Abstract
Advancement in the Internet of Medical Things (IoMT), along with machine learning, deep learning, and artificial intelligence techniques, initiated a world of possibilities in healthcare. It has an extensive range of applications: when connected to the Internet, ordinary medical devices and sensors can collect valuable data, deep learning, and artificial intelligence techniques utilize this data and give an insight of symptoms, trends and enable remote care. Recently, Covid-19 pandemic outbreak caused the death of a large number of people. This virus has infected millions of people, and still, the rate of infected people is increasing day by day. Researchers are endeavoring to utilize medical images and deep learning-based models for the detection of Covid-19. Various techniques have been presented that utilize X-Ray images of the chest for the detection of Covid-19. However, the importance of regional-based convolutional neural networks (CNNs) is currently confined. Thus, this research aimed to introduce an IoT-based deep learning framework for early assessment of Covid-19. This framework can reduce the working pressure of medical experts/radiologists and contribute to the pandemic control. A deep learning-based model, i.e., faster regions with CNNs (Faster-RCNN) with ResNet-101, is applied on X-Ray images of the chest for Covid-19 detection. It uses region proposal network (RPN) to perform detection. By employing the model, we achieve a detection accuracy of 98%. Therefore, we believe that the system might be capable in order to assist medical expert/radiologist, to verify early assessment toward Covid-19.
Keywords: Covid-19, deep learning, faster regions with CNN (Faster-RCNN), Internet of Medical Things (IoMT), ResNet-101
I. Introduction
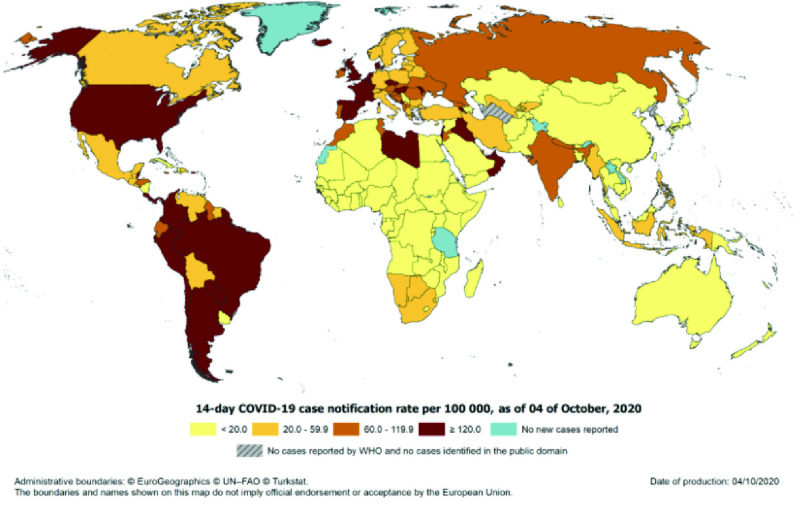
Internet of Medical Things (IoMT) plays a pivotal part in the healthcare sector and increases the accuracy, reliability, and productivity of electronic devices. Researchers continuously pay attention to a digitized healthcare system via interconnecting the convenient medical devices/resources and healthcare services. IoMT helps in reducing unnecessary appointments and the burden on healthcare organizations by connecting subjects to their medical experts and supporting the transfer of medical data. In December 2019, the Covid-19 infection (virus originated from animals) appeared in Wuhan Province, China, and quickly spread worldwide [1]. The virus transmits through the air, and physical contact with an infected person [2] and inserts itself into the lungs through the respiratory system, where it replicates and destroys lung cells [3]. On March 11, 2020, the disease is declared a pandemic by the World Health Organization. It is recently considered the leading cause of fatality for thousands of countries, including China, Iran, Italy, the USA, Spain, and the United Kingdom. The latest number of infected peopled due to pandemic is shown in Fig. 1.
Fig. 1.
Worldwide Statistics: Covid-19 infected people [4].
At the early stages, the detection of Covid-19 is crucially vital and significant. The medical industry is seeking novel technologies and methods to monitor and control the spread of the virus. The IoMT, along with artificial intelligence and deep learning techniques, might enable the healthcare system to properly monitor Covid-19 subjects. It helps to enhance patient satisfaction and decreases readmission rates in the hospital. It might help to trace the virus spread quickly, recognizes the high-risk patients, and is beneficial for infection control. Likewise, it can help to predict the fatality risk by sufficiently investigating the patients’ earlier data.
IoMT, along with artificial intelligence and deep learning, helps to fight with the virus through medical assistance, population screening, notification, and recommendations about infection control [5]. As an evidence-based medical tool, this technology can enhance the treatment, planning, and reported issues of the Covid-19 [6]. To diagnose Covid-19, several techniques have been introduced, including numerous medical imaging techniques, polymerase chain reaction (PCR), and blood tests (CBCs) [7].
The problem statement is, how two Covid-19 patients, one with normal and the other with infection in the lungs caused by Covid-19, can be treated the same? Therefore, the significance of using X-Ray images parallel with PCR and CBC is that it can give a better estimation of Covid-19. Using other test data with X-Ray images, we might better diagnose the severity of diseases and then perform appropriate treatment. In the traditional X-Ray analysis methods, Covid-19 detection is a comparatively complicated task, as shown in Fig. 2(a). To diagnose Covid-19, X-Ray modality is used, which is economical and low-risk from radiation hazards to human health [8] and [9]. In X-Ray images, the radiologist needs to attentively recognize the white spots or viruses that contain pus and water, which is quite problematic and lengthy. A specialist doctor or radiologist might mistakenly diagnose other diseases such as Covid-19 as pulmonary tuberculosis [10].
Fig. 2.
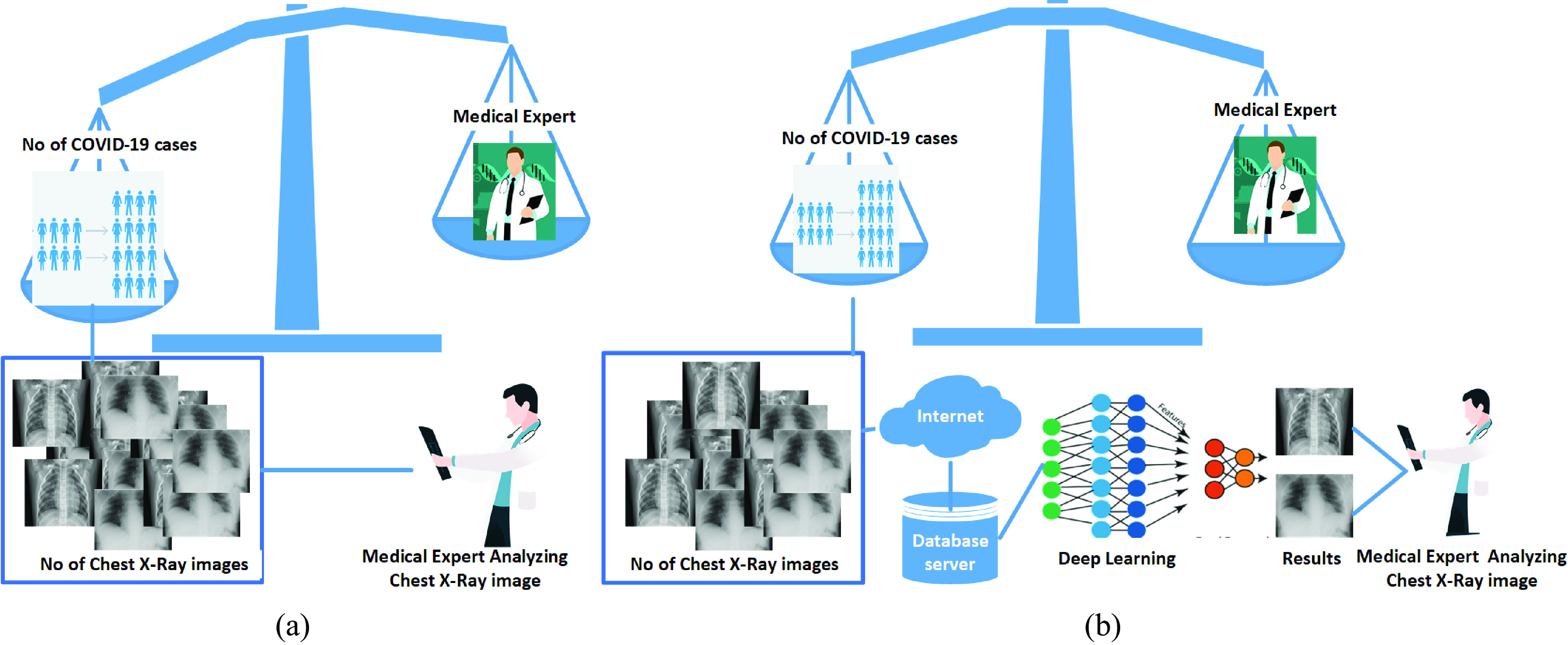
(a) Traditional workflow applied for screening and clinically diagnosing of Covid-19. The number of radiologists or medical experts is relatively small in comparison with the number of cases reported. (b) Analysis of X-Ray images can be significantly improved for Covid-19 diagnosis with IoMT and deep learning.
Inspired from successful results of earlier methods [11], in this work, an Internet of Things (IoT)-based deep learning framework is introduced for Covid-19 detection. The framework can assist the medical expert and radiologist and may help to decrease the workload pressure (examination of X-Rays), stimulating the diagnosis and treatment process of patients, hence contributing to the control of the pandemic Fig. 2(b). For detection of Covid-19 in X-Ray samples, we applied a deep learning architecture, i.e., faster regions with CNN (Faster-RCNN), [12] with ResNet-101 [13] as a backbone network. To the best of our knowledge, Faster-RCNN with ResNet-101 architecture is used for the first time for Covid-19 detection. The X-Ray images are collected from different online available data sources for testing and training of the model. This article mainly focuses on the following.
-
1)
An IoT-based framework is introduced for the early assessment of Covid-19. The medical sensors/devices collected chest X-Ray samples that are directly fed into a deep learning architecture for the detection of Covid-19.
-
2)
The framework is capable of assisting medical experts or radiologists, relieve the working pressure, and might help in the control of pandemic.
-
3)
Regional-based convolutional neural networks (RCNNs), i.e., Faster-RCNN and ResNet-101, are utilized for Covid-19 detection.
-
4)
For training and testing of the model, Chest X-Ray images are customized using different online available data sets.
-
5)
The detection results are compared with other deep learning approaches of Covid-19.
The remainder of this article is organized as follows. The literature work summarizes in Section II. A concise overview of the data sets utilized in this work is presented in Section III. The method used for Covid-19 detection is elaborated in Section IV. The detail of the experimental outcomes is elaborated in Section V, and finally, the conclusion of the work done in this article, and future guidelines, is presented in Section VI.
II. Literature Survey
Researchers have done much work until now to provide an efficient and effective solution for Covid-19 prediction and detection. Singh et al. [14] and Yang et al. [15] provided examples of the IoT and the IoMT applications in healthcare. The applications can be practiced to offer assistance to medical experts in hospitals, assure quarantine implementation, and track pandemic outbreaks. Vafea et al. [16] presented a review of various emerging technologies applied for the treatment and diagnosis of Covid-19 subjects. Researchers used different artificial intelligence [17], machine learning [18], and deep learning approaches [7], [11], and [19] for Covid-19 classification, and detection as shown in Fig. 3. Some researchers [17] did a review of artificial intelligence-based methods applied for segmentation and investigation of Covid-19 X-Rays. In the literature, most of the developed methods employed a limited number of CT-scans and X-Rays for examination and detection of Covid-19 [20], and [21] as presented in Table I. Hemdan et al. [22] presented a comparison of seven deep learning architectures using a limited data set with 50 sample images containing 25 of positive (Covid-19) and 25 samples of healthy subjects. Wang and Wong [23] introduced convolutional neural network (CNN)-based architecture named COVID-net for X-Ray samples classification into Covid-19, normal, and pneumonia, using a data set consisting of 800 images. The reported overall accuracy is 92.4%, and sensitivity is 80%. Farooq and Hafeez [24] used the ResNet-50 model to classify X-Rays samples into infected, healthy, viral, and bacterial pneumonia. The reported results are better as compared to COVID-Net [23]. The overall accuracy is 96.23% with 100% sensitivity. The data set used by the authors contains 68 Covid-19 X-Rays of 45 Covid-19 subjects, 1203 healthy subjects, 660 subjects of Non-Covid-19 viral pneumonia, and 931 subjects of bacterial pneumonia. Apostolopoulos and Mpesiana [25] developed an automatic detection model employing transfer learning with neural networks utilizing X-Ray samples. Pereira et al. [26] performed the task of Covid-19 detection in X-Rays of the chest. The data set used in their work was created from different public data sets, comprising 1144 X-Rays, including 90 images of Covid-19, remaining are five different kinds of pneumonia and healthy type images.
Fig. 3.
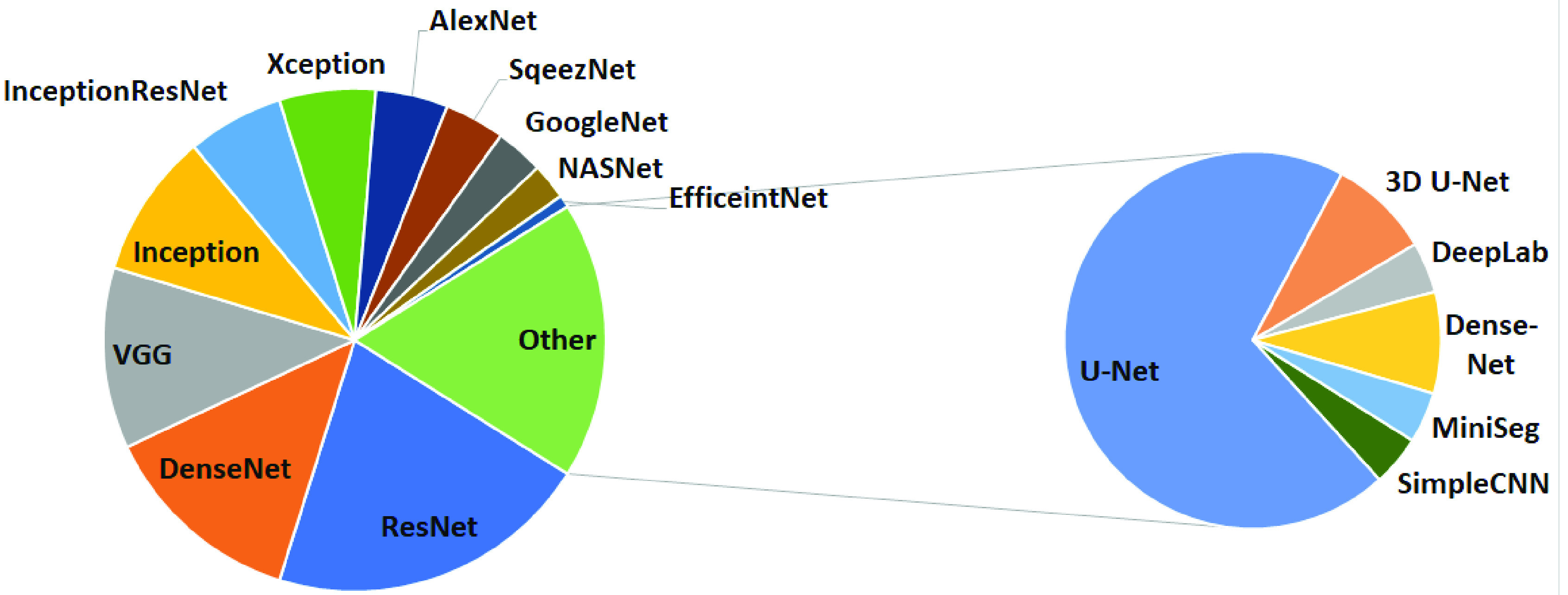
Different deep learning methods used by researchers in literature for Covid-19 detection [7] and [11].
TABLE I. List of Some Available Benchmark Data Sets Used for Covid-19 Detection.
To the best of our knowledge and according to [7] and [11], we provide a review of different deep learning and artificial intelligence methods used for classification of Covid-19. According to the survey, mostly researchers used classification-based methods, including Resnet-50, Resnet-101, DenseNet, VGG, Inception, InceptionResNet, Xception, AlexNet, and SqueezeNet for chest X-Ray images classification as depicted in Fig. 3. Some researchers also used segmentation-based models, including U-Net, 3-D U-Net, VB-Net, DeepLab, Dense-Net, and MiniSeg. Mostly researchers in the literature used pneumonia data set as Chest X-Ray sample images. The summary of various deep learning architectures used for Covid-19 classification and detection is provided in Fig. 3. To the best of our knowledge, Faster-RCNN with ResNet-101 has not been utilized for Covid-19 detection, although [27] utilizes Faster-RCNN for Covid-19 detection but using VGG as base network. Similarly, Ismail et al. [28] used Faster-RCNN but for pathological Chest X-Ray image analysis using a limited data set.
III. Data Set
In the literature, for Covid-19 detection, researchers used various public data sets, including X-Ray and CT images, as shown in Table I. Among both types of medical images, the X-Ray images data sets are mostly used. Most of the researchers used COVID-chest X-Ray-data set [22], [29], [30]. Some practiced Kaggle RSNA Pneumonia detection data sets, such as [31], Covid-19 database, e.g., [32], Chest X-Rays (Pneumonia) [33] for training and evaluation of their models. The most common data set for Chest X-Ray-based Covid-19 research is also shown in Table I. In this work, we customized an X-Ray image data set collected from different available online data sources, as highlighted in Table II, the images contain X-Rays of Covid-19 abnormalities. From different online available sources, approximately 4000 samples of Covid-19 (positive) and 7000 samples of Non-Covid-19 (negative) are obtained, as presented in Table II.
TABLE II. Data Set Used for Training and Testing of the Model.
| S.No | Images | Non-Covid-19 | Covid-19 | Total |
|---|---|---|---|---|
| 1 | Training | 5600 | 3200 | 8800 |
| 2 | Testing | 1400 | 800 | 2200 |
| 3 | Total | 7000 | 4000 | 11000 |
IV. Methodology
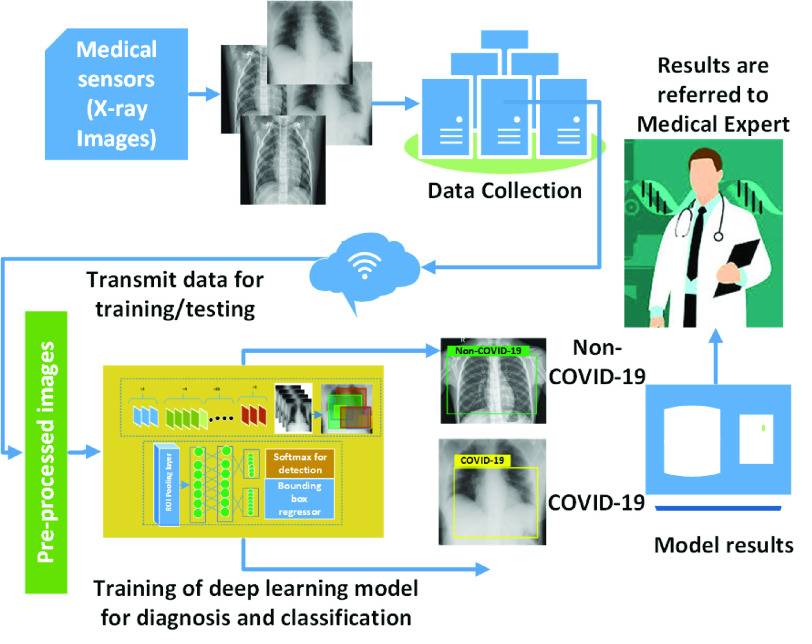
In this work, an IoT-based deep learning framework is presented for Covid-19 detection. The overall framework is shown in Fig. 4; the medical sensors/X-Ray machines collected radiogram images of subjects—the collected data set is given to the model in order to detect the Non-Covid-19 and Covid-19 X-Ray samples. For the validation of the model, results are further referred to a medical expert for opinions. As discussed in the literature, utilizing X-Ray images, different deep learning-based architectures are utilized for Covid-19 detection. In this work, for detection purposes, Faster-RCNN [12] along with ResNet-101 [13] architecture is used. In recent years, it has shown remarkable performance for various classification and detection applications. It utilizes the same traditional network for region proposal generation and detection. The model’s output includes a bounding box (containing detected X-Rays as Non-Covid-19 or Covid-19). The detection results can help the medical expert or radiologist reduce the working pressure and might be beneficial for pandemic control. The detail of the deep learning-based detection model consisting of Faster-RCNN with ResNet-101 is provided in the following section.
Fig. 4.
IoT-based deep learning framework for early assessment of Covid-19.
A. Detection of Covid-19 Using Faster-RCNN With ResNet-101
The deep learning-based architectures are utilized broadly over traditional machine learning-based techniques because it does not require either traditional feature extraction-based methods or any specific segmentation techniques. In this work, Faster-RCNN [12] is employed for Covid-19 detection utilizing X-Ray sample images of the chest, as depicted in Fig. 5. It is also known as a two-stage detection model as it essentially has two stages; the initial stage provides region anchors using region proposal network (RPN). The second stage is employed for X-Ray images classification using bounding boxes and detected regions’ information.
Fig. 5.
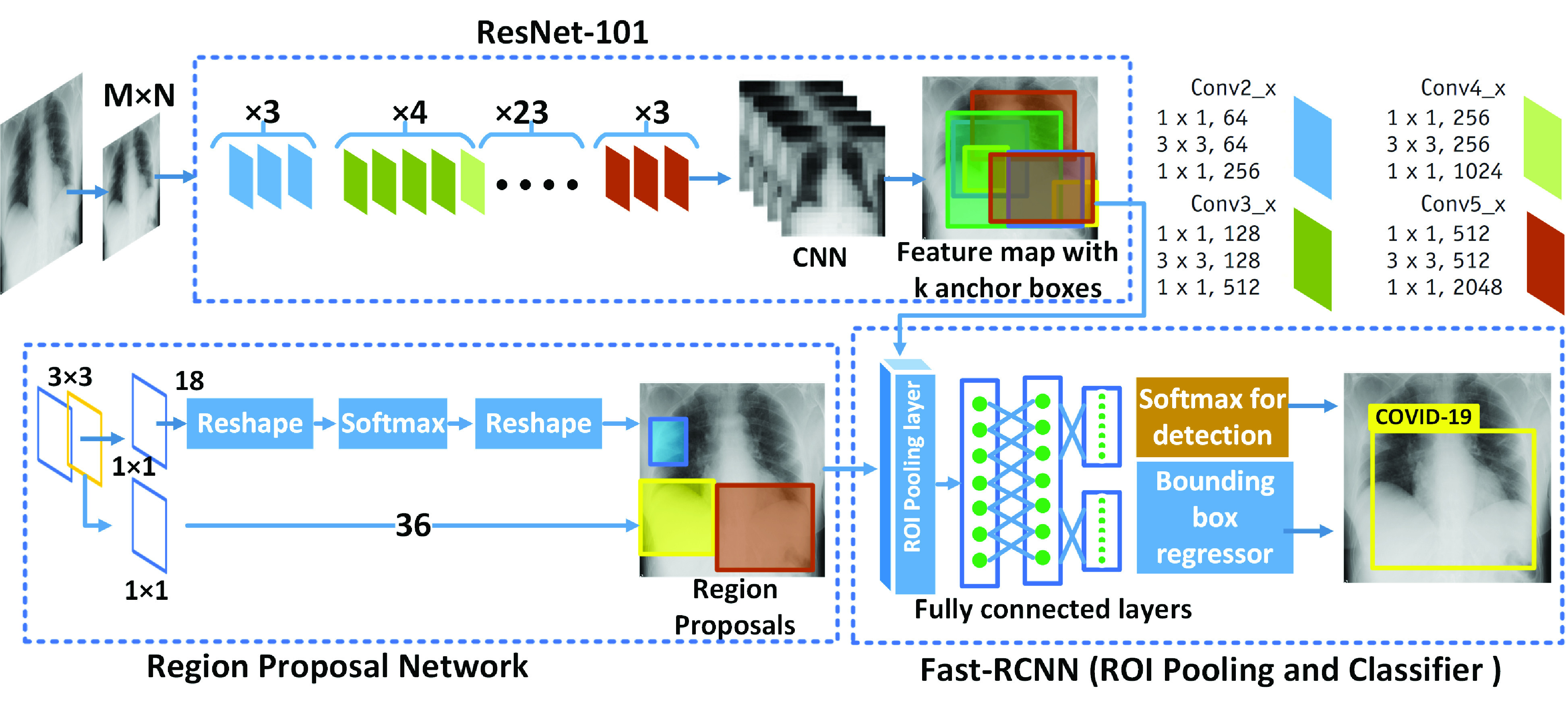
Using Faster-RCNN [12] with ResNet-101 [13] architecture as backbone for detection of Covid-19.
In the literature, [27] also utilizes Faster-RCNN for Covid-19 detection but using VGG as a base network with a limited data set. While in this work, for backbone architecture ResNet-101 [13] is used. ResNet utilizes skip connection (or shortcut connection), allows a deeper network to match the input from the previous layer to the subsequent layer without transforming the input. Traditional deep learning models like VGG-Net normally have Conv layers for classification tasks, instead of fully connected (FC) layers, without any skip/shortcut connection named as plain networks. In that case, when layers are increased or the plain network becomes deeper, vanishing/exploding gradients occur. To resolve the vanishing/exploding gradients, a skip/shortcut connection is added. (for details, readers are referred to [13]). The process shown in Fig. 5 is mainly based on three steps.
-
1)
First, ResNet-101 CNN architecture is used for feature extraction and generation of convolution feature maps.
-
2)
In the second step, using the sliding window strategy,
 anchor boxes are produced. These anchor boxes are further refined to define the exact region of interest, as shown in Fig. 5 using RPN, which is finally given to the Fast R-CNN for bounding box regression and classification.
anchor boxes are produced. These anchor boxes are further refined to define the exact region of interest, as shown in Fig. 5 using RPN, which is finally given to the Fast R-CNN for bounding box regression and classification. -
3)
In the final step, a small network is used to refined anchors, and the loss function is determined, selecting the best anchor regions.
In Fig. 5, it can be seen that X-Rays sample images of the chest are fed into the conventional layers that produce feature maps. For feature extraction, ResNet-101-based CNN architecture is used. For anchor selection, the anchors are subdivided into two classes (positive and negative). To determine where the anchor regions overlapped with ground-truth bounding boxes, the Intersection over the Union method (IoU) is used, and the overlap ratio is defined. The IoU overlap ratio is given as [12]
 |
After selecting anchor regions, the loss function is calculated at the end of the RPN. A network is utilized for detection of X-Ray samples as Non-Covid-19 or Covid-19. The regression function is employed to define the predicted bounding box positions. The loss function is defined to measure the regression and classification loss [12] as
 |
In (2),
 represents classification loss, and
represents classification loss, and
 shows regression loss. The normalization coefficients are represented with
shows regression loss. The normalization coefficients are represented with
 and
and
 , and the weight parameter between two losses is shown with
, and the weight parameter between two losses is shown with
 .
.
 is applied as an anchor index, and predicted probability Covid-19 is represented as
is applied as an anchor index, and predicted probability Covid-19 is represented as
 . The ground truth for Covid-19 classification is
. The ground truth for Covid-19 classification is
 , and if the value of
, and if the value of
 , then anchor relates to a positive class (Covid-19), and in the case of 0, the anchor belongs to a negative class (Non-Covid-19).
, then anchor relates to a positive class (Covid-19), and in the case of 0, the anchor belongs to a negative class (Non-Covid-19).
 shows a predicted bounding box vector, while
shows a predicted bounding box vector, while
 represents ground truth. The RPN’s chosen features are provided to the ROI pooling layer, which detects X-Ray image as Covid-19 or Non-Covid-19. For classification loss
represents ground truth. The RPN’s chosen features are provided to the ROI pooling layer, which detects X-Ray image as Covid-19 or Non-Covid-19. For classification loss
 of Covid-19 or Non-Covid-19, a logarithmic loss is defined of two categories and provided as
of Covid-19 or Non-Covid-19, a logarithmic loss is defined of two categories and provided as
 |
Using (4), the regression loss is given as [12]
 |
where
 is defined as [12]
is defined as [12]
 |
The model outputs the X-Ray image of the chest with bounding box information containing (detected Covid-19 region), as shown in Fig. 5. A Tensorflow library is used for building and training of the model. The data set is randomly split into 20% of the testing set and 80% of the training set. The detail of the testing and training set is already provided in Table II. The training set is utilized for learning, and the testing set is used for evaluation of the model.
V. Experimental Results
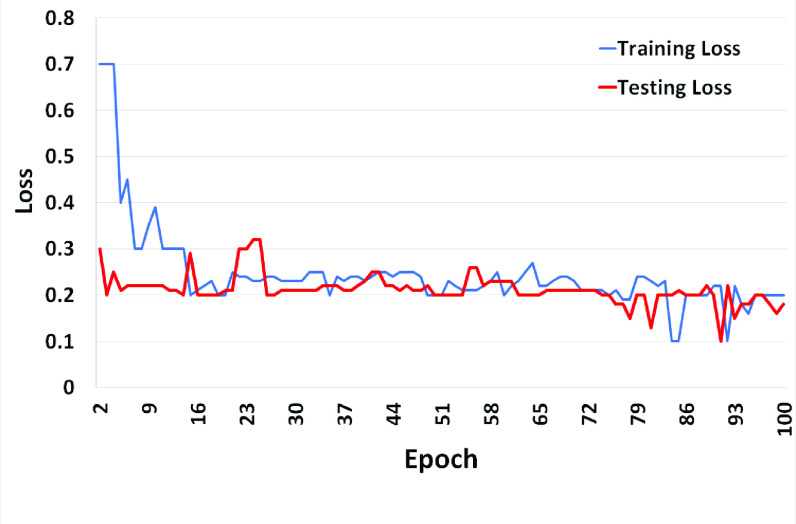
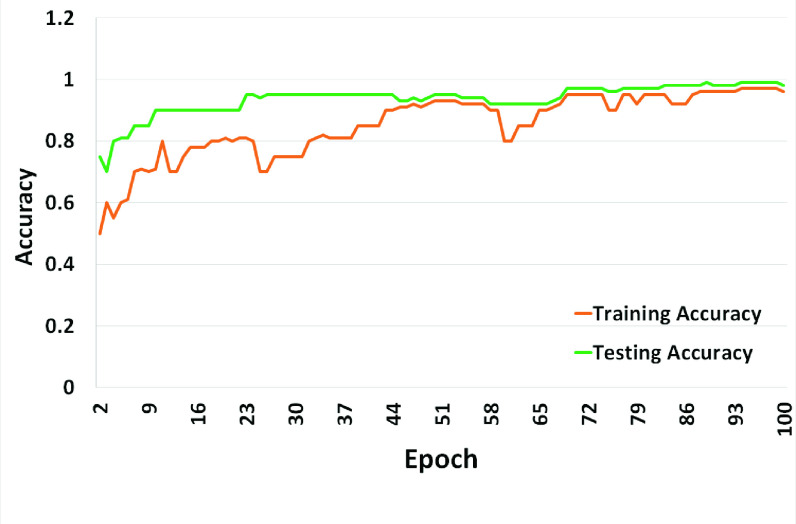
The evaluation and visualization results of the above-explained model are elaborated in this section. The testing experiments are performed by utilizing X-Ray sample images. First, the observation of the model after training using chest X-ray samples has been discussed. The training, testing loss, and accuracy are presented in Figs. 6 and 7. It can be observed that the training and testing loss are decreasing steadily after every ten epoch, as shown in Fig. 6. From Fig. 7, it is noteworthy that training and testing accuracy rates raised significantly at the initial epoch because we practiced only specific class data as Covid-19 data.
Fig. 6.
Training and testing loss of faster-RCNN with Reset-101.
Fig. 7.
Training and testing accuracy of faster-RCNN with Reset-101.
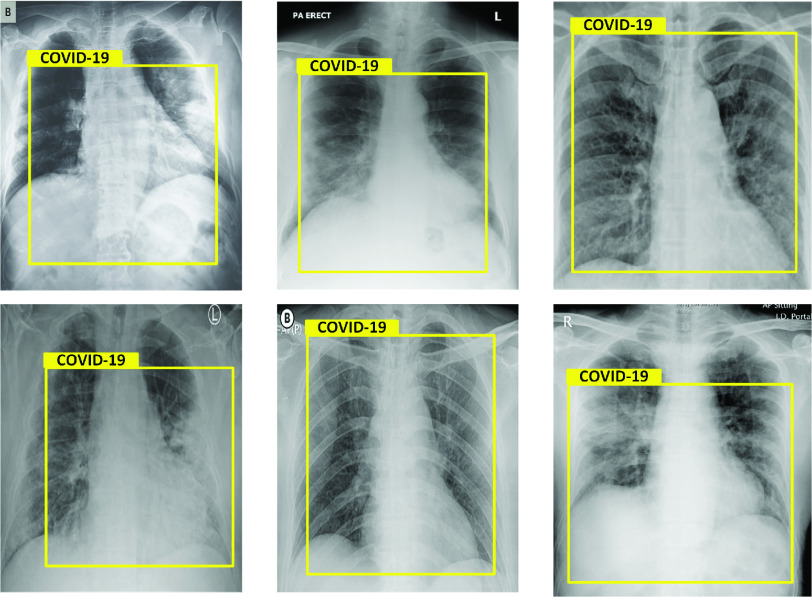
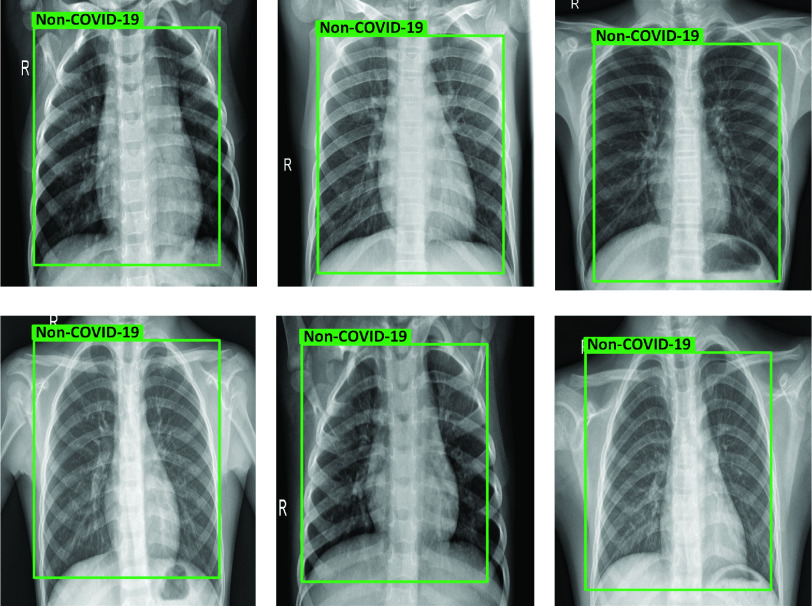
The visualization results of a deep learning model are presented in Figs. 8 and 9. The testing results of X-Ray samples of the chest detected as Covid-19 is shown in Fig. 8. In all images, the model accurately recognizes the infection (white spots that contain pus and water). It can be seen that in some cases, the spread of the virus is severed, for which expert opinion is needed. Therefore, these results can be are further referred to a medical expert for further analysis and examination. Similarly, in Fig. 9, the healthy or Non-Covid-19 detected results are depicted. The deep learning model effectively classified both cases.
Fig. 8.
Results of chest X-Rays, detected as Covid-19.
Fig. 9.
Results of Chest X-Rays, detected as Non-Covid-19.
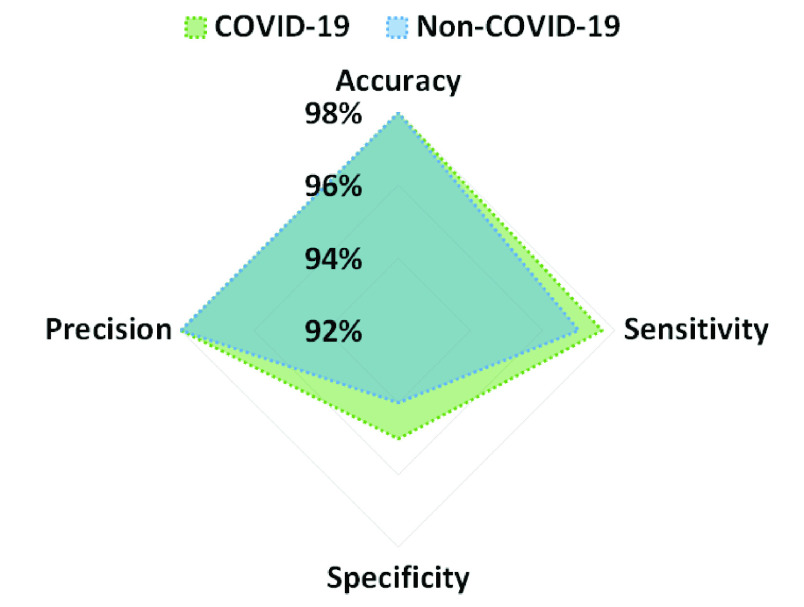
For evaluation purposes, different parameters have been utilized, including false-positive, true-positive, false-negative, and true-negative. To show the performance of the model, accuracy, precision, recall, true-positive rate (TPR), and false-positive rate (FPR) are estimated using these parameters. The precision, sensitivity, accuracy, and specificity results are visualized using Fig. 10. It can be seen that the accuracy of the model is 98% for both classes. The sensitivity is 98% and 97% while Specificity is 95 and 94% for Non-Covid-19 and Covid-19 images, respectively.
Fig. 10.
Accuracy, sensitivity, precision, and specificity.
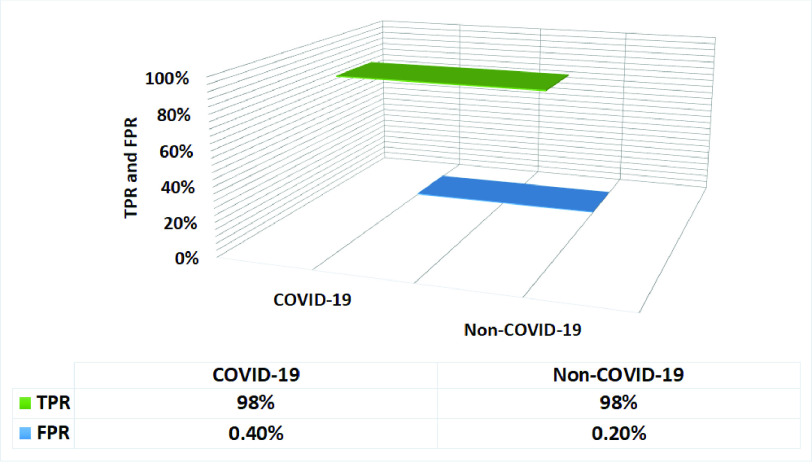
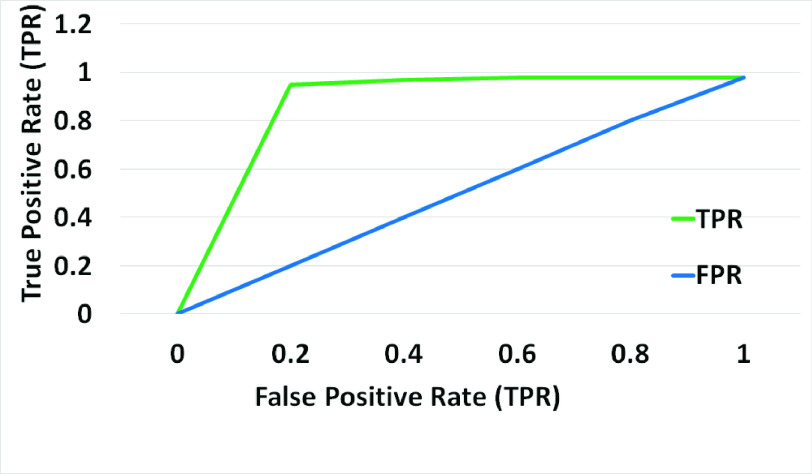
The TPR and FPR of the above-discussed model are depicted in Fig. 11; the model achieves TPR of 98%, while the FPR is 0.4%. The ROC curve is also plotted using TPR versus FPR, as shown in Fig. 12. It can be noted that the model produces good results.
Fig. 11.
True positive rate and false positive rate.
Fig. 12.
ROC curve of the model used for Covid-19 detection.
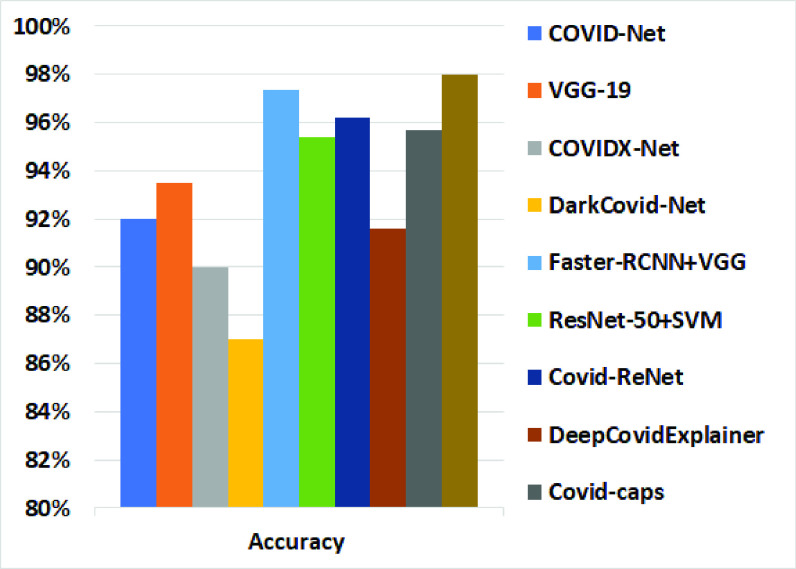
The accuracy results of the above-discussed model are also compared with different deep learning methods, as illustrated in Fig. 13. The comparison results are provided in Table III. For a fair comparison, the results presented in the table are the same as provided in the original work. Most of these methods are developed using limited data sets.
Fig. 13.
Comparison results with deep learning methods.
TABLE III. Comparison Results With Some Deep Learning-Based Methods.
| S.No | Ref | Method | Image Type | Training | Testing | Accuracy |
|---|---|---|---|---|---|---|
| 1 | [23] | COVID-Net | Chest X Ray | 258 | 100 | 92% |
| 2 | [25] | VGG-19 | Chest X Ray | 202 | 22 | 93.48% |
| 3 | [22] | COVIDX-Net | Chest X Ray | 20 | 5 | 90% |
| 4 | [34] | DarkCovid-Net | Chest X ray | 4500 | 1550 | 87.02% |
| 5 | [27] | Faster-RCNN+VGG | Chest X Ray | 17749 | 1500 | 97.36% |
| 6 | [35] | ResNet50 + SVM | Chest X Ray | NA | NA | 95.38% |
| 7 | [24] | Covid-ResNet | Chest X Ray | NA | NA | 96.23% |
| 8 | [36] | DeepCovidExplainer | Chest X Ray | 181 | 78 | 91.60% |
| 9 | [37] | Covid-caps | Chest X Ray | 70 | 50 | 95.70% |
| 10 | Ours | Faster-RCNN+ResNet-101 | Chest X ray | 7000 | 4000 | 98% |
VI. Conclusion and Future Directions
An IoT-based deep learning framework has been introduced for early assessment of Covid-19. The framework is capable of relieving medical experts/radiologists’ working pressure by diagnosing infection in X-Rays of the chest and controlling the pandemic spread. A deep learning-based model, i.e., Faster-RCNN with ResNet-101, is applied for Covid-19 detection using online available data sets. The model uses RPN in order to produce region proposals and perform detection. For training and testing, a data set is customized from different available online data sources. We utilized a total of 7000 Non-Covid-19 and 4000 Covid-19 X-Ray sample mages. The model achieves a 98% detection accuracy. From experimental results, we believe that the system may assist medial expert/radiologist to support early assessment toward Covid-19. The accuracy results are also compared with some different deep learning-based approaches. Regrettably, due to the current public health emergency, the collection of the extensive data set for the training of the deep learning model is delicate. Although we used almost all freely available online data sets in this research, even then, a significant increase in data set is needed compared to the number of cases reported throughout the globe. Nevertheless, a pure IoT-based model is capable of generating a vast amount of data set. In the future, the framework might be developed using vast X-Ray images that might be further tuned with different backbone architectures.
Funding Statement
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea Government under Grant 2018045330.
Contributor Information
Imran Ahmed, Email: imran.ahmed@imsciences.edu.pk.
Awais Ahmad, Email: aahmad.marwat@gmail.com.
Gwanggil Jeon, Email: ggjeon@gmail.com.
References
- [1].Chan J. F.-W.et al. , “A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster,” Lancet, vol. 395, no. 10223, pp. 514–523, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Peng X., Xu X., Li Y., Cheng L., Zhou X., and Ren B., “Transmission routes of 2019-nCoV and controls in dental practice,” Int. J. Oral Sci., vol. 12, no. 1, pp. 1–6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Tian S., Hu W., Niu L., Liu H., Xu H., and Xiao S.-Y., “Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer,” J. Thor. Oncol., vol. 15, no. 5, pp. 700–704, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].(2020). COVID-19 Situation Update Worldwide, as of 4 November 2020. [Online]. Available: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases
- [5].Vaishya R., Javaid M., Khan I. H., and Haleem A., “Artificial intelligence (AI) applications for COVID-19 pandemic,” Diabetes Metab. Synd. Clin. Res. Rev., vol. 14, no. 4, pp. 337–339, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Joyia G. J., Liaqat R. M., Farooq A., and Rehman S., “Internet of Medical Things (IoMT): Applications, benefits and future challenges in healthcare domain,” J. Commun., vol. 12, no. 4, pp. 240–247, 2017. [Google Scholar]
- [7].Shoeibi A.et al. , “Automated detection and forecasting of COVID-19 using deep learning techniques: A review,” 2020. [Online]. Available: http://www.arXiv:2007.10785 [Google Scholar]
- [8].Self H., Courtney D. M., McNaughton C. D., Wunderink R. G., and Kline J. A., “High discordance of chest X-ray and computed tomography for detection of pulmonary opacities in ed patients: Implications for diagnosing pneumonia,” Amer. J. Emerg. Med., vol. 31, no. 2, pp. 401–405, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Rubin G. D.et al. , “The role of chest imaging in patient management during the COVID-19 pandemic: A multinational consensus statement from the fleischner society,” Chest, vol. 158, pp. 106–116, Jul. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Orioli , Hermans M. P., Thissen J.-P., Maiter D., Vandeleene B., and Yombi J.-C., “COVID-19 in diabetic patients: Related risks and specifics of management,” Annales D’endocrinologie, vol. 81, pp. 101–109, Jun. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Joy S. K. S.et al. (Jul. 2020). A Comprehensive Survey of COVID-19 Detection Using Medical Images. [Online]. Available: https://engrxiv.org/9fdyp/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ren S., He K., Girshick R., and Sun J., “Faster R-CNN: Towards real-time object detection with region proposal networks,” IEEE Trans. Pattern Anal. Mach. Intell., vol. 39, no. 6, pp. 1137–1149, Jun. 2017. [Online]. Available: https://ieeexplore.ieee.org/document/7485869 [DOI] [PubMed] [Google Scholar]
- [13].He K., Zhang X., Ren S., and Sun J., “Deep residual learning for image recognition,” in Proc. IEEE Conf. Comput. Vis. Pattern Recognit., Las Vegas, NV, USA, 2016, pp. 770–778. [Google Scholar]
- [14].Singh R. P., Javaid M., Haleem A., Vaishya R., and Al S., “Internet of Medical Things (IoMT) for orthopaedic in COVID-19 pandemic: Roles, challenges, and applications,” J. Clin. Orthopaedics Trauma, vol. 11, no. 4, pp. 713–717, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Yang T., Gentile M., Shen C.-F., and Cheng C.-M., “Combining point-of-care diagnostics and Internet of Medical Things (IoMT) to combat the COVID-19 pandemic,” Diagnostics (Basel), vol. 10, no. 4, p. 224, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Vafea M. T.et al. , “Emerging technologies for use in the study, diagnosis, and treatment of patients with COVID-19,” Cell. Mol. Bioeng., vol. 13, no. 4, pp. 249–257, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Shi F.et al. , “Review of artificial intelligence techniques in imaging data acquisition, segmentation and diagnosis for COVID-19,” IEEE Rev. Biomed. Eng., early access, Apr. 16, 2020, doi: 10.1109/RBME.2020.2987975. [DOI] [PubMed]
- [18].Wynants L.et al. , “Prediction models for diagnosis and prognosis of COVID-19 infection: Systematic review and critical appraisal,” Brit. Med. J., vol. 369, p. m1328, Apr. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang S.et al. (2020). A Deep Learning Algorithm Using CT Images to Screen for Coronavirus Disease (COVID-19). [Online]. Available: https://www.medrxiv.org/content/10.1101/2020.02.14.20023028v5 [Google Scholar]
- [20].Hassanien A. E., Mahdy L. N., Ezzat K. A., Elmousalami H. H., and Ella H. A.. (2020). Automatic X-Ray COVID-19 Lung Image Classification System Based on Multi-Level Thresholding and Support Vector Machine. [Online]. Available: https://www.medrxiv.org/content/10.1101/2020.03.30.20047787v1 [Google Scholar]
- [21].Kadry S., Rajinikanth V., Rho S., Raja N. S. M., Rao V. S., and Thanaraj K. P., “Development of a machine-learning system to classify lung ct scan images into normal/COVID-19 class,” 2020. [Online]. Available: http://www.arXiv:2004.13122 [Google Scholar]
- [22].Hemdan E. E.-D., Shouman M. A., and Karar M. E., “COVIDX-net: A framework of deep learning classifiers to diagnose COVID-19 in X-ray images,” 2020. [Online]. Available: http://www.arXiv:2003.11055 [Google Scholar]
- [23].Wang L. and Wong A., “COVID-net: A tailored deep convolutional neural network design for detection of COVID-19 cases from chest X-ray images,” 2020. [Online]. Available: http://www.arXiv:2003.09871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Farooq M. and Hafeez A., “COVID-ResNet: A deep learning framework for screening of COVID19 from radiographs,” 2020. [Online]. Available: http://www.arXiv:2003.14395 [Google Scholar]
- [25].Apostolopoulos I. D. and Mpesiana T. A., “COVID-19: Automatic detection from x-ray images utilizing transfer learning with convolutional neural networks,” Phys. Eng. Sci. Med., vol. 43, pp. 635–640, Apr. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Pereira R. M., Bertolini D., Teixeira L. O., Silla C. N. Jr., and Costa Y. M., “COVID-19 identification in chest X-ray images on flat and hierarchical classification scenarios,” Comput. Methods Programs Biomed., vol. 194, Oct. 2020, Art. no. 105532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Shibly K. H., Dey S. K., Islam M. T.-U., and Rahman M. M., “COVID faster R-CNN: A novel framework to diagnose novel coronavirus disease (COVID-19) in X-ray images,” Informat. Med. Unlocked, vol. 20, 2020, Art. no. 100405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ismail A., Rahmat T., and Aliman S., “Chest X-ray image classification using faster R-CNN,” Malaysian J. Comput., vol. 4, no. 1, pp. 225–236, 2019. [Google Scholar]
- [29].Punn N. S. and Agarwal S., “Automated diagnosis of COVID-19 with limited posteroanterior chest X-ray images using fine-tuned deep neural networks,” 2020. [Online]. Available: http://www.arXiv:2004.11676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Singh K. K., Siddhartha M., and Singh A., “Diagnosis of coronavirus disease (COVID-19) from chest X-ray images using modified xceptionnet,” Romanian J. Inf. Sci. Technol., vol. 23, pp. S91–S105, Jan. 2020. [Google Scholar]
- [31].Rahimzadeh M. and Attar A., “A new modified deep convolutional neural network for detecting COVID-19 from X-ray images,” 2020. [Online]. Available: http://www.arXiv:2004.08052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Apostolopoulos I. D., Aznaouridis S. I., and Tzani M. A., “Extracting possibly representative COVID-19 biomarkers from X-ray images with deep learning approach and image data related to pulmonary diseases,” J. Med. Biolog. Engi., vol. 40, p. 1, Jun. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kassani S. H., Kassasni P. H., Wesolowski M. J., Schneider K. A., and Deters R., “Automatic detection of coronavirus disease (COVID-19) in X-ray and CT images: A machine learning-based approach,” 2020. [Online]. Available: http://www.arXiv:2004.10641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ozturk T., Talo M., Yildirim E. A., Baloglu U. B., Yildirim O., and Acharya U. R., “Automated detection of COVID-19 cases using deep neural networks with X-ray images,” Comput. Biol. Med., vol. 121, Jun. 2020, Art. no. 103792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Sethy P. K. and Behera S. K., Detection of Coronavirus Disease (COVID-19) Based on Deep Features, Preprints, Basel, Switzerland, 2020, p. 2020. [Google Scholar]
- [36].Karim M., Döhmen T., Rebholz-Schuhmann D., Decker S., Cochez M., and Beyan O., “DeepCOVIDExplainer: Explainable COVID-19 diagnosis based on chest X-ray images,” 2020. [Online]. Available: http://www.arXiv:2004.04582 [Google Scholar]
- [37].Afshar P., Heidarian S., Naderkhani F., Oikonomou A., Plataniotis K. N., and Mohammadi A., “COVID-CAPS: A capsule network-based framework for identification of COVID-19 cases from X-ray images,” 2020. [Online]. Available: http://www.arXiv:2004.02696 [DOI] [PMC free article] [PubMed] [Google Scholar]