Abstract
The COVID-19 pandemic caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) has negatively impacted the global healthcare and economic systems worldwide. The COVID-19 pandemic has also created an emotional and psychological pandemic among people of all ages irrespective of economic status and physical wellbeing. As a consequence of prolonged lockdowns, one of the most severely affected age groups globally is the young adults' group, especially students. Uncertainties in the academic calendar, restricted outdoor activities, and unusual daily routines during lockdowns led to higher incidences of stress, anxiety, and depression among students worldwide. In this review, we summarise the available evidence on the effect of lockdowns on students and discuss possible positive impacts of yoga and meditation on various psychological, emotional, and immunological parameters, which can significantly influence the general wellbeing and academic performance of students. Perspectives shared in the review will also bring awareness on how yoga and meditation could boost students' performance and assist them in maintaining physical and mental wellbeing during stressful conditions such as future epidemics and pandemics with novel infections. This information could help create better educational curriculums and healthy routines for students.
Keywords: Yoga, Meditation, Students, Stress, Anxiety, Depression, Wellbeing, Immunity
Highlights
-
•
COVID-19 pandemic has created an emotional and psychological pandemic among students.
-
•
Prolonged lockdown, lack of social interaction, and changed lifestyle has led to Stress, Anxiety, and Depression in young adults, including students.
-
•
Yoga and meditation positively impact students' psychological, emotional, and immunological parameters.
-
•
Awareness of yoga and meditation could assist students in maintaining physical and mental wellbeing during stressful conditions.
1. Introduction
On March 11, 2020, COVID-19, caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2), was declared a pandemic by the World Health Organization (WHO). The Coronavirus disease, COVID-19, is primarily a respiratory illness and also shows the symptoms associated with the gastrointestinal tract (GI), hepatobiliary, cardiovascular, renal, and central nervous systems (Luo et al., 2020; Rothan et al., 2020; Vodnar et al., 2020; Wang et al., 2020). The most common symptoms of COVID-19 include fever, cough, fatigue, sputum production, headache, diarrhea, dyspnoea (difficulty in breathing), lymphopenia (reduced lymphocytes in the blood), and may include signs of pneumonia (C. Huang et al., 2020; Ren et al., 2020). A chest CT scan of COVID-19 patients with moderate to severe disease may show signs of pneumonia, acute respiratory distress syndrome, acute cardiac injury, and ground-glass opacities in the lungs (Pullen et al., 2020).
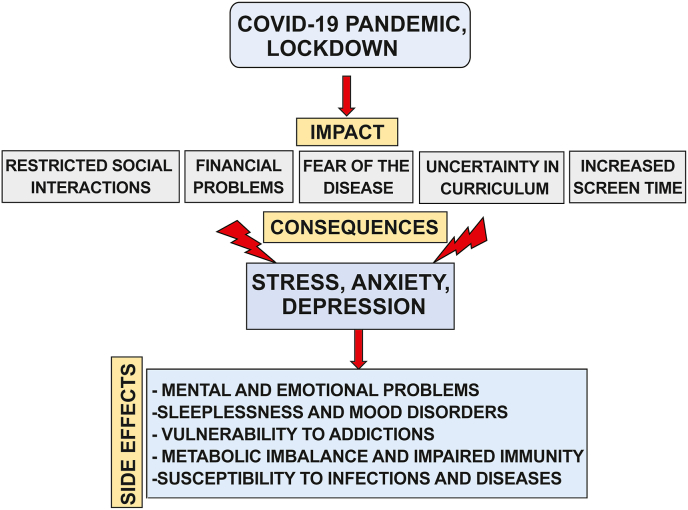
As an immediate and effective measure to stop the spread of the SARS CoV-2 infection and give enough time for the readiness of the hospitals to deal with the increased numbers of A&E attendances and hospitalizations, the governments of most of the countries imposed “lockdowns” (closures of services, businesses and schools, known as “lockdowns”) at different stages of the pandemic and with varying levels of restrictions (Lancet, 2020). The imposition of rigorous home quarantine and social isolation ultimately resulted in significant adverse effects on the psycho-emotional wellbeing of people worldwide (Silva et al., 2021). According to the World Economic Forum, an average of 2.6 billion people worldwide were under social isolation and quarantine, leading to a stress-related disorder pandemic, emotional distress, and psychological consequences in the second half of 2020 (Ganesan et al., 2021). It was also documented that the recovered patients, their family members, and many others went through some degree of common mental disorders, such as depression and anxiety, which affected their quality of life (Grover et al., 2020; Salari et al., 2020; Xiong et al., 2020). According to the latest reports, the utmost elements that created stress, anxiety, and depression were the agitation of getting the SARS CoV-2 infection, loss of loved ones, and financial problems (Al Mamun et al., 2021; Boyraz et al., 2020; Elbogen et al., 2021; Sahni et al., 2021) (Figure-1). Similarly, an electronic health record cohort study performed by the researchers from Oxford University in collaboration with TriNetX, USA, with data from 69 million individuals from which 62, 354 had a diagnosis of COVID-19 between January 2020 to August 2020, showed that survivors of COVID-19 are at higher risk of developing psychiatric sequelae such as depression, posttraumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD) and psychotic symptoms (Maxime Taquet et al., 2021). Besides healthcare, public services, and other aspects of day-to-day life, the education system suffered a considerable setback. The uncertainties about the academic year, examinations, enhanced screen time due to educational resources and lecture delivery being online, restricted social interactions created a tremendous amount of emotional and psychological stress among students all over the globe (Aucejo et al., 2020; Limone et al., 2021). Thus, in addition to physical health, the COVID-19 pandemic has significantly affected the mental health of people of all ages worldwide (Fig. 1).
Fig. 1.
Impacts, consequences, and side effects of the COVID-19 pandemic on students: This figure describes the impacts of the COVID-19 pandemic and associated lockdown on the students' daily life, such as restricted social interaction, fear of contracting SARS CoV-2 infection, uncertainty in academic curriculum, and increased screen time. Such changes during lockdown during COVID -19 pandemic have led to significant stress, anxiety, and depression, causing emotional, psychological, immunological, and metabolic imbalances.
Several lines of evidence have shown that stress can also delay wound healing and compromise immunity through different physiological pathways (Pinto et al., 2016). Long-term stress-related chronic inflammations is also linked with higher risk for several diseases such as cardiovascular disease, cancers, diabetes, and autoimmune diseases (Dhabhar, 2014; Furman et al., 2019; Liu et al., 2017). Several reports have shown that the presence of underlying comorbidities such as cerebrovascular diseases, chronic lung diseases, cancer, diabetes, and hypertension could increase the incidence and severity of SARS COV-2 infection (Callender et al., 2020; Ejaz et al., 2020; Gupta et al., 2021; Honardoost et al., 2021). With current day lifestyle, incidences of diabetes, hypertension, and mental health-related diseases are increasing in young adults (Asif, 2014; Di Renzo et al., 2020; C. Zheng et al., 2020). Such disorders accompanied by stress and chronic inflammatory conditions could impact the general wellbeing and functioning of a healthy immune system to defend against emerging infections (Morens et al., 2004; Netea et al., 2020; Yazdanpanah et al., 2020). Thus, the current scenario could propel humans to equip themselves with ways to overcome the stressful effects of such pandemics and boost their physical and mental wellbeing.
1.1. Yoga and wellbeing
Yoga is considered a sacred practice that is effective in obtaining physical strength, mental balance, and spiritual growth. Yoga includes exercise and relaxation of the mind. Yoga comprises a variety of techniques and practices that include yogic positions (asanas), inhalations or breathing exercises (Pranayama), meditation, chanting of mantras, lifestyle changes, and practicing certain spiritual beliefs (Birdee et al., 2008). A commonly practiced form of yoga is Hatha Yoga that comprises asanas, postures, pranayama, and meditation (Riley, 2004). Yoga has been an essential part of Indian culture for thousands of years to alleviate stress and improve physical wellbeing. People performing meditation reportedly had relatively better mental health (Sahni et al., 2021). Recently, several yogic therapies have also been demonstrated to improve the recovery rate in patients with depression (Sathyanarayanan et al., 2019; Venkatesh et al., 2020). A study conducted by Elstad et al. with 202 healthy students in which 24 yoga interventions were given for 12 weeks showed a significant and long-term effect on reducing distress and improving sleep quality in participants (Elstad et al., 2020). In another study that was conducted between the year 2011–2016 by enrolling students from various yoga schools that practiced different yoga asana (yoga postures) techniques such as Ananda, Ashtanga, Bikram, Iyengar, integral, Kundalini, Power, and Vinyasa, showed that yoga interventions effectively decreased depression among these students (Bridges et al., 2017). In recent times, people have become more aware of the benefits of regular yogic practices (Vagga et al., 2020).
To date, evidence from extensive research on yoga and meditation have provided scientific data supporting yoga and meditation on stress and anxiety management (Breedvelt et al., 2019; Cramer et al., 2014; Manocha et al., 2011; Sarkar et al., 2021; Shohani et al., 2018; Smith et al., 2007). In addition to mental wellbeing, researchers have also endorsed the beneficial effects of regular yogic practices in improving metabolic and vascular functions of the human body (Erogul et al., 2014; Falsafi, 2016; Kim, 2016; Nemati, 2013; Oman et al., 2008; Ross et al., 2015). Besides the extensive beneficial effects of yoga in improving the quality of life and mental health, yoga and meditation have gained popularity for boosting immunity by improving circulation, removing toxins, modulating inflammatory mediators, and strengthening the immune system (Gopal et al., 2011; Sarkar et al., 2021; Venkatesh et al., 2020).
This review focuses on the effect of the COVID-19 pandemic and associated lockdown on the psychological and emotional wellbeing of students. We have also discussed the possible consequences of stress, anxiety, and depression on the immune system and made an effort to present evidence supporting the beneficial effects of yoga and meditation on the wellbeing of students who have faced challenging phases during the COVID-19 pandemic. This understanding could help prepare well for such future epidemics and pandemics that may simulate lockdowns and uncertainties in academic schedules for students.
1.2. Impact of COVID-19 pandemic on the stress, anxiety, and depression in students
According to the literature, the consequence of an adverse situation or very demanding circumstances is termed as stress, which is associated with anxious thoughts, physical, mental and emotional changes (Schneiderman et al., 2005; Trivedi et al., 2010; Yaribeygi et al., 2017). Around 322 million people, or 4.4% of the global population, were affected by depression in 2015 (Friedrich, 2017). Additionally, according to the Global Burden of Disease (GBD) 2010 study, Major Depressive Disorder (MDD) was considered as the primary cause for prolonged dysfunction (Ferrari et al., 2013). Specifically, a prolonged period of the imposed lockdown and the Government restrictions due to COVID-19 have negatively impacted the levels of stress, anxiety, and depression in all groups of people (Al Omari et al., 2020). According to several studies, sleeplessness, addictions with vulnerability for relapse, and psychological symptoms in young adults occur due to excessive stress (Cuijpers et al., 2021; Dessauvagie et al., 2021; Sadeh et al., 2004; Sweileh et al., 2011). Major depressive disorder is a mood disorder that results in a persistent and long-term feeling of sadness and loss of interest. This disorder can affect how one can think, feel, and change behaviour, leading to various physical (e.g., reduced appetite, weight loss, weight gain, tiredness, lack of energy and sleep disturbances), emotional (e.g., feelings of sadness, tearfulness, emptiness or hopelessness, angry outbursts, irritability, and frustrations) and immunological (e.g., increased inflammation, rise in the levels of pro-inflammatory cytokines, glucocorticoids) effects (Bains N, 2021; Lee et al., 2019; Leonard, 2010; Vagga et al., 2020). Depression could affect the quality of life, especially for college students, because they experience the transition from adolescence to adulthood and may encounter different scenarios such as changes in social and family relationships, peer pressure for academic success, academic overload (Reyes-Rodríguez et al., 2013). Another study showed that the clinical depressive symptoms such as hopelessness, loss of pleasure and interest, negative self-thinking, fatigue, and concentration could be more prominent in college students than other groups of populations (Geisner et al., 2006). Teenage students may also face social depressive related behaviours such as internet overuse, smoking, frequent consumption of alcohol, presenting insomnia, and low self-esteem, which are associated with depression, anxiety, and stress (Ramón-Arbués et al., 2020).
As mentioned earlier, after the onset of the COVID-19 pandemic, governments of different countries imposed strict lockdown and social isolation for several months (Lancet, 2020). While the rising cases of SARS-CoV-2 infections and associated mortality aggravated physical and mental trauma, closure of educational institutions without any possibility of their reopening for in-person classes made students of all age groups, especially young adults of intermediate and higher educational institutions, more anxious about their curriculum and future. Many students pursuing specialized educational programs such as medicine, management, and engineering have lost track of the semester completion plans and delays in getting job offers after receiving their degrees (Aucejo et al., 2020). Various factors of the COVID-19 pandemic, such as its evolution, high transmissibility of novel mutations, challenges in vaccination worldwide, and the lack of immunity against the virus, further created a fearful condition for all, including young adults leading to the development of stress, anxiety, and depression (Orellana et al., 2020; Ornell et al., 2020; Rodríguez-Rey et al., 2020). In addition to the above factors, initiation of classes in online mode enhanced the stressful conditions in some families and students due to the non-availability of high-speed internet connections or digital devices and sometimes difficulty in understanding the course contents and the limited access to the online study materials (Alawamleh et al., 2020; Kapasia et al., 2020; Nambiar, 2020).
Screen time refers to the time spent performing online activities using different electronic devices ("Global digital overview," 2020). Initiation of academic and official activities via online mode increased the contact time with electronic devices such as laptops, smartphones, computers, and tablets and increased the screen time. Several reports suggest that radiations emitted by digital devices may negatively impact students' mental health (Limone et al., 2021). Additionally, virtual meetings and reduced social connections during COVID-19 lockdown, lowering students' wellbeing (Pandya et al., 2021; Rosen et al., 2014; Twenge et al., 2018). Thus, the conflicts between the parents and students also became one of the critical factors for increased stress and anxiety among students (Almroth et al., 2019; Behere et al., 2017; Spinelli et al., 2020).
1.3. Effect of yoga and meditation on the factors affecting wellbeing and academic performance in students
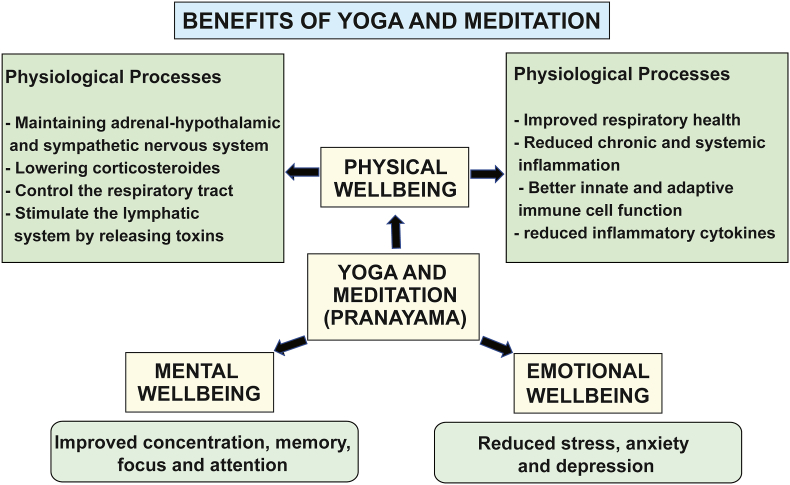
Following the Patanjali yoga sutra, yoga implements ‘Chitta vritti nirodha,’ which means managing or cooling the mind. In conjunction with enhancing physical strength and flexibility, it is also debated that yogic asanas help build attentiveness too (Cowen et al., 2005). In the following paragraphs, we further present the evidence available on the effect of yoga and meditation on various physical and mental wellness factors associated with students' academic performance (Figure-2).
Fig. 2.
Beneficial effects of yoga and meditation for students:
The schematic diagram shows the beneficial effects of regular yogic exercises, pranayama (breathing exercises), and other self-improvement routines in various parameters such as mental (e.g., attention, concentration, memory, alertness, sleep quality), emotional (e.g., reduced stress, anxiety and depression) and physical (e.g., strength, tome and flexibility of musculoskeletal system) wellbeing including physiological processes (e.g., metabolism) and immunological defence mechanisms (respiratory health, reduced inflammation, better innate and adaptive immune cell function) which have influence on academic performance and day today life of students.
1.3.1. Role of yoga and meditation for a healthy life
According to prior research, pranayama or yogic breathing techniques calms the nervous system and aids in maintaining blood pressure and stress responses (Goyal et al., 2014; Shetty et al., 2017). Physical relaxation, consciousness, and exultation are the effects of yogic practices such as Surya namaskar, which is an ancient yogic practice where twelve yoga postures are performed in sequence following a specific breathing pattern (Sun salutation routine) (Rocha et al., 2012). Different studies have ascertained that yoga can bring a productive conversion in mental and physical health by maintaining the adrenal-hypothalamic system, lowering corticosteroids, maintaining the sympathetic nervous system, and enhancing immunity (Arora et al., 2008; Büssing et al., 2012; Woodyard, 2011). Such observations were supported by the findings that yoga practices led to an increase in fasting blood sugar level, heart rate, cholesterol, CD4 T cell response, and LDL (Low-Density-Lipoprotein) irrespective of the age (Joseph et al., 2015; Kiecolt-Glaser et al., 2010; Pascoe et al., 2017). Regular yogic practice regulates the elimination of carbon dioxide and ultimately enhances the body's activeness by increasing peripheral oxygen saturation (Pal et al., 2015). Similarly, practicing yoga, meditation with pranayama are shown to reduce stress hormones and enhance the body's innate immune systems (Lim and Cheong, 2015). Previous studies have also shown a beneficial effect of pranayama in balancing the adrenal-pituitary-hypothalamic axis and inflammatory processes (Bower et al., 2016; Kaliman et al., 2014; Kiecolt-Glaser et al., 2010). Besides, pranayama techniques are also shown to control the respiratory tract, stimulate the lymphatic system, reduce inflammation, and influence virus-specific immune responses to vaccination (Morgan et al., 2014). Moreover, yoga is suggested as one of the non-pharmacological modes of stress management and wellbeing in anxious college students as it triggers neurohormonal mechanisms that bring about health benefits, reduces stress and anxiety, improves autonomic and higher neural centre functioning, and also improves the physical health of cancer patients (Sengupta, 2012).
Physical wellbeing is an essential part of a student's academic life and influences temperament and social performance (Preoteasa et al., 2016). A longer period of inactivity and confinement is known to affect the body's physical functions, such as the musculoskeletal system, whose optimum function is highly essential for young adults and students. Concerning physical wellbeing, it is known that less oxygen supply causes muscles stiffness that ultimately results in restricted body movements, and regular yogic practice helps in the functioning of the joints and tissue flexibility (Lau et al., 2015). Sitting on a bench for a more extended period in case of the students leads to poor blood circulation, which causes fluid retention and swelling within the body, which can be maintained by practicing various yoga postures such as, headstand, inverted poses, and child's pose (Chaya et al., 2008). So yoga could be considered the non-pharmacological way of maintaining physical and mental wellbeing and contributing to maintaining a healthy life and ultimately improving academic performance.
For school and college students, general wellbeing is also reflected in attention, concentration, and memory, which are an essential part of academic performance. Studies have suggested that relaxation is highly essential for good concentration, memory, and attention, which can be achieved by practicing yoga and meditation (Sheela Joice et al., 2018). It is well understood that the students' ability to focus, concentrate, and learn is directly related to academic performance and could be challenged under conditions such as the COVID-19 pandemic (El-Mir, 2019). Yoga and meditation practices are helpful in reducing depression, fear, and tension and is considered a holistic alternative and complementary therapy (Shohani et al., 2018) Importantly, it is shown that students' academic performance increases with the implementation of yoga by adjusting the stress level and helps increase neurological functions such as mental balance and visualization attention, especially in school age students (Kauts et al., 2009). Thus, a habit of practicing yoga and meditation and similar relation techniques can aid in enhancing their concentration, memory, and attention in challenging life events such as the COVID-19 pandemic.
A healthy sleep cycle is highly essential for students' performance (Okano et al., 2019). Lack of physical activity and poor nutrition during confinement periods such as lockdown and stressful conditions can affect the sleep cycle (Gualano et al., 2020). The amount and quality of sleep and circadian rhythm are known to affect the brain's functioning significantly and could alter immunological parameter Sergio (Garbarino et al., 2020). Studies show that regular practice of Surya namaskar is helpful in terms of improving alertness and reducing worry and negative emotions (Rocha et al., 2012). Yogic practices, meditation, and proper sleep contribute to enhancing daily functioning, emotional perception, attentiveness, and mental alertness (Ganpat et al., 2014; Godse et al., 2015; Sheela et al., 2013). Sex hormones influence the susceptibility to various infections, including their possible role in COVID-19 severity and outcomes (Haitao et al., 2020; Marzieh Saei Ghare Naz et al., 2021). Males are more susceptible to infection than females because of sex hormones (Draper et al., 2018; Klein, 2000). The menstrual cycle is one of the physiological rhythms of life that reflects the health of females. It could be associated with discomfort, pain, anxiety, and changes in the sleep cycle (i.e., peri-menstrual symptoms) and may affect the academic performance in females (Fernández-Martínez et al., 2020; Munro et al., 2021). Studies show that systematic yoga practice could have beneficial effects in alleviating such discomfort and symptoms associated with the menstrual cycle in females by stabilizing the neuro-endocrinal axis (Udupa et al., 2003). In conclusion, yoga and meditation could provide many beneficial effects that could help maintain students' physical and mental wellbeing and help with coping with stressful times such as pandemics and lockdowns.
1.3.2. Role of yoga in improving metabolism
The metabolic rate varies from person to person depending on various factors such as age, gender, and muscle to fat ratio, genetic makeup, physical activity, and hormonal balance (Park et al., 2016; Stefano Lazzer, 2012; Vishram et al., 2014). Metabolic rate is also associated with the control of various metabolic mediators (e.g., C reactive protein, IL-6, n-3 fatty acids, lactate), which can boost the body's immunity and promote wellbeing (Huang et al., 2016; Kominsky et al., 2010; Radzikowska et al., 2019; Swanson et al., 2012). The reduced outdoor activities and change in eating patterns experienced during the COVID-19 associated global lockdown became one reason for obesity among young adults (Robinson et al., 2021). Reports suggest that yoga can enhance metabolism and help burn the accumulated adipose tissue due to lifestyle (Na Nongkhai et al., 2021). Maintaining a balanced metabolic rate indicates healthy life, which is essential for the wellbeing and better performance of students (Rioux et al., 2019). Thus, yoga could be an essential tool to maintain good metabolism during the periods of prolonged inactivity, such as lockdowns.
The gut microbiome consists of thousands of organisms that help in food absorption, digestion, and energy production and ultimately enhance the immune system's functioning (Cronin et al., 2016; Mach et al., 2017). Psychological illnesses such as depression, anxiety, and cognitive disorders have been associated with gut microbiome dysbacteriosis (Foster et al., 2013; Nastasi et al., 2015). Thus, to maintain gut health, physical exercise and yoga could be a therapeutic factor as many friendly bacteria such as Lactobacillus and Bifidobacterium genera are known to respond to exercise (Dalton et al., 2019). The gut microbiome is also known to regulate the functions of the immune system. Importantly, microbiota and innate immunity are known to communicate bidirectionally; in other words, the immune systems of the body help in the maintenance of the host-microbes symbiosis. In turn, microbes help develop innate and adaptive immune systems responsible for protecting the body from various infections (Chu and Mazmanian, 2013, Zheng et al., 2020). Under stress-free conditions, a healthy microbiota is known to produce short-chain fatty acids that exert anti-inflammatory and antitumor effects in the absence of stress. Psychological stress is known to trigger the production of corticotropin-releasing hormone and catecholamine in various parts of the body, which may disturb the gut microbiota (Househam et al., 2017; Madison et al., 2019). During stress, an altered gut microbial population could affect the regulation of neurotransmitters mediated by the microbiome and gut barrier function (Carabotti et al., 2015). Reports show that meditation helps regulate the stress response, suppressing chronic inflammation states and maintaining a healthy gut-barrier function (Househam et al., 2017). Yoga and meditation could boost young people's immunity by indirectly affecting the gut microbiome. It could help in maintaining a healthy gut by regulating the stress responses that may trigger chronic inflammation (Househam et al., 2017). In addition, enhanced metabolism, which is one of the beneficial effects of practicing yoga and meditation, could help the students perform better as an associated factor.
1.3.3. Psycho-neuro-immunological effects of yoga and meditation in students
Stress can have significant effects on a variety of physiological systems, including the autonomic nervous system, the hypothalamic-pituitary-adrenal axis, and the immune system (Kemeny, 2003). Reports show that students undergo many short immunomodulating and possibly immunosuppressive stressful conditions during their study career (Kapasia et al., 2020). Two studies conducted on students have demonstrated that examination related stress could change the cytokine profile of the body from Th1 (e.g., IL2, IFNγ) towards Th2 (IL-4, IL-5, IL-6) response (Assaf et al., 2017; Dhabhar, 2014; Duck- Hee Kang, 2001). Thus, it is conceivable that prolonged academic uncertain conditions due to lockdowns could induce immunosuppressive responses in students and can alter their resistance to new infections. For example, examination periods are known to influence immune defences in students (Yasmin et al., 2020).
With the onset of the COVID-19 pandemic, substantial efforts were made to increase scientific research on boosting people's immunity with traditional and natural remedies (Khanna et al., 2021). To this end, yoga, meditation, and Ayurveda emerged as complementary immune boosters (Mishra et al., 2021). Yogic practices are known to regulate the functions of different organ systems of the body such as respiratory, circulatory, digestive, nervous, endocrine, and reproductive systems by altering physiological and psychological processes (Balaji et al., 2012; Sengupta, 2012). Reports show that yogic practices also modulate the functions of immune cells (Arora et al., 2008; Balaji et al., 2012; Sengupta, 2012). For example, in one of the studies, it was demonstrated that the practice of yoga could increase the natural killer cells that are highly important for the body's defence against viruses and tumor cells. This study also showed that yoga could reduce the inflammatory cytokines such as TNF-α and IL-6 (Agarwal et al., 2018; Vijayaraghava et al., 2015). In a meta-analysis of the results from several studies showed that combining pranayama and yogic postures could reduce inflammatory responses in chronic conditions (Djalilova et al., 2019). In the same line, a separate study showed that in rheumatoid arthritis patients practice of yoga significantly reduced the levels of pro-inflammatory cytokines (e.g., IL-6, IL-17, and TNF-α) and increased the levels of anti-inflammatory cytokine TGF-β (Gautam et al., 2020). Besides autoimmune diseases, yoga has therapeutic benefits on inhibiting the replication of hematopoiesis in HIV-1 infected patients (Bhargav H, 2010). The practice of yoga is also shown to prevent infection by increasing the salivary human β-defensin 2 (HBD-2) levels. HBD-2 is an antimicrobial peptide and helps destroy the lipid bilayers and hydrophobic core of microbes (Eda et al., 2013). Interestingly, one of the latest studies by Chandran et al. demonstrated that participation in an eight-day Inner Engineering meditation program resulted in differential expression of 220 genes in study subjects which are directly associated with immune response (Chandran et al., 2021). Additionally, the study showed that meditation could help in reducing oxidative stress, assist with detoxification and cell cycle regulation (Chandran et al., 2021). In conclusion, yoga and meditation could boost immunity in a natural way to maintain psychological wellbeing, which is an important factor in enhancing the overall performance of students.
2. Conclusions
From the presented evidence, it is conceivable that regular practice of yoga and meditation and have the potential to positively impact students' physiological, emotional, and immunological factors, affecting their wellbeing and academic performance. However still, there is a need for in-depth scientific studies exploring the relationship between yoga and students' mental, physical and psychological health. The COVID-19 pandemic has proven to be a wake-up call for humanity in many aspects.
COVID-19 pandemic has provided many lessons on possible issues students may encounter during such stressful times. Higher educational institutions have also strived to adopt innovative approaches such as digital learning platforms to streamline the educational system, facilitate learning and assist students in coping with stressful situations. Similarly, many institutions have also initiated virtual yoga and mindfulness meditation sessions to promote the mental health of their student and faculty. Hopefully, this review persuades the readership that performing a regular yoga routine has many benefits, including physical and mental wellbeing, and can help create a healthier younger generation with robust immune systems, essential to fight emerging infections such as COVID-19. Additionally, during prolonged lockdowns, several measures such as proper nutrition, adequate sleep routine, less exposure to social media and incorrect news, and support from family and institute authorities could help improve wellbeing and reduce anxiety in students. These lifestyle guidelines could be introduced in academic curriculum and traditionally taught alongside physical postures, adding to the holistic benefits that a yoga practice can bring to students.
Thus, adding regular yogic practices and other self-improvement routines to students' academic curriculum and daily practices in co-curricular activities or proficiency programs could help the younger generation take up the day-to-day challenges and stressful situations like lockdowns and pandemics and succeed in their personal and professional life.
Funding support
This work is funded by the Department of Science and Technology, Govt of India (Grant Number: DST/SATYAM/COVID-19/2020/386) to Pranita P. Sarangi and Shikha Jain.
Competing interests
The authors declare no competing interests.
Declaration of competing interest
The authors declare no competing interests.
Acknowledgments
The authors thank Prof. Barry T. Rouse, Distinguished Professor, University of Tennessee, Knoxville, USA, for proofreading the manuscript.
Contributor Information
Nibedita Dalpati, Email: dalpatinibedita1@gmail.com.
Pranita P. Sarangi, Email: pranita.sarangi@bt.iitr.ac.in.
References
- Agarwal R.P., Maroko-Afek A. Yoga into cancer care: a review of the evidence-based research. Int. J. Yoga. 2018;11(1):3. doi: 10.4103/ijoy.IJOY_42_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Mamun F., Hosen I., Misti J.M., Kaggwa M.M., Mamun M.A. Mental disorders of Bangladeshi students during the COVID-19 pandemic: a systematic review. Psychol. Res. Behav. Manag. 2021;14:645–654. doi: 10.2147/PRBM.S315961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Omari O., Al Sabei S., Al Rawajfah O., Abu Sharour L., Aljohani K., Alomari K., Al Zubidi B. Depression research and treatment; 2020. Prevalence and Predictors of Depression, Anxiety, and Stress Among Youth at the Time of COVID-19: an Online Cross-Sectional Multicountry Study. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alawamleh M., Al-Twait L.M., Al-Saht G.R. Asian Education and Development Studies; 2020. The Effect of Online Learning on Communication between Instructors and Students during Covid-19 Pandemic. [Google Scholar]
- Almroth M., László K.D., Kosidou K., Galanti M.R. Academic expectations and mental health in adolescence: a longitudinal study involving parents' and their children's perspectives. J. Adolesc. Health. 2019;64(6):783–789. doi: 10.1016/j.jadohealth.2018.11.015. [DOI] [PubMed] [Google Scholar]
- Arora S., Bhattacharjee J. Modulation of immune responses in stress by Yoga. Int. J. Yoga. 2008;1 doi: 10.4103/0973-6131.43541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asif M. The prevention and control the type-2 diabetes by changing lifestyle and dietary pattern. J. Educ. Health Promot. 2014;3:1. doi: 10.4103/2277-9531.127541. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assaf A.M., Al-Abbassi R., Al-Binni M. Academic stress-induced changes in Th1- and Th2-cytokine response. Saudi Pharmaceut. J. 2017;25(8):1237–1247. doi: 10.1016/j.jsps.2017.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aucejo E.M., French J., Araya M.P.U., Zafar B. The impact of COVID-19 on student experiences and expectations: evidence from a survey. J. Publ. Econ. 2020;191:104271. doi: 10.1016/j.jpubeco.2020.104271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bains N A.S. StatPearls. 2021. Major depressive disorder. [Internet] [Google Scholar]
- Balaji P.A., Varne S.R., Ali S.S. Physiological effects of yogic practices and transcendental meditation in health and disease. N. Am. J. Med. Sci. 2012;4(10):442–448. doi: 10.4103/1947-2714.101980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behere A.P., Basnet P., Campbell P. Effects of family structure on mental health of children: a preliminary study. Indian J. Psychol. Med. 2017;39(4):457–463. doi: 10.4103/0253-7176.211767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhargav H.R.N., Rao N.H., Tekur P., Koka P.S. Potential yoga modules for treatment of hematopoietic inhibition in HIV-1 infection. J. Stem Cell. 2010;5(3):129. [PubMed] [Google Scholar]
- Birdee G.S., Legedza A.T., Saper R.B., Bertisch S.M., Eisenberg D.M., Phillips R.S. Characteristics of yoga users: results of a national survey. J. Gen. Intern. Med. 2008;23(10):1653–1658. doi: 10.1007/s11606-008-0735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower J.E., Irwin M.R. Mind–body therapies and control of inflammatory biology: a descriptive review. Brain Behav. Immun. 2016;51:1–11. doi: 10.1016/j.bbi.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyraz G., Legros D.N., Tigershtrom A. COVID-19 and traumatic stress: the role of perceived vulnerability, COVID-19-related worries, and social isolation. J. Anxiety Disord. 2020;76:102307. doi: 10.1016/j.janxdis.2020.102307. 102307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breedvelt J.J.F., Amanvermez Y., Harrer M., Karyotaki E., Gilbody S., Bockting C.L.H.…Ebert D.D. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: a meta-analysis. Front. Psychiatr. 2019;10:193. doi: 10.3389/fpsyt.2019.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridges L., Sharma M. The efficacy of yoga as a form of treatment for depression. J. Evidence-Based Compl. Alternative Med. 2017;22(4):1017–1028. doi: 10.1177/2156587217715927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Büssing A., Michalsen A., Khalsa S.B.S., Telles S., Sherman K.J. Effects of yoga on mental and physical health: a short summary of reviews. Evid. base Compl. Alternative Med. 2012:165410. doi: 10.1155/2012/165410. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callender L.A., Curran M., Bates S.M., Mairesse M., Weigandt J., Betts C.J. The impact of pre-existing comorbidities and therapeutic interventions on COVID-19. Front. Immunol. 2020:11. doi: 10.3389/fimmu.2020.01991. 1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carabotti M., Scirocco A., Maselli M.A., Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 2015;28(2):203–209. [PMC free article] [PubMed] [Google Scholar]
- Chandran V., Bermúdez M.-L., Koka M., Chandran B., Pawale D., Vishnubhotla R., Sadhasivam S. Large-scale genomic study reveals robust activation of the immune system following advanced Inner Engineering meditation retreat. Proc. Natl. Acad. Sci. Unit. States Am. 2021;118(51) doi: 10.1073/pnas.2110455118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaya M., Ramakrishnan G., Shastry S., Kishore R., Nagendra H., Nagarathna R., Kurpad A. Insulin sensitivity and cardiac autonomic function in young male practitioners of yoga. Natl. Med. J. India. 2008;21(5):217–221. [PubMed] [Google Scholar]
- Chu H., Mazmanian S.K. Innate immune recognition of the microbiota promotes host-microbial symbiosis. Nat. Immunol. 2013;14(7):668–675. doi: 10.1038/ni.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowen V.S., Adams T.B. Physical and perceptual benefits of yoga asana practice: results of a pilot study. J. Bodyw. Mov. Ther. 2005;9(3):211–219. [Google Scholar]
- Cramer H., Lauche R., Dobos G. Characteristics of randomized controlled trials of yoga: a bibliometric analysis. BMC Compl. Alternative Med. 2014;14(1):328. doi: 10.1186/1472-6882-14-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin O., Molloy M.G., Shanahan F. Exercise, fitness, and the gut. Curr. Opin. Gastroenterol. 2016;32(2):67–73. doi: 10.1097/MOG.0000000000000240. [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Miguel C., Ciharova M., Aalten P., Batelaan N., Salemink E.…Karyotaki E. Prevention and treatment of mental health and psychosocial problems in college students: an umbrella review of meta-analyses. Clin. Psychol. Sci. Pract. 2021;28(3):229–244. doi: 10.1037/cps0000030. [DOI] [Google Scholar]
- Dalton A., Mermier C., Zuhl M. Exercise influence on the microbiome–gut–brain axis. Gut Microb. 2019;10(5):555–568. doi: 10.1080/19490976.2018.1562268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessauvagie A.S., Dang H.-M., Nguyen T.A.T., Groen G. Mental health of university students in southeastern asia: a systematic review. Asia Pac. J. Publ. Health. 2021 doi: 10.1177/10105395211055545. 10105395211055545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabhar F.S. Effects of stress on immune function: the good, the bad, and the beautiful. Immunol. Res. 2014;58(2):193–210. doi: 10.1007/s12026-014-8517-0. [DOI] [PubMed] [Google Scholar]
- Di Renzo L., Gualtieri P., Pivari F., Soldati L., Attinà A., Cinelli G.…De Lorenzo A. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J. Transl. Med. 2020;18(1):229. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djalilova D.M., Schulz P.S., Berger A.M., Case A.J., Kupzyk K.A., Ross A.C. Impact of yoga on inflammatory biomarkers: a systematic review. Biol. Res. Nurs. 2019;21(2):198–209. doi: 10.1177/1099800418820162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Draper C.F., Duisters K., Weger B., Chakrabarti A., Harms A.C., Brennan L.…van der Greef J. Menstrual cycle rhythmicity: metabolic patterns in healthy women. Sci. Rep. 2018;8(1):14568. doi: 10.1038/s41598-018-32647-0. 14568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duck-Hee Kang C.F. Th1 and Th2 cytokine responses to academic stress. Res. Nurs. Health. 2001;24(4):245–257. doi: 10.1002/nur.1027. [DOI] [PubMed] [Google Scholar]
- Eda N., Shimizu K., Suzuki S., Tanabe Y., Lee E., Akama T. Effects of yoga exercise on salivary beta-defensin 2. Eur. J. Appl. Physiol. 2013;113(10):2621–2627. doi: 10.1007/s00421-013-2703-y. [DOI] [PubMed] [Google Scholar]
- Ejaz H., Alsrhani A., Zafar A., Javed H., Junaid K., Abdalla A.E.…Younas S. COVID-19 and comorbidities: deleterious impact on infected patients. J. Infect. Public Health. 2020;13(12):1833–1839. doi: 10.1016/j.jiph.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Mir M. Vol. 4. 2019. Impact of Memory on School Performance; pp. 176–188. [DOI] [Google Scholar]
- Elbogen E.B., Lanier M., Blakey S.M., Wagner H.R., Tsai J. Suicidal ideation and thoughts of self-harm during the COVID-19 pandemic: the role of COVID-19-related stress, social isolation, and financial strain. Depress. Anxiety. 2021 doi: 10.1002/da.23162. 10.1002/da.23162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elstad T., Ulleberg P., Klonteig S., Hisdal J., Dyrdal G.M., Bjorndal A. The effects of yoga on student mental health: a randomised controlled trial. Health Psychol. Behav. Med. 2020;8(1):573–586. doi: 10.1080/21642850.2020.1843466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erogul M., Singer G., McIntyre T., Stefanov D.G. Abridged mindfulness intervention to support wellness in first-year medical students. Teach. Learn. Med. 2014;26(4):350–356. doi: 10.1080/10401334.2014.945025. [DOI] [PubMed] [Google Scholar]
- Falsafi N. A randomized controlled trial of mindfulness versus yoga: effects on depression and/or anxiety in college students. J. Am. Psychiatr. Nurses Assoc. 2016;22(6):483–497. doi: 10.1177/1078390316663307. [DOI] [PubMed] [Google Scholar]
- Fernández-Martínez E., Fernández-Villa T., Amezcua-Prieto C., Suárez-Varela M.M., Mateos-Campos R., Ayán-Pérez C.…Alguacil J. Menstrual problems and lifestyle among Spanish university women. Int. J. Environ. Res. Publ. Health. 2020;17(20):7425. doi: 10.3390/ijerph17207425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrari A.J., Charlson F.J., Norman R.E., Patten S.B., Freedman G., Murray C.J.…Whiteford H.A. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10(11) doi: 10.1371/journal.pmed.1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster J.A., Neufeld K.-A.M. Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305–312. doi: 10.1016/j.tins.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Friedrich M.J. Depression is the leading cause of disability around the World. JAMA. 2017;317:1517. doi: 10.1001/jama.2017.3826. [DOI] [PubMed] [Google Scholar]
- Furman D., Campisi J., Verdin E., Carrera-Bastos P., Targ S., Franceschi C.…Slavich G.M. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019;25(12):1822–1832. doi: 10.1038/s41591-019-0675-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganesan B., Al-Jumaily A., Fong K.N.K., Prasad P., Meena S.K., Tong R.K.-Y. Impact of coronavirus disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front. Psychiatr. 2021;12(471) doi: 10.3389/fpsyt.2021.565190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganpat T.S., Dash S., Ramarao N.H. Yoga therapy for promoting emotional sensitivity in University students. J. Educ. Health Promot. 2014;3 doi: 10.4103/2277-9531.131933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbarino S., Lanteri P., Sannita W.G., Bragazzi N.L., Scoditti E. Circadian rhythms, sleep, immunity, and fragility in the elderly: the model of the susceptibility to infections. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.558417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gautam S., Kumar M., Kumar U., Dada R. Effect of an 8-week yoga-based lifestyle intervention on psycho-neuro-immune Axis, disease activity, and perceived quality of life in rheumatoid arthritis patients: a randomized controlled trial. Front. Psychol. 2020;11(2259) doi: 10.3389/fpsyg.2020.02259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner I.M., Neighbors C., Larimer M.E. A randomized clinical trial of a brief, mailed intervention for symptoms of depression. J. Consult. Clin. Psychol. 2006;74(2):393–399. doi: 10.1037/0022-006X.74.2.393. [DOI] [PubMed] [Google Scholar]
- global digital overview 2020. https://datareportal.com/reports/digital-2020-global-digital-overview Retrieved from.
- Godse A.S., Shejwal B.R., Godse A.A. Effects of suryanamaskar on relaxation among college students with high stress in Pune, India. Int. J. Yoga. 2015;8(1):15. doi: 10.4103/0973-6131.146049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopal A., Mondal S., Gandhi A., Arora S., Bhattacharjee J. Effect of integrated yoga practices on immune responses in examination stress - a preliminary study. Int. J. Yoga. 2011;4(1):26–32. doi: 10.4103/0973-6131.78178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal R., Lata H., Walia L., Narula M.K. Effect of pranayama on rate pressure product in mild hypertensives. Int. J. Appl. Basic Med. Res. 2014;4(2):67–71. doi: 10.4103/2229-516X.136776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover S., Sahoo S., Mehra A., Avasthi A., Tripathi A., Subramanyan A.…Janardran Reddy Y.C. Psychological impact of COVID-19 lockdown: an online survey from India. Indian J. Psychiatr. 2020;62(4):354–362. doi: 10.4103/psychiatry.IndianJPsychiatry_427_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gualano M.R., Lo Moro G., Voglino G., Bert F., Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int. J. Environ. Res. Publ. Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S., Rouse B.T., Sarangi P.P. Did climate change influence the emergence, transmission, and expression of the COVID-19 pandemic? Front. Med. 2021;8(2549) doi: 10.3389/fmed.2021.769208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haitao T., Vermunt J.V., Abeykoon J., Ghamrawi R., Gunaratne M., Jayachandran M.…Garovic V.D. COVID-19 and sex differences: mechanisms and biomarkers. Mayo Clin. Proc. 2020;95(10):2189–2203. doi: 10.1016/j.mayocp.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honardoost M., Janani L., Aghili R., Emami Z., Khamseh M.E. The association between presence of comorbidities and COVID-19 severity: a systematic review and meta-analysis. Cerebrovasc. Dis. 2021;50(2):132–140. doi: 10.1159/000513288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Househam P.C., Mills P.J., Chopra D. The effects of stress and meditation on the immune system, human microbiota, and epigenetics. Adv. Mind Body Med. 2017;31(4):10–25. [PubMed] [Google Scholar]
- Huang C.-W., Chien Y.-S., Chen Y.-J., Ajuwon K.M., Mersmann H.M., Ding S.-T. Role of n-3 polyunsaturated fatty acids in ameliorating the obesity-induced metabolic syndrome in animal models and humans. Int. J. Mol. Sci. 2016;17(10) doi: 10.3390/ijms17101689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y.…Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet (London, England) 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph B., Nair P.M., Nanda A. Effects of naturopathy and yoga intervention on CD4 count of the individuals receiving antiretroviral therapy-report from a human immunodeficiency virus sanatorium, Pune. Int. J. Yoga. 2015;8(2):122–127. doi: 10.4103/0973-6131.158475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaliman P., Alvarez-Lopez M.J., Cosín-Tomás M., Rosenkranz M.A., Lutz A., Davidson R.J. Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators. Psychoneuroendocrinology. 2014;40:96–107. doi: 10.1016/j.psyneuen.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapasia N., Paul P., Roy A., Saha J., Zaveri A., Mallick R. Children and Youth Services Review Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Child. Youth Serv. Rev. 2020;116:105194. doi: 10.1016/j.childyouth.2020.105194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauts A., Sharma N. Effect of yoga on academic performance in relation to stress. Int. J. Yoga. 2009;2(1):39–43. doi: 10.4103/0973-6131.53860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemeny M.E. The psychobiology of stress. Curr. Dir. Psychol. Sci. 2003;12(4):124–129. doi: 10.1111/1467-8721.01246. [DOI] [Google Scholar]
- Khanna K., Kohli S.K., Kaur R., Bhardwaj A., Bhardwaj V., Ohri P.…Ahmad P. Herbal immune-boosters: substantial warriors of pandemic Covid-19 battle. Phytomedicine. 2021;85:153361. doi: 10.1016/j.phymed.2020.153361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser J.K., Christian L., Preston H., Houts C.R., Malarkey W.B., Emery C.F., Glaser R. Stress, inflammation, and yoga practice. Psychosom. Med. 2010;72(2):113–121. doi: 10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.-D. Effects of yogic eye exercises on eye fatigue in undergraduate nursing students. J. Phys. Ther. Sci. 2016;28(6):1813–1815. doi: 10.1589/jpts.28.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein S.L. The effects of hormones on sex differences in infection: from genes to behavior. Neurosci. Biobehav. Rev. 2000;24(6):627–638. doi: 10.1016/S0149-7634(00)00027-0. [DOI] [PubMed] [Google Scholar]
- Kominsky D.J., Campbell E.L., Colgan S.P. Metabolic shifts in immunity and inflammation. J. Immunol. 2010;184(8):4062–4068. doi: 10.4049/jimmunol.0903002. Baltimore, Md. : 1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancet T. India under COVID-19 lockdown. Lancet. 2020;395(10233):1315. doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau C., Yu R., Woo J. Effects of a 12-week hatha yoga intervention on cardiorespiratory endurance, muscular strength and endurance, and flexibility in Hong Kong Chinese adults: a controlled clinical trial. Evid. base Compl. Alternative Med. 2015;2015 doi: 10.1155/2015/958727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.-H., Giuliani F. The role of inflammation in depression and fatigue. Front. Immunol. 2019;10:1696. doi: 10.3389/fimmu.2019.01696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard B.E. The concept of depression as a dysfunction of the immune system. Curr. Immunol. Rev. 2010;6(3):205–212. doi: 10.2174/157339510791823835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim Sung-Ah, Cheong Kwang-Jo. Regular yoga practice improves antioxidant status, immune function, and stress hormone releases in young healthy people: a randomized, double-blind, controlled pilot study. J. Alternative Compl. Med. 2015;21(9):530–538. doi: 10.1089/acm.2014.0044. [DOI] [PubMed] [Google Scholar]
- Limone P., Toto G.A. Psychological and emotional effects of digital technology on children in covid-19 pandemic. Brain Sci. 2021;11(9):1126. doi: 10.3390/brainsci11091126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y.-Z., Wang Y.-X., Jiang C.-L. Inflammation: the common pathway of stress-related diseases. Front. Hum. Neurosci. 2017;11:316. doi: 10.3389/fnhum.2017.00316. 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo X., Zhou G.-Z., Zhang Y., Peng L.-H., Zou L.-P., Yang Y.-S. Coronaviruses and gastrointestinal diseases. Military Med. Res. 2020;7(1):49. doi: 10.1186/s40779-020-00279-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mach N., Fuster-Botella D. Endurance exercise and gut microbiota: a review. J. Sport Health Sci. 2017;6(2):179–197. doi: 10.1016/j.jshs.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madison A., Kiecolt-Glaser J.K. Stress, depression, diet, and the gut microbiota: human-bacteria interactions at the core of psychoneuroimmunology and nutrition. Current Opinion Behav. Sci. 2019;28:105–110. doi: 10.1016/j.cobeha.2019.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manocha R., Black D., Sarris J., Stough C. A randomized, controlled trial of meditation for work stress, anxiety and depressed mood in full-time workers. Evid. base Compl. Alternative Med. 2011;2011:960583. doi: 10.1155/2011/960583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzieh Saei Ghare Naz M.B., Dashti Sareh, Ramezani Tehrani Fahimeh. An overview of sex hormones in relation to SARS-CoV-2 infection. Future Virol. 2021;16(8) doi: 10.2217/fvl-2021-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxime Taquet S.L., Geddes John R., Harrison Paul J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62354COVID -19cases in the USA. Lancet Psychiatr. 2021;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mishra A., Bentur S.A., Thakral S., Garg R., Duggal B. The use of integrative therapy based on Yoga and Ayurveda in the treatment of a high-risk case of COVID-19/SARS-CoV-2 with multiple comorbidities: a case report. J. Med. Case Rep. 2021;15(1):95. doi: 10.1186/s13256-020-02624-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morens D.M., Folkers G.K., Fauci A.S. The challenge of emerging and re-emerging infectious diseases. Nature. 2004;430(6996):242–249. doi: 10.1038/nature02759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan N., Irwin M.R., Chung M., Wang C. The effects of mind-body therapies on the immune system: meta-analysis. PLoS One. 2014;9(7):e100903. doi: 10.1371/journal.pone.0100903. e100903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munro A.K., Hunter E.C., Hossain S.Z., Keep M. A systematic review of the menstrual experiences of university students and the impacts on their education: a global perspective. PLoS One. 2021;16(9):e0257333. doi: 10.1371/journal.pone.0257333. e0257333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Na Nongkhai M.P., Yamprasert R., Punsawad C. Effects of continuous yoga on body composition in obese adolescents. Evid. base Compl. Alternative Med. 2021;2021 doi: 10.1155/2021/6702767. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nambiar D. The impact of online learning: student's views. Int. J. Indian Psychol. 2020;8(2) [Google Scholar]
- Nastasi C., Candela M., Bonefeld C.M., Geisler C., Hansen M., Krejsgaard T.…Ødum N. The effect of short-chain fatty acids on human monocyte-derived dendritic cells. Sci. Rep. 2015;5(1):1–10. doi: 10.1038/srep16148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemati A. The effect of pranayama on test anxiety and test performance. Int. J. Yoga. 2013;6(1):55. doi: 10.4103/0973-6131.105947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netea M.G., Domínguez-Andrés J., Barreiro L.B., Chavakis T., Divangahi M., Fuchs E., Latz E. Defining trained immunity and its role in health and disease. Nat. Rev. Immunol. 2020;20(6):375–388. doi: 10.1038/s41577-020-0285-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okano K., Kaczmarzyk J.R., Dave N., Gabrieli J.D., Grossman J.C. Sleep quality, duration, and consistency are associated with better academic performance in college students. NPJ Sci. Learn. 2019;4(1):1–5. doi: 10.1038/s41539-019-0055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oman D., Shapiro S.L., Thoresen C.E., Plante T.G., Flinders T. Meditation lowers stress and supports forgiveness among college students: a randomized controlled trial. J. Am. Coll. Health. 2008;56(5):569–578. doi: 10.3200/JACH.56.5.569-578. [DOI] [PubMed] [Google Scholar]
- Orellana C.I., Orellana L.M. Predictores de síntomas emocionales durante la cuarentena domiciliar por pandemia de COVID-19 en El Salvador. Actual. Psicol. 2020;34(128):103–120. [Google Scholar]
- Ornell F., Schuch J.B., Sordi A.O., Kessler F.H.P. “Pandemic fear” and COVID-19: mental health burden and strategies. Brazilian J. Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pal R., Singh S.N., Halder K., Tomer O.S., Mishra A.B., Saha M. Effects of yogic practice on metabolism and antioxidant–redox status of physically active males. J. Phys. Activ. Health. 2015;12(4):579–587. doi: 10.1123/jpah.2013-0059. [DOI] [PubMed] [Google Scholar]
- Pandya A., Lodha P. Social connectedness, excessive screen time during COVID-19 and mental health: a review of current evidence. Front. Hum. Dynam. 2021;45 [Google Scholar]
- Park J., Kim S. Validity of muscle-to-fat ratio as a predictor of adult metabolic syndrome. J. Phys. Ther. Sci. 2016;28(3):1036–1045. doi: 10.1589/jpts.28.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe M.C., Thompson D.R., Ski C.F. Yoga, mindfulness-based stress reduction and stress-related physiological measures: a meta-analysis. Psychoneuroendocrinology. 2017;86:152–168. doi: 10.1016/j.psyneuen.2017.08.008. [DOI] [PubMed] [Google Scholar]
- Pinto A., Faiz O., Davis R., Almoudaris A., Vincent C. Surgical complications and their impact on patients' psychosocial well-being: a systematic review and meta-analysis. BMJ Open. 2016;6(2) doi: 10.1136/bmjopen-2014-007224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preoteasa C.T., Axante A., Cristea A.D., Preoteasa E. Education Research International; 2016. The Relationship between Positive Well-Being and Academic Assessment: Results from a Prospective Study on Dental Students. 2016. [Google Scholar]
- Pullen M.F., Skipper C.P., Hullsiek K.H., Bangdiwala A.S., Pastick K.A., Okafor E.C.…Boulware D.R. Symptoms of COVID-19 outpatients in the United States. Open Forum Infect. Dis. 2020;7(7) doi: 10.1093/ofid/ofaa271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radzikowska U., Rinaldi A.O., Çelebi Sözener Z., Karaguzel D., Wojcik M., Cypryk K., Sokolowska M. The influence of dietary fatty acids on immune responses. Nutrients. 2019;11(12):2990. doi: 10.3390/nu11122990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramón-Arbués E., Gea-Caballero V., Granada-López J.M., Juárez-Vela R., Pellicer-García B., Antón-Solanas I. The prevalence of depression, anxiety and stress and their associated factors in college students. Int. J. Environ. Res. Publ. Health. 2020;17(19):7001. doi: 10.3390/ijerph17197001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren L.-L., Wang Y.-M., Wu Z.-Q., Xiang Z.-C., Guo L., Xu T.…Wang J.-W. Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chin. Med. J. 2020;133(9):1015–1024. doi: 10.1097/CM9.0000000000000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes-Rodríguez M.L., Rivera-Medina C.L., Cámara-Fuentes L., Suárez-Torres A., Bernal G. Depression symptoms and stressful life events among college students in Puerto Rico. J. Affect. Disord. 2013;145(3):324–330. doi: 10.1016/j.jad.2012.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley D. Hatha yoga and the treatment of illness. Alternative Ther. Health Med. 2004;10(2):20. [PubMed] [Google Scholar]
- Rioux J., Howerter A. Outcomes from a whole-systems ayurvedic medicine and yoga therapy treatment for obesity pilot study. J. Alternative Compl. Med. 2019;25(S1):S124–S137. doi: 10.1089/acm.2018.0448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L.…Hardman C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: a study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha K.K.F., Ribeiro A., Rocha K., Sousa M.B. C.d., Albuquerque F., Ribeiro S., Silva R. Improvement in physiological and psychological parameters after 6 months of yoga practice. Conscious. Cognit. 2012;21(2):843–850. doi: 10.1016/j.concog.2012.01.014. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Rey R., Garrido-Hernansaiz H., Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020;11:1540. doi: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen L.D., Lim A.F., Felt J., Carrier L.M., Cheever N.A., Lara-Ruiz J.M.…Rokkum J. Media and technology use predicts ill-being among children, preteens and teenagers independent of the negative health impacts of exercise and eating habits. Comput. Hum. Behav. 2014;35:364–375. doi: 10.1016/j.chb.2014.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross A., Williams L., Pappas-Sandonas M., Touchton-Leonard K., Fogel D. Incorporating yoga therapy into primary care: the Casey Health Institute. Int. J. Yoga Therapy. 2015;25(1):43–49. doi: 10.17761/1531-2054-25.1.43. [DOI] [PubMed] [Google Scholar]
- Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. 102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A., Keinan G., Daon K. Effects of stress on sleep: the moderating role of coping style. Health Psychol. 2004;23(5):542. doi: 10.1037/0278-6133.23.5.542. [DOI] [PubMed] [Google Scholar]
- Sahni P.S., Singh K., Sharma N., Garg R. Yoga an effective strategy for self-management of stress-related problems and wellbeing during COVID19 lockdown: a cross-sectional study. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0245214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salari N., Hosseinian-Far A., Jalali R., Vaisi-Raygani A., Rasoulpoor S., Mohammadi M.…Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health. 2020;16(1):57. doi: 10.1186/s12992-020-00589-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar S., Sa B., Singh K., Gaur U., Bharatha A., Victor V.…Majumder M.A.A. Psychophysiological effects of yoga on stress management among medical and allied health professional students during COVID-19 pandemic: a narrative review. Adv. Human Biol. 2021;11(4):3. [Google Scholar]
- Sathyanarayanan G., Vengadavaradan A., Bharadwaj B. Role of yoga and mindfulness in severe mental illnesses: a narrative review. Int. J. Yoga. 2019;12(1):3–28. doi: 10.4103/ijoy.IJOY_65_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneiderman N., Ironson G., Siegel S.D. Stress and health: psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005;1:607–628. doi: 10.1146/annurev.clinpsy.1.102803.144141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int. J. Prev. Med. 2012;3(7):444–458. [PMC free article] [PubMed] [Google Scholar]
- Sheela H.R.R.N., Ganpat T.S. Efficacy of Yoga for sustained attention in university students. Ayu. 2013;34(3):270. doi: 10.4103/0974-8520.123117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheela Joice P.P., Manik K.A., Sudhir P.K. Role of yoga in attention, concentration, and memory of medical students. Natl. J. Physiol. Pharm. Pharmacol. 2018;8(11):1526–1528. doi: 10.5455/njppp.2018.8.0723521082018. [DOI] [Google Scholar]
- Shetty P., Reddy B K.K., Lakshmeesha D.R., Shetty S.P., Kumar G S., Bradley R. Effects of sheetali and sheetkari pranayamas on blood pressure and autonomic function in hypertensive patients. Integr. Med. 2017;16(5):32–37. [PMC free article] [PubMed] [Google Scholar]
- Shohani M., Badfar G., Nasirkandy M.P., Kaikhavani S., Rahmati S., Modmeli Y., Azami M. The effect of yoga on stress, anxiety, and depression in women. Int. J. Prev. Med. 2018;9 doi: 10.4103/ijpvm.IJPVM_242_16. 21-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva P.G.d.B., de Oliveira C.A.L., Borges M.M.F., Moreira D.M., Alencar P.N.B., Avelar R.L.…Sousa F.B. Distance learning during social seclusion by COVID-19: improving the quality of life of undergraduate dentistry students. Eur. J. Dent. Educ. 2021;25(1):124–134. doi: 10.1111/eje.12583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C., Hancock H., Blake-Mortimer J., Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Compl. Ther. Med. 2007;15(2):77–83. doi: 10.1016/j.ctim.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents' stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020;11:1713. doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefano Lazzer G.B., Claudio L Lafortuna, Nicoletta Marazzi, Carlo Busti, Raffaela Galli, Alessandra De Col, Fiorenza Agosti, Alessandro Sartorio. Relationship between basal metabolic rate, gender, age, and body composition in 8,780 white obese subjects. Obesity. 2012;18(1):71–78. doi: 10.1038/oby.2009.162. [DOI] [PubMed] [Google Scholar]
- Swanson D., Block R., Mousa S.A. Omega-3 fatty acids EPA and DHA: health benefits throughout life. Adv. Nutr. 2012;3(1):1–7. doi: 10.3945/an.111.000893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweileh W.M., Ali I.A., Sawalha A.F., Abu-Taha A.S., Sa'ed H.Z., Al-Jabi S.W. Sleep habits and sleep problems among Palestinian students. Child Adolesc. Psychiatr. Ment. Health. 2011;5(1):1–8. doi: 10.1186/1753-2000-5-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi J.K., Gupta P.K. An overview of Indian research in anxiety disorders. Indian J. Psychiatr. 2010;52(Suppl. 1):S210–S218. doi: 10.4103/0019-5545.69234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J.M., Campbell W.K. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev. Med. Rep. 2018;12:271–283. doi: 10.1016/j.pmedr.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udupa K., Bhavanani A.B., Vijayalakshmi P., Krishnamurthy N. Effect of pranayam training on cardiac function in normal young volunteers. Indian J. Physiol. Pharmacol. 2003;47(1):27–33. [PubMed] [Google Scholar]
- Vagga A.A., Dhok A.J. Blessings in disguise: yoga and meditation during corona lockdown. J. Evol. Med. Dent. Sci. 2020;9(35):2540–2545. [Google Scholar]
- Venkatesh H.N., Ravish H., Wilma Delphine Silvia C.R., Srinivas H. Molecular signature of the immune response to yoga therapy in stress-related chronic disease conditions: an insight. Int. J. Yoga. 2020;13(1):9–17. doi: 10.4103/ijoy.IJOY_82_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vijayaraghava A., Doreswamy V., Narasipur O.S., Kunnavil R., Srinivasamurthy N. Effect of yoga practice on levels of inflammatory markers after moderate and strenuous exercise. J. Clin. Diagn. Res.: J. Clin. Diagn. Res. 2015;9(6):CC08. doi: 10.7860/JCDR/2015/12851.6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vishram J.K., Borglykke A., Andreasen A.H., Jeppesen J., Ibsen H., Jørgensen T., Kee F. Impact of age and gender on the prevalence and prognostic importance of the metabolic syndrome and its components in Europeans. The MORGAM Prospective Cohort Project. PLoS One. 2014;9(9) doi: 10.1371/journal.pone.0107294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vodnar D.-C., Mitrea L., Teleky B.-E., Szabo K., Călinoiu L.-F., Nemeş S.-A., Martău G.-A. Coronavirus disease (COVID-19) caused by (SARS-CoV-2) infections: a real challenge for human gut microbiota. Front. Cell. Infect. Microbiol. 2020;10 doi: 10.3389/fcimb.2020.575559. 575559-575559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H.-Y., Li X.-L., Yan Z.-R., Sun X.-P., Han J., Zhang B.-W. Potential neurological symptoms of COVID-19. Therapeutic Adv. Neurol. Dis. 2020;13 doi: 10.1177/1756286420917830. 1756286420917830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int. J. Yoga. 2011;4(2):49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L.…McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaribeygi H., Panahi Y., Sahraei H., Johnston T.P., Sahebkar A. The impact of stress on body function: a review. EXCLI J. 2017;16:1057–1072. doi: 10.17179/excli2017-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasmin H., Khalil S., Mazhar R. Covid 19: stress management among students and its impact on their effective learning. Int. Technol. Educ. J. 2020;4(2):65–74. [Google Scholar]
- Yazdanpanah F., Hamblin M.R., Rezaei N. The immune system and COVID-19: friend or foe? Life Sci. 2020;256:117900. doi: 10.1016/j.lfs.2020.117900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng C., Huang W.Y., Sheridan S., Sit C.H.-P., Chen X.-K., Wong S.H.-S. COVID-19 pandemic brings a sedentary lifestyle in young adults: a cross-sectional and longitudinal study. Int. J. Environ. Res. Publ. Health. 2020;17(17):6035. doi: 10.3390/ijerph17176035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng D., Liwinski T., Elinav E. Interaction between microbiota and immunity in health and disease. Cell Res. 2020;30(6):492–506. doi: 10.1038/s41422-020-0332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]