke as well as a history of neurosurgery. We found that documentation of key history and exam features was frequently inadequate, and charts with minimal neurologic exams documented at the ED index treat-and-release visit were more frequent among headache patients with subsequent CVD hospitalization (cases). Using a modified version of the Safer Stroke-Dx Instrument we found 15% of cases had missed diagnostic opportunities, but there was no clear difference between cases and controls. There were two headache patients with a missed stroke on imaging at index ED visit that were not addressed prior to discharge.
The yield of detailed medical record review to identify diagnostic process failures was constrained by missing elements. Nearly half (45.6%; 26/57) of all included patients with a subsequent cerebrovascular disease hospitalization in a SPADE-style analysis had an index ED encounter that could not be fully evaluated either because of inadequate documentation (n=22) or leaving AMA before being seen by a provider (n=4). We found that cases were more likely than controls to have ED records lacking critical information regarding chief complaint or have no more than one component of the 12-item neurological exam documented (inadequate records).
Others have noted a lack of information in the ED medical record for treat-and-release visit patients. Among patients who present with dizziness, a frequent presenting complaint in stroke misdiagnosis,5 a single center study found that 50% of ED patients lacked documentation of relevant diagnostic information.28 Another study found that the documentation of exam findings regarding nystagmus enabled a meaningful inference about the cause of dizziness in only 5.4% of ED visits.29 Finally, when reviewing ED visits that occur within 7 days of another ED visit as a marker of diagnostic error, researchers found that 20% of all ED encounters contained no usable information in the medical record.31 Whether or not missing ED documentation can serve as a marker or trigger tool for potential misdiagnosis requires further study.32 Based on our findings, relying on ED chart review alone to identify sources of possible diagnostic error is low-yield, but there appears to be substantial room for improvement in documentation (and perhaps performance of) bedside neurologic assessments.
Our rate of CVD hospitalization after ED treat-and-release headache visits of 0.6% is similar to previously published rates. A prior study using administrative claims data from 6 US states found that the rate of hospitalization for any dangerous neurological disease after an ED headache visit was 0.5%.10 A single center study reported that 0.4% of headache patients had a subsequent CVD hospitalization within a year of index ED visit.15
A major advantage of our study compared to prior work is that we were able to capture outcome events at unaffiliated centers using a health information exchange as well as assure all ED encounters were eligible for study inclusion via detailed chart review. Our finding that 44% of included ED treat-and-release headache patients were subsequently hospitalized at an unaffiliated center is consistent with previous research. In a Canadian study of missed SAH in the ED, a 37% health-system crossover rate was reported.13 These findings highlight the importance of using multi-institutional data sets (e.g., regional health information exchanges, administrative claims data) when evaluating for potential ED misdiagnosis. At the very least, single institutions without such data must be aware that their true rate of CVD hospitalizations after ED visits for neurological symptoms is likely to be meaningfully higher than the one measured using only internal data.
Another important finding from our study is that prior stroke and evidence of chronic infarct on imaging during an ED headache treat-and-release visit was associated with subsequent CVD hospitalization. This finding is in keeping with a previous case-control study of ED headache patients with subsequent stroke hospitalizations where only history of stroke or TIA was associated with increased odds of stroke hospitalization in a multivariable model.14 In combination, these results suggest that ED headache visits for patients with a history of or radiographic evidence of prior stroke or neurosurgery are important opportunities to assure evidence based secondary stroke prevention strategies are in place. Whether index ED headache visits in this subgroup of patients represent a biological trigger for subsequent stroke or reflects diagnostic error at the index ED visit remains somewhat uncertain based on available evidence.
Limitations
Our current study has a number of important limitations. To begin with, the results are based on retrospective EMR abstraction, so incorrect and potentially biased ED documentation of clinical features may have contributed to the findings, with unknown direction and magnitude of impact. Additionally, all evaluated ED visits occurred within a single academic health-system which may limit the generalizability of our results. Secondly, single reviewer evaluated all included encounters and, even though this reviewer was fully blinded to outcome events and applied previously established tools to evaluate the diagnostic processes at index visit, inter-rater reliability of data abstraction for the EMR was only partially assessed. The Safer Stroke-Dx tool was modified to account for the reviewer’s lack of knowledge regarding final diagnosis. Thirdly, outcome ascertainment for subsequent CVD was imperfect as it relied on subsequent hospitalization in the region, identified outcome events using ICD-10-CM codes, and could not identify patients who were never hospitalized (i.e., those who suffered cerebrovascular events at home and did not seek care, who presented to clinic and were never admitted, or who died). We also do not know the clinical severity of any CVD hospitalization. Fourthly, we did not use patient sex to match cases to controls because we wanted to study sex as a predictor. Given known sex differences in both ED diagnostic formulation following minor neurological events33 and migraine prevalence,34 our study design could have biased our results, again, with unknown magnitude and direction. Finally, we matched cases to controls before detailed medical record review requiring us to re-match a few patients, resulting in 3 case-control pairs that were not as well matched as all other pairs.
Conclusions
We found that 0.6% of patients with an ED headache treat-and-release visit returned with CVD in the year following their index ED visit using SPADE methods. On detailed EMR review, roughly one third of all included ED records lacked documentation of either essential headache specific history or contained only a single component of the neurologic exam. Furthermore, charts with less than two components of the neurological exam were more common among cases than controls, so this appears to be an important area for diagnostic process improvement. Headache patients with a subsequent CVD hospitalization were more likely to have had a prior stroke or prior neurosurgery, so index ED visits for these patients may represent important opportunities to assure all evidence based stroke prevention strategies are in place. Finally, quality improvement and research efforts seeking to measure misdiagnosis rates should account for health-system crossover and those assessing diagnostic care process or causes of diagnostic error should consider strategies beyond chart review.
Supplementary Material
Funding:
NIH research grant K23NS107643 supports Dr. Liberman. Dr. Newman-Toker’s effort was supported by the Armstrong Institute Center for Diagnostic Excellence.
Disclosures:
Dr. Newman-Toker serves as a paid consultant, reviewing medicolegal cases for both plaintiff and defense firms related to misdiagnosis of neurologic conditions, including stroke. He has conducted government and foundation funded research related to diagnostic error and stroke. He has been loaned research equipment related to diagnosis of stroke by two commercial companies (GN Otometrics and Interacoustics) and Johns Hopkins has licensed related diagnostic decision-support technology to GN Otometrics for which Dr. Newman-Toker has received royalties. Dr. Lipton reports receiving research support from the NIH, FDA as well as the National Headache Foundation and the Marx Foundation. Dr. Lipton also receives research support from Allergan/Abbvie, Amgen, Eli Lilly and Electrocore. He receives personal fees as a consultant or advisor from from Allergan/Abbvie, Amgen, Biohaven Holdings, Dr. Reddy’s, GlaxoSmithKline, Grifols, Lundbeck, Merck, Novartis and Teva Pharmaceuticals. He holds stock or options in Biohaven Holdings and CtrlM Health. In addition, he receives royalties for Wolff’s Headache 7th and 8th Edition.
References
- 1.Richoz B, Hugli O, Dami F, Carron PN, Faouzi M, Michel P. Acute stroke chameleons in a university hospital: Risk factors, circumstances, and outcomes. Neurology 2015;85:505–11. [DOI] [PubMed] [Google Scholar]
- 2.Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432–42. [DOI] [PubMed] [Google Scholar]
- 3.Ois A, Vivas E, Figueras-Aguirre G, et al. Misdiagnosis Worsens Prognosis in Subarachnoid Hemorrhage With Good Hunt and Hess Score. Stroke 2019;50:3072–6. [DOI] [PubMed] [Google Scholar]
- 4.Colton K, Richards CT, Pruitt PB, et al. Early Stroke Recognition and Time-based Emergency Care Performance Metrics for Intracerebral Hemorrhage. J Stroke Cerebrovasc Dis 2020;29:104552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tarnutzer AA, Lee SH, Robinson KA, Wang Z, Edlow JA, Newman-Toker DE. ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: A meta-analysis. Neurology 2017;88:1468–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newman-Toker DE, Moy E, Valente E, Coffey R, Hines AL. Missed diagnosis of stroke in the emergency department: a cross-sectional analysis of a large population-based sample. Diagnosis (Berl) 2014;1:155–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madsen TE, Khoury J, Cadena R, et al. Potentially Missed Diagnosis of Ischemic Stroke in the Emergency Department in the Greater Cincinnati/Northern Kentucky Stroke Study. Acad Emerg Med 2016;23:1128–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goldstein JN, Camargo CA Jr., Pelletier AJ, Edlow JA. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia 2006;26:684–90. [DOI] [PubMed] [Google Scholar]
- 9.Koudstaal PJ, van Gijn J, Kappelle LJ. Headache in transient or permanent cerebral ischemia. Dutch TIA Study Group. Stroke 1991;22:754–9. [DOI] [PubMed] [Google Scholar]
- 10.Arboix A, Massons J, Oliveres M, Arribas MP, Titus F. Headache in acute cerebrovascular disease: a prospective clinical study in 240 patients. Cephalalgia 1994;14:37–40. [DOI] [PubMed] [Google Scholar]
- 11.Ferro JM, Canhao P, Stam J, Bousser MG, Barinagarrementeria F, Investigators I. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004;35:664–70. [DOI] [PubMed] [Google Scholar]
- 12.Dubosh NM, Edlow JA, Goto T, Camargo CA Jr., Hasegawa K. Missed Serious Neurologic Conditions in Emergency Department Patients Discharged With Nonspecific Diagnoses of Headache or Back Pain. Ann Emerg Med 2019;74:549–61. [DOI] [PubMed] [Google Scholar]
- 13.Vermeulen MJ, Schull MJ. Missed diagnosis of subarachnoid hemorrhage in the emergency department. Stroke 2007;38:1216–21. [DOI] [PubMed] [Google Scholar]
- 14.Liberman AL, Lu J, Wang C, Cheng NT, Moncrieffe K, Lipton RB. Factors associated with hospitalization for ischemic stroke and TIA following an emergency department headache visit. Am J Emerg Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberman AL, Wang C, Friedman BW, et al. Head Computed tomography during emergency department treat-and-release visit for headache is associated with increased risk of subsequent cerebrovascular disease hospitalization. Diagnosis (Berl) 2020. [DOI] [PubMed] [Google Scholar]
- 16.Liberman AL, Newman-Toker DE. Symptom-Disease Pair Analysis of Diagnostic Error (SPADE): a conceptual framework and methodological approach for unearthing misdiagnosis-related harms using big data. BMJ Qual Saf 2018;27:557–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chesepeake Regional Information System for Our Patients (CRISP). 2020. Available from: https://crisphealth.org/. Accessed: July 1, 2020.
- 18.McCormick N, Bhole V, Lacaille D, Avina-Zubieta JA. Validity of Diagnostic Codes for Acute Stroke in Administrative Databases: A Systematic Review. PLoS One 2015;10:e0135834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Do TP, Remmers A, Schytz HW, et al. Red and orange flags for secondary headaches in clinical practice: SNNOOP10 list. Neurology 2019;92:134–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perry JJ, Sivilotti MLA, Sutherland J, et al. Validation of the Ottawa Subarachnoid Hemorrhage Rule in patients with acute headache. CMAJ 2017;189:E1379–E85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American College of Emergency Physicians Clinical Policies Subcommittee on Acute H, Godwin SA, Cherkas DS, et al. Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Acute Headache. Ann Emerg Med 2019;74:e41–e74. [DOI] [PubMed] [Google Scholar]
- 22.Singh H Editorial: Helping health care organizations to define diagnostic errors as missed opportunities in diagnosis. Jt Comm J Qual Patient Saf 2014;40:99–101. [DOI] [PubMed] [Google Scholar]
- 23.Singh H, Khanna A, Spitzmueller C, Meyer AND. Recommendations for using the Revised Safer Dx Instrument to help measure and improve diagnostic safety. Diagnosis (Berl) 2019;6:315–23. [DOI] [PubMed] [Google Scholar]
- 24.Al-Mutairi A, Meyer AN, Thomas EJ, et al. Accuracy of the Safer Dx Instrument to Identify Diagnostic Errors in Primary Care. J Gen Intern Med 2016;31:602–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Safer Stroke-Dx Instrument: Identifying Stroke Misdiagnosis in the Emergency Department. [DOI] [PubMed]
- 26.Dolmans LS, Lebedeva ER, Veluponnar D, et al. Diagnostic Accuracy of the Explicit Diagnostic Criteria for Transient Ischemic Attack: A Validation Study. Stroke 2019;50:2080–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lebedeva ER, Gurary NM, Gilev DV, Christensen AF, Olesen J. Explicit diagnostic criteria for transient ischemic attacks to differentiate it from migraine with aura. Cephalalgia 2018;38:1463–70. [DOI] [PubMed] [Google Scholar]
- 28.Newman-Toker DE. Charted records of dizzy patients suggest emergency physicians emphasize symptom quality in diagnostic assessment. Ann Emerg Med 2007;50:204–5. [DOI] [PubMed] [Google Scholar]
- 29.Kerber KA, Morgenstern LB, Meurer WJ, et al. Nystagmus assessments documented by emergency physicians in acute dizziness presentations: a target for decision support? Acad Emerg Med 2011;18:619–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Amarenco P, Lavallee PC, Labreuche J, et al. One-Year Risk of Stroke after Transient Ischemic Attack or Minor Stroke. N Engl J Med 2016;374:1533–42. [DOI] [PubMed] [Google Scholar]
- 31.Calder L, Pozgay A, Riff S, et al. Adverse events in patients with return emergency department visits. BMJ Qual Saf 2015;24:142–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shenvi EC, El-Kareh R. Clinical criteria to screen for inpatient diagnostic errors: a scoping review. Diagnosis (Berl) 2015;2:3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu AYX, Penn AM, Lesperance ML, et al. Sex Differences in Presentation and Outcome After an Acute Transient or Minor Neurologic Event. JAMA Neurol 2019;76:962–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buse DC, Loder EW, Gorman JA, et al. Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache 2013;53:1278–99. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


