Abstract
Background:
Extreme heat exposures are increasing with climate change. Health effects are well documented in adults, but the risks to children are not well characterized.
Objectives:
We estimated the association between warm season (May to September) temperatures and cause-specific emergency department (ED) visits among U.S. children and adolescents.
Methods:
This multicenter time-series study leveraged administrative data on ED visits by children and adolescents of age to the EDs of 47 U.S. children’s hospitals from May to September from 2016 to 2018. Daily maximum ambient temperature was estimated in the county of the hospital using a spatiotemporal model. We used distributed-lag nonlinear models with a quasi-Poisson distribution to estimate the association between daily maximum temperature and the relative risk (RR) of ED visits, adjusting for temporal trends. We then used a random-effects meta-analytic model to estimate the overall cumulative association.
Results:
Extreme heat was associated with an RR of all-cause ED visits of 1.17 (95% CI: 1.12, 1.21) relative to hospital-specific minimum morbidity temperature. Associations were more pronounced for ED visits due to heat-related illness including dehydration and electrolyte disorders ( 1.83; 95% CI: 1.31, 2.57), bacterial enteritis (1.35; 95% CI: 1.02, 1.79), and otitis media and externa (1.30; 95% CI: 1.11, 1.52). Taken together, temperatures above the minimum morbidity temperature accounted for an estimated 11.8% [95% empirical 95% confidence interval (eCI): 9.9%, 13.3%] of warm season ED visits for any cause and 31.0% (95% eCI: 17.9%, 36.5%) of ED visits for heat-related illnesses.
Conclusion:
During the warm season, days with higher temperatures were associated with higher rates of visits to children’s hospital EDs. Higher ambient temperatures may contribute to a significant proportion of ED visits among U.S. children and adolescents. https://doi.org/10.1289/EHP8083
Introduction
High ambient temperature or heat leads to substantial excess morbidity and mortality (Hess et al. 2014; Sarofim et al. 2016). This assessment is based on a large body of evidence, predominantly among older adults, documenting associations between heat exposure and mortality, as well as health care utilization for heat-related illness, cardiovascular events, and suicide, among other conditions (Bobb et al. 2014; Chen et al. 2017; Gronlund et al. 2014; Guo et al. 2017; Hess et al. 2014; Kim et al. 2019; Lavados et al. 2018; Madrigano et al. 2013; Sun et al. 2019b).
Children have often been identified as vulnerable to heat given their physiologic differences in thermoregulatory capacity in comparison with adults and their dependence on adults for protection from heat exposure (Falk and Dotan 2008; Stanberry et al. 2018; Vanos 2015). However, relatively few studies have quantified the association between heat and health in children (Iñiguez et al. 2016; Knowlton et al. 2009; Sheffield et al. 2018; Son et al. 2019; van Loenhout et al. 2018; Xu et al. 2014a), and none of these studies have done so on a large scale across the United States. The limited existing evidence suggests that heat is associated with higher risk of sudden death among infants (Basu and Ostro 2008), emergency department (ED) visits for heat-related illnesses (Knowlton et al. 2009; Sheffield et al. 2018), injuries (Sheffield et al. 2018), and diarrheal diseases (Xu et al. 2014b), with the magnitude of the associations varying by age. The consequences of heat exposure in infants, children, and adolescents may differ from those in adults given the relatively higher prevalence of specific conditions in children (e.g., ear infections, diarrheal disease), as well as the unique susceptibility of children due to their developing organ systems and different behavior patterns vs. adults (American Academy of Pediatrics Council on Environmental Health 2018).
Identifying the health risks to children from heat is of particular importance given the growing number of extreme heat days due to continued climate change (Vose et al. 2017). To characterize the relevance of heat to children’s health, we analyzed data on more than ED visits from May to September from 2016 to 2018 to standalone children’s hospitals in 27 states. We estimated the relative risk (RR) of ED visits for any cause and for specific causes and evaluated the fraction and number of these visits attributable to warm season days with nonoptimum ambient temperature for each location during May to September.
Methods
Study Population
The institutional review board at Boston Children’s Hospital determined that this project did not constitute human subjects research and was granted a waiver of informed consent on that basis. We obtained data on ED visits between May and September from 2016 to 2018 from 47 children’s hospitals that were participating in the Pediatric Health Information System (PHIS) (https://www.childrenshospitals.org/phis) during this interval. PHIS is a pediatric database that includes clinical and resource utilization data for inpatient, observation, ambulatory surgery, and ED patient encounters for 50 children’s hospitals in 27 states (https://www.childrenshospitals.org/phis).
For each visit, we obtained data on admission date, primary discharge diagnosis code from the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) (National Center for Health Statistics 2019), age, sex, race, health insurance status, and hospital name. We restricted the analyses to children and adolescents of age, who accounted for 96.2% of all ED visits over the study period. Administrative staff at each hospital assigned codes for race during the clinical encounter based upon patient or guardian self-report using PHIS-designated categories that included “White,” “Black or African American,” “Asian,” “Native Hawaiian or Pacific Islander,” “American Indian or Alaskan Native,” or “Other.” Ethnicity was similarly assigned as “Hispanic or Latino,” “Not Hispanic or Latino,” or “Other.” Some states prohibit hospitals from asking families about race and ethnicity and, in these places, hospital staff used their judgment to assign race and ethnicity codes. We defined a priori broad categories of ED visit cause based upon primary discharge diagnosis using a combination of findings from prior research and pathophysiologically plausible but previously unexplored links, with the intent of considering a broad scope of potential health impacts of heat (Table 1). Groupings of ED visit causes were mutually exclusive, with the exception of asthma (also included in diseases of the respiratory system), bacterial enteritis (also included in infectious and parasitic diseases), and suicidality and depression (also included in mental, behavioral, and neurodevelopmental disorders, as well as other signs and symptoms). We calculated the daily number of ED visits to each hospital, overall and aggregated by cause, age (0–5, 6–12, and 13–18 y), sex (male or female), and insurance status (public, private, other/unknown). Race was grouped as White or other race group (i.e., those identified as “Black or African American,” “Asian,” “Native Hawaiian or Pacific Islander,” “American Indian or Alaskan Native,” or “Other”) given uncertainty in the correct assignment of race by hospital staff.
Table 1.
Mean number of daily ED visits for all and specific causes across 47 participating children’s hospitals, May to September from 2016 to 2018.
| Causes of ED visits | ICD-10 codes | Mean (SD) | Percentile | ||
|---|---|---|---|---|---|
| 25th | 50th | 75th | |||
| All-cause | A00–U99 | 8,306 (802) | 7,622 | 8,236 | 8,867 |
| Infectious and parasitic diseases | A00–B99 | 586 (67) | 541 | 582 | 624 |
| Bacterial enteritis | A00–A09 | 90 (16) | 79 | 88 | 98 |
| Blood and immune system disorders | D50–D89 | 72 (10) | 64 | 71 | 79 |
| Endocrine, nutritional, and metabolic diseases | E00–E85, E88–E89 | 56 (13) | 46 | 56 | 64 |
| Mental, behavioral, and neurodevelopmental disordersa | F00–F99 | 152 (54) | 113 | 134 | 194 |
| Nervous system diseases | G00–G99 | 147 (28) | 126 | 143 | 164 |
| Otitis media and externa | H60, H65–H67 | 295 (56) | 252 | 289 | 328 |
| Cardiovascular diseases | I00–I99 | 40 (8) | 34 | 40 | 45 |
| Respiratory system diseases | J00–J99 | 1,277 (355) | 937 | 1,266 | 1,572 |
| Asthma | J45 | 256 (103) | 162 | 241 | 342 |
| Digestive system diseases | K00–K93 | 570 (51) | 534 | 562 | 599 |
| Skin and soft tissue infections | L00–L08 | 210 (28) | 192 | 209 | 229 |
| Other skin and soft tissue diseases | L09–L99 | 201(24) | 184 | 198 | 215 |
| Musculoskeletal system diseases | M00–M99 | 224 (42) | 192 | 214 | 251 |
| Genitourinary system diseases | N00–N99 | 236 (22) | 220 | 236 | 249 |
| Perinatal conditions | P00–P96 | 101 (14) | 92 | 101 | 110 |
| Other signs and symptomsa | R00–R99 | 1,632 (157) | 1,512 | 1,599 | 1,726 |
| Injury and poisoning | S00–T66, T68–T88 | 2,025 (147) | 1,908 | 2,017 | 2,126 |
| External causes and other health factors | V01–Z99 | 182 (27) | 164 | 179 | 196 |
| Heat-related illness | T67, E86, E87 | 63 (11) | 56 | 62 | 69 |
| Suicidality and depressiona | R45.85, R45.86, R45.87, R45.1, R45.4, R45.5, R45.6, F32, F33 | 72 (37) | 46 | 60 | 94 |
Note: Sample sizes for specific causes are the same as indicated in Figure 2. ED, emergency department; ICD-10, International Classification of Diseases, Tenth Revision, Clinical Modification; SD, standard deviation.
Diagnoses included in “suicidality and depression,” “mental, behavioral, and neurodevelopmental disorders,” and “other signs and symptoms” partially overlap.
Assessment of Ambient Temperature
We estimated daily maximum ambient temperature using the Parameter-elevation Relationships on Independent Slopes Model (PRISM), an established spatiotemporal model with approximately 4-km horizontal grid spacing (Daly et al. 2008). This model provides spatially resolved estimates of meteorological variables, in contrast to point-based observations at individual weather stations, which may not always adequately represent the temperature across large and geographically heterogenous areas (Spangler et al. 2019). Because we did not have information on patients’ residential addresses, we calculated the population-weighted mean of daily maximum temperatures () in the county in which the hospital is located as a proxy for patients’ exposure (Sun et al. 2019b; Weinberger et al. 2020). Specifically, we calculated the spatially resolved county mean by first extracting the PRISM pixels at the population centroids for each census tract within a county and multiplied this daily value by the proportion of the county population falling within that census tract (Spangler et al. 2019). We then summed the resulting values across all census tracts within each county of interest to obtain the county population-weighted mean value. We used an analogous approach to obtain population-weighted estimates of maximum, minimum, and mean daily temperature and heat index. For heat index, we used the weathermetrics R package, which follows the calculations used by the National Weather Service (Anderson et al. 2013). We computed Pearson correlation coefficients among different temperature metrics to determine whether alternative metrics should be considered.
Assessment of Air Pollution
We obtained daily mean fine particulate matter [PM in aerodynamic diameter ()] and ozone () from the air pollution monitoring station network of the U.S. Environmental Protection Agency (U.S. EPA 2020). We obtained daily mean and concentrations from the monitoring station that was closest to each hospital. If air pollution data were missing, we imputed missing values by linear interpolation using the na.approx function in the R zoo package (Pun et al. 2015; Sun et al. 2019a).
Statistical Analysis
We used a well-established two-stage analytic approach (Gasparrini et al. 2015, 2016) to quantify the association between maximum daily temperature and RR of all-cause and cause-specific ED visits between May and September from 2016 to 2018. In the first-stage analysis, we used distributed-lag nonlinear models with a quasi-Poisson distribution to estimate the association between day-to-day variation in maximum temperature and the RR of ED visits separately for each of the 47 hospitals participating in PHIS at the time of analysis, adjusting for temporal trends. We modeled the exposure–response function using a quadratic B-spline with one internal knot placed at the 50th percentile of hospital-specific warm season temperature distribution and modeled the time–response function using a natural cubic B-spline with two knots placed at equal intervals on the log scale with lags up to 7 d. We controlled for seasonality using a natural cubic B-spline of day of the warm season (May to September) with 4 degrees of freedom (df) per year; controlled for long-term trends using a natural cubic B-spline of time with approximately 1 df every 10 y; adjusted for same-day maximum relative humidity using a natural cubic spline with 3 df; and adjusted for day of week and federal holidays using indicator variables.
In the second stage of the analyses, we used a random-effects meta-analytic model to estimate the overall cumulative association between heat and ED visits across the 47 hospitals (Gasparrini et al. 2012). To account for residual interhospital heterogeneity due to differing temperature distributions across hospitals, we included hospital-specific median high daily temperature and range of over the 3 y studied as predictors in the second-stage meta-regression. From this model, we extracted the best linear unbiased prediction (BLUP) of the temperature–morbidity association for each hospital. The BLUP approach allows estimates for locations with less information to borrow from locations with more information. For ease of communication, we defined days of extreme heat as those at or above the 95th percentile of the cause-specific, hospital-specific warm season distribution and defined days of moderate temperature as those days with temperatures between the cause-specific, hospital-specific minimum morbidity temperature (MMT) and the 95th percentile of the hospital-specific warm season distribution. The MMT was derived from the BLUP of the overall cumulative exposure–response association in each hospital and corresponds to an MMT percentile between the first and the 99th percentiles.
Sensitivity Analysis
We conducted a series of sensitivity analyses to assess the robustness of our findings. First, to assess potential confounding air pollution, we adjusted for and (in separate models) as linear continuous variables. We note that it may or may not be appropriate to adjust for air pollutants when considering the health effects of temperature (Buckley et al. 2014; Reid et al. 2012). Second, to ensure appropriate control for seasonality, we repeated the analyses using a natural cubic B-spline of the day of the season with 6 df/y rather than 4 df.
Estimation of Attributable Risk
We estimated the fraction and number of ED visits attributable [(i.e., attributable fraction (AF) and attributable number (AN)] to ambient temperatures above the MMT, as previously described (Gasparrini and Leone 2014). Briefly, for each location, we first calculated the number of ED visits attributable to heat () as follows:
where is the cumulative RR of ED visits for hospital on day associated with vs. MMT for hospital i during May to September, and is the moving average of daily ED visits in hospital on day (lag 0) and the 7 d after day t (lags 1–7). We then estimated the total number of ED visits attributable to heat by summing the attributable number of ED visits each day with maximum temperature above the MMT for hospital i during May to September.
We subsequently estimated the AF by dividing the AN associated with s above the MMT by the total number of ED visits for the corresponding cause. To quantify the uncertainty in these estimates, we derived empirical 95% confidence intervals (eCIs) for the AN and AF using Monte Carlo simulations (5,000 random samples), assuming a multivariate normal distribution of the BLUP of the reduced coefficients.
We applied the Bonferroni-Holm method to control for type I error due to multiple comparisons and an adjusted was considered statistically significant (Holm 1979). The 95% confidence intervals (CIs) were corrected by using , where D is the number of disease groups considered (Dunn 1961).
Subgroup Analyses
Using fully stratified models, we evaluated whether the association between temperature and risks of ED visits varied across subgroups defined by age (0–5, 6–12, and 13–18 y), sex (male vs. female), race (White vs. other groups), and insurance status (public, private, other/unknown). These subgroups were chosen because we expected that age, sex, race, and insurance status might all influence the likelihood that a child may be brought to an ED for medical care. Children of different races, ethnicities, ages, and genders present to EDs at different rates (National Center for Health Statistics 2019) Differences observed by race and ethnicity may reflect structural racism that has resulted in differential access to care (Bailey et al. 2017). Insurance status also has been associated with ED utilization. Notably, children on Medicaid and children in households at of the federal poverty level as compared with those in households at of that level use EDs at about twice the rate as children with private insurance (National Center for Health Statistics 2019). This suggests that ED use may be driven more by social determinants of health, such as income and health literacy, than out-of-pocket costs or insurance status per se (Morrison et al. 2014; Schlichting et al. 2017). We implemented a Wald statistic to test whether the association between ED visits and daily temperature was homogeneous across strata. We considered a as heterogeneous across strata.
We conducted all analyses in R (version 3.4.3; R Development Core Team). We used the dlnm package for the distributed-lag nonlinear time-series analysis and the mvmeta package for the second-stage meta-analysis (Gasparrini 2011; Gasparrini et al. 2012). Annotated R code for this analysis is provided at the end of the Supplemental Material.
Results
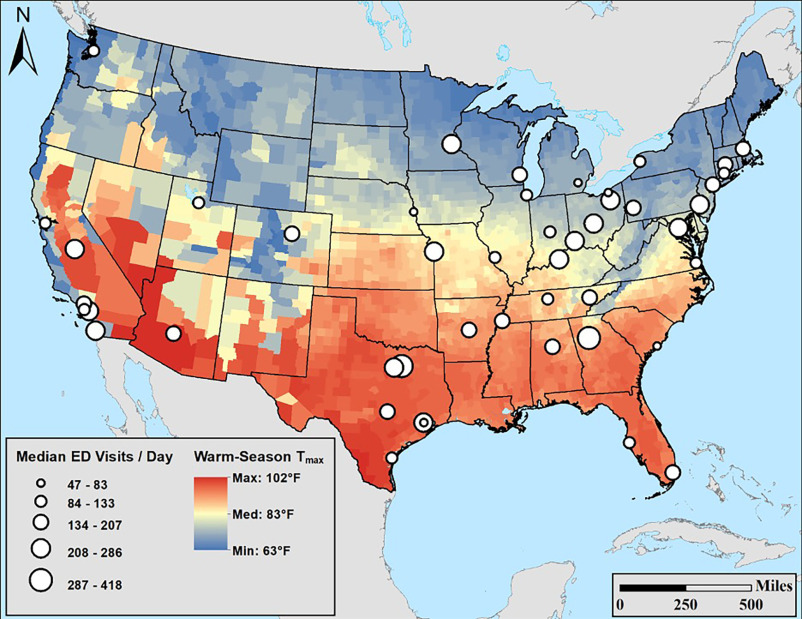
Between May and September from 2016 to 2018, there were ED visits to 47 participating children’s hospitals in 27 states across the United States (Figure 1). Patients were slightly more likely to be male (53.1% vs. 46.9%) and younger (54.4%, 0–5; 27.8%, 6–12; and 17.8%, 13–18 years of age) (Table S1). Of the patients with ED visits, 64.2% had public insurance and 26.9% had private insurance (Table S1). Among the groupings of discharge codes considered, ED visits for injury and poisonings were most common, followed by those for nonspecific signs and symptoms and those for diseases of the respiratory system (Table 1).
Figure 1.
Map showing the locations of participating children’s hospitals (), median numbers of ED visits among children and adolescents of age, and mean daily maximum temperatures during May to September from 2016 to 2018. Note: ED, emergency department; ; mean daily maximum temperature.
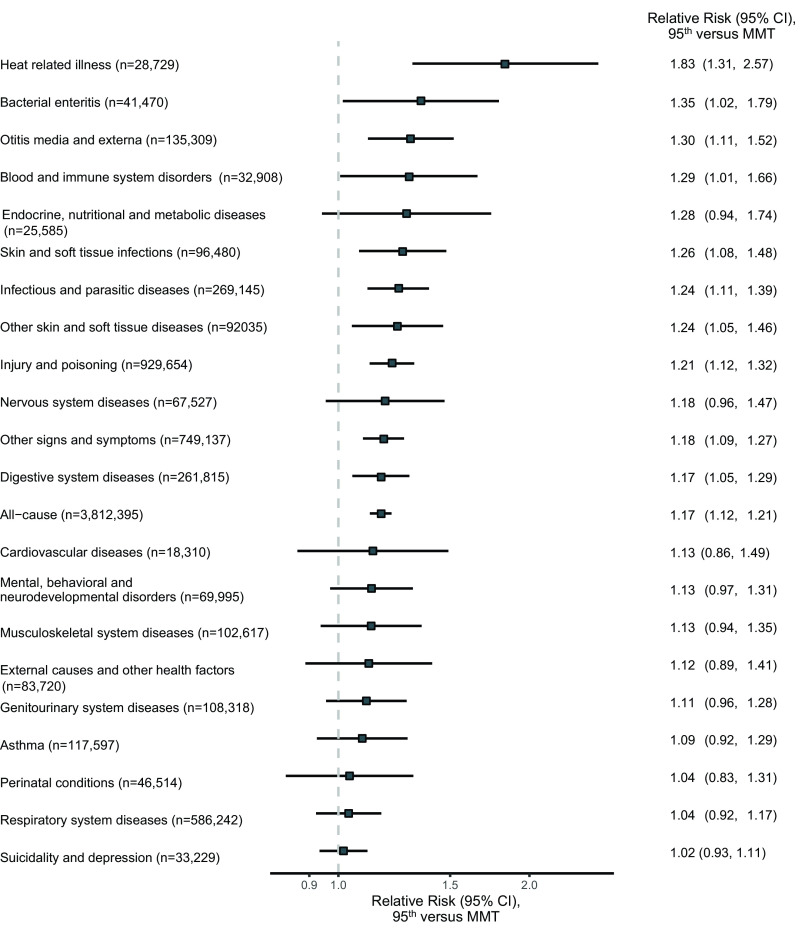
The shape of the exposure–response curves was approximately linear, with some variation across categories of causes, suggesting a continuum of risk across the warm season temperature range (Figures S1 and S2). The exposure–response curve was not monotonic for bacterial enteritis, and outcomes that were not as strongly associated with heat were less likely to have monotonic associations (e.g., musculoskeletal system diseases, injury, poisoning) when a quadratic B-spline was applied (Figure S1). Associations were usually strongest with the maximum daily temperature on the day of the ED visit (lag 0). However, for some specific causes, higher maximum daily temperatures were associated with ED visits 1–7 d later (Figure S3). For illustration, we present the RR at the hospital-specific 95th percentile of maximum daily temperature vs. the MMT. Extreme heat was positively associated with a higher rate of ED visits for all causes ( 1.17; 95% CI: 1.12, 1.21) over the next 7 d, as well as higher rates of ED visits for a number of specific causes (Figure 2). Days of extreme heat were most strongly associated with higher rates of ED visits for heat-related illness ( 1.83, 95% CI: 1.31, 2.57), bacterial enteritis ( 1.35, 95% CI: 1.02, 1.79), and otitis media and externa ( 1.30, 95% CI: 1.11, 1.52). ED visits for several conditions, including “asthma,” “respiratory system diseases,” and “mental, behavioral, and neurodevelopmental disorders,” were not clearly associated with higher temperatures (Figure 2; Figure S1).
Figure 2.
RRs and 95% CIs of the association of specific causes of emergency department visits with . RRs contrast the 95th percentile of the hospital-specific warm season (May to September) distribution to the hospital-specific minimum morbidity temperature (MMT) over lag 0–7 d among 47 participating children’s hospitals from May to September from 2016 to 2018. The temperature–ED visit association was modeled with a quasi-Poisson regression with distributed-lag nonlinear model for each hospital, controlling for temporal trends, seasonality, relative humidity, federal holidays, and day of the week. RRs are then pooled across the 47 participating hospitals using multivariate random-effect meta-analyses with hospital-specific mean and range of temperatures as the predictors. Note: CI, confidence interval; RR, relative risk; , mean daily maximum temperature.
RRs were very similar in sensitivity analyses that additionally included adjustment for air pollutants or controlling for seasonality using a natural cubic B-spline of the day of the season with 6 df/y (Figure S4). Minimum, mean, and maximum daily values of temperature and heat index were moderately to highly correlated (Figure S5).
To characterize the potential burden of disease, we estimated the fraction and number of ED visits potentially attributable to hot days using a distributed-lag nonlinear model with estimated numbers of visits summed over 0–7 d (Table 2; Table S2). Temperatures greater than the MMT accounted for 11.8% (95% eCI: 9.9, 13.3) of all warm season ED visits, 31% (95% eCI: 17.9, 36.5%) of visits for heat-related illnesses, and 25.2% (95% eCI: 13.2, 31.1%) of visits for bacterial enteritis. More common causes of ED visits were associated with a greater absolute number of visits attributable to heat, notably all-cause ED visits and visits for injuries and poisonings.
Table 2.
The attributable number and fraction for specific causes of ED visits attributable to temperatures above the minimum morbidity temperature over lag 0–7 d during May to September from 2016 to 2018 in 47 participating U.S. children’s hospitals.
| Causes of ED visits | Attributable fraction (95% eCI) (%) | Attributable number (95% eCI) |
|---|---|---|
| Heat-related illness | 31.0 (17.9, 36.5) | 8,895 (5,152, 10,494) |
| Otitis media and externa | 13.5 (8.4, 17.0) | 18,204 (11,433, 23,008) |
| Bacterial enteritis | 25.2 (13.2, 31.1) | 10,443 (5,457, 12,896) |
| Infectious and parasitic diseases | 13.8 (11.6, 15.6) | 37,269 (31,263, 41,863) |
| Blood and immune system disorders | 17.1 (11.2, 21.7) | 5,614 (3,672, 7,139) |
| Nervous system diseases | 14.5 (6.1, 19.3) | 9,797 (4,112, 13,028) |
| Skin and soft tissue infections | 17.7 (15.1, 20.1) | 17,119 (14,603, 19,404) |
| Other skin and soft tissue diseases | 16.7 (13.3, 19.4) | 15,408 (12,256, 17,814) |
| Other signs and symptoms | 11.3 (8.4, 13.7) | 84,794 (62,995, 102,441) |
| Endocrine, nutritional, and metabolic diseases | 19.2 (8.8, 24.2) | 4,922 (2,243, 6,185) |
| Cardiovascular diseases | 10.7 (, 16.8) | 1,967 (, 3,074) |
| Digestive system diseases | 11.7 (8.1, 14.7) | 30,738 (21,129, 38,540) |
| All-cause | 11.8 (9.9, 13.3) | 448,096 (378,388, 508,309) |
| Mental, behavioral, and neurodevelopmental disorders | 9.9 (6.2, 12.7) | 6,937 (4,315, 8,858) |
| Injury and poisoning | 17.7 (14.9, 20.0) | 164,894 (138,089, 185,536) |
| Genitourinary system diseases | 9.5 (6.2, 12.4) | 10,343 (6,716, 13,470) |
| External causes and other health factors | 12.0 (3.4, 16.9) | 10,063 (2,857, 14,114) |
| Respiratory system diseases | 8.7 (5.0, 11.5) | 50,925 (29,056, 67,599) |
| Musculoskeletal system diseases | 10.6 (4.5, 14.8) | 10,912 (4,591, 15,157) |
| Asthma | 11.7 (6.3, 15.5) | 13,813 (7,364, 18,172) |
| Perinatal conditions | 6.7 (, 11.6) | 3,118 (, 5,410) |
| Suicidality and depression | 3.8 (, 7.3) | 1,263 (, 2,409) |
Note: We fitted a time-series Poisson regression for each hospital, controlling for temporal trends, seasonality, relative humidity, federal holiday, and day of the week. We estimated temperature–ED visits associations with a distributed-lag nonlinear model with 7 d of lag, and then pooled them in a multivariate random-effect meta-analyses with hospital-specific mean and range of as the predictors. We then calculated the attributable number and fraction of ED visits based on the best linear unbiased prediction of the overall cumulative exposure–response association in each hospital. eCI, empirical confidence interval; ED, emergency department; , mean daily maximum temperature.
We assessed whether the association between days of heat and risk of all-cause and heat-related ED visits varied across subgroups defined by age, sex, race, or health insurance (Figure 3). Days of extreme heat were more strongly associated with ED visits for all causes among children who belonged to minority racial groups (1.21; 95% CI: 1.15, 1.28) vs. White children (1.12; 95% CI: 1.05, 1.19; ), and in children with public health insurance (1.18; 95% CI: 1.09, 1.27) or other/unknown insurance (1.14; 95% CI: 0.94, 1.37) than in children with private insurance (1.12; 95% CI: 1.06, 1.17; ).
Figure 3.
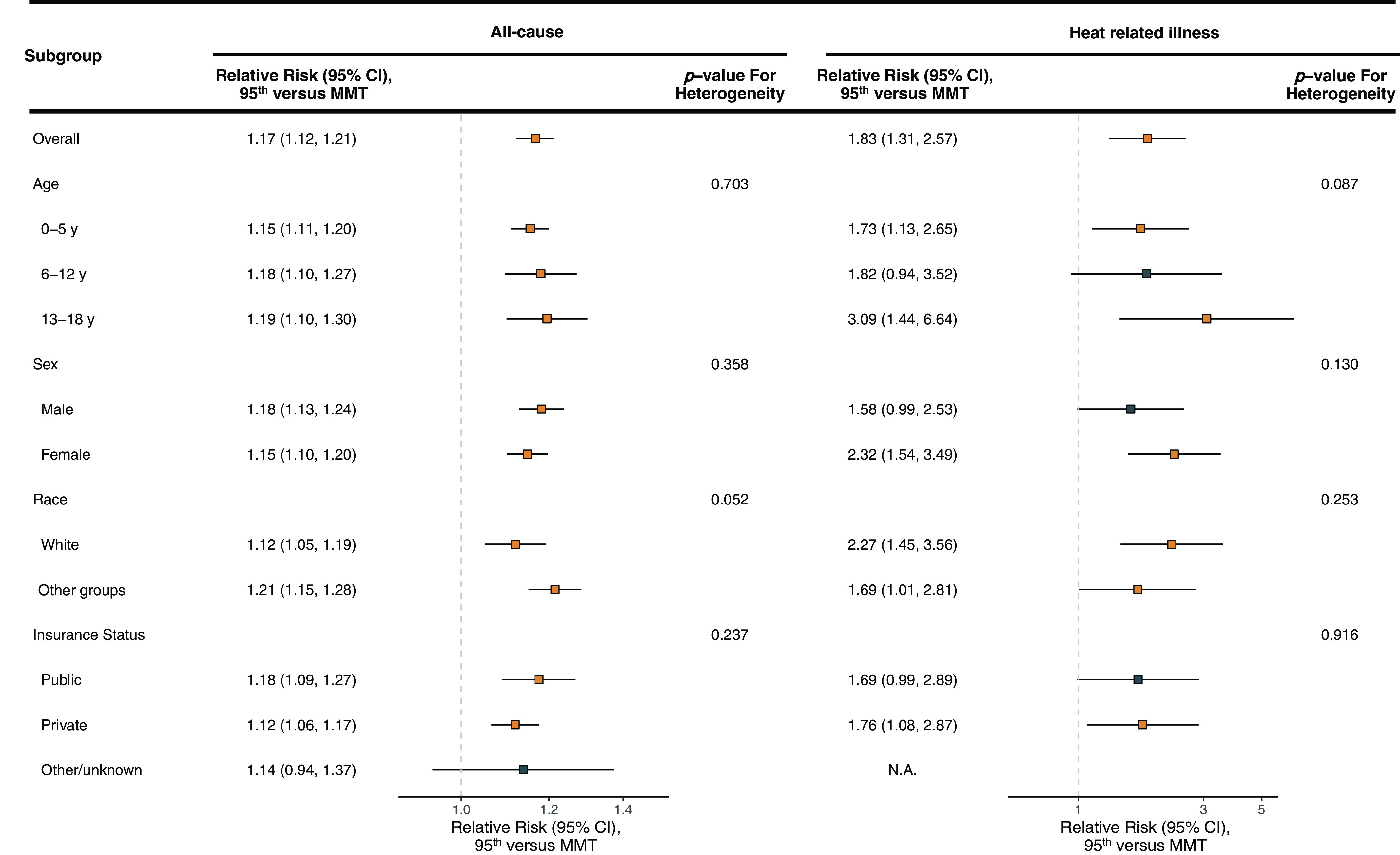
Pooled RRs and 95% CIs of ED visits for all causes and heat-related illness overall and stratified by patient demographics. RRs contrast the 95th percentile of the hospital-specific warm season (May to September) distribution to the hospital-specific minimum morbidity temperature (MMT), over lag 0–7 d, 2016–2018. The temperature–ED visit association was modeled with a quasi-Poisson distribution with a distributed-lag nonlinear model for each hospital, controlling for temporal trends, seasonality, humidity, and day of the week. RRs were then pooled across the 47 participating hospitals using random-effect meta-analyses. We calculated based on stratum-specific RRs and the pooled RR. We obtained the -value for the heterogeneity based on the statistic in a table. A Wald test with was considered as indicative of heterogeneity across strata. See Tables S3 and S4 for results for other specific causes. Note: CI, confidence interval; ED, emergency department; RR, relative risk; , mean daily maximum temperature; N.A., not available.
For specific causes of ED visitation, days of extreme heat were more strongly associated with ED visits in teenagers for otitis media and externa (1.24; 95% CI: 1.1, 1.39; 1.7; 95% CI:1.5, 1.93; 1.68; 95% CI: 1.39–2.04; ), whereas children 0–5 years of age were more likely to visit an ED for an infectious or parasitic disease (1.32; 95% CI: 1.21, 1.44; 1.11; 95% CI: 1.01, 1.22; 1.09; 95% CI: 0.89, 1.32; ) (Table S3). Minority racial-group children were more likely to visit EDs than White children for otitis media and externa; nervous system diseases; endocrine, neurological, and metabolic diseases; mental, behavioral, and neurodevelopmental disorders; injury and poisoning; and external causes and other health factors (Table S4). Children with public or other nonprivate insurance were more likely to visit EDs on days with extreme heat for bacterial enteritis and musculoskeletal system diseases (Table S5).
Discussion
Children are thought to be more vulnerable to heat exposure than adults (Stanberry et al. 2018; Vanos 2015; Xu et al. 2014a), but relatively few empirical studies have evaluated this hypothesis. To address this knowledge gap, we analyzed data from ED visits during the warm season to 47 children’s hospitals across 27 states in the United States. Our results suggest that higher maximum daily temperatures during the warm season may increase the risk of ED visits among children and adolescents. Specifically, we found that hotter days were associated with higher RRs of ED visits for all causes and for specific groups of causes, including heat-related illnesses, bacterial enteritis, otitis media and externa, infectious and parasitic diseases, and nervous system diseases, among others. These findings were robust to alternative modeling choices.
Our results are broadly consistent with the limited number of prior studies that suggest that heat is associated with higher risk of ED visits, hospitalizations, and ambulance dispatches among children (Corcuera Hotz and Hajat 2020; Sheffield et al. 2018; van Loenhout et al. 2018; Xu et al. 2014a). For example, a large study leveraging data on hospital admissions from across the Netherlands between 2002 and 2007 found that, among children of age, heat was associated with a higher risk of hospitalization for heat-related illnesses and respiratory diseases (van Loenhout et al. 2018). Sheffield et al. (2018) found that, among children 0–4 years of age living in New York City, summertime was associated with a higher risk of ED visits for heat-related illnesses, general symptoms, injuries, and viral and ear infections but not for digestive or respiratory diseases.
Most prior studies of children have been limited to a single or small number of locations and none have comprehensively evaluated a wide range of potential causes of morbidity. In the present study, heat was associated with higher risk of ED visits for any cause and for heat-related illness. Consistent with past studies, we found that heat was associated with ED visits for bacterial enteritis, and otitis media and externa (Sheffield et al. 2018; Xu et al. 2014b). We also identified ailments—such as nervous system diseases, skin and soft tissue diseases, and digestive system diseases—that have not previously been found to be associated with heat exposure in children. Additional large-scale studies are needed to confirm or refute these novel findings.
The unique physiology, behaviors, and social standing of children may heighten the risk for these outcomes. Bacterial enteritis, for example, can be a greater risk to children than adults, and especially to infants or children with chronic medical problems given their potentially limited ability to remain hydrated or their greater likelihood to develop complications when sick. Otitis media is a disease of childhood because the eustachian tubes are smaller in children than adults, the immune system may be less able to control the causative bacteria than adults, and the adenoid lymph nodes (which involute by adulthood) can serve as repositories for bacteria to ascend into the middle ear. Both bacterial enteritis and otitis media infections may be caused by Gram-negative organisms, which in some settings have been found to be more prevalent in summer months (Schwab et al. 2014).
Asthma is among the most common diagnoses for children presenting to the ED during the summer months, and heat may provoke lung irritation and worsen lung function (Bernstein and Rice 2013; Lepeule et al. 2018). Some (Corcuera Hotz and Hajat 2020; van Loenhout et al. 2018; Winquist et al. 2016; Xu et al. 2013, 2014b), but not all (Sheffield et al. 2018), prior studies have found an association between heat and asthma or other respiratory diseases. Our results suggest ED visits for asthma specifically, and respiratory diseases broadly, are not associated with higher temperatures during the warm season, even in sensitivity analyses with additional adjustment for ambient and (Figure S4).
In older adolescents and adults, temperature has previously been associated with greater mental health symptoms and risk of suicidality (Basu et al. 2018; Burke et al. 2018; Thompson et al. 2018). Although many studies have found heat to be associated with suicides in adolescents and young adults (Basu et al. 2018; Burke et al. 2018; Thompson et al. 2018), we did not identify a clear association between heat and ED visits for suicidality and depression, which is consistent with the findings of Wang et al. (2014). We also did not find a strong association with the larger category of “mental, behavioral, and neurodevelopmental disorders” (Figure 2).
In evaluating the relationship between heat and ED visits, we considered a suite of demographic variables. We found that visits to the ED for all-causes among minority racial-group children and children with public insurance showed a stronger association with heat compared with White children or those with private insurance, respectively. In stratified analyses, no clear pattern emerged for greater risk of ED visit with heat exposure based on race or insurance status. However, minority racial-group children had a much greater likelihood of ED visitation for some specific causes, including “bacterial enteritis,” “endocrine, nutritional, and metabolic diseases,” “mental, behavioral, and neurodevelopmental disorders,” and “injury and poisoning.” These findings are consistent with other data showing disparities in ED utilization in the United States with more visits from low-income children and children of color, particularly Black children. (McDermott et al. 2018; Schlichting et al. 2017).
Our results offer important insights for clinicians caring for children. First, children and adolescents may present on or after hot days with a variety of ailments that may not be intuitively linked to heat, including injuries, infections, and digestive diseases. Second, although heat was most strongly associated with ED visits on the same day, the elevated risk of ED visits was apparent even in the subsequent 2 or 3 d. Lagged effects of heat have been well documented in adults and previously noted in children as well (Sheffield et al. 2018; van Loenhout et al. 2018). Third, associations between high-temperature days and ED visitation were not confined to the hottest days but, rather, were evident across a range of warm season temperatures. The shape of the curve describing the association with heat varied by cause of ED visit. For example, we observed an approximately linear association for all-cause ED visits vs. an association that grew steeper at higher temperatures for heat-related illnesses and otitis media and externa. A vast literature in adults indicates a U- or V-shaped relationship between outdoor temperature and morbidity and mortality, whereby the risk of adverse health events increases monotonically (but not necessarily linearly) as daily temperatures deviate from the MMT (Song et al. 2017).
Our results suggest that a significant proportion of illness was attributable to days that are between the MMT and the 95th percentile of and not extremely hot. Pediatric care providers may not consider temperatures in this range as a risk to child health. Children with comorbid health conditions or genetic susceptibilities, or who are subject to adverse social determinants of health, may be at particular risk of heat exposure and the ensuing health effects (Liem 2018; Ziad et al. 2005).
The findings here are limited in several ways. First, the patient sample may not fully represent the underlying health status or demographics of the communities in which they live because PHIS hospitals primarily serve children, whereas most U.S. children receive emergency care at community hospitals that primarily treat adults (Gausche-Hill et al. 2007). Second, ED visits may be a more sensitive marker of heat-related illnesses than inpatient hospitalizations, but primary care visits may, in some instances, be a yet more sensitive end point. Third, patients in large counties may be exposed to different temperatures than are represented by the population-weighted county average and exposure misclassification may, therefore, have influenced our findings. Fourth, our findings may not be generalizable to countries with more universal or consistent access to health care because ED utilization in the United States is strongly related to health insurance (Schlichting et al. 2017), and our findings suggest that health insurance may modify the association between heat and ED visits. Fifth, rates of ED visitation for specific causes are seasonal (e.g., respiratory conditions are more prevalent from October to March) (McDermott et al. 2018). Our findings are limited to days of moderate and extreme heat from May to September and do not address risks outside these months. Finally, our results cannot address differential risks associated with race and ethnicity given the limitations in how race and ethnicity data were obtained.
On the other hand, to our knowledge this is the largest and most comprehensive analysis of the association between heat and ED visits in children in the United States, leveraging data from ED visits across 27 states. The geographic diversity and large size of our study sample is uncommon in studies of children’s environmental health. The large sample size led to estimates of associations that were relatively precise, even in analyses by cause of ED visits or within subgroups of the population, whereas the geographic extent of the study suggests that these results may be more broadly generalizable vs. prior studies that were limited to one or a few locations in the country.
The results of the analysis must be interpreted in the context of continued climate change. Greenhouse gas emissions have led to higher average temperatures globally and in the United States over the past century, accompanied by more frequent and intense days of extreme heat (Vose et al. 2017). The growing evidence that heat presents substantial risk to children underscores the need for more aggressive adaptation measures and suggests that continued climate change will have important implications for the health and well-being of children in the years ahead.
Supplementary Material
Acknowledgments
This research was made possible by provision of data from the Children’s Hospital Association (https://www.childrenshospitals.org/phis). Funding for this research was provided by grants R01-ES029950 (to S.S., K.R.W., K.R.S., G.A.W.), R01 ES030717 (P.E.S.), F32-ES027742 (to K.R.W.), and P30ES023515 (to P.E.S.) from the National Institutes of Health/National Institute of Environmental Health Sciences awards and by grant 216033-Z-19-Z from the Wellcome Trust (to S.S., K.R.S., G.A.W.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- American Academy of Pediatrics Council on Environmental Health. 2018. Children’s unique vulnerabilities to environmental hazards. In: Pediatric Environmental Health. 4th ed. Etzel RA, Balk SJ, eds. Itasca, IL: American Academy of Pediatrics, 17–31. [Google Scholar]
- Anderson GB, Bell ML, Peng RD. 2013. Methods to calculate the heat index as an exposure metric in environmental health research. Environ Health Perspect 121(10):1111–1119, PMID: , 10.1289/ehp.1206273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. 2017. Structural racism and health inequities in the USA: evidence and interventions. Lancet 389(10077):1453–1463, PMID: , 10.1016/S0140-6736(17)30569-X. [DOI] [PubMed] [Google Scholar]
- Basu R, Gavin L, Pearson D, Ebisu K, Malig B. 2018. Examining the association between apparent temperature and mental health-related emergency room visits in California. Am J Epidemiol 187(4):726–735, PMID: , 10.1093/aje/kwx295. [DOI] [PubMed] [Google Scholar]
- Basu R, Ostro BD. 2008. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am J Epidemiol 168(6):632–637, PMID: , 10.1093/aje/kwn170. [DOI] [PubMed] [Google Scholar]
- Bernstein AS, Rice MB. 2013. Lungs in a warming world: climate change and respiratory health. Chest 143(5):1455–1459, PMID: , 10.1378/chest.12-2384. [DOI] [PubMed] [Google Scholar]
- Bobb JF, Obermeyer Z, Wang Y, Dominici F. 2014. Cause-specific risk of hospital admission related to extreme heat in older adults. JAMA 312(24):2659–2667, PMID: , 10.1001/jama.2014.15715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley JP, Samet JM, Richardson DB. 2014. Commentary: does air pollution confound studies of temperature? Epidemiology 25(2):242–245, PMID: , 10.1097/EDE.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Burke M, González F, Baylis P, Heft-Neal S, Baysan C, Basu S, et al. 2018. Higher temperatures increase suicide rates in the United States and Mexico. Nat Clim Chang 8(8):723–729, 10.1038/s41558-018-0222-x. [DOI] [Google Scholar]
- Chen T, Sarnat SE, Grundstein AJ, Winquist A, Chang HH. 2017. Time-series analysis of heat waves and emergency department visits in Atlanta, 1993 to 2012. Environ Health Perspect 125(5):057009, PMID: , 10.1289/EHP44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corcuera Hotz I, Hajat S. 2020. The effects of temperature on accident and emergency department attendances in London: a time-series regression analysis. Int J Environ Res Public Health 17(6):1957, PMID: , 10.3390/ijerph17061957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly C, Halbleib M, Smith JI, Gibson WP, Doggett MK, Taylor GH, et al. 2008. Physiographically sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol 28(15):2031–2064, 10.1002/joc.1688. [DOI] [Google Scholar]
- Dunn OJ. 1961. Multiple comparisons among means. J Am Stat Assoc 56(293):52–64, 10.1080/01621459.1961.10482090. [DOI] [Google Scholar]
- Falk B, Dotan R. 2008. Children’s thermoregulation during exercise in the heat—a revisit. Appl Physiol Nutr Metab 33(2):420–427, PMID: , 10.1139/H07-185. [DOI] [PubMed] [Google Scholar]
- Gasparrini A. 2011. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 43(8):1–20, PMID: , 10.18637/jss.v043.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2012. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med 31(29):3821–3839, PMID: , 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Kinney PL, Petkova EP, Lavigne E, et al. 2015. Temporal variation in heat–mortality associations: a multicountry study. Environ Health Perspect 123(11):1200–1207, PMID: , 10.1289/ehp.1409070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Tobias A, Zanobetti A, et al. 2016. Changes in susceptibility to heat during the summer: a multicountry analysis. Am J Epidemiol 183(11):1027–1036, PMID: , 10.1093/aje/kwv260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Leone M. 2014. Attributable risk from distributed lag models. BMC Med Res Methodol 14:55, PMID: , 10.1186/1471-2288-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gausche-Hill M, Schmitz C, Lewis RJ. 2007. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics 120(6):1229–1237, PMID: , 10.1542/peds.2006-3780. [DOI] [PubMed] [Google Scholar]
- Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. 2014. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ Health Perspect 122(11):1187–1192, PMID: , 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Gasparrini A, Armstrong BG, Tawatsupa B, Tobias A, Lavigne E, et al. 2017. Heat wave and mortality: a multicountry, multicommunity study. Environ Health Perspect 125(8):087006, PMID: , 10.1289/EHP1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess JJ, Saha S, Luber G. 2014. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environ Health Perspect 122(11):1209–1215, PMID: , 10.1289/ehp.1306796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm S. 1979. A simple sequentially rejective multiple test procedure. Scand J Stat 6(2):65–70, 10.2307/4615733. [DOI] [Google Scholar]
- Iñiguez C, Schifano P, Asta F, Michelozzi P, Vicedo-Cabrera A, Ballester F. 2016. Temperature in summer and children’s hospitalizations in two Mediterranean cities. Environ Res 150:236–244, PMID: , 10.1016/j.envres.2016.06.007. [DOI] [PubMed] [Google Scholar]
- Kim Y, Kim H, Gasparrini A, Armstrong B, Honda Y, Chung Y, et al. 2019. Suicide and ambient temperature: a multi-country multi-city study. Environ Health Perspect 127(11):117007, PMID: , 10.1289/EHP4898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. 2009. The 2006 California heat wave: impacts on hospitalizations and emergency department visits. Environ Health Perspect 117(1):61–67, PMID: , 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavados PM, Olavarría VV, Hoffmeister L. 2018. Ambient temperature and stroke risk: evidence supporting a short-term effect at a population level from acute environmental exposures. Stroke 49(1):255–261, PMID: , 10.1161/STROKEAHA.117.017838. [DOI] [PubMed] [Google Scholar]
- Lepeule J, Litonjua AA, Gasparrini A, Koutrakis P, Sparrow D, Vokonas PS, et al. 2018. Lung function association with outdoor temperature and relative humidity and its interaction with air pollution in the elderly. Environ Res 165:110–117, PMID: , 10.1016/j.envres.2018.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liem RI. 2018. Balancing exercise risk and benefits: lessons learned from sickle cell trait and sickle cell anemia. Hematology Am Soc Hematol Educ Program 2018(1):418–425, PMID: , 10.1182/asheducation-2018.1.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madrigano J, Mittleman MA, Baccarelli A, Goldberg R, Melly S, von Klot S, et al. 2013. Temperature, myocardial infarction, and mortality: effect modification by individual- and area-level characteristics.. Epidemiology 24(3):439–446, PMID: , 10.1097/EDE.0b013e3182878397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott KW, Stocks C, Freeman WJ. 2018. Overview of Pediatric Emergency Department Visits, 2015. HCUP Statistical Brief #242 August 2018. Rockville, MD: Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/reports/statbriefs/sb242-Pediatric-ED-Visits-2015.pdf [accessed 27 November 2021]. [PubMed] [Google Scholar]
- Morrison AK, Schapira MM, Gorelick MH, Hoffmann RG, Brousseau DC. 2014. Low caregiver health literacy is associated with higher pediatric emergency department use and nonurgent visits. Acad Pediatr 14(3):309–314, PMID: , 10.1016/j.acap.2014.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2019. Table 36. In: International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Pun VC, Tian L, Yu ITS, Kioumourtzoglou MA, Qiu H. 2015. Differential distributed lag patterns of source-specific particulate matter on respiratory emergency hospitalizations. Environ Sci Technol 49(6):3830–3838, PMID: , 10.1021/es505030u. [DOI] [PubMed] [Google Scholar]
- Reid CE, Snowden JM, Kontgis C, Tager IB. 2012. The role of ambient ozone in epidemiologic studies of heat-related mortality. Environ Health Perspect 120(12):1627–1630, PMID: , 10.1289/ehp.1205251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarofim MC, Saha S, Hawkins MD, Mills DM, Hess J, Horton R, et al. 2016. Ch. 2: Temperature-related death and illness. In: The Impacts of Climate Change on Human Health in the United States: a Scientific Assessment. Washington, DC: U.S. Global Change Research Program, 43–68. https://health2016.globalchange.gov/ [accessed 27 November 2021]. [Google Scholar]
- Schlichting LE, Rogers ML, Gjelsvik A, Linakis JG, Vivier PM. 2017. Pediatric emergency department utilization and reliance by insurance coverage in the United States. Acad Emerg Med 24(12):1483–1490, PMID: , 10.1111/acem.13281. [DOI] [PubMed] [Google Scholar]
- Schwab F, Gastmeier P, Meyer E. 2014. The warmer the weather, the more gram-negative bacteria—impact of temperature on clinical isolates in intensive care units. PLoS One 9(3):e91105, PMID: , 10.1371/journal.pone.0091105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffield PE, Herrera MT, Kinnee EJ, Clougherty JE. 2018. Not so little differences: variation in hot weather risk to young children in New York City. Public Health 161:119–126, PMID: , 10.1016/j.puhe.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Son JY, Liu JC, Bell ML. 2019. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ Res Lett 14(7):073004, 10.1088/1748-9326/ab1cdb. [DOI] [Google Scholar]
- Song X, Wang S, Hu Y, Yue M, Zhang T, Liu Y, et al. 2017. Impact of ambient temperature on morbidity and mortality: an overview of reviews. Sci Total Environ 586:241–254, PMID: , 10.1016/j.scitotenv.2017.01.212. [DOI] [PubMed] [Google Scholar]
- Spangler KR, Weinberger KR, Wellenius GA. 2019. Suitability of gridded climate datasets for use in environmental epidemiology. J Expo Sci Environ Epidemiol 29(6):777–789, PMID: , 10.1038/s41370-018-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanberry LR, Thomson MC, James W. 2018. Prioritizing the needs of children in a changing climate. PLoS Med 15(7):e1002627, PMID: , 10.1371/journal.pmed.1002627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Cao W, Pun VC, Qiu H, Ge Y, Tian L. 2019a. Respirable particulate constituents and risk of cause-specific mortality in the Hong Kong population. Environ Sci Technol 53(16):9810–9817, PMID: , 10.1021/acs.est.9b01635. [DOI] [PubMed] [Google Scholar]
- Sun S, Weinberger KR, Spangler KR, Eliot MN, Braun JM, Wellenius GA. 2019b. Ambient temperature and preterm birth: a retrospective study of 32 million US singleton births. Environ Int 126:7–13, PMID: , 10.1016/j.envint.2019.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson R, Hornigold R, Page L, Waite T. 2018. Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health 161:171–191, PMID: , 10.1016/j.puhe.2018.06.008. [DOI] [PubMed] [Google Scholar]
- U.S. EPA (U.S. Environmental Protection Agency). 2020. Air data: air quality data collected at outdoor monitors across the US. Washington, DC: U.S. EPA, Office of Air and Radiation. https://www.epa.gov/outdoor-air-quality-data [accessed 24 November 2020]. [Google Scholar]
- van Loenhout JAF, Delbiso TD, Kiriliouk A, Rodriguez-Llanes JM, Segers J, Guha-Sapir D. 2018. Heat and emergency room admissions in the Netherlands. BMC Public Health 18(1):108, PMID: , 10.1186/s12889-017-5021-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanos JK. 2015. Children’s health and vulnerability in outdoor microclimates: a comprehensive review. Environ Int 76:1–15, PMID: , 10.1016/j.envint.2014.11.016. [DOI] [PubMed] [Google Scholar]
- Vose RS, Easterling DR, Kunkel KE, LeGrande AN, Wehner MF. 2017. Ch. 6: Temperature changes in the United States. In: Climate Science Special Report: Fourth National Climate Assessment (NCA4), Volume I. Wuebbles DJ, Fahey DW, Hibbard KA, Dokken DJ, Stewart BC, Maycock TK, eds. Washington, DC: US. Global Change Research Program. 10.7930/J0N29V45. [DOI] [Google Scholar]
- Wang X, Lavigne E, Ouellette-Kuntz H, Chen BE. 2014. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J Affect Disord 155:154–161, PMID: , 10.1016/j.jad.2013.10.042. [DOI] [PubMed] [Google Scholar]
- Weinberger KR, Harris D, Spangler KR, Zanobetti A, Wellenius GA. 2020. Estimating the number of excess deaths attributable to heat in 297 United States counties. Environ Epidemiol 4(3):e096, PMID: , 10.1097/EE9.0000000000000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winquist A, Grundstein A, Chang HH, Hess J, Sarnat SE. 2016. Warm season temperatures and emergency department visits in Atlanta, Georgia. Environ Res 147:314–323, PMID: , 10.1016/j.envres.2016.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z, Hu W, Su H, Turner LR, Ye X, Wang J, et al. 2014a. Extreme temperatures and paediatric emergency department admissions. J Epidemiol Community Health 68(4):304–311, PMID: , 10.1136/jech-2013-202725. [DOI] [PubMed] [Google Scholar]
- Xu Z, Liu Y, Ma Z, Toloo GS, Hu W, Tong S. 2014b. Assessment of the temperature effect on childhood diarrhea using satellite imagery. Sci Rep 4:5389, PMID: , 10.1038/srep05389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z, Huang C, Hu W, Turner LR, Su H, Tong S. 2013. Extreme temperatures and emergency department admissions for childhood asthma in Brisbane, Australia. Occup Environ Med 70(10):730–735, PMID: , 10.1136/oemed-2013-101538. [DOI] [PubMed] [Google Scholar]
- Ziad EK, Rahi AC, Hamdan SA, Mikati MA. 2005. Age, dose, and environmental temperature are risk factors for topiramate-related hyperthermia. Neurology 65(7):1139–1140, PMID: , 10.1212/01.wnl.0000179004.97114.97. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.