Abstract
Colchicine is an ancient herbal drug derived from Colchicum autumnale. It was first used to treat familial Mediterranean fever and gout. Based on its unique efficacy as an anti-inflammatory agent, colchicine has been used in the therapy of cardiovascular diseases including coronary artery disease, atherosclerosis, recurrent pericarditis, vascular restenosis, heart failure, and myocardial infarction. More recently, colchicine has also shown therapeutic efficacy in alleviating cardiovascular complications of COVID-19. COLCOT and LoDoCo2 are two milestone clinical trials that confirm the curative effect of long-term administration of colchicine in reducing the incidence of cardiovascular events in patients with coronary artery disease. There is growing interest in studying the anti-inflammatory mechanisms of colchicine. The anti-inflammatory action of colchicine is mediated mainly through inhibiting the assembly of microtubules. At the cellular level, colchicine inhibits the following: (1) endothelial cell dysfunction and inflammation; (2) smooth muscle cell proliferation and migration; (3) macrophage chemotaxis, migration, and adhesion; (4) platelet activation. At the molecular level, colchicine reduces proinflammatory cytokine release and inhibits NF-κB signaling and NLRP3 inflammasome activation. In this review, we summarize the current clinical trials with proven curative effect of colchicine in treating cardiovascular diseases. We also systematically discuss the mechanisms of colchicine action in cardiovascular therapeutics. Altogether, colchicine, a bioactive constituent from an ancient medicinal herb, exerts unique anti-inflammatory effects and prominent cardiovascular actions, and will charter a new page in cardiovascular medicine.
Keywords: colchicine, anti-inflammatory drug, cardiovascular diseases, coronary artery disease, atherosclerosis, recurrent pericarditis, restenosis, heart failure, myocardial infarction, cardiovascular complications of COVID-19, microtubules, NF-κB, NLRP3 inflammasome
Introduction
Inflammation is a series of local and systemic immune system responses that our body activates in response to an encounter with harmful stimuli. The inflammatory response can be considered as a combination of nonspecific immunity response. The protective function of inflammation includes removing harmful invading pathogens, repairing organ damage, and maintaining tissue homeostasis [1]. Upon the initiation of an inflammatory response, immune cells are mobilized to migrate into the site of an inflammation. At the same time, blood vessels at the inflammatory site are constricted and capillary permeability is increased [2]. The flow of blood slows and some endogenous and exogenous pyrogens are produced. These changes in the vasculature lead to the dysregulation of inflammation. Cardiovascular disease (CVD) as a non-communicable disease, is the major world-wide threat to human life. According to the latest statistics, the number of CVD patients around the world has increased from 271 million in 1990 to 523 million in 2019 [3]. The number of deaths caused by coronary artery disease (CAD) in the world has increased from 1.2 million in 1990 to 18.6 million in 2019 [4]. In recent years, studies have supported the notion that chronic inflammation is closely associated with the progression and development of CVD. The canakinumab anti-inflammatory thrombosis outcome study (CANTOS) of an anti-inflammatory biological intervention provided direct proof that the inflammatory process plays an important role in the pathogenesis of CAD and related complications. Thus anti-inflammatory strategies may reduce or mitigate the risk of cardiovascular events [5]. From canakinumab [5] to colchicine [6], anti-inflammatory therapies are poised to create a revolution in the treatment of CVD.
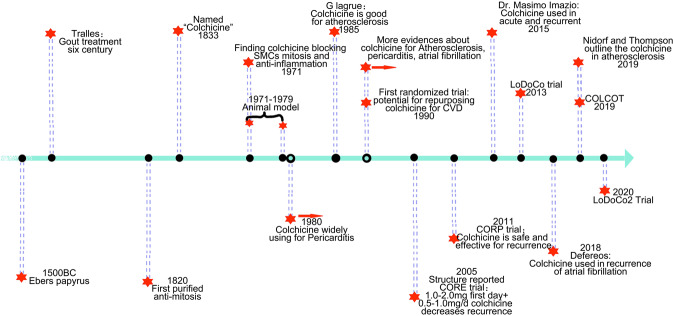
Colchicine is an alkaloid isolated and purified from an ancient medicinal plant, autumn crocus (or named Colchicum autumnale). Such products have been used to treat pain and reduce tissue swelling [7] for thousands of years in China. The research timeline of colchicine in medicinal history is shown in Fig. 1. The earliest use of colchicine dates back to Ebers papyrus [8] before 1550 BC. However, there still exists more uncertainties about the safety profile of colchicine. Until the sixth century, one of the most eminent Byzantine physicians Alexander of Tralles first used colchicine to treat gout [9]. In 1820, this legendary drug, colchicine, was purified for the first time by two French chemists, Jean Bienaime Caventou and Pierre Joseph Pelletier. At the same time, a pathologist of Sicilian Biaggio Pernice [10] discovered the anti-mitotic action of colchicine. In 1833, Geiger et al. purified and named colchicine. In 2005, the structure of colchicine as a bioactive component in tricyclic alkaloid category, was reported. Colchicine has shown good anti-inflammatory effects and thus is considered as a potential treatment for acute inflammatory phase of gout. In 2009, colchicine was approved by the US FDA for familial Mediterranean fever (FMF) and for preventing and treating gout attacks. Mechanistic studies revealed that colchicine binds to microtubules, which affects many cellular processes, and colchicine also inhibits the expression of many inflammatory cytokines. Now that the concept that chronic inflammation contributes to CVDs such as CAD is gaining more scientific attraction. Colchicine’s unique anti-inflammatory mechanism has fostered further studies in the area of cardiovascular medicine. Currently, the use of colchicine in cardiovascular therapy remains very limited. Recently, the disease of COVID-19 has caused serious economic losses, casualties, and deaths worldwide. The cytokine storm caused by the SARS-CoV2 is also a serious risk for CVD in terms of endotheliitis and thrombosis [11]. In terms of the prominent protective effects of colchicine in infectious and inflammatory diseases which include CVD, here, we have summarized the history of the discovery of colchicine and its clinical applications in patients suffering from CVD. In particular, we systematically review the molecular targets and mechanisms of colchicine in treating and preventing CVD. The protective effects of colchicine in infections and inflammatory diseases suggest it may have therapeutic potential against CVD.
Fig. 1. Timeline and milestone of colchicine in medicinal history.
The use of colchicine dates back to Ebers papyrus. Until 1833, the legendary drug was named as “Colchicine”. From 1971 to 1979, many preclinical studies demonstrated the efficacy of colchicine in the treatment of inflammatory diseases. At the end of the 20th century, mounting evidences proved that colchicine is beneficial to cardiovascular diseases, such as atherosclerosis, pericarditis, atrial fibrillation. Until 2005, the structure of colchicine was first reported, and then clinical trials involving colchicine for cardiovascular disease were actively pursued.
Colchicine-based-clinical trials
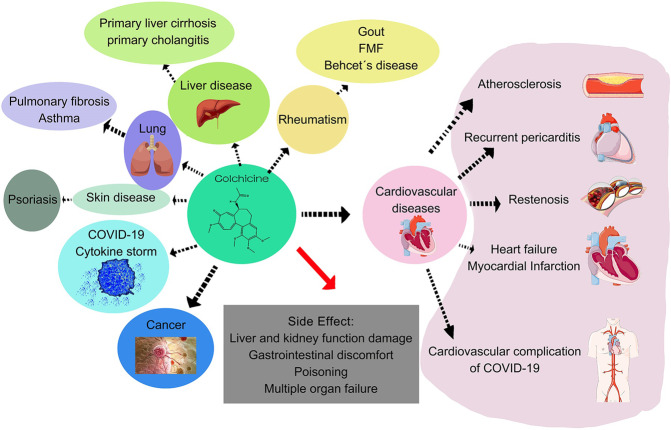
Colchicine has been used as an anti-inflammatory agent to treat disease in China for thousands of years. It has been mainly used in the treatment of FMF, gout, pericarditis, and other diseases in the last hundred years (Fig. 2). Meanwhile, the role of colchicine in the progression of atherosclerotic CVD has been clearly elucidated [1]. However, there are contradicting findings in relation to the use of colchicine in cardiovascular disease. Canakinumab (a monoclonal antibody that inhibits the IL-1β signaling pathway) decreased by about 15% of CVD events in CANTOS [5]. The evidence from CANTOS trials provided the proof-of-concept evidence that targeting inflammation is therapeutically efficacious. As a potent anti-inflammatory drug in treating inflammation-associated disorders, colchicine is proposed to exhibit cardiovascular protective action in patients with CVD. In the later sections, we will address the clinical trials of colchicine, including the LoDoCo, LoDoCo2, and COLCOT trials. We will also introduce clinical trials and experimental studies of colchicine in treating different types of CVD. Clinical CVD trials with the treatment of colchicine are summarized in Table 1 (completed clinical trials) and Table 2 (ongoing clinical trials).
Fig. 2. Usage of colchicine in various diseases.
As an ancient anti-inflammatory drug, colchicine was effective for some liver diseases, lung diseases, and infectious diseases (such as COVID-19), cancer, and cardiovascular diseases (including atherosclerosis, recurrent pericarditis, restenosis, heart failure, or myocardial infarction). Colchicine has some side effects such as injury to the liver and kidney function and toxicity.
Table 1.
Clinical trials of colchicine in treating cardiovascular diseases (completed).
| Study | Setting | Patient | Colchicine regimen | Outcome | Findings | Conclusion | Ref. |
|---|---|---|---|---|---|---|---|
| Atherosclerosis | |||||||
| LoDoCo |
Receiving Colchicine (n = 282) Control (n = 250) |
Patients with stable CAD (n = 532), followed up for median of 3 years. | 0.5 mg/day | Acute coronary syndrome (ACS), fatal, out-of-hospital cardiac arrest, noncardioembolic ischemic stroke. |
Lower endpoint in colchicine treatment (5.3%: 16%; P < 0.001) Lower risk of ACS in colchicine group (4.6%: 13.4%; P < 0.001) |
Standard therapy compared with colchicine (0.5 mg/day) reduces the risk of cardiovascular events, including noncardioembolic ischemic stroke, out-of-hospital cardiac arrest, and ACS. | [12] |
| LoDoCo2 |
Receiving Colchicine (n = 2,762) Placebo (n = 2,760) |
Patients of coronary disease (n = 5,522), followed up for 28.6 months. | 0.5 mg/day | Cardiovascular death, spontaneous myocardial infarction, ischemic stroke, coronary revascularization driven by ischemia. |
Lower risk of endpoint shown in colchicine group (6.8%: 9.6%; HR: 0.69; 95% CI: 0.57–0.83, P < 0.001) Lower risk of ischemia-driven coronary or revascularization spontaneous myocardial infarction or, cardiovascular death or spontaneous MI in colchicine group. |
Colchicine (0.5 mg/day) decreases 31% risk of cardiovascular events, including spontaneous myocardial infarction, death, ischemic stroke. | [170] |
| COLCOT |
Receiving Colchicine (n = 2,322) Placebo (n = 2,339) |
Patients within 30 day post-MI (n = 4,661), followed up for 22.7 months. | 0.5 mg/day, | Cardiovascular death, MI, urgent hospitalization for angina requiring coronary resuscitated cardiac arrest, and stroke. | After MI, uptake of colchicine in the first 3 days could reduce the risk of endpoint (4.3%: 8.3%; P < 0.007). | It is more beneficial for patients to get early colchicine treatment in hospital. | |
| Raju et al. |
Receiving Colchicine (n = 40) Placebo (n = 40) |
Patients with acute ischemic stroke (n = 7) or ACS (n = 73), followed up for 30 days. | 1 mg/day | Death, level of hsCRP, and stroke or MI at 30 days as clinical outcomes. | No difference in level of hsCRP in colchicine and placebo group (1.0 mg/L: 4.5 mg/L; P = 0.22). | 1.0 mg/day of colchicine does not reduce blood level of hsCRP. Colchicine has no effect on platelet function. | [171] |
| Martinez et al. |
Receiving Colchicine (n = 21 + 13) Control (n = 19 + 20) |
Patients with cardiac catheterization (Stable CAD n = 33; ACS n = 40; control n = 10) | 1 mg followed by 0.5 mg 1 h later | Level of IL-1β, IL-6, and IL-18 in 6–24 h prior to cardiac catheterization. | Colchicine decreases the level of cytokines in ACS patients by 40%–88% (P = 0.028, 0.032, and 0.032 for IL-1β, IL-6, and IL-18, respectively) | Short-term colchicine administration significantly decreases the level of inflammatory cytokines. | [172] |
| MBBS et al. |
Receiving Colchicine + OMT (n = 40) OMT (n = 40) |
Patients with recent ACS (<1 month, n = 80), followed up for 1 year. | 0.5 mg/day | Low attenuation plaque volume (LAPV) |
Colchicine significantly reduces the level of hsCRP (1.1 mg/L: 0.38 mg/L; P < 0.001) and LAPV (15.9 mm3: 6.6 mm3; P = 0.008). No difference in low-density lipoprotein (0.44 mmol/L: 0.49 mmol/L; P = 0.21). |
Low-dose colchicine reduces coronary plaque, independent of low-density lipoprotein. | [173] |
| COPS |
Receiving Colchicine (n = 396) Placebo (n = 399) |
Patients with ACS and CAD on coronary angiography, followed up for 12 months. | First months: 0.5 mg twice a day, 0.5 mg/day for 11 months. | ACS, noncardioembolic ischemic stroke, ischemia-driven urgent revascularization, and all-cause mortality. |
Higher total death rate in colchicine (8: 1; P = 0.017), and non-cardiovascular death (5: 0; P = 0.024). No difference for endpoint between two groups (61.0%: 9.5%; P = 0.09). |
There is no significant effect on cardiovascular outcomes for adding colchicine to standard medical therapy at 12 months in patients with ACS, but with higher rate of mortality. | [174] |
| Pericarditis | |||||||
|
CORE Imazio et al. |
Receiving Aspirin + Colchicine n = 42) Aspirin (n = 42) |
Patients first suffering from recurrent pericarditis (n = 84), followed up for 6 months | First day: 1.0–2.0 mg; 0.5–1.0 mg/d for 6 months |
Recurrence rate; Symptom persistence 72 h after treatment onset. |
Colchicine decreases the recurrence rate (24%: 50.6%; P = 0.02). No severe adverse events are observed. |
Colchicine decreases the risk of recurrence of pericarditis in patients first suffering from recurrent pericarditis. | [27] |
|
COPE Imazio et al. |
Receiving Aspirin + Colchicine n = 60) Aspirin (n = 60) |
Patients first suffering from recurrent pericarditis (n = 120), followed up for 3 months | First day: 1.0–2.0 mg and 0.5–1 mg/day for 3 months | Recurrence rate; |
Colchicine decreases the risk of symptom persistence at 72 h (11.7%: 36.7%; P = 0.003) and recurrence (10.7%: 32.3%; P = 0.004). No serious adverse effect is observed. |
Colchicine is beneficial over conventional treatment. It decreases the rate of recurrence in patient first suffering from recurrent pericarditis. | [175] |
|
CORP Imazio et al. |
Receiving Colchicine n = 60) Placebo (n = 60) |
Patients first suffering from recurrent pericarditis (n = 120), followed up for 6 months | 1.0–2.0 mg on the first day and 0.5–1 mg/day for 6 months | Recurrence rate at 18 months. |
Lower risk of recurrence is observed in colchicine group (24%: 55%; P < 0.001). Colchicine decreases the persistent symptoms at 72 h (23%: 53%; P = 0.001) |
Colchicine is efficacious and relatively safe for preventing recurrent pericarditis. | [28] |
| Imazio et al. |
Receiving Colchicine n = 120) Aspirin (n = 120) |
Patients first suffering from recurrent pericarditis (n = 240), followed up for 3 months | Weight >70 kg: 0.5 mg twice a day; weight ≤70 kg: 0.5 mg/day in 3 months | Incessant or recurrent pericarditis | Colchicine decreases the occurrence of incessant or recurrent pericarditis (16.7%: 37.5%; P < 0.001) and symptom persistence at 72 h (19.2%: 40.4%; P = 0.001). | Colchicine reduces incessant or recurrent pericarditis risk in patients with acute pericarditis. | [176] |
| Guindo et al. | Receiving Colchicine (n = 9) | Patients with recurrent pericarditis, and at least experienced three recurrences., followed up for mean 24.3 months. | 1 mg/day | / |
No recurrence has been observed after colchicine treatment in mean 24.3 months. Seven of nine patients have double period without symptom compared with before colchicine treatment. They supposed that colchicine prevents recurrences effectively when the flare-up is controlled by a corticosteroid. |
[26] | |
| Papageorgiou et al. |
Receiving Colchicine (n = 2,082) Control (n = 1,982) |
Meta-analysis 17 studies involving 4,064 patients, followed up for mean 12 months |
/ | Pericarditis recurrence and postpericardiotomy syndrome; recurrence of atrial fibrillation; in-stent restenosis; | Colchicine decreases the risk of pericarditis recurrence (18.4%: 42%; P = 0.001) | Colchicine shows a good effect on recurrent pericarditis. | [29] |
| Restenosis | |||||||
| James et al. |
Receiving Colchicine (n = 111) Placebo (n = 58) |
Patients with coronary angioplasty, followed up for 3–6 months. | 0.5 mg twice a day | Angiographic restenosis | After 6 months lesions had restenosed to 47% of lumen diameter narrowing in the placebo group, and 46% in colchicine group. | Colchicine was ineffective for preventing restenosis after coronary angioplasty. | [35] |
| Deftereos et al. |
Receiving Colchicine (n = 100) Placebo (n = 96) |
Diabetic patients with the contraindication of drug-eluting-stent, undergoing PCI with a BMS (n = 196), followed up for 6 months. | 0.5 mg twice a day. | Angiographic ISR and IVUS-ISR | Lower rate of angiographic ISR in colchicine treatment group (16%: 33%; P = 0.007). IVUS-ISR is similar in two groups. Less lumen area loss in colchicine group (1.6 mm2: 2.9 mm2; P = 0.002) | Colchicine is helpful in reducing ISR rate in diabetic patients after PCI with a BMS. | [40] |
| Heart failure and myocardial infarction | |||||||
| Deftereos et al. |
Receiving Colchicine (n = 140) Placebo (n = 139) |
Patients (n = 267) with stable NYHA I-III HF symptoms with LVEF ≤ 40%, followed up for 6 months. | 0.5 mg twice daily | The proportion of patients achieving at least one-grade improvement in NYHA functional status classification |
The endpoint occurring in colchicine group is 14%, but 11% in control group. Higher rate of hospitalization from heart failure and death in colchicine group (10.1%: 9.4%; P = 0.839) |
Colchicine treatment in patient with stable CHF does not affect the likelihood of hospitalization from heart failure and death. | [177] |
| Deftereos et al. |
Receiving Colchicine (n = 77) Control (n = 74) |
Patients (n = 151) with STEMI (<12 h), followed up for 5 days | Initially 1.5 mg plus 0.5 mg after 1 h and continuing with 0.5 mg twice daily | The area under the curve of creatine kinase-myocardial brain fraction concentration | Colchicine decreases the infarct size (18.3: 23.2; P = 0.019), and the creatine kinase-myocardial brain fraction curve (3,144: 6,184; P < 0.001) | Colchicine is beneficial for ST-segment-elevation in myocardial infarction. | [45] |
| Hemkens et al. | / |
Meta-analysis 39 trials involving 4,992 patients |
/ | All-cause mortality, myocardial infarction, and adverse events | The risk for myocardial infarction was reduced (HR 0.20; 95% CI: 0.07–0.57; 2 trials) | colchicine was associated with a lower risk for MI. | [44] |
| Tardif, et al. |
Receiving Colchicine (n = 2,366) Placebo (n = 2,769) |
Patients with time of MI occurring within 30 days, followed up for 22 months. | 0.5 mg/day | MI, resuscitated cardiac arrest, coronary revascularization following urgent hospitalization for angina, and stroke. | Lower risk of endpoint shown in colchicine group (5.5%: 7.1%; P = 0.02) | Lower risk of ischemic cardiovascular event in colchicine treatment group. | [6] |
| Meng et al. |
Receiving Colchicine (n = 5,906) Control (n = 5,884) |
Meta-analysis including five trials 11,790 patients with CAD, followed up for 6–29 months |
0.5 mg once or twice daily | Major adverse cardiovascular events (MACE) | Colchicine significantly decreases the risk of MI (P = 0.04) | Colchicine is beneficial to patients with CAD for reducing the risk of cardiovascular events. | [47] |
| Shah et al. |
Receiving Colchicine (n = 206) Placebo (n = 194) |
Patients referred for possible PCI (n = 400) | 1.2 mg 1–2 h before coronary angiography, followed by colchicine 0.6 mg 1 h later or immediately before PCI | PCI-related myocardial injury. | No difference of PCI-related myocardial injury (57.3%: 64.2%; P = 0.19). Composite outcome of death, target vessel revascularization, nonfatal myocardial infarction at 30 day did not differ in two groups Preprocedural colchicine reduces the increase in IL-6 and hsCRP after PCI. | Preprocedural colchicine reduces the increase of IL-6 and hsCRP, but does not decrease the PCI-related myocardial injury risk. | [173] |
| Abrantes et al. |
Receiving Colchicine (n = 6,230) Control (n = 6,144) |
Meta-analysis 314 articles involving 12,374 patients with CAD |
≤ 1.5 mg/day colchicine | Cardiovascular mortality and major adverse cardiac events. | No difference in cardiovascular mortality (HR: 0.79; 95% CI: 0.53–1.18), but lower risk of major adverse cardiac events in colchicine group. Colchicine reduced the risk of ACS (lower 36% risk) and stroke events (51% risk) | Colchicine is beneficial for patients with CAD on prognosis. | [48] |
| Cardiovascular complications of COVID-19 | |||||||
| GRECCO-19 Deftereos et al. |
Receiving Colchicine (n = 56) Control (n = 54) |
Colchicine effect on COVID-19 patients (n = 105), followed up for 3 weeks. | 1.5 mg loading dose plus 0.6 mg after 1 h and 0.5 mg twice a day maintenance dose. | Level of hs-cardiactroponin; time to grade 7 clinical deterioration 2 points; time for C-active protein reaching over 3 times upper than reference limit. | Lower rate of endpoint in colchicine treatment group (1.8%: 14.0%; P = 0.02). Event-free survival time was longer in colchicine group (20.7 d: 18.6 d; P = 0.03) | Colchicine significantly improved the time to clinical deterioration | [51] |
|
COLCORONA Tardif et al. |
Receiving Colchicine (n = 2,235) Placebo (n = 2,253) |
Colchicine effect on COVID-19 patients (n = 4,488), followed up for 30 days. | First three days: 1 mg colchicine in two doses; after the first three days and for the consecutive 27 days: 0.5 mg/day | The combination of hospital admission or death for COVID-19. | Lower rate of primary endpoint in colchicine group (4.7%: 5.8%; P = 0.08). Among the 4,159 of patients with COVID-19 confirmed by PCR, the risk of primary endpoint is 4.6 in colchicine group (4.6%: 6.0%; P = 0.04) | Colchicine decreased the composite rate of hospitalization and death in non-hospitalized patients. | |
Table 2.
Colchicine treatment for cardiovascular diseases (Ongoing)a.
| Study | Colchicine regimen | Patient | Endpoint | NCT number |
|---|---|---|---|---|
| Atherosclerosis | ||||
| Low dose colchicine in patients with peripheral artery disease to address the residual vascular risk (LEADER-PAD) | Colchicine 0.5 mg/day | Participants with peripheral artery diseases (n = 150), followed up for 12 months | Mean number of patients recruited per center per month. | NCT04774159 |
| Canadian study of arterial inflammation in patients with diabetes and vascular events: evaluation of colchicine (CADENCE) | Colchicine 0.6 mg/day | Participants with cardiovascular diseases (n = 115), followed up for 6 months. | Six months change in FDG uptake TBR (tissue to blood ratio) in the MDS (maximum disease segment). | NCT04181996 |
| The colchicine hypertension trial (COHERENT) | Colchicine 0.5 mg/day | Patients with hypertension (n = 150), followed up for 6 months. | Between-group difference in change in carotid-femoral pulse wave velocity at 6 months | NCT04916522 |
| Recurrent pericarditis | / | Patients with recurrent pericarditis (n = 119), followed up for 3 years | Immune cell phenotype; immune cell gene expression. | NCT04996108 |
| Pericarditis: Auto-inflammation in recurrent disease (PAIRED) | ||||
| Post-ablation pericarditis reduction study (PAPERS) | Colchicine 0.6 mg twice a day twice daily for 7 days | Patients with atrial fibrillation ablation (n = 248), followed up for 30 days. | Proportion of patients with pericarditis | NCT04906720 |
| Dexamethasone compared to non-steroidal anti-inflammatory drugs in the treatment of acute pericarditis (Dexa-P) | Colchicine 0.5 mg/day (<70 kg); 0.5 mg twice a day (>70 kg) during 3 months (adding ibuprofen) | Patients with acute pericarditis (n = 208), followed up for 3 months. | Occurrence of recurrent pericarditis within 12 months | NCT04323280 |
| Restenosis | ||||
| Oral colchicine in Argentina to prevent restenosis (ORCA) | Colchicine 0.5 mg twice daily during 3 months after stent implantation | Patients with indication for myocardial revascularization with PC (n = 450), followed up for 12 months | Composite of death, MI, and ischemic target vessel revascularization (TVR) death included cardiac, non-cardiac, and non-determined. | NCT04382443 |
| Heart failure and myocardial infarction | ||||
| Randomized double-blind trial to study the benefit of colchicine in patients with acutely decompensated heart failure (COLICA) | Colchicine 0.5 mg/day treatment 8 weeks. | Patients with acute decompensated (n = 278), followed up for 8 weeks. | Decreased NT-proBNP levels. | NCT04705987 |
| Colchicine in HFpEF (COLPEF) | Colchicine 0.5 mg/day | Patients having heart failure with preserved ejection fraction (HFpEF) (n = 426), followed up for 6 months. | Change in hs-CRP (C reactive protein) | NCT04857931 |
| Colchicine to prevent sympathetic denervation after an acute myocardial infarction (COLD-MI) | 1 mg (or 0.5 mg) tablet of colchicine taken once a day for 1 month | Patients who have suffered a documented de novo myocardial infarction and completed a revascularization procedure (n = 56), followed up for 6 months. | Percentage of myocardial denervation | NCT04420624 |
| Cardiovascular complications of COVID-19 | ||||
| Colchicine to reduce cardiac injury in COVID-19 (COLHEART-19) | Colchicine 0.6 mg po BID based on current care per UCLA treating physicians during 30 days. | Patients infected with COVID-19 (n = 91), followed up for 90 days. | Combination of need for mechanical circulatory support (MCS) or need for mechanical ventilation, and all-cause mortality. | NCT04355143 |
| Colchicine for the treatment of cardiac injury in hospitalized patients with COVID-19 (COLHEART-19) | Colchicine 0.6 mg/day during 30 days, and decreasing dose by symptom. | COVID-19 patients with cardiac manifestations of disease (n = 75), followed up for 90 days. | Mortality; mechanical ventilation. | NCT04762771 |
| Colchicine vs current standard of care in hospitalized patients with COVID-19 and cardiac injury (COLHEART-19) | Colchicine 0.6 mg/day during 30 days, and decreasing dose by symptom. | COVID-19 patients (n = 75), followed up for 90 days. | All caused mortality; mechanical ventilation; mechanical circulatory support. | NCT04510038 |
aData from U.S. National Library of Medicine. Website is https://clinicaltrials.gov/ct2/home.
The LoDoCo, LoDoCo2 and COLCOT clinical trials
The outcome of the low-dose colchicine for secondary prevention of CVD (LoDoCo) trial [12], was published in 2013. It was a randomized, prospective, and observer-blinded endpoint design trial. Patients (532) with CAD were enrolled in this trial and patients were randomly assigned to either a colchicine (0.5 mg/day) group or no drug group, and followed up for 3 years. The primary endpoint of this trial was the combination of the acute coronary syndrome (ACS), non-cardiometabolic ischemic stroke, or cardiac arrest out of the hospital. Patients in the colchicine group showed fewer cardiovascular events. Colchicine reduced the risk of the primary outcome (4.5%: 16.0%; P < 0.001). Due to the limited sample size and lack of a placebo control, the finding in this trial needed to be validated by other larger clinical trials.
In 2020, the LoDoCo2 trial [13] was completed and its results were published by Nidorf et al. Patients (5,522) with ischemic heart disease were recruited in this trial, and patients were randomly assigned to either a colchicine group (0.5 mg/day) or a placebo group. The primary endpoint was the combination of cardiovascular death, ischemic stroke, spontaneous MI, and coronary revascularization driven by ischemia. After 28.6 months, a lower rate of primary and key secondary endpoint was observed in colchicine treated group (6.8%: 9.6%; P < 0.001. 4.2%: 5.7%; P = 0.007). In addition, colchicine treatment also reduced the incidence of gout.
The colchicine cardiovascular outcomes trial (COLCOT) [14], was reported by Tardif et al. in 2019. Patients (4,661) were recruited within 30 days of a post-MI. Patients were randomly assigned to treatment with colchicine (n = 2,322; 0.5 mg/day) or placebo (n = 2,339). The primary endpoint of COLCOT was the combination of stroke, MI, cardiovascular death, urgent hospitalization for requiring coronary revascularization, and resuscitated cardiac arrest. After 22.7 months, the study showed a lower risk of the primary endpoint in patients treated with colchicine in the first 3 days (4.3%: 8.3%; P < 0.007). The result exhibited that the initiation of colchicine therapy is beneficial to the composite endpoint of cardiovascular death. More benefits were obtained for patients who received hospital-initiated colchicine therapy after MI.
Efficacy of colchicine against atherosclerosis
Atherosclerosis is currently considered to be a progressive inflammatory disease initiated when apoB100 containing lipids, mainly LDL-cholesterol, accumulate in the arterial wall due to binding and trapping by modified proteoglycans with hyperelongated glycosaminoglycan (GAG) chains [15–17]. Atherosclerosis commences with endothelial dysfunction [18], accompanied by the process of smooth muscle cell (SMC) migration and proliferation from the media layer to the subendothelial space, where atherosclerotic lesions or fibrous lipid plaque lesions are formed. Foam cells and debris mixed extracellular matrix accumulate on the inner wall of blood vessels to form a necrotic core. In atherosclerosis, differentiated macrophages migrate to the vascular wall and avidly take in modified LDL, and become macrophage-derived foam cells [19]. The core, an atherosclerotic plaque, is covered with a fibrous cap which consists principally of SMCs and collagen. The rupture and/or superficial erosion of atherosclerotic plaques are two stimuli for thrombosis formation [20]. Inflammation and cellular activities determine the process of the plaque erosion and plaque healing. SMCs secrete collagen to stabilize the plaque, whereas inflammation inhibits the secretion of collagen or activates macrophages to produce matrix metalloproteinases to digest the extracellular matrix, which in turn promotes the erosion of the plaque. In addition, increased lipid accumulation triggers the apoptosis of cells followed by profound ROS produced by ER stress, which increases the secretion of proinflammatory cytokines (IL-1α, IL-1β, IL-6, and TNF-α). Increased expression of these proinflammatory cytokines promotes the infiltration of immune cells to exacerbate atherosclerosis [21].
In this regard, the unique anti-inflammatory effects of colchicine block mitosis of vascular smooth muscle cells (VSMCs) [22], implying its potential application for treating atherosclerosis. From 1971 to 1979, many scientists studied the pharmacological actions of colchicine in different animal models, but many animal experiments have exhibited no significant effects of colchicine in decreasing the risk of atherosclerosis [16, 17]. Colchicine has demonstrated efficacy against atherosclerosis in swine by Lee et al. [23], but not in rabbits by Hollander et al. [24]. In 1985, Lagrue et al. [25] investigated whether or not colchicine decreased the risk of hypertension. This study included 51 subjects with several other vascular risk factors. The results were that 1 mg/day colchicine treatment for last 3–4 months did not change the lipid profile in the blood, and also has no effect on blood pressure. However, colchicine improves the microcirculatory parameters, and reduces atherosclerosis. Until 2013, LoDoCo trial [12] addressed the efficacy of colchicine in atherosclerosis: colchicine (0.5 mg/day) treatment significantly decreased the primary combined endpoint. In 2020, LoDoCo2 trial [13] was completed and result on primary endpoint also confirmed that colchicine (0.5 mg/day) decreased the incidence of CVD.
Efficacy of colchicine against recurrent pericarditis
Based on the observation that colchicine is effective in treating FMF by reducing system inflammatory processes, scientists explored the therapeutic potential of colchicine in other inflammatory diseases such as recurrent pericarditis. In 1990, Guindo and Serna [26] reported the effect of colchicine treatment on 9 cases of recurrent pericarditis. Patients also receive treatment with other drugs such as acetyl-salicylic acid, prednisone, indomethacin, or a combination before treatment with colchicine. No recurrence was observed after colchicine treatment in a mean of 24.3 months. The symptom-free period of seven patients after colchicine treatment was more than twice the longest period before treatment. The authors suggested that colchicine prevented the recurrence of pericarditis effectively under the condition of flare-up controlled by corticosteroid. In 2005, a randomized, prospective, and open-label design study of colchicine for recurrent pericarditis (CORE) by Imazio et al. [27] was reported. Eighty-four patients with first-time pericardium recurrence were enrolled in this trial. Patients are randomly divided into two groups, receiving colchicine (first day: 1.0–2.0 mg colchicine; after the first day and for the consecutive 6 months: 0.5–1.0 mg/day) or not on the basis of standard treatment, and the follow-up period was 20 months. The recurrence rate was the primary endpoint of this trial. The result was that the primary endpoint was significantly decreased in the colchicine-treated group (24.0%: 50.6%; P = 0.02). In 2011, a multicenter CORP trial [28] confirmed the efficacy and safety of colchicine in treating patients with recurrent pericarditis. One hundred and twenty patients with first recurrence of pericarditis were rerolled in this trial. Patients were randomly assigned to receive colchicine (first day: 1.0–2.0 mg of colchicine; after the first day and for the consecutive 6 months: 0.5–1.0 mg/day) or placebo. After 18 months of follow-up, the lower risk of the primary endpoint was observed in colchicine treating group (24%: 55%; P < 0.001). In 2016, Papageorgiou et al. [29] performed a meta-analysis of the efficacy of colchicine in preventing and treating patients with cardiac diseases. The authors identified 17 prospective studies with 4,064 patients (2,082 treated with colchicine and 1,982 with controls). Patients were followed up for mean 12 months. The result was that colchicine decreased the risk of postpericardiotomy or recurrent pericarditis (P < 0.001).
Efficacy of colchicine against vascular restenosis
Coronary restenosis is vascular lumenal narrowing resulting from a “healing” response to a local injury of the coronary artery [30, 31]. Restenosis normally occurs in 6 months after percutaneous transluminal coronary angioplasty (PTCA) [32, 33]. Restenosis is caused by hyperplasia of smooth muscle cells resulting from injury to the arterial wall, and accompanied by excess secretion and accumulation of matrix components including collagen and elastin forming scar tissue [34]. However, the precise mechanism of restenosis is unclear. Colchicine is an effective anti-inflammatory medicine for CVD. However, it remains unclear whether or not colchicine is also beneficial for restenosis. Chaldakov et al. [7] have recommended the use of anti-inflammatory drugs in the treatment of coronary restenosis after bypass grafting and angioplasty. Several studies confirmed the therapeutic potential of colchicine against restenosis, but some studies also suggested the agent has no effects on restenosis. In 1992, H.O’Keefe et al. [35] reported a trial including 197 patients (130 treated with colchicine and 67 treated with placebo). Patients were followed up for 6 months. Treatment began between 12 and 24 h after angioplasty. After 6 months, lesions had restenosed to 46% lumen diameter narrowing in patients treated with colchicine but 47% in placebo-treated group. Forty-one percent of patients developed restenosis in at least one lesion in colchicine group and 45% in the placebo group. This study showed no therapeutic effect of colchicine in the prevention of restenosis after coronary angioplasty. The proliferation of VSMCs plays an important role in restenosis after angioplasty or vascular injury. In 1994, March et al. [36] discovered that colchicine analog-contained biodegradable microspheres inhibited DNA synthesis in VSMCs suggesting the potential effect of colchicine in preventing or decreasing the severity of restenosis. In 1995, Freed et al. [37] discovered that colchicine combined with lovastatin and enalapril exhibited no preventive effect in restenosis after PTCA.
Restenosis is worse in some subsets of patients with CAD, as well as those with diabetes [38, 39]. Restenosis is also a prominent challenge in patients using bare-metal stents (BMS) inplants. Drug-eluting stents are designed to inhibit the formation of in-stent neointima to decrease the restenosis rate. Some patients with diabetes have contraindications to the implantation of drug-eluting stents. Colchicine has antiproliferative anti-inflammatory effects and can inhibit in-coronary-stent neointima formation, and reduce the rate of in-stent restenosis (ISR). In 2013, Deftereos et al. [40] tested whether 6 months of colchicine treatment could decrease ISR. This study including 196 patients (100 treated with colchicine and 96 with placebo) showed that the rate of angiographic ISR was 16% and 33% in colchicine treatment group and placebo group (P = 0.007), respectively. Decreased ISR rate and less neointimal tickening were observed in patients in the colchicine group after PCI with a BMS, which supported the contention that colchicine is useful for preventing BMS restenosis in diabetic patients. In 2015, Kong et al. [41] studied sixty coronary arteries from induced ISR mini-pigs by implanting oversized BMS and found that colchicine can reduce restenosis after balloon angioplasty treatment for ISR.
Percutaneous coronary intervention (PCI) is one of the major methods for the therapy of coronary heart disease, which has immensely improved the prognosis of patients with coronary heart disease, but restenosis after interventional treatment has always been an undesirable outcome and a procedure-limiting response. Colchicine may potentially be used to decrease the risk of restenosis in patients after PCI [42, 43].
Colchicine treatment and heart failure and myocardial infarction
There is a popular belief that inflammatory responses play a role in acute coronary events (ACE). Targeting inflammation could be an effective strategy against ACE. The CANTOS [5] trial has demonstrated the efficacy of IL-1β monoclonal antibody therapy in decreasing the risk of myocardial infarction (MI) via inhibiting IL-1β signaling pathway, which supports the contention that anti-inflammatory therapy is an effective strategy in treating MI. In 2015, Hemkens et al. [44] reported the association between colchicine and lower risk of MI (1.2%: 5.8%; P = 0.003). In the same year, Deftereos et al. [45] reported that colchicine is potentially beneficial in ST-segment-elevated MI. COLCOT [6] is a milestone clinical trial to elucidate the effective action of colchicine in treating MI. COLCOT investigated 4,745 patients within 30 days post-MI who were randomly divided into colchicine (0.5 mg/day) group or placebo group, and followed up for 22.7 months. In 2019, Tardif et al. [14] reported the result of COLCOT that 0.5 mg/day of colchicine statistically decreased the risk of the primary endpoint (5.5%: 7.1%; P = 0.02). Patients benefit from early, in-hospital-initiated colchicine treatment after MI. Nowadays, COLCOT-T2D trial [46] is ongoing, which enrolled 10,000 patients with type-2 diabetes mellitus without known CAD to further explore the potential effects of colchicine on MI. Meng et al. [47] performed a meta-analysis to evaluate all the eligible studies in Cochrane Library and PubMed from inception to August 2020. Result exhibited that colchicine decreased the risk of MI in CAD patients. In 2021, Abrantes et al. [48] reported a meta-analysis about low-dose colchicine in CAD. Three hundred and fourteen articles were involved for analysis from all available randomized controlled trials (RCTs) including patients with CAD (including MI or ACS and stable or chronic coronary disease), in spite of the presence of other comorbidities. A total of 12,374 patients (6,230 patients taking ≤ 1.5 mg/day of colchicine and 6,144 patients taking placebo or with standard treatment), were followed up for 12.7 months. There were no significant differences in cardiovascular mortality between the two groups. But a lower risk of major adverse cardiac events was observed in the colchicine group. In particular, colchicine reduced the risk of ACS (36% risk) and stroke events (51% risk) [48].
Colchicine treatment and cardiovascular complications of COVID-19
COVID-19 is an ongoing pandemic that commenced in December 2019. It is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). According to World Health Organization (WHO, https://covid19.who.int/), until 26 October 2021 (Central European Time), the cumulative number of confirmed cases worldwide has reached 243,857,028 and the death toll reached 4,953,246. The virus attachment receptor, angiotensin-converting enzyme 2 (ACE2), is a pivotal enzyme in renin-angiotensin system (RAS), which is associated with vasoconstriction, fibrosis, and inflammation. Plasma ACE2 concentration is a risk factor for death, heart failure, MI, and stroke [49]. COVID-19 can cause systemic inflammation and affect the cardiovascular system, which leads to a variety of conditions, including heart failure, MI, myocarditis, myocardial injury, dysrhythmias, and venous thromboembolic events. Recent research suggested that the virus may also utilize ACE2 receptors located on the surface of the cardiac muscle cell to attack heart tissue directly [50].
Considering cardiovascular complications are important in cardiac injury accompanying COVID-19, cardiovascular medications could potentially help treat COVID-19 patients. In this regard, several recent studies have demonstrated the efficacy of colchicine in patients infected with SARA-CoV-2. In a randomized clinical trial named GRECCO-19, Deftereoset et al. [51] found colchicine greatly delayed the time of clinical deterioration (1.8%: 14.0%; P = 0.02), although no difference was observed in the level of C-reactive protein and cardiac Troponin (4.5 mg/dL: 3.1 mg/dL; P = 0.73). Papadopoulos et al. [52] suggested that colchicine could minimize cytokine storm induced by COVID-19 as a viable treatment option. In February 2021, Anton-Vanesa et al. [53] reported a case study of colchicine in COVID-19 associated cardiac injury. A 46-year-old man with cardiac injury and infected with COVID-19, was treated orally with colchicine 0.5 mg for 8 h. Excitingly, the patient was improved rapidly after treatment. Colchicine resolved his chest pain, improved his dyspnea, and decreased oxygen requirements, after taking colchicine for 48 h. The patient’s symptoms of hypoxia disappeared completely on the twelfth day. When the patient was discharged from the hospital, all symptoms of cardiac injury were relieved.
The latest research about colchicine treatment and cardiovascular complications of COVID-19 was the “Colchicine for community-treated patients with COVID-19 (COLCORONA)” study. This study was published in July 2021 from the Canada Montreal Heart Institute. This research enrolled a total of 4,488 patients from five countries. Patients were treated with colchicine (first three days: 1 mg colchicine in two doses; after the first three days and for the consecutive 27 days: 0.5 mg/day) or placebo. The combination of hospital admission and death for COVID-19 is the primary endpoint of this trial. For the patients with PCR-confirmed COVID-19, the result was that colchicine reduced the risk of the primary endpoint in the colchicine group (4.6%: 6.0%; P = 0.04), and colchicine also decreased the incidence of serious events (4.9%: 6.3%; P = 0.05). The mechanism may be that colchicine prevents the “cytokine storm” and reduces the complications associated with COVID-19 [54]. Current studies highlight the potential of colchicine in treating acute respiratory distress syndrome and COVID-19-induced pneumonia. In 34 clinical trials registered in the U.S. National Library of Medicine, only two trials focused on the cardiovascular complications of COVID-19. One of the trials is entitled “Colchicine vs. current standard of care in hospitalized patients with COVID-19 and cardiac injury (COLHEART-19)”, focused on colchicine and current standard treatment in COVID-19 patients with cardiac injury. Although some early results are very encouraging clearly, more studies are required to further characterize the effects and mechanisms of action of colchicine for the treatment and prevention of the cardiovascular complications of COVID-19.
In summary, from an analysis of the findings gathered from clinical trials, colchicine shows positive effects in the treatment of CVD. However, some clinical trials have had inherent weakness including limited sample size and lack of placebo controls. In addition, a few trials are case studies, which also fail to reach general conclusions. The findings in these trials need to be validated by other large-scale clinical trials.
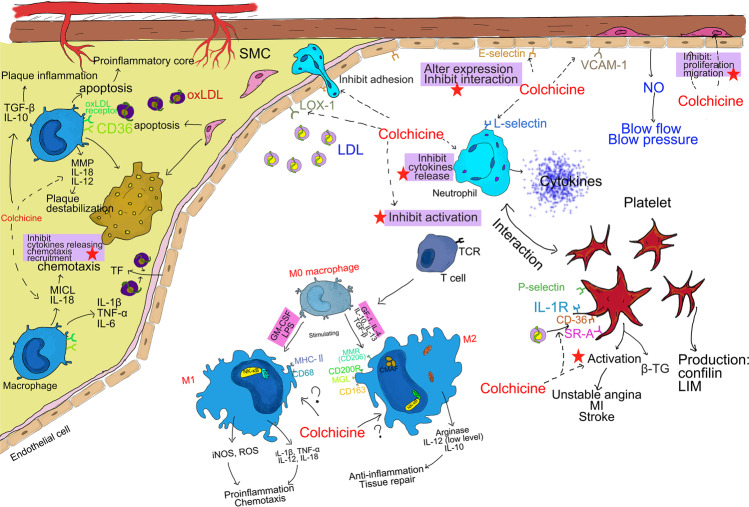
Mechanism of action of colchicine in cardiovascular disease prevention
Atherosclerotic cardiovascular disease is the result of endothelial dysfunction, SMC dysfunction, and macrophage dysregulation [18, 55, 56]. On one hand, endothelial cells, SMCs, and immune cells converge on the vascular system and determine the vascular tone and homeostasis [57]. On the other hand, endothelial cell and SMC dysfunction could activate immune cells contributing to the progression of CVD [18]. Additionally, leukocyte chemotaxis and adhesion contribute to vascular inflammation. The mechanisms of action of colchicine are as below. (1) At the cellular level (Fig. 3): colchicine inhibits endothelial cell E-selectin expression, smooth muscle cell proliferation, macrophage adhesion, and platelet activation to decrease inflammation. (2) At the molecular level (Fig. 4): colchicine binds to tubulin [58]; inhibits the cytokine release and inflammasome (such as NLRP3) assembly and activation [59]. In this section, we will systematically summarize the molecular targets and mechanisms of action of colchicine in disease prevention and treatment.
Fig. 3. The mechanisms of action of colchicine in cardiovascular disease protection.
This figure shows the pathogenesis of atherosclerosis and multiple cells interaction in this progress. Colchicine inhibits: (1) endothelial dysfunction; (2) the release of proinflammatory cytokines; (3) macrophage migration, chemotaxis, and adhesion; (4) platelets and immune cells activation.
Fig. 4. Molecular targets of colchicine in cardiovascular protection.
a Mechanism of colchicine blocking β-tubulin and then disrupting the assembly of microtubules; b mechanism of colchicine targeting NF-κB and then inhibiting many important processes in atherosclerosis; c mechanism of colchicine inhibiting NLRP3 inflammasome activation.
Endothelial dysfunction and colchicine treatment
The endothelium is a cellular monolayer lining the vasculature. Its functions include vascular tone regulation, angiogenesis, hemostasis, and as a layer to prevent oxidative damage, inflammation, and thrombosis [60]. Endothelial cells are an important safeguard for the physiological functions of the endothelium that maintains cardiovascular health. There are various factors and regulators that impact on endothelial dysfunction in CVD, such as oxidative stress, inflammation, drugs, and aging, and compromise the essential physiological role of the endothelium [60, 61].
Vascular tone is maintained in part by vasodilatory and contracting substances produced by endothelial cells [61, 62]. The main vasodilator is nitric oxide (NO). Endothelial cells produce NO via endothelial nitric oxide synthase (eNOS) in the vessel wall [63], which hence regulates blood pressure and blood flow and it also inhibits oxidation of LDL [18, 64]. Endothelial cells adhere to circulating leukocytes via vascular cell adhesion molecule-1 (VCAM-1) on their cell surface [65]. Endothelial cells assimilate oxidized LDL via low-density lipoprotein receptor-1 (LOX-1), which is conducive to the development of atherosclerotic plaques [66]. Many studies have reported the relationship between endothelial dysfunction and coronary disease. Some risk factors of coronary disease are associated with endothelial dysfunction, such as hypertension, hypercholesterolemia, insulin resistance, diabetes, and smoking [67, 68]. In 1986, Ludmer et al. [69] reported the first evidence of endothelial dysfunction in atherosclerosis. Endothelial dysfunction alters the vascular tone, and increases aortic stiffness, which further contributes to hypertension (Fig. 3).
Colchicine has a variety of effects on endothelial cells. Lower doses of colchicine (1.4 nmol/L) inhibit microtubule dynamics and cell migration, and higher concentration (11.0 nmol/L) inhibits cell division [70]. Treatment of FMF patients with colchicine reduced the level of asymmetric dimethlarginine (ADMA), thrombomodulin (TM), and osteoprotegerin (OPG), suggesting an endothelial protective effect of colchicine [71]. OxLDL could induce the expression of tissue factor (TF) in many cell types including endothelial cells, which may cause coronary thrombosis after atherosclerosis. The higher expression of TF can also be caused by the interactions between endothelial cells and leukocytes or platelets. Cimmino et al. [72] reported that colchicine reduced the expression of TF gene and the level of TF protein (Fig. 3) to inhibit endothelial cell dysfunction. More studies are warranted to further reveal other mechanisms of action of colchicine in endothelial cell function under diseased conditions.
Smooth muscle cells and colchicine treatment
Smooth muscle cells (SMCs) are localized in the tunica media of the vessel. The functions of SMCs include extracellular matrix generation and vascular contraction. SMC phenotype can switch from contractile to synthetic state under pressure or pathological conditions [34, 56]. The change of SMC structure and function is the pathological basis of hypertension, atherosclerosis, restenosis after angioplasty, and other cardiovascular diseases [73]. VSMC dysfunction is thus a hallmark of CVD.
In atherosclerosis, the lipid is deposited and accumulates in sub-endothelium space [74]. SMCs migrate to the inner layer and proliferate, leading to the formation of initial plaques. SMCs also secrete extracellular matrix proteins (such as collagen and proteoglycans) to stabilize plaques via the formation of fibrous caps at advanced stage. SMCs take up oxLDL leading to the formation of SMC-derived foam cells. SMCs undergo apoptosis by activating caspase and downregulating BCL-2 [75]. Apoptotic SMCs release IL-1α and IL-1β that induce surrounding VSMCs to produce proinflammatory cytokines [48], which further promotes the formation of atherosclerotic plaques. Moreover, α-SMA+ cell content in fibrous cap is a positive marker of plaque stability [73, 76]. SMCs play an important role in inflammation by recruiting macrophages in plaques (Fig. 3).
In this regard, colchicine has been reported to attenuate SMC proliferation and migration. March et al. [21] reported that a colchicine analog in the form of biodegradable microspheres inhibits DNA synthesis in SMCs. Colchicine inhibits the microtubule polymerization and depolymerization, thereby inhibiting the proliferation of SMCs [77]. Bauriedel et al. [78] have discovered the antagonistic action of low concentrations of colchicine in inhibiting SMC proliferation, migration, and secretory processes (Fig. 3). The antagonistic action of colchicine was confirmed by Ganesh et al. [79] Additionally, colchicine decreased collagen-secretory activity and decreased the cGMP level of SMCs [80]. Thus, SMCs play a critical role in the process of CVD, and it remains to be determined whether colchicine prevents intima-media thickness in patients with early stage of atherosclerosis and plaque rupture in advanced stage of atherosclerosis.
Macrophage function and colchicine treatment
The monocyte/macrophages are the classical immune cell type associated with the processes of atherosclerosis. Macrophages infiltrate the vessel wall, take up modified lipids and become foam cells [81] (Fig. 3). Accumulated foam cells often die through apoptosis, form the necrotic core, and trigger vascular inflammation. Macrophages further produce proinflammatory cytokines (IL-18, IL-12, and TNF-α), thereby aggravating inflammation and promoting plaque destabilization [55]. Macrophages ingest modified LDL through CD36 and other oxLDL receptors such as LOX-1 [82] (Fig. 4c), and removed lipids via Apolipoprotein A-1 (ApoA-1) and HDL mediated cholesterol efflux. ABCA1 and ABCG1 [83] are the main efflux transporters. Lack of ABCA1 or ABCG1 in mice enhanced atherosclerosis lesion formation. Apart from foam cell formation, macrophages are an important cell type for inflammasome activation. NLRP3 inflammasomes are activated by the intracellular level of K+, Ca2+, ROS, and cholesterol crystal [84] (Fig. 4c). A study in patients with ACS found that the level NLRP3 was higher compared with normal controls [85]. The mechanism of NLRP3 causing inflammation will be detailed later.
Macrophage phenotypes can be categorized into M1 and M2 [86] (Fig. 3). Macrophages stimulated by IFN-γ and LPS become M1 which is a proinflammatory phenotype associated with the high expression of proinflammatory cytokines, chemokines, iNOS, and ROS [87–89]. However, by stimulating IL-4 and IL-3, macrophages become of the M2 phenotype which is associated with tissue repair. M2 macrophages secrete transforming growth factor-beta (TGF-β) and IL-10. Macrophage polarization induced by CXCL4, heme, and oxidized phospholipids may be associated with atherosclerosis [21, 90]. Hirata et al. [91] have shown a positive correlation between the M1/M2 macrophage ratio and proinflammatory cytokine expression. The M1/M2 macrophage ratio was positively associated with severity of CAD (P = 0.039; r = 0.312). Macrophage autophagy is another contributor to macrophage dysregulation as well as hyperactivation of inflammation leading to atherosclerosis [92].
Colchicine has been reported to inhibit leukocyte chemotaxis, adhesion, and recruitment [93]. Colchicine inhibits C-type lectin-like receptor (MICL) and IL-18 production, thereby inhibiting macrophage and neutrophil chemotaxis [94]. Colchicine disturbs neutrophil adhesion and recruitment by inhibiting microtubule dynamics [2] and altering the expression of L-selectin on neutrophils and E-selectin on endothelial cells [95]. Sukeishi et al. [96] demonstrated the efficacy of colchicine in mitigating acute postoperative pain is associated with its inhibition on macrophage polarization toward the M1 phenotype. This result was confirmed by Wang et al. [97] in their study of colchicine delivery system dependent upon calcium carbonate nanoparticles (ColCaNPs). Wang and colleagues discovered colchicine promoted the transformation of macrophage polarization toward the M2 phenotype and colchicine inhibited macrophage pyroptosis. Additionally, colchicine delivered by macrophage membrane-coated nanoparticles could inhibit the formation of foam cells [98]. Another important mechanism is that colchicine increases the level of cyclic adenosine monophosphate (cAMP) in leukocyte, thereby inhibiting IL-1 production. Colchicine reduces the production of neutrophil extracellular traps (NETs) to inhibit inflammatory cytokine released from activated endothelial cells and macrophages thereby decreasing the risk of PCI [99].
Platelet activation and colchicine treatment
Platelets play a fundamental role in hemostasis, tumor development, inflammatory responses, and CVD, especially in ACS, PCI thrombosis, and embolization processes. Circulating platelets bind to vascular injury sites to mediate clotting. In atherosclerosis, atheromatous plaques containing lipids and LDL are vulnerable. Platelets are activated by lipids with the mediation of CD36 and scavenger receptor-A [100] during rupture of vulnerable plaques [101] (Fig. 3). Platelets deform, aggregate and release procoagulant factors after being activated, which contributes to the intravascular thrombus formation. This may lead to acute ischemic syndromes such as MI, stroke, and unstable angina pectoris.
Platelet activation is regulated by microtubular dynamic depolymerization and repolymerization [102] (Fig. 4a). Colchicine binds to microtubules and thus inhibits the progression of platelet activation. In 1980, Menche et al. [103] suggested that colchicine inhibited platelet aggregation and secretion. Cimmino et al. [104] reported a possible molecular mechanism of colchicine action by interfering with platelet aggregation. Colchicine may inhibit cofilin and LIM (two mainly phosphorylated forms of myosin in cytoskeleton rearrangement [105]) domain kinase-1 to reduce platelet aggregation. β-Thromboglobulin (β-TG) is a platelet-derived protein, which is released during platelet activation. It is regarded as a sensitive biomarker of platelet activation [106]. A study in FMF patients treated with colchicine found that colchicine decreases the level of β-TG [107]. Previous studies demonstrated that colchicine decreases platelet aggregation through regulating the production of collagen, epinephrine, and ADP in vitro [108, 109]. Colchicine also inhibits the release of serotonin in response to the Ca2+ ionophore A23187 [110]. In CVD therapy, β-TG and mean platelet volume are lower in patients treated with colchicine [107, 111]. Pennings et al. [112] studied the impact of colchicine on platelet activation. They found that pharmacologically relevant concentrations of colchicine (20 nmol/L) in vivo significantly inhibited platelet aggregation through the collagen glycoprotein receptor and P2Y12 receptors. Higher concentration of colchicine (2 mmol/L) inhibited another pathway of platelet activation including GPII/IIa and P-selectin. Colchicine may also regulate platelets activation through influencing the level of IL-1 and IL-1 receptors [113]. In the LoDoCo2 trial, colchicine was shown to inhibit the interaction between platelets and leukocytes, obstruct the polymerization of NLRP3 inflammasomes, and inhibit the secretion of inflammatory cytokines [13].
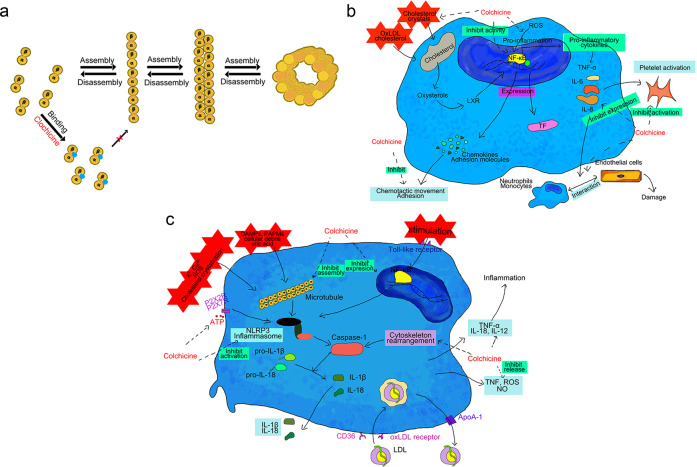
Molecular and biochemical targets of colchicine
Inhibition of microtubule polymerization
Microtubules are hollow tubular structures, composed of α-tubulin and β-tubulin heterodimers [114]. They are the key components of the cytoskeleton and assume various functions such as maintaining cell shape, intracellular transporting, secretion, organelle organization, cell migration, and division [115]. Dynamic polymerization and depolymerization of microtubule are critical regulators of inflammatory status. Both inflammatory infiltration of immune cells and directional migration of smooth muscle cells rely on microtubule dynamics [116]. Moreover, microtubules provide specific locations for the activation of inflammatory molecules and are also the pathways for the secretion of inflammatory molecules for extracellular transport. Microtubules dynamics take part in the pyrin inflammasome activation [117]. Microtubules promote the colocalization of mitochondria and NLRP3 through motor proteins such as kinesin and dynein, and thus provide the conditions for NLRP3 activation [118].
The primary mechanism of action of colchicine is to bind to β-tubulins through its C ring crossing with the 1–46 and 214–241 amino acid residues of tubulin. Other tubulins cannot bind to the end of microtubes when colchicine binds to β-tubulin. Colchicine disturbs microtubule polymerization and disrupts the cytoskeleton, which influences all the cellular processes requiring microtube repolymerization and depolymerization. Colchicine binds to microtubules thereby inhibiting phagocytosis, leukocyte recruitment, and function [58, 119] (Fig. 4a).
Inhibition of NF-κB
Nuclear factor-kappa B (NF-κB) was first discussed in the study of B lymphoid lineage, which could specifically bind to κB enhancer sequence (GGGACTTTCC) of κ light-chain of immunoglobulin [120]. The NF-κB pathway is an essential cellular signal transduction pathway dependent on some regulated proteolytic enzymes. Its functions are involved in every aspect of physiologic processes and pathological conditions, such as immune function, inflammation, and cell fate determination (differentiation, apoptosis, and survival) [121]. The classical NF-κB signaling pathway drives inflammation and coagulation. NF-κB is activated by various environmental insults, including genetic mutation, infection, pathogenic autoantibodies, proinflammatory cytokines [122], and cigarette smoking. After activation, NF-κB promotes the production of IL-6, IL-8, and TNF-α, thereby activating endothelial cells, neutrophils and monocytes and causing endothelial cell damage [123]. TNF-α and IL-1β also may affect plasminogen activators and inhibitors which causes the formation of microvascular thrombosis [124]. The NF-κB pathway regulates oxLDL-induced TF expression in many cell types including endothelial cells [125]. The formation of intracellular ROS also upregulates NF-κB contributing to the secretion of cytokines, and chemokines [88]. Additionally, NF-κB is associated with other human inflammatory diseases such as rheumatoid arthritis [126], atherosclerosis [127], and sepsis [128] (Fig. 4b).
Inhibition of NF-κB is an important mechanism of action of colchicine. Mackenzie et al. [129] reported the reduced nuclear NF-κB binding action of colchicine. Jackman et al. [130] observed that colchicine inhibited the activation of NF-κB in HeLa cells. This is also observed in colchicine-treated FMF patients [131]. Cimmino et al. [72] observed the decreased nuclear level of NF-κB and reduced level of TF induced by oxLDL, after colchicine treatment. Colchicine inhibits NK-κB expression or NF-κB in nuclear fraction by regulating many upstream factors including ROS, and thereby regulates the expression of inflammatory cytokines (Fig. 4b).
Inhibition of NLRP3 inflammasome activation
Inflammasomes are a type of pattern-recognition receptors (PRRs) existing in the cytoplasm of many kinds of immune cells, which is characterized by nucleotide-binding oligomerization domain-like receptor. NLRP3 is pyrin domain-containing protein complex, with a molecular weight of about 700,000. It is also named as NALP3 or cryopyrin [132], existing in monocytes, eosinophils, and neutrophils [133]. The NLRP3 inflammasome is composed of NLRP3, apoptosis-associated-speck-like protein containing a CARD (ASC), and pro-caspase-1. Caspase-1 is activated by NLRP3 and promotes the production of IL-1β and IL-18, which in turns induces inflammation contributing to atherogenesis (Fig. 4c). Signals of pathogen-associated molecular patterns (PAPMs), damage-associated molecular patterns (DAMPs), uric acid, cholesterol crystals, and cellular debris [84] are required to activate NLRP3 in atherogenesis. There are two key steps between NLRP3 activation and inflammation: firstly priming, in which stimuli activate NF-κB signaling via Toll-like receptors, IL-1 receptors, TNFR1 and TNFR2; NF-κB improves the level of transcription of pro-IL-1β, pro-IL-18, and NLRP3, and secondly, activation, in which DAMPs and other stimuli promote inflammasome assembly via activating BRCC3 to deubiquitinate NLRP3 [134]. NLRP3 inflammasomes activate caspase-1 and lead to profound cytokine production. NLRP3 inflammasome is a medium of obesity signals and participates in the process of macrophage phenotype switch from M2 phenotype to M1 proinflammatory phenotype [135]. NLRP3 inflammasome abnormal activation is associated with the development of many conditions, such as the metabolic syndrome, T2D, gout, and atherosclerosis.
Martinon et al. [136] first discovered that colchicine inhibited NLRP3 inflammasome activation, when they used urate crystals to treat the monocytic cell line, THP1. Since this study, many studies have confirmed that colchicine is capable of inhibiting NLRP3 inflammasomes [137–139]. The inhibitory effect of colchicine on NLRP3 is non-selective, thereby decreasing the proinflammatory cytokine (IL-18 and IL-1β) release [59]. Microtubules play an essential role in NLRP3 inflammasome assembly. Colchicine disturbs microtubule dynamics through binding to tubulin and then inhibits the process of cleavage of pro-IL-18 and pro-IL-1β into IL-18 and IL-1β, respectively. Colchicine reduces ROS formation [58, 112], as well as NO and IL-1β release in mouse macrophages [58]. Colchicine suppresses pore formation, such as P2X7 and P2X2, to inhibit ATP-induced NLRP3 inflammasome activation [140] (Fig. 4C). Nidorf et al. [141] suggested that colchicine is capable of inhibiting pyrin (MEFV) gene expression, which decreases the material basis of NLRP3 inflammasomes. Otani et al. [142] showed that colchicine inhibits NLRP3 inflammasome activation through inhibiting the expression of protein of mature IL-1β and cleaved caspase-1. The recent study reported by Silvis et al. [143] investigated the inhibitory action of colchicine on NLRP3. This study analyzed the serum from 278 patients from the LoDoCo2 trial and found that NLRP3 protein was present in extracellular vesicles (EV). Lower levels of NLRP3 protein in EV were observed in colchicine treatment group (1.38 ng/mL: 1.58 ng/mL; P = 0.025). The inhibitory effect of colchicine on EV NLRP3 protein may also be another way to protect patients against CAD.
Anti-fibrotic effects
Fibrosis is a prominent pathophysiological tissue response in numerous diseases specially of the heart, liver, and kidneys. Anti-fibrotic effects of colchicine have been observed in mouse models. Colchicine suppresses cappase-3 and promotes B-cell lymphoma 2 (Bcl-2) to inhibit tubulointerstitial fibrosis [144]. Colchicine promotes the apoptosis of hepatic stellate cells to inhibit liver fibrosis [145]. Colchicine inhibits activation of TGF-β1[146] and expression of VEGF [147] in canine models. Sandbo et al. [148] reported that colchicine inhibits human lung myofibroblast through Rho/serum response factor (SRF). Entzian et al. [149] reported that colchicine inhibits neutrophil penetration into the intimal layer and colchicine exhibits anti-fibrotic actions by reducing collagen production and fibroblast proliferation. Wu et al. [150] reported on a sterile pericarditis model of rat treated with colchicine. Colchicine inhibited the fibrosis-related gene expression, such as collagen-1, collagen-3, α-SMA, and proinflammatory markers such as IL-1β-induced IL-6. Colchicine inhibits atrial fibrosis through STAT3, AKT, and p38 signaling pathways to prevent atrial fibrillation.
Other molecular and biochemical effects of colchicine
In addition to the above pharmacological and therapeutic actions, colchicine also exerts other anti-inflammatory effects at high concentrations. Colchicine inhibits phospholipase A2 activation (10 nmol/L–1 mmol/L) [151], and suppresses lysosomal enzyme release, and phagocytosis (1 mmol/L of colchicine) [152]. Colchicine may influence signal transduction in leukocytes, for example inhibiting tyrosine phosphorylation [153] and superoxide anion [154] production induced by inflammatory crystals such as monosodium urate [155]. Colchicine also regulates the expression of genes (include caspase-1, tubulin-β5, MAPK-1, PI3K, CDC42, eNOS3, and BPA) associated with neutrophil migration and inflammatory processes [156].
Side effects and pharmacokinetic properties of colchicine
Colchicine has had limited clinical use because of its toxicity. The toxicity of colchicine is thought as the result of its overaction. Colchicine binds tubulin and destroys the microtubular network [157], which decreases endocytosis and exocytosis, damages organelle localization and protein assembly, alters cell shape, inhibits cell migration and division. Most cells of the body will be affected by colchicine, actively dividing cells in particular[158].
The pharmacokinetic properties of colchicine are now well described. Colchicine is absorbed by gastrointestinal tract and distributes rapidly around the body. The bioavailability of colchicine is 44% after oral ingestion and uptake in jejunum and ileum [159]. Higher concentrations of colchicine are observed in erythrocytes and leukocytes rather than plasma and its retention is up to 7 days [160], which indicated that the circulating concentrations of colchicine are maintained for a few days after a single oral dose. Many patients experience gastrointestinal discomfort after 24 h of medication, and common side effects are vomiting, diarrhea, and abdominal cramps [161] (side effects were shown in Fig. 2). Colchicine is metabolized by the liver and eliminated by the kidney. It will aggravate liver and kidney burden in patients with liver damage and renal failure or dysfunction [162], which will lead to the side effects even when given in low-dose. Cytochrome CYP3A4 [163] and P-glycoprotein [164] are two important elements in colchicine metabolism. CYP3A4, an isoform of cytochrome P450, is associated with demethylation and deacetylation of colchicine in liver [165]. P-glycoprotein, an integral membrane ATPase-dependent efflux pump is a colchicine transporter to expel colchicine out of the cell [166]. Specific inhibitory drugs of P-glycoprotein and CYP3A4, such as clarithromycin [167] will increase blood drug concentration and metabolic burden and even cause acute colchicine toxicity.
The safe dose of colchicine in various diseases and different ethnic groups varies. However, the prophylactic dosage of colchicine to prevent cardiovascular diseases is not clear. Referring to “Guidelines for Gout” published by American College of Rheumatology (ACR) in 2012, patients are recommended to take 0.5–1.0 mg/day of colchicine orally [168]. Most cardiovascular clinical trials recommend 0.5–1.0 mg/day of colchicine. Overdosing of colchicine (6.0–8.0 mg) leads to acute colchicine poisoning, multiple organ failure, and death when the dose exceeds 0.8 mg/kg [157]. Long-term use of colchicine leads to testicular and ovarian dysfunction [163]. The “2015 ESC Guidelines for the diagnose and management of pericardial diseases” recommends 0.5 mg bid of colchicine in treating patients with recurrent pericarditis (patients cannot tolerate the maximum dose or weight over 70 kg) [169]. There is no specific antidote for colchicine overdose, and the treatment of poisoning is limited to conservative treatment, such as gastric lavage, and measures to prevent shock and symptomatic and supportive treatment. Hence, the use of colchicine should closely follow appropriate clinical guidelines and its use should be monitored in accordance with professional advice from doctors and patients need to be aware of side effects and first-aid treatment after drug overdose.
Concluding remarks and future perspective
Colchicine is an ancient drug of preeminent standing in traditional medicine. Dependent upon its unique anti-inflammatory properties and the recent recognition of the contribution of chronic inflammation to multiple human diseases, the applications of colchicine have been extended from the management of gout and FMF to CVD. In the modern therapeutic vernacular, the recent use of colchicine in the CVD context is an example of successful drug repurposing. These multiple successful clinical trials have broadened our horizons of controlling inflammation in cardiovascular disease treatment and provided insights into the contribution of inflammation to CVD.
Several clinical trials such as LoDoCo, LoDoCo2, CoLCoT have demonstrated the efficacy of colchicine in treating CVDs including restenosis, atherosclerosis, heart failure, myocardial infarction, atrial fibrillation, and excitingly the cardiovascular complications of COVID-19. With the rapid expansion of basic research, the mechanisms of action of colchicine have been gradually uncovered. The predominant mechanism by which colchicine addresses CVD is through its anti-inflammatory action. The most fundamental function of colchicine is to target microtubules. At the cellular level, colchicine inhibits: (1) proliferation and migration of SMCs; (2) chemotaxis and adhesion of macrophage; (3) platelet activation. At the molecular level, colchicine blocks the assembly of NLRP3 via preventing microtubule polymerization and inhibits the production of IL-8 and IL-1β, thereby inhibiting the process of inflammation. Colchicine can also directly decrease the production and release of inflammatory molecules. The inhibitory effect of colchicine on epoxidase COX-1 and COX-2 may also be associated with colchicine-mediated anti-inflammatory effects.
In conclusion, due to its anti-inflammatory actions, colchicine represents a promising naturally-occurring cardiovascular medicine and its demonstrated efficacy has provided additional support for the athero-inflammatory hypothesis of CVD.
Acknowledgements
This study was supported by grants from National Natural Science Foundation of China (Grant Nos. 82070464, and Anhui Provincial Key Research and Development Program (Grant No. 202104j07020051). Figure 2 was created using elements from Servier Medical Arts. This study was also supported by grants from National Key R&D Program of China (Grant No. 2021YFC2500500), National Natural Science Foundation of China (Grant Nos. 81941022, 815300254) and Strategic Priority Research Program of Chinese Academy of Sciences (Grant No. XDB38010100). This work was also supported by the Program for Innovative Research Team of The First Affiliated Hospital of USTC (Grant No. CXGG02), Local Innovative and Research Teams Project of Guangdong Pearl River Talents Program (Grant No. 2017BT01S131), Hefei Comprehensive National Science Center (Grant No. BJ9100000005), and Hefei Municipal Development and Reform Commission.
Author contributions
Conceptualization: SWX Writing: FSZ Revision: SWX, QZH, CHQ, PJL, JPW, and FSZ.
Competing interests
The authors declare no competing interests.
References
- 1.Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32:2045–51. doi: 10.1161/atvbaha.108.179705.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Asako H, Kubes P, Baethge BA, Wolf RE, Granger DN. Colchicine and methotrexate reduce leukocyte adherence and emigration in rat mesenteric venules. Inflammation. 1992;16:45–56. doi: 10.1007/bf00917514.. [DOI] [PubMed] [Google Scholar]
- 3.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990−2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi: 10.1016/j.jacc.2020.11.010.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao D. Epidemiological features of cardiovascular disease in Asia. JACC: Asia. 2021;1:1–13. doi: 10.1016/j.jacasi.2021.04.007.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377:1119–31. doi: 10.1056/NEJMoa1707914.. [DOI] [PubMed] [Google Scholar]
- 6.Tardif JC, Kouz S, Waters DD, Bertrand OF, Diaz R, Maggioni AP, et al. Efficacy and safety of low-dose colchicine after myocardial infarction. N Engl J Med. 2019;381:2497–505. doi: 10.1056/NEJMoa1912388.. [DOI] [PubMed] [Google Scholar]
- 7.Chaldakov GN. Colchicine, a microtubule-disassembling drug, in the therapy of cardiovascular diseases. Cell Biol Int. 2018;42:1079–84. doi: 10.1002/cbin.10988.. [DOI] [PubMed] [Google Scholar]
- 8.GRAHAM W, ROBERTS JB. Intravenous colchicine in the management of gouty arthritis. Ann Rheum Dis. 1953;12:16–9. doi: 10.1136/ard.12.1.16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.HARTUNG EF. History of the use of colchicum and related medicaments in gout; with suggestions for further research. Ann Rheum Dis. 1954;13:190–200. doi: 10.1136/ard.13.3.190.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayer TU, Marx A. Five molecules we would take to a remote island. Chem Biol. 2010;17:556–60. doi: 10.1016/j.chembiol.2010.06.002.. [DOI] [PubMed] [Google Scholar]
- 11.Huang Q, Wu X, Zheng X, Luo S, Xu S, Weng J. Targeting inflammation and cytokine storm in COVID-19. Pharmacol Res. 2020;159:105051. doi: 10.1016/j.phrs.2020.105051.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nidorf SM, Eikelboom JW, Budgeon CA, Thompson PL. Low-dose colchicine for secondary prevention of cardiovascular disease. J Am Coll Cardiol. 2013;61:404–10. doi: 10.1016/j.jacc.2012.10.027.. [DOI] [PubMed] [Google Scholar]
- 13.Nidorf SM, Fiolet A, Eikelboom JW, Schut A, Opstal T, Bax WA, et al. The effect of low-dose colchicine in patients with stable coronary artery disease: the LoDoCo2 trial rationale, design, and baseline characteristics. Am Heart J. 2019;218:46–56. doi: 10.1016/j.ahj.2019.09.011.. [DOI] [PubMed] [Google Scholar]
- 14.Klingenberg R, Nitschmann S. Colchicine treatment after myocardial infarction: Colchicine Cardiovascular Outcomes Trial (COLCOT) Internist. 2020;61:766–9. doi: 10.1007/s00108-020-00768-2.. [DOI] [PubMed] [Google Scholar]
- 15.Nigro J, Osman N, Dart AM, Little PJ. Insulin resistance and atherosclerosis. Endocr Rev. 2006;27:242–59. doi: 10.1210/er.2005-0007.. [DOI] [PubMed] [Google Scholar]
- 16.Little PJ, Ballinger ML, Burch ML, Osmana N. Biosynthesis of natural and hyperelongated chondroitin sulfate. Open Biochem J. 2008;2:135–42. doi: 10.2174/1874091X00802010135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Little PJ, Osman N, O’Brien KD. Hyperelongated biglycan: the surreptitious initiator of atherosclerosis. Curr Opin Lipido. 2008;19:448–54. doi: 10.1097/MOL.0b013e32830dd7c4.. [DOI] [PubMed] [Google Scholar]
- 18.Davignon J, Ganz P. Role of endothelial dysfunction in atherosclerosis. Circulation. 2004;109:III27–32. doi: 10.1161/01.CIR.0000131515.03336.f8.. [DOI] [PubMed] [Google Scholar]
- 19.Wang D, Yang Y, Lei Y, Tzvetkov NT, Liu X, Yeung AWK, et al. Targeting foam cell formation in atherosclerosis: therapeutic potential of natural products. Pharmacol Rev. 2019;71:596–670. doi: 10.1124/pr.118.017178.. [DOI] [PubMed] [Google Scholar]
- 20.Vergallo R, Jarcho JA, Crea F. Atherosclerotic plaque healing. N Engl J Med. 2020;383:846–57. doi: 10.1056/NEJMra2000317.. [DOI] [PubMed] [Google Scholar]
- 21.Cochain C, Zernecke A. Macrophages and immune cells in atherosclerosis: recent advances and novel concepts. Basic Res Cardiol. 2015;110:34. doi: 10.1007/s00395-015-0491-8.. [DOI] [PubMed] [Google Scholar]
- 22.Cavallero C, Turolla E, Ricevuti G. Cell proliferation in the atherosclerotic plaques of cholesterol-fed rabbits. 1. Colchicine (3H)thymidine studies. Atherosclerosis. 1971;13:9–20. doi: 10.1016/0021-9150(71)90003-7. [DOI] [PubMed] [Google Scholar]
- 23.Lee WM, Morrison ES, Scott RF, Lee KT, Kroms M. Effects of methyl prednisolone and colchicine on the development of aortic atherosclerosis in swine. Atherosclerosis. 1976;25:213–24. doi: 10.1016/0021-9150(76)90028-9.. [DOI] [PubMed] [Google Scholar]
- 24.Hollander W, Paddock J, Nagraj S, Colombo M, Kirkpatrick B. Effects of anticalcifying and antifibrobrotic drugs on pre-established atherosclerosis in the rabbit. Atherosclerosis. 1979;33:111–23. doi: 10.1016/0021-9150(79)90202-8.. [DOI] [PubMed] [Google Scholar]
- 25.Lagrue G, Wegrowski J, Rhabar K, Meyer-Heine A, Balanger S, Robert AM, et al. Effect of colchicine on atherosclerosis. I. Clinical and biological studies. Clin Physiol Biochem. 1985;3:221–5. [PubMed] [Google Scholar]
- 26.Guindo J, Rodriguez DLSA, Ramio J, de Miguel DM, Subirana MT, Perez AM, et al. Recurrent pericarditis. Relief with colchicine. Circulation. 1990;82:1117–20. doi: 10.1161/01.cir.82.4.1117. [DOI] [PubMed] [Google Scholar]
- 27.Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial. Arch Intern Med. 2005;165:1987–91. doi: 10.1001/archinte.165.17.1987.. [DOI] [PubMed] [Google Scholar]
- 28.Imazio M, Brucato A, Cemin R, Ferrua S, Belli R, Maestroni S, et al. Colchicine for recurrent pericarditis (CORP): a randomized trial. Ann Intern Med. 2011;155:409–14. doi: 10.7326/0003-4819-155-7-201110040-00359.. [DOI] [PubMed] [Google Scholar]
- 29.Papageorgiou N, Briasoulis A, Lazaros G, Imazio M, Tousoulis D. Colchicine for prevention and treatment of cardiac diseases: a meta-analysis. Cardiovasc Ther. 2017;35:10–8. doi: 10.1111/1755-5922.12226.. [DOI] [PubMed] [Google Scholar]
- 30.Bauters C, Isner JM. The biology of restenosis. Prog Cardiovasc Dis. 1997;40:107–16. doi: 10.1016/s0033-0620(97)80003-5.. [DOI] [PubMed] [Google Scholar]
- 31.Welt FG, Rogers C. Inflammation and restenosis in the stent era. Arterioscler Thromb Vasc Biol. 2002;22:1769–76. doi: 10.1161/01.atv.0000037100.44766.5b.. [DOI] [PubMed] [Google Scholar]
- 32.Cowley MJ, Dorros G, Kelsey SF, Van Raden M, Detre KM. Acute coronary events associated with percutaneous transluminal coronary angioplasty. Am J Cardiol. 1984;53:12C–6C. doi: 10.1016/0002-9149(84)90738-0.. [DOI] [PubMed] [Google Scholar]
- 33.Landau C, Lange RA, Hillis LD. Percutaneous transluminal coronary angioplasty. N Engl J Med. 1994;330:981–93. doi: 10.1056/NEJM199404073301407.. [DOI] [PubMed] [Google Scholar]
- 34.Hao H, Gabbiani G, Bochaton-Piallat ML. Arterial smooth muscle cell heterogeneity: implications for atherosclerosis and restenosis development. Arterioscler Thromb Vasc Biol. 2003;23:1510–20. doi: 10.1161/01.ATV.0000090130.85752.ED.. [DOI] [PubMed] [Google Scholar]
- 35.O’Keefe JJ, McCallister BD, Bateman TM, Kuhnlein DL, Ligon RW, Hartzler GO. Ineffectiveness of colchicine for the prevention of restenosis after coronary angioplasty. J Am Coll Cardiol. 1992;19:1597–600. doi: 10.1016/0735-1097(92)90624-v.. [DOI] [PubMed] [Google Scholar]
- 36.March KL, Mohanraj S, Ho PP, Wilensky RL, Hathaway DR. Biodegradable microspheres containing a colchicine analogue inhibit DNA synthesis in vascular smooth muscle cells. Circulation. 1994;89:1929–33. doi: 10.1161/01.cir.89.5.1929.. [DOI] [PubMed] [Google Scholar]
- 37.Freed M, Safian RD, O’Neill WW, Safian M, Jones D, Grines CL. Combination of lovastatin, enalapril, and colchicine does not prevent restenosis after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1995;76:1185–8. doi: 10.1016/s0002-9149(99)80334-8.. [DOI] [PubMed] [Google Scholar]
- 38.Carrozza JP, Jr., Kuntz RE, Fishman RF, Baim DS. Restenosis after arterial injury caused by coronary stenting in patients with diabetes mellitus. Ann Intern Med. 1993;118:344–9. doi: 10.7326/0003-4819-118-5-199303010-00004.. [DOI] [PubMed] [Google Scholar]
- 39.Sobel BE. Acceleration of restenosis by diabetes: pathogenetic implications. Circulation. 2001;103:1185–7. doi: 10.1161/01.cir.103.9.1185.. [DOI] [PubMed] [Google Scholar]
- 40.Deftereos S, Giannopoulos G, Raisakis K, Kossyvakis C, Kaoukis A, Panagopoulou V, et al. Colchicine treatment for the prevention of bare-metal stent restenosis in diabetic patients. J Am Coll Cardiol. 2013;61:1679–85. doi: 10.1016/j.jacc.2013.01.055.. [DOI] [PubMed] [Google Scholar]
- 41.Kong J, Deng Y, Dong Q, Liu W, Lu Y. Colchicine reduces restenosis after balloon angioplasty treatment for in-stent restenosis. Arch Med Res. 2015;46:101–6. doi: 10.1016/j.arcmed.2015.01.004.. [DOI] [PubMed] [Google Scholar]
- 42.Cole J, Lew R, Quinn S, Htun N, Freilich M, Layland J. 806 COlchicine to prevent PeriprocEdural Myocardial injury in percutaneous coronary intervention (COPE-PCI Trial) Heart, Lung, Circulation. 2020;29:S400. doi: 10.1016/j.hlc.2020.09.813.. [DOI] [Google Scholar]
- 43.Rodriguez-Granillo AM, Swieszkowski S, Correa-Sadouet C, Curotto MV, Gallardo C, Fernandez-Pereira C, et al. Efficacy and outcomes of colchicine for reduction of adverse outcomes in patients undergoing Pci with Bms. The Orca Registry. J Am Coll Cardiol. 2021. 10.1016/s0735-1097(21)02545-6.
- 44.Hemkens LG, Ewald H, Gloy VL, Arpagaus A, Olu KK, Nidorf M, et al. Cardiovascular effects and safety of long-term colchicine treatment: Cochrane review and meta-analysis. Heart. 2016;102:590–6. doi: 10.1136/heartjnl-2015-308542.. [DOI] [PubMed] [Google Scholar]
- 45.Deftereos S, Giannopoulos G, Angelidis C, Alexopoulos N, Filippatos G, Papoutsidakis N, et al. Anti-inflammatory treatment with colchicine in acute myocardial infarction: a pilot study. Circulation. 2015;132:1395–403. doi: 10.1161/CIRCULATIONAHA.115.017611.. [DOI] [PubMed] [Google Scholar]
- 46.Lim GB. Anti-inflammatory therapy for secondary prevention after MI. Nat Rev Cardiol. 2020;17:70–1. doi: 10.1038/s41569-019-0323-x.. [DOI] [PubMed] [Google Scholar]
- 47.Xia M, Yang X, Qian C. Meta-analysis evaluating the utility of colchicine in secondary prevention of coronary artery disease. Am J Cardiol. 2021;140:33–8. doi: 10.1016/j.amjcard.2020.10.043.. [DOI] [PubMed] [Google Scholar]
- 48.Abrantes AM, Nogueira-Garcia B, Alves M, Teixeira Passos D, Brito D, Pinto FJ, et al. Low-dose colchicine in coronary artery disease—systematic review and meta-analysis. Circ Rep. 2021;3:457–64. doi: 10.1253/circrep.CR-21-0065.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Narula S, Yusuf S, Chong M, Ramasundarahettige C, Rangarajan S, Bangdiwala SI, et al. Plasma ACE2 and risk of death or cardiometabolic diseases: a case-cohort analysis. Lancet. 2020;396:968–76. doi: 10.1016/S0140-6736(20)31964-4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen L, Li X, Chen M, Feng Y, Xiong C. The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2. Cardiovasc Res. 2020;116:1097–100. doi: 10.1093/cvr/cvaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Deftereos SG, Giannopoulos G, Vrachatis DA, Siasos GD, Giotaki SG, Gargalianos P, et al. Effect of colchicine vs standard care on cardiac and inflammatory biomarkers and clinical outcomes in patients hospitalized with coronavirus disease 2019: the GRECCO-19 randomized clinical trial. JAMA Netw Open. 2020;3:e2013136. doi: 10.1001/jamanetworkopen.2020.13136.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Papadopoulos C, Patoulias D, Teperikidis E, Mouselimis D, Tsarouchas A, Toumpourleka M, et al. Colchicine as a potential therapeutic agent against cardiovascular complications of COVID-19: an exploratory review. SN Compr Clin Med. 2020:1–11. 10.1007/s42399-020-00421-x. [DOI] [PMC free article] [PubMed]
- 53.Anton-Vazquez V, Byrne L, Anderson L, Hamzah L. COVID-19 cardiac injury and the use of colchicine. BMJ Case Rep. 2021. 10.1136/bcr-2020-241047. [DOI] [PMC free article] [PubMed]
- 54.Tardif JC, Bouabdallaoui N, L’Allier PL, Gaudet D, Shah B, Pillinger MH, et al. Colchicine for community-treated patients with COVID-19 (COLCORONA): a phase 3, randomised, double-blinded, adaptive, placebo-controlled, multicentre trial. Lancet Respir Med. 2021;9:924–32. doi: 10.1016/S2213-2600(21)00222-8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cochain C, Zernecke A. Macrophages in vascular inflammation and atherosclerosis. Pflug Arch. 2017;469:485–99. doi: 10.1007/s00424-017-1941-y.. [DOI] [PubMed] [Google Scholar]
- 56.Gomez D, Owens GK. Smooth muscle cell phenotypic switching in atherosclerosis. Cardiovasc Res. 2012;95:156–64. doi: 10.1093/cvr/cvs115.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rubanyi GM. The role of endothelium in cardiovascular homeostasis and diseases. J Cardiovasc Pharmacol. 1993;22:S1–14. doi: 10.1097/00005344-199322004-00002.. [DOI] [PubMed] [Google Scholar]
- 58.Leung YY, Yao HL, Kraus VB. Colchicine—Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum. 2015;45:341–50. doi: 10.1016/j.semarthrit.2015.06.013.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Martinez GJ, Celermajer DS, Patel S. The NLRP3 inflammasome and the emerging role of colchicine to inhibit atherosclerosis-associated inflammation. Atherosclerosis. 2018;269:262–71. doi: 10.1016/j.atherosclerosis.2017.12.027.. [DOI] [PubMed] [Google Scholar]
- 60.Kinlay S, Libby P, Ganz P. Endothelial function and coronary artery disease. Curr Opin Lipidol. 2001;12:383–9. doi: 10.1097/00041433-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 61.Helmut Drexler M. Factors involved in the maintenance of endothelial function. Am J Cardiol. 1998. 10.1016/S0002-9149(98)00667-5. [DOI] [PubMed]
- 62.Thomas F. Lüscher M.D., Matthias Barton M.D. Biology of the Endothelium. Clinical Cardiology. 1997;20:ii-3–ii-10. 10.1002/j.1932-8737.1997.tb00006.x. [PubMed]
- 63.Leo F, Suvorava T, Heuser SK, Li J, LoBue A, Barbarino F, et al. Red blood cell and endothelial eNOS independently regulate circulating nitric oxide metabolites and blood pressure. Circulation. 2021 doi: 10.1161/circulationaha.120.049606.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rubbo H, Trostchansky A, Botti H, Batthyány C. Interact nitric oxide peroxynitrite low-density lipoprotein. Biol Chem. 2002;383:547–52. doi: 10.1515/BC.2002.055. [DOI] [PubMed] [Google Scholar]
- 65.Schunk SJ, Triem S, Schmit D, Zewinger S, Sarakpi T, Becker E, et al. Interleukin-1alpha (IL-1alpha) is a central regulator of leukocyte-endothelial adhesion in myocardial infarction and in chronic kidney disease. Circulation. 2021 doi: 10.1161/circulationaha.121.053547.. [DOI] [PubMed] [Google Scholar]
- 66.Akhmedov A, Sawamura T, Chen CH, Kraler S, Vdovenko D, Luscher TF. Lectin-like oxidized low-density lipoprotein receptor-1 (LOX-1): a crucial driver of atherosclerotic cardiovascular disease. Eur Heart J. 2021;42:1797–807. doi: 10.1093/eurheartj/ehaa770.. [DOI] [PubMed] [Google Scholar]
- 67.Schachinger V, Britten MB, Elsner M, Walter DH, Scharrer I, Zeiher AM. A positive family history of premature coronary artery disease is associated with impaired endothelium-dependent coronary blood flow regulation. Circulation. 1999;100:1502–8. doi: 10.1161/01.cir.100.14.1502.. [DOI] [PubMed] [Google Scholar]
- 68.Vita JA, Treasure CB, Nabel EG, McLenachan JM, Fish RD, Yeung AC, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation. 1990;81:491–7. doi: 10.1161/01.cir.81.2.491.. [DOI] [PubMed] [Google Scholar]
- 69.Ludmer PL, Selwyn AP, Shook TL, Wayne RR, Mudge GH, Alexander RW, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315:1046–51. doi: 10.1056/nejm198610233151702.. [DOI] [PubMed] [Google Scholar]
- 70.Ganguly A, Yang H, Zhang H, Cabral F, Patel KD. Microtubule dynamics control tail retraction in migrating vascular endothelial cells. Mol Cancer Ther. 2013;12:2837–46. doi: 10.1158/1535-7163.MCT-13-0401.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pamuk BO, Sari I, Selcuk S, Gokce G, Kozaci DL. Evaluation of circulating endothelial biomarkers in familial Mediterranean fever. Rheumatol Int. 2013;33:1967–72. doi: 10.1007/s00296-013-2681-8.. [DOI] [PubMed] [Google Scholar]
- 72.Cimmino G, Conte S, Morello A, Pellegrino G, Marra L, Cali G, et al. Colchicine inhibits the prothrombotic effects of oxLDL in human endothelial cells. Vasc Pharmacol. 2021;137:106822. doi: 10.1016/j.vph.2020.106822.. [DOI] [PubMed] [Google Scholar]
- 73.Jacobsen K, Lund MB, Shim J, Gunnersen S, Fuchtbauer EM, Kjolby M, et al. Diverse cellular architecture of atherosclerotic plaque derives from clonal expansion of a few medial SMCs. JCI Insight. 2017;2:e95890. 10.1172/jci.insight.95890. [DOI] [PMC free article] [PubMed]
- 74.Chen Z, Ichetovkin M, Kurtz M, Zycband E, Kawka D, Woods J, et al. Cholesterol in human atherosclerotic plaque is a marker for underlying disease state and plaque vulnerability. Lipids Health Dis. 2010;9:61. doi: 10.1186/1476-511x-9-61.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Okura Y, Brink M, Itabe H, Scheidegger KJ, Kalangos A, Delafontaine P. Oxidized low-density lipoprotein is associated with apoptosis of vascular smooth muscle cells in human atherosclerotic plaques. Circulation. 2000;102:2680–6. doi: 10.1161/01.cir.102.22.2680.. [DOI] [PubMed] [Google Scholar]
- 76.Yu H, Stoneman V, Clarke M, Figg N, Xin HB, Kotlikoff M, et al. Bone marrow-derived smooth muscle-like cells are infrequent in advanced primary atherosclerotic plaques but promote atherosclerosis. Arterioscler Thromb Vasc Biol. 2011;31:1291–9. doi: 10.1161/atvbaha.110.218578.. [DOI] [PubMed] [Google Scholar]
- 77.Clarke MC, Talib S, Figg NL, Bennett MR. Vascular smooth muscle cell apoptosis induces interleukin-1-directed inflammation: effects of hyperlipidemia-mediated inhibition of phagocytosis. Circ Res. 2010;106:363–72. doi: 10.1161/circresaha.109.208389. [DOI] [PubMed] [Google Scholar]
- 78.Bauriedel G, Heimerl J, Beinert T, Welsch U, Hofling B. Colchicine antagonizes the activity of human smooth muscle cells cultivated from arteriosclerotic lesions after atherectomy. Coron Artery Dis. 1994;5:531–9. [PubMed] [Google Scholar]
- 79.Bauriedel G, Ganesh S, Uberfuhr P, Welsch U, Hofling B. Growth-inhibiting effect of colchicine on cultured vascular wall myocytes from arteriosclerotic lesions. Z Kardiol. 1992;81:92–8. [PubMed] [Google Scholar]
- 80.Mehta UM, Kaul D. Effect of trifluoperazine and colchicine on smooth muscle cellular proliferative and secretory activity induced by hypercholesterolemic medium in vitro. Biochem Int. 1990;21:107–16. [PubMed] [Google Scholar]
- 81.Tabas I, Williams KJ, Boren J. Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation. 2007;116:1832–44. doi: 10.1161/circulationaha.106.676890.. [DOI] [PubMed] [Google Scholar]
- 82.Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, et al. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science. 2009;325:612–6. doi: 10.1126/science.1175202.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yvan-Charvet L, Wang N, Tall AR. Role of HDL, ABCA1, and ABCG1 transporters in cholesterol efflux and immune responses. Arterioscler Thromb Vasc Biol. 2010;30:139–43. doi: 10.1161/atvbaha.108.179283.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, et al. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357–61. doi: 10.1038/nature08938.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Altaf A, Qu P, Zhao Y, Wang H, Lou D, Niu N. NLRP3 inflammasome in peripheral blood monocytes of acute coronary syndrome patients and its relationship with statins. Coron Artery Dis. 2015;26:409–21. doi: 10.1097/mca.0000000000000255.. [DOI] [PubMed] [Google Scholar]
- 86.Martinez FO, Gordon S. The M1 and M2 paradigm of macrophage activation: time for reassessment. F1000Prime Rep. 2014;6:13. doi: 10.12703/p6-13.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.McLaren JE, Michael DR, Salter RC, Ashlin TG, Calder CJ, Miller AM, et al. IL-33 reduces macrophage foam cell formation. J Immunol. 2010;185:1222–9. doi: 10.4049/jimmunol.1000520.. [DOI] [PubMed] [Google Scholar]
- 88.Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41:14–20. doi: 10.1016/j.immuni.2014.06.008.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rong JX, Shapiro M, Trogan E, Fisher EA. Transdifferentiation of mouse aortic smooth muscle cells to a macrophage-like state after cholesterol loading. Proc Natl Acad Sci USA. 2003;100:13531–6. doi: 10.1073/pnas.1735526100.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chung EY, Kim SJ, Ma XJ. Regulation of cytokine production during phagocytosis of apoptotic cells. Cell Res. 2006;16:154–61. doi: 10.1038/sj.cr.7310021. [DOI] [PubMed] [Google Scholar]
- 91.Hirata Y, Tabata M, Kurobe H, Motoki T, Akaike M, Nishio C, et al. Coronary atherosclerosis is associated with macrophage polarization in epicardial adipose tissue. J Am Coll Cardiol. 2011;58:248–55. doi: 10.1016/j.jacc.2011.01.048.. [DOI] [PubMed] [Google Scholar]
- 92.Babaev VR, Ding L, Zhang Y, May JM, Lin PC, Fazio S, et al. Macrophage IKKalpha deficiency suppresses Akt phosphorylation, reduces cell survival, and decreases early atherosclerosis. Arterioscler Thromb Vasc Biol. 2016;36:598–607. doi: 10.1161/ATVBAHA.115.306931.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Perico N, Ostermann D, Bontempeill M, Morigi M, Amuchastegui CS, Zoja C, et al. Colchicine interferes with L-selectin and leukocyte function-associated antigen-1 expression on human T lymphocytes and inhibits T cell activation. J Am Soc Nephrol. 1996;7:594–601. doi: 10.1681/asn.V74594.. [DOI] [PubMed] [Google Scholar]
- 94.Gagne V, Marois L, Levesque JM, Galarneau H, Lahoud MH, Caminschi I, et al. Modulation of monosodium urate crystal-induced responses in neutrophils by the myeloid inhibitory C-type lectin-like receptor: potential therapeutic implications. Arthritis Res Ther. 2013;15:R73. doi: 10.1186/ar4250.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cronstein BN, Molad Y, Reibman J, Balakhane E, Levin RI, Weissmann G. Colchicine alters the quantitative and qualitative display of selectins on endothelial cells and neutrophils. J Clin Invest. 1995;96:994–1002. doi: 10.1172/jci118147.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sukeishi A, Isami K, Hiyama H, Imai S, Nagayasu K, Shirakawa H, et al. Colchicine alleviates acute postoperative pain but delays wound repair in mice: roles of neutrophils and macrophages. Mol Pain. 2017;13:1744806917743680. doi: 10.1177/1744806917743680.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang L, Peng Y, Song L, Xia D, Li C, Li Z, et al. Colchicine-containing nanoparticles attenuates acute myocardial infarction injury by inhibiting inflammation. Cardiovasc Drugs Ther. 2021. 10.1007/s10557-021-07239-2. [DOI] [PubMed]
- 98.Li Y, Che J, Chang L, Guo M, Bao X, Mu D, et al. CD47 and integrin alpha4/beta1 Co-modified macrophage membrane-coated nanoparticles enable delivery of colchicine to atherosclerotic plaque. Adv Healthc Mater. 2021:e2101788. 10.1002/adhm.202101788. [DOI] [PubMed]
- 99.Vaidya K, Tucker B, Kurup R, Khandkar C, Pandzic E, Barraclough J, et al. Colchicine inhibits neutrophil extracellular trap formation in patients with acute coronary syndrome after percutaneous coronary intervention. J Am Heart Assoc. 2021;10:e018993. doi: 10.1161/jaha.120.018993.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Korporaal SJ, Van Eck M, Adelmeijer J, Ijsseldijk M, Out R, Lisman T, et al. Platelet activation by oxidized low density lipoprotein is mediated by CD36 and scavenger receptor-A. Arterioscler Thromb Vasc Biol. 2007;27:2476–83. doi: 10.1161/atvbaha.107.150698.. [DOI] [PubMed] [Google Scholar]
- 101.Rother E, Brandl R, Baker DL, Goyal P, Gebhard H, Tigyi G, et al. Subtype-selective antagonists of lysophosphatidic Acid receptors inhibit platelet activation triggered by the lipid core of atherosclerotic plaques. Circulation. 2003;108:741–7. doi: 10.1161/01.Cir.0000083715.37658.C4.. [DOI] [PubMed] [Google Scholar]
- 102.Fox JE. Cytoskeletal proteins and platelet signaling. Thromb Haemost. 2001;86:198–213. doi: 10.1055/s-0037-1616218. [DOI] [PubMed] [Google Scholar]
- 103.Menche D, Israel A, Karpatkin S. Platelets and microtubules. Effect of colchicine and D2O on platelet aggregation and release induced by calcium ionophore A23187. J Clin Invest. 1980;66:284–91. doi: 10.1172/jci109855.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cimmino G, Tarallo R, Conte S, Morello A, Pellegrino G, Loffredo FS, et al. Colchicine reduces platelet aggregation by modulating cytoskeleton rearrangement via inhibition of cofilin and LIM domain kinase 1. Vasc Pharmacol. 2018;111:62–70. doi: 10.1016/j.vph.2018.09.004.. [DOI] [PubMed] [Google Scholar]
- 105.Muranyi A, MacDonald JA, Deng JT, Wilson DP, Haystead TA, Walsh MP, et al. Phosphorylation of the myosin phosphatase target subunit by integrin-linked kinase. Biochem J. 2002;366:211–6. doi: 10.1042/bj20020401.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.D’Andrea G, Cananzi AR, Toldo M, Ferro-Milone F. Platelet activity in cluster headache. Cephalalgia. 1986;6:163–7. doi: 10.1046/j.1468-2982.1986.0603163.x.. [DOI] [PubMed] [Google Scholar]
- 107.Abanonu GB, Daskin A, Akdogan MF, Uyar S, Demirtunc R. Mean platelet volume and beta-thromboglobulin levels in familial Mediterranean fever: effect of colchicine use? Eur J Intern Med. 2012;23:661–4. doi: 10.1016/j.ejim.2012.04.007.. [DOI] [PubMed] [Google Scholar]
- 108.Ribbi-Jaffe A, Apitz-Castro R. The effect of colchicine on human blood platelets under conditions of short-term incubation. Biochem J. 1979;178:449–54. doi: 10.1042/bj1780449.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Soppitt GD, Mitchell JR. The effect of colchicine on human platelet behaviour. J Atheroscler Res. 1969;10:247–52. doi: 10.1016/s0368-1319(69)80012-8.. [DOI] [PubMed] [Google Scholar]
- 110.Korkmaz S, Erturan I, Naziroglu M, Uguz AC, Cig B, Ovey IS. Colchicine modulates oxidative stress in serum and neutrophil of patients with Behcet disease through regulation of Ca2+ release and antioxidant system. J Membr Biol. 2011;244:113–20. doi: 10.1007/s00232-011-9404-4.. [DOI] [PubMed] [Google Scholar]
- 111.Terekeci HM, Oktenli C, Ozgurtas T, Nalbant S, Top C, Celik S, et al. Increased asymmetric dimethylarginine levels in young men with familial Mediterranean fever (FMF): is it early evidence of interaction between inflammation and endothelial dysfunction in FMF? J Rheumatol. 2008;35:2024–9. [PubMed] [Google Scholar]
- 112.Pennings GJ, Reddel CJ, Traini M, Campbell H, Chen V, Kritharides L. Colchicine inhibits ROS generation in response to glycoprotein VI stimulation. Sci Rep. 2021;11:11965.. doi: 10.1038/s41598-021-91409-7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Beaulieu LM, Lin E, Mick E, Koupenova M, Weinberg EO, Kramer CD, et al. Interleukin 1 receptor 1 and interleukin 1beta regulate megakaryocyte maturation, platelet activation, and transcript profile during inflammation in mice and humans. Arterioscler Thromb Vasc Biol. 2014;34:552–64. doi: 10.1161/atvbaha.113.302700.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Downing H, EvaNogales K. Tubulin and microtubule structure. Curr Opin Cell Biol. 1998;10:16–22. doi: 10.1016/S0955-0674(98)80082-3.. [DOI] [PubMed] [Google Scholar]
- 115.Stephens RE, Edds KT. Microtubules: structure, chemistry, and function. Physiol Rev. 1976;56:709–77. doi: 10.1152/physrev.1976.56.4.709.. [DOI] [PubMed] [Google Scholar]
- 116.Ouyang C, Mu J, Lu Q, Li J, Zhu H, Wang Q, et al. Autophagic degradation of KAT2A/GCN5 promotes directional migration of vascular smooth muscle cells by reducing TUBA/alpha-tubulin acetylation. Autophagy. 2020;16:1753–70. doi: 10.1080/15548627.2019.1707488.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gao W, Yang J, Liu W, Wang Y, Shao F. Site-specific phosphorylation and microtubule dynamics control Pyrin inflammasome activation. Proc Natl Acad Sci USA. 2016;113:E4857–66. doi: 10.1073/pnas.1601700113.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Misawa T, Takahama M, Kozaki T, Lee H, Zou J, Saitoh T, et al. Microtubule-driven spatial arrangement of mitochondria promotes activation of the NLRP3 inflammasome. Nat Immunol. 2013;14:454–60. doi: 10.1038/ni.2550.. [DOI] [PubMed] [Google Scholar]
- 119.Bhattacharyya B, Panda D, Gupta S, Banerjee M. Anti-mitotic activity of colchicine and the structural basis for its interaction with tubulin. Med Res Rev. 2008;28:155–83. doi: 10.1002/med.20097.. [DOI] [PubMed] [Google Scholar]
- 120.Sen R, Baltimore D. Multiple nuclear factors interact with the immunoglobulin enhancer sequences. Cell. 1986;46:705–16. [DOI] [PubMed]
- 121.Sarkar FH, Li Y, Wang Z, Kong D. NF-kappaB signaling pathway and its therapeutic implications in human diseases. Int Rev Immunol. 2008;27:293–319. doi: 10.1080/08830180802276179.. [DOI] [PubMed] [Google Scholar]
- 122.Taniguchi K, Karin M. NF-kappaB, inflammation, immunity and cancer: coming of age. Nat Rev Immunol. 2018;18:309–24. doi: 10.1038/nri.2017.142. [DOI] [PubMed] [Google Scholar]
- 123.Gul A. Behcet’s disease: an update on the pathogenesis. Clin Exp Rheumatol. 2001;19:S6–12. [PubMed] [Google Scholar]
- 124.Steinhubl SR, Badimon JJ, Bhatt DL, Herbert JM, Luscher TF. Clinical evidence for anti-inflammatory effects of antiplatelet therapy in patients with atherothrombotic disease. Vasc Med. 2007;12:113–22. doi: 10.1177/1358863x07077462.. [DOI] [PubMed] [Google Scholar]
- 125.Oeth P, Parry GC, Mackman N. Regulation of the tissue factor gene in human monocytic cells. Role of AP-1, NF-kappa B/Rel, and Sp1 proteins in uninduced and lipopolysaccharide-induced expression. Arterioscler Thromb Vasc Biol. 1997;17:365–74. doi: 10.1161/01.atv.17.2.365.. [DOI] [PubMed] [Google Scholar]
- 126.Simmonds RE, Foxwell BM. Signalling, inflammation, and arthritis: NF-kappaB and its relevance to arthritis and inflammation. Rheumatology. 2008;47:584–90. doi: 10.1093/rheumatology/kem298.. [DOI] [PubMed] [Google Scholar]
- 127.Hajra L, Evans AI, Chen M, Hyduk SJ, Collins T, Cybulsky MI. The NF-kappa B signal transduction pathway in aortic endothelial cells is primed for activation in regions predisposed to atherosclerotic lesion formation. Proc Natl Acad Sci USA. 2000;97:9052–7. doi: 10.1073/pnas.97.16.9052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Brown MA, Jones WK. NF-kappaB action in sepsis: the innate immune system and the heart. Front Biosci. 2004;9:1201–17. doi: 10.2741/1304. [DOI] [PubMed] [Google Scholar]
- 129.Mackenzie GG, Keen CL, Oteiza PI. Microtubules are required for NF-kappaB nuclear translocation in neuroblastoma IMR-32 cells: modulation by zinc. J Neurochem. 2006;99:402–15. doi: 10.1111/j.1471-4159.2006.04005.x.. [DOI] [PubMed] [Google Scholar]
- 130.Jackman RW, Rhoads MG, Cornwell E, Kandarian SC. Microtubule-mediated NF-kappaB activation in the TNF-alpha signaling pathway. Exp Cell Res. 2009;315:3242–9. doi: 10.1016/j.yexcr.2009.08.020.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ben-David H, Livneh A, Lidar M, Feld O, Haj YS, Grossman C, et al. Toll-like receptor 2 is overexpressed in Familial Mediterranean fever patients and is inhibited by colchicine treatment. Best Pr Res Clin Rheumatol. 2018;32:651–61. doi: 10.1016/j.berh.2019.01.012.. [DOI] [PubMed] [Google Scholar]
- 132.Martinon F, Mayor A, Tschopp J. The inflammasomes: guardians of the body. Annu Rev Immunol. 2009;27:229–65. doi: 10.1146/annurev.immunol.021908.132715.. [DOI] [PubMed] [Google Scholar]
- 133.Centola M, Wood G, Frucht DM, Galon J, Aringer M, Farrell C, et al. The gene for familial Mediterranean fever, MEFV, is expressed in early leukocyte development and is regulated in response to inflammatory mediators. Blood. 2000;95:3223–31. doi: 10.1182/blood.V95.10.3223. [DOI] [PubMed] [Google Scholar]
- 134.Stutz A, Golenbock DT, Latz E. Inflammasomes: too big to miss. J Clin Invest. 2009;119:3502–11. doi: 10.1172/jci40599.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Vandanmagsar B, Youm YH, Ravussin A, Galgani JE, Stadler K, Mynatt RL, et al. The NLRP3 inflammasome instigates obesity-induced inflammation and insulin resistance. Nat Med. 2011;17:179–88. doi: 10.1038/nm.2279.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440:237–41. doi: 10.1038/nature04516.. [DOI] [PubMed] [Google Scholar]
- 137.Van Gorp H, Saavedra PH, de Vasconcelos NM, Van Opdenbosch N, Vande WL, Matusiak M, et al. Familial Mediterranean fever mutations lift the obligatory requirement for microtubules in Pyrin inflammasome activation. Proc Natl Acad Sci USA. 2016;113:14384–9. doi: 10.1073/pnas.1613156113.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Park YH, Wood G, Kastner DL, Chae JJ. Pyrin inflammasome activation and RhoA signaling in the autoinflammatory diseases FMF and HIDS. Nat Immunol. 2016;17:914–21. doi: 10.1038/ni.3457.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Fernando S, Schwarz N, Williamson A, Toledo D, Zareh J, Di Bartolo B, et al. Anti-inflammatory effects of colchicine on oxidised low-density lipoproteins and cholesterol crystal-induced macrophage activation in vitro. Heart, Lung, Circulation. 2017;26:S69–S70. doi: 10.1016/j.hlc.2017.06.060.. [DOI] [Google Scholar]
- 140.Pelegrin P. Many ways to dilate the P2X7 receptor pore. Br J Pharmacol. 2011;163:908–11. doi: 10.1111/j.1476-5381.2011.01325.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nidorf SM, Eikelboom JW, Thompson PL. Targeting cholesterol crystal-induced inflammation for the secondary prevention of cardiovascular disease. J Cardiovasc Pharmacol Ther. 2014;19:45–52. doi: 10.1177/1074248413499972.. [DOI] [PubMed] [Google Scholar]
- 142.Robertson S, Martinez GJ, Payet CA, Barraclough JY, Celermajer DS, Bursill C, et al. Colchicine therapy in acute coronary syndrome patients acts on caspase-1 to suppress NLRP3 inflammasome monocyte activation. Clin Sci. 2016;130:1237–46. doi: 10.1042/CS20160090.. [DOI] [PubMed] [Google Scholar]
- 143.Silvis MJM, Fiolet ATL, Opstal TSJ, Dekker M, Suquilanda D, Zivkovic M, et al. Colchicine reduces extracellular vesicle NLRP3 inflammasome protein levels in chronic coronary disease: a LoDoCo2 biomarker substudy. Atherosclerosis. 2021;334:93–100. doi: 10.1016/j.atherosclerosis.2021.08.005.. [DOI] [PubMed] [Google Scholar]
- 144.Guan T, Gao B, Chen G, Chen X, Janssen M, Uttarwar L, et al. Colchicine attenuates renal injury in a model of hypertensive chronic kidney disease. Am J Physiol Ren Physiol. 2013;305:F1466–76. doi: 10.1152/ajprenal.00057.2013.. [DOI] [PubMed] [Google Scholar]
- 145.Shu JC, He YJ, Lv X, Ye GR, Wang LX. Curcumin prevents liver fibrosis by inducing apoptosis and suppressing activation of hepatic stellate cells. J Nat Med. 2009;63:415–20. doi: 10.1007/s11418-009-0347-3.. [DOI] [PubMed] [Google Scholar]
- 146.Bozkurt D, Bicak S, Sipahi S, Taskin H, Hur E, Ertilav M, et al. The effects of colchicine on the progression and regression of encapsulating peritoneal sclerosis. Perit Dial Int. 2008;28:S53–7. doi: 10.1177/089686080802805S11. [DOI] [PubMed] [Google Scholar]
- 147.Atta HM, El-Rehany MA, Abdel RS, Fouad R, Galal AM. Colchicine inhibits intimal hyperplasia and leukocyte VEGF expression in dogs. J Surg Res. 2008;146:184–9. doi: 10.1016/j.jss.2007.04.029.. [DOI] [PubMed] [Google Scholar]
- 148.Sandbo N, Ngam C, Torr E, Kregel S, Kach J, Dulin N. Control of myofibroblast differentiation by microtubule dynamics through a regulated localization of mDia2. J Biol Chem. 2013;288:15466–73. doi: 10.1074/jbc.M113.464461.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Entzian P, Schlaak M, Seitzer U, Bufe A, Acil Y, Zabel P. Antiinflammatory and antifibrotic properties of colchicine: implications for idiopathic pulmonary fibrosis. Lung. 1997;175:41–51. doi: 10.1007/pl00007555.. [DOI] [PubMed] [Google Scholar]
- 150.Wu Q, Liu H, Liao J, Zhao N, Tse G, Han B, et al. Colchicine prevents atrial fibrillation promotion by inhibiting IL-1beta-induced IL-6 release and atrial fibrosis in the rat sterile pericarditis model. Biomed Pharmacother. 2020;129:110384. doi: 10.1016/j.biopha.2020.110384.. [DOI] [PubMed] [Google Scholar]
- 151.Paya M, Terencio MC, Ferrandiz ML, Alcaraz MJ. Involvement of secretory phospholipase A2 activity in the zymosan rat air pouch model of inflammation. Br J Pharmacol. 1996;117:1773–9. doi: 10.1111/j.1476-5381.1996.tb15353.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zurier RB, Hoffstein S, Weissmann G. Mechanisms of lysosomal enzyme release from human leukocytes. I. Effect of cyclic nucleotides and colchicine. J Cell Biol. 1973;58:27–41. doi: 10.1083/jcb.58.1.27.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Roberge CJ, Gaudry M, de Medicis R, Lussier A, Poubelle PE, Naccache PH. Crystal-induced neutrophil activation. IV. Specific inhibition of tyrosine phosphorylation by colchicine. J Clin Invest. 1993;92:1722–9. doi: 10.1172/jci116759.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Roberge CJ, Gaudry M, Gilbert C, Malawista SE, de Medicis R, Lussier A, et al. Paradoxical effects of colchicine on the activation of human neutrophilis by chemotactic factors and inflammatory microcrystal. J Leukoc Biol. 1996;59:864–71. doi: 10.1002/jlb.59.6.864.. [DOI] [PubMed] [Google Scholar]
- 155.Gaudry M, Roberge CJ, de Medicis R, Lussier A, Poubelle PE, Naccache PH. Crystal-induced neutrophil activation. III. Inflammatory microcrystals induce a distinct pattern of tyrosine phosphorylation in human neutrophils. J Clin Invest. 1993;91:1649–55. doi: 10.1172/JCI116373.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ben-Chetrit E, Bergmann S, Sood R. Mechanism of the anti-inflammatory effect of colchicine in rheumatic diseases: a possible new outlook through microarray analysis. Rheumatology. 2006;45:274–82. doi: 10.1093/rheumatology/kei140.. [DOI] [PubMed] [Google Scholar]
- 157.Rochdi M, Sabouraud A, Baud FJ, Bismuth C, Scherrmann. JM. Toxicokinetics of colchicine in humans: analysis of tissue, plasma and urine data in ten cases. Hum Exp Toxicol. 1992;11:510–6. doi: 10.1177/096032719201100612.. [DOI] [PubMed] [Google Scholar]
- 158.Folpini A, Furfori P. Colchicine toxicity—clinical features and treatment. Massive overdose case report. J Toxicol Clin Toxicol. 1995;33:71–7. doi: 10.3109/15563659509020219.. [DOI] [PubMed] [Google Scholar]
- 159.Ferron GM, Rochdi M, Jusko WJ, Scherrmann JM. Oral absorption characteristics and pharmacokinetics of colchicine in healthy volunteers after single and multiple doses. J Clin Pharmacol. 1996;36:874–83. doi: 10.1002/j.1552-4604.1996.tb04753.x.. [DOI] [PubMed] [Google Scholar]
- 160.Chappey ON, Niel E, Wautier JL, Hung PP, Dervichian M, Cattan D, et al. Colchicine disposition in human leukocytes after single and multiple oral administration. Clin Pharmacol Ther. 1993;54:360–7. doi: 10.1038/clpt.1993.161.. [DOI] [PubMed] [Google Scholar]
- 161.Emmerson BT. The management of gout. N Engl J Med. 1996;334:445–51. doi: 10.1056/nejm199602153340707.. [DOI] [PubMed] [Google Scholar]
- 162.Rochdi M, Sabouraud A, Girre C, Venet R, Scherrmann JM. Pharmacokinetics and absolute bioavailability of colchicine after i.v. and oral administration in healthy human volunteers and elderly subjects. Eur J Clin Pharmacol. 1994;46:351–4. doi: 10.1007/bf00194404. [DOI] [PubMed] [Google Scholar]
- 163.Terkeltaub RA. Colchicine update: 2008. Semin Arthritis Rheum. 2009;38:411–9. doi: 10.1016/j.semarthrit.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 164.Finkelstein Y, Aks SE, Hutson JR, Juurlink DN, Nguyen P, Dubnov-Raz G, et al. Colchicine poisoning: the dark side of an ancient drug. Clin Toxicol (Philos) 2010;48:407–14. doi: 10.3109/15563650.2010.495348. [DOI] [PubMed] [Google Scholar]
- 165.Tateishi T, Soucek P, Caraco Y, Guengerich FP, Wood AJ. Colchicine biotransformation by human liver microsomes. Identification of CYP3A4 as the major isoform responsible for colchicine demethylation. Biochem Pharmacol. 1997;53:111–6. doi: 10.1016/s0006-2952(96)00693-4. [DOI] [PubMed] [Google Scholar]
- 166.Decleves X, Niel E, Debray M, Scherrmann JM. Is P-glycoprotein (ABCB1) a phase 0 or a phase 3 colchicine transporter depending on colchicine exposure conditions? Toxicol Appl Pharmacol. 2006;217:153–60. doi: 10.1016/j.taap.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 167.Dogukan A, Oymak FS, Taskapan H, Guven M, Tokgoz B, Utas C. Acute fatal colchicine intoxication in a patient on continuous ambulatory peritoneal dialysis (CAPD). Possible role of clarithromycin administration. Clin Nephrol. 2001;55:181–2. [PubMed] [Google Scholar]
- 168.ACR releases new guidelines for gout. Pharmacoecon. Outcomes News 2012;666:2. 10.2165/00151234-201206660-00002.
- 169.Adler Y, Charron P, Imazio M, Badano L, Barón-Esquivias G, Bogaert J, et al.. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015;68:1126. 10.1016/j.rec.2015.10.008. [DOI] [PubMed]
- 170.Nidorf SM, Fiolet A, Mosterd A, Eikelboom JW, Schut A, Opstal T, et al. Colchicine in patients with chronic coronary disease. N Engl J Med. 2020;383:1838–47. doi: 10.1056/NEJMoa2021372.. [DOI] [PubMed] [Google Scholar]
- 171.Raju NC, Yi Q, Nidorf M, Fagel ND, Hiralal R, Eikelboom JW. Effect of colchicine compared with placebo on high sensitivity C-reactive protein in patients with acute coronary syndrome or acute stroke: a pilot randomized controlled trial. J Thromb Thrombolysis. 2012;33:88–94. doi: 10.1007/s11239-011-0637-y.. [DOI] [PubMed] [Google Scholar]
- 172.Martinez GJ, Robertson S, Barraclough J, Xia Q, Mallat Z, Bursill C, et al. Colchicine acutely suppresses local cardiac production of inflammatory cytokines in patients with an acute coronary syndrome. J Am Heart Assoc. 2015;4:e002128. doi: 10.1161/JAHA.115.002128.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Vaidya K, Arnott C, Martinez GJ, Ng B, McCormack S, Sullivan DR, et al. Colchicine therapy and plaque stabilization in patients with acute coronary syndrome: a CT coronary angiography study. JACC Cardiovasc Imaging. 2018;11:305–16. doi: 10.1016/j.jcmg.2017.08.013.. [DOI] [PubMed] [Google Scholar]
- 174.Shah B, Pillinger M, Zhong H, Cronstein B, Xia Y, Lorin JD, et al. Effects of acute colchicine administration prior to percutaneous coronary intervention: COLCHICINE-PCI randomized trial. Circ Cardiovasc Inter. 2020;13:e008717. doi: 10.1161/circinterventions.119.008717.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, et al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial. Circulation. 2005;112:2012–6. doi: 10.1161/circulationaha.105.542738.. [DOI] [PubMed] [Google Scholar]
- 176.Imazio M, Brucato A, Cemin R, Ferrua S, Maggiolini S, Beqaraj F, et al. A randomized trial of colchicine for acute pericarditis. N Engl J Med. 2013;369:1522–8. doi: 10.1056/NEJMoa1208536.. [DOI] [PubMed] [Google Scholar]
- 177.Deftereos S, Giannopoulos G, Panagopoulou V, Bouras G, Raisakis K, Kossyvakis C, et al. Anti-inflammatory treatment with colchicine in stable chronic heart failure: a prospective, randomized study. JACC Heart Fail. 2014;2:131–7. doi: 10.1016/j.jchf.2013.11.006.. [DOI] [PubMed] [Google Scholar]