Abstract
Background: Sedentariness is a substantial risk for many chronic diseases. We aimed to investigate the correlation of sedentary behavior and its indicators with low back pain (LBP) among adults and children.
Methods: Original articles published up to April 28, 2020, using PubMed, Embase, Web of Science and Scopus were evaluated. Odds ratio (OR, 95% CI) was considered the overall effect size for desired associations.
Results: We reviewed 49 English articles with analytical observational study design, of which, 27 studies with cross sectional/survey design were retained in the meta-analysis. Among adults, sedentary lifestyle was a considerable risk factor for LBP (OR=1.24, 1.02-1.5); prolonged sitting time (OR=1.42, 1.09-1.85) and driving time (OR=2.03, 1.22-3.36) were the significant risk factors. Sedentary behavior was associated with LBP in office workers (OR=1.23). Moreover, excess weight (OR=1.35, 1.14-1.59) and smoking (OR=1.28, 1.03-1.60) were associated with LBP. Among children, sedentary lifestyle was a remarkable risk factor for LBP (OR=1.41, 1.24- 1.60); prolonged TV watching (OR=1.23, 1.08-1.41) and computer/mobile using and console playing time (OR=1.63, 1.36-1.95) were significant risk factors for LBP. Consumption of coffee, however, has yield conflicting results to be considered as a risk factor. Moreover, the researches on the correlation between sedentariness and high-intensity LBP are scarce and inconclusive.
Conclusion: Sedentary behavior, whether in work or leisure time, associates with a moderate increase in the risk of LBP in adults, children and adolescents.
Keywords: Sedentary behavior, Screen time, Smoking, Obesity, Coffee, Low back pain
Introduction
Low back pain (LBP) is a paramount public health concern contributing to self-perceived disability and a high economic burden worldwide.1,2 It is associated with quality of life,3 long-term sickness, and early retirement as well.4 It is estimated that about 80% of the population has experienced an episode of LBP in their lives.5 LBP is more common in females and those between 40-69 years. LBP prevalence increases with aging, and the LBP in childhood associates with the corresponding figure in adulthood.6 It is shown that musculoskeletal symptoms in the lower back are correlated with other body segments, including the neck, upper back, and shoulders.7
Sedentary behaviors, on the other hand, are defined as activities with low energy expenditure, performed in rest positions. Sedentary behavior is a predictor of metabolic risk independent of physical inactivity.8 The health concerns associated with sedentariness are not merely attributable to lack of movement, but also to other simulations such as leisure or work screen time activities, including computer and internet use, TV (television) watching, cell phone use, and playing videogames.9 Besides, sedentary behavior is related with all-cause mortality concomitant with overweight and obesity, diabetes, and cardiovascular diseases.10,11 The association of sedentary behavior with musculoskeletal conditions such as LBP has been widely investigated among the population of workers and non-workers.12
With respect to sitting time, the findings regarding the association between sitting periods and LBP are inconsistent. One study among 704 participants demonstrated no independent association of sitting time in work time or the whole day with LBP. In this study, the body mass index moderated the mentioned association.13 In addition, the previous reviews did not mention any association between sitting time itself and LBP in leisure time or at work.14-16 However, a mixture of whole-body vibration, awkward postures, and prolonged sitting increased the risk of LBP.14 On the other hand, a study among 136 teaching staff reported that physical inactivity was related to LBP; but tobacco use and level of alcohol intake did not have such association with LBP.17 In a research among 665 blue-collar workers, a longer duration of sitting periods at work was beneficial for LBP.18 The difference in study design, measurement methods, and participants (or occupational groups) with different sedentary tasks may contribute to inconsistency for the correlation of sitting time and LBP in previous research.18
Excessive consumption of coffee and cigarette smoking were associated with an elevated likelihood of recurring LBP among 609 Polish residents. In this study hyperlipidemia, type 2 diabetes, and hypertension, were significantly associated with an increased likelihood of chronic LBP as well.19 Furthermore, in a cross-sectional study among 1221 school adolescents, playing video games (≥2 hours/day) and watching television (≥12 hours/week) were proposed as independent risk factors of LBP.20
Given the controversies in different articles, in this study, we investigated the relationship of different indicators of sedentary behavior and inactivity (including sitting time, screen time, smoking, consumption of coffee, and excess weight) with LBP, whether in leisure time or work time. We aimed to synthesize the available data to quantify the abovementioned associations to address inconsistencies in previous research. A brief systematic review has been presented in the case of a lack of required data for meta-analysis. In addition, we addressed the mentioned association among children and adolescents with a particular focus.
Methods
Search strategy
We performed a comprehensive search through electronic databases, including PubMed, Embase, Web of Science and Scopus for records published up to April 28, 2020. Based on a PEO framework (Patient/Population/Problem, Exposure, and Outcome) for the eligibility of the research question, we combined the indicators or equivalents of sedentary behavior on the one hand and the equivalents of LBP, on the other hand, for building the search strings. To facilitate the process of screening, we refined the results via the following filters wherever those were available in the search engines: article, journals, English language, full text, human studies. Appendix 1 shows the search strings in the abovementioned databases.
Study design
All the analytical observational studies (cross-sectional, case-control, or longitudinal designs) in which the association between sedentary behavior and LBP was investigated, were favorable to be contained in our review. We did not include the experimental studies in which the effects of behavior intervention or experiment on LBP were studied.
Patient/population/problem
Studies with individuals with a specific medical condition such as scoliosis or renal failure who may spend most of their time for sedentary activities were excluded. Age range and type of occupation were not considered as limiting factors, i.e., children and adults with sedentary behavior and LBP were considered to be the subjects of our review.
Exposure
Factors contributing to sedentary behavior, including sitting time, screen time, smoking, consumption of coffee, and body mass index, were considered to be the individuals’ exposures.
Outcome
The onset or recurrence of nonspecific or mechanical LBP measured via different methods was the desired outcome in our study. We excluded the studies in which sciatica or any kind of radicular pain was investigated.
Eligibility criteria and study selection
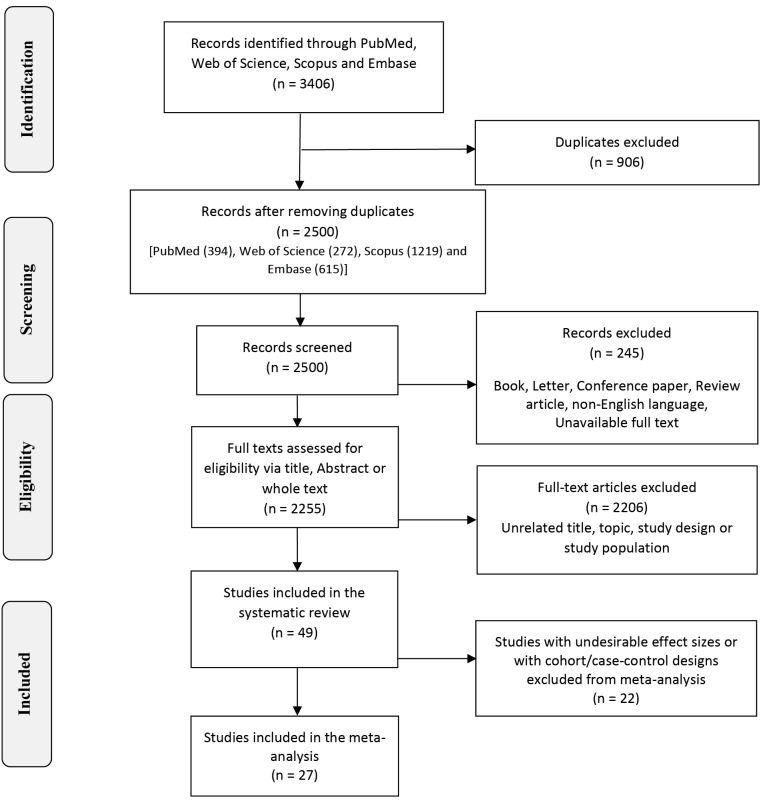
Two independent reviewers (S.B.M and R.R) screened the relevant records using Endnote software (version 18) after removing duplicates. Thereafter, additional letters, books, review or conference papers, non-English language, and unavailable full texts that were not excluded in refining results in the search engines were excluded. Then, we reviewed the full texts of remained records entirely at the next step. We excluded the articles with topics, study design, or participants irrelevant to our review (Figure 1). Any disagreement was solved via a discussion for reaching consensus in the whole process.
Figure 1.
Flowchart of study selection for systematic review and meta-analysis.
Assessment of study quality
Two of the researchers (S.B.M and B.V) performed the study quality assessment independently. The STROBE scale, which consists of 22 items (combined version, 2007), was used for this purpose.21 One score to each item was given by each reviewer separately, if the criteria were fulfilled. For each paper, a mean STROBE scores ≥16.5, in the range 11 to 16.5 and lower than 11 were considered as high, moderate and low with respect to study quality, respectively.22 The agreement coefficient between researcher’s scores was more than 0.5.
Statistical analysis
The desired effect size was considered as an odds ratio with 95% confidence interval (OR, 95% CI). Cochran’s Q and inconsistency index (I2) were used to explore the heterogeneity of the included articles. The random-effects model with DerSimonian and Liard method23 was used when data accumulated from studies, differed in ways that would have impacted on the results (e.g. subjects, exposure), otherwise the fixed effect model with inverse variance method was conducted. Then, the effect of each study on the pooled OR was assessed using sensitivity analysis. We performed subgroup analyses to evaluate the source of heterogeneity based on the following possible variables; type of sedentary behaviors and occupation type. The Begg’s and Egger’s tests were performed to explore publication bias. P value < 0.05 from both tests indicated remarkable publication bias. All analyses were conducted in the Stata, version 11.2 (STATA Corp, College Station, TX, USA).
Review writing style
The items included in the current review have been written according to the checklist and flow diagram of the PRISMA version 2009.24
Results
Characteristics of included studies
Overall, 3406 records were recognized via a comprehensive search through biomedical sources. With excluding duplicates, books, letters, conference papers, review articles, non-English records, and unavailable full texts, 2255 records remained to be screened via title, abstract or whole text. Finally, we included 49 studies in this review, of which 27 were retained in the meta-analysis for different purposes,19,20,25-49 18 were excluded due to undesirable effect sizes1,5,13,50-64 and 4 were excluded due to cohort/case-control designs.65-68 Figure 1 shows the process of study selection through a schematic flowchart.
With respect to study design of included articles in the review, 8 have been conducted in cohort/prospective design,51,52,54,56,58,65-67 1 in case-control design,55 1 in retrospective nested case-control design68 and the rest in cross-sectional/survey design. Among all studies, 15 were conducted in children or under graduated students.20,26,29,31,35,38,40,46,47,51,53,55,61,62,66 Only four studies investigated the association of coffee drinking with LBP.19,32,57,62 Complete information of these 49 articles has been presented in Table 1 and ordered chronologically from old studies to new ones.
Table 1. Summary of included studies in the systematic review .
|
First author;
(year) a |
Study design; Study participant | Sample size |
Age
(years) |
Sedentary behavior | Outcome | Assessment of low back pain | Main finding | Adjustment factors | Study quality b | Ref. |
| A. Burdorf (1993)c |
Cross-sectional Sedentary worker in Rotterdam |
275 | 41.5 | Prolong sedentary posture belong work | LBP | Nordic musculoskeletal questionnaire | The adjusted risk for LBP among carne operator and straddle-carrier was significantly higher than office workers who spent lower sedentary daily work time. | Age, Physical activity, whole-body vibration, prolonged sitting, cold and draught in current work, working under severe pressure, and job satisfaction. | Moderate | 50 |
| T. Skov (1996) |
Cross-sectional Danish salespeople |
1306 | 39.3 | Sedentary work (proportion of work time) |
Chronic LBP | Self-reported Nordic questionnaire | Driving and sedentary work were related to neck and low back pain. | - | Moderate | 25 |
| R. Gunzburg (1999)c |
Cohort Belgian students |
392 | 9 | Watching TV and playing video game (> 2 hours/day) | LBP | Questionnaire | More LBP in children who reported playing video games (> 2 hours/day). | - | High | 51 |
| P. R. Croft (1999)c |
Cohort UK general population |
4501 | 46.5 | Watching TV more than 3h/day | Overall LBP | Questionnaire | There is no significant link between watching TV more than 3 hour with risk of overall LBP. | Self-related health and psychological distress | High | 52 |
| C. Thorbjörnsson (1999) c |
Nested case-control Swedish general population |
484 | 26 | Sedentary work | LBP | Interview | Sedentary work was associated with an excess risk of LBP. | Age | High | 68 |
| D. K. Shehab (2003)c |
Cross-sectional Schoolchildren in Kuwait |
400 | 14.4 | Watching TV time. | LBP | Interview | back pain is associated with TV watching time. | - | Moderate | 53 |
| A. N. Sjolie (2004) |
Cross-sectional Norwegian adolescents |
88 | 14.7 | television or computer use | LBP | Self-reported Questionnaire | LBP was associated with the use of television or computer (>15 hours/week). | Gender, distances to school and physical activity | High | 26 |
| V. Yip (2004)c |
Cohort Hong Kong nurses |
144 | 31.1 | Sedentary leisure time activity and prolong setting and standing | New LBP | Face-to-face interview | leisure time sedentariness was not associated with new low back pain. | - | High | 54 |
| S. Andrusaitis (2006)c |
Cross-sectional Brazilian truck drivers |
410 | 40.2 | Number of working hours | LBP | Questionnaire | Working hours were associated with LBP. | Weight, height, number of working hours, ethnic group, age and body mass index. | Moderate | 5 |
| V.M. Mattila (2007) |
Survey; Finland Military |
7040 | 19 | No leisure-time physical activity | lifetime LBP | Visit to a physician | use of smokeless tobacco (OR 1.4) was a risk factor for LBP. | Age | High | 27 |
| P. Spyropoulos (2007) |
Cross-sectional Greek office workers |
648 | 44.5 | Sitting time | Point, one year, two year, and lifetime LBP | Self-reported Questionnaire | Sitting time (>6 hours) is a significant determinant for lifetime LBP. | Gender, age, BMI, Body distance from computer screen, psychosocial factors |
High | 28 |
| J. Auvinen (2008) |
Cross-sectional Finland adolescents |
5999 | 16 | TV viewing, playing or working on a computer, reading books and other sitting activities | LBP | One-item question | Among girls, high amount of sitting associated with consultation or reporting LBP. | Smoking, levels of physical activity and BMI | High | 29 |
| A. Karahan (2008) |
Cross-sectional Turkish hospital staff |
1600 | 28 | Standing and sitting in a working day | LBP | Questionnaire | Overall standing time in a work day was significantly associated with LBP in univariate analysis. | Occupation, gender, working year, Smoking, exercise, Perceived stress level in work environment, performing risky activities as below | High | 30 |
| B. Skoffer (2008) |
Cross-sectional Danish schoolchildren |
546 | 15.5 | Standing talking during school break, hours of watching TV or video | LBP, function-limiting LBP | Self-reported Questionnaire | Homework and TV watching time were associated with LBP. | Age, gender, inactivity indicators, weight, BMI and smoking | Moderate | 31 |
| S. Ahn (2009) |
Cross-sectional Korean postmenopausal women |
143 | 59 | Being inactive during leisure time | LBP | One-item question | leisure time inactivity was a risk for back pain. | health factors related to BMI, parity, osteoarthritis, BMD, drinking coffee and inactivity |
High | 32 |
| F. Tissot (2009) |
Population survey Canadian worker |
7730 | 41.5 | Standing at work without freedom | LBP | Standardized Nordic questionnaire |
Standing at work is associated with low back pain. | - | High | 33 |
| W. Yao (2012)c |
Case-control Chinese adolescents |
1214 | 15.1 | Prolong TV watching, computer using, and homework time | LBP | - | There was no significant association between sedentary activity and LBP. | - | High | 55 |
| N. Aggarwal (2013)c |
Cross-sectional Indian undergraduate medical students |
160 | 20.6 | Regular watching TV, and working on PC/laptop | LBP | Questionnaire | No associations between watching television or computer use with LBP. | - | High | 62 |
| M. Mohseni Bandpei (2014) |
Cross-sectional Iranian teacher |
586 | 37.9 | Standing or sitting time, computer working hours | Lifetime LBP | Oswestry LBP and disability questionnaire | Greater risk of LBP was observed in participants with prolonged sitting and standing, higher computer working hours and correcting examination. | General health, years of teaching, do exercise, pain intensifiers, sex, age, BMI, and job satisfaction | High | 34 |
| P. Mikkonen (2015)c |
Cohort Finland Students |
1625 | 16 | working on a computer, watching television, reading books, and other sedentary activities |
Chronic LBP | Self-reported or consultation-reported | No association between the sedentary behavior and LBP | - | High | 66 |
| J. Fernandes (2015) |
Cross-sectional Brazilian schoolchildren |
1461 | 12.6 | Watching TV/ week | Chronic LBP | Nordic Questionnaire | Low back pain was associated with watching TV (>3 times/week and 3 hours/day) | Age, gender | High | 35 |
| G. Inoue (2015) |
Cross-sectional Japanese sitting worker |
1329 | 40 | Routine standing work | LBP | RDQ | standing was not a significant risk factor for LBP. | working status, height, age, gender, BMI, smoking habit, and frequency of exercise | High | 36 |
| N. Gupta (2015)c |
Cross-sectional Danish blue-collar workers |
201 | 44.7 | Total sitting time (hour per day) | Intensity of LBP | Standardized Nordic questionnaire | Positive association between total sitting time and high LBP intensity (OR = 1.43) was found. | Age, gender, smoking, BMI, occupational time, sitting time in the opposite domain | High | 63 |
| J. Stričević (2015) |
Cross-sectional Nursing personnel in Slovenia |
659 | - | Working with computer or watching TV ≥ 2 h per day |
LBP | Questionnaire | Work with the computer reduced the risk for LBP (OR = 0.6) | Preventive exercises, Duration of employment, Frequent manual lifting | Moderate | 37 |
| M. Dolphens (2016) |
Cross-sectional Belgian adolescents |
842 | 11.6 | screen time, homework time and reading outside of school. | LBP | Questionnaire | Sedentary behaviors were not associated with LBP. | - | High | 38 |
| S. Hussain (2016)c |
Cohort Australian adults |
5058 | - | Total time spent watching Television ≥ 2h/day | disability of LBP LBP intensity |
Self-administered Chronic Pain Grade Questionnaire | ≥ 2 hours/day TV watching was associated with greater prevalence of LBP in women | Age, smoking status, dietary index score, BMI, education, | High | 65 |
| M. Ardahan (2016) |
Cross-sectional Turkish computer-using office workers |
395 | 45 | Daily working hours at computer | LB disorder | Turkish-Cornell Musculoskeletal Discomfort Questionnaire | Using a computer (> 7 hours/day) was associated with LB disorder. | - | High | 39 |
| L. Lunde (2017)c |
Cohort Norwegian construction and healthcare workers |
124 | 42.2 | sitting and standing during work | LBP intensity | - | The duration of sitting during work and leisure time was associated with LBP intensity. | Age, gender, smoking, BMI, heavy lifting, and sitting or standing time | High | 56 |
| S. Şimşek (2017) |
Cross-sectional healthcare workers (Turkey) |
1682 | 37.9 | Prolong standing & siting at work & using computer for more than 4 hours |
Lifetime; Recent and previous year LBP |
SNMA Questionnaire Pain level with visual analogue scale |
Working for more than 4 hours (standing or sitting at desk) and using computer for more than 4 hours were associated with low back pain. | - | High | 49 |
| Y. Yabe (2017) |
Cross-sectional Japanese school-aged athletes |
6441 | 11 | Video playing and TV viewing time | LBP | Self-reported questionnaire | Long video playing time/day was associated with low back pain. | Gender, age, BMI, TV-viewing time per day, and video playing time per day | High | 40 |
| S. Ganesan (2017)c |
Cross-sectional Indian young adult |
1355 | 24.5 | Study time more than 5h/day | LBP score | Questionnaire | LBP is triggered by >5 hours studying. | - | Moderate | 57 |
| M. Balling (2017)c |
Cohort Danish adults |
76438 | 47.6 | Total sitting time 6h/day or more | LBP | National Patient Register | No statistically significant association between total sitting time and low back pain was found. | Sex, age, smoking, BMI and physical activity at work | High | 58 |
| S. Ye (2017)c |
Cross-sectional Chicness office workers |
417 | 29.1 | Computer use ≥8 hours/day | LBP | Oswestry Low Back Pain Disability Index | Computer use (>8 hours/day) was not associated with high LBP. | - | High | 64 |
| H. Yang (2018) |
Cross-sectional USA adult population |
122,337 | 51.5 | Leisure time physical activity |
Chronic LBP | Self-reported LBP | Higher prevalence of LBP among inactive people in leisure time. | Gender, age, ethnicity, socioeconomic status, and serious psychological distress | High | 41 |
| Sh. Sen Sribastav (2018) |
Cross-sectional; Patient with LBP (Chi na) |
1046 | 37.2 | Long time driving | Non-specific LBP and pain level | Self-assessment questionnaire | Smoking, long driving time, and higher BMI were associated with LBP pain. | Gender, age, BMI, smoking habits, duration of driving or riding, drinking habits | High | 42 |
| S. Park (2018) |
Cross-sectional General Korean population |
5364 | 65.4 | sitting time | Chronic LBP | Self-reported LBP | Sitting time more than 7 hours/day was notably associated with LBP. | Age, socioeconomic factors, sex, BMI, smoking history, alcohol consumption, and physical activity | High | 43 |
| M. Korshøj (2018)c |
Cross-sectional | 704 | 45 | Sitting at work | Intensity of LBP | Nordic Questionnaire | No significant associations were found between total duration and temporal patterns of sitting with LBP. | Interaction between sitting and BMI | High | 13 |
| A. Citko (2018) |
Survey Poland medical personnel |
609 | 41 | Sedentary lifestyle | Recurrent and chronic LBP | Nordic musculoskeletal questionnaire | Sedentary lifestyle associated with a 3.5-fold increase in the incidence of LBP. | - | High | 19 |
| S. Çelik (2018)c |
Cross-sectional Office worker |
528 | 38.6 | Time spent standing and continuously sitting in workplace | LBP | Questionnaire | There is no significant association time spent standing and sitting with risk of LBP. | - | High | 59 |
| R. Shiri (2018)c |
Cohort Finnish population |
3505 | - | Sitting hours/day | LBP | Questionnaire | No significant associations between sitting time/day and LBP for more than 7 or 30 days. | Age, sex | High | 67 |
| S. Kulandaivelan (2018) |
Cross-sectional HISAR urban population |
1540 | 48.2 | Long sitting or watching TV time (> 2h/day) | LBP | Modified Nordic musculoskeletal questionnaire | No statistically significant association between long sitting and sleeping time and LBP | - | High | 44 |
| C. Tavares (2018)c |
Cross-sectional Brazilian medical students |
629 | 23 | Sitting hours per day | LBP | Questionnaire | The number of sitting hours was not associated with LBP. | - | High | 60 |
| Q. Zhang (2019) |
Cross-sectional Emergency ambulance workers (driver). (China) |
1560 (543 drivers) |
38.4 | Sitting time | Chronic LBP | Nordic Musculoskeletal Questionnaire | BMI and sitting time were associated with chronic LBP study sample. | Age, BMI, sex, Psychosocial factors | High | 45 |
| B. Minghelli (2019) |
Cross-sectional Portuguese students |
304 | 13.7 | Sedentary habits (Watching television, Mobile phones use, Console/computer games) | Lifetime and 6- and 12-month LBP | Self-Questionnaire | Mobile use more than 10 hours/week is associated with LBP in adolescents. | Sex, sedentary habits, physical activity |
High | 46 |
| T. Bento (2019) |
Cross-sectional Brazilian students |
1628 | 15 | Daily use time of TV/day, cell phone, tablet more than 3 h | Chronic LBP | Nordic Questionnaire | Daily TV use, cell phone use and tablet use (>3 hours) were significantly associated with LBP. | Sex, TV watching hours, daily use time of cell-phone and tablet | High | 47 |
| H. Ayed (2019) |
Cross-sectional Tunisia schoolchildren |
1221 | 15.6 | Watching TV more than 12h/week and playing video game for more than 2h/week | LBP | Nordic Questionnaire | Playing videogames (≥2 hours/day), and watching TV (≥12 hours/week) were significant risk factors for LBP. | - | High | 20 |
| F. Hanna (2019) |
Cross-sectional Qatari University Employees |
479 | - | Prolong sitting hour | LBP | ALBPSQ | Too much sitting was significantly associated with LBP or UBP | Age, gender, and profession. | High | 48 |
| D. Schwertner (2019)c |
Cross-sectional Brazilian young |
330 | 16 | TV watching time and computer use | LBP | Oliveira Questionnaire on Low Back Pain in Youths | No association of LBP with sedentary lifestyle was found. | Sex, age and BMI | High | 61 |
| C. Bontrup (2019)c |
Cross-sectional Swedish call-center employees |
70 | 43 | Occupational sitting habits | LBP | CPG questionnaire and BPI | Small association between general sitting behavior and chronic LBP was found. | - | High | 1 |
Abbreviations: STROBE; STrengthening the Reporting of OBservational studies in Epidemiology; BMI, body mass index; BMD, bone mass density; LBP, low back pain; RDQ, Roland-Morris Disability Questionnaire; CPG, Chronic Pain Grade;
BPI, Brief Pain Inventory; ALBPSQ, Acute Low Back Pain Screening Questionnaire.
aArranged chronologically.
b Mean STROBE score ≥ 16.5 (from two reviewers) was considered as high quality and 11 to 16.5 was considered as moderate quality.
c Not included in metanalyses.
Assessment of study quality
Mean STROBE scores from two reviewers revealed 42 studies conducted in high quality and 7 studies in a moderate quality. We used all these studies in data synthesis or meta-analysis since, concerning moderate quality studies, none of those had small sample sizes or inaccurate estimates. Besides, in the sensitivity analyses, all of the studies were excluded, and the effect sizes were estimated again to ensure the accuracy of data. The quality of each selected study is presented in Table 1. More details about the assessment of study qualities are presented in Appendix 2.
Main findings of the meta-analysis
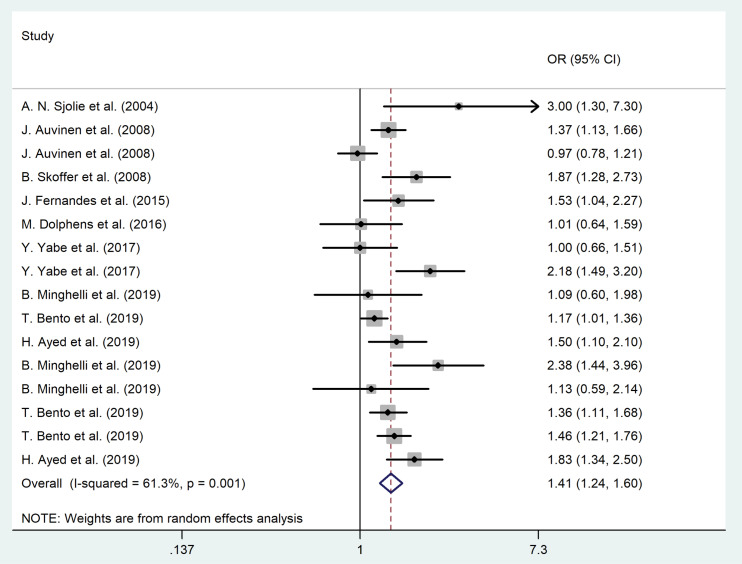
The forest plot for the association between sedentary behaviors and LBP among children and adolescents is shown in Figure 2. The pooled odds ratio (based on cross-sectional studies) illustrated that sedentary lifestyle was a remarkable risk factor for LBP among children and adolescents (OR = 1.41, 95% CI = 1.24–1.60, P = 0.002; I2 = 66.5%, P = 0.001). No evidence of publication bias was noted (for all studies, P value of Egger’s test = 0.40, and P value of Begg’s tests = 0.19).
Figure 2.
The association between sedentary lifestyle and LBP among children and adolescents.
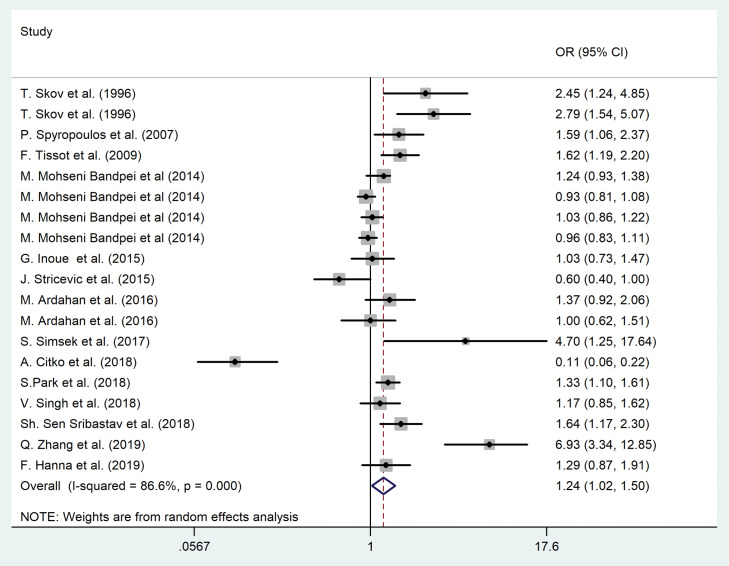
The forest plot for the correlation of sedentary behaviors and LBP among the adult population is shown in Figure 3. The pooled odds ratio (based on cross-sectional studies) illustrated that the sedentary lifestyle was a considerable risk factor for LBP among the adult population (OR = 1.24, 95% CI = 1.02-1.50, P <0.001; I2 = 84.8%, P < 0.001). No evidence of publication bias was noted (for all studies, P value of Egger’s test = 0.91, and P value of Begg’s tests = 0.08).
Figure 3.
The association between sedentary lifestyle and LBP among adult population.
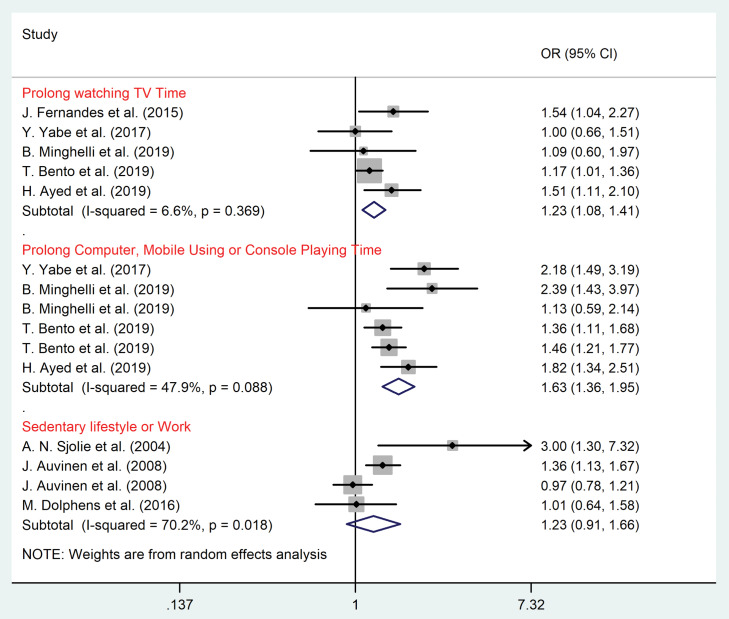
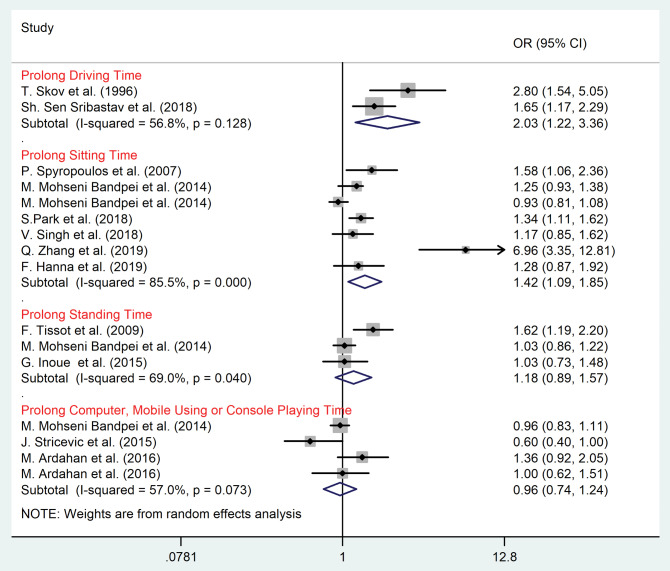
Subgroup meta-analysis according to the type of sedentary behaviors
Results of subgroup analysis based on the type of sedentary behaviors among children/adolescents and adult populations are shown in Figure 4 and Figure 5, respectively. Among children and adolescents prolonged watching TV (OR = 1.23, 95% CI = 1.08–1.41, P = 0.003; I2 = 6.6%, P = 0.37), computer/mobile using and console playing time (OR = 1.63, 95% CI = 1.36–1.95, P = 0.001; I2 = 47.9%, P = 0.09) were significant risk factors for LBP (P value < 0.05) (Figure 4).
Figure 4.
Subgroup analysis according to sedentary lifestyle among children and adolescents.
Figure 5.
Subgroup analysis according to sedentary lifestyle among adult population.
Among adult population prolonged sitting time (OR = 1.42, 95% CI = 1.09–1.85, P = 0.03; I2 = 85.5%, P < 0.001), and driving time (OR = 2.03, 95% CI = 1.22–3.36, P <0.001; I2 = 56.8%, P = 0.13) were the significant risk factors for LBP (Figure 5).
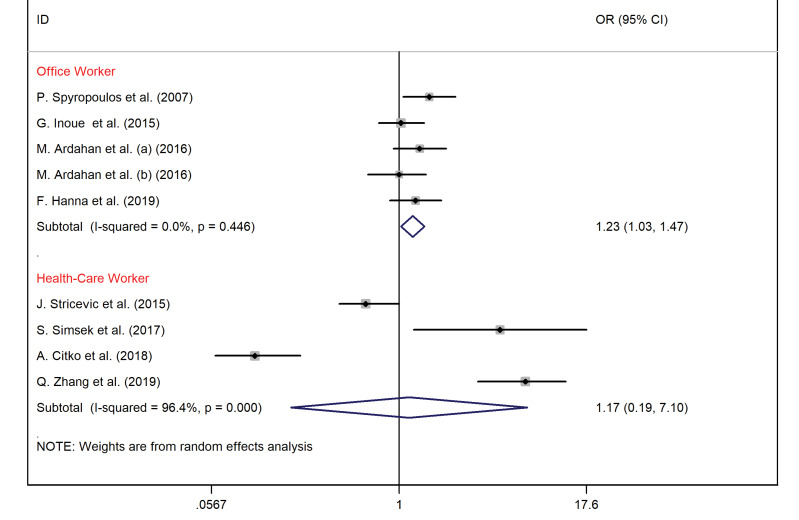
Subgroup meta-analysis according to occupation type
Among office workers, sedentary lifestyle was an essential risk for LBP (OR = 1.23, 95% CI = 1.03–1.47, I2 = 0%) (Figure 6).
Figure 6.
The association between the sedentary lifestyle and LBP according to occupation type.
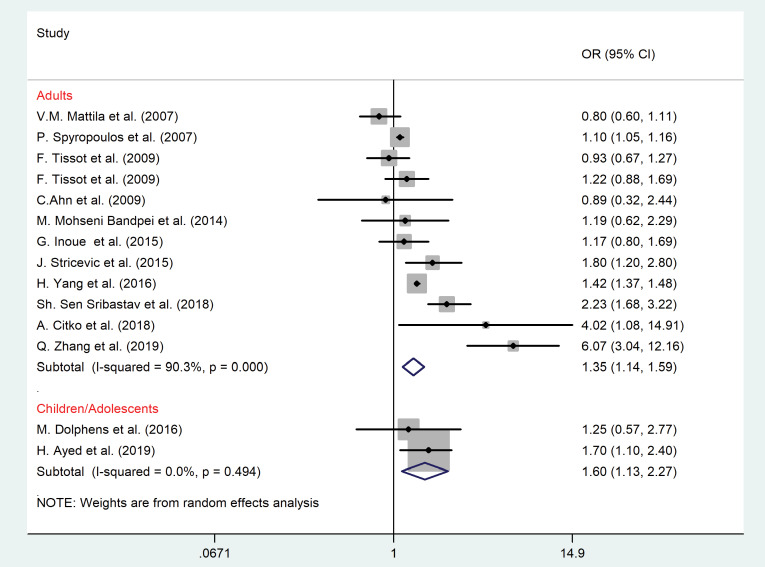
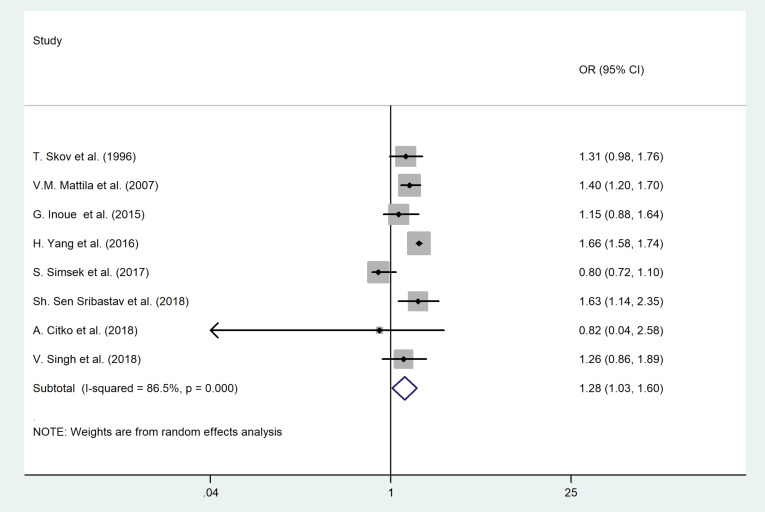
Body mass index and smoking status
As shown in Figures 7 and 8, overweight or obesity (OR = 1.35, 95% CI = 1.14–1.59, P = 0.02; I2 = 90.3%, P < 0.001) and smoking (OR = 1.28, 95% CI = 1.03–1.60, P = 0.01; I2 = 86.5%, P < 0.001) were the significant risk factors for LBP among adult population. In children, excess wight (OR = 1.60, 95% CI = 1.13–2.27, P = 0.021; I2 = 0.00, P = 0.49) was associated with LBP as well.
Figure 7.
The association between Body Mass Index (BMI) and LBP according to the age group.
Figure 8.
The association between smoking and LBP among adult population.
No evidence of publication bias for BMI was found (P value of Egger’s test = 0.41, and P value of Begg’s tests = 0.68).
We found publication bias for smoking (P value of Egger’s test = 0.71, and P value of Begg’s tests = 0.03). Therefore, we conducted the Trim and Fill method to explore the effect of publication bias on the meta-analysis results. However, no significant change in the pooled OR was noted.
Leisure time inactivity
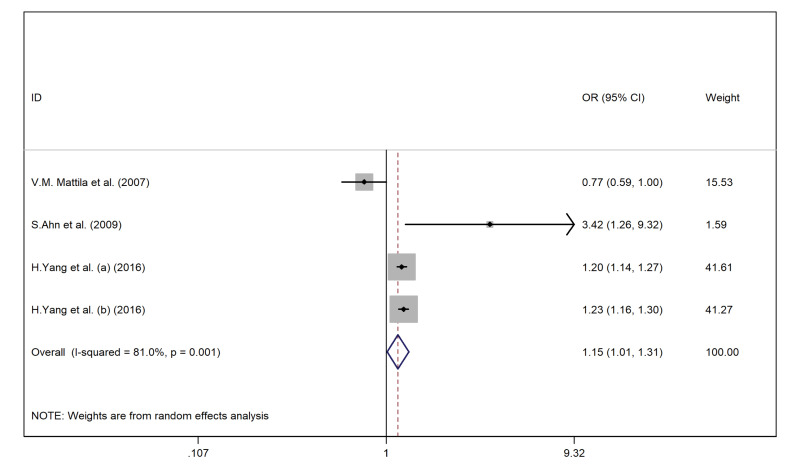
As shown in Figure 9, leisure time inactivity was an essential risk factor for LBP (OR = 1.28, 95% CI = 0.92–1.77, I2 = 81%).
Figure 9.
The association between leisure-time inactivity and LBP.
Sensitivity analysis
We found no significant changes between the before-after sensitivity pooled OR for the association between sedentary lifestyle and LBP among children and adolescents. However, results showed a remarkable effect between before-after sensitivity pooled OR for the correlation between the sedentary lifestyle and LBP among adult population after excluding Zhang et al45 study (OR = 1.16, 95% CI = 0.99–1.36).
Also, results showed significant changes between the before-after sensitivity pooled OR for the association between smoking and LBP among the adult population after excluding Mattila et al27 study and Sribastav et al42 study (OR = 1.26, 95% CI = 0.97–1.56).
Besides, no remarkable changes between the before-after sensitivity pooled OR for the association between the sedentary lifestyle and LBP among healthcare workers and office workers were noted.
Overview of studies not included in the meta-analysis
Sedentary behavior at work with non-neutral posture correlates with LBP among workers.50 Bending postures but not sedentary leisure time itself have been proposed to be associated with new LBP in nurses.54 However, three studies stated no association between sedentary habits and LBP.55,61,62
Sitting behavior was associated with chronic LBP and functional disfunction among 70 call center employees.1 Among a population of truck drivers, the only factor correlated to LBP was the number of working hours.5 Also, the daily number of studying hours (>5 hours) precipitated the LBP in young adults.57 On the other hand, sitting time was not considered a risk factor for LBP in 3 studies.58-60
LBP was reported more in school children playing videogames >2 hours/day and not for television watchers in the Gunzburg et al study.51 Similar to this finding, a cohort study by Croft et al reported that watching television > 3 hours/day did not enhanced the risk of recurrent LBP in the UK general population.52 Similarly, in a cohort study among Finnish children, the sedentary class boys (derived from latent class analysis) did not presented with increased risk for reporting LBP or consultation for LBP.66 More conflicting results have been reported in Shehab et al study in which the LBP correlated with female gender and TV watching time in children and adolescents.53
In Hussain et al. study, TV watching time in women was associated with greater LBP disability. The authors suggested that targeting the time spent TV watching would be effective in reducing LBP disability in adults at the level of community.65 A retrospective study revealed that sedentary work was associated with LBP in both genders after a 24 year period.68 Also, in Shiri et al study, lifestyle including abdominal obesity and smoking increased the risk of LBP. Reduced risk of LBP was obtained via walking and cycling to work (OR = 0.75).67
Regarding the intensity of LBP, Gupta et al showed a notable association between total sitting time and high LBP intensity among 201 participants (OR = 1.43).63 The duration of sitting time both in work and leisure time was associated with LBP intensity in another study.56 Such a relationship was investigated in Ye et al study among 417 office workers. In contrast, in this study computer use ≥ 8 hours/day was not associated with high intensity LBP.64 In the Korshøj et al study, the sitting pattern was not correlated with the intensity of LBP.13 Moreover, in Hussain et al. cohort study on 5058 individuals, no significant associations between < 2.5 hours/week physical activity and ≥ 2 hours/day TV watching, with LBP intensity at follow-up were reported.65 Thus, further research is necessary to better elucidate the effect of sedentariness on the risk of high-intensity LBP.
Coffee drinking and LBP
In a survey, Citko et al showed that coffee drinking, 6 cups per day or more, increased the risk of non-specific LBP recurrence by 16 times compared to smaller amounts in medical personnel.19 Also, a survey of 134 postmenopausal women reported a significant association of drinking coffee (yes/no) with LBP (OR = 3.1).32 However, in the Aggarwal study, regular or occasional coffee intake was not associated with LBP among undergraduate students.62 The absence of association was found in the Ganesan et al study as well.57 Abovementioned studies were all cross-sectional in their design. The effect of coffee on back pain may be dose-dependent or through indirect mechanisms such as via affecting bone health.32 To better clarify this issue, further exploration is necessary, with a standard measurement of coffee/caffeine intake, especially in longitudinal research.
Discussion
Our study explored the association of sedentary behavior and LBP. The results demonstrate the role of sedentary behavior as a risk factor for the increased incidence of LBP, both in adults and children (OR = 1.24 and 1.41, respectively).
A similar systematic review to ours, published in 2009, was performed on 15 observational studies up to 2006 and revealed that there was no correlation between sedentary behavior both in work or leisure time with LBP.12 However, given that more articles have been published in recent years, we were able to obtain the pooled OR for the abovementioned association for adults and children separately. In addition, in the previous review, only prolonged sitting was considered as sedentary behavior, whereas we conducted subgroup meta-analyses according to the type of sedentary behaviors and occupation type.
The time spent in sedentary lifestyle has become a significant health concern. The sedentary behavior prevalence is high, even in developed countries.69 One study showed that children spend 51.4% of their working time in sedentary lifestyle. These common behaviors may be established in childhood and track through later life.70 Sedentary behavior is linked to various musculoskeletal pain conditions.71
Despite the controversies observed in included articles in our systematic review, the pooled effects sizes obtained from meta-analysis of other studies revealed that prolonged sitting time and prolonged driving time are significant risk factors of LBP among adults (OR = 1.42, 2.03 respectively). However, prolonged screen time and standing time were not associated with LBP in adults. Also, among children, prolonged TV watching (OR = 1.23), and computer/mobile using or console playing time (OR = 1.63) were associated with LBP. A meta-analysis study indicated that excess weight is a risk factor for LBP in both genders.72 Another study revealed that smokers have a higher incidence of LBP compared to nonsmokers; these associations were fairly modest (OR = 1.32 for former and OR = 1.31 for the current smokers). Of note, the association between current smoking and LBP was more remarkable in adolescents than in adults (OR = 1.82 vs. 1.16).73 Similarly, we found that increased body mass index in adults and children and smoking in adults, are risk factors for LBP (OR = 1.35, 1.60 and 1.28 respectively), in whom the sedentary behavior has been investigated. These finding suggest that smoking and body mass index interact with sitting and LBP.13 In addition, to avoid heterogeneity, we identified two main occupation categories as healthcare workers and office workers among the included studies. We found that sedentary behavior is a risk for LBP in office workers (OR = 1.23). In previous research, prolonged sitting and computer use were contributed to LBP in office workers.48
As for underlying pathways, decreased level of water supply to the vertebral disc, which in turn leads to degenerative changes and disk herniations, reduced strength and muscular power, and developing hyperlordosis are some proposed pathophysiological mechanisms for sedentary behavior contributing to LBP.19 Specifically, prolonged sitting is contributed to decreased postural change, as well as muscle strength and disk degenerations.13 Obesity or overweight causes overload on the spinal tissues and contributes to disk herniation and LBP. On the other hand, obesity is associated with other disorders such as diabetes and hyperlipidemia that are also correlated to LBP by different mechanisms.74 Smoking can alter the blood supply of vertebral disks via the processes of vasoconstriction and atherosclerosis. Impaired perfusion of vertebral structures leads to degenerative changes and LBP. Besides, smoking is a risk factor of osteoporosis or is a behavior seen only the people with massive physical works; thus, it has direct and indirect effects on the LBP.73 Moreover, coffee consumption is proposed to be associated with flushing magnesium from the body and increased painful contractions of paraspinal muscles.75
The data heterogeneity of included studies in our review can be explained in part by variations in study designs, study population, sample sizes, occupation type, gender, race, and age range. However, beyond those, some factors seem to be more important, as follows.
First, the definition of LBP and its measurement scales were considerably different in the studies. For instance, experiencing LBP during the current week for at least 48 hours via the Roland-Morris Disability Questionnaire was measured in the Inoue et al. study.36 In the Ben Ayed et al study, however, participants were asked about discomfort and pain in the low back area during the prior month.20 Some authors, though, defined recurrent LBP as pain episodes of at least three times in the last 12 months and chronic LBP as the pain persisted for at least 12 weeks based on the Nordic Musculoskeletal Questionnaire.19 Many studies, however, did not differentiate chronic LBP from acute LBP.
Second, sedentary behavior has diverse definitions and types in various studies. While some authors explored the association of sitting time merely with LBP,28 some others have turned their attention to the screen time or a combination of both.49 In some other studies, sedentary habits were not categorized into any different types.68 In addition, the common measurement tool for sedentary behavior is subjective self-reported questionnaires, which, in turn, are prone to information bias from participants. However, a few studies used objective-based tools such as an accelerometer or textile pressure mat to estimate the sitting time.1,63 Thus, to make accurate estimations, we performed subgroup analyses for specified sedentary behavior in the papers, both for adults and children separately. For future research, focusing on objective-based measurement of sedentary behaviors is highly suggested.
The third is that LBP, as a complex multifactorial disease, is affected by psychological conditions and the tasks performed in non-sitting positions at work or leisure time. Therefore, just a part of the variation in LBP is because of sedentary-related risk factors.33,48 Thus, the variety in the combination of these factors in different participants seems to be accounted for the data heterogeneity.
Strengths of the study
We applied different statistical methods to obtain the desired associations for adults and children separately, as the risk factors of LBP may be different in these age groups. We found new data and demonstrated significant but moderate associations between different sedentary behaviors and LBP. Regarding the large number of studies conducted in this field (which were retained in the meta-analysis), the results can be well generalized to different communities.
Health implications
A recent meta-analysis evaluating the lifestyle interventions to reduce sedentary behavior among five categories of population with a clinical condition (including musculoskeletal conditions) demonstrated that after multicomponent interventions, individuals with different medical conditions successfully reduced their sedentary behavior (by 64 minutes/day). The interventions consisted of the use of technologies, social facilitation, motivational counselling and self-monitoring.76 As LBP is a complex disorder, health education to reduce the prevalence or occurrence of LBP should be address the risk factors as much as possible including sedentary behavior.
Conclusion
In brief, according to our meta-analysis, sufficient evidence exists from recent studies that indicate the association of different types of sedentary behavior with the occurrence or recurrence of LBP both in adults and children. Given the increasing trend of sedentary behavior worldwide, especially in the era of the COVID-19 pandemic, meticulous and robust preventive strategies are suggested to be applied to avoid the establishment of sedentariness early in childhood and to prevent its’ musculoskeletal consequences such as LBP.
Acknowledgments
We want to thank our colleagues in Isfahan University of medical Sciences who helped us working on this project.
Funding
This study was funded and supported by Isfahan University of Medical Sciences, Isfahan, Iran.
Competing interests
None to declare.
Ethical approval
The protocol of the current review has been qualified in the Isfahan University of Medical Sciences, Isfahan, Iran (code: 199298) and has been approved in the National regulatory ethics committee (IR.MUI.MED.REC.1399.507). The study protocol and its details have been registered in the international prospective register of systematic reviews, PROSPERO with identification code: CRD42020187175.
Authors’ contributions
SBM contributed to the conception of the work, data search, screening of records, study quality assessment, data extraction, manuscript preparation, manuscript revision, final approval of the manuscript, and agreed to be accountable for all aspects of the work. RR contributed to the screening of records, study quality assessment, data extraction, statistical analysis, interpretation of data, manuscript preparation, manuscript revision, final approval of the manuscript, and agreed to be accountable for all aspects of the work. BV contributed to study quality assessment, manuscript preparation, manuscript revision, final approval of the manuscript, and agreed to be accountable for all aspects of the work. RK contributed to the conception of the work, manuscript preparation, manuscript revision, final approval of the manuscript, and agreed to be accountable for all aspects of the work. All authors approved the final version of manuscript and took the responsibility for all aspects of the work.
Appendix 1
Search string for PubMed
((((«Sedentary Behavior»[Mesh] OR «Screen Time»[Mesh]) OR «Coffee»[Mesh]) OR «Tea»[Mesh]) OR ((«tea»[MeSH Terms] OR «tea»[All Fields]) OR («coffee»[MeSH Terms] OR «coffee»[All Fields]) OR («caffeine»[MeSH Terms] OR «caffeine»[All Fields]) OR «sedentary lifestyle»[All Fields] OR «physical inactivity»[All Fields] OR «sedentary behavior*»[All Fields] OR «screen time»[All Fields] OR «sitting time»[All Fields] OR sedentary[All Fields] OR «watching TV»[All Fields] OR «playing video game*»[All Fields] OR ((«work»[MeSH Terms] OR «work»[All Fields] OR «working»[All Fields]) AND («computers»[MeSH Terms] OR «computers»[All Fields] OR «computer»[All Fields])))) AND («Low Back Pain»[Mesh] OR («low back pain»[All Fields] OR «back pain»[All Fields] OR «spinal pain»[All Fields] OR «spine pain»[All Fields] OR («low back pain»[MeSH Terms] OR («low»[All Fields] AND «back»[All Fields] AND «pain»[All Fields]) OR «low back pain»[All Fields] OR «lumbago»[All Fields]) OR («back pain»[MeSH Terms] OR («back»[All Fields] AND «pain»[All Fields]) OR «back pain»[All Fields] OR «backache»[All Fields]) OR «lumbar spondylosis»[All Fields] OR «postural low back pain»[All Fields] OR «mechanical low back pain»[All Fields]))
548 Records [with these filters: full text, humans, English]
Search string for Web of Science
TOPIC: (tea OR coffee OR caffeine OR “sedentary lifestyle” OR “physical inactivity” OR “sedentary behavior*” OR “screen time” OR “sitting time” OR sedentary OR “watching TV” OR “playing video game*” OR “working on a computer”) AND TOPIC: (“low back pain” OR “back pain” OR “spinal pain” OR “spine pain” OR lumbago OR backache OR “lumbar spondylosis” OR “postural low back pain” OR “mechanical low back pain”)
492 Records [with these filters: article, English]
Search string for Scopus
( ALL ( tea OR coffee OR caffeine OR «sedentary lifestyle» OR «physical inactivity» OR «sedentary behavior*» OR «screen time» OR «sitting time» OR sedentary OR «watching TV» OR «playing video game*» OR «working on a computer» ) AND TITLE-ABS-KEY ( «low back pain» OR «back pain» OR «spinal pain» OR «spine pain» OR lumbago OR backache OR «lumbar spondylosis» OR «postural low back pain» OR «mechanical low back pain» ) ) AND ( LIMIT-TO ( DOCTYPE, «ar» ) ) AND ( LIMIT-TO ( LANGUAGE, «English» ) ) AND ( LIMIT-TO ( SRCTYPE, «j» ) )
1744 Records [with these filters: article, journals, English]
Search string for Embase
(tea OR coffee OR caffeine OR ‹sedentary lifestyle› OR ‹physical inactivity› OR ‹sedentary behavior*› OR ‹screen time› OR ‹sitting time› OR sedentary OR ‹watching tv› OR ‹playing video game*› OR ‹working on a computer›) AND (‹low back pain› OR ‹back pain› OR ‹spinal pain› OR ‹spine pain› OR lumbago OR backache OR ‹lumbar spondylosis› OR ‹postural low back pain› OR ‹mechanical low back pain›)
622 Records [with this filter: article]
Appendix 2
Appendix 2. Quality assessment of included articles using the STROBE checklist .
|
Author;
(year) |
STROBE score (Reviewer 1: S.B.M) | STROBE score (Reviewer 2: B.V) | Mean STROBE score | Study quality 1 |
| A. Burdorf (1993) |
16 | 16 | 16 | Moderate |
| T. Skov (1996) |
16 | 16 | 16 | Moderate |
| R. Gunzburg (1999) |
17 | 16 | 16.5 | High |
| P. R.Craft (1999) |
21 | 18 | 19.5 | High |
| C. Thorbjornsson (1999) |
19 | 17 | 18 | High |
| D. K. Shehab (2003) |
15 | 12 | 13.5 | Moderate |
| A. N.Sjolie (2004) |
17 | 16 | 16.5 | High |
| V. Yip (2004) |
18 | 19 | 18.5 | High |
| S. Andrusaitis (2006) |
17 | 14 | 15.5 | Moderate |
| V.M. Mattila (2007) |
19 | 17 | 18 | High |
| P. Spyropoulos (2007) |
19 | 19 | 19 | High |
| J. Auvinen (2008) |
21 | 19 | 20 | High |
| A. Karahan (2008) |
20 | 20 | 20 | High |
| B. Skoffer (2008) |
17 | 15 | 16 | Moderate |
| S. Ahn (2009) |
19 | 20 | 19.5 | High |
| F.Tissot (2009) |
19 | 20 | 19.5 | High |
| W. Yao (2012) |
20 | 19 | 19.5 | High |
| N. Aggarwal (2013) |
19 | 18 | 18.5 | High |
| M. Mohseni Bandpei (2014) |
19 | 18 | 18.5 | High |
| P.Mikkonen (2015) |
20 | 17 | 18.5 | High |
| J. Fernandes (2015) |
18 | 15 | 16.5 | High |
| G. Inoue (2015) |
17 | 17 | 17 | High |
| N. Gupta (2015) |
22 | 20 | 21 | High |
| J. Stricevic (2015) |
15 | 14 | 14.5 | Moderate |
| M. Dolphens (2016) |
19 | 18 | 18.5 | High |
| S. Hussain (2016) |
21 | 19 | 20 | High |
| M. Ardahan (2016) |
19 | 15 | 17 | High |
| L. Lunde (2017) |
20 | 18 | 19 | High |
| S. ŞIMŞEK (2017) |
17 | 19 | 18 | High |
| Y. Yabe (2017) |
21 | 18 | 19.5 | High |
| S. Ganesan (2017) |
15 | 17 | 16 | Moderate |
| M. Balling (2017) |
21 | 20 | 20.5 | High |
| S.Ye (2017) |
17 | 18 | 17.5 | High |
| H. Yang (2016) |
17 | 18 | 17.5 | High |
| Sh. Sen Sribastav (2018) |
18 | 19 | 18.5 | High |
| S.Park (2018) |
21 | 17 | 19 | High |
| M. Korshøj (2018) |
21 | 20 | 20.5 | High |
| A. Citko (2018) |
18 | 17 | 17.5 | High |
| S. Celik (2018) |
16 | 18 | 17 | High |
| R. Shiri (2018) |
21 | 18 | 19.5 | High |
| S. Kulandaivelan (2018) |
17 | 17 | 17 | High |
| C. Tavares (2018) |
18 | 16 | 17 | High |
| Q. Zhang (2019) |
18 | 18 | 18 | High |
| B. Minghelli (2019) |
15 | 18 | 16.5 | High |
| T. Bento (2019) |
20 | 20 | 20 | High |
| H. Ayed (2019) |
20 | 20 | 20 | High |
| F. Hanna (2019) |
18 | 19 | 18.5 | High |
| D. Schwertner (2019) |
18 | 18 | 18 | High |
| C. Bontrup (2019) |
16 | 18 | 17 | High |
STROBE: STrengthening the Reporting of OBservational studies in Epidemiology.
1: Mean STROBE score ≥ 16.5 (from two reviewers) was considered as high quality and 11 to 16.5 was considered as moderate quality.
References
- 1.Bontrup C, Taylor WR, Fliesser M, Visscher R, Green T, Wippert PM. et al. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl Ergon. 2019;81:102894. doi: 10.1016/j.apergo.2019.102894. [DOI] [PubMed] [Google Scholar]
- 2.Amorim AB, Levy GM, Pérez-Riquelme F, Simic M, Pappas E, Dario AB. et al. Does sedentary behavior increase the risk of low back pain? a population-based co-twin study of Spanish twins. Spine J. 2017;17(7):933–42. doi: 10.1016/j.spinee.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Jonsdottir S, Ahmed H, Tómasson K, Carter B. Factors associated with chronic and acute back pain in Wales, a cross-sectional study. BMC Musculoskelet Disord. 2019;20(1):215. doi: 10.1186/s12891-019-2477-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lötters F, Burdorf A. Prognostic factors for duration of sickness absence due to musculoskeletal disorders. Clin J Pain. 2006;22(2):212–21. doi: 10.1097/01.ajp.0000154047.30155.72. [DOI] [PubMed] [Google Scholar]
- 5.Andrusaitis SF, Oliveira RP, Barros Filho TE. Study of the prevalence and risk factors for low back pain in truck drivers in the state of São Paulo, Brazil. Clinics (Sao Paulo) 2006;61(6):503–10. doi: 10.1590/s1807-59322006000600003. [DOI] [PubMed] [Google Scholar]
- 6.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–47. doi: 10.1016/s0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 7.Daraiseh NM, Cronin SN, Davis LS, Shell RL, Karwowski W. Low back symptoms among hospital nurses, associations to individual factors and pain in multiple body regions. Int J Ind Ergon. 2010;40(1):19–24. doi: 10.1016/j.ergon.2009.11.004. [DOI] [Google Scholar]
- 8.Booth FW, Lees SJ. Fundamental questions about genes, inactivity, and chronic diseases. Physiol Genomics. 2007;28(2):146–57. doi: 10.1152/physiolgenomics.00174.2006. [DOI] [PubMed] [Google Scholar]
- 9.Panahi S, Tremblay A. Sedentariness and health: is sedentary behavior more than just physical inactivity? Front Public Health. 2018;6:258. doi: 10.3389/fpubh.2018.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chau JY, Grunseit AC, Chey T, Stamatakis E, Brown WJ, Matthews CE. et al. Daily sitting time and all-cause mortality: a meta-analysis. PLoS One. 2013;8(11):e80000. doi: 10.1371/journal.pone.0080000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bjørk Petersen C, Bauman A, Grønbæk M, Wulff Helge J, Thygesen LC, Tolstrup JS. Total sitting time and risk of myocardial infarction, coronary heart disease and all-cause mortality in a prospective cohort of Danish adults. Int J Behav Nutr Phys Act. 2014;11:13. doi: 10.1186/1479-5868-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen SM, Liu MF, Cook J, Bass S, Lo SK. Sedentary lifestyle as a risk factor for low back pain: a systematic review. Int Arch Occup Environ Health. 2009;82(7):797–806. doi: 10.1007/s00420-009-0410-0. [DOI] [PubMed] [Google Scholar]
- 13.Korshøj M, Hallman DM, Mathiassen SE, Aadahl M, Holtermann A, Jørgensen MB. Is objectively measured sitting at work associated with low-back pain? a cross sectional study in the DPhacto cohort. Scand J Work Environ Health. 2018;44(1):96–105. doi: 10.5271/sjweh.3680. [DOI] [PubMed] [Google Scholar]
- 14.Lis AM, Black KM, Korn H, Nordin M. Association between sitting and occupational LBP. Eur Spine J. 2007;16(2):283–98. doi: 10.1007/s00586-006-0143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bakker EW, Verhagen AP, van Trijffel E, Lucas C, Koes BW. Spinal mechanical load as a risk factor for low back pain: a systematic review of prospective cohort studies. Spine (Phila Pa 1976) 2009;34(8):E281–93. doi: 10.1097/BRS.0b013e318195b257. [DOI] [PubMed] [Google Scholar]
- 16.Hartvigsen J, Leboeuf-Yde C, Lings S, Corder EH. Is sitting-while-at-work associated with low back pain? a systematic, critical literature review. Scand J Public Health. 2000;28(3):230–9. [PubMed] [Google Scholar]
- 17.Diallo SYK, Mweu MM, Mbuya SO, Mwanthi MA. Prevalence and risk factors for low back pain among university teaching staff in Nairobi, Kenya: a cross-sectional study. F1000Res. 2019;8:808. doi: 10.12688/f1000research.19384.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Korshøj M, Jørgensen MB, Hallman DM, Lagersted-Olsen J, Holtermann A, Gupta N. Prolonged sitting at work is associated with a favorable time course of low-back pain among blue-collar workers: a prospective study in the DPhacto cohort. Scand J Work Environ Health. 2018;44(5):530–8. doi: 10.5271/sjweh.3726. [DOI] [PubMed] [Google Scholar]
- 19.Citko A, Górski S, Marcinowicz L, Górska A. Sedentary lifestyle and nonspecific low back pain in medical personnel in North-East Poland. Biomed Res Int. 2018;2018:1965807. doi: 10.1155/2018/1965807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ben Ayed H, Yaich S, Trigui M, Ben Hmida M, Ben Jemaa M, Ammar A. et al. Prevalence, risk factors and outcomes of neck, shoulders and low-back pain in secondary-school children. J Res Health Sci. 2019;19(1):e00440. [PMC free article] [PubMed] [Google Scholar]
- 21.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 22.Baradaran Mahdavi S, Daniali SS, Farajzadegan Z, Bahreynian M, Riahi R, Kelishadi R. Association between maternal smoking and child bone mineral density: a systematic review and meta-analysis. Environ Sci Pollut Res Int. 2020;27(19):23538–49. doi: 10.1007/s11356-020-08740-1. [DOI] [PubMed] [Google Scholar]
- 23. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1. 0 (Updated March 2011). The Cochrane Collaboration; 2011. Available from: https://handbook-5-1.cochrane.org/.
- 24.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Skov T, Borg V, Orhede E. Psychosocial and physical risk factors for musculoskeletal disorders of the neck, shoulders, and lower back in salespeople. Occup Environ Med. 1996;53(5):351–6. doi: 10.1136/oem.53.5.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sjolie AN. Associations between activities and low back pain in adolescents. Scand J Med Sci Sports. 2004;14(6):352–9. doi: 10.1111/j.1600-0838.2004.377.x. [DOI] [PubMed] [Google Scholar]
- 27.Mattila VM, Sahi T, Jormanainen V, Pihlajamäki H. Low back pain and its risk indicators: a survey of 7,040 Finnish male conscripts. Eur Spine J. 2008;17(1):64–9. doi: 10.1007/s00586-007-0493-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spyropoulos P, Papathanasiou G, Georgoudis G, Chronopoulos E, Koutis H, Koumoutsou F. Prevalence of low back pain in Greek public office workers. Pain Physician. 2007;10(5):651–9. [PubMed] [Google Scholar]
- 29.Auvinen J, Tammelin T, Taimela S, Zitting P, Karppinen J. Associations of physical activity and inactivity with low back pain in adolescents. Scand J Med Sci Sports. 2008;18(2):188–94. doi: 10.1111/j.1600-0838.2007.00672.x. [DOI] [PubMed] [Google Scholar]
- 30.Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 2009;65(3):516–24. doi: 10.1111/j.1365-2648.2008.04905.x. [DOI] [PubMed] [Google Scholar]
- 31.Skoffer B, Foldspang A. Physical activity and low-back pain in schoolchildren. Eur Spine J. 2008;17(3):373–9. doi: 10.1007/s00586-007-0583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ahn S, Song R. Bone mineral density and perceived menopausal symptoms: factors influencing low back pain in postmenopausal women. J Adv Nurs. 2009;65(6):1228–36. doi: 10.1111/j.1365-2648.2009.04983.x. [DOI] [PubMed] [Google Scholar]
- 33.Tissot F, Messing K, Stock S. Studying the relationship between low back pain and working postures among those who stand and those who sit most of the working day. Ergonomics. 2009;52(11):1402–18. doi: 10.1080/00140130903141204. [DOI] [PubMed] [Google Scholar]
- 34.Mohseni Bandpei MA, Ehsani F, Behtash H, Ghanipour M. Occupational low back pain in primary and high school teachers: prevalence and associated factors. J Manipulative Physiol Ther. 2014;37(9):702–8. doi: 10.1016/j.jmpt.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 35.Fernandes JA, Dos Santos Genebra CV, Maciel NM, Fiorelli A, de Conti MH, De Vitta A. Low back pain in schoolchildren: a cross-sectional study in a western city of São Paulo State, Brazil. Acta Ortop Bras. 2015;23(5):235–8. doi: 10.1590/1413-785220152305148842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inoue G, Miyagi M, Uchida K, Ishikawa T, Kamoda H, Eguchi Y. et al. The prevalence and characteristics of low back pain among sitting workers in a Japanese manufacturing company. J Orthop Sci. 2015;20(1):23–30. doi: 10.1007/s00776-014-0644-x. [DOI] [PubMed] [Google Scholar]
- 37.Stričević J, Papež BJ. Non-specific low back pain: occupational or lifestyle consequences? Wien Klin Wochenschr. 2015;127 Suppl 5:S277–81. doi: 10.1007/s00508-015-0770-2. [DOI] [PubMed] [Google Scholar]
- 38.Dolphens M, Vansteelandt S, Cagnie B, Vleeming A, Nijs J, Vanderstraeten G. et al. Multivariable modeling of factors associated with spinal pain in young adolescence. Eur Spine J. 2016;25(9):2809–21. doi: 10.1007/s00586-016-4629-7. [DOI] [PubMed] [Google Scholar]
- 39.Ardahan M, Simsek H. Analyzing musculoskeletal system discomforts and risk factors in computer-using office workers. Pak J Med Sci. 2016;32(6):1425–9. doi: 10.12669/pjms.326.11436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yabe Y, Hagiwara Y, Sekiguchi T, Momma H, Tsuchiya M, Kuroki K. et al. Late bedtimes, short sleeping time, and longtime video-game playing are associated with low back pain in school-aged athletes. Eur Spine J. 2018;27(5):1112–8. doi: 10.1007/s00586-017-5177-5. [DOI] [PubMed] [Google Scholar]
- 41.Yang H, Haldeman S. Behavior-related factors associated with low back pain in the US adult population. Spine (Phila Pa 1976) 2018;43(1):28–34. doi: 10.1097/brs.0000000000001665. [DOI] [PubMed] [Google Scholar]
- 42.Sribastav SS, Long J, He P, He W, Ye F, Li Z. et al. Risk factors associated with pain severity in patients with non-specific low back pain in Southern China. Asian Spine J. 2018;12(3):533–43. doi: 10.4184/asj.2018.12.3.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park SM, Kim HJ, Jeong H, Kim H, Chang BS, Lee CK. et al. Longer sitting time and low physical activity are closely associated with chronic low back pain in population over 50 years of age: a cross-sectional study using the sixth Korea National Health and Nutrition Examination Survey. Spine J. 2018;18(11):2051–8. doi: 10.1016/j.spinee.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 44.Kulandaivelan S, Ateef M, Singh V, Chaturvedi R, Joshi S. One-year prevalence of low back pain and its correlates in Hisar urban population. J Musculoskelet Res. 2018;21(2):1850011. doi: 10.1142/s0218957718500112. [DOI] [Google Scholar]
- 45.Zhang Q, Dong H, Zhu C, Liu G. Low back pain in emergency ambulance workers in tertiary hospitals in China and its risk factors among ambulance nurses: a cross-sectional study. BMJ Open. 2019;9(9):e029264. doi: 10.1136/bmjopen-2019-029264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Minghelli B. Musculoskeletal spine pain in adolescents: epidemiology of non-specific neck and low back pain and risk factors. J Orthop Sci. 2020;25(5):776–80. doi: 10.1016/j.jos.2019.10.008. [DOI] [PubMed] [Google Scholar]
- 47.Bento TPF, Cornelio GP, de Oliveira Perrucini P, Simeão S, de Conti MHS, de Vitta A. Low back pain in adolescents and association with sociodemographic factors, electronic devices, physical activity and mental health. J Pediatr (Rio J) 2020;96(6):717–24. doi: 10.1016/j.jped.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hanna F, Daas RN, El-Shareif TJ, Al-Marridi HH, Al-Rojoub ZM, Adegboye OA. The relationship between sedentary behavior, back pain, and psychosocial correlates among university employees. Front Public Health. 2019;7:80. doi: 10.3389/fpubh.2019.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Şimşek Ş, Yağcı N, Şenol H. Prevalence of and risk factors for low back pain among healthcare workers in Denizli. Agri. 2017;29(2):71–8. doi: 10.5505/agri.2017.32549. [DOI] [PubMed] [Google Scholar]
- 50.Burdorf A, Naaktgeboren B, de Groot HC. Occupational risk factors for low back pain among sedentary workers. J Occup Med. 1993;35(12):1213–20. [PubMed] [Google Scholar]
- 51.Gunzburg R, Balagué F, Nordin M, Szpalski M, Duyck D, Bull D. et al. Low back pain in a population of school children. Eur Spine J. 1999;8(6):439–43. doi: 10.1007/s005860050202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Croft PR, Papageorgiou AC, Thomas E, Macfarlane GJ, Silman AJ. Short-term physical risk factors for new episodes of low back pain. Prospective evidence from the South Manchester Back Pain Study. Spine (Phila Pa 1976) 1999;24(15):1556–61. doi: 10.1097/00007632-199908010-00009. [DOI] [PubMed] [Google Scholar]
- 53.Shehab DK, Al-Jarallah KF. Nonspecific low-back pain in Kuwaiti children and adolescents: associated factors. J Adolesc Health. 2005;36(1):32–5. doi: 10.1016/j.jadohealth.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 54.Yip VY. New low back pain in nurses: work activities, work stress and sedentary lifestyle. J Adv Nurs. 2004;46(4):430–40. doi: 10.1111/j.1365-2648.2004.03009.x. [DOI] [PubMed] [Google Scholar]
- 55.Yao W, Luo C, Ai F, Chen Q. Risk factors for nonspecific low-back pain in Chinese adolescents: a case-control study. Pain Med. 2012;13(5):658–64. doi: 10.1111/j.1526-4637.2012.01369.x. [DOI] [PubMed] [Google Scholar]
- 56.Lunde LK, Koch M, Knardahl S, Veiersted KB. Associations of objectively measured sitting and standing with low-back pain intensity: a 6-month follow-up of construction and healthcare workers. Scand J Work Environ Health. 2017;43(3):269–78. doi: 10.5271/sjweh.3628. [DOI] [PubMed] [Google Scholar]
- 57.Ganesan S, Acharya AS, Chauhan R, Acharya S. Prevalence and risk factors for low back pain in 1,355 young adults: a cross-sectional study. Asian Spine J. 2017;11(4):610–7. doi: 10.4184/asj.2017.11.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Balling M, Holmberg T, Petersen CB, Aadahl M, Meyrowitsch DW, Tolstrup JS. Total sitting time, leisure time physical activity and risk of hospitalization due to low back pain: The Danish Health Examination Survey cohort 2007-2008. Scand J Public Health. 2019;47(1):45–52. doi: 10.1177/1403494818758843. [DOI] [PubMed] [Google Scholar]
- 59.Celik S, Celik K, Dirimese E, Taşdemir N, Arik T, Büyükkara İ. Determination of pain in musculoskeletal system reported by office workers and the pain risk factors. Int J Occup Med Environ Health. 2018;31(1):91–111. doi: 10.13075/ijomeh.1896.00901. [DOI] [PubMed] [Google Scholar]
- 60.Tavares C, Salvi CS, Nisihara R, Skare T. Low back pain in Brazilian medical students: a cross-sectional study in 629 individuals. Clin Rheumatol. 2019;38(3):939–42. doi: 10.1007/s10067-018-4323-8. [DOI] [PubMed] [Google Scholar]
- 61.Schwertner DS, Oliveira R, Koerich M, Motta AF, Pimenta AL, Gioda FR. Prevalence of low back pain in young Brazilians and associated factors: sex, physical activity, sedentary behavior, sleep and body mass index. J Back Musculoskelet Rehabil. 2020;33(2):233–44. doi: 10.3233/bmr-170821. [DOI] [PubMed] [Google Scholar]
- 62.Aggarwal N, Anand T, Kishore J, Ingle GK. Low back pain and associated risk factors among undergraduate students of a medical college in Delhi. Educ Health (Abingdon) 2013;26(2):103–8. doi: 10.4103/1357-6283.120702. [DOI] [PubMed] [Google Scholar]
- 63.Gupta N, Christiansen CS, Hallman DM, Korshøj M, Carneiro IG, Holtermann A. Is objectively measured sitting time associated with low back pain? a cross-sectional investigation in the NOMAD study. PLoS One. 2015;10(3):e0121159. doi: 10.1371/journal.pone.0121159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ye S, Jing Q, Wei C, Lu J. Risk factors of non-specific neck pain and low back pain in computer-using office workers in China: a cross-sectional study. BMJ Open. 2017;7(4):e014914. doi: 10.1136/bmjopen-2016-014914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hussain SM, Urquhart DM, Wang Y, Dunstan D, Shaw JE, Magliano DJ. et al. Associations between television viewing and physical activity and low back pain in community-based adults: a cohort study. Medicine (Baltimore) 2016;95(25):e3963. doi: 10.1097/md.0000000000003963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mikkonen P, Heikkala E, Paananen M, Remes J, Taimela S, Auvinen J. et al. Accumulation of psychosocial and lifestyle factors and risk of low back pain in adolescence: a cohort study. Eur Spine J. 2016;25(2):635–42. doi: 10.1007/s00586-015-4065-0. [DOI] [PubMed] [Google Scholar]
- 67.Shiri R, Falah-Hassani K, Heliövaara M, Solovieva S, Amiri S, Lallukka T. et al. Risk factors for low back pain: a population-based longitudinal study. Arthritis Care Res (Hoboken) 2019;71(2):290–9. doi: 10.1002/acr.23710. [DOI] [PubMed] [Google Scholar]
- 68.Thorbjörnsson CB, Alfredsson L, Fredriksson K, Michélsen H, Punnett L, Vingård E. et al. Physical and psychosocial factors related to low back pain during a 24-year period. A nested case-control analysis. Spine (Phila Pa 1976) 2000;25(3):369–75. doi: 10.1097/00007632-200002010-00019. [DOI] [PubMed] [Google Scholar]
- 69.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR. et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167(7):875–81. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pereira JR, Cliff DP, Sousa-Sá E, Zhang Z, Santos R. Prevalence of objectively measured sedentary behavior in early years: systematic review and meta-analysis. Scand J Med Sci Sports. 2019;29(3):308–28. doi: 10.1111/sms.13339. [DOI] [PubMed] [Google Scholar]
- 71.Baradaran Mahdavi S, Kelishadi R. Impact of sedentary behavior on bodily pain while staying at home in COVID-19 pandemic and potential preventive strategies. Asian J Sports Med. 2020;11(2):e103511. doi: 10.5812/asjsm.103511. [DOI] [Google Scholar]
- 72.Zhang TT, Liu Z, Liu YL, Zhao JJ, Liu DW, Tian QB. Obesity as a risk factor for low back pain: a meta-analysis. Clin Spine Surg. 2018;31(1):22–7. doi: 10.1097/bsd.0000000000000468. [DOI] [PubMed] [Google Scholar]
- 73.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123(1):87.e7–87. doi: 10.1016/j.amjmed.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 74.Ha JY. Evaluation of metabolic syndrome in patients with chronic low back pain: using the fourth Korea national health and nutrition examination survey data. Chonnam Med J. 2011;47(3):160–4. doi: 10.4068/cmj.2011.47.3.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alghadir AH, Gabr SA, Al-Eisa ES. Mechanical factors and vitamin D deficiency in schoolchildren with low back pain: biochemical and cross-sectional survey analysis. J Pain Res. 2017;10:855–65. doi: 10.2147/jpr.s124859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nieste I, Franssen WMA, Spaas J, Bruckers L, Savelberg H, Eijnde BO. Lifestyle interventions to reduce sedentary behaviour in clinical populations: a systematic review and meta-analysis of different strategies and effects on cardiometabolic health. Prev Med. 2021;148:106593. doi: 10.1016/j.ypmed.2021.106593. [DOI] [PubMed] [Google Scholar]