Abstract
Purpose:
To describe a modification to the traditional Gundersen flap technique that expands eligible eyes to include those with severe conjunctival scarring and to report results from a clinical case.
Methods:
A 68-year old woman with a history of herpes simplex keratitis, multiple failed penetrating keratoplasties, lagophthalmos, persistent epithelial defect and low visual potential in the left eye presented for evaluation for a Gundersen flap. Severe superior bulbar conjunctival scarring precluded a traditional approach. A modified Gundersen flap technique using a contiguous flap of inferior palpebral-bulbar conjunctiva extending from the inferior tarsal border to the limbus was devised and performed.
Results:
The modified Gundersen flap technique successfully stabilized the ocular surface, obviating the need for a cosmetically disfiguring permanent tarsorrhaphy or an evisceration.
Conclusion:
This modified Gundersen flap technique expands the indications to eyes with severe conjunctival scarring and can be offered in eyes with prior trabeculectomies, glaucoma drainage implants, and scleral buckles which were previously excluded from the globe-preserving option.
Keywords: Gundersen conjunctival flap, neurotropic keratopathy, exposure keratopathy, lagophthalmos, cornea ulcer
Introduction
For eyes with poor visual potential and challenging ocular surface disorders, a Gundersen flap is an excellent, if under-utilized, globe-preserving option. While it can be technically challenging to perform well, a Gundersen flap offers a less invasive option that avoids the risks associated with intraocular surgery. For example, in eyes with low visual potential and bullous keratopathy where cornea transplantation is not recommended, a Gundersen flap can treat ocular surface pain as well as an endothelial keratoplasty. For infectious corneal ulcers refractory to medical treatment, a conjunctival flap can eradicate infection and avoid a therapeutic penetrating keratoplasty.
Originally described by Trygve Gundersen in 1958,1 his namesake technique involves creating a 360 degree conjunctival peritomy, removing the corneal epithelium, and mobilizing a large flap of superior bulbar conjunctiva over the cornea. Significant scarring of the bulbar conjunctiva may preclude a traditional Gundersen flap, which requires healthy, freely mobile superior conjunctiva. In this report of a patient with substantial superior bulbar conjunctival scarring, we describe a modification to the Gundersen flap technique highlighted by the mobilization of an inferior palpebral-bulbar conjunctival flap to cover the cornea.
Case Report
A 68 year-old woman with a complex ocular history leaving her with low visual potential in the left eye presented for evaluation. In childhood, she had received numerous eyelid surgeries for congenital bilateral ptosis, blepharophimosis, and telecanthus. As an adult, persistent lagophthalmos, exposure keratopathy and acquired neurotrophic cornea secondary to herpes simplex keratitis resulted in numerous complications including recurrent bacterial and fungal corneal ulcers (Fig 1a) that subsequently required four penetrating keratoplasties (Fig 1b). She eventually underwent cataract surgery but unfortunately visual improvement was limited to hand motions and a fundus examination revealed severe optic nerve pallor consistent with a prior ischemic optic neuropathy or post-infectious optic nerve injury. Multiple reconstructive eyelid procedures were performed to improve eyelid closure, including posterior lamella recession with full thickness skin grafting, posterior lamellar spacer grafting and fornix reconstruction with mucous membrane placement. Unfortunately, the patient continued to develop persistent corneal epithelial defects and neurotropic ulcers. A permanent tarsorrhaphy was cosmetically unacceptable to the patient so an exhaustive list of alternative options were pursued to maintain corneal epithelial integrity, including frequent lubrication with ointment, placement of amniotic membrane grafts, bandage contact lenses, cenegermin nerve growth factor, autologous serum tears, as well as additional eyelid surgeries including cicatricial upper eyelid retraction using a posterior lamella spacer graft, full thickness blepharotomy, hard palate graft for additional tarsal support and multiple temporary tarsorrhaphies. Despite all of these attempts, her corneal surface remained tenuous. She developed a sensory exotropia and the patient was aesthetically displeased with her eyelid ptosis and ocular surface appearance.
Figure 1.
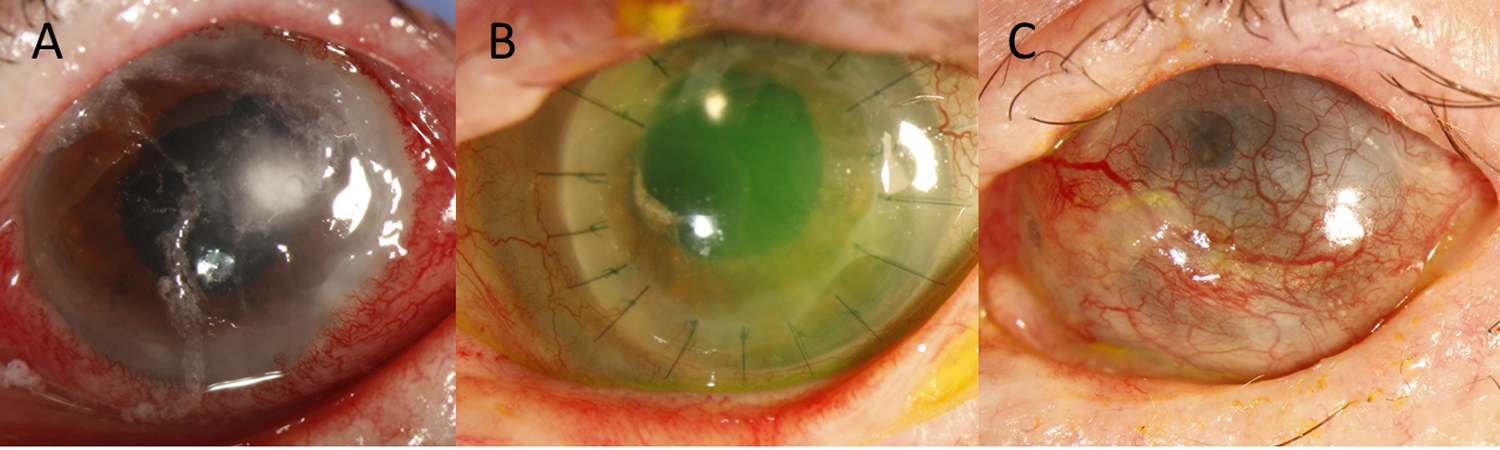
Clinical case progression from initial presentation to final outcome. (A) Slit-lamp photo at initial presentation with Candida albicans corneal ulcer. (b) Slit-lamp photo following final penetrating keratoplasty with a persistent central epithelial defect. (c) Slit-lamp photo status post modified palpebral-bulbar conjunctival Gundersen flap.
In light of her low visual potential, an evisceration with prosthesis versus a modified Gundersen flap were offered and the patient opted for the latter. Due to the extensive prior surgical history, there was significant scarring of the superior bulbar conjunctiva, precluding a traditional Gundersen flap. As such, a modified approach was designed to cover the cornea with a contiguous flap of inferior palpebral-bulbar conjunctiva.
Surgical Technique
A 4–0 silk suture was placed through the inferior eyelid margin to retract the lower eyelid. A 6–0 vicryl traction suture was placed through the inferior peripheral cornea and the eye supraducted to provide exposure. The distance between the inferior tarsal border to the inferior limbus was marked and measured. Subconjunctival 2% lidocaine was injected adjacent to the inferior tarsal border, creating a bleb that partially extended across the inferior palpebral, forniceal, and bulbar conjunctiva due to conjunctival scarring. Sharp Westcott scissors were used to incise the conjunctiva along the inferior border of the tarsus. Blunt Westcott scissors, with tips turned away from the conjunctiva, were used to separate the conjunctiva from the lower lid retractors to the level of the inferior fornix (Fig 2a, 3a). The conjunctiva was grasped gently with tissue forceps while toothed forceps were used to provide counter traction on the retractors. Horizontal dissection extended from the medial to the temporal fornix and vertically from the inferior tarsal border, past the fornix, and onto the bulbar conjunctiva to the limbus (Fig 2b, 3b). A mixture of blunt and sharp dissection was performed with Westcott scissors to lyse conjunctival scar tissue, with meticulous care to avoid buttonholing and tearing the conjunctiva by keeping the scissor tips directed away from the flap (Supplemental Digital Content Video 1). Using blunt Westcott scissors, the bulbar conjunctival dissection was extended to the inferior limbus and then into medial and lateral pockets from 2 to 10 o’clock (Fig 2c, 3c), part of the overarching principle of creating a generous, broad conjunctival dissection to ensure sufficient size of the flap as well as to facilitate mobility. A conjunctival peritomy from 3 to 9:00 o’clock was performed (Fig 2d, 3d). A 15 mm by 20 mm mucous membrane graft was harvested and secured over the inferior palpebral defect using fibrin glue (Fig 2e, 3e) and trimmed to size. The corneal epithelium was removed using a #69 blade and the flap mobilized onto the cornea and secured in place with interrupted 8–0 vicryl sutures along the inferior and superior limbus (Fig 2f, 3f). The inferior bulbar conjunctiva defect was then covered with a 1.0 cm by 1.5 cm amniotic membrane graft using fibrin glue (Fig 3f). A symblepharon ring was placed, followed by a Frost suture for eyelid closure.
Figure 2.

Surgical steps of the modified Gundersen flap using palpebral-bulbar conjunctiva. (A) The inferior palpebral conjunctival dissection is initiated, (B) extending to the inferior bulbar conjunctiva, (C) and further medially and laterally. (D) A conjunctival peritomy is created. (E) A mucous membrane graft is secured to the inferior palpebral area using Tisseel glue. The modified Gundersen flap is mobilized to cover the cornea, (F) and secured in place with 8–0 vicryl sutures.
Figure 3.
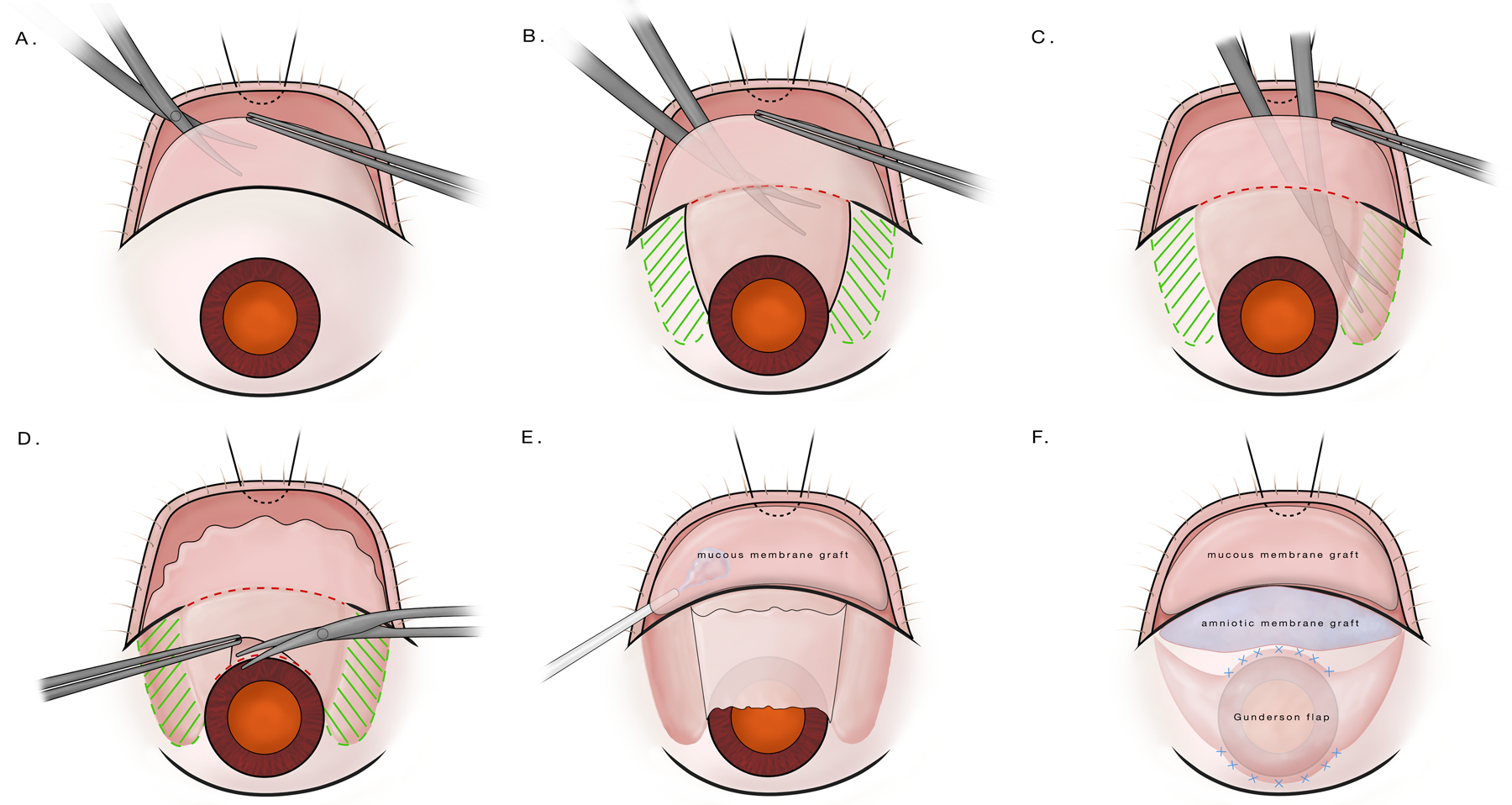
Illustrated surgical steps of the modified Gundersen flap using palpebral-bulbar conjunctiva. (A) The inferior palpebral conjunctival dissection is initiated, (B) extending to the inferior bulbar conjunctiva, (C) and further medially and laterally. (D) A conjunctival peritomy is created. (E) A mucous membrane graft is secured to the inferior palpebral area using Tisseel glue. The modified Gundersen flap is mobilized to cover the cornea, (F) and secured in place with 8–0 vicryl sutures.
Three weeks post-operatively, a 3 mm x 1.5 mm area of inferonasal flap retraction with cornea thinning was observed, corresponding to appositional pressure from the symblepharon ring. The ring was removed and a multi-layered amniotic membrane graft was secured over the area of cornea thinning using fibrin glue. This resulted in rapid epithelialization and there has been no further flap retraction or epithelial breakdown over 6 months of follow up (Fig 1c).
Discussion
Eyes with neurotropic corneas, lagophthalmos, and exposure keratopathy are among the most challenging of conditions for cornea specialists. These eyes often benefit from a scleral lens, which unfortunately was not possible in this case due to a tight palpebral fissure and scarred eyelids. Newer therapies such as cenegermin nerve growth factor, serum tears, and plasma rich in growth factor are promising approaches to treat persistent corneal epithelial defects, but are often insufficient in maintaining ocular surface stability in the most extreme cases, such as this one.2–4 The newer surgical approach of cornea neurotization has demonstrated success in some cases of neurotrophic keratopathy, but its role and efficacy are still being investigated.5 An exhaustive list of therapies had been tried for this patient, and only the simple permanent tarsorrhaphy provided reliable success. However, due to its cosmetically disfiguring nature, a tarsorrhaphy was not an acceptable long-term option for this patient. As a last resort option prior to evisceration, we turned to another oldie but goodie: the Gundersen flap.
By providing metabolic and mechanical support, pedicle and total conjunctival flaps can be used to heal corneal ulcers refractory to treatment and provide ocular surface stability to prevent further epithelial breakdown and infection.6 In addition, a successfully performed Gundersen flap offers ocular surface pain control7 as well as improved cosmesis compared to advanced corneal scarring and band keratopathy. Sufficiently mobile conjunctiva is needed for a Gundersen flap, a requirement that may not be met in severely diseased eyes such as with our patient.
In this case, in light of the superior symblepharon, short superior fornix, and extensive superior bulbar conjunctival scarring rendering it non-mobile, we modified the Gundersen flap technique by mobilizing a contiguous flap of inferior palpebral-bulbar conjunctiva. This created a nasal and temporal bi-pedicled flap which was secured over the entire cornea, thus achieving the same goals of a traditional Gundersen flap. Additionally, the bare palpebral donor site was covered with oral mucous membrane graft, a combination approach that has been reported to improve outcome by preventing symblepharon formation.8
Our modified technique expands the clinical scenarios for which a Gundersen flap can be offered. Severe corneal disease often co-present with glaucoma and retinal pathology, conditions that may require surgeries that leave only limited healthy conjunctiva. Low visual potential eyes with a trabeculectomy, glaucoma drainage implant, or scleral buckle that don’t qualify for a traditional Gundersen flap may be successfully managed with this modified technique as a globe-preserving option.
As with a traditional Gundersen flap, success of this modified approach requires meticulous surgical technique. Careful dissection must be performed to avoid buttonholing or tearing the flap, which can lead to retraction. The goal should be to obtain a thin flap, but the inferior palpebral conjunctival portion will likely be thicker due to greater adherence of tissue in that area. This thicker portion of the flap does have a silver lining as it is less prone to inadvertent buttonholing and provides a more robust covering over the inferior area most affected by lagophthalmos. Close monitoring in the early post-operative course is crucial. In our case, early inferonasal peripheral flap retraction caused by mechanical pressure from a symblepharon ring was diagnosed promptly and successfully managed with multi-layered amniotic membrane transplantation.
This case emphasizes the importance of close collaboration with an oculoplastics specialist to manage severe ocular surface disease, a partnership that culminated in a creative modification of a Gundersen flap to preserve the globe. Even with careful follow-up and close collaboration between cornea and oculoplastics specialists, a spiral of complications can ensue. Various surgical solutions can be pursued to address the exposure and rehabilitate the ocular surface. However, in extreme cases of intractable lagophthalmos and poor visual potential, a Gundersen conjunctival flap is a good globe-preserving option.
Supplementary Material
Supplemental Digital Content Video 1. Modified Gundersen Flap. In this surgical video, a contiguous inferior palpebral-bulbar conjunctival flap is created and mobilized to cover the entire cornea. A mucous membrane graft and amniotic membrane graft are secured with Tisseel glue to the inferior palpebral and bulbar areas, respectively.
Acknowledgments
Financial Support: This work was supported by National Eye Institute core grant P30–026877 (Stanford) and Research to Prevent Blindness. The sponsors or funding organizations had no role in the design or conduct of this research.
Footnotes
Conflict of Interest: None of the authors have a proprietary/financial interest to disclose.
References:
- 1.Gundersen T Conjunctival flaps in the treatment of corneal disease with reference to a new technique of application. AMA Arch Ophthalmol. 1958;60(5):880–888. [DOI] [PubMed] [Google Scholar]
- 2.Pflugfelder SC, Massaro-Giordano M, Perez VL, et al. Topical Recombinant Human Nerve Growth Factor (Cenegermin) for Neurotrophic Keratopathy: A Multicenter Randomized Vehicle-Controlled Pivotal Trial. Ophthalmology. 2020;127(1):14–26. [DOI] [PubMed] [Google Scholar]
- 3.Semeraro F, Forbice E, Braga O, Bova A, Di Salvatore A, Azzolini C. Evaluation of the efficacy of 50% autologous serum eye drops in different ocular surface pathologies. Biomed Res Int. 2014;2014:826970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez-Plandolit S, Morales MC, Freire V, Etxebarria J, Duran JA. Plasma rich in growth factors as a therapeutic agent for persistent corneal epithelial defects. Cornea. 2010;29(8):843–848. [DOI] [PubMed] [Google Scholar]
- 5.Park JK, Charlson ES, Leyngold I, Kossler AL. Corneal Neurotization: A Review of Pathophysiology and Outcomes. Ophthalmic Plast Reconstr Surg. 2020;36(5):431–437. [DOI] [PubMed] [Google Scholar]
- 6.Zemba M, Stamate AC, Tataru CP, Branisteanu DC, Balta F. Conjunctival flap surgery in the management of ocular surface disease (Review). Exp Ther Med. 2020;20(4):3412–3416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khodadoust A, Quinter AP. Microsurgical approach to the conjunctival flap. Arch Ophthalmol. 2003;121(8):1189–1193. [DOI] [PubMed] [Google Scholar]
- 8.Cheng KC, Chang CH. Modified gunderson conjunctival flap combined with an oral mucosal graft to treat an intractable corneal lysis after chemical burn: a case report. Kaohsiung J Med Sci. 2006;22(5):247–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content Video 1. Modified Gundersen Flap. In this surgical video, a contiguous inferior palpebral-bulbar conjunctival flap is created and mobilized to cover the entire cornea. A mucous membrane graft and amniotic membrane graft are secured with Tisseel glue to the inferior palpebral and bulbar areas, respectively.


