Abstract
Background
Coronavirus disease 2019 (COVID-19) vaccine acceptance is essential in controlling the virus. Vaccine knowledge influences vaccine acceptance and understanding this is vital in planning immunization strategies.
Objectives
This study aimed to examine the public COVID-19 vaccine knowledge levels and predictors of low knowledge levels in Vietnam.
Methods
A cross-sectional, community-based survey was conducted between April 16 and July 16, 2021. To examine the community knowledge levels regarding the vaccine essentialness and efficacy, a self-administered questionnaire was developed and comprised 7 questions with 5 Likert scale responses corresponding to the levels of agreement or disagreement with the provided statements and scores ranging from 0 to 4. An individual’s knowledge score above the mean score of all participants was defined as “acceptable” and that below was defined as “low.”
Results
Among 1708 respondents, the mean age was 34.3 ± 13.4 years, 942 (55.2%) were females, and 797 (46.7%) had acceptable knowledge levels. Age (adjusted odds ratio [AOR] 0.984 [95% CI 0.972–0.995], P = 0.005) and being vaccinated against COVID-19 (0.653 [0.431–0.991], P = 0.045) were inversely associated with lower knowledge levels. Those with a Gapminder income of $8 to < $15 per day (1.613 [1.117–2.329], P = 0.001), $2 to < $8 (2.093 [1.313–3.335], P = 0.002), and < $2 (3.341 [1.951–5.722], P < 0.001), less than a high school education (4.214 [1.616–10.988], P = 0.003), and nonclinical professionals and nonhealth lecturers (1.83 [1.146–2.922], P = 0.01) were positively associated with lower knowledge levels.
Conclusion
To ensure a successful vaccine rollout, it is crucial to improve community knowledge about vaccine essentialness and efficacy. Those who are at young age, who have low income or education levels, and working in nonclinical and nonhealth education fields should be the target of the intervention programs. Community education programs may benefit from using those who have been immunized as role models.
Key Points.
Background
-
•
Vaccines play an important role in paving the way for controlling the coronavirus disease 2019 (COVID-19) pandemic.
-
•
Vaccine uptake is complex and multifactorial.
-
•
COVID-19 vaccine knowledge influences vaccine acceptance.
Findings
-
•
The study identifies people whose vaccine knowledge is low.
-
•
It is crucial to improve the knowledge about vaccine essentialness and efficacy in the community.
-
•
The target of the community education programs should be those who are at young age, who have low income or education levels, and working in nonclinical and nonhealth education fields.
Background
The coronavirus disease 2019 (COVID-19) pandemic has caused enormous economic hardship, morbidity, and mortality.1 Preventive measures including quarantine and social distancing, regular hand hygiene, and use of face masks in public have been implemented worldwide.2, 3, 4, 5 However, these efforts alone have proven insufficient to completely control viral transmission and hospitalizations owing to COVID-19.4 Vaccination remains one of the most effective measures in the fight against infectious diseases.1 In the context of COVID-19, in addition to other control measures, vaccination plays an important role in paving the way to eliminate COVID-19.6 Hence, development of a safe and effective COVID-19 immunization is the long-term solution toward averting the pandemic for most countries.7 However, the availability of a vaccine does not guarantee sufficient population vaccination coverage.8 Like other vaccine preventable diseases, uptake of COVID-19 vaccine is multifactorial and includes the knowledge about the vaccine.9, 10, 11 Giving people information or education to assist them in making informed decisions about their health is an important part of all patient-centered health systems.10 Given that COVID-19 vaccines are being used, identifying those in most need of this information is crucial to improving vaccine uptake and ensuring equity within health systems.10 , 12 General knowledge about COVID-19 vaccines is highly variable with surveys reporting “correct answers” between 26% and 86% in Ethiopia, Jordan, Oman, Bangladesh, India, Libya, and Italy.9 , 12, 13, 14, 15, 16, 17 COVID-19 vaccine knowledge is associated with age, income and education levels, medical-related professions, and COVID-19 immunization status; however, these may also be context dependent.14 , 16 , 17
Despite the successful control of the first wave of COVID-19, Vietnam has experienced ongoing domestic outbreaks.5 , 18 Like other countries, large-scale COVID-19 vaccine coverage is among the most important control strategies in Vietnam.19 In Vietnam, studies suggest that uptake of vaccines that are not included in the National Expanded Program on Immunization such as influenza vaccine is suboptimal even among health professionals.20 , 21 In addition, concern over adverse events has led to large reductions in the coverage of vaccines such as hepatitis B vaccine in recent years.22 However, the public COVID-19 vaccine knowledge remains unknown in Vietnam.
Objectives
The objective of this study was to examine the general community’s COVID-19 vaccine knowledge and associated predictors in Vietnam. This study was important because it will assist Vietnam and comparable countries in guiding interventional measures aimed at building and maintaining community’s receptiveness of COVID-19 vaccine.
Methods
Study context
Vietnam has experienced the fourth COVID-19 wave starting on April 27, 2021.23 This is considered the first “real wave” with 40,609 cumulative incident cases being reported in more than half of cities (52.4%, 33 of 63) across Vietnam as of the end of the study period.23 Of these affected areas, Ho Chi Minh City—one of the 2 research sites for the paper-based survey—was hit hard by the outbreak with 23,913 cumulative incident cases (58.9%).23 , 24 Considering this situation, we were able to examine the public COVID-19 vaccine knowledge in the context of an ongoing severe COVID-19 outbreak. During this time, the AstraZeneca/Oxford COVID-19 vaccine was available to priority groups including frontline health care workers and those working in COVID-19 prevention and control. A few fatal cases related to COVID-19 vaccine were reported.25 , 26 Vietnam has started its largest-ever COVID-19 vaccination campaign since July 10, 2021.27
Study design
A cross-sectional, anonymous survey using a self-administered questionnaire was conducted across Vietnam between April 16, 2021, and July 16, 2021. The questionnaire was administered by 2 different data collection methods including online and paper-based questionnaires. The paid SurveyMonkey platform (www.surveymonkey.com) was used for the online component of the survey given favorable characteristics of SurveyMonkey including easier access, avoidance of input and data coding errors, and faster distribution.28 Participants were asked to read the online participant information sheet and consent form and answer a yes-no question to confirm their willingness to participate voluntarily in the survey. After answering this question, participants were directed to complete the online questionnaire. This informed consent procedure is validated elsewhere.29 In the paper-based survey, participants were asked to read a hard copy of the participant information sheet and complete a written informed consent form and a hard copy of the questionnaire. Only participants who fully understood and agreed to participate in the study were enrolled in the study. Vietnamese people aged 18 years and older who were able to read and answer the survey were eligible to participate in the study. After the survey, information on the year of birth of participants was used to cross-check their age. Data of those participants aged younger than 18 years were excluded from the analysis. At the end of the data collection period, to prevent duplicate entries obtained from the online survey, entries submitted from the same Internet protocol address were separately reviewed by the researchers (M.C.D. and H.T.N.) and included in the analysis once consensus was reached. The study was approved by the Phenikaa University Ethics Committee (reference 216/QĐ-ĐHP-KHCN).
To recruit both online and paper-based participants, a snowball sampling technique was used, using the authors’ current social networks including family members, friends, and colleagues in Vietnam who were health professionals, university lecturers, students, and people in the general community. Essentially, this method is a chain-referral sampling where existing participants recruit future participants from among their acquaintances.30 A recruitment poster together with the survey link was e-mailed to the authors’ social networks and posted to their accounts on LinkedIn, Zalo, and Facebook, which are the most common social media applications in Vietnam. A request to disseminate the poster and the survey link to the recipients’ social networks was also included in the poster so that online responses could be from across Vietnam. The paper-based survey was conducted in Ho Chi Minh City, which is the largest city and located in southern Vietnam, and Hanoi, which is the capital and located in northern Vietnam. The rationale for selecting these cities as research sites was that these cities are the 2 largest cities and the main destinations of internal migration in Vietnam.31 Therefore, selecting these research sites would enable us to have study participants from different socioeconomic backgrounds and regions in Vietnam. Paper-based participants may opt to complete the online survey, if they had an Internet-enabled device or Internet connection.
A self-administered questionnaire was designed specifically to be completed by respondents without intervention of the researchers and comprised 2 parts: demographics and COVID-19 vaccine knowledge. Demographic variables included year of birth, gender, region of current residence (southern, northern and middle Vietnam as per administrative division),32 household composition (living alone, with family or with friends), education levels, jobs, income categorized based on the Gapminder Institute income levels,33 chronic health conditions (having chronic communicable or noncommunicable diseases), being vaccinated against COVID-19, and COVID-19 disease experience (acquiring COVID-19 or having family members or friends/colleagues acquiring COVID-19) (Appendix 1). The vaccine knowledge section focused on the essentialness and efficacy of COVID-19 vaccine and vaccination including the ability to protect the community through herd immunity. This section included 7 Likert scale questions with 5 options corresponding to the levels of agreement or disagreement with the provided statements and scores ranging from 0 to 4. The scores were evenly distributed for 7 categories without any leading questions. Therefore, the total maximum knowledge score was 28. These 7 questions were developed based on the available literature about COVID-19 vaccines and information from the manufacturers, World Health Organization (WHO), and Vietnam Ministry of Health.24 , 27 , 34, 35, 36, 37, 38, 39, 40 Pilot online and paper-based surveys were conducted and included 100 individuals (i.e., 50 participants each) from different backgrounds to help refine the final survey and confirm its validity and reliability.41 To ensure study participants’ understanding of the questionnaire, the online and paper-based surveys used a questionnaire that was written in Vietnamese. Contact details of the researchers (M.C.D. and H.T.N.) were provided so that study participants could contact for assistance.
Statistical analysis
Data were analyzed using the SPSS version 26 (IBM Corp, Armonk, NY). Continuous variables were displayed as mean ± 1 SD and range. Categorical variables were presented as a count and percentage. Study participants’ vaccine knowledge levels were defined in relation to the mean score achieved by all participants. Scores above the mean were defined as “acceptable” and those below were defined as “low.” This analysis approach has been validated elsewhere.18 Chi-square test and chi-square test for trend were used to compare categorical data. t test was used to compare continuous data. A binary logistic regression model was developed to examine predictors of a low vaccine knowledge. All independent variables were entered into the model. Alpha was set at 5% level.
Maintenance of study standard
The online survey was a part of this study. Like the online survey, the paper-based survey used the snowball sampling technique to recruit participants. Therefore, to increase the study’s transparency and possibilities for interpreting the results, this paper was reported in accordance with the recommended Checklist for Reporting Results of Internet E-Surveys42 , 43 and the Strengthening the Reporting of Observational Studies in Epidemiology Statement guidelines for reporting observational studies.44
Results
Baseline characteristics
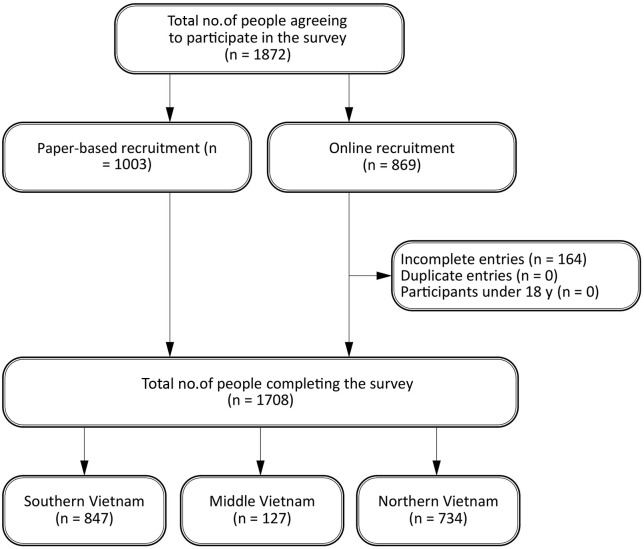
A total of 1872 people including 1003 paper-based (53.6%) and 869 online participants (46.4%) agreed to participate in the study (Figure 1 ). Of these 1872 people, 164 online participants (8.8%) had missing answers and were removed from the analysis. Therefore, 1708 (91.2%) people were included in the study. The mean age of all participants was 34.3 ± 13.4 years (Table 1 ). Female participants accounted for 55.2% (942 of 1708). Just less than half of participants (49.6%, 847 of 1708) was from southern Vietnam, more than two-thirds (69.3%, 1184 of 1708) earned less than $15 per day, and 74.5% (1272 of 1708) lived with their family. Most participants (81.9%, 1399 of 1708) had an undergraduate or a postgraduate degree, and 72.2% (1234 of 1708) were students of nonhealth-related subjects or people working in nonhealth-related fields. Only 222 participants (13%) had chronic health conditions, 48 (2.8%) had experiences with COVID-19 disease, and 129 (7.6%) were vaccinated.
Figure 1.
Flowchart of study participants.
Table 1.
Baseline characteristics of study participants (N = 1708)
| Characteristics | Summary statisticsa |
|---|---|
| Age (y) | 34.3 ± 13.4 (18–80) |
| Age groups (y) | |
| ≤ 20 | 379 (22.2) |
| 21–40 | 818 (47.9) |
| 41–60 | 430 (25.2) |
| ≥ 61 | 81(4.7) |
| Female | 942 (55.2) |
| Region of current residence | |
| Northern Vietnam | 734 (43) |
| Middle of Vietnam | 127 (7.4) |
| Southern Vietnam | 847 (49.6) |
| Gapminder income levels (US$ per day) | |
| < 2 | 348 (20.4) |
| 2 to < 8 | 253 (14.8) |
| 8 to < 15 | 583 (34.1) |
| 15–32 | 343 (20.1) |
| ≥ 32 | 181 (10.6) |
| Household composition | |
| Alone | 135 (7.9) |
| With family | 1272 (74.5) |
| With friends | 301 (17.6) |
| Education levels | |
| < high school | 29 (1.7) |
| High school | 140 (8.2) |
| College | 140 (8.2) |
| ≥ Undergraduate level | 1399 (81.9) |
| Jobs | |
| Health students | 126 (7.4) |
| Nonhealth students | 378 (22.1) |
| Working in nonhealth-related fields | 856 (50.1) |
| Clinical doctors and/or health lecturers | 152 (8.9) |
| Working in other health-related fields | 196 (11.5) |
| Chronic health conditionsb | 222 (13) |
| Experiences with COVID-19 diseasec | 48 (2.8) |
| Vaccinated against COVID-19 | 129 (7.6) |
Abbreviation used: COVID-19, coronavirus disease 2019.
Mean ± SD (minimum–maximum) for continuous variables and n (%) for categorical variables.
Chronic communicable and/or noncommunicable diseases.
Acquiring COVID-19 and/or having family members or friends/colleagues acquiring COVID-19.
COVID-19 vaccine knowledge score
Given that the maximum number of points awarded for correct answers of each of 7 knowledge questions was 4, the percentage of participants who got 4 points for each question ranged from 2.2% to 41.6% (Appendix 2). Only 2.2% (38 of 1708) strongly disagreed that they are completely protected against COVID-19 and 36.4% (621 of 1708) strongly disagreed that they do not need to undertake any other preventive measures after they fully complete the vaccination schedule. Less than one-third strongly agreed that being vaccinated themselves contributes to the protection of the community against COVID-19 (30.3%, 518 of 1708) and getting vaccinated is a good way to protect oneself from COVID-19 (20.6%, 352 of 1708). Less than half (41.6%, 710 of 1708) strongly disagreed that they do not need to get vaccinated because the outbreak was controlled very well in Vietnam. Less than one-fifth strongly agreed that vaccines developed by different manufacturers have different levels of efficacy (17.1%, 292 of 1708), and the available vaccines may not be effective on new variants compared with the original strain detected in Wuhan (12.8%, 219 of 1708).
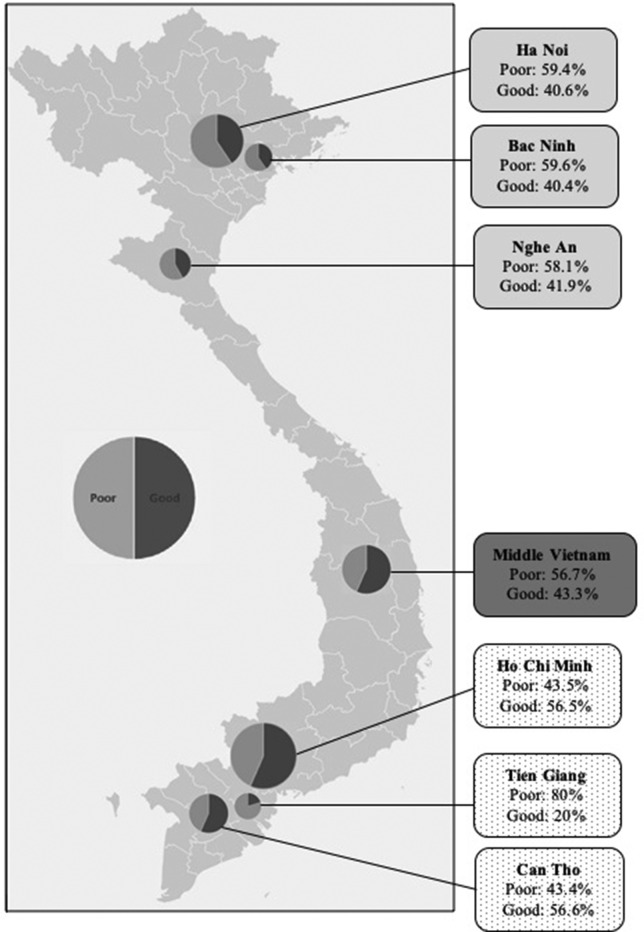
The mean knowledge score of all participants was 19.2 ± 2.8 (Table 2 ). Hence, a score at least 20 indicated an acceptable level of COVID-19 vaccine knowledge and accounted for 46.7% of study participants (797 of 1708). In large cities in northern Vietnam, the proportion of participants having a low knowledge level was 59.6% (31 of 52) in Bac Ninh, 59.4% (231 of 389) in Hanoi, and 58.1% (25 of 43) in Nghe An, whereas that of the middle of Vietnam was 56.7% (72 of 127) (Appendix 3). In southern Vietnam, this proportion was 80% (44 of 55) in Tien Giang, 43.5% (254 of 548) in Ho Chi Minh City, and 43.4% (53 of 122) in Can Tho.
Table 2.
COVID-19 vaccine knowledge score of study participants (N = 1708)
| Characteristics | Summary statisticsa |
|---|---|
| Knowledge score (points) | 19.2 ± 2.8 (11–28) |
| Score groups | |
| ≤ 14 | 134 (7.8) |
| 15–19 | 777 (45.5) |
| 20–24 | 768 (45.0) |
| ≥ 25 | 29 (1.7) |
| Knowledge levels | |
| Low | 911 (53.3) |
| Acceptable | 797 (46.7) |
Abbreviation used: COVID-19, coronavirus disease 2019.
Mean ± SD (minimum–maximum) for continuous variables and n (%) for categorical variables.
Predictors of a low level of vaccine knowledge
A low knowledge level was significantly associated with age, gender, region, Gapminder income levels and jobs (P < 0.001), and education levels (P = 0.035) (Table 3 ). There was no statistically significant association between knowledge level and household composition, chronic health conditions, experiences with COVID-19 disease, and being vaccinated (P > 0.05).
Table 3.
Unadjusted predictors tested for a low level of COVID-19 vaccine knowledge among study participants (N = 1708)
| Predictors | COVID-19 knowledge levelsa |
P value OR (95% CI) |
|
|---|---|---|---|
| Poor (n = 911) | Acceptable (n = 797) | ||
| Age (y) | 32.6 ± 12.9 | 36.2 ± 13.7 | < 0.001b |
| Female | 526 (57.7) | 416 (52.2) | 0.02b 1.25 (1.03–1.52) |
| Region | |||
| Northern Vietnam | 435 (47.8) | 299 (37.5) | < 0.001c |
| Middle Vietnam | 72 (7.9) | 55 (6.9) | |
| Southern Vietnam | 404 (44.3) | 443 (55.6) | |
| Gapminder income levels (US$ per day) | |||
| < 2 | 238 (26.1) | 110 (13.8) | < 0.001d |
| 2 to < 8 | 155 (17.0) | 98 (12.3) | |
| 8 to < 15 | 297 (32.6) | 286 (35.9) | |
| 15–32 | 154 (16.9) | 189 (23.7) | |
| ≥ 32 | 67 (7.4) | 114 (14.3) | |
| Household composition | |||
| Alone | 64 (7.0) | 71 (8.9) | 0.133c |
| With family | 674 (74.0) | 598 (75.0) | |
| With friends | 173 (19.0) | 128 (16.1) | |
| Education levels | |||
| < high school | 23 (2.5) | 6 (0.8) | < 0.035d |
| High school | 70 (7.7) | 70 (8.8) | |
| College | 76 (8.3) | 64 (8.0) | |
| ≥ Undergraduate level | 742 (81.5) | 657 (82.4) | |
| Jobs | |||
| Health students | 93 (10.2) | 33 (4.1) | < 0.001c |
| Nonhealth students | 222 (24.4) | 156 (19.6) | |
| Working in nonhealth-related fields | 405 (44.4) | 451 (56.6) | |
| Clinical doctors and/or health lecturers | 68 (7.5) | 84 (10.5) | |
| Working in other health-related fields | 123 (13.5) | 73 (9.2) | |
| Chronic health conditionse | 113 (12.4) | 109 (13.7) | 0.471c |
| Experiences with COVID-19 diseasef | 24 (2.6) | 24 (3.0) | 0.662c |
| Vaccinated against COVID-19 | 63 (6.9) | 66 (8.3) | 0.313c |
Abbreviations used: COVID-19, coronavirus disease 2019; OR, odds ratio.
Mean ± SD for continuous variables and number (%) for categorical variables.
t test.
Chi-square test.
Chi-square test for trend.
Chronic communicable and/or noncommunicable diseases.
Acquiring COVID-19 and/or having family members or friends/colleagues acquiring COVID-19.
Model for predicting a low level of vaccine knowledge
Age (adjusted odds ratio [AOR] 0.984 [95% CI 0.972–0.995], P = 0.005) and being vaccinated ( 0.653 [0.431–0.991], P = 0.045) were negatively associated with a low knowledge level (Table 4 ). Having a Gapminder income of $8 to < $15 per day (1.613 [1.117–2.329], P = 0.001), $2 to < $8 (2.093 [1.313–3.335], P = 0.002), and < $2 (3.341 [1.951–5.722], P < 0.001) corresponded with higher odds of having a low knowledge level compared with those whose Gapminder income was $32 or more per day. Having an education level of less than high school was positively associated with a low knowledge level compared with those whose education levels was undergraduate or above (4.214 [1.616–10.988], P = 0.003). Working in other health-related fields was positively associated with a low knowledge level compared with those who worked as clinical doctors or health lecturers (1.83 [1.146–2.922], P = 0.01).
Table 4.
Binary logistic regression analysis for predictors of a low level of COVID-19 vaccine knowledge among study participants (N = 1708)
| Predictors | P | Adjusted OR (95% CI) |
|---|---|---|
| Age (y) | 0.005 | 0.984 (0.972–0.995) |
| Female | 0.518 | 0.933 (0.756–1.151) |
| Region | ||
| Northern Vietnam | 0.725 | 0.928 (0.613–1.405) |
| Southern Vietnam | 0.318 | 0.812 (0.54–1.221) |
| Middle Vietnama | ||
| Gapminder income levels (US per day) | ||
| < 2 | 0.000 | 3.341 (1.951–5.722) |
| 2 to < 8 | 0.002 | 2.093 (1.313–3.335) |
| 8 to < 15 | 0.011 | 1.613 (1.117–2.329) |
| 15–32 | 0.258 | 1.248 (0.85–1.833) |
| ≥ 32a | ||
| Household composition | ||
| Alone | 0.441 | 0.839 (0.538–1.31) |
| With family | 0.245 | 1.189 (0.888–1.591) |
| With friendsa | ||
| Education levels | ||
| < High school | 0.003 | 4.214 (1.616–10.988) |
| High school | 0.975 | 1.006 (0.684–1.481) |
| College | 0.515 | 1.133 (0.779–1.648) |
| ≥ Undergraduate levela | ||
| Jobs | ||
| Health students | 0.34 | 1.345 (0.732–2.471) |
| Nonhealth students | 0.09 | 0.644 (0.387–1.072) |
| Working in nonhealth-related fields | 0.921 | 0.981 (0.671–1.434) |
| Working in other health-related fields | 0.01 | 1.83 (1.146–2.922) |
| Chronic health conditionsb | 0.27 | 1.207 (0.864–1.686) |
| Experiences with COVID-19 diseasec | 0.641 | 1.157 (0.628–2.13) |
| Vaccinated against COVID-19 | 0.045 | 0.653 (0.431–0.991) |
Abbreviations used: COVID-19, coronavirus disease 2019; OR, odds ratio.
Reference group.
Chronic communicable and/or noncommunicable diseases.
Acquiring COVID-19 and/or having family members or friends/colleagues acquiring COVID-19.
Discussion
Although there are similar studies conducted in other countries,9 , 12, 13, 14, 15 there was no study in Vietnam. To the best of our knowledge, this is the first study examining the level of COVID-19 vaccine knowledge in the general community in Vietnam. Our study identifies priority groups for intervention. The study also allowed us to get insight into the vaccine knowledge levels of different health professional groups who are central to vaccination education and role models, particularly those who are not clinical doctors such as nurses and pharmacists.
The study included 1708 selected individuals across Vietnam, including large cities and those with a high COVID-19 burden. The distribution of our participants by region of residence was skewed to southern Vietnam (49.6%) provided that this region accounts for 36% of the total population in Vietnam.45 This may also explain the low number of participants experiencing COVID disease in our study given that the fourth COVID-19 wave started in northern Vietnam. The number of participants getting vaccinated was low because the vaccine was exclusively available to frontline health care workers during the study period. Participants aged between 21 and 60 years and female gender were predominant in our study, which were comparable with the age and gender distributions in Vietnam.45 Given that the average income per day in Vietnam is $9.8,46 more than two-thirds of our participants (69.3%) earned less than $15 per day.
We found that more than half of participants (53.3%) had low vaccine knowledge levels. Given the mean knowledge score of 19.2 achieved by all participants, high proportions of participants having low knowledge levels, defined as their knowledge scores lower than this mean score, were documented in large cities across Vietnam. Our overall rate of low vaccine knowledge was comparable with that reported in community surveys conducted in India and Jordan.15 , 16 However, our proportion was higher than that reported in Bangladesh (43%, 713 of 1658) and Ethiopia (26%, 128 of 492).9 , 14 Although the questionnaires used in these studies were not the same, all questionnaires aim to explore essential aspects of COVID-19 vaccine knowledge including the vaccine availability, essentialness, eligibility, efficacy, and adverse effects, all of which play a role in facilitating the community’s vaccine confidence and acceptance.9 , 47 In Vietnam, our finding regarding the proportion of people having low vaccine knowledge levels was inconsistent with studies examining the levels of knowledge toward COVID-19 disease and associated nonvaccine prevention and control measures. In detail, acceptable knowledge levels toward COVID-19 disease and associated nonvaccine prevention and control measures were documented in both the general community and specific groups including pharmacists and university students.5 , 18 , 48, 49, 50
We found that young age, low income, and education levels were associated with low vaccine knowledge levels. Our findings were consistent with previous studies in other countries.14 , 16 It has been documented that young age, low income, and educations levels are significantly related to low levels of health knowledge in general probably because these groups are less likely to have heard of the health information.51 In contrast, people with high education levels are more knowledgeable and concerned about their health and life events that could affect them, such as COVID-19 vaccinations, through access to more sources of health information.14 In line with another study, we found that being vaccinated against COVID-19 was associated with a good vaccine knowledge level.17 It is documented that health care workers who are willing to be COVID-19 vaccinated serve as an important role model function for the public.52 , 53 It has also been found that the public vaccine acceptance is influenced by their peers and social networks.54 Considering our finding of a positive association between being vaccinated against COVID-19 and acceptable vaccine knowledge levels, we believe that, regardless of the professions, people who are vaccinated can present role models for the community. Future research is needed to examine how the community education programs using these role models could effectively approach different population groups.
In our study, participants working in health-related fields rather than clinical doctors and health lecturers such as nurses and pharmacists were more likely to have lower knowledge levels compared with clinical doctors and health lecturers. To the best of our knowledge, there is no study examining the levels of COVID-19 vaccine knowledge among different health professional groups in Vietnam. However, a study conducted on Vietnamese health students found a difference in the levels of COVID-19 vaccine acceptance by their specialist fields with more public health students but less preventive medicine students accepting the vaccine compared with general medicine students although the differences in levels of vaccine knowledge between these students were not examined.55 Similarly, a study in the United States found that direct medical care providers had higher vaccine acceptance (49%, 595 of 1207) than other health professionals although the vaccine knowledge levels among health professionals were not examined.56 It should be noted that this U.S. study was conducted between October 7 and November 9, 2020, and thus, vaccine acceptance rate of this study population may have increased owing to the recent changes in the local COVID-19 situations and community education regarding COVID-19 vaccination. Studies in Jordan and Italy found that health care workers had higher vaccine knowledge levels than nonmedical-related professions.16 , 17 The finding of our study was different than the Jordanian and Italian studies probably because of the difference in selecting the reference group. Based on our experience with the Vietnam context, clinical doctors and health lecturers are updated with medical scientific publications more regularly than those working in other health and nonhealth-related fields and, thus, were selected as our reference group. By doing this, we could be able to compare the vaccine knowledge levels of other health professionals who were not physicians and health lecturers with those of physicians and health lecturers. Unlike us, none of the Jordanian and Italian studies examined the differences in the vaccine knowledge levels between different health professional groups. Our study makes it possible to highlight the differences in the vaccine knowledge levels between health professional groups and, therefore, helps in developing more targeted intervention programs. It is clear that, in addition to vaccine knowledge, COVID-19 vaccine acceptance was influenced by other factors including enabling environments (e.g., convenient vaccination places and easy and accessible vaccination booking), social influences (e.g., salient social norms in favor of vaccination), and motivation (e.g., increasing motivation to get vaccinated through building timely trust in vaccines).36 However, like our study, the varied vaccine acceptance rates in different occupational roles in health care found in the U.S. study implied that the nonclinical professionals should be targeted—with educational interventions to ensure a successful COVID-19 vaccination. It should be noted that health professionals such as pharmacists, rather than physicians, have been identified as a professional figure in the health section who is qualified to improve the public vaccine acceptance in general.57 Indeed, a study in Vietnam also found that community pharmacists could take an important part in disseminating COVID-19 related knowledge to the public.49 Hence, to ensure a successful COVID-19 vaccine rollout, education programs in Vietnam should focus on improving the vaccine knowledge in those who are working in health-related fields but are not clinical doctors and health lecturers, such as nurses and pharmacists. Further studies are needed to examine the reasons for the low levels of vaccine knowledge in this group.
We found that only 41.6% of participants believed that vaccination was needed, despite the ongoing COVID-19 outbreak in Vietnam. In addition, only 20.6% of participants strongly agreed that getting vaccinated was a good way to protect oneself from COVID-19. At the time this manuscript was developed, the local government had been implemented the largest-ever vaccination campaign together with other preventive measures to control the outbreak.27 This implies that vaccination together with these measures may be the only way to achieve this goal as can be seen in other vaccine preventable diseases.6 , 58 In light of this, community education needs to emphasize the importance of the combined vaccination and nonvaccine measures in controlling the outbreak.
Our participants’ vaccine knowledge regarding vaccine efficacy and essentialness needs to be improved because 16.2% of participants strongly agreed that they were completely protected against COVID-19 after they fully completed the vaccination schedule. Only 36.4% of participants strongly disagreed that they did not need to undertake any other preventive measures after they fully completed the vaccination schedule. In addition, less than one-fifth of participants strongly agreed that vaccines developed by different manufacturers had different levels of efficacy (17.1%), and the available vaccines may not be effective on new variants compared with the original strain (12.8%). The WHO has emphasized the importance of managing the community’s expectations toward the vaccine to ensure that those who have been vaccinated do not stop practicing protective behaviors.36 Another issue is that only 30.3% of our participants strongly agreed that being vaccinated themselves contributed to the protection of the community against COVID-19. Vaccination not only protects oneself from COVID-19 but also helps create herd immunity to stop its spread and protect vulnerable groups who cannot get vaccinated.37 It is estimated that 65%-70% of the population needs to be vaccinated to achieve herd immunity against COVID-19.37 Hence, vaccination can be conceptualized as a social responsibility, which plays an important role in educating the community regarding the essentialness of COVID-19 vaccination.59 Indeed, it is documented that social responsibility is positively associated with COVID-19 vaccination intention.60 Considering the loss of life and economic consequences owing to COVID-19, social responsibility attached to vaccination should be emphasized by governments.59 Our findings highlight the need to tailor the current education program to enhance the community knowledge regarding both the essentialness and efficacy of vaccine.
Our study has some limitations. First, the government started the largest-ever COVID-19 vaccination program and enhanced the community education toward COVID-19 vaccines on the media to respond to an outbreak of COVID-19 during the study period. This may have influenced our participants’ responses to the survey. However, we believe that it is negligible given that we ended the study when the program started. Nevertheless, we have identified room for improvement of the community education programs. Second, many cities in Vietnam had been under lockdown during the study period making the online survey the most efficient method to collect data at large. Given the online survey, duplicate entries may be an issue and affect the validity of the study. However, before completing the survey, participants were asked to read the participant information sheet outlining the research purposes and what participants were required to do. Only participants who fully understood and agreed to participate in the study were enrolled in the study. We screened and reviewed potentially duplicate entries, and although we could not remove duplicates completely, these strategies should make them negligible. Third, given our study aimed to target the community at large, recruiting participants using a snowball sampling technique could cause selection bias. However, in addition to the online survey, we used a paper-based recruitment procedure in 2 largest cities in Vietnam to include those who were unable to complete the online survey such as the older and those who did not have an Internet-enabled device or Internet connection. The use of a combination of 2 different, complementary data collection methods helped include a diverse study population in our study, which increased the generalizability of the study’s results. Finally, responses to our vaccine knowledge questions can be influenced by study participants’ antivaccination attitudes, which were not assessed in this study. Consequently, our study may underestimate the true vaccine knowledge level among participants who want to avoid all vaccination or COVID-19 vaccination (antivaxxers).
Conclusion
People who are at young age, have low income or education levels, and work in nonclinical and nonhealth education fields have low COVID-19 vaccine knowledge levels. To ensure a successful COVID-19 vaccine rollout and sustainable control and prevention of COVID-19, it is crucial to improve the knowledge about vaccine essentialness and efficacy in the community. Community education programs may be beneficial from using those who have been vaccinated as role models.
Biographies
Minh Cuong Duong, MD, MMed, PhD, Lecturer, University of New South Wales, New South Wales, Australia
Bich Thuy Duong, MD, PhD, Clinical Doctor, Hospital for Tropical Diseases, Ho Chi Minh City, Vietnam
Hong Trang Nguyen, MD, MSc, Lecturer, Phenikaa University, Hanoi, Vietnam
Trang Nguyen Thi Quynh, BNurse, MPH, Lecturer, Phenikaa University, Hanoi, Vietnam
Duy Phong Nguyen, MD, MMed, PhD, Professor, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
Footnotes
Authors M.C. Duong and B.T. Duong contributed equally to this work.
Disclosure: The authors declare no relevant conflicts of interest or financial relationships.
Funding: Minh Cuong Duong is funded by the Australian Government through the Australian Alumni Grants Fund (AAGF-R3-00086).
ORCID Minh Cuong Duong: http://orcid.org/0000-0002-9300-0047
Appendix
Appendix 1
Questionnaire
I. General information:
|
………. |
|
□ Male □ Female |
|
…………. |
|
□ Northern Vietnam □ Middle Vietnam □ Southern Vietnam |
|
□ <2 □ 2 - <8 □ 8 - ≤15 □ 15 - <32 □ ≥32 |
|
□ Living alone □ Living with family □ Living with friends |
|
□ Less than high school □ High school □ College □ Undergraduate level or above |
|
□ Health students □ Non--health students □ Working in non-health related fields □ Being clinical doctor and/or health lecturer □ Working in other health related fields |
|
□ Do not have chronic conditions □ Having chronic, noncommunicable diseases □ Having chronic, communicable diseases |
|
□ Having COVID-19 or acquired COVID-19 previously □ Having a family member who has COVID-19 or acquired COVID-19 previously □ Having a friend/colleague who has COVID-19 or acquired COVID-19 previously □ Never acquire COVID-19, or know anyone who has COVID-19 or acquired COVID-19 previously |
∗To assist study participants in completing the questionnaire easily, the currency was converted to VND and the unit was VND per month in the Vietnamese version of the questionnaire.
II. COVID-19 vaccine knowledge:
1. I am completely protected against COVID-19 after I fully complete the COVID-19 vaccination schedule
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
2. I do not need to undertake any other COVID-19 preventive measures after I fully complete the COVID-19 vaccination schedule
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
3. Being vaccinated for COVID-19 myself contributes to the protection of the community against COVID-19
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
4. Getting vaccinated for COVID-19 is a good way to protect myself from COVID-19
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
5. I do not need to get vaccinated for COVID-19 because the COVID-19 outbreak is controlled very well in Vietnam.
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
6. COVID-19 vaccines developed by different manufacturers have different levels of efficacy
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
7. The available COVID-19 vaccines may be less effective on new variants compared with the original strain
| Strongly agree | Agree | Neutral/no opinion | Disagree | Strongly disagree |
|---|---|---|---|---|
Appendix 2
Details of participants’ responses to COVID-19 vaccine knowledge questions
| Questions response (assigned score) | Summary statistics n (%) |
|---|---|
| |
| Strongly agree (0) | 277 (16.2) |
| Agree (1) | 745 (43.6) |
| Neutral/no opinion (2) | 389 (22.8) |
| Disagree (3) | 259 (15.2) |
| Strongly disagree (4) | 38 (2.2) |
| |
| Strongly agree (0) | 25 (1.5) |
| Agree (1) | 55 (3.2) |
| Neutral/no opinion (2) | 199 (11.6) |
| Disagree (3) | 808 (47.3) |
| Strongly disagree (4) | 621 (36.4) |
| |
| Strongly agree (4) | 518 (30.3) |
| Agree (3) | 919 (53.8) |
| Neutral/no opinion (2) | 228 (13.4) |
| Disagree (1) | 31 (1.8) |
| Strongly disagree (0) | 12 (0.7) |
| |
| Strongly agree (4) | 352 (20.6) |
| Agree (3) | 885 (51.8) |
| Neutral/no opinion (2) | 323 (18.9) |
| Disagree (1) | 133 (7.8) |
| Strongly disagree (0) | 15 (0.9) |
| |
| Strongly agree (0) | 17 (1) |
| Agree (1) | 28 (1.6) |
| Neutral/no opinion (2) | 208 (12.2) |
| Disagree (3) | 745 (43.6) |
| Strongly disagree (4) | 710 (41.6) |
| |
| Strongly agree (4) | 292 (17.1) |
| Agree (3) | 819 (48) |
| Neutral/no opinion (2) | 463 (27.1) |
| Disagree (1) | 113 (6.6) |
| Strongly disagree (0) | 21 (1.2) |
| |
| Strongly agree (4) | 219 (12.8) |
| Agree (3) | 877 (51.3) |
| Neutral/no opinion (2) | 552 (32.3) |
| Disagree (1) | 54 (3.2) |
| Strongly disagree (0) | 6 (0.4) |
Appendix 3: Distribution of levels of COVID-19 vaccine knowledge in Vietnam.
References
- 1.Case J.B., Winkler E.S., Errico J.M., Diamond M.S. On the road to ending the COVID-19 pandemic: are we there yet? Virology. 2021;557:70–85. doi: 10.1016/j.virol.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang Chan E.Y., Shahzada T.S., Sham T.S.T., et al. Narrative review of nonpharmaceutical behavioural measures for the prevention of COVID-19 (SARS-CoV-2) based on the Health-EDRM framework. Br Med Bull. 2020;136(1):46–87. doi: 10.1093/bmb/ldaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Advice for the public: coronavirus disease (COVID-19) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Available at:
- 4.Kaur S.P., Gupta V. COVID-19 vaccine: a comprehensive status report. Virus Res. 2020;288:198114. doi: 10.1016/j.virusres.2020.198114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duong M.C., Nguyen H.T., Duong B.T. A cross-sectional study of knowledge, attitude, and practice towards face mask use amid the COVID-19 pandemic amongst university students in Vietnam. J Community Health. 2021;46(5):975–981. doi: 10.1007/s10900-021-00981-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kadkhoda K. Herd immunity to COVID-19. Am J Clin Pathol. 2021;155(4):471–472. doi: 10.1093/ajcp/aqaa272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edwards B., Biddle N., Gray M., Sollis K. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS One. 2021;16(3):e0248892. doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dror A.A., Eisenbach N., Taiber S., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abebe H., Shitu S., Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015–2025. doi: 10.2147/IDR.S312116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saeterdal I., Lewin S., Austvoll-Dahlgren A., Glenton C., Munabi-Babigumira S. Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst Rev. 2014;11(11):CD010232. doi: 10.1002/14651858.CD010232.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freeman D, Loe BS, Chadwick A, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II [e-pub ahead of print]. Psychol Med. https://doi.org/10.1017/S0033291720005188. Accessed May 10, 2021. [DOI] [PMC free article] [PubMed]
- 12.Al-Marshoudi S., Al-Balushi H., Al-Wahaibi A., et al. Knowledge, attitudes, and practices (KAP) toward the COVID-19 vaccine in Oman: a pre-campaign cross-sectional study. Vaccines (Basel) 2021;9(6):602. doi: 10.3390/vaccines9060602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elhadi M., Alsoufi A., Alhadi A., et al. Knowledge, attitude, and acceptance of healthcare workers and the public regarding the COVID-19 vaccine: a cross-sectional study. BMC Public Health. 2021;21(1):955. doi: 10.1186/s12889-021-10987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Islam M.S., Siddique A.B., Akter R., et al. Knowledge, attitudes and perceptions towards COVID-19 vaccinations: a cross-sectional community survey in Bangladesh. BMC Public Health. 2021;21(1):1851. doi: 10.1186/s12889-021-11880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumari A., Ranjan P., Chopra S., et al. Knowledge, barriers and facilitators regarding COVID-19 vaccine and vaccination programme among the general population: a cross-sectional survey from one thousand two hundred and forty-nine participants. Diabetes Metab. Syndr. 2021;15(3):987–992. doi: 10.1016/j.dsx.2021.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abu Hammour K., Abu Farha R., Manaseer Q., Al-Manaseer B. Factors affecting the public’s knowledge about COVID-19 vaccines and the influence of knowledge on their decision to get vaccinated. J Am Pharm Assoc (2003) 2022;62(1):309–316. doi: 10.1016/j.japh.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallè F., Sabella E.A., Roma P., et al. Knowledge and acceptance of COVID-19 vaccination among undergraduate students from central and Southern Italy. Vaccines (Basel) 2021;9(6):638. doi: 10.3390/vaccines9060638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duong M.C., Nguyen H.T., Duong B.T., Vu M.T. The levels of COVID-19 related health literacy among university students in Vietnam. Infect Chemother. 2021;53(1):107–117. doi: 10.3947/ic.2020.0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoang T.D., Colebunders R., Fodjo J.N.S., Nguyen N.P.T., Tran T.D., Vo T.V. Well-being of healthcare workers and the General Public during the COVID-19 pandemic in Vietnam: an online survey. Int J Environ Res Public Health. 2021;18(9):4737. doi: 10.3390/ijerph18094737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le X.T.T., Nguyen H.T., Le H.T., et al. Rural-urban differences in preferences for influenza vaccination among women of childbearing age: implications for local vaccination service implementation in Vietnam. Trop Med Int Health. 2021;26(2):228–236. doi: 10.1111/tmi.13515. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen T.T.M., Lafond K.E., Nguyen T.X., et al. Acceptability of seasonal influenza vaccines among health care workers in Vietnam in 2017. Vaccine. 2020;38(8):2045–2050. doi: 10.1016/j.vaccine.2019.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li X., Wiesen E., Diorditsa S., et al. Impact of Adverse Events Following Immunization in Viet Nam in 2013 on chronic hepatitis B infection. Vaccine. 2016;34(6):869–873. doi: 10.1016/j.vaccine.2015.05.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ministry of Health COVID-19 bulletin on the evening of July 16: Hanoi, Ho Chi Minh City and 23 provinces added 1,883 new cases. https://ncov.moh.gov.vn/vi/web/guest/-/6847426-5839 Available at:
- 24.Ministry of Health Vietnam Ministry of Health's Covid-19 pandemic information portal. https://ncov.moh.gov.vn/en/web/guest/trang-chu Available at:
- 25.Ministry of Health Information on a death after receiving vaccine against COVID-19: an anaphylaxis occurred in a patient with a history of NSAIDS hypersensitivity. https://moh.gov.vn/tin-lien-quan/-/asset_publisher/vjYyM7O9aWnX/content/ca-tu-cong-sau-tiem-vaccine-phong-covid-19-soc-phan-ve-tren-nen-co-ia-di-ung-non-steroid Available at:
- 26.Ministry of Health Hanoi officially provided information on the death of a young, male teacher after receiving a COVID-19 vaccine. https://ncov.moh.gov.vn/en/web/guest/-/6847426-4938 Available at:
- 27.Ministry of Health Expanding eligible groups for COVID-19 vaccination in the largest-ever vaccination campaign. https://ncov.moh.gov.vn/en/-/6847912-298 Available at:
- 28.Varela C., Ruiz J., Andrés A., Roy R., Fusté A., Saldaña C. Advantages and disadvantages of using the website SurveyMonkey in a real study: psychopathological profile in people with normal-weight, overweight and obesity in a community sample. E-Methodology. 2016;3:77–89. [Google Scholar]
- 29.Zhong B.L., Luo W., Li H.M., et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745–1752. doi: 10.7150/ijbs.45221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sharma G. Pros and cons of different sampling techniques. Int J Appl Res. 2017;3(7):749. [Google Scholar]
- 31.Coxhead I., Nguyen C.V., Vu L.H. Migration in Vietnam: new evidence from recent surveys. http://documents.worldbank.org/curated/en/969411468197949288/pdf/102310-NWP-Migration-in-Vietnam-Nov-18-clean-Box-394830B-PUBLIC.pdf Available at:
- 32.Ministry of Land Infrastructure, Transport and Tourism. An Overview of Spatial Policy in Asian and European Countries: Vietnam. https://www.mlit.go.jp/kokudokeikaku/international/spw/general/vietnam/index_e.html Available at:
- 33.Gapminder Income levels. 2021. https://www.gapminder.org/fw/income-levels/ Available at:
- 34.AstraZeneca COVID-19 vaccine AstraZeneca confirms 100% protection against severe disease, hospitalisation and death in the primary analysis of Phase III trials. https://www.astrazeneca.com/media-centre/press-releases/2021/covid-19-vaccine-astrazeneca-confirms-protection-against-severe-disease-hospitalisation-and-death-in-the-primary-analysis-of-phase-iii-trials.html?fbclid=IwAR2Wj5ZeAxfasHfTcB1SKhsC49s0fIVprg7K-E4XM9y5D3jym0cPUb0Pdn4 Available at:
- 35.World Health Organization COVID-19 advice for the public: getting vaccinated. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines/advice Available at:
- 36.World Health Organization Behavioural considerations for acceptance and uptake of COVID-19 vaccines. https://www.who.int/publications/i/item/9789240016927 Available at:
- 37.Fontanet A., Cauchemez S. COVID-19 herd immunity: Where are we? Nat Rev Immunol. 2020;20(10):583–584. doi: 10.1038/s41577-020-00451-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Polack F.P., Thomas S.J., Kitchin N., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lopez Bernal J., Andrews N., Gower C., et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med. 2021;385(7):585–594. doi: 10.1056/NEJMoa2108891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Garcia-Beltran W.F., Lam E.C., St Denis K., et al. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell. 2021;184(9):2372–2383.e9. doi: 10.1016/j.cell.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qunaibi E.A., Helmy M., Basheti I., Sultan I. A high rate of COVID-19 vaccine hesitancy in a large-scale survey on Arabs. eLife. 2021;10:e68038. doi: 10.7554/eLife.68038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [Published correction appears in J Med Internet Res. 2012;14(1):e8] J Med Internet Res. 2004;6(3):e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boni R.B. Web surveys in the time of COVID-19. Cad Saude Publica. 2020;36(7):e00155820. doi: 10.1590/0102-311x00155820. [DOI] [PubMed] [Google Scholar]
- 44.Equator Network The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Available at. https://www.equator-network.org/reporting-guidelines/strobe/ [DOI] [PMC free article] [PubMed]
- 45.General Statistics Office Completed results of the 2019 Vietnam population and housing census. Statistical Publishing House. https://www.gso.gov.vn/wp-content/uploads/2019/12/Ket-qua-toan-bo-Tong-dieu-tra-dan-so-va-nha-o-2019.pdf Available at:
- 46.CEIC Data Vietnam monthly earnings. https://www.ceicdata.com/en/indicator/vietnam/monthly-earnings Available at:
- 47.Centers for Disease Control and Prevention Building confidence in COVID-19 vaccines. https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence.html Available at: [PubMed]
- 48.Van Nhu H., Tuyet-Hanh T.T., Van N.T.A., Linh T.N.Q., Tien T.Q. Knowledge, attitudes, and practices of the Vietnamese as key factors in controlling COVID-19. J Community Health. 2020;45(6):1263–1269. doi: 10.1007/s10900-020-00919-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nguyen H.T.T., Dinh D.X., Nguyen V.M. Knowledge, attitude and practices of community pharmacists regarding COVID-19: a paper-based survey in Vietnam. PLoS One. 2021;16(7):e0255420. doi: 10.1371/journal.pone.0255420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duong MC, Nguyen HT, Duong BT, Vu MT. Assessment of hand hygiene practices of university students in Vietnam amid the COVID-19 pandemic: a brief report [e-pub ahead of print]. Disaster Med Public Health Prep. https://doi.org/10.1017/dmp.2021.256. Accessed August 24, 2021. [DOI] [PMC free article] [PubMed]
- 51.Islam J.Y., Khatun F., Alam A., et al. Knowledge of cervical cancer and HPV vaccine in Bangladeshi women: a population based, cross-sectional study. BMC Womens Health. 2018;18(1):15. doi: 10.1186/s12905-018-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Biswas N., Mustapha T., Khubchandani J., Price J.H. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qunaibi E., Basheti I., Soudy M., Sultan I. Hesitancy of Arab healthcare workers towards COVID-19 vaccination: a large-scale multinational study. Vaccines (Basel) 2021;9(5):446. doi: 10.3390/vaccines9050446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Larson H.J. Negotiating vaccine acceptance in an era of reluctance. Hum Vaccin Immunother. 2013;9(8):1779–1781. doi: 10.4161/hv.25932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nguyen V.T., Nguyen M.Q., Le N.T., Nguyen T.N.H., Huynh G. Predictors of intention to get a COVID-19 vaccine of health science students: a cross-sectional study. Risk Manag Healthc Policy. 2021;2021(14):4023–4030. doi: 10.2147/RMHP.S328665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shekhar R., Sheikh A.B., Upadhyay S., et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines (Basel) 2021;9(2):119. doi: 10.3390/vaccines9020119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Petrelli F., Tiffi F., Scuri S., Nguyen C.T.T., Grappasonni I. The pharmacist's role in health information, vaccination and health promotion. Ann Ig. 2019;31(4):309–315. doi: 10.7416/ai.2019.2264. [DOI] [PubMed] [Google Scholar]
- 58.Orenstein W.A., Ahmed R. Simply put: vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114(16):4031–4033. doi: 10.1073/pnas.1704507114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Calnan M., Douglass T. Hopes, hesitancy and the risky business of vaccine development. Health Risk Soc. 2020;22(5–6):291–304. [Google Scholar]
- 60.Yu Y, Luo S, Mo PK, et al. Prosociality and social responsibility were associated with intention of COVID-19 vaccination among university students in China [e-pub ahead of print]. Int J Health Policy Manag. https://doi.org/10.34172/ijhpm.2021.64. Accessed August 24, 2021. [DOI] [PMC free article] [PubMed]