Abstract
Background
Studies have shown improved survival of newborn infants maintained in the thermoneutral range. Incubators with a double plexiglass wall for additional insulation may help to provide an improved thermoneutral environment for very low birth weight infants.
Objectives
To assess the effects of double walled incubator versus a single wall incubator on insensible water loss, rate of oxygen consumption, episodes of hypothermia, time to regain birth weight, duration of hospitalization and infant mortality in premature infants.
Search methods
The standard search strategy of the Cochrane Neonatal Review Group was used. This included searches of electronic databases: Oxford Database of Perinatal Trials, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2006), MEDLINE (1966 to 2006), EMBASE, previous reviews including cross references, abstracts, conference and symposia proceedings, expert informants in all published languages, and CINAHL (1982 to 2006). The electronic search was updated in July 2009.
Selection criteria
Only studies using random or quasi‐random methods of allocation were considered for this review. Eligible studies assessed at least one of the outcome variables identified as important to this topic.
Data collection and analysis
Independent data extraction and quality assessment of included trials was conducted by the review authors. Data were analyzed using generic inverse variance methodology and weighted mean difference (WMD). Results are presented with 95% confidence intervals. Meta‐analysis was undertaken using a fixed effect model.
Main results
Three studies met the criteria. Four other studies were excluded, as they did not compare double versus single wall incubators. Double wall incubators have the advantage of decreasing heat loss, decreasing heat production and decreasing radiant heat loss when compared to single wall incubators. There is also the advantage of reduced oxygen consumption. A minimal increase in conductive heat loss was noted when compared to single wall incubators. All of these effects are small and do not support the proposition that double wall incubators have a beneficial effect on long‐term outcomes including mortality or the duration of hospitalization.
Authors' conclusions
Although it appears that caring for extremely small infants in double wall incubators may theoretically result in shorter hospitalization and may have metabolic advantages, this review was unable to find any data in the literature to support or refute this hypothesis. The studies do not provide any evidence that the small decrease in heat loss improves clinical outcome. Therefore, the available data is insufficient to directly guide clinical practice.
Plain language summary
Double wall versus single wall incubator for reducing heat loss in very low birth weight infants in incubators
Newborn infants maintained in the appropriate temperature range have a better chance of surviving. When newborn infants are within the appropriate temperature range, they burn less energy and have improved growth. The concept of an incubator with additional insulation, namely a double wall of plexiglass, is appealing as it may help very low birth weight infants maintain this appropriate temperature environment. We assessed the effects of double wall incubators compared to single wall incubators on the energy needs and water balance of very low birth weight infants. In addition, we looked at important clinical outcomes such as growth, length of hospital stay and survival. Three studies were found that met our criteria. The double wall incubators had advantages as far as decreasing heat loss and decreasing heat production. These infants seemed to be in the best temperature range, as their need to burn energy was less. However, these effects were small and did not provide any evidence of any long‐term improvement regarding duration of hospitalization or survival. Although it appears that caring for extremely small infants in double wall incubators may result in certain metabolic advantages, this review was unable to find any data in the literature to support or refute this theory. Available data is insufficient to directly guide clinical practice.
Background
Description of the condition
An association between survival of the newborn and environmental temperature has been long recognized. Incubators were first used by the obstetrician Tarnier in Paris in the 1830s (Berthod 1887; Southwick 1890). In the United States, commercial manufacture of an incubator was first begun in 1893. With the end of World War II, newly designed incubators with walls made of thin lucite were introduced. The practice of placing infants in these transparent boxes, without clothing, quickly became routine. Silverman and colleagues, in a series of randomized controlled trials published in the 1950's and 1960's using humidity and varying ambient temperatures, showed that the survival of the premature infant could be increased by reducing heat loss by either increasing ambient temperature or by increasing ambient humidity (Silverman 1957; Silverman 1958).
Description of the intervention
The modern incubator incorporates a transparent plastic hood with various access ports. A warming device is positioned under the bed surface and air is forced over the warming element. The infant's temperature is regulated by controlling the air temperature within the hood (to provide an optimal thermoneutral environment) or by servo‐controlling the heating device to the infant's skin temperature. Four different modes of heat loss (conduction, convection, radiation and evaporation) are involved in the maintenance of a stable body temperature. Heat transfer by conduction occurs directly from the skin of the infant to the mattress surface. Convection is dependent on air flow, which is kept at a minimum, and on air temperature (not permitted to exceed 39oC) in the incubator. Radiation is direct heat transfer by electromagnetic radiation in the infrared spectrum. Heat may be gained by radiation if an external radiant energy source is used, or lost by radiation to the cooler walls of the incubator. Evaporative processes result in heat loss from the baby and can be limited by providing maximum relative humidity within the incubator.
How the intervention might work
The relative importance of the four mechanisms of heat loss (convection, conduction, radiation and evaporation) were studied in the 1950's and 1960's for a clothed infant cared for in a bassinet and for a naked infant cared for in an incubator. Nursing a naked infant in a single wall incubator, heated convectively by recirculating warm air, resulted in an increase in heat loss by radiation to the cool walls of the incubator. Raising the incubator air temperature reduced this radiation loss by reducing the differential between the infant and the now warmer walls of the incubator. Double wall incubators (with an additional inner wall suspended several centimeters from the outer wall), were introduced in the 1980's. Radiant heat loss to the walls of the incubator (inner walls) directly exposed to the infant's skin was significantly reduced in the double wall incubators. Paradoxically, convective heat loss was higher because less warm air temperature was required to warm the infant when radiant heat loss was thus reduced. Double wall incubators were found to be especially helpful in the maintenance of a stable temperature in infants less than 1500 gms. Studies in the 1960's showed that a carefully regulated skin temperature at 36oC further reduced the death rate of low birth weight infants (Buetow 1964; Day 1964).
The exchange of heat between the infant's skin and the environment is influenced by the metabolic rate, insulation and permeability of the skin, as well as environmental factors such as the ambient temperature and humidity. The ability of an infant to maintain a normal temperature is dependent on the relative role each of these mechanisms of heat loss play and the ability of the infant's metabolic processes to compensate for these heat losses. A thermoneutral environment has been defined as the temperature at which the metabolic rate and oxygen consumption are the lowest. Silverman, Sinclair and Agate showed that oxygen consumption was lowest when the infant's temperature had been regulated by servo‐controlling the air temperature to maintain a constant abdominal skin temperature between 36.2 and 36.5oC (Silverman 1966).
Objectives
The primary objective of this review is to evaluate the effect of using double wall incubators versus single wall incubators on neonatal morbidity and mortality in premature infants. Secondary objectives include assessment of the effect of double versus single wall on the rate of insensible water loss, rate of oxygen consumption, episodes of hypothermia, time to regain birth weight and duration of hospitalization.
Methods
Criteria for considering studies for this review
Types of studies
All randomized or quasi‐randomized controlled trials that test the effects of double wall versus single wall incubators on preterm infants.
Types of participants
Preterm infants (defined as less than 37 weeks or 2500 gms) cared for in incubators. All preterm infants will be included (clothed or unclothed).
Types of interventions
Double versus single wall incubators; with or without humidification; duration of treatment ‐ from birth to at least two weeks of age.
Types of outcome measures
Primary outcomes
Death (postnatal age and by birth weight if data permits) prior to hospital discharge.
Secondary outcomes
Oxygen consumption (metabolic rate).
Length of hospitalization (days).
Time to regain birth weight (days).
Incidence of PDA.
A priori subgroup analysis:
infants tested under isothermic body temperature conditions (servo‐control of skin temperature)
with or without added humidification
clothed versus unclothed
preterm < 28 weeks gestation or birthweight < 1000 gms
preterm < 32 weeks gestation or birthweight < 1500 gms
Search methods for identification of studies
Electronic searches
The standard strategy of the Cochrane Neonatal Review Group was used. This included searches of the Oxford Database of Perinatal Trials, The Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2006), MEDLINE (1966 to 2006), and EMBASE. Only studies using random or quasi‐random methods of allocation were considered for this review. Eligible studies were selected if at least one of the outcome variables was identified a priori as important to this topic. Search terms: incubator, isolette, heat, heating, body temperature, body temperature regulation, MeSH terms infant‐newborn and publication type clinical‐trial, randomized‐controlled‐trials).
In July 2009, we updated the search as follows: MEDLINE (search via PubMed), CINAHL, EMBASE and CENTRAL (The Cochrane Library) were searched from 2006 to 2009. Search terms: incubator OR isolette OR heat OR heating OR body temperature OR body temperature regulation. Limits: human, infant and clinical trial. No language restrictions were applied.
Searching other resources
The search also included previous reviews including cross references, abstracts, conference and symposia proceedings and expert informants in all published languages.
Data collection and analysis
The standard review methods of the Cochrane Neonatal Review Group as documented in The Cochrane Library were used.
Selection of studies
The primary review author (NL) assessed the content of all reports retrieved by the search strategy to determine by title and abstract, if possible, those articles that were relevant to the question. The criteria for relevance were: Double wall compared to single wall incubators; human; premature infants; measured outcomes (at least one)
The second review author (DLP) also reviewed a random 20 retrieved references to determine if there was consistency in this initial screening to select the relevant reports. All relevant reports are discussed (included or excluded) in this review.
Data extraction and management
All publications retrieved from the search and deemed relevant by initial screening were reviewed independently by the two review authors with the second review author being blinded to the trial authors and institution. The two review authors then independently extracted the outcome data from each of the reports that were included in the meta‐analysis. The methodological quality of each trial was assessed by the two review authors (NL, DLP) and then compared, with any differences resolved following discussion.
Assessment of risk of bias in included studies
The systematic review followed the method described in the Cochrane Collaboration Handbook. Assessment was done independently by both review authors to determine whether each report should be included or excluded from the meta‐analysis. Methodological quality assessment was performed with consideration of four major sources of potential bias and methods of avoidance as follows: 1. Selection bias ‐ blinding of randomization 2. Performance bias ‐ blinding of intervention 3. Attrition bias ‐ complete follow‐up 4. Detection bias ‐ blinding of outcome assessment
The reviewer authors (NL, DLP) made a judgement whether each of the criteria for method of avoidance of bias was met. Each criterion was given a rating of either "A" if Yes (Adequate), "B" if Can't Tell (Unclear), or "C" if No (Inadequate) and potential impact considered.
For the updated review in 2009, the Risk of Bias table was completed. The two review authors independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions. Any disagreement was resolved by discussion.
The Risk of Bias table addressed the following questions:
1. Sequence generation: Was the allocation sequence adequately generated?
For each included study, we described the method used to generate the allocation sequence as: adequate (any truly random process e.g. random number table; computer random number generator); inadequate (any nonrandom process e.g. odd or even date of birth; hospital or clinic record number); or unclear.
2. Allocation concealment: Was allocation adequately concealed?
For each included study, we described the method used to conceal the allocation sequence as: adequate (e.g. telephone or central randomization; consecutively numbered sealed opaque envelopes); inadequate (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or unclear.
3. Blinding of participants, personnel and outcome assessors: Was knowledge of the allocated intervention adequately prevented during the study? At study entry? At the time of outcome assessment?
For each included study, we described the methods used to blind study participants and personnel from knowledge of which intervention a participant received. We assessed the methods as: adequate, inadequate or unclear for participants; adequate, inadequate or unclear for study personnel; and adequate, inadequate or unclear for outcome assessors and specific outcomes assessed.
4. Incomplete outcome data: Were incomplete outcome data adequately addressed?
For each included study and for each outcome, we described the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. We assessed methods as: adequate (< 20% missing data); inadequate (≥ 20% missing data) or unclear.
5. Selective outcome reporting: Are reports of the study free of suggestion of selective outcome reporting?
For each included study, we assessed the possibility of selective outcome reporting bias as: adequate (where it is clear that all of the study's pre‐specified outcomes and all expected outcomes of interest to the review have been reported); inadequate (where not all the study's pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported); or unclear.
6. Other sources of bias: Was the study apparently free of other problems that could put it at a high risk of bias?
For each included study, we described any important concerns regarding other possible sources of bias (for example, whether there was a potential source of bias related to the specific study design or whether the trial was stopped early due to some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as: yes; no; or unclear.
Measures of treatment effect
Standard methods of Cochrane Neonatal Review Group with the use of relative risk and risk difference with 95% confidence intervals for continuous data was used in the analysis. The weighted mean difference with 95% confidence intervals was calculated for outcomes measured on a continuous scale. If appropraite, we planned on reporting the number needed to treat. The inverse variance methodology, more applicable to the meta‐analysis of crossover studies, was used. Two studies ((Bell 1983; Marks 1981) had adequate data available for analysis. For the Yeh 1980 study, we did not have access to the raw data. We only had access to the estimated means, standard deviations (SDs) and standard errors (SEs) separately for double wall and single wall incubators. The mean difference in each measure (double minus single) was easily estimated as just the differences in the corresponding means. However, estimates of the SDs and SEs for the differences could not be directly obtained. For two random variables, X and Y, the variance of the difference X‐Y is var(X)+var(Y)‐2cov(X,Y). Because we did not have access to the raw data, we could not estimate the covariance. However, we expect the correlation (and hence covariance) to be positive. Therefore, an upper bound on the variance can be obtained by setting cov(X,Y) to 0. For each measure, we obtained estimates of the SDs and SEs of the differences using this approach. These estimates are likely conservative (too large). In the meta‐analysis, the results from Yeh 1980 study will be slightly down weighted (due to overestimated SEs). We believe this is an appropriate approach, as, intuitively, it makes sense to down weight a study for which we have less information. An alternative approach would be to estimate the covariance for each measure from the other two studies. However, this could potentially result in an underestimate of the SEs in the Yeh 1980 study (if the covariance in that study were less than that from the other studies), and putting too much weight on that study in the meta‐analysis. Adequate data was not available for analysis and authors of the study could not be reached to obtain raw data from the crossover trial. Subgroup analyses were performed as proposed when data permitted. JR assisted with the statistical analyses.
Assessment of heterogeneity
We examined heterogeneity between trials by inspecting the forest plots and quantifying the impact of heterogeneity using the I‐squared statistic. If we detected statistical heterogeneity, we planned to explore the possible causes (for example, differences in study quality, participants, intervention regimens, or outcome assessments) using post hoc sub group analyses.
Data synthesis
Meta‐analysis was performed using Review Manager software (RevMan 5) supplied by the Cochrane Collaboration. For estimates of typical relative risk and risk difference, we planned to use the Mantel‐Haenszel method. For measured quantities, we used the inverse variance method. All meta‐analyses were to be done using the fixed effect model.
Subgroup analysis and investigation of heterogeneity
Proposed a priori subgroup analysis included:
infants tested under isothermic body temperature conditions (servo‐control of skin temperature);
with or without added humidification;
clothed versus unclothed;
preterm < 28 weeks gestation or birthweight < 1000 gms;
preterm < 32 weeks gestation or birthweight < 1500 gms.
Results
Description of studies
Included studies
Three studies were included in the review (Bell 1983;Marks 1981;Yeh 1980). Details of the studies are included in the table, Characteristics of Included Studies.
Participants in the included trials were similar. All three studies enrolled preterm neonates (gestational age 30 to 35 wks), who were appropriate for gestational age (between 10 and 90th percentile) with the exception of Marks 1981, where three of the 15 babies studied were small for gestational age (SGA). Infants were two to nineteen days old at the time of testing. All of the three studies were performed in a quiet, temperature controlled room on the same day. The studies did not assess any long term outcomes.
Temperature measurements were made every fifteen minutes (Bell 1983) or every half hour (Marks 1981; Yeh 1980). Oxygen consumption and carbon dioxide production were measured by open circuit technique in all three studies. Barometric pressure was recorded from an aneroid barometer, and relative humidity inside the incubator was determined from wet bulb and dry bulb temperatures (Bell 1983; Marks 1981), and precalibrated standard hygrometer (Yeh 1980). Infant heart rate and respiratory rate were recorded every 15 minutes. No other outcomes were measured.
Heat production was calculated using VO2 and VCO2 (Bell 1983;Yeh 1980). Heat production was not reported by Marks 1981.
None of the studies measured mortality or morbidity under these conditions. No other hospitalization data was discussed in any study.
Excluded studies
A further four studies (Bell 1983 (b); Chessex 1988; Sarman 1992; Short 1998) were identified that evaluated premature infants in double or single wall incubators. These studies were excluded as they did not use human subjects, or compared two double wall incubators under differing conditions.
Risk of bias in included studies
Each of the included studies was a crossover design with the infant serving as his own control. The studies were quasi randomized (Marks 1981 replicated latin square design; Yeh 1980 sequence of study conditions alternated; Bell 1983 assigned order, but no details stated). None of the studies attempted blinding of intervention or outcome. Yeh 1980 did not explain why or how 15 studies were carried out in 10 infants (multiple attempts were made to contact the authors) and Marks 1981 intended to study 15, but excluded five infants (one for tachycardia and the other four for failure to establish thermal equilibrium within the time period of the experiment).
Only short term outcomes including oxygen consumption, heat production and heat loss, physiologic parameters (heart and respiratory rate), and heat exchange data were reported in the studies. Each outcome was measured for three to five and one‐half hours under each experimental condition. Given the crossover design, no attempt was made by the authors to study any long term outcome (i.e. death, length of hospitalization, time to regain birthweight, incidence of PDA). Marks 1981 did not state whether infants were clothed or naked, while Yeh 1980 and Bell 1983 studied all infants naked and did not make any comparisons with clothed infants. No infants smaller than 30 weeks were studied by any of the authors, therefore, no data are available for the smaller gestational age infants. No data are available for infants < 1200 gms or for those small or large for gestational age.
Effects of interventions
The results of three crossover trials with a total of 28 infants (33 observations) are presented in this review. The data were analyzed using the weighted mean difference with 95% confidence intervals in RevMan 4.2 software. As stated in the methodology, weighted mean differences were used given the constraints of the available data.
Comparison 01: Double wall versus single wall incubators Oxygen consumption (Outcome 1.1): All three studies examined oxygen consumption as an outcome parameter. Two studies (Marks 1981; Yeh 1980) reported reduction in oxygen consumption for infants managed in double wall incubators, whereas Bell 1983 did not find any difference in the oxygen consumption in double wall versus single wall incubators when the abdominal wall temperature was regulated by servo‐control. In the overall analysis comparing double wall versus single wall incubators, there was a decrease in oxygen consumption in infants nursed in double wall incubators when compared to single wall incubators [WMD ‐0.59 (95% CI ‐1.09, ‐0.09)].
Heat production and heat loss (Outcome 1.2): Both Bell 1983 and Yeh 1980 studied heat production and heat loss. Both studies servo‐controlled abdominal skin temperature to 36.5oC. There was an apparent reduction in total heat production in the double wall incubator [WMD ‐0.27 (95%CI ‐0.37, ‐0.17)] and Yeh 1980 showed a reduction in heat loss in the double wall incubator. However, this effect was not borne out in the meta‐analysis of the two studies [WMD ‐0.17 (95% CI ‐0.41, 0.06)]. Bell 1983 did not show any significant difference in heat storage, but Yeh 1980 was able to demonstrate a statistically significant advantage in heat storage under the conditions of the double wall incubator. Overall, heat storage was favored in the single wall incubator [WMD 0.11 (95%CI 0.06, 0.16)]. Heat exchange (Outcome 1.3): No significant difference in evaporative heat loss was demonstrated by Bell 1983 and Yeh 1980. Under the conditions of servo‐control of skin temperature, Bell 1983 noted that the double wall incubator caused a reduction in radiant heat loss [WMD 0.86 (95% CI 0.76, 0.98)], with an increase in the convective heat loss [WMD 1.38 (95% CI 1.03, 1.84)]. Incubator temperatures(Outcome 1.4): Incubator air temperature was not significantly different in the two modes [WMD ‐0.21 (95% CI ‐0.48, 0.06)] (Bell 1983; Marks 1981; Yeh 1980). The incubator outer wall temperature was higher in the single wall incubator [WMD 0.78 (95% CI 0.57, 0.99)].
Infant temperatures (Outcome 1.5): All three studies reported abdominal wall temperatures and two studies reported rectal temperatures (Bell 1983; Yeh 1980). Abdominal wall temperatures were higher in the double wall incubator [WMD 0.15 (95% CI 0.08, 0.22)]. No significant difference was noted in the rectal temperatures [WMD 0.05 (95% CI ‐0.03, 0.13)].
Physiologic parameters (Outcome 1.6): Heart rate and respiratory rates were reported by Marks 1981 and Yeh 1980. No significant differences were noted during the study conditions in either environment.
Operative conditions (Outcome 1.7): Operative temperature was reported by Bell 1983 and Yeh 1980, and operative air humidity inside the incubators was reported by Marks 1981 and Yeh 1980. Operative air temperature was higher in the single wall incubator [WMD 0.51 (95% CI 0.22, 0.81)]. No difference was noted in the study environment with respect to incubator air humidity.
Discussion
This review includes three trials that evaluated the short term effects of double wall incubators versus single wall incubators in 28 infants 1200 to 1890 gms. All studies used the crossover design, limiting them to the study of short term effects only. No publications were identified regarding clinical outcomes, such as effects on length of hospitalization, fluid balance, time to regain birthweight or survival.
Two of the three studies (Marks 1981; Yeh 1980) demonstrated that operative conditions like humidity were similar under both experimental conditions. Two of the three studies (Bell 1983; Yeh 1980) used servo‐control to regulate the infants temperature. In the study of Marks 1981, the incubator temperature was similar in both experimental groups. It has been argued that the single wall incubator would require a higher air temperature because of the cooler outer wall (Bell 1983). Therefore, perhaps the infants cared for in single wall incubator were below the thermoneutral zone, leading to a higher metabolic rate under those conditions. Contrary to expectation, heat storage was favored in the single wall incubators. Heat storage is of special importance in a period of growth. Energy storage is the major factor contributing to the energy cost of growth. Bell 1983 and Yeh 1980 used servo‐control for maintaining the skin temperatures at 36.5oC. Despite the use of servo‐control, Yeh 1980 was able to show a significant difference in abdominal wall temperatures between the two study conditions. In their study, the infants in a double wall incubator had higher abdominal wall temperatures. Bell 1983 criticized the study as the mean abdominal temperature was < 36oC in the single wall incubator, suggesting that these infants were not in the thermoneutral zone and, therefore, had higher metabolic rates. Bell 1983 was able to show a difference in the incubator air temperature and temperature of the inner incubator wall in the double wall incubator as compared to the single wall incubator, suggesting that there was a higher radiant heat loss to the cooler walls of the single wall incubator. They also showed that there was an increase in convective loss (skin to air gradient). No other studies made these comparisons.
Bell 1983 concluded that under the conditions of servo‐control, there was no clear advantage to double wall incubators. However, they suggested that the double wall incubator may offer added protection against rapid fluctuations in ambient air temperature when the incubator doors were opened. No studies actually tested this hypothesis.
Each of these studies used a very small sample size, and the crossover trial design did not lend itself to the study of any long term outcomes. Further randomized controlled trials in which larger numbers of infants are allocated to double wall incubator versus single wall incubator from birth to 32 ‐ 34 weeks gestation during their hospitalization are necessary, especially in the smaller premature infants. Many long term issues need to be addressed: thermal and non thermal effects, mortality, morbidity including intraventricular hemorrhage, patent ductus arteriosus, bronchopulmonary dysplasia, incidence of nosocomial infections. Other effects such as time to regain birth weight, overall rate of growth and time to discharge will be important outcomes in order to guide clinical practice. It will be important to evaluate conditions such as addition of humidity, use of clothing, and sleep regulation.
Authors' conclusions
Implications for practice.
Double wall incubators have the advantage of decreasing heat loss, decreasing heat production, and slightly reducing radiant heat loss when compared to single wall incubators. There is also an advantage in reduced oxygen consumption. A slight increase in conductive heat loss is noted. All of these effects are small. Because the studies only looked at immediate outcomes, it is not known if these short term outcomes continue over the duration of hospitalization. The results of these studies do not provide any evidence demonstrating the long term effects of these changes in the various compartments of heat loss and gain. They do not provide any evidence to directly guide clinical practice.
Implications for research.
Although caring for extremely small infants in double wall incubators may theoretically result in improvements in long term clinical outcomes such as shorter hospitalization, and may have metabolic advantages, this review is unable to find any data in the literature to support or refute this hypothesis. Randomized trials with sufficient numbers of infants are needed. Special emphasis should be placed on studying the extremely low birth weight infant. Studies should include appropriate, small and large for gestational age infants. Special care is needed in the design of the studies so that not only short term and immediate clinical consequences are studied, but also clinically relevant outcomes such as weight gain, duration of hospitalization and other clinically relevant morbidities.
What's new
| Date | Event | Description |
|---|---|---|
| 22 December 2009 | New search has been performed | This review updates the existing review "Double wall versus single wall incubator for reducing heat loss in very low birth weight infants in incubators" published in the Cochrane Database of Systematic Reviews (Laroia 2007). Updated search found no new trials. No changes to conclusions. |
History
Protocol first published: Issue 2, 2003 Review first published: Issue 2, 2007
| Date | Event | Description |
|---|---|---|
| 15 September 2008 | Amended | Converted to new review format. |
Acknowledgements
The Cochrane Neonatal Review Group has been funded in part with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
Data and analyses
Comparison 1. Double wall versus single wall Incubator.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Oxygen consumption | 3 | 66 | Oxygen consumption (Fixed, 95% CI) | ‐0.59 [‐1.09, ‐0.09] |
| 2 Heat production and heat loss | 2 | Heat production (Fixed, 95% CI) | Subtotals only | |
| 2.1 Heat production | 2 | 46 | Heat production (Fixed, 95% CI) | ‐0.27 [‐0.37, ‐0.17] |
| 2.2 Heat loss | 2 | 46 | Heat production (Fixed, 95% CI) | ‐0.17 [‐0.41, 0.06] |
| 2.3 Heat storage | 2 | 46 | Heat production (Fixed, 95% CI) | 0.11 [0.06, 0.16] |
| 3 Heat exchange data | 2 | Heat exchange (Fixed, 95% CI) | Subtotals only | |
| 3.1 Evaporative heat loss | 2 | Heat exchange (Fixed, 95% CI) | 0.93 [0.81, 1.06] | |
| 3.2 Radiant heat loss | 1 | Heat exchange (Fixed, 95% CI) | 0.86 [0.76, 0.98] | |
| 3.3 Convective heat loss | 1 | Heat exchange (Fixed, 95% CI) | 1.38 [1.03, 1.84] | |
| 4 Incubator temperatures | 3 | Incubator measures (Fixed, 95% CI) | Subtotals only | |
| 4.1 Incubator air | 3 | Incubator measures (Fixed, 95% CI) | ‐0.21 [‐0.48, 0.06] | |
| 4.2 Incubator ‐ inner wall | 3 | Incubator measures (Fixed, 95% CI) | 1.48 [1.09, 1.88] | |
| 4.3 Incubator wall ‐ outer wall | 2 | Incubator measures (Fixed, 95% CI) | 0.78 [0.57, 0.99] | |
| 5 Infant temperatures | 3 | Infant temperatures (Fixed, 95% CI) | Subtotals only | |
| 5.1 Abdominal wall temperature | 3 | 66 | Infant temperatures (Fixed, 95% CI) | 0.15 [0.08, 0.22] |
| 5.2 Rectal temperature | 2 | 46 | Infant temperatures (Fixed, 95% CI) | 0.05 [‐0.03, 0.13] |
| 6 Physiologic parameters | 2 | Physiologic (Fixed, 95% CI) | Subtotals only | |
| 6.1 Heart Rate | 2 | 50 | Physiologic (Fixed, 95% CI) | ‐1.71 [‐4.26, 0.84] |
| 6.2 Respiratory rate | 2 | 50 | Physiologic (Fixed, 95% CI) | 0.44 [‐2.35, 3.24] |
| 7 Operative conditions | 3 | Operative conditions (Fixed, 95% CI) | Subtotals only | |
| 7.1 Operative temperature | 2 | Operative conditions (Fixed, 95% CI) | 0.51 [0.22, 0.81] | |
| 7.2 Incubator air humidity | 2 | Operative conditions (Fixed, 95% CI) | 0.46 [‐0.43, 1.35] |
1.1. Analysis.
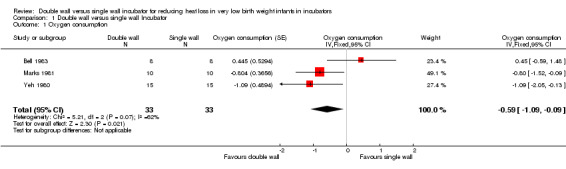
Comparison 1 Double wall versus single wall Incubator, Outcome 1 Oxygen consumption.
1.2. Analysis.
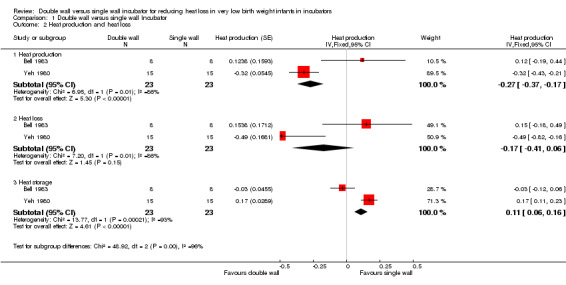
Comparison 1 Double wall versus single wall Incubator, Outcome 2 Heat production and heat loss.
1.3. Analysis.
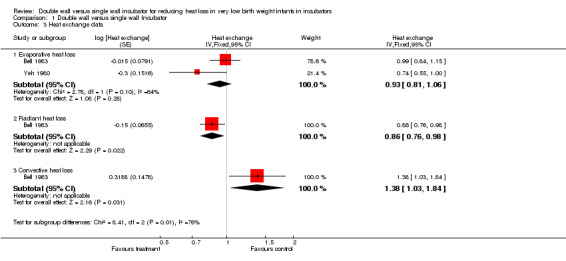
Comparison 1 Double wall versus single wall Incubator, Outcome 3 Heat exchange data.
1.4. Analysis.
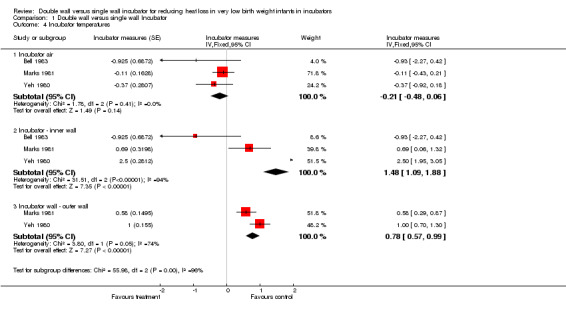
Comparison 1 Double wall versus single wall Incubator, Outcome 4 Incubator temperatures.
1.5. Analysis.
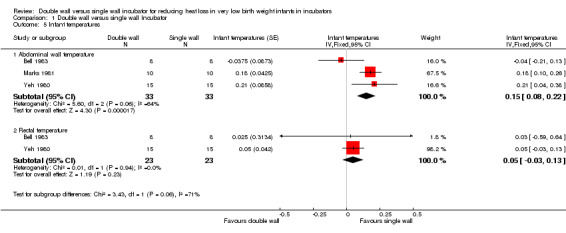
Comparison 1 Double wall versus single wall Incubator, Outcome 5 Infant temperatures.
1.6. Analysis.
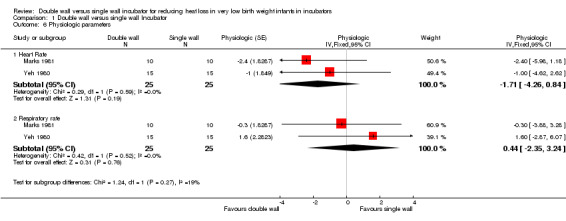
Comparison 1 Double wall versus single wall Incubator, Outcome 6 Physiologic parameters.
1.7. Analysis.
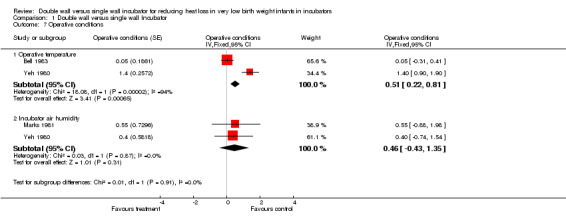
Comparison 1 Double wall versus single wall Incubator, Outcome 7 Operative conditions.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bell 1983.
| Methods | Cross‐over design, quasi‐ randomized, order of subjects: four infants studied first in each incubator. Blinding of randomization ‐ no Blinding of intervention ‐ no Complete follow up ‐ yes Blinding of outcome measure ‐ no | |
| Participants | 8 subjects Birthweight 1440 ‐ 1890 g (median 1540g) Gestational age 30‐35 (median 32 wk), AGA, Age 6‐19 days (median 13.5d) | |
| Interventions | Single vs double walled incubator. Isolette, Air Shields, Model C‐86. Skin temperature at servo‐control at 36.5oC. 2‐period cross‐over, own control. Each infant studied for two, 2 hour periods with 1 hour in between for stabilization. Each infant studied during consecutive periods on the same day. | |
| Outcomes | Oxygen consumption, carbon dioxide production, Body temperatures, heart rate and respiratory rate. Metabolic heat production, heat loss, heat gain, were calculated. | |
| Notes | Infants abdominal skin temperature servo controlled to 36.5 C quiet, temperature controlled room. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Cross‐over design, quasi‐ randomized, order of subjects: four infants studied first in each incubator. Blinding of randomization ‐ no |
| Allocation concealment? | High risk | Blinding of randomization ‐ no |
| Blinding? All outcomes | High risk | Blinding of intervention ‐ no Blinding of outcome measure ‐ no |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete follow up ‐ yes |
Marks 1981.
| Methods | Cross‐over design, quasi‐ randomized, order of subjects: randomization using replicated latin square design. Blinding of randomization ‐ no Blinding of intervention ‐ no Complete follow up ‐ no Blinding of outcome measure ‐ no | |
| Participants | 15 preterm 32‐34 wks (mean 32.7 +‐1.3 SD), 2‐16 days age, results reflect 10 infants (four infants eliminated because of failure to establish thermal equilibrium within the time period of the study). One infant excluded because of tachycardia. | |
| Interventions | Cross‐over design, each infant own control, duration of study 3‐5 1/2 hr period depending on the time required to reach equilibrium. Isolette infant incubator model, C‐86 double wall model. | |
| Outcomes | Oxygen consumption, body temperatures, heart rate and respiratory rate were measured. Room air temperature and relative humidity, and incubator temperatures measured. | |
| Notes | 4 infants excluded as they failed to establish thermal equilibrium within period of study. One infant excluded because of tachycardia to >175 bpm. Experiments in the day, same section of the nursery. Duration of study periods (3‐5 hrs). VO2 measured during quiet sleep Temperature recorded every half hour, skin temp 6 sites, core temp mid esophagus. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Cross‐over design, quasi‐ randomized, order of subjects: randomization using replicated Latin square design. |
| Allocation concealment? | High risk | Blinding of randomization ‐ no |
| Blinding? All outcomes | High risk | Blinding of intervention ‐ no Blinding of outcome measure ‐ no |
| Incomplete outcome data addressed? All outcomes | High risk | Complete follow up ‐ no |
Yeh 1980.
| Methods | Cross‐over design, quasi randomized, sequence of study alternated. Blinding of randomization ‐ no Blinding of intervention ‐ no Complete follow up ‐ yes Blinding of outcome measure ‐ no | |
| Participants | 10 infants BW 1200‐1820g (mean 1444+‐250g), GA 31‐34 wks (32.7+‐ 1.0 wks), AGA, 4‐15 days age. 15 sets of observations made, no details provided about multiple values on infants. | |
| Interventions | Cross‐over design, Single vs double walled incubator. Infant own control, simultaneous measurements of IWL, VO2 under single walled incubator (Ohio Servo Care) and double walled incubator (Ohio Intensive Care). Study Period 3 hrs each condition, sequence of study condition alternated. Insensible water loss measurement using Potter bed scale. | |
| Outcomes | Insensible water loss, oxygen consumption and carbon dioxide production under two conditions. Heat balance was calculated from oxygen consumption. Total heat loss, heat storage, heat loss, heat loss were calculated from temperatures measured. Heart rate and respiratory rate were recorded every 30 minutes. | |
| Notes | Incubators in specific quiet area of nursery, 1m from wall farthest from the window. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Cross‐over design, quasi randomized, sequence of study alternated. |
| Allocation concealment? | High risk | Blinding of randomization ‐ no |
| Blinding? All outcomes | High risk | Blinding of intervention ‐ no Blinding of outcome measure ‐ no |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete follow up ‐ yes |
Abdominal skin temperature was maintained by servocontrol at 36.5 C
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bell 1983 (b) | Performance characteristics of two double walled infant incubators. The study compared two incubators, and evaluated for performance. No human subjects were used. |
| Chessex 1988 | Infants < 1000 g, in two sets of experiments comprising of incubator and infant temperatures were performed under either controlled or standard clinical care. Two different double walled incubators used. No comparison with single walled incubator. |
| Sarman 1992 | Assessment of thermal conditions in neonatal care: use of a manikin of premature baby size. No human subjects, only single walled incubator. |
| Short 1998 | A comparison of temperature in VLBW infants swaddled vs unswaddled in double walled incubator in skin control mode. No comparison with single walled incubator. |
Contributions of authors
Nirupama Laroia (NL) and Dale Phelps (DP) reviewed the literature, NL wrote the text with DP as the editor. The reviewers worked collaboratively on each stage of the review. Jason Roy (JR) assisted with calculations for generic inverse variance.
The recent update (July 2009) was conducted centrally by the Cochrane Neonatal Review Group staff (Yolanda Montagne, Diane Haughton and Roger Soll) and reviewed and approved by NL.
Declarations of interest
None
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bell 1983 {published data only}
- Bell EF, Rios GR. A double‐walled incubator alters partition of body heat loss of premature infants. Pediatric Research 1983;17:135‐40. [DOI] [PubMed] [Google Scholar]
Marks 1981 {published data only}
- Marks KH, Lee CA, Bolan CD Jr, Maisels MJ. Oxygen consumption and temperature control of premature infants in a double‐wall incubator. Pediatrics 1981;68:93‐8. [PubMed] [Google Scholar]
Yeh 1980 {published data only}
- Yeh TF, Voora S, Lillien LD, Matwynshym J, Srinivasan G, Pildes RS. Oxygen consumption and insensible water loss in premature infants in single‐ versus double‐walled incubators. Journal of Pediatrics 1980;97:967‐71. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bell 1983 (b) {published data only}
- Bell EF, Rios GR. Performance charecteristics of two double‐walled infant incubators. Critical Care Medicine 1983;11:663‐7. [DOI] [PubMed] [Google Scholar]
Chessex 1988 {published data only}
- Chessex P, Blouet S, Vaucher J. Environmental temperature control in very low birth weight infants (less than 1000 grams) cared for in double‐walled incubators. Journal of Pediatrics 1988;113:373‐80. [DOI] [PubMed] [Google Scholar]
Sarman 1992 {published data only}
- Sarman I, Bolin D, Holmer I, Tunell R. Assessment of thermal conditions in neonatal care: use of a manikin of premature baby size. American Journal of Perinatology 1992;9:239‐46. [DOI] [PubMed] [Google Scholar]
Short 1998 {published data only}
- Short MA. A comparison of temperature in VLBW infants swaddled versus unswaddled in a double‐walled incubator in skin control mode. Neonatal Network 1998;17:25‐31. [PubMed] [Google Scholar]
Additional references
Berthod 1887
- Berthod, P. La couveuse et le gavage a la Maternite de Paris. Thesis/Dissertation 1887.
Buetow 1964
- Buetow KC, Klein SW. Effect of maintanence of 'normal' skin temperature on survival of infants of low birth weight. Pediatrics 1964;34:163‐70. [PubMed] [Google Scholar]
Chien 1996
- Chien CH, Tsou Yau KI. The influenece of incubator wall on the irradiation intensity of phototherapy. Chung‐Hua Min Kuo Hsiao Erh Ko i Hsueh Hui Tsa Chih 1996;2:92‐5. [PubMed] [Google Scholar]
Day 1964
- Day RL, Caliguiri I, Kamenski C, Ehrlich F. Body temperature and survival of premature infants. Pediatrics 1964;34:171‐81. [PubMed] [Google Scholar]
LeBlanc 1984
- LeBlanc MH. Evaluation of two devices for improving thermal control of premature infants in transport. Critical Care Medicine 1984;12:593‐5. [DOI] [PubMed] [Google Scholar]
Silverman 1957
- Silverman WA, Blanc WA. The effect of humidity on survival of newly born premature infants. Pediatrics 1957;20:477‐87. [PubMed] [Google Scholar]
Silverman 1958
- Silverman WA, Fertig JW, Berger AP. The influence of the thermal environment on the survival of the newly born premature infant. Pediatrics 1958;22:876‐86. [PubMed] [Google Scholar]
Silverman 1966
- Silverman WA, Sinclair JC, Agate FJ Jr. The oxygen cost of minor changes in heat balance of small newborn infants. Acta Paediatrica Scandinavica 1966;55:294‐300. [DOI] [PubMed] [Google Scholar]
Southwick 1890
- Southwick, GR. Care of the weak or prematurely born infants. New England Medical Gazette 1890;25:310. [Google Scholar]
References to other published versions of this review
Laroia 2007
- Laroia N, Phelps D, Roy J. Double wall versus single wall incubator for reducing heat loss in very low birth weight infants in incubators. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD004215.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


