Abstract
Objectives
Many guidelines for septic olecranon bursitis recommend aspiration of the bursa prior to initiation of antimicrobial therapy despite the absence of robust clinical data to support this practice and known risk of aspiration complications. Our objective was to describe outcomes associated with empiric antibiotic therapy without bursal aspiration among emergency department (ED) patients with suspected septic olecranon bursitis.
Methods
We conducted a retrospective observational cohort study of patients presenting to an academic ED from January 1, 2011, to December 31, 2018, with olecranon bursitis. The health record was reviewed to assess patient characteristics and outcomes within 6 months of the ED visit. Olecranon bursitis was considered “suspected septic” if the patient was treated with antibiotics. The primary outcome of interest was complicated versus uncomplicated bursitis resolution. Uncomplicated resolution was defined as bursitis resolution without subsequent bursal aspiration, surgery, or hospitalization.
Results
During the study period, 264 ED patients were evaluated for 266 cases of olecranon bursitis. The median age was 57 years and 85% were men. Four (1.5%) patients had bursal aspiration during their ED visit, 39 (14.7%) were admitted to the hospital, 76 (28.6%) were dismissed without antibiotic therapy, and 147 (55.3%) were dismissed with empiric antibiotic therapy for suspected septic olecranon bursitis. Among these 147 patients, 134 had follow‐up available including 118 (88.1%, 95% confidence interval [CI] = 81.1%–92.8%) with an uncomplicated resolution, eight (6.0%, 95% CI = 2.8%–11.8%) who underwent subsequent bursal aspiration, and nine (6.7%, 95% CI = 3.3%–12.7%) who were subsequently admitted for inpatient antibiotics.
Conclusions
Eighty‐eight percent of ED patients with suspected septic olecranon bursitis treated with empiric antibiotics without aspiration had resolution without need for subsequent bursal aspiration, hospitalization, or surgery. Our findings suggest that empiric antibiotics without bursal aspiration may be a reasonable initial approach to ED management of select patients with suspected septic olecranon bursitis.
Keywords: aspiration, emergency department, management, olecranon bursitis, septic bursitis
INTRODUCTION
Patients with symptomatic olecranon bursitis commonly present to the emergency department (ED) for evaluation. 1 Up to 50% of all olecranon bursitis cases in the ED are septic in nature. 2 It is important to recognize and appropriately treat these cases to prevent complications including septic arthritis and sepsis. 3
The ED evaluation and diagnosis of septic bursitis is widely variable and often based on anecdotal evidence. 4 Diagnostic aspiration of the olecranon bursa to assess for septic bursitis is commonly recommended and performed 1 , 2 , 3 , 5 , 6 despite the paucity of evidence to support this practice. 3 Aspiration may increase the risk for complications including chronic fistula formation, infection, and need for a future bursectomy. 2 , 3 , 7
There are only limited studies focused on ED evaluation and management of septic bursitis. Additionally, the efficacy of conservative management of suspected septic olecranon bursitis with empiric antibiotic therapy is unknown. The objective of our study was to describe outcomes associated with empiric antibiotic therapy without bursal aspiration among ED patients with suspected septic olecranon bursitis.
METHODS
Study design
We conducted a retrospective observational cohort study. The study was deemed exempt by the Mayo Clinic institutional review board. The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for reporting observational studies were followed. 8
Study setting and population
This study was conducted at the ED of Mayo Clinic Hospital–Saint Mary's Campus, Rochester, Minnesota, a quaternary care academic ED that has a volume of approximately 77,000 annual patient visits. Most patients come from Olmsted County and six adjacent counties in southeastern Minnesota. All adult ED patients (age ≥ 18 years) with olecranon bursitis between January 1, 2011, and December 31, 2018, were eligible for inclusion. Patients with an ED diagnosis containing “olecranon bursitis” or “bursitis,” but not “prepatellar bursitis,” were identified and the electronic health record (EHR) was manually reviewed to determine whether the patient had olecranon bursitis. All diagnoses associated with the ED visit were assessed for potential inclusion in the study. We considered the olecranon bursitis to be “suspected septic” if the patient was treated with antibiotics. Patients who declined research authorization, had an underlying fracture, or had surgery on the joint within 3 months prior to their presentation were excluded. Follow up was considered to be bursitis related if the provider specifically addressed the bursitis in the visit note. If the patient continued to have documented care in the EMR but the bursitis was not addressed, the visits were reviewed as part of the follow‐up period for 6 months but not considered bursitis‐related follow‐up. Patients were considered lost to follow‐up if they had less than 14 days of follow‐up available in the EHR.
Study protocol
All data were abstracted from the EHR using a standardized extraction process. Study data were collected and managed using REDCap (Research Electronic Data Capture, Nashville, TN) electronic data capture tools hosted at Mayo Clinic. 9 ED visits were independently extracted by two medical students (A.B. and A.T.) and an emergency nurse practitioner (I.K.). Extractors were trained on 10 random charts, and coding rules were developed. Abstractors were not blinded to study objectives. Random chart numbers were generated by www.random.org. Coding rules included using the first recorded value for vital signs with more than one measurement; a history of acute trauma was defined as trauma within the past 1 month; fever was defined as a temperature of 38° C or higher; steroid use was defined as present if the patient was taking steroids at the time of the index ED visit; patient‐reported fever was defined as present if a patient reported a fever at any point in the illness. Investigators met on numerous occasions with the principal investigator (R.C.) to discuss the abstraction process, ambiguities, and inconsistencies. Inter‐rater agreement was assessed for the key variables including aspiration of the bursa in the ED, subsequent hospitalization, need for subsequent aspiration of the bursa, development of complications from initial bursal aspiration, complications from antibiotic use, and need for surgical procedure. New extraction guidelines were developed as needed to ensure consistency and accuracy. Repeated rounds of extraction and assessment were performed until there was near perfect agreement for all key variables. Approximately 20% of charts were extracted in triplicate during the training and assessment process. All charts with a bursal aspiration in the ED or following the ED visit were also reviewed by the principal investigator to ensure accuracy.
Measures
Demographic data, presenting symptoms, comorbidities (history of diabetes, rheumatoid arthritis, gout, human immunodeficiency virus, immunocompromised, steroid use, or other immunocompromised states at the time of the ED visit), ED evaluation and management, outpatient management, and complications within 6 months of the initial ED visit were collected. Complications from antibiotic management including anaphylaxis, allergic reaction, Clostridioides difficile colitis, any clinically significant diarrhea, or other clinically significant complications that were recorded. An uncomplicated resolution was defined as resolution of bursitis without need for subsequent aspiration of the bursa, surgery, or hospitalization.
Data analysis
Continuous features were summarized with medians, interquartile ranges (IQRs), and ranges; categorical features were summarized with frequency counts and percentages. Patient characteristics, ED management, and outcomes were compared using Kruskal‐Wallis, chi‐square, and Fisher’s exact tests based on the type and distribution of the feature under study. Confidence intervals (CIs) for key frequency counts were computed using an asymptotic binomial approximation. Statistical analyses were performed using R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria). All tests were two‐sided and p‐values < 0.05 were considered statistically significant. p‐values were not adjusted based on multiple comparisons.
RESULTS
Participant identification
A total of 458 ED patient visits between January 1, 2011, and December 31, 2018, had a diagnosis of olecranon or nonprepatellar bursitis. After exclusion criteria were applied, a total of 266 ED visits from 264 distinct patients with olecranon bursitis were included. A detailed flowchart of patient enrollment and outcomes is shown in Figure 1. Among the 266 patient visits, medical doctors were the providers for 227 (85.3%) of the visits, and the remaining visits were covered by advanced practice providers. There were 67 total providers included in our study.
FIGURE 1.
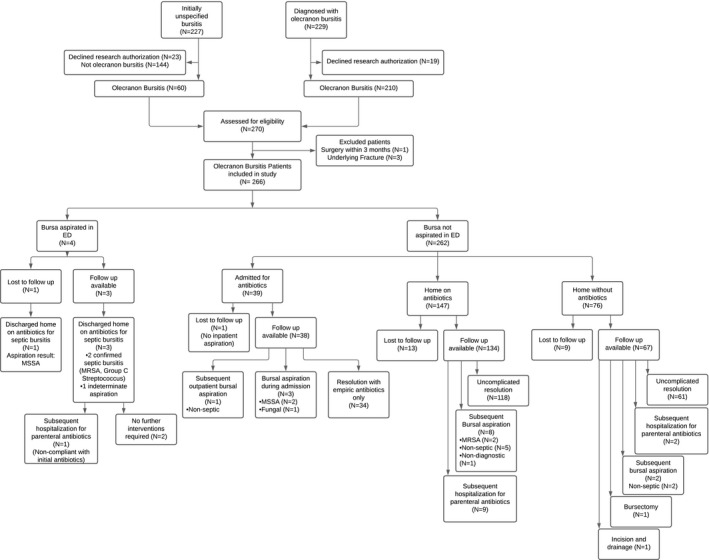
Patient enrollment and outcomes.1One patient had both a subsequent bursal aspiration and subsequent hospitalization for parenteral antibiotics. MRSA, methicillin‐resistant Staphylococcus aureus; MSSA, methicillin‐sensitive Staphylococcus aureus
Descriptive data
The median (IQR) patient age of the cohort was 57 (42–69) years and 85% were male (Table 1). Swelling (94%), erythema (77%), and pain (85%) were the most common presenting symptoms. A total of 39 (15%) patients were taking steroids at the time of their ED visit and 37 (14%) had diabetes. Twenty‐four (9.0%) patients were lost to follow‐up, of which 20 (83%) were males with a median (IQR) age of 51.5 (40–65) years. A total of 229 (86%) had at least 3 months of follow‐up in the EMR and 220 (83%) had at least 6 months of follow‐up.
TABLE 1.
Olecranon bursitis patient and ED management based on ED bursal aspiration and ED disposition
| Characteristic | Patients, No. (%) a | |||||
|---|---|---|---|---|---|---|
| ED bursal aspiration (n = 4) | Admitted (n = 39) | Dismissed with antibiotics (n = 147) | Dismissed without antibiotics (n = 76) | All patients (N = 266) | p value e | |
| Age (years), median (IQR) | 45 (39–52) | 54 (42–61) | 58 (45–70) | 59 (47–69) | 57 (42–69) | 0.583 |
| Sex | 0.041 | |||||
| Female | 0 (0) | 11 (28) | 21 (14) | 7 (9) | 39 (14.6) | |
| Male | 4 (100) | 28 (72) | 126 (86) | 69 (91) | 227 (85.3) | |
| Race | 0.503 | |||||
| White | 4 (100) | 35 (90) | 138 (94) | 69 (91) | 246 (92.8) | |
| Black | 0 (0) | 3 (8) | 3 (2) | 1 (1) | 7 (2.6) | |
| Asian | 0 (0) | 0 (0) | 1 (1) | 1 (1) | 2 (0.7) | |
| Other | 0 (0) | 1 (3) | 5 (3) | 5 (7) | 11 (4.1) | |
| ED presentation | ||||||
| Reported fever | 2 (50) | 9 (23) | 17 (12) | 0 (0) | 28 (10.4) | <0.001 |
| Fever in ED | 0 (0) | 2 (5) | 2 (1) | 0 (0) | 4 (1.5) | 0.144 |
| Erythema | 4 (100) | 39 (100) | 133 (91) | 28 (37) | 204 (77.0) | <0.001 |
| Cellulitis | 0 (0) | 17 (44) | 36 (24) | 4 (5) | 57 (21.4) | <0.001 |
| Warmth | 3 (75) | 30 (77) | 97 (66) | 19 (25) | 149 (56.0) | <0.001 |
| Swelling | 4 (100) | 37 (95) | 142 (97) | 67 (88) | 250 (94.0) | 0.070 |
| Abrasion/wound | 1 (25) | 9 (23) | 49 (33) | 7 (9) | 66 (24.8) | <0.001 |
| Tenderness | 3 (75) | 28 (72) | 100 (68) | 32 (42) | 163 (61.3) | 0.002 |
| Pain | 4 (100) | 36 (92) | 126 (86) | 59 (78) | 225 (84.6) | 0.159 |
| Comorbid conditions | ||||||
| Steroids | 1 (25) | 5 (13) | 22 (15) | 11 (14) | 39 (14.6) | 0.677 |
| HIV | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 1 (0.4) | >0.99 |
| Gout | 0 (0) | 4 (10) | 9 (6) | 9 (12) | 22 (8.2) | 0.420 |
| Arthritis | 0 (0) | 2 (5) | 2 (1) | 0 (0) | 4 (1.5) | 0.136 |
| History of MRSA | 0 (0) | 2 (5) | 4 (3) | 1 (1) | 7 (2.6) | 0.474 |
| Diabetes | 0 (0) | 7 (18) | 17 (12) | 13 (17) | 37 (13.8) | 0.502 |
| Other immunocompromised | 0 (0) | 3 (8) | 2 (1) | 1 (1) | 6 (2.2) | 0.172 |
| Imaging/laboratory values | ||||||
| Radiograph | 2 (50) | 31 (80) | 88 (60) | 40 (53) | 161 (60.5) | 0.030 |
| Ultrasound | 2 (50) | 2 (5) | 10 (7) | 1 (1) | 15 (5.6) | 0.007 |
| WBCs b (cells/mm3) |
10 (9–11) [N = 2] |
10 (7–12) [N = 38] |
10 (8–12) [N = 70] |
9 (8–10) [N = 13] |
10 (8–12) [N = 123] |
0.739 |
| CRP b (µg/dL) |
— [N = 0] |
50 (22–89) [N = 36] |
32 (14–50) [N = 53] |
11 (5–61) [N = 8] |
36 (14–62) [N = 97] |
0.006 |
| ESR b (mm/h) |
— [N = 0] |
19 (10–41) [N = 32] |
11 (6–24) [N = 52] |
12 (7–41) [N = 7] |
14 (7–31) [N = 91] |
0.112 |
| ED orthopedic consult | 0 (0) | 29 (74) | 36 (25) | 4 (5) | 69 (25.9) | <0.001 |
| Antibiotics prescribed at dismissal | 4 (100) | 32 (82) | 147 (100) | 0 (0) | 183 (68.8) | — |
| Cephalosporin (first/second generation) | 0 (0) | 10 (26) | 75 (51) | 0 (0) | 85 (32.0) | — |
| Cephalosporin (third generation) | 0 (0) | 4 (10) | 1 (1) | 0 (0) | 5 (1.9) | — |
| Penicillin | 2 (50) | 1 (3) | 21 (14) | 0 (0) | 23 (8.6) | — |
| Clindamycin | 1 (25) | 0 (0) | 11 (7) | 0 (0) | 12 (4.5) | — |
| Trimethoprim/sulfamethoxazole | 1 (25) | 5 (13) | 11 (7) | 0 (0) | 17 (6.4) | — |
| IV vancomycin | 0 (0) | 3 (8) | 2 (1) | 0 (0) | 5 (1.9) | — |
| Doxycycline | 0 (0) | 3 (8) | 6 (4) | 0 (0) | 9 (3.3) | — |
| Other | 0 (0) | 2 (5) c | 4 (3) d | 0 (0) | 7 (2.6) | — |
| Cephalosporin + trimethoprim/sulfamethoxazole | 0 (0) | 2 (5) | 10 (7) | 0 (0) | 12 (4.5) | — |
| Cephalosporin + doxycycline | 0 (0) | 1 (3) | 2 (1) | 0 (0) | 3 (1.1) | — |
| Penicillin + trimethoprim/sulfamethoxazole | 0 (0) | 1 (3) | 3 (2) | 0 (0) | 4 (1.5) | — |
| Penicillin + doxycycline | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 1 (0.4) | — |
| Inpatient antibiotics | ||||||
| Cephalosporin (first/second generation) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 1 (0.4) | — |
| Trimethoprim/sulfamethoxazole | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 1 (0.4) | — |
| Doxycycline | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 1 (0.4) | — |
| IV cefazolin | 0 (0) | 6 (15) | 0 (0) | 0 (0) | 6 (2.3) | — |
| IV trimethoprim/sulfamethoxazole | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 1 (0.4) | — |
| IV vancomycin | 0 (0) | 15 (38) | 0 (0) | 0 (0) | 15 (5.6) | — |
| Cephazolin + vancomycin | 0 (0) | 4 (10) | 0 (0) | 0 (0) | 4 (1.5) | — |
| Ceftriaxone + vancomycin | 0 (0) | 3 (8) | 0 (0) | 0 (0) | 3 (1.1) | — |
| Vancomycin + other | 0 (0) | 5 (13) | 0 (0) | 0 (0) | 5 (1.9) | — |
| Lost to follow‐up | 1 (25) | 1 (3) | 13 (9) | 9 (12) | 24 (9.0) | 0.174 |
| At least 6 months of follow‐up | 3 (75) | 34 (87) | 122 (83) | 61 (80) | 220 (82.7) | 0.792 |
| At least 3 months of follow‐up | 3 (75) | 34 (87) | 128 (87) | 64 (84) | 229 (86.1) | 0.851 |
Data are reported as n (%) unless otherwise specified. SI conversion factors: To convert WBC to 109/L multiply by 1. To convert CRP to mg/L multiply by 10.
Abbreviations: CRP, C‐reactive protein; ESR, erythrocyte sedimentation rate; HIV, human immunodeficiency virus; IQR, interquartile range; MRSA, methicillin‐resistant Staphylococcus aureus; WBC, white blood cell count.
Unless otherwise noted.
Medians and IQRs are given only for patients with available data, indicated for each entry.
Both patients were dismissed on IV daptomycin.
Two of the four patients were dismissed with MRSA coverage (one IV daptomycin, one minocycline).
p‐values are from comparisons between the four disposition groups given in the table using Kruskal‐Wallis tests for continuous features and chi‐square or Fisher's exact tests for categorical features.
ED diagnostic evaluation and disposition
Diagnostic evaluation included a white blood cell count in 123 (46%) patients, a sedimentation rate in 91 (34%), a C‐reactive protein (CRP) in 97 (36%), and an X‐ray in 161 (61%; Table 1). The orthopedic service was consulted in 69 (26%) of cases.
Overall, among the 266 patients with olecranon bursitis, four (1.5%) patients underwent aspiration of the olecranon bursa during their ED visit. Of the 262 patients who were not aspirated in the ED, 39 (15%) were admitted to the hospital from the ED, 76 (29%) were dismissed from the ED without antibiotic therapy, and 147 (56%) were dismissed from the ED with antibiotic therapy for suspected septic olecranon bursitis (Figure 1). Two patients underwent arthrocentesis to assess for septic arthritis in the ED. Both were negative.
Comparison of patient characteristics based on ED disposition
When patients were compared based on ED disposition, we found that the median (IQR) CRP was highest in patients admitted to the hospital (50 [22–89] µg/dL) and the lowest in patients dismissed without antibiotics (11 [5–61] mg/dL; Table 1). However, there was no significant difference between the median sedimentation rate or median white blood cell count based on disposition. Patients who were initially admitted to the hospital at the time of the index ED visit were the most likely to have reported a fever (23%), have associated cellulitis (44%), and have an orthopedics consult in the ED (74%). Among patients who were dismissed to home without antibiotics, none reported a fever or had a documented fever in the ED. In addition, patients dismissed without antibiotics had the lowest rates of erythema (37%), warmth (25%), and tenderness (42%).
Post‐ED bursitis management and outcomes
Among the four (1.5%) patients who underwent bursal aspiration in the ED, one patient was lost to follow‐up (Table 2). This patient's aspiration culture grew methicillin‐sensitive Staphylococcus aureus. Of the remaining three patients, one aspiration culture grew methicillin‐resistant S. aureus, one grew group C Streptococcus, and one did not show microbial growth or crystals. There were no known complications from the bursal aspirations including future bursectomy or chronic fistula formation.
TABLE 2.
Patient outcomes based on ED bursal aspiration and ED disposition among patients with olecranon bursitis for whom follow‐up was available
| Characteristic | Patients a | |||||
|---|---|---|---|---|---|---|
| ED bursal aspiration (n = 3) | Admitted (n = 38) | Dismissed with antibiotics (n = 134) | Dismissed without antibiotics (n = 67) | All patients (N = 242) | p‐value d | |
| Uncomplicated resolution | 2 (66) | 34 (89) | 118 (88) | 61 (91) | 215 (88.8) | 0.496 |
| Subsequent interventions | ||||||
| Subsequent hospitalization | 1 (25) | 0 (0) | 9 (7) | 2 (3) | 12 (5.0) | 0.053 |
| Bursal surgery | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 1 (0.4) | — |
| Subsequent bursal aspiration | 0 (0) | 4 (10) | 8 (6) | 2 (3) | 14 (5.8) | 0.411 |
| Incision and drainage | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 1 (0.4) | 0.446 |
| Non‐ED aspiration provider b | — | |||||
| Primary care | 0 (0) | 0 (0) | 3 (38) | 2 (100) | 5 (36) | |
| Rheumatology | 0 (0) | 0 (0) | 3 (38) | 0 (0) | 3 (21) | |
| Orthopedics | 0 (0) | 3 (75) | 0 (0) | 0 (0) | 3 (21) | |
| Other | 0 (0) | 1 (25) | 2 (25) | 0 (0) | 3 (21) | |
| Bursitis‐related subsequent visits | 2 (67) | 31 (82) | 79 (59) | 26 (39) | 139 (57.8) | 0.002 |
| Subsequent visits c | ||||||
| Primary care | 1 (50) | 21 (66) | 49 (61) | 19 (73) | 90 (64.3) | |
| Rheumatology | 0 (0) | 0 (0) | 0 (0) | 1 (4) | 1 (0.7) | |
| Orthopedics | 0 (0) | 1 (3) | 3 (4) | 2 (8) | 6 (4.3) | |
| Infectious disease | 0 (0) | 6 (19) | 1 (1) | 0 (0) | 7 (5.0) | |
| ED | 1 (50) | 1 (3) | 23 (29) | 3 (12) | 28 (20) | |
| Other or multiple | 0 (0) | 2 (6) | 3 (4) | 1 (4) | 6 (4.3) | |
| Antibiotic complications | — | |||||
| Allergic reaction | 0 (0) | 0 (0) | 1 (1) | 0 (0) | 1 (0.4) | |
| Anaphylaxis | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
|
C. difficile colitis |
0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Clinically significant diarrhea | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| Other | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
Data are reported as n (%).
Unless otherwise noted.
Includes both outpatient and inpatient aspirations. Percentages are given relative to the number of follow‐up aspirations.
Percentages are given relative to the number of patients with bursitis‐related subsequent visits.
p‐values are from comparisons between the four disposition groups given in the table using Fisher's exact tests for categorical features.
A total of 147 (55%) patients were dismissed home from the ED on empiric antibiotic therapy, including 48 (33%) with coverage for methicillin‐resistant S. aureus (Table 1). Among the 147 patients, 13 (8.8%) were lost to follow‐up. Among the 134 patients with follow‐up available, 118 (88.1%, 95% CI = 81.1%–92.8%) had an uncomplicated resolution and none required subsequent bursa surgery (Figure 1, Table 2). Eight (6.0%, 95% CI = 2.8%–11.8%) patients underwent a bursal aspiration after their ED visit. Of these eight patients, two had confirmed septic bursitis, one had inadequate fluid volume for analysis thought to be due to improvement on the antibiotics, and five had findings consistent with nonseptic bursitis. Nine (6.7%, 95% CI = 3.3%–12.7%) of the 134 patients had a subsequent hospital stay related to their septic bursitis. Among these patients, three (33%) had initially been dismissed from the ED with coverage for methicillin‐resistant S. aureus (MRSA). The median (IQR) time between the index ED visit and subsequent hospitalization was 2 (1–2) days. All of the patients with subsequent hospital stays received inpatient parenteral antibiotics with subsequent full resolution of the bursitis and none underwent bursal aspiration. Twenty‐three (17.2%, 95% CI = 11.4%–25.9%) patients who were dismissed from the ED on antibiotics had a subsequent bursitis‐related ED visit. Among these patients, five (21%) had initially been dismissed from the ED with coverage for MRSA. The median (IQR) time between the initial and subsequent ED visits was 2 (1–3) days. Known antibiotic complications were limited to a single patient who reported an allergic rash. If all patients who were lost to follow‐up were assumed to have had a complicated resolution, 118/147 (80.3%, 95% CI = 72.7%–86.2%) would have had an uncomplicated resolution.
Among the 76 (29%) patients who were dismissed from the ED without antibiotics, nine (12%) were lost to follow‐up. Among the 67 patients with follow‐up available, 65 (97%, 95% CI = 89%–99%) had resolution without any antibiotics, and 61 (91%, 95% CI = 81%–96%) had an uncomplicated resolution (i.e., did not require subsequent aspiration, hospitalization, or surgery; Figure 1, Table 2). One (1%, 95% CI = 0%–9%) patient underwent a subsequent therapeutic aspiration and one (1%, 95% CI = 0%–9%) patient underwent a subsequent diagnostic aspiration that yielded an inadequate sample for analysis and was believed to be nonseptic. One (1%, 95% CI = 0%–9%) patient underwent an olecranon bursectomy and partial ostectomy of the olecranon due to recurrent bursitis thought to be secondary to sports‐related overuse. One patient had a subsequent arthrocentesis to assess for septic arthritis, which was negative. Two (3%, 95% CI = 1%–11%) patients had a subsequent hospital stay and received inpatient antibiotics before obtaining a full resolution. Of the patients with a hospital stay, none underwent a bursal aspiration.
Among the 39 (15%) patients who were admitted to the hospital at the time of the index ED visit for inpatient antibiotic therapy, 30 (77%) were treated with antibiotics covering MRSA (Table 1). One patient was lost to follow‐up (Figure 1). Among the 38 patients for which follow‐up was available, 34 (89%, 95% CI = 74%–97%) had an uncomplicated resolution with only empiric antibiotics. Three (8%) of the 38 patients with follow‐up had resolution after aspiration during their admission. Two of the aspiration cultures grew methicillin‐sensitive S. aureus and one grew Prototheca wickerhamii. One (3%) patient among the 38 with follow‐up had a subsequent outpatient aspiration which was non‐septic. No patients underwent subsequent surgeries or hospital stays related to their olecranon bursitis (Table 2). Thirty‐one (82%) had a subsequent bursitis‐related outpatient follow‐up, including one (3%, 95% CI = 0%–15%) who had a subsequent bursitis‐related ED visit.
DISCUSSION
We studied the management of ED patients presenting with acute olecranon bursitis and found that among 266 patients included in our study only four (1.5%) underwent bursal aspiration at the time of their initial ED visit. To our knowledge, this represents the largest study of ED patients with olecranon bursitis. Among patients who did not undergo bursal aspiration in the ED and were dismissed home on oral antibiotics for suspected septic olecranon bursitis, 88% had an uncomplicated resolution, 7% were subsequently hospitalized, and 6% subsequently underwent bursal aspiration, including two patients with confirmation of septic bursitis and five patients with septic bursitis ruled out. In addition, among patients admitted for suspected septic bursitis, 89% did not undergo bursal aspiration at any point and all of these patients had an uncomplicated resolution on antibiotics. Among patients dismissed without antibiotics, only two patients (3%) required subsequent hospitalization for parenteral antibiotics for a possible, although unconfirmed, septic bursitis. None of the patients in our cohort with confirmed or suspected septic bursitis went on to develop a chronic wound or require operative management. Taken together, these findings suggest that empiric antibiotic administration for suspected septic bursitis without bursal aspiration may be an appropriate first‐line management strategy among select ED patients with suspected septic olecranon bursitis who are reliable, understand return precautions, and are at low risk of antibiotic complications and treatment failure.
While it is known that physical examination is not reliable for establishing the diagnosis of septic versus nonseptic bursitis, 5 it has not been established if bursal aspiration is necessary for definitive diagnosis or if empiric antibiotic administration is a reasonable initial approach for management of suspected septic olecranon bursitis at the time of ED evaluation. 5 Many guidelines advocate for bursal aspiration if there is suspicion of septic bursitis. 1 , 2 , 3 , 5 , 6 However, aspiration of the bursa has been shown to lead to potential complications including fistula formation, infection, and future bursectomies. 3 , 7 Fifty‐five percent of patients in our cohort were dismissed on empiric antibiotics, which is consistent with a prior ED study that found that approximately 50% of olecranon bursitis cases were septic. 2 A recent study of 30 patients referred to an orthopedic surgical department demonstrated that, among patients who had undergone an olecranon bursal aspiration for septic bursitis, 55% developed a chronic draining wound at the aspiration site and 73% went on to eventual bursectomy. 3 In comparison, none of the patients in that study who had been treated with empiric antibiotics went on to develop a chronic wound or require bursectomy. In another study of 31 patients admitted to the hospital for septic olecranon bursitis after undergoing bursal aspiration, 10% required an operative intervention. 10 Similarly, in a study of 22 ED patients with septic olecranon bursitis based on bursal aspirates, three (14%) patients developed a chronic fistula tract and one (4.5%) required incision and drainage. 2
Initial management of suspected septic olecranon bursitis with empiric antibiotic management among ED patients has not been well described. Two findings in our study suggest that empiric antibiotics may be a reasonable initial management strategy, including: (1) 89% of the patients admitted to the hospital for empiric antibiotic management for whom follow‐up was available did not undergo bursal aspiration in the ED or after admission and 100% of these patients had an uncomplicated resolution, and (2) among patients dismissed on empiric antibiotics with follow‐up available, 88% of had an uncomplicated resolution. Additionally, if all of the 14 patients initially treated with empiric antibiotics without bursal aspiration who were lost to follow‐up were assumed to have experienced a complication, 82% would have had an uncomplicated resolution. Although findings among patients referred to an orthopedic surgical department, as discussed above, also favor empiric antibiotic management without bursal aspiration, they are not definitive given that the patient population was likely biased toward those with recalcitrant or complicated courses. 3
Contemporary studies of olecranon bursitis management among ED patients not undergoing bursal aspiration are lacking. A study conducted among patients with septic olecranon bursitis who had been referred to a home parenteral therapy program reported that 49% of patients with suspected septic bursitis were not aspirated and were only treated with antibiotics. They reported no difference in outcome among patients who were aspirated and those who were not, although 38% of those who underwent a drainage procedure required more than one drainage procedure. 11 Studies conducted several decades ago reported that among patients with septic bursitis treated with outpatient antibiotics, 38%–75% went on to require inpatient parenteral antibiotics. 12 , 13 In contrast, only 6% of patients treated with empiric outpatient antibiotics in our study went on to require hospitalization for inpatient antibiotics, although they were more likely to have a subsequent bursitis‐related ED visit.
Empiric antibiotic management has been criticized as possibly leading to lowered diagnostic accuracy and poor antibiotic stewardship. 11 Eight patients who were initially dismissed from the ED on empiric antibiotics in our study for suspected septic bursitis did not have resolution with empiric antibiotic therapy and underwent a subsequent aspiration. Five of these patients were found to have nonseptic bursitis. These patients as well as some patients who did have resolution after empiric antibiotics may have received antibiotics unnecessarily, placing them at unnecessary risk for antibiotic complications. With increasing antibiotic resistance and complications such as C. difficile colitis, these risks are important to consider when assessing the benefits of empiric antibiotic management. 14
Among patients who were dismissed home on empiric antibiotic coverage, 33% received MRSA coverage, in contrast to 77% of patients who were admitted to the hospital. This is likely because admitted patients were more systemically ill as demonstrated by higher rates of associated fever, cellulitis, and elevated CRP.
Only three patients in our cohort underwent arthrocentesis to assess for possible concomitant septic arthritis and none had septic arthritis. Rates of concomitant presentations of septic bursitis with septic arthritis have not been described, to our knowledge, likely because the presence of septic arthritis is often an exclusion criterion for studies of bursitis. 3 , 10 Furthermore, to our knowledge, there have been no studies evaluating the reliability of physical examination for distinguishing septic bursitis from septic arthritis. However, anecdotally, septic arthritis is typically suspected in the presence of substantial pain throughout range of motion while allowing for discomfort due to tension on the bursa with maximal flexion. 3
LIMITATIONS
Our study has several limitations. All patients were included retrospectively and the data quality is dependent on the accuracy of the medical records. To mitigate these limitations, we adhered to standardized guidelines for observational studies and used a data abstraction form that was designed to optimize precision and accuracy of collected variables and minimize random and systematic errors. Abstractors were not blinded to the study objectives. We conducted our study in a single quaternary care ED and most of our visits were covered by medical doctors. Practice patterns and provider distribution may vary at other institutions. Our ED has a robust follow‐up system and a high percentage of patients who have a primary care provider. This is not the case for all EDs. Because most patients did not undergo an aspiration of the bursa, some nonseptic cases could have been included in the cohort of suspected septic bursitis. An additional limitation was the lack of diversity in our patient population, which was predominantly white, limiting generalizability; however, 85% were males with a median age of 57 years, which is similar to prior studies. 3 , 15 Finally, 24 patients were lost to follow‐up and therefore outcomes for these patients are unknown.
CONCLUSIONS
Eighty‐eight percent of ED patients with suspected septic olecranon bursitis treated with empiric outpatient antibiotics without aspiration had resolution without need for subsequent bursal aspiration, hospitalization, or surgery. Eighty‐nine percent of patients admitted to the hospital for empiric antibiotic management for whom follow‐up was available did not undergo bursal aspiration in the ED or after admission and 100% of these patients had an uncomplicated resolution. Our findings suggest that empiric antibiotics without bursal aspiration is a reasonable initial approach to ED management of select patients with suspected septic olecranon bursitis who have adequate access to follow‐up care, are immunocompetent, are able to tolerate oral antibiotics, and are at low risk for antibiotic complications.
CONFLICT OF INTEREST
The authors have no potential conflicts to disclose.
AUTHOR CONTRIBUTIONS
Study concept and design: Ronna L. Campbell, Kristina M. Colbenson, Benjamin J. Sandefur, Alexa L. Thomas, Adrian Beyde. Acquisition of data: Alexa L. Thomas, Adrian Beyde, Imtithal Kisirwan, Benjamin J. Sandefur, Ronna L. Campbell. Analysis and interpretation of the data: Ronna L. Campbell, Alexa L. Thomas, Aidan F. Mullan, Shawn W. O’Driscoll. Drafting of the manuscript: Ronna L. Campbell, Alexa L. Thomas, Aidan F. Mullan, Adrian Beyde. Critical revision of the manuscript: all authors. Statistical expertise: Aidan F. Mullan.
ACKNOWLEDGMENT
The authors thank Jennifer L. Condon for her assistance with data acquisition.
Beyde A, Thomas AL, Colbenson KM, et al. Efficacy of empiric antibiotic management of septic olecranon bursitis without bursal aspiration in emergency department patients. Acad Emerg Med. 2022;29:6–14. doi: 10.1111/acem.14406
Presented at the Society for Academic Emergency Medicine Virtual Meeting, May 2020.
Supervising Editor: Michael S. Runyon, MD, MPH.
Funding information
This publication was made possible in part by the Mayo Clinic CTSA through grant number UL1TR002377 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
REFERENCES
- 1. Lormeau C, Cormier G, Sigaux J, Arvieux C, Semerano L. Management of septic bursitis. Joint Bone Spine. 2019;86:583‐588. [DOI] [PubMed] [Google Scholar]
- 2. Stell IM. Management of acute bursitis: outcome study of a structured approach. J R Soc Med. 1999;92:516‐521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Deal JB Jr, Vaslow AS, Bickley RJ, Verwiebe EG, Ryan PM. Empirical treatment of uncomplicated septic olecranon bursitis without aspiration. J Hand Surg Am. 2020;45:20‐25. [DOI] [PubMed] [Google Scholar]
- 4. Sayegh ET, Strauch RJ. Treatment of olecranon bursitis: a systematic review. Arch Orthop Trauma Surg. 2014;134:1517‐1536. [DOI] [PubMed] [Google Scholar]
- 5. Baumbach SF, Lobo CM, Badyine I, Mutschler W, Kanz KG. Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Arch Orthop Trauma Surg. 2014;134:359‐370. [DOI] [PubMed] [Google Scholar]
- 6. McFarland EG, Mamanee P, Queale WS, Cosgarea AJ. Olecranon and prepatellar bursitis: treating acute, chronic, and inflamed. Phys Sportsmed. 2000;28:40‐52. [DOI] [PubMed] [Google Scholar]
- 7. Degreef I, De Smet L. Complications following resection of the olecranon bursa. Acta Orthop Belg. 2006;72:400‐403. [PubMed] [Google Scholar]
- 8. Elm EV, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806‐808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata‐driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lieber SB, Fowler ML, Zhu C, Moore A, Shmerling RH, Paz Z. Clinical characteristics and outcomes of septic bursitis. Infection. 2017;45:781‐786. [DOI] [PubMed] [Google Scholar]
- 11. Laupland KB, Davies HD; Calgary Home Parenteral Therapy Program Study Group . Olecranon septic bursitis managed in an ambulatory setting. The Calgary Home Parenteral Therapy Program Study Group. Clin Invest Med. 2001;24:171‐178. [PubMed] [Google Scholar]
- 12. Ho G Jr, Tice AD, Kaplan SR. Septic bursitis in the prepatellar and olecranon bursae: an analysis of 25 cases. Ann Intern Med. 1978;89:21‐27. [DOI] [PubMed] [Google Scholar]
- 13. Raddatz DA, Hoffman GS, Franck WA. Septic bursitis: presentation, treatment and prognosis. J Rheumatol. 1987;14:1160‐1163. [PubMed] [Google Scholar]
- 14. Frieri M, Kumar K, Boutin A. Antibiotic resistance. J Infect Public Health. 2017;10:369‐378. [DOI] [PubMed] [Google Scholar]
- 15. Garcia‐Porrua C, Gonzalez‐Gay MA, Ibanez D, Garcia‐Pais MJ. The clinical spectrum of severe septic bursitis in northwestern Spain: a 10 year study. J Rheumatol. 1999;26:663‐667. [PubMed] [Google Scholar]


