Abstract
Background
Circumcision is a painful procedure that many newborn males undergo in the first few days after birth. Interventions are available to reduce pain at circumcision; however, many newborns are circumcised without pain management.
Objectives
The objective of this review was to assess the effectiveness and safety of interventions for reducing pain at neonatal circumcision.
Search methods
We searched Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 2, 2004), MEDLINE (1966 ‐ April 2004), EMBASE (1988 ‐ 2004 week 19), CINAHL (1982 ‐ May week 1 2004), Dissertation Abstracts (1986 ‐ May 2004), Proceedings of the World Congress on Pain (1993 ‐ 1999), and reference lists of articles. Language restrictions were not imposed.
Selection criteria
Randomised controlled trials comparing pain interventions with placebo or no treatment or comparing two active pain interventions in male term or preterm infants undergoing circumcision.
Data collection and analysis
Two independent reviewers assessed trial quality and extracted data. Ten authors were contacted for additional information. Adverse effects information was obtained from the trial reports. For meta‐analysis, data on a continuous scale were reported as weighted mean difference (WMD) or, when the units were not compatible, as standardized mean difference.
Main results
Thirty‐five trials involving 1,997 newborns were included. Thirty‐three trials enrolled healthy, full term neonates, and two enrolled infants born preterm. Fourteen trials involving 592 newborns compared dorsal penile nerve block (DPNB) with placebo or no treatment. Compared to placebo/no treatment, DPNB demonstrated significantly lower heart rate [WMD ‐35 bpm, 95% CI ‐41 to ‐30], decreased time crying [WMD ‐54 %, 95% CI ‐64 to ‐44], and increased oxygen saturation [WMD 3.7 %, 95% CI 2.7 to 3.7]. Six trials involving 200 newborns compared eutectic mixture of analgesics (EMLA) with placebo. EMLA demonstrated significantly lower facial action scores [WMD ‐46.5, 95% CI ‐80.4 to ‐12.6], decreased time crying [WMD ‐ 15.2 %, 95% CI ‐21 to ‐9.3] and lower heart rate [WMD ‐15 bpm, 95% CI ‐19 to ‐10]. DPNB, compared with EMLA in three trials involving 139 newborns (133 of whom were included in the analysis), demonstrated significantly lower heart rate [WMD ‐17 bpm, 95% CI ‐23 to ‐11] and pain scores. When compared with sucrose in two trials involving 127 newborns, DPNB demonstrated less time crying [MD ‐166 s, 95% CI ‐211 to ‐121], and lower heart rate [WMD ‐27 bpm, 95% CI ‐33 to ‐20]. Results obtained for trials comparing oral sucrose and oral analgesics to placebo, and trials of environmental modification were either inconsistent or were not significantly different.
Adverse effects included gagging, choking, and emesis in placebo/untreated groups. Minor bleeding, swelling and hematoma were reported with DPNB. Erythema and mild skin pallor were observed with the use of EMLA. Methaemoglobin levels were evaluated in two trials of EMLA, and results were within normal limits.
Authors' conclusions
DPNB was the most frequently studied intervention and was the most effective for circumcision pain. Compared to placebo, EMLA was also effective, but was not as effective as DPNB. Both interventions appear to be safe for use in newborns. None of the studied interventions completely eliminated the pain response to circumcision.
Plain language summary
Pain relief for neonatal circumcision
Circumcision is a painful procedure frequently performed on newborn baby boys without using pain relief. Available treatments include dorsal penile nerve block (DPNB), which involves injecting anesthetic at the base of the penis. Ring block is another form of penile block. Locally applied anesthetic creams include EMLA, a water‐based cream including lidocaine and prilocaine. Based on 35 clinical trials involving 1,997 newborns, it can be concluded that DPNB and EMLA do not eliminate circumcision pain, but are both more effective than placebo or no treatment in diminishing it. Compared head to head, DPNB is substantially more effective than EMLA cream. Ring block and lidocaine creams other than EMLA also reduced pain but did not eliminate it. Trials of oral acetaminophen, sugar solutions, pacifiers, music, and other environmental modifications to reduce circumcision pain did not prove them effective. DPNB can cause minor bruising, bleeding, or swelling at the injection site. EMLA and other lidocaine creams can cause skin color changes or local skin irritation. There is a rare risk with lidocaine creams of causing methaemoglobinaemia (blue‐baby syndrome, where the baby's blood lacks sufficient oxygen). However, two trials of EMLA for circumcision pain relief measured methaemoglobin levels and found them normal. The circumcision procedure itself, especially without pain relief, can cause short term effects such as choking, gagging, and vomiting. Long term effects of circumcision without pain relief are not well understood. Strict comparability between trials was rare. Trials used a variety of indicators to measure baby's pain. Crying time, facial expression, and sweating palms can indicate infant pain, as can increased heart rate, breathing rate, and blood pressure. Levels of chemical indicators that can be part of a pain or stress response and are present in the blood or saliva are another gauge of pain levels. Also, procedures were not generally performed in just the same way in different trials. Type of clamp used (8sing a Mogen clamp can shorten the duration of the procedure), length of wait time after injection or application of anesthetic and procedure techniques varied.
Background
Neither the American Academy of Pediatrics nor the Canadian Paediatric Society recommends routine or elective circumcision of the male newborn. Nevertheless, elective circumcision of male newborns is commonly performed in the first few days after birth. Approximately 1.2 million newborn males are circumcised in the United States annually at a cost of 150 to 270 million dollars (AAP 1999). Precise Canadian data are not available because the procedure has been delisted in many provinces, but it is estimated that 48% of male neonates born in Canada are circumcised (CPS 1996). The practice of male neonatal circumcision is not limited to North America; it is performed worldwide for religious and cultural reasons.
As an invasive, painful procedure, unanaesthetized circumcision elicits systemic stress responses in the vulnerable newborn which negatively affect major body systems. Documented physiological and behavioral responses include increased output of adrenal corticoids (Gunnar 1981; Talbert 1976), increased heart rate and respiratory rate, decreased arterial oxygen (Rawlings 1980), skin flushing, vomiting and cyanosis (Poma 1980), changes in sleep/wake state, increased crying (Anders 1974; Gunnar 1981), and diminished responsiveness to parents (Dixon 1984). Unanaesthetized circumcision has also been linked with complications such as apnea and choking (Lander 1997), gastric rupture (Connelly 1992), and recurrence of pneumothorax (Auerbach 1978). Infants circumcised without anaesthesia exhibit stronger pain responses to routine immunizations during the first six months of life than infants who were not circumcised (Taddio 1997b), suggesting that circumcision pain may exert long term effects on infant behavior.
INTERVENTIONS FOR CIRCUMCISION PAIN
Numerous interventions to prevent or reduce circumcision pain have been examined. These include penile blocks, topical anaesthetics, oral analgesia and sucrose administration, non‐nutritive sucking, music and other environmental interventions.
The technique of dorsal penile nerve block (DPNB) for newborn circumcision was first described in 1978 (Kirya 1978), and it has since been extensively evaluated. More recently, subpubic (Dalens 1989) and penile ring block techniques (Hardwick Smith 1998; Lander 1997) have been examined. Adverse effects of penile blocks appear to be limited to bruising and slight bleeding at the injection site (Snellman 1995). Of note, the rapidity of onset of the anaesthetic used for penile blocks (generally 1% lidocaine without epinephrine) is intermediate and a "wait time" of 5 minutes is recommended to achieve anaesthesia (Taddio 2001). Wait time is a concern for clinicians because it increases the total time required for the circumcision surgery; however, inadequate "wait time" influences anaesthetic effect (Kharasch 2003).
Several types of topical anaesthetics have been used for neonatal circumcision, including eutectic mixture of local anaesthetics (EMLA) and 4 to 30% lidocaine creams. EMLA is a water‐based cream that contains 2.5% lidocaine and 2.5% prilocaine. Compared with placebo, EMLA attenuates the pain responses of increased heart rate, facial activity and crying, and decreased oxygen saturation (Lander 1997; Taddio 1997). A meta‐analysis of three studies examining this intervention indicated that the use of EMLA results in a significantly lower increase in heart rate (from baseline) and less crying during the various phases of circumcision surgery compared to placebo. In two of the included studies, lower facial action scores suggested less pain in the EMLA treated groups compared to placebo (Taddio 2002).
Potential difficulties with drug administration and the presurgical wait time may limit the feasibility of topical anaesthesia as a pain intervention for circumcision in many settings (Lander 1997). Considerable technical skill is required to apply the drug, and to secure the occlusive dressing needed to keep it in place. For adequate absorption, EMLA must be applied for at least 60 minutes prior to surgery (Taddio 1998), and must be reapplied if the infant voids during the wait time.
Methaemoglobinaemia (MetHb), caused by oxidation of haemoglobin by the metabolites of prilocaine, is a serious but relatively rare risk associated with EMLA use in infants less than 12 months of age. A recent systematic review of the use of EMLA for acute pain in infants demonstrated that the risk of significant MetHb is low with single dose applications of 0.5 to 2g applied for 10 ‐ 180 minutes for full term neonates, and 0.5 to 1.25g applied for 3 to 180 minutes for preterm neonates (Taddio 1998). Local skin reactions, such as blanching, erythema, and edema of the skin have been reported with the use of EMLA , but these are usually transient and not considered serious.
Sucrose or other sugar solutions alone or in combination with non‐nutritive sucking have recently been recommended as interventions for procedural pain management (Mitchell 2000). Oral sucrose is thought to activate central endogenous pathways, and may stimulate release of endorphins from the hypothalamus. Non nutritive sucking (NNS) is also thought to have an analgesic‐like effect through stimulation of orotactile and mechanoreceptor mechanisms (Gibbons 2001; Mitchell 2003). The sensations created by NNS may deflect attention away from pain and facilitate self regulation because the infant is in control of the sucking. Sucrose and NNS appear to operate synergistically when offered in combination, and may provide more effective pain relief (Carbajal 1999; Gibbons 2001; Gibbons 2002). The analgesic effect of sucrose is activated within two minutes, and lasts for three to five minutes (Haouari 1999; Mitchell 2003). Although sucrose in a wide variety of dosages (concentrations from 12 to 24%, and volumes from 0.05 to 2.0 ml) has generally been found to decrease acute, procedural pain responses in neonates (Mitchell 2000; Stevens 1997), the optimal dose has not yet been identified. Meta‐analyses results indicate that a 0.24g dose is effective to reduce pain responses in term infants, and higher doses do not appear to increase effectiveness (Stevens 1997). In comparison, relatively small doses (0.01 to 0.02g) appear to be effective for preterm infants (Johnston 1997). Interest in sucrose or other sugar solutions as a single or adjunctive intervention for circumcision pain is reflected in the design of recent research (e.g. Kass 2001; Kaufman 2002).
Acetaminophen is the most frequently prescribed non‐opioid oral analgesic used to treat mild to moderate pain in pediatric populations (Berde 2002; McGrath 1990). Acetaminophen is safe and effective for neonates and can be administered orally or rectally (Stevens 1999). Acetaminophen has been used as an intervention for circumcision pain (Howard 1994). A variety of non‐pharmacological interventions have been evaluated for treatment of acute procedural pain in neonates. In theory, these interventions provide nonpainful stimuli that compete with painful stimuli for the neonate's attention, and thus may blunt the perception of pain (Bellieni 2002). Interventions such as rocking, massage, facilitated tucking, and cuddling reduce pain responses during invasive procedures (Campos 1994; Corff 1995; Gray 2000). Music and other sounds (intrauterine, heartbeat) provide an auditory stimulus which may modulate pain perception and these have been evaluated as interventions for circumcision pain (Marchette 1989; Marchette 1991).
NEONATAL PAIN RESPONSES
It is difficult to evaluate the effectiveness of interventions for circumcision pain because newborns are non‐verbal and display stereotypic responses to a variety of painful and non‐painful stimuli. To maximize the validity of pain assessment in newborn populations three classes of pain indicators or outcomes, biochemical, physiological, and behavioural, are generally employed for research. Salivary and serum cortisol, the most frequently measured biochemical indicators, serve as markers of the stress response to pain because hormones of the hypothalamic‐pituitary‐adrenal axis are assayed. Physiological indicators include heart rate, respiratory rate, blood pressure, transcutaneous oxygen saturation (Tc pO2), transcutaneous carbon dioxide (Tc pCO2), oxygen saturation (SaO2), palmar sweat, intracranial pressure (ICP) and vagal tone. In newborn populations, heart rate is the most frequently studied physiological indicator (Sweet 1998). Behavioral indicators include facial expression, cry, gross motor movement, and changes in behavioral state. Facial expression (Grunau 1987) is the most comprehensively studied behavioral indicator for neonatal pain.
Multidimensional measurement tools that employ more than one parameter usually contain physiological and behavioral indicators, and occasionally add contextual information to obtain an overall pain score. The Neonatal Infant Pain Scale (NIPS) (Lawrence 1993) and the Premature Infant Pain Profile (PIPP) (Stevens 1996) are multidimensional tools frequently utilized as outcome measures for investigation of acute procedural pain in term and preterm neonates. Although a number of pain measures are available for use with neonatal populations, no single measure has proven to be the best for all situations. Accordingly, all outcomes evaluated in the included studies as measures of neonatal pain were included in this review.
SUMMARY
The substantial amount of research conducted to date suggests a willingness to address the problem of circumcision pain. However, the majority of neonates are circumcised without interventions for pain (Myron 1991; Ryan 1994; Snellman 1995; Wellington 1993). This situation persists despite growing awareness that newborns may perceive pain more intensely than older children or adults (Anand 2001; Fitzgerald 1993) and can be significantly compromised by it.
It has been suggested that training to manage circumcision pain is inadequate to promote consistent use of available interventions (Howard 1998). Recent surveys indicate that significant numbers of obstetricians (75%), family practitioners (44%), and pediatricians (29%) do not use analgesia/anaesthesia for circumcision because of concerns about adverse drug effects or because they believe that the procedure does not require pain management (Maxwell 1999; Stang 1991; Stang 1998).
Although a wide variety of interventions for circumcision pain have been examined, the individual and relative effectiveness of each has not been systematically assessed. Thus, the apparent reluctance of practitioners to adopt the regular use of pain interventions for circumcision may reflect beliefs that the findings of research conducted to date are collectively un‐interpretable. At the same time, negative perceptions of the technical and practical difficulties associated with pain interventions may diminish clinician motivation to implement their regular use.
A systematic review of the research in this area was needed to summarize and identify implications arising from the existing evidence, and to provide an informed basis for practice and to identify gaps in knowledge which require further investigation. This review adds to knowledge gained from a previous systematic review which examined the efficacy of a single intervention for circumcision pain (Taddio 2002) by evaluating the efficacy and safety of all interventions for reducing pain at neonatal circumcision.
Objectives
To determine the safety and effectiveness of interventions to relieve pain associated with neonatal circumcision. Subgroup analyses were prespecified according to wait time (after anaesthetic administration and prior to start of surgery) for penile blocks, and for dose delivered for sucrose interventions.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs). Studies reported only as abstracts were included if relevant.
Types of participants
Male term or preterm neonates undergoing circumcision during the neonatal period (with postnatal age maximum of 28 days after reaching 40 weeks corrected gestational age).
Types of interventions
Any intervention intended to relieve pain during the circumcision procedure, for example, penile blocks, topical anaesthetics, oral sucrose administration, oral analgesics, surgical devices or techniques, or environmental manipulation such as music therapy or special restraints. This review included trials of interventions for circumcision pain in which any intervention was compared with placebo, no treatment, or with another active intervention.
Types of outcome measures
The primary outcome was pain as assessed by:
1. Physiological variables, such as heart rate (HR), respiratory rate (RR), oxygen saturation, or blood pressure (whether reported as change in, mean or absolute values) 2. Biochemical variables, such as salivary or serum cortisol levels (whether reported as pre‐ and post‐ measures or as change from baseline values) 3. Cry variables, for example, latency and duration of first cry, total cry duration, and/or percentage of time crying during the circumcision procedure 4. Validated pain measures, for example: ‐ Neonatal Infant Pain Score (Lawrence 1993); ‐ Neonatal Facial Action Coding System (Grunau 1987); ‐ Premature Infant Pain Profile (Stevens 1996); ‐ Other pain measures.
Secondary outcomes:
Complications of pain interventions were assessed as secondary outcomes. The outcomes included but were not limited to: 1) occurrence/incidence of methaemoglobinaemia (topical anaesthesia) 2) blanching and local skin irritations (topical anaesthesia) 3) bleeding, bruising and hematoma formation (penile blocks) 4) behavioral responses such a choking, spitting up, etc. during circumcision (all interventions)
Difficulties encountered in implementation of pain interventions, as reported by researchers, were noted.
Search methods for identification of studies
Standard methods as per the guidelines of the Cochrane Neonatal Review Group (CNRG) were utilized. 1. CIRCUMCISION/exp 2. circumcision surgery.mp 3. newborn circumcision.mp 4. 1 OR 2 OR 3 5. local anaesthes* 6. penile block.mp/exp 7. dorsal penile nerve block.mp/exp 8. ring block.mp/exp 9. 5 OR 6 OR 7 OR 8 10. eutectic mixture of local anaesthetics.mp/exp 11. EMLA.mp/exp 12. LIDOCAINE.mp/exp 13. 10 OR 11 OR 12 14. acetaminophen.mp/ OR paracetamol.mp/exp 15. sucrose.mp 16. pacifiers.mp 17. music therapy.mp 18. Gomco clamp.mp 19. Mogen clamp.mp 20. 9 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 21. 4 AND 20 22. HUMAN 23. MALE 24. 22 and 23 25. infant, newborn 26. neonat* 27. 25 OR 26 28. 24 AND 27 29. 21 AND 28 30. clinical trial 31. 29 AND 30
Databases searched included: Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 2, 2004; MEDLINE 1966 ‐ April 2004; EMBASE 1988 ‐ 2004 week 19; CINAHL 1982 ‐ May week 1 2004; PubMed 1966 ‐ May 2004; Web of Science 1975 ‐ May 2004; Dissertation Abstracts 1986 ‐ May 2004. Keywords and (MeSH) terms included infant/newborn, male, circumcision, penile blocks, sucrose, lidocaine, EMLA, acetaminophen. Abstracts of the World Congress on Pain were searched for the years 1993 ‐ 1999 inclusive. Reference lists of all articles were screened to identify any additional studies. Language restrictions were not imposed.
Data collection and analysis
Study Selection
The titles and abstracts of all reports identified through the electronic and other searches were scanned independently by two reviewers and full study reports were obtained for those that appeared to meet the inclusion criteria. Study reports were then evaluated independently by two reviewers for possible inclusion in the review. Disagreements were resolved by consensus. Studies rejected at this stage were included in the Table of Excluded Studies. Quality Assessment
Assessment of the quality of all included studies was undertaken independently by two reviewers as a component of the data extraction process. Standard methods of the CNRG were used to assess: 1) the randomisation procedure, 2) concealment of allocation/blinding of randomisation, 3) blinding of intervention, 4) subject attrition and follow‐up, and 5) blinding of outcome measurement. As per the CNRG guidelines, an overall quality score was not assigned. Reviewers were not blind to trial authors or institutions during the study selection or quality assessment processes.
Data Extraction
Data were extracted from included studies by two independent reviewers using a data extraction form designed specifically for this review. The data extraction form was developed in a draft format and piloted on several studies and modified as required before use. The reviewers abstracted data independently, compared results and resolved differences.
Sixteen trials included in this review either did not report outcome data, or did not report data in a format that could be analysed in this review (Arnett 1990; Benini 1993; Blass 1991 A; Holliday 1999; Holve 1983, Joyce 2001; Kass 2001; Marchette 1989; Marchette 1991; Maxwell 1987; Mohan 1998; Mudge 1989; Spencer 1992; Williamson 1997; Zahorodny 1998; Zahorodny 1999). Additional information was sought from ten authors and means and standard deviations were subsequently obtained for three trials (Benini 1993; Joyce 2001; Kass 2001). Where means and standard deviations were not available, data were imputed or derived from graphs contained in the reports (Arnett 1990; Benini 1993; Blass 1991 A; Holliday 1999; Maxwell 1987; Mohan 1998; Mudge 1989; Taddio 1997). Missing standard deviations were either calculated from other summary statistics or imputed using singular or mean standard deviations from similar trials.
Several authors reported total sample size only and information about the number of subjects per group was obtained from the authors (Benini 1993; Joyce 2001). When additional information about sample size could not be obtained from the authors, we assumed equal distribution to study groups in our data analyses (Blass 1991 A; Zahorodny 1998; Zahorodny 1999).
Data Analysis
The outcomes presented in this review were reported as results obtained during the whole circumcision procedure. Usually, the circumcision surgery was described as commencing with application of forceps to the dorsal foreskin of the penis (referred to as dorsal or lateral clamping) and ending with removal of the surgical clamp (the Gomco, Mogen, or Plastibell surgical device, also referred to as a clamp). Some authors reported a single numerical outcome result for the entire circumcision procedure (e.g. Butler O'Hara 1998; Howard 1999; Maxwell 1987; Taddio 1997). Others reported numerical results by procedure phase or step (e.g. dorsal foreskin grasped with forceps, adhesion lysis, dorsal incision, surgical clamp application, foreskin amputation, surgical clamp removal) (Benini 1993; Lander 1997; Woodman 1999). For the latter studies, depending on the outcome, we calculated either the arithmetic mean (e.g. heart rate) or total (e.g. time crying) across the phases or steps of the circumcision (as defined by the authors), and did not include the baseline or recovery phase data. Variance formulae for these arithmetic means and these totals were derived according to the general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)). We assumed a correlation of 0.5 as proposed by Follmann 1992. Additional Tables 1 ‐ 7 (Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7) provide specific details on summary estimate extractions from the included studies.
1. Trials assessing pain/behavior scores.
| Study ID | scale | measurement method | data reported | data preparation |
| Arnett 1990 | infant irritability irritabilify graded subjectively on a scale of 1 to 6 with 1 representing the least crying/agitation and 6 the most | nurse and physician rating of infant irritability graded before, during and 1 hour after circumsion | mean/SD of assessment during procedure | data entered into meta‐analysis as reported |
| Benini 1993 | Neonatal Facial Action Coding System (Grunau , 1990b) 10 facial actions scored, 7 (brow bulge, eye squeeze, nasolabial furrow, open mouth, vertical stretching of mouth, horizontal stretching of mouth, taut tongue) entered into analysis | facial actions videotaped continuously, second by analysis of facial actions 10 facial actions scored, 7 facial actions entered into analysis total score computed by summing 7 categories | outcome data (means/SDs) obtained from authors | calculate arithmetic mean of scores across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [application of dorsal clamp, incision, adhesion lysis, Gomco clamp on, foreskin excision, Gomco clamp off, restraints removed] |
| Butler‐O'Hara 1998 | Neonatal Infant Pain Scale (NIPS) consists fo 6 behavioral components with a composite score of 0 to 6 5 components used ‐ facial expression, cry, breathing pattern, arm movements, state of arousal (Lawrence, 1993) | procedure videotaped NIPS scores assigned for each of 6 events (clamping of foreskin, adhesion lysis, dorsal cut, adhesion lysis, tying of Plastibell, foreskin excision) mean NIPS score calculated for each infant | mean(SD) NIPS score/group | data entered into meta‐analysis as reported |
| Dixon 1984 (Holve 1983 is primary study report) | Brazelton Neonatal Assessment Scale (BNAS) consists of 27 behavioral items, each scored on scale of 1 to 9, and 20 reflexes scored on 3 point scale scale examines organization and integration of behavior in response to positive and adversive situations | examinations conducted prior to (exam 1), following the circumcision (exam 2), and 1 day after circumcision (exam 3) | mean scores/item for 3 exam times | states "variation in item scores precluded determination of statistically significant differences between groups' not included in meta‐analysis |
| Hardwick‐Smith 1998 | behavioral state (Stang et al 1988) score 1 ‐ 6 in order of increasing arousal | scored at baseline, 10 intervals during procedure, and 2 hr post‐circumcision | p values | not included in meta‐analysis |
| Holliday 1999 | behavioral scale ‐ includes 8 behavior state variables (sleep state, cry, facial expression, torso movement, soothability, response to distress, need for tactile stimulation, environmental noise) each variable scored 1 to 6, scores totaled for each infant | assessed 20 min before, during and after circumcision | means scores/group reported in graph format | graph extractions to obtain mean/SD |
| Howard 1994 | Postoperative Comfort Score (Attia 1987) 10 behaviors, each scored 0, 1, or 2, possible scores 0 to 20, lower score = less comfortable | assessed baseline, and postcircumcision at 30, 60, 90, 120, 360 min | mean/SD scores/group/interval mean/SD change from baseline scores/group/interval | data entered into meta‐analysis as reported for 30 min post‐circumcision scores |
| Howard 1999 | behavioral distress scale (from Stang et al 1997) score 0 ‐ 3 based on Brazelton statte assessment score 0 = neutral to 3 = sustained cry | videotape of procedure assessed and scores assigned every 30 s of the procedure | mean/SE scores / group for stages 2 to 6 of procedure | data entered into meta‐analysis as reported "procedure" = [block administration to recovery; includes 4 min WT and Gomco clamp left on for 5 min] |
| Joyce 2001 | Riley Infant Pain Scale 6 categories of behavior (vocal, facial expression, body movement, sleep, consolability, response to touch) rates on scale of 0 (no pain) to 3 (severe pain) | videotape of procedure assessed at baseline, undressing, restraints, cleanse, clamping, cutting, end of procedure, 15 min post and 30 min post | RIPS score / group / phase presented in graphic format p values | not included in meta‐analysis |
| Kass 2001 | MBPS ‐ modified behavioral pain scale (Taddio et al, 1995) rates facial expression, crying, and body movements to obtain a score of 0 to 10 | scored at 30 s intervals | mean/SD for baseline and procedure MBPS / group obtained from authors | mean/SD procedure scores entered into meta‐analysis |
| Macke 2001 | Nursing Child Assessment Feeding Scale (NCAFS) 76 behavioral binary items (yes,no) grouped into 6 subscales based on concepts of adaptation and synchronism | scored during feeding interaction before and after circumcision | mean/SD score pre/post circumcision | data included as reported |
| Newton 1999 | Brazelton Neonatal Assessment Scale ‐ scale categorized to 6 level\s ‐ (deep sleep (1), light sleep (2) drowsy (3), quiet alert (4) active alert (5) crying (6) (Brazelton, 1984) | 3 evaluations ‐ baseline, injection, clamp application | modal state/group | data not included |
| Stang 1988 | behavioral state 6 levels = quiet sleep (1), active sleep (2), drowsy (3), alert (4), active awake (5), crying (6) (Brazelton, 1973) | assessed at baseline, during injection, during circumcision, and 30 min from the start of the circumcision | modal response / group / time period | data not included |
| Stang 1997 | behavioral state scale and behavioral distress scale 4 levels ‐ neutral (0), minimal fuss (1), moderate fuss (2), sustained cry (3) (Brazelton, 1973) | behavioral state and distress scored every 30 s beginning 2 min before circumcision scores averaged for 5 periods ‐ preinjection, injection, 2 min post‐injection, 4 min post‐injection, circumcision | mean/SD /group / study period | mean/SD for circumcision period included |
| Taddio 1997 | Neonatal Facial Coding System (Grunau et al, 1987; 1990) codes presence or absence of 10 discrete facial actions (brow bulge, eye squeeze, nasolabial furrow, open mouth, vertical stretching of mouth, horizontal stretching of mouth, lip pursing, taut tongue, chin quiver, tongue protrusion) higher score = more pain | facial actions continuously recorded on videotape facial actions scored from videotape in 2 s intervals for first 20 s of each phase raw scores of each facial action expressed as proportion of time observed/phase; poorly correlated facial actions deleted leaving 6 facial actions; the six scores were weighted and totaled to arrive at overal score for facial action | mean/95% confidence intervals for facial activity score / group / 13 phases reported in graph format data extracted from graphs | data extraction to obtain mean/SD facial score for circumcision phases circumcision (7 phases) = [application of forceps to foreskin excision] calculate arithmetic mean/group across phases of circumcision calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) SE = ((high CI ‐ low CI)/2)/1.96 SD = SE (sqrt(n)) |
| Weatherstone 1993 | newborn pain behavior scale adapted from 3 other scales (Brazelton 1973; Yarrow 1975; Ross 1988) score includes assessment of behavioral state, leg and arm movement, facial expression, torso movement, respiratory pattern, soothability, response to distress by caregivers, tactile stimulation | videotape of procedure scored in 30 s intervals | increase in mean/SD % of time behavior observed post‐cirucmcision compared to pre‐ circumcision/group | data not included |
2. Trials assessing heart rate outcome variables.
| Study ID | measurement method | data reported | preparation of data |
| Arnett 1990 | HR measured by pulse oximetry at baseline, every min for 4 min, and 5 min post‐circumcision | mean HR/group/phase reported in graph format | graph extraction for means graph extraction for SDs (averaged over 4 phases of the circumcision procedure) "procedure" = [min 1 to min 4]; steps not described or standardized |
| Benini 1993 | HR measured continuously by pulse oximeter | outcome data (mean/SDs) obtained from authors | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [application of dorsal clamp, incision, adhesion lysis, Gomco clamp on, foreskin excision, Gomco clamp off, restraints removed] |
| Butler‐O'Hara 1998 | HR monitored continuously using cardiac monitor | mean/SD heart rate (bpm) at completion of circumcision by group mean/SD heart rate (bpm) change from baseline at completion of circumcision by group | data entered into meta‐analysis as reported |
| Joyce 2001 | HR monitored continuously using cardiac monitor | data (bpm) obtained from authors | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [cut, end of procedure] |
| Hardwick‐Smith 1998 | HR monitored continuously using cardiac monitor highest HR recorded at start of each interval | increase in HR from baseline per group for operative interval reported in graph format | graphs did not depict SDs (whiskers); researchers reported control infants had signifcantly greater increase over baseline during 7 out 10 operative intervals; they did not comment on differences between the groups/interval |
| Herschel 1998 | HR monitored continuously using cardiac monitor | mean/SD HR (bpm) change from baseline during procedure by group | data entered into meta‐analysis as reported "procedure" = lateral clamp of foreskin to foreskin excision |
| Holliday 1999 | HR monitored continuously using cardiac monitor HR recorded every 5 min before, during, 5 and 20 min after circumcision | mean/SD HR (bpm)/group reported in graph format for 4 time points (before, during, 5 min after, 20 min after) | graph extraction to obtain mean/SD during procedure |
| Holve 1983 | HR continuously recorded using monitor | mean change in HR from baseline (bpm) weighted averages/group for 6 phases reported in graphic format | no SDs, SEs depicted on graphs |
| Howard 1994 | HR counted via auscultation every 30 s | mean/SD HR (bpm) / group / phase mean/SD HR (bpm) change from baseline by group/phase | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [dissection, clamp on, excision, clamp off] |
| Howard 1999 | HR recorded every 60 s using cardiac monitor | ‐ mean/SE HR (bpm) during procedure by group | means included as reported convert SE to SD using formula: SD = SE (sqrt (n)) "procedure" = [block administration to recovery; includes 4 min WT and Gomco clamp left on for 5 min] |
| Kass 2001 | HR monitored at 1 min intervals during procedure | mean/SD HR (bpm) during procedure by group obtained from authors | mean/SD entered into meta‐analysis |
| Kurtis 1999 | HR monitored continuously using cardiac monitor | mean/SD % HR change from baseline during procedure by clamp used (Mogen, Gomco) and by penile block status (block, no block) | data entered into meta‐analysis as reported "procedure" = [lysing adhesions to 60 sec after closing clamp] |
| Lander 1997 | HR monitored continuously using cardiac monitor | mean/SD HR (bpm) change from baseline by phase by group | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [separation, clamp on, clamp off] |
| Macke 2001 | HR recorded every 15 s using cardiac monitor | mean/SD HR (bpm) during circumcision by group | data included as reported |
| Marchette 1989 | HR monitored | mean HR /phase / group no SDs reported | not included |
| Marchette 1991 | HR monitored and data collected during 14 cirumcision steps | RMANOVA over 14 steps | not included |
| Masciello 1990 | HR monitored continuously using cardiac monitor peak HR during each step recorded | mean HR as a percent of baseline HR reported in graphic format | not included |
| Maxwell 1987 | HR monitored continuously by pulse oximeter peak HR during each period recorded | mean/SD HR change / group / period as a % of control (baseline) reported in graph format | graph extraction to obtain mean/SD during circumcision procedure |
| Mohan 1998 | HR monitored continuously by pulse oximeter HR recorded at each of 9 steps | mean HR / group / procedure step reported in graph format | graph extraction to obtain mean HR / group / procedure step substituted weighted average treatment‐specific SDs from 5 studies: Benini 1993, Joyce 2001, Lander 1997, Taddio 1997, Woodman 1999 for EMLA and from 3 studies: Herschel 1998, Kass 2001, Zolnoski 1993 for sucrose |
| Mudge 1989 | HR measured by monitor at 5 time points during circumcision | mean HR / group / event reported in graph format RMANOVA for 4 events (adhesion breakdown to clamp off) | graph extraction to obtain mean HR/group for events 2 ‐ 5 calculate arithmetic mean HR / group across 4 phases of the procedure (adhesion breakdown, clamp on, tighten clamp, clamp off) substitute SDs from Woodman 1999 who applies same outcome to same comparison |
| Newton 1999 | HR monitored continuouslly by pulse oximeter HR recorded at 10 s intervals | mean/SD HR / group at baseline, injection, clamp application | included as reported |
| Spencer 1992 | HR monitored by pulse oximeter recorded highest HR for each of 6 events | mean change in HR (bpm) from baseline / group / event | no SDs, not included |
| Taddio 1997 | HR continuously monitored by cardiac monitor | mean/SD HR (bpm) change from baseline during procedure | data included as reported "procedure" = [forcep application, lysis of adhesions, dorsal incision, clamp application, pull foreskin through clamp, tighten clamp, cut foreskin] procedure does not include clamp removal at 5 min after cut foreskin |
| Weatherstone 1993 | HR monitored at 5 min intervals for 20 min | none | not included |
| Williamson 1983 | HR monitored continuously | mean/SD HR (bpm) change from baseline for 3 min "dissection" period | mean/SD data included as reported dissection does not include clamp application |
| Woodman 1999 | HR monitored continuously using pulse oximeter recorded peak heart rate during or immediately following 7 stages of circumcision procedure | mean/SD peak HR (bpm) / group | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [clamp, adhesionlysis, dorsal clamp, bell on, clamp tightening, bell off] |
| Zolnoski 1993 | HR monitored continuously using cardiac monitor HR (bpm) recorded at beginning of 7 procedure steps | ‐ mean/SD HR (bpm) /group for 4 procedure steps | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) |
3. Trials assessing cry outcome variables.
| Study ID | measurement method | data reported | data preparation |
| Benini 1993 | cry tape recorded | % time crying/phase (duration of time crying) reported in graph format | means, SEs (assumed) extracted from graph; calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [dorsal clamp, incision, lysis, clamp on, foreskin cut, clamp off, unrestrained] |
| Blass 1991 | cry tape recorded | mean % time crying (duration of time crying) during entire procedure reported in graph format | ‐ graph extraction of group mean/SE; ‐ SD calulated using formula: SD = SE (sqrt (n)) |
| Holve 1983 | cry tape recorded | mean % time crying /interval reported in graphic format | no SDs, not included |
| Hardwick‐ Smith 1998 | cry tape recorded | mean/SD minutes crying/group during operative interval (lateral clamping to clamp removal) | convert reported time to seconds data included in meta‐analysis |
| Howard 1994 | used stopwatch to time crying during each phase | mean/SD % time crying by group/phase mean/SD % time crying change from baseline/group/phase | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [dissection, clamp on, excision, clamp off] |
| Joyce 2001 | behavior videotaped calculated total time crying from start of foreskin cut until crying ceased or 30 min elapsed | cry time (min) for each subject obtained from authors | calculate mean/SD time crying in min and sec/group |
| Kass 2001 | primary outcome variable behavior videotaped | mean/SD time crying (s) /group during procedure obtained from authors | mean/SD included in meta‐analysis |
| Kurtis 1999 | behavior videotaped calculated time crying using stopwatch | mean/SD % time crying during procedure reported by clamp used (Mogen, Gomco) and by penile block status (block, no block) | mean/SD included as reported |
| Lander 1997 | behavior videotaped proportion of time crying calculated/subject | mean/SD % time crying/interval | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y))‐ "procedure" = [separation, clamp on, clamp off) |
| Macke 2001 | continuous vocalizations of 15 s or more classified as crying and tape recorded total s used to calculate % time crying | mean/SD % time crying during circumcision period by group | data included as reported |
| Mohan 1998 | stopwatch used to measure duration of crying | mean % time crying / group during entire procedure | not included |
| Mudge 1989 | crying time tape recorded during procedure measured by stop watch | mean total crying time (s)/group for entire procedure t‐statistic, p value | mean crying time included as reported SD imputed from t statistic procedure includes 5 events (baseline, adhesion breakdown, clamp on, tighten clamp, clamp off) |
| Spencer 1992 | cry duration measured by modified Brazelton Neonatal behavioral Scale (Stang et al, 1988) 6 behavioral states recorded for each of 6 events | mean % change from baseline / group | no SDs, not included |
| Stang 1988 | not described | mean/SEM % time crying during circumcision period/group | means included as reported SEM converted to SD using formula: SD = SEM (sqrt (n)) |
| Taddio 1997 | behavior videotaped calculated % of time crying during each phase | mean/SD % increase from baseline in time crying during procedure | data included as reported "procedure" = [forcep application, lysis of adhesions, dorsal incision, clamp application, pull foreskin through clamp, tighten clamp, cut foreskin] does not include clamp removal at 5 min after foreskin cut |
| Williamson 1983 | time crying recorded using event marker | mean/SD % time crying change from baseline during 3 min dissection period | mean/SD data included as reported |
| Woodman 1999 | behavior videotaped recorded time crying based on facial actions with or without audible cry | mean/SD time crying (s) for 6 phases by group | add time crying for 6 of 8 stages (clamp, adhesionlysis, dorsal clamp, clamp on, clamp tightening, clamp off) to obtain total time crying during procedure add SD to obtain total SD for group |
| Zahorodny 1998 | not reported | mean % time crying/group | substituted weighted average treatment‐specific SDs from three other studies: Benini 1993, Lander 1997, Taddio 1997 for EMLA vs placebo/ no treatment substituted treatment‐specific SDs from Blass 1991 A (also versus water) for sucrose vs placebo/ no treatment substituted with the SDs used in the two above comparisons for EMLA vs sucrose |
| Zolnoski 1993 | cry tape recorded, measured using stopwatch | time cry (s)/infant | mean/SD cry time (s)/group calculated |
4. Trials assessing oxygen saturation outcome variables.
| Study ID | measurement method | data reported | data preparation |
| Arnett 1990 | measured by pulse oximetry at baseline, every min for 4 min during procedure, and 5 min postcircumcision | mean oxygen saturation (%) / group / phase and SDs presented graphically | graph extraction of means, graph extraction of SDs, averaged over 4 phases |
| Benini 1997 | O2sat continuously monitored using pulse oximeter | outcome data (mean/SD) obtained from authors | calculate arithmetic mean/group across phases of the procedure calculate variance for arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) procedure = [application of dorsal clamp, incision, adhesion lysis, Gomco clamp on, foreskin excision, Gomco clamp off, restraints removed] |
| Hardwick‐Smith 1998 | O2sat monitored continuously by pulse oximeter, lowest O2sat recorded at the start of each interval during some intervals of procedure, O2sat not recorded in up to 50% of infants | mean/SD of O2sat (%)/group for operative intervals | data included in meta‐analysis as reported "operative interval" = [llateral clamp, blunt dissection, dorsal clamp, adhesion takedown, Gomco bell on, Gomco clamp applied, Gomco clamp removed] |
| Herschel 1998 | O2sat continuously monitored via pulse oximetry substantial proportion of data lost due to excessive motion (31% control, 10% DPNB, 8% sucrose) | mean/SD O2sat (%) change from baseline during operative procedure by group | data included in meta‐analysis as reported "operative procedure" = [lateral clamp of foreskin, adhesion lysis, dorsal clamp, dorsal cut, foreskin retraction, Gomco application, Gomco tightened, foreskin excision] |
| Holliday 1999 | O2sat continuously monitored, recorded every 5 min before, during, 5min and 20 min after circumcision | mean/SD O2sat (%)/group reported in graph format for 4 time points (before, during, 5 min after, 20 min after) | graph extraction for mean/SD during procedure |
| Joyce 2001 | O2sat monitored continuously using pulse oximeter recorded O2sat (%) at each of 6 data collection points | raw data per subject per 6 phases obtained from authors | calculate mean/SD by group/phase calculate arithmetic mean/group across phases of the procedure calculate variance for arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) procedure = [cut, end] |
| Kass 2001 | monitored O2sat at 1 min intervals during procedure | mean/SD O2sat during procedure by group data obtained from authors | mean/SD included in meta‐analysis |
| Kurtis 1999 | O2sat (%) monitored continuously and transferred to computer | ‐ mean/SD % change from baseline during procedure reported by clamp used (Mogen, Gomco) and by penile block status (block, no block) | data included in meta‐analysis as reported procedure = [lysing adhesions to 60 sec after closing clamp] |
| Marchette 1991 | tcpO2 monitored and recorded during 14 circumcision steps | RMANOVA over 14 steps | not included |
| Masciello 1990 | O2sat monitored continuously by pulse oximeter lowest level during each interval recorded | mean O2sat / group / interval reported in graphic format | not included |
| Maxwell 1987 | O2sat monitored continuously using pulse oximeter peak value during period recorded | mean/SD O2sat /group / period reported in graph format | graph extraction to obtain mean/SD during circumcision period |
| Mohan 1998 | O2sat monitored continuously using pulse oximeter recorded at each of 9 procedure steps | mean O2sat / group / procedure step reported in graph format | graph extraction to obtain mean O2sat / group / step substituted weighted average treatment‐specific SDs from 3 trials: Benini 1993, Joyce 2001, Woodman 1999 for EMLA and from 2 trials: Herschel 1998, Kass 2001 for sucrose |
| Mudge 1989 | O2sat measured by pulse oximeter and recorded at five time points during circumcision | mean O2sat (%) /group/event reported in graph format | graph extraction to obtain mean O2sat/group for events 2 ‐ 5 calculate arithmetic mean O2sat / group across 4 phases of the procedure (adhesion breakdown, clamp on, tighten clamp, clamp off) |
| Spencer 1992 | O2sat monitored by pulse oximeter recorded lowest level for each of 6 events | mean O2sat % change from baseline / group / event | no SDs, not included |
| Weatherstone 1993 | O2sat monitored at 5 min intervals for 20 min | none | not included |
| Williamson 1983 | O2sat measured using transcutaneous electrode (tcpO2) | mean/SD O2sat (torr) change from baseline for 3 min dissection period | data included in meta‐analysis as reported dissection does not include clamp application |
| Woodman 1999 | O2sat monitored continuously using pulse oximeter recorded peak/nadir during or immediately following 7 stages of circumcision procedure | ‐ mean/SD peak/nadir O2sat / stage / group | calculate arithmetic mean/group across phases of the procedure calculate variance for arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) procedure = [clamp, adhesiolysis, dorsal clamp, clamp on, clamp tightening, clamp off) |
5. Trials assessing respiratory rate outcome variables.
| Study ID | measurement method | data reported | preparation of data |
| Butler‐OHara 1998 | RR monitored continuously starting after anesthetic administration, and 1 and 4 hr after procedure | RR variable and difficult to evaluate not reported | not included in meta‐analysis |
| Hardwick‐Smith 1998 | highest RR recorded at start of each interval (anesthesia/restraint, 3 min post restraint/anesthesia, lateral clamp, blunt dissection, dorsal clamp, adhesion breakdown, Gomco bell on, Gomco clamp on, Gomco clamp removed) | mean/SD increase from baseline RR/group for operative intervals (lateral clamping to Gomco clamp removal) | data included in meta‐analysis as reported |
| Holliday 1999 | RR monitored continuously using cardiac monitor HR recorded every 5 min before, during, 5 and 20 min after circumcision | mean/SD RR (bpm)/group reported in graph format for 4 time points (before, during, 5 min after, 20 min after) | graph extraction for mean/SD during procedure |
| Howard 1994 | RR assessed by visual observation every 30 s | mean/SD RR (rpm) / group / phase mean/SD RR (rpm) change from baseline by group/phase | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [dissection, clamp on, excision, clamp off] |
| Howard 1999 | RR counted and recorded every 60 s | mean/SE RR (rpm) by group for procedure | means included as reported convert SE to SD using formula: SD = SE (sqrt (n)) "procedure" = [block administration to recovery; includes 4 min WT and Gomco clamp left on for 5 min] |
| Joyce 2001 | RR monitored continuously, recorded at 6 data collection points | raw data obtained from authors | calculate arithmetic mean/group across phases of the procedure calculate variance for the arithmetic mean using general formula for linear combinations of variance (i.e. Var (X+Y) = Var(x) + Var(Y) + 2Cov(X,Y)) "procedure" = [cut, end of procedure] |
| Kurtis 1999 | RR monitored continuously using physiologic monitor | mean/SD % change from baseline during procedure reported by clamp used (Mogen, Gomco) and by penile block status (block, no block) | data entered into meta‐analysis as reported "procedure" = [lysing adhesions to 60 sec after closing clamp] |
| Mudge 1989 | RR measured by pneumography monitor at 5 time points | mean RR / group / event reported in graph format RMANOVA for 4 events (adhesion breakdown to clamp off) | graph extraction to obtain mean RR/group for events 2 ‐ 5 calculate arithmetic mean RR / group across 4 phases of the procedure (adhesion breakdown, clamp on, tighten clamp, clamp off) |
| Weatherstone 1993 | RR monitored at 5 min intervals for 20 min | none | not included |
6. Trials assessing biochemical outcome variables.
| Study ID | measurement method | data reported | data preparation |
| Masciello 1990 | blood drawn via heel stick 30 minutes post‐circumcision | mean/SD plasma cortisol levels in mg/dL | mg/dL multiplied by 27.59 = nmol/L nmol/L included in meta‐analysis |
| Stang 1988 | blood drawn via heel stick for 1/2 subjects at 30 min post‐circumcision, and 90 min for remaining 1/2 subjects | mean/SEM plasma cortisol levels in nmol/L and ug/dL | means (nmol/L) included in meta‐analysis SEM converted to SD using formula: SD = SEM (sqrt(n)) |
| Williamson 1986 | blood drawn by heel stick at baseline and 30 min post‐circumcision | mean/SEM plasma cortisol levels in ug/dL | SEM converted to SD using formula: SD = SEM (sqrt(n)) ug/dL |
| Holliday 1999 | serum B‐endorphin levels ‐ blood sample taken before and 20 min post‐circumcision | mean/SD / group in pmol/L | data included as reported |
| Joyce 2001 | salivary cortisol samples collected at baseline abd 30 min after procedure | mean/SD before/after no units of measurement results not broken down by group | not included |
| Kurtis 1999 | salivary cortisol | collected sample at baseline and 30 min post‐circumcision | mean/SD included as reported |
| Stang 1997 | plasma cortisol 30 min after beginning of circumcision | mean/SD / group nmol/dL and ug/dL | mean /SD (nmol/dL) included as reported |
| Weatherstone 1993 | serum B‐endorphin level taken pre‐operatively and 15 min after circumcision | mean/SD B‐endorphin level (pg/mL) for pre and post circumcision period/group | mean/SD level for post‐circumcision period included as reported |
| Williamson 1986 | plasma cortisol obtained at baseline and 30 min after Gomco clamp applied | mean/SEM plasma cortisol levels (ug/dL)/group | ug/dL multiplied by 27.59 = nmol/L SEM converted to SD using formula: SD = SEM (sqrt(n)) |
7. Trials assessing blood pressure outcome variables.
| Study ID | measurement method | data reported | data preparation |
| Holliday 1999 | systolic BP monitored continuously using cardiac monitor HR recorded every 5 min before, during, 5 and 20 min after circumcision | mean/SD BP (mmHg)/group reported in graph format for 4 time points (before, during, 5 min after, 20 min after) | graph extraction for mean/SD during procedure |
| Marchette 1991 | systolic and diastolic BP monitored and recorded during 14 steps of the cirumcision procedure | RMANOVA over 14 steps | not included |
| Maxwell 1987 | BP measured by Doppler every 5 min | mean/SD systolic BP change as a % of control / group / period reported in graph format | graph extraction to obtain mean/SD during circumcision period |
| Mohan 1998 | systolic and diastolic BP measured over upper arm at each of 9 procedural steps | mean systolic and diastolic BP (mm Hg) reported in graph format | graph extraction to obtain mean / group / step substituted treatment‐specific SDs from Taddio 1997 for EMLA; no SDs available for sucrose |
| Taddio 1997 | systolic and diastolic BP measured at baseline and during lysis of adhesions | mean/SD increase mm Hg in systolic and diastolic BP | data included as reported |
| Weatherstone 1993 | BP monitored at 5 min intervals for 20 min | none | not included |
Data were analysed using the statistical package (RevMan 4.2) provided by the Cochrane Collaboration. When two or more studies were identified that examined the same comparison and clinically similar outcomes, data were pooled using fixed effects. Random effects accounting for inter‐study heterogeneity were considered in sensitivity analyses. Studies that compared an active intervention with placebo were analysed separately from those that compared the same active intervention with no treatment.
Continuous data summaries are reported as weighted mean differences (WMD) when the units provided were compatible. When the units were not compatible, the standardized mean difference (SMD) is reported. The SMD describes the difference between the treatments in terms of units of standard deviations (SDs). To improve interpretability, we also report estimates of WMDs derived from the estimated SMDs. To derive the WMDs from the SMDs, we selected either the unit used in the majority of the trials or the most clinically relevant unit under a particular comparison and pooled the available SDs from the trials that used that unit. We then multiplied this pooled SD by the SMD to obtain an estimate of the WMD. The WMDs thus derived are reported along side the SMDs in the results. An example of how a SMD was converted to a WMD is provided in Figure 1.
1.
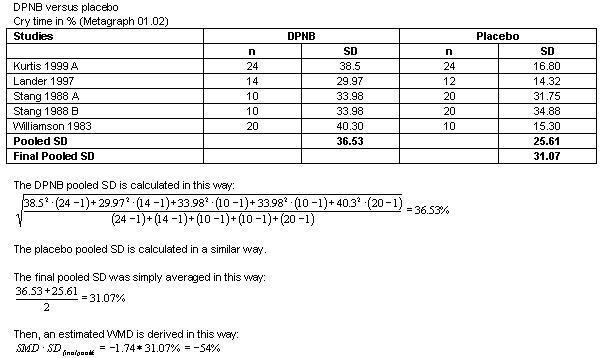
Individual study outcomes were reported as both final values (FVs) and change from baseline values (CVs). It is appropriate to combine FVs and CVs when combining mean differences to calculate a WMD. However, it is not appropriate, generally, to combine FVs and CVs when combining SMD to calculate an overall SMD. CVs often have smaller standard errors (SEs) than FVs since some of the intra‐patient variation is removed from their SEs. Thus the individual study CV SMD tend to be in smaller SD units than the individual study FV SMD. However, in this systematic review, many of the SEs for CVs were either within the range of the FV SEs or they were larger, which is counterintuitive to the argument presented here. Hence, some of the SMD calculated in this review do combine CVs and FVs (Metagraphs 01.03; 01.08; 01.09; 03.02). Additional Tables 1 ‐ 7 (Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7) provide specific details on summary estimate extractions from the included studies.
Heterogeneity was assessed quantitatively with the I‐squared statistic (Higgins 2003). The I‐squared statistic indicates the percent variability due to between study (or inter‐study) variability as opposed to within study (or intra‐study) variability. An I‐squared greater than 50% may be considered large. Only non‐null heterogeneity statistics are presented here. Too few studies under a single comparison did not allow for any assessment of publication bias nor extensive sub‐group or sensitivity analyses. However, post‐hoc, we selected heart rate (the most frequently reported outcome) for between‐study subgroup analyses using a chi‐square method proposed by Deeks 2001. We selected the following subgroup analyses a priori: for penile block interventions, "wait time" from anaesthesia administration to start of the circumcision procedure were considered by the following three categories: no wait time reported, wait time </= 5 minutes, wait time >/= 5 minutes; for sucrose administration interventions, dose of sucrose administered was to be considered but could not be due to the lack of information provided in the reports. Surgical clamp type, use of pacifiers as a co‐intervention, and choice of control group were selected for consideration post‐hoc.
Results
Description of studies
210 unique references were identified through search of the electronic databases. The full text of forty‐two potentially relevant articles were obtained and reviewed for possible inclusion in this review. Six studies were excluded (see Table ‐ Characteristics of Excluded Studies). In two excluded studies, subjects were not randomised and the intervention was chosen by the attending physician (Malnory 2003; Olson 1998). Two of the excluded studies had no comparison group (Mintz 1989, Russell 1996). One study was a cohort design and the outcome data for the control group was obtained from a previously conducted trial (Taddio 2000), and one (Taeusch 2002) was a head to head comparison of surgical clamps used for the circumcision procedure rather than a direct comparison of interventions for pain relief.
Thirty‐five studies (thirty‐six reports) were included in this systematic review. Details of each are given in the Table ‐ Characteristics of Included Studies. Two reports outlined different outcome data from the same trial (Dixon 1984, Holve 1983). Two trials were reported as abstracts only (Zahorodny 1998, Zahorodny 1999) and we were unable to obtain additional information from the authors. One unpublished report of Master's thesis research was included (Zolnoski 1993).
Thirty‐three of the thirty‐five included studies enrolled healthy, full term neonates. One trial included infants born preterm (and less than 28 days age after reaching 40 weeks corrected gestational age) who were ready for discharge from the neonatal intensive care unit (NICU) at the time of circumcision (Butler O'Hara 1998), and one trial enrolled infants born preterm and weighing 1600 ‐ 2500g at the time of circumcision (Holliday 1999).
Nineteen trials examined the effectiveness of penile blocks (Arnett 1990; Butler O'Hara 1998; Hardwick Smith 1998; Herschel 1998; Holliday 1999; Holve 1983; Howard 1999; Kass 2001; Kurtis 1999 A; Lander 1997; Masciello 1990; Maxwell 1987; Newton 1999; Spencer 1992; Stang 1988 A; Stang 1997; Williamson 1983; Williamson 1986; Williamson 1997). Twelve trials assessed topical anaesthetics (EMLA, lidocaine creams) (Benini 1993; Butler O'Hara 1998; Holliday 1999; Howard 1999; Joyce 2001; Lander 1997; Mohan 1998; Mudge 1989; Taddio 1997; Weatherstone 1993; Woodman 1999; Zahorodny 1998), and nine evaluated oral sucrose in a variety of concentrations and doses (Blass 1991 A; Herschel 1998; Kass 2001; Kaufman 2002; Mohan 1998; Stang 1997; Zahorodny 1998; Zahorodny 1999; Zolnoski 1993). In two trials, subjects received an oral analgesic (acetaminophen) (Howard 1994; Macke 2001). Three trials evaluated forms of environmental manipulation (e.g. music, intrauterine sounds) (Joyce 2001; Marchette 1989; Marchette 1991). For trial details see Table ‐ Characteristics of Included Studies.
In the trials, the interventions were compared with placebo/sham treatments (e.g. saline penile block or inactive topical cream), no treatment, or with other active interventions. In several trials, all subjects received an active baseline intervention (e.g. EMLA cream or DPNB) prior to administration of the study intervention (Butler O'Hara 1998; Kaufman 2002; Stang 1997).
Risk of bias in included studies
All of the studies included in this systematic review were described as RCTs. However, fifteen of the study reports provided insufficient information or described inadequate procedures for assurance of blinding of randomisation (see Table ‐ Characteristics of Included Studies). Nine were double‐blind for delivery of all interventions (Howard 1994; Howard 1999; Joyce 2001; Macke 2001; Mudge 1989; Taddio 1997; Weatherstone 1993; Woodman 1999; Zolnoski 1993). Some studies compared interventions which could not be masked, for example, block techniques (Masciello 1990; Newton 1999; Spencer 1992). Partial blinding was achieved in several trials through inclusion of a sham or placebo group (Arnett 1990; Blass 1991 A; Holve 1983; Kass 2001; Kaufman 2002; Lander 1997; Stang 1988 A; Stang 1997). Blinding was occasionally achieved on a temporary basis during baseline assessments (Butler O'Hara 1998; Holliday 1999). There was considerable methodologic diversity between the included studies. For example, there was variation between all of the trials as to what constituted the circumcision "procedure". In one trial (Williamson 1983), outcome data were reported for an undefined three minute "dissection period". In other trials, data were reported for each of multiple steps of a standardized procedure (Benini 1993; Hardwick Smith 1998; Herschel 1998; Lander 1997; Woodman 1999), or reported as a single summary statistic for the entire procedure (Taddio 1997). Other authors did not describe any details of the circumcision procedure followed for the trial (Blass 1991 A; Holliday 1999; Maxwell 1987; Stang 1988 A; Weatherstone 1993). In general, not enough information was provided by authors to be certain that outcome results were directly comparable across studies, as the events that constituted the procedure may not have been equivalent.
There were differences within the group of trials of DPNB (the most frequently studied intervention) in length of time fasting prior to surgery, anaesthetic dose, wait time after anaesthetic administration, and in type of surgical clamp used. In some cases, a single operator performed all circumcisions (Butler O'Hara 1998; Hardwick Smith 1998; Howard 1994), in others, the circumcisions were performed by a number of different operators (Howard 1999; Macke 2001; Stang 1997). Differences in operator technique or in the circumcision procedure could have effected outcome results. For most of the trials, subjects were required to fast prior to the surgery, however, the fasting period varied between trials from 30 ‐ 90 minutes (Arnett 1990; Blass 1991 A; Herschel 1998; Kurtis 1999 A; Maxwell 1987) to 2 ‐ 4 hours (Butler O'Hara 1998; Howard 1994; Kaufman 2002; Masciello 1990). Hunger could have influenced outcomes such as duration of infant crying or other behavioral responses. In a number of studies, subjects were offered pacifiers (Holliday 1999; Howard 1994; Howard 1999; Kurtis 1999 A; Mohan 1998; Spencer 1992; Stang 1997) although pacifiers were not the study intervention. In one trial, all subjects were offered sugar pacifiers (Butler O'Hara 1998). The potential effect of NNS on the outcomes measured in the trials providing pacifiers was not addressed in the reports.
Effects of interventions
ACTIVE VERSUS PLACEBO OR NO TREATMENT COMPARISONS
Penile block interventions
Dorsal penile nerve block
Fourteen trials compared dorsal penile nerve block (DPNB) to no treatment or placebo (sham injection). A total of 592 infants were included. Three trials employed pain scores (Metagraph 01.01) as an outcome measure (Arnett 1990; Holliday 1999; Kass 2001). These trials were not combined for meta‐analysis of effect on pain because the scores used are not similar in conceptual development or measurement technique. However, outcomes significantly favoured DPNB using all four scores reported: infant irritability score [MD ‐1.8, 95% CI ‐2.4 to ‐1.2], modified behavioral pain scale (MBPS) [MD ‐3.2 , 95% CI ‐4.5 to ‐1.9], Holliday's behaviour score [MD ‐8.8, 95% CI ‐11.1 to ‐6.5], and the crying component of the same behavioral score [MD ‐9.8, 95% CI ‐13 to ‐6.6]. Another behavioral measure, time crying, also significantly favoured the DPNB group [WMD ‐54 %, 95% CI ‐64 to ‐44; SMD ‐1.74, 95% CI ‐2.1 to ‐1.4; Metagraph 01.02; SMD displayed, WMD derived from SMD; data not shown].
Among the physiological measures, heart rate significantly favoured DPNB [WMD ‐ 35 bpm, 95% CI ‐41 to ‐30; SMD ‐1.6, 95% CI ‐1.8 to ‐1.3; I2 = 73%; Metagraph 01.03; ; SMD displayed, WMD derived from SMD; data not shown]. Oxygen saturation results also significantly favoured DPNB [WMD 3.2 %, 95% CI 2.7 to 3.7; I2 = 97%; Metagraph 01.06]. Results were heterogeneous, and one author reported the loss of large amounts of data (Herschel 1998). A single trial (Williamson 1983) reported results for transcutaneous oxygen saturation that also significantly favoured DPNB [MD 9.3 torr, 95% CI 1.8 to 16.9; Metagraph 01.07].
Respiratory rate (Metagraph 01.08) and serum B‐endorphin (Metagraph 01.12) were not significantly different. Systolic blood pressure was reported in two studies. The combined result was significant and favoured DPNB [WMD ‐9 mmHg, 95% CI ‐16 to ‐ 2; SMD ‐0.66, 95% CI ‐1.18 to ‐0.13; I2=92%; Metagraph 01.09; SMD displayed, WMD derived from SMD; data not shown] but the effect was not significant in the random effects model or when Maxwell 1987 was removed. The populations for these two trials were different. Maxwell 1987 recruited healthy newborns in the first few days of life, while Holliday 1999 enrolled low birthweight preterm infants. The preterm infants were cared for NICU and experience with other invasive procedures prior to circumcision may have affected their pain responses.
Serum cortisol (Metagraph 01.10) outcomes were reported in mg/dL, ug/dL and nmol/dL. Results were converted to nmol/dL using standard conversion factors and the outcomes expressed in these units were combined but were not significantly different. A single study (Kurtis 1999 A) reported salivary cortisol results and these were not significantly different.
In two studies (comparing DPNB to no treatment), authors did not report means and SDs. Williamson 1997 found significantly lower oxygen saturation and higher heart rates in the no treatment group during adhesion lysis and application of the surgical clamp (p< 0.001). There was a significant difference in duration of crying between the groups (p <0.001) with the DPNB group crying less. The second study found that the mean increase in heart rate and percent of time crying during circumcision was 50% less for infants in the DPNB group (p< 0.01) (Holve 1983). The DPNB group infants were more attentive to stimuli following circumcision, and were better able to quiet themselves when disturbed (Dixon 1984).
Ring block Two trials compared ring block to no treatment and included 65 subjects (Hardwick Smith 1998; Lander 1997). Percent time crying was significantly reduced in the ring block group [WMD ‐26.3%, 95% CI ‐38 to ‐15, SMD ‐1.25, 95% CI ‐1.82 to ‐0.69; I2 = 68%; Metagraph 02.01; SMD displayed, WMD derived from SMD; data not shown]. Only single studies reported other measures. In one (Lander 1997) heart rate significantly favoured the ring block group [MD ‐29 bpm, 95% CI ‐52 to ‐ 7; Metagraph 02.02]. Oxygen saturation (Metagraph 02.03) and respiratory rate (Metagraph 02.04) were reported by Hardwick Smith 1998 and were not significantly different.
Topical anaesthetics
EMLA
Six studies compared EMLA to placebo for a total 200 patients (Benini 1993; Joyce 2001; Lander 1997; Taddio 1997; Woodman 1999; Zahorodny 1998). Two studies measured infant behavioral responses using the same pain score, the Neonatal Facial Coding System (Grunau 1987). The trials used the same measure, but the researchers scored a different set of facial actions (see Additional Table 1), and calculated the summary pain score differently. In both summation techniques, a lower score indicated less facial action and less pain. When combined, the results significantly favoured EMLA [WMD ‐46.5, 95% CI ‐80.4 to ‐12.6; SMD ‐0.6, 95% CI ‐1.0 to ‐0.2; Metagraph 03.01; SMD displayed, WMD derived from SMD; data not shown].
Cry time was also significantly decreased with EMLA treatment [WMD ‐ 15.2 %, 95% CI ‐21 to ‐ 9.3; SMD ‐0.78, 95% CI ‐1.08 to ‐ 0.48; Metagraph 03.02; SMD displayed, WMD derived from SMD; data not shown]. One study (Joyce 2001) did not favour the EMLA treatment, but for this study cry time was measured from the start of circumcision until crying stopped or until 30 minutes elapsed. The other studies measured cry time by phases of the procedure or gave a summary value for the procedure and thus only time spent crying during circumcision surgery could be calculated.
Heart rate was significantly decreased for infants treated with EMLA [WMD ‐15 bpm, 95% CI ‐19 to ‐10; Metagraph 03.03]. The effect on oxygen saturation was not significant [WMD 0.9%, 95% CI ‐0.2 to 2.0; Metagraph 03.04], and heterogeneity was large (I2= 86%). Respiratory rate, systolic and diastolic blood pressure (Metagraphs 03.05, 03.06, 03.07) were not significantly different.
Lidocaine cream
Three trials compared topical lidocaine to placebo and included 115 patients (Mudge 1989; Weatherstone 1993; Woodman 1999). One study measured percentage of time spent in Brazelton behavioral state 6 (full cry) as a proxy for pain (Weatherstone 1993) and the results were insignificant [MD ‐8, 95% CI ‐23 to 7; Metagraph 04.01]. Cry time was significantly reduced [WMD ‐60 s, 95% CI ‐99 to ‐20; Metagraph 04.02] and favoured lidocaine. Heart rate was also significantly reduced [WMD ‐9 bpm, 95% CI ‐14 to ‐ 4; I2=12%; Metagraph 04.03]. A single study examined B‐endorphin levels, and these were significantly reduced for the group treated with lidocaine [MD ‐49 pg/mL, 95% CI ‐89 to ‐9; Metagraph 04.06]. One study (Mudge 1989) did not report standard deviations for oxygen saturation (Metagraph 04.04) and respiratory rate (Metagraph 04.05) and these could not be calculated from the information available. However, the direction of results favoured treatment with lidocaine. Oxygen saturation results for another study (Woodman 1999) were not significantly different.
Oral sucrose/dextrose
Eight trials compared sugar solutions to water and/or no treatment and included 360 subjects (Blass 1991 A; Herschel 1998; Kass 2001; Kaufman 2002; Stang 1997; Zahorodny 1998; Zahorodny 1999; Zolnoski 1993). A variety of concentrations (24 to 50%) and volumes (1.5 to 10 ml) of sucrose or dextrose were tested. Two studies measured pain scores (Kass 2001; Stang 1997). The results were not combined because the measures are not similar in conceptual development or measurement technique. For example, distress scores (Stang 1997) ranging from 0 to 3 indicated no crying to sustained cry respectively. The modified behavioral pain scale (MBPS) scores (Kass 2001) ranged from 0 to 10 and incorporated ratings for facial expression, crying and body movements. Results using the behavioral distress score significantly favoured sucrose [MD ‐0.7 units, 95% CI ‐1.1 to ‐0.3], while the MBPS results were not significantly different (Metagraph 05.01).
Cry time results were not significantly different overall [WMD ‐ 1.3 %, 95% CI ‐5.8 to ‐8.3; SMD 0.07, 95% CI ‐0.31 to 0.44; I2 = 78%; Metagraph 05.02; SMD displayed, WMD derived from SMD; data not shown]. Individual results from five trials were inconsistent in direction. Zahorodny 1998 reported means only and SDs were substituted from another study using the same intervention and same outcome measure. One study (Kaufman 2002) reported a different measure of cry time. They averaged time spent crying in 10 second intervals, then took the cumulative average of that for each group. In this study, cry time was statistically significant and favoured the sucrose group (56 vs 86 s; P=0.0001). Zahorodny 1999 did not report means or standard deviations, but did report that both the sucrose and the water group cried much less than the no treatment group (p<0.001), and that subjects receiving the sucrose pacifier cried the least (p<.03). The sucrose and water groups in this trial also had smaller increases in heart rate compared to those receiving no intervention (p<.017). These authors did not comment on any differences between the sucrose group and the water group.
The effect on heart rate was not significant [WMD ‐4 bpm, 95% CI ‐9 to 2; Metagraph 05.03] overall in three trials. Heterogeneity was large (I2=55%) with two trials favouring the water treatment and one trial favouring the sucrose treatment. In two trials (Herschel 1998; Kass 2001) oxygen saturation was significantly greater in the sucrose group [WMD 1.8%, 95% CI 0.5 to 3.1; Metagraph 05.04] although heterogeneity was again large (I2=88%) and the random effects estimate was not significant [WMD 1.3%, 95% CI ‐2.7 to 5.2]. Serum cortisol (Metagraph 05.05) was measured in a single study (Stang 1997) and results were not significant.
The inconsistent results in these trials may be related to the volume and concentration of sucrose provided and to the sucrose delivery method. For example, in two studies the treatment group received a dose of 10 ml of 50% sucrose as the treatment intervention (Herschel 1998; Zahorodny 1999), while in two other studies, the treatment group received 2 ml of 50% sucrose (Kass 2001; Zahorodny 1998). The treatment groups in the other trials received 1.5 ml (Blass 1991 A), 2.3 ml (Zolnoski 1993) or an unspecified volume of 24% sucrose (Kaufman 2002; Stang 1997) respectively. The delivery method for the sugar solution also varied between studies. Five administered the sugar/water solution via a nipple/pacifier (Blass 1991 A; Herschel 1998; Kaufman 2002; Stang 1997; Zahorodny 1999) thus providing the opportunity for non‐nutritive sucking. In one trial (Herschel 1998), the sucrose group had a nipple (and the opportunity for non‐nutritive sucking throughout the circumcision procedure), while the no treatment control group did not receive a pacifier at all. In two studies, the sugar solution was delivered using oral syringes (Kass 2001; Zolnoski 1993). In one trial, the method of delivery was not specified (Zahorodny 1998).
Oral analgesics
Acetaminophen
Two trials compared acetaminophen to placebo with a total of 104 patients (Howard 1994; Macke 2001). The studies employed two different pain scales, and the results were not combined because the measures are not similar in conceptual development or measurement technique. Howard 1994 used a comfort score that measures 10 behaviours (sleep, facial expression, motor activity, tone, etc.) to arrive at a composite score of 0 to 20. The lower the score, the more uncomfortable the infant. Macke 2001 used the Nursing Child Assessment Feeding Scale (NCAFS) which measures mother‐infant feeding interactions using 76 behavioral items based on the concepts of synchronism and adaptation. Lower scores on the NCAFS indicate less positive responses on the part of the infant. Results using the post‐operative comfort score were not significant, but the total infant scores on the NCAFS were significant and favoured acetaminophen [MD 4.0, 95% CI 1.0 to 7.1; Metagraph 06.01]. All other outcomes (cry time, heart rate, respiratory rate Metagraphs 06.02, 06.03, 06.04) were not statistically significant.
ACTIVE VERSUS ACTIVE TREATMENT COMPARISONS
DPNB versus EMLA
Three studies compared DPNB to EMLA for a total of 139 patients (Butler O'Hara 1998; Howard 1999; Lander 1997). Two studies measured different pain scores (Metagraph 07.01). The results were not combined because of conceptual and measurement differences between the scales. The Neonatal Infant Pain Scale (NIPS) consists of 6 behavioral components with a composite score of 0 to 6 based on facial expression, crying, breathing pattern, body movement and arousal. The behavioral distress score measures crying on a scale of 0 (no crying) to 3 (sustained crying). Lower scores indicate less pain for both measures. Results using both scales were statistically significant and favoured DPNB; NIPS [MD ‐2.5, 95% CI ‐3.3 to ‐1.7]; behavioral distress score [MD ‐0.3, 95% CI ‐0.5 to ‐0.03].
Cry time was measured in a single study and was not significantly different [MD ‐10%, 95% CI ‐30 to 10; Metagraph 07.02]. Heart rate was significantly reduced for the DPNB group [WMD ‐17 bpm, 95% CI ‐23 to ‐11; Metagraph 07.03] but heterogeneity was large (I2=93%). The random effects estimate was not statistically significant. Butler O'Hara 1998 had a large mean difference [MD ‐40 bpm, 95% CI ‐51 to ‐29 ]; when this study was removed, heterogeneity was absent and the overall fixed effects WMD was no longer significant [WMD ‐7 bpm, 95% CI ‐14 to 0.5]. The large heterogeneity may be related to differences in the characteristics of the study subjects. Infants enrolled in the Butler O'Hara 1998 trial were born prematurely and hospitalised in the neonatal intensive care unit (NICU). Postnatal age was 3 ‐ 105 days by the time of circumcision (but less than 28 days after reaching 40 weeks corrected gestational age). Exposure to invasive treatments during their NICU stay may have caused the infants to become sensitized and thus respond differently than infants in the other two trials who were healthy newborns in the first few days of life. Respiratory rate (Metagraph 07.05), measured by a single study, was not significantly different.
DPNB versus sucrose
Two trials compared DPNB to sucrose for 127 patients. In one trial, pain was measured using the modified behavioral pain scale (MPBS) (Kass 2001) and the results significantly favoured DPNB [MD ‐3.2, 95% CI ‐4.7 to ‐1.8; Metagraph 08.01]. Cry time was measured in one trial and significantly favoured the DPNB group [MD ‐166 s, 95% CI ‐211 to ‐121; Metagraph 08.02]. Heart rate also significantly favoured DPNB [WMD ‐27 bpm, 95% CI ‐33 to ‐20; Metagraph 08.03]. Heterogeneity was large (I2=94%) however, both trials measuring heart rate favoured the DPNB group. The effect on oxygen saturation (Metagraph 08.04) was not significant, heterogeneity was large (I2=96%), and the individual trial estimates were not consistent in direction of effect. The authors of one study (Herschel 1998) reported that a significant amount of oxygen saturation data (measured using pulse oximetry) was lost due to excessive motion. Also of note, the dose and delivery method of the sugar solution differed between the two studies. In one study (Kass 2001) subjects received 2 ml of 50% dextrose by oral syringe. In the other (Herschel 1998), subjects received up to 10 ml of 50% sucrose by nipple and had a pacifier throughout the procedure.
DPNB versus ring block
One trial compared DPNB to ring block (Lander 1997) and included 27 patients. Results for cry time and heart rate were not significantly different between the groups (Metagraphs 09.01, 09.02).
DPNB versus local block
A single trial compared DPNB to local block using 1% lidocaine (Masciello 1990) and included 20 patients. Local block was performed by injecting lidocaine subcutaneously into the foreskin at the 10 and 2 o'clock positions at the level of the corona. Results for serum cortisol significantly favoured the local block administration group [MD 306 nmol/dL, 95% CI 141 to 471; Metagraph 10.01].
Ring block versus EMLA
Ring block was compared to EMLA in a single trial that included 28 patients (Lander 1997). Results for heart rate [MD ‐3 bpm, 95% CI ‐20 to 14; Metagraph 11.01] and cry time [MD ‐16 %, CI ‐36 to 3; Metagraph 11.02] were not significantly different between the groups.
Buffered lidocaine DPNB versus lidocaine DPNB
Two trials compared buffered lidocaine DPNB to lidocaine DPNB and included 234 patients (Newton 1999; Stang 1997). In clinical trials with adult subjects, buffering lidocaine with sodium bicarbonate had shown potential to decrease the burning sensation of injection, and enhance the speed of anaesthesia. The results for all outcomes measured (behavioral distress score, cry time, heart rate, oxygen saturation and serum cortisol; Metagraphs 12.01, 12.02, 12.03, 12.04, 12.05) were not significantly different between the groups.
EMLA versus topical lidocaine
One trial compared EMLA to 30% topical lidocaine, and included 40 patients (Woodman 1999). Cry time and oxygen saturation (Metagraphs 13.01, 13.03) were not significantly different. Heart rate was significant and favoured EMLA [MD ‐12 bpm, 95% CI ‐19 to ‐4; Metagraph 13.02].
EMLA versus sucrose
Two studies (Mohan 1998; Zahorodny 1998) compared EMLA to sucrose (67 patients). Cry time, heart rate, oxygen saturation (Metagraphs 14.01, 14.02, 14.03) were not significant. Systolic and diastolic blood pressures mean differences could not be calculated because no standard deviations were provided (Metagraphs 14.04, 14.05), but both means were larger in the sucrose group, indicating higher mean blood pressure.
EMLA versus music
A small pilot study (Joyce 2001) compared EMLA to music, and included 12 patients. None of the outcome results (cry time, heart rate, oxygen saturation, respiratory rate; Metagraphs 15.01, 15.02, 15.03, 15.04) were significantly different.
ENVIRONMENTAL COMPARISONS
Music versus no treatment
Three studies compared the provision of music or other soothing sounds during the circumcision procedure (Joyce 2001; Marchette 1989; Marchette 1991). In one trial that included 12 patients (Joyce 2001) the effect of the intervention on the outcomes of cry time, heart rate, oxygen saturation and respiratory rate (Metagraphs 16.01, 16.02, 16.03, 16.04) was not significant. In a second study, music was compared with intrauterine sounds and no treatment (Marchette 1989). Although 103 infants were randomised, 45 records were deleted from analysis due to missing data or prolonged circumcisions related to physician training. The researchers did not report standard deviations, but they did report that during all steps of the circumcision procedure in which infants were touched with surgical instruments the interventions did not offset pain as indicated by heart rate, systolic blood pressure, facial expression, and behavioral state outcomes. In the third study (Marchette 1991) 121 infants were randomised to six groups and received either classical music, intrauterine sounds, a pacifier, music and a pacifier, intrauterine sounds and a pacifier, or no treatment. The researchers did not report means and standard deviations but they did state that the interventions tested did not greatly reduce circumcision pain as assessed by heart rate, blood pressure, transcutaneous oxygen saturation, and time crying.
COMPLICATIONS/ADVERSE EFFECTS Ten studies reported adverse effects (see Additional Tables ‐ Table 8). Adverse effects including gagging, choking, and emesis were reported in untreated groups, while DPNB groups exhibited minor bleeding, swelling and hematoma at the block injection site post‐circumcision. EMLA use was associated with erythema and minor skin pallor. In one study (Holliday 1999), two subjects who received EMLA had redness and blistering of the foreskin, leading to closure of the EMLA arm of the study. Methaemoglobin levels were measured in two trials of EMLA and found to be within normal limits (Lander 1997; Taddio 1997). All adverse effects of pain interventions were reported to be transient in nature and were not considered serious. Several authors reported on the questionable clinical utility of topical anaesthetic interventions (Herschel 1998; Howard 1999; Lander 1997) given the dexterity required to apply the creams properly and the lengthy application time.
8. Trials reporting adverse effects.
| Study ID | intervention(s) | adverse effects |
| Arnett 1990 | 0.4 ml lidocaine DPNB (n=23) 0.4 ml saline DPNB (n=22) control (n=7) | lidocaine group ‐ 1 emesis treated with suction saline group ‐ 2 bleeding post‐procedure, 1 required suture control ‐ 1 bleeding post‐procedure controlled with pressure |
| Butler‐O'Hara 1998 | 0.5 ml LP cream (n=21) 0.7 ml ‐ 1.0 ml lidocaine DPNB + placebo cream (n=23) | DPNB group ‐ 10 hematoma; 1 penile edema on day 5 LP cream group ‐ 3 erythema |
| Holve 1983 & (primary study) Dixon 1984 | 0.8 ml lidocaine DPNB (n=15) 0.8 ml saline DPNB (n=8) control (n=8) | lidocaine group ‐ 1 small unilateral hematoma |
| Holliday 1999 | 0.8 ml lidocaine DPNB + placebo cream (n=19) placebo cream (n=19) original protocol included LP cream group (n=12) | LP cream group ‐ 2 redness and blistering of foreskin, LP cream group discontinued |
| Lander 1997 | 2 g LP cream (n=15) placebo cream (n=12) 0.8 ml lidocaine DPNB (n=14) 0.8 ml lidocaine RB (n=13) | placebo group ‐ 1 apnea and emesis, 1 choking and apnea |
| Newton 1999 | 0.8 ml lidocaine DPNB (n=92) 0.8 ml buffered lidocaine DPNB (n=102) | lidocaine group ‐ 4 had minor bleeding buffered lidocaine group ‐ 6 had minor bleeding |
| Stang 1988 | 0.8 ml lidocaine DPNB (n=20) 0.8 ml saline DPNB (n=20) control (n=20) | occasional insignificant bleeding ‐ groups and numbers not specified |
| Taddio 1997 | 1 g LP cream (n=29) 1 g placebo cream (n=30) | LP cream group ‐ 12 minor foreskin pallor, 1 mild edema placebo group ‐ 4 minor foreskin pallor |
| Williamson 1997 | lidocaine DPNB (n=20) control (n=10) | DPNB group ‐ 9 bleeding, 12 swelling, 1 erythema control group ‐ 5 bleeding, 5 swelling, 1 hematoma, 3 erythema |
| Zolnoski 1993 | 2.4 ml 24% sucrose (n=10) 2.4 ml water (n=10) | sucrose group ‐ 1 gagging water group ‐ 2 regurgitation after circumcision |
SUBGROUP AND SENSITIVITY ANALYSES
We examined two subgroups: length of wait time after penile block interventions (a priori) and choice of clamp for all procedures (post‐hoc) on the most frequently reported outcome heart rate. One study compared different lengths of wait time and two anaesthetics (Spencer 1992) but did not report means and SDs. The authors did report that DPNB groups that received either anaesthetic exhibited decreased pain responses compared to the control group. We made indirect (or between study) comparisons. Six trials comparing DPNB to no treatment prescribed and reported wait times. The trials with the longer wait time (>5 minutes) did not perform significantly better than short wait time trials (</=5 minutes) [Metagraph 01.04]. In fact, the probability under the null hypothesis was close to significant (P=0.09 vs P=0.65) when Maxwell 1987 was removed and favoured shorter wait times. A similar and statistically significant result was calculated when comparing wait times in DPNB vs EMLA (P=0.04; Metagraph 07.04). Using an indirect comparison, the Mogen clamp trial performed significantly better on reducing heart rate compared to the Gomco clamp trials when Maxwell 1987 was again removed (P=0.05 vs P=0.07) under the DPNB versus no treatment comparison (Metagraph 01.05). Sucrose dose (a priori) was not analysed because there were too few studies under the same comparison and not enough information was provided. Post‐hoc, we considered two other potential treatment effect size modifiers: control intervention and choice of pacifiers. For ethical considerations, use of saline DPNB in pain research was generally abandoned since the early 1990's. Among the included studies for this review, three used both saline DPNB treatment (sham) and no treatment control arms (Arnett 1990, Holve 1983, Stang 1988 A). In one study saline DPNB was used to blind comparison of lidocaine DPNB with another active intervention (Howard 1999). The researchers wanted to control for the effects of the injection and fluid volume compression on penile sensation. None of the studies found statistical differences between these control arms. In our review, the two control arms were displayed separately in the metagraphs when the data were reported separately in the referenced study (Stang 1988 A). Visually, we also see no difference. Other concerns for blinding involve placebo creams. One study (Mohan 1998) did not use a placebo cream and one study (Benini 1993) reported using petroleum jelly as a placebo for EMLA cream.
In nine trials pacifiers were made available to all patients (Butler O'Hara 1998; Holliday 1999; Howard 1994; Howard 1999; Kurtis 1999 A; Mohan 1998; Spencer 1992; Stang 1988 A; Stang 1997). In one (Butler O'Hara 1998) all infants were provided with sugar pacifiers although sucrose was not the intervention under study and its use may have affected results obtained on outcome measures. In another (Herschel 1998) only one out of the three study groups received a pacifier because it was used to deliver a sucrose intervention. At least two studies (Kass 2001; Zolnoski 1993) strictly prohibited the use of pacifiers and used oral syringes to deliver the sucrose intervention. The remaining studies did not report pacifier use. There were too few studies to compare within outcomes, and we could not identify obvious deviations with use or non‐use of pacifiers. Of mention, Blass 1991 A and Zahorodny 1999 both found that in a water via pacifier group, cry time was significantly reduced compared with the no treatment control group (P<0.001; P<0.001).
Discussion
This systematic review incorporates data from 35 trials enrolling 1997 neonates to examine a variety of interventions for circumcision pain relief. Although the results are generally applicable to current practice, the review identified a number of important limitations of the primary studies included in the review and thus the results should be interpreted with some caution. Sample size in the majority of the trials was small (total sample size was < or = to 80 in 32 out of 35 trials), and there were some differences in the characteristics of the study subjects. Butler O'Hara 1998 enrolled neonates from an NICU that were between 3 and 105 days postnatal age at the time of circumcision (although still less than 28 days after reaching 40 weeks corrected gestational age). Holliday 1999 enrolled low birthweight neonates aged 25 ‐ 27 days at circumcision. Each of these groups of subjects could have experienced numerous painful or invasive treatments during their stay in NICU prior to circumcision. Accordingly, their responses during circumcision, regardless of the intervention, could have been different from those of the healthy newborns that were recruited for the remainder of the trials.
All of the studies included in this review were described as randomised, but 15 of the trial reports did not include sufficient information or describe adequate procedures for assurance of blinding of randomisation. Nine of the trials were double‐blind for all interventions, but some interventions such as block technique could not be blinded. In six trials of DPNB, a standardized approach to the circumcision procedure was not described in the reports, making it impossible to tell whether every infant underwent exactly the same surgical process. The impact of this could be intensified within individual trials where more than one operator performed the circumcisions (e.g. Howard 1999, Macke 2001). Other differences that may have affected outcome results between trials of the same comparison include the variability in wait time after block administration, length of fasting prior to circumcision, provision of pacifiers or other non‐study interventions, and use of different surgical clamps. Finally, differences between trials in the structure of pain interventions were evident, especially in trials of oral sucrose where the dose and method of delivery varied substantially.
The studies included in this review reported on measurement of a variety of pain outcomes (physiological, behavioral, biochemical). Techniques and methods for measurement of outcomes were more dissimilar than similar across the trials, even within a single outcome variable (e.g. heart rate), and this presented significant challenges to combining outcome results. In particular, the dissimilarity in outcome measures severely limited the feasibility of combining pain scores across the included studies. None of the reports included in this review offered a definition of pain, and in general, the reports did not differentiate between the painful versus the distressing/stressful aspects of the circumcision procedure (e.g. removal of foreskin versus application of restraints). Reasons for selection of pain scores as outcome measures were not articulated in most cases, and among the included studies, a variety were used that differed in conceptual development and in measurement technique. Some pain scores were author‐devised measures with no reported psychometric testing (Arnett 1990; Holliday 1999; Weatherstone 1993), while others measured behavioral indicators that were not conceptually linked to the neonate's experience of pain (Dixon 1984; Macke 2001; Newton 1999; Stang 1988 A). Others were subjective in their measurement technique (Howard 1999; Stang 1997). In six trials, researchers employed validated pain scales developed specifically to measure neonatal pain (Benini 1993; Butler O'Hara 1998; Howard 1994; Joyce 2001; Kass 2001; Taddio 1997).
Sixteen trials included in this review either did not report outcome data, or did not report data in a format that could be analysed in this review. One of the strengths of this review was that we were able to obtain additional information for three trials. Where means and standard deviations were not available, data were imputed or derived from graphs contained in the reports, and missing standard deviations were either calculated from other summary statistics or substituted with singular or mean standard deviations from similar trials allowing us to maximize the data included under each comparison.
DPNB was identified as the most effective intervention and demonstrated decreases in time crying and heart rate that were statistically and clinically significant (time crying 54% less, heart rate 30 beats per minute less) when compared with placebo or no treatment. EMLA also reduced pain responses when compared with placebo but the differences in time crying (15% less) and heart rate (15 beats per minutes less) were not as large as those observed with DPNB. Topical lidocaine demonstrated statistically significant decreases in time crying (60 seconds less), heart rate (9 beats per minute less) and serum B‐endorphin levels (49 pg/ml less) compared to placebo. The issue of the statistical versus clinical significance of the outcome results was not discussed in any of the study reports, and no author identified a threshold for clinically significant (as opposed to statistically significant) intervention effects. It should be emphasized that none of the interventions examined in these trials completely eliminated pain responses to circumcision.
Ease of administration of the pain interventions will influence the applicability of the results of this review to current clinical practice. The relative ease of establishing the different penile blocks was not systematically evaluated, but it was suggested that the ring block technique is easier and safer because it eliminates the risk of injection of lidocaine into the dorsal vessels (Hardwick Smith 1998). A single study reported on use of local penile block (Masciello 1990) which appears to be similar in technique to ring block. Few adverse effects were reported with use of any of the penile blocks. EMLA and lidocaine topical anaesthetics are effective for circumcision pain when compared with placebo or no treatment, but their use may be precluded because of difficulties in application and the time required for maximum anaesthetic effect. Adverse effects such as transient skin reactions were reported but not considered serious, and methaemoglobin levels, when measured, were within normal range.
Authors' conclusions
Implications for practice.
Circumcision is a painful procedure and routine or elective newborn circumcision is not recommended by either the American Academy of Pediatrics or the Canadian Paediatric Society. However, if circumcision is performed, the results of this review show that DPNB, RB and the topical anaesthetics EMLA and lidocaine cream can be recommended over no treatment for attenuation of circumcision pain. DPNB demonstrated the most consistent results, has been the most comprehensively studied, and was the most effective in terms of clinically significant reductions in pain responses. RB is also effective to reduce circumcision pain compared with placebo. The RB technique may be easier and safer to use because it eliminates the risk of injection of lidocaine into the dorsal vessels.
EMLA and lidocaine topical anaesthetics are effective for circumcision pain when compared with placebo or no treatment, but their use may be precluded because of difficulties in application and the time required for maximum anaesthetic effect. Adverse effects with EMLA use such as transient skin reactions were reported but not considered serious, and methaemoglobin levels, when measured, were within normal range. Topical anaesthetics are a less effective alternative to no treatment when expertise with penile blocks is not readily available.
Results for oral sucrose, oral analgesics and environmental modification interventions were either inconsistent or did not produce significantly different outcome results. These therapies cannot be recommended as treatments for circumcision pain.
None of the studied interventions completely eliminated the pain response to circumcision.
Circumcisions performed using the Mogen clamp take less time than is required using Gomco clamps. Shorter procedure time may reduce the total amount of pain experienced during circumcision, and may be important in terms of practitioner time to do the surgery.
Implications for research.
Future studies should compare two or more active interventions for pain relief ‐ a placebo or no‐treatment control group is no longer acceptable. The impact of different "wait times" on the effectiveness of penile blocks and the relative acceptability and ease of administration of DPNB versus RB for practitioners should be systematically investigated. Use of the Mogen clamp in combination DPNB and RB should be investigated further to identify an optimal target time for circumcision surgery and to maximize anaesthetic effect. Although sucrose cannot be recommended as an intervention for circumcision pain at this time, research to determine the optimal dose and delivery method and the effect of combining oral sucrose with other interventions and comfort measures (e.g. nonnutritive sucking) should be pursued.
Lidocaine block and topical anaesthetic interventions could be useful in other situations where neonates undergo acute procedural pain. The pain associated with chest tube insertion, lumbar puncture, insertion of percutaneous central lines and other procedures commonly performed on high risk neonates may be significantly reduced with use of an appropriately adapted lidocaine block technique or topical anaesthetics. Further research should be pursued to identify situations where this potential can be examined.
What's new
| Date | Event | Description |
|---|---|---|
| 28 October 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 2003 Review first published: Issue 3, 2004
| Date | Event | Description |
|---|---|---|
| 3 August 2005 | New search has been performed | This review updates the existing review "Pain relief for neonatal circumcision" which was published in The Cochrane Library Issue 3, 2004 (Brady‐Fryer 2004). The review has been updated to correct the numbers reported for total patients randomized for the included trials. Results of meta‐analyses were not effected except in one case, comparison 03.02 where the effect size changed from [WMD = 15.8%, 95% CI ‐20.8 to ‐6.8] to [WMD = 15.22%; 95% CI 21.08 to 9.36]. Abstract was changed to note that data from three (not four) trials of DPNB versus EMLA including 133 patients were subjected to meta‐analysis. No new trials were identified as a result of the most recent search. |
| 1 May 2004 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We are grateful to Dr. J. R Holman, Dr. C Johnston, and Dr. J. F. Keck for their willingness to provide us with additional data from their studies.
Data and analyses
Comparison 1. DPNB versus no treatment or sham.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 infant irritability score | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐1.80 [‐2.41, ‐1.19] |
| 1.2 modified behavioral pain scale (MBPS) | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐3.23 [‐4.54, ‐1.92] |
| 1.3 author‐created behavioural score | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐8.80 [‐11.08, ‐6.52] |
| 1.4 crying component of behavioural score | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐9.80 [‐12.98, ‐6.62] |
| 2 Cry time (by unit) | 6 | 211 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.73 [‐2.06, ‐1.40] |
| 2.1 in % | 5 | 163 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.67 [‐2.04, ‐1.29] |
| 2.2 in seconds | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.97 [‐2.67, ‐1.27] |
| 3 Heart rate (by unit) | 8 | 348 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐1.89, ‐1.38] |
| 3.1 in bpm | 3 | 135 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [0.00, ‐1.21] |
| 3.2 in bpm change‐from‐baseline | 3 | 135 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.47 [‐1.87, ‐1.08] |
| 3.3 in % change‐from‐baseline | 2 | 78 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.11 [‐2.72, ‐1.50] |
| 4 Heart rate (by wait time) | 7 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 wait time after anesthetic administration </= 5 min | 3 | 158 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐2.01, ‐1.27] |
| 4.2 wait time after anesthetic administration > 5 min | 3 | 93 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.50 [‐2.01, ‐0.99] |
| 4.3 wait time after anesthetic administration ‐ other wait time reported | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.98 [‐2.69, ‐1.28] |
| 5 Heart rate (by clamp) | 9 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Gomco | 8 | 316 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐1.87, ‐1.34] |
| 5.2 Mogen | 1 | 32 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.51 [‐3.46, ‐1.56] |
| 6 Oxygen saturation (by unit) | 6 | 293 | Mean Difference (IV, Fixed, 95% CI) | 3.21 [2.69, 3.73] |
| 6.1 in % | 4 | 165 | Mean Difference (IV, Fixed, 95% CI) | 5.48 [4.73, 6.23] |
| 6.2 in % change‐from‐baseline | 2 | 128 | Mean Difference (IV, Fixed, 95% CI) | 1.12 [0.40, 1.84] |
| 7 Transcutaneous oxygen saturation ‐ change from baseline | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 9.3 [1.75, 16.85] |
| 7.1 torr (TcpO2) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 9.3 [1.75, 16.85] |
| 8 Respiratory rate (by unit) | 3 | 86 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.50, 0.36] |
| 8.1 rpm | 1 | 38 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐1.32, ‐0.01] |
| 8.2 in % change‐from‐baseline | 2 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.39 [‐0.19, 0.96] |
| 9 Systolic blood pressure (by unit) | 2 | 68 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.66 [‐1.18, ‐0.13] |
| 9.1 in mmHg | 1 | 38 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.66, 0.61] |
| 9.2 in % change‐from‐baseline | 1 | 30 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.03 [‐2.97, ‐1.09] |
| 10 Serum cortisol (nmol/dL) 30 min post | 4 | 102 | Mean Difference (IV, Fixed, 95% CI) | ‐70.11 [‐142.12, 1.91] |
| 11 Salivary cortisol increase (ug/dL) from baseline to 30 min post | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐0.54 [‐1.08, ‐0.00] |
| 12 B‐endorphin (pmol/L) | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | 21.0 [‐73.45, 115.45] |
1.1. Analysis.
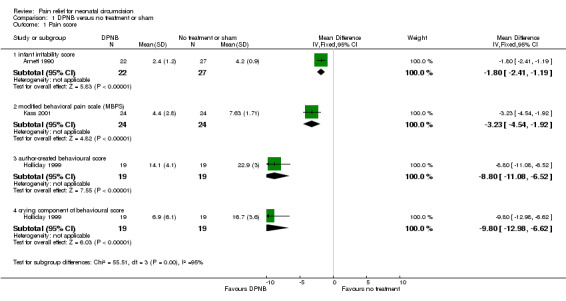
Comparison 1 DPNB versus no treatment or sham, Outcome 1 Pain score.
1.2. Analysis.
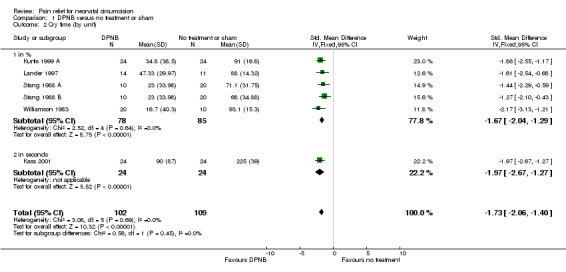
Comparison 1 DPNB versus no treatment or sham, Outcome 2 Cry time (by unit).
1.3. Analysis.
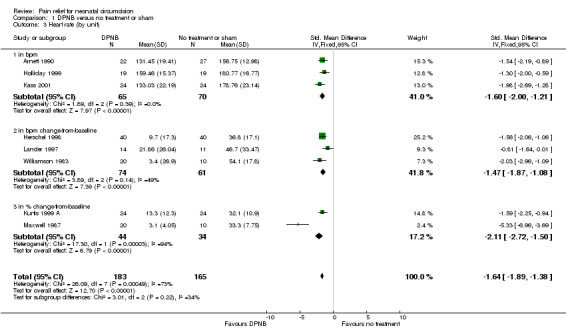
Comparison 1 DPNB versus no treatment or sham, Outcome 3 Heart rate (by unit).
1.4. Analysis.
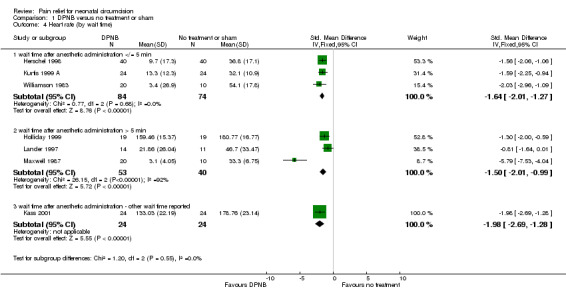
Comparison 1 DPNB versus no treatment or sham, Outcome 4 Heart rate (by wait time).
1.5. Analysis.
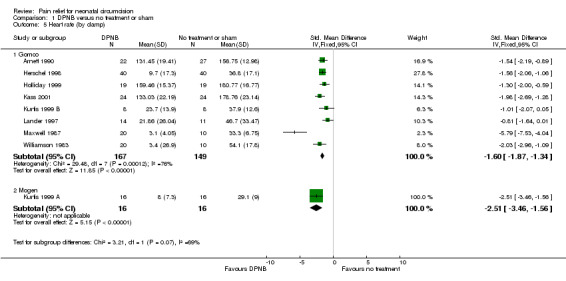
Comparison 1 DPNB versus no treatment or sham, Outcome 5 Heart rate (by clamp).
1.6. Analysis.

Comparison 1 DPNB versus no treatment or sham, Outcome 6 Oxygen saturation (by unit).
1.7. Analysis.
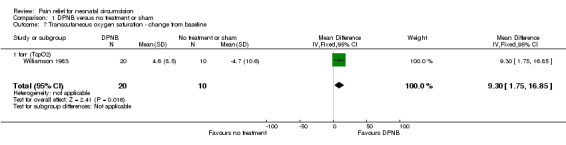
Comparison 1 DPNB versus no treatment or sham, Outcome 7 Transcutaneous oxygen saturation ‐ change from baseline.
1.8. Analysis.
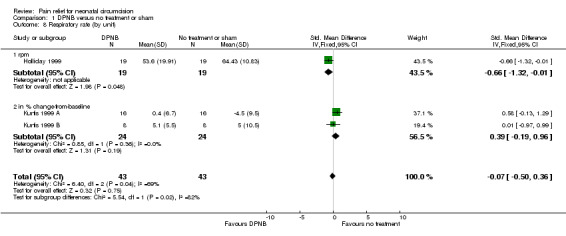
Comparison 1 DPNB versus no treatment or sham, Outcome 8 Respiratory rate (by unit).
1.9. Analysis.

Comparison 1 DPNB versus no treatment or sham, Outcome 9 Systolic blood pressure (by unit).
1.10. Analysis.

Comparison 1 DPNB versus no treatment or sham, Outcome 10 Serum cortisol (nmol/dL) 30 min post.
1.11. Analysis.
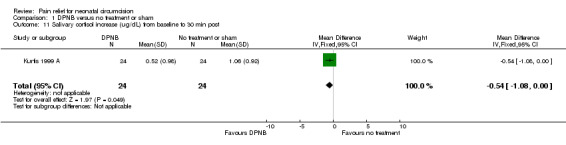
Comparison 1 DPNB versus no treatment or sham, Outcome 11 Salivary cortisol increase (ug/dL) from baseline to 30 min post.
1.12. Analysis.
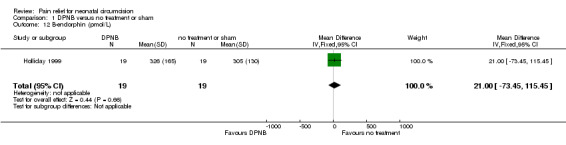
Comparison 1 DPNB versus no treatment or sham, Outcome 12 B‐endorphin (pmol/L).
Comparison 2. Ring block versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (by unit) | 2 | 63 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.25 [‐1.80, ‐0.69] |
| 1.1 in % | 1 | 23 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐2.01 [‐3.05, ‐0.98] |
| 1.2 in seconds | 1 | 40 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.94 [‐1.60, ‐0.29] |
| 2 Heart rate (bpm) change‐from‐baseline | 1 | 23 | Mean Difference (IV, Fixed, 95% CI) | ‐29.27 [‐52.94, ‐5.60] |
| 3 Oxygen saturation (%) change‐from‐baseline | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 3.84 [‐0.94, 8.62] |
| 4 Respiratory rate (rpm) change‐from‐baseline | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐5.69 [‐16.02, 4.64] |
2.1. Analysis.
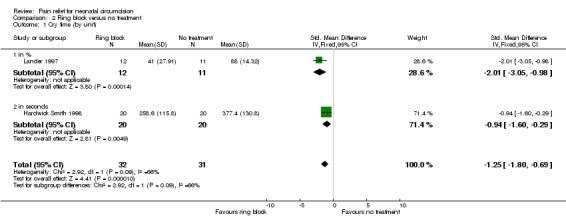
Comparison 2 Ring block versus no treatment, Outcome 1 Cry time (by unit).
2.2. Analysis.
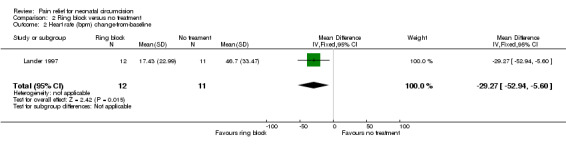
Comparison 2 Ring block versus no treatment, Outcome 2 Heart rate (bpm) change‐from‐baseline.
2.3. Analysis.

Comparison 2 Ring block versus no treatment, Outcome 3 Oxygen saturation (%) change‐from‐baseline.
2.4. Analysis.
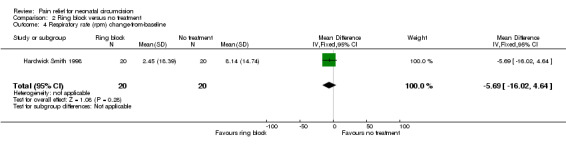
Comparison 2 Ring block versus no treatment, Outcome 4 Respiratory rate (rpm) change‐from‐baseline.
Comparison 3. EMLA versus placebo or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 2 | 86 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐1.02, ‐0.16] |
| 1.1 neonatal facial coding system (NFCS) | 1 | 27 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.82 [‐1.61, ‐0.03] |
| 1.2 NFCS ‐ author‐devised summary score | 1 | 59 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.49 [‐1.01, 0.03] |
| 2 Cry time (by unit) | 6 | 189 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.78 [‐1.08, ‐0.48] |
| 2.1 in % | 3 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.27, ‐0.33] |
| 2.2 in minutes | 2 | 51 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.57 [‐1.13, ‐0.01] |
| 2.3 percent increase in time crying | 1 | 59 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.95 [‐1.49, ‐0.41] |
| 3 Heart rate (by unit) | 5 | 143 | Mean Difference (IV, Fixed, 95% CI) | ‐14.59 [‐19.34, ‐9.84] |
| 3.1 in bpm | 3 | 78 | Mean Difference (IV, Fixed, 95% CI) | ‐15.80 [‐21.50, ‐10.10] |
| 3.2 in bpm change‐from‐baseline | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | ‐11.83 [‐20.42, ‐3.23] |
| 4 Oxygen saturation (%) | 3 | 78 | Mean Difference (IV, Fixed, 95% CI) | 0.90 [‐0.19, 2.00] |
| 5 Respiratory rate (rpm) | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | ‐4.31 [‐20.79, 12.17] |
| 6 Systolic blood pressure (mmHg) change‐from‐baseline | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐15.50, 9.50] |
| 7 Diastolic blood pressure (mmHg) change‐from‐baseline | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐5.0 [‐23.60, 13.60] |
3.1. Analysis.
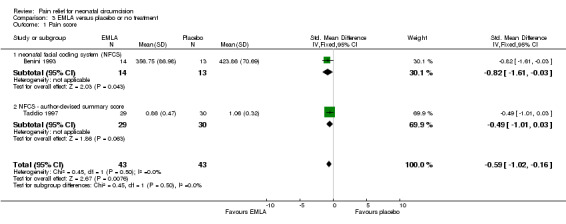
Comparison 3 EMLA versus placebo or no treatment, Outcome 1 Pain score.
3.2. Analysis.
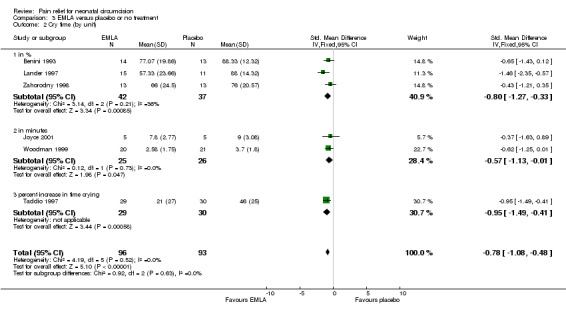
Comparison 3 EMLA versus placebo or no treatment, Outcome 2 Cry time (by unit).
3.3. Analysis.
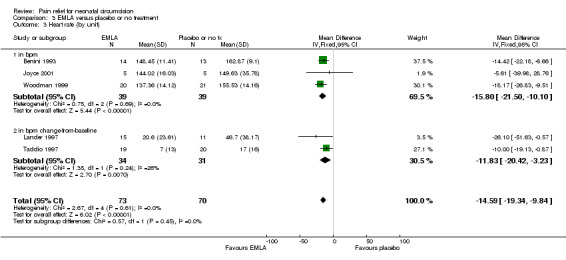
Comparison 3 EMLA versus placebo or no treatment, Outcome 3 Heart rate (by unit).
3.4. Analysis.
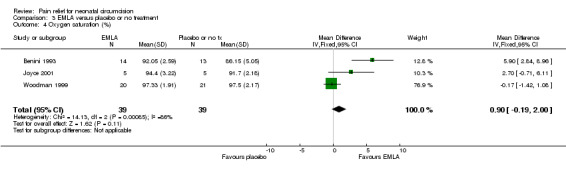
Comparison 3 EMLA versus placebo or no treatment, Outcome 4 Oxygen saturation (%).
3.5. Analysis.
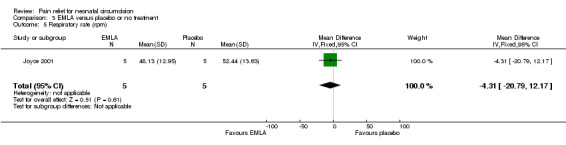
Comparison 3 EMLA versus placebo or no treatment, Outcome 5 Respiratory rate (rpm).
3.6. Analysis.
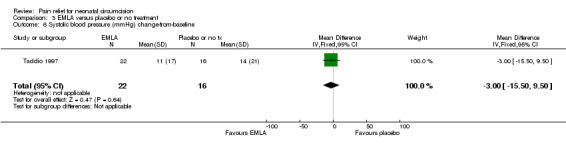
Comparison 3 EMLA versus placebo or no treatment, Outcome 6 Systolic blood pressure (mmHg) change‐from‐baseline.
3.7. Analysis.
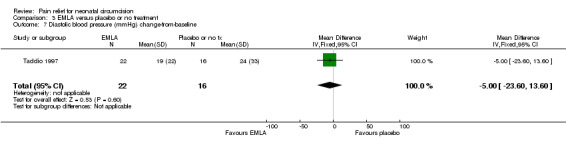
Comparison 3 EMLA versus placebo or no treatment, Outcome 7 Diastolic blood pressure (mmHg) change‐from‐baseline.
Comparison 4. Topical lidocaine versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 % change‐ from‐baseline in time spent in Brazelton state 6 (full cry) | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐8.0 [‐22.90, 6.90] |
| 2 Cry time (s) | 2 | 85 | Mean Difference (IV, Fixed, 95% CI) | ‐59.75 [‐99.14, ‐20.36] |
| 3 Heart rate (bpm) | 2 | 85 | Mean Difference (IV, Fixed, 95% CI) | ‐9.20 [‐14.32, ‐4.07] |
| 4 Oxygen saturation (%) | 2 | 85 | Mean Difference (IV, Fixed, 95% CI) | ‐0.5 [‐1.75, 0.75] |
| 5 Respiratory rate (rpm) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 B‐endorphin (pg/mL) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐49.0 [‐88.73, ‐9.27] |
4.1. Analysis.
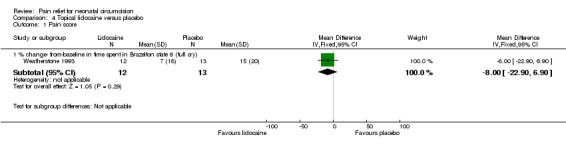
Comparison 4 Topical lidocaine versus placebo, Outcome 1 Pain score.
4.2. Analysis.

Comparison 4 Topical lidocaine versus placebo, Outcome 2 Cry time (s).
4.3. Analysis.
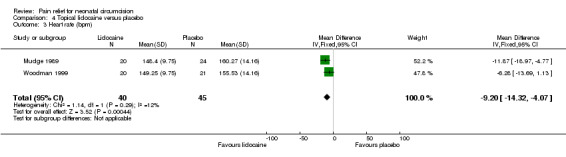
Comparison 4 Topical lidocaine versus placebo, Outcome 3 Heart rate (bpm).
4.4. Analysis.
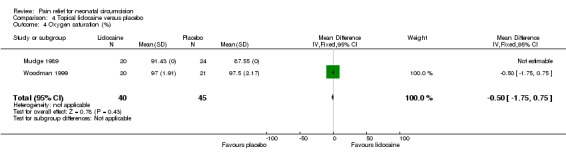
Comparison 4 Topical lidocaine versus placebo, Outcome 4 Oxygen saturation (%).
4.5. Analysis.
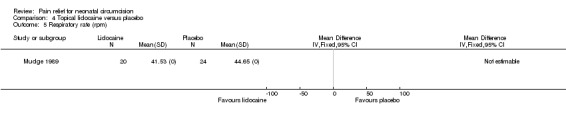
Comparison 4 Topical lidocaine versus placebo, Outcome 5 Respiratory rate (rpm).
4.6. Analysis.
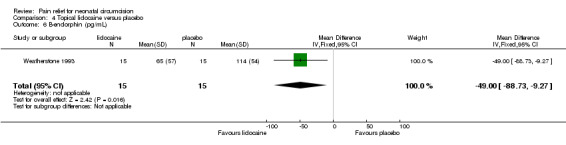
Comparison 4 Topical lidocaine versus placebo, Outcome 6 B‐endorphin (pg/mL).
Comparison 5. Sucrose versus water or no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 behavioral distress score | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.08, ‐0.26] |
| 1.2 modified behavioral pain scale (MBPS) | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.11, 1.11] |
| 2 Cry time (by unit) | 5 | 123 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.31, 0.44] |
| 2.1 in % | 3 | 56 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.63 [‐1.22, ‐0.05] |
| 2.2 in seconds | 2 | 67 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.56 [0.07, 1.04] |
| 3 Heart rate (by unit) | 3 | 146 | Mean Difference (IV, Fixed, 95% CI) | ‐3.46 [‐8.98, 2.07] |
| 3.1 in bpm | 2 | 67 | Mean Difference (IV, Fixed, 95% CI) | 2.16 [‐5.45, 9.78] |
| 3.2 in bpm change‐from‐baseline | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐9.70 [‐17.72, ‐1.68] |
| 4 Oxygen saturation (by unit) | 2 | 126 | Mean Difference (IV, Fixed, 95% CI) | 1.82 [0.51, 3.13] |
| 4.1 in % | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐3.07, 1.41] |
| 4.2 in % change‐from‐baseline | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | 3.2 [1.59, 4.81] |
| 5 Serum cortisol (nmol/dL) 30 min post | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 68.90 [‐53.93, 191.73] |
5.1. Analysis.
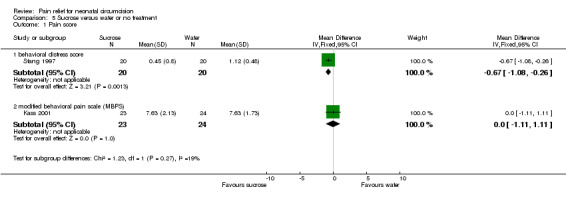
Comparison 5 Sucrose versus water or no treatment, Outcome 1 Pain score.
5.2. Analysis.
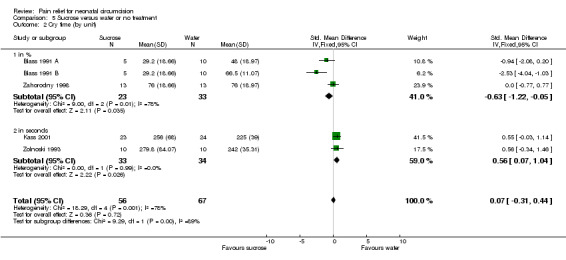
Comparison 5 Sucrose versus water or no treatment, Outcome 2 Cry time (by unit).
5.3. Analysis.

Comparison 5 Sucrose versus water or no treatment, Outcome 3 Heart rate (by unit).
5.4. Analysis.

Comparison 5 Sucrose versus water or no treatment, Outcome 4 Oxygen saturation (by unit).
5.5. Analysis.

Comparison 5 Sucrose versus water or no treatment, Outcome 5 Serum cortisol (nmol/dL) 30 min post.
Comparison 6. Acetaminophen versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain / behavior score | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 comfort score ‐ change from baseline score at 30 min post | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.23, 1.63] |
| 1.2 Nursing Child Assessment Feeding Scale (NCAFS) ‐ total infant score | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 4.00 [0.95, 7.05] |
| 2 Cry time (%) | 2 | 104 | Mean Difference (IV, Fixed, 95% CI) | ‐1.76 [‐8.26, 4.74] |
| 3 Heart rate (bpm) | 2 | 104 | Mean Difference (IV, Fixed, 95% CI) | 2.27 [‐2.89, 7.44] |
| 4 Respiratory rate (rpm) | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐3.73 [‐9.00, 3.54] |
6.1. Analysis.
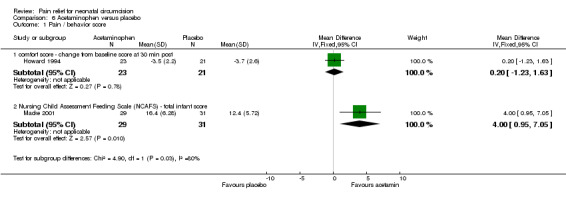
Comparison 6 Acetaminophen versus placebo, Outcome 1 Pain / behavior score.
6.2. Analysis.
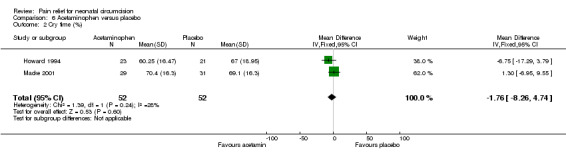
Comparison 6 Acetaminophen versus placebo, Outcome 2 Cry time (%).
6.3. Analysis.
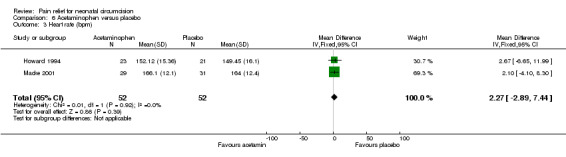
Comparison 6 Acetaminophen versus placebo, Outcome 3 Heart rate (bpm).
6.4. Analysis.
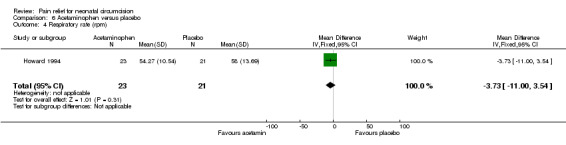
Comparison 6 Acetaminophen versus placebo, Outcome 4 Respiratory rate (rpm).
Comparison 7. DPNB versus EMLA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 neonatal infant pain scale (NIPS) | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐2.5 [‐3.29, ‐1.71] |
| 1.2 behavioral distress score | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.53, ‐0.03] |
| 2 Cry time (%) | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐29.74, 9.74] |
| 3 Heart rate (by unit) | 3 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐16.85 [‐22.69, ‐11.00] |
| 3.1 in bpm | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐7.90 [‐15.52, ‐0.28] |
| 3.2 in bpm change‐from‐baseline | 2 | 73 | Mean Difference (IV, Fixed, 95% CI) | ‐29.61 [‐38.71, ‐20.51] |
| 4 Heart rate by wait time | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 wait time after anesthetic administration </= 5 min | 2 | 104 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐1.05 [‐1.48, ‐0.62] |
| 4.2 wait time after anesthetic administration > 5 min | 1 | 29 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.68, 0.78] |
| 5 Respiratory rate (rpm) | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.90 [‐7.47, 1.67] |
7.1. Analysis.
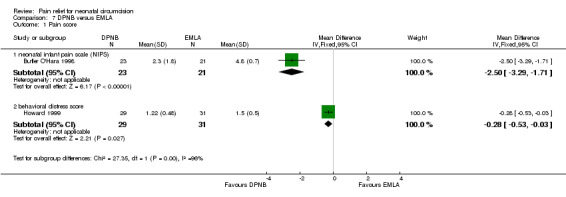
Comparison 7 DPNB versus EMLA, Outcome 1 Pain score.
7.2. Analysis.

Comparison 7 DPNB versus EMLA, Outcome 2 Cry time (%).
7.3. Analysis.
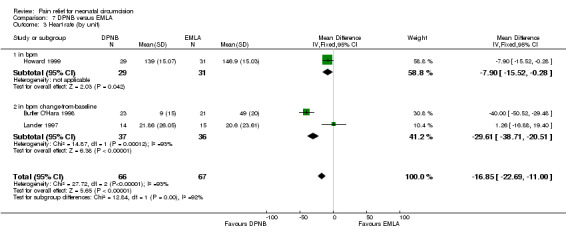
Comparison 7 DPNB versus EMLA, Outcome 3 Heart rate (by unit).
7.4. Analysis.
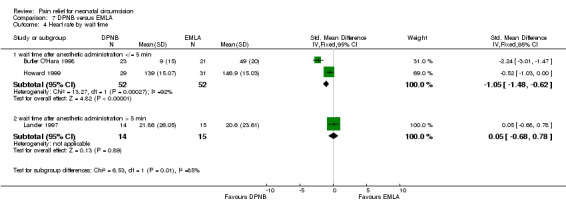
Comparison 7 DPNB versus EMLA, Outcome 4 Heart rate by wait time.
7.5. Analysis.

Comparison 7 DPNB versus EMLA, Outcome 5 Respiratory rate (rpm).
Comparison 8. DPNB versus sucrose.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐3.23 [‐4.65, ‐1.81] |
| 1.1 modified behavioral pain scale | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐3.23 [‐4.65, ‐1.81] |
| 2 Cry time (s) | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐166.00 [‐210.54, ‐121.46] |
| 3 Heart rate (by unit) | 2 | 126 | Mean Difference (IV, Fixed, 95% CI) | ‐26.56 [‐33.36, ‐19.76] |
| 3.1 in bpm | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐49.08 [‐61.72, ‐36.44] |
| 3.2 in bpm change‐from‐baseline | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐17.40 [‐25.47, ‐9.33] |
| 4 Oxygen saturation (by unit) | 2 | 126 | Mean Difference (IV, Fixed, 95% CI) | 0.25 [‐0.78, 1.27] |
| 4.1 in % | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 3.85 [2.06, 5.64] |
| 4.2 in % change‐from‐baseline | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐2.75, ‐0.25] |
8.1. Analysis.
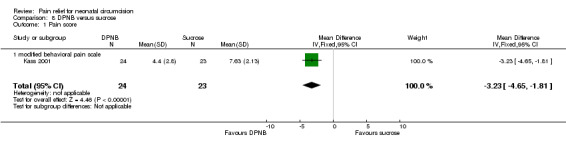
Comparison 8 DPNB versus sucrose, Outcome 1 Pain score.
8.2. Analysis.

Comparison 8 DPNB versus sucrose, Outcome 2 Cry time (s).
8.3. Analysis.
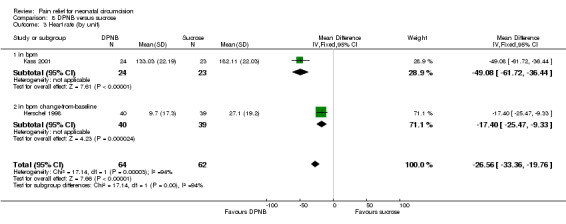
Comparison 8 DPNB versus sucrose, Outcome 3 Heart rate (by unit).
8.4. Analysis.
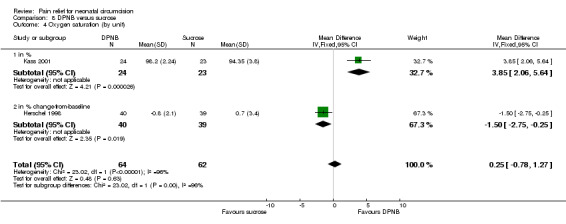
Comparison 8 DPNB versus sucrose, Outcome 4 Oxygen saturation (by unit).
Comparison 9. DPNB versus ring block.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (%) | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 6.33 [‐15.94, 28.60] |
| 2 Heart rate (bpm) change‐from‐baseline | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 4.43 [‐14.42, 23.28] |
9.1. Analysis.
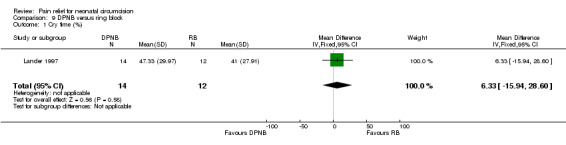
Comparison 9 DPNB versus ring block, Outcome 1 Cry time (%).
9.2. Analysis.
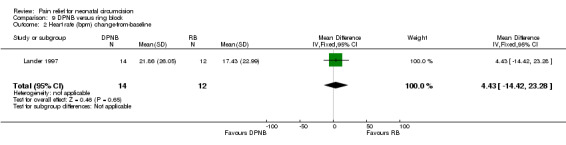
Comparison 9 DPNB versus ring block, Outcome 2 Heart rate (bpm) change‐from‐baseline.
Comparison 10. DPNB versus local block.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serum cortisol (nmol/dL) 30 min post | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 306.27 [141.33, 471.21] |
10.1. Analysis.

Comparison 10 DPNB versus local block, Outcome 1 Serum cortisol (nmol/dL) 30 min post.
Comparison 11. Ring block versus EMLA.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Heart rate (bpm) change‐from‐baseline | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | ‐3.17 [‐20.84, 14.50] |
| 2 Cry time (%) | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | ‐16.33 [‐36.15, 3.49] |
11.1. Analysis.

Comparison 11 Ring block versus EMLA, Outcome 1 Heart rate (bpm) change‐from‐baseline.
11.2. Analysis.

Comparison 11 Ring block versus EMLA, Outcome 2 Cry time (%).
Comparison 12. Buffered lidocaine DPNB versus plain lidocaine DPNB.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 behavioral distress score | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.30, 0.50] |
| 2 Cry time (%) | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | 9.0 [‐11.71, 29.71] |
| 3 Heart rate (bpm) | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | ‐4.20 [‐10.51, 2.11] |
| 4 Oxygen saturation (%) | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐0.87, 1.87] |
| 5 Serum cortisol (nmol/dL) 30 min post | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 35.80 [‐105.62, 177.22] |
12.1. Analysis.

Comparison 12 Buffered lidocaine DPNB versus plain lidocaine DPNB, Outcome 1 Pain score.
12.2. Analysis.
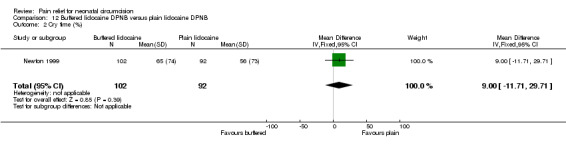
Comparison 12 Buffered lidocaine DPNB versus plain lidocaine DPNB, Outcome 2 Cry time (%).
12.3. Analysis.
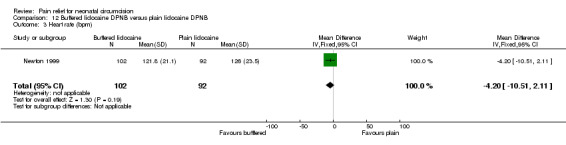
Comparison 12 Buffered lidocaine DPNB versus plain lidocaine DPNB, Outcome 3 Heart rate (bpm).
12.4. Analysis.
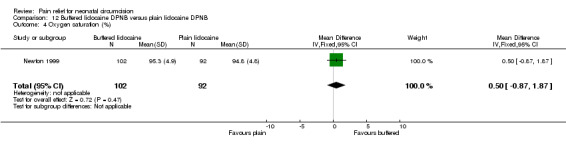
Comparison 12 Buffered lidocaine DPNB versus plain lidocaine DPNB, Outcome 4 Oxygen saturation (%).
12.5. Analysis.
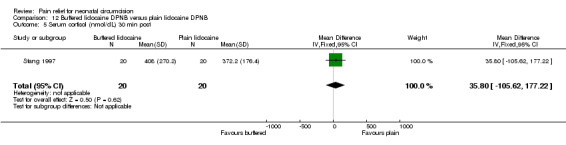
Comparison 12 Buffered lidocaine DPNB versus plain lidocaine DPNB, Outcome 5 Serum cortisol (nmol/dL) 30 min post.
Comparison 13. EMLA versus 30% topical lidocaine.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (s) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐17.0 [‐75.00, 41.00] |
| 2 Heart rate (bpm) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐11.88 [‐19.40, ‐4.36] |
| 3 Oxygen saturation (%) | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐1.44, 1.10] |
13.1. Analysis.
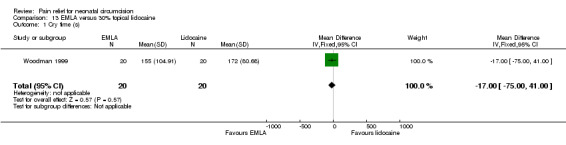
Comparison 13 EMLA versus 30% topical lidocaine, Outcome 1 Cry time (s).
13.2. Analysis.
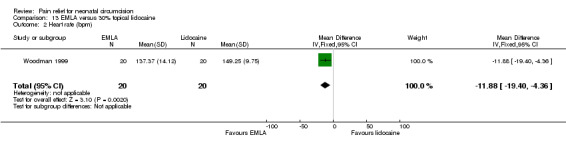
Comparison 13 EMLA versus 30% topical lidocaine, Outcome 2 Heart rate (bpm).
13.3. Analysis.
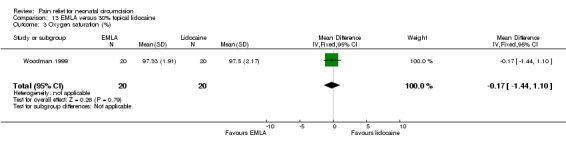
Comparison 13 EMLA versus 30% topical lidocaine, Outcome 3 Oxygen saturation (%).
Comparison 14. EMLA versus sucrose.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (%) | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐26.74, 6.74] |
| 2 Heart rate (bpm) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐9.35 [‐20.08, 1.38] |
| 3 Oxygen saturation (%) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | ‐0.82 [‐2.63, 0.99] |
| 4 Systolic blood pressure (mmHg) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Diastolic blood pressure (mmHg) | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
14.1. Analysis.
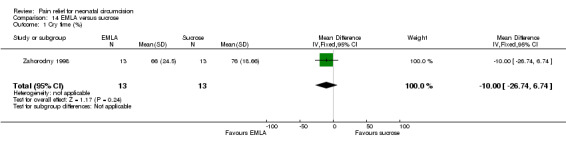
Comparison 14 EMLA versus sucrose, Outcome 1 Cry time (%).
14.2. Analysis.
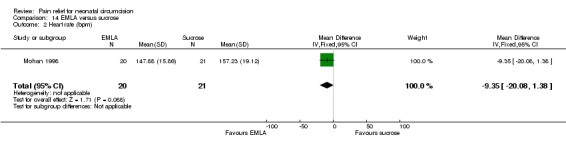
Comparison 14 EMLA versus sucrose, Outcome 2 Heart rate (bpm).
14.3. Analysis.
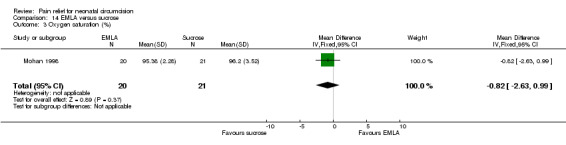
Comparison 14 EMLA versus sucrose, Outcome 3 Oxygen saturation (%).
14.4. Analysis.
Comparison 14 EMLA versus sucrose, Outcome 4 Systolic blood pressure (mmHg).
14.5. Analysis.

Comparison 14 EMLA versus sucrose, Outcome 5 Diastolic blood pressure (mmHg).
Comparison 15. EMLA versus music.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (min) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | 0.38 [‐3.68, 4.44] |
| 2 Heart rate (bpm) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | 2.31 [‐15.99, 20.61] |
| 3 Oxygen saturation (%) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐3.56, 3.94] |
| 4 Respiratory rate (rpm) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | 1.52 [‐13.60, 16.64] |
15.1. Analysis.
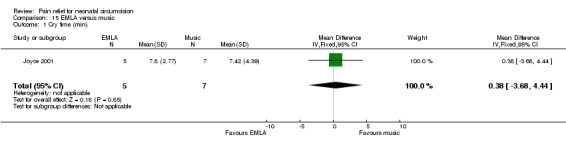
Comparison 15 EMLA versus music, Outcome 1 Cry time (min).
15.2. Analysis.

Comparison 15 EMLA versus music, Outcome 2 Heart rate (bpm).
15.3. Analysis.
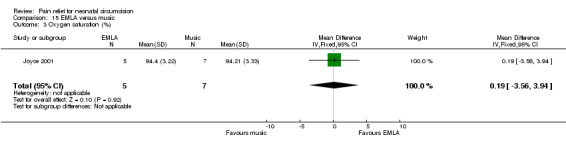
Comparison 15 EMLA versus music, Outcome 3 Oxygen saturation (%).
15.4. Analysis.
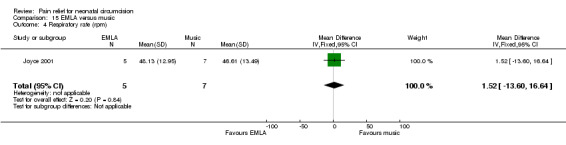
Comparison 15 EMLA versus music, Outcome 4 Respiratory rate (rpm).
Comparison 16. Music versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cry time (min) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | ‐1.58 [‐5.81, 2.65] |
| 2 Heart rate (bpm) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | ‐7.89 [‐41.37, 25.59] |
| 3 Oxygen saturation (%) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | 2.51 [‐0.62, 5.64] |
| 4 Respiratory rate (rpm) | 1 | 12 | Mean Difference (IV, Fixed, 95% CI) | ‐5.83 [‐21.41, 9.75] |
16.1. Analysis.
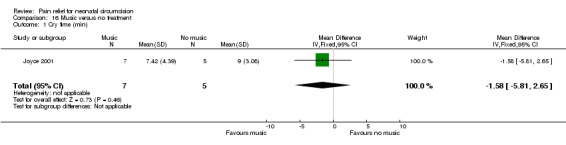
Comparison 16 Music versus no treatment, Outcome 1 Cry time (min).
16.2. Analysis.
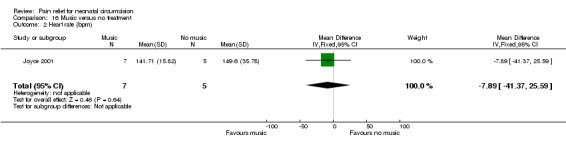
Comparison 16 Music versus no treatment, Outcome 2 Heart rate (bpm).
16.3. Analysis.
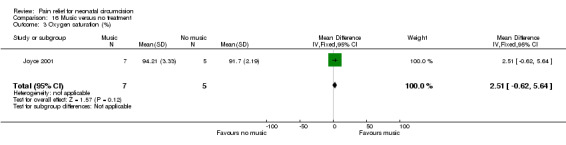
Comparison 16 Music versus no treatment, Outcome 3 Oxygen saturation (%).
16.4. Analysis.

Comparison 16 Music versus no treatment, Outcome 4 Respiratory rate (rpm).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Arnett 1990.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ no Blinding of outcome measurement ‐ can't tell | |
| Participants | 52 male NB; FT; BW > 2000 g; 5 min Apgar scores >/= 6 | |
| Interventions | 0.4 ml lidocaine DPNB (n=23) 0.4 ml saline DPNB (n=22) no treatment control (n=7) WT not reported; mean length for entire procedure was 4.4 minutes | |
| Outcomes | HR, infant irritability, O2sat | |
| Notes | ‐ no treatment control group added after study start; results for saline DPNB group and no treatment group were combined for analysis (n=29) ‐ data missing for 3 subjects (1 in each group) and cases deleted from analysis ‐ procedure not standardized ‐ lower dose lidocaine used (0.4 ml total) ‐ subjects fasted 90 minutes prior to circumcision ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Benini 1993.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ yes | |
| Participants | 28 male NB; FT; BW > 2500g; 5 min Apgar > 7; < 7 d age | |
| Interventions | 0.5 ml (0.5g) LP cream (n=14) 0.5 ml (0.5 g) petroleum jelly (n=14) applied and covered with occlusive dressing 45 ‐ 60 min prior | |
| Outcomes | HR, O2sat, % time crying, facial action | |
| Notes | ‐ 1 withdrawal from placebo group because infant not FT ‐ procedure standardized to 9 phases ‐ Gomco clamp ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Blass 1991 A.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ partial Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ yes | |
| Participants | 30 male NB, FT; 28 ‐ 54 h age; Apgars > 8 | |
| Interventions | 1.5 ml 24% sucrose by nipple 1.5 ml water by nipple no treatment control *comparison is sucrose versus water (placebo) number subjects per group not specified 3 min WT after intervention | |
| Outcomes | % time crying | |
| Notes | ‐ assumed distribution was equal (10/group) for data analysis ‐ procedure not standardized ‐ infants fasted for at least 1 hr prior ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Blass 1991 B.
| Methods | see Blass A | |
| Participants | see Blass A | |
| Interventions | * comparison is sucrose versus no treatment | |
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Butler O'Hara 1998.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ yes | |
| Participants | 50 male infants in NICU; >/= 34.5 weeks (post‐menstrual) at time of circumcision and stable for discharge participants were 3 ‐105 days age at time of circumcision | |
| Interventions | 0.5 ml (0.5g) LP cream (n=25) 0.7 ‐ 1.0 ml lidocaine DPNB + placebo cream (n=25) creams applied 60 min prior and covered with occlusive dressing 3 min WT after DPNB | |
| Outcomes | HR; RR; NIPS score (primary outcome) | |
| Notes | ‐ non‐randomized, no treatment group (n=20) also had data collected
‐ outcome data for 6 subjects (4 LP cream, 2 DPNB) lost due to technical difficulties
‐ infants fasted for 2 to 3 hours before circumcision
‐ all subjects had sugar pacifiers during procedure
‐ procedure standardized
‐ Plastibell clamp ‐ adverse effects reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Dixon 1984.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ can't tell Complete follow‐up ‐ yes Blinding of outcome measurement ‐ partial | |
| Participants | 31 male NB, FT, AGA, < 7 days age, > 2500 gm, 5 min Apgar > 7 | |
| Interventions | 0.8 ml lidocaine DPNB (n=15) 0.8 ml saline DPNB (n=8) no treatment control (n=8) 4 ‐ 5 min WT | |
| Outcomes | Brazelton Neonatal Assessment Scale | |
| Notes | ‐ Holve 1983 is primary study report ‐ circumcision procedure not standardized ‐ all circumcisions performed by single physician ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hardwick Smith 1998.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ no | |
| Participants | 40 male NB; FT; Apgar >/= 7; 6 hr ‐ 5 days age; fasting 30 ‐120 min prior; normal exam | |
| Interventions | 1.0 ml 5% lidocaine RB (n=20) no treatment control (n=20) 3 min WT | |
| Outcomes | HR; RR; O2sat; behavioral state; cry time | |
| Notes | ‐ O2sat not recorded in up to 50% of infants ‐ single operator performed all circumcisions ‐ Gomco clamp ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Herschel 1998.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ yes | |
| Participants | 120 male NB; FT; > 2500g; Apgar >/= 8 at 5 min; >/= 12 hr age | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=40) 10 ml 50% oral sucrose via nipple (n=40) no treatment control (n=40) 3 min WT for DPNB; 2 min WT for sucrose group | |
| Outcomes | HR; O2sat (%) | |
| Notes | ‐ 1 withdrawal from sucrose group, circumcision contraindicated ‐ O2 sat data missing ‐ 31% intervals control, 10% intervals DPNB, 8% sucrose ‐ infants fasted 30 min prior to circumcision ‐ sucrose group had nipple throughout procedure, other groups did not have pacifier ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Holliday 1999.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ can't tell | |
| Participants | 50 male preterm/low birthweight NICU patients, subjects weighed 1600 to 2500g at time of circumcision 25‐27 days age, 36 week GA at circumcision | |
| Interventions | 0.8 ml 1% lidocaine DPNB + placebo cream (n= 19) LP cream (n=12) (group enrollment stopped, excluded from data analyses) placebo cream (n=19) DPNB 5 min WT cream applied 1 hr prior and covered with occlusive dressing | |
| Outcomes | HR, RR, O2sat, systolic BP, behavioral score, serum B‐endorphin | |
| Notes | ‐ LP cream group discontinued due to redness and blistering of foreskin in 2 infants ‐ procedure not standardized ‐ all circumcisions performed by single operator ‐ pacifiers provided ‐ Gomco clamp ‐ no adverse effects reported for DPNB group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Holve 1983.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ partial Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 31 male NB; FT, < 7 days age, > 2500 gm, 5 min Apgar > 7 | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=15) 0.8 ml saline DPNB (n=8) no treatment control (n=8) 4‐5 min WT | |
| Outcomes | HR; % time crying per interval; clinical observation of anesthesia effectiveness (good, fair, poor) | |
| Notes | ‐ procedure standardized ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Howard 1994.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 44 male NB, healthy, AGA, FT, Apgars > 7, >/= 24 h age | |
| Interventions | acetaminophen 15 mg/kg/dose (n= 23) placebo (n= 21) given 2 hr prior and q 6H X 24 hr following | |
| Outcomes | HR; RR; cry time; post‐operative comfort score; feeding behavior pre/post | |
| Notes | ‐ infants fasted 2 ‐ 3 h prior to circumcision ‐ all had pacifiers ‐ procedure standardized ‐ single operator performed all circumcisions ‐ Gomco clamp ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Howard 1999.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ unclear Blinding of outcome measurement ‐ yes | |
| Participants | 62 male NB; healthy; AGA; FT | |
| Interventions | 1g LP cream + 0.8 ml saline DPNB (n=31) 0.8 ml 1% lidocaine DPNB + 1g placebo cream (n=31) 4 min WT for DPNB creams applied 1 hr prior and covered with occlusive dressing | |
| Outcomes | HR; RR; behavioral distress score | |
| Notes | ‐ 2 infants withdrawn (1 tachypnea, 1 parents withdrew consent) ‐ procedure standardized ‐ 3 operators performed the circumcisions ‐ all subjects had pacifiers ‐ Gomco clamp ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Joyce 2001.
| Methods | RCT; Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 23 male NB, FT; 5 min Apgar > 7; BW > 2500 g; age < 7 d | |
| Interventions | LP cream (1 ‐ 2 g) + music (n=6) LP cream + no music (n=5) placebo cream + music (n=7) placebo cream + no music (n=5) cream applied 1 hr prior and covered with occlusive dressing music started just prior to procedure and continued to 10 min post procedure | |
| Outcomes | HR, O2sat, cry duration; RR, Riley Infant pain scale, salivary cortisol, infant state | |
| Notes | ‐ pilot study ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Kass 2001.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ no Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 71 healthy male NB | |
| Interventions | lidocaine DPNB (n=24) 2ml D50W orally (n=23) 2 ml H2O orally (n=24) WT 2 to 6 min | |
| Outcomes | time cry (primary outcome); HR; O2sat ; modified behavioral pain scale | |
| Notes | ‐ additional data obtained from authors ‐ no pacifiers used ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kaufman 2002.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ partial Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 57 NB; healthy; male; FT; Apgar > 7 at 5 min | |
| Interventions | Mogen + water pacifier (15) Mogen + 24% sucrose pacifier (n=14) Gomco+ water pacifier (n=14) Gomco + 24% sucrose pacifier (n=14) | |
| Outcomes | time crying; grimacing, procedure length | |
| Notes | ‐ all subjects had EMLA cream applied between 1 and 3 hr before procedure ‐ single operator performed all circumcisions ‐procedure standardized ‐ infants fasted from 15 min to 4 hr before procedure ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kurtis 1999 A.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ no Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 48 male NB; FT; 5 min Apgar >/= 7 | |
| Interventions | Mogen clamp and 0.8 ml 1% lidocaine DPNB (n=16) Mogen clamp and no DPNB (n=16) Gomco clamp and 0.8 mL 1% lidocaine DPNB (n=8) Gomco clamp and no DPNB (n=8) 5 minute WT | |
| Outcomes | time crying, HR, O2sat, salivary cortisol, RR | |
| Notes | ‐ all subjects had pacifiers ‐ infants fasted 1 ‐ 2 hr before procedure ‐ Mogen = 8 procedural steps; Gomco = 13 procedural steps | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kurtis 1999 B.
| Methods | see Kurtis 1999 A | |
| Participants | see Kurtis 1999 A | |
| Interventions | comparison is Mogen versus Gomco for patients receiving no DPNB | |
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Lander 1997.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ partial Complete follow‐up ‐ no Blinding of outcome measurement ‐ yes | |
| Participants | 54 male NB; FT; AGA; 1‐3 d age | |
| Interventions | 2g LP cream (n=15) placebo cream (n=12) 0.8 ml 1% lidocaine DPNB (n=14) 0.8 ml 1% lidocaine RB (n=13) ‐ penile blocks 8 min WT; creams applied 90 min prior and covered with occlusive dressing | |
| Outcomes | HR; time cry; O2 sat, RR, palmar sweat, metHgb level | |
| Notes | ‐ 2 withdrawals, 1 in placebo group, 1 in RB group (1 parents unable to remain in hospital, 1 required phototherapy) ‐ procedure standardized ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Macke 2001.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 60 male NB; FT; Apgar >/= 8 | |
| Interventions | acetaminophen 10 mg/kg (n=29) placebo (n=31) given 1 hr prior to circumcision | |
| Outcomes | HR , Nursing Child Assessment Feeding Scale, cry time, infant state | |
| Notes | ‐ 12 operators performed circumcisions in analgesia group, 21 performed circumcisions in placebo group ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Marchette 1989.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ can't tell Complete follow‐up ‐ no Blinding of outcome measurement ‐ can't tell | |
| Participants | 103 male NB; Apgar >/= 8 | |
| Interventions | classical music (n=25) intrauterine sounds (n=15) control (no nurse present) (n=18) | |
| Outcomes | HR; heart rhythm; BP; TcpO2; MDFMCS; BNAS | |
| Notes | ‐ 103 subjects randomized, 45 cases deleted due to missing data or prolonged circumcisions ‐ procedure standardized ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Marchette 1991.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ can't tell Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 121 male NB; Apgar =/> 6; normal delivery; 2 ‐ 9 days age | |
| Interventions | taped music (n=20) intrauterine sounds (n=20) pacifier (n=20) music and pacifier (n=20) intrauterine sounds and pacifier (n=20) control ‐ no treatment (n=21) | |
| Outcomes | HR, rhythm, BP; tcPO2; rate pressure product, BNAS; crying | |
| Notes | ‐ cases excluded if circumcision longer than 15 min or if bleeding ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Masciello 1990.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ can't tell | |
| Participants | 30 male NB, healthy, FT | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=10) 0.8 ml 1% lidocaine local block (n=10) no treatment control (n=10) 5 min WT | |
| Outcomes | plasma cortisol, HR, O2sat, cry | |
| Notes | ‐ cortisol levels obtained for first 3 cases lost (1 in each group) ‐ all fasted for at least 3 hours prior ‐ procedure standardized ‐ single operator performed all circumcisions ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Maxwell 1987.
| Methods | RCT; Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 30 male NB; FT; healthy | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=20) no treatment control (n=10) 5 min WT | |
| Outcomes | HR, O2sat, BP, plasma lidocaine | |
| Notes | ‐ subjects fasted for 2 hr prior ‐ procedure not standardized ‐ Gomco clamp ‐ no adverse effects observed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Mohan 1998.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ can't tell Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 60 male NB; FT; BW>/= 2500 g; 5 min Apgar >/= 7; < 5 days age | |
| Interventions | 5 g LP cream + 2 ml 24% sucrose via pacifier (n=19) 5 g LP cream + water via pacifier (n=20) 2 ml 24% sucrose via pacifier (n=21) water via pacifier (n=19) ‐ non‐randomized control ‐ cream applied 45‐60 min prior, covered with occlusive dressing | |
| Outcomes | HR; O2sat; BP; cry duration | |
| Notes | ‐ control group not randomized ‐ all received pacifiers ‐ procedure standardized ‐ Gomco clamp ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Mudge 1989.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 44 male NB; 5 min Apgar > 7; BW 2.5 ‐ 4.5 kg; FT; age 12 ‐ 72 h | |
| Interventions | 4% lidocaine cream (n=20) placebo cream (n=24) cream applied 2 hr prior covered with occlusive dressing | |
| Outcomes | HR, RR, O2sat, cry time, behavior | |
| Notes | ‐ Gomco clamp ‐ procedure standardized | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Newton 1999.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ no Blinding of outcome measurement ‐ can't tell | |
| Participants | 194 male NB; healthy | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=92) 0.8 ml 1% buffered lidocaine (n=102) | |
| Outcomes | HR (primary outcome variable); O2sat; number crying/phase; modified BNAS | |
| Notes | ‐ complete data on crying for 165 subjects; complete data on BNAS for 194 ‐ complete data on HR, O2 sat for 143 subjects due to technical difficulties ‐ procedure standardized ‐ Mogen clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Spencer 1992.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ can't tell Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 75 male NB; BW 2500 ‐ 4500 g; >12 hr age; 5 min Apgar > 6; normal exam | |
| Interventions | lidocaine DPNB ‐ 5 min WT (n=15) lidocaine DPNB with 2 min WT (n=15) 1% chloroprocaine DPNB with 3 min WT (n=15) 1% chloroprocaine DPNB with 5 min WT (n=15) no treatment control (n=15) | |
| Outcomes | cry duration, O2Sat, HR, BNAS | |
| Notes | ‐ all received pacifiers ‐ fed 60 to 90 min prior to circumcision ‐ procedure standardized ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stang 1988 A.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ partial Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 60 male NB; > 24 hr age; BW > 3000 g; 5 min Apgar > 7; uncomplicated delivery | |
| Interventions | 0.8 ml 1% lidocaine DPNB (n=20) saline DPNB (n=20) no treatment control (n=20) 5 min WT *comparison is DPNB versus no treatment | |
| Outcomes | % time cry, modal behavior state, plasma cortisol | |
| Notes | ‐ all handling avoided for 2 hr prior ‐ 1/2 had blood sample for cortisol at 30 min, 1/2 at 90 min ‐ all received pacifiers and continuously soothed ‐ procedure standardized to 3 periods ‐ Gomco and Plastibell used at operator's discretion ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stang 1988 B.
| Methods | see Stang A | |
| Participants | see Stang A | |
| Interventions | *comparison is DPNB versus sham (saline) treatment | |
| Outcomes | see Stang A | |
| Notes | see Stang A | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Stang 1997.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ partial Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 83 male NB, > 20 hr age; BW 3000 ‐ 4000 gm; 5 min Apgar >/= 8; FT | |
| Interventions | group 1 = 0.8 ml 1% lidocaine DPNB, padded restraint , water via pacifier (n=20) group 2 = 0.8 ml 1% lidocaine DPNB, regular restraint, 24% sucrose via pacifier (n=20) group 3 = 0.8 ml 1% buffered lidocaine DPNB, regular restraint, water via pacifier (n=20) group 4 = 0.8 ml 1% lidocaine DPNB, regular restraint, water via pacifier (n=20) (control) 5 min WT | |
| Outcomes | behavioral distress scale, plasma cortisol 30 min post‐circ | |
| Notes | ‐ 5th arm of study (24% sucrose only) abandoned due to high behavioral distress scores ‐ no forced preoperative fasting period ‐ all handling avoided for 1 hr prior ‐ procedure standardized ‐ all given pacifiers ‐ Gomco and Plastibell methods used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Taddio 1997.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ yes Complete follow‐up ‐ no Blinding of outcome measurement ‐ yes | |
| Participants | 68 male NB, BW >/= 2500 g; FT; no jaundice or metHgb | |
| Interventions | 1 g (1ml) LP cream (n=38) 1 g (1ml) placebo cream (n=30) creams covered with occlusive dressing for 60 ‐ 80 min prior | |
| Outcomes | HR, time cry, NFCS, systolic/diastolic BP, metHgb | |
| Notes | ‐ 68 subjects randomized, 8 in the LP group included in safety analysis only, 59 subjects in the efficacy analysis ‐ 1 withdrawal ‐ procedure standardized ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Weatherstone 1993.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 30 male NB; BW >/= 2500 g; FT; Apgar >/= 7; 6‐72 hr age | |
| Interventions | 0.5 g 30% lidocaine cream (n=15) placebo cream (n=15) applied 20 min prior to circumcision and covered with occlusive dressing | |
| Outcomes | HR, RR, O2 sat, BP, Newborn Pain Behavior Scale, serum B‐endophin (15 min post), serum lidocaine | |
| Notes | ‐ procedure not standardized ‐ Gomco and Plastibell clamps ‐ no adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Williamson 1983.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 30 male NB; BW = 2500 ‐ 4000 g; 24 ‐ 72 hr age; FT; Apgar score > 7; systolic BP > 40 mm Hg | |
| Interventions | 0.6 to 0.8 1% ml lidocaine DPNB (n=20) no treatment control (n=10) 4 min WT | |
| Outcomes | TcpO2, time cry; HR, RR | |
| Notes | ‐ fasted at least 2 hr prior ‐ PI performed all circumcisions ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Williamson 1986.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 24 male NB; Apgar > 7; BW 2500 ‐ 4500 g; FT; 24 ‐ 72 hr age; normal physical exam | |
| Interventions | lidocaine DPNB (n= 11) no treatment control (n=13) 5 min WT | |
| Outcomes | plasma cortisol pre and 30 min post circumcision | |
| Notes | ‐ 6 additional infants circumcised after study completed to serve as controls for blood sampling/injections ‐ all circumcisions done by PI ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Williamson 1997.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ no Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 30 male NB; FT; >/= 24 hr age; BW 2500‐ 4500g; Apgar > 7 | |
| Interventions | lidocaine DPNB (n=20) no treatment control (n=10) | |
| Outcomes | TcPO2, RR, HR, cardiac rhythm, cry time and type | |
| Notes | ‐ procedure standardized ‐ fasting at least 2 hr prior ‐ Gomco clamp ‐ adverse effects reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Woodman 1999.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ yes Complete follow‐up ‐ yes Blinding of outcome measurement ‐ can't tell | |
| Participants | 61 male NB; Apgar > 7; FT; BW > 2500 g; 6‐72 hr age | |
| Interventions | 1 g (1 ml) LP cream (n=20) 30% lidocaine cream (n=20) placebo cream (n=21) creams applied 1 hr prior and covered with occlusive dressing | |
| Outcomes | HR; time crying; O2sat | |
| Notes | ‐ all subjects fasted for at least 1 hr prior ‐ procedure standardized ‐ all circumcisions performed by same operator ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Zahorodny 1998.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ yes Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 53 healthy male NB | |
| Interventions | 1g LP cream + 2 ml 50% sucrose 1g LP cream + 2 ml H2O 1g placebo cream + 2 ml 50% sucrose 1g placebo cream + 2mL H2O creams applied 1 hr prior; sucrose or H2O oral 2 min prior total n=53, allocation not clear | |
| Outcomes | time cry | |
| Notes | abstract only, number of subjects per group not reported assumed equal distribution to groups unable to obtain additional data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Zahorodny 1999.
| Methods | RCT Blinding of randomization ‐ can't tell Blinding of intervention ‐ yes Complete follow‐up ‐ can't tell Blinding of outcome measurement ‐ can't tell | |
| Participants | 61; healthy male NB | |
| Interventions | 10 ml 50% sucrose via pacifier 10 ml H2O via pacifier no treatment control total n=61, allocation not clear | |
| Outcomes | HR, time cry | |
| Notes | abstract only, unable to obtain additional data assumed equal distribution to groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Zolnoski 1993.
| Methods | RCT Blinding of randomization ‐ yes Blinding of intervention ‐ can't tell Complete follow‐up ‐ yes Blinding of outcome measurement ‐ yes | |
| Participants | 20 male NB, 8 ‐ 120 hr age, FT; no maternal medication, BW > 2700 g, 5 min Apgar >/= 7 | |
| Interventions | 2.4 ml 24% sucrose (n=10) 2.4 ml water via syringe (n=10) given 3 min prior | |
| Outcomes | cry time, HR | |
| Notes | ‐ pilot study ‐ Master's thesis ‐ procedure standardized ‐ Gomco clamp | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Participant Characteristics: NB = newborn; AGA = growth appropriate for gestational age; BW = birthweight; FT = full‐term >/= 37 weeks gestation; NICU ‐ neonatal intensive care unit; Interventions: DPNB = dorsal penile nerve block as described in Kirya (1978) using 1% lidocaine without epinephrine; RB = ring block following the procedure outlined by Broadman (1987); local block = local anesthesia performed by injecting 0.4 ml of 1% lidocaine without epinephrine subcutaneously into two positions on the foreskin at the level of the corona; LP cream = a lidocaine‐prilocaine cream commonly known as EMLA (eutectic mixture of local anesthetics); D50W = 50% dextrose oral solution; control/no treatment group = group receiving no intervention for pain; placebo group = group receiving sham intervention which mimics active interventions; WT = the time from completion of administration of pain relief intervention to the start of circumcision procedure; Scales: NIPS = Neonatal Infant Pain Scale consisting of six behavioral components with a composite score of 0 to 7 (Lawrence, 1993); NFCS score = evaluates the presence or absence of 10 discrete facial actions at outlined in Grunau (1987), scored from videotape in 2 sec intervals for the first 20 sec of each circumcision phase; BNAS = Brazelton Neonatal Behavioral Assessment Scale; MDFMCS = Maximally Discriminative Facial Movement Coding System for coding facial movements of three facial regions to determine emotions demonstrated; NCAFS = Nursing Child Assessment Feeding Scale measures mother‐infant interaction using 76 behavioral items grouped into six subscales based on concepts of adaptation and synchronism ‐ mother and infant are observed during natural feeding session; MBPS = modified behavioral pain scale; Physiological measures: HR= heart rate in beats/minute (bpm); TcpO2 = transcutaneous oxygen saturation; O2sat = % oxygen saturation in the blood; BP = blood pressure; RR = respiratory rate in breaths/minute; Biochemical measures: [PC] = plasma cortisol concentration; metHgb = methemoglobin
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Malnory 2003 | Study subjects not randomized to treatment groups, intervention chosen by physician |
| Mintz 1989 | Not a clinical trial, no comparison between groups |
| Olson 1998 | Study subjects not randomized to treatment groups, intervention chosen by physician |
| Russell 1996 | Not a clinical trial, all subjects received EMLA, Plastibell technique |
| Taddio 2000 | Cohort design with two study groups; all recruited subjects assigned to Group 1; Group 2 data obtained from previously conducted RCT |
| Taeusch 2002 | Trial of head to head comparison of surgical devices (clamps) used for circumcision procedure, procedural differences have indirect effect on circumcision pain |
Contributions of authors
Brady‐Fryer ‐ protocol development; study selection; data extraction; contact authors; data preparation & analysis; write report Wiebe ‐ data extraction; data preparation & analysis; write report Lander ‐ protocol development and review; review draft and final report Brankston ‐ study selection; data extraction
Sources of support
Internal sources
Capital Health, Canada.
Faculty of Nursing, University of Alberta, Canada.
External sources
Alberta Association of Registered Nurses, Canada.
Canadian Nurses Association, Canada.
Canadian Health Services Research Foundation, Canada.
Declarations of interest
Two of the reviewers, Brady‐Fryer and Lander, were authors of a trial, Lander 1997, included in this review.
Edited (no change to conclusions)
References
References to studies included in this review
Arnett 1990 {published data only}
- Arnett RM, Jones JS, Horger EO. Effectiveness of 1% lidocaine dorsal penile nerve block in infant circumcision. Americal Journal of Obstetrics and Gynecology 1990;163:1074‐80. [DOI] [PubMed] [Google Scholar]
Benini 1993 {published data only}
- Benini F, Johnston CC, Faucher D, Aranda J V. Topical anesthesia during circumcision in newborn infants. JAMA 1993;270:850‐3. [PubMed] [Google Scholar]
Blass 1991 A {published data only}
- Blass EM, Hoffmeyer LB. Sucrose as an analgesic for newborn infants. Pediatrics 1991;87:215‐18. [PubMed] [Google Scholar]
Blass 1991 B {published data only}
- Blass EM, Hoffmeyer LB. Sucrose as an analgesic for newborn infants. Pediatrics 1991;87:215‐18. [PubMed] [Google Scholar]
Butler O'Hara 1998 {published data only}
- Butler‐O'Hara M, LeMoine C, Guillet R. Analgesia for neonatal circumcision: A randomized controlled trial of EMLA cream versus dorsal penile nerve block. Pediatrics 1998;101:e5. [DOI] [PubMed] [Google Scholar]
Dixon 1984 {published data only}
- Dixon S, Snyder J, Holve R, Bromberger P. Behavioral effects of circumcision with and without anesthesia. Journal of Developmental and Behavioral Pediatrics 1984;5:246‐50. [PubMed] [Google Scholar]
Hardwick Smith 1998 {published data only}
- Hardwick‐Smith S, Mastrobattista JM, Wallace PA, Ritchey ML. Ring block for neonatal circumcision. Obstetrics and Gynecology 1998;91:930‐4. [DOI] [PubMed] [Google Scholar]
Herschel 1998 {published data only}
- Herschel M, Khoshnood B, Ellman C, Maydew N, Mittendorf R. Randomized trial of a sucrose pacifier for pain control. Archives of Pediatrics & Adolescent Medicine 1998;152:279‐84. [DOI] [PubMed] [Google Scholar]
Holliday 1999 {published data only}
- Holliday MA, Pinckert TL, Kiernan SC, Kunos I, Angelus P, Keszler M. Dorsal penile nerve block vs topical placebo for circumcision in low‐birth‐weight neonates. Archives of Pediatrics & Adolescent Medicine 1999;153:476‐80. [DOI] [PubMed] [Google Scholar]
Holve 1983 {published data only}
- Holve RL, Bromberger PJ, Groveman HD, Klauber MR, Dixon SD, Snyder JM. Regional anesthesia during newborn circumcision. Effect on infant in pain response. Clinical Pediatrics 1983;22:813‐8. [DOI] [PubMed] [Google Scholar]
Howard 1994 {published data only}
- Howard CR, Howard FM, Weitzman ML. Acetaminophen analgesia in neonatal circumcision: the effect on pain. Pediatrics 1994;93:641‐6. [PubMed] [Google Scholar]
Howard 1999 {published data only}
- Howard CR, Howard FM, Fortune K, Generelli P, Zolnoun D, tenHoopen C, et al. A randomized, controlled trial of a eutectic mixture of local anesthetic cream (lidocaine and prilocaine) versus penile block for pain relief during circumcision. American Journal of Obstetrics and Gynecology 1999;181:1506‐11. [DOI] [PubMed] [Google Scholar]
Joyce 2001 {published data only}
- Joyce BA, Keck JF, Gerkensmeyer J. Evaluation of pain management interventions for neonatal circumcision pain. Journal of Pediatric Health Care 2001;15:105‐14. [DOI] [PubMed] [Google Scholar]
Kass 2001 {published data only}
- Kass FC, Holman JR. Oral glucose solution for analgesia in infant circumcision. Journal of Family Practice 2001;50:785‐8. [PubMed] [Google Scholar]
Kaufman 2002 {published data only}
- Kaufman GE, Cimo S, Miller LW, Blass EM. An evaluation of the effects of sucrose on neonatal pain with 2 commonly used circumcision methods. American Journal of Obstetrics and Gynecology 2002;186:564‐8. [DOI] [PubMed] [Google Scholar]
Kurtis 1999 A {published data only}
- Kurtis PS, DeSilva HN, Bernstein BA, Malakh L, Schechter NL. A comparison of the Mogen and Gomco clamps in combination with dorsal penile nerve block in minimizing the pain of neonatal circumcision. Pediatrics 1999;103:e23. [DOI] [PubMed] [Google Scholar]
Kurtis 1999 B {published data only}
- Kurtis PS, DeSilva HN, Bernstein BA, Malakh L, Schechter NL. A comparison of the Mogen and Gomco clamps in combination with dorsal penile nerve block in minimizing the pain of neonatal circumcision. Pediatrics 1999;103:e23. [DOI] [PubMed] [Google Scholar]
Lander 1997 {published data only}
- Lander J, Brady‐Fryer B, Metcalfe J, Nazarali S, Muttitt S. Comparison of ring block, dorsal penile nerve block, and topical anesthesia for neonatal circumcision: a randomized controlled trial. JAMA 1997;278:2157‐62. [PubMed] [Google Scholar]
Macke 2001 {published data only}
- Macke JK. Analgesia for circumcision: Effects on newborn behavior and mother/infant interaction. Journal of Obstetric, Gynecologic, and Neonatal Nursing 2001;30:507‐14. [DOI] [PubMed] [Google Scholar]
Marchette 1989 {published data only}
- Marchette L, Main R, Redick E. Pain reduction during neonatal circumcision. Pediatric Nursing 1989;15:207‐10. [PubMed] [Google Scholar]
Marchette 1991 {published data only}
- Marchette L, Main R, Redick E, Bagg A, Leatherland J. Pain reduction interventions during neonatal circumcision. Nursing Research 1991;40:241‐4. [PubMed] [Google Scholar]
Masciello 1990 {published data only}
- Masciello A L. Anesthesia for neonatal circumcision: Local anesthesia is better than dorsal penile block. Obstetrics and Gynecology 1990;75:834‐8. [PubMed] [Google Scholar]
Maxwell 1987 {published data only}
- Maxwell LG, Yaster M, Wetzel RC, Niebyl JR. Penile nerve block for newborn circumcision. Obstetrics and Gynecology 1987;70:415‐19. [PubMed] [Google Scholar]
Mohan 1998 {published data only}
- Mohan CG, Risucci DA, Casimir M, Gulrajani‐LaCorte, M. Comparison of analgesics in ameliorating the pain of circumcision. Journal of Perinatology 1998;18:13‐9. [PubMed] [Google Scholar]
Mudge 1989 {published data only}
- Mudge D, Younger J B. The effects of topical lidocaine on infant response to circumcision. Journal of Nurse‐Midwifery 1989;34:335‐40. [DOI] [PubMed] [Google Scholar]
Newton 1999 {published data only}
- Newton CW, Mulnix N, Baer L, Bovee T. Plain and buffered lidocaine for neonatal circumcision. Obstetrics and Gynecology 1999;93:350‐2. [DOI] [PubMed] [Google Scholar]
Spencer 1992 {published data only}
- Spencer DM, Miller K A, O'Quin M, Tomsovic J P, Anderson B, Wong D, et al. Dorsal penile nerve block in neonatal circumcision: Chloroprocaine versus lidocaine. American Journal of Perinatology 1992;9:214‐8. [DOI] [PubMed] [Google Scholar]
Stang 1988 A {published data only}
- Stang H J, Gunnar M R, Snellman L, Condon L M, Kestenbaum R. Local anesthesia for neonatal circumcision ‐ Effects on distress and cortisol response. JAMA 1988;259:1507‐11. [PubMed] [Google Scholar]
Stang 1988 B {published data only}
- Stang HJ, Gunnar MR, Snellman L, Condon LM, Kestenbaum R. Local anesthesia for neonatal circumcision ‐ Effects on distress and cortisol response. JAMA 1988;259:1507‐11. [PubMed] [Google Scholar]
Stang 1997 {published data only}
- Stang HJ, Snellman LW, Condon LM, Conroy MM, Liebo R, Brodersen L, et al. Beyond dorsal penile nerve block: A more humane circumcision. Pediatrics 1997;100:e3. [DOI] [PubMed] [Google Scholar]
Taddio 1997 {published data only}
- Taddio A, Stevens B, Craig K, Rastogi P, Ben‐David S, Shennan A, et al. Efficacy and safety of lidocaine‐prilocaine cream for pain during circumcision. New England Journal of Medicine 1997;336:1197‐1201. [DOI] [PubMed] [Google Scholar]
Weatherstone 1993 {published data only}
- Weatherstone KB, Rasmussen LB, Erenberg A, Jackson EM, Claflin KS, Leff RD. Safety and efficacy of a topical anesthetic for neonatal circumcision. Pediatrics 1993;92:710‐4. [PubMed] [Google Scholar]
Williamson 1983 {published data only}
- Williamson PS, Williamson ML. Physiologic stress reduction by a local anesthetic during newborn circumcision. Pediatrics 1983;71:36‐40. [PubMed] [Google Scholar]
Williamson 1986 {published data only}
- Williamson PS, Evans ND. Neonatal cortisol response to circumcision with anesthesia. Clinical Pediatrics 1986;25:412‐5. [DOI] [PubMed] [Google Scholar]
Williamson 1997 {published data only}
- Williamson ML. Circumcision anesthesia: A study of nursing implications for dorsal penile nerve block. Pediatric Nursing 1997;23:59‐63. [PubMed] [Google Scholar]
Woodman 1999 {published data only}
- Woodman PJ. Topical lidocaine‐prilocaine versus lidocaine for neonatal circumcision: A randomized controlled trial. Obstetrics and Gynecology 1999;93:775‐9. [DOI] [PubMed] [Google Scholar]
Zahorodny 1998 {published data only}
- Zahorodny W, Surez Y, Marshall R, Regan M, Holland B, Brendel D. Efficacy of EMLA and sucrose for crying associated with circumcision. Pediatrric Research. 1998; Vol. 43 Supplement 2:204A.
Zahorodny 1999 {published data only}
- Zahorodny W, David ES, Estrada P, Co J, Marshall R. Efficacy of a sucrose pacifier for newborn pain. Pediatric Research. 1999; Vol. 45 PART 2 of 2:17A.
Zolnoski 1993 {unpublished data only}
- Zolnoski BAP. Effect of sucrose ingestion on pain during newborn circumcision [Masters thesis]. Univ. of Florida, 1993. [Digital Dissertations ‐ AAT 1358079] [Google Scholar]
References to studies excluded from this review
Malnory 2003 {published data only}
- Malnory M, Johnson TS, Kirby RS. Newborn behavioral and physiological responses to circumcision. MCN. The American Journal of Maternal Child Nursing 2003;28:313‐7. [DOI] [PubMed] [Google Scholar]
Mintz 1989 {published data only}
- Mintz MR, Grillo R. Dorsal penile nerve block for circumcision. Clinical Pediatrics 1989;28:590‐1. [DOI] [PubMed] [Google Scholar]
Olson 1998 {published data only}
- Olson T, Wessman Downey V. Infant physiological responses to noxious stimuli of circumcision with anesthesia and analgesia. Pediatric Nursing 1998;24:385‐9. [PubMed] [Google Scholar]
Russell 1996 {published data only}
- Russell CT, Chaseling J. Topical anesthesia in neonatal circumcision: a study of 208 consecutive cases. Australian Family Physician 1996;25:530‐4. [PubMed] [Google Scholar]
Taddio 2000 {published data only}
- Taddio A, Pollock N, Gilbert‐MacLeod C, Ohlsson K, Koren G. Combined analgesia and local anesthesia to minimize pain during circumcision. Archives of Pediatrics & Adolescent Medicine 2000;154:620‐3. [DOI] [PubMed] [Google Scholar]
Taeusch 2002 {published data only}
- Taeusch HW, Martinez AM, Partridge JC, Sniderman S, Armstrong‐Wells J, Fuentes‐Afflick E. Pain during Mogen or Plastibell circumcision. Journal of Perinatology 2002;22:214‐8. [DOI] [PubMed] [Google Scholar]
Additional references
AAP 1999
- American Academy of Pediatrics Task Force on Circumcision. Circumcision Policy Statement. Pediatrics 1999;103:686‐93. [PubMed] [Google Scholar]
Abu‐Saad 1998
- Abu‐Saad H, Bours G, Stevens B, Hamers J. Assessment of pain in the neonate. Seminars in Perinatology 1998;22:402‐16. [DOI] [PubMed] [Google Scholar]
Anand 2001
- Anand KJS. Consensus statement for the prevention and management of pain in the newborn. Archives of Pediatrics & Adolescent Medicine 2001;155:173‐80. [DOI] [PubMed] [Google Scholar]
Anders 1974
- Anders TF, Chalemian RJ. The effects of circumcision on sleep‐wake states in human neonates. Psychosomatic Medicine 1974;36:174‐9. [DOI] [PubMed] [Google Scholar]
Auerbach 1978
- Auerbach MR, Scanlon JW. Recurrence of pneumothroax as a possible complication of circumcision. American Journal of Obstetrics and Gynecology 1978;132:583. [DOI] [PubMed] [Google Scholar]
Bellieni 2002
- Bellieni CV, et al. Effect of multisensory stimulation on analgesia in term neonates: A randomized controlled trial. Pediatric Research 2002;51:460‐3. [DOI] [PubMed] [Google Scholar]
Berde 2002
- Berde CB, Sethna NF. Analgesics for the treatment of pain in children. New England Journal of Mecicine 2002;347:1094‐1103. [DOI] [PubMed] [Google Scholar]
Brazelton 1973
- Brazelton TB. Neonatal behavioral assessment scale. Clinics in Developmental Medicine. Vol. 50, Philadelphia, PA: JB Lippincott, 1973:1‐66. [Google Scholar]
Brazelton 1984
- Brazelton TB. Neonatal behavioral assessment scale. Philadelphia: J B Lippincott, 1984. [Google Scholar]
Campos 1994
- Campos RG. Rocking and pacifiers: two comforting interventions for heelstick pain. Research in Nursing & Health 1994;17:321‐31. [DOI] [PubMed] [Google Scholar]
Carbajal 1999
- Carbajal R, Chauvet X, Couderc S, Olivier‐Martin M. Randomized trial of analgesic effects of sucrose, glucose, and pacifiers in term infants. BMJ 1999;319:1393‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Connelly 1992
- Connelly KP, Shropshire LC, Salzberg A. Gastric rupture associated with prolonged crying in a newborn undergoing circumcision. Clinical Pediatrics 1992;31:560‐1. [DOI] [PubMed] [Google Scholar]
Corff 1995
- Corff KE, Seideman R, Venkataraman PS, Lutes L, Yates B. Facilitated tucking: a nonpharmacologic comfort measure for pain in preterm neonates. Journal of Obstetric, Gynecologic, and Neonatal Nursing 1995;24:143‐7. [DOI] [PubMed] [Google Scholar]
CPS 1996
- Canadian Pediatric Society Fetus and Newborn Committee. Neonatal circumcision revisited. CMAJ 1996;154:769‐80. [PMC free article] [PubMed] [Google Scholar]
Dalens 1989
- Dalens B, Vanneuvile G, Dechelotte P. Penile block via the subpubic space in 100 children. Anesthesia and Analgesia 1989;69:41‐5. [PubMed] [Google Scholar]
Deeks 2001
- Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta‐analysis. Egger M, Davey Smith G, and Altman DG. Systematic reviews in health care. 2nd Edition. London, UK: BMJ Books, 2001:300. [Google Scholar]
Fitzgerald 1993
- Fitzgerald M, Anand KJS. Developmental neuroanatomy and neurophysiology of pain. In: Schecter N L, Berde C B, Yaster M editor(s). Pain in infants, children and adolescents. Baltimore: Williams & Wilkins, 1993:11‐31. [Google Scholar]
Follmann 1992
- Follmann D, Elliot P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology 1992;45:769‐73. [DOI] [PubMed] [Google Scholar]
Frank 1997
- Frank LS, Miaskowski C. Measurement of neonatal responses to painful stimuli: A research review. Journal of Pain and Symptom Management 1997;14:343‐78. [DOI] [PubMed] [Google Scholar]
Gibbons 2001
- Gibbons S, Stevens B. Mechanisms of sucrose and non‐nutritive sucking in procedural pain management in infants. Pain Research & Management 2001;6:21‐8. [DOI] [PubMed] [Google Scholar]
Gibbons 2002
- Gibbonns S, Stevens B, Hodnett E, Pinelli J, Ohlsson A, Darlington G. Efficiacy and safety of sucrose for procedural pain relief in preterm and term neonates. Nursing Research 2002;51:375‐82. [DOI] [PubMed] [Google Scholar]
Gray 2000
- Gray L, Watt L, Blass EM. Skin‐to‐skin contact is analgesic in healthy newborns. Pediatrics 2000;105:e14. [DOI] [PubMed] [Google Scholar]
Grunau 1987
- Grunau RVE, Craig KD. Pain expression in neonates: facial action and cry. Pain 1987;28:395‐410. [DOI] [PubMed] [Google Scholar]
Gunnar 1981
- Gunnar MR, Fisch RO, Korsvik S, Donhowe JM. The effects of circumcision on serum cortisol and behavior. Psychoneuroendocrinology 1981;6:269‐75. [DOI] [PubMed] [Google Scholar]
Haouari 1999
- Haouri N, Wood C, Griffiths G, Levene M. The analgesic effect of sucrose in full term infants: a randomized controlled trial. BMJ 1999;310:1498‐1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Howard 1998
- Howard CR, Howard FM, Garfunkel LC, Blieck EA, Weitzman M. Neonatal circumcision and pain relief: Current training practices. Pediatrics 1998;101:423‐8. [DOI] [PubMed] [Google Scholar]
Johnston 1997
- Johnston C, Stremler R, Stevens B, Horton L. Effectiveness of oral sucrose and simulated rocking on pain response in preterm neonates. Pain 1997;72:193‐9. [DOI] [PubMed] [Google Scholar]
Kharasch 2003
- Kharasch S, Saxe G, Zuckerman B. Pain treatment: opportunities and challenges. Archives of Pediatrics & Adolescent Medicine 2003;157:1054‐6. [DOI] [PubMed] [Google Scholar]
Kirya 1978
- Kirya C, Werthmann MW. Neonatal circumcision and penile dorsal nerve block ‐ a painless procedure. Journal of Pediatrics 1978;92:998‐1000. [DOI] [PubMed] [Google Scholar]
Lawrence 1993
- Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C. The development of a tool to assess neonatal pain. Neonatal Network 1993;12:59‐66. [PubMed] [Google Scholar]
Maxwell 1999
- Maxwell LG, Yaster M. Analgesia for neonatal circumcision: No more studies, just do it. Archives of Pediatrics & Adolescent Medicine 1999;153:444‐5. [DOI] [PubMed] [Google Scholar]
McGrath 1990
- McGrath PA. Pain in children. New York: The Guilford Press, 1990. [Google Scholar]
Mitchell 2000
- Mitchell A, Brooks S, Roane D. The premature infant and painful procedures. Pain Management Nursing 2000;1:58‐65. [DOI] [PubMed] [Google Scholar]
Mitchell 2003
- Mitchell A, Waltman P A. Oral sucrose and pain relief for preterm infants. Pain Management Nursing 2003;4:62‐9. [DOI] [PubMed] [Google Scholar]
Myron 1991
- Myron AV, Maguire DP. Pain perception in the neonate: Implications for circumcision. Journal of Professional Nursing 1991;7:188‐95. [DOI] [PubMed] [Google Scholar]
Poma 1980
- Poma PA. Painless neonatal circumcision. International Journal of Gynaecology and Obstetrics 1980;18:308‐9. [DOI] [PubMed] [Google Scholar]
Rawlings 1980
- Rawlings DJ, Miller A, Engel RR. The effect of circumcision on transcutaneous pO2 in term infants. American journal of diseases of children 1980;134:676‐8. [DOI] [PubMed] [Google Scholar]
Ross 1988
- Ross DM, Ross SA. Childhood pain. Baltimore: Urban & Schwarzenberg, 1988. [Google Scholar]
Ryan 1994
- Ryan CA, Finer NN. Changing attitudes and practices regarding local anesthesia for newborn circumcision. Pediatrics 1994;94:230‐3. [PubMed] [Google Scholar]
Snellman 1995
- Snellman LW, Stang HJ. Prospective evaluation of complications of dorsal penile block for neonatal circumcision. Pediatrics 1995;95:705‐8. [PubMed] [Google Scholar]
Stang 1991
- Stang HJ. Response to : Pain perception in the neonate: Implications for circumcision. Journal of Professional Nursing 2001;7:194‐5. [DOI] [PubMed] [Google Scholar]
Stang 1998
- Stang HJ, Snellman LW. Circumcision practice patterns in the United States. Pediatrics 1998;101:e5. [DOI] [PubMed] [Google Scholar]
Stevens 1996
- Stevens B, Johnston CC, Petryshun P, Taddio A. Premature infant pain profile: Development and initial validation. Clinical Journal of Pain 1996;12:13‐22. [DOI] [PubMed] [Google Scholar]
Stevens 1997
- Stevens B, Taddio A, Ohlsson A, Einarson T. The efficacy of sucrose for relieving procedural pain in neonates ‐ a systematic review and meta‐analysis. Acta Paediatrica 1997;86:837‐42. [DOI] [PubMed] [Google Scholar]
Stevens 1999
- Stevens B. Pain in infants. In: McCaffery M, Pasero C editor(s). Pain Clinical Manual. 2nd Edition. St. Louis: Mosby, 1999:626‐673. [Google Scholar]
Sweet 1998
- Sweet SD, McGrath PJ. Physiological measures of pain. In: Finley G A, McGrath P J editor(s). Measurement of pain in infants and children. Seattle: IASP Press, 1998:59‐81. [Google Scholar]
Taddio 1997b
- Taddio A, Katz J, Ilersich A L, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet 1997;349:599‐603. [DOI] [PubMed] [Google Scholar]
Taddio 1998
- Taddio A, Ohlsson A, Einarson TR, Stevens B, Koren G. A systematic review of lidocaine‐prilocaine cream (EMLA) in the treatment of acute pain in neonates. Pediatrics 1998;101:e1. [DOI] [PubMed] [Google Scholar]
Taddio 2001
- Taddio A. Pain management for neonatal circumcision. Paediatric Drugs 2001;3:101‐11. [DOI] [PubMed] [Google Scholar]
Taddio 2002
- Taddio A, Ohlsson K, Ohlsson A. Lidocaine‐prilocaine cream for analgesia during circumcision in newborn boys (Cochrane Review). The Cochrane Library 2002, Issue 4. [DOI] [PubMed] [Google Scholar]
Talbert 1976
- Talbert LM, Kraybill EN, Potter HD. Adrenal cortical response to circumcision in the neonate. Obstetrics and Gynecology 1976;48:208‐10. [PubMed] [Google Scholar]
Wellington 1993
- Wellington N, Rieder MJ. Attitudes and practices regarding analgesia for neonatal circumcision. Pediatrics 1993;92:541‐54. [PubMed] [Google Scholar]
Yarrow 1975
- Yarrow L, Rubenstein JL, Pedersen FA. Infant and environment. New York: John Wiley and Sons, 1975. [Google Scholar]
References to other published versions of this review
Brady‐Fryer 2004
- Brady‐Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. The Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI] [PMC free article] [PubMed] [Google Scholar]


