Abstract
Background
The COVID-19 pandemic has generated a significant amount of psychological burden in the form of stress, anxiety, uncertainty, depression, anger, and helplessness. The caregivers of children with chronic diseases in particular are at a higher risk of mental stress and burden.
Material and Methods
We conducted an online survey among caregivers of children with kidney diseases to assess the psychosocial impact of COVID-19. The psychosocial impact of COVID-19 pandemic on their mental health was assessed through standardized psychological scales (Peritraumatic Distress Inventory, Insomnia Severity Scale [ISI], Depression Anxiety and Stress Scale [DASS], and Positive and Negative Aspect Scale) and a semi-structured interview was conducted telephonically.
Results
A total of 200 caregivers participated in the study. The mean age of the participants was 36±5.56 years, and 76% were males. Participants experienced maximum distress in terms of life threat (6.27±4.64), followed by helplessness and anger (2.66 ± 1.65). Among participants, 38% of them exhibited significant distress. The majority scored below the cut-off on positive affect (98%), and thus could not experience positive emotions and interaction, and 37.5% of participants were feeling significant negative affect. On the ISI, 38.5% of participants experienced significant sleep problems. On the DASS, 65% of participants exhibited significant stress, 76% anxiety, and 78.5% depression.
Conclusion
A high prevalence of stress, anxiety, and depression along with insomnia was detected among the caregivers of children with kidney diseases during the COVID-19 pandemic.
Keywords: Anxiety, Caregivers, Children, Depression, Stress
Abbreviations: AKI, Acute Kidney Injury; CKD, Chronic Kidney Disease; DASS II, Depression Anxiety Stress Scale; ISI, Insomnia Severity Index; NS, Nephrotic Syndrome; PANAS-SF, Positive and Negative Affect Schedule; PDI, Peritraumatic Distress Inventory
1. Introduction
The COVID-19 pandemic has affected the treatment/care of children with various comorbidities, either because of the lockdown or for fear of acquiring the infection by attending hospital. Children with a chronic disease such as chronic kidney disease (CKD), nephrotic syndrome (NS), and other kidney diseases need to visit healthcare facilities frequently. During the COVID-19 pandemic, health-related emergencies in the management of children with kidney diseases, pandemic- and lockdown-related distress among caregivers, along with disease-associated stress contributed to a very challenging situation. Since medical advances have led to increased life expectancy in children with chronic diseases, the psychological complications and burden of their diseases become increasingly important [1].
The World Federation of Mental Health stresses the need for psychological support to caregivers of patients with chronic diseases. According to them, these individuals are less healthy, have more chronic illnesses, poorer immune function, and prone to exhaustion. They may neglect their own care and have higher mortality rates than non-caregivers of the same age. Further, they suffer from more stress, depression, and anxiety. Since 1980, there has been growing recognition of the unique challenges to families and caregivers who look after a child with kidney disease [2], [3], [4], [5]. These children are highly susceptible to COVID-19 infection due to the chronic disease-related issues and poor immunity [6,7].
Caregiving plays an important role in the well-being of children with chronic diseases such as CKD, and this is enhanced if the caregivers are healthy and caring [8,9]. Distress associated with the role of caregivers arises because of emotional and physical responses to meet the demands of new challenges during the care of their sick child. Caregiving is a multifaceted concept that compasses the psychological, emotional, social, and financial concept of delivering caregiving duties. In view of the increasing mental burden due to the pandemic on caregivers, we performed a cross-sectional observational study to assess the psychosocial impact of COVID-19 on caregivers of children with kidney diseases through an online survey.
2. Materials and methods
A cross-sectional observational study was conducted through an online survey among caregivers of children with kidney diseases to assess the psychosocial impact of COVID-19 on them from June 2020 to October 2020 by using the snowball purposive sampling method. The study was approved by Institute Ethical Committee (vide no. INT/IEC/2020/SPL-726, dated 23.06.2020).
Participants were parents/caregivers of children undergoing treatment at the Pediatric Nephrology Unit of the Department of Pediatrics. We contacted 250 parents of children with acute kidney injury (AKI), nephrotic syndrome, and CKD being treated through outpatient status/teleconsultation during the study period; 50 could not be contacted due to unavailability of network/social media facility, not giving consent, or change of phone number. Thus, a total of 200 caregivers were recruited for the present study. An online survey was carried out and the survey questionnaire was designed in Google Forms, the link to which was circulated through emails and WhatsApp to all the participants and through semi-structured telephone interview. The nature and purpose of the study were explained to the caregivers, and subsequently electronic or verbal consent was obtained. Telephone and text reminders were sent to the non-respondent participants to make sure that no item was left unanswered in each item of the survey questionnaire that was completed before and successfully submitted in the Google Forms.
After obtaining their consent, caregivers were invited to participate in this online survey by answering multiple-choice questions in Google Forms in three stages. In the first stage, participants were asked to provide demographic and disease-related information (age, gender, education, occupation, income, type and duration of disease). In the second stage, the psychosocial impact of the COVID-19 pandemic on their mental health was assessed through standardized psychological scales (Peritraumatic Distress Inventory, Insomnia Severity Scale, Depression Anxiety and Stress Scale, and Positive and Negative Aspect Scale). In the third part, a semi-structured interview was conducted telephonically by an expert psychologist to assess the pandemic-, lockdown-, family-, and disease-related stress among participants. The following questions were asked:
-
-
COVID-19 related stress: To what extent is washing hands important to avoid getting infected with COVID-19? To what extent were you maintaining social distancing?
-
-
Lockdown-related stress: To what extent were you worried about the availability of daily essentials during a lockdown? To what extent had lockdown affected your life/routine activities?
-
-
Emotional- and family-related stress: To what extent do you feel like not talking to anyone? To what extent you were worried about family members getting infected from community spread?
-
-
Disease-related stress: To what extent were you worried about the effects of COVID-19 on your child's disease? To what extent were you satisfied with the help/ medical advice given to you by the doctors during the epidemic?
In the absence of any validated questionnaire, to assess the stress among caregivers of patients with kidney disease during the pandemic, we specially designed a questionnaire after reviewing the available literature during and before the COVID-19 pandemic [10], [11], [12], [13], [14]. The questionnaire included 17 questions in the English language, assessing the COVID-19-related stress, lockdown-related stress, emotional- and family-related stress, and disease-related stress among caregivers of children with kidney diseases during the COVID-19 pandemic. Piloting work was done, and the scale was administered on 10 caregivers of children with kidney diseases admitted in the ward; these caregivers were excluded from the final study. The face validity of this questionnaire was assessed by two pediatric nephrologists, two psychologists, and one postdoctoral pediatric nephrology fellow.
2.1. Psychological measures/tools
Peritraumatic distress inventory (PDI)
This scale developed by Brunet et al. [15] is a 13-item self-reported inventory. It measures distress exhibited by a person during and after a traumatic event. It measures painful experiences in four domains; life threat, loss of control, helplessness and anger, and guilt and shame on a five-point Likert scale (0 = not at all true; 1 = slightly true; 2 = somewhat true; 3 = very true; and 4 = extremely true). The total PDI score range is 0–52 and the cut-off score is 15. It also has good internal consistency (Cronbach's α = 0.83) and good test–retest reliability (0.74) in various measures of peritraumatic distress.
2.2. Insomnia severity index (ISI) [16]
This scale measures the severity of insomnia through seven self-report items on a five-point Likert scale (0 = no problem at all to 4= very severe problem). The respondents have to recall the last month's experiences with their sleep pattern. The total score range for the ISI is 0–28 and the cut-off score is 7. Further, the severity of insomnia is classified: Scores of 0–7 indicate no clinical insomnia, 8–14 sub-threshold insomnia, 15–21 moderate insomnia, and 22–28 severe insomnia. The scale has good psychometric properties [16].
2.3. Depression anxiety stress scale (DASS II)
The DASS was developed by Lovibond and Lovibond in 1995 [17]. This is a self-report scale and has three sub-scales: depression, anxiety, and stress. Each sub-scale has seven items, and each item is rated on a four-point scale (0 = not at all; 1 = some degree; 2 = considerable degree; and 4 = very much). Cut-off scores for three sub-scales are also given, from normal to extremely severe stress, anxiety, and depression. This scale has good psychometric properties, good reliability (0.94; Cronbach's α = 0.86–0.90), and good convergent validity (0.84 depression, 0.75 anxiety, and 0.90 stress).
2.4. Positive and negative affect schedule (PANAS-SF)
This is a 20-item self-report scale developed by Watson et al. [18] It measures two different dimensions of mood: positive and negative affect. Items are rated on a five-point Likert scale (1 = very slightly or not at all to 5 = extremely). Positive affect measures an individual's enthusiasm, activeness, and alertness and negative affect measures subjective distress and aversive feelings. The internal consistency of the PANAS-SF is 0.87 and it has good discriminative and predictive validity.
2.5. COVID stress survey questionnaire [10], [11], [12], [13], [14]
This questionnaire comprises 17 questions with different psychological components: increased susceptibility of children having coronavirus infection, managing daily essentials in hospital, maintaining social distancing and washing hands, worrying about family members and children staying at home, indifferent attitude of others, and lockdown-related stress. Items were divided into three domains: COVID-19-related stress; lockdown-related stress; and emotional- and family-related stress. The psychometric properties of these questions (content and face validity) were assessed and verified by two pediatric nephrologists, two senior fellows in the pediatric nephrology unit, and one clinical and child psychologist. The parents’ subjective experiences were recorded on a 5-point Likert scale, i.e., not at all; a little bit; sometimes; most of the time; and always (Table 1 ).
Table 1.
Frequency distribution survey questionnaire items.
| Not at all | Mild | Moderate | Severe | Extremely Severe | |
|---|---|---|---|---|---|
| COVID-related stress | |||||
| To what extent do you think everything (COVID-19 pandemic) will be fine soon? | 6% | 17% | 26.5% | 19% | 31.5% |
| To what extent do you have a feeling of being avoided by others? | 29.5% | 24% | 24% | 16.5% | 6% |
| To what extent were you maintaining social distancing? | 13% | 13.5% | 11.5% | 38% | 24% |
| To what extent is washing hands important to avoid getting infected with COVID-19? | 5.5% | 9.5% | 12% | 27.5% | 45.5% |
| To what extent are you satisfied that our government is taking protective measures? | 25.5% | 9% | 27.5% | 28.5% | 9.5% |
| Disease-related stress | |||||
| To what extent were you worried that your child may get infected with COVID-19? | 4% | 10% | 22.5% | 38% | 25.5% |
| To what extent did you face problems in getting appointments for medical advice? | 59.5% | 14.5% | 11% | 14% | 1% |
| To what extent was it difficult for you to get regular tests done and procure medication during the lockdown in the COVID-19 pandemic? | 45% | 28% | 13.5% | 9.5% | 4% |
| To what extent were you satisfied with the help/ medical advice/assistance given to you by the treating doctors during the pandemic? | 10.5% | 15% | 17% | 19.5% | 38% |
| Lockdown-related stress | |||||
| To what extents were you worried about relapse/aggravation of your child's disease during COVID-19 lockdown? | 18.5% | 21.5% | 30% | 28.5% | 1.5% |
| To what extent were you worried about availability of daily essentials during lockdown? | 43% | 20% | 22.5% | 6.5% | 8% |
| To what extent did lockdown affect your life/routine activities? | 10.5% | 11% | 17.5% | 30% | 31% |
| Did you face any difficulty in getting medical help for your child during the lockdown? | 33.5% | 23% | 14.5% | 13.5% | 15.5% |
| Emotional- and family-related stress | |||||
| To what extent do you feel like not talking to anyone/low mood? | 26.5% | 24.5% | 37% | 9% | 3% |
| To what extent have you experienced stress/worry? | 27.5% | 11.5% | 17% | 24.5% | 19.5% |
| To what extent you were worried about family members getting infected from community spread? | 27% | 12% | 22.5% | 21% | 17.5% |
| To what extent you were worried that any of your family members could die due to COVID-19? | 39.5% | 15% | 18.5% | 16% | 11% |
2.6. Statistical analysis
The complete recorded data were transferred to an Excel database and analyzed by using the software SPSS Statistics 23 (IBM SPSS Statistics, New York, USA). Descriptive statistics were used to compute frequency percentages, mean, and standard deviation for different variables. Bivariate correlation was also computed and used for analyses of the association between clinical and sociodemographic variables. Regression analysis was used to estimate the effect of some explanatory variables on the dependent variable.
3. Results
3.1. Participant demographics
Of the 250 participants invited to the study, 200 participants were included in the final sample. The non-respondent participants (50) were those who could not be contacted due to unavailability of network/social media facility, not giving consent, or change of phone number. The mean age of the participants was 36 ± 5.56 years; 76% were males and 24% were females. In terms of education, 92 (46%) had attained education up to intermediate level, 51 (25.5%) were educated up to high school level, and 49 (24.5%) up to graduation. More than half of the participants (n = 107; 53.5%) were engaged in clerical/ministerial jobs, 67 (33.5%) were skilled (craft-, agriculture-related work) workers, and 10 (5%) were in senior administrative roles or professionals. Of the participants, 132 (66%) were living in joint families and 68 (34%) in nuclear families, 94 (47%) were living in urban and 166 (53%) in semi-urban/rural localities. Approximately 95 (47.5%) belonged to lower-middle and 61 (30.5%) to upper-middle socioeconomic status. The demographic description of the participants is summarized in Table 2 .
Table 2.
Demographic and clinical details of parents of hospitalized patients with acute kidney injury, nephrotic syndrome, and chronic kidney disease (N = 200).
| Mean ± SD | Frequency (%) | |
|---|---|---|
| Age (years) | 36.00±5.56 | |
| Diagnosis | Acute kidney injury Nephrotic syndrome Chronic kidney disease |
8 (4%) 159 (79.5%) 33 (16.5%) |
| Gender | Male Female |
152 (76%) 48 (24%) |
| Education of parents | Illiterate Middle Intermediate Graduation/post-graduation |
8 (4%) 51 (25.5%) 92 (46%) 49 (24.5%) |
| Occupation of parents | Professional/senior officials Clerical/ministerial jobs Skilled Unemployed |
10 (5%) 107 (53.5%) 67 (33.5%) 16 (8%) |
| Income (in rupees) | Less than 11,707 11,708–19,515 19,516–39,032 39,033–78,062 More than 78,063 |
51 (25.5%) 71 (35.5) 44 (22%) 12 (6%) 22 (11%) |
| Socioeconomic status | Upper lower Lower middle Upper middle Upper |
36 (18%) 95 (47.5%) 61 (30.5%) 8 (4%) |
| Family type | Nuclear Joint |
68 (34%) 132 (66%) |
| Locality | Urban Rural/semi-urban |
94 (47%) 106 (53%) |
SD: standard deviation.
3.2. Clinical profile of participants
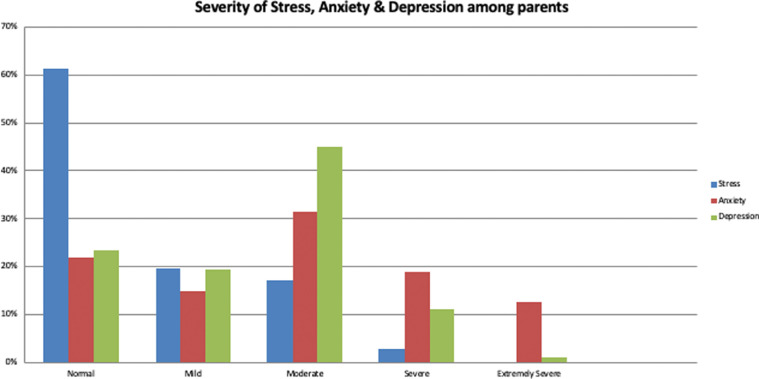
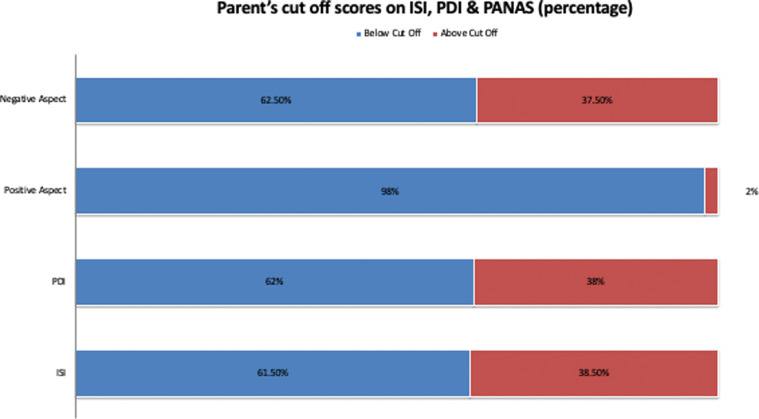
The clinical profile of the participants is given in Table 3 . Participants experienced maximum distress in terms of life threat (6.27 ± 4.64), followed by helplessness and anger (2.66 ± 1.65), with the mean score of distress being 13.95 ± 8.24. Among participants, 38% exhibited significant distress. Since facing a tough time during the pandemic, the majority of them scored below the cut-off on positive affect (98%), and thus could not experience positive emotions and interaction, and 37.5% of participants were feeling significant negative affect (Fig. 1 ). The parents’ scores on clinical measures were above the cut-off for the PDI, ISI, and PANAS, as depicted in Fig. 2 . On the ISI, 38.5% of participants experienced significant sleep problems during the pandemic, 41.5% experienced significant severity of sleep-onset problems, and 49% reported dissatisfaction with their current sleep pattern. One fourth of participants (25%) reported sub-threshold, 13% moderate, and 0.5% severe insomnia.
Table 3.
Scores of parents of children with kidney diseases on clinical measures.
| Minimum | Maximum | Mean | SD | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|
| Peritraumatic Distress Inventory | ||||||
| Life threat | 0.00 | 16.00 | 6.27 | 4.64 | 0.551 | −0.955 |
| Loss of control | 0.00 | 9.00 | 2.51 | 1.78 | 0.998 | 0.953 |
| Helplessness/anger | 0.00 | 6.00 | 2.66 | 1.65 | 0.313 | 0.588 |
| Guilt/shame | 0.00 | 8.00 | 2.48 | 2.19 | 0.449 | −1.117 |
| Total PDI scores | 2.00 | 34.00 | 13.95 | 8.24 | 0.546 | −0.902 |
| Positive and Negative Symptoms | ||||||
| Positive aspect | 5.00 | 35.00 | 19.90 | 7.44 | 0.035 | −0.835 |
| Negative aspect | 0.00 | 35.00 | 14.87 | 7.50 | 0.048 | −0.421 |
| Insomnia Severity Index | ||||||
| Severity of sleep onset | 0.00 | 11.00 | 2.68 | 3.07 | 0.845 | −0.593 |
| Degree of satisfaction/dissatisfaction with current sleep pattern SaSatisfaction/Dissatisfaction with Current Sleep Pattern |
0.00 | 12.00 |
3.86 | 3.25 | 0.646 | −0.536 |
| Insomnia severity scores | 0.00 | 22.00 | 6.54 | 5.78 | 0.584 | −0.905 |
| Depression Anxiety Stress Scale | ||||||
| Stress | 0.00 | 16.00 | 6.86 | 3.00 | 0.165 | −0.302 |
| Anxiety | 0.00 | 16.00 | 5.97 | 3.11 | 0.507 | 0.031 |
| Depression | 0.000 | 16.00 | 6.98 | 3.09 | 0.038 | −0.520 |
SD: standard deviation.
Fig. 1.
Description of psychopathology among parents of children with kidney diseases.
Fig. 2.
Parent scores above cut-off on peritraumatic stress inventory (PDI), insomnia severity index (ISI), and positive and negative aspect scale (PANAS).
On the DASS, 65% of participants exhibited significant stress, 76% anxiety, and 78.5% had depression. The severity of stress, anxiety, and depression was also assessed, and mild stress was exhibited by 19.5%, moderate by 17%, and severe stress by 2.5% of participants. Approximately 15% of participants reported mild anxiety, 31.5% moderate anxiety, 19% severe, and 12.5% extremely severe anxiety. On the depression sub-scale, 19.5% of the study population had mild depression, 45% moderate depression, 11% severe depression, and 1% had extremely severe depression.
3.3. Stress among caregivers due to COVID-19
The majority of caregivers (94%) were hopeful that the pandemic would be over very soon; approximately 70.5% had experienced being avoided by others during the pandemic, 94.5% were of the view that washing hands and maintaining social distance (87%) was important to avoid getting COVID-19 and 74.5% were satisfied with the precautionary steps taken by the government. The majority of them (96%) were worried that their child may get infected, 40.5% found it difficult to get medical consultations during lockdown, more than half of them (55%) faced difficulties in getting tests done and procuring medication, and 89.5% of caregivers were satisfied with the help/medical advice or assistance given to them by the treating doctors.
Almost 90% of caregivers reported that the lockdown had affected their daily routine and activities, 81.5% of caregivers were worried their sick child may relapse or experience aggravation of their disease during the COVID-19 lockdown, 57% were stressed about getting daily essentials during the lockdown, and 66.5% faced difficulty in getting medical help for their child during the lockdown. The pandemic affected 73.5% of caregivers in terms of them not feeling like talking to anyone, 72.5% experiencing symptoms of stress, 72% worrying that family members may get infected from community spread, and 40.5% being stressed that family members could die because of COVID-19.
3.4. Association between demographic and clinical variables
Parental age was found to be positively associated with stress; caregivers aged ≥40 years were significantly more stressed than caregivers ≤40 years (p = 0.026). Gender-related significant differences were assessed using the t-test. Mothers exhibited significantly more stress than fathers (−3.370; p = 0.001), were more depressed (−2.267; p = 0.024), found the situation more life-threatening (−3.821; p = 0.000), and lost control of their emotions more frequently (−2.962; p = 0.003) than their counterparts. Fathers experienced significant insomnia-related problem (−2.495; p = 0.013), anxiety (−3.800; p = 0.000), helplessness and anger (−3.284; p = 0.001), and guilt and shame (−2.466; p = 0.015) than mothers. Another significant finding of the study was that caregivers living in joint families lost control of their emotions more frequently than caregivers living in nuclear families (−2.555; p = 0.011), while those living in urban areas felt more helpless and more aggressive than caregivers living in rural areas (−2.595; p = 0.010).
Differences in education and occupation were assessed using ANOVA. Caregivers who had attained higher secondary education experienced more sleep-related problems than caregivers with high-school level education (F = 4.302; p = 0.006). Caregivers from upper SES were more helpless and were more aggressive (F = 4.461; p = 0.005), and experienced significantly more overall distress (F = 4.959; p = 0.002) than caregivers of other SES.
Professionals/senior officials reported significant sleep problems (F = 3.282, p = 0.022), were more anxious (F = 6.775, p = 0.000), lost control of their emotions (F = 4.903, p = 0.003), and also felt more guilty about their actions (F = 7.849, p = 0.000) than other occupation groups. Unemployed caregivers were significantly more stressed than their counterparts (F = 3.282, p = 0.022), experienced this situation as life-threatening (F = 7.484, p = 0.000), were also feeling helpless (F = 7.097, p = 0.000), and scored low on the positive aspect scale.
Insomnia was found to be positively correlated with stress (r = 0.450, p = 0.000), anxiety (r = 0.450, p = 0.000), depression (r = 0.411, p = 0.000), and distress (r = 0.519, p = 0.000). Distress was positively correlated with stress (r = 0.440, p = 0.000), anxiety (r = 0.443, p = 0.000), and depression (r = 0.393, p = 0.000). Positive aspect was negatively correlated with distress (r=−0.268, p = 0.000), insomnia (r=−0.209, p = 0.003), stress (r=−0.178, p = 0.012), anxiety (r=−0.158, p = 0.025), and negative aspect (r=−0.272, p = 0.000). Caregivers who experienced more sleep-related problems were more distressed and also scored high on anxiety and depression.
4. Discussion
The study shows that caregivers of children with kidney diseases have a high prevalence of stress during COVID-19 pandemic lockdowns. A significant difference was observed among parents on how they felt during the pandemic. Mothers exhibited significantly more stress, and were more depressed, found it more life-threatening, and lost control of their emotions more frequently than their counterparts. Fathers experienced significantly more insomnia-related problems, anxiety, helplessness, anger, guilt, and shame than mothers did. There was also a significant association between demographic variables and various clinical variables, which we feel are of clinical significance, suggesting a high psychological burden on caregivers of children with kidney diseases during this COVID-19 pandemic.
The study observed a high prevalence of depression (78.5%), anxiety (76%), and significant stress (65%) among caregivers. The findings are similar to those from the study by Yuan et al. [14], where the mental health problems of parents during the COVID-19 pandemic were more serious, with more obvious anxiety and depression. A study from Jordan found that mothers with lower income and lower education and who were unemployed or living outside the capital of Jordan reported more depression, anxiety, and stress symptoms [19]. They demonstrated that loss of a paid job due to quarantine increased the economic burden on the family and there was an increase in familial violence at home, which might have aggravated the mental health symptoms. In our study, we also found that unemployed parents were significantly more stressed than their counterparts, which could be attributed to the financial burden. The adverse psychosocial effects on the primary caregivers of children with chronic illness are significant, with an obvious high prevalence of probable depression and low quality of life [4].
Another important finding in our study was the significant sleep problems experienced in caregivers during the pandemic (38.5%), which was similar to the study by Kim et al. [13], who studied the behavioral and psychological responses and stressors among caregivers duringCOVID-19 quarantine and found that sleep disturbance was seen in 30.6%. This can be explained by the various psychological problems added due to the burden of the pandemic, which caused worry and nervousness with fear of infection for their child and themselves.
Fear that their sick child's condition might deteriorate during the pandemic was seen in 81.5% of caregivers, with 40.5% finding it difficult to get a medical consultation during the lockdown and more than half of them (55%) facing difficulty in getting tests done and procuring medication. However, 89.5% of caregivers were satisfied with the help or medical advice/assistance given to them by the treating doctors during the pandemic via teleconsultation. With the advances in technology, telemedicine has been a boon to both the treating physician as well as the patients, by providing healthcare services to patients living at a distance [20], [21], [22].
We found that several demographic and clinical variables associated with the care of the child were related to the psychological burden of caregivers such as stress, depression, anxiety, helplessness, anger, guilt, shame, and insomnia. Studies have shown that the perception of the difficulty of quarantine is a critical factor in determining the well-being of both the parents and the children [10], [11], [12], [13]. The stressful experience of caregivers during the pandemic makes it difficult to balance family life and work in professional life, causing feelings of uncertainty. This leads to an increased risk of distress among caregivers, which in turn impairs their ability to be supportive [12]. There is a need for policies aimed at the mental health of caregivers and of children with chronic disorders so that supportive interventions can be offered to those in need during these difficult times; this will help improve the quality of life as well as the care and support given to these children with chronic diseases.
There were certain limitations in our study. We did not enroll a control population to compare the impact of the psychological burden. Some of the parents were already under stress with other psychological issues, which may have prevented the true depiction of the current burden during the pandemic.
5. Conclusion
A high prevalence of stress, anxiety, and depression along with insomnia was detected among the caregivers of children with kidney diseases during the COVID-19 pandemic. Caregivers who experienced more sleep-related problems were more distressed and also scored high on anxiety and depression. To maintain the well-being of caregivers, issues related to the psychosocial impact of COVID-19 should be dealt with appropriately through a systematic approach to decrease the burden of mental health problems in caregivers of children with chronic diseases.
Disclosure of Potential Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Kogon A.J., Vander Stoep A., Weiss N.S., et al. Depression and its associated factors in pediatric chronic kidney disease. Pediatr Nephrol Berl Ger. 2013;28:1855–1861. doi: 10.1007/s00467-013-2497-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gayomali C., Sutherland S., Finkelstein F.O. The challenge for the caregiver of the patient with chronic kidney disease. Nephrol Dial Transpl. 2008;23:3749–3751. doi: 10.1093/ndt/gfn577. [DOI] [PubMed] [Google Scholar]
- 3.Kiliś-Pstrusińska K., Wasilewska A., Medyńska A., et al. Psychosocial aspects of children and families of children treated with automated peritoneal dialysis. Pediatr Nephrol Berl Ger. 2013;28:2157–2167. doi: 10.1007/s00467-013-2532-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsai T.C., Liu S.I., Tsai J.D., et al. Psychosocial effects on caregivers for children on chronic peritoneal dialysis. Kidney Int. 2006;70:1983–1987. doi: 10.1038/sj.ki.5001811. [DOI] [PubMed] [Google Scholar]
- 5.Fielding D., Brownbridge G. Factors related to psychosocial adjustment in children with end-stage renal failure. Pediatr Nephrol Berl Ger. 1999;13:766–770. doi: 10.1007/s004670050695. [DOI] [PubMed] [Google Scholar]
- 6.Chiu M.C. Suggested management of immunocompromized kidney patients suffering from SARS. Pediatr Nephrol Berl Ger. 2003;18:1204–1205. doi: 10.1007/s00467-003-1325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwan B.C.H., Leung C.B., Szeto C.C., et al. Severe acute respiratory syndrome in dialysis patients. J Am Soc Nephrol JASN. 2004;15:1883–1888. doi: 10.1097/01.asn.0000131522.16404.1f. [DOI] [PubMed] [Google Scholar]
- 8.van Exel J., de Graaf G., Brouwer W. Give me a break! Informal caregiver attitudes towards respite care. Health Policy Amst Neth. 2008;88:73–87. doi: 10.1016/j.healthpol.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Vincent C., Desrosiers J., Landreville P., et al. Burden of caregivers of people with stroke: evolution and predictors. Cerebrovasc Dis Basel Switz. 2009;27:456–464. doi: 10.1159/000210092. [DOI] [PubMed] [Google Scholar]
- 10.Dhiman S., Sahu P.K., Reed W.R., et al. Impact of COVID-19 outbreak on mental health and perceived strain among caregivers tending children with special needs. Res Dev Disabil. 2020;107 doi: 10.1016/j.ridd.2020.103790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marchetti D., Fontanesi L., Mazza C., et al. Parenting-related exhaustion during the Italian COVID-19 Lockdown. J Pediatr Psychol. 2020;45:1114–1123. doi: 10.1093/jpepsy/jsaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spinelli M., Lionetti F., Pastore M., et al. Parents’ stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Front Psychol. 2020;11:1713. doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim H., Park K.J., Shin Y.W., et al. Psychological impact of quarantine on caregivers at a children's hospital for contact with case of COVID-19. J Korean Med Sci. 2020;35:e255. doi: 10.3346/jkms.2020.35.e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yuan R., Xu Q.H., Xia C.C., et al. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brunet A., Weiss D.S., Metzler T.J., et al. The peritraumatic distress inventory: a proposed measure of PTSD criterion A2. Am J Psychiatry. 2001;158:1480–1485. doi: 10.1176/appi.ajp.158.9.1480. [DOI] [PubMed] [Google Scholar]
- 16.Bastien C.H., Vallières A., Morin C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 17.Lovibond P.F., Lovibond S.H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety Inventories. Behav Res Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- 18.Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 19.Malkawi S.H., Almhdawi K., Jaber A.F., et al. COVID-19 quarantine-related mental health symptoms and their correlates among mothers: a cross sectional study. Matern Child Health J. 2021;25:695–705. doi: 10.1007/s10995-020-03034-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gulati S., Shruthi N.M., Panda P.K., et al. Telephone-based follow-up of children with epilepsy: comparison of accuracy between a specialty nurse and a pediatric neurology fellow. Seizure. 2020;83:98–103. doi: 10.1016/j.seizure.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panda P.K., Dawman L., Panda P., et al. Feasibility and effectiveness of teleconsultation in children with epilepsy amidst the ongoing COVID-19 pandemic in a resource-limited country. Seizure. 2020;81:29–35. doi: 10.1016/j.seizure.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharawat I.K., Panda P.K. Caregiver satisfaction and effectiveness of teleconsultation in children and adolescents with migraine during the ongoing COVID-19 pandemic. J Child Neurol. 2021;36:296–303. doi: 10.1177/0883073820968653. [DOI] [PubMed] [Google Scholar]