Abstract
Aim
We investigated longitudinal relations between individual willingness to undergo vaccination against COVID-19 and three social factors: conspiracy mentality, prosociality, and authoritarianism.
Method
This longitudinal study comprised four measurement points. The first wave sample included 1130 responses and was representative of the Polish population in terms of gender, age, and place of residence. Analyses were performed using random intercept cross-lagged panel models.
Results
We observed bidirectional positive cross-lagged relationships between prosociality and willingness to undergo vaccination in the first three waves of measurement. Authoritarianism and conspiracy mentality translated into a lower willingness to vaccinate between the third and fourth points of measurement when the vaccination became a near-term possibility.
Conclusions
Eliciting prosocial motivation to vaccinate can be paramount in overcoming vaccine hesitancy. Because conspiracy thinking may be a crucial barrier to willingness to be vaccinated, it is critical to focus on planning interventions and campaigns undermining conspiracy theories about COVID-19.
Keywords: COVID-19, Prosociality, Conspiracy mentality, Right-Wing Authoritarianism, Vaccine hesitation, Vaccination intentions, Longitudinal study
The COVID-19 pandemic has required various preventive measures, ranging from individual efforts, such as maintaining social distance and wearing masks, to complex collective policies, such as lockdowns. While many of these measures are proven to be effective in slowing down the spread of the disease, increasing COVID-19 vaccination coverage remains the most effective way to achieve control of the pandemic (Christie et al., 2021; Thompson et al., 2021). At the end of 2020, Pfizer, BioNTech, and Moderna reported that their vaccine had a 94–95% efficacy rate and that no serious safety concerns were observed across all trial populations (Cohen, 2020; Oliver et al., 2020). Currently, global studies in the real-world setting demonstrate that the approved vaccines are highly protective against COVID-19-related symptoms (Zheng et al., 2022); additionally, research shows that a booster dose of the mRNA-based vaccine sharply lowers a person's likelihood of contracting COVID-19 and falling ill (Dolgin, 2021). However, governments are still confronted with the challenge of convincing citizens of the vaccine's effectiveness and safety. In the context of the continuous emergence of new COVID-19 variants, improving vaccination coverage is of high importance. However, despite the benefit and importance of vaccination, anti-vaccine movements are growing worldwide and considered one of the greatest threats to public health (WHO, 2019; Pullan & Dey, 2021) given that vaccine hesitancy may be a major obstacle to obtaining the necessary level of vaccination to guarantee herd immunity (Dror et al., 2020). During the pandemic, these movements are gaining additional popularity due to false information and conspiracy theories provided by anti-vaccine activists, which can undermine the implementation of any vaccination programme. For example, Miller (2020) demonstrates that 46% of the USA population believes Bill Gates is creating a tracking device to be injected along with the COVID-19 vaccine. Loomba et al. (2021) provided experimental evidence for the link between exposure to pandemic-related misinformation and vaccination hesitancy. Therefore, this paper aimed to examine different social predictors of vaccine hesitancy.
1. Vaccine hesitancy during the COVID-19 pandemic
Vaccine hesitancy is a broad term that is usually associated with vaccine reluctance and anti-vaccine attitude (e.g. Peretti-Watel et al., 2015) and which may be considered a delay in vaccine uptake or refusal to undergo vaccination (Pullan & Dey, 2021). In this paper, we understand this term as unwillingness to take a vaccine against COVID-19.
Vaccine hesitancy causes concern all over the world, including in post-communist countries. There is evidence (Lazarus et al., 2021) that distrust towards authorities is related to vaccine hesitancy. According to Cichocka and Jost (2014), post-communist countries have a lower level of system justification than capitalist countries, which may cause the population to distrust the government and, consequently, lead to a high level of vaccine hesitancy. Thus, it is necessary to study this problem in post-communist countries, particularly Poland.
The anti-vaccination movement was a serious problem in Poland even before the COVID-19 pandemic: Larson et al. (2018) demonstrated that among all 27 EU countries, Poland had the lowest level of vaccine confidence and the largest decrease in vaccine confidence between 2015 and 2018. According to Lazarus et al. (2020), who conducted a cross-national survey in June 2020 researching people's willingness to undergo COVID-19 vaccination, Poland had the highest level of negative responses (27.3%) when the respondents were asked if they would take a ‘proven, safe and effective vaccine’. According to a study conducted by Sowa et al. (2021) in March 2021 involving a quota sample of Polish citizens, representative in quota concerning age, gender, education and place of residence, as many as 43.5% of Polish people declared that they would not get vaccinated. The current data (Our World in Data, 2021) shows that 55% of Polish people are fully vaccinated (i.e. received at least two doses of vaccination or one dose in the case of Johnson & Johnson vaccine), which is a relatively low level compared to other Western countries, such as the UK (70.1%) or Austria (71.1%). Therefore, the key challenge is to characterise the social factors that may increase or decrease people's willingness to undergo vaccination.
Researching the factors that can influence scepticism related to COVID-19 vaccination, we examined the dynamics between individual willingness to receive vaccination against COVID-19 and social factors: conspiracy mentality, prosociality and authoritarianism, in a four-wave representative panel study in Poland. On the one hand, the decision to undergo vaccination may result from the feeling of obligation to follow governmental health guidelines (Moran et al., 2021); on the other hand, it may exemplify prosocial action (Böhm & Betsch, 2022). Thus, we examined authoritarianism related to the tendency to follow health recommendations from the authorities and the tendency towards prosocial behaviours associated with taking a vaccine to protect oneself and others. Finally, we investigated the role of conspiracy mentality, associated in numerous studies with increased scepticism towards science and government recommendations (Landrum & Olshansky, 2019). Importantly, recent research has shown that conspiracy is related to an extreme concern for the self rather than for others (Hornsey et al., 2021). These factors have already been investigated in the context of vaccine hesitancy (e.g. Chadwick et al., 2021; Böhm & Betsch, 2022; Travis et al., 2021); however, the majority of studies are correlational, which does not allow us to establish causal relationships between the factors. Therefore, to address the limitations of previous research, this study employed advanced longitudinal analysis to examine the causality between variables (the random-intercepts cross-lagged panel models).
2. Vaccine hesitancy during COVID-19: the role of prosociality
Selfish motives may play a vital role in shaping people's behaviour during a pandemic (e.g. van Bavel et al., 2020; Exley, 2016; Haisley & Weber, 2010); however, crises can also inspire acts of prosociality and solidarity (Aguirre et al., 2011; Ntontis & Rocha, 2020). According to Pfattheicher et al. (2020), the COVID-19 vaccination can be perceived as a prosocial behaviour, considering its benefits to the unvaccinated people owing to herd immunity as well as individual costs related to getting vaccinated, such as dealing with uncertainty related to vaccine effectiveness, risk of adverse effects or investment of one's time and effort. This prosocial component of the decision to undergo vaccination can be crucial when the perceived risk associated with personal consequences of the disease is relatively low, as is often the case with COVID-19 (Jetten et al., 2020). There is research showing an association between prosociality and more positive attitudes towards the COVID-19 vaccine: for example, Sun et al. (2021) and Yu et al. (2021) indicated a correlation between prosocial behaviours (supporting others during the pandemic, etc.) and a stronger motivation to enrol in vaccine trials. Moreover, Pfattheicher et al. (2020) revealed that the motivation to get vaccinated was enhanced by empathy, a known precursor of prosocial behaviour. Thus, we hypothesised that prosociality can predict changes in the willingness to undergo vaccination during a pandemic.
3. Vaccine hesitancy during COVID-19: the role of authoritarianism
Korn et al. (2020) argue that vaccination can be perceived as a social contract that every member of society is morally obliged to obey for two reasons: first, vaccination is related to numerous social benefits, such as the protection of vulnerable members of society; second, due to individual costs, some may feel a temptation to have a ‘free ride’ by relying on the protection provided by others. For these reasons, society is interested in ensuring that this social contract is respected.
Korn et al. (2020) also demonstrated that vaccinated individuals tended to punish those who did not comply with the norms related to vaccination. Research on right-wing authoritarianism (RWA) showed that authoritarian people comply with medical or governmental experts' recommendations and anti-Covid-19 measures (Fischer et al., 2020; Manson, 2020; Wnuk et al., 2020). The core components of RWA involve adherence to tradition, submission to authorities, and negative attitudes towards people who break social norms (Altemeyer, 1998). Higher RWA is related to the endorsement of societal stability and control, even if it requires strict restrictions and punishments (Sinclair et al., 2020). Thus, as long as vaccination is considered a social norm, people high in RWA should adhere to this recommendation. However, RWA may be linked to greater vaccine hesitancy due to its association with political conservatism (Nisbet et al., 2015; Rutjens et al., 2021), general scepticism about science (Hornsey et al., 2018), lower concerns about the health impacts of COVID-19 (Prichard & Christman, 2020). Therefore, our study's third objective was to examine how authoritarian tendencies can be associated with willingness to undergo vaccination (WTV) during the COVID-19 pandemic.
4. Vaccine hesitancy during COVID-19: the role of conspiracy theories
The observed resistance to vaccination can also be fed by a growing number of conspiracy theories stating that vaccination is a major threat to life and/or individual freedom (Verger & Dubé, 2020; Flaherty et al., 2021). In addition to the existing conspiracy theories about vaccination (e.g. Jolley & Douglas, 2014), the COVID-19 pandemic has brought in new narratives: for example, about the elites wanting to inject microchips into people via the COVID-19 vaccine and control them or about governments hiding the effective vaccine from the public (e.g. Hotez, 2020; Sturm & Albrecht, 2020; Walkowiak & Walkowiak, 2021). People are often worried about the politicisation of the vaccine, when it will appear important to achieve immediate benefits at the cost of forgoing time-consuming testing of the vaccine's efficacy and safety (Chou & Budenz, 2020; Tyson et al., 2020). The rumours and scepticism about the COVID-19 vaccination grew as more successes in vaccine preparation were reported. For example, Pullan and Dey (2021) demonstrated that spikes in anti-vaccination rhetoric in internet search engines coincided with announcements of advancements in vaccine development and continued growing (Wawrzuta et al., 2021). These concerns may be related to the trend of decreasing trust in science (Funk, 2017; Gauchat, 2012; Lewandowsky & Oberauer, 2016) or questioning the objectivity of scientists (Aksoy et al., 2020), which may further translate into decreased willingness to undergo vaccination (e.g. Allington et al., 2021; Romer & Jamieson, 2020).
Existing studies (including those focusing on the Polish population) indicate that beliefs in conspiracy theories on vaccination as well as conspiracy mentality are associated with a greater reluctance to be vaccinated or to take pro-health measures (e.g. Sowa et al., 2021); however, these associations have been only correlational. By contrast, we used a longitudinal design, which enabled us to examine whether the conspiracy mentality can predict the changes in WTV over time.
5. Context of the study
The study was conducted by analysing four measurement points that took place between May and December 2020.
The first measurement took place between 4 and 7 May 2020. At that time, two months had passed since the detection of the first case of coronavirus infection in Poland and six weeks since the implementation of strong restrictions, such as suspension of classes at the universities, schools and preschools, a ban on movement except for essential activities and banned access to forests and national parks. The total number of people infected with coronavirus surpassed 14,000; the number of fatalities reached 700; nearly 4000 people recovered. Following the surge in coronavirus cases, wearing a face mask started to be obligatory and remained so for about two weeks. From the second half of April, all Poles were required to wear masks, but the most restrictive recommendations that locked people down in their homes had started to be lifted (Krzysztofik et al., 2020; Włodarczyk, 2020, Włodarczyk, 2020).
The second measurement took place between 4 and 17 June 2020, when the total number of people infected with coronavirus approached 28,200, the number of fatalities exceeded 1200 and about 13,700 people recovered. The situation worsened in several voivodeships, and there were large outbreaks of infections in mines, nursing homes and hospitals. However, the gradual lifting of restrictions continued, with almost all restrictions introduced to contain the pandemic removed, although wearing masks in shops, public transport and closed spaces as well as keeping social distance were still obligatory: the Prime Minister of Poland emphasised that Poland was ‘emerging victorious in the fight against the epidemic’ (Włodarczyk, 2020, Włodarczyk, 2020).
The third measurement took place between 7 and 17 July 2020. The total number of people infected with coronavirus exceeded 38,700, the number of fatalities approached 1600 and about 28,500 people recovered. The daily number of cases in Poland remained between 200 and 400. The outbreaks of infections occurred in some hospitals, at workplaces, weddings, baptisms, funerals and in holiday centres. During this time, there was the second round of the presidential election in Poland, and, assuring that the situation related to the coronavirus was stabilizing and the virus was in retreat, the Prime Minister encouraged Poles, including the elderly people, to vote during the election.
The fourth measurement occurred between 3 and 22 December 2020. The total number of people infected with coronavirus exceeded 1,028,000, the number of fatalities approached 18,800, and about 640,000 people recovered. Further restrictions (distance learning at primary and secondary schools and universities, closure of cultural and sports facilities and restaurants, ban on mass events) was implemented due to high increases in the number of COVID-19 cases at the end of October and beginning of November in Poland. After the increase in infections, with the daily cases soaring to about 20,000, the number of infections decreased at the time of the second wave of the Covid-19 pandemic and was at the level of 10–15,000. The dates when the first batch of vaccines would be received were still known, but the government started preparing vaccination plans.
6. Method
6.1. Participants and procedure
To grasp different phases of the pandemic in Poland, the study consists of the analysis of four measuring points: on 4–7 May 2020 (T1), 4–17 June 2020 (T2), 7–17 July 2020 (T3) and 3–22 December 2020 (T4). First, it was planned to conduct the study of three measurement points at equal time intervals in the first months of the pandemic (between May and July 2020). However, over the course of the pandemic, we decided to add one more measurement point, December 2020, to investigate the changes in the relations between our variables at the time when COVID-19 cases and restrictions in Poland increased.
The sample in the first measurement point was representative of Polish people in terms of gender, age and place of residence. To ensure data quality, 49 outliers were removed: 24 participants choosing only the highest or lowest scale levels in the whole survey, and 25 participants choosing only the midpoint of the scale. The final sample of the first measurement included 1130 participants who were followed up in the subsequent measurements: measurement point 2 (n = 971), measurement point 3 (n = 818) and measurement point 4 (n = 688). The demographic characteristics of the participants of all four waves are presented in Table 1 . The participants were recruited online from the Polish research panel Ariadna. Participation was anonymous, and the participants were rewarded with points that they could exchange for small gifts. The presented findings are part of a larger research project on the psychological aspects of the COVID-19 pandemic among the Polish population.
Table 1.
Sociodemographic characteristics in the four measurement points of the study.
| Variable | Category | Measurement points |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 (N = 1130) |
T2 (N = 971) |
T3 (N = 818) |
T4 (N = 688) |
||||||
| M | SD | M | SD | M | SD | M | SD | ||
| Age | 44,53 | 15,83 | 45,79 | 15,45 | 46,27 | 15,07 | 47,30 | 14,89 | |
| Variable | Category | Measurement points |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| T1 (N = 1130) |
T2 (N = 971) |
T3 (N = 818) |
T4 (N = 688) |
||||||
| M |
SD |
M |
SD |
M |
SD |
M |
SD |
||
| N | % | N | % | N | % | N | % | ||
| Gender | Female | 569 | 50.4% | 473 | 48.7% | 387 | 47.3% | 315 | 45.8% |
| Male | 561 | 49.6% | 498 | 51.3% | 431 | 52.7% | 373 | 54.2% | |
| Education | Primary education | 36 | 3.2% | 29 | 3% | 23 | 2.8% | 20 | 2.9% |
| Vocational training | 102 | 9% | 91 | 9.4% | 82 | 10% | 72 | 10.5% | |
| Secondary education | 361 | 31.9% | 300 | 30.9% | 251 | 30.7% | 209 | 30.4% | |
| Post-secondary education | 114 | 10.1% | 89 | 9.2% | 74 | 9% | 64 | 9.3% | |
| University degree | 517 | 45.8% | 462 | 47.6% | 388 | 47.5% | 323 | 47.0% | |
| Place of residence | Village | 425 | 37,6% | 371 | 38,2% | 315 | 38,5% | 270 | 39,2% |
| Small town (up to 20,000 inhabitants) | 135 | 11,9% | 112 | 11,5% | 89 | 10,9% | 76 | 11,0% | |
| Medium town (from 20 to 99 thousand inhabitants) | 242 | 21,4% | 205 | 21,1% | 182 | 22,2% | 156 | 22,7% | |
| Big town (from 100 to 500 thousand inhabitants) | 195 | 17,3% | 169 | 17,4% | 133 | 16,3% | 103 | 15,0% | |
| Big city (over 500,000 inhabitants) | 133 | 11,8% | 114 | 11,7% | 99 | 12,1% | 83 | 12,1% | |
6.2. Measures
Willingness to undergo vaccination (WTV) was measured with one question: ‘If there was a possibility to get vaccinated against the coronavirus now, would you do it?’. The responses of the participants were graded using a five-point scale from 1 = ‘definitely not’ to 5 = ‘definitely yes’.
Prosociality was measured with seven items based on the types of social support that were distinguished by House (1981) and Tardy (1985). The items included the following statements: (during the past week) ‘I have shown heartiness to the people I am in contact with’, ‘I have encouraged my family and friends to take actions that may slow down the spread of the pandemic’, ‘I have helped those around me to deal with the difficulties and obstacles associated with the pandemic’. The participants' answers were graded on a five-point scale, from 1 = ‘definitely not’ to 5 = ‘definitely yes’. The reliability of the scale in each measurement point was as follows: T1: α = 0.86; T2: α = 0.90; T3: α = 0.90 and T4: α = 0.89.
Right-wing authoritarianism (RWA) was measured with three items based on the scale developed by Funke (2005). An example item: “What our country really needs instead of more ‘civil rights’ is a good stiff dose of law and order”. The reliability of the scale in each measurement point was as follows: T1: α = 0.74; T2: α = 0.77; T3: α = 0.82, and T4: α = 0.79. The participants' responses were graded on a seven-point scale from 1 = ‘definitely not’ to 7 = ‘definitely yes’. Due to the limited space in the questionnaire, we used a shortened version of this scale.
Conspiracy mentality was measured with the Polish version (Świderska & Winiewski, 2018) of the five-point scale developed by Bruder et al. (2013). An example item: ‘I think that there are many critical things happening in the world which the public is never informed about’. The participants' responses were graded on a five-point scale from 1 = ‘definitely not’ to 5 = ‘definitely yes’. The scale had a very good reliability: T1: α = 0.83; T2: α = 0.86; T3: α = 0.86; T4: α = 0.83.
6.3. Analytical strategy
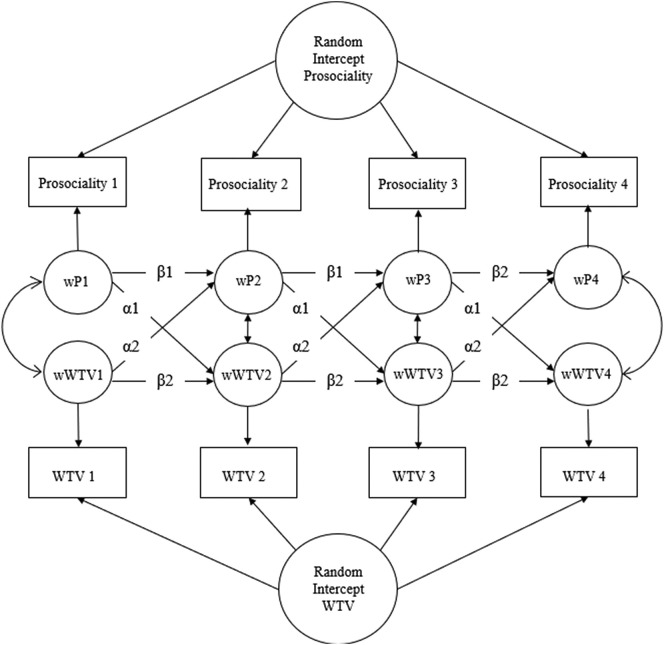
First, we used latent growth curve modelling (LGCM) (Bollen & Curran, 2006) to examine changes in WTV over the course of the pandemic. Next, we used a random-intercept cross-lagged panel model (RI-CLPM) (Hamaker et al., 2015). The RI-CLPM models allow us to investigate whether an individual's deviation from their expected score of a variable predicts their future deviations in the other variables: whether different from the expected belief in prosociality in T1 predicts similar deviations from individuals' WTV in T2 after adjustment for autoregression effects (see Fig. 1 ). We modelled three RI-CLPMs, one for each variable, hypothesised to predict WTV (RWA, prosociality and conspiracy thinking). This approach could be justified by the complexity of these models and potential convergence issues, particularly when more than two variables are analysed simultaneously (Meagher & Cheadle, 2020; Schwaba & Bleidorn, 2021). To increase model parsimony, we held auto-regressive and cross-lagged paths to be equal over time (Hamaker et al., 2015). All analyses were computed using the R-package Iavaan (Rosseel, 2012).
Fig. 1.
Example of random intercept cross-lagged panel model (RI-CLPM) for the estimation of the relationship between prosociality and willingness to undergo vaccination (WTV) for the four-wave panel data. Each observed score is divided into two parts: a within-person part and a between-person part. The wWTV and wP factors represent the within-person part. The two random intercepts capture the between-person part.
Each observed score was divided into two parts: a within-person part and a between-person part. The wWTV and wP factors represent the within-person part, and the two random intercepts capture the between-person part.
6.4. Attrition analysis
We examined systematic patterns of attrition by comparing incomplete responders (n = 442) to complete responders (n = 688) on key demographic variables and the main variables used in the models. Complete responders were more likely to be men than women (χ 2 (1) = 10.98, p = .001) and older than incomplete responders (t(1128) = −6.06, p < .001); no difference was observed in their education level (t(1128) = −0.17, p = .86). We observed certain differences according to WTV (t(1128) = −2.59, p = .01) and conspiracy mentality (t(1128) = −2.42, p = .02), whereas there were no differences in terms of prosociality (t(1128) = 1.01, p = .31) and authoritarianism (t(1128) = 0.45, p = .65). Next, we used a binary logistic regression model to examine whether being a complete or incomplete respondent was predicted by the variables used. The model explained a small portion of the variance in attrition over time (R2 Cox & Snell = 0.07, 7%). Age [odds ratio (OR) = 1.03, p < .001] and gender (OR = 1.58, p = .001) significantly predicted attrition. None of the variables related to conspiracy theories significantly predicted the attrition panel, except for conspiracy mentality (OR = 0.82, p = .031). Thus, we assumed that the inclusion of demographic variables in the models would allow us to treat the missing data as missing at random (MAR) (see Young & Johnson, 2015). Accordingly, to handle the missing data, we used full information maximum likelihood (FIML), providing unbiased parameter estimates when the data were MAR (Enders & Bandalos, 2001). The LGCM and RI-CLPM analyses were conducted with robust maximum likelihood estimation (MLR) to account for non-normally distributed data.
7. Results
We investigated the changes in WTV over time by comparing univariate latent growth curve models, including latent intercept factor only (no-growth models), with the models involving linear change slope factors (growth models). The model fit improved significantly when the slope factors were added (χ2 (8) = 66.94, p < .001, CFI = 0.97, RMSEA = 0.09 vs. no-growth model χ2 (11) = 386.27, p < .001, CFI = 0.80, RMSEA = 0.19), confirming the linear decrease of WTV over time. Next, we performed RI-CLPM analyses. All three RI-CLPM models indicated a good fit to the data (Table 2 ). However, because the lag for the fourth wave was much longer than between the three previous waves, we analysed a model in which the final lag differed from the others in its path weight. Because the model fit improved significantly for all three variables (Table 2), we decided to proceed with those models.
Table 2.
RI-CLPM models parameters.
| Model | χ2 | Df | P | CFI | RMSEA | SRMR |
|---|---|---|---|---|---|---|
Prosociality WTV WTV | ||||||
| Constrained | 95.37 | 23 | <0.001 | 0.98 | 0.06 | 0.04 |
| T3-T4 not constrained | 54.11 | 19 | <0.001 | 0.99 | 0.04 | 0.02 |
RWA WTV WTV | ||||||
| Constrained | 91.00 | 23 | <0.001 | 0.98 | 0.04 | 0.04 |
| T3-T4 not constrained | 56.15 | 19 | <0.001 | 0.99 | 0.04 | 0.02 |
CM WTV WTV | ||||||
| Constrained | 94.29 | 23 | <0.001 | 0.98 | 0.05 | 0.04 |
| T3-T4 not constrained | 54.97 | 19 | <0.001 | 0.99 | 0.04 | 0.02 |
Note: WTV - willingness to undergo vaccination, CM - conspiracy mentality, RWA - right wing authoritarianism.
The results revealed bidirectional within-subject relations between prosociality and WTV in the first three waves, but during the third and fourth waves, only one cross-lagged path was significant; WTV significantly predicted prosociality. We did not find a significant relationship between RWA and WTV during the first three waves; however, between the third and fourth waves, RWA became a significant negative predictor of WTV. Moreover, conspiracy mentality significantly predicted WTV between the third and fourth waves but not during the first three waves (Table 3 ).
Table 3.
Results of random-intercept cross-lagged panel models.
| T1-T3 |
T3-T4 |
|||||
|---|---|---|---|---|---|---|
| B | SE | p | B | SE | p | |
RI-CLPM 1: Prosociality WTV WTV |
||||||
| Autoregressive paths | ||||||
| Prosociality | 0.340 | 0.067 | 0.000 | 0.221 | 0.066 | 0.001 |
| WTV | 0.461 | 0.050 | 0.000 | 0.083 | 0.086 | 0.337 |
| Cross-lagged path | ||||||
Prosociality WTV WTV |
0.175 | 0.064 | 0.006 | 0.183 | 0.101 | 0.069 |
WTV Prosociality Prosociality |
0.083 | 0.028 | 0.003 | 0.128 | 0.035 | 0.000 |
| 4-Waves between subject correlation | T1-T4 | |||||
| B | SE | p | ||||
| 0.147 | 0.035 | 0.000 | ||||
RI-CLPM 2: RWA WTV WTV |
||||||
| Autoregressive paths | ||||||
| RWA | 0.091 | 0.47 | 0.052 | 0.153 | 0.072 | 0.032 |
| WTV | 0.441 | 0.053 | 0.000 | 0.079 | 0.089 | 0.375 |
| Cross-lagged path | ||||||
RWA WTV WTV |
−0.005 | 0.034 | 0.886 | −0.123 | 0.062 | 0.046 |
WTV RWA RWA |
−0.023 | 0.044 | 0.601 | −0.059 | 0.069 | 0.391 |
| 4-Waves between subject correlation | T1-T4 | |||||
| B | SE | p | ||||
| −0.067 | 0.055 | 0.224 | ||||
RI-CLPM 3: CM WTV WTV |
||||||
| Autoregressive paths | ||||||
| CM | 0.036 | 0.058 | 0.538 | −0.011 | 0.063 | 0.863 |
| WTV | 0.454 | 0.054 | 0.000 | 0.093 | 0.083 | 0.264 |
| Cross-lagged path | ||||||
CM WTV WTV |
−0.058 | 0.064 | 0.359 | −0.399 | 0.109 | 0.000 |
WTV CM CM |
−0.032 | 0.023 | 0.160 | −0.057 | 0.033 | 0.083 |
| 4-Waves between subject correlation | T1-T4 | |||||
| B | SE | p | ||||
| −0.170 | 0.027 | 0.000 | ||||
Note: WTV - willingness to undergo vaccination, CM - conspiracy mentality, RWA - right wing authoritarianism.
8. Discussion
Covid-19 vaccines have been demonstrated to be the most effective way to achieve control of the pandemic (Christie et al., 2021; Thompson et al., 2021). However, there is a major obstacle to achieving this control: people's hesitancy to be vaccinated. Compared with existing, mostly correlational, studies on predictors of vaccination intentions, the main strength of this research lies in applying a longitudinal design (covering the period from May to December 2020) on a representative sample and using advanced statistical methods to infer causality between variables of interest. The analyses of latent growth models demonstrated that the willingness to undergo vaccination gradually decreased over the course of the pandemic, from T1 mean slightly above the midpoint to T4 mean a bit below the midpoint of the scale. This means that despite the second wave of COVID-19 starting around October, the participants were less willing to undergo vaccination than during the first wave of the COVID-19 pandemic, in May 2020.
Our results are in line with the studies conducted in other countries; for example, a national survey conducted among US adults in September 2020 on the willingness to get a COVID-19 vaccine found a decline of 21% compared with a similar research in May 2020 (de Albuquerque Veloso Machado et al., 2021). We can suppose that when the perspective of vaccination against COVID-19 became increasingly real (between May and December 2020), it started to arouse uncertainties, fears and doubts. The fast process of vaccine development could have raised doubts as to whether or not it has been sufficiently tested and verified (Islam et al., 2021; Wawrzuta et al., 2021). Many authors have pointed out that the decreased willingness to undergo vaccination may have been caused by increased exposure to COVID-19 vaccine misinformation on social media (e.g. Diaz et al., 2021; Wilson & Wiysonge, 2020). The link between the salience of vaccination and the increasing number of false information is also indicated by the trends in internet search queries (Diaz et al., 2021). There is a growing presence of anti-vaccine searches related to COVID-19 during the pandemic (Pullan & Dey, 2021). An alternative explanation for the decrease in willingness to undergo vaccination could also be a result of pandemic threats decrease over time. However, additional analyses we conducted did not show a decrease in COVID-19 threat between the first and last measurement points (see Appendix).
The RI-CLPM analysis revealed a reciprocal, bidirectional relationship between prosociality and willingness to undergo vaccination (the within-person changes in prosociality preceded the within-person changes in willingness to undergo vaccination and vice versa) during the first three waves of our study. Thus, using more robust methods, we confirmed and extended the correlational research on the role of prosocial behaviours in shaping attitudes towards vaccination (e.g. Sun et al., 2021). These results contribute to the findings by Pfattheicher et al. (2020), which indicated that information related to others' suffering increases the willingness to be vaccinated against COVID-19. Engaging in prosocial behaviour may signal a person's values (Carrizales et al., 2021), i.e., recognising actions to counteract the negative consequences of a pandemic as meaningful and necessary. A person who can make a personal commitment to helping others may also be more willing to accept the need to get vaccinated as the most effective way to combat a pandemic. This effect may also be reinforced because prosocial behaviours provide more opportunities for people to learn about others' perspectives and hardships during a pandemic and further strengthen their desire to help others (e.g. Carrizales et al., 2021; Malti et al., 2009).
The effect of willingness to undergo vaccination driven by prosocial behaviour can be explained by the need for self-verification, a process of authentication of one's self-views by actions (Swann & Read, 1981). When one wants to take a vaccine, they are likely to take the need to counteract a pandemic seriously; as a result, their desire to be involved in prosocial actions increases. The willingness to undergo vaccination may also be related to receiving appraisal from those around them, reinforcing the perception of oneself as a responsible and rational person (e.g. Crocetti et al., 2016). This positive feedback may lead to stronger social ties with others and ultimately to an even greater desire to help those in need (Carrizales et al., 2021).
The effect of WTV on prosociality can also be explained from the perspective of moral elevation theory (see e.g. Pohling & Diessner, 2016). In a society as polarised on vaccination as in Poland, vaccine supporters may perceive their views as a manifestation of moral excellence and compassion towards humanity affected by COVID-19 in comparison to the anti-vaxxers, perceived as violating moral obligations (e.g. Bernstein, 2021). Studies show that moral elevation may lead to more frequent prosocial behaviour and actions consistent with professed values (e.g., Schnall & Roper, 2012). We believe that this bidirectional effect between WTV and prosociality could be of interest in the context of motivating people to continue pandemic control efforts; however, further research (especially experimental studies) is required to confirm this result and examine, on the one hand, to what extent the perceived proximity of a medical intervention influences the attitude towards it and, on the other hand, whether attitudes towards vaccination are related to the perceptions of oneself as having exceptional moral qualities.
Because our study covered four time points during one year of the pandemic, we can demonstrate that the relationship between prosociality and vaccination intentions changed over time. Between the third and the fourth waves, when the possibility of being vaccinated became increasingly realistic, willingness to undergo vaccination significantly predicted prosociality, not the other way round. This may suggest that when the probability of vaccination was a distant option, prosociality was a significant motive for vaccination; however, it seems that when vaccination became a tangible possibility, mere willingness to undergo vaccination influenced people's prosocial behaviour. However, since we did not examine whether the participants perceived vaccination as an option that was near or distant in time, this interpretation should be treated with caution. Willingness to undergo vaccination may raise the hope that the pandemic will be under control in the future and could thus contribute to adopting an active attitude towards overcoming difficulties caused by COVID-19; in particular, it could stir people to help others deal with the obstacles and hardships of the pandemic.
Finally, our results suggest that appealing to prosocial motives (e.g. by the governments and other authorities) can be a viable strategy to increase vaccination rates and potentially long-term positive attitudes towards vaccination, but the efficiency of this approach may be the highest when the possibility of vaccination is a distant option, which is in line with other research demonstrating that the messages intended to elicit prosocial motives and highlighting the benefit of vaccination to others are useful for promoting, for example, flu vaccination (Li et al., 2016) as well as providing experimental evidence for the link between exposure to the information about prosocial aspects of vaccination and willingness to undergo vaccination (Betsch et al., 2013). There are also several studies proving that the messages intended to elicit prosocial motives can activate prosocial motivation towards COVID-19 vaccination (Böhm & Betsch, 2022). Particularly, interventions based on increasing knowledge about community protection and concerns about others were found to be useful in increasing vaccination intentions (Böhm & Betsch, 2022). Moreover, James et al. (2021), who tested several different interventions, found that messages focused on a community interest yielded a robust effect on vaccination intentions, including even the individuals who were initially sceptical about vaccines.
Appealing to prosocial motivations can also more efficiently combat vaccine hesitancy than appealing to social norms or authorities as, contrary to our hypothesis, there was no evidence of a direct relationship between RWA and vaccination intentions during the first three waves. One of the reasons for the lack of expected relations may be very high political polarisation in Poland. Although populist voters still hold the majority of voices, almost half of the citizens oppose the current government (see Sieradzka, 2020). Also, among the voters with right-wing views (those who should be characterised by higher RWA), there is a significant disagreement about the official recommendations issued by the authorities. Voters for the ruling Law and Justice party are more likely to comply with the recommendations than voters for the extreme right-wing Confederation party, who view anti-COVID-19 actions as an attack on civil liberties and an attempt to introduce a totalitarian regime. In addition, politicians from the ruling party continue to hold ambiguous views on the need for vaccinations. For example, the Prime Minister and the President of Poland declared different levels of vaccine hesitancy at the time of the survey. Due to this complex situation, the perception of vaccination as a strong social norm may have been severely hampered. Waszkiewicz et al. (2021) demonstrated that anti-vaccine attitudes in Poland are related to anti-establishment attitudes and people being undecided about their voting preferences rather than right-wing political views, which supports our conclusion. Interestingly, a higher tendency to follow the authorities' recommendations (high RWA) did translate into a lower willingness to undergo vaccination between the third and fourth waves, when vaccination was a real possibility. This outcome is in line with the research on anti-vaccination attitudes in times of the COVID-19 pandemic conducted by Kempthorne and Terrizzi (2021). A plausible explanation for this outcome is that RWA comprises a conservative and right-wing attitude, which was shown to relate to vaccination scepticism (Nisbet et al., 2015; Rutjens et al., 2021). Political conservatism was also related to science scepticism, such as disbelief in climate change, and paranoid thinking (Hornsey et al., 2018). It is possible that as the perception of COVID-19 vaccination as a social norm is not fully settled, the RWA in our research reflected a more conservative and sceptical attitude towards science. An important limitation of our study was the use of an abbreviated RWA scale; therefore, future studies would need to determine whether the results are confirmed using the full version of the scale. Also, it would be worthwhile to include a measure of social dominance orientation - the second facet of political ideology, emphasizing a preference for hierarchy and high-status group dominance (see e.g., Clarke et al., 2021).
As in the case of RWA, we observed a significant cross-lagged effect between conspiracy mentality and WTV only between the third and the fourth waves, which can be explained by the rising popularity of conspiracy theories about vaccination during this period (Diaz et al., 2021; Pullan & Dey, 2021). For example, Wawrzuta et al. (2021) showed that suspicions about the intentions of vaccines' producers increased in Poland in parallel with the announced completion of new vaccines. It is possible that those characterised by a higher conspiracy mentality focused more on the theories regarding the origin of COVID-19 (e.g. bioweapon vs. hoax conspiracy) in the early phases of the pandemic (Imhoff & Lamberty, 2020), and when the vaccines' feasibility approached, they began to pay increasing attention to conspiracy theories regarding vaccination. Recent studies have shown that the content of endorsed conspiracy theories has implications for pro-health behaviours and other social issues (Imhoff & Lamberty, 2020; Oleksy et al., 2021). Therefore, if individuals with a high conspiracy mentality began to place more importance on the theories about vaccination, it may have made them more reluctant to be vaccinated. Thus, our data confirm the findings of previous correlational studies, reporting that endorsing conspiracy theories may be related to a decrease in pro-health attitudes and behaviour (e.g. Imhoff & Lamberty, 2020; Oleksy et al., 2021).
Because conspiracy thinking can threaten vaccination rates, authorities should focus on information campaigns to undermine belief in conspiracy theories about COVID-19: for example, through psychological inoculation against fake news (see e.g. Basol et al., 2021; Van der Linden et al., 2020). Such campaigns may help increase WTV and decrease conspiracy mentality. In other words, trust in scientific solutions (in particular, vaccines) may increase one's resistance to conspiratorial explanations of reality. Rzymski et al. (2021a) proposed several strategies to support the COVID-19 vaccination with evidence-based communication and tackling misinformation, such as tracking and tackling emerging and circulating conspiracy theories and fake news on COVID-19 vaccines and organising groups communicating science on COVID-19. Finally, false claims, among conspiracy theories, about COVID-19 vaccines made by politicians, health professionals, scientists and academics should not be tolerated.
This study presents certain limitations. First, although the survey was longitudinal and representative, it was limited to only one country. It is worth comparing these results with reports from other countries even though the pandemic situation in most European countries was, to some extent, similar. Second, our study used only declarative measures and not actual behaviour, and WTV was measured with only one item. Third, the study was conducted online, which presents a risk of invalid responses (Al-Salom & Miller, 2017). Moreover, only users of the Internet and members of the online panel participated in the study; therefore, although the sample was representative in terms of age, sex and place of residence, it was not such in terms of education level and other sociodemographic variables. Finally, as in every longitudinal study, the sample was prone to attrition bias. Considering the direct threats posed by conspiracy thinking (one of which is hesitancy to undergo vaccination), it is crucial to focus on planning effective interventions and campaigns that undermine conspiracy theories concerning COVID-19. According to Feleszko et al. (2021), 49% of people with low WTV can change their minds under certain circumstances, including presentation of scientific research on vaccine safety or recommendation of vaccination by their family doctor. A recent study by Guan et al. (2021) found that debunking conspiracy theories by science- and fact-focused interventions is effective in mitigating conspiracy beliefs. This suggests that educational interventions concerning COVID-19 vaccination may be efficient, but precluding conspiracy theories is suggested to be more effective than their refutation (Cichocka, 2020). Nevertheless, further research is needed to test the actual effectiveness of such interventions.
Future research is needed to examine current vaccination attitudes and their predictors while the vaccination campaign is underway and new variants of coronavirus are emerging. For example, the current data (Our World in Data, December 2021) shows that about 57% of the world population has received at least one dose of a COVID-19 vaccine, ranging from about 1–2% in low-income African countries to about 90% in West European Countries (e.g. Portugal) and the United Arab Emirates. Additionally, research shows that a booster dose of an mRNA-based vaccine sharply lowers the person's likelihood of contracting COVID-19 and falling sick. In the light of the threat of new variants, the current challenge is to persuade larger part of population to receive booster doses (Rzymski et al., 2021b).
CRediT authorship contribution statement
Tomasz Oleksy: Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. Anna Wnuk: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. Małgorzata Gambin: Investigation, Methodology, Writing – original draft, Writing – review & editing. Agnieszka Łyś: Investigation, Methodology, Writing – original draft, Writing – review & editing. Kamilla Bargiel-Matusiewicz: Writing – original draft, Writing – review & editing. Ewa Pisula: Investigation, Methodology, Writing – original draft, Writing – review & editing.
References
- Aguirre B.E., Torres M.R., Gill K.B., Lawrence Hotchkiss H. Normative collective behavior in the station building fire. Social Science Quarterly. 2011;92(1):100–118. doi: 10.1111/j.1540-6237.2011.00759.x. [DOI] [PubMed] [Google Scholar]
- Aksoy C., Eichengreen B., Saka O. 2020. Revenge of the Experts: Will COVID-19 Renew or Diminish Public Trust in Science? [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Albuquerque Veloso Machado M., Roberts B., Wong B.L.H., van Kessel R. The relationship between the COVID-19 pandemic and vaccine hesitancy: a scoping review. Frontiers in public health. 2021:1370. doi: 10.3389/fpubh.2021.747787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allington D., McAndrew S., Moxham-Hall V., Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychological Medicine. 2021:1–12. doi: 10.1017/S0033291721001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Salom P., Miller C.J. The problem with online data collection: Predicting invalid responding in undergraduate samples. Current Psychology. 2017;38:1258–1264. doi: 10.1007/s12144-017-9674-9. [DOI] [Google Scholar]
- Altemeyer B. Advances in experimental social psychology. Vol. 30. Academic Press; 1998. The other “authoritarian personality”; pp. 47–92. [Google Scholar]
- Basol M., Roozenbeek J., Berriche M., Uenal F., McClanahan W.P., Linden S.V.D. Towards psychological herd immunity: Cross-cultural evidence for two prebunking interventions against COVID-19 misinformation. Big Data & Society. 2021;8(1) 20539517211013868. [Google Scholar]
- Bernstein J. Anti-vaxxers, anti-anti-vaxxers, fairness, and anger. Kennedy Institute of Ethics Journal. 2021;31(1):17–52. doi: 10.1353/ken.2021.0003. [DOI] [PubMed] [Google Scholar]
- Betsch C., Böhm R., Korn L. Inviting free-riders or appealing to prosocial behavior? Game-theoretical reflections on communicating herd immunity in vaccine advocacy. Health Psychology. 2013;32(9):978. doi: 10.1037/a0031590. [DOI] [PubMed] [Google Scholar]
- Böhm R., Betsch C. Prosocial vaccination. Current Opinion in Psychology. 2022;43:307–311. doi: 10.1016/j.copsyc.2021.08.010. [DOI] [PubMed] [Google Scholar]
- Bollen K.A., Curran P.J. Latent curve models: A structural equation perspective. Vol. 467. John Wiley & Sons; 2006. [Google Scholar]
- Bruder M., Haffke P., Neave N., Nouripanah N., Imhoff R. Measuring individual differences in generic beliefs in conspiracy theories across cultures: Conspiracy mentality questionnaire. Frontiers in Psychology. 2013;4:225. doi: 10.3389/fpsyg.2013.00225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrizales A., Branje S., Lannegrand L. Disentangling between-and within-person associations between empathy and prosocial behaviours during early adolescence. Journal of Adolescence. 2021;93:114–125. doi: 10.1016/j.adolescence.2021.10.006. [DOI] [PubMed] [Google Scholar]
- Chadwick A., Kaiser J., Vaccari C., Freeman D., Lambe S., Loe B.S., Yu L.M. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Social Media+ Society. 2021;7(2) 20563051211008817. [Google Scholar]
- Chou W.Y.S., Budenz A. Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Communication. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- Christie A., Brooks J.T., Hicks L.A., Sauber-Schatz E.K., Yoder J.S., Honein M.A., Team R. Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. Morbidity and Mortality Weekly Report. 2021;70(30):1044. doi: 10.15585/mmwr.mm7030e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cichocka A. To counter conspiracy theories, boost well-being. Nature. 2020;587:177. doi: 10.1038/d41586-020-03130-6. [DOI] [PubMed] [Google Scholar]
- Cichocka A., Jost J.T. Stripped of illusions? Exploring system justification processes in capitalist and post-communist societies. International Journal of Psychology. 2014;49(1):6–29. doi: 10.1002/ijop.12011. [DOI] [PubMed] [Google Scholar]
- Clarke E.J., Klas A., Dyos E. The role of ideological attitudes in responses to COVID-19 threat and government restrictions in Australia. Personality and Individual Differences. 2021;175 doi: 10.1016/j.paid.2021.110734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Incredible milestone for science. Pfizer and BioNTech update their promising COVID-19 vaccine result. Science. 2020;10 [Google Scholar]
- Crocetti E., Moscatelli S., Van der Graaff J., Rubini M., Meeus W., Branje S. The interplay of self-certainty and prosocial development in the transition from late adolescence to emerging adulthood. European Journal of Personality. 2016;30(6):594–607. [Google Scholar]
- Diaz P., Reddy P., Ramasahayam R., Kuchakulla M., Ramasamy R. COVID-19 vaccine hesitancy linked to increased internet search queries for side effects on fertility potential in the initial rollout phase following emergency use authorization. Andrologia. 2021;53(9) doi: 10.1111/and.14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolgin E. Omicron is supercharging the COVID vaccine booster debate. News. 2021. https://www.icpcovid.com/sites/default/files/2021-12/Ep%20197-5%20Omicron%20is%20supercharging%20the%20COVID%20vaccine%20booster%20debate.pdf Retrieved from: [DOI] [PubMed]
- Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., Sela E.… Vaccine hesitancy: The next challenge in the fight against COVID-19. European Journal of Epidemiology. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C.K., Bandalos D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural equation modeling. 2001;8(3):430–457. [PubMed] [Google Scholar]
- Exley C.L. Excusing selfishness in charitable giving: The role of risk. The Review of Economic Studies. 2016;83(2):587–628. [Google Scholar]
- Feleszko W., Lewulis P., Czarnecki A., Waszkiewicz P. Flattening the curve of COVID-19 vaccine rejection-an international overview. Vaccines. 2021;9(1):44. doi: 10.3390/vaccines9010044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer K., Chaudhuri A., Atkinson Q. 2020. Responses to the COVID-19 pandemic reflect the dual evolutionary foundations of political ideology. [Preprint] [DOI] [PubMed] [Google Scholar]
- Flaherty E., Sturm T., Farries E. The conspiracy of Covid-19 and 5G: Spatial analysis fallacies in the age of data democratization. Social Science & Medicine. 2021;114546 doi: 10.1016/j.socscimed.2021.114546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk C. Issues in Science and Technology. 2017. Real numbers: Mixed messages about public Trust in Science; p. 34. [Google Scholar]
- Funke F. The dimensionality of right-wing authoritarianism: Lessons from the dilemma between theory and measurement. Political Psychology. 2005;26(2):195–218. [Google Scholar]
- Gauchat G. Politicization of science in the public sphere: A study of public trust in the United States, 1974 to 2010. American Sociological Review. 2012;77(2):167–187. [Google Scholar]
- Guan T., Liu T., Yuan R. Facing disinformation: Five methods to counter conspiracy theories amid the COVID-19 pandemic. Comunicar. 2021;29(69):71–83. [Google Scholar]
- Haisley E.C., Weber R.A. Self-serving interpretations of ambiguity in other-regarding behavior. Games and Economic Behavior. 2010;68(2):614–625. [Google Scholar]
- Hamaker E.L., Kuiper R.M., Grasman R.P. A critique of the cross-lagged panel model. Psychological Methods. 2015;20(1):102. doi: 10.1037/a0038889. [DOI] [PubMed] [Google Scholar]
- Hornsey M.J., Chapman C.M., Alvarez B., Bentley S., Salvador Casara B.G., Crimston C.R.…Jetten J. To what extent are conspiracy theorists concerned for self versus others? A COVID-19 test case. European Journal of Social Psychology. 2021;51(2):285–293. doi: 10.1002/ejsp.2737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornsey M.J., Harris E.A., Fielding K.S. Relationships among conspiratorial beliefs, conservatism and climate scepticism across nations. Nature Climate Change. 2018;8(7):614–620. [Google Scholar]
- Hotez P.J. COVID19 meets the antivaccine movement. Microbes and Infection. 2020;22(4):162. doi: 10.1016/j.micinf.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J.S. Addison-Wesley; Reading, Massachusetts: 1981. Work stress and social support. [Google Scholar]
- Imhoff R., Lamberty P. A bioweapon or a hoax? The link between distinct conspiracy beliefs about the coronavirus disease (COVID-19) outbreak and pandemic behavior. Social Psychological and Personality Science. 2020;11(8):1110–1118. doi: 10.1177/1948550620934692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.S., Kamal A.H.M., Kabir A., Southern D.L., Khan S.H., Hasan S.M., Seale H.… COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021;16(5) doi: 10.1371/journal.pone.0251605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James E.K., Bokemper S.E., Gerber A.S., Omer S.B., Huber G.A. Persuasive messaging to increase COVID-19 vaccine uptake intentions. Vaccine. 2021;39(49):7158–7165. doi: 10.1016/j.vaccine.2021.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetten J., Reicher S., Haslam A., Cruwys T. The psychology of COVID-19. Sage Publications; London: 2020. A social identity analysis of COVID-19. Together apart; pp. 20–31. [Google Scholar]
- Jolley D., Douglas K.M. The effects of anti-vaccine conspiracy theories on vaccination intentions. PloS one. 2014;9(2) doi: 10.1371/journal.pone.0089177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempthorne J.C., Terrizzi J.A., Jr. The behavioral immune system and conservatism as predictors of disease-avoidant attitudes during the COVID-19 pandemic. Personality and Individual Differences. 2021;178 doi: 10.1016/j.paid.2021.110857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn L., Böhm R., Meier N.W., Betsch C. Vaccination as a social contract. Proceedings of the National Academy of Sciences. 2020;117(26):14890–14899. doi: 10.1073/pnas.1919666117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzysztofik R., Kantor-Pietraga I., Spórna T. Spatial and functional dimensions of the COVID-19 epidemic in Poland. Eurasian Geography and Economics. 2020;61(4–5):573–586. [Google Scholar]
- Landrum A.R., Olshansky A. The role of conspiracy mentality in denial of science and susceptibility to viral deception about science. Politics and the Life Sciences. 2019;38(2):193–209. doi: 10.1017/pls.2019.9. [DOI] [PubMed] [Google Scholar]
- Larson H., de Figueiredo A., Karafillakis E., Rawal M. Publications Office of the European Union; Luxembourg: 2018. State of vaccine confidence in the EU 2018. [Google Scholar]
- Lazarus J.V., Binagwaho A., El-Mohandes A.A., Fielding J.E., Larson H.J., Plasència A., Ratzan S.C.… Keeping governments accountable: The COVID-19 assessment scorecard (COVID-SCORE) Nature Medicine. 2020;26(7):1005–1008. doi: 10.1038/s41591-020-0950-0. [DOI] [PubMed] [Google Scholar]
- Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., et al. A global survey of potential acceptance of a COVID-19 vaccine. Nature Medicine. 2021;27(2):225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowsky S., Oberauer K. Motivated rejection of science. Current Directions in Psychological Science. 2016;25(4):217–222. [Google Scholar]
- Li M., Taylor E.G., Atkins K.E., Chapman G.B., Galvani A.P. Stimulating influenza vaccination via prosocial motives. PLoS One. 2016;11(7) doi: 10.1371/journal.pone.0159780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loomba S., de Figueiredo A., Piatek S.J., de Graaf K., Larson H.J. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour. 2021;5(3):337–348. doi: 10.1038/s41562-021-01056-1. [DOI] [PubMed] [Google Scholar]
- Malti T., Gummerum M., Keller M., Buchmann M. Children’s moral motivation, sympathy, and prosocial behavior. Child Development. 2009;80(2):442–460. doi: 10.1111/j.1467-8624.2009.01271.x. [DOI] [PubMed] [Google Scholar]
- Manson J.H. Right-wing authoritarianism, left-wing authoritarianism, and pandemic-mitigation authoritarianism. Personality and Individual Differences. 2020;167 doi: 10.1016/j.paid.2020.110251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meagher B.R., Cheadle A.D. Distant from others, but close to home: The relationship between home attachment and mental health during COVID-19. Journal of Environmental Psychology. 2020;72 doi: 10.1016/j.jenvp.2020.101516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller J.M. Psychological, political, and situational factors combine to boost COVID-19 conspiracy theory beliefs. Canadian Journal of Political Science/Revue canadienne de science politique. 2020;53(2):327–334. [Google Scholar]
- Moran C., Campbell D.J., Campbell T.S., Roach P., Bourassa L., Collins Z.…McLane P. Predictors of attitudes and adherence to COVID-19 public health guidelines in Western countries: A rapid review of the emerging literature. Journal of public health (Oxford, England). 2021;43(4):739–753. doi: 10.1093/pubmed/fdab070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisbet E.C., Cooper K.E., Garrett R.K. The partisan brain: How dissonant science messages lead conservatives and liberals to (dis) trust science. The Annals of the American Academy of Political and Social Science. 2015;658(1):36–66. [Google Scholar]
- Ntontis E., Rocha C. Sage; London: 2020. Solidarity. Together apart: The psychology of COVID-19. [Google Scholar]
- Oleksy T., Wnuk A., Maison D., Łyś A. Content matters. Different predictors and social consequences of general and government-related conspiracy theories on COVID-19. Personality and Individual Differences. 2021;168 doi: 10.1016/j.paid.2020.110289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver S.E., Gargano J.W., Marin M., Wallace M., Curran K.G., Chamberland M., Dooling K. The Advisory Committee on Immunization Practices’ Interim recommendation for use of Moderna COVID-19 vaccine—United States, December 2020. MMWR. Morbidity and mortality weekly report. 2020;69 doi: 10.15585/mmwr.mm695152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Our World in Data. 2021. (Accessed 12 December 2021).
- Peretti-Watel P., Larson H.J., Ward J.K., Schulz W.S., Verger P. Vaccine hesitancy: Clarifying a theoretical framework for an ambiguous notion. PLoS Currents. 2015;7 doi: 10.1371/currents.outbreaks.6844c80ff9f5b273f34c91f71b7fc289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfattheicher S., Petersen M.B., Böhm R. Information about herd immunity and empathy promote COVID-19 vaccination intentions. 2020. https://psyarxiv.com/wzu6k/ [DOI] [PubMed]
- Pohling R., Diessner R. Moral elevation and moral beauty: A review of the empirical literature. Review of General Psychology. 2016;20(4):412–425. [Google Scholar]
- Prichard E.C., Christman S.D. Authoritarianism, conspiracy beliefs, gender and COVID-19: Links between individual differences and concern about COVID-19, mask wearing behaviors, and the tendency to blame China for the virus. Frontiers in Psychology. 2020;11:3130. doi: 10.3389/fpsyg.2020.597671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pullan S., Dey M. Vaccine hesitancy and anti-vaccination in the time of COVID-19: A Google trends analysis. Vaccine. 2021;39(14):1877–1881. doi: 10.1016/j.vaccine.2021.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the US. Social Science & Medicine. 2020;263 doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA) Journal of Statistical Software. 2012;48(2):1–36. [Google Scholar]
- Rutjens B.T., van der Linden S., van der Lee R. Science skepticism in times of COVID-19. Group Processes & Intergroup Relations. 2021;24(2):276–283. [Google Scholar]
- Rzymski P., Borkowski L., Drąg M., Flisiak R., Jemielity J., Krajewski J., Fal A.… The strategies to support the COVID-19 vaccination with evidence-based communication and tackling misinformation. Vaccines. 2021;9(2):109. doi: 10.3390/vaccines9020109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rzymski P., Poniedziałek B., Fal A. Willingness to Receive the Booster COVID-19 Vaccine Dose in Poland. Vaccines. 2021;9(11):1286. doi: 10.3390/vaccines9111286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnall S., Roper J. Elevation puts moral values into action. Social Psychological and Personality Science. 2012;3(3):373–378. [Google Scholar]
- Schwaba T., Bleidorn W. Log on and prosper? Little evidence for codevelopment between psychological adjustment and technology use in older adulthood. The Journals of Gerontology: Series B. 2021;76(1):67–77. doi: 10.1093/geronb/gbaa073. [DOI] [PubMed] [Google Scholar]
- Sieradzka M. Anti-vaccine sentiment rife in Poland. Deutsche Welle. 2020. https://www.dw.com/en/anti-vaccine-sentiment-rife-in-poland/a-56100878 Retrieved from:
- Sinclair A.H., Stanley M.L., Seli P. Closed-minded cognition: Right-wing authoritarianism is negatively related to belief updating following prediction error. Psychonomic Bulletin & Review. 2020;27(6):1348–1361. doi: 10.3758/s13423-020-01767-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowa P., Kiszkiel Ł., Laskowski P.P., Alimowski M., Szczerbiński Ł., Paniczko M., Kamiński K.… COVID-19 vaccine hesitancy in Poland—multifactorial impact trajectories. Vaccines. 2021;9(8):876. doi: 10.3390/vaccines9080876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm T., Albrecht T. Constituent Covid-19 apocalypses: Contagious conspiracism, 5G, and viral vaccinations. Anthropology & Medicine. 2020:1–18. doi: 10.1080/13648470.2020.1833684. [DOI] [PubMed] [Google Scholar]
- Sun S., Lin D., Operario D. Interest in COVID-19 vaccine trials participation among young adults in China: Willingness, reasons for hesitancy, and demographic and psychosocial determinants. Preventive Medicine Reports. 2021;22(101350) doi: 10.1016/j.pmedr.2021.101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swann W.B., Jr., Read S.J. Self-verification processes: How we sustain our self-conceptions. Journal of Experimental Social Psychology. 1981;17(4):351–372. [Google Scholar]
- Świderska A., Winiewski M. In: Uprzedzenia w Polsce 2017. Oblicza przemocy międzygrupowej [Prejudices in Poland 2017. Faces of intergroup violence.] Stefaniak A., Winiewski M., editors. Liberi Libri; Warsaw: 2018. Polski Sondaż Uprzedzeń 2017. Metodologia badania [Polish survey of prejudices 2017. Methodology of the study.] pp. 365–379. 20563051211008817. [Google Scholar]
- Tardy C.H. Social support measurement. American Journal of Community Psychology. 1985;13(2):187. [Google Scholar]
- Thompson M.G., Stenehjem E., Grannis S., Ball S.W., Naleway A.L., Ong T.C., Klein N.P.… Effectiveness of Covid-19 vaccines in ambulatory and inpatient care settings. New England Journal of Medicine. 2021;385(15):1355–1371. doi: 10.1056/NEJMoa2110362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis J., Harris S., Fadel T., Webb G. Identifying the determinants of COVID-19 preventative behaviors and vaccine intentions among South Carolina residents. Plos one. 2021;16(8) doi: 10.1371/journal.pone.0256178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyson A., Johnson C., Funk C. U.S. public now divided over whether to get COVID-19 vaccine. Pew Research Center: Science & Society. 2020. https://www.pewresearch.org/science/2020/09/17/u-s-public-now-divided-over-whether-to-get-covid-19-vaccine/ Sept. 17.
- Van der Linden S., Roozenbeek J., Compton J. Inoculating against fake news about COVID-19. Frontiers in Psychology. 2020;11:2928. doi: 10.3389/fpsyg.2020.566790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verger P., Dubé E. Restoring confidence in vaccines in the COVID-19 era. Expert Review of Vaccines. 2020;19(11):991–993. doi: 10.1080/14760584.2020.1825945. [DOI] [PubMed] [Google Scholar]
- Walkowiak M.P., Walkowiak D. Predictors of COVID-19 vaccination campaign success: Lessons learnt from the pandemic so far. A case study from Poland. Vaccines. 2021;9(10):1153. doi: 10.3390/vaccines9101153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wawrzuta D., Jaworski M., Gotlib J., Panczyk M. Characteristics of antivaccine messages on social media: Systematic review. Journal of Medical Internet Research. 2021;23(6) doi: 10.2196/24564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Global Health. 2020;5(10) doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Włodarczyk W.C. Vol. 2. 2020. Uwagi o pandemii Covid-19 w Polsce. Perspektywa polityki zdrowotnej. Zdrowie Publiczne i Zarządzanie, 2020. [Google Scholar]
- Włodarczyk W.C. Vol. 2. 2020. Uwagi o pandemii Covid-19 w Polsce. Perspektywa polityki zdrowotnej. Zdrowie Publiczne i Zarządzanie, 2020. [Google Scholar]
- Wnuk A., Oleksy T., Maison D. The acceptance of Covid-19 tracking technologies: The role of perceived threat, lack of control, and ideological beliefs. PloS one. 2020;15(9) doi: 10.1371/journal.pone.0238973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation Ten threats to global health in 2019. 2019. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 Available from:
- Young R., Johnson D.R. Handling missing values in longitudinal panel data with multiple imputation. Journal of Marriage and Family. 2015;77(1):277–294. doi: 10.1111/jomf.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y., Luo S., Mo P.K.H., Wang S., Zhao J., Zhang G., Lau J.T.F. Prosociality and social responsibility were associated with intention of COVID-19 vaccination among university students in China. International journal of health policy and management. 2021:1–8. doi: 10.34172/ijhpm.2021.64. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Shao W., Chen X., Zhang B., Wang G., Zhang W. Real-world effectiveness of COVID-19 vaccines: A literature review and meta-analysis. International Journal of Infectious Diseases. 2022;114:252–260. doi: 10.1016/j.ijid.2021.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]